Abstract
The aim of this study is to systematically retrieve, synthesize, and assess methodologies employed in the development of paclitaxel-induced peripheral neuropathic pain (PIPNP) animal models, with the objective of optimizing protocols for model construction and evaluation. A structured search strategy was implemented using the terms “Paclitaxel-induced peripheral neuropathic pain” OR “Chemotherapy-induced peripheral neuropathic pain” AND “animal models” OR “rats” OR “mice” OR “experimental animals” across the China National Knowledge Infrastructure, Wanfang, and VIP databases. Identical search criteria were applied to the PubMed and Web of Science platforms. The literature search covered publications from database inception through December 31, 2024. A total of 128 articles were reviewed, including 18 in Chinese and 110 in English. All studies employed rodent models, including 16 strains and including both sexes, with ages ranging from 5 weeks to 10 months. In rats, 28 distinct modeling protocols were identified: 4 involving continuous paclitaxel injections, 23 employing alternate-day injections, and 1 using a single administration. For mice, 21 methods were recorded, comprising 6 continuous, 13 alternate-day, and 2 single-injection protocols. Upon successful model induction, six behavioral pain alterations were consistently documented, evaluated using 16 different assessment techniques. Current PIPNP models predominantly utilize 6- to 8-week-old male Sprague-Dawley (SD) rats, with paclitaxel administered at 2 mg/kg on either days 0, 2, 4, and 6 or days 1, 3, 5, and 7. Based on data mining and comparative evaluation of modeling approaches, the use of 6- to 8-week-old male SD rats or 8- to 10-week-old male C57BL/6J mice with paclitaxel administered at 2 mg/kg on days 1, 3, 5, and 7 is recommended for establishing PIPNP models. The translational alignment between PIPNP models and clinical phenotypes remains insufficient and requires further refinement.
1 Introduction
Malignant tumors remain the leading cause of death worldwide, significantly impeding efforts to enhance global life expectancy [1]. Data from the International Agency for Research on Cancer indicate that approximately 20 million new cancer cases were diagnosed globally in 2022, accompanied by 9.7 million cancer-related deaths, both figures inclusive of non-melanoma skin cancers. By 2050, the global cancer burden is projected to escalate to 35 million new cases annually [2]. This trajectory firmly establishes malignant tumors as the dominant global health threat [3]. Paclitaxel, a broad-spectrum chemotherapeutic primarily extracted from medicinal plants such as the yew and Taxus chinensis [4], continues to serve as a standard first-line treatment for multiple malignancies, including breast, lung, and ovarian cancers [5]. Despite its efficacy, paclitaxel therapy is frequently compromised by severe side effects, particularly paclitaxel-induced peripheral neuropathic pain (PIPNP), which affects up to 87% of recipients [6]. Characterized by persistent sensory disturbances – numbness, tingling, and pain in the extremities – PIPNP may also impair motor function, often persisting for extended periods and leading to significant treatment interruptions and deterioration in patients’ quality of life [7]. The pathogenesis of PIPNP remains poorly understood, hindering the development of effective preventive and therapeutic strategies. Current interventions for chronic PIPNP are limited, with duloxetine being the sole pharmacological agent conditionally endorsed by the American Society of Clinical Oncology guidelines, primarily for cases associated with platinum compounds rather than taxanes [8]. Despite growing interest in mitigating PIPNP, its underlying mechanisms and preventive measures continue to present substantial research challenges. Progress in this area relies on the establishment of a robust and reproducible animal model; however, agreement is lacking regarding optimal species selection, modeling protocols, and assessment methodologies. This study presents a comprehensive analysis of preclinical models to inform the development of a standardized framework, emphasizing critical variables including animal species, induction methods, pain-related behaviors, evaluation strategies, and relevant biomarkers.
2 Materials and methods
2.1 Data sources and search strategy
A comprehensive search was performed across China National Knowledge Infrastructure, Wanfang, and VIP databases (from inception to December 31, 2024) using the following terms: (“Paclitaxel-induced peripheral neuropathic pain” OR “Chemotherapy-induced peripheral neuropathic pain”) AND (“animal models” OR “mice” OR “rats” OR “experimental animals”). The same strategy was applied to PubMed and Web of Science for the same period. Only documented queries were retained, with detailed search terms presented in Table 1.
List of main search formats
| Serial number | Search formats |
|---|---|
| 1 | Themes = “Paclitaxel-induced peripheral neuropathic pain” + “animal models” |
| 2 | Themes = “Paclitaxel-induced peripheral neuropathic pain” + “rats” |
| 3 | Themes = “Paclitaxel-induced peripheral neuropathic pain” + “mice” |
| 4 | Themes = “Paclitaxel-induced peripheral neuropathic pain” + “experimental animals” |
| 5 | Themes = “Chemotherapy-induced peripheral neuropathic pain” + “animal models” |
| 6 | Themes = “Chemotherapeutic alcohol-induced peripheral neuropathic pain” + “rats” |
| 7 | Themes = “Chemotherapy-induced peripheral neuropathic pain” + “mice” |
| 8 | Themes = “Chemotherapy-induced peripheral neuropathic pain” + “experimental animals” |
2.2 Literature screening and selection criteria
A total of 467 records were initially retrieved. Following the removal of duplicates from both Chinese and English databases, the remaining entries underwent further screening to enhance literature quality. Conference abstracts, monographs, reviews, and records with incomplete data were excluded. Ultimately, 128 studies involving animal experiments on PIPNP were selected based on predefined inclusion criteria.
2.3 Statistical analysis
The experimental animal specifications adhered to the guidelines outlined in Experimental Animals and Animal Experimental Techniques. Data concerning animal selection (species, gender, and age), modeling approach, paclitaxel administration method, pain behavior during model induction, detection protocols, solvent choice for paclitaxel, safety profile, application contexts, and relevant experimental indicators were systematically recorded in Microsoft Excel 2021 to construct the PIPNP animal model database. Subsequent data processing – including summarization, cleaning, and analysis – was conducted using the same software. Due to missing information in some cases, the sum of individual data points in the statistical results may not add up to the total, and the final statistical results shall prevail.
3 Results
3.1 Experimental animal attributes
The 128 included documents contained 16 rodent species and strains, comprising two rat species – Sprague-Dawley (SD) and Wistar rats – with SD rats used more frequently (68 instances, 51.91%), and 14 mouse strains, including C57BL, C57BL/6, C57BL/NRj, C57BL/c, ICR, CD1, Swiss albino, ddY, CF-1, NMRI, s1-KO CD-1, and σ1R-KO CD-1. C57BL/6, C57BL/6J, and CD1 mice appeared most frequently (8 instances, 6.11%). Three studies lacked specific strain identification, referring only to rats or mice, while another three employed dual mouse strains for modeling. In total, rodent species were cited 128 times, as presented in Table 2. Male animals were predominantly used (96 instances, 75.00%), although eight studies omitted gender specification. Gender-related data are detailed in Table 3. Most subjects were aged 8–12 weeks (23 instances, 17.97%), followed by those aged 6–8 weeks (17 instances, 13.28%), and 7–9 weeks (5 instances, 3.91%). Eighteen studies indicated the use of adult mice without further age clarification, while 53 provided no age information. Age-related data are summarized in Table 4.
PIPNP model – animal species and their usage frequency
| Species | Frequency (instances) | Frequency/total (%) | Refs. |
|---|---|---|---|
| SD rats | 68 | 51.91 | [9,10,11,12,13,14,15,16,17,18,19,20,21,22, 23,24,25,26,27,28,29,30,31,32,33,34, 35,36,37,38,39,40,41,42,43, 44,45,46,47,48,49,50,51,52,53,54,55,56,57,58, 59,60,61,62,63,64,65,66,67, 68,69,70,71,72,73,74,75,76] |
| Wistar rats | 13 | 9.92 | [77,78,79,80,81,82,83, 84,85,86,87,88,89] |
| C57BL mice | 2 | 1.53 | [90,91] |
| C57 BL/6 mice | 8 | 6.11 | [92,93,94, 95,96,97,98,99] |
| C57 BL/6J mice | 8 | 6.11 | [100,101, 102,103,104,105,106,107] |
| C57BL/6N mice | 2 | 1.53 | [108,109] |
| C57BL/NRj mice | 1 | 0.76 | [110] |
| C57BL/c mice | 6 | 4.58 | [111,112,113,114,115,116] |
| ICR mice | 6 | 4.58 | [26,117,118,119,120,121] |
| CD1 mice | 8 | 6.11 | [122,123,124,125,126,127,128,129] |
| Swiss albino | 1 | 0.76 | [130] |
| ddY mice | 1 | 0.76 | [131] |
| CF-1 mice | 1 | 0.76 | [132] |
| NMRI mice | 1 | 0.76 | [133] |
| s1-KO CD-1 mice | 1 | 0.76 | [88] |
| σ1R-KO CD-1 mice | 1 | 0.76 | [89] |
| Not mentioned | 3 | 2.29 | [134,135,136] |
| Total | 131 | 100 |
PIPNP model – animal gender and their usage frequency
| Gender | Frequency (instances) | Frequency/total (%) | Refs. |
|---|---|---|---|
| Both male and female | 12 | 9.38 | [20,30,36,85,97,104,107,109,110,121,127,128] |
| Female | 12 | 9.38 | [38,69,72,80,88,89,101,111,113,114,117,124] |
| Male | 96 | 75.00 | [9,10,11,12,13,14,15,16,17,18, 19,21,22,23,24,25,26,27,29,31,32,33,34,35,37,39,40,41, 42,43,44,45,46,47,48,49,50,51,52,53,54,55,56, 57,58,59,60,61,62,63,64,65,66,67,68, 69,70,71,73,74,75,76,77,78,79,81,82,84,86,87,91,92,93,95,96,98,100,102,103,105,106,108,112,115,117,118,119,120,122,123,126,129,130,131,132,134] |
| Not mentioned | 8 | 6.25 | [28,83,90,94,125,133,135,136] |
| Total | 128 | 100 |
PIPNP model – animal age and their usage frequency
| Age | Frequency (instances) | Frequency/total (%) | Refs. |
|---|---|---|---|
| 10 months | 1 | 0.78 | [130] |
| 3–4 months | 2 | 1.56 | [40,123] |
| 12–14 weeks | 2 | 1.56 | [100,103] |
| 10 weeks | 2 | 1.56 | [28,104] |
| 8–12 weeks | 23 | 17.97 | [59,61,65,67,71,78,85,90,91,93,97, 99,107,108,110,111,113,114,115,116,120,121,129] |
| 6–12 weeks | 1 | 0.78 | [109] |
| 7–9 weeks | 5 | 3.91 | [9,51,87,95,122] |
| 6–8 weeks | 17 | 13.28 | [17,23,25,33,44,58,73,81,86,92,94,96, 98,102,106,126,127] |
| 5–8 weeks | 1 | 0.78 | [43] |
| 5–6 weeks | 3 | 2.34 | [24,101,117] |
| Adult | 18 | 14.06 | [10,11,14,18,21,26,30,32,34, 35,39,45,53,57,76,82,84,132] |
| Not mentioned | 53 | 41.41 | [12,13,15,16,19,20,22,27,29,31, 36,37,38,41,42,46,47,48,49,50,52,54, 55,56,60,62,63,64,66,68,69,70,72,74,75,77,79,80,83,88, 89,105,112,118,119,124,125,128,131,133,134,135,136] |
| Total | 128 | 100 |
3.2 Paclitaxel solvent
Of the 128 documents reviewed, 18 distinct methods for paclitaxel solvent preparation were identified. The most commonly reported combinations included Cremophor EL/ethanol (1:1) with 0.9% saline (38 instances, 29.69%) and 0.9% saline alone (24 instances, 18.75%). In 23 documents, the solvent preparation method was either omitted or not specified. A comprehensive summary is presented in Table 5.
PIPNP model – paclitaxel solvent and their usage frequency
| Paclitaxel solvent | Frequency (instances) | Frequency/total (%) | Refs. |
|---|---|---|---|
| 0.9% saline solution | 24 | 18.75 | [11,14,19,26,41,47,49,52,55,56, 60,62,65,67,69, 71,75,112,120,124,126,127,131] |
| Cremophor EL/ethanol (1:1) | 13 | 10.16 | [9,13,18,34,35,42,73,84,87,89,121,129,132] |
| Cremophor EL/ethanol (1:1) + 0.9% saline solution | 38 | 29.69 | [15,27,29,31,32,36,37,40,43,44,46, 50,51,58,64, 70,72,85,88,92,93,99,100,103,104,105, 108,109,110,111,113,114,115,116,117,122,135,136] |
| Cremophor EL/ethanol (1:1) + PBS solution | 8 | 6.25 | [81,91,94,96,98,102,106,128] |
| Cremophor EL/ethanol (1:1) + PBS solution + DMSO | 1 | 0.78 | [107] |
| 5% DMSO + 40% PEG 300 + 5%Tween 80 + ddH2O | 1 | 0.78 | [123] |
| 40% DMSO | 2 | 1.56 | [21,118] |
| 10% DMSO | 1 | 0.78 | [39] |
| 10% DMSO + 20%PEG300 + 10%Tween 80 + 0.9% saline solution | 1 | 0.78 | [53] |
| 10% DMSO + 40%PEG300 + 5%Tween 80 + 0.9% saline solution | 1 | 0.78 | [17] |
| 4% DMSO + 4%Tween80 + 0.9% saline solution | 1 | 0.78 | [54] |
| 2%DMSO + 0.9% saline solution | 1 | 0.78 | [78] |
| DMSO/Tween80 (1:1) + 0.9%saline solution | 1 | 0.78 | [16] |
| Cremophor EL | 2 | 1.56 | [63,76] |
| DMSO (concentration not mentioned) + 0.9% saline solution | 6 | 4.69 | [10,23,24,48,83,95] |
| PBS solution | 1 | 0.78 | [22] |
| 99.9% HPLC-grade methanol + 0.9% saline solution | 1 | 0.78 | [82] |
| Cremophor EL + 10% saline solution | 1 | 0.78 | [125] |
| 5% DMSO | 1 | 0.78 | [119] |
| Not mentioned | 23 | 17.97 | [12,20,25,28,30,33,38,45,57,59,61,66, 74,77,79, 80,86,90,97,101,130,133,134] |
| Total | 128 | 100 |
3.3 Paclitaxel injection methods
Of the 128 studies reviewed, model induction was predominantly achieved via intraperitoneal injection, accounting for 127 instances (99.22%) in rats or mice. In contrast, intravenous administration was rarely applied, appearing in only a single instance (0.78%), as presented in Table 6.
PIPNP model – paclitaxel injection methods and their usage frequency
| Injection methods | Frequency (instances) | Frequency/total (%) | Refs. |
|---|---|---|---|
| Intraperitoneal injection | 127 | 99.22 | [9,10,11,12,13,14,15,16,17,18,19,20,21,22, 23,24,25,26,27,28,29,30,31,32,33,34, 35,36,37,38,39,40,41,42,43,44,45,46, 47,48,49,50,51,52,53,54,55,56,57,58,59,60,61, 62,63,64,65,66,67,68,69,70,71,73,74, 75,76,77,78,79,80,81,82,83,84,85,86,87,88,89, 90,91,92,93,94,95,96,97,98,99,100,101,102,103,104, 105,106,107,108,109,110,111,112,113,114,115,116,117,118,119,120,121,122,123,124,125,126,127,128, 129,130,131,132,133,134,135,136] |
| Intravenous injection | 1 | 0.78 | [72] |
| Total | 128 | 100 |
3.4 Modeling protocols
In patients with malignant tumors receiving paclitaxel chemotherapy, acute neuropathic symptoms typically emerge within 24–72 h following a single dose of 135 or 175 mg/m2 (equivalent to 3.6 and 4.7 mg/kg, respectively), in the absence of detectable changes in joint or musculoskeletal structures. These transient symptoms usually resolve within 1 week post-infusion. When paclitaxel is administered intravenously every 3 weeks over 3–24 h, with cumulative doses ranging from 1,400 to 1,500 mg/m2 (37.8–40.5 mg/kg), patients frequently exhibit chronic manifestations, including sensory deficits, paresthesia, or functional impairments impacting daily life. Consequently, current rat and mouse PIPNP models predominantly replicate chronic pain phenotypes, while validated models of the acute phase remain lacking [137,138]. Literature mining identified 28 rat model induction protocols, comprising 4 continuous dosing strategies, 23 alternating-day regimens, and 1 single-dose protocol. The most prevalent schedules involved 2 mg/kg injections on days 0, 2, 4, and 6 (17 instances, 20.48%) and on days 1, 3, 5, and 7 (24 instances, 28.92%), as summarized in Table 7. For mouse models, 21 distinct approaches were documented, including 6 continuous dosing regimens, 13 alternating-day protocols, and 2 single-dose methods. The most frequently reported included 2 mg/kg on days 1–5 (12 instances, 24.49%) and on days 0, 2, 4, and 6 (9 instances, 18.37%), with details outlined in Table 8. Among the 128 studies reviewed, 80 employed rat-based modeling strategies, 45 utilized mouse-based approaches (including 1 study applying both), and 3 incorporated both species for model development.
PIPNP rat model – modeling protocols and their usage frequency
| Modeling protocols | Specific protocols | Frequency (instances) | Frequency/total (%) | Refs. |
|---|---|---|---|---|
| Alternate-day injection protocols | 2 mg/kg, injected once every other day, for a total of four injections | 4 | 4.82 | [28,36,51,134] |
| 2 mg/kg, injected every 5 days, for a total of five injections | 1 | 1.20 | [84] | |
| 2 mg/kg, injected every 4 days for a total of four injections | 1 | 1.20 | [76] | |
| 3 mg/kg, injected once every other day, for a total of four injections | 1 | 1.20 | [70] | |
| 6 mg/kg, injected once a week for 4 weeks | 1 | 1.20 | [74] | |
| 16 mg/kg, injected once a week for 5 weeks | 1 | 1.20 | [75] | |
| 1 mg/kg, injected on days 1, 3, 5, and 7 | 3 | 3.61 | [21,39,63] | |
| 1 mg/kg, injected on days 0, 2, 4, and 6 | 2 | 2.41 | [41,83] | |
| 2.47 mg/kg, injected on days 1, 3, 5, and 7 | 3 | 3.61 | [60,65,71] | |
| 2 mg/kg, injected on days 0, 2, 4, and 6 | 17 | 20.48 | [11,15,16,17,19,20,22,23,30,42, 45,53,54,64,80,81,87] | |
| 2 mg/kg, injected on days 1, 3, 5, and 7 | 24 | 28.92 | [13,14,18,24,26,29,31,32,34, 35,43,45,48,50,58,59,61,62, 66,67,68,78,79,136] | |
| 2 mg/kg, injected on days 1, 3, 5, 7, and 9 | 1 | 1.20 | [10] | |
| 3, 6 mg/kg, injected on days 1, 2, 8, 9, 15, 16, 22, and 23 | 1 | 1.20 | [9] | |
| 4 mg/kg, injected on days 0, 2, 4, and 6 | 1 | 1.20 | [56] | |
| 4 mg/kg, injected on days 1, 3, 5, and 7 | 2 | 2.41 | [12,38] | |
| 4 mg/kg, injected on days 1, 4, 8, and 11 | 1 | 1.20 | [73] | |
| 4, 6 mg/kg, injected on days 1, 8, and 15 | 1 | 1.20 | [57] | |
| 5 mg/kg, injected on days 0, 2, 4, and 6 | 1 | 1.20 | [69] | |
| 5 mg/kg, injected on days 0, 7, 14, and 21 | 1 | 1.20 | [27] | |
| 8 mg/kg, injected on days 1, 4, and 7 | 5 | 6.02 | [40,47,49,52,55] | |
| 8 mg/kg, injected on days 0, 3, and 6 | 1 | 1.20 | [85] | |
| 8 mg/kg, injected on days1, 3, 5, 7, and 9 | 1 | 1.20 | [25] | |
| 9 mg/kg, injected on days 0, 2, 4, and 6 | 1 | 1.20 | [77] | |
| Continuous injection protocols | 2 mg/kg, injection on days 1–4 | 1 | 1.20 | [44] |
| 2 mg/kg, injection on days 1–5 | 4 | 4.82 | [33,86,88,89] | |
| 2 mg/kg, injection on days 0–6 | 1 | 1.20 | [82] | |
| 3–7 mg/kg, injection on days 1–5 | 1 | 1.20 | [72] | |
| Single administration protocols | 5, 10 mg/kg, injected once | 1 | 1.20 | [37] |
| Total | 83 | 100 |
PIPNP mouse model – modeling protocols and their usage frequency
| Modeling protocols | Specific protocol | Frequency (instances) | Frequency/total (%) | Refs. |
|---|---|---|---|---|
| Alternate-day injection protocols | 4 mg/kg, injected once every other day, for a total of four injections | 1 | 2.04 | [129] |
| 4 mg/kg, injected once every other day, for a total of six injections | 1 | 2.04 | [93] | |
| 4 mg/kg, injected once every other day, for a total of eight injections | 1 | 2.04 | [122] | |
| 1 mg/kg, injected on days 0, 2, 4, and 6 | 1 | 2.04 | [118] | |
| 1 mg/kg, injected on days 1, 3, 5, and 7 | 1 | 2.04 | [117] | |
| 2 mg/kg, injected on days 0, 2, 4, and 6 | 9 | 18.37 | [91,94,96,98,102,106,109,110,120] | |
| 2 mg/kg, injected on days 1, 3, 5, and 7 | 3 | 6.12 | [26,99,112] | |
| 2 mg/kg, injected on days 1, 3, 5, and 8 | 1 | 2.04 | [125] | |
| 2 mg/kg, injected on days 1, 4, 7, and 11 | 1 | 2.04 | [107] | |
| 4 mg/kg, injected on days 0, 2, 4, and 6 | 3 | 6.12 | [110,103,105] | |
| 4 mg/kg, injected on days 1, 3, 5, and 7 | 2 | 6.12 | [104,121] | |
| 8 mg/kg, injected on days 1, 3, 5, and 7 | 2 | 4.08 | [101,123] | |
| 20 mg/kg, injected on days 15, 17, 19, and 21 | 1 | 2.04 | [92] | |
| Continuous injection protocols | 1 mg/kg, injection on days 1–4 | 1 | 2.04 | [95] |
| 1, 3, 6 mg/kg, injection on days 1–7 | 1 | 2.04 | [90] | |
| 2 mg/kg, injection on days 1–5 | 12 | 24.49 | [88,89,111,113,114,115,116,124,130,131,132,133] | |
| 4 mg/kg, injection on days 1–4 | 1 | 2.04 | [128] | |
| 4 mg/kg, injection on days 1–5 | 2 | 4.08 | [119,135] | |
| 4 mg/kg, injection on days 1–8 | 1 | 2.04 | [108] | |
| Single administration protocols | 6 mg/kg, injected once | 2 | 4.08 | [97,109] |
| 8 mg/kg, injected once | 2 | 4.08 | [126,127] | |
| Total | 49 | 100 |
3.5 Modeling safety
Of the 128 reviewed publications, 33 explicitly reported an absence of fatalities in both rats and mice. A single study documented two deaths during PIPNP model induction using a regimen of 16 mg/kg administered weekly over 5 weeks; one rat died following the initial dose, and another after the fourth injection [75]. The remaining 94 publications did not mention mortality outcomes. The specific data are summarized in Table 9.
PIPNP model – modeling safety and their usage frequency
| Safety | Frequency (instances) | Frequency/total (%) | Refs. |
|---|---|---|---|
| Clearly document that no animal deaths occurred | 33 | 25.78 | [13,15,19,21,22,29,30,36,38,39,43,45,46, 51,53,58,61,62,64, 68,70,80, 87,91,96,98,100,103,110,112,117,120] |
| Clearly record the number of deaths | 1 | 0.78 | [75] |
| Deathless description | 94 | 73.44 | [9,10,11,12,14,16,17,18,20,23, 24,25,26,27,28,31,32,33,34, 35,37,40,41,42,44,47,48,49,50,42,54, 55,56,57, 59,60,63,65,66,67,69,71,72, 73,74,76,77,78,79,81,82,83,84,85,86, 88,89,90,92,93,94,95,97,101,102,104,105, 106,107,108,109,111,113,114,115,116,118,119, 121, 122,123,124,125,126,127,128,129,130,131,132,133,134,135,136] |
| Total | 128 | 100 |
3.6 Pain-related behaviors in established model
PIPNP in clinical populations typically presents as numbness, tingling, pain, and sensory disturbances in the extremities. Comparable behavioral phenotypes have been observed in rodent models, mirroring the sensory abnormalities reported in humans. Based on established interspecies dose-conversion formulas and pharmacokinetic differences, a single paclitaxel dose of 1.0–32.0 mg/kg and cumulative exposure of 8.0–82.0 mg/kg in humans correspond to 1.3–12.9 mg/kg in rats. Similarly, human regimens involving single doses of 4.0–18.0 mg/kg and cumulative doses of 4.0–38.0 mg/kg translate to 0.33–3.1 mg/kg in mice. Within these dosage ranges, both rats and mice consistently exhibit characteristic behavioral alterations following paclitaxel administration, initially including pallor of distal limbs, elevated toe-licking frequency, and increased paw-lifting episodes. As nociceptive alterations progress, hallmark signs such as mechanical allodynia and thermal hypersensitivity emerge [139,140]. In the development of rodent PIPNP models, mechanical allodynia (111 instances, 48.47%) and thermal hyperalgesia (63 instances, 27.51%) represented the most frequently reported and widely adopted behavioral endpoints for model validation. A total of 229 pain-related behavioral responses were documented, with individual studies often reporting multiple endpoints. Refer to Table 10 for detailed quantitative data.
PIPNP model – pain behaviors and their usage frequency
| Pain-related behaviors | Frequency (instances) | Frequency/total (%) | Refs. |
|---|---|---|---|
| +MA | 111 | 48.47 | [9,10,11,12,13,14,15,16,17,18,19,20,21,22,23, 24,25,26,27,28,29,30,31,34,35,36,37,38,39,40, 41,42,43,44,45,46,47,48,49,50,51,52,53,54,55, 56,57,58,59,61,62,63,64,65,66,67,68,69,70,71, 73,74,75,76,77,78,79,80,85,87,88,89, 90,91,93,100,103,114,116,117,118,119,120,122,123,124,126, 129,130,131,132,133,134,135,136] |
| +MH | 18 | 7.86 | [31,32,34,35,42,46,60,75,76,81,84, 86,92,101,121,123,127,128] |
| +CA | 27 | 11.79 | [12,31,38,41,56,77,78,82,83,86,88,89,91,92,94, 96,98,100,102,103,106,112, 118,124,130,133,135] |
| +CH | 5 | 2.18 | [9,44,73,120,122] |
| +TA | 5 | 2.18 | [33,75,83,111,115] |
| +TH | 63 | 27.51 | [11,12,18,20,21,23,24,26,29,30,31, 33,37,38,39,43,45,47,48,52,56,57,58, 60,62,65,68,71,75,77,78,82,90,92,93, 97,99,101,104,108,109,111,112,113,114,115, 118, 119,120,122,123,124,126,127,129,130,132,133,134,135] |
| Total | 229 | 100 |
Note: MA: Mechanical allodynia, MH: Mechanical hyperalgesia, CA: Cold allodynia, CH: Cold hyperalgesia, TA: Thermal allodynia, TH: Thermal hyperalgesia. Symbols: +, This behavior was assessed as pain-like following paclitaxel administration.
3.7 Assessment techniques for established model
Evaluation of model validity and drug efficacy relies on specific detection methods designed to quantify alterations in pain-related behaviors. Analysis of 128 publications identified 17 distinct validation techniques, cumulatively applied 238 times, as individual studies often incorporated multiple assessments. Among methods targeting mechanical allodynia and hyperalgesia, the Von Frey test emerged as the most prevalent, accounting for 103 instances (43.28%), followed by the Randall-Selitto paw pressure test with 12 instances (5.04%). Cold sensitivity was evaluated using four techniques, with the acetone test being the most frequently employed (26 instances, 26%). Assessment of thermal sensitivity involved five methodologies, with the plantar test – applying thermal stimuli to the hind paw – being the most widely adopted (41 instances, 16.82%). Comprehensive data are summarized in Table 11.
PIPNP model – assessment techniques and their usage frequency
| Pain-related behaviors | Assessment techniques | Frequency (instances) | Frequency/total (%) | Refs. |
|---|---|---|---|---|
| +MA, +MH | Von Frey test | 103 | 43.28 | [9–21,23–27,29–32,34–60,63–66,69–71,73,78,81,84,85,88,90,91, 93,101,103, 104,106,109,111,112,117–124,126–129,131–136] |
| Plantar dynamic test | 9 | 3.78 | [22,28,67,89,92,110,113,114,116] | |
| Mechanical claw pressure test | 3 | 1.26 | [61,87,105] | |
| Randall-Selitto foot pressure test | 12 | 5.04 | [34,35,42,46,62,68,75, 76,79,80,101,123] | |
| Pin prick test | 2 | 0.84 | [86,130] | |
| Tail pinch test | 1 | 0.42 | [130] | |
| Dynamic brush test | 1 | 0.42 | [31] | |
| +CA, +CH | Acetone test | 26 | 10.92 | [9,12,38,41,44,73,78,82,86,88,89,91,94, 96,98,100,102,103,106, 112,118,120,124,130,133,135] |
| Cold plate test | 4 | 1.68 | [56,111,122,125] | |
| Cold water bath and tail withdrawal method | 5 | 2.10 | [12,38,82,83,92] | |
| Cold water soaking test | 1 | 0.42 | [77] | |
| +TA, +TH | Hot plate test | 21 | 8.82 | [12,20,24,30,31,33,37,38,48,58, 78,90,101,111,115,127,132,133] |
| Thermal radiation rat rear foot method | 40 | 16.81 | [11,18,21,23,29, 31,39,43,45,47, 52,56,57,60,61,62,65,68,71,75,92,93, 97,99,101,104, 108,109,118,119,122, 124,126,129,130,134,135] | |
| Thermal radiation rat tail method | 4 | 1.68 | [72,77,82,130] | |
| Hot water bath and tail withdrawal method | 5 | 2.10 | [12,26,38,75,120] | |
| Hot-tail test | 1 | 0.42 | [83] | |
| Total | 238 | 100 |
3.8 Applications of the PIPNP model
Among the 128 reviewed studies, 96 (75%) established PIPNP models in rats or mice primarily for pharmacodynamic evaluation and mechanistic investigations. Of these, 27 studies (21.09%) concentrated on pharmacodynamic assessments, while 4 (3.13%) explored the underlying pathogenesis of PIPNP using animal models. A single study (0.78%) focused on characterizing behavioral phenotypes associated with the condition. Comprehensive data are provided in Table 12.
PIPNP model – applications and their usage frequency
| Applications | Frequency (instances) | Frequency/total (%) | Refs. |
|---|---|---|---|
| Pharmacodynamic evaluation + mechanistic investigations | 96 | 75.00 | [9,10,11,12,13,14,15,17,18,20,21,22,23,24,25, 26,28,29,30,31,32,34,35,36, 37,38,39,40,42,44,45,46,47,48,49,50, 52,53,54,55,56,58,59,60,61,62,63,64,65,66,67, 68,69,71,74,76,77,78,84,85,86,87,88,89,90,91, 92,95,97,98,99,100,101,102,104,106,108,109, 110,112,114,115,118,119,120,121,122,125,126,127,128,129,130,132,134,135] |
| Pharmacodynamic evaluation | 27 | 21.09 | [16,19,27,33,41,51,70,72,73,79,94, 96,103,105,107,111,113,116,117,123,124,131,133] |
| Underlying pathogenesis | 4 | 3.13 | [43,57,93,136] |
| Characterizing behavioral phenotypes | 1 | 0.78 | [75] |
| Total | 128 | 100 |
3.9 Experimental indicators
Current rat and mouse models of PIPNP were predominantly employed for pharmacodynamic evaluation, mechanistic exploration, and investigations into disease pathogenesis. Literature mining indicated that, depending on specific research aims, commonly examined tissues included the spinal cord, sciatic nerve, nerve root, and serum. Analytical methods such as Western blotting (WB), immunohistochemistry, and ELISA were frequently applied to quantify protein and mRNA expression levels associated with PIPNP. These molecular indicators supported both the interpretation of drug mechanisms and the investigation of PIPNP pathophysiology. For example, McCormick B’s study [51] demonstrated that MitoVitE attenuated paclitaxel-induced oxidative stress and mitochondrial dysfunction while reducing mechanical hyperalgesia in a rat model, implicating oxidative and mitochondrial disturbances in the condition’s etiology. The validity of the animal model was thereby reinforced by paclitaxel’s capacity to replicate these pathological features. To elucidate the methodological basis for model establishment, key experimental indicators and their usage frequencies are extracted from 128 studies and summarized in Table 13.
PIPNP model – experimental indicators and their usage frequency
| Experimental indicators | Specific indicator | Frequency (instances) | Frequency/total (%) | Refs. |
|---|---|---|---|---|
| Expression of related proteins | TPPV1 | 11 | 3.38 | [24,26,30,31,35,44,48,98,106,109,114] |
| TPPV4 | 2 | 0.62 | [44,48] | |
| Nrf2 | 3 | 0.92 | [54,101,120] | |
| HIF-1α | 4 | 1.23 | [16,29,80,105] | |
| HO-1 | 4 | 1.23 | [16,54,101,120] | |
| Iba1 | 17 | 5.23 | [25,48,49,52,54,57,60,64,71,77,110,114,125,127,135,136] | |
| CREB | 2 | 0.62 | [44,122] | |
| GFAP | 30 | 9.23 | [22,29,32,37,40,42,45,47,48,49,50,52,53,54,55,57, 60,65,71,76,77, 84,110,115,121,125,126,132,135,136] | |
| NLRP3 | 2 | 0.62 | [66,101] | |
| ERK1/2 | 4 | 1.23 | [46,88,92,99] | |
| P-ERK1/2 | 5 | 1.54 | [32,46,88,92,99] | |
| NF-κB | 4 | 1.23 | [57,71,92,127] | |
| NF-κB P65 | 5 | 1.54 | [22,40,46,78,90] | |
| P-NF-κB | 1 | 0.31 | [127] | |
| P-P38 | 3 | 0.92 | [32,46,101] | |
| MAPK | 2 | 0.62 | [46,101] | |
| IB4 | 4 | 1.23 | [44,47,50,127] | |
| P-AKT | 4 | 1.23 | [18,55,85,101] | |
| DNMT3a | 3 | 0.92 | [49,122,129] | |
| CGRP | 5 | 1.54 | [12,44,50,126,127] | |
| NeuN | 5 | 1.54 | [28,49,50,52,54] | |
| NGF | 1 | 0.31 | [62] | |
| NKCC1 | 1 | 0.31 | [64] | |
| GLT-1 | 4 | 1.23 | [10,29,32,42] | |
| TLR4 | 2 | 0.62 | [22,95] | |
| iNOS | 1 | 0.31 | [127] | |
| PI3K | 2 | 0.62 | [55,101] | |
| c-FOS | 4 | 1.23 | [28,108,110,127] | |
| c-Jun | 2 | 0.62 | [90,122] | |
| P-JNK | 2 | 0.62 | [32,90] | |
| PGC-1α | 1 | 0.31 | [17] | |
| RIP3 | 1 | 0.31 | [15] | |
| MAP2 | 2 | 0.62 | [28,45] | |
| CD68 | 4 | 1.23 | [37,77,85,120] | |
| CD11b | 3 | 0.92 | [84,114,132] | |
| OX-42 | 3 | 0.92 | [42,45,50] | |
| PGC-1α | 3 | 0.92 | [17,18,39] | |
| Expression of related mRNA | OX-42 | 3 | 0.92 | [42,45,50] |
| Nav1.7 | 2 | 0.62 | [44,50] | |
| K2p1.1 | 2 | 0.62 | [56,128] | |
| TNF-α | 29 | 8.92 | [12,15,21,22,23,37,40,42, 44,48,55,57,59,60,65,71,78,84,90, 92,95,97,99,104,120,123,134] | |
| IL-1β | 26 | 8.00 | [12,14,15,18,21,22,23,29,37,38, 40,46,48,55,57,59,60,61,66,78, 79,92,95,120,123,134] | |
| IL-6 | 15 | 4.62 | [12,21,37,40,44,48,57,60,61,84, 92,99,104,123,134] | |
| IL-4 | 4 | 1.23 | [42,47,61,120] | |
| IL-10 | 11 | 3.38 | [18,23,42,46,47,57,61,84,99,120,121] | |
| MDA | 6 | 1.85 | [18,38,39,66,79,130] | |
| SOD | 7 | 2.15 | [18,21,39,42,66,86,114] | |
| GSH | 4 | 1.23 | [38,79,86,130] | |
| ROS | 2 | 0.62 | [66,120] | |
| Acetylated histone H4 | 2 | 0.62 | [40,52] | |
| Acetylated histone H3 | 4 | 1.23 | [52,56,122,129] | |
| Mitochondrial membrane potential (MMP) | 1 | 0.31 | [49] | |
| TRPV1 | 3 | 0.92 | [44,98,114] | |
| Iba1 | 1 | 0.31 | [52] | |
| NEuN | 1 | 0.31 | [28] | |
| GFAP | 2 | 0.62 | [84,115] | |
| c-FOS | 2 | 0.62 | [28,44] | |
| TLR4 | 1 | 0.31 | [57] | |
| NF-κB p65 | 1 | 0.31 | [57] | |
| DNMT3a | 1 | 0.31 | [49] | |
| c-Jun | 1 | 0.31 | [44] | |
| Nav1.7 | 2 | 0.62 | [44,50] | |
| GLT-1 | 1 | 0.31 | [115] | |
| GLuA1 | 1 | 0.31 | [115] | |
| PGC-1α | 1 | 0.31 | [39] | |
| Nrf2 | 1 | 0.31 | [114] | |
| CCL2 | 1 | 0.31 | [84] | |
| CD11b | 1 | 0.31 | [84] | |
| KCNQ5 | 1 | 0.31 | [136] | |
| TNF-α | 6 | 1.85 | [12,21,38,84,123,134] | |
| IL-1β | 6 | 1.85 | [12,38,44,120,123,134] | |
| IL-6 | 6 | 1.85 | [12,38,44,84,123,134] | |
| IL-4 | 1 | 0.31 | [120] | |
| IL-10 | 3 | 0.92 | [47,84,120] | |
| Cytological examination | Transmission electron microscopy (TEM) was employed to examine mitochondrial morphology | 1 | 0.31 | [89] |
| Ultrastructural alterations in the sciatic nerve were visualized using TEM | 2 | 0.62 | [67,68] | |
| Toluidine blue staining was utilized to evaluate axonal degeneration | 1 | 0.31 | [74] | |
| Plasma biochemical indexes | NO (nitric oxide) | 2 | 0.62 | [38,39] |
| 5-HT | 1 | 0.31 | [63] | |
| Total | 325 | 100 |
4 Evaluation and application analysis of the PIPNP animal model
The pathogenesis of PIPNP remains poorly understood. Current evidence indicates a multifactorial origin involving chemotherapy-induced mitochondrial impairment, oxidative stress, dysregulation of ion channel activity, neuroimmune dysfunction, dorsal root ganglion sensory neuron injury, and microvascular alterations [141]. This limited mechanistic insight continues to constrain the development of effective preventive and therapeutic interventions. Establishing a reproducible and reliable PIPNP animal model necessitates rigorous parameter optimization, including selection of animal strain, sex, developmental stage, paclitaxel dosage, modeling protocol, and outcome measures.
4.1 Evaluation and application analysis of animal species
The bibliometric analysis reveals that the rodent models are exclusively employed in current PIPNP model establishment, primarily due to their cost-effectiveness in husbandry, rapid reproductive cycle, and accelerated growth characteristics. Among rat models, SD rats predominate (68 instances, 51.91%), demonstrating enhanced pharmacological sensitivity compared to Wistar rats, which may potentiate intervention efficacy [142,143,144]. In mouse models, C57BL/6J and CD1 strains are frequently utilized (8 instances, 6.11%). However, CD1 mice as closed-colony stocks exhibit genetic heterogeneity and substantial phenotypic variability, potentially compromising experimental reproducibility [145]. In contrast, C57BL/6J – the inaugural mouse strain with fully sequenced genome – possesses a homogeneous genetic background that minimizes experimental variability [146]. Moreover, their immune system shares notable homology with humans, rendering this strain particularly suitable for mechanistic investigations into disease pathogenesis and pharmacological actions [147]. These comparative advantages strongly support the preferential selection of SD rats or C57BL/6J mice for optimized PIPNP model development.
4.2 Evaluation and application analysis of animal age
The 128 studies included 11 developmental stages, with animal ages ranging from 5 weeks to 10 months in both rats and mice. The most commonly selected age intervals were 6–8 weeks (17 instances, 13.28%) and 8–12 weeks (23 instances, 17.97%). Evidence suggests that early-life stressors, including maternal separation, may predispose young rats to depressive phenotypes in adulthood [148]. Accordingly, experimental modeling should utilize sexually mature adult rodents, with established maturation thresholds at 8–10 weeks for SD rats and 6–8 weeks for C57BL/6J mice, to avoid developmental variability associated with juvenile specimens.
4.3 Evaluation and application analysis of animal gender
Analysis of the literature revealed that male rodents were predominantly used for model induction, accounting for 96 sessions (75%). Although human studies have demonstrated greater experimental pain sensitivity in females across various modalities [149], no significant differences in the incidence or severity of PIPNP have been identified between sexes in preclinical models [150], indicating comparable pain responses during PIPNP progression. Nonetheless, numerous studies have shown that estrogen influences multiple signaling pathways within the nervous system. It alleviates neuropathic pain by suppressing microglial and astrocytic activation and downregulating pro-inflammatory cytokines such as IL-1β and IL-6 [151]. Additionally, estrogen enhances inhibitory neurotransmission via upregulation of NMDA receptor 1 and provides neuroprotection by mitigating oxidative neuronal damage [152,153]. Through its regulatory effects on neuroinflammation, neuronal excitability, and oxidative stress, estrogen exerts a multifactorial role in neuropathic pain modulation. Given these neuroregulatory functions, estrogen may confound the evaluation of paclitaxel-induced neurotoxicity when female rodents are employed in PIPNP models. Although direct sex-based comparative data in PIPNP modeling are limited, the established influence of estrogen on the peripheral nervous system supports the continued use of male rodents to minimize hormonal interference and improve model consistency.
4.4 Evaluation and application analysis of paclitaxel solvent
Literature mining identified Cremophor EL/ethanol (1:1) combined with 0.9% saline as the most frequently utilized solvent system for paclitaxel (38 instances, 29.69%), followed by direct dilution with 0.9% saline (24 instances, 18.75%). The choice of solvent largely depends on the formulation of paclitaxel. Owing to its poor aqueous solubility, conventional paclitaxel injections often require solubilizing excipients such as polyoxyethylene castor oil and ethanol. In preclinical models, alternative agents like DMSO and Tween 80 are also employed, though their inherent toxicity necessitates stringent control over concentration and dosing. Albumin-bound paclitaxel, formulated with human albumin as a carrier and stabilizer, exhibits high aqueous solubility and typically requires only dilution with 0.9% saline prior to administration [154,155,156]. Solvent selection should therefore align with the physicochemical properties of the paclitaxel formulation applied in each study.
4.5 Evaluation and application analysis of modeling protocols
Comprehensive analysis of the literature identified three primary paclitaxel-based modeling approaches: continuous injection, alternate-day injection, and single administration. All were validated as effective through various behavioral assessments. Among these, the 2 mg/kg dosing regimen administered on days 1, 3, 5, and 7 is recommended for both rats and mice, as it demonstrates superior alignment with clinical PIPNP symptomatology. This protocol most accurately replicates the characteristic phenotypes observed in PIPNP patients, who commonly present with distal limb numbness, tingling, and exaggerated responses to normally non-noxious stimuli. In rodent models, these clinical manifestations are paralleled by measurable reductions in mechanical pain thresholds and increased nociceptive sensitivity – key behavioral endpoints used to quantify symptom severity [157]. Data mining results indicate that 111 of 128 studies reported altered mechanical pain thresholds, with 25 of these employing the 2 mg/kg, days 1, 3, 5, and 7 protocol – the highest incidence among all dosing regimens. Similarly, among 63 studies documenting thermal hyperalgesia, 15 utilized this same schedule, again representing the highest proportion. Comprehensive data are provided in Table 14. These findings highlight a strong correlation between this dosing strategy and the induction of pain behaviors most representative of the PIPNP clinical symptomatology. This may be related to the prolonged half-life of paclitaxel in the body, as alternate-day injections can lead to repeated accumulation of the drug in the nervous system, preventing complete metabolism and resulting in prolonged exposure of nerves to toxic environments, thereby enhancing neuropathological responses [158,159,160]. Accordingly, we support its preferential adoption in preclinical modeling. From a pathological perspective, although the mechanisms underlying PIPNP remain unresolved, clinical trials have reported that certain patients undergoing paclitaxel chemotherapy exhibit not only neuropathic pain but also elevated serum IL-6 and IL-10 levels [161,162,163,164]. Data mining of 128 studies revealed that IL-6 levels were assessed in 16 cases, with 3 employing the 2 mg/kg dosing protocol on days 1, 3, 5, and 7 – representing the highest frequency among all regimens. Similarly, among the 11 studies measuring IL-10, this protocol appeared in 3 instances, again constituting a higher proportion. Comprehensive data are provided in Table 15. These patterns suggest a closer alignment between the 2 mg/kg, days 1, 3, 5, and 7 regimen and the inflammatory biomarkers observed in clinical PIPNP. Additionally, this protocol reflects the clinical pharmacological profile more accurately than single or continuous injections. The standard paclitaxel monotherapy regimen involves 175 mg/m2 administered intravenously over 3 h every 3 weeks [165]. The alternate-day dosing schedule better mirrors this clinical cadence. Furthermore, the 2 mg/kg dosage corresponds to the human equivalent dose derived from established interspecies conversion formulas, ensuring both translational relevance and safety in preclinical settings. Overall, the 2 mg/kg injection administered on days 1, 3, 5, and 7 establishes an animal model that better replicates the clinical and pathological attributes of PIPNP, offering a more representative platform for mechanistic investigation and therapeutic development.
Modeling protocols for mechanical allodynia and thermal hyperalgesia: Frequency analysis
| Pain-related behavior | Modeling protocols | Frequency (instances) | Frequency/total (%) | Refs. |
|---|---|---|---|---|
| +MA | 2 mg/kg, injected once every other day, for a total of four injections | 4 | 3.60 | [28,36,51,134] |
| 2 mg/kg, injected every 4 days for a total of four injections | 1 | 0.90 | [76] | |
| 3 mg/kg, injected once every other day, for a total of four injections | 1 | 0.90 | [70] | |
| 4 mg/kg, injected once every other day, for a total of four injections | 1 | 0.90 | [129] | |
| 4 mg/kg, injected once every other day, for a total of six injections | 1 | 0.90 | [122] | |
| 4 mg/kg, injected once every other day, for a total of eight injections | 1 | 0.90 | [93] | |
| 6 mg/kg, injected once a week for 4 weeks | 1 | 0.90 | [74] | |
| 16 mg/kg, injected once a week for 5 weeks | 1 | 0.90 | [72] | |
| 1 mg/kg, injected on days 1, 3, 5, and 7 | 4 | 3.60 | [75] | |
| 1 mg/kg, injected on days 0, 2, 4, and 6 | 2 | 1.80 | [41,118] | |
| 2 mg/kg, injected on days 0, 2, 4, and 6 | 24 | 21.62 | [11,15,17,19,20,22,23,30,42,46, 53,54,64, 80,87,91,94,96,98,106,109,110,120] | |
| 2 mg/kg, injected on days 1, 3, 5, 7, and 9 | 1 | 0.90 | [10] | |
| 2 mg/kg, injected on days 1, 3, 5, and 7 | 25 | 22.52 | [13,14,18,24,26,29,31,34,35,43,45,48,50, 58,59,61,62,66,67,68,78,79,99,112,136] | |
| 2 mg/kg, injected on days 1, 4, 7, and 11 | 1 | 0.90 | [107] | |
| 2.47 mg/kg, injected on days 1, 3, 5, and 7 | 2 | 1.80 | [65,71] | |
| 3, 6 mg/kg, injected on days 1, 2, 8, 9, 15, 16, 22, and 23 | 1 | 0.90 | [9] | |
| 4 mg/kg, injected on days 1, 4, 8, and 11 | 1 | 0.90 | [73] | |
| 4 mg/kg, injected on days 0, 2, 4, and 6 | 4 | 3.60 | [56,100,103,105] | |
| 4 mg/kg, injected on days 1, 3, 5, and 7 | 3 | 2.70 | [12,38,104] | |
| 4, 6 mg/kg, injected on days 1, 8, and 15 | 1 | 0.90 | [57] | |
| 5 mg/kg, injected on days 0, 2, 4, and 6 | 1 | 0.90 | [69] | |
| 5 mg/kg, injected on days 0, 7, 14, and 21 | 1 | 0.90 | [27] | |
| 8 mg/kg, injected on days 1, 4, and 7 | 5 | 4.50 | [40,47,49,52,55] | |
| 8 mg/kg, injected on days 0, 3, and 6 | 1 | 0.90 | [85] | |
| 8 mg/kg, injected on days 1, 3, 5, and 7 | 1 | 0.90 | [125] | |
| 8 mg/kg, injected on days 1, 3, 5, 7, and 9 | 1 | 0.90 | [25] | |
| 9 mg/kg, injected on days 0, 2, 4, and 6 | 1 | 0.90 | [77] | |
| 1 mg/kg, injected on days 1–4 | 1 | 0.90 | [95] | |
| 1, 3, 6 mg/kg, injected on days 1–7 | 1 | 0.90 | [90] | |
| 2 mg/kg, injected on days 1–4 | 1 | 0.90 | [44] | |
| 2 mg/kg, injected on days 1–5 | 11 | 9.91 | [86,89,111,113,114, 116,124,130,131,132,133] | |
| 4 mg/kg, injected on days 1–5 | 1 | 0.90 | [119,135] | |
| 4 mg/kg, injected on days 1–8 | 2 | 1.80 | [108] | |
| 6 mg/kg, injected once | 1 | 0.90 | [109] | |
| 8 mg/kg, injected once | 1 | 0.90 | [126] | |
| 5, 10 mg/kg, injected once | 1 | 0.90 | [37] | |
| Total | 111 | 100 | ||
| +TH | 2 mg/kg, injected once every other day, for a total of four injections | 1 | 1.59 | [134] |
| 3 mg/kg, injected once every other day, for a total of four injections | 1 | 1.59 | [70] | |
| 4 mg/kg, injected once every other day, for a total of four injections | 1 | 1.59 | [129] | |
| 4 mg/kg, injected once every other day, for a total of six injections | 1 | 1.59 | [122] | |
| 4 mg/kg, injected once every other day, for a total of eight injections | 1 | 1.59 | [93] | |
| 16 mg/kg, injected once a week for 5 weeks | 1 | 1.59 | [75] | |
| 1 mg/kg, injected on days 0, 2, 4, and 6 | 1 | 1.59 | [118] | |
| 1 mg/kg, injected on days 1, 3, 5, and 7 | 2 | 3.17 | [21,39] | |
| 2.47 mg/kg, injected on days 1, 3, 5, and 7 | 3 | 4.76 | [60,65,71] | |
| 2 mg/kg, injected on days 0, 2, 4, and 6 | 6 | 9.52 | [11,20,23,30,109,120] | |
| 2 mg/kg, injected on days 1, 3, 5, and 7 | 15 | 23.81 | [18,24,26,29,31,43,45, 48,58,61,62,68, 78,99,112] | |
| 4 mg/kg, injected on days 0, 2, 4, and 6 | 1 | 1.59 | [56] | |
| 4 mg/kg, injected on days 1, 3, 5, and 7 | 3 | 4.76 | [12,38,104] | |
| 4, 6 mg/kg, injected on days 1, 8, and 15 | 1 | 1.59 | [57] | |
| 5 mg/kg, injected on days 0, 2, 4, and 6 | 1 | 1.59 | [69] | |
| 8 mg/kg, injected on days 1, 4, and 7 | 2 | 3.17 | [47,52] | |
| 8 mg/kg, injected on days 1, 3, 5, and 7 | 2 | 3.17 | [101,123] | |
| 9 mg/kg, injected on days 0, 2, 4, and 6 | 1 | 1.59 | [77] | |
| 20 mg/kg, injected on days 15, 17, 19, and 21 | 1 | 1.59 | [92] | |
| 1, 3, 6 mg/kg, injected on days 1–7 | 1 | 1.59 | [90] | |
| 2 mg/kg, injected on days 0–6 | 1 | 1.59 | [82] | |
| 2 mg/kg, injected on days 1–5 | 9 | 14.29 | [33,111,113,114,115,124,130,132,133] | |
| 4 mg/kg, injected on days 1–5 | 1 | 1.59 | [119,135] | |
| 4 mg/kg, injected on days 1–8 | 2 | 3.17 | [108] | |
| 5, 10 mg/kg, injected once | 1 | 1.59 | [37] | |
| 6 mg/kg, injected once | 1 | 1.59 | [107] | |
| 8 mg/kg, injected once | 2 | 3.17 | [126,127] | |
| Total | 63 | 100 |
Modeling protocols for IL-6 and IL-10 detection: Frequency analysis
| Experimental indicators | Modeling protocols | Frequency (instances) | Frequency/total (%) | Refs. |
|---|---|---|---|---|
| IL6 | 2 mg/kg, injected once every other day, for a total of four injections | 1 | 6.25 | [134] |
| 2 mg/kg, injected every 5 days, for a total of five injections | 1 | 6.25 | [84] | |
| 1 mg/kg, injected on days 1, 3, 5, and 7 | 1 | 6.25 | [21] | |
| 2.47 mg/kg, injected on days 1, 3, 5, and 7 | 1 | 6.25 | [60] | |
| 2 mg/kg, injected on days 1, 3, 5, and 7 | 3 | 18.75 | [48,61,99] | |
| 4 mg/kg, injected on days 1, 3, 5, and 7 | 3 | 18.75 | [12,38,104] | |
| 4, 6 mg/kg, injected on days 1, 8, and 15 | 1 | 6.25 | [57] | |
| 8 mg/kg, injected on days 1, 3, 5, and 7 | 1 | 6.25 | [123] | |
| 8 mg/kg, injected on days 1, 4, and 7 | 1 | 6.25 | [40] | |
| 20 mg/kg, injected on days 15, 17, 19, and 21 | 1 | 6.25 | [92] | |
| 2 mg/kg, injected on days 1–4 | 1 | 6.25 | [44] | |
| 5, 10 mg/kg, injected once | 1 | 6.25 | [37] | |
| Total | 16 | 100 | ||
| IL10 | 2 mg/kg, injected every 5 days, for a total of five injections | 1 | 9.09 | [84] |
| 2 mg/kg, injected on days 0, 2, 4, and 6 | 4 | 36.36 | [23,42,46,120] | |
| 2 mg/kg, injected on days 1, 3, 5, and 7 | 3 | 27.27 | [18,61,99] | |
| 2 mg/kg, injected on days 1, 3, 5, and 7 | 1 | 9.09 | [121] | |
| 4, 6 mg/kg, injected on days 1, 8, and 15 | 1 | 9.09 | [57] | |
| 8 mg/kg, injected on days 1, 4, and 7 | 1 | 9.09 | [47] | |
| Total | 11 | 100 |
4.6 Evaluation and application analysis of pain behavior and assessment techniques
Literature mining indicated that mechanical allodynia (111 instances, 48.47%) and thermal hyperalgesia (63 instances, 27.51%) were the most frequently evaluated behavioral endpoints for validating PIPNP animal models. Mechanical hypersensitivity is conventionally assessed by delivering incremental mechanical stimuli to determine the minimum force eliciting a withdrawal response. This approach provides a reliable method for pain quantification in non-verbal subjects, as it enables objective assessment and yields reproducible results. Furthermore, the presence of mechanical allodynia correlates with the severity and duration of neuropathic pain, serving as a predictor of patient prognosis and risk for chronic pain development [166,167]. The widespread adoption of the Von Frey filament test underscores its methodological robustness in detecting mechanical pain thresholds [168]. The Thermal Nociceptive Sensitivity Assay enables consistent evaluation of pain sensitivity in laboratory animals by applying controlled heat stimuli and determining the threshold temperature that elicits a nociceptive response. Similar to mechanical pain assessments, it is particularly appropriate for subjects incapable of self-reporting. In addition, thermal hyperalgesia demonstrates high sensitivity to alterations in pain perception thresholds, capable of detecting even subtle changes in nociceptive thresholds. This not only mirrors peripheral nociceptor sensitization but also provides insights into central nervous system pain modulation dynamics [169,170]. Among thermal-based methods, the hot plate test remains the benchmark for quantifying nociceptive sensitization in rodents, offering high reproducibility through standardized temperature settings and precise measurement of response latency. Compared to other methodologies such as tail flick, thermal radiation, or paw/incisor assays, the hot plate test inflicts minimal somatic trauma on animals while mitigating stress-related confounding variables. This ensures more reliable quantifications of pain sensitivity with enhanced experimental reproducibility and specificity [171,172,173]. Therefore, we propose the implementation of both hot plate and Von Frey testing to evaluate alterations in mechanical allodynia and thermal hyperalgesia during PIPNP animal model establishment, serving as critical criteria for validating model success.
4.7 Specific operation methods
4.7.1 Von Frey test
Animals were individually housed in chambers and permitted a 30 min acclimatization period. Commencing with a 2 g filament, a standardized series of Von Frey filaments (1, 1.4, 2, 4, 6, 8, 10, and 15 g) were applied perpendicularly to the plantar mid-region of the hind paw, exerting sufficient force to induce filament bending. A positive response was defined as either abrupt paw withdrawal or licking behavior upon filament stimulation. The minimum force (in grams) required to elicit a positive response was recorded as the paw withdrawal threshold. Given paclitaxel’s induction of bilateral allodynia, threshold values from both hind paws were averaged to yield a final measure [9,11].
4.7.2 Hot plate test
The subject was retrieved from its housing cage and positioned on the heated surface of the hot plate apparatus for a 10–15 min habituation period. During this phase, the plate remained at ambient temperature, and ambulatory activity was restricted to a cylindrical acrylic enclosure featuring a ventilated upper portion. Following environmental acclimatization, the hot plate was equilibrated to and sustained at 52.0°C ± 0.1°C. Thermal stimulation was initiated upon temperature stabilization, with response timing synchronized via a foot-operated switch integrated with the apparatus. Nociceptive behaviors, defined as hind paw elevation or directed licking, immediately terminated the trial, and corresponding latency measurements were documented. A safety cutoff of 30 s was enforced to mitigate thermal injury risk, in compliance with ethical guidelines for thermal nociception assays [12,20].
4.8 Analysis of experimental indicators
Paclitaxel has been shown to trigger neuroinflammation through the release of pro-inflammatory and chemotactic mediators, alongside the recruitment of non-resident macrophages into the spinal cord and dorsal root ganglia (DRG). This cascade promotes glial activation and accumulation, ultimately contributing to the development of neuropathic pain [174]. Literature mining highlights a higher frequency of reported expression for several proteins and mRNAs – namely, Iba1, GFAP, CD68, CD11b, CCL2, TNF-α, IL-1β, and IL-6 – compared to other molecular markers. Among them, TNF-α, IL-1β, and IL-6 are well-established pro-inflammatory cytokines implicated in neuropathic mechanisms [175]; CCL2, a chemokine with strong chemotactic activity, mediates a range of pro-inflammatory responses [176]; CD68 and CD11b are markers predominantly expressed by macrophages and mononuclear phagocytes; GFAP indicates astrocyte reactivity [177]; and Iba1 serves as a hallmark of microglial activation [178]. Inflammatory signaling pathways such as NF-κB, MAPK, and TLR4 are also frequently reported, suggesting a consistent mechanistic pattern across studies. Collectively, these observations support the association between successful PIPNP model establishment and paclitaxel-induced neuroimmune alterations. In parallel, accumulating evidence links chemotherapeutic agents to ion channel dysregulation in DRG neurons. Altered channel function leads to increased action potential amplitude and firing frequency, heightened neuronal excitability, and spontaneous ectopic discharges, all of which contribute to neuropathic pain pathogenesis [179]. Literature mining further identifies Nav1.7, a voltage-gated sodium channel primarily expressed in peripheral nociceptors, as a key modulator of nociceptive signal propagation [180]. These data converge on the conclusion that paclitaxel disrupts ion channel homeostasis, playing a significant role in model pathophysiology. Additionally, elevated reactive oxygen species (ROS) levels in DRG neurons have been implicated in the maintenance of hypersensitivity in paclitaxel-induced neuropathic pain states [181]. Furthermore, paclitaxel-induced mechanical hyperalgesia has been linked to spinal oxidative stress, which sustains central sensitization and contributes to nociceptive signaling. Excessive ROS production activates aberrant ion channel responses, leading to mitochondrial membrane depolarization, disruption of respiratory chain complexes, and release of pro-apoptotic proteins – cascading into mitochondrial dysfunction. This compromise in mitochondrial integrity disrupts intracellular signaling and interferes with physiological transmission pathways [182]. Literature mining identified MDA, SOD, ROS, GSH, and MMP as commonly employed biomarkers. Among them, MDA, SOD, ROS, and GSH serve as established indicators of oxidative stress, whereas MMP provides a quantitative measure of mitochondrial function. These data corroborate the mechanistic framework described above, indicating that the PIPNP model reflects paclitaxel-induced mitochondrial impairment and redox imbalance in DRG neurons. Moreover, chemotherapeutic agents have been reported to induce persistent NET accumulation, triggering microcirculatory impairment in peripheral tissues, including limbs, sciatic nerves, and DRGs, ultimately resulting in localized ischemia and hypoxia [141]. The frequent citation of HIF-1α across studies further supports its involvement in mediating cellular adaptation to hypoxic stress. Collectively, the literature-based analysis substantiates the role of paclitaxel-induced microvascular dysfunction as a core mechanism underlying PIPNP pathogenesis. Furthermore, research conducted by Li et al. identified TRPV1 as a key mediator in pain perception, with a prominent role in the progression of PIPNP [31]. Literature mining indicated consistent upregulation of TRPV1 at both the protein and mRNA levels, corroborating earlier mechanistic insights and linking paclitaxel administration to altered TRPV1 expression during model development. Beyond molecular profiling, TEM has been utilized to evaluate sensory neuron ultrastructure and detect cytological damage. This approach, highlighted in multiple studies, reinforces the association between paclitaxel exposure and structural neuronal injury, thereby supporting model validity. Collectively, the observed molecular and morphological alterations establish a mechanistic rationale for the effective construction of the PIPNP model.
In summary, analysis of data mining outcomes and comparative evaluation of modeling protocols supports the use of 6- to 8-week-old male SD rats or 8- to 10-week-old male C57BL/6J mice as the preferred model organisms. Induction of the PIPNP model is achieved through intraperitoneal administration of paclitaxel at 2 mg/kg on days 1, 3, 5, and 7, a regimen that elicits mitochondrial dysfunction, oxidative stress, ion channel imbalance, neuroimmune alterations, sensory neuron damage within the DRG, and microcirculatory impairment. Mechanical allodynia and thermal hyperalgesia can be quantitatively assessed using the Von Frey and hot plate tests, respectively, to validate model establishment. The detailed experimental protocol is presented in Figure 1.
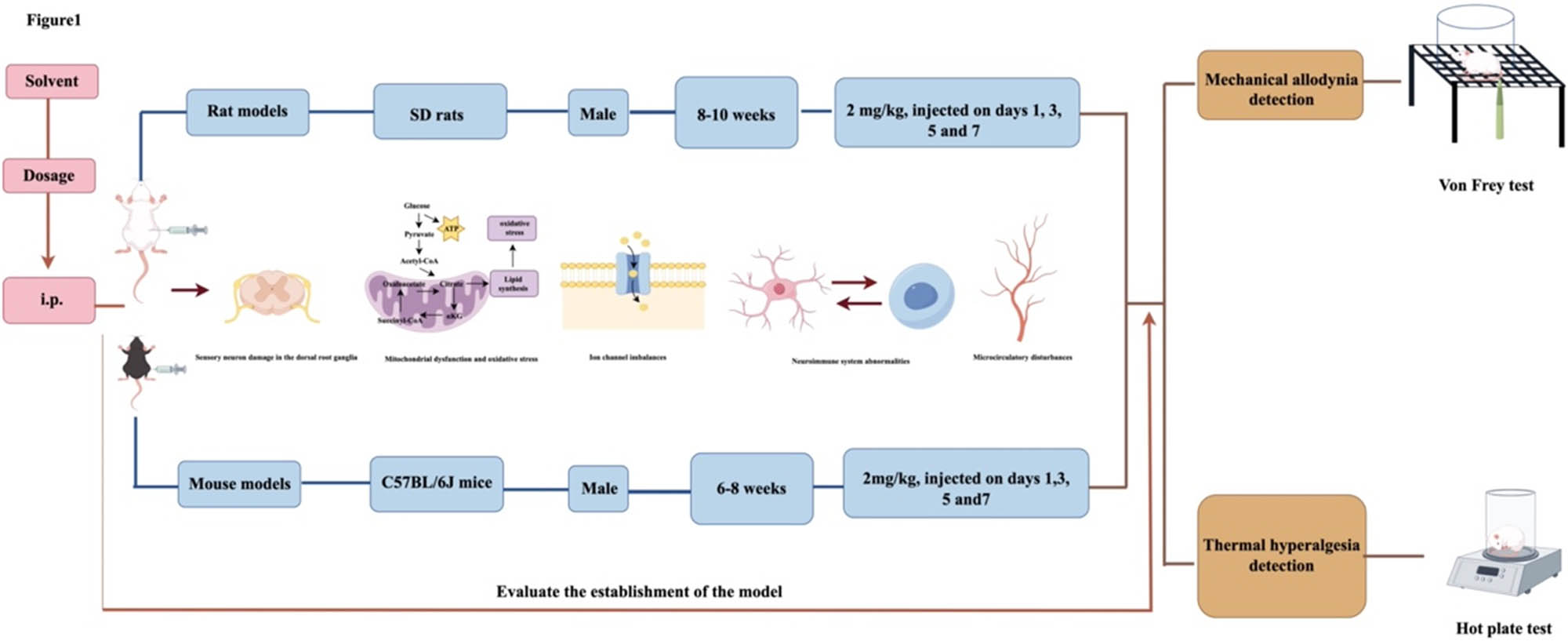
Flowchart for the development of a PIPNP animal model based on data mining outcomes and modeling evaluation analysis.
5 Discussion
The pathogenesis of PIPNP remains unclear, and selecting an appropriate animal model has become essential for advancing research in this area. An optimized PIPNP model not only supports the elucidation of underlying mechanisms but also serves as a foundational platform for drug screening and target validation, thereby enhancing the transition from preclinical pharmacodynamic studies to clinical applications. Moreover, effective models contribute to the refinement of therapeutic strategies and the development of preventive interventions. Rat and mouse PIPNP models provide distinct advantages, including methodological simplicity, reliable detection metrics, and broad applicability. These features have positioned rodent models as indispensable tools for investigating PIPNP-related neurobiological processes and evaluating emerging therapeutic approaches with translational potential.
In experimental research, aligning the selection of animal models with both the study objective and the specific attributes of each model is fundamental for ensuring data validity. A chronological review of the literature indicates that early PIPNP modeling efforts remained largely exploratory, primarily demonstrating mechanical hypersensitivity as the predominant phenotype. With the advancement of hypotheses regarding PIPNP pathogenesis, models have progressively incorporated additional pain modalities, including thermal and cold hypersensitivity, along with broader behavioral alterations. Contemporary model construction now involves multi-system, multi-dimensional evaluation strategies, accompanied by a gradual expansion in the scope of assessment parameters. Attention has increasingly shifted from purely behavioral endpoints toward integrative analyses including serological, cytological, and molecular dimensions. Technologies such as proteomics, cytomics, and genomics have become more widely implemented, reflecting a progression in research focus from organ-level observations to cellular and molecular interrogation. This methodological evolution has strengthened the robustness and translational relevance of criteria used to evaluate model fidelity.
In summary, current research on PIPNP animal models remains in a phase of refinement, with the primary challenge being the alignment between experimental models and clinical phenotypes. Enhancing this translational relevance requires addressing several limitations identified through literature mining. First, the implementation of a dynamic dose-adjustment strategy is warranted. Clinically, PIPNP represents a dose-dependent neurotoxic response, where symptom severity escalates with cumulative exposure [160]. However, most existing studies adopt fixed-dose regimens – typically involving alternate-day or continuous paclitaxel administration – without incorporating the adaptive dosing strategies common in clinical practice. While such approaches simulate general treatment patterns, they fail to capture the clinical course of PIPNP onset and progression. Future models should therefore integrate dose modulation, including reductions or temporary cessation upon the emergence of marked neurotoxicity. Monitoring the reversibility of symptoms following dose adjustment would further clarify the extent to which the model reflects the clinical dose-response relationship, thereby enhancing its predictive validity. Enhancing the alignment between PIPNP animal models and clinical phenotypes requires methodological refinement. Second, extending the observation window and optimizing the intervals for pain behavior assessments are essential. Recent evidence indicates that approximately 30% of paclitaxel-treated patients continue to experience PIPNP symptoms years after chemotherapy completion [44]. Correspondingly, preclinical studies have shown that pronounced nociceptive hypersensitivity in animals emerges around week 3 [92], with thermal hyperalgesia persisting beyond 8 weeks and mechanical allodynia extending up to 12 weeks [183]. Despite this, most current PIPNP models, both domestically and internationally, limit the modeling period to 21 days and the observation window to 56 days [89], resulting in behavioral assessments conducted almost exclusively within the first 3 weeks. Such temporal constraints may hinder accurate modeling of the chronic nature of clinical PIPNP. To improve translational relevance, future protocols should extend monitoring durations and refine the timing of behavioral evaluations accordingly. Third, a shift toward multimodal assessment strategies is warranted. Current model validation primarily relies on passively elicited responses, such as altered mechanical thresholds and evoked nociceptive hypersensitivity. However, clinical PIPNP is often characterized by spontaneous pain and sensory disturbances, including numbness – features not adequately captured by existing paradigms. This mismatch suggests that sole dependence on reflexive behavioral endpoints limits the model’s capacity to replicate the full clinical spectrum. Incorporating complementary assessment tools capable of detecting spontaneous pain behaviors may enhance model fidelity and provide a more comprehensive representation of clinical symptomatology. The nerve conduction velocity assay evaluates motor axonal function by stimulating the sciatic nerve and recording evoked muscle action potentials [184], while neuromuscular ultrasound enables real-time visualization of nerve swelling and muscle denervation [185]. These techniques provide dynamic, objective assessments of nociceptive alterations in PIPNP animal models, addressing the limitations inherent to behavioral testing. Future studies would benefit from a multimodal assessment framework that integrates behavioral, electrophysiological, and neuroimaging approaches to enhance model validity and better approximate the complexity of clinical pain. Fourth, the development of a PIPNP animal model aligned with both disease presentation and syndrome differentiation is essential. Literature mining on PIPNP mechanisms in traditional chinese medicine (TCM) indicates that existing models lack clear correspondence with clinical diagnostic patterns such as qi deficiency, blood deficiency, cold congealment, and blood stasis. Future investigations should prioritize constructing models that incorporate TCM pathophysiological classifications alongside established Western biomedical indicators. This integrative approach would strengthen the translational relevance of preclinical models by improving alignment with clinically observed phenotypes. While the present study primarily sourced literature from English databases, strategic incorporation of findings from Chinese repositories has established a methodological foundation for international utilization of PIPNP animal models. However, to facilitate global adoption of the optimized PIPNP model proposed herein, subsequent investigations should (1) conduct comparative analyses with established international models (e.g., spared nerve injury, chronic constriction injury) to validate superior alignment with human chronic pain pathophysiology and (2) develop alternative validation protocols for resource-constrained research settings, particularly through identification of molecular biomarkers potentially substituting traditional behavioral pain assessments.
Addressing the four aforementioned challenges demands continued methodological refinement to develop a robust animal model of PIPNP that more precisely recapitulates the pathophysiological complexity and clinical heterogeneity observed in human patients. A model with greater translational relevance would provide a robust framework for elucidating disease mechanisms and guiding the development of frontline therapeutic strategies aimed at effective prevention and symptom control, thereby enhancing patient quality of life.
Acknowledgments
The authors would like to express their gratitude to all members of Mingzhu Li and Haozhe Piao’s group for their support and help. This manuscript was supported by China National Natural Science Foundation (82104838), China Promotion Foundation Spark Program (XH-D001), and Liaoning Provincial Key Research and Development Program (2024JH2/102500062), which is gratefully acknowledged. Figure 1 was drawn using Figdraw.
-
Funding information: This work was supported by China National Natural Science Foundation (82104838), China Promotion Foundation Spark Program (XH-D001), and Liaoning Provincial Key Research and Development Program (2024JH2/102500062).
-
Author contributions: Jun Yu: conceptualization, writing – original draft, and writing – review and editing. Mingzhu Li and Haozhe Piao: conceptualization, writing – revision, project administration, and funding acquisition. Shengbo Jin: performed the literature search. All authors read and approved the final manuscript.
-
Conflict of interest: Authors state no conflict of interest.
-
Data availability statement: The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
[1] Santucci C, Carioli G, Bertuccio P, Malvezzi M, Pastorino U, Boffetta P, et al. Progress in cancer mortality, incidence, and survival: a global overview. Eur J Cancer Prev. 2020;29(5):367–81.10.1097/CEJ.0000000000000594Search in Google Scholar PubMed
[2] Bray F, Laversanne M, Sung H, Ferlay J, Siegel RL, Soerjomataram I, et al. Global cancer statistics 2022: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2024;74(3):229–63.10.3322/caac.21834Search in Google Scholar PubMed
[3] Zhang X, Yang L, Liu S, Cao LL, Wang N, Li HC, et al. Interpretation on the report of global cancer statistics 2022. Zhonghua Zhong Liu Za Zhi. 2024;46(7):710–21.Search in Google Scholar
[4] Martin V. Overview of paclitaxel (TAXOL). Semin Oncol Nurs. 1993;9(4):2–5.10.1016/S0749-2081(16)30035-3Search in Google Scholar
[5] Sharifi-Rad J, Quispe C, Patra JK, Singh YD, Panda MK, Das G, et al. Paclitaxel: application in modern oncology and nanomedicine-based cancer therapy. Oxid Med Cell Longev. 2021;2021(1):3687700.10.1155/2021/3687700Search in Google Scholar PubMed PubMed Central
[6] Burgess J, Ferdousi M, Gosal D, Boon C, Matsumoto K, Marshall A, et al. Chemotherapy-induced peripheral neuropathy: epidemiology, pathomechanisms and treatment. Oncol Ther. 2021;9(2):385–450.10.1007/s40487-021-00168-ySearch in Google Scholar PubMed PubMed Central
[7] Velasco-González R, Coffeen U. Neurophysiopathological aspects of paclitaxel-induced peripheral neuropathy. Neurotox Res. 2022;40(6):1673–89.10.1007/s12640-022-00582-8Search in Google Scholar PubMed
[8] Hershman DL, Lacchetti C, Dworkin RH, Lavoie Smith EM, Bleeker J, Cavaletti G, et al. Prevention and management of chemotherapy-induced peripheral neuropathy in survivors of adult cancers: American Society of Clinical Oncology clinical practice guideline. J Clin Oncol. 2014;32(18):1941–67.10.1200/JCO.2013.54.0914Search in Google Scholar PubMed
[9] Yamashita Y, Irie K, Kochi A, Kimura N, Hayashi T, Matsuo K, et al. Involvement of Charcot-Marie-Tooth disease gene mitofusin 2 expression in paclitaxel-induced mechanical allodynia in rats. Neurosci Lett. 2017;653:337–40.10.1016/j.neulet.2017.05.069Search in Google Scholar PubMed
[10] Bin XY, Wei YD, Huang J, Yang CY, Wei TT, Huang RR, et al. Changes in the expression of GLT-1 in the dorsal horn of the spinal cord in rats with paclitaxel-induced neuropathic pain. Youjiang Med J Natl. 2016;38(2):136–38+142.Search in Google Scholar
[11] Zhu HQ, Xu J, Shen KF, Pang RP, Wei XH, Liu XG. Bulleyaconitine A depresses neuropathic pain and potentiation at C-fiber synapses in spinal dorsal horn induced by paclitaxel in rats. Exp Neurol. 2015;273:263–72.10.1016/j.expneurol.2015.09.006Search in Google Scholar PubMed
[12] Ullah R, Ali G, Subhan F, Naveed M, Khan A, Khan J, et al. Attenuation of nociceptive and paclitaxel-induced neuropathic pain by targeting inflammatory, CGRP and substance P signaling using 3-Hydroxyflavone. Neurochem Int. 2021;144:104981.10.1016/j.neuint.2021.104981Search in Google Scholar PubMed
[13] Chen SR, Zhu L, Chen H, Wen L, Laumet G, Pan HL. Increased spinal cord Na+ -K+ -2Cl− cotransporter-1 (NKCC1) activity contributes to impairment of synaptic inhibition in paclitaxel-induced neuropathic pain. J Biol Chem. 2014;289(45):31111–20.10.1074/jbc.M114.600320Search in Google Scholar PubMed PubMed Central
[14] Jia M, Wu C, Gao F, Xiang H, Sun N, Peng P, et al. Activation of NLRP3 inflammasome in peripheral nerve contributes to paclitaxel-induced neuropathic pain. Mol Pain. 2017;13:1744806917719804.10.1177/1744806917719804Search in Google Scholar PubMed PubMed Central
[15] Ma D, Wang X, Liu X, Li Z, Liu J, Cao J, et al. Macrophage infiltration initiates RIP3/MLKL-dependent necroptosis in paclitaxel-induced neuropathic pain. Mediators Inflamm. 2022;2022:1–10.10.1155/2022/1567210Search in Google Scholar PubMed PubMed Central
[16] Zhou YQ, Liu DQ, Chen SP, Chen N, Sun J, Wang XM, et al. Nrf2 activation ameliorates mechanical allodynia in paclitaxel-induced neuropathic pain. Acta Pharmacol Sin. 2020;41(8):1041–8.10.1038/s41401-020-0394-6Search in Google Scholar PubMed PubMed Central
[17] Chen N, Ge MM, Li DY, Wang XM, Liu DQ, Ye DW, et al. β2-adrenoreceptor agonist ameliorates mechanical allodynia in paclitaxel-induced neuropathic pain via induction of mitochondrial biogenesis. Biomed Pharmacother. 2021;144:112331.10.1016/j.biopha.2021.112331Search in Google Scholar PubMed
[18] Li X, Yang S, Wang L, Liu P, Zhao S, Li H, et al. Resveratrol inhibits paclitaxel-induced neuropathic pain by the activation of PI3K/Akt and SIRT1/PGC1α pathway. J Pain Res. 2019;12:879–90.10.2147/JPR.S185873Search in Google Scholar PubMed PubMed Central
[19] Choi SS, Koh WU, Nam JS, Shin JW, Leem JG, Suh JH. Effect of ethyl pyruvate on Paclitaxel-induced neuropathic pain in rats. Korean J Pain. 2013;26(2):135–41.10.3344/kjp.2013.26.2.135Search in Google Scholar PubMed PubMed Central
[20] Yeh CM, Lai CY, Peng HY, Lin TB, Chou D, Wang HH, et al. Protein arginine methyltransferase 5 contributes to paclitaxel-induced neuropathic pain by activating transient receptor potential vanilloid 1 epigenetic modification in dorsal root ganglion. Anesth Analg. 2024;138(5):1107–19.10.1213/ANE.0000000000006595Search in Google Scholar PubMed
[21] Zhao X, Liu L, Wang Y, Wang G, Zhao Y, Zhang Y. Electroacupuncture enhances antioxidative signal pathway and attenuates neuropathic pain induced by chemotherapeutic paclitaxel. Physiol Res. 2019;68(3):501–10.10.33549/physiolres.934084Search in Google Scholar PubMed
[22] Zhao YX, Yao MJ, Liu Q, Xin JJ, Gao JH, Yu XC. Electroacupuncture treatment attenuates paclitaxel-induced neuropathic pain in rats via inhibiting spinal glia and the TLR4/NF-κB pathway. J Pain Res. 2020;13:239–50.10.2147/JPR.S241101Search in Google Scholar PubMed PubMed Central
[23] Wang J, Zhou F, Zhang S, Mao M, Feng S, Wang X. Participation of transient receptor potential vanilloid 1 in the analgesic effect of duloxetine for paclitaxel induced peripheral neuropathic pain. Neurosci Lett. 2022;773:136512.10.1016/j.neulet.2022.136512Search in Google Scholar PubMed
[24] Wu Y, Chen J, Wang R. Puerarin suppresses TRPV1, calcitonin gene-related peptide and substance P to prevent paclitaxel-induced peripheral neuropathic pain in rats. Neuroreport. 2019;30(4):288–94.10.1097/WNR.0000000000001199Search in Google Scholar PubMed
[25] Yokomi H, Kato T, Narasaki S, Kamiya S, Taguchi S, Horikawa YT, et al. The Serotonin-mediated anti-allodynic effect of Yokukansan on paclitaxel-induced neuropathic pain. Medicina (Mex). 2024;60(3):359.10.3390/medicina60030359Search in Google Scholar PubMed PubMed Central
[26] Gao W, Zan Y, Wang ZJ, Hu X, Huang F. Quercetin ameliorates paclitaxel-induced neuropathic pain by stabilizing mast cells, and subsequently blocking PKCε-dependent activation of TRPV1. Acta Pharmacol Sin. 2016;37(9):1166–77.10.1038/aps.2016.58Search in Google Scholar PubMed PubMed Central
[27] Xu F, Xu S, Wang L, Chen C, Zhou X, Lu Y, et al. Antinociceptive efficacy of verticinone in murine models of inflammatory pain and paclitaxel induced neuropathic pain. Biol Pharm Bull. 2011;34(9):1377–82.10.1248/bpb.34.1377Search in Google Scholar PubMed
[28] Yoon CS, Lee GW, Kim MH, Kang SM, Youn CK, Yang JH, et al. Analgesic effects and metabolome analyses of laser- and electro-acupuncture combined therapies in paclitaxel-induced neuropathic pain model. Front Vet Sci. 2023;10:1153903.10.3389/fvets.2023.1153903Search in Google Scholar PubMed PubMed Central
[29] Gao M, Yan X, Weng HR. Inhibition of glycogen synthase kinase 3β activity with lithium prevents and attenuates paclitaxel-induced neuropathic pain. Neuroscience. 2013;254:301–11.10.1016/j.neuroscience.2013.09.033Search in Google Scholar PubMed PubMed Central
[30] Hsieh MC, Lai CY, Cho WL, Lin LT, Yeh CM, Yang PS, et al. Phosphate NIMA-related kinase 2-dependent epigenetic pathways in dorsal root ganglion neurons mediates paclitaxel-induced neuropathic pain. Anesth Analg. 2023;137(6):1289–301.10.1213/ANE.0000000000006397Search in Google Scholar PubMed
[31] Li WW, Zhao Y, Liu HC, Liu J, Chan SO, Zhong YF, et al. Roles of thermosensitive transient receptor channels TRPV1 and TRPM8 in paclitaxel-induced peripheral neuropathic pain. Int J Mol Sci. 2024;25(11):5813.10.3390/ijms25115813Search in Google Scholar PubMed PubMed Central
[32] Xu Y, Cheng G, Zhu Y, Zhang X, Pu S, Wu J, et al. Anti-nociceptive roles of the glia-specific metabolic inhibitor fluorocitrate in paclitaxel-evoked neuropathic pain. Acta Biochim Biophys Sin. 2016;48(10):902–8.10.1093/abbs/gmw083Search in Google Scholar PubMed
[33] Amoateng P, Adjei S, Osei-Safo D, Kukuia KKE, Kretchy IA, Sarkodie JA, et al. Analgesic effects of a hydro-ethanolic whole plant extract of Synedrella nodiflora (L.) Gaertn in paclitaxel-induced neuropathic pain in rats. BMC Res Notes. 2017;10(1):226.10.1186/s13104-017-2551-7Search in Google Scholar PubMed PubMed Central
[34] Xie JD, Chen SR, Chen H. Presynaptic N-methyl-d-aspartate (NMDA) receptor activity is increased through protein kinase C in paclitaxel-induced neuropathic pain. J Biol Chem. 2016;291(37):19364–73.10.1074/jbc.M116.732347Search in Google Scholar PubMed PubMed Central
[35] Hsieh MC, Lai CY, Lin LT, Chou D, Yeh CM, Cheng JK, et al. Melatonin relieves paclitaxel-induced neuropathic pain by regulating pNEK2-dependent epigenetic pathways in DRG neurons. ACS Chem Neurosci. 2023;14(23):4227–39.10.1021/acschemneuro.3c00616Search in Google Scholar PubMed
[36] Galley HF, McCormick B, Wilson KL, Lowes DA, Colvin L, Torsney C. Melatonin limits paclitaxel-induced mitochondrial dysfunction in vitro and protects against paclitaxel-induced neuropathic pain in the rat. J Pineal Res. 2017;63(4):e12444.10.1111/jpi.12444Search in Google Scholar PubMed PubMed Central
[37] Wang J, Jiang C, Ba X, Yang S, Wu J, Huang Z, et al. Selective activation of metabotropic glutamate receptor 7 blocks paclitaxel-induced acute neuropathic pain and suppresses spinal glial reactivity in rats. Psychopharmacol (Berl). 2021;238(1):107–19.10.1007/s00213-020-05662-1Search in Google Scholar PubMed
[38] Naveed M, Ullah R, Khan A, Shal B, Khan AU, Khan SZ, et al. Anti-neuropathic pain activity of a cationic palladium (II) dithiocarbamate by suppressing the inflammatory mediators in paclitaxel-induced neuropathic pain model. Mol Biol Rep. 2021;48(12):7647–56.10.1007/s11033-021-06754-7Search in Google Scholar PubMed
[39] Wu P, Chen Y. Evodiamine ameliorates paclitaxel-induced neuropathic pain by inhibiting inflammation and maintaining mitochondrial anti-oxidant functions. Hum Cell. 2019;32(3):251–9.10.1007/s13577-019-00238-4Search in Google Scholar PubMed
[40] Gui Y, Zhang J, Chen L, Duan S, Tang J, Xu W, et al. Icariin, a flavonoid with anti-cancer effects, alleviated paclitaxel-induced neuropathic pain in a SIRT1-dependent manner. Mol Pain. 2018;14:1744806918768970.10.1177/1744806918768970Search in Google Scholar PubMed PubMed Central
[41] Zhang Y, Brewer AL, Nelson JT, Smith PT, Shirachi DY, Quock RM. Hyperbaric oxygen produces a nitric oxide synthase-regulated anti-allodynic effect in rats with paclitaxel-induced neuropathic pain. Brain Res. 2019;1711:41–7.10.1016/j.brainres.2019.01.009Search in Google Scholar PubMed
[42] Doyle T, Chen Z, Muscoli C, Bryant L, Esposito E, Cuzzocrea S, et al. Targeting the overproduction of peroxynitrite for the prevention and reversal of paclitaxel-induced neuropathic pain. J Neurosci. 2012;32(18):6149–60.10.1523/JNEUROSCI.6343-11.2012Search in Google Scholar PubMed PubMed Central
[43] Li Y, Yin C, Liu B, Nie H, Wang J, Zeng D, et al. Transcriptome profiling of long noncoding RNAs and mRNAs in spinal cord of a rat model of paclitaxel-induced peripheral neuropathy identifies potential mechanisms mediating neuroinflammation and pain. J Neuroinflamm. 2021;18(1):48.10.1186/s12974-021-02098-ySearch in Google Scholar PubMed PubMed Central
[44] Zhong S, Liu F, Giniatullin R, Jolkkonen J, Li Y, Zhou Z, et al. Blockade of CCR5 suppresses paclitaxel-induced peripheral neuropathic pain caused by increased deoxycholic acid. Cell Rep. 2023;42(11):113386.10.1016/j.celrep.2023.113386Search in Google Scholar PubMed
[45] Yadav R, Yan X, Maixner DW, Gao M, Weng H. Blocking the GABA transporter GAT-1 ameliorates spinal GABAergic disinhibition and neuropathic pain induced by paclitaxel. J Neurochem. 2015;133(6):857–69.10.1111/jnc.13103Search in Google Scholar PubMed PubMed Central
[46] Janes K, Esposito E, Doyle T, Cuzzocrea S, Tosh DK, Jacobson KA, et al. A3 adenosine receptor agonist prevents the development of paclitaxel-induced neuropathic pain by modulating spinal glial-restricted redox-dependent signaling pathways. Pain. 2014;155(12):2560–7.10.1016/j.pain.2014.09.016Search in Google Scholar PubMed PubMed Central
[47] Nie B, Liu C, Bai X, Chen X, Wu S, Zhang S, et al. AKAP150 involved in paclitaxel-induced neuropathic pain via inhibiting CN/NFAT2 pathway and downregulating IL-4. Brain Behav Immun. 2018;68:158–68.10.1016/j.bbi.2017.10.015Search in Google Scholar PubMed
[48] Ba X, Wang J, Zhou S, Luo X, Peng Y, Yang S, et al. Cinobufacini protects against paclitaxel-induced peripheral neuropathic pain and suppresses TRPV1 up-regulation and spinal astrocyte activation in rats. Biomed Pharmacother. 2018;108:76–84.10.1016/j.biopha.2018.09.018Search in Google Scholar PubMed
[49] Wang H, Shen YJ, Li XJ, Xia J, Sun L, Xu Y, et al. DNMT3b SUMOylation mediated MMP-2 upregulation contribute to paclitaxel induced neuropathic pain. Neurochem Res. 2021;46(5):1214–23.10.1007/s11064-021-03260-xSearch in Google Scholar PubMed
[50] Li Y, North RY, Rhines LD, Tatsui CE, Rao G, Edwards DD, et al. DRG voltage-gated sodium channel 1.7 is upregulated in paclitaxel-induced neuropathy in rats and in humans with neuropathic pain. J Neurosci. 2018;38(5):1124–36.10.1523/JNEUROSCI.0899-17.2017Search in Google Scholar PubMed PubMed Central
[51] McCormick B, Lowes DA, Colvin L, Torsney C, Galley HF. MitoVitE, a mitochondria-targeted antioxidant, limits paclitaxel-induced oxidative stress and mitochondrial damage in vitro, and paclitaxel-induced mechanical hypersensitivity in a rat pain model. Br J Anaesth. 2016;117(5):659–66.10.1093/bja/aew309Search in Google Scholar PubMed
[52] Liu M, Zhang SB, Luo YX, Yang YL, Zhang XZ, Li B, et al. NFATc2-dependent epigenetic upregulation of CXCL14 is involved in the development of neuropathic pain induced by paclitaxel. J Neuroinflammation. 2020;17(1):310.10.1186/s12974-020-01992-1Search in Google Scholar PubMed PubMed Central
[53] Li DY, Gao SJ, Sun J, Zhang LQ, Wu JY, Song FH, et al. Notch signaling activation contributes to paclitaxel-induced neuropathic pain via activation of A1 astrocytes. Eur J Pharmacol. 2022;928:175130.10.1016/j.ejphar.2022.175130Search in Google Scholar PubMed
[54] Zhou YQ, Liu DQ, Chen SP, Chen N, Sun J, Wang XM, et al. PPARγ activation mitigates mechanical allodynia in paclitaxel-induced neuropathic pain via induction of Nrf2/HO-1 signaling pathway. Biomed Pharmacother. 2020;129:110356.10.1016/j.biopha.2020.110356Search in Google Scholar PubMed
[55] Huang J, Chen D, Yan F, Wu S, Kang S, Xing W, et al. JTC-801 alleviates mechanical allodynia in paclitaxel-induced neuropathic pain through the PI3K/Akt pathway. Eur J Pharmacol. 2020;883:173306.10.1016/j.ejphar.2020.173306Search in Google Scholar PubMed
[56] Jia S, Wei G, Bono J, Pan Z, Zheng B, Wang B, et al. TET1 overexpression attenuates paclitaxel-induced neuropathic pain through rescuing K2p1.1 expression in primary sensory neurons of male rats. Life Sci. 2022;297:120486.10.1016/j.lfs.2022.120486Search in Google Scholar PubMed PubMed Central
[57] Chen XL, Liu SJ, Su WY, Yan HC, Dou J, Li ZW, et al. Effects and mechanism of albumin-bound paclitaxel-induced neuropathic pain in rats. Acta Univ Med Natl Sin. 2022;51(12):1102–8+1115.Search in Google Scholar
[58] Wu CX, Gao B, Wang L, Zhang R, Sun JL. Effects of vitamin D3 on paclitaxel-induced peripheral neuropathic pain in rats. Mod Pract Med. 2022;34(9):1131–3+1213+1116+1261.Search in Google Scholar
[59] Zhang SL, Li SJ, Yuan F, Feng D. Molecular role of calcium/calmodulin-dependent protein kinase II in paclitaxel-induced peripheral neuropathic pain. Chin J Gerontol. 2021;41(16):3501–6.Search in Google Scholar
[60] Wei X, Ma L, Wang L, Wang Y, Li WM, Zhou YQ, et al. Role and mechanism of simvastatin in alleviating neuropathic pain induced by nab-paclitaxel in rats. J Shanxi Med Univ. 2022;53(8):1004–10.Search in Google Scholar
[61] Wang WK, Li HC, Li XL, Feng DH, Zhang HY, Zhang QW, et al. Effect of miR-124 on neuropathic pain induced by paclitaxel via regulating early growth response1 EGR1. J Env Health. 2024;41(9):768–76+847.Search in Google Scholar
[62] Zhong MY, Luo XL. Curative effect of tetramethylpyrazine on paclitaxel-induced neuropathic pain in rats and effect of it on expression of nerve growth factor in sciatic nerve of the rats. J Clin Neurol. 2016;29(3):198–202.Search in Google Scholar
[63] Liu XJ, Cao F, Bu HL, Gao F, Yang H, Tian YK. Changes of 5-hydroxytryptamine contents in spinal cord dorsal horns of paclitaxel induced neuropathic pain rats. J Clin Anesthesiol. 2012;28(3):262–4.Search in Google Scholar
[64] Ouyang J, Zhao HQ, Kong Y, Niu Q, Chen Y, Si YY. The effect of electroacupuncture on paclitaxel-induced neuropathic pain in rats. Tianjin Med J. 2024;52(11):1141–6.Search in Google Scholar
[65] Wei X, Ma L, Li WM, Zhou YQ, Zhao YL. Expression of HMGB1/TLR4 pathway in the spinal cord of rats with albumin-bound paclitaxel-induced neuropathic pain. J Shanxi Med Univ. 2022;53(9):1113–9.Search in Google Scholar
[66] Zeng WY, Gu WY, Xu L, Zhang Y, Han C. Alleviating effect of miR-99b-5p on paclitaxel-induced neuropathic pain in rats and its impact on neuronal pyroptosis and apoptosis. Chin J Appl Physiol. 2022;38(5):438–42.Search in Google Scholar
[67] Zhong MY. Effect of antiangiogenic targeted therapy on paclitaxel-induced neuropathic pain in rats. J Clin Neurol. 2021;34(1):41–5.Search in Google Scholar
[68] Zhong MY, Luo XL. The influence of etramethylpyrazine injection on rats with malignant neuropathic pain due to tetramethylpyrazin. Henan Tradit Chin Med. 2015;35(12):2921–4.Search in Google Scholar
[69] Peng YC, Zhang SH, Ke JY, Zhang SY, Xiao Y. Effect of MicroRNA-513b-5p on paclitaxel-induced neuropathic pain in rats by regulating the expression of mGluR5. J Hubei Univ Med. 2022;41(6):549–54, 560.Search in Google Scholar
[70] Zheng WH, Liu CQ, Lv BR. Effect of asarum on paclitaxel-induced neuropathic pain in rats. Chin J Pain Med. 2011;17(10):620–3.Search in Google Scholar
[71] Wang L, Ma L, Jia LJ, Zhou YQ, Zhao YL. Role and mechanism of high mobility group box 1 inhibitor in alleviating neuropathic pain induced by nab-paclitaxel in rats. J Shanxi Med Univ. 2022;53(9):1120–6.Search in Google Scholar
[72] Cavaletti G, Cavalletti E, Montaguti P, Oggioni N, De Negri O, Tredici G. Effect on the peripheral nervous system of the short-term intravenous administration of paclitaxel in the rat. Neurotoxicology. 1997;18(1):137–45.Search in Google Scholar
[73] Nakamura H, Kawashiri T, Kobayashi D, Uchida M, Egashira N, Shimazoe T. Analgesic effects of sokeikakketsuto on chemotherapy-induced mechanical allodynia and cold hyperalgesia in rats. Biol Pharm Bull. 2021;44(2):271–4.10.1248/bpb.b20-00620Search in Google Scholar PubMed
[74] Mori K, Kawashiri T, Mine K, Inoue M, Kudamatsu H, Uchida M, et al. Inhibitory effect of α1 receptor antagonists on paclitaxel-induced peripheral neuropathy in a rodent model and clinical database. Toxics. 2022;10(11):669.10.3390/toxics10110669Search in Google Scholar PubMed PubMed Central
[75] Authier N, Gillet JP, Fialip J, Eschalier A, Coudore F. Description of a short-term Taxol-induced nociceptive neuropathy in rats. Brain Res. 2000;887(2):239–49.10.1016/S0006-8993(00)02910-3Search in Google Scholar PubMed
[76] Ganugula R, Deng M, Arora M, Pan HL, Kumar MNVR. Polyester nanoparticle encapsulation mitigates paclitaxel-induced peripheral neuropathy. ACS Chem Neurosci. 2019;10(3):1801–12.10.1021/acschemneuro.8b00703Search in Google Scholar PubMed PubMed Central
[77] Beh ST, Kuo YM, Chang WSW, Wilder-Smith E, Tsao CH, Tsai CH, et al. Preventive hypothermia as a neuroprotective strategy for paclitaxel-induced peripheral neuropathy. Pain. 2019;160(7):1505–21.10.1097/j.pain.0000000000001547Search in Google Scholar PubMed
[78] Khalilzadeh M, Ghasemi M, Faghir-Ghanesefat H, Ghafouri Esfahani M, Dehpour AR, Shafaroodi H. Aprepitant mitigates paclitaxel-induced neuropathic pain in rats via suppressing inflammatory pathways in dorsal root ganglia. Drug Chem Toxicol. 2025;48(1):62–71.10.1080/01480545.2024.2425992Search in Google Scholar PubMed
[79] Kuyrukluyildiz U, Kupeli I, Bedir Z, Ozmen O, Onk D, Suleyman B, et al. The effect of anakinra on paclitaxel-induced peripheral neuropathic pain in rats. Turk J Anesth Reanim. 2017;44(6):287–94.10.5152/TJAR.2016.02212Search in Google Scholar PubMed PubMed Central
[80] Hacimuftuoglu A, Mohammadzadeh M, Taghizadehghalehjoughi A, Taspinar N, Togar B, Nalcı KA, et al. The analgesic effect of metformin on paclitaxel-induced neuropathic pain model in rats: By considering pathological results. J Cancer Res Ther. 2020;16(1):34–9.10.4103/jcrt.JCRT_1455_16Search in Google Scholar PubMed
[81] Choi J, Jeon C, Lee J, Jang J, Quan F, Lee K, et al. Suppressive effects of bee venom acupuncture on paclitaxel-induced neuropathic pain in rats: Mediation by spinal α₂-adrenergic receptor. Toxins. 2017;9(11):351.10.3390/toxins9110351Search in Google Scholar PubMed PubMed Central
[82] Mangaiarkkarasi A, Rameshkannan S, Ali RM. Effect of gabapentin and pregabalin in rat model of taxol induced neuropathic pain. J Clin Diagn Res. 2015;9(5):FF11–4.10.7860/JCDR/2015/13373.5955Search in Google Scholar PubMed PubMed Central
[83] Saha L, Hota D, Chakrabarti A. Evaluation of lercanidipine in Paclitaxel-induced neuropathic pain model in rat: a preliminary study. Pain Res Treat. 2012;2012:1–5.10.1155/2012/143579Search in Google Scholar PubMed PubMed Central
[84] Kalynovska N, Diallo M, Sotakova‐Kasparova D, Palecek J. Losartan attenuates neuroinflammation and neuropathic pain in paclitaxel-induced peripheral neuropathy. J Cell Mol Med. 2020;24(14):7949–58.10.1111/jcmm.15427Search in Google Scholar PubMed PubMed Central
[85] Adamek P, Heles M, Bhattacharyya A, Pontearso M, Slepicka J, Palecek J. Dual PI3Kδ/γ inhibitor duvelisib prevents development of neuropathic pain in model of paclitaxel-induced peripheral neuropathy. J Neurosci. 2022;42(9):1864–81.10.1523/JNEUROSCI.1324-21.2021Search in Google Scholar PubMed PubMed Central
[86] Joshi P, Patel S, Paliwal A, Jain S, Verma K, Dwivedi J, et al. Tinospora cordifolia ameliorates paclitaxel-induced neuropathic pain in albino rats. J Ethnopharmacol. 2024;321:117559.10.1016/j.jep.2023.117559Search in Google Scholar PubMed
[87] Okubo K, Takahashi T, Sekiguchi F, Kanaoka D, Matsunami M, Ohkubo T, et al. Inhibition of T-type calcium channels and hydrogen sulfide-forming enzyme reverses paclitaxel-evoked neuropathic hyperalgesia in rats. Neuroscience. 2011;188:148–56.10.1016/j.neuroscience.2011.05.004Search in Google Scholar PubMed
[88] Nieto FR, Cendán CM, Sánchez-Fernández C, Cobos EJ, Entrena JM, Tejada MA, et al. Role of sigma-1 receptors in paclitaxel-induced neuropathic pain in mice. J Pain. 2012;13(11):1107–21.10.1016/j.jpain.2012.08.006Search in Google Scholar PubMed
[89] Nieto FR, Cendán CM, Cañizares FJ, Cubero MA, Vela JM, Fernández-Segura E, et al. Genetic inactivation and pharmacological blockade of sigma-1 receptors prevent paclitaxel-induced sensory-nerve mitochondrial abnormalities and neuropathic pain in mice. Mol Pain. 2014;10:1744–8069-10–1.10.1186/1744-8069-10-11Search in Google Scholar PubMed PubMed Central
[90] Yan JH, Han KY, Xia J, Hu HS. Effect and mechanism of quercetin on pain relief induced by paclitaxel in neuropathic rats. Nat Prod Res Dev. 2019;31(12):2065–70, 2181.Search in Google Scholar
[91] Park KT, Kim S, Choi I, Han IH, Bae H, Kim W. The involvement of the noradrenergic system in the antinociceptive effect of cucurbitacin D on mice with paclitaxel-induced neuropathic pain. Front Pharmacol. 2023;13:1055264.10.3389/fphar.2022.1055264Search in Google Scholar PubMed PubMed Central
[92] Suo J, Wang M, Zhang P, Lu Y, Xu R, Zhang L, et al. Siwei Jianbu decoction improves painful paclitaxel-induced peripheral neuropathy in mouse model by modulating the NF-κB and MAPK signaling pathways. Regen Med Res. 2020;8:2.10.1051/rmr/200001Search in Google Scholar PubMed PubMed Central
[93] Mao Q, Tian L, Wei J, Zhou X, Cheng H, Zhu X, et al. Transcriptome analysis of microRNAs, circRNAs, and mRNAs in the dorsal root ganglia of paclitaxel-induced mice with neuropathic pain. Front Mol Neurosci. 2022;15:990260.10.3389/fnmol.2022.990260Search in Google Scholar PubMed PubMed Central
[94] Lee JH, Kim B, Ko SG, Kim W. Analgesic effect of SH003 and Trichosanthes kirilowii Maximowicz in paclitaxel-induced neuropathic pain in mice. Curr Issues Mol Biol. 2022;44(2):718–30.10.3390/cimb44020050Search in Google Scholar PubMed PubMed Central
[95] Moraes TR, Veras FP, Barchuk AR, Nogueira ESC, Kanashiro A, Galdino G. Spinal HMGB1 participates in the early stages of paclitaxel-induced neuropathic pain via microglial TLR4 and RAGE activation. Front Immunol. 2024;15:1303937.10.3389/fimmu.2024.1303937Search in Google Scholar PubMed PubMed Central
[96] Kim MJ, Lee JH, Jang JU, Quan FS, Kim SK, Kim W. The efficacy of combination treatment of gabapentin and electro-acupuncture on paclitaxel-induced neuropathic pain. Korean J Physiol Pharmacol. 2017;21(6):657–66.10.4196/kjpp.2017.21.6.657Search in Google Scholar PubMed PubMed Central
[97] Luo X, Huh Y, Bang S, He Q, Zhang L, Matsuda M, et al. Macrophage toll-like receptor 9 contributes to chemotherapy-induced neuropathic pain in male mice. J Neurosci. 2019;39(35):6848–64.10.1523/JNEUROSCI.3257-18.2019Search in Google Scholar PubMed PubMed Central
[98] Park KT, Ko SG, Kim W. Phlomidis Radix extract alleviates paclitaxel-induced neuropathic pain by modulating spinal TRPV1 in mice. Plants. 2023;12(22):3819.10.3390/plants12223819Search in Google Scholar PubMed PubMed Central
[99] Zhang X, Wang J, Ran R, Peng Y, Xiao Y. FSC231 alleviates paclitaxel-induced neuralgia by inhibiting the interactions between PICK1 and GluA2 and activates GSK-3β and ERK1/2. Brain Behav. 2021;11(11):e2380.10.1002/brb3.2380Search in Google Scholar PubMed PubMed Central
[100] Slivicki RA, Mali SS, Hohmann AG. Voluntary exercise reduces both chemotherapy-induced neuropathic nociception and deficits in hippocampal cellular proliferation in a mouse model of paclitaxel-induced peripheral neuropathy. Neurobiol Pain. 2019;6:100035.10.1016/j.ynpai.2019.100035Search in Google Scholar PubMed PubMed Central
[101] Kumar Kalvala A, Bagde A, Arthur P, Kumar Surapaneni S, Ramesh N, Nathani A, et al. Role of Cannabidiol and Tetrahydrocannabivarin on Paclitaxel-induced neuropathic pain in rodents. Int Immunopharmacol. 2022;107:108693.10.1016/j.intimp.2022.108693Search in Google Scholar PubMed PubMed Central
[102] Kim N, Chung G, Son SR, Park JH, Lee YH, Park KT, et al. Magnolin inhibits paclitaxel-induced cold allodynia and ERK1/2 activation in mice. Plants. 2023;12(12):2283.10.3390/plants12122283Search in Google Scholar PubMed PubMed Central
[103] Slivicki RA, Xu Z, Mali SS, Hohmann AG. Brain permeant and impermeant inhibitors of fatty-acid amide hydrolase suppress the development and maintenance of paclitaxel-induced neuropathic pain without producing tolerance or physical dependence in vivo and synergize with paclitaxel to reduce tumor cell line viability in vitro. Pharmacol Res. 2019;142:267–82.10.1016/j.phrs.2019.02.002Search in Google Scholar PubMed PubMed Central
[104] Li Y, Kang J, Xu Y, Li N, Jiao Y, Wang C, et al. Artesunate alleviates paclitaxel-induced neuropathic pain in mice by decreasing metabotropic glutamate receptor 5 activity and neuroinflammation in primary sensory neurons. Front Mol Neurosci. 2022;15:902572.10.3389/fnmol.2022.902572Search in Google Scholar PubMed PubMed Central
[105] Uchida H, Nagai J, Ueda H. Lysophosphatidic acid and its receptors LPA1 and LPA3 mediate paclitaxel-induced neuropathic pain in mice. Mol Pain. 2014;10:1744–8069.10.1186/1744-8069-10-71Search in Google Scholar PubMed PubMed Central
[106] Park KT, Jeon YJ, Kim HI, Kim W. Antinociceptive effect of Dendrobii caulis in paclitaxel-induced neuropathic pain in mice. Life. 2023;13(12):2289.10.3390/life13122289Search in Google Scholar PubMed PubMed Central
[107] Son DB, Choi W, Kim M, Go EJ, Jeong D, Park CK, et al. Decursin alleviates mechanical allodynia in a paclitaxel-induced neuropathic pain mouse model. Cells. 2021;10(3):547.10.3390/cells10030547Search in Google Scholar PubMed PubMed Central
[108] Cao J, Liu X, Liu JX, Zhao S, Guo YX, Wang GY, et al. Inhibition of glutamatergic neurons in layer II/III of the medial prefrontal cortex alleviates paclitaxel-induced neuropathic pain and anxiety. Eur J Pharmacol. 2022;936:175351.10.1016/j.ejphar.2022.175351Search in Google Scholar PubMed
[109] Sisignano M, Angioni C, Park CK, Meyer Dos Santos S, Jordan H, Kuzikov M, et al. Targeting CYP2J to reduce paclitaxel-induced peripheral neuropathic pain. Proc Natl Acad Sci. 2016;113(44):12544–9.10.1073/pnas.1613246113Search in Google Scholar PubMed PubMed Central
[110] Wedel S, Hahnefeld L, Schreiber Y, Namendorf C, Heymann T, Uhr M, et al. SAFit2 ameliorates paclitaxel-induced neuropathic pain by reducing spinal gliosis and elevating pro-resolving lipid mediators. J Neuroinflamm. 2023;20(1):149.10.1186/s12974-023-02835-5Search in Google Scholar PubMed PubMed Central
[111] Qabazard B, Masocha W, Khajah M, Phillips OA. H2S donor GYY4137 ameliorates paclitaxel-induced neuropathic pain in mice. Biomed Pharmacother. 2020;127:110210.10.1016/j.biopha.2020.110210Search in Google Scholar PubMed
[112] Zafar S, Luo Y, Zhang L, Li CH, Khan A, Khan MI, et al. Daidzein attenuated paclitaxel-induced neuropathic pain via the down-regulation of TRPV1/P2Y and up-regulation of Nrf2/HO-1 signaling. Inflammopharmacology. 2023;31(4):1977–92.10.1007/s10787-023-01225-wSearch in Google Scholar PubMed
[113] Thangamani D, Edafiogho IO, Masocha W. The anticonvulsant enaminone E139 attenuates paclitaxel-induced neuropathic pain in rodents. Sci World J. 2013;2013(1):240508.10.1155/2013/240508Search in Google Scholar PubMed PubMed Central
[114] Al-Romaiyan A, Barakat A, Jose L, Masocha W. An aqueous Commiphora myrrha extract ameliorates paclitaxel-induced peripheral neuropathic pain in mice. Front Pharmacol. 2023;14:1295096.10.3389/fphar.2023.1295096Search in Google Scholar PubMed PubMed Central
[115] Masocha W. Astrocyte activation in the anterior cingulate cortex and altered glutamatergic gene expression during paclitaxel-induced neuropathic pain in mice. PeerJ. 2015;3:e1350.10.7717/peerj.1350Search in Google Scholar PubMed PubMed Central
[116] Thomas A, Okine BN, Finn DP, Masocha W. Peripheral deficiency and antiallodynic effects of 2-arachidonoyl glycerol in a mouse model of paclitaxel-induced neuropathic pain. Biomed Pharmacother. 2020;129:110456.10.1016/j.biopha.2020.110456Search in Google Scholar PubMed
[117] Ami N, Okamoto K, Oshima H. Analgesic effect of magnetic stimulation on paclitaxel-induced peripheral neuropathic pain in mice. Brain Res. 2012;1461:24–9.10.1016/j.brainres.2012.04.044Search in Google Scholar PubMed
[118] Chen Y, Yang C, Wang ZJ. Proteinase-activated receptor 2 sensitizes transient receptor potential vanilloid 1, transient receptor potential vanilloid 4, and transient receptor potential ankyrin 1 in paclitaxel-induced neuropathic pain. Neuroscience. 2011;193:440–51.10.1016/j.neuroscience.2011.06.085Search in Google Scholar PubMed
[119] Choi JW, Kang SY, Choi JG, Kang DW, Kim SJ, Lee SD, et al. Analgesic effect of electroacupuncture on paclitaxel-induced neuropathic pain via spinal opioidergic and adrenergic mechanisms in mice. Am J Chin Med. 2015;43(1):57–70.10.1142/S0192415X15500044Search in Google Scholar PubMed
[120] Su CJ, Zhang JT, Zhao FL, Xu DL, Pan J, Liu T. Resolvin D1/N-formyl peptide receptor 2 ameliorates paclitaxel-induced neuropathic pain through the activation of IL-10/Nrf2/HO-1 pathway in mice. Front Immunol. 2023;14:1091753.10.3389/fimmu.2023.1091753Search in Google Scholar PubMed PubMed Central
[121] Sankaranarayanan I, Tavares-Ferreira D, Mwirigi JM, Mejia GL, Burton MD, Price TJ. Inducible co-stimulatory molecule (ICOS) alleviates paclitaxel-induced neuropathic pain via an IL-10-mediated mechanism in female mice. J Neuroinflamm. 2023;20(1):32.10.1186/s12974-023-02719-8Search in Google Scholar PubMed PubMed Central
[122] Yang Y, Wen J, Zheng B, Wu S, Mao Q, Liang L, et al. CREB participates in paclitaxel-induced neuropathic pain genesis through transcriptional activation of Dnmt3a in primary sensory neurons. Neurotherapeutics. 2021;18(1):586–600.10.1007/s13311-020-00931-5Search in Google Scholar PubMed PubMed Central
[123] Cristiano C, Avagliano C, Cuozzo M, Liguori FM, Calignano A, Russo R. The beneficial effects of ultramicronized palmitoylethanolamide in the management of neuropathic pain and associated mood disorders induced by paclitaxel in mice. Biomolecules. 2022;12(8):1155.10.3390/biom12081155Search in Google Scholar PubMed PubMed Central
[124] Nieto FR, Entrena JM, Cendán CM, Del Pozo E, Vela JM, Baeyens JM. Tetrodotoxin inhibits the development and expression of neuropathic pain induced by paclitaxel in mice. Pain. 2008;137(3):520–31.10.1016/j.pain.2007.10.012Search in Google Scholar PubMed
[125] Micheli L, Testai L, Angeli A, Carrino D, Pacini A, Margiotta F, et al. Inhibitors of mitochondrial human carbonic anhydrases VA and VB as a therapeutic strategy against paclitaxel-induced neuropathic pain in mice. Int J Mol Sci. 2022;23(11):6229.10.3390/ijms23116229Search in Google Scholar PubMed PubMed Central
[126] Mei C, Pan C, Xu L, Miao M, Lu Q, Yu Y, et al. Trimethoxyflavanone relieves paclitaxel-induced neuropathic pain via inhibiting expression and activation of P2X7 and production of CGRP in mice. Neuropharmacology. 2023;236:109584.10.1016/j.neuropharm.2023.109584Search in Google Scholar PubMed
[127] Pan C, Xu Y, Jiang Z, Fan C, Chi Z, Zhang Y, et al. Naringenin relieves paclitaxel-induced pain by suppressing calcitonin gene-related peptide signalling and enhances the anti-tumour action of paclitaxel. Br J Pharmacol. 2024;181(17):3136–59.10.1111/bph.16397Search in Google Scholar PubMed
[128] Sankaranarayanan I, Tavares-Ferreira D, He L, Kume M, Mwirigi JM, Madsen TM, et al. Meteorin alleviates paclitaxel-induced peripheral neuropathic pain in mice. J Pain. 2023;24(4):555–67.10.1016/j.jpain.2022.10.015Search in Google Scholar PubMed PubMed Central
[129] Mao Q, Wu S, Gu X, Du S, Mo K, Sun L, et al. DNMT3a-triggered downregulation of K2p 1.1 gene in primary sensory neurons contributes to paclitaxel-induced neuropathic pain. Int J Cancer. 2019;145(8):2122–34.10.1002/ijc.32155Search in Google Scholar PubMed PubMed Central
[130] Kaur S, Muthuraman A. Ameliorative effect of gallic acid in paclitaxel-induced neuropathic pain in mice. Toxicol Rep. 2019;6:505–13.10.1016/j.toxrep.2019.06.001Search in Google Scholar PubMed PubMed Central
[131] Katsuyama S, Sato K, Yagi T, Kishikawa Y, Nakamura H. Effects of repeated milnacipran and fluvoxamine treatment on mechanical allodynia in a mouse paclitaxel-induced neuropathic pain model. Biomed Res. 2013;34(2):105–11.10.2220/biomedres.34.105Search in Google Scholar PubMed
[132] Lobos N, Lux S, Zepeda RJ, Pelissier T, Marcos JL, Bustos-Quevedo G, et al. Rosuvastatin Synergistically Enhances the Antinociceptive Efficacy of Duloxetine in Paclitaxel-Induced Neuropathic Pain in Mice. Int J Mol Sci. 2023;24(9):8359.10.3390/ijms24098359Search in Google Scholar PubMed PubMed Central
[133] Abed A, Khoshnoud MJ, Taghian M, Aliasgharzadeh M, Mesdaghinia A. Quetiapine reverses paclitaxel-induced neuropathic pain in mice: Role of alpha2- adrenergic receptors. Iran J Basic Med Sci. 2017;20:1182–8.Search in Google Scholar
[134] Han C, Xu L, Zeng WY, Gu WY, Liu Q. miR-99b-5p targeting FGFR3 inhibits the paclitaxel-induced chronic neuralgia. Chin J Pain Med. 2021;27(10):737–43.Search in Google Scholar
[135] Takanashi K, Shibata K, Mizuno K, Komatsu R, Koizumi S. Goshajinkigan attenuates paclitaxel-induced neuropathic pain via cortical astrocytes. Pharmacol Res Perspect. 2021;9(6):e00850.10.1002/prp2.850Search in Google Scholar PubMed PubMed Central
[136] Li L, Li J, Zuo Y, Dang D, Frost JA, Yang Q. Activation of KCNQ channels prevents paclitaxel-induced peripheral neuropathy and associated neuropathic pain. J Pain. 2019;20(5):528–39.10.1016/j.jpain.2018.11.001Search in Google Scholar PubMed PubMed Central
[137] Miltenburg NC, Boogerd W. Chemotherapy-induced neuropathy: A comprehensive survey. Cancer Treat Rev. 2014;40(7):872–82.10.1016/j.ctrv.2014.04.004Search in Google Scholar PubMed
[138] Wolf S, Barton D, Kottschade L, Grothey A, Loprinzi C. Chemotherapy-induced peripheral neuropathy: prevention and treatment strategies. Eur J Cancer. 2008;44(11):1507–15.10.1016/j.ejca.2008.04.018Search in Google Scholar PubMed
[139] Hama A, Takamatsu H. Chemotherapy-induced peripheral neuropathic pain and rodent models. CNS Neurol Disord - Drug Targets. 2016;15(1):7–19.10.2174/1871527315666151110125325Search in Google Scholar PubMed
[140] Al Moundhri MS, Al-Salam S, Al Mahrouqee A, Beegam S, Ali BH. The effect of curcumin on oxaliplatin and cisplatin neurotoxicity in rats: some behavioral, biochemical, and histopathological studies. J Med Toxicol. 2013;9(1):25–33.10.1007/s13181-012-0239-xSearch in Google Scholar PubMed PubMed Central
[141] Committee of Neoplastic Supportive-Care, China Anti-Cancer Association, Cancer Clinical Chemotherapy Committee, China Anti-Cancer Association. Chinese expert consensus on the diagnosis and treatment of chemotherapy-induced peripheral neuropathy (2022 edition). Zhonghua Zhong Liu Za Zhi. 2022;44(9):928–34.Search in Google Scholar
[142] Wang W, Teresa M, Cai J, Zhang C, Wong S, Yan Z, et al. Comparative assessment for rat strain differences in metabolic profiles of 14 drugs in Wistar Han and Sprague Dawley hepatocytes. Xenobiotica. 2021;51(1):15–23.10.1080/00498254.2020.1795949Search in Google Scholar PubMed
[143] Chen X, Zhang W, Rios S, Morkos MB, Ye X, Li G, et al. An HPLC tandem mass spectrometry for quantification of ET-26-HCl and its major metabolite in plasma and application to a pharmacokinetic study in rats. J Pharm Biomed Anal. 2018;149:381–6.10.1016/j.jpba.2017.11.017Search in Google Scholar PubMed
[144] Xiong S, Deng Z, Sun P, Mu Y, Xue M. Development and validation of a rapid and sensitive LC-MS/MS method for the pharmacokinetic study of osimertinib in rats. J AOAC Int. 2017;100(6):1771–5.10.5740/jaoacint.16-0362Search in Google Scholar PubMed
[145] Hart ML, Ericsson AC, Lloyd KCK, Grimsrud KN, Rogala AR, Godfrey VL, et al. Development of outbred CD1 mouse colonies with distinct standardized gut microbiota profiles for use in complex microbiota targeted studies. Sci Rep. 2018;8(1):10107.10.1038/s41598-018-28448-0Search in Google Scholar PubMed PubMed Central
[146] Mouse Genome Sequencing Consortium. Initial sequencing and comparative analysis of the mouse genome. Nature. 2002;420(6915):520–62.10.1038/nature01262Search in Google Scholar PubMed
[147] Yi C, Ezan P, Fernández P, Schmitt J, Sáez JC, Giaume C, et al. Inhibition of glial hemichannels by boldine treatment reduces neuronal suffering in a murine model of Alzheimer’s disease. Glia. 2017;65(10):1607–25.10.1002/glia.23182Search in Google Scholar PubMed
[148] Liu H, Patki G, Salvi A, Kelly M, Salim S. Behavioral effects of early life maternal trauma witness in rats. Prog Neuropsychopharmacol Biol Psychiatry. 2018;81:80–7.10.1016/j.pnpbp.2017.10.013Search in Google Scholar PubMed PubMed Central
[149] Riley JL, Robinson ME, Wise EA, Myers CD, Fillingim RB. Sex differences in the perception of noxious experimental stimuli: a meta-analysis. Pain. 1998;74(2):181–7.10.1016/S0304-3959(97)00199-1Search in Google Scholar PubMed
[150] Hwang BY, Kim ES, Kim CH, Kwon JY, Kim HK. Gender differences in paclitaxel-induced neuropathic pain behavior and analgesic response in rats. Korean J Anesthesiol. 2012;62(1):66.10.4097/kjae.2012.62.1.66Search in Google Scholar PubMed PubMed Central
[151] Lee JY, Choi HY, Ju BG, Yune TY. Estrogen alleviates neuropathic pain induced after spinal cord injury by inhibiting microglia and astrocyte activation. Biochim Biophys Acta (BBA) - Mol Basis Dis. 2018;1864(7):2472–80.10.1016/j.bbadis.2018.04.006Search in Google Scholar PubMed
[152] Deng C, Gu Y, Zhang H, Zhang J. Estrogen affects neuropathic pain through upregulating N-methyl-D-aspartate acid receptor 1 expression in the dorsal root ganglion of rats. Neural Regen Res. 2017;12(3):464.10.4103/1673-5374.202925Search in Google Scholar PubMed PubMed Central
[153] Duong P, Tenkorang MAA, Trieu J, McCuiston C, Rybalchenko N, Cunningham RL. Neuroprotective and neurotoxic outcomes of androgens and estrogens in an oxidative stress environment. Biol Sex Differ. 2020;11(1):12.10.1186/s13293-020-0283-1Search in Google Scholar PubMed PubMed Central
[154] Cecco S, Aliberti M, Baldo P, Giacomin E, Leone R. Safety and efficacy evaluation of albumin-bound paclitaxel. Expert Opin Drug Saf. 2014;13(4):511–20.10.1517/14740338.2014.893293Search in Google Scholar PubMed
[155] Li Y, Zhang G, Pfeifer BA. Current and emerging options for taxol production. Adv Biochem Eng Biotechnol. 2014;148:405–25.10.1007/10_2014_292Search in Google Scholar PubMed
[156] Wang Y, Liu X. Safety signals of albumin-bound paclitaxel: Data mining of the Food and Drug Administration adverse event reporting system. Indian J Pharmacol. 2023;55(3):167–73.10.4103/ijp.ijp_640_22Search in Google Scholar PubMed PubMed Central
[157] Tofthagen C, McAllister RD, Visovsky C. Peripheral neuropathy caused by paclitaxel and docetaxel: an evaluation and comparison of symptoms. J Adv Pract Oncol. 2013;4(4):204–15.10.6004/jadpro.2013.4.4.2Search in Google Scholar
[158] Marmiroli P, Scuteri A, Cornblath DR, Cavaletti G. Pain in chemotherapy-induced peripheral neurotoxicity. J Peripher Nerv Syst. 2017;22(3):156–61.10.1111/jns.12226Search in Google Scholar PubMed
[159] Stage TB, Bergmann TK, Kroetz DL. Clinical pharmacokinetics of paclitaxel monotherapy: an updated literature review. Clin Pharmacokinet. 2018;57(1):7–19.10.1007/s40262-017-0563-zSearch in Google Scholar PubMed PubMed Central
[160] Staff NP, Fehrenbacher JC, Caillaud M, Damaj MI, Segal RA, Rieger S. Pathogenesis of paclitaxel-induced peripheral neuropathy: A current review of in vitro and in vivo findings using rodent and human model systems. Exp Neurol. 2020;324:113121.10.1016/j.expneurol.2019.113121Search in Google Scholar PubMed PubMed Central
[161] Liu SJ, Liu MY, Chen YT, Su WY, Cao RH, Chang LJ, et al. A study on the correlation between taxane-induced neuropathic pain and serum IL-6 levels in breast cancer patients. Chin J Clin N Med. 2022;15(11):1012–6.Search in Google Scholar
[162] Penson RT, Kronish K, Duan Z, Feller AJ, Stark P, Cook SE, et al. Cytokines IL-1beta, IL-2, IL-6, IL-8, MCP-1, GM-CSF and TNFalpha in patients with epithelial ovarian cancer and their relationship to treatment with paclitaxel. Int J Gynecol Cancer. 2000;10(1):33–41.10.1046/j.1525-1438.2000.00003.xSearch in Google Scholar PubMed
[163] Long X, Zheng M, Yang Y, Chen Y, Zhang X, Zhang H. circ_ZFR is linked to paclitaxel resistance in cervical cancer via miR-944 sponging and IL-10 upregulation. Anal Cell Pathol. 2022;2022:1–10.10.1155/2022/4807287Search in Google Scholar PubMed PubMed Central
[164] Krukowski K, Eijkelkamp N, Laumet G, Hack CE, Li Y, Dougherty PM, et al. CD8+ T cells and endogenous IL-10 are required for resolution of chemotherapy-induced neuropathic pain. J Neurosci. 2016;36(43):11074–83.10.1523/JNEUROSCI.3708-15.2016Search in Google Scholar PubMed PubMed Central
[165] Bevers TB, Niell BL, Baker JL, Bennett DL, Bonaccio E, Camp MS, et al. NCCN Guidelines® insights: breast cancer screening and diagnosis, version 1.2023. J Natl Compr Cancer Netw. 2023;21(9):900–9.10.6004/jnccn.2023.0046Search in Google Scholar PubMed
[166] Dworkin RH, O’Connor AB, Audette J, Baron R, Gourlay GK, Haanpää ML, et al. Recommendations for the pharmacological management of neuropathic pain: an overview and literature update. Mayo Clin Proc. 2010;85(3):S3–14.10.4065/mcp.2009.0649Search in Google Scholar PubMed PubMed Central
[167] Baron R. Peripheral neuropathic pain: from mechanisms to symptoms. Clin J Pain. 2000;16:S12–20.10.1097/00002508-200006001-00004Search in Google Scholar PubMed
[168] Feng CC, Yan XJ, Chen X, Wang EM, Liu Q, Zhang LY, et al. Vagal anandamide signaling via cannabinoid receptor 1 contributes to luminal 5-HT modulation of visceral nociception in rats. Pain. 2014;155(8):1591–604.10.1016/j.pain.2014.05.005Search in Google Scholar PubMed
[169] Ji WJ, Liang JX, Zhao GD. Role of the vanilloid receptor in endothelin-1-induced thermal hyperalgesia. J South Med Univ. 2007;1:101–3, 106.Search in Google Scholar
[170] Baron R, Binder A, Wasner G. Neuropathic pain: diagnosis, pathophysiological mechanisms, and treatment. Lancet Neurol. 2010;9(8):807–19.10.1016/S1474-4422(10)70143-5Search in Google Scholar PubMed
[171] Cavalcanti MRM, Passos FRS, Monteiro BS, Gandhi SR, Heimfarth L, Lima BS, et al. HPLC-DAD-UV analysis, anti-inflammatory and anti-neuropathic effects of methanolic extract of Sideritis bilgeriana (lamiaceae) by NF-κB, TNF-α, IL-1β and IL-6 involvement. J Ethnopharmacol. 2021;265:113338.10.1016/j.jep.2020.113338Search in Google Scholar PubMed
[172] Eddy NB, Leimbach D. Synthetic analgesics. II. Dithienylbutenyl- and dithienylbutylamines. J Pharmacol Exp Ther. 1953;107(3):385–93.10.1016/S0022-3565(25)05180-8Search in Google Scholar
[173] Chaplan SR, Bach FW, Pogrel JW, Chung JM, Yaksh TL. Quantitative assessment of tactile allodynia in the rat paw. J Neurosci Methods. 1994;53(1):55–63.10.1016/0165-0270(94)90144-9Search in Google Scholar PubMed
[174] Vermeer CJC, Hiensch AE, Cleenewerk L, May AM, Eijkelkamp N. Neuro-immune interactions in paclitaxel-induced peripheral neuropathy. Acta Oncol. 2021;60(10):1369–82.10.1080/0284186X.2021.1954241Search in Google Scholar PubMed
[175] Li QY, Xu HY, Yang HJ. Effect of proinflammatory factors TNF-α, IL-1β, IL-6 on neuropathic pain. Zhongguo Zhong Yao Za Zhi. 2017;42(19):3709–12.Search in Google Scholar
[176] Singh S, Anshita D, Ravichandiran V. MCP-1: Function, regulation, and involvement in disease. Int Immunopharmacol. 2021;101(Pt B):107598.10.1016/j.intimp.2021.107598Search in Google Scholar PubMed PubMed Central
[177] Konnova EA, Deftu AF, Chu Sin Chung P, Pertin M, Kirschmann G, Decosterd I, et al. Characterisation of GFAP-expressing glial cells in the dorsal root ganglion after spared nerve injury. Int J Mol Sci. 2023;24(21):15559.10.3390/ijms242115559Search in Google Scholar PubMed PubMed Central
[178] Sasaki Y, Ohsawa K, Kanazawa H, Kohsaka S, Imai Y. Iba1 is an actin-cross-linking protein in macrophages/microglia. Biochem Biophys Res Commun. 2001;286(2):292–7.10.1006/bbrc.2001.5388Search in Google Scholar PubMed
[179] Pozzi E, Terribile G, Cherchi L, Di Girolamo S, Sancini G, Alberti P. Ion Channel and transporter involvement in chemotherapy-induced peripheral neurotoxicity. Int J Mol Sci. 2024;25(12):6552.10.3390/ijms25126552Search in Google Scholar PubMed PubMed Central
[180] Vasylyev DV, Zhao P, Schulman BR, Waxman SG. Interplay of Nav1.8 and Nav1.7 channels drives neuronal hyperexcitability in neuropathic pain. J Gen Physiol. 2024;156(11):e202413596.10.1085/jgp.202413596Search in Google Scholar PubMed PubMed Central
[181] Duggett NA, Griffiths LA, McKenna OE, De Santis V, Yongsanguanchai N, Mokori EB, et al. Oxidative stress in the development, maintenance and resolution of paclitaxel-induced painful neuropathy. Neuroscience. 2016;333:13–26.10.1016/j.neuroscience.2016.06.050Search in Google Scholar PubMed PubMed Central
[182] Barrière DA, Rieusset J, Chanteranne D, Busserolles J, Chauvin MA, Chapuis L, et al. Paclitaxel therapy potentiates cold hyperalgesia in streptozotocin-induced diabetic rats through enhanced mitochondrial reactive oxygen species production and TRPA1 sensitization. Pain. 2012;153(3):553–61.10.1016/j.pain.2011.11.019Search in Google Scholar PubMed
[183] Casals-Díaz L, Casas C, Navarro X. Changes of voltage-gated sodium channels in sensory nerve regeneration and neuropathic pain models. Restor Neurol Neuros. 2015;33(3):321–34.10.3233/RNN-140444Search in Google Scholar PubMed
[184] Oğğuzhanoğğlu A, Erdoğğan Ç, Tabak E, Cenikli U. Comparison of conduction velocities of nerve fibers to smaller and larger muscles in rats. Int J Neurosci. 2010;120(1):76–9.10.3109/00207450903389370Search in Google Scholar PubMed
[185] Chahal PS, Sohail W, Cartwright MS. Neuromuscular ultrasound in the diagnosis of focal neuropathies superimposed on polyneuropathy: a case report. Clin Neurophysiol. 2012;123(3):626–7.10.1016/j.clinph.2011.07.032Search in Google Scholar PubMed PubMed Central
© 2025 the author(s), published by De Gruyter
This work is licensed under the Creative Commons Attribution 4.0 International License.
Articles in the same Issue
- Biomedical Sciences
- Mechanism of triptolide regulating proliferation and apoptosis of hepatoma cells by inhibiting JAK/STAT pathway
- Maslinic acid improves mitochondrial function and inhibits oxidative stress and autophagy in human gastric smooth muscle cells
- Comparative analysis of inflammatory biomarkers for the diagnosis of neonatal sepsis: IL-6, IL-8, SAA, CRP, and PCT
- Post-pandemic insights on COVID-19 and premature ovarian insufficiency
- Proteome differences of dental stem cells between permanent and deciduous teeth by data-independent acquisition proteomics
- Optimizing a modified cetyltrimethylammonium bromide protocol for fungal DNA extraction: Insights from multilocus gene amplification
- Preliminary analysis of the role of small hepatitis B surface proteins mutations in the pathogenesis of occult hepatitis B infection via the endoplasmic reticulum stress-induced UPR-ERAD pathway
- Efficacy of alginate-coated gold nanoparticles against antibiotics-resistant Staphylococcus and Streptococcus pathogens of acne origins
- Battling COVID-19 leveraging nanobiotechnology: Gold and silver nanoparticle–B-escin conjugates as SARS-CoV-2 inhibitors
- Neurodegenerative diseases and neuroinflammation-induced apoptosis
- Impact of fracture fixation surgery on cognitive function and the gut microbiota in mice with a history of stroke
- COLEC10: A potential tumor suppressor and prognostic biomarker in hepatocellular carcinoma through modulation of EMT and PI3K-AKT pathways
- High-temperature requirement serine protease A2 inhibitor UCF-101 ameliorates damaged neurons in traumatic brain-injured rats by the AMPK/NF-κB pathway
- SIK1 inhibits IL-1β-stimulated cartilage apoptosis and inflammation in vitro through the CRTC2/CREB1 signaling
- Rutin–chitooligosaccharide complex: Comprehensive evaluation of its anti-inflammatory and analgesic properties in vitro and in vivo
- Knockdown of Aurora kinase B alleviates high glucose-triggered trophoblast cells damage and inflammation during gestational diabetes
- Calcium-sensing receptors promoted Homer1 expression and osteogenic differentiation in bone marrow mesenchymal stem cells
- ABI3BP can inhibit the proliferation, invasion, and epithelial–mesenchymal transition of non-small-cell lung cancer cells
- Changes in blood glucose and metabolism in hyperuricemia mice
- Rapid detection of the GJB2 c.235delC mutation based on CRISPR-Cas13a combined with lateral flow dipstick
- IL-11 promotes Ang II-induced autophagy inhibition and mitochondrial dysfunction in atrial fibroblasts
- Short-chain fatty acid attenuates intestinal inflammation by regulation of gut microbial composition in antibiotic-associated diarrhea
- Application of metagenomic next-generation sequencing in the diagnosis of pathogens in patients with diabetes complicated by community-acquired pneumonia
- NAT10 promotes radiotherapy resistance in non-small cell lung cancer by regulating KPNB1-mediated PD-L1 nuclear translocation
- Phytol-mixed micelles alleviate dexamethasone-induced osteoporosis in zebrafish: Activation of the MMP3–OPN–MAPK pathway-mediating bone remodeling
- Association between TGF-β1 and β-catenin expression in the vaginal wall of patients with pelvic organ prolapse
- Primary pleomorphic liposarcoma involving bilateral ovaries: Case report and literature review
- Effects of de novo donor-specific Class I and II antibodies on graft outcomes after liver transplantation: A pilot cohort study
- Sleep architecture in Alzheimer’s disease continuum: The deep sleep question
- Ephedra fragilis plant extract: A groundbreaking corrosion inhibitor for mild steel in acidic environments – electrochemical, EDX, DFT, and Monte Carlo studies
- Langerhans cell histiocytosis in an adult patient with upper jaw and pulmonary involvement: A case report
- Inhibition of mast cell activation by Jaranol-targeted Pirin ameliorates allergic responses in mouse allergic rhinitis
- Aeromonas veronii-induced septic arthritis of the hip in a child with acute lymphoblastic leukemia
- Clusterin activates the heat shock response via the PI3K/Akt pathway to protect cardiomyocytes from high-temperature-induced apoptosis
- Research progress on fecal microbiota transplantation in tumor prevention and treatment
- Low-pressure exposure influences the development of HAPE
- Stigmasterol alleviates endplate chondrocyte degeneration through inducing mitophagy by enhancing PINK1 mRNA acetylation via the ESR1/NAT10 axis
- AKAP12, mediated by transcription factor 21, inhibits cell proliferation, metastasis, and glycolysis in lung squamous cell carcinoma
- Association between PAX9 or MSX1 gene polymorphism and tooth agenesis risk: A meta-analysis
- A case of bloodstream infection caused by Neisseria gonorrhoeae
- Case of nasopharyngeal tuberculosis complicated with cervical lymph node and pulmonary tuberculosis
- p-Cymene inhibits pro-fibrotic and inflammatory mediators to prevent hepatic dysfunction
- GFPT2 promotes paclitaxel resistance in epithelial ovarian cancer cells via activating NF-κB signaling pathway
- Transfer RNA-derived fragment tRF-36 modulates varicose vein progression via human vascular smooth muscle cell Notch signaling
- RTA-408 attenuates the hepatic ischemia reperfusion injury in mice possibly by activating the Nrf2/HO-1 signaling pathway
- Decreased serum TIMP4 levels in patients with rheumatoid arthritis
- Sirt1 protects lupus nephritis by inhibiting the NLRP3 signaling pathway in human glomerular mesangial cells
- Sodium butyrate aids brain injury repair in neonatal rats
- Interaction of MTHFR polymorphism with PAX1 methylation in cervical cancer
- Convallatoxin inhibits proliferation and angiogenesis of glioma cells via regulating JAK/STAT3 pathway
- The effect of the PKR inhibitor, 2-aminopurine, on the replication of influenza A virus, and segment 8 mRNA splicing
- Effects of Ire1 gene on virulence and pathogenicity of Candida albicans
- Small cell lung cancer with small intestinal metastasis: Case report and literature review
- GRB14: A prognostic biomarker driving tumor progression in gastric cancer through the PI3K/AKT signaling pathway by interacting with COBLL1
- 15-Lipoxygenase-2 deficiency induces foam cell formation that can be restored by salidroside through the inhibition of arachidonic acid effects
- FTO alleviated the diabetic nephropathy progression by regulating the N6-methyladenosine levels of DACT1
- Clinical relevance of inflammatory markers in the evaluation of severity of ulcerative colitis: A retrospective study
- Zinc valproic acid complex promotes osteoblast differentiation and exhibits anti-osteoporotic potential
- Primary pulmonary synovial sarcoma in the bronchial cavity: A case report
- Metagenomic next-generation sequencing of alveolar lavage fluid improves the detection of pulmonary infection
- Uterine tumor resembling ovarian sex cord tumor with extensive rhabdoid differentiation: A case report
- Genomic analysis of a novel ST11(PR34365) Clostridioides difficile strain isolated from the human fecal of a CDI patient in Guizhou, China
- Effects of tiered cardiac rehabilitation on CRP, TNF-α, and physical endurance in older adults with coronary heart disease
- Changes in T-lymphocyte subpopulations in patients with colorectal cancer before and after acupoint catgut embedding acupuncture observation
- Modulating the tumor microenvironment: The role of traditional Chinese medicine in improving lung cancer treatment
- Alterations of metabolites related to microbiota–gut–brain axis in plasma of colon cancer, esophageal cancer, stomach cancer, and lung cancer patients
- Research on individualized drug sensitivity detection technology based on bio-3D printing technology for precision treatment of gastrointestinal stromal tumors
- CEBPB promotes ulcerative colitis-associated colorectal cancer by stimulating tumor growth and activating the NF-κB/STAT3 signaling pathway
- Oncolytic bacteria: A revolutionary approach to cancer therapy
- A de novo meningioma with rapid growth: A possible malignancy imposter?
- Diagnosis of secondary tuberculosis infection in an asymptomatic elderly with cancer using next-generation sequencing: Case report
- Hesperidin and its zinc(ii) complex enhance osteoblast differentiation and bone formation: In vitro and in vivo evaluations
- Research progress on the regulation of autophagy in cardiovascular diseases by chemokines
- Anti-arthritic, immunomodulatory, and inflammatory regulation by the benzimidazole derivative BMZ-AD: Insights from an FCA-induced rat model
- Immunoassay for pyruvate kinase M1/2 as an Alzheimer’s biomarker in CSF
- The role of HDAC11 in age-related hearing loss: Mechanisms and therapeutic implications
- Evaluation and application analysis of animal models of PIPNP based on data mining
- Therapeutic approaches for liver fibrosis/cirrhosis by targeting pyroptosis
- Fabrication of zinc oxide nanoparticles using Ruellia tuberosa leaf extract induces apoptosis through P53 and STAT3 signalling pathways in prostate cancer cells
- Haplo-hematopoietic stem cell transplantation and immunoradiotherapy for severe aplastic anemia complicated with nasopharyngeal carcinoma: A case report
- Modulation of the KEAP1-NRF2 pathway by Erianin: A novel approach to reduce psoriasiform inflammation and inflammatory signaling
- The expression of epidermal growth factor receptor 2 and its relationship with tumor-infiltrating lymphocytes and clinical pathological features in breast cancer patients
- Innovations in MALDI-TOF Mass Spectrometry: Bridging modern diagnostics and historical insights
- BAP1 complexes with YY1 and RBBP7 and its downstream targets in ccRCC cells
- Hypereosinophilic syndrome with elevated IgG4 and T-cell clonality: A report of two cases
- Electroacupuncture alleviates sciatic nerve injury in sciatica rats by regulating BDNF and NGF levels, myelin sheath degradation, and autophagy
- Polydatin prevents cholesterol gallstone formation by regulating cholesterol metabolism via PPAR-γ signaling
- RNF144A and RNF144B: Important molecules for health
- Analysis of the detection rate and related factors of thyroid nodules in the healthy population
- Artesunate inhibits hepatocellular carcinoma cell migration and invasion through OGA-mediated O-GlcNAcylation of ZEB1
- Endovascular management of post-pancreatectomy hemorrhage caused by a hepatic artery pseudoaneurysm: Case report and review of the literature
- Efficacy and safety of anti-PD-1/PD-L1 antibodies in patients with relapsed refractory diffuse large B-cell lymphoma: A meta-analysis
- SATB2 promotes humeral fracture healing in rats by activating the PI3K/AKT pathway
- Overexpression of the ferroptosis-related gene, NFS1, corresponds to gastric cancer growth and tumor immune infiltration
- Understanding risk factors and prognosis in diabetic foot ulcers
- Atractylenolide I alleviates the experimental allergic response in mice by suppressing TLR4/NF-kB/NLRP3 signalling
- FBXO31 inhibits the stemness characteristics of CD147 (+) melanoma stem cells
- Immune molecule diagnostics in colorectal cancer: CCL2 and CXCL11
- Inhibiting CXCR6 promotes senescence of activated hepatic stellate cells with limited proinflammatory SASP to attenuate hepatic fibrosis
- Cadmium toxicity, health risk and its remediation using low-cost biochar adsorbents
- Pulmonary cryptococcosis with headache as the first presentation: A case report
- Solitary pulmonary metastasis with cystic airspaces in colon cancer: A rare case report
- RUNX1 promotes denervation-induced muscle atrophy by activating the JUNB/NF-κB pathway and driving M1 macrophage polarization
- Morphometric analysis and immunobiological investigation of Indigofera oblongifolia on the infected lung with Plasmodium chabaudi
- The NuA4/TIP60 histone-modifying complex and Hr78 modulate the Lobe2 mutant eye phenotype
- Experimental study on salmon demineralized bone matrix loaded with recombinant human bone morphogenetic protein-2: In vitro and in vivo study
- A case of IgA nephropathy treated with a combination of telitacicept and half-dose glucocorticoids
- Analgesic and toxicological evaluation of cannabidiol-rich Moroccan Cannabis sativa L. (Khardala variety) extract: Evidence from an in vivo and in silico study
- Wound healing and signaling pathways
- Combination of immunotherapy and whole-brain radiotherapy on prognosis of patients with multiple brain metastases: A retrospective cohort study
- To explore the relationship between endometrial hyperemia and polycystic ovary syndrome
- Research progress on the impact of curcumin on immune responses in breast cancer
- Biogenic Cu/Ni nanotherapeutics from Descurainia sophia (L.) Webb ex Prantl seeds for the treatment of lung cancer
- Dapagliflozin attenuates atrial fibrosis via the HMGB1/RAGE pathway in atrial fibrillation rats
- Glycitein alleviates inflammation and apoptosis in keratinocytes via ROS-associated PI3K–Akt signalling pathway
- ADH5 inhibits proliferation but promotes EMT in non-small cell lung cancer cell through activating Smad2/Smad3
- Apoptotic efficacies of AgNPs formulated by Syzygium aromaticum leaf extract on 32D-FLT3-ITD human leukemia cell line with PI3K/AKT/mTOR signaling pathway
- Novel cuproptosis-related genes C1QBP and PFKP identified as prognostic and therapeutic targets in lung adenocarcinoma
- Bee venom promotes exosome secretion and alters miRNA cargo in T cells
- Treatment of pure red cell aplasia in a chronic kidney disease patient with roxadustat: A case report
- Comparative bioinformatics analysis of the Wnt pathway in breast cancer: Selection of novel biomarker panels associated with ER status
- Kynurenine facilitates renal cell carcinoma progression by suppressing M2 macrophage pyroptosis through inhibition of CASP1 cleavage
- RFX5 promotes the growth, motility, and inhibits apoptosis of gastric adenocarcinoma cells through the SIRT1/AMPK axis
- ALKBH5 exacerbates early cardiac damage after radiotherapy for breast cancer via m6A demethylation of TLR4
- Phytochemicals of Roman chamomile: Antioxidant, anti-aging, and whitening activities of distillation residues
- Circadian gene Cry1 inhibits the tumorigenicity of hepatocellular carcinoma by the BAX/BCL2-mediated apoptosis pathway
- The TNFR-RIPK1/RIPK3 signalling pathway mediates the effect of lanthanum on necroptosis of nerve cells
- Longitudinal monitoring of autoantibody dynamics in patients with early-stage non-small-cell lung cancer undergoing surgery
- The potential role of rutin, a flavonoid, in the management of cancer through modulation of cell signaling pathways
- Construction of pectinase gene engineering microbe and its application in tobacco sheets
- Construction of a microbial abundance prognostic scoring model based on intratumoral microbial data for predicting the prognosis of lung squamous cell carcinoma
- Sepsis complicated by haemophagocytic lymphohistiocytosis triggered by methicillin-resistant Staphylococcus aureus and human herpesvirus 8 in an immunocompromised elderly patient: A case report
- Sarcopenia in liver transplantation: A comprehensive bibliometric study of current research trends and future directions
- Advances in cancer immunotherapy and future directions in personalized medicine
- Can coronavirus disease 2019 affect male fertility or cause spontaneous abortion? A two-sample Mendelian randomization analysis
- Heat stroke associated with novel leukaemia inhibitory factor receptor gene variant in a Chinese infant
- PSME2 exacerbates ulcerative colitis by disrupting intestinal barrier function and promoting autophagy-dependent inflammation
- Hyperosmolar hyperglycemic state with severe hypernatremia coexisting with central diabetes insipidus: A case report and literature review
- Efficacy and mechanism of escin in improving the tissue microenvironment of blood vessel walls via anti-inflammatory and anticoagulant effects: Implications for clinical practice
- Merkel cell carcinoma: Clinicopathological analysis of three patients and literature review
- Genetic variants in VWF exon 26 and their implications for type 1 Von Willebrand disease in a Saudi Arabian population
- Lipoxin A4 improves myocardial ischemia/reperfusion injury through the Notch1-Nrf2 signaling pathway
- High levels of EPHB2 expression predict a poor prognosis and promote tumor progression in endometrial cancer
- Knockdown of SHP-2 delays renal tubular epithelial cell injury in diabetic nephropathy by inhibiting NLRP3 inflammasome-mediated pyroptosis
- Exploring the toxicity mechanisms and detoxification methods of Rhizoma Paridis
- Concomitant gastric carcinoma and primary hepatic angiosarcoma in a patient: A case report
- Ecology and Environmental Science
- Optimization and comparative study of Bacillus consortia for cellulolytic potential and cellulase enzyme activity
- The complete mitochondrial genome analysis of Haemaphysalis hystricis Supino, 1897 (Ixodida: Ixodidae) and its phylogenetic implications
- Epidemiological characteristics and risk factors analysis of multidrug-resistant tuberculosis among tuberculosis population in Huzhou City, Eastern China
- Indices of human impacts on landscapes: How do they reflect the proportions of natural habitats?
- Genetic analysis of the Siberian flying squirrel population in the northern Changbai Mountains, Northeast China: Insights into population status and conservation
- Diversity and environmental drivers of Suillus communities in Pinus sylvestris var. mongolica forests of Inner Mongolia
- Global assessment of the fate of nitrogen deposition in forest ecosystems: Insights from 15N tracer studies
- Fungal and bacterial pathogenic co-infections mainly lead to the assembly of microbial community in tobacco stems
- Influencing of coal industry related airborne particulate matter on ocular surface tear film injury and inflammatory factor expression in Sprague-Dawley rats
- Temperature-dependent development, predation, and life table of Sphaerophoria macrogaster (Thomson) (Diptera: Syrphidae) feeding on Myzus persicae (Sulzer) (Homoptera: Aphididae)
- Eleonora’s falcon trophic interactions with insects within its breeding range: A systematic review
- Agriculture
- Integrated analysis of transcriptome, sRNAome, and degradome involved in the drought-response of maize Zhengdan958
- Variation in flower frost tolerance among seven apple cultivars and transcriptome response patterns in two contrastingly frost-tolerant selected cultivars
- Heritability of durable resistance to stripe rust in bread wheat (Triticum aestivum L.)
- Molecular mechanism of follicular development in laying hens based on the regulation of water metabolism
- Animal Science
- Effect of sex ratio on the life history traits of an important invasive species, Spodoptera frugiperda
- Plant Sciences
- Hairpin in a haystack: In silico identification and characterization of plant-conserved microRNA in Rafflesiaceae
- Widely targeted metabolomics of different tissues in Rubus corchorifolius
- The complete chloroplast genome of Gerbera piloselloides (L.) Cass., 1820 (Carduoideae, Asteraceae) and its phylogenetic analysis
- Field trial to correlate mineral solubilization activity of Pseudomonas aeruginosa and biochemical content of groundnut plants
- Correlation analysis between semen routine parameters and sperm DNA fragmentation index in patients with semen non-liquefaction: A retrospective study
- Plasticity of the anatomical traits of Rhododendron L. (Ericaceae) leaves and its implications in adaptation to the plateau environment
- Effects of Piriformospora indica and arbuscular mycorrhizal fungus on growth and physiology of Moringa oleifera under low-temperature stress
- Effects of different sources of potassium fertiliser on yield, fruit quality and nutrient absorption in “Harward” kiwifruit (Actinidia deliciosa)
- Comparative efficiency and residue levels of spraying programs against powdery mildew in grape varieties
- The DREB7 transcription factor enhances salt tolerance in soybean plants under salt stress
- Using plant electrical signals of water hyacinth (Eichhornia crassipes) for water pollution monitoring
- Food Science
- Phytochemical analysis of Stachys iva: Discovering the optimal extract conditions and its bioactive compounds
- Review on role of honey in disease prevention and treatment through modulation of biological activities
- Computational analysis of polymorphic residues in maltose and maltotriose transporters of a wild Saccharomyces cerevisiae strain
- Optimization of phenolic compound extraction from Tunisian squash by-products: A sustainable approach for antioxidant and antibacterial applications
- Liupao tea aqueous extract alleviates dextran sulfate sodium-induced ulcerative colitis in rats by modulating the gut microbiota
- Toxicological qualities and detoxification trends of fruit by-products for valorization: A review
- Polyphenolic spectrum of cornelian cherry fruits and their health-promoting effect
- Optimizing the encapsulation of the refined extract of squash peels for functional food applications: A sustainable approach to reduce food waste
- Advancements in curcuminoid formulations: An update on bioavailability enhancement strategies curcuminoid bioavailability and formulations
- Impact of saline sprouting on antioxidant properties and bioactive compounds in chia seeds
- The dilemma of food genetics and improvement
- Bioengineering and Biotechnology
- Impact of hyaluronic acid-modified hafnium metalorganic frameworks containing rhynchophylline on Alzheimer’s disease
- Emerging patterns in nanoparticle-based therapeutic approaches for rheumatoid arthritis: A comprehensive bibliometric and visual analysis spanning two decades
- Application of CRISPR/Cas gene editing for infectious disease control in poultry
- Preparation of hafnium nitride-coated titanium implants by magnetron sputtering technology and evaluation of their antibacterial properties and biocompatibility
- Preparation and characterization of lemongrass oil nanoemulsion: Antimicrobial, antibiofilm, antioxidant, and anticancer activities
- Corrigendum
- Corrigendum to “Utilization of convolutional neural networks to analyze microscopic images for high-throughput screening of mesenchymal stem cells”
- Corrigendum to “Effects of Ire1 gene on virulence and pathogenicity of Candida albicans”
- Retraction
- Retraction of “Down-regulation of miR-539 indicates poor prognosis in patients with pancreatic cancer”
Articles in the same Issue
- Biomedical Sciences
- Mechanism of triptolide regulating proliferation and apoptosis of hepatoma cells by inhibiting JAK/STAT pathway
- Maslinic acid improves mitochondrial function and inhibits oxidative stress and autophagy in human gastric smooth muscle cells
- Comparative analysis of inflammatory biomarkers for the diagnosis of neonatal sepsis: IL-6, IL-8, SAA, CRP, and PCT
- Post-pandemic insights on COVID-19 and premature ovarian insufficiency
- Proteome differences of dental stem cells between permanent and deciduous teeth by data-independent acquisition proteomics
- Optimizing a modified cetyltrimethylammonium bromide protocol for fungal DNA extraction: Insights from multilocus gene amplification
- Preliminary analysis of the role of small hepatitis B surface proteins mutations in the pathogenesis of occult hepatitis B infection via the endoplasmic reticulum stress-induced UPR-ERAD pathway
- Efficacy of alginate-coated gold nanoparticles against antibiotics-resistant Staphylococcus and Streptococcus pathogens of acne origins
- Battling COVID-19 leveraging nanobiotechnology: Gold and silver nanoparticle–B-escin conjugates as SARS-CoV-2 inhibitors
- Neurodegenerative diseases and neuroinflammation-induced apoptosis
- Impact of fracture fixation surgery on cognitive function and the gut microbiota in mice with a history of stroke
- COLEC10: A potential tumor suppressor and prognostic biomarker in hepatocellular carcinoma through modulation of EMT and PI3K-AKT pathways
- High-temperature requirement serine protease A2 inhibitor UCF-101 ameliorates damaged neurons in traumatic brain-injured rats by the AMPK/NF-κB pathway
- SIK1 inhibits IL-1β-stimulated cartilage apoptosis and inflammation in vitro through the CRTC2/CREB1 signaling
- Rutin–chitooligosaccharide complex: Comprehensive evaluation of its anti-inflammatory and analgesic properties in vitro and in vivo
- Knockdown of Aurora kinase B alleviates high glucose-triggered trophoblast cells damage and inflammation during gestational diabetes
- Calcium-sensing receptors promoted Homer1 expression and osteogenic differentiation in bone marrow mesenchymal stem cells
- ABI3BP can inhibit the proliferation, invasion, and epithelial–mesenchymal transition of non-small-cell lung cancer cells
- Changes in blood glucose and metabolism in hyperuricemia mice
- Rapid detection of the GJB2 c.235delC mutation based on CRISPR-Cas13a combined with lateral flow dipstick
- IL-11 promotes Ang II-induced autophagy inhibition and mitochondrial dysfunction in atrial fibroblasts
- Short-chain fatty acid attenuates intestinal inflammation by regulation of gut microbial composition in antibiotic-associated diarrhea
- Application of metagenomic next-generation sequencing in the diagnosis of pathogens in patients with diabetes complicated by community-acquired pneumonia
- NAT10 promotes radiotherapy resistance in non-small cell lung cancer by regulating KPNB1-mediated PD-L1 nuclear translocation
- Phytol-mixed micelles alleviate dexamethasone-induced osteoporosis in zebrafish: Activation of the MMP3–OPN–MAPK pathway-mediating bone remodeling
- Association between TGF-β1 and β-catenin expression in the vaginal wall of patients with pelvic organ prolapse
- Primary pleomorphic liposarcoma involving bilateral ovaries: Case report and literature review
- Effects of de novo donor-specific Class I and II antibodies on graft outcomes after liver transplantation: A pilot cohort study
- Sleep architecture in Alzheimer’s disease continuum: The deep sleep question
- Ephedra fragilis plant extract: A groundbreaking corrosion inhibitor for mild steel in acidic environments – electrochemical, EDX, DFT, and Monte Carlo studies
- Langerhans cell histiocytosis in an adult patient with upper jaw and pulmonary involvement: A case report
- Inhibition of mast cell activation by Jaranol-targeted Pirin ameliorates allergic responses in mouse allergic rhinitis
- Aeromonas veronii-induced septic arthritis of the hip in a child with acute lymphoblastic leukemia
- Clusterin activates the heat shock response via the PI3K/Akt pathway to protect cardiomyocytes from high-temperature-induced apoptosis
- Research progress on fecal microbiota transplantation in tumor prevention and treatment
- Low-pressure exposure influences the development of HAPE
- Stigmasterol alleviates endplate chondrocyte degeneration through inducing mitophagy by enhancing PINK1 mRNA acetylation via the ESR1/NAT10 axis
- AKAP12, mediated by transcription factor 21, inhibits cell proliferation, metastasis, and glycolysis in lung squamous cell carcinoma
- Association between PAX9 or MSX1 gene polymorphism and tooth agenesis risk: A meta-analysis
- A case of bloodstream infection caused by Neisseria gonorrhoeae
- Case of nasopharyngeal tuberculosis complicated with cervical lymph node and pulmonary tuberculosis
- p-Cymene inhibits pro-fibrotic and inflammatory mediators to prevent hepatic dysfunction
- GFPT2 promotes paclitaxel resistance in epithelial ovarian cancer cells via activating NF-κB signaling pathway
- Transfer RNA-derived fragment tRF-36 modulates varicose vein progression via human vascular smooth muscle cell Notch signaling
- RTA-408 attenuates the hepatic ischemia reperfusion injury in mice possibly by activating the Nrf2/HO-1 signaling pathway
- Decreased serum TIMP4 levels in patients with rheumatoid arthritis
- Sirt1 protects lupus nephritis by inhibiting the NLRP3 signaling pathway in human glomerular mesangial cells
- Sodium butyrate aids brain injury repair in neonatal rats
- Interaction of MTHFR polymorphism with PAX1 methylation in cervical cancer
- Convallatoxin inhibits proliferation and angiogenesis of glioma cells via regulating JAK/STAT3 pathway
- The effect of the PKR inhibitor, 2-aminopurine, on the replication of influenza A virus, and segment 8 mRNA splicing
- Effects of Ire1 gene on virulence and pathogenicity of Candida albicans
- Small cell lung cancer with small intestinal metastasis: Case report and literature review
- GRB14: A prognostic biomarker driving tumor progression in gastric cancer through the PI3K/AKT signaling pathway by interacting with COBLL1
- 15-Lipoxygenase-2 deficiency induces foam cell formation that can be restored by salidroside through the inhibition of arachidonic acid effects
- FTO alleviated the diabetic nephropathy progression by regulating the N6-methyladenosine levels of DACT1
- Clinical relevance of inflammatory markers in the evaluation of severity of ulcerative colitis: A retrospective study
- Zinc valproic acid complex promotes osteoblast differentiation and exhibits anti-osteoporotic potential
- Primary pulmonary synovial sarcoma in the bronchial cavity: A case report
- Metagenomic next-generation sequencing of alveolar lavage fluid improves the detection of pulmonary infection
- Uterine tumor resembling ovarian sex cord tumor with extensive rhabdoid differentiation: A case report
- Genomic analysis of a novel ST11(PR34365) Clostridioides difficile strain isolated from the human fecal of a CDI patient in Guizhou, China
- Effects of tiered cardiac rehabilitation on CRP, TNF-α, and physical endurance in older adults with coronary heart disease
- Changes in T-lymphocyte subpopulations in patients with colorectal cancer before and after acupoint catgut embedding acupuncture observation
- Modulating the tumor microenvironment: The role of traditional Chinese medicine in improving lung cancer treatment
- Alterations of metabolites related to microbiota–gut–brain axis in plasma of colon cancer, esophageal cancer, stomach cancer, and lung cancer patients
- Research on individualized drug sensitivity detection technology based on bio-3D printing technology for precision treatment of gastrointestinal stromal tumors
- CEBPB promotes ulcerative colitis-associated colorectal cancer by stimulating tumor growth and activating the NF-κB/STAT3 signaling pathway
- Oncolytic bacteria: A revolutionary approach to cancer therapy
- A de novo meningioma with rapid growth: A possible malignancy imposter?
- Diagnosis of secondary tuberculosis infection in an asymptomatic elderly with cancer using next-generation sequencing: Case report
- Hesperidin and its zinc(ii) complex enhance osteoblast differentiation and bone formation: In vitro and in vivo evaluations
- Research progress on the regulation of autophagy in cardiovascular diseases by chemokines
- Anti-arthritic, immunomodulatory, and inflammatory regulation by the benzimidazole derivative BMZ-AD: Insights from an FCA-induced rat model
- Immunoassay for pyruvate kinase M1/2 as an Alzheimer’s biomarker in CSF
- The role of HDAC11 in age-related hearing loss: Mechanisms and therapeutic implications
- Evaluation and application analysis of animal models of PIPNP based on data mining
- Therapeutic approaches for liver fibrosis/cirrhosis by targeting pyroptosis
- Fabrication of zinc oxide nanoparticles using Ruellia tuberosa leaf extract induces apoptosis through P53 and STAT3 signalling pathways in prostate cancer cells
- Haplo-hematopoietic stem cell transplantation and immunoradiotherapy for severe aplastic anemia complicated with nasopharyngeal carcinoma: A case report
- Modulation of the KEAP1-NRF2 pathway by Erianin: A novel approach to reduce psoriasiform inflammation and inflammatory signaling
- The expression of epidermal growth factor receptor 2 and its relationship with tumor-infiltrating lymphocytes and clinical pathological features in breast cancer patients
- Innovations in MALDI-TOF Mass Spectrometry: Bridging modern diagnostics and historical insights
- BAP1 complexes with YY1 and RBBP7 and its downstream targets in ccRCC cells
- Hypereosinophilic syndrome with elevated IgG4 and T-cell clonality: A report of two cases
- Electroacupuncture alleviates sciatic nerve injury in sciatica rats by regulating BDNF and NGF levels, myelin sheath degradation, and autophagy
- Polydatin prevents cholesterol gallstone formation by regulating cholesterol metabolism via PPAR-γ signaling
- RNF144A and RNF144B: Important molecules for health
- Analysis of the detection rate and related factors of thyroid nodules in the healthy population
- Artesunate inhibits hepatocellular carcinoma cell migration and invasion through OGA-mediated O-GlcNAcylation of ZEB1
- Endovascular management of post-pancreatectomy hemorrhage caused by a hepatic artery pseudoaneurysm: Case report and review of the literature
- Efficacy and safety of anti-PD-1/PD-L1 antibodies in patients with relapsed refractory diffuse large B-cell lymphoma: A meta-analysis
- SATB2 promotes humeral fracture healing in rats by activating the PI3K/AKT pathway
- Overexpression of the ferroptosis-related gene, NFS1, corresponds to gastric cancer growth and tumor immune infiltration
- Understanding risk factors and prognosis in diabetic foot ulcers
- Atractylenolide I alleviates the experimental allergic response in mice by suppressing TLR4/NF-kB/NLRP3 signalling
- FBXO31 inhibits the stemness characteristics of CD147 (+) melanoma stem cells
- Immune molecule diagnostics in colorectal cancer: CCL2 and CXCL11
- Inhibiting CXCR6 promotes senescence of activated hepatic stellate cells with limited proinflammatory SASP to attenuate hepatic fibrosis
- Cadmium toxicity, health risk and its remediation using low-cost biochar adsorbents
- Pulmonary cryptococcosis with headache as the first presentation: A case report
- Solitary pulmonary metastasis with cystic airspaces in colon cancer: A rare case report
- RUNX1 promotes denervation-induced muscle atrophy by activating the JUNB/NF-κB pathway and driving M1 macrophage polarization
- Morphometric analysis and immunobiological investigation of Indigofera oblongifolia on the infected lung with Plasmodium chabaudi
- The NuA4/TIP60 histone-modifying complex and Hr78 modulate the Lobe2 mutant eye phenotype
- Experimental study on salmon demineralized bone matrix loaded with recombinant human bone morphogenetic protein-2: In vitro and in vivo study
- A case of IgA nephropathy treated with a combination of telitacicept and half-dose glucocorticoids
- Analgesic and toxicological evaluation of cannabidiol-rich Moroccan Cannabis sativa L. (Khardala variety) extract: Evidence from an in vivo and in silico study
- Wound healing and signaling pathways
- Combination of immunotherapy and whole-brain radiotherapy on prognosis of patients with multiple brain metastases: A retrospective cohort study
- To explore the relationship between endometrial hyperemia and polycystic ovary syndrome
- Research progress on the impact of curcumin on immune responses in breast cancer
- Biogenic Cu/Ni nanotherapeutics from Descurainia sophia (L.) Webb ex Prantl seeds for the treatment of lung cancer
- Dapagliflozin attenuates atrial fibrosis via the HMGB1/RAGE pathway in atrial fibrillation rats
- Glycitein alleviates inflammation and apoptosis in keratinocytes via ROS-associated PI3K–Akt signalling pathway
- ADH5 inhibits proliferation but promotes EMT in non-small cell lung cancer cell through activating Smad2/Smad3
- Apoptotic efficacies of AgNPs formulated by Syzygium aromaticum leaf extract on 32D-FLT3-ITD human leukemia cell line with PI3K/AKT/mTOR signaling pathway
- Novel cuproptosis-related genes C1QBP and PFKP identified as prognostic and therapeutic targets in lung adenocarcinoma
- Bee venom promotes exosome secretion and alters miRNA cargo in T cells
- Treatment of pure red cell aplasia in a chronic kidney disease patient with roxadustat: A case report
- Comparative bioinformatics analysis of the Wnt pathway in breast cancer: Selection of novel biomarker panels associated with ER status
- Kynurenine facilitates renal cell carcinoma progression by suppressing M2 macrophage pyroptosis through inhibition of CASP1 cleavage
- RFX5 promotes the growth, motility, and inhibits apoptosis of gastric adenocarcinoma cells through the SIRT1/AMPK axis
- ALKBH5 exacerbates early cardiac damage after radiotherapy for breast cancer via m6A demethylation of TLR4
- Phytochemicals of Roman chamomile: Antioxidant, anti-aging, and whitening activities of distillation residues
- Circadian gene Cry1 inhibits the tumorigenicity of hepatocellular carcinoma by the BAX/BCL2-mediated apoptosis pathway
- The TNFR-RIPK1/RIPK3 signalling pathway mediates the effect of lanthanum on necroptosis of nerve cells
- Longitudinal monitoring of autoantibody dynamics in patients with early-stage non-small-cell lung cancer undergoing surgery
- The potential role of rutin, a flavonoid, in the management of cancer through modulation of cell signaling pathways
- Construction of pectinase gene engineering microbe and its application in tobacco sheets
- Construction of a microbial abundance prognostic scoring model based on intratumoral microbial data for predicting the prognosis of lung squamous cell carcinoma
- Sepsis complicated by haemophagocytic lymphohistiocytosis triggered by methicillin-resistant Staphylococcus aureus and human herpesvirus 8 in an immunocompromised elderly patient: A case report
- Sarcopenia in liver transplantation: A comprehensive bibliometric study of current research trends and future directions
- Advances in cancer immunotherapy and future directions in personalized medicine
- Can coronavirus disease 2019 affect male fertility or cause spontaneous abortion? A two-sample Mendelian randomization analysis
- Heat stroke associated with novel leukaemia inhibitory factor receptor gene variant in a Chinese infant
- PSME2 exacerbates ulcerative colitis by disrupting intestinal barrier function and promoting autophagy-dependent inflammation
- Hyperosmolar hyperglycemic state with severe hypernatremia coexisting with central diabetes insipidus: A case report and literature review
- Efficacy and mechanism of escin in improving the tissue microenvironment of blood vessel walls via anti-inflammatory and anticoagulant effects: Implications for clinical practice
- Merkel cell carcinoma: Clinicopathological analysis of three patients and literature review
- Genetic variants in VWF exon 26 and their implications for type 1 Von Willebrand disease in a Saudi Arabian population
- Lipoxin A4 improves myocardial ischemia/reperfusion injury through the Notch1-Nrf2 signaling pathway
- High levels of EPHB2 expression predict a poor prognosis and promote tumor progression in endometrial cancer
- Knockdown of SHP-2 delays renal tubular epithelial cell injury in diabetic nephropathy by inhibiting NLRP3 inflammasome-mediated pyroptosis
- Exploring the toxicity mechanisms and detoxification methods of Rhizoma Paridis
- Concomitant gastric carcinoma and primary hepatic angiosarcoma in a patient: A case report
- Ecology and Environmental Science
- Optimization and comparative study of Bacillus consortia for cellulolytic potential and cellulase enzyme activity
- The complete mitochondrial genome analysis of Haemaphysalis hystricis Supino, 1897 (Ixodida: Ixodidae) and its phylogenetic implications
- Epidemiological characteristics and risk factors analysis of multidrug-resistant tuberculosis among tuberculosis population in Huzhou City, Eastern China
- Indices of human impacts on landscapes: How do they reflect the proportions of natural habitats?
- Genetic analysis of the Siberian flying squirrel population in the northern Changbai Mountains, Northeast China: Insights into population status and conservation
- Diversity and environmental drivers of Suillus communities in Pinus sylvestris var. mongolica forests of Inner Mongolia
- Global assessment of the fate of nitrogen deposition in forest ecosystems: Insights from 15N tracer studies
- Fungal and bacterial pathogenic co-infections mainly lead to the assembly of microbial community in tobacco stems
- Influencing of coal industry related airborne particulate matter on ocular surface tear film injury and inflammatory factor expression in Sprague-Dawley rats
- Temperature-dependent development, predation, and life table of Sphaerophoria macrogaster (Thomson) (Diptera: Syrphidae) feeding on Myzus persicae (Sulzer) (Homoptera: Aphididae)
- Eleonora’s falcon trophic interactions with insects within its breeding range: A systematic review
- Agriculture
- Integrated analysis of transcriptome, sRNAome, and degradome involved in the drought-response of maize Zhengdan958
- Variation in flower frost tolerance among seven apple cultivars and transcriptome response patterns in two contrastingly frost-tolerant selected cultivars
- Heritability of durable resistance to stripe rust in bread wheat (Triticum aestivum L.)
- Molecular mechanism of follicular development in laying hens based on the regulation of water metabolism
- Animal Science
- Effect of sex ratio on the life history traits of an important invasive species, Spodoptera frugiperda
- Plant Sciences
- Hairpin in a haystack: In silico identification and characterization of plant-conserved microRNA in Rafflesiaceae
- Widely targeted metabolomics of different tissues in Rubus corchorifolius
- The complete chloroplast genome of Gerbera piloselloides (L.) Cass., 1820 (Carduoideae, Asteraceae) and its phylogenetic analysis
- Field trial to correlate mineral solubilization activity of Pseudomonas aeruginosa and biochemical content of groundnut plants
- Correlation analysis between semen routine parameters and sperm DNA fragmentation index in patients with semen non-liquefaction: A retrospective study
- Plasticity of the anatomical traits of Rhododendron L. (Ericaceae) leaves and its implications in adaptation to the plateau environment
- Effects of Piriformospora indica and arbuscular mycorrhizal fungus on growth and physiology of Moringa oleifera under low-temperature stress
- Effects of different sources of potassium fertiliser on yield, fruit quality and nutrient absorption in “Harward” kiwifruit (Actinidia deliciosa)
- Comparative efficiency and residue levels of spraying programs against powdery mildew in grape varieties
- The DREB7 transcription factor enhances salt tolerance in soybean plants under salt stress
- Using plant electrical signals of water hyacinth (Eichhornia crassipes) for water pollution monitoring
- Food Science
- Phytochemical analysis of Stachys iva: Discovering the optimal extract conditions and its bioactive compounds
- Review on role of honey in disease prevention and treatment through modulation of biological activities
- Computational analysis of polymorphic residues in maltose and maltotriose transporters of a wild Saccharomyces cerevisiae strain
- Optimization of phenolic compound extraction from Tunisian squash by-products: A sustainable approach for antioxidant and antibacterial applications
- Liupao tea aqueous extract alleviates dextran sulfate sodium-induced ulcerative colitis in rats by modulating the gut microbiota
- Toxicological qualities and detoxification trends of fruit by-products for valorization: A review
- Polyphenolic spectrum of cornelian cherry fruits and their health-promoting effect
- Optimizing the encapsulation of the refined extract of squash peels for functional food applications: A sustainable approach to reduce food waste
- Advancements in curcuminoid formulations: An update on bioavailability enhancement strategies curcuminoid bioavailability and formulations
- Impact of saline sprouting on antioxidant properties and bioactive compounds in chia seeds
- The dilemma of food genetics and improvement
- Bioengineering and Biotechnology
- Impact of hyaluronic acid-modified hafnium metalorganic frameworks containing rhynchophylline on Alzheimer’s disease
- Emerging patterns in nanoparticle-based therapeutic approaches for rheumatoid arthritis: A comprehensive bibliometric and visual analysis spanning two decades
- Application of CRISPR/Cas gene editing for infectious disease control in poultry
- Preparation of hafnium nitride-coated titanium implants by magnetron sputtering technology and evaluation of their antibacterial properties and biocompatibility
- Preparation and characterization of lemongrass oil nanoemulsion: Antimicrobial, antibiofilm, antioxidant, and anticancer activities
- Corrigendum
- Corrigendum to “Utilization of convolutional neural networks to analyze microscopic images for high-throughput screening of mesenchymal stem cells”
- Corrigendum to “Effects of Ire1 gene on virulence and pathogenicity of Candida albicans”
- Retraction
- Retraction of “Down-regulation of miR-539 indicates poor prognosis in patients with pancreatic cancer”

