Longitudinal monitoring of autoantibody dynamics in patients with early-stage non-small-cell lung cancer undergoing surgery
-
Jinming Miao
Abstract
Lung cancer is one of the most common and deadly malignancies worldwide, underscoring the need for reliable biomarkers that can inform prognosis and guide postoperative surveillance. This prospective study examined longitudinal changes in 10 tumor-associated autoantibodies in 71 patients with early-stage non-small-cell lung cancer (NSCLC) who underwent surgical resection. Blood samples were collected preoperatively and at 3-, 6-, and 12-month post-surgery. Enzyme-linked immunosorbent assays were used to measure serum autoantibodies against p53, MUC1, NY-ESO-1, APE1, PGP9.5, SOX2, GBU4-5, GAGE7, CAGE, and MAGE1. Logistic regression models assessed associations with 1-year recurrence, while Cox proportional hazards models evaluated overall survival. Substantial reductions in p53, GBU4-5, and CAGE autoantibodies correlated with lower recurrence risk and improved 1-year survival, even after false discovery rate adjustment (p < 0.05). NY-ESO-1 showed borderline significance for recurrence, and SOX2 was borderline for survival but did not remain significant after correction. These findings suggest that monitoring dynamic declines in certain autoantibodies (most notably CAGE) may offer clinically meaningful prognostic information following surgical resection. While further validation in larger, independent cohorts is required, our results highlight the potential of serial autoantibody profiling as a noninvasive tool for personalized postoperative management in early-stage NSCLC patients.
1 Introduction
Lung cancer remains the foremost cause of cancer‑related death worldwide, placing a considerable burden on public health [1]. Recent advances in computed tomography screening have increased the detection of early‑stage disease, thereby shifting the overall spectrum of lung‑cancer diagnoses toward earlier stages [2]. Surgical resection – most commonly lobectomy – remains the standard of care for early‑stage non‑small-cell lung cancer (NSCLC) [3]. Emerging evidence suggests that anatomic segmentectomy can deliver oncologic outcomes comparable to lobectomy in appropriately selected patients [4].
Postoperative prognosis now hinges increasingly on advanced surveillance modalities and predictive modeling. Circulating tumor DNA has emerged as a sensitive biomarker for minimal residual disease, enabling early identification of relapse risk [5]. Low-dose computed tomography surveillance protocols further improve recurrence-free and overall survival (OS) compared with conventional CT [6]. Concurrently, machine-learning algorithms are being developed to generate individualized predictions of postoperative life expectancy and complication risk [7,8]. Together, these innovations promise to refine post-surgical management and enhance long-term outcomes for patients undergoing lung-cancer resection.
Tumor‑associated antigens (TAAs) displayed on cancer‑cell surfaces can trigger host immune responses, generating circulating autoantibodies that are now recognized as promising biomarkers for cancer diagnosis. Although no FDA-approved autoantibody test for lung cancer, a commercial test with a seven-autoantibody assay (EarlyCDT-Lung) already exists and has been evaluated in technical-validation studies, nodule-management cohorts, and the large early detection of cancer of the Lung Scotland (ECLS) randomized trial [9,10,11]. A five‑autoantibody panel has been shown to outperform conventional markers such as CA 19‑9 in pancreatic ductal adenocarcinoma [12]. Likewise, multiplex panels targeting several TAAs markedly enhance early lung‑cancer detection, with certain combinations achieving up to 65% sensitivity while maintaining 100% specificity [13]. A multicenter Chinese study developed a nine-marker “CN9” autoantibody panel that improved nodule-malignancy discrimination when added to Mayo or Brock risk models [14]. More recently, Guo et al. reported that a seven-autoantibody signature, combined with machine-learning, achieved an AUC ≈ 0.93 for ground-glass nodular adenocarcinoma (≤3 cm) [15].
Autoantibodies have also emerged as promising biomarkers for disease progression, recurrence, and survival across various cancer types. In gastrointestinal malignancies, autoantibodies against p53 and NY-ESO-1 track with tumor progression – particularly in esophageal squamous-cell carcinoma and gastric cancer – underscoring their prognostic potential [16]. In gastric cancer, serum NY-ESO-1 and p53 autoantibodies are associated with postoperative recurrence, with NY-ESO-1 seropositivity at 3 and 12 months after surgery independently predicting shorter recurrence-free survival [17]. Elevated titers of multiple autoantibodies likewise correlate with prognosis in lung cancer [18,19]. Although a recent study documented postoperative shifts in the autoantibody repertoire of lung-cancer patients [20], the influence of these changes on long-term outcomes after resection remains largely unexplored.
This study will characterize the peri‑operative kinetics of a ten‑autoantibody panel – p53, MUC1, NY‑ESO‑1, APE1, PGP9.5, SOX2, GBU4‑5, GAGE7, CAGE, and MAGE1 – in patients undergoing lung‑cancer resection. By mapping postoperative trajectories and correlating them with recurrence, metastasis, and survival, we aim to elucidate each autoantibody’s prognostic value. If validated, such profiling could be incorporated into routine follow‑up as a non‑invasive, personalized surveillance tool to inform adjuvant‑therapy decisions and improve long‑term outcomes.
2 Materials and methods
This study was a prospective observational cohort study conducted at Dandong No. 1 Hospital from August 2019 to December 2023. Patients with confirmed primary lung cancer scheduled for surgical resection were enrolled based on predefined inclusion and exclusion criteria. All patients were treated with an identical cisplatin + pemetrexed regimen; no radiotherapy or immunotherapy was administered during the first postoperative year. Eligible participants were adults (≥18 years) with histologically confirmed primary NSCLC who were considered suitable for curative surgical resection. Patients were excluded if they had a prior malignancy, had received neoadjuvant therapy, or had autoimmune disorders or other conditions known to alter autoantibody levels (Figure 1).
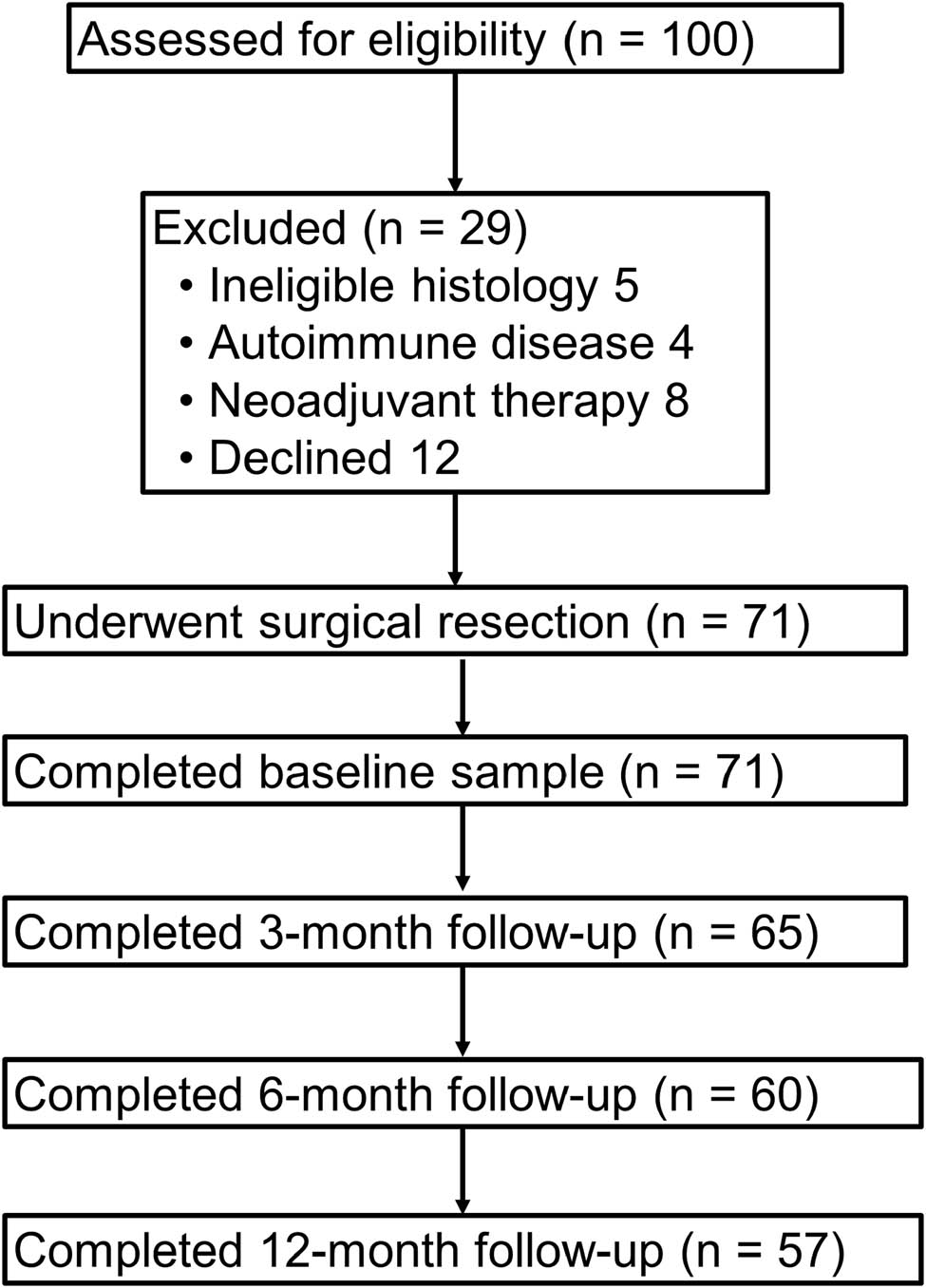
Flowchart of participant selection.
2.1 Sample size considerations
No formal statistical power calculation was performed for this exploratory study. We aimed to enroll consecutive, eligible patients until we achieved a sufficiently sized cohort (n ≥ 70) that would permit preliminary subgroup and regression analyses. This number was guided by practical feasibility and prior literature on autoantibody biomarker studies in early-stage lung cancer, which often involve similar sample sizes.
-
Informed consent: Informed consent has been obtained from all individuals included in this study.
-
Ethical approval: The research related to human use has been complied with all the relevant national regulations, institutional policies, and in accordance with the tenets of the Helsinki Declaration, and has been approved by the Institutional Review Board of Dandong First Hospital (DDSDYYY-2022-08-20-01).
2.2 Performance status
Prior to surgery, each patient’s functional capacity was assessed using the ECOG Performance Status scale. Patients with ECOG PS 0–2 were considered suitable candidates for curative-intent surgical resection, in line with institutional guidelines. Consequently, all 71 enrolled patients had ECOG PS ≤2 at baseline.
2.3 Sample collection and laboratory measurements
2.3.1 Time points
Patients underwent scheduled blood draws at four time points: baseline (pre-surgery), 3, 6, and 12 months post-surgery. These time points were selected to capture the perioperative immune response and its evolution over time.
2.3.2 Blood sample processing
Blood samples were collected into vacutainer tubes and allowed to clot at room temperature for 30 min. Serum was separated by centrifugation at 3,000 rpm for 10 min and immediately aliquoted into cryogenic vials. All serum samples were stored at −80°C until analysis.
2.3.3 Autoantibody-panel selection rationale
The ten TAAs assayed in this study – p53, MUC1, NY-ESO-1, APE1, PGP9.5, SOX2, GBU4-5, GAGE7, CAGE, and MAGE1 – were chosen a priori using three complementary criteria: (i) reproducible over-expression or mutation in NSCLC tissue together with seropositivity ≥20% in at least one independent cohort [13,21,22]; (ii) mechanistic representation of key oncogenic processes – genomic instability/p53, aberrant mucin glycosylation/MUC1, cancer-testis antigenicity/NY-ESO-1 and MAGE1, DNA-repair dysregulation/APE1, neuronal-protein re-expression/PGP9.5 and GAGE7, developmental transcription factors/SOX2, and stress-induced chaperone-like proteins/GBU4-5 and CAGE [13]; and (iii) prior evidence that circulating autoantibodies to the antigen aid early detection or predict postoperative recurrence or survival in at least two external studies [13,19,23]. Limiting the panel to these ten well-validated TAAs balanced biological diversity with assay practicality and avoided redundancy while excluding markers such as HER2, survivin, and ENO1, whose published seroprevalence in early-stage NSCLC is <10% or whose longitudinal prognostic performance is inconsistent [22,24].
2.3.4 Autoantibody assays
Autoantibody levels for P53, MUC1, NY-ESO-1, APE1, PGP9.5, SOX2, GBU4-5, GAGE7, CAGE, and MAGE1 were measured in duplicate using indirect enzyme-linked immunosorbent assays (ELISA). Purified human recombinant proteins (TP53, MUC1, NY-ESO-1, APE1, PGP9.5, SOX2, GBU4-5, GAGE7, CAGE, and MAGE1) were dissolved to 0.25 µg/µL. Each protein, diluted in coating buffer (50 mM sodium carbonate/bicarbonate, pH 9.6), was added at 100 µL per well to 96-well plates and incubated overnight at 4°C. Human IgG (#I4506, Sigma-Aldrich) was diluted (300–0 ng/mL) to create standard curves. After blocking with 2% BSA overnight at 4°C, plates were washed three times with PBST (PBS + 0.05% Tween 20). Serum samples (diluted 1:100) were added (100 µL/well) and incubated at 37°C for 1 h. Following five washes, 100 µL of Rec-Protein A-HRP (Cat#101123, Invitrogen, 1:10,000 in 1% BSA) was added and incubated at 37°C for 1 h. After another five washes, tumor mutational burden substrate was added, and the reaction was stopped with 2 M H2SO4. Optical density was read at 450 nm, and autoantibody concentrations were calculated from the IgG standard curve. Positive and negative controls for each tumor-associated autoantibody were included on each plate for quality control.
We estimated assay sensitivity (limit of detection) by testing decreasing concentrations of human IgG reference standard. For each autoantibody, both high-positive and low-positive controls were analyzed in duplicate within the same plate and across different plates. The average intra-assay coefficient of variation (CV) ranged from 5 to 8%, and the inter-assay CV ranged from 7 to 10% across all markers, meeting established quality control standards for clinical research ELISAs. Positive, negative, and blank (no-antigen) controls were included on each 96-well plate.
3 Clinical assessments and follow-up
3.1 Outcome measures
Recurrence: It is defined as radiological or histopathological evidence of new tumor growth at the surgical bed or within the ipsilateral lung. Surveillance CT or PET‑CT scans were obtained at protocol‑specified intervals, and suspicious lesions were confirmed histologically whenever feasible.
Metastasis: Diagnosed when cross‑sectional imaging (CT, MRI, or PET‑CT) and clinical assessment demonstrate tumor deposits at distant sites. Follow‑up evaluations were performed every 3 months during the first postoperative year and subsequently at routine clinic visits.
Survival: OS was the interval from the date of surgery to death from any cause; disease‑specific survival was the interval from surgery to death attributable to lung cancer. Vital status was ascertained through electronic medical records and telephone follow‑up.
3.2 Data collection
Demographic, clinical, and histopathologic variables – including age, sex, smoking history, tumor stage, and histologic subtype – were abstracted from the electronic medical record. Follow‑up information (imaging reports, clinical notes, and laboratory results) was prospectively documented at scheduled postoperative visits. All data were entered into a secure, de‑identified database to ensure patient confidentiality.
3.3 Statistical analysis
Descriptive statistics summarized patient demographics, baseline clinical features, and autoantibody concentrations. Continuous variables are reported as means ± standard deviations, whereas categorical variables are expressed as counts and percentages. Pearson correlation coefficients were calculated to explore associations between autoantibody levels and clinical outcomes, including recurrence and metastasis. Univariable and multivariable logistic regression models were constructed to identify autoantibodies independently associated with adverse events – recurrence, metastasis, and OS – while adjusting for age, sex, and tumor stage. Statistical significance was set at P < 0.05.
4 Results
4.1 Demographic and baseline autoantibody profiles in lung cancer patients
Table 1 summarizes the demographic features and baseline autoantibody profiles of the 71 patients who underwent lung‑cancer resection. The cohort’s mean age was 61.7 ± 9.9 years, and women outnumbered men (60.6 vs 39.4%). Mean body‑mass index was 22.4 kg m−2. Baseline serum concentrations for each of the ten autoantibodies are also listed.
Demographic characteristics and baseline autoantibody levels
| Characteristic | Value |
|---|---|
| Age (years), mean ± SD | 61.7 ± 9.9 |
| Sex | |
| Male, n (%) | 28 (39.4%) |
| Female, n (%) | 43 (60.6%) |
| Body Mass Index, mean ± SD | 22.4 ± 3.2 |
| Smoking Status | |
| Current/Ex-smoker, n (%) | 14 (19.7%) |
| Never, n (%) | 57 (80.3%) |
| Tumor Stage, n (%) | |
| Stage I | 32 (45.1%) |
| Stage II | 39 (54.9%) |
| Histology, n (%) | |
| Adenocarcinoma | 69 (97.2%) |
| Squamous cell carcinoma | 1 (1.4%) |
| Adenosquamous carcinoma | 1 (1.4%) |
| Comorbidities | |
| Hypertension, n (%) | 18 (25.3%) |
| Diabetes Mellitus, n (%) | 12 (16.9%) |
| Autoantibody Baseline Levels (U/mL), mean ± SD | |
| P53 | 18.5 ± 5.2 |
| MUC1 | 22.1 ± 4.8 |
| NY-ESO-1 | 12.6 ± 3.5 |
| APE1 | 14.9 ± 4.2 |
| PGP9.5 | 16.3 ± 3.9 |
| SOX2 | 13.4 ± 4.1 |
| GBU4-5 | 18.9 ± 3.3 |
| GAGE7 | 11.5 ± 3.2 |
| CAGE | 14.3 ± 3.8 |
| MAGE1 | 17.6 ± 4.9 |
Most participants were never‑smokers (57/71, 80.3%), while 14 (19.7%) were current or former smokers. At diagnosis, 32 patients (45.1%) had stage I disease and 39 (54.9%) had stage II. Adenocarcinoma was overwhelmingly predominant (69/71, 97.2%); squamous‑cell carcinoma and adenosquamous carcinoma each accounted for one case (1.4% per subtype).
Baseline serum autoantibody concentrations (mean ± SD, U mL−1) were: P53 (18.5 ± 5.2), MUC1 (22.1 ± 4.8), NY-ESO-1 (12.6 ± 3.5), APE1 (14.9 ± 4.2), PGP9.5 (16.3 ± 3.9), SOX2 (13.4 ± 4.1), GBU4-5 (18.9 ± 3.3), GAGE7 (11.5 ± 3.2), CAGE (14.3 ± 3.8), and MAGE1 (17.6 ± 4.9) (Table 1).
4.2 Dynamics of autoantibody responses post-lung cancer surgery
Table 2 depicts serial autoantibody kinetics from baseline through 3, 6, and 12 months after resection. p53 titers rose modestly at 3 months, then declined sharply at 6 months and continued to fall at 12 months. A similar “early‑rise, late‑fall” pattern was evident for SOX2, MUC1, and MAGE1. NY‑ESO‑1 reached a more subdued peak at 3 months before tapering gradually over subsequent visits. Collectively, these trajectories underscore a dynamic postoperative immune landscape, suggesting that shifts in tumor micro‑environment or host immune surveillance evolve over the first postoperative year.
Autoantibody level changes over time
| Autoantibody | Baseline | 3 months | p-value vs baseline | 6 months | p-value vs baseline | 12 months | p-value vs baseline |
|---|---|---|---|---|---|---|---|
| p53 | 18.5 ± 5.2 | 20.1 ± 5.4 | 0.050 | 13.7 ± 4.2 | 0.001 | 5.5 ± 0.8 | <0.001 |
| GBU4-5 | 18.9 ± 3.3 | 17.2 ± 3.5 | 0.044 | 12.4 ± 3.3 | 0.010 | 7.1 ± 1.1 | <0.001 |
| CAGE | 14.3 ± 3.8 | 13.7 ± 3.4 | 0.012 | 9.1 ± 3.2 | 0.010 | 6.4 ± 2.9 | <0.001 |
| NY-ESO-1 | 12.6 ± 3.5 | 11.7 ± 3.8 | 0.045 | 7.8 ± 3.1 | 0.050 | 4.5 ± 0.9 | <0.001 |
| SOX2 | 13.4 ± 4.1 | 14.3 ± 3.9 | 0.314 | 8.7 ± 3.6 | 0.005 | 5.0 ± 1.8 | <0.001 |
| MUC1 | 22.1 ± 4.8 | 24.1 ± 4.5 | 0.043 | 14.9 ± 3.9 | 0.080 | 6.3 ± 1.7 | 0.010 |
| APE1 | 14.9 ± 4.2 | 14.2 ± 3.7 | 0.651 | 11.2 ± 3.5 | 0.120 | 8.8 ± 1.0 | 0.020 |
| PGP9.5 | 16.3 ± 3.9 | 16.1 ± 4.1 | 0.247 | 10.8 ± 3.6 | 0.050 | 5.2 ± 2.4 | 0.010 |
| GAGE7 | 11.5 ± 3.2 | 10.8 ± 2.9 | 0.062 | 8.9 ± 2.7 | 0.080 | 4.8 ± 1.4 | 0.020 |
| MAGE1 | 17.6 ± 4.9 | 18.4 ± 4.9 | 0.085 | 9.6 ± 4.0 | 0.050 | 5.1 ± 2.5 | 0.010 |
4.3 Logistic-regression analysis of factors influencing recurrence in lung cancer patients
Autoantibodies dynamic in recurrence and non-recurrence patients were presented in Figure 2a. Univariable logistic‑regression analysis showed that postoperative reductions in several autoantibody titers were significantly associated with the odds of recurrence; these associations remained robust after adjustment for age, sex, tumor stage, and smoking status in the multivariable model (Table 3).
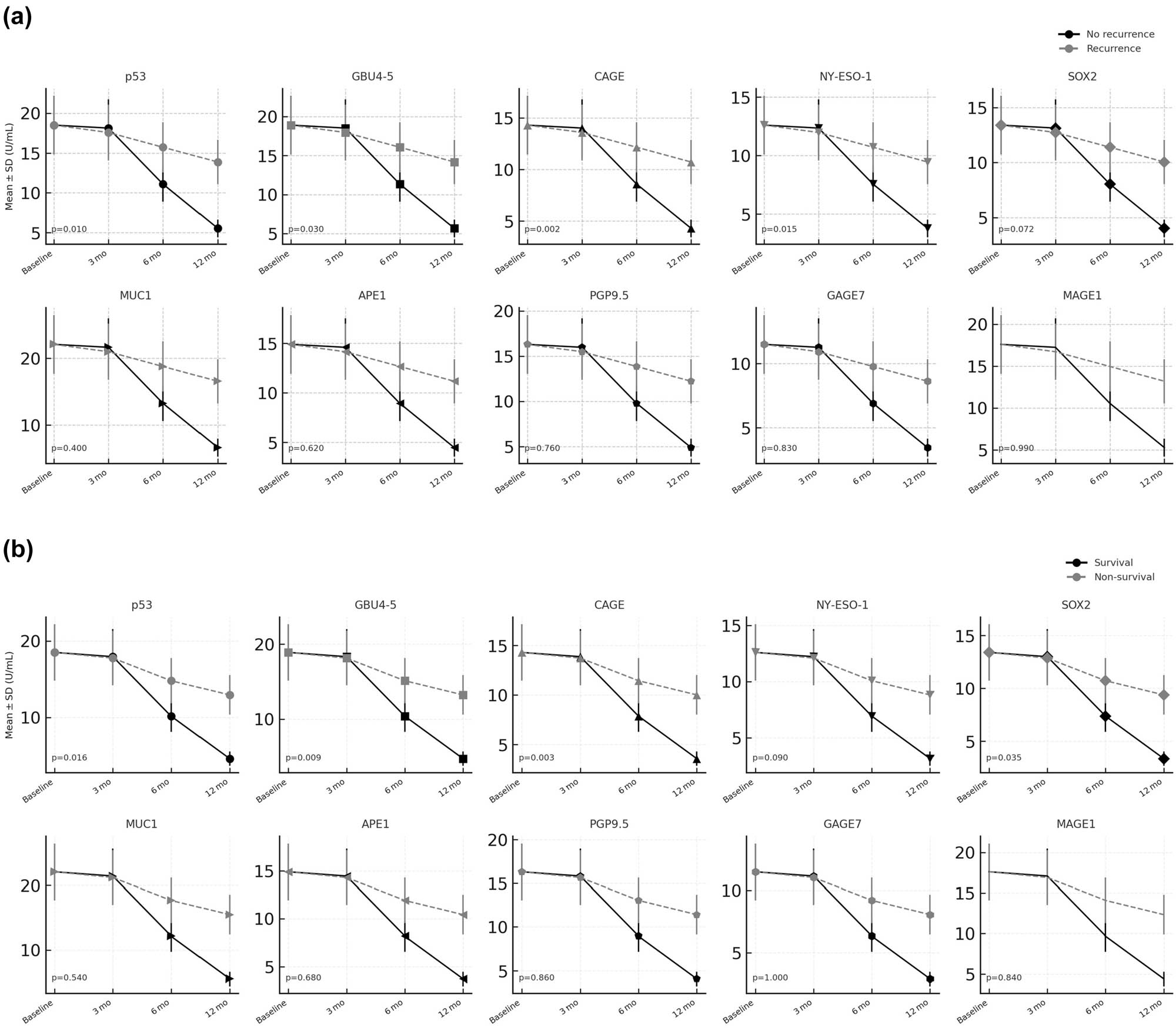
Longitudinal Autoantibodies Dynamics. (a) Longitudinal distribution of autoantibody titers after resection. (b) Individual postoperative trajectories of autoantibodies across time‑points.
Univariable and multivariable analyses for 1-year recurrence
| Variable | Univariable | Multivariable | ||||
|---|---|---|---|---|---|---|
| OR (95% CI) | p | FDR p | OR (95% CI) | p | FDR p | |
| p53 (≥50% reduction) | 0.50 (0.30–0.85) | 0.010 | 0.065 | 0.55 (0.32–0.95) | 0.032 | 0.058 |
| GBU4-5 (≥45% reduction) | 0.56 (0.33–0.95) | 0.030 | 0.078 | 0.60 (0.35–1.02) | 0.058 | 0.058 |
| CAGE (≥50% reduction) | 0.42 (0.25–0.72) | 0.002 | 0.026 | 0.48 (0.27–0.82) | 0.007 | 0.035 |
| NY-ESO-1 (≥50% reduction) | 0.52 (0.31–0.88) | 0.015 | 0.065 | 0.55 (0.31–0.96) | 0.039 | 0.058 |
| SOX2 (≥45% reduction) | 0.60 (0.34–1.05) | 0.072 | 0.134 | — | — | — |
| MUC1 (≥40% reduction) | 0.80 (0.47–1.35) | 0.400 | 0.650 | — | — | — |
| APE1 (≥40% reduction) | 0.88 (0.52–1.47) | 0.620 | 0.806 | — | — | — |
| PGP9.5 (≥50% reduction) | 0.92 (0.54–1.56) | 0.760 | 0.897 | — | — | — |
| GAGE7 (≥50% reduction) | 0.95 (0.57–1.58) | 0.830 | 0.899 | — | — | — |
| MAGE1 (≥50% reduction) | 1.00 (0.60–1.66) | 0.990 | 0.990 | — | — | — |
| Age (per 1-year increase) | 1.03 (0.99–1.07) | 0.070 | 0.152 | — | — | — |
| Stage II vs Stage I | 1.30 (1.02–2.30) | 0.021 | 0.068 | 1.25 (0.99–2.09) | 0.055 | 0.058 |
| Sex (female vs male) | 0.85 (0.48–1.53) | 0.600 | 0.867 | — | — | — |
| Smoking (current/ex vs never) | 1.12 (0.62–2.05) | 0.690 | 0.812 | |||
| Hypertension | 1.05 (0.56–1.98) | 0.870 | 0.899 | |||
| Diabetes | 1.21 (0.60–2.46) | 0.590 | 0.756 | |||
| Charlson ≥ 2 | 1.18 (0.63–2.23) | 0.610 | 0.767 | |||
In the univariate analysis, significant associations were found for reductions in several autoantibodies. p53 (≥50% reduction), GBU4-5 (≥45% reduction), CAGE (≥50% reduction), and NY-ESO-1 (≥50% reduction) each showed a significant association with lower recurrence risk (raw p < 0.05), after applying the Benjamini–Hochberg correction for multiple tests, CAGE remained significant (false discovery rate [FDR] p = 0.026), while p53, GBU4-5, and NY-ESO-1 were borderline (Table 3). The multivariate analysis, which adjusts for other variables, only CAGE retained significance as the most robust predictor of lower recurrence, retaining statistical significance after FDR adjustment (FDR p = 0.035). Notably, other autoantibodies did not show significant associations in either univariate or multivariate models (Table 3).
4.4 Prognostic significance of autoantibody reductions in lung cancer survival
Autoantibodies dynamic in survival and non-survival patients are presented in Figure 2b. Cox regression analysis was conducted to evaluate the impact of autoantibody reductions on OS in lung cancer patients (Table 4). In the univariate analysis, p53 (≥50% reduction), GBU4-5 (≥45% reduction), and CAGE (≥50% reduction) demonstrated significant associations with improved 1-year OS (raw p < 0.05), With FDR correction, only CAGE remained below the 0.05 threshold (FDR p = 0.039) (Table 4). In the multivariate model, CAGE (FDR p = 0.020), GBU4-5 (FDR p = 0.034), and p53 (FDR p = 0.045) all achieved significance, indicating that reductions in these autoantibodies are each associated with improved 1-year survival (Table 4). By contrast, SOX2 remained only borderline significant (raw p = 0.070, FDR p = 0.070) when included and was eventually excluded from the final model. These results highlight CAGE as a particularly strong marker of survival benefit, with additional support for GBU4-5 and p53 once multiple testing is taken into account.
Univariable and multivariable analyses for 1-year OS
| Variable | Univariable | Multivariable | ||||
|---|---|---|---|---|---|---|
| HR (95% CI) | p | FDR p | HR (95% CI) | p | FDR p | |
| p53 (≥50% reduction) | 0.58 (0.37–0.90) | 0.016 | 0.069 | 0.60 (0.37–0.96) | 0.034 | 0.045 |
| GBU4-5 (≥45% reduction) | 0.50 (0.29–0.84) | 0.009 | 0.059 | 0.52 (0.30–0.89) | 0.017 | 0.034 |
| CAGE (≥50% reduction) | 0.45 (0.27–0.75) | 0.003 | 0.039 | 0.47 (0.28–0.79) | 0.005 | 0.020 |
| NY-ESO-1 (≥50% reduction) | 0.65 (0.40–1.07) | 0.090 | 0.195 | — | — | — |
| SOX2 (≥45% reduction) | 0.56 (0.33–0.96) | 0.035 | 0.114 | 0.59 (0.34–1.04) | 0.070 | 0.070 |
| MUC1 (≥40% reduction) | 0.85 (0.51–1.41) | 0.540 | 0.780 | — | — | — |
| APE1 (≥40% reduction) | 0.90 (0.55–1.47) | 0.680 | 0.884 | — | — | — |
| PGP9.5 (≥50% reduction) | 0.96 (0.58–1.59) | 0.860 | 0.931 | — | — | — |
| GAGE7 (≥50% reduction) | 1.00 (0.60–1.67) | 1.000 | 1.000 | — | — | — |
| MAGE1 (≥50% reduction) | 1.05 (0.64–1.74) | 0.840 | 0.991 | — | — | — |
| Age (per 1-year increase) | 1.05 (1.00–1.09) | 0.052 | 0.135 | — | — | — |
| Stage II vs Stage I | 1.40 (0.90–2.35) | 0.110 | 0.204 | — | — | — |
| Sex (female vs male) | 0.82 (0.48–1.39) | 0.460 | 0.748 | — | — | — |
| Smoking (current/ex vs never) | 1.08 (0.58–2.02) | 0.800 | 0.888 | |||
| Hypertension | 1.02 (0.54–1.93) | 0.960 | 0.960 | |||
| Diabetes | 1.27 (0.64–2.53) | 0.490 | 0.700 | |||
| Charlson ≥ 2 | 1.33 (0.70–2.52) | 0.380 | 0.570 | |||
5 Discussion
TAA‑associated autoantibodies are recognized as promising biomarkers for cancer detection, progression, and prognosis. In our study, dynamic shifts in autoantibody levels after lung‑cancer surgery provided valuable insights into patient outcomes. Postoperative decreases in specific autoantibodies – p53, GBU4‑5, CAGE, and NY‑ESO‑1 – may serve as potential prognostic markers for lung cancer.
Immediately after thoracic resection, tissue-damage-associated molecular patterns trigger a systemic cytokine surge (IL-6, IL-8) and a brief lymphopenia/NK-cell dip that can last several days; this “danger-signal” phase is now recognized as a normal, self-limiting response that resolves more quickly after minimally invasive surgery [25]. Concomitantly, myeloid-derived suppressor cells and regulatory T cells expand, creating a transient window of immunosuppression during which residual tumor cells may evade surveillance [26]. Over subsequent weeks, adaptive immunity rebounds, cytotoxic T/NK activity is restored and – provided that viable tumor antigen has been removed – circulating autoantibody titers fall. Optimized peri-operative strategies can blunt the early inflammatory spike and accelerate immune recovery, reinforcing our observation that durable reductions in p53, NY-ESO-1, and related autoantibodies are most evident once the pro-inflammatory milieu has subsided and effective tumor immunity is re-established [27].
The autoantibody panel evaluated in this study – P53, MUC1, NY‑ESO‑1, APE1, PGP9.5, SOX2, GBU4‑5, GAGE7, CAGE, and MAGE1 – was purposefully chosen for their well‑documented roles in lung‑cancer biology and host immune surveillance. These TAAs are often over‑expressed in lung tumors, triggering robust immune responses that yield measurable circulating autoantibodies. Anti‑P53 autoantibodies, for instance, mirror mutations in the tumor‑suppressor gene and are reliable markers of tumor activity and recurrence [23,28]. Similarly, the cancer‑testis antigens NY‑ESO‑1 and MAGE1 are strongly expressed in lung cancer, and their corresponding autoantibodies correlate with poor prognosis and elevated recurrence risk [13,21]. Incorporating MUC1 – a glycoprotein whose aberrant glycosylation drives adenocarcinoma progression – broadens the panel’s diagnostic utility [22]. Autoantibodies such as GBU4‑5 and CAGE have also demonstrated predictive value for disease recurrence [19,24]. By integrating markers with proven clinical relevance, this panel allows nuanced assessment of tumor dynamics, immune response, and recurrence risk. Longitudinal monitoring has shown that postoperative declines in autoantibodies such as P53, NY‑ESO‑1, and CAGE are associated with favorable outcomes, underlining their potential in personalized postoperative care [29].
Extensive evidence now shows that TAA autoantibodies predict key clinical outcomes, including recurrence‑free and OS. Their value as lung‑cancer biomarkers was first recognized nearly two decades ago [13]. Subsequent studies have linked autoantibodies to cancer‑testis antigens such as MAGE to both diagnosis and prognosis [21] and have demonstrated that TAA‑directed autoantibodies predict responses to immune‑checkpoint inhibitors in NSCLC [23]. A highly predictive autoantibody panel has likewise been reported to guide postoperative management in early‑stage NSCLC [19]. In line with these findings, our study identifies postoperative declines in P53 and MAGE autoantibody titers as markers of lower recurrence risk and improved survival, underscoring the close relationship between immune surveillance and clinical outcome.
High circulating anti-p53 titers almost invariably originate from conformationally altered (mutant) p53 that accumulates in tumor cells; these mutants not only mark heavy tumor burden but actively dampen innate‐immune sensors such as cGAS-STING and NF-κB signaling pathways [30,31]. Surgical resection removes the antigen source, precipitating a rapid fall in anti-p53 antibodies; the concurrent relief of mutant-p53-mediated immunosuppression helps restore antitumor immunity, a pattern echoed in NSCLC cohorts where persistently high anti-p53 titers predicted early relapse and shorter survival [32].
NY-ESO-1, in contrast, is a highly immunogenic cancer-testis antigen whose expression surges with hypomethylation in proliferating tumor cells. Robust humoral and CD8⁺ T-cell responses arise once the antigen load is high, and antibody levels track closely with viable tumor mass. Multicenter data show that durable post-therapy declines in NY-ESO-1 antibodies signify minimal residual disease and translate into longer disease-free and OS [17,33]. Moreover, simultaneous NY-ESO-1-specific antibody and CD8⁺ responses correlate with superior outcomes in immunotherapy, suggesting that once tumor antigen is removed, falling antibody titers accompany a shift from chronic antigenic stimulation to effective effector-T-cell surveillance [34]. Together, these observations provide a biological rationale for the survival advantage observed in our cohort when p53 or NY-ESO-1 autoantibodies decline.
The robust associations we observed between postoperative declines in specific autoantibodies and improved outcomes support integrating autoantibody profiling into routine surveillance. Persistently elevated titers – particularly of CAGE or GBU4‑5 – could trigger closer monitoring or adjuvant therapy to address residual disease or micrometastases. Because these assays are blood‑based, they offer a non‑invasive, cost‑effective complement to imaging for tracking tumor dynamics after surgery. Our findings therefore underscore the clinical value of incorporating autoantibody testing into standard follow‑up protocols to enhance recurrence detection and improve survival in lung‑cancer patients.
As certain autoantibodies (e.g., SOX2 at the 3-month time point) exhibited changes approaching but not reaching conventional significance (p < 0.05). While these borderline results should be interpreted with caution, they may still have clinical relevance, particularly in a pilot or exploratory context. Consequently, while results like the SOX2 trend at 3 months are not definitively significant in this study, they underline the importance of continued investigation into the dynamic behavior of autoantibodies post-surgery. Clinicians may still find value in monitoring these markers as part of a broader risk assessment panel, pending validation in more extensive cohorts.
Although our results are promising, they are derived from a single-center study and have not been validated in an independent patient cohort. This limitation restricts the generalizability of our findings, as patient demographics, tumor biology, and treatment protocols may vary between institutions and geographic regions. To overcome this, future research should incorporate prospective, multi-center trials or external validation sets to confirm the prognostic significance of these autoantibody changes in broader and more heterogeneous populations. One notable limitation of this study is the absence of a non-malignant control group (e.g., individuals with benign lung conditions or healthy volunteers). Such a comparator could have clarified whether the baseline autoantibody levels observed in our lung cancer cohort diverge significantly from those in non-cancer populations. Although the primary objective was to investigate longitudinal changes post-surgery and their prognostic value, a proper control group would enhance our ability to discern disease-specific patterns and improve specificity for lung cancer. Future larger studies or multi-center collaborations should include an appropriate control arm to better contextualize baseline autoantibody titers and refine their clinical interpretation. Moreover, the absence of standardized cut‑off thresholds for autoantibody positivity remains a major obstacle, impeding cross‑study comparisons and limiting reproducibility. Conducting larger, methodologically harmonized studies and adopting consensus diagnostic criteria will strengthen the clinical applicability and translational potential of autoantibody profiling in lung‑cancer management. Expanding analyses to include additional TAAs could uncover biomarkers with complementary diagnostic and prognostic value [29]. Developing a comprehensive, multi‑marker “autoantibody signature” would further enhance risk stratification and enable truly personalized patient care. Pursuing these directions will help establish standardized, clinically actionable tools to improve lung‑cancer monitoring and therapeutic outcomes.
Our study demonstrates that longitudinal assessment of autoantibody levels before and after lung‑cancer surgery has significant predictive value for recurrence, metastasis, and OS. Tracking these changes enables tailored therapeutic strategies based on individual risk profiles. Collectively, the evidence supports integrating autoantibody monitoring into routine postoperative care for lung‑cancer patients to improve outcomes through more precise, personalized management.
-
Funding information: This study was supported by the Department of Science and Technology of Liaoning Province (2022-MS-453).
-
Author contributions: Supervision and conceptualization: YW; study concepts: YW; study design: JM, ZW; definition of intellectual content: JM, and ZW; Literature research: JM, ZW, LL, SP, JC, BG, XL, and YZ; investigation: JM, ZW, LL, SP, JC, BG, XL, YZ; data acquisition and analysis: JM, ZW, LL, SP, JC, BG, XL, and YZ; statistical analysis: JM, ZW, LL, SP, JC, BG, XL, and YZ; manuscript preparation: JM, and ZW manuscript review: JM, ZW, and YW.
-
Conflict of interest: Authors state no conflict of interest.
-
Data availability statement: The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
[1] Xiao Y, Zang D. On progress in surgical treatment of lung cancer. J Clin Med Res. 2022;3(2):53. 10.32629/jcmr.v3i2.819.Search in Google Scholar
[2] Vachani A, Carroll NM, Simoff MJ, Neslund-Dudas C, Honda S, Greenlee RT, et al. Stage migration and lung cancer incidence after initiation of low-dose computed tomography screening. J Thorac Oncol. 2022;17(12):1355–64. 10.1016/j.jtho.2022.08.011.Search in Google Scholar PubMed PubMed Central
[3] Lackey A, Donington JS. Surgical management of lung cancer. Semin Intervent Radiol. 2013;30(2):133–40. 10.1055/s-0033-1342954.Search in Google Scholar PubMed PubMed Central
[4] Venkitaraman B, Lei J, Kajamohideen S. Segmental resection in early-stage lung cancer. In Segmental Resection in Early-Stage Lung Cancer. London: IntechOpen; 2022. 10.5772/intechopen.106626.Search in Google Scholar
[5] Li N, Wang BX, Ou W, Wang T, Pu Y, Zhu TF, et al. Dynamic monitoring circulating tumor DNA in plasma samples by PEAC technology for patients with early-stage non-small cell lung cancer after surgery. J Clin Oncol. 2022;40(16 suppl):8547. 10.1200/JCO.2022.40.16_suppl.8547.Search in Google Scholar
[6] Nakada T, Takahashi Y, Sakakura N, Masago K, Iwata H, Ohtsuka T, et al. Postoperative surveillance using low-dose computed tomography for non-small-cell lung cancer. Eur J Cardiothorac Surg. 2023;63(1):ezac549. 10.1093/ejcts/ezac549.Search in Google Scholar PubMed
[7] Desuky AS, Bakrawy LM. Improved prediction of post-operative life expectancy after thoracic surgery. Adv Syst Sci Appl. 2016;16:70–80.Search in Google Scholar
[8] Namitha M, Anusha MS, Bhavana G, Chinta M. Prediction of severity after lung cancer surgery. In 2022 8th Int Conf Smart Structures Syst (ICSSS). IEEE; 2022. p. 1–5.10.1109/ICSSS54381.2022.9782291Search in Google Scholar
[9] Lam S, Boyle P, Healey GF, Maddison P, Peek L, Murray A, et al. EarlyCDT-Lung: an immunobiomarker test as an aid to early detection of lung cancer. Cancer Prev Res (Phila). 2011;4(7):1126–34. 10.1158/1940-6207.CAPR-10-0328.Search in Google Scholar PubMed
[10] Massion PP, Healey GF, Peek LJ, Fredericks L, Sewell HF, Murray A, et al. Autoantibody signature enhances the positive predictive power of computed tomography and nodule-based risk models for detection of lung cancer. J Thorac Oncol. 2017;12(4):578–84. 10.1016/j.jtho.2016.08.143.Search in Google Scholar PubMed PubMed Central
[11] Sullivan FM, Mair FS, Anderson W, Armory P, Briggs A, Chew C, et al. Earlier diagnosis of lung cancer in a randomised trial of an autoantibody blood test followed by imaging. Eur Respir J. 2021;57(4):2000670. 10.1183/13993003.00670-2020.Search in Google Scholar PubMed PubMed Central
[12] Zhuang L, Huang C, Ning Z, Yang L, Zou W, Wang P, et al. Circulating tumor-associated autoantibodies as novel diagnostic biomarkers in pancreatic adenocarcinoma. Int J Cancer. 2023;152(5):1013–24. 10.1002/ijc.34334.Search in Google Scholar PubMed
[13] Li P, Shi JX, Xing MT, Dai LP, Li JT, Zhang JY. Evaluation of serum autoantibodies against tumor-associated antigens as biomarkers in lung cancer. Tumour Biol. 2017;39(10):1010428317711662. 10.1177/1010428317711662.Search in Google Scholar PubMed
[14] Tong L, Sun J, Zhang X, Ge D, Li Y, Zhou J, et al. Development of an autoantibody panel for early detection of lung cancer in the Chinese population. Front Med (Lausanne). 2023;10:1209747. 10.3389/fmed.2023.1209747.Search in Google Scholar PubMed PubMed Central
[15] Guo H, Zhao W, Li C, Wu Z, Yu L, Wang M, et al. The diagnostic efficacy of seven autoantibodies in early detection of ground glass nodular lung adenocarcinoma. Front Oncol. 2024;14:1499140. 10.3389/fonc.2024.1499140.Search in Google Scholar PubMed PubMed Central
[16] Hoshino I, Nabeya Y, Takiguchi N, Gunji H, Ishige F, Iwatate Y, et al. Prognostic impact of p53 and/or NY-ESO-1 autoantibody induction in patients with gastroenterological cancers. Ann Gastroenterol Surg. 2020;4(3):275–82. 10.1002/ags3.12325.Search in Google Scholar PubMed PubMed Central
[17] Saito T, Kurokawa Y, Fujitani K, Kawabata R, Takeno A, Mikami J, et al. Serum NY-ESO-1 antibody as a predictive biomarker for postoperative recurrence of gastric cancer: a multicenter prospective observational study. Br J Cancer. 2024;130(7):1157–65. 10.1038/s41416-023-02540-3.Search in Google Scholar PubMed PubMed Central
[18] Li S, Ma Y, Xiong Y, Zhang P, Wang X, Wang Y, et al. Five tumor-associated autoantibodies expression levels in serum predict lung cancer and associate with poor outcome. Transl Cancer Res. 2019;8(4):1364–73.10.21037/tcr.2019.07.25Search in Google Scholar PubMed PubMed Central
[19] Patel AJ, Tan TM, Richter AG, Naidu B, Blackburn JM, Middleton GW. A highly predictive autoantibody-based biomarker panel for prognosis in early-stage NSCLC with potential therapeutic implications. Br J Cancer. 2022;126(2):238–46. 10.1038/s41416-021-01572-x.Search in Google Scholar PubMed PubMed Central
[20] Li Y, Li CQ, Guo SJ, Guo W, Jiang HW, Li HC, et al. Longitudinal serum autoantibody repertoire profiling identifies surgery-associated biomarkers in lung adenocarcinoma. EBioMedicine. 2020;53:102689.10.1016/j.ebiom.2020.102674Search in Google Scholar PubMed PubMed Central
[21] Wang T, Liu H, Pei L, Wang K, Song C, Wang P, et al. Screening of tumor-associated antigens based on Oncomine database and evaluation of diagnostic value of autoantibodies in lung cancer. Clin Immunol. 2020;210:108262. 10.1016/j.clim.2019.108262.Search in Google Scholar PubMed
[22] Huang H, Luo W, Ni Y, Sun S, Wang C, Zhang L. The diagnostic efficiency of seven autoantibodies in lung cancer. Eur J Cancer Prev. 2020;29(4):315–20. 10.1097/CEJ.0000000000000559.Search in Google Scholar PubMed
[23] Zhou J, Zhao J, Jia Q, Chu Q, Zhou F, Chu X, et al. Peripheral blood autoantibodies against tumor-associated antigen predict clinical outcome to immune checkpoint inhibitor-based treatment in advanced non-small cell lung cancer. Front Oncol. 2021;11:625578. 10.3389/fonc.2021.625578.Search in Google Scholar PubMed PubMed Central
[24] Chin A, Choi MY, Fritzler MJ. Gaps and trends in autoantibody testing. J Appl Lab Med. 2022;7(1):362–6. 10.1093/jalm/jfab153.Search in Google Scholar PubMed
[25] Furák J, Németh T, Lantos J, Fabó C, Zombori-Tóth N, Paróczai D, et al. Perioperative systemic inflammation in lung cancer surgery. Front Surg. 2022;9:883322. 10.3389/fsurg.2022.883322.Search in Google Scholar PubMed PubMed Central
[26] Tang F, Tie Y, Tu C, Wei X. Surgical trauma-induced immunosuppression in cancer: recent advances and potential therapies. Clin Transl Med. 2020;10(1):199–223. 10.1002/ctm2.24.Search in Google Scholar PubMed PubMed Central
[27] Guo R, Yang W, Zhong M, Rao P, Luo X, Liao B, et al. The relationship between anesthesia, surgery and postoperative immune function in cancer patients: a review. Front Immunol. 2024;15:1441020. 10.3389/fimmu.2024.1441020.Search in Google Scholar PubMed PubMed Central
[28] Tang ZM, Ling ZG, Wang CM, Wu YB, Kong JL. Serum tumor-associated autoantibodies as diagnostic biomarkers for lung cancer: a systematic review and meta-analysis. PLoS One. 2017;12(7):e0182117.10.1371/journal.pone.0182117Search in Google Scholar PubMed PubMed Central
[29] Volkov M, Coppola M, Huizinga R, Eftimov F, Huizinga TWJ, van der Kooi AJ, et al. Comprehensive overview of autoantibody isotype and subclass distribution. J Allergy Clin Immunol. 2022;150(5):999–1010. 10.1016/j.jaci.2022.05.023.Search in Google Scholar PubMed
[30] Ghosh M, Saha S, Bettke J, Nagar R, Parrales A, Iwakuma T, et al. Mutant p53 suppresses innate immune signalling to promote tumorigenesis. Cancer Cell. 2021;39(4):494–508.e5. 10.1016/j.ccell.2021.01.003.Search in Google Scholar PubMed PubMed Central
[31] Guo G, Yu M, Xiao W, Celis E, Cui Y. Local activation of p53 in the tumour microenvironment overcomes immune suppression and enhances antitumour immunity. Cancer Res. 2017;77(9):2292–305. 10.1158/0008-5472.CAN-16-2832.Search in Google Scholar PubMed PubMed Central
[32] Mattioni M, Soddu S, Prodosmo A, Visca P, Conti S, Alessandrini G, et al. Prognostic role of serum p53 antibodies in lung cancer. BMC Cancer. 2015;15:148. 10.1186/s12885-015-1174-4.Search in Google Scholar PubMed PubMed Central
[33] Ohue Y, Kurose K, Karasaki T, Isobe M, Yamaoka T, Futami J, et al. Serum antibody against NY-ESO-1 and XAGE1 antigens potentially predicts clinical responses to anti-programmed cell death-1 therapy in non-small cell lung cancer. J Thorac Oncol. 2019;14(11):2071–83. 10.1016/j.jtho.2019.08.008.Search in Google Scholar PubMed
[34] Yuan J, Adamow M, Ginsberg BA, Rasalan TS, Ritter E, Gallardo HF, et al. Integrated NY-ESO-1 antibody and CD8⁺ T-cell responses correlate with clinical benefit in advanced melanoma patients treated with ipilimumab. Proc Natl Acad Sci U S A. 2011;108(40):16723–8. 10.1073/pnas.1110814108.Search in Google Scholar PubMed PubMed Central
© 2025 the author(s), published by De Gruyter
This work is licensed under the Creative Commons Attribution 4.0 International License.
Articles in the same Issue
- Biomedical Sciences
- Mechanism of triptolide regulating proliferation and apoptosis of hepatoma cells by inhibiting JAK/STAT pathway
- Maslinic acid improves mitochondrial function and inhibits oxidative stress and autophagy in human gastric smooth muscle cells
- Comparative analysis of inflammatory biomarkers for the diagnosis of neonatal sepsis: IL-6, IL-8, SAA, CRP, and PCT
- Post-pandemic insights on COVID-19 and premature ovarian insufficiency
- Proteome differences of dental stem cells between permanent and deciduous teeth by data-independent acquisition proteomics
- Optimizing a modified cetyltrimethylammonium bromide protocol for fungal DNA extraction: Insights from multilocus gene amplification
- Preliminary analysis of the role of small hepatitis B surface proteins mutations in the pathogenesis of occult hepatitis B infection via the endoplasmic reticulum stress-induced UPR-ERAD pathway
- Efficacy of alginate-coated gold nanoparticles against antibiotics-resistant Staphylococcus and Streptococcus pathogens of acne origins
- Battling COVID-19 leveraging nanobiotechnology: Gold and silver nanoparticle–B-escin conjugates as SARS-CoV-2 inhibitors
- Neurodegenerative diseases and neuroinflammation-induced apoptosis
- Impact of fracture fixation surgery on cognitive function and the gut microbiota in mice with a history of stroke
- COLEC10: A potential tumor suppressor and prognostic biomarker in hepatocellular carcinoma through modulation of EMT and PI3K-AKT pathways
- High-temperature requirement serine protease A2 inhibitor UCF-101 ameliorates damaged neurons in traumatic brain-injured rats by the AMPK/NF-κB pathway
- SIK1 inhibits IL-1β-stimulated cartilage apoptosis and inflammation in vitro through the CRTC2/CREB1 signaling
- Rutin–chitooligosaccharide complex: Comprehensive evaluation of its anti-inflammatory and analgesic properties in vitro and in vivo
- Knockdown of Aurora kinase B alleviates high glucose-triggered trophoblast cells damage and inflammation during gestational diabetes
- Calcium-sensing receptors promoted Homer1 expression and osteogenic differentiation in bone marrow mesenchymal stem cells
- ABI3BP can inhibit the proliferation, invasion, and epithelial–mesenchymal transition of non-small-cell lung cancer cells
- Changes in blood glucose and metabolism in hyperuricemia mice
- Rapid detection of the GJB2 c.235delC mutation based on CRISPR-Cas13a combined with lateral flow dipstick
- IL-11 promotes Ang II-induced autophagy inhibition and mitochondrial dysfunction in atrial fibroblasts
- Short-chain fatty acid attenuates intestinal inflammation by regulation of gut microbial composition in antibiotic-associated diarrhea
- Application of metagenomic next-generation sequencing in the diagnosis of pathogens in patients with diabetes complicated by community-acquired pneumonia
- NAT10 promotes radiotherapy resistance in non-small cell lung cancer by regulating KPNB1-mediated PD-L1 nuclear translocation
- Phytol-mixed micelles alleviate dexamethasone-induced osteoporosis in zebrafish: Activation of the MMP3–OPN–MAPK pathway-mediating bone remodeling
- Association between TGF-β1 and β-catenin expression in the vaginal wall of patients with pelvic organ prolapse
- Primary pleomorphic liposarcoma involving bilateral ovaries: Case report and literature review
- Effects of de novo donor-specific Class I and II antibodies on graft outcomes after liver transplantation: A pilot cohort study
- Sleep architecture in Alzheimer’s disease continuum: The deep sleep question
- Ephedra fragilis plant extract: A groundbreaking corrosion inhibitor for mild steel in acidic environments – electrochemical, EDX, DFT, and Monte Carlo studies
- Langerhans cell histiocytosis in an adult patient with upper jaw and pulmonary involvement: A case report
- Inhibition of mast cell activation by Jaranol-targeted Pirin ameliorates allergic responses in mouse allergic rhinitis
- Aeromonas veronii-induced septic arthritis of the hip in a child with acute lymphoblastic leukemia
- Clusterin activates the heat shock response via the PI3K/Akt pathway to protect cardiomyocytes from high-temperature-induced apoptosis
- Research progress on fecal microbiota transplantation in tumor prevention and treatment
- Low-pressure exposure influences the development of HAPE
- Stigmasterol alleviates endplate chondrocyte degeneration through inducing mitophagy by enhancing PINK1 mRNA acetylation via the ESR1/NAT10 axis
- AKAP12, mediated by transcription factor 21, inhibits cell proliferation, metastasis, and glycolysis in lung squamous cell carcinoma
- Association between PAX9 or MSX1 gene polymorphism and tooth agenesis risk: A meta-analysis
- A case of bloodstream infection caused by Neisseria gonorrhoeae
- Case of nasopharyngeal tuberculosis complicated with cervical lymph node and pulmonary tuberculosis
- p-Cymene inhibits pro-fibrotic and inflammatory mediators to prevent hepatic dysfunction
- GFPT2 promotes paclitaxel resistance in epithelial ovarian cancer cells via activating NF-κB signaling pathway
- Transfer RNA-derived fragment tRF-36 modulates varicose vein progression via human vascular smooth muscle cell Notch signaling
- RTA-408 attenuates the hepatic ischemia reperfusion injury in mice possibly by activating the Nrf2/HO-1 signaling pathway
- Decreased serum TIMP4 levels in patients with rheumatoid arthritis
- Sirt1 protects lupus nephritis by inhibiting the NLRP3 signaling pathway in human glomerular mesangial cells
- Sodium butyrate aids brain injury repair in neonatal rats
- Interaction of MTHFR polymorphism with PAX1 methylation in cervical cancer
- Convallatoxin inhibits proliferation and angiogenesis of glioma cells via regulating JAK/STAT3 pathway
- The effect of the PKR inhibitor, 2-aminopurine, on the replication of influenza A virus, and segment 8 mRNA splicing
- Effects of Ire1 gene on virulence and pathogenicity of Candida albicans
- Small cell lung cancer with small intestinal metastasis: Case report and literature review
- GRB14: A prognostic biomarker driving tumor progression in gastric cancer through the PI3K/AKT signaling pathway by interacting with COBLL1
- 15-Lipoxygenase-2 deficiency induces foam cell formation that can be restored by salidroside through the inhibition of arachidonic acid effects
- FTO alleviated the diabetic nephropathy progression by regulating the N6-methyladenosine levels of DACT1
- Clinical relevance of inflammatory markers in the evaluation of severity of ulcerative colitis: A retrospective study
- Zinc valproic acid complex promotes osteoblast differentiation and exhibits anti-osteoporotic potential
- Primary pulmonary synovial sarcoma in the bronchial cavity: A case report
- Metagenomic next-generation sequencing of alveolar lavage fluid improves the detection of pulmonary infection
- Uterine tumor resembling ovarian sex cord tumor with extensive rhabdoid differentiation: A case report
- Genomic analysis of a novel ST11(PR34365) Clostridioides difficile strain isolated from the human fecal of a CDI patient in Guizhou, China
- Effects of tiered cardiac rehabilitation on CRP, TNF-α, and physical endurance in older adults with coronary heart disease
- Changes in T-lymphocyte subpopulations in patients with colorectal cancer before and after acupoint catgut embedding acupuncture observation
- Modulating the tumor microenvironment: The role of traditional Chinese medicine in improving lung cancer treatment
- Alterations of metabolites related to microbiota–gut–brain axis in plasma of colon cancer, esophageal cancer, stomach cancer, and lung cancer patients
- Research on individualized drug sensitivity detection technology based on bio-3D printing technology for precision treatment of gastrointestinal stromal tumors
- CEBPB promotes ulcerative colitis-associated colorectal cancer by stimulating tumor growth and activating the NF-κB/STAT3 signaling pathway
- Oncolytic bacteria: A revolutionary approach to cancer therapy
- A de novo meningioma with rapid growth: A possible malignancy imposter?
- Diagnosis of secondary tuberculosis infection in an asymptomatic elderly with cancer using next-generation sequencing: Case report
- Hesperidin and its zinc(ii) complex enhance osteoblast differentiation and bone formation: In vitro and in vivo evaluations
- Research progress on the regulation of autophagy in cardiovascular diseases by chemokines
- Anti-arthritic, immunomodulatory, and inflammatory regulation by the benzimidazole derivative BMZ-AD: Insights from an FCA-induced rat model
- Immunoassay for pyruvate kinase M1/2 as an Alzheimer’s biomarker in CSF
- The role of HDAC11 in age-related hearing loss: Mechanisms and therapeutic implications
- Evaluation and application analysis of animal models of PIPNP based on data mining
- Therapeutic approaches for liver fibrosis/cirrhosis by targeting pyroptosis
- Fabrication of zinc oxide nanoparticles using Ruellia tuberosa leaf extract induces apoptosis through P53 and STAT3 signalling pathways in prostate cancer cells
- Haplo-hematopoietic stem cell transplantation and immunoradiotherapy for severe aplastic anemia complicated with nasopharyngeal carcinoma: A case report
- Modulation of the KEAP1-NRF2 pathway by Erianin: A novel approach to reduce psoriasiform inflammation and inflammatory signaling
- The expression of epidermal growth factor receptor 2 and its relationship with tumor-infiltrating lymphocytes and clinical pathological features in breast cancer patients
- Innovations in MALDI-TOF Mass Spectrometry: Bridging modern diagnostics and historical insights
- BAP1 complexes with YY1 and RBBP7 and its downstream targets in ccRCC cells
- Hypereosinophilic syndrome with elevated IgG4 and T-cell clonality: A report of two cases
- Electroacupuncture alleviates sciatic nerve injury in sciatica rats by regulating BDNF and NGF levels, myelin sheath degradation, and autophagy
- Polydatin prevents cholesterol gallstone formation by regulating cholesterol metabolism via PPAR-γ signaling
- RNF144A and RNF144B: Important molecules for health
- Analysis of the detection rate and related factors of thyroid nodules in the healthy population
- Artesunate inhibits hepatocellular carcinoma cell migration and invasion through OGA-mediated O-GlcNAcylation of ZEB1
- Endovascular management of post-pancreatectomy hemorrhage caused by a hepatic artery pseudoaneurysm: Case report and review of the literature
- Efficacy and safety of anti-PD-1/PD-L1 antibodies in patients with relapsed refractory diffuse large B-cell lymphoma: A meta-analysis
- SATB2 promotes humeral fracture healing in rats by activating the PI3K/AKT pathway
- Overexpression of the ferroptosis-related gene, NFS1, corresponds to gastric cancer growth and tumor immune infiltration
- Understanding risk factors and prognosis in diabetic foot ulcers
- Atractylenolide I alleviates the experimental allergic response in mice by suppressing TLR4/NF-kB/NLRP3 signalling
- FBXO31 inhibits the stemness characteristics of CD147 (+) melanoma stem cells
- Immune molecule diagnostics in colorectal cancer: CCL2 and CXCL11
- Inhibiting CXCR6 promotes senescence of activated hepatic stellate cells with limited proinflammatory SASP to attenuate hepatic fibrosis
- Cadmium toxicity, health risk and its remediation using low-cost biochar adsorbents
- Pulmonary cryptococcosis with headache as the first presentation: A case report
- Solitary pulmonary metastasis with cystic airspaces in colon cancer: A rare case report
- RUNX1 promotes denervation-induced muscle atrophy by activating the JUNB/NF-κB pathway and driving M1 macrophage polarization
- Morphometric analysis and immunobiological investigation of Indigofera oblongifolia on the infected lung with Plasmodium chabaudi
- The NuA4/TIP60 histone-modifying complex and Hr78 modulate the Lobe2 mutant eye phenotype
- Experimental study on salmon demineralized bone matrix loaded with recombinant human bone morphogenetic protein-2: In vitro and in vivo study
- A case of IgA nephropathy treated with a combination of telitacicept and half-dose glucocorticoids
- Analgesic and toxicological evaluation of cannabidiol-rich Moroccan Cannabis sativa L. (Khardala variety) extract: Evidence from an in vivo and in silico study
- Wound healing and signaling pathways
- Combination of immunotherapy and whole-brain radiotherapy on prognosis of patients with multiple brain metastases: A retrospective cohort study
- To explore the relationship between endometrial hyperemia and polycystic ovary syndrome
- Research progress on the impact of curcumin on immune responses in breast cancer
- Biogenic Cu/Ni nanotherapeutics from Descurainia sophia (L.) Webb ex Prantl seeds for the treatment of lung cancer
- Dapagliflozin attenuates atrial fibrosis via the HMGB1/RAGE pathway in atrial fibrillation rats
- Glycitein alleviates inflammation and apoptosis in keratinocytes via ROS-associated PI3K–Akt signalling pathway
- ADH5 inhibits proliferation but promotes EMT in non-small cell lung cancer cell through activating Smad2/Smad3
- Apoptotic efficacies of AgNPs formulated by Syzygium aromaticum leaf extract on 32D-FLT3-ITD human leukemia cell line with PI3K/AKT/mTOR signaling pathway
- Novel cuproptosis-related genes C1QBP and PFKP identified as prognostic and therapeutic targets in lung adenocarcinoma
- Bee venom promotes exosome secretion and alters miRNA cargo in T cells
- Treatment of pure red cell aplasia in a chronic kidney disease patient with roxadustat: A case report
- Comparative bioinformatics analysis of the Wnt pathway in breast cancer: Selection of novel biomarker panels associated with ER status
- Kynurenine facilitates renal cell carcinoma progression by suppressing M2 macrophage pyroptosis through inhibition of CASP1 cleavage
- RFX5 promotes the growth, motility, and inhibits apoptosis of gastric adenocarcinoma cells through the SIRT1/AMPK axis
- ALKBH5 exacerbates early cardiac damage after radiotherapy for breast cancer via m6A demethylation of TLR4
- Phytochemicals of Roman chamomile: Antioxidant, anti-aging, and whitening activities of distillation residues
- Circadian gene Cry1 inhibits the tumorigenicity of hepatocellular carcinoma by the BAX/BCL2-mediated apoptosis pathway
- The TNFR-RIPK1/RIPK3 signalling pathway mediates the effect of lanthanum on necroptosis of nerve cells
- Longitudinal monitoring of autoantibody dynamics in patients with early-stage non-small-cell lung cancer undergoing surgery
- The potential role of rutin, a flavonoid, in the management of cancer through modulation of cell signaling pathways
- Construction of pectinase gene engineering microbe and its application in tobacco sheets
- Construction of a microbial abundance prognostic scoring model based on intratumoral microbial data for predicting the prognosis of lung squamous cell carcinoma
- Sepsis complicated by haemophagocytic lymphohistiocytosis triggered by methicillin-resistant Staphylococcus aureus and human herpesvirus 8 in an immunocompromised elderly patient: A case report
- Sarcopenia in liver transplantation: A comprehensive bibliometric study of current research trends and future directions
- Advances in cancer immunotherapy and future directions in personalized medicine
- Can coronavirus disease 2019 affect male fertility or cause spontaneous abortion? A two-sample Mendelian randomization analysis
- Heat stroke associated with novel leukaemia inhibitory factor receptor gene variant in a Chinese infant
- PSME2 exacerbates ulcerative colitis by disrupting intestinal barrier function and promoting autophagy-dependent inflammation
- Hyperosmolar hyperglycemic state with severe hypernatremia coexisting with central diabetes insipidus: A case report and literature review
- Efficacy and mechanism of escin in improving the tissue microenvironment of blood vessel walls via anti-inflammatory and anticoagulant effects: Implications for clinical practice
- Merkel cell carcinoma: Clinicopathological analysis of three patients and literature review
- Genetic variants in VWF exon 26 and their implications for type 1 Von Willebrand disease in a Saudi Arabian population
- Lipoxin A4 improves myocardial ischemia/reperfusion injury through the Notch1-Nrf2 signaling pathway
- High levels of EPHB2 expression predict a poor prognosis and promote tumor progression in endometrial cancer
- Knockdown of SHP-2 delays renal tubular epithelial cell injury in diabetic nephropathy by inhibiting NLRP3 inflammasome-mediated pyroptosis
- Exploring the toxicity mechanisms and detoxification methods of Rhizoma Paridis
- Concomitant gastric carcinoma and primary hepatic angiosarcoma in a patient: A case report
- Ecology and Environmental Science
- Optimization and comparative study of Bacillus consortia for cellulolytic potential and cellulase enzyme activity
- The complete mitochondrial genome analysis of Haemaphysalis hystricis Supino, 1897 (Ixodida: Ixodidae) and its phylogenetic implications
- Epidemiological characteristics and risk factors analysis of multidrug-resistant tuberculosis among tuberculosis population in Huzhou City, Eastern China
- Indices of human impacts on landscapes: How do they reflect the proportions of natural habitats?
- Genetic analysis of the Siberian flying squirrel population in the northern Changbai Mountains, Northeast China: Insights into population status and conservation
- Diversity and environmental drivers of Suillus communities in Pinus sylvestris var. mongolica forests of Inner Mongolia
- Global assessment of the fate of nitrogen deposition in forest ecosystems: Insights from 15N tracer studies
- Fungal and bacterial pathogenic co-infections mainly lead to the assembly of microbial community in tobacco stems
- Influencing of coal industry related airborne particulate matter on ocular surface tear film injury and inflammatory factor expression in Sprague-Dawley rats
- Temperature-dependent development, predation, and life table of Sphaerophoria macrogaster (Thomson) (Diptera: Syrphidae) feeding on Myzus persicae (Sulzer) (Homoptera: Aphididae)
- Eleonora’s falcon trophic interactions with insects within its breeding range: A systematic review
- Agriculture
- Integrated analysis of transcriptome, sRNAome, and degradome involved in the drought-response of maize Zhengdan958
- Variation in flower frost tolerance among seven apple cultivars and transcriptome response patterns in two contrastingly frost-tolerant selected cultivars
- Heritability of durable resistance to stripe rust in bread wheat (Triticum aestivum L.)
- Molecular mechanism of follicular development in laying hens based on the regulation of water metabolism
- Animal Science
- Effect of sex ratio on the life history traits of an important invasive species, Spodoptera frugiperda
- Plant Sciences
- Hairpin in a haystack: In silico identification and characterization of plant-conserved microRNA in Rafflesiaceae
- Widely targeted metabolomics of different tissues in Rubus corchorifolius
- The complete chloroplast genome of Gerbera piloselloides (L.) Cass., 1820 (Carduoideae, Asteraceae) and its phylogenetic analysis
- Field trial to correlate mineral solubilization activity of Pseudomonas aeruginosa and biochemical content of groundnut plants
- Correlation analysis between semen routine parameters and sperm DNA fragmentation index in patients with semen non-liquefaction: A retrospective study
- Plasticity of the anatomical traits of Rhododendron L. (Ericaceae) leaves and its implications in adaptation to the plateau environment
- Effects of Piriformospora indica and arbuscular mycorrhizal fungus on growth and physiology of Moringa oleifera under low-temperature stress
- Effects of different sources of potassium fertiliser on yield, fruit quality and nutrient absorption in “Harward” kiwifruit (Actinidia deliciosa)
- Comparative efficiency and residue levels of spraying programs against powdery mildew in grape varieties
- The DREB7 transcription factor enhances salt tolerance in soybean plants under salt stress
- Using plant electrical signals of water hyacinth (Eichhornia crassipes) for water pollution monitoring
- Food Science
- Phytochemical analysis of Stachys iva: Discovering the optimal extract conditions and its bioactive compounds
- Review on role of honey in disease prevention and treatment through modulation of biological activities
- Computational analysis of polymorphic residues in maltose and maltotriose transporters of a wild Saccharomyces cerevisiae strain
- Optimization of phenolic compound extraction from Tunisian squash by-products: A sustainable approach for antioxidant and antibacterial applications
- Liupao tea aqueous extract alleviates dextran sulfate sodium-induced ulcerative colitis in rats by modulating the gut microbiota
- Toxicological qualities and detoxification trends of fruit by-products for valorization: A review
- Polyphenolic spectrum of cornelian cherry fruits and their health-promoting effect
- Optimizing the encapsulation of the refined extract of squash peels for functional food applications: A sustainable approach to reduce food waste
- Advancements in curcuminoid formulations: An update on bioavailability enhancement strategies curcuminoid bioavailability and formulations
- Impact of saline sprouting on antioxidant properties and bioactive compounds in chia seeds
- The dilemma of food genetics and improvement
- Bioengineering and Biotechnology
- Impact of hyaluronic acid-modified hafnium metalorganic frameworks containing rhynchophylline on Alzheimer’s disease
- Emerging patterns in nanoparticle-based therapeutic approaches for rheumatoid arthritis: A comprehensive bibliometric and visual analysis spanning two decades
- Application of CRISPR/Cas gene editing for infectious disease control in poultry
- Preparation of hafnium nitride-coated titanium implants by magnetron sputtering technology and evaluation of their antibacterial properties and biocompatibility
- Preparation and characterization of lemongrass oil nanoemulsion: Antimicrobial, antibiofilm, antioxidant, and anticancer activities
- Corrigendum
- Corrigendum to “Utilization of convolutional neural networks to analyze microscopic images for high-throughput screening of mesenchymal stem cells”
- Corrigendum to “Effects of Ire1 gene on virulence and pathogenicity of Candida albicans”
- Retraction
- Retraction of “Down-regulation of miR-539 indicates poor prognosis in patients with pancreatic cancer”
Articles in the same Issue
- Biomedical Sciences
- Mechanism of triptolide regulating proliferation and apoptosis of hepatoma cells by inhibiting JAK/STAT pathway
- Maslinic acid improves mitochondrial function and inhibits oxidative stress and autophagy in human gastric smooth muscle cells
- Comparative analysis of inflammatory biomarkers for the diagnosis of neonatal sepsis: IL-6, IL-8, SAA, CRP, and PCT
- Post-pandemic insights on COVID-19 and premature ovarian insufficiency
- Proteome differences of dental stem cells between permanent and deciduous teeth by data-independent acquisition proteomics
- Optimizing a modified cetyltrimethylammonium bromide protocol for fungal DNA extraction: Insights from multilocus gene amplification
- Preliminary analysis of the role of small hepatitis B surface proteins mutations in the pathogenesis of occult hepatitis B infection via the endoplasmic reticulum stress-induced UPR-ERAD pathway
- Efficacy of alginate-coated gold nanoparticles against antibiotics-resistant Staphylococcus and Streptococcus pathogens of acne origins
- Battling COVID-19 leveraging nanobiotechnology: Gold and silver nanoparticle–B-escin conjugates as SARS-CoV-2 inhibitors
- Neurodegenerative diseases and neuroinflammation-induced apoptosis
- Impact of fracture fixation surgery on cognitive function and the gut microbiota in mice with a history of stroke
- COLEC10: A potential tumor suppressor and prognostic biomarker in hepatocellular carcinoma through modulation of EMT and PI3K-AKT pathways
- High-temperature requirement serine protease A2 inhibitor UCF-101 ameliorates damaged neurons in traumatic brain-injured rats by the AMPK/NF-κB pathway
- SIK1 inhibits IL-1β-stimulated cartilage apoptosis and inflammation in vitro through the CRTC2/CREB1 signaling
- Rutin–chitooligosaccharide complex: Comprehensive evaluation of its anti-inflammatory and analgesic properties in vitro and in vivo
- Knockdown of Aurora kinase B alleviates high glucose-triggered trophoblast cells damage and inflammation during gestational diabetes
- Calcium-sensing receptors promoted Homer1 expression and osteogenic differentiation in bone marrow mesenchymal stem cells
- ABI3BP can inhibit the proliferation, invasion, and epithelial–mesenchymal transition of non-small-cell lung cancer cells
- Changes in blood glucose and metabolism in hyperuricemia mice
- Rapid detection of the GJB2 c.235delC mutation based on CRISPR-Cas13a combined with lateral flow dipstick
- IL-11 promotes Ang II-induced autophagy inhibition and mitochondrial dysfunction in atrial fibroblasts
- Short-chain fatty acid attenuates intestinal inflammation by regulation of gut microbial composition in antibiotic-associated diarrhea
- Application of metagenomic next-generation sequencing in the diagnosis of pathogens in patients with diabetes complicated by community-acquired pneumonia
- NAT10 promotes radiotherapy resistance in non-small cell lung cancer by regulating KPNB1-mediated PD-L1 nuclear translocation
- Phytol-mixed micelles alleviate dexamethasone-induced osteoporosis in zebrafish: Activation of the MMP3–OPN–MAPK pathway-mediating bone remodeling
- Association between TGF-β1 and β-catenin expression in the vaginal wall of patients with pelvic organ prolapse
- Primary pleomorphic liposarcoma involving bilateral ovaries: Case report and literature review
- Effects of de novo donor-specific Class I and II antibodies on graft outcomes after liver transplantation: A pilot cohort study
- Sleep architecture in Alzheimer’s disease continuum: The deep sleep question
- Ephedra fragilis plant extract: A groundbreaking corrosion inhibitor for mild steel in acidic environments – electrochemical, EDX, DFT, and Monte Carlo studies
- Langerhans cell histiocytosis in an adult patient with upper jaw and pulmonary involvement: A case report
- Inhibition of mast cell activation by Jaranol-targeted Pirin ameliorates allergic responses in mouse allergic rhinitis
- Aeromonas veronii-induced septic arthritis of the hip in a child with acute lymphoblastic leukemia
- Clusterin activates the heat shock response via the PI3K/Akt pathway to protect cardiomyocytes from high-temperature-induced apoptosis
- Research progress on fecal microbiota transplantation in tumor prevention and treatment
- Low-pressure exposure influences the development of HAPE
- Stigmasterol alleviates endplate chondrocyte degeneration through inducing mitophagy by enhancing PINK1 mRNA acetylation via the ESR1/NAT10 axis
- AKAP12, mediated by transcription factor 21, inhibits cell proliferation, metastasis, and glycolysis in lung squamous cell carcinoma
- Association between PAX9 or MSX1 gene polymorphism and tooth agenesis risk: A meta-analysis
- A case of bloodstream infection caused by Neisseria gonorrhoeae
- Case of nasopharyngeal tuberculosis complicated with cervical lymph node and pulmonary tuberculosis
- p-Cymene inhibits pro-fibrotic and inflammatory mediators to prevent hepatic dysfunction
- GFPT2 promotes paclitaxel resistance in epithelial ovarian cancer cells via activating NF-κB signaling pathway
- Transfer RNA-derived fragment tRF-36 modulates varicose vein progression via human vascular smooth muscle cell Notch signaling
- RTA-408 attenuates the hepatic ischemia reperfusion injury in mice possibly by activating the Nrf2/HO-1 signaling pathway
- Decreased serum TIMP4 levels in patients with rheumatoid arthritis
- Sirt1 protects lupus nephritis by inhibiting the NLRP3 signaling pathway in human glomerular mesangial cells
- Sodium butyrate aids brain injury repair in neonatal rats
- Interaction of MTHFR polymorphism with PAX1 methylation in cervical cancer
- Convallatoxin inhibits proliferation and angiogenesis of glioma cells via regulating JAK/STAT3 pathway
- The effect of the PKR inhibitor, 2-aminopurine, on the replication of influenza A virus, and segment 8 mRNA splicing
- Effects of Ire1 gene on virulence and pathogenicity of Candida albicans
- Small cell lung cancer with small intestinal metastasis: Case report and literature review
- GRB14: A prognostic biomarker driving tumor progression in gastric cancer through the PI3K/AKT signaling pathway by interacting with COBLL1
- 15-Lipoxygenase-2 deficiency induces foam cell formation that can be restored by salidroside through the inhibition of arachidonic acid effects
- FTO alleviated the diabetic nephropathy progression by regulating the N6-methyladenosine levels of DACT1
- Clinical relevance of inflammatory markers in the evaluation of severity of ulcerative colitis: A retrospective study
- Zinc valproic acid complex promotes osteoblast differentiation and exhibits anti-osteoporotic potential
- Primary pulmonary synovial sarcoma in the bronchial cavity: A case report
- Metagenomic next-generation sequencing of alveolar lavage fluid improves the detection of pulmonary infection
- Uterine tumor resembling ovarian sex cord tumor with extensive rhabdoid differentiation: A case report
- Genomic analysis of a novel ST11(PR34365) Clostridioides difficile strain isolated from the human fecal of a CDI patient in Guizhou, China
- Effects of tiered cardiac rehabilitation on CRP, TNF-α, and physical endurance in older adults with coronary heart disease
- Changes in T-lymphocyte subpopulations in patients with colorectal cancer before and after acupoint catgut embedding acupuncture observation
- Modulating the tumor microenvironment: The role of traditional Chinese medicine in improving lung cancer treatment
- Alterations of metabolites related to microbiota–gut–brain axis in plasma of colon cancer, esophageal cancer, stomach cancer, and lung cancer patients
- Research on individualized drug sensitivity detection technology based on bio-3D printing technology for precision treatment of gastrointestinal stromal tumors
- CEBPB promotes ulcerative colitis-associated colorectal cancer by stimulating tumor growth and activating the NF-κB/STAT3 signaling pathway
- Oncolytic bacteria: A revolutionary approach to cancer therapy
- A de novo meningioma with rapid growth: A possible malignancy imposter?
- Diagnosis of secondary tuberculosis infection in an asymptomatic elderly with cancer using next-generation sequencing: Case report
- Hesperidin and its zinc(ii) complex enhance osteoblast differentiation and bone formation: In vitro and in vivo evaluations
- Research progress on the regulation of autophagy in cardiovascular diseases by chemokines
- Anti-arthritic, immunomodulatory, and inflammatory regulation by the benzimidazole derivative BMZ-AD: Insights from an FCA-induced rat model
- Immunoassay for pyruvate kinase M1/2 as an Alzheimer’s biomarker in CSF
- The role of HDAC11 in age-related hearing loss: Mechanisms and therapeutic implications
- Evaluation and application analysis of animal models of PIPNP based on data mining
- Therapeutic approaches for liver fibrosis/cirrhosis by targeting pyroptosis
- Fabrication of zinc oxide nanoparticles using Ruellia tuberosa leaf extract induces apoptosis through P53 and STAT3 signalling pathways in prostate cancer cells
- Haplo-hematopoietic stem cell transplantation and immunoradiotherapy for severe aplastic anemia complicated with nasopharyngeal carcinoma: A case report
- Modulation of the KEAP1-NRF2 pathway by Erianin: A novel approach to reduce psoriasiform inflammation and inflammatory signaling
- The expression of epidermal growth factor receptor 2 and its relationship with tumor-infiltrating lymphocytes and clinical pathological features in breast cancer patients
- Innovations in MALDI-TOF Mass Spectrometry: Bridging modern diagnostics and historical insights
- BAP1 complexes with YY1 and RBBP7 and its downstream targets in ccRCC cells
- Hypereosinophilic syndrome with elevated IgG4 and T-cell clonality: A report of two cases
- Electroacupuncture alleviates sciatic nerve injury in sciatica rats by regulating BDNF and NGF levels, myelin sheath degradation, and autophagy
- Polydatin prevents cholesterol gallstone formation by regulating cholesterol metabolism via PPAR-γ signaling
- RNF144A and RNF144B: Important molecules for health
- Analysis of the detection rate and related factors of thyroid nodules in the healthy population
- Artesunate inhibits hepatocellular carcinoma cell migration and invasion through OGA-mediated O-GlcNAcylation of ZEB1
- Endovascular management of post-pancreatectomy hemorrhage caused by a hepatic artery pseudoaneurysm: Case report and review of the literature
- Efficacy and safety of anti-PD-1/PD-L1 antibodies in patients with relapsed refractory diffuse large B-cell lymphoma: A meta-analysis
- SATB2 promotes humeral fracture healing in rats by activating the PI3K/AKT pathway
- Overexpression of the ferroptosis-related gene, NFS1, corresponds to gastric cancer growth and tumor immune infiltration
- Understanding risk factors and prognosis in diabetic foot ulcers
- Atractylenolide I alleviates the experimental allergic response in mice by suppressing TLR4/NF-kB/NLRP3 signalling
- FBXO31 inhibits the stemness characteristics of CD147 (+) melanoma stem cells
- Immune molecule diagnostics in colorectal cancer: CCL2 and CXCL11
- Inhibiting CXCR6 promotes senescence of activated hepatic stellate cells with limited proinflammatory SASP to attenuate hepatic fibrosis
- Cadmium toxicity, health risk and its remediation using low-cost biochar adsorbents
- Pulmonary cryptococcosis with headache as the first presentation: A case report
- Solitary pulmonary metastasis with cystic airspaces in colon cancer: A rare case report
- RUNX1 promotes denervation-induced muscle atrophy by activating the JUNB/NF-κB pathway and driving M1 macrophage polarization
- Morphometric analysis and immunobiological investigation of Indigofera oblongifolia on the infected lung with Plasmodium chabaudi
- The NuA4/TIP60 histone-modifying complex and Hr78 modulate the Lobe2 mutant eye phenotype
- Experimental study on salmon demineralized bone matrix loaded with recombinant human bone morphogenetic protein-2: In vitro and in vivo study
- A case of IgA nephropathy treated with a combination of telitacicept and half-dose glucocorticoids
- Analgesic and toxicological evaluation of cannabidiol-rich Moroccan Cannabis sativa L. (Khardala variety) extract: Evidence from an in vivo and in silico study
- Wound healing and signaling pathways
- Combination of immunotherapy and whole-brain radiotherapy on prognosis of patients with multiple brain metastases: A retrospective cohort study
- To explore the relationship between endometrial hyperemia and polycystic ovary syndrome
- Research progress on the impact of curcumin on immune responses in breast cancer
- Biogenic Cu/Ni nanotherapeutics from Descurainia sophia (L.) Webb ex Prantl seeds for the treatment of lung cancer
- Dapagliflozin attenuates atrial fibrosis via the HMGB1/RAGE pathway in atrial fibrillation rats
- Glycitein alleviates inflammation and apoptosis in keratinocytes via ROS-associated PI3K–Akt signalling pathway
- ADH5 inhibits proliferation but promotes EMT in non-small cell lung cancer cell through activating Smad2/Smad3
- Apoptotic efficacies of AgNPs formulated by Syzygium aromaticum leaf extract on 32D-FLT3-ITD human leukemia cell line with PI3K/AKT/mTOR signaling pathway
- Novel cuproptosis-related genes C1QBP and PFKP identified as prognostic and therapeutic targets in lung adenocarcinoma
- Bee venom promotes exosome secretion and alters miRNA cargo in T cells
- Treatment of pure red cell aplasia in a chronic kidney disease patient with roxadustat: A case report
- Comparative bioinformatics analysis of the Wnt pathway in breast cancer: Selection of novel biomarker panels associated with ER status
- Kynurenine facilitates renal cell carcinoma progression by suppressing M2 macrophage pyroptosis through inhibition of CASP1 cleavage
- RFX5 promotes the growth, motility, and inhibits apoptosis of gastric adenocarcinoma cells through the SIRT1/AMPK axis
- ALKBH5 exacerbates early cardiac damage after radiotherapy for breast cancer via m6A demethylation of TLR4
- Phytochemicals of Roman chamomile: Antioxidant, anti-aging, and whitening activities of distillation residues
- Circadian gene Cry1 inhibits the tumorigenicity of hepatocellular carcinoma by the BAX/BCL2-mediated apoptosis pathway
- The TNFR-RIPK1/RIPK3 signalling pathway mediates the effect of lanthanum on necroptosis of nerve cells
- Longitudinal monitoring of autoantibody dynamics in patients with early-stage non-small-cell lung cancer undergoing surgery
- The potential role of rutin, a flavonoid, in the management of cancer through modulation of cell signaling pathways
- Construction of pectinase gene engineering microbe and its application in tobacco sheets
- Construction of a microbial abundance prognostic scoring model based on intratumoral microbial data for predicting the prognosis of lung squamous cell carcinoma
- Sepsis complicated by haemophagocytic lymphohistiocytosis triggered by methicillin-resistant Staphylococcus aureus and human herpesvirus 8 in an immunocompromised elderly patient: A case report
- Sarcopenia in liver transplantation: A comprehensive bibliometric study of current research trends and future directions
- Advances in cancer immunotherapy and future directions in personalized medicine
- Can coronavirus disease 2019 affect male fertility or cause spontaneous abortion? A two-sample Mendelian randomization analysis
- Heat stroke associated with novel leukaemia inhibitory factor receptor gene variant in a Chinese infant
- PSME2 exacerbates ulcerative colitis by disrupting intestinal barrier function and promoting autophagy-dependent inflammation
- Hyperosmolar hyperglycemic state with severe hypernatremia coexisting with central diabetes insipidus: A case report and literature review
- Efficacy and mechanism of escin in improving the tissue microenvironment of blood vessel walls via anti-inflammatory and anticoagulant effects: Implications for clinical practice
- Merkel cell carcinoma: Clinicopathological analysis of three patients and literature review
- Genetic variants in VWF exon 26 and their implications for type 1 Von Willebrand disease in a Saudi Arabian population
- Lipoxin A4 improves myocardial ischemia/reperfusion injury through the Notch1-Nrf2 signaling pathway
- High levels of EPHB2 expression predict a poor prognosis and promote tumor progression in endometrial cancer
- Knockdown of SHP-2 delays renal tubular epithelial cell injury in diabetic nephropathy by inhibiting NLRP3 inflammasome-mediated pyroptosis
- Exploring the toxicity mechanisms and detoxification methods of Rhizoma Paridis
- Concomitant gastric carcinoma and primary hepatic angiosarcoma in a patient: A case report
- Ecology and Environmental Science
- Optimization and comparative study of Bacillus consortia for cellulolytic potential and cellulase enzyme activity
- The complete mitochondrial genome analysis of Haemaphysalis hystricis Supino, 1897 (Ixodida: Ixodidae) and its phylogenetic implications
- Epidemiological characteristics and risk factors analysis of multidrug-resistant tuberculosis among tuberculosis population in Huzhou City, Eastern China
- Indices of human impacts on landscapes: How do they reflect the proportions of natural habitats?
- Genetic analysis of the Siberian flying squirrel population in the northern Changbai Mountains, Northeast China: Insights into population status and conservation
- Diversity and environmental drivers of Suillus communities in Pinus sylvestris var. mongolica forests of Inner Mongolia
- Global assessment of the fate of nitrogen deposition in forest ecosystems: Insights from 15N tracer studies
- Fungal and bacterial pathogenic co-infections mainly lead to the assembly of microbial community in tobacco stems
- Influencing of coal industry related airborne particulate matter on ocular surface tear film injury and inflammatory factor expression in Sprague-Dawley rats
- Temperature-dependent development, predation, and life table of Sphaerophoria macrogaster (Thomson) (Diptera: Syrphidae) feeding on Myzus persicae (Sulzer) (Homoptera: Aphididae)
- Eleonora’s falcon trophic interactions with insects within its breeding range: A systematic review
- Agriculture
- Integrated analysis of transcriptome, sRNAome, and degradome involved in the drought-response of maize Zhengdan958
- Variation in flower frost tolerance among seven apple cultivars and transcriptome response patterns in two contrastingly frost-tolerant selected cultivars
- Heritability of durable resistance to stripe rust in bread wheat (Triticum aestivum L.)
- Molecular mechanism of follicular development in laying hens based on the regulation of water metabolism
- Animal Science
- Effect of sex ratio on the life history traits of an important invasive species, Spodoptera frugiperda
- Plant Sciences
- Hairpin in a haystack: In silico identification and characterization of plant-conserved microRNA in Rafflesiaceae
- Widely targeted metabolomics of different tissues in Rubus corchorifolius
- The complete chloroplast genome of Gerbera piloselloides (L.) Cass., 1820 (Carduoideae, Asteraceae) and its phylogenetic analysis
- Field trial to correlate mineral solubilization activity of Pseudomonas aeruginosa and biochemical content of groundnut plants
- Correlation analysis between semen routine parameters and sperm DNA fragmentation index in patients with semen non-liquefaction: A retrospective study
- Plasticity of the anatomical traits of Rhododendron L. (Ericaceae) leaves and its implications in adaptation to the plateau environment
- Effects of Piriformospora indica and arbuscular mycorrhizal fungus on growth and physiology of Moringa oleifera under low-temperature stress
- Effects of different sources of potassium fertiliser on yield, fruit quality and nutrient absorption in “Harward” kiwifruit (Actinidia deliciosa)
- Comparative efficiency and residue levels of spraying programs against powdery mildew in grape varieties
- The DREB7 transcription factor enhances salt tolerance in soybean plants under salt stress
- Using plant electrical signals of water hyacinth (Eichhornia crassipes) for water pollution monitoring
- Food Science
- Phytochemical analysis of Stachys iva: Discovering the optimal extract conditions and its bioactive compounds
- Review on role of honey in disease prevention and treatment through modulation of biological activities
- Computational analysis of polymorphic residues in maltose and maltotriose transporters of a wild Saccharomyces cerevisiae strain
- Optimization of phenolic compound extraction from Tunisian squash by-products: A sustainable approach for antioxidant and antibacterial applications
- Liupao tea aqueous extract alleviates dextran sulfate sodium-induced ulcerative colitis in rats by modulating the gut microbiota
- Toxicological qualities and detoxification trends of fruit by-products for valorization: A review
- Polyphenolic spectrum of cornelian cherry fruits and their health-promoting effect
- Optimizing the encapsulation of the refined extract of squash peels for functional food applications: A sustainable approach to reduce food waste
- Advancements in curcuminoid formulations: An update on bioavailability enhancement strategies curcuminoid bioavailability and formulations
- Impact of saline sprouting on antioxidant properties and bioactive compounds in chia seeds
- The dilemma of food genetics and improvement
- Bioengineering and Biotechnology
- Impact of hyaluronic acid-modified hafnium metalorganic frameworks containing rhynchophylline on Alzheimer’s disease
- Emerging patterns in nanoparticle-based therapeutic approaches for rheumatoid arthritis: A comprehensive bibliometric and visual analysis spanning two decades
- Application of CRISPR/Cas gene editing for infectious disease control in poultry
- Preparation of hafnium nitride-coated titanium implants by magnetron sputtering technology and evaluation of their antibacterial properties and biocompatibility
- Preparation and characterization of lemongrass oil nanoemulsion: Antimicrobial, antibiofilm, antioxidant, and anticancer activities
- Corrigendum
- Corrigendum to “Utilization of convolutional neural networks to analyze microscopic images for high-throughput screening of mesenchymal stem cells”
- Corrigendum to “Effects of Ire1 gene on virulence and pathogenicity of Candida albicans”
- Retraction
- Retraction of “Down-regulation of miR-539 indicates poor prognosis in patients with pancreatic cancer”

