Abstract
Malignant pleural effusion (MPE) is a serious complication of advanced tumor, with relatively high morbidity and mortality rates, and can severely affect the quality of life and survival of patients. The mechanisms of MPE development are not well defined, but much research has been conducted to gain a deeper understanding of this process. In recent decades, although great progress has been made in the management of MPE, the diagnosis and treatment of MPE are still major challenges for clinicians. In this article, we provide a review of the research advances in the mechanisms of MPE development, diagnosis and treatment approaches. We aim to offer clinicians an overview of the latest evidence on the management of MPE, which should be individualized to provide comprehensive interventions for patients in accordance with their wishes, health status, prognosis and other factors.
1 Introduction
Malignant pleural effusion (MPE) is a pleural effusion (PE) that is caused by a malignant tumor originating in the pleura or by a metastatic malignant tumor from another site that has invaded the pleura [1]. Almost all advanced malignant tumors can invade the pleura and cause MPE. Among the tumors that cause MPE, adenocarcinoma is the most common pathological type, and lung cancer is the most common cause, leading to approximately 1/3 of all MPEs, followed by breast cancer, lymphoma and malignant mesothelioma [2]. Lung cancer is currently the most prevalent malignancy with the highest morbidity and mortality rates globally, and 50–60% of lung cancer patients already have advanced disease at the time of diagnosis. Approximately 10–15% of patients with advanced lung cancer at the initial diagnosis are affected by MPE [3], and the incidence of MPE among re-diagnosed patients is even higher, at more than 50% [4]. Each year, there are one hundred and fifty thousand new cases of MPE in the USA and one hundred thousand in Europe [2,5]. The development of MPE indicates that the tumor has spread or progressed to an advanced stage, and significantly shortening the patients’ survival. The median survival duration of patients at the first diagnosis of MPE is only 3–12 months [6].
In recent decades, research on the mechanisms of MPE has progressed, but there is a lack of effective diagnostic methods and treatments. The management of MPE is currently focused on relieving the symptoms of dyspnea, but the efficacy of such approaches is poor, and patients experience a high recurrence rate and many adverse effects. As molecular targeted therapies have been developed, new diagnostic procedures and treatments are available for patients with advanced tumors. Therefore, it is meaningful to explore new diagnostic and therapeutic treatments for MPE to enhance the quality of life and prolong the survival of patients with MPE. In this article, we review the mechanisms of MPE development, and progress made in diagnosis and treatment techniques.
2 Mechanism and composition of MPE
In the past few years, the mechanisms of MPE development have been increasingly studied and have shifted from a single factor, initially considered to be a blockage of lymphatic return, in favor of a combination of multiple factors, even down to the level of molecular mechanisms. A variety of cells are present in the pleural cavity microenvironment, including host cells (e.g., pleural mesothelial cells and endothelial cells) as well as cells of myeloid origin and the lymphatic system, which interact with tumor cells to accelerate angiogenesis and increase vascular permeability and inflammatory responses in tumor tissues, ultimately leading to the development of MPE [7,8]. MPE is the result of integrated interactions between host and tumor cells, as summarized by Stathopoulos and Kalomenidis [7]. Many effector molecules, from either the host or tumor cells, are involved in its pathogenesis. These effectors can generally be classified into two categories, including immunoregulatory effectors and modulators, which increase vascular permeability (Figure 1). The immunoregulatory factors include interleukin (IL)-2, tumor necrosis factor (TNF) and interferons. Important regulators of the induction of vascular permeability are vascular endothelial growth factor (VEGF), matrix metalloproteinases (MMPs) [9]. Among these effector regulators, VEGF plays a central role in PEs [10].
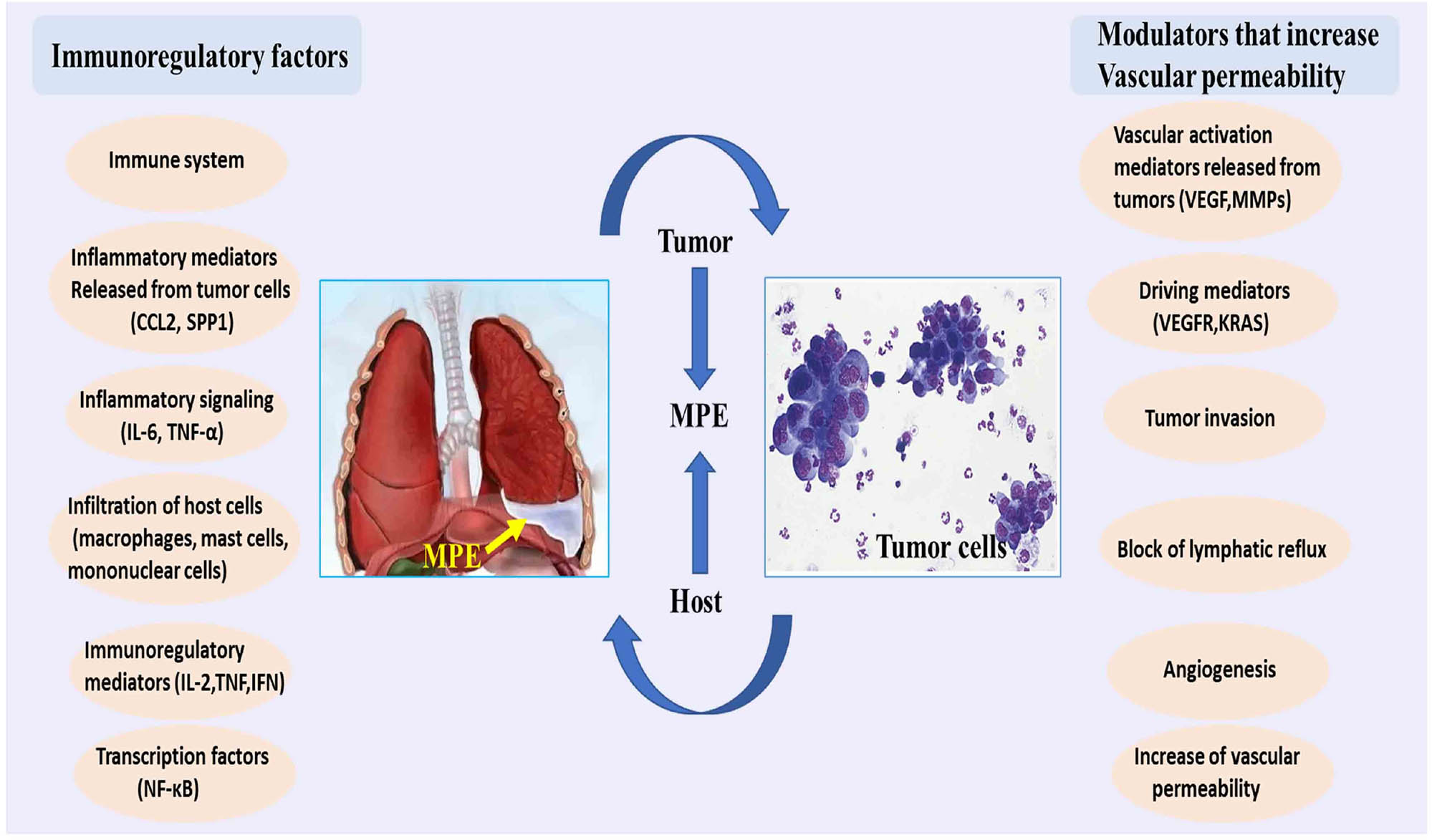
Pathogenesis of MPE. Many effector molecules from host cells or tumor cells are involved in the pathogenesis of MPE. These effectors can generally be divided into two categories. The first kind of effector molecules are important immune regulatory factors, including IL-2, TNF and interferons (IFNs). The second group of effector molecules is an effective regulator to increase vascular permeability, including VEGF, MMPs and many other molecules. CCL, IL, KRAS, MMPs, TNF; VEGF and VEGFR.
MPE is mostly hematogenous, massive, rapidly, growing composed of lymphocytes with protein content more than 30 g/L and LDH more than 500 U/L [11,12]. Approximately 40–90% of MPEs have been found to contain malignant tumor cells. Malignant tumor cells in MPE often have enlarged nuclei of different sizes, aberrant nuclei, and hyperchromatic nuclei. If the range of pleural lesions is widespread, it is difficult for glucose and acidic metabolites to penetrate the pleura. Both glucose and pH are low, indicating that the tumor is widely infiltrated and the patient’s survival time is short [13,14].
2.1 Tumor angiogenesis and increased vascular permeability
Tumor angiogenesis and increased vascular permeability are vital factors in the formation of MPE. VEGF has been found to maintain endothelial cell survival through tyrosine phosphorylation of focal adhesion kinase, which plays a key role in the chemotactic response of VEGF and can also influence angiogenic signaling pathways, unlike in benign PE [10,15]. VEGF is mainly mediated by vascular endothelial growth factor receptor 2 (VEGFR-2), which promotes increased vascular permeability by disrupting endothelial cell integrity, disrupting junctions and increasing cellular gaps [16]. Angiopoietin 1/2, a factor secreted by tumor cells, also has a role in promoting increased vascular permeability [17]. In addition, it has been shown that mast cells have a significant effect on the formation of MPE and that the release of trypsin-α/β1 and interleukin-1β increases pulmonary vascular permeability and induces the activation of inhibiting nuclear transcription factor (NF-κB) in the pulmonary vasculature, promoting fluid accumulation and tumor growth [18]. The above findings provide new directions for the treatment of MPE, and therapeutic approaches targeting increased tumor angiogenesis and permeability, such as a recombinant human vascular endothelial inhibitors and VEGF monoclonal antibodies, have improved efficacy in the treatment of MPE.
2.2 Immune microenvironment
Due to the increasing interest in the cellular microenvironment and immune responses, there has been increasing attention on the immune microenvironment of the MPE locus, including the interaction of immune cells, cytokines and tumor cells, which together form a microenvironment that promotes MPE development. Mononuclear macrophages are the main immunoinflammatory cells involved in MPE formation, and CD14+ macrophages are specifically highly expressed in MPE and therefore can serve as an immunodiagnostic marker for MPE [19]. Principe et al. showed that autocrine Interleukin-6 (IL-6) from tumor cells promoted MPE development by inducing activation of the Stat3 pathway and upregulating VEGF expression [20]. In addition, the number of Th1, Th17, Th9 and Th22 cells, which also play a role in the PE microenvironment by secreting cytokines, was increased in MPE compared to in peripheral blood [21]. In addition, chemokine (CC motif) ligand 20 (CCL20) and CCL22 can recruit peripheral blood Th17 cells to infiltrate the pleural space [22]. Thus, an imbalance of immune cells can also induce angiogenesis, increase vascular permeability, and promote the development of tumor metastasis and inflammatory responses, ultimately fostering the formation of MPE.
3 MPE diagnosis
3.1 Chest ultrasonography
Ultrasound of the chest is recommended to examine PE, and is an accurate indicator of the volume and depth of PE, the presence of contralateral PE, echogenicity, compartmentalization, intracavitary effusion, presence of pleural thickening and nodules, and diaphragm position and motion [23]. Metastatic pleural tumors show the typical ultrasound findings of relatively small hypoechoic crystalloid-like masses, blunt chest wall margins, or masses or nodules with complex echogenic intensity [24]. Only 9% of patients with nonmalignant PE present with this phenomenon. Another retrospective study analyzing the ultrasound characteristics of 104 patients with MPE found that 95 (91.35%) had nonmalignant PE, and nine (8.65%) had MPE, additionally the pleural nodules with intercostal wall thickening >10 mm and diaphragmatic thickening >7 mm were significant predictors of MPE on ultrasound (sensitivity 73% and specificity 100%) [25]. Both studies indicated that on ultrasound, pleural thickening, nodules and non-encapsulated effusions are reliable indicators for diagnosing MPE. The use of ultrasound guidance during pleural surgery can result in greater success rates and a reduced risk of complications, including parenchymatous organ injury. Ultrasound guidance also provides valuable information about the accessibility of the PE sac, and Doppler imaging helps to localize and avoid intercostal vessel injury prior to pleural intervention, contributing to a reduction in complications [23].
3.2 Computed tomography (CT)
Chest CT can be useful in identifying benign and malignant pleural diseases, including through signs such as thickening of the wall pleura or mediastinal pleura greater than 1 cm. Irregular pleural cavities and pleural nodules suggest a high probability of MPE with a high specificity (88–94%) but low sensitivity (36–51%), and approximately 50% of patients with MPE show no pleural abnormalities on CT [26,27]. Chest CT should be performed before the fluid is completely drained so that the pleural phase contrast can be used to obtain better clarity to better visualize pleural abnormalities [28]. Mediastinal and pleural thickening and pleural nodules suggest a possible MPE [27]. Although CT scans may not necessarily reveal abnormalities other than PE, CT scans can also provide evidence of underlying primary tumor and metastases.
3.3 Positron emission tomography-computed tomography (PET-CT)
The fluorodeoxyglucose PET imaging is based on the different metabolism between normal and abnormal tissues, in which the metabolism of fluorodeoxyglucose is accelerated and reflected by higher uptake in tumor cells; however, this method has a false-positive rate in the presence of metabolically active inflammation and infection [29]. Although its popularity influenced by false-positive results for inflammation and infection, PET-CT can be applied to stage pleural disease [30]. Nonetheless, one study showed that PET-CT can identify benign and MPE with a sensitivity of 83.3% and specificity of 92.2% and developed and validated a PET-CT parameter score, which can help physicians distinguish PE [31].
3.4 Cytology
The criteria for the diagnosis of MPE are the detection of cancer cells by pleural fluid cytology or the detection of cancer cells by pleural biopsy. Cytological diagnosis is used as a traditional diagnostic tool, but its sensitivity is not high if there are few tumor cells [32]. Several studies have shown that the sensitivity of pleural fluid cytology is approximately 40–87%, with low positive rates. The volume of cytological fluid extracted by diagnostic thoracentesis is currently controversial, and some studies have shown that at least 75 mL of pleural fluid is required for cytopathological diagnosis [15]. The sensitivity of a pleural fluid cytology sample taken in the first thoracentesis for the diagnosis of malignancy is 60%, with an increased sensitivity of 27% in the second procedure, but after the third, the diagnostic rate no longer increases, and the additional procedure instead delays diagnosis and treatment [33]. The use of cytology in combination with pleural biopsy increases the sensitivity of the diagnosis [34]. Although pleural fluid cytology is the least invasive, slowest and least effective method for diagnosing malignancy, the cytological diagnosis is also dependent on the underlying primary tumor, sample preparation and the experience of the cytologist [1].
3.5 Pleural biopsy
Pleural biopsy is the gold standard for the diagnosis of MPE [6]. In CT-guided or ultrasound-guided biopsies can be performed to collect pleural tissue for diagnosis, and this method has a sensitivity of 76–88% and specificity of up to 100% for the diagnosis of MPE [6]. When pleural thickening >1 cm is found in MPE, the diagnostic sensitivity of CT-guided pleural biopsy is comparable to that of thoracoscopy (96 versus 95%) [35]. Pleural biopsy in addition to of pleural fluid cytology can increase the diagnostic sensitivity for MPE by 7–27% [27]. When pleural thickening is obvious, pleural biopsy via thoracoscopic surgery can help simultaneously visualize the pleura, biopsy the involved area and drain the effusion. In addition, if the pleura is infiltrated and there is no trapped lung, pleural fixation can be performed [23].
3.6 Medical thoracoscopy (MT)
MT is both a diagnostic and a therapeutic method, and this method has a sensitivity of 92–97% and a specificity of 99–100% for the diagnosis of MPE [36,37]. The indications for MT, from a diagnostic point of view, include: cytologically negative and predominantly lymphocytic exudate, and the need for tumor staging, for additional tissue for molecular analysis, and to identify lung cancer, breast cancer and mesothelioma; from a therapeutic point of view, the goals of MT include pleural fixation by spraying in talcum powder, and drainage of MPE, especially complex pneumonia-like MPE, and the absolute contraindications, include extensive adhesions of the lung to the mural pleura, hypercapnia, severe dyspnea, uncontrollable cough, and myocardial infarction within the last 4 weeks [38]. Endoscopic thoracoscopy is a safe procedure with low complications and mortality rates and high diagnostic performance. Procedures requiring general anesthesia are very useful if more invasive procedures, such as video-assisted thoracic surgery (VATS), are performed for patients considered unsuitable for surgery or who are at increased risk for complications [39,40]. These procedures (medical or surgical thoracoscopy) have similar performances, with low mortality and major complication rates (between 0–0.34% and 1.2–1.8%, respectively [41,42].
3.7 Liquid biopsy
Gene expression of different tumors has become a pillar of diagnosis, therapeutic monitoring and precise medical guidelines. Numerous studies on liquid biopsies have demonstrated this diagnostic utility of this method in diagnosing disease, predicting prognosis and detecting cell-free deoxyribonucleic acid (DNA) in plasma [43]. MPE is often enriched with tumor cells, and extracellular vesicles and cell-free DNA are the two main targets currently explored in MPE. Therefore, MPE can be used as a source of biomarkers for the study of tumor mutations in liquid biopsies. Compared to tissue biopsy, the liquid biopsy method is less invasive and can show dynamic changes in the tumor in real time by using circulating biomarkers, including cell-free DNA, circulating tumor DNA, extracellular vesicles, messenger ribonucleic acid (mRNA), micro-ribonucleic acid (miRNA), circulating tumor cells and exosomes [44–46]. With the continuous development of detection technologies, multigene sequencing and second-generation sequencing (NGS) methods to detect the differences between mutations in pleural fluid and tissue specimens are also a hot topic of research [47,48]. Lin et al. simultaneously collected pleural fluid and plasma specimens from 63 patients and extracted free DNA and precipitated cell-free DNA from the pleural fluid supernatant and cell precipitate, respectively. All samples were analyzed through received NGS for 416 cancer-associated genes and showed that in cohort 1 with matched tumor tissues, 93.1% of tissue-assayed driver mutations were detected in MPE cell-free DNA, including activin-like kinase (ALK), v-raf murine sarcoma viral oncogene homolog B1, EGFR, kirsten rats arcomaviral oncogene homolog (KRAS), neuro kinin, neurofibromin 1, phosphatidylinositol-4,5-bisphosphate 3-kinase catalytic subunit alpha and proto-oncogene tyrosine-protein kinase receptor ret, whereas only 62.1% were detected in plasma cell-free DNA [49]. PE cell-free DNA had the highest detection rate of EGFR mutations in the entire cohort (71% overall, 68 and 59% for PE cell-free DNA and plasma cell-free DNA, respectively) [50]. In bleeding or cytology-negative PE samples, PE cell-free DNA had a higher sensitivity for mutation detection than plasma cell-free DNA. This suggests that MPE sampling could be a potential alternative to liquid biopsies and that genetic analysis of disease by detecting circulating tumor cells and exosomes in PEs could be explored in the future [51,52]. In addition, the different sensitivities and specificities of different sequencing platforms still require further study in clinical studies and standardization and are worthy of further investigation in the future.
3.8 MPE diagnostic summary
The sensitivity of the first PE cytology sample to diagnose malignant tumors was 60%, and the sensitivity of the second PE cytology sample increased by 27% [53]. However, after the third pleural puncture, the diagnostic rate would not increase, and the diagnosis and treatment would be delayed. Therefore, when the second cytological examination is negative yet MPE is highly suspected, the next step should be imaging guided pleural biopsy or thoracoscopic pleural biopsy. It has been reported that pleural biopsy based on pleural fluid cytology can increase the diagnostic rate of MPE by 7–27% [54]. The sensitivity of ultrasound or CT guided pleural biopsy was higher than that of blind pleural biopsy. The sensitivity of ultrasound guided pleural biopsy in the diagnosis of MPE was 70–94% [54]. Some studies believed that five-eight needles of image guided pleural biopsy have high diagnostic sensitivity, and six needles are recommended at least [53]. The sensitivity and specificity of MT in the diagnosis of MPE were 92–97.0 and 99–100%, respectively, which were similar to those of VATS [36]. The methods for diagnosing MPE and its causes are increasingly updated, which has improved the diagnostic accuracy of MPE to a certain extent, but they still have certain limitations. It is still to be confirmed by prospective studies with large samples to determine whether any better or integrated approach, which can make the diagnosis more accurate in the future.
4 Management of MPE
The aim of MPE treatment is to relieve symptoms such as dyspnea, improve quality of life and prolong survival. The British Thoracic Society guidelines for the management of MPE and the American Thoracic Society (ATS) guidelines recommend that patients with MPE should be observed for only if the MPE is asymptomatic [55], and that for symptomatic patients, it should first be determined if their symptoms are related to MPE, and these patients should be assessed for lung distension [4]. Treatments for MPE currently include therapeutic pleurodesis, chemical pleural fixation, thoracoscopic pleural fixation, long-term tube drainage, pleurodesis and thoraco-abdominal shunts. Pleural fixation and thoracic drainage are the two most commonly used methods in clinical practice. It is also worth exploring whether a difference exists in the efficacy of tyrosine kinase inhibit (TKI) therapy for patients with EGFR mutations and MPE and intrathecal therapy in combination with TKI, as the standard first-line treatment option for patients with EGFR mutations [56].
4.1 Thoracentesis
Thoracentesis is the most commonly used clinical modality to treat MPE and provides rapid relief of dyspnea symptoms; furthermore, confirmatory evidence of diagnosis can be obtained by thoracentesis in more than two-third of patients [57]. Repeated thoracentesis may be considered for patients with short expected survival duration and those who are unable to tolerate more invasive procedures and treatments, but clinicians need to adequately prevent the various complications that may arise from repeated thoracentesis, such as infection, bleeding and pneumothorax. The timing and scope of thoracentesis depends on the type and location of the primary tumor and the general condition of the patient. In the early stages of MPE, the effusion can be left untreated, but a clear diagnosis is needed as soon as possible, while progressive MPE needs to be treated promptly; otherwise, the patients are prone to developing irreversible pulmonary atelectasis and lung atrophy. Repeat chest CT or X-ray is required after thoracentesis to avoid medically induced pneumothorax or hemothorax [4]. Care should also be taken to avoid the rapid extraction of fluid by thoracentesis. Rapidly extracting more than 1.5 L of fluid from the pleural cavity in a 24 h period may result in redundant pulmonary edema in the affected lung, a complication that has a mortality rate of up to 20%, so it is recommended that each thoracentesis aspiration be limited to 1.0–1.5 L [4]. Successful thoracentesis can provide the patient with a clear diagnosis of MPE, as well as rapid recovery from the compressed lung tissue, which is relevant to the success of subsequent chemical pleural fixation [58].
4.2 Pleurodesis
The purpose of pleural fixation is to induce an inflammatory response in the pleura, forcing the two layers of the pleura to adhere in order to prevent fluid accumulation. The main focus of pleural fixation is the choice of sclerosing agents, including chemotherapeutic agents, bio-immunotherapy agents, talc, iodophor, silver nitrate, herbal preparations and autologous blood. Of these, talc is the most widely used and effective pleural fixation agent [23]. A thin flexible catheter is placed under ultrasound or CT guidance and secured to the chest wall, and a drainage bag or water seal bottle is attached to drain the pleural fluid; these devices have the advantage of being easy to operate, safe and not especially painful for the patient. Adequate chest drainage can be followed by the intrapleural application of antitumor drugs (e.g., bleomycin) or nontumor drugs (e.g., talcum powder) as sclerosing agents and adhesives to achieve pleural fixation. As the most commonly used clinical pleural adhesion agent, medical talc has the advantages of a high success rate for pleural fixation (approximately 93%) and low cost [59]. Talc can be injected into the chest cavity not only through a drainage tube, but also as a dry powder that can be sprayed uniformly throughout the chest cavity during surgical thoracoscopy [60]. The most significant side effect of pleural fixation is a local inflammatory response in the pleura leading to fever and chest pain, and pleural inflammation is thought to be directly related to successful pleural fixation, although a recent analysis of the TIME 1 trial dataset showed no difference in pain scores between patients with successful and unsuccessful pleural fixation, and elevated C-reactive protein levels were associated with successful pleural fixation [61]. Other rare complications include local infection, chest sepsis, arrhythmias, cardiac arrest, myocardial infarction and hypotension. Complications such as acute respiratory distress syndrome, acute pneumonia, and respiratory failure have also been occasionally reported [60]. In a multicenter retrospective study, none of the 558 patients who underwent pleural fixation with talc developed acute respiratory distress syndrome [62], and another study showed that pleural fixation with talc resulted in a lower recurrence rate for pleural fluid than pleural fixation with bleomycin (relative risk [RR] 0.64; 95% confidence interval [CI] 0.34–1.20), compared with the use of a talc solution. Spraying dry talc powder resulted in more effective fixation of the pleura and a lower recurrence rate for pleural fluid (RR 0.21; 95% CI 0.05–0.93) than other pleural fixation methods [63]. Nonrandomized studies have shown that patients who underwent successful pleural fixation survived longer than those who did not, which may indicate a biological role for pleural fluid in cancer progression [64]. A recent meta-analysis found no correlation between large and smallbore chest drains for successful pleural fixation between groups of patients [65]. Other factors such as turning the patient after sclerotherapy injection, intermittent open chest tube drainage and the application of multiple chest tube drains did not lead to a difference in fixation outcomes.
4.3 Indwelling pleural catheter (IPC)
The IPC is a silicone catheter placed in the pleural cavity and is carried through a subcutaneous tunnel. It has a cuff at the distal end that forms fibrous adhesions in the subcutaneous tissue over time, holding the IPC in place and preventing ascending infection. The IPC is discharged through a vacuum bottle with a one-way valve that uses negative suction to monitor flow and volume. The IPC offers the advantage of outpatient/home management of MPE and has gained great popularity in the last decade due to the reduction in hospital admission time [66–68]. A meta-analysis of 1,348 patients with MPE treated with IPC showed that 95.6% of patients had improved dyspnea symptoms and 45.6% had spontaneous pleural adhesions after a mean of 52 days [69]. Given their ease of insertion and management, IPC has become the management modality of choice in many centers around the world. However, IPC is associated with a higher rate of complications, among which, the complication of greatest concern is pleural infection, particularly in patients receiving chemotherapy [70]. In a large multicenter study of 1,021 patients with IPC, pleural infections occurred in 50 (4.9%) patients, 94% of whom had a mortality rate of less than 0.3%, with the mortalities being associated with the control of pleural infections by antibiotics [71]. In patients with irreversible atelectasis or pulmonary atrophy due to prolonged fluid compression or recurrent massive MPE following chest tube drainage, chest tube drainage may not adequately and effectively drain the pleural fluid; additionally, if the patient requires outpatient treatment or treatment at home with a tube, chest tube drainage may be a suitable alternative to closed chest tube drainage because it requires more medical care (e.g., tube management). However, closed chest drainage can be used as an alternative to chest tube drainage [70,72], allowing patients to be more easily treated in outpatient clinics with easier care [73]. A drain thicker than a subclavian venipuncture tube can be placed subcutaneously for a longer distance, which reduces the chance of infection, and several studies have shown that closed chest drains are safe and effective, with a treatment efficiency of approximately 90% and low rate of long-term complications (including pain, local cellulitis and chest tube dislodgement) [74]. Additionally, approximately 26–58% of patients develop spontaneous pleural fixation and eventually have their chest tubes removed after a period of closed chest drainage [75]. In a single-center retrospective study from the Netherlands, 17 patients with recurrent MPE underwent closed chest drainage, with 70–80% of patients experiencing significant symptomatic relief. The mean indwelling time of the tube was 2.3 months (range 1–6 months), and the mean drainage volume was 360 ml (range 150–1,000 mL) [76]. For patients requiring long-term drainage, the overall results of closed chest drainage are satisfactory and can significantly improve patient quality of life.
4.4 Anti-angiogenic agents
In recent years, intracavitary biotherapy has been a hot research topic in MPE treatment. Domestic studies have confirmed that recombinant human vascular endothelial inhibitor combined with the intracavitary administration of chemotherapy can control malignant plasma cavity effusion with a control rate of approximately 60% [77], suggesting the promising application of anti-angiogenic drugs in the treatment of malignant thoracic and abdominal effusion; moreover, combinations with other thoracic drugs (cisplatin, etc.) have improved efficiency compared with single drugs. Bevacizumab is a recombinant humanized monoclonal antibody that binds to VEGF, thereby preventing neovascularization [78]. Du et al. reported that among 72 patients with MPE were randomly assigned to an intracavitary bevacizumab combined with cisplatin group and groups, combination treatment was more effective than treatment with a single agent (83.3 vs 50.0%, P < 0.05), leading to prolonged progression-free survival (PFS) 5.3 vs 4.5 months, P < 0.05), with a trend toward longer overall survival (OS) [79]. In a study by Tao et al. [80] 21 patients with advanced lung adenocarcinoma with MPE treated with bevacizumab in combination with chemotherapy (paclitaxel in combination with platinum, gemcitabine in combination with platinum and pemetrexed alone) had a median PFS and median OS of 7.8 and 25.8 months, respectively. The MPE control rates at weeks 6, 12, 24, 48 and 96 were 95.2, 90.0, 89.5, 73.7 and 43.8%, respectively. Thus, bevacizumab, whether administered intrathecally or intravenously, may be more effective in controlling MPE than chemotherapy alone.
4.5 EGFR-TKI targeted agents
Most non-small cell lung cancer (NSCLC) patients are in advanced stage at the time of diagnosis, and the probability of accepting surgical resection is less than 30% [3]. Among them, patients with EGFR gene mutation and echinoderm microtubule-associated protein-like 4 (EML4-ALK) gene rearrangement can use targeted drug therapy [81,82]. Several studies have now established EGFR-TKI as the treatment of choice in patients with EGFR mutations [83]. It is worth considering whether intrathecal drugs can control MPE patients better with EGFR mutations and MPE, or whether receiving single-agent TKI therapy can control MPE while avoiding the adverse effects of intrathecal drugs such as fever, bone marrow suppression and chest pain. Kashiwabara et al. [56] analyzed the efficacy of EGFR-TKI in combination with talcum powder in patients with MPE and lung adenocarcinoma, 34 of whom received TKI as first-line therapy. It was suggested that TKI-targeted therapy combined with pleural fixation is more effective than pleural fixation alone in controlling MPE in patients with EGFR mutations and MPE. EGFR-TKIs treatment can significantly improve the prognosis of patients with advanced NSCLC, especially those with EGFR gene mutation. However, a retrospective study showed that the response of PE of lung cancer patients with EGFR mutation and MPE to EGFR-TKIs (including gefitinib, alfatinib and oxitinib) was worse than that of solid malignant tumors [84]. In NSCLC patients, anaplastic lymphoma kinase (ALK) gene or ROS proto-oncogene 1, receptor tyrosine kinase (ROS1) rearrangement accounts for 5 and 1%, respectively [85]. They are sensitive to the treatment of coxotinib, seretinib, aletinib and bugatinib. Compared with chemotherapy, all ALK inhibitors can significantly improve the PFS of lung cancer patients in this group. Compared with coxotinib and seretinib, aletinib and bugatinib can better improve the PFS of patients, especially in patients with advanced stage [86,87]. However, there is no large clinical study confirmed that the prognosis of patients with advanced lung cancer with MPE is different from that of patients with advanced lung cancer without MPE.
4.6 The thoracoperitoneal shunt
For patients whose lungs cannot be expanded or trapped due to MPE, a thoracoabdominal shunt tube can be placed, which is a subcutaneous tunnel from the chest to the abdomen [88]. The liquid is pumped manually, but due to the limited capacity of the pump chamber, it needs to be pumped frequently [89]. A retrospective study on thoracoperitoneal shunt showed that the remission rate was 95%, but the complication rate was 15%, including technical failure and infection [90]. The presence of ascites is a contraindication of thoracoperitoneal shunt.
4.7 Biological agent treatment
The commonly used biological agents in clinic are mainly IL-2 and TNF [91]. IL-2 is a thymus dependent lymphocyte growth factor, which can induce the secretion of interferon and a variety of cytokines, including promoting the long-term survival of T cells, enhancing the killing activity of T cells, promoting the proliferation and activation of natural killer (NK) cells, lymphokine activated killer cells, tumor infiltrating lymphocyte cells, etc. [92]. It is clinically used for tumor adjuvant therapy and the treatment of cancerous PE. Studies have shown that the use of IL-2 alone or in combination with other anti-cancer therapies can bring survival benefits to patients with advanced cancer. TNF-α is a cytokine secreted by monocytes/macrophages [93]. Its anti-tumor mechanisms mainly include directly killing tumor cells to induce tumor cell apoptosis, anti-tumor angiogenesis and enhancing immune function. TNF-α thoracic perfusion therapy for MPE has shown good efficacy whether alone or in combination [94]. The clinical application is limited due to its expensive price, high fever and other side effects.
4.8 Immunotherapy
Immunotherapy consists mainly of immune cell therapy and immune checkpoint (programmed death-1/programmed cell death-ligand-1 and cytotoxic T lymphocyte-associated antigen-4) inhibitor therapy [95,96]. Intrathoracic autoimmune cell infusion therapy is an alternative approach to control MPE, and the effectiveness correlates with a higher frequency of peripheral blood effector T cells [97]. Although the efficacy is limited, it is less adverse, well tolerated, and not limited by the patient’s liver or kidney function status or physical status score, and has good promise in the palliative treatment of MPE. For advanced non-squamous NSCLC and squamous lung cancer with negative driver genes, including patients with combined MPE, immune checkpoint inhibitors alone or in combination with chemotherapy and anti-angiogenic drugs can improve patient prognosis [98].
5 Future directions
Most of the interest is the early translational work which shows that the proliferation of cancer cell culture is promoted by seeding cells in pleural fluid [99]. This growth-promoting property of pleural fluid opens up the possibility that pleural fluid may not be a bystander to malignant disease, requiring only drainage to relieve symptoms, but may be an active promoter of cancer progression, thus emphasizing the importance of early control of PE. Current treatment strategies are focused on mechanical drainage and pleural cavity sealing [28]; however, significant efforts should be directed toward more complex areas of biomarker analysis and validation, and subsequent treatment with intrapleural immune agents and targeted therapies, for many years to come. If successful, this therapeutic strategy has the potential to bring about real step change in the management of MPE [100]. However, there are significant challenges in this regard, especially the research evidence that the clinical heterogeneity of MPE depends on primary tumors and intrapleural therapy. So far, the results of MPE are mixed.
6 Prognosis
Researchers have investigated several predictors of survival in patients with MPE. The most established method for predicting the prognosis of MPE patients is the LENT score [101] which includes the human l-lactate dehydrogenase (L-LDH) level, Eastern Cooperative Oncology Group (E-ECOG), N-neutrophil to lymphocyte ratio, T-tumor type and divides patients into low (score 0–1), moderate (score 2–4) or high (5–7) risk with a median survival of 319, 130 and 44 days. Additionally, as the LENT score (Table 1) has been developed using patients presenting with their first episode of MPE, regardless of previous cancer treatment, it is widely applicable and relevant in the clinical setting. It not only guides the treatment of MPE, but also helps predict the survival of MPE patients. It is the first validated risk stratification system for predicting the survival of MPE patients and is superior to ECOG performance status alone in predicting survival in individual patients.
The LENT score calculation
| Variable | Score | ||
|---|---|---|---|
| L -LDH level in pleural fluid (IU/L) | <1,500 | 0 | |
| >1,500 | 1 | ||
| E-ECOG PS | 0 | 0 | |
| 1 | 1 | ||
| 2 | 2 | ||
| 3–4 | 3 | ||
| N-NLR | <9 | 0 | |
| >9 | 1 | ||
| T-tumor type | Lowest risk tumor types | Mesothelioma hematological malignancy | 0 |
| Moderate risk tumor types | Breast cancer gynecological cancer | 1 | |
| Highest risk tumor types | Renal cell carcinoma | ||
| Lung cancer other tumors types | 2 | ||
| Total score | |||
| Risk categories | Low risk | 0–1 | |
| Moderate risk | 2–4 | ||
| High risk | 5–7 |
Patients with MPE are a highly diverse group of patients, with great variation in primary tumor involvement (particularly the ability to expand the lungs), major comorbidities, performance status, expected survival and patient wishes. More patient-based studies are likely to be performed in the future. In addition to research studies on pain, dyspnea and quality of life as well as studies on supportive treatments such as exercise training, nutritional interventions and psychological support should be conducted and may play an important role for MPE and may also offer useful adjuncts to interventions for MPE. Adjunctive treatments, such as exercise and dietary interventions, may also be useful adjuncts to pleural interventions [102].
7 Conclusions
There have been significant advances in the management of MPE. However, patients with advanced malignancies remain severely ill. Recent discoveries in the pathophysiological mechanisms of MPE have highlighted the role of molecular factors and mutations in the disease. There remains a need for individualized treatment. Predictive scores in clinical practice help to determine prognosis and guide treatment.
The current treatment for MPE is individualized and multidisciplinary. Some patients in poor general condition, especially those with an expected survival of only a few weeks to a few months, typically opt for less invasive methods of pleural fluid control, such as repeated thoracentesis or closed chest drainage, which are ideal for reducing both the length of hospital stay and discomfort of the patient. With the continuous development of treatment techniques and tools, VATS techniques can not only relieve the clinical symptoms associated with MPE but also allow for clear pathological results and direct observation of tumors progression in the thoracic cavity, as well as facilitate various therapeutic operations such as pleurectomy and pleural fixation. Because it is performed under direct vision, surgical thoracoscopic pleural fixation is more uniform and thorough in spraying sclerosing or adhesive agents. This method is therefore more accurate, and a combination of treatments is recommended based on patient’s specific situation. In the near future, improved treatment for oncological disease and a better understanding of the pathophysiological mechanisms of MPE will help to improve the prognosis of patients with MPE. Many unanswered questions remain and ongoing research will help clinicians to enhance the care for this group of patients with MPE.
Acknowledgements
The authors would like to thank the anonymous reviewers for their contribution to the improvement of the manuscript.
-
Funding information: This work was supported by Science and Technology Development Plan Project of Jilin Province, China (No. 20200603006SF).
-
Author contributions: All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
-
Conflict of interest: Authors state no conflict of interest.
-
Data availability statement: The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
[1] Psallidas I, Kalomenidis I, Porcel JM, Robinson BW, Stathopoulos GT. Malignant pleural effusion: from bench to bedside. Eur Respir Rev. 2016;25:189–98.10.1183/16000617.0019-2016Search in Google Scholar PubMed PubMed Central
[2] Penz E, Watt KN, Hergott CA, Rahman NM, Psallidas I. Management of malignant pleural effusion: challenges and solutions. Cancer Manag Res. 2017;9:229–41.10.2147/CMAR.S95663Search in Google Scholar PubMed PubMed Central
[3] Siegel RL, Miller KD, Fuchs HE, Jemal A. Cancer statistics, 2022. CA Cancer J Clin. 2022;72:7–33.10.3322/caac.21708Search in Google Scholar PubMed
[4] Feller-Kopman DJ, Reddy CB, DeCamp MM, Diekemper RL, Gould MK, Henry T, et al. Management of malignant pleural effusions. An official ATS/STS/STR clinical practice guideline. Am J Respir Crit Care Med. 2018;198:839–49.10.1164/rccm.201807-1415STSearch in Google Scholar PubMed
[5] Shafiq M, Ma X, Taghizadeh N, Kharrazi H, Feller-Kopman DJ, Tremblay A, et al. Healthcare costs and utilization among patients hospitalized for malignant pleural effusion. Respiration. 2020;99:257–63.10.1159/000506210Search in Google Scholar PubMed
[6] Bibby AC, Dorn P, Psallidas I, Porcel JM, Janssen J, Froudarakis M, et al. ERS/EACTS statement on the management of malignant pleural effusions. Eur Respir J. 2018;52:1800349.10.1183/13993003.00349-2018Search in Google Scholar PubMed
[7] Stathopoulos GT, Kalomenidis I. Malignant pleural effusion: tumor–host interactions unleashed. Am J Respir Crit Care Med. 2012;186:487–92.10.1164/rccm.201203-0465PPSearch in Google Scholar PubMed PubMed Central
[8] Beaudoin S, Gonzalez AV. Evaluation of the patient with pleural effusion. CMAJ. 2018;190:E291–E95.10.1503/cmaj.170420Search in Google Scholar PubMed PubMed Central
[9] Hamed EA, El-Noweihi AM, Mohamed AZ, Mahmoud A. Vasoactive mediators (VEGF and TNF-alpha) in patients with malignant and tuberculous pleural effusions. Respirology. 2004;9:81–6.10.1111/j.1440-1843.2003.00529.xSearch in Google Scholar PubMed
[10] Chen Y, Mathy NW, Lu H. The role of VEGF in the diagnosis and treatment of malignant pleural effusion in patients with non‑small cell lung cancer (review). Mol Med Rep. 2018;17:8019–30.10.3892/mmr.2018.8922Search in Google Scholar PubMed PubMed Central
[11] Gupta R, Arul AO, Sasikumar JR, Prabhu AJ, James P. Imprint cytology of thoracoscopic pleural biopsy tissue for early etiological diagnosis of pleural effusion: a pilot study from India. J Bronchol Interv Pulmonol. 2021;28:98–102.10.1097/LBR.0000000000000724Search in Google Scholar PubMed
[12] Kulandaisamy PC, Kulandaisamy S, Kramer D, McGrath C. Malignant pleural effusions – a review of current guidelines and practices. J Clin Med. 2021;10:5535.10.3390/jcm10235535Search in Google Scholar PubMed PubMed Central
[13] Akram MJ, Khalid U, Ashraf MB, Bakar MA, Butt FM, Khan F. Predicting the survival in patients with malignant pleural effusion undergoing indwelling pleural catheter insertion. Ann Thorac Med. 2020;15:223–9.10.4103/atm.ATM_289_20Search in Google Scholar PubMed PubMed Central
[14] Gayen S. Malignant pleural effusion: presentation, diagnosis, and management. Am J Med. 2022;135:1188–92.10.1016/j.amjmed.2022.04.017Search in Google Scholar PubMed
[15] Wu DW, Chang WA, Liu KT, Yen MC, Kuo PL. Vascular endothelial growth factor and protein level in pleural effusion for differentiating malignant from benign pleural effusion. Oncol Lett. 2017;14:3657–62.10.3892/ol.2017.6631Search in Google Scholar PubMed PubMed Central
[16] Damianovich M, Hout Siloni G, Barshack I, Simansky DA, Kidron D, Dar E, et al. Structural basis for hyperpermeability of tumor vessels in advanced lung adenocarcinoma complicated by pleural effusion. Clin Lung Cancer. 2013;14:688–98.10.1016/j.cllc.2013.06.007Search in Google Scholar PubMed
[17] Fang SC, Zhang HT, Hu HD, Wang CY, Zhang YM. Effect of endostar combined with angiopoietin-2 inhibitor on malignant pleural effusion in mice. Med Oncol. 2015;32:410.10.1007/s12032-014-0410-0Search in Google Scholar PubMed
[18] Giannou AD, Marazioti A, Spella M, Kanellakis NI, Apostolopoulou H, Psallidas I, et al. Mast cells mediate malignant pleural effusion formation. J Clin Invest. 2015;125:2317–34.10.1172/JCI79840Search in Google Scholar PubMed PubMed Central
[19] Song Z, Luo W, Zheng H, Zeng Y, Wang J, Chen T. Translational nanotherapeutics reprograms immune microenvironment in malignant pleural effusion of lung adenocarcinoma. Adv Healthc Mater. 2021;10:e2100149.10.1002/adhm.202100149Search in Google Scholar PubMed
[20] Principe N, Kidman J, Lake RA, Lesterhuis WJ, Nowak AK, McDonnell AM, et al. Malignant pleural effusions-a window into local anti-tumor T cell immunity? Front Oncol. 2021;11:672747.10.3389/fonc.2021.672747Search in Google Scholar PubMed PubMed Central
[21] Muruganandan S, Azzopardi M, Thomas R, Fitzgerald DB, Kuok YJ, Cheah HM, et al. The pleural effusion and symptom evaluation (PLEASE) study of breathlessness in patients with a symptomatic pleural effusion. Eur Respir J. 2020;55:1900980.10.1183/13993003.00980-2019Search in Google Scholar PubMed
[22] Baas P, Scherpereel A, Nowak AK, Fujimoto N, Peters S, Tsao AS, et al. First-line nivolumab plus ipilimumab in unresectable malignant pleural mesothelioma (CheckMate 743): a multicentre, randomised, open-label, phase 3 trial. Lancet. 2021;397:375–86.10.1016/S0140-6736(20)32714-8Search in Google Scholar PubMed
[23] Desai NR, Lee HJ. Diagnosis and management of malignant pleural effusions: state of the art in 2017. J Thorac Dis. 2017;9:S1111–S22.10.21037/jtd.2017.07.79Search in Google Scholar PubMed PubMed Central
[24] Piskac Zivkovic N, Cikara I, Novak NP, Brkljacic B, Tudoric N. A retrospective study of ultrasound characteristics and macroscopic findings in confirmed malignant pleural effusion. Pulm Med. 2019;2019:5628267.10.1155/2019/5628267Search in Google Scholar PubMed PubMed Central
[25] Jiang B, Li XL, Yin Y, Zhang Q, Zang T, Song WS, et al. Ultrasound elastography: a novel tool for the differential diagnosis of pleural effusion. Eur Respir J. 2019;54:1802018.10.1183/13993003.02018-2018Search in Google Scholar PubMed
[26] Porcel JM, Pardina M, Bielsa S, Gonzalez A, Light RW. Derivation and validation of a CT scan scoring system for discriminating malignant from benign pleural effusions. Chest. 2015;147:513–9.10.1378/chest.14-0013Search in Google Scholar PubMed
[27] Asciak R, Rahman NM. Malignant pleural effusion: from diagnostics to therapeutics. Clin Chest Med. 2018;39:181–93.10.1016/j.ccm.2017.11.004Search in Google Scholar PubMed
[28] Jacobs B, Sheikh G, Youness HA, Keddissi JI, Abdo T. Diagnosis and management of malignant pleural effusion: a decade in review. Diagnostics (Basel). 2022;12:1016.10.3390/diagnostics12041016Search in Google Scholar PubMed PubMed Central
[29] Malik D. Comment on: “The FDG PET/CT score” for the diagnosis of malignant pleural effusion. Eur J Nucl Med Mol Imaging. 2020;47:5–6.10.1007/s00259-019-04512-3Search in Google Scholar PubMed
[30] Porcel JM, Hernandez P, Martinez-Alonso M, Bielsa S, Salud A. Accuracy of fluorodeoxyglucose-PET imaging for differentiating benign from malignant pleural effusions: a meta-analysis. Chest. 2015;147:502–12.10.1378/chest.14-0820Search in Google Scholar PubMed
[31] Yang MF, Tong ZH, Wang Z, Zhang YY, Xu LL, Wang XJ, et al. Development and validation of the PET-CT score for diagnosis of malignant pleural effusion. Eur J Nucl Med Mol Imaging. 2019;46:1457–67.10.1007/s00259-019-04287-7Search in Google Scholar PubMed PubMed Central
[32] Tang Y, Wang Z, Li Z, Kim J, Deng Y, Li Y, et al. High-throughput screening of rare metabolically active tumor cells in pleural effusion and peripheral blood of lung cancer patients. Proc Natl Acad Sci U S A. 2017;114:2544–9.10.1073/pnas.1612229114Search in Google Scholar PubMed PubMed Central
[33] Li S, You WJ, Zhang JC, Zhou Q, Shi HZ. Immune regulation of interleukin-27 in malignant pleural effusion. Chin Med J. 2015;128:1932–41.10.4103/0366-6999.160556Search in Google Scholar PubMed PubMed Central
[34] Herrera Lara S, Fernandez-Fabrellas E, Juan Samper G, Marco Buades J, Andreu Lapiedra R, Pinilla, et al. Predicting malignant and paramalignant pleural effusions by combining clinical, radiological and pleural fluid analytical parameters. Lung. 2017;195:653–60.10.1007/s00408-017-0032-3Search in Google Scholar PubMed
[35] Metintas M, Ak G, Dundar E, Yildirim H, Ozkan R, Kurt E, et al. Medical thoracoscopy vs CT scan-guided Abrams pleural needle biopsy for diagnosis of patients with pleural effusions: a randomized, controlled trial. Chest. 2010;137:1362–8.10.1378/chest.09-0884Search in Google Scholar PubMed
[36] Anevlavis S, Froudarakis ME. Advances in pleuroscopy. Clin Respir J. 2018;12:839–47.10.1111/crj.12597Search in Google Scholar PubMed
[37] Gokce M, Altinsoy B, Piskin O, Bahadir B. Uniportal VATS pleural biopsy in the diagnosis of exudative pleural effusion: awake or intubated? J Cardiothorac Surg. 2021;16:95.10.1186/s13019-021-01461-7Search in Google Scholar PubMed PubMed Central
[38] Bashour SI, Mankidy BJ, Lazarus DR. Update on the diagnosis and management of malignant pleural effusions. Respir Med. 2022;196:106802.10.1016/j.rmed.2022.106802Search in Google Scholar PubMed
[39] Yap KH, Phillips MJ, Lee YC. Medical thoracoscopy: rigid thoracoscopy or flexi-rigid pleuroscopy? Curr Opin Pulm Med. 2014;20:358–65.10.1097/MCP.0000000000000059Search in Google Scholar PubMed
[40] Tousheed SZ, Ranganatha R, Hemanth Kumar M, Manjunath PH, Philip DS, Punitha M, et al. Role of medical thoracoscopy in the diagnosis of pleural effusions. Indian J Tuberc. 2022;69:584–89.10.1016/j.ijtb.2021.09.005Search in Google Scholar PubMed
[41] Hooper C, Lee YC, Maskell N, Group , BTSPG. Investigation of a unilateral pleural effusion in adults: British Thoracic Society Pleural Disease guideline 2010. Thorax. 2010;65:4–17.10.1136/thx.2010.136978Search in Google Scholar PubMed
[42] Agarwal R, Aggarwal AN, Gupta D. Diagnostic accuracy and safety of semirigid thoracoscopy in exudative pleural effusions: a meta-analysis. Chest. 2013;144:1857–67.10.1378/chest.13-1187Search in Google Scholar PubMed
[43] Guo Z, Xie Z, Shi H, Du W, Peng L, Han W, et al. Malignant pleural effusion supernatant is an alternative liquid biopsy specimen for comprehensive mutational profiling. Thorac Cancer. 2019;10:823–31.10.1111/1759-7714.13006Search in Google Scholar PubMed PubMed Central
[44] Mathai RA, Vidya RVS, Reddy BS, Thomas L, Udupa K, Kolesar J, et al. Potential utility of liquid biopsy as a diagnostic and prognostic tool for the assessment of solid tumors: implications in the precision oncology. J Clin Med. 2019;8:373.10.3390/jcm8030373Search in Google Scholar PubMed PubMed Central
[45] Pasini L, Ulivi P. Liquid biopsy for the detection of resistance mechanisms in NSCLC: comparison of different blood biomarkers. J Clin Med. 2019;8:998.10.3390/jcm8070998Search in Google Scholar PubMed PubMed Central
[46] Shojaee S, Romano G, Sanchez TM, Yermakhanova G, Saviana M, Le P, et al. Extracellular vesicle microRNA in malignant pleural effusion. Genes. 2022;13:2159.10.3390/genes13112159Search in Google Scholar PubMed PubMed Central
[47] Chen J, Yang Y, Wang Z, Shen X, Zhang Z, Wang C, et al. A multicancer malignant pleural effusion diagnostic test using hexokinase 2 and single-cell sequencing. Clin Chem. 2022;68:680–90.10.1093/clinchem/hvac003Search in Google Scholar PubMed
[48] Fan X, Liu Y, Liang Z, Wang S, Yang J, Wu A. Diagnostic value of six tumor markers for malignant pleural effusion in 1,230 patients: a single-center retrospective study. Pathol Oncol Res. 2022;28:1610280.10.3389/pore.2022.1610280Search in Google Scholar PubMed PubMed Central
[49] Tong L, Ding N, Tong X, Li J, Zhang Y, Wang X, et al. Tumor-derived DNA from pleural effusion supernatant as a promising alternative to tumor tissue in genomic profiling of advanced lung cancer. Theranostics. 2019;9:5532–41.10.7150/thno.34070Search in Google Scholar PubMed PubMed Central
[50] Liu L, Zhan P, Zhou X, Song Y, Zhou X, Yu L, et al. Detection of EML4-ALK in lung adenocarcinoma using pleural effusion with FISH, IHC, and RT-PCR methods. PLoS One. 2015;10:e0117032.10.1371/journal.pone.0117032Search in Google Scholar PubMed PubMed Central
[51] Wang Z, Wu X, Han X, Cheng G, Mu X, Zhang Y, et al. ALK gene expression status in pleural effusion predicts tumor responsiveness to crizotinib in Chinese patients with lung adenocarcinoma. Chin J Cancer Res. 2016;28:606–16.10.21147/j.issn.1000-9604.2016.06.07Search in Google Scholar PubMed PubMed Central
[52] Baburaj G, Damerla RR, Udupa KS, Parida P, Munisamy M, Kolesar J, et al. Liquid biopsy approaches for pleural effusion in lung cancer patients. Mol Biol Rep. 2020;47:8179–87.10.1007/s11033-020-05869-7Search in Google Scholar PubMed
[53] Aboudara M, Maldonado F. Update in the management of pleural effusions. Med Clin North Am. 2019;103:475–85.10.1016/j.mcna.2018.12.007Search in Google Scholar PubMed
[54] Sachdeva A, Shepherd RW, Lee HJ. Thoracentesis and thoracic ultrasound. Clin Chest Med. 2013;34:1–9.10.1016/j.ccm.2012.11.005Search in Google Scholar PubMed
[55] Porcel JM, Gasol A, Bielsa S, Civit C, Light RW, Salud A. Clinical features and survival of lung cancer patients with pleural effusions. Respirology. 2015;20:654–9.10.1111/resp.12496Search in Google Scholar PubMed
[56] Kashiwabara K, Fuji S, Tsumura S, Sakamoto K. Prognosis of EGFR-mutant lung adenocarcinoma patients with malignant pleural effusion receiving first-line EGFR-TKI therapy without pleurodesis: a single-institute retrospective study. Anticancer Res. 2020;40:1117–21.10.21873/anticanres.14051Search in Google Scholar PubMed
[57] Ost DE, Niu J, Zhao H, Grosu HB, Giordano SH. Quality gaps and comparative effectiveness of management strategies for recurrent malignant pleural effusions. Chest. 2018;153:438–52.10.1016/j.chest.2017.08.026Search in Google Scholar PubMed PubMed Central
[58] Ferreiro L, Suarez-Antelo J, Alvarez-Dobano JM, Toubes ME, Riveiro V, Valdes L. Malignant pleural effusion: diagnosis and management. Can Respir J. 2020;2020:2950751.10.1155/2020/2950751Search in Google Scholar PubMed PubMed Central
[59] Hojski A, Leitgeb M, Crnjac A. Release of growth factors after mechanical and chemical pleurodesis for treatment of malignant pleural effusion: a randomized control study. Radiol Oncol. 2015;49:386–94.10.1515/raon-2015-0002Search in Google Scholar PubMed PubMed Central
[60] Bhatnagar R, Piotrowska HEG, Laskawiec-Szkonter M, Kahan BC, Luengo-Fernandez R, Pepperell JCT, et al. Effect of thoracoscopic talc poudrage vs talc slurry via chest tube on pleurodesis failure rate among patients with malignant pleural effusions: a randomized clinical trial. JAMA. 2020;323:60–9.10.1001/jama.2019.19997Search in Google Scholar PubMed PubMed Central
[61] Mercer RM, Macready J, Jeffries H, Speck N, Kanellakis NI, Maskell NA, et al. Clinically important associations of pleurodesis success in malignant pleural effusion: analysis of the TIME1 data set. Respirology. 2020;25:750–55.10.1111/resp.13755Search in Google Scholar PubMed
[62] Janssen JP, Collier G, Astoul P, Tassi GF, Noppen M, Rodriguez-Panadero F, et al. Safety of pleurodesis with talc poudrage in malignant pleural effusion: a prospective cohort study. Lancet. 2007;369:1535–9.10.1016/S0140-6736(07)60708-9Search in Google Scholar PubMed
[63] Tan C, Sedrakyan A, Browne J, Swift S, Treasure T. The evidence on the effectiveness of management for malignant pleural effusion: a systematic review. Eur J Cardiothorac Surg. 2006;29:829–38.10.1016/j.ejcts.2005.12.025Search in Google Scholar PubMed
[64] Hassan M, Mercer RM, Maskell NA, Asciak R, McCracken DJ, Bedawi EO, et al. Survival in patients with malignant pleural effusion undergoing talc pleurodesis. Lung Cancer. 2019;137:14–8.10.1016/j.lungcan.2019.09.003Search in Google Scholar PubMed
[65] Thethi I, Ramirez S, Shen W, Zhang D, Mohamad M, Kaphle U, et al. Effect of chest tube size on pleurodesis efficacy in malignant pleural effusion: a meta-analysis of randomized controlled trials. J Thorac Dis. 2018;10:355–62.10.21037/jtd.2017.11.134Search in Google Scholar PubMed PubMed Central
[66] Clive AO, Bhatnagar R, Psallidas I, Maskell NA. Individualised management of malignant pleural effusion. Lancet Respir Med. 2015;3:505–6.10.1016/S2213-2600(15)00183-6Search in Google Scholar PubMed
[67] Thomas R, Fysh ETH, Smith NA, Lee P, Kwan BCH, Yap E, et al. Effect of an indwelling pleural catheter vs talc pleurodesis on hospitalization days in patients with malignant pleural effusion: the AMPLE randomized clinical trial. JAMA. 2017;318:1903–12.10.1001/jama.2017.17426Search in Google Scholar PubMed PubMed Central
[68] Foo CT, Pulimood T, Knolle M, Marciniak SJ, Herre J. Ambulatory thoracoscopic pleurodesis combined with indwelling pleural catheter in malignant pleural effusion. Front Surg. 2021;8:738719.10.3389/fsurg.2021.738719Search in Google Scholar PubMed PubMed Central
[69] Iyer NP, Reddy CB, Wahidi MM, Lewis SZ, Diekemper RL, Feller-Kopman D, et al. Indwelling pleural catheter versus pleurodesis for malignant pleural effusions. A systematic review and meta-analysis. Ann Am Thorac Soc. 2019;16:124–31.10.1513/AnnalsATS.201807-495OCSearch in Google Scholar PubMed
[70] Asciak R, Hallifax RJ, Mercer RM, Hassan M, Wigston C, Wrightson JM, et al. The hospital and patient burden of indwelling pleural catheters: a retrospective case series of 210 indwelling pleural catheter insertions. Respiration. 2019;97:70–7.10.1159/000491934Search in Google Scholar PubMed
[71] Fysh ETH, Tremblay A, Feller-Kopman D, Mishra EK, Slade M, Garske L, et al. Clinical outcomes of indwelling pleural catheter-related pleural infections: an international multicenter study. Chest. 2013 Nov;144(5):1597–602.10.1378/chest.12-3103Search in Google Scholar PubMed
[72] Agrawal A, Murgu S. Multimodal approach to the management of malignant pleural effusions: role of thoracoscopy with pleurodesis and tunneled indwelling pleural catheters. J Thorac Dis. 2020;12:2803–11.10.21037/jtd.2020.03.57Search in Google Scholar PubMed PubMed Central
[73] Bibby AC, Clive AO, Slade GC, Morley AJ, Fallon J, Psallidas I, et al. Survival in patients with malignant pleural effusions who developed pleural infection: a retrospective case review from six UK centers. Chest. 2015;148:235–41.10.1136/thoraxjnl-2014-206260.123Search in Google Scholar
[74] Wahidi MM, Reddy C, Yarmus L, Feller-Kopman D, Musani A, Shepherd RW, et al. Randomized trial of pleural fluid drainage frequency in patients with malignant pleural effusions. The ASAP trial. Am J Respir Crit Care Med. 2017;195:1050–7.10.1164/rccm.201607-1404OCSearch in Google Scholar PubMed
[75] Lui MM, Thomas R, Lee YC. Complications of indwelling pleural catheter use and their management. BMJ Open Respir Res. 2016;3:e000123.10.1136/bmjresp-2015-000123Search in Google Scholar PubMed PubMed Central
[76] van den Toorn LM, Schaap E, Surmont VF, Pouw EM, van der Rijt KC, van Klaveren RJ. Management of recurrent malignant pleural effusions with a chronic indwelling pleural catheter. Lung Cancer. 2005;50:123–7.10.1016/j.lungcan.2005.05.016Search in Google Scholar PubMed
[77] Zhao WY, Chen DY, Chen JH, Ji ZN. Effects of intracavitary administration of Endostar combined with cisplatin in malignant pleural effusion and ascites. Cell Biochem Biophys. 2014;70:623–8.10.1007/s12013-014-9965-9Search in Google Scholar PubMed
[78] Donnenberg AD, Luketich JD, Dhupar R, Donnenberg VS. Treatment of malignant pleural effusions: the case for localized immunotherapy. J Immunother Cancer. 2019;7(1):110.10.1186/s40425-019-0590-4Search in Google Scholar PubMed PubMed Central
[79] Du N, Li X, Li F, Zhao H, Fan Z, Ma J, et al. Intrapleural combination therapy with bevacizumab and cisplatin for non-small cell lung cancer‑mediated malignant pleural effusion. Oncol Rep. 2013;29:2332–40.10.3892/or.2013.2349Search in Google Scholar PubMed
[80] Tao H, Meng Q, Li M, Shi L, Tang J, Liu Z. Outcomes of bevacizumab combined with chemotherapy in lung adenocarcinoma-induced malignant pleural effusion. Thorac Cancer. 2018;9:298–304.10.1111/1759-7714.12582Search in Google Scholar PubMed PubMed Central
[81] McCoach CE, Le AT, Gowan K, Jones K, Schubert L, Doak A, et al. Resistance mechanisms to targeted therapies in ROS1( +) and ALK( +) non-small cell lung cancer. Clin Cancer Res. 2018;24:3334–47.10.1158/1078-0432.CCR-17-2452Search in Google Scholar PubMed PubMed Central
[82] Tao J, Zheng C, Zhang C, Zhou L, Liu Z, Zhou Y, et al. First-line treatments for patients with advanced ALK gene rearrangements in NSCLC: a systematic review and network meta-analysis. J Int Med Res. 2022;50:1–14.10.1177/03000605221132703Search in Google Scholar PubMed PubMed Central
[83] Hibino M, Hiranuma O, Takemura Y, Katayama Y, Chihara Y, Harada T, et al. Osimertinib and bevacizumab cotreatment for untreated EGFR-mutated NSCLC with malignant pleural or pericardial effusion (SPIRAL II): a single-arm, open-label, phase 2 clinical trial. JTO Clin Res Rep. 2022;3:100424.10.1016/j.jtocrr.2022.100424Search in Google Scholar PubMed PubMed Central
[84] Yang J, Lee OJ, Son SM, Woo CG, Jeong Y, Yang Y, et al. EGFR mutation status in lung adenocarcinoma-associated malignant pleural effusion and efficacy of EGFR tyrosine kinase inhibitors. Cancer Res Treat. 2018;50:908–16.10.4143/crt.2017.378Search in Google Scholar PubMed PubMed Central
[85] Clinical Lung Cancer Genome P, Network Genomic M. A genomics-based classification of human lung tumors. Sci Transl Med. 2013;5:209ra153.10.1126/scitranslmed.3006802Search in Google Scholar PubMed PubMed Central
[86] Asao T, Takahashi F, Takahashi K. Resistance to molecularly targeted therapy in non-small-cell lung cancer. Respir Investig. 2019;57:20–6.10.1016/j.resinv.2018.09.001Search in Google Scholar PubMed
[87] Jiang J, Zhao C, Zhang F, Liu Z, Zhou K, Ren X, et al. ALK inhibitors in ALK-rearranged non-small cell lung cancer with and without brain metastases: systematic review and network meta-analysis. BMJ Open. 2022 Sep;12:e060782.10.1136/bmjopen-2022-060782Search in Google Scholar PubMed PubMed Central
[88] Clive AO, Jones HE, Bhatnagar R, Preston NJ, Maskell N. Interventions for the management of malignant pleural effusions: a network meta-analysis. Cochrane Database Syst Rev. 2016;2016:CD010529.10.1002/14651858.CD010529.pub2Search in Google Scholar PubMed PubMed Central
[89] Koegelenberg CFN, Shaw JA, Irusen EM, Lee YCG. Contemporary best practice in the management of malignant pleural effusion. Ther Adv Respir Dis. 2018;12:1–13.10.1177/1753466618785098Search in Google Scholar PubMed PubMed Central
[90] Saleh ME, Awad G, Sanad M. Chemical pleurodesis for malignant pleural effusion: which agent is perfect? Cardiothorac Surg. 2020;28:12.10.1186/s43057-020-00022-3Search in Google Scholar
[91] Zeng Y, Wang L, Zhou H, Qi Y. A meta-analysis of Th1 and Th2 cytokine profiles differentiating tuberculous from malignant pleural effusion. Sci Rep. 2022;12:2743.10.37766/inplasy2022.1.0005Search in Google Scholar
[92] Niu Y, Zhou Q. Th17 cells and their related cytokines: vital players in progression of malignant pleural effusion. Cell Mol Life Sci. 2022;79:194.10.1007/s00018-022-04227-zSearch in Google Scholar PubMed
[93] Hsu LH, Soong TC, Chu NM, Huang CY, Kao SH, Lin YF. The inflammatory cytokine profile of patients with malignant pleural effusion treated with pleurodesis. J Clin Med. 2020;9:4010.10.3390/jcm9124010Search in Google Scholar PubMed PubMed Central
[94] Fu T, Lin Y, Zeng Q, Yao W, Han L. Thoracic perfusion of recombinant mutant human tumor necrosis factor (rmhTNF) can be considered as a good adjunct in the treatment of malignant pleural effusion caused by lung cancer. BMC Pulm Med. 2020;20:175.10.1186/s12890-020-01210-xSearch in Google Scholar PubMed PubMed Central
[95] Liu Y, Wang L, Song Q, Ali M, Crowe WN, Kucera GL, et al. Intrapleural nano-immunotherapy promotes innate and adaptive immune responses to enhance anti-PD-L1 therapy for malignant pleural effusion. Nat Nanotechnol. 2022;17:206–16.10.1038/s41565-021-01032-wSearch in Google Scholar PubMed PubMed Central
[96] Wu J, Zhu R, Wang Z, Chen X, Xu T, Liu Y, et al. Exosomes in malignant pleural effusion from lung cancer patients impaired the cytotoxicity of double-negative T cells. Transl Oncol. 2023;27:101564.10.1016/j.tranon.2022.101564Search in Google Scholar PubMed PubMed Central
[97] Zhang S, Chen L, Zong Y, Li Q, Zhu K, Li Z, et al. Research progress of tumor-derived extracellular vesicles in the treatment of malignant pleural effusion. Cancer Med. 2022;00:1–12.10.1002/cam4.5005Search in Google Scholar PubMed PubMed Central
[98] Doroshow DB, Sanmamed MF, Hastings K, Politi K, Rimm DL, Chen L, et al. Immunotherapy in non-small cell lung cancer: facts and hopes. Clin Cancer Res. 2019;25:4592–602.10.1158/1078-0432.CCR-18-1538Search in Google Scholar PubMed PubMed Central
[99] Asciak R, Kanellakis NI, Yao X, Abd Hamid M, Mercer RM, Hassan M, et al. Pleural fluid has pro-growth biological properties which enable cancer cell proliferation. Front Oncol. 2021;11:658395.10.3389/fonc.2021.658395Search in Google Scholar PubMed PubMed Central
[100] Addala DN, Kanellakis NI, Bedawi EO, Dong T, Rahman NM. Malignant pleural effusion: updates in diagnosis, management and current challenges. Front Oncol. 2022;12:1053574.10.3389/fonc.2022.1053574Search in Google Scholar PubMed PubMed Central
[101] Clive AO, Kahan BC, Hooper CE, Bhatnagar R, Morley AJ, Zahan-Evans N, et al. Predicting survival in malignant pleural effusion: development and validation of the LENT prognostic score. Thorax. 2014;69:1098–104.10.1136/thoraxjnl-2014-205285Search in Google Scholar PubMed PubMed Central
[102] Fitzgerald DB, Koegelenberg CFN, Yasufuku K, Lee YCG. Surgical and non-surgical management of malignant pleural effusions. Expert Rev Respir Med. 2018;12:15–26.10.1080/17476348.2018.1398085Search in Google Scholar PubMed
© 2023 the author(s), published by De Gruyter
This work is licensed under the Creative Commons Attribution 4.0 International License.
Articles in the same Issue
- Biomedical Sciences
- Systemic investigation of inetetamab in combination with small molecules to treat HER2-overexpressing breast and gastric cancers
- Immunosuppressive treatment for idiopathic membranous nephropathy: An updated network meta-analysis
- Identifying two pathogenic variants in a patient with pigmented paravenous retinochoroidal atrophy
- Effects of phytoestrogens combined with cold stress on sperm parameters and testicular proteomics in rats
- A case of pulmonary embolism with bad warfarin anticoagulant effects caused by E. coli infection
- Neutrophilia with subclinical Cushing’s disease: A case report and literature review
- Isoimperatorin alleviates lipopolysaccharide-induced periodontitis by downregulating ERK1/2 and NF-κB pathways
- Immunoregulation of synovial macrophages for the treatment of osteoarthritis
- Novel CPLANE1 c.8948dupT (p.P2984Tfs*7) variant in a child patient with Joubert syndrome
- Antiphospholipid antibodies and the risk of thrombosis in myeloproliferative neoplasms
- Immunological responses of septic rats to combination therapy with thymosin α1 and vitamin C
- High glucose and high lipid induced mitochondrial dysfunction in JEG-3 cells through oxidative stress
- Pharmacological inhibition of the ubiquitin-specific protease 8 effectively suppresses glioblastoma cell growth
- Levocarnitine regulates the growth of angiotensin II-induced myocardial fibrosis cells via TIMP-1
- Age-related changes in peripheral T-cell subpopulations in elderly individuals: An observational study
- Single-cell transcription analysis reveals the tumor origin and heterogeneity of human bilateral renal clear cell carcinoma
- Identification of iron metabolism-related genes as diagnostic signatures in sepsis by blood transcriptomic analysis
- Long noncoding RNA ACART knockdown decreases 3T3-L1 preadipocyte proliferation and differentiation
- Surgery, adjuvant immunotherapy plus chemotherapy and radiotherapy for primary malignant melanoma of the parotid gland (PGMM): A case report
- Dosimetry comparison with helical tomotherapy, volumetric modulated arc therapy, and intensity-modulated radiotherapy for grade II gliomas: A single‑institution case series
- Soy isoflavone reduces LPS-induced acute lung injury via increasing aquaporin 1 and aquaporin 5 in rats
- Refractory hypokalemia with sexual dysplasia and infertility caused by 17α-hydroxylase deficiency and triple X syndrome: A case report
- Meta-analysis of cancer risk among end stage renal disease undergoing maintenance dialysis
- 6-Phosphogluconate dehydrogenase inhibition arrests growth and induces apoptosis in gastric cancer via AMPK activation and oxidative stress
- Experimental study on the optimization of ANM33 release in foam cells
- Primary retroperitoneal angiosarcoma: A case report
- Metabolomic analysis-identified 2-hydroxybutyric acid might be a key metabolite of severe preeclampsia
- Malignant pleural effusion diagnosis and therapy
- Effect of spaceflight on the phenotype and proteome of Escherichia coli
- Comparison of immunotherapy combined with stereotactic radiotherapy and targeted therapy for patients with brain metastases: A systemic review and meta-analysis
- Activation of hypermethylated P2RY1 mitigates gastric cancer by promoting apoptosis and inhibiting proliferation
- Association between the VEGFR-2 -604T/C polymorphism (rs2071559) and type 2 diabetic retinopathy
- The role of IL-31 and IL-34 in the diagnosis and treatment of chronic periodontitis
- Triple-negative mouse breast cancer initiating cells show high expression of beta1 integrin and increased malignant features
- mNGS facilitates the accurate diagnosis and antibiotic treatment of suspicious critical CNS infection in real practice: A retrospective study
- The apatinib and pemetrexed combination has antitumor and antiangiogenic effects against NSCLC
- Radiotherapy for primary thyroid adenoid cystic carcinoma
- Design and functional preliminary investigation of recombinant antigen EgG1Y162–EgG1Y162 against Echinococcus granulosus
- Effects of losartan in patients with NAFLD: A meta-analysis of randomized controlled trial
- Bibliometric analysis of METTL3: Current perspectives, highlights, and trending topics
- Performance comparison of three scaling algorithms in NMR-based metabolomics analysis
- PI3K/AKT/mTOR pathway and its related molecules participate in PROK1 silence-induced anti-tumor effects on pancreatic cancer
- The altered expression of cytoskeletal and synaptic remodeling proteins during epilepsy
- Effects of pegylated recombinant human granulocyte colony-stimulating factor on lymphocytes and white blood cells of patients with malignant tumor
- Prostatitis as initial manifestation of Chlamydia psittaci pneumonia diagnosed by metagenome next-generation sequencing: A case report
- NUDT21 relieves sevoflurane-induced neurological damage in rats by down-regulating LIMK2
- Association of interleukin-10 rs1800896, rs1800872, and interleukin-6 rs1800795 polymorphisms with squamous cell carcinoma risk: A meta-analysis
- Exosomal HBV-DNA for diagnosis and treatment monitoring of chronic hepatitis B
- Shear stress leads to the dysfunction of endothelial cells through the Cav-1-mediated KLF2/eNOS/ERK signaling pathway under physiological conditions
- Interaction between the PI3K/AKT pathway and mitochondrial autophagy in macrophages and the leukocyte count in rats with LPS-induced pulmonary infection
- Meta-analysis of the rs231775 locus polymorphism in the CTLA-4 gene and the susceptibility to Graves’ disease in children
- Cloning, subcellular localization and expression of phosphate transporter gene HvPT6 of hulless barley
- Coptisine mitigates diabetic nephropathy via repressing the NRLP3 inflammasome
- Significant elevated CXCL14 and decreased IL-39 levels in patients with tuberculosis
- Whole-exome sequencing applications in prenatal diagnosis of fetal bowel dilatation
- Gemella morbillorum infective endocarditis: A case report and literature review
- An unusual ectopic thymoma clonal evolution analysis: A case report
- Severe cumulative skin toxicity during toripalimab combined with vemurafenib following toripalimab alone
- Detection of V. vulnificus septic shock with ARDS using mNGS
- Novel rare genetic variants of familial and sporadic pulmonary atresia identified by whole-exome sequencing
- The influence and mechanistic action of sperm DNA fragmentation index on the outcomes of assisted reproduction technology
- Novel compound heterozygous mutations in TELO2 in an infant with You-Hoover-Fong syndrome: A case report and literature review
- ctDNA as a prognostic biomarker in resectable CLM: Systematic review and meta-analysis
- Diagnosis of primary amoebic meningoencephalitis by metagenomic next-generation sequencing: A case report
- Phylogenetic analysis of promoter regions of human Dolichol kinase (DOLK) and orthologous genes using bioinformatics tools
- Collagen changes in rabbit conjunctiva after conjunctival crosslinking
- Effects of NM23 transfection of human gastric carcinoma cells in mice
- Oral nifedipine and phytosterol, intravenous nicardipine, and oral nifedipine only: Three-arm, retrospective, cohort study for management of severe preeclampsia
- Case report of hepatic retiform hemangioendothelioma: A rare tumor treated with ultrasound-guided microwave ablation
- Curcumin induces apoptosis in human hepatocellular carcinoma cells by decreasing the expression of STAT3/VEGF/HIF-1α signaling
- Rare presentation of double-clonal Waldenström macroglobulinemia with pulmonary embolism: A case report
- Giant duplication of the transverse colon in an adult: A case report and literature review
- Ectopic thyroid tissue in the breast: A case report
- SDR16C5 promotes proliferation and migration and inhibits apoptosis in pancreatic cancer
- Vaginal metastasis from breast cancer: A case report
- Screening of the best time window for MSC transplantation to treat acute myocardial infarction with SDF-1α antibody-loaded targeted ultrasonic microbubbles: An in vivo study in miniswine
- Inhibition of TAZ impairs the migration ability of melanoma cells
- Molecular complexity analysis of the diagnosis of Gitelman syndrome in China
- Effects of maternal calcium and protein intake on the development and bone metabolism of offspring mice
- Identification of winter wheat pests and diseases based on improved convolutional neural network
- Ultra-multiplex PCR technique to guide treatment of Aspergillus-infected aortic valve prostheses
- Virtual high-throughput screening: Potential inhibitors targeting aminopeptidase N (CD13) and PIKfyve for SARS-CoV-2
- Immune checkpoint inhibitors in cancer patients with COVID-19
- Utility of methylene blue mixed with autologous blood in preoperative localization of pulmonary nodules and masses
- Integrated analysis of the microbiome and transcriptome in stomach adenocarcinoma
- Berberine suppressed sarcopenia insulin resistance through SIRT1-mediated mitophagy
- DUSP2 inhibits the progression of lupus nephritis in mice by regulating the STAT3 pathway
- Lung abscess by Fusobacterium nucleatum and Streptococcus spp. co-infection by mNGS: A case series
- Genetic alterations of KRAS and TP53 in intrahepatic cholangiocarcinoma associated with poor prognosis
- Granulomatous polyangiitis involving the fourth ventricle: Report of a rare case and a literature review
- Studying infant mortality: A demographic analysis based on data mining models
- Metaplastic breast carcinoma with osseous differentiation: A report of a rare case and literature review
- Protein Z modulates the metastasis of lung adenocarcinoma cells
- Inhibition of pyroptosis and apoptosis by capsaicin protects against LPS-induced acute kidney injury through TRPV1/UCP2 axis in vitro
- TAK-242, a toll-like receptor 4 antagonist, against brain injury by alleviates autophagy and inflammation in rats
- Primary mediastinum Ewing’s sarcoma with pleural effusion: A case report and literature review
- Association of ADRB2 gene polymorphisms and intestinal microbiota in Chinese Han adolescents
- Tanshinone IIA alleviates chondrocyte apoptosis and extracellular matrix degeneration by inhibiting ferroptosis
- Study on the cytokines related to SARS-Cov-2 in testicular cells and the interaction network between cells based on scRNA-seq data
- Effect of periostin on bone metabolic and autophagy factors during tooth eruption in mice
- HP1 induces ferroptosis of renal tubular epithelial cells through NRF2 pathway in diabetic nephropathy
- Intravaginal estrogen management in postmenopausal patients with vaginal squamous intraepithelial lesions along with CO2 laser ablation: A retrospective study
- Hepatocellular carcinoma cell differentiation trajectory predicts immunotherapy, potential therapeutic drugs, and prognosis of patients
- Effects of physical exercise on biomarkers of oxidative stress in healthy subjects: A meta-analysis of randomized controlled trials
- Identification of lysosome-related genes in connection with prognosis and immune cell infiltration for drug candidates in head and neck cancer
- Development of an instrument-free and low-cost ELISA dot-blot test to detect antibodies against SARS-CoV-2
- Research progress on gas signal molecular therapy for Parkinson’s disease
- Adiponectin inhibits TGF-β1-induced skin fibroblast proliferation and phenotype transformation via the p38 MAPK signaling pathway
- The G protein-coupled receptor-related gene signatures for predicting prognosis and immunotherapy response in bladder urothelial carcinoma
- α-Fetoprotein contributes to the malignant biological properties of AFP-producing gastric cancer
- CXCL12/CXCR4/CXCR7 axis in placenta tissues of patients with placenta previa
- Association between thyroid stimulating hormone levels and papillary thyroid cancer risk: A meta-analysis
- Significance of sTREM-1 and sST2 combined diagnosis for sepsis detection and prognosis prediction
- Diagnostic value of serum neuroactive substances in the acute exacerbation of chronic obstructive pulmonary disease complicated with depression
- Research progress of AMP-activated protein kinase and cardiac aging
- TRIM29 knockdown prevented the colon cancer progression through decreasing the ubiquitination levels of KRT5
- Cross-talk between gut microbiota and liver steatosis: Complications and therapeutic target
- Metastasis from small cell lung cancer to ovary: A case report
- The early diagnosis and pathogenic mechanisms of sepsis-related acute kidney injury
- The effect of NK cell therapy on sepsis secondary to lung cancer: A case report
- Erianin alleviates collagen-induced arthritis in mice by inhibiting Th17 cell differentiation
- Loss of ACOX1 in clear cell renal cell carcinoma and its correlation with clinical features
- Signalling pathways in the osteogenic differentiation of periodontal ligament stem cells
- Crosstalk between lactic acid and immune regulation and its value in the diagnosis and treatment of liver failure
- Clinicopathological features and differential diagnosis of gastric pleomorphic giant cell carcinoma
- Traumatic brain injury and rTMS-ERPs: Case report and literature review
- Extracellular fibrin promotes non-small cell lung cancer progression through integrin β1/PTEN/AKT signaling
- Knockdown of DLK4 inhibits non-small cell lung cancer tumor growth by downregulating CKS2
- The co-expression pattern of VEGFR-2 with indicators related to proliferation, apoptosis, and differentiation of anagen hair follicles
- Inflammation-related signaling pathways in tendinopathy
- CD4+ T cell count in HIV/TB co-infection and co-occurrence with HL: Case report and literature review
- Clinical analysis of severe Chlamydia psittaci pneumonia: Case series study
- Bioinformatics analysis to identify potential biomarkers for the pulmonary artery hypertension associated with the basement membrane
- Influence of MTHFR polymorphism, alone or in combination with smoking and alcohol consumption, on cancer susceptibility
- Catharanthus roseus (L.) G. Don counteracts the ampicillin resistance in multiple antibiotic-resistant Staphylococcus aureus by downregulation of PBP2a synthesis
- Combination of a bronchogenic cyst in the thoracic spinal canal with chronic myelocytic leukemia
- Bacterial lipoprotein plays an important role in the macrophage autophagy and apoptosis induced by Salmonella typhimurium and Staphylococcus aureus
- TCL1A+ B cells predict prognosis in triple-negative breast cancer through integrative analysis of single-cell and bulk transcriptomic data
- Ezrin promotes esophageal squamous cell carcinoma progression via the Hippo signaling pathway
- Ferroptosis: A potential target of macrophages in plaque vulnerability
- Predicting pediatric Crohn's disease based on six mRNA-constructed risk signature using comprehensive bioinformatic approaches
- Applications of genetic code expansion and photosensitive UAAs in studying membrane proteins
- HK2 contributes to the proliferation, migration, and invasion of diffuse large B-cell lymphoma cells by enhancing the ERK1/2 signaling pathway
- IL-17 in osteoarthritis: A narrative review
- Circadian cycle and neuroinflammation
- Probiotic management and inflammatory factors as a novel treatment in cirrhosis: A systematic review and meta-analysis
- Hemorrhagic meningioma with pulmonary metastasis: Case report and literature review
- SPOP regulates the expression profiles and alternative splicing events in human hepatocytes
- Knockdown of SETD5 inhibited glycolysis and tumor growth in gastric cancer cells by down-regulating Akt signaling pathway
- PTX3 promotes IVIG resistance-induced endothelial injury in Kawasaki disease by regulating the NF-κB pathway
- Pancreatic ectopic thyroid tissue: A case report and analysis of literature
- The prognostic impact of body mass index on female breast cancer patients in underdeveloped regions of northern China differs by menopause status and tumor molecular subtype
- Report on a case of liver-originating malignant melanoma of unknown primary
- Case report: Herbal treatment of neutropenic enterocolitis after chemotherapy for breast cancer
- The fibroblast growth factor–Klotho axis at molecular level
- Characterization of amiodarone action on currents in hERG-T618 gain-of-function mutations
- A case report of diagnosis and dynamic monitoring of Listeria monocytogenes meningitis with NGS
- Effect of autologous platelet-rich plasma on new bone formation and viability of a Marburg bone graft
- Small breast epithelial mucin as a useful prognostic marker for breast cancer patients
- Continuous non-adherent culture promotes transdifferentiation of human adipose-derived stem cells into retinal lineage
- Nrf3 alleviates oxidative stress and promotes the survival of colon cancer cells by activating AKT/BCL-2 signal pathway
- Favorable response to surufatinib in a patient with necrolytic migratory erythema: A case report
- Case report of atypical undernutrition of hypoproteinemia type
- Down-regulation of COL1A1 inhibits tumor-associated fibroblast activation and mediates matrix remodeling in the tumor microenvironment of breast cancer
- Sarcoma protein kinase inhibition alleviates liver fibrosis by promoting hepatic stellate cells ferroptosis
- Research progress of serum eosinophil in chronic obstructive pulmonary disease and asthma
- Clinicopathological characteristics of co-existing or mixed colorectal cancer and neuroendocrine tumor: Report of five cases
- Role of menopausal hormone therapy in the prevention of postmenopausal osteoporosis
- Precisional detection of lymph node metastasis using tFCM in colorectal cancer
- Advances in diagnosis and treatment of perimenopausal syndrome
- A study of forensic genetics: ITO index distribution and kinship judgment between two individuals
- Acute lupus pneumonitis resembling miliary tuberculosis: A case-based review
- Plasma levels of CD36 and glutathione as biomarkers for ruptured intracranial aneurysm
- Fractalkine modulates pulmonary angiogenesis and tube formation by modulating CX3CR1 and growth factors in PVECs
- Novel risk prediction models for deep vein thrombosis after thoracotomy and thoracoscopic lung cancer resections, involving coagulation and immune function
- Exploring the diagnostic markers of essential tremor: A study based on machine learning algorithms
- Evaluation of effects of small-incision approach treatment on proximal tibia fracture by deep learning algorithm-based magnetic resonance imaging
- An online diagnosis method for cancer lesions based on intelligent imaging analysis
- Medical imaging in rheumatoid arthritis: A review on deep learning approach
- Predictive analytics in smart healthcare for child mortality prediction using a machine learning approach
- Utility of neutrophil–lymphocyte ratio and platelet–lymphocyte ratio in predicting acute-on-chronic liver failure survival
- A biomedical decision support system for meta-analysis of bilateral upper-limb training in stroke patients with hemiplegia
- TNF-α and IL-8 levels are positively correlated with hypobaric hypoxic pulmonary hypertension and pulmonary vascular remodeling in rats
- Stochastic gradient descent optimisation for convolutional neural network for medical image segmentation
- Comparison of the prognostic value of four different critical illness scores in patients with sepsis-induced coagulopathy
- Application and teaching of computer molecular simulation embedded technology and artificial intelligence in drug research and development
- Hepatobiliary surgery based on intelligent image segmentation technology
- Value of brain injury-related indicators based on neural network in the diagnosis of neonatal hypoxic-ischemic encephalopathy
- Analysis of early diagnosis methods for asymmetric dementia in brain MR images based on genetic medical technology
- Early diagnosis for the onset of peri-implantitis based on artificial neural network
- Clinical significance of the detection of serum IgG4 and IgG4/IgG ratio in patients with thyroid-associated ophthalmopathy
- Forecast of pain degree of lumbar disc herniation based on back propagation neural network
- SPA-UNet: A liver tumor segmentation network based on fused multi-scale features
- Systematic evaluation of clinical efficacy of CYP1B1 gene polymorphism in EGFR mutant non-small cell lung cancer observed by medical image
- Rehabilitation effect of intelligent rehabilitation training system on hemiplegic limb spasms after stroke
- A novel approach for minimising anti-aliasing effects in EEG data acquisition
- ErbB4 promotes M2 activation of macrophages in idiopathic pulmonary fibrosis
- Clinical role of CYP1B1 gene polymorphism in prediction of postoperative chemotherapy efficacy in NSCLC based on individualized health model
- Lung nodule segmentation via semi-residual multi-resolution neural networks
- Evaluation of brain nerve function in ICU patients with Delirium by deep learning algorithm-based resting state MRI
- A data mining technique for detecting malignant mesothelioma cancer using multiple regression analysis
- Markov model combined with MR diffusion tensor imaging for predicting the onset of Alzheimer’s disease
- Effectiveness of the treatment of depression associated with cancer and neuroimaging changes in depression-related brain regions in patients treated with the mediator-deuterium acupuncture method
- Molecular mechanism of colorectal cancer and screening of molecular markers based on bioinformatics analysis
- Monitoring and evaluation of anesthesia depth status data based on neuroscience
- Exploring the conformational dynamics and thermodynamics of EGFR S768I and G719X + S768I mutations in non-small cell lung cancer: An in silico approaches
- Optimised feature selection-driven convolutional neural network using gray level co-occurrence matrix for detection of cervical cancer
- Incidence of different pressure patterns of spinal cerebellar ataxia and analysis of imaging and genetic diagnosis
- Pathogenic bacteria and treatment resistance in older cardiovascular disease patients with lung infection and risk prediction model
- Adoption value of support vector machine algorithm-based computed tomography imaging in the diagnosis of secondary pulmonary fungal infections in patients with malignant hematological disorders
- From slides to insights: Harnessing deep learning for prognostic survival prediction in human colorectal cancer histology
- Ecology and Environmental Science
- Monitoring of hourly carbon dioxide concentration under different land use types in arid ecosystem
- Comparing the differences of prokaryotic microbial community between pit walls and bottom from Chinese liquor revealed by 16S rRNA gene sequencing
- Effects of cadmium stress on fruits germination and growth of two herbage species
- Bamboo charcoal affects soil properties and bacterial community in tea plantations
- Optimization of biogas potential using kinetic models, response surface methodology, and instrumental evidence for biodegradation of tannery fleshings during anaerobic digestion
- Understory vegetation diversity patterns of Platycladus orientalis and Pinus elliottii communities in Central and Southern China
- Studies on macrofungi diversity and discovery of new species of Abortiporus from Baotianman World Biosphere Reserve
- Food Science
- Effect of berrycactus fruit (Myrtillocactus geometrizans) on glutamate, glutamine, and GABA levels in the frontal cortex of rats fed with a high-fat diet
- Guesstimate of thymoquinone diversity in Nigella sativa L. genotypes and elite varieties collected from Indian states using HPTLC technique
- Analysis of bacterial community structure of Fuzhuan tea with different processing techniques
- Untargeted metabolomics reveals sour jujube kernel benefiting the nutritional value and flavor of Morchella esculenta
- Mycobiota in Slovak wine grapes: A case study from the small Carpathians wine region
- Elemental analysis of Fadogia ancylantha leaves used as a nutraceutical in Mashonaland West Province, Zimbabwe
- Microbiological transglutaminase: Biotechnological application in the food industry
- Influence of solvent-free extraction of fish oil from catfish (Clarias magur) heads using a Taguchi orthogonal array design: A qualitative and quantitative approach
- Chromatographic analysis of the chemical composition and anticancer activities of Curcuma longa extract cultivated in Palestine
- The potential for the use of leghemoglobin and plant ferritin as sources of iron
- Investigating the association between dietary patterns and glycemic control among children and adolescents with T1DM
- Bioengineering and Biotechnology
- Biocompatibility and osteointegration capability of β-TCP manufactured by stereolithography 3D printing: In vitro study
- Clinical characteristics and the prognosis of diabetic foot in Tibet: A single center, retrospective study
- Agriculture
- Biofertilizer and NPSB fertilizer application effects on nodulation and productivity of common bean (Phaseolus vulgaris L.) at Sodo Zuria, Southern Ethiopia
- On correlation between canopy vegetation and growth indexes of maize varieties with different nitrogen efficiencies
- Exopolysaccharides from Pseudomonas tolaasii inhibit the growth of Pleurotus ostreatus mycelia
- A transcriptomic evaluation of the mechanism of programmed cell death of the replaceable bud in Chinese chestnut
- Melatonin enhances salt tolerance in sorghum by modulating photosynthetic performance, osmoregulation, antioxidant defense, and ion homeostasis
- Effects of plant density on alfalfa (Medicago sativa L.) seed yield in western Heilongjiang areas
- Identification of rice leaf diseases and deficiency disorders using a novel DeepBatch technique
- Artificial intelligence and internet of things oriented sustainable precision farming: Towards modern agriculture
- Animal Sciences
- Effect of ketogenic diet on exercise tolerance and transcriptome of gastrocnemius in mice
- Combined analysis of mRNA–miRNA from testis tissue in Tibetan sheep with different FecB genotypes
- Isolation, identification, and drug resistance of a partially isolated bacterium from the gill of Siniperca chuatsi
- Tracking behavioral changes of confined sows from the first mating to the third parity
- The sequencing of the key genes and end products in the TLR4 signaling pathway from the kidney of Rana dybowskii exposed to Aeromonas hydrophila
- Development of a new candidate vaccine against piglet diarrhea caused by Escherichia coli
- Plant Sciences
- Crown and diameter structure of pure Pinus massoniana Lamb. forest in Hunan province, China
- Genetic evaluation and germplasm identification analysis on ITS2, trnL-F, and psbA-trnH of alfalfa varieties germplasm resources
- Tissue culture and rapid propagation technology for Gentiana rhodantha
- Effects of cadmium on the synthesis of active ingredients in Salvia miltiorrhiza
- Cloning and expression analysis of VrNAC13 gene in mung bean
- Chlorate-induced molecular floral transition revealed by transcriptomes
- Effects of warming and drought on growth and development of soybean in Hailun region
- Effects of different light conditions on transient expression and biomass in Nicotiana benthamiana leaves
- Comparative analysis of the rhizosphere microbiome and medicinally active ingredients of Atractylodes lancea from different geographical origins
- Distinguish Dianthus species or varieties based on chloroplast genomes
- Comparative transcriptomes reveal molecular mechanisms of apple blossoms of different tolerance genotypes to chilling injury
- Study on fresh processing key technology and quality influence of Cut Ophiopogonis Radix based on multi-index evaluation
- An advanced approach for fig leaf disease detection and classification: Leveraging image processing and enhanced support vector machine methodology
- Erratum
- Erratum to “Protein Z modulates the metastasis of lung adenocarcinoma cells”
- Erratum to “BRCA1 subcellular localization regulated by PI3K signaling pathway in triple-negative breast cancer MDA-MB-231 cells and hormone-sensitive T47D cells”
- Retraction
- Retraction to “Protocatechuic acid attenuates cerebral aneurysm formation and progression by inhibiting TNF-alpha/Nrf-2/NF-kB-mediated inflammatory mechanisms in experimental rats”
Articles in the same Issue
- Biomedical Sciences
- Systemic investigation of inetetamab in combination with small molecules to treat HER2-overexpressing breast and gastric cancers
- Immunosuppressive treatment for idiopathic membranous nephropathy: An updated network meta-analysis
- Identifying two pathogenic variants in a patient with pigmented paravenous retinochoroidal atrophy
- Effects of phytoestrogens combined with cold stress on sperm parameters and testicular proteomics in rats
- A case of pulmonary embolism with bad warfarin anticoagulant effects caused by E. coli infection
- Neutrophilia with subclinical Cushing’s disease: A case report and literature review
- Isoimperatorin alleviates lipopolysaccharide-induced periodontitis by downregulating ERK1/2 and NF-κB pathways
- Immunoregulation of synovial macrophages for the treatment of osteoarthritis
- Novel CPLANE1 c.8948dupT (p.P2984Tfs*7) variant in a child patient with Joubert syndrome
- Antiphospholipid antibodies and the risk of thrombosis in myeloproliferative neoplasms
- Immunological responses of septic rats to combination therapy with thymosin α1 and vitamin C
- High glucose and high lipid induced mitochondrial dysfunction in JEG-3 cells through oxidative stress
- Pharmacological inhibition of the ubiquitin-specific protease 8 effectively suppresses glioblastoma cell growth
- Levocarnitine regulates the growth of angiotensin II-induced myocardial fibrosis cells via TIMP-1
- Age-related changes in peripheral T-cell subpopulations in elderly individuals: An observational study
- Single-cell transcription analysis reveals the tumor origin and heterogeneity of human bilateral renal clear cell carcinoma
- Identification of iron metabolism-related genes as diagnostic signatures in sepsis by blood transcriptomic analysis
- Long noncoding RNA ACART knockdown decreases 3T3-L1 preadipocyte proliferation and differentiation
- Surgery, adjuvant immunotherapy plus chemotherapy and radiotherapy for primary malignant melanoma of the parotid gland (PGMM): A case report
- Dosimetry comparison with helical tomotherapy, volumetric modulated arc therapy, and intensity-modulated radiotherapy for grade II gliomas: A single‑institution case series
- Soy isoflavone reduces LPS-induced acute lung injury via increasing aquaporin 1 and aquaporin 5 in rats
- Refractory hypokalemia with sexual dysplasia and infertility caused by 17α-hydroxylase deficiency and triple X syndrome: A case report
- Meta-analysis of cancer risk among end stage renal disease undergoing maintenance dialysis
- 6-Phosphogluconate dehydrogenase inhibition arrests growth and induces apoptosis in gastric cancer via AMPK activation and oxidative stress
- Experimental study on the optimization of ANM33 release in foam cells
- Primary retroperitoneal angiosarcoma: A case report
- Metabolomic analysis-identified 2-hydroxybutyric acid might be a key metabolite of severe preeclampsia
- Malignant pleural effusion diagnosis and therapy
- Effect of spaceflight on the phenotype and proteome of Escherichia coli
- Comparison of immunotherapy combined with stereotactic radiotherapy and targeted therapy for patients with brain metastases: A systemic review and meta-analysis
- Activation of hypermethylated P2RY1 mitigates gastric cancer by promoting apoptosis and inhibiting proliferation
- Association between the VEGFR-2 -604T/C polymorphism (rs2071559) and type 2 diabetic retinopathy
- The role of IL-31 and IL-34 in the diagnosis and treatment of chronic periodontitis
- Triple-negative mouse breast cancer initiating cells show high expression of beta1 integrin and increased malignant features
- mNGS facilitates the accurate diagnosis and antibiotic treatment of suspicious critical CNS infection in real practice: A retrospective study
- The apatinib and pemetrexed combination has antitumor and antiangiogenic effects against NSCLC
- Radiotherapy for primary thyroid adenoid cystic carcinoma
- Design and functional preliminary investigation of recombinant antigen EgG1Y162–EgG1Y162 against Echinococcus granulosus
- Effects of losartan in patients with NAFLD: A meta-analysis of randomized controlled trial
- Bibliometric analysis of METTL3: Current perspectives, highlights, and trending topics
- Performance comparison of three scaling algorithms in NMR-based metabolomics analysis
- PI3K/AKT/mTOR pathway and its related molecules participate in PROK1 silence-induced anti-tumor effects on pancreatic cancer
- The altered expression of cytoskeletal and synaptic remodeling proteins during epilepsy
- Effects of pegylated recombinant human granulocyte colony-stimulating factor on lymphocytes and white blood cells of patients with malignant tumor
- Prostatitis as initial manifestation of Chlamydia psittaci pneumonia diagnosed by metagenome next-generation sequencing: A case report
- NUDT21 relieves sevoflurane-induced neurological damage in rats by down-regulating LIMK2
- Association of interleukin-10 rs1800896, rs1800872, and interleukin-6 rs1800795 polymorphisms with squamous cell carcinoma risk: A meta-analysis
- Exosomal HBV-DNA for diagnosis and treatment monitoring of chronic hepatitis B
- Shear stress leads to the dysfunction of endothelial cells through the Cav-1-mediated KLF2/eNOS/ERK signaling pathway under physiological conditions
- Interaction between the PI3K/AKT pathway and mitochondrial autophagy in macrophages and the leukocyte count in rats with LPS-induced pulmonary infection
- Meta-analysis of the rs231775 locus polymorphism in the CTLA-4 gene and the susceptibility to Graves’ disease in children
- Cloning, subcellular localization and expression of phosphate transporter gene HvPT6 of hulless barley
- Coptisine mitigates diabetic nephropathy via repressing the NRLP3 inflammasome
- Significant elevated CXCL14 and decreased IL-39 levels in patients with tuberculosis
- Whole-exome sequencing applications in prenatal diagnosis of fetal bowel dilatation
- Gemella morbillorum infective endocarditis: A case report and literature review
- An unusual ectopic thymoma clonal evolution analysis: A case report
- Severe cumulative skin toxicity during toripalimab combined with vemurafenib following toripalimab alone
- Detection of V. vulnificus septic shock with ARDS using mNGS
- Novel rare genetic variants of familial and sporadic pulmonary atresia identified by whole-exome sequencing
- The influence and mechanistic action of sperm DNA fragmentation index on the outcomes of assisted reproduction technology
- Novel compound heterozygous mutations in TELO2 in an infant with You-Hoover-Fong syndrome: A case report and literature review
- ctDNA as a prognostic biomarker in resectable CLM: Systematic review and meta-analysis
- Diagnosis of primary amoebic meningoencephalitis by metagenomic next-generation sequencing: A case report
- Phylogenetic analysis of promoter regions of human Dolichol kinase (DOLK) and orthologous genes using bioinformatics tools
- Collagen changes in rabbit conjunctiva after conjunctival crosslinking
- Effects of NM23 transfection of human gastric carcinoma cells in mice
- Oral nifedipine and phytosterol, intravenous nicardipine, and oral nifedipine only: Three-arm, retrospective, cohort study for management of severe preeclampsia
- Case report of hepatic retiform hemangioendothelioma: A rare tumor treated with ultrasound-guided microwave ablation
- Curcumin induces apoptosis in human hepatocellular carcinoma cells by decreasing the expression of STAT3/VEGF/HIF-1α signaling
- Rare presentation of double-clonal Waldenström macroglobulinemia with pulmonary embolism: A case report
- Giant duplication of the transverse colon in an adult: A case report and literature review
- Ectopic thyroid tissue in the breast: A case report
- SDR16C5 promotes proliferation and migration and inhibits apoptosis in pancreatic cancer
- Vaginal metastasis from breast cancer: A case report
- Screening of the best time window for MSC transplantation to treat acute myocardial infarction with SDF-1α antibody-loaded targeted ultrasonic microbubbles: An in vivo study in miniswine
- Inhibition of TAZ impairs the migration ability of melanoma cells
- Molecular complexity analysis of the diagnosis of Gitelman syndrome in China
- Effects of maternal calcium and protein intake on the development and bone metabolism of offspring mice
- Identification of winter wheat pests and diseases based on improved convolutional neural network
- Ultra-multiplex PCR technique to guide treatment of Aspergillus-infected aortic valve prostheses
- Virtual high-throughput screening: Potential inhibitors targeting aminopeptidase N (CD13) and PIKfyve for SARS-CoV-2
- Immune checkpoint inhibitors in cancer patients with COVID-19
- Utility of methylene blue mixed with autologous blood in preoperative localization of pulmonary nodules and masses
- Integrated analysis of the microbiome and transcriptome in stomach adenocarcinoma
- Berberine suppressed sarcopenia insulin resistance through SIRT1-mediated mitophagy
- DUSP2 inhibits the progression of lupus nephritis in mice by regulating the STAT3 pathway
- Lung abscess by Fusobacterium nucleatum and Streptococcus spp. co-infection by mNGS: A case series
- Genetic alterations of KRAS and TP53 in intrahepatic cholangiocarcinoma associated with poor prognosis
- Granulomatous polyangiitis involving the fourth ventricle: Report of a rare case and a literature review
- Studying infant mortality: A demographic analysis based on data mining models
- Metaplastic breast carcinoma with osseous differentiation: A report of a rare case and literature review
- Protein Z modulates the metastasis of lung adenocarcinoma cells
- Inhibition of pyroptosis and apoptosis by capsaicin protects against LPS-induced acute kidney injury through TRPV1/UCP2 axis in vitro
- TAK-242, a toll-like receptor 4 antagonist, against brain injury by alleviates autophagy and inflammation in rats
- Primary mediastinum Ewing’s sarcoma with pleural effusion: A case report and literature review
- Association of ADRB2 gene polymorphisms and intestinal microbiota in Chinese Han adolescents
- Tanshinone IIA alleviates chondrocyte apoptosis and extracellular matrix degeneration by inhibiting ferroptosis
- Study on the cytokines related to SARS-Cov-2 in testicular cells and the interaction network between cells based on scRNA-seq data
- Effect of periostin on bone metabolic and autophagy factors during tooth eruption in mice
- HP1 induces ferroptosis of renal tubular epithelial cells through NRF2 pathway in diabetic nephropathy
- Intravaginal estrogen management in postmenopausal patients with vaginal squamous intraepithelial lesions along with CO2 laser ablation: A retrospective study
- Hepatocellular carcinoma cell differentiation trajectory predicts immunotherapy, potential therapeutic drugs, and prognosis of patients
- Effects of physical exercise on biomarkers of oxidative stress in healthy subjects: A meta-analysis of randomized controlled trials
- Identification of lysosome-related genes in connection with prognosis and immune cell infiltration for drug candidates in head and neck cancer
- Development of an instrument-free and low-cost ELISA dot-blot test to detect antibodies against SARS-CoV-2
- Research progress on gas signal molecular therapy for Parkinson’s disease
- Adiponectin inhibits TGF-β1-induced skin fibroblast proliferation and phenotype transformation via the p38 MAPK signaling pathway
- The G protein-coupled receptor-related gene signatures for predicting prognosis and immunotherapy response in bladder urothelial carcinoma
- α-Fetoprotein contributes to the malignant biological properties of AFP-producing gastric cancer
- CXCL12/CXCR4/CXCR7 axis in placenta tissues of patients with placenta previa
- Association between thyroid stimulating hormone levels and papillary thyroid cancer risk: A meta-analysis
- Significance of sTREM-1 and sST2 combined diagnosis for sepsis detection and prognosis prediction
- Diagnostic value of serum neuroactive substances in the acute exacerbation of chronic obstructive pulmonary disease complicated with depression
- Research progress of AMP-activated protein kinase and cardiac aging
- TRIM29 knockdown prevented the colon cancer progression through decreasing the ubiquitination levels of KRT5
- Cross-talk between gut microbiota and liver steatosis: Complications and therapeutic target
- Metastasis from small cell lung cancer to ovary: A case report
- The early diagnosis and pathogenic mechanisms of sepsis-related acute kidney injury
- The effect of NK cell therapy on sepsis secondary to lung cancer: A case report
- Erianin alleviates collagen-induced arthritis in mice by inhibiting Th17 cell differentiation
- Loss of ACOX1 in clear cell renal cell carcinoma and its correlation with clinical features
- Signalling pathways in the osteogenic differentiation of periodontal ligament stem cells
- Crosstalk between lactic acid and immune regulation and its value in the diagnosis and treatment of liver failure
- Clinicopathological features and differential diagnosis of gastric pleomorphic giant cell carcinoma
- Traumatic brain injury and rTMS-ERPs: Case report and literature review
- Extracellular fibrin promotes non-small cell lung cancer progression through integrin β1/PTEN/AKT signaling
- Knockdown of DLK4 inhibits non-small cell lung cancer tumor growth by downregulating CKS2
- The co-expression pattern of VEGFR-2 with indicators related to proliferation, apoptosis, and differentiation of anagen hair follicles
- Inflammation-related signaling pathways in tendinopathy
- CD4+ T cell count in HIV/TB co-infection and co-occurrence with HL: Case report and literature review
- Clinical analysis of severe Chlamydia psittaci pneumonia: Case series study
- Bioinformatics analysis to identify potential biomarkers for the pulmonary artery hypertension associated with the basement membrane
- Influence of MTHFR polymorphism, alone or in combination with smoking and alcohol consumption, on cancer susceptibility
- Catharanthus roseus (L.) G. Don counteracts the ampicillin resistance in multiple antibiotic-resistant Staphylococcus aureus by downregulation of PBP2a synthesis
- Combination of a bronchogenic cyst in the thoracic spinal canal with chronic myelocytic leukemia
- Bacterial lipoprotein plays an important role in the macrophage autophagy and apoptosis induced by Salmonella typhimurium and Staphylococcus aureus
- TCL1A+ B cells predict prognosis in triple-negative breast cancer through integrative analysis of single-cell and bulk transcriptomic data
- Ezrin promotes esophageal squamous cell carcinoma progression via the Hippo signaling pathway
- Ferroptosis: A potential target of macrophages in plaque vulnerability
- Predicting pediatric Crohn's disease based on six mRNA-constructed risk signature using comprehensive bioinformatic approaches
- Applications of genetic code expansion and photosensitive UAAs in studying membrane proteins
- HK2 contributes to the proliferation, migration, and invasion of diffuse large B-cell lymphoma cells by enhancing the ERK1/2 signaling pathway
- IL-17 in osteoarthritis: A narrative review
- Circadian cycle and neuroinflammation
- Probiotic management and inflammatory factors as a novel treatment in cirrhosis: A systematic review and meta-analysis
- Hemorrhagic meningioma with pulmonary metastasis: Case report and literature review
- SPOP regulates the expression profiles and alternative splicing events in human hepatocytes
- Knockdown of SETD5 inhibited glycolysis and tumor growth in gastric cancer cells by down-regulating Akt signaling pathway
- PTX3 promotes IVIG resistance-induced endothelial injury in Kawasaki disease by regulating the NF-κB pathway
- Pancreatic ectopic thyroid tissue: A case report and analysis of literature
- The prognostic impact of body mass index on female breast cancer patients in underdeveloped regions of northern China differs by menopause status and tumor molecular subtype
- Report on a case of liver-originating malignant melanoma of unknown primary
- Case report: Herbal treatment of neutropenic enterocolitis after chemotherapy for breast cancer
- The fibroblast growth factor–Klotho axis at molecular level
- Characterization of amiodarone action on currents in hERG-T618 gain-of-function mutations
- A case report of diagnosis and dynamic monitoring of Listeria monocytogenes meningitis with NGS
- Effect of autologous platelet-rich plasma on new bone formation and viability of a Marburg bone graft
- Small breast epithelial mucin as a useful prognostic marker for breast cancer patients
- Continuous non-adherent culture promotes transdifferentiation of human adipose-derived stem cells into retinal lineage
- Nrf3 alleviates oxidative stress and promotes the survival of colon cancer cells by activating AKT/BCL-2 signal pathway
- Favorable response to surufatinib in a patient with necrolytic migratory erythema: A case report
- Case report of atypical undernutrition of hypoproteinemia type
- Down-regulation of COL1A1 inhibits tumor-associated fibroblast activation and mediates matrix remodeling in the tumor microenvironment of breast cancer
- Sarcoma protein kinase inhibition alleviates liver fibrosis by promoting hepatic stellate cells ferroptosis
- Research progress of serum eosinophil in chronic obstructive pulmonary disease and asthma
- Clinicopathological characteristics of co-existing or mixed colorectal cancer and neuroendocrine tumor: Report of five cases
- Role of menopausal hormone therapy in the prevention of postmenopausal osteoporosis
- Precisional detection of lymph node metastasis using tFCM in colorectal cancer
- Advances in diagnosis and treatment of perimenopausal syndrome
- A study of forensic genetics: ITO index distribution and kinship judgment between two individuals
- Acute lupus pneumonitis resembling miliary tuberculosis: A case-based review
- Plasma levels of CD36 and glutathione as biomarkers for ruptured intracranial aneurysm
- Fractalkine modulates pulmonary angiogenesis and tube formation by modulating CX3CR1 and growth factors in PVECs
- Novel risk prediction models for deep vein thrombosis after thoracotomy and thoracoscopic lung cancer resections, involving coagulation and immune function
- Exploring the diagnostic markers of essential tremor: A study based on machine learning algorithms
- Evaluation of effects of small-incision approach treatment on proximal tibia fracture by deep learning algorithm-based magnetic resonance imaging
- An online diagnosis method for cancer lesions based on intelligent imaging analysis
- Medical imaging in rheumatoid arthritis: A review on deep learning approach
- Predictive analytics in smart healthcare for child mortality prediction using a machine learning approach
- Utility of neutrophil–lymphocyte ratio and platelet–lymphocyte ratio in predicting acute-on-chronic liver failure survival
- A biomedical decision support system for meta-analysis of bilateral upper-limb training in stroke patients with hemiplegia
- TNF-α and IL-8 levels are positively correlated with hypobaric hypoxic pulmonary hypertension and pulmonary vascular remodeling in rats
- Stochastic gradient descent optimisation for convolutional neural network for medical image segmentation
- Comparison of the prognostic value of four different critical illness scores in patients with sepsis-induced coagulopathy
- Application and teaching of computer molecular simulation embedded technology and artificial intelligence in drug research and development
- Hepatobiliary surgery based on intelligent image segmentation technology
- Value of brain injury-related indicators based on neural network in the diagnosis of neonatal hypoxic-ischemic encephalopathy
- Analysis of early diagnosis methods for asymmetric dementia in brain MR images based on genetic medical technology
- Early diagnosis for the onset of peri-implantitis based on artificial neural network
- Clinical significance of the detection of serum IgG4 and IgG4/IgG ratio in patients with thyroid-associated ophthalmopathy
- Forecast of pain degree of lumbar disc herniation based on back propagation neural network
- SPA-UNet: A liver tumor segmentation network based on fused multi-scale features
- Systematic evaluation of clinical efficacy of CYP1B1 gene polymorphism in EGFR mutant non-small cell lung cancer observed by medical image
- Rehabilitation effect of intelligent rehabilitation training system on hemiplegic limb spasms after stroke
- A novel approach for minimising anti-aliasing effects in EEG data acquisition
- ErbB4 promotes M2 activation of macrophages in idiopathic pulmonary fibrosis
- Clinical role of CYP1B1 gene polymorphism in prediction of postoperative chemotherapy efficacy in NSCLC based on individualized health model
- Lung nodule segmentation via semi-residual multi-resolution neural networks
- Evaluation of brain nerve function in ICU patients with Delirium by deep learning algorithm-based resting state MRI
- A data mining technique for detecting malignant mesothelioma cancer using multiple regression analysis
- Markov model combined with MR diffusion tensor imaging for predicting the onset of Alzheimer’s disease
- Effectiveness of the treatment of depression associated with cancer and neuroimaging changes in depression-related brain regions in patients treated with the mediator-deuterium acupuncture method
- Molecular mechanism of colorectal cancer and screening of molecular markers based on bioinformatics analysis
- Monitoring and evaluation of anesthesia depth status data based on neuroscience
- Exploring the conformational dynamics and thermodynamics of EGFR S768I and G719X + S768I mutations in non-small cell lung cancer: An in silico approaches
- Optimised feature selection-driven convolutional neural network using gray level co-occurrence matrix for detection of cervical cancer
- Incidence of different pressure patterns of spinal cerebellar ataxia and analysis of imaging and genetic diagnosis
- Pathogenic bacteria and treatment resistance in older cardiovascular disease patients with lung infection and risk prediction model
- Adoption value of support vector machine algorithm-based computed tomography imaging in the diagnosis of secondary pulmonary fungal infections in patients with malignant hematological disorders
- From slides to insights: Harnessing deep learning for prognostic survival prediction in human colorectal cancer histology
- Ecology and Environmental Science
- Monitoring of hourly carbon dioxide concentration under different land use types in arid ecosystem
- Comparing the differences of prokaryotic microbial community between pit walls and bottom from Chinese liquor revealed by 16S rRNA gene sequencing
- Effects of cadmium stress on fruits germination and growth of two herbage species
- Bamboo charcoal affects soil properties and bacterial community in tea plantations
- Optimization of biogas potential using kinetic models, response surface methodology, and instrumental evidence for biodegradation of tannery fleshings during anaerobic digestion
- Understory vegetation diversity patterns of Platycladus orientalis and Pinus elliottii communities in Central and Southern China
- Studies on macrofungi diversity and discovery of new species of Abortiporus from Baotianman World Biosphere Reserve
- Food Science
- Effect of berrycactus fruit (Myrtillocactus geometrizans) on glutamate, glutamine, and GABA levels in the frontal cortex of rats fed with a high-fat diet
- Guesstimate of thymoquinone diversity in Nigella sativa L. genotypes and elite varieties collected from Indian states using HPTLC technique
- Analysis of bacterial community structure of Fuzhuan tea with different processing techniques
- Untargeted metabolomics reveals sour jujube kernel benefiting the nutritional value and flavor of Morchella esculenta
- Mycobiota in Slovak wine grapes: A case study from the small Carpathians wine region
- Elemental analysis of Fadogia ancylantha leaves used as a nutraceutical in Mashonaland West Province, Zimbabwe
- Microbiological transglutaminase: Biotechnological application in the food industry
- Influence of solvent-free extraction of fish oil from catfish (Clarias magur) heads using a Taguchi orthogonal array design: A qualitative and quantitative approach
- Chromatographic analysis of the chemical composition and anticancer activities of Curcuma longa extract cultivated in Palestine
- The potential for the use of leghemoglobin and plant ferritin as sources of iron
- Investigating the association between dietary patterns and glycemic control among children and adolescents with T1DM
- Bioengineering and Biotechnology
- Biocompatibility and osteointegration capability of β-TCP manufactured by stereolithography 3D printing: In vitro study
- Clinical characteristics and the prognosis of diabetic foot in Tibet: A single center, retrospective study
- Agriculture
- Biofertilizer and NPSB fertilizer application effects on nodulation and productivity of common bean (Phaseolus vulgaris L.) at Sodo Zuria, Southern Ethiopia
- On correlation between canopy vegetation and growth indexes of maize varieties with different nitrogen efficiencies
- Exopolysaccharides from Pseudomonas tolaasii inhibit the growth of Pleurotus ostreatus mycelia
- A transcriptomic evaluation of the mechanism of programmed cell death of the replaceable bud in Chinese chestnut
- Melatonin enhances salt tolerance in sorghum by modulating photosynthetic performance, osmoregulation, antioxidant defense, and ion homeostasis
- Effects of plant density on alfalfa (Medicago sativa L.) seed yield in western Heilongjiang areas
- Identification of rice leaf diseases and deficiency disorders using a novel DeepBatch technique
- Artificial intelligence and internet of things oriented sustainable precision farming: Towards modern agriculture
- Animal Sciences
- Effect of ketogenic diet on exercise tolerance and transcriptome of gastrocnemius in mice
- Combined analysis of mRNA–miRNA from testis tissue in Tibetan sheep with different FecB genotypes
- Isolation, identification, and drug resistance of a partially isolated bacterium from the gill of Siniperca chuatsi
- Tracking behavioral changes of confined sows from the first mating to the third parity
- The sequencing of the key genes and end products in the TLR4 signaling pathway from the kidney of Rana dybowskii exposed to Aeromonas hydrophila
- Development of a new candidate vaccine against piglet diarrhea caused by Escherichia coli
- Plant Sciences
- Crown and diameter structure of pure Pinus massoniana Lamb. forest in Hunan province, China
- Genetic evaluation and germplasm identification analysis on ITS2, trnL-F, and psbA-trnH of alfalfa varieties germplasm resources
- Tissue culture and rapid propagation technology for Gentiana rhodantha
- Effects of cadmium on the synthesis of active ingredients in Salvia miltiorrhiza
- Cloning and expression analysis of VrNAC13 gene in mung bean
- Chlorate-induced molecular floral transition revealed by transcriptomes
- Effects of warming and drought on growth and development of soybean in Hailun region
- Effects of different light conditions on transient expression and biomass in Nicotiana benthamiana leaves
- Comparative analysis of the rhizosphere microbiome and medicinally active ingredients of Atractylodes lancea from different geographical origins
- Distinguish Dianthus species or varieties based on chloroplast genomes
- Comparative transcriptomes reveal molecular mechanisms of apple blossoms of different tolerance genotypes to chilling injury
- Study on fresh processing key technology and quality influence of Cut Ophiopogonis Radix based on multi-index evaluation
- An advanced approach for fig leaf disease detection and classification: Leveraging image processing and enhanced support vector machine methodology
- Erratum
- Erratum to “Protein Z modulates the metastasis of lung adenocarcinoma cells”
- Erratum to “BRCA1 subcellular localization regulated by PI3K signaling pathway in triple-negative breast cancer MDA-MB-231 cells and hormone-sensitive T47D cells”
- Retraction
- Retraction to “Protocatechuic acid attenuates cerebral aneurysm formation and progression by inhibiting TNF-alpha/Nrf-2/NF-kB-mediated inflammatory mechanisms in experimental rats”

