Abstract
Some of the millions of patients infected with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) have developed new sequelae after recovering from the initial disease, termed post-acute sequelae of coronavirus disease 2019 (PASC). One symptom is anxiety, which is likely due to three etiologies: brain structural changes, neuroendocrine disruption, and neurotransmitter alterations. This review provides an overview of the current literature on the pathophysiological pathways linking coronavirus disease 2019 to anxiety, as well as the possible mechanisms of action in which an increasingly scrutinized treatment method, enhanced external counter-pulsation (EECP), is able to alleviate anxiety. SARS-CoV-2 triggers increased inflammatory cytokine production, as well as oxidative stress; these processes contribute to the aforementioned three etiologies. The potential treatment approach of EECP, involving sequenced inflation and deflation of specifically-placed airbags, has become of increasing interest, as it has been found to alleviate PASC-associated anxiety by improving patient cardiovascular function. These functional improvements were achieved by EECP stimulating anti-inflammatory and pro-angiogenic processes, as well as improving endothelial cell function and coronary blood flow, partially via counteracting against the negative effects of SARS-CoV-2 infection on the renin–angiotensin–aldosterone system. Therefore, EECP could promote both psychosomatic and cardiac rehabilitation. Further research, though, is still needed to fully determine its benefits and mechanism of action.
1 Introduction
Since December 2019, coronavirus disease 2019 (COVID-19), caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), has had a huge impact globally. As of October 2023, >770 million infections and ∼7 million deaths have been reported worldwide (source: World Health Organization [WHO]). Some patients infected with SARS-CoV-2 develop new symptoms or sequelae after the disease, which can last for months or years; these manifestations are known as long covid, or post-acute sequelae of COVID-19 (PASC) [1], which has been defined by the WHO as a condition occurring in likely/confirmed SARS-CoV-2-infected individuals at least 3 months from COVID-19 onset, with symptoms lasting for ≥2 months, and unable to be explained with alternative diagnoses. The impact of PASC can be severe, affecting multiple organ systems, as demonstrated in a retrospective matched cohort study of 47,780 cases, which found that compared to the general population, those with acute COVID-19 had an increased risk for developing multiple organ dysfunction [2]. Furthermore, on top of damaging multiple organ systems, long COVID-19 could lead to negative alterations in psychological performance. Indeed, anxiety has been found to be one of the most common psychiatric symptoms among long COVID patients [3], as demonstrated in a meta-analysis of 132 studies, involving 9,320,687 patients, in which anxiety prevalence among PASC patients was 23% [4]. In line with this observation, a direct link between SARS-CoV-2 infection and anxiety has also been documented, further supporting the close relation between physical and psychological symptoms [5]. More specifically, stress, anxiety, and depression prevalence among the general population during the pandemic were, respectively, 29.6, 31.9, and 33.7% [6]; in particular, anxiety and depression prevalence in 2020 grew, correspondingly, by 27.6 and 25.6%, representing 76 and 53.2 million more cases [7]. PASC also has significant economic and social impacts, in that a prospective cohort study found that over a 3-month period, some patients had negative changes in their occupational status [8]. Considering that >65 million people suffer from PASC, the disease thus has a significant detrimental impact on employment and economic conditions.
In light of those findings, a number of potential strategies to alleviate the effects of PASC have been investigated, one of which is enhanced external counter-pulsation (EECP), a non-invasive assisted circulatory device developed in China. EECP was initially applied for treating various cardiovascular diseases (CVD), in which special airbags are used to arrange the calves, thighs, and buttocks of a patient in specified conformations. A computer then receives information regarding the diastolic and systolic phases of the heartbeat of the patient, based on their electrocardiogram R-wave, followed by inflation and deflation of the airbags in an orderly manner. More specifically, during diastole, the three groups of airbags are sequentially inflated, from the distal to the proximally located one, with a time difference of ∼50 ms between each inflation, leading to increases in diastolic pressure, as well as squeezing of the arterial and venous system of the lower half of the body. This results in more blood being supplied to the upper half of the body, in turn, improving perfusion of the heart, brain, and other important upper body organs. The sequential airbag inflation also simultaneously increases the venous return of the right heart, leading to improvements in heart volume per heartbeat and cardiac output. At the systolic phase, all airbags are synchronized to deflate, lowering the afterload and ejection resistance of the heart. This EECP procedure has also been found to have beneficial effects in treating COVID-19 sequelae in some studies [9,10,11], of which one of the most prominent sequelae is anxiety in PASC, which has increasingly become a topic of investigation. As anxiety has been demonstrated to be prevalent, and an important risk factor, among CVD patients [12], additional research regarding the underlying mechanisms behind anxiety and possible treatments to improve the quality of life among CVD patients would also be greatly beneficial for long COVID-19 patients. In fact, more and more research has been focused on how to decrease anxiety, rehabilitate sequelae, and help restore patient physical functions after PASC. In this review, we will describe the current literature on the pathophysiological pathways linking COVID-19 to anxiety, as well as the possible mechanisms of action in which EECP is able to alleviate anxiety and COVID-19 sequelae.
2 Mechanisms associated with PASC-associated anxiety
The main etiologies behind PASC-associated anxiety likely include brain structural changes, neuroendocrine disruption, and neurotransmitter alterations, all of which inflammation and oxidative stress (OS) play important roles. These three etiologies will be described below.
2.1 Brain structural changes
SARS-CoV-2 infection has been associated with neurologic manifestations, particularly in the form of brain structural changes; this has been documented in multiple case reports, but the underlying mechanisms have still not been fully elucidated. These mechanisms, though, may likely be related to SARS-CoV-2 neuro-invasiveness, -tropism, and -virulence [13,14], in which it has been found that compared to healthy controls, PASC patients with neuropsychiatric symptoms have significantly increased gray matter volume in various brain regions, including frontotemporal, cerebellum, hippocampus, amygdala, basal ganglia, and thalamus [15]. Additionally, a neuroimaging study has shown that patients with anxiety had structural and functional abnormalities in the prefrontal-limbic neural circuits, including prefrontal cortex, hippocampus, amygdala, insula, orbital frontal cortex, and cingulate gyrus, which may be closely related to anxiety onset [16]. In particular, the structures associated with the limbic system, comprising of different midbrain, diencephalon, and telencephalon components, are the most affected. This system is involved in numerous cognitive-associated processes, such as spatial memory, motivation, as well as emotional and social processing [17]. As a result, alterations in limbic system structure and function significantly correlate to psychiatric symptoms. This has been demonstrated in multiple studies, such as a meta-analysis of 320 studies, where patients with major depressive/anxiety disorders, and/or chronic pain had wide-ranging gray matter volume reductions in the insula and dorsomedial prefrontal/anterior cingulate cortices [18], as well as another meta-analysis of seven studies, where patients with anxiety disorders had significantly reduced spontaneous brain activity in regions such as the right putamen, right inferior orbitofrontal gyrus, and right temporal pole [19].
2.2 The contribution of inflammation and OS on neuroendocrine disruption
Inflammation and OS have been recognized as two major mechanisms contributing to COVID-19-caused anxiety (Table 1). In particular, an excessive inflammatory response has been observed to be triggered by the invasion of angiotensin-converting enzyme 2 (ACE2)-expressing immune cells with SARS-CoV-2. Indeed, ACE2 is widely expressed among human cells and has been identified as the host surface receptor for SARS-CoV-2 [20], whose spike (S) protein binds to it, facilitating viral entry. The excessive inflammatory response involves monocytes and macrophages producing copious amounts of inflammatory factors, such as interleukins (IL-1β, IL-6, IL-8, IL-18), tumor necrosis factor (TNF)-α, interferon (IFN)-γ, granulocyte colony-stimulating factor (G-CSF), monocyte chemoattractant protein-1 (MCP-1/CCL 2), macrophage inflammatory protein (MIP), and other chemokines. Elevated levels for those factors are characteristic of a “cytokine storm (CS)”, which has been documented to occur in some COVID-19 patients, such as in a meta-analysis of 28 studies involving 346 COVID-19 patients, in which 60% of COVID-19 patients had elevated IL-6 and 51% IL-8 in cerebrospinal fluid [21]. A 2024 meta-analysis, involving 103 studies and 5502 PASC patients, also found that those patients, versus control, had significantly higher levels of C-reactive protein (CRP) and 21 other cytokines; thus, PASC was associated with enhanced immune activation [22]. Additionally, PASC patients with neurological defects were found to have significantly higher IL-1β and IL-8 levels in a 2024 analysis of blood markers [23]. Furthermore, serum IL-6 and TNF-α have been particularly noted to be independent and significant predictors for disease severity and death [24], and PASC patients have been found to possess, mean IL-6 levels that were 29% higher in early recovery and 44% higher in late recovery stages, compared to controls [25]. This has been coupled with numerous other studies finding that COVID-19 patients had elevated IL-6 expression and decreased lymphocyte counts [26,27,28]. All of those observations were in line with Peluso et al. who found that persistent symptoms after COVID-19 may be associated with continued immune activation [25].
The major mechanisms contributing to COVID-19-caused anxiety
| Mechanism | Explanation |
|---|---|
| Inflammation [13] | Spike (S) protein of SARS-CoV-2 binds to ACE 2 expressed on the surface of host cells and mediates the entry of SARS-CoV-2 into the cells. As a result, SARS-CoV-2 could trigger CS |
| Oxidative stress [19,20,21] | High ROS and RNS levels stem from SARS-CoV-2 interactions with ACE2. After binding to ACE2, both ACE2 and SARS-CoV-2 are endocytosed by the host cell, leading to ACE2 downregulation, increases in Ang II and AT1R expression. AT1R promotes vasoconstriction, inflammation, and oxidative stress |
SARS-CoV-2 = Severe acute respiratory syndrome coronavirus 2; ACE2 = angiotensin-converting enzyme 2; CS = cytokine storm; Ang II = angiotensin II; AT1R = angiotensin receptor type 1; ROS = reactive oxygen species; RNS = reactive nitrogen species.
Another process that has been linked with COVID-19-caused anxiety is OS, a state of altered redox homeostasis caused by psychological, physiological, or environmental stresses, which involves abnormally high reactive oxygen species (ROS) and reactive nitrogen species (RNS) levels, along with impaired antioxidant capacity and malfunctioning redox control in vivo. ROS and RNS are redox-active molecules with unstable oxygen and nitrogen molecules, possessing ≥1 unpaired electrons. They play important roles under physiological conditions, such as cell signaling and regulating redox homeostasis, but they have also been found to play important roles in SARS-CoV-2 pathogenesis and progression. More specifically, high ROS and RNS levels stem from SARS-CoV-2 interactions with ACE2, which have been found to play an important role in SARS-CoV-2-induced injury through multiple mechanisms: direct myocardial injury upon SARS-CoV-2 interaction with ACE2, as well as ACE2 downregulation and subsequent overstimulation of the renin–angiotensin–aldosterone system (RAAS) [29]. Notably, after binding to ACE2, both ACE2 and SARS-CoV-2 are endocytosed by the host cell, leading to ACE2 downregulation [30]. Lowered ACE2 expression, in turn, yields increase in angiotensin (Ang) II [31], which stimulates angiotensin receptor type 1 (AT1R) expression. AT1R promotes vasoconstriction, inflammation, and OS, particularly via Ang II binding to that receptor, leading to nicotinamide adenine dinucleotide phosphate (NADPH) oxidase activation and production of superoxide anions that result in mitochondrial damage and further ROS generation [32]. This ROS and RNS overproduction in SARS-CoV-2, owing to massive viral replication, leads to OS and damage to various host cell components, including proteins and mitochondria, yielding endothelial cell damage, disrupted lymphocyte and macrophage function, as well as exacerbated inflammation. Indeed, one study found that SARS-CoV-2-infected patients had higher OS biomarker levels compared to controls [33], demonstrating that OS is involved in tissue damage caused by SARS-CoV-2 infection. Moreover, another study conducted in 2023 found that compared to control, PASC patients were less able to resist oxidative damage, as indicated by lowered plasma total antioxidant capacity, glutathione peroxidase, and zinc levels [34]. Therefore, SARS-CoV-2 is associated not just with increased ROS and RNS production but also with lowered antioxidative defenses. As for PSAC-induced anxiety, it has been linked with elevated pro-inflammatory markers [35], such as in a cohort study showing that elevated CRP was observed in male patients with anxiety disorders [36]; another study found increased TNF-α in patients with anxiety disorders [37]. However, the specific mechanisms linking inflammatory factors to anxiety are still not fully elucidated and require further research.
The hypothalamic–pituitary–adrenal (HPA) axis, connecting the central nervous and endocrine systems, is an important structure in anxiety pathogenesis. It is involved in regulating hormones and the stress response. Upon stress and inflammation onset, the hypothalamus activates the HPA axis, via releasing corticotropin-releasing hormone, which subsequently stimulates adrenocorticotropic hormone (ACTH) release from the anterior pituitary gland; ACTH then acts on the adrenal cortex to induce cortisol synthesis and release. However, HPA regulatory mechanisms are altered under chronic stress, manifesting as sustained, elevated cortisol levels, and lowered sensitivity to cortisol feedback inhibition, resulting in decreased cortisol metabolism and higher plasma levels. Chronic cortisol dysregulation could lead to a variety of health problems, including anxiety [38]. Therefore, stress-induced neuroendocrine changes could serve as an important mechanism in the development of anxiety and other disorders [39]; the pathophysiological mechanisms are summarized in Figure 1.
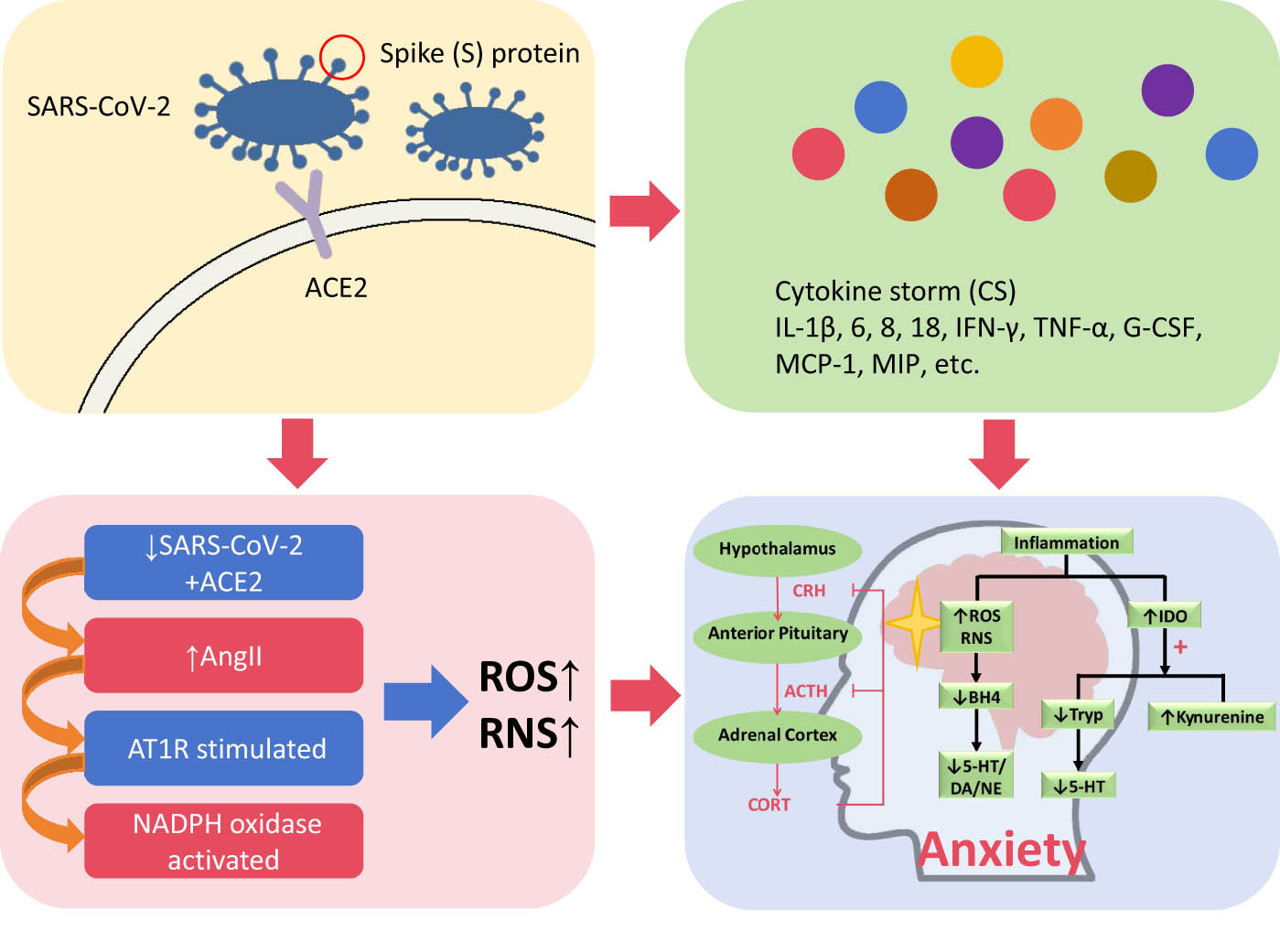
SARS-CoV-2 S protein binds to ACE2 on host cell surfaces, facilitating viral infection and triggering an excessive inflammatory response, entailing a CS comprising of IL-1β, IL-6, IL-8, IL-18, IFN-γ, TNF-α, G-CSF, MCP-1, and MIP. Additionally, SARS-CoV-2 binding to ACE2 lowers ACE2 expression levels, leading to increased Ang II levels, which subsequently increases AT1R and NADPH oxidase stimulation. The resulting increase in ROS and RNS, along with CS, yields alterations of hypothalamic–pituitary–adrenal (HPA) axis function and IDO activation, leading to increased anxiety, via cortisol dysregulation and inhibition of 5-HT production, owing to IDO conversion of tryptophan (Tryp) to kynurenine. Furthermore, ROS, RNS, and CS increases BH4 degradation, thereby negatively affecting 5-HT, DA, and NE synthesis. CRH = corticotropin-releasing hormone; CORT = cortisol.
2.3 Neurotransmitter disruption
Neurotransmitters have been documented to be important inflammatory mediators in the brain, in which peripheral inflammation could enter via three major pathways: humoral, neural, and cellular. The humoral pathway entails circulating cytokines entering the brain through “leaky” regions in the blood–brain barrier, followed by active transport into brain parenchyma via cytokine-specific saturable transport proteins, while the neural pathway involves cytokine signals being transmitted in the brain via afferent nerve fiber activation. The cellular pathway consists of activated microglia attracting peripheral inflammatory cells to the meninges and brain parenchyma. Therefore, cytokines and their associated signaling pathways play key roles in influencing anxiety-related neurotransmitter systems, as well as being involved in neurotransmitter synthesis, reuptake, and release; one prominent example is their activation of indoleamine 2,3 dioxygenase (IDO), which converts tryptophan, the primary amino acid for the neurotransmitter 5-hydroxytryptamine (5-HT), to kynurenine, thereby inhibiting 5-HT synthesis in the brain. Other mechanisms in which cytokines influence neurotransmitter activity are by facilitating the destruction of tetrahydrobiopterin (BH4) via increased ROS and RNS production, as it is extremely OS sensitive, resulting in its irreversible degradation to dihydroxyanthopterin. BH4 is an essential cofactor for tryptophan hydroxylase and tyrosine hydroxylase, both of which are rate-limiting enzymes for 5-HT, dopamine (DA), and norepinephrine (NE) synthesis; as a result, BH4 availability significantly impacts 5-HT, DA, and NE availability [40]. Furthermore, inflammatory cytokines increase the transporter protein expression and function for serotonin, DA, and NE, as well as upregulating neurotransmitter/precursor re-uptake and lowering their release. It should be noted that other neurotransmitter systems, such as gamma-aminobutyric acid and acetylcholine, may also play a role in anxiety development, though further investigation is needed to fully clarify the underlying mechanisms [41].
3 Mechanisms through which EECP treats COVID-19 sequelae
With respect to EECP, a number of recent studies, involving different patient populations, reported that it could aid in treating COVID-19 sequelae. One such study examined 51 patients with long COVID-19 and found that EECP treatment improved patient cognitive performances [9]. This was further reinforced by a retrospective analysis of 80 long-COVID-19 patients, of whom 38 had cognitive impairments and 42 did not; there, EECP substantially improved cognitive functioning in the impaired group [42]. Another COVID-19 sequela, which favorably responded to EECP, is fatigue, as observed in a systematic review of 20 studies, involving 5,629 PASC patients, where fatigue symptoms improved after receiving EECP [43]. This result was replicated for a single 38-year-old female with PASC symptoms after acute COVID-19, who had fatigue, headache, body aches, and shortness of breath during the acute infection phase. Even after most symptoms had been resolved, she still had periodic fatigue, headache, and “brain fog” for several months, which, however, improved with EECP treatment [10], thereby demonstrating the effectiveness of EECP in treating fatigue symptoms. Aside from psychological and mental improvements, EECP was also found to significantly improve cardiac function and exercise capacities, such as in one investigation where EECP, compared to baseline, yielded improvements in New York Heart Association functional classifications and left ventricular ejection fraction [11]. This finding was further supported by a study of 50 patients with refractory angina pectoris, where during the EECP treatment period, the average number of daily anginal episodes fell from 2.7 to 0.9, along with >70% of the patients having ≥1 grade reduction in their Canadian Cardiovascular Society classification, plus significant improvements in quality of life and exercise capacity, at 12 months post-EECP [44]. Cardiac functional and exercise capability improvements post-EECP administration were also found in a retrospective analysis of long-COVID-19 patients from seven different outpatient centers, where compared to baseline, they had improved scores on several functional tests after EECP, including the Seattle Angina Questionnaire and 6-min walk test [45]. Therefore, EECP has been noted to alleviate long covid symptoms and improve cardiac function, though it is still not fully clarified as to its mechanism of action in doing so. Nevertheless, some investigations have already been conducted regarding the mechanisms in which EECP exerts its beneficial effects, particularly in regard to hemodynamics and endothelial shear stresses [46]. These beneficial impacts, in turn, may serve as the basis behind EECP being able to alleviate PASC-associated anxiety (Table 2).
Mechanisms of EECP on PASC-associated anxiety
| Mechanism | Explanation |
|---|---|
| Hemodynamics [33,34,35] | EECP improves left ventricular hemodynamics by modulating aortic pressure, thereby increasing diastolic and decreasing systolic pressures, and subsequently increasing coronary blood flow velocity and pressure |
| EECP reduces myocardial oxygen demand, in turn improving ventricular diastolic and systolic function, as well as increasing myocardial oxygen supply by promoting coronary artery collateral growth | |
| ESS [38,39] | EECP induces increases in systemic ESS, which contributes to endothelial functional improvement. Additionally, ESS, through triggering multiple endothelial gene expression and signaling pathways, is able to inhibit abnormal cell proliferation, inflammation, and atherosclerosis; all of these processes aid in alleviating anxiety |
EECP = enhanced external counter-pulsation; ESS = Endothelial shear stress.
3.1 EECP positively impacts hemodynamics and endothelial shear stress
EECP has been found to improve left ventricular hemodynamics by modulating aortic pressure, thereby increasing diastolic and decreasing systolic pressures, and subsequently increasing coronary blood flow velocity and pressure [47]. Additionally, EECP reduces myocardial oxygen demand, in turn, improving ventricular diastolic and systolic function [48], as well as increasing myocardial oxygen supply by promoting coronary artery collateral growth [49]. Indeed, a study of 50 patients found significant improvement in cardiac function classification and anxiety scale scores after just 1 course of EECP [50], while another study highlighted significant psychological improvements post-EECP among refractory angina patients [51].
EECP also induces increases in systemic endothelial shear stress (ESS), an important physiological stimulus for maintaining proper vascular endothelial function [52]. ESS has been noted to be a phenomenon associated with regulating the release of vascular endothelial factors, which, along with inhibiting inflammation, contributes to endothelial functional improvements. Therefore, EECP can affect OS and inflammation levels by increasing ESS, as previously documented in the literature [53,54]. Additionally, ESS, through triggering multiple endothelial gene expression and signaling pathways, is able to inhibit abnormal cell proliferation, inflammation, and atherosclerosis [55]. This was observed by Casey et al., where 35 h of EECP treatment increased both overall and local ESS, which subsequently lowered the expression levels of pro-inflammatory TNF-α and MCP-1 by, respectively, 29 and 20% [56]. As a result, EECP promoted anti-inflammatory and anti-atherosclerotic effects by increasing ESS and promoting NO release from endothelial cells; ultimately, all of these processes aid in alleviating anxiety.
3.2 EECP promotes cardiac and psychosomatic rehabilitation processes
EECP could also aid in cardiac rehabilitation, particularly in terms of recovery from SARS-CoV-2-linked myocardial injury and improving patient quality of life. This recovery is likely facilitated by EECP regulation of RAAS, along with stimulating increases in coronary perfusion and lowering endothelial injury. With respect to RAAS, ACE catalyzes Ang I conversion to Ang II, while ACE2 degrades both Ang I and II to, respectively, Ang 1–9 and Ang 1–7 [57]. SARS-CoV-2, though, lowers ACE2 expression in RAAS, resulting in increased ACE-catalyzed conversion of Ang I to Ang II. As Ang II binds to AT1R, this ultimately yields vasoconstriction and increased expression of cellular injury pathways. By contrast, EECP has been found in animal experiments to inhibit ACE expression, thereby counteracting against cardiomyocyte damage associated with the negative impact of SARS-CoV-2 on RAAS. This postulation is further supported by findings confirming that EECP increases diastolic coronary perfusion pressure and blood supply, with a meta-analysis showing a 150% increase in coronary flow velocity and a 28% increase in coronary flow after EECP [58]. Therefore, EECP augments myocardial perfusion via increasing coronary vasodilation, as well as promoting the angiogenesis of neoplastic collateral vessels in the myocardium. In particular, EECP stimulates the release of vasoactive factors, such as α-actinin, von Willebrand, and vascular endothelial growth factors (VEGF); in a randomized controlled study of 240 coronary artery disease (CAD) patients, VEGF1 and VEGFR2 expression levels were significantly higher in EECP versus control group after the 1-year follow-up period, and EECP-treated patients also had significantly improved endothelial function [59]. Additionally, EECP was associated with significant improvements in flow-mediated dilatation (FMD) among patients with left ventricular dysfunction, demonstrating that the treatment could significantly improve endothelial function [60]. Indeed, a controlled clinical study of coronary slow flow patients found significantly increased FMD and lowered CRP in EECP-treated, compared to control, suggesting that EECP is able to improve vascular inflammation and endothelial function [61].
Psychosomatic factors have been closely linked to heart disease occurrence and development, such as mental stress serving as an important trigger for myocardial ischemia in coronary heart disease. In fact, multiple studies have identified higher stress levels being associated with increased CVD risk [62], and strong correlations between abnormal psychosomatic states and adverse cardiac events [63,64,65]. Based on those findings, EECP may be able to provide beneficial effects, to a greater extent than conventional approaches, on psychological health factors.
3.3 Comparison with other treatments
EECP also ranks favorably with other non-invasive treatments for post-COVID anxiety, yielding comparable improvements to them. One of those other treatments is physical exercise, as found in a systematic meta-analysis of 8 randomized clinical trials, where compared to control patients who did not exercise, the exercise group had greater improvements in anxiety levels [66]. Another approach is prescribing anti-depressants, such as oxytocin and lithium salts [67], or herbal remedies, including valerian root [68] and passionflower extract [69], as well as kava-kava rhizome [70]. In particular, Silexan, a proprietary essential oil from Lavandula angustifolia, has been found in a meta-analysis of 13 studies by Kasper et al. to be effective in treating post-COVID-19 patients, particularly with respect to anxiety, owing to the therapeutic profile of Silexan overlapping with the range of psychiatric symptoms in those patients [71]. Additionally, an alternative electrical stimulation approach, transcranial direct current stimulation, has been found to be effective in alleviating fatigue [72] and anxiety [67]. However, it is still unclear precisely how effective these treatments are; future studies will thus be required to determine whether they are more or less effective than EECP and/or whether any complementary effects between these therapies are present.
4 Conclusion
This review summarizes the possible mechanisms underlying PASC-associated anxiety and explores the possible role and underlying mechanisms of EECP in serving as a treatment approach. SARS-CoV-2 results in anxiety via multiple pathways, including brain structural changes, neuroendocrine disruption, and neurotransmitter alterations, all of which inflammation and OS play important roles. EECP is able to counteract against the negative effects of SARS-CoV-2, by lowering inflammation, in turn promoting cardiac functional recovery, and ultimately decreasing patient anxiety. Therefore, EECP could serve as a potential treatment approach, in which it plays a dual role in psychosomatic and cardiac rehabilitation. Further research, though, is still needed to fully determine the benefits and mechanism of action for EECP, as few clinical studies have been conducted on EECP in treating long COVID sequelae. Therefore, future studies, involving multiple centers, double-blinding, and larger patient cohorts, should be carried out to further confirm the effectiveness of EECP for treating PASC-associated anxiety. These studies should also further identify the precise mechanisms/mediators underlying the anti-inflammatory and anti-oxidative effects of EECP, which ultimately counteract against the adverse brain structural changes, neuroendocrine disruption, and neurotransmitter alterations responsible for PASC-associated anxiety. Furthermore, these studies should compare the effectiveness of other treatment strategies, such as Silexan, to that of EECP for anxiety treatment, and formulate the optimal protocol for treating this disease, possibly involving additive or synergistic effects from a combination of those different strategies.
Acknowledgment
All authors contributed to the study and agreed to be listed as authors. We thank Alina Yao for her assistance in manuscript preparation and editing. We thank Gangcheng Shen for his assistance with technical support from EECP.
-
Funding information: This work was supported by the National Natural Science Foundation (Project # 82200315), the Guangdong Basic and Applied Basic Research Foundation (2021A1515111145), Sanming Project of Medicine in Shenzhen (No. SZSM201412012), and Major Scientific Research Project of Shenzhen People’s Hospital (SYWGSJCYJ202301).
-
Author contributions: Jiecheng Huang and Jingjin Liu are responsible for writing the manuscript; Jiecheng Huang and Yongshun Wang are responsible for collecting literature; Jiecheng Huang is responsible for creating images; Jingjin Liu is responsible for guiding the content of the article; Yuxuan Fan is responsible for editing the manuscript before final submission.
-
Conflict of interest: The authors declare that they have no conflicts of interest.
-
Data availability statement: The data could be obtained by contacting the corresponding author.
References
[1] Proal AD, VanElzakker MB. Long COVID or post-acute sequelae of COVID-19 (PASC): An overview of biological factors that may contribute to persistent symptoms. Front Microbiol. 2021;12:698169.10.3389/fmicb.2021.698169Search in Google Scholar PubMed PubMed Central
[2] Ayoubkhani D, Khunti K, Nafilyan V, Maddox T, Humberstone B, Diamond I, et al. Post-covid syndrome in individuals admitted to hospital with covid-19: Retrospective cohort study. BMJ. 2021;372:n693.10.1136/bmj.n693Search in Google Scholar PubMed PubMed Central
[3] Siddiq MAB, Rasker JJ. COVID-19, long COVID, and psychosomatic manifestations: A possible burden on existing rheumatology facilities. Heart Mind. 2022;6(3):195–202.10.4103/hm.hm_63_21Search in Google Scholar
[4] Seighali N, Abdollahi A, Shafiee A, Amini MJ, Teymouri Athar MM, Safari O, et al. The global prevalence of depression, anxiety, and sleep disorder among patients coping with Post COVID-19 syndrome (long COVID): A systematic review and meta-analysis. BMC Psychiatry. 2024;24(1):105.10.1186/s12888-023-05481-6Search in Google Scholar PubMed PubMed Central
[5] Mazza M, Gaetani E, Marano G, Sani G. Body and mind: Two maps but one territory. mental coaching in support of somatic correlates in times of COVID-19. Heart Mind. 2021;5(4):161–2.10.4103/hm.hm_50_21Search in Google Scholar
[6] Salari N, Hosseinian-Far A, Jalali R, Vaisi-Raygani A, Rasoulpoor S, Mohammadi M, et al. Prevalence of stress, anxiety, depression among the general population during the COVID-19 pandemic: A systematic review and meta-analysis. Globalization Health. 2020;16(1):57.10.1186/s12992-020-00589-wSearch in Google Scholar PubMed PubMed Central
[7] COVID-19 Mental Disorders Collaborators. Global prevalence and burden of depressive and anxiety disorders in 204 countries and territories in 2020 due to the COVID-19 pandemic. Lancet (London, Engl). 2021;398(10312):1700–12.Search in Google Scholar
[8] Dryden M, Mudara C, Vika C, Blumberg L, Mayet N, Cohen C, et al. Post-COVID-19 condition 3 months after hospitalisation with SARS-CoV-2 in South Africa: a prospective cohort study. Lancet Global Health. 2022;10(9):e1247–56.10.1016/S2214-109X(22)00286-8Search in Google Scholar PubMed PubMed Central
[9] Sathyamoorthy M, Sevak R, Verduzco-Gutierrez M, Cabrera J, Lopez M, Shah SA. Abstract 14980: Enhanced external counterpulsation improves cognitive function in long covid patients. Circulation. 2022;146(Suppl_1):A14980.10.1161/circ.146.suppl_1.14980Search in Google Scholar
[10] Dayrit JK, Verduzco-Gutierrez M, Teal A, Shah SA. Enhanced external counterpulsation as a novel treatment for post-acute COVID-19 sequelae. Cureus. 2021;13(4):e14358.10.7759/cureus.14358Search in Google Scholar PubMed PubMed Central
[11] Kozdag G, Ertas G, Aygun F, Emre E, Kirbas A, Ural D, et al. Clinical effects of enhanced external counterpulsation treatment in patients with ischemic heart failure. Anadolu Kardiyol Derg. 2012;12(3):214–21.10.5152/akd.2012.064Search in Google Scholar PubMed
[12] Jiang W. Anxiety in individuals with cardiovascular diseases: A narrative review and expert opinion. Heart Mind. 2022;6(2):52–7.10.4103/hm.hm_5_22Search in Google Scholar
[13] Ellul MA, Benjamin L, Singh B, Lant S, Michael BD, Easton A, et al. Neurological associations of COVID-19. Lancet Neurol. 2020;19(9):767–83.10.1016/S1474-4422(20)30221-0Search in Google Scholar PubMed PubMed Central
[14] Bauer L, Laksono BM, de Vrij FMS, Kushner SA, Harschnitz O, van Riel D. The neuroinvasiveness, neurotropism, and neurovirulence of SARS-CoV-2. Trends Neurosci. 2022;45(5):358–68.10.1016/j.tins.2022.02.006Search in Google Scholar PubMed PubMed Central
[15] Besteher B, Machnik M, Troll M, Toepffer A, Zerekidze A, Rocktaschel T, et al. Larger gray matter volumes in neuropsychiatric long-COVID syndrome. Psychiatry Res. 2022;317:114836.10.1016/j.psychres.2022.114836Search in Google Scholar PubMed PubMed Central
[16] Craske MG, Stein MB. Anxiety. Lancet. 2016;388(10063):3048–59.10.1016/S0140-6736(16)30381-6Search in Google Scholar PubMed
[17] Kamali A, Milosavljevic S, Gandhi A, Lano KR, Shobeiri P, Sherbaf FG, et al. The cortico-limbo-thalamo-cortical circuits: An update to the original papez circuit of the human limbic system. Brain Topogr. 2023;36(3):371–89.10.1007/s10548-023-00955-ySearch in Google Scholar PubMed PubMed Central
[18] Brandl F, Weise B, Mulej Bratec S, Jassim N, Hoffmann Ayala D, Bertram T, et al. Common and specific large-scale brain changes in major depressive disorder, anxiety disorders, and chronic pain: a transdiagnostic multimodal meta-analysis of structural and functional MRI studies. Neuropsychopharmacol: Off Publ Am Coll Neuropsychopharmacol. 2022;47(5):1071–80.10.1038/s41386-022-01271-ySearch in Google Scholar PubMed PubMed Central
[19] Wang Q, Wang C, Deng Q, Zhan L, Tang Y, Li H, et al. Alterations of regional spontaneous brain activities in anxiety disorders: A meta-analysis. J Affect Disord. 2022;296:233–40.10.1016/j.jad.2021.09.062Search in Google Scholar PubMed
[20] Letko M, Marzi A, Munster V. Functional assessment of cell entry and receptor usage for SARS-CoV-2 and other lineage B betacoronaviruses. Nat Microbiol. 2020;5(4):562–9.10.1038/s41564-020-0688-ySearch in Google Scholar PubMed PubMed Central
[21] Devlin L, Gombolay GY. Cerebrospinal fluid cytokines in COVID-19: A review and meta-analysis. J Neurol. 2023;270(11):5155–61.10.1007/s00415-023-11928-3Search in Google Scholar PubMed PubMed Central
[22] Almulla AF, Thipakorn Y, Zhou B, Vojdani A, Maes M. Immune activation and immune-associated neurotoxicity in Long-COVID: A systematic review and meta-analysis of 103 studies comprising 58 cytokines/chemokines/growth factors. Brain Behav Immun. 2024;122:75–94.10.1016/j.bbi.2024.07.036Search in Google Scholar PubMed
[23] Tang N, Kido T, Shi J, McCafferty E, Ford JM, Dal Bon K, et al. Blood markers show neural consequences of longCOVID-19. Cells. 2024;13(6):478.10.3390/cells13060478Search in Google Scholar PubMed PubMed Central
[24] Del Valle DM, Kim-Schulze S, Huang HH, Beckmann ND, Nirenberg S, Wang B, et al. An inflammatory cytokine signature predicts COVID-19 severity and survival. Nat Med. 2020;26(10):1636–43.10.1038/s41591-020-1051-9Search in Google Scholar PubMed PubMed Central
[25] Peluso MJ, Lu S, Tang AF, Durstenfeld MS, Ho HE, Goldberg SA, et al. Markers of immune activation and inflammation in individuals with postacute sequelae of severe acute respiratory syndrome coronavirus 2 infection. J Infect Dis. 2021;224(11):1839–48.10.1093/infdis/jiab490Search in Google Scholar PubMed PubMed Central
[26] Chen T, Chen H, Chen P, Zhu L, Mao W, Yao Y. High expression of IL6 and decrease in immune cells in COVID-19 patients combined with myocardial injury. Front Immunol. 2023;14:1190644.10.3389/fimmu.2023.1190644Search in Google Scholar PubMed PubMed Central
[27] Zhou W, Song L, Wang X, Xu Z, Wang S, Wang J, et al. Cardiac injury prediction and lymphocyte immunity and inflammation analysis in hospitalized patients with coronavirus disease 2019 (COVID-19). Int J Cardiol. 2021;326:237–42.10.1016/j.ijcard.2020.10.049Search in Google Scholar PubMed PubMed Central
[28] Giustino G, Croft LB, Stefanini GG, Bragato R, Silbiger JJ, Vicenzi M, et al. Characterization of myocardial injury in patients with COVID-19. J Am Coll Cardiol. 2020;76(18):2043–55.10.1016/j.jacc.2020.08.069Search in Google Scholar PubMed PubMed Central
[29] Pannucci P, Jefferson SR, Hampshire J, Cooper SL, Hill SJ, Woolard J. COVID-19-induced myocarditis: Pathophysiological roles of ACE2 and toll-like receptors. Int J Mol Sci. 2023;24(6):5374.10.3390/ijms24065374Search in Google Scholar PubMed PubMed Central
[30] Beyerstedt S, Casaro EB, Rangel EB. COVID-19: Angiotensin-converting enzyme 2 (ACE2) expression and tissue susceptibility to SARS-CoV-2 infection. Eur J Clin Microbiol Infect Dis. 2021;40(5):905–19.10.1007/s10096-020-04138-6Search in Google Scholar PubMed PubMed Central
[31] Liu Y, Yang Y, Zhang C, Huang F, Wang F, Yuan J, et al. Clinical and biochemical indexes from 2019-nCoV infected patients linked to viral loads and lung injury. Sci China Life Sci. 2020;63(3):364–74.10.1007/s11427-020-1643-8Search in Google Scholar PubMed PubMed Central
[32] Lee SH, Fujioka S, Takahashi R, Oe T. Angiotensin II-induced oxidative stress in human endothelial cells: Modification of cellular molecules through lipid peroxidation. Chem Res Toxicol. 2019;32(7):1412–22.10.1021/acs.chemrestox.9b00110Search in Google Scholar PubMed
[33] Coronel PMV, Pereira IC, Basilio D, Espinoca IT, de Souza KFS, Ota RSN, et al. Biomarkers of oxidative stress and inflammation in subjects with COVID-19: Characterization and prognosis of the disease. Microb Pathog. 2023;184:106339.10.1016/j.micpath.2023.106339Search in Google Scholar PubMed
[34] Al-Hakeim HK, Al-Rubaye HT, Al-Hadrawi DS, Almulla AF, Maes M. Long-COVID post-viral chronic fatigue and affective symptoms are associated with oxidative damage, lowered antioxidant defenses and inflammation: A proof of concept and mechanism study. Mol Psychiatry. 2023;28(2):564–78.10.1038/s41380-022-01836-9Search in Google Scholar PubMed PubMed Central
[35] Michopoulos V, Powers A, Gillespie CF, Ressler KJ, Jovanovic T. Inflammation in fear- and anxiety-based disorders: PTSD, GAD, and Beyond. Neuropsychopharmacology. 2017;42(1):254–70.10.1038/npp.2016.146Search in Google Scholar PubMed PubMed Central
[36] Vogelzangs N, Beekman AT, de Jonge P, Penninx BW. Anxiety disorders and inflammation in a large adult cohort. Transl Psychiatry. 2013;3(4):e249.10.1038/tp.2013.27Search in Google Scholar PubMed PubMed Central
[37] Vieira MM, Ferreira TB, Pacheco PA, Barros PO, Almeida CR, Araujo-Lima CF, et al. Enhanced Th17 phenotype in individuals with generalized anxiety disorder. J Neuroimmunol. 2010;229(1–2):212–8.10.1016/j.jneuroim.2010.07.018Search in Google Scholar PubMed
[38] Russell G, Lightman S. The human stress response. Nat Rev Endocrinol. 2019;15(9):525–34.10.1038/s41574-019-0228-0Search in Google Scholar PubMed
[39] Liu M. Spotlight on the relationship between heart disease and mental stress. Heart Mind. 2021;5(1):1–3.10.4103/hm.hm_12_21Search in Google Scholar
[40] Felger JC. Imaging the role of inflammation in mood and anxiety-related disorders. Curr Neuropharmacol. 2018;16(5):533–58.10.2174/1570159X15666171123201142Search in Google Scholar PubMed PubMed Central
[41] Miller AH, Haroon E, Raison CL, Felger JC. Cytokine targets in the brain: Impact on neurotransmitters and neurocircuits. Depress Anxiety. 2013;30(4):297–306.10.1002/da.22084Search in Google Scholar PubMed PubMed Central
[42] Sathyamoorthy M, Sevak RJ, Cabrera J, Lopez M, Fox J, Shah SA, et al. Enhanced external counterpulsation improves cognitive function of persons with long COVID. Am J Phys Med Rehabil. 2024;103(8):734–9.10.1097/PHM.0000000000002433Search in Google Scholar PubMed
[43] Joli J, Buck P, Zipfel S, Stengel A. Post-COVID-19 fatigue: A systematic review. Front Psychiatry. 2022;13:947973.10.3389/fpsyt.2022.947973Search in Google Scholar PubMed PubMed Central
[44] May O, Lynggaard V, Mortensen JC, Malczynski J. Enhanced external counterpulsation - effect on angina pectoris, QoL and exercise capacity after 1 year. Scand Cardiovasc J. 2015;49(1):1–6.10.3109/14017431.2014.994028Search in Google Scholar PubMed
[45] Sathyamoorthy M, Verduzco-Gutierrez M, Varanasi S, Ward R, Spertus J, Shah S. Enhanced external counterpulsation for management of symptoms associated with long COVID. Am Heart J Plus: Cardiol Res Pract. 2022;13:100105.10.1016/j.ahjo.2022.100105Search in Google Scholar PubMed PubMed Central
[46] Raza A, Steinberg K, Tartaglia J, Frishman WH, Gupta T. Enhanced external counterpulsation therapy: Past, present, and future. Cardiol Rev. 2017;25(2):59–67.10.1097/CRD.0000000000000122Search in Google Scholar PubMed
[47] Michaels AD, Accad M, Ports TA, Grossman W. Left ventricular systolic unloading and augmentation of intracoronary pressure and Doppler flow during enhanced external counterpulsation. Circulation. 2002;106(10):1237–42.10.1161/01.CIR.0000028336.95629.B0Search in Google Scholar PubMed
[48] Casey DP, Beck DT, Nichols WW, Conti CR, Choi CY, Khuddus MA, et al. Effects of enhanced external counterpulsation on arterial stiffness and myocardial oxygen demand in patients with chronic angina pectoris. Am J Cardiol. 2011;107(10):1466–72.10.1016/j.amjcard.2011.01.021Search in Google Scholar PubMed PubMed Central
[49] Gloekler S, Meier P, de Marchi SF, Rutz T, Traupe T, Rimoldi SF, et al. Coronary collateral growth by external counterpulsation: A randomised controlled trial. Heart. 2010;96(3):202–7.10.1136/hrt.2009.184507Search in Google Scholar PubMed
[50] Wu E, Desta L, Brostrom A, Martensson J. Effectiveness of enhanced external counterpulsation treatment on symptom burden, medication profile, physical capacity, cardiac anxiety, and health-related quality of life in patients with refractory angina pectoris. J Cardiovasc Nurs. 2020;35(4):375–85.10.1097/JCN.0000000000000638Search in Google Scholar PubMed
[51] May O, Sogaard HJ. Enhanced external counterpulsation is an effective treatment for depression in patients with refractory angina pectoris. Prim Care Companion CNS Disord. 2015;17(4):26325.10.4088/PCC.14m01748Search in Google Scholar PubMed PubMed Central
[52] Davies PF. Hemodynamic shear stress and the endothelium in cardiovascular pathophysiology. Nat Clin Pract Cardiovasc Med. 2009;6(1):16–26.10.1038/ncpcardio1397Search in Google Scholar PubMed PubMed Central
[53] Xu L, Cui M, Zhao W. The effect of EECP on Ischemic Heart Failure: A systematic review. Curr Cardiol Rep. 2023;25(10):1291–8.10.1007/s11886-023-01943-1Search in Google Scholar PubMed PubMed Central
[54] Traub O, Berk BC. Laminar shear stress: Mechanisms by which endothelial cells transduce an atheroprotective force. Arterioscler Thromb Vasc Biol. 1998;18(5):677–85.10.1161/01.ATV.18.5.677Search in Google Scholar
[55] Zhou J, Li YS, Chien S. Shear stress-initiated signaling and its regulation of endothelial function. Arterioscler Thromb Vasc Biol. 2014;34(10):2191–8.10.1161/ATVBAHA.114.303422Search in Google Scholar PubMed PubMed Central
[56] Casey DP, Conti CR, Nichols WW, Choi CY, Khuddus MA, Braith RW. Effect of enhanced external counterpulsation on inflammatory cytokines and adhesion molecules in patients with angina pectoris and angiographic coronary artery disease. Am J Cardiol. 2008;101(3):300–2.10.1016/j.amjcard.2007.08.031Search in Google Scholar PubMed PubMed Central
[57] Wiese O, Zemlin AE, Pillay TS. Molecules in pathogenesis: Angiotensin converting enzyme 2 (ACE2). J Clin Pathol. 2021;74(5):285–90.10.1136/jclinpath-2020-206954Search in Google Scholar PubMed
[58] Qin X, Deng Y, Wu D, Yu L, Huang R. Does enhanced external counterpulsation (EECP) significantly affect myocardial perfusion?: A systematic review & meta-analysis. PLoS One. 2016;11(4):e0151822.10.1371/journal.pone.0151822Search in Google Scholar PubMed PubMed Central
[59] Yang H, Song L, Ning X, Ma Y, Xue A, Zhao H, et al. Enhanced external counterpulsation ameliorates endothelial dysfunction and elevates exercise tolerance in patients with coronary artery disease. Front Cardiovasc Med. 2022;9:997109.10.3389/fcvm.2022.997109Search in Google Scholar PubMed PubMed Central
[60] Beck DT, Martin JS, Casey DP, Avery JC, Sardina PD, Braith RW. Enhanced external counterpulsation improves endothelial function and exercise capacity in patients with ischaemic left ventricular dysfunction. Clin Exp Pharmacol Physiol. 2014;41(9):628–36.10.1111/1440-1681.12263Search in Google Scholar PubMed PubMed Central
[61] Luo C, Liu D, Wu G, Hu C, Zhang Y, Du Z, et al. Effect of enhanced external counterpulsation on coronary slow flow and its relation with endothelial function and inflammation: a mid-term follow-up study. Cardiology. 2012;122(4):260–8.10.1159/000339876Search in Google Scholar PubMed
[62] Zhan Y, Zhang Y, Zhang A, Xiang J. Perceived stress and cardiovascular disease in a community-based population. Heart Mind. 2022;6(4):262–6.10.4103/hm.hm_55_22Search in Google Scholar
[63] Moser DK, McKinley S, Riegel B, Doering LV, Meischke H, Pelter M, et al. Relationship of persistent symptoms of anxiety to morbidity and mortality outcomes in patients with coronary heart disease. Psychosom Med. 2011;73(9):803–9.10.1097/PSY.0b013e3182364992Search in Google Scholar PubMed
[64] Roest AM, Martens EJ, Denollet J, de Jonge P. Prognostic association of anxiety post myocardial infarction with mortality and new cardiac events: A meta-analysis. Psychosom Med. 2010;72(6):563–9.10.1097/PSY.0b013e3181dbff97Search in Google Scholar PubMed
[65] de Miranda Azevedo R, Roest AM, Hoen PW, de Jonge P. Cognitive/affective and somatic/affective symptoms of depression in patients with heart disease and their association with cardiovascular prognosis: A meta-analysis. Psychol Med. 2014;44(13):2689–703.10.1017/S0033291714000063Search in Google Scholar PubMed
[66] Piva T, Masotti S, Raisi A, Zerbini V, Grazzi G, Mazzoni G, et al. Exercise program for the management of anxiety and depression in adults and elderly subjects: Is it applicable to patients with post-covid-19 condition? A systematic review and meta-analysis. J Affect Disord. 2023;325:273–81.10.1016/j.jad.2022.12.155Search in Google Scholar PubMed PubMed Central
[67] Gómez L, Vidal B, Cabrera Y, Hernández L, Rondón Y. Successful treatment of post-COVID symptoms with transcranial direct current stimulation. Prim Care Companion CNS Disord. 2021;23(6):21cr03059.10.4088/PCC.21cr03059Search in Google Scholar PubMed
[68] Hattesohl M, Feistel B, Sievers H, Lehnfeld R, Hegger M, Winterhoff H. Extracts of Valeriana officinalis L. s.l. show anxiolytic and antidepressant effects but neither sedative nor myorelaxant properties. Phytomed: Int J Phytother Phytopharmacol. 2008;15(1–2):2–15.10.1016/j.phymed.2007.11.027Search in Google Scholar PubMed
[69] Akhondzadeh S, Naghavi HR, Vazirian M, Shayeganpour A, Rashidi H, Khani M. Passionflower in the treatment of generalized anxiety: a pilot double-blind randomized controlled trial with oxazepam. J Clin Pharm Ther. 2001;26(5):363–7.10.1046/j.1365-2710.2001.00367.xSearch in Google Scholar PubMed
[70] Nawrot J, Gornowicz-Porowska J, Budzianowski J, Nowak G, Schroeder G, Kurczewska J. Medicinal herbs in the relief of neurological, cardiovascular, and respiratory symptoms after COVID-19 infection a literature review. Cells. 2022;11(12):1897.10.3390/cells11121897Search in Google Scholar PubMed PubMed Central
[71] Kasper S, Eckert A, Möller HJ, Volz HP, Seifritz E. Psychiatric manifestations of post-COVID-19 syndrome: The potential benefit of Silexan. Int J Psychiatry Clin Pract. 2023;27(3):285–91.10.1080/13651501.2023.2187308Search in Google Scholar PubMed
[72] Santana K, França E, Sato J, Silva A, Queiroz M, de Farias J, et al. Non-invasive brain stimulation for fatigue in post-acute sequelae of SARS-CoV-2 (PASC). Brain Stimul. 2023;16(1):100–7.10.1016/j.brs.2023.01.1672Search in Google Scholar PubMed PubMed Central
© 2025 the author(s), published by De Gruyter
This work is licensed under the Creative Commons Attribution 4.0 International License.
Articles in the same Issue
- Research Articles
- Network pharmacological analysis and in vitro testing of the rutin effects on triple-negative breast cancer
- Impact of diabetes on long-term survival in elderly liver cancer patients: A retrospective study
- Knockdown of CCNB1 alleviates high glucose-triggered trophoblast dysfunction during gestational diabetes via Wnt/β-catenin signaling pathway
- Risk factors for severe adverse drug reactions in hospitalized patients
- Analysis of the effect of ALA-PDT on macrophages in footpad model of mice infected with Fonsecaea monophora based on single-cell sequencing
- Development and validation of headspace gas chromatography with a flame ionization detector method for the determination of ethanol in the vitreous humor
- CMSP exerts anti-tumor effects on small cell lung cancer cells by inducing mitochondrial dysfunction and ferroptosis
- Predictive value of plasma sB7-H3 and YKL-40 in pediatric refractory Mycoplasma pneumoniae pneumonia
- Antiangiogenic potential of Elaeagnus umbellata extracts and molecular docking study by targeting VEGFR-2 pathway
- Comparison of the effectiveness of nurse-led preoperative counseling and postoperative follow-up care vs standard care for patients with gastric cancer
- Comparing the therapeutic efficacy of endoscopic minimally invasive surgery and traditional surgery for early-stage breast cancer: A meta-analysis
- Adhered macrophages as an additional marker of cardiomyocyte injury in biopsies of patients with dilated cardiomyopathy
- Association between statin administration and outcome in patients with sepsis: A retrospective study
- Exploration of the association between estimated glucose disposal rate and osteoarthritis in middle-aged and older adults: An analysis of NHANES data from 2011 to 2018
- A comparative analysis of the binary and multiclass classified chest X-ray images of pneumonia and COVID-19 with ML and DL models
- Lysophosphatidic acid 2 alleviates deep vein thrombosis via protective endothelial barrier function
- Transcription factor A, mitochondrial promotes lymph node metastasis and lymphangiogenesis in epithelial ovarian carcinoma
- Serum PM20D1 levels are associated with nutritional status and inflammatory factors in gastric cancer patients undergoing early enteral nutrition
- Hydromorphone reduced the incidence of emergence agitation after adenotonsillectomy in children with obstructive sleep apnea: A randomized, double-blind study
- Vitamin D replacement therapy may regulate sleep habits in patients with restless leg syndrome
- The first-line antihypertensive nitrendipine potentiated the therapeutic effect of oxaliplatin by downregulating CACNA1D in colorectal cancer
- Health literacy and health-related quality of life: The mediating role of irrational happiness
- Modulatory effects of Lycium barbarum polysaccharide on bone cell dynamics in osteoporosis
- Mechanism research on inhibition of gastric cancer in vitro by the extract of Pinellia ternata based on network pharmacology and cellular metabolomics
- Examination of the causal role of immune cells in non-alcoholic fatty liver disease by a bidirectional Mendelian randomization study
- Clinical analysis of ten cases of HIV infection combined with acute leukemia
- Investigating the cardioprotective potential of quercetin against tacrolimus-induced cardiotoxicity in Wistar rats: A mechanistic insights
- Clinical observation of probiotics combined with mesalazine and Yiyi Baitouweng Decoction retention enema in treating mild-to-moderate ulcerative colitis
- Diagnostic value of ratio of blood inflammation to coagulation markers in periprosthetic joint infection
- Sex-specific associations of sex hormone binding globulin and risk of bladder cancer
- Core muscle strength and stability-oriented breathing training reduces inter-recti distance in postpartum women
- The ERAS nursing care strategy for patients undergoing transsphenoidal endoscopic pituitary tumor resection: A randomized blinded controlled trial
- The serum IL-17A levels in patients with traumatic bowel rupture post-surgery and its predictive value for patient prognosis
- Impact of Kolb’s experiential learning theory-based nursing on caregiver burden and psychological state of caregivers of dementia patients
- Analysis of serum NLR combined with intraoperative margin condition to predict the prognosis of cervical HSIL patients undergoing LEEP surgery
- Commiphora gileadensis ameliorate infertility and erectile dysfunction in diabetic male mice
- The correlation between epithelial–mesenchymal transition classification and MMP2 expression of circulating tumor cells and prognosis of advanced or metastatic nasopharyngeal carcinoma
- Tetrahydropalmatine improves mitochondrial function in vascular smooth muscle cells of atherosclerosis in vitro by inhibiting Ras homolog gene family A/Rho-associated protein kinase-1 signaling pathway
- A cross-sectional study: Relationship between serum oxidative stress levels and arteriovenous fistula maturation in maintenance dialysis patients
- A comparative analysis of the impact of repeated administration of flavan 3-ol on brown, subcutaneous, and visceral adipose tissue
- Identifying early screening factors for depression in middle-aged and older adults: A cohort study
- Perform tumor-specific survival analysis for Merkel cell carcinoma patients undergoing surgical resection based on the SEER database by constructing a nomogram chart
- Unveiling the role of CXCL10 in pancreatic cancer progression: A novel prognostic indicator
- High-dose preoperative intraperitoneal erythropoietin and intravenous methylprednisolone in acute traumatic spinal cord injuries following decompression surgeries
- RAB39B: A novel biomarker for acute myeloid leukemia identified via multi-omics and functional validation
- Impact of peripheral conditioning on reperfusion injury following primary percutaneous coronary intervention in diabetic and non-diabetic STEMI patients
- Clinical efficacy of azacitidine in the treatment of middle- and high-risk myelodysplastic syndrome in middle-aged and elderly patients: A retrospective study
- The effect of ambulatory blood pressure load on mitral regurgitation in continuous ambulatory peritoneal dialysis patients
- Expression and clinical significance of ITGA3 in breast cancer
- Single-nucleus RNA sequencing reveals ARHGAP28 expression of podocytes as a biomarker in human diabetic nephropathy
- rSIG combined with NLR in the prognostic assessment of patients with multiple injuries
- Toxic metals and metalloids in collagen supplements of fish and jellyfish origin: Risk assessment for daily intake
- Exploring causal relationship between 41 inflammatory cytokines and marginal zone lymphoma: A bidirectional Mendelian randomization study
- Gender beliefs and legitimization of dating violence in adolescents
- Effect of serum IL-6, CRP, and MMP-9 levels on the efficacy of modified preperitoneal Kugel repair in patients with inguinal hernia
- Effect of smoking and smoking cessation on hematological parameters in polycythemic patients
- Pathogen surveillance and risk factors for pulmonary infection in patients with lung cancer: A retrospective single-center study
- Necroptosis of hippocampal neurons in paclitaxel chemotherapy-induced cognitive impairment mediates microglial activation via TLR4/MyD88 signaling pathway
- Celastrol suppresses neovascularization in rat aortic vascular endothelial cells stimulated by inflammatory tenocytes via modulating the NLRP3 pathway
- Cord-lamina angle and foraminal diameter as key predictors of C5 palsy after anterior cervical decompression and fusion surgery
- GATA1: A key biomarker for predicting the prognosis of patients with diffuse large B-cell lymphoma
- Influencing factors of false lumen thrombosis in type B aortic dissection: A single-center retrospective study
- MZB1 regulates the immune microenvironment and inhibits ovarian cancer cell migration
- Integrating experimental and network pharmacology to explore the pharmacological mechanisms of Dioscin against glioblastoma
- Trends in research on preterm birth in twin pregnancy based on bibliometrics
- Four-week IgE/baseline IgE ratio combined with tryptase predicts clinical outcome in omalizumab-treated children with moderate-to-severe asthma
- Single-cell transcriptomic analysis identifies a stress response Schwann cell subtype
- Acute pancreatitis risk in the diagnosis and management of inflammatory bowel disease: A critical focus
- Effect of subclinical esketamine on NLRP3 and cognitive dysfunction in elderly ischemic stroke patients
- Interleukin-37 mediates the anti-oral tumor activity in oral cancer through STAT3
- CA199 and CEA expression levels, and minimally invasive postoperative prognosis analysis in esophageal squamous carcinoma patients
- Efficacy of a novel drainage catheter in the treatment of CSF leak after posterior spine surgery: A retrospective cohort study
- Comprehensive biomedicine assessment of Apteranthes tuberculata extracts: Phytochemical analysis and multifaceted pharmacological evaluation in animal models
- Relation of time in range to severity of coronary artery disease in patients with type 2 diabetes: A cross-sectional study
- Dopamine attenuates ethanol-induced neuronal apoptosis by stimulating electrical activity in the developing rat retina
- Correlation between albumin levels during the third trimester and the risk of postpartum levator ani muscle rupture
- Factors associated with maternal attention and distraction during breastfeeding and childcare: A cross-sectional study in the west of Iran
- Mechanisms of hesperetin in treating metabolic dysfunction-associated steatosis liver disease via network pharmacology and in vitro experiments
- The law on oncological oblivion in the Italian and European context: How to best uphold the cancer patients’ rights to privacy and self-determination?
- The prognostic value of the neutrophil-to-lymphocyte ratio, platelet-to-lymphocyte ratio, and prognostic nutritional index for survival in patients with colorectal cancer
- Factors affecting the measurements of peripheral oxygen saturation values in healthy young adults
- Comparison and correlations between findings of hysteroscopy and vaginal color Doppler ultrasonography for detection of uterine abnormalities in patients with recurrent implantation failure
- The effects of different types of RAGT on balance function in stroke patients with low levels of independent walking in a convalescent rehabilitation hospital
- Causal relationship between asthma and ankylosing spondylitis: A bidirectional two-sample univariable and multivariable Mendelian randomization study
- Correlations of health literacy with individuals’ understanding and use of medications in Southern Taiwan
- Correlation of serum calprotectin with outcome of acute cerebral infarction
- Comparison of computed tomography and guided bronchoscopy in the diagnosis of pulmonary nodules: A systematic review and meta-analysis
- Curdione protects vascular endothelial cells and atherosclerosis via the regulation of DNMT1-mediated ERBB4 promoter methylation
- The identification of novel missense variant in ChAT gene in a patient with gestational diabetes denotes plausible genetic association
- Molecular genotyping of multi-system rare blood types in foreign blood donors based on DNA sequencing and its clinical significance
- Exploring the role of succinyl carnitine in the association between CD39⁺ CD4⁺ T cell and ulcerative colitis: A Mendelian randomization study
- Dexmedetomidine suppresses microglial activation in postoperative cognitive dysfunction via the mmu-miRNA-125/TRAF6 signaling axis
- Analysis of serum metabolomics in patients with different types of chronic heart failure
- Diagnostic value of hematological parameters in the early diagnosis of acute cholecystitis
- Pachymaran alleviates fat accumulation, hepatocyte degeneration, and injury in mice with nonalcoholic fatty liver disease
- Decrease in CD4 and CD8 lymphocytes are predictors of severe clinical picture and unfavorable outcome of the disease in patients with COVID-19
- METTL3 blocked the progression of diabetic retinopathy through m6A-modified SOX2
- The predictive significance of anti-RO-52 antibody in patients with interstitial pneumonia after treatment of malignant tumors
- Exploring cerebrospinal fluid metabolites, cognitive function, and brain atrophy: Insights from Mendelian randomization
- Development and validation of potential molecular subtypes and signatures of ocular sarcoidosis based on autophagy-related gene analysis
- Widespread venous thrombosis: Unveiling a complex case of Behçet’s disease with a literature perspective
- Uterine fibroid embolization: An analysis of clinical outcomes and impact on patients’ quality of life
- Discovery of lipid metabolism-related diagnostic biomarkers and construction of diagnostic model in steroid-induced osteonecrosis of femoral head
- Serum-derived exomiR-188-3p is a promising novel biomarker for early-stage ovarian cancer
- Enhancing chronic back pain management: A comparative study of ultrasound–MRI fusion guidance for paravertebral nerve block
- Peptide CCAT1-70aa promotes hepatocellular carcinoma proliferation and invasion via the MAPK/ERK pathway
- Electroacupuncture-induced reduction of myocardial ischemia–reperfusion injury via FTO-dependent m6A methylation modulation
- Hemorrhoids and cardiovascular disease: A bidirectional Mendelian randomization study
- Cell-free adipose extract inhibits hypertrophic scar formation through collagen remodeling and antiangiogenesis
- HALP score in Demodex blepharitis: A case–control study
- Assessment of SOX2 performance as a marker for circulating cancer stem-like cells (CCSCs) identification in advanced breast cancer patients using CytoTrack system
- Risk and prognosis for brain metastasis in primary metastatic cervical cancer patients: A population-based study
- Comparison of the two intestinal anastomosis methods in pediatric patients
- Factors influencing hematological toxicity and adverse effects of perioperative hyperthermic intraperitoneal vs intraperitoneal chemotherapy in gastrointestinal cancer
- Endotoxin tolerance inhibits NLRP3 inflammasome activation in macrophages of septic mice by restoring autophagic flux through TRIM26
- Lateral transperitoneal laparoscopic adrenalectomy: A single-centre experience of 21 procedures
- Petunidin attenuates lipopolysaccharide-induced retinal microglia inflammatory response in diabetic retinopathy by targeting OGT/NF-κB/LCN2 axis
- Procalcitonin and C-reactive protein as biomarkers for diagnosing and assessing the severity of acute cholecystitis
- Factors determining the number of sessions in successful extracorporeal shock wave lithotripsy patients
- Development of a nomogram for predicting cancer-specific survival in patients with renal pelvic cancer following surgery
- Inhibition of ATG7 promotes orthodontic tooth movement by regulating the RANKL/OPG ratio under compression force
- A machine learning-based prognostic model integrating mRNA stemness index, hypoxia, and glycolysis‑related biomarkers for colorectal cancer
- Glutathione attenuates sepsis-associated encephalopathy via dual modulation of NF-κB and PKA/CREB pathways
- FAHD1 prevents neuronal ferroptosis by modulating R-loop and the cGAS–STING pathway
- Association of placenta weight and morphology with term low birth weight: A case–control study
- Investigation of the pathogenic variants induced Sjogren’s syndrome in Turkish population
- Nucleotide metabolic abnormalities in post-COVID-19 condition and type 2 diabetes mellitus patients and their association with endocrine dysfunction
- TGF-β–Smad2/3 signaling in high-altitude pulmonary hypertension in rats: Role and mechanisms via macrophage M2 polarization
- Ultrasound-guided unilateral versus bilateral erector spinae plane block for postoperative analgesia of patients undergoing laparoscopic cholecystectomy
- Profiling gut microbiome dynamics in subacute thyroiditis: Implications for pathogenesis, diagnosis, and treatment
- Delta neutrophil index, CRP/albumin ratio, procalcitonin, immature granulocytes, and HALP score in acute appendicitis: Best performing biomarker?
- Anticancer activity mechanism of novelly synthesized and characterized benzofuran ring-linked 3-nitrophenyl chalcone derivative on colon cancer cells
- H2valdien3 arrests the cell cycle and induces apoptosis of gastric cancer
- Prognostic relevance of PRSS2 and its immune correlates in papillary thyroid carcinoma
- Association of SGLT2 inhibition with psychiatric disorders: A Mendelian randomization study
- Motivational interviewing for alcohol use reduction in Thai patients
- Luteolin alleviates oxygen-glucose deprivation/reoxygenation-induced neuron injury by regulating NLRP3/IL-1β signaling
- Polyphyllin II inhibits thyroid cancer cell growth by simultaneously inhibiting glycolysis and oxidative phosphorylation
- Relationship between the expression of copper death promoting factor SLC31A1 in papillary thyroid carcinoma and clinicopathological indicators and prognosis
- CSF2 polarized neutrophils and invaded renal cancer cells in vitro influence
- Proton pump inhibitors-induced thrombocytopenia: A systematic literature analysis of case reports
- The current status and influence factors of research ability among community nurses: A sequential qualitative–quantitative study
- OKAIN: A comprehensive oncology knowledge base for the interpretation of clinically actionable alterations
- The relationship between serum CA50, CA242, and SAA levels and clinical pathological characteristics and prognosis in patients with pancreatic cancer
- Identification and external validation of a prognostic signature based on hypoxia–glycolysis-related genes for kidney renal clear cell carcinoma
- Engineered RBC-derived nanovesicles functionalized with tumor-targeting ligands: A comparative study on breast cancer targeting efficiency and biocompatibility
- Relationship of resting echocardiography combined with serum micronutrients to the severity of low-gradient severe aortic stenosis
- Effect of vibration on pain during subcutaneous heparin injection: A randomized, single-blind, placebo-controlled trial
- The diagnostic performance of machine learning-based FFRCT for coronary artery disease: A meta-analysis
- Comparing biofeedback device vs diaphragmatic breathing for bloating relief: A randomized controlled trial
- Serum uric acid to albumin ratio and C-reactive protein as predictive biomarkers for chronic total occlusion and coronary collateral circulation quality
- Multiple organ scoring systems for predicting in-hospital mortality of sepsis patients in the intensive care unit
- Single-cell RNA sequencing data analysis of the inner ear in gentamicin-treated mice via intraperitoneal injection
- Suppression of cathepsin B attenuates myocardial injury via limiting cardiomyocyte apoptosis
- Influence of sevoflurane combined with propofol anesthesia on the anesthesia effect and adverse reactions in children with acute appendicitis
- Identification of hub genes related to acute kidney injury caused by sevoflurane anesthesia and endoplasmic reticulum stress
- Efficacy and safety of PD-1/PD-L1 inhibitors in pancreatic ductal adenocarcinoma: a systematic review and Meta-analysis of randomized controlled trials
- The value of diagnostic experience in O-RADS MRI score for ovarian-adnexal lesions
- Health education pathway for individuals with temporary enterostomies using patient journey mapping
- Serum TLR8 as a potential diagnostic biomarker of coronary heart disease
- Intraoperative temperature management and its effect on surgical outcomes in elderly patients undergoing lichtenstein unilateral inguinal hernia repair
- Immunohistochemical profiling and neuroepithelial heterogeneity in immature ovarian teratomas: a retrospective digital pathology-based study
- Associated risk factors and prevalence of human papillomavirus infection among females visiting tertiary care hospital: a cross-sectional study from Nepal
- Comparative evaluation of various disc elution methods for the detection of colistin-resistant gram-negative bacteria
- Effect of timing of cholecystectomy on weight loss after sleeve gastrectomy in morbidly obese individuals with cholelithiasis: a retrospective cohort study
- Causal association between ceramide levels and central precocious puberty: a mendelian randomization study
- Novel predictive model for colorectal liver metastases recurrence: a radiomics and clinical data approach
- Relationship between resident physicians’ perceived professional value and exposure to violence
- Multiple sclerosis and type 1 diabetes: a Mendelian randomization study of European ancestry
- Rapid pathogen identification in peritoneal dialysis effluent by MALDI-TOF MS following blood culture enrichment
- Comparison of open and percutaneous A1 pulley release in pediatric trigger thumb: a retrospective cohort study
- Impact of combined diaphragm-lung ultrasound assessment on postoperative respiratory function in patients under general anesthesia recovery
- Development and internal validation of a nomogram for predicting short-term prognosis in ICU patients with acute pyelonephritis
- The association between hypoxic burden and blood pressure in patients with obstructive sleep apnea
- Promotion of asthenozoospermia by C9orf72 through suppression of spermatogonia activity via fructose metabolism and mitophagy
- Review Articles
- The effects of enhanced external counter-pulsation on post-acute sequelae of COVID-19: A narrative review
- Diabetes-related cognitive impairment: Mechanisms, symptoms, and treatments
- Microscopic changes and gross morphology of placenta in women affected by gestational diabetes mellitus in dietary treatment: A systematic review
- Review of mechanisms and frontier applications in IL-17A-induced hypertension
- Research progress on the correlation between islet amyloid peptides and type 2 diabetes mellitus
- The safety and efficacy of BCG combined with mitomycin C compared with BCG monotherapy in patients with non-muscle-invasive bladder cancer: A systematic review and meta-analysis
- The application of augmented reality in robotic general surgery: A mini-review
- The effect of Greek mountain tea extract and wheat germ extract on peripheral blood flow and eicosanoid metabolism in mammals
- Neurogasobiology of migraine: Carbon monoxide, hydrogen sulfide, and nitric oxide as emerging pathophysiological trinacrium relevant to nociception regulation
- Plant polyphenols, terpenes, and terpenoids in oral health
- Laboratory medicine between technological innovation, rights safeguarding, and patient safety: A bioethical perspective
- End-of-life in cancer patients: Medicolegal implications and ethical challenges in Europe
- The maternal factors during pregnancy for intrauterine growth retardation: An umbrella review
- Intra-abdominal hypertension/abdominal compartment syndrome of pediatric patients in critical care settings
- PI3K/Akt pathway and neuroinflammation in sepsis-associated encephalopathy
- Screening of Group B Streptococcus in pregnancy: A systematic review for the laboratory detection
- Giant borderline ovarian tumours – review of the literature
- Leveraging artificial intelligence for collaborative care planning: Innovations and impacts in shared decision-making – A systematic review
- Cholera epidemiology analysis through the experience of the 1973 Naples epidemic
- Risk factors of frailty/sarcopenia in community older adults: Meta-analysis
- Supplement strategies for infertility in overweight women: Evidence and legal insights
- Scurvy, a not obsolete disorder: Clinical report in eight young children and literature review
- A meta-analysis of the effects of DBS on cognitive function in patients with advanced PD
- Protective role of selenium in sepsis: Mechanisms and potential therapeutic strategies
- Strategies for hyperkalemia management in dialysis patients: A systematic review
- C-reactive protein-to-albumin ratio in peripheral artery disease
- Research progress on autophagy and its roles in sepsis induced organ injury
- Neuronutrition in autism spectrum disorders
- Pumilio 2 in neural development, function, and specific neurological disorders
- Antibiotic prescribing patterns in general dental practice- a scoping review
- Clinical and medico-legal reflections on non-invasive prenatal testing
- Smartphone use and back pain: a narrative review of postural pathologies
- Targeting endothelial oxidative stress in hypertension
- Exploring links between acne and metabolic syndrome: a narrative review
- Case Reports
- Delayed graft function after renal transplantation
- Semaglutide treatment for type 2 diabetes in a patient with chronic myeloid leukemia: A case report and review of the literature
- Diverse electrophysiological demyelinating features in a late-onset glycogen storage disease type IIIa case
- Giant right atrial hemangioma presenting with ascites: A case report
- Laser excision of a large granular cell tumor of the vocal cord with subglottic extension: A case report
- EsoFLIP-assisted dilation for dysphagia in systemic sclerosis: Highlighting the role of multimodal esophageal evaluation
- Molecular hydrogen-rhodiola as an adjuvant therapy for ischemic stroke in internal carotid artery occlusion: A case report
- Coronary artery anomalies: A case of the “malignant” left coronary artery and its surgical management
- Combined VAT and retroperitoneoscopy for pleural empyema due to nephro-pleuric fistula in xanthogranulomatous pyelonephritis
- A rare case of Opalski syndrome with a suspected multiple sclerosis etiology
- Newly diagnosed B-cell acute lymphoblastic leukemia demonstrating localized bone marrow infiltration exclusively in the lower extremities
- Rapid Communication
- Biological properties of valve materials using RGD and EC
-
A single oral administration of flavanols enhances short
-term memory in mice along with increased brain-derived neurotrophic factor - Repeat influenza incidence across two consecutive influenza seasons
- Letter to the Editor
- Role of enhanced external counterpulsation in long COVID
- Expression of Concern
- Expression of concern “A ceRNA network mediated by LINC00475 in papillary thyroid carcinoma”
- Expression of concern “Notoginsenoside R1 alleviates spinal cord injury through the miR-301a/KLF7 axis to activate Wnt/β-catenin pathway”
- Expression of concern “circ_0020123 promotes cell proliferation and migration in lung adenocarcinoma via PDZD8”
- Corrigendum
- Corrigendum to “Empagliflozin improves aortic injury in obese mice by regulating fatty acid metabolism”
- Corrigendum to “Comparing the therapeutic efficacy of endoscopic minimally invasive surgery and traditional surgery for early-stage breast cancer: A meta-analysis”
- Corrigendum to “The progress of autoimmune hepatitis research and future challenges”
- Retraction
- Retraction of “miR-654-5p promotes gastric cancer progression via the GPRIN1/NF-κB pathway”
- Retraction of: “LncRNA CASC15 inhibition relieves renal fibrosis in diabetic nephropathy through downregulating SP-A by sponging to miR-424”
- Retraction of: “SCARA5 inhibits oral squamous cell carcinoma via inactivating the STAT3 and PI3K/AKT signaling pathways”
- Special Issue Advancements in oncology: bridging clinical and experimental research - Part II
- Unveiling novel biomarkers for platinum chemoresistance in ovarian cancer
- Lathyrol affects the expression of AR and PSA and inhibits the malignant behavior of RCC cells
- The era of increasing cancer survivorship: Trends in fertility preservation, medico-legal implications, and ethical challenges
- Bone scintigraphy and positron emission tomography in the early diagnosis of MRONJ
- Meta-analysis of clinical efficacy and safety of immunotherapy combined with chemotherapy in non-small cell lung cancer
- Special Issue Computational Intelligence Methodologies Meets Recurrent Cancers - Part IV
- Exploration of mRNA-modifying METTL3 oncogene as momentous prognostic biomarker responsible for colorectal cancer development
- Special Issue The evolving saga of RNAs from bench to bedside - Part III
- Interaction and verification of ferroptosis-related RNAs Rela and Stat3 in promoting sepsis-associated acute kidney injury
- The mRNA MOXD1: Link to oxidative stress and prognostic significance in gastric cancer
- Special Issue Exploring the biological mechanism of human diseases based on MultiOmics Technology - Part II
- Dynamic changes in lactate-related genes in microglia and their role in immune cell interactions after ischemic stroke
- A prognostic model correlated with fatty acid metabolism in Ewing’s sarcoma based on bioinformatics analysis
- Red cell distribution width predicts early kidney injury: A NHANES cross-sectional study
- Special Issue Diabetes mellitus: pathophysiology, complications & treatment
- Nutritional risk assessment and nutritional support in children with congenital diabetes during surgery
- Correlation of the differential expressions of RANK, RANKL, and OPG with obesity in the elderly population in Xinjiang
- A discussion on the application of fluorescence micro-optical sectioning tomography in the research of cognitive dysfunction in diabetes
- A review of brain research on T2DM-related cognitive dysfunction
- Metformin and estrogen modulation in LABC with T2DM: A 36-month randomized trial
- Special Issue Innovative Biomarker Discovery and Precision Medicine in Cancer Diagnostics
- CircASH1L-mediated tumor progression in triple-negative breast cancer: PI3K/AKT pathway mechanisms
Articles in the same Issue
- Research Articles
- Network pharmacological analysis and in vitro testing of the rutin effects on triple-negative breast cancer
- Impact of diabetes on long-term survival in elderly liver cancer patients: A retrospective study
- Knockdown of CCNB1 alleviates high glucose-triggered trophoblast dysfunction during gestational diabetes via Wnt/β-catenin signaling pathway
- Risk factors for severe adverse drug reactions in hospitalized patients
- Analysis of the effect of ALA-PDT on macrophages in footpad model of mice infected with Fonsecaea monophora based on single-cell sequencing
- Development and validation of headspace gas chromatography with a flame ionization detector method for the determination of ethanol in the vitreous humor
- CMSP exerts anti-tumor effects on small cell lung cancer cells by inducing mitochondrial dysfunction and ferroptosis
- Predictive value of plasma sB7-H3 and YKL-40 in pediatric refractory Mycoplasma pneumoniae pneumonia
- Antiangiogenic potential of Elaeagnus umbellata extracts and molecular docking study by targeting VEGFR-2 pathway
- Comparison of the effectiveness of nurse-led preoperative counseling and postoperative follow-up care vs standard care for patients with gastric cancer
- Comparing the therapeutic efficacy of endoscopic minimally invasive surgery and traditional surgery for early-stage breast cancer: A meta-analysis
- Adhered macrophages as an additional marker of cardiomyocyte injury in biopsies of patients with dilated cardiomyopathy
- Association between statin administration and outcome in patients with sepsis: A retrospective study
- Exploration of the association between estimated glucose disposal rate and osteoarthritis in middle-aged and older adults: An analysis of NHANES data from 2011 to 2018
- A comparative analysis of the binary and multiclass classified chest X-ray images of pneumonia and COVID-19 with ML and DL models
- Lysophosphatidic acid 2 alleviates deep vein thrombosis via protective endothelial barrier function
- Transcription factor A, mitochondrial promotes lymph node metastasis and lymphangiogenesis in epithelial ovarian carcinoma
- Serum PM20D1 levels are associated with nutritional status and inflammatory factors in gastric cancer patients undergoing early enteral nutrition
- Hydromorphone reduced the incidence of emergence agitation after adenotonsillectomy in children with obstructive sleep apnea: A randomized, double-blind study
- Vitamin D replacement therapy may regulate sleep habits in patients with restless leg syndrome
- The first-line antihypertensive nitrendipine potentiated the therapeutic effect of oxaliplatin by downregulating CACNA1D in colorectal cancer
- Health literacy and health-related quality of life: The mediating role of irrational happiness
- Modulatory effects of Lycium barbarum polysaccharide on bone cell dynamics in osteoporosis
- Mechanism research on inhibition of gastric cancer in vitro by the extract of Pinellia ternata based on network pharmacology and cellular metabolomics
- Examination of the causal role of immune cells in non-alcoholic fatty liver disease by a bidirectional Mendelian randomization study
- Clinical analysis of ten cases of HIV infection combined with acute leukemia
- Investigating the cardioprotective potential of quercetin against tacrolimus-induced cardiotoxicity in Wistar rats: A mechanistic insights
- Clinical observation of probiotics combined with mesalazine and Yiyi Baitouweng Decoction retention enema in treating mild-to-moderate ulcerative colitis
- Diagnostic value of ratio of blood inflammation to coagulation markers in periprosthetic joint infection
- Sex-specific associations of sex hormone binding globulin and risk of bladder cancer
- Core muscle strength and stability-oriented breathing training reduces inter-recti distance in postpartum women
- The ERAS nursing care strategy for patients undergoing transsphenoidal endoscopic pituitary tumor resection: A randomized blinded controlled trial
- The serum IL-17A levels in patients with traumatic bowel rupture post-surgery and its predictive value for patient prognosis
- Impact of Kolb’s experiential learning theory-based nursing on caregiver burden and psychological state of caregivers of dementia patients
- Analysis of serum NLR combined with intraoperative margin condition to predict the prognosis of cervical HSIL patients undergoing LEEP surgery
- Commiphora gileadensis ameliorate infertility and erectile dysfunction in diabetic male mice
- The correlation between epithelial–mesenchymal transition classification and MMP2 expression of circulating tumor cells and prognosis of advanced or metastatic nasopharyngeal carcinoma
- Tetrahydropalmatine improves mitochondrial function in vascular smooth muscle cells of atherosclerosis in vitro by inhibiting Ras homolog gene family A/Rho-associated protein kinase-1 signaling pathway
- A cross-sectional study: Relationship between serum oxidative stress levels and arteriovenous fistula maturation in maintenance dialysis patients
- A comparative analysis of the impact of repeated administration of flavan 3-ol on brown, subcutaneous, and visceral adipose tissue
- Identifying early screening factors for depression in middle-aged and older adults: A cohort study
- Perform tumor-specific survival analysis for Merkel cell carcinoma patients undergoing surgical resection based on the SEER database by constructing a nomogram chart
- Unveiling the role of CXCL10 in pancreatic cancer progression: A novel prognostic indicator
- High-dose preoperative intraperitoneal erythropoietin and intravenous methylprednisolone in acute traumatic spinal cord injuries following decompression surgeries
- RAB39B: A novel biomarker for acute myeloid leukemia identified via multi-omics and functional validation
- Impact of peripheral conditioning on reperfusion injury following primary percutaneous coronary intervention in diabetic and non-diabetic STEMI patients
- Clinical efficacy of azacitidine in the treatment of middle- and high-risk myelodysplastic syndrome in middle-aged and elderly patients: A retrospective study
- The effect of ambulatory blood pressure load on mitral regurgitation in continuous ambulatory peritoneal dialysis patients
- Expression and clinical significance of ITGA3 in breast cancer
- Single-nucleus RNA sequencing reveals ARHGAP28 expression of podocytes as a biomarker in human diabetic nephropathy
- rSIG combined with NLR in the prognostic assessment of patients with multiple injuries
- Toxic metals and metalloids in collagen supplements of fish and jellyfish origin: Risk assessment for daily intake
- Exploring causal relationship between 41 inflammatory cytokines and marginal zone lymphoma: A bidirectional Mendelian randomization study
- Gender beliefs and legitimization of dating violence in adolescents
- Effect of serum IL-6, CRP, and MMP-9 levels on the efficacy of modified preperitoneal Kugel repair in patients with inguinal hernia
- Effect of smoking and smoking cessation on hematological parameters in polycythemic patients
- Pathogen surveillance and risk factors for pulmonary infection in patients with lung cancer: A retrospective single-center study
- Necroptosis of hippocampal neurons in paclitaxel chemotherapy-induced cognitive impairment mediates microglial activation via TLR4/MyD88 signaling pathway
- Celastrol suppresses neovascularization in rat aortic vascular endothelial cells stimulated by inflammatory tenocytes via modulating the NLRP3 pathway
- Cord-lamina angle and foraminal diameter as key predictors of C5 palsy after anterior cervical decompression and fusion surgery
- GATA1: A key biomarker for predicting the prognosis of patients with diffuse large B-cell lymphoma
- Influencing factors of false lumen thrombosis in type B aortic dissection: A single-center retrospective study
- MZB1 regulates the immune microenvironment and inhibits ovarian cancer cell migration
- Integrating experimental and network pharmacology to explore the pharmacological mechanisms of Dioscin against glioblastoma
- Trends in research on preterm birth in twin pregnancy based on bibliometrics
- Four-week IgE/baseline IgE ratio combined with tryptase predicts clinical outcome in omalizumab-treated children with moderate-to-severe asthma
- Single-cell transcriptomic analysis identifies a stress response Schwann cell subtype
- Acute pancreatitis risk in the diagnosis and management of inflammatory bowel disease: A critical focus
- Effect of subclinical esketamine on NLRP3 and cognitive dysfunction in elderly ischemic stroke patients
- Interleukin-37 mediates the anti-oral tumor activity in oral cancer through STAT3
- CA199 and CEA expression levels, and minimally invasive postoperative prognosis analysis in esophageal squamous carcinoma patients
- Efficacy of a novel drainage catheter in the treatment of CSF leak after posterior spine surgery: A retrospective cohort study
- Comprehensive biomedicine assessment of Apteranthes tuberculata extracts: Phytochemical analysis and multifaceted pharmacological evaluation in animal models
- Relation of time in range to severity of coronary artery disease in patients with type 2 diabetes: A cross-sectional study
- Dopamine attenuates ethanol-induced neuronal apoptosis by stimulating electrical activity in the developing rat retina
- Correlation between albumin levels during the third trimester and the risk of postpartum levator ani muscle rupture
- Factors associated with maternal attention and distraction during breastfeeding and childcare: A cross-sectional study in the west of Iran
- Mechanisms of hesperetin in treating metabolic dysfunction-associated steatosis liver disease via network pharmacology and in vitro experiments
- The law on oncological oblivion in the Italian and European context: How to best uphold the cancer patients’ rights to privacy and self-determination?
- The prognostic value of the neutrophil-to-lymphocyte ratio, platelet-to-lymphocyte ratio, and prognostic nutritional index for survival in patients with colorectal cancer
- Factors affecting the measurements of peripheral oxygen saturation values in healthy young adults
- Comparison and correlations between findings of hysteroscopy and vaginal color Doppler ultrasonography for detection of uterine abnormalities in patients with recurrent implantation failure
- The effects of different types of RAGT on balance function in stroke patients with low levels of independent walking in a convalescent rehabilitation hospital
- Causal relationship between asthma and ankylosing spondylitis: A bidirectional two-sample univariable and multivariable Mendelian randomization study
- Correlations of health literacy with individuals’ understanding and use of medications in Southern Taiwan
- Correlation of serum calprotectin with outcome of acute cerebral infarction
- Comparison of computed tomography and guided bronchoscopy in the diagnosis of pulmonary nodules: A systematic review and meta-analysis
- Curdione protects vascular endothelial cells and atherosclerosis via the regulation of DNMT1-mediated ERBB4 promoter methylation
- The identification of novel missense variant in ChAT gene in a patient with gestational diabetes denotes plausible genetic association
- Molecular genotyping of multi-system rare blood types in foreign blood donors based on DNA sequencing and its clinical significance
- Exploring the role of succinyl carnitine in the association between CD39⁺ CD4⁺ T cell and ulcerative colitis: A Mendelian randomization study
- Dexmedetomidine suppresses microglial activation in postoperative cognitive dysfunction via the mmu-miRNA-125/TRAF6 signaling axis
- Analysis of serum metabolomics in patients with different types of chronic heart failure
- Diagnostic value of hematological parameters in the early diagnosis of acute cholecystitis
- Pachymaran alleviates fat accumulation, hepatocyte degeneration, and injury in mice with nonalcoholic fatty liver disease
- Decrease in CD4 and CD8 lymphocytes are predictors of severe clinical picture and unfavorable outcome of the disease in patients with COVID-19
- METTL3 blocked the progression of diabetic retinopathy through m6A-modified SOX2
- The predictive significance of anti-RO-52 antibody in patients with interstitial pneumonia after treatment of malignant tumors
- Exploring cerebrospinal fluid metabolites, cognitive function, and brain atrophy: Insights from Mendelian randomization
- Development and validation of potential molecular subtypes and signatures of ocular sarcoidosis based on autophagy-related gene analysis
- Widespread venous thrombosis: Unveiling a complex case of Behçet’s disease with a literature perspective
- Uterine fibroid embolization: An analysis of clinical outcomes and impact on patients’ quality of life
- Discovery of lipid metabolism-related diagnostic biomarkers and construction of diagnostic model in steroid-induced osteonecrosis of femoral head
- Serum-derived exomiR-188-3p is a promising novel biomarker for early-stage ovarian cancer
- Enhancing chronic back pain management: A comparative study of ultrasound–MRI fusion guidance for paravertebral nerve block
- Peptide CCAT1-70aa promotes hepatocellular carcinoma proliferation and invasion via the MAPK/ERK pathway
- Electroacupuncture-induced reduction of myocardial ischemia–reperfusion injury via FTO-dependent m6A methylation modulation
- Hemorrhoids and cardiovascular disease: A bidirectional Mendelian randomization study
- Cell-free adipose extract inhibits hypertrophic scar formation through collagen remodeling and antiangiogenesis
- HALP score in Demodex blepharitis: A case–control study
- Assessment of SOX2 performance as a marker for circulating cancer stem-like cells (CCSCs) identification in advanced breast cancer patients using CytoTrack system
- Risk and prognosis for brain metastasis in primary metastatic cervical cancer patients: A population-based study
- Comparison of the two intestinal anastomosis methods in pediatric patients
- Factors influencing hematological toxicity and adverse effects of perioperative hyperthermic intraperitoneal vs intraperitoneal chemotherapy in gastrointestinal cancer
- Endotoxin tolerance inhibits NLRP3 inflammasome activation in macrophages of septic mice by restoring autophagic flux through TRIM26
- Lateral transperitoneal laparoscopic adrenalectomy: A single-centre experience of 21 procedures
- Petunidin attenuates lipopolysaccharide-induced retinal microglia inflammatory response in diabetic retinopathy by targeting OGT/NF-κB/LCN2 axis
- Procalcitonin and C-reactive protein as biomarkers for diagnosing and assessing the severity of acute cholecystitis
- Factors determining the number of sessions in successful extracorporeal shock wave lithotripsy patients
- Development of a nomogram for predicting cancer-specific survival in patients with renal pelvic cancer following surgery
- Inhibition of ATG7 promotes orthodontic tooth movement by regulating the RANKL/OPG ratio under compression force
- A machine learning-based prognostic model integrating mRNA stemness index, hypoxia, and glycolysis‑related biomarkers for colorectal cancer
- Glutathione attenuates sepsis-associated encephalopathy via dual modulation of NF-κB and PKA/CREB pathways
- FAHD1 prevents neuronal ferroptosis by modulating R-loop and the cGAS–STING pathway
- Association of placenta weight and morphology with term low birth weight: A case–control study
- Investigation of the pathogenic variants induced Sjogren’s syndrome in Turkish population
- Nucleotide metabolic abnormalities in post-COVID-19 condition and type 2 diabetes mellitus patients and their association with endocrine dysfunction
- TGF-β–Smad2/3 signaling in high-altitude pulmonary hypertension in rats: Role and mechanisms via macrophage M2 polarization
- Ultrasound-guided unilateral versus bilateral erector spinae plane block for postoperative analgesia of patients undergoing laparoscopic cholecystectomy
- Profiling gut microbiome dynamics in subacute thyroiditis: Implications for pathogenesis, diagnosis, and treatment
- Delta neutrophil index, CRP/albumin ratio, procalcitonin, immature granulocytes, and HALP score in acute appendicitis: Best performing biomarker?
- Anticancer activity mechanism of novelly synthesized and characterized benzofuran ring-linked 3-nitrophenyl chalcone derivative on colon cancer cells
- H2valdien3 arrests the cell cycle and induces apoptosis of gastric cancer
- Prognostic relevance of PRSS2 and its immune correlates in papillary thyroid carcinoma
- Association of SGLT2 inhibition with psychiatric disorders: A Mendelian randomization study
- Motivational interviewing for alcohol use reduction in Thai patients
- Luteolin alleviates oxygen-glucose deprivation/reoxygenation-induced neuron injury by regulating NLRP3/IL-1β signaling
- Polyphyllin II inhibits thyroid cancer cell growth by simultaneously inhibiting glycolysis and oxidative phosphorylation
- Relationship between the expression of copper death promoting factor SLC31A1 in papillary thyroid carcinoma and clinicopathological indicators and prognosis
- CSF2 polarized neutrophils and invaded renal cancer cells in vitro influence
- Proton pump inhibitors-induced thrombocytopenia: A systematic literature analysis of case reports
- The current status and influence factors of research ability among community nurses: A sequential qualitative–quantitative study
- OKAIN: A comprehensive oncology knowledge base for the interpretation of clinically actionable alterations
- The relationship between serum CA50, CA242, and SAA levels and clinical pathological characteristics and prognosis in patients with pancreatic cancer
- Identification and external validation of a prognostic signature based on hypoxia–glycolysis-related genes for kidney renal clear cell carcinoma
- Engineered RBC-derived nanovesicles functionalized with tumor-targeting ligands: A comparative study on breast cancer targeting efficiency and biocompatibility
- Relationship of resting echocardiography combined with serum micronutrients to the severity of low-gradient severe aortic stenosis
- Effect of vibration on pain during subcutaneous heparin injection: A randomized, single-blind, placebo-controlled trial
- The diagnostic performance of machine learning-based FFRCT for coronary artery disease: A meta-analysis
- Comparing biofeedback device vs diaphragmatic breathing for bloating relief: A randomized controlled trial
- Serum uric acid to albumin ratio and C-reactive protein as predictive biomarkers for chronic total occlusion and coronary collateral circulation quality
- Multiple organ scoring systems for predicting in-hospital mortality of sepsis patients in the intensive care unit
- Single-cell RNA sequencing data analysis of the inner ear in gentamicin-treated mice via intraperitoneal injection
- Suppression of cathepsin B attenuates myocardial injury via limiting cardiomyocyte apoptosis
- Influence of sevoflurane combined with propofol anesthesia on the anesthesia effect and adverse reactions in children with acute appendicitis
- Identification of hub genes related to acute kidney injury caused by sevoflurane anesthesia and endoplasmic reticulum stress
- Efficacy and safety of PD-1/PD-L1 inhibitors in pancreatic ductal adenocarcinoma: a systematic review and Meta-analysis of randomized controlled trials
- The value of diagnostic experience in O-RADS MRI score for ovarian-adnexal lesions
- Health education pathway for individuals with temporary enterostomies using patient journey mapping
- Serum TLR8 as a potential diagnostic biomarker of coronary heart disease
- Intraoperative temperature management and its effect on surgical outcomes in elderly patients undergoing lichtenstein unilateral inguinal hernia repair
- Immunohistochemical profiling and neuroepithelial heterogeneity in immature ovarian teratomas: a retrospective digital pathology-based study
- Associated risk factors and prevalence of human papillomavirus infection among females visiting tertiary care hospital: a cross-sectional study from Nepal
- Comparative evaluation of various disc elution methods for the detection of colistin-resistant gram-negative bacteria
- Effect of timing of cholecystectomy on weight loss after sleeve gastrectomy in morbidly obese individuals with cholelithiasis: a retrospective cohort study
- Causal association between ceramide levels and central precocious puberty: a mendelian randomization study
- Novel predictive model for colorectal liver metastases recurrence: a radiomics and clinical data approach
- Relationship between resident physicians’ perceived professional value and exposure to violence
- Multiple sclerosis and type 1 diabetes: a Mendelian randomization study of European ancestry
- Rapid pathogen identification in peritoneal dialysis effluent by MALDI-TOF MS following blood culture enrichment
- Comparison of open and percutaneous A1 pulley release in pediatric trigger thumb: a retrospective cohort study
- Impact of combined diaphragm-lung ultrasound assessment on postoperative respiratory function in patients under general anesthesia recovery
- Development and internal validation of a nomogram for predicting short-term prognosis in ICU patients with acute pyelonephritis
- The association between hypoxic burden and blood pressure in patients with obstructive sleep apnea
- Promotion of asthenozoospermia by C9orf72 through suppression of spermatogonia activity via fructose metabolism and mitophagy
- Review Articles
- The effects of enhanced external counter-pulsation on post-acute sequelae of COVID-19: A narrative review
- Diabetes-related cognitive impairment: Mechanisms, symptoms, and treatments
- Microscopic changes and gross morphology of placenta in women affected by gestational diabetes mellitus in dietary treatment: A systematic review
- Review of mechanisms and frontier applications in IL-17A-induced hypertension
- Research progress on the correlation between islet amyloid peptides and type 2 diabetes mellitus
- The safety and efficacy of BCG combined with mitomycin C compared with BCG monotherapy in patients with non-muscle-invasive bladder cancer: A systematic review and meta-analysis
- The application of augmented reality in robotic general surgery: A mini-review
- The effect of Greek mountain tea extract and wheat germ extract on peripheral blood flow and eicosanoid metabolism in mammals
- Neurogasobiology of migraine: Carbon monoxide, hydrogen sulfide, and nitric oxide as emerging pathophysiological trinacrium relevant to nociception regulation
- Plant polyphenols, terpenes, and terpenoids in oral health
- Laboratory medicine between technological innovation, rights safeguarding, and patient safety: A bioethical perspective
- End-of-life in cancer patients: Medicolegal implications and ethical challenges in Europe
- The maternal factors during pregnancy for intrauterine growth retardation: An umbrella review
- Intra-abdominal hypertension/abdominal compartment syndrome of pediatric patients in critical care settings
- PI3K/Akt pathway and neuroinflammation in sepsis-associated encephalopathy
- Screening of Group B Streptococcus in pregnancy: A systematic review for the laboratory detection
- Giant borderline ovarian tumours – review of the literature
- Leveraging artificial intelligence for collaborative care planning: Innovations and impacts in shared decision-making – A systematic review
- Cholera epidemiology analysis through the experience of the 1973 Naples epidemic
- Risk factors of frailty/sarcopenia in community older adults: Meta-analysis
- Supplement strategies for infertility in overweight women: Evidence and legal insights
- Scurvy, a not obsolete disorder: Clinical report in eight young children and literature review
- A meta-analysis of the effects of DBS on cognitive function in patients with advanced PD
- Protective role of selenium in sepsis: Mechanisms and potential therapeutic strategies
- Strategies for hyperkalemia management in dialysis patients: A systematic review
- C-reactive protein-to-albumin ratio in peripheral artery disease
- Research progress on autophagy and its roles in sepsis induced organ injury
- Neuronutrition in autism spectrum disorders
- Pumilio 2 in neural development, function, and specific neurological disorders
- Antibiotic prescribing patterns in general dental practice- a scoping review
- Clinical and medico-legal reflections on non-invasive prenatal testing
- Smartphone use and back pain: a narrative review of postural pathologies
- Targeting endothelial oxidative stress in hypertension
- Exploring links between acne and metabolic syndrome: a narrative review
- Case Reports
- Delayed graft function after renal transplantation
- Semaglutide treatment for type 2 diabetes in a patient with chronic myeloid leukemia: A case report and review of the literature
- Diverse electrophysiological demyelinating features in a late-onset glycogen storage disease type IIIa case
- Giant right atrial hemangioma presenting with ascites: A case report
- Laser excision of a large granular cell tumor of the vocal cord with subglottic extension: A case report
- EsoFLIP-assisted dilation for dysphagia in systemic sclerosis: Highlighting the role of multimodal esophageal evaluation
- Molecular hydrogen-rhodiola as an adjuvant therapy for ischemic stroke in internal carotid artery occlusion: A case report
- Coronary artery anomalies: A case of the “malignant” left coronary artery and its surgical management
- Combined VAT and retroperitoneoscopy for pleural empyema due to nephro-pleuric fistula in xanthogranulomatous pyelonephritis
- A rare case of Opalski syndrome with a suspected multiple sclerosis etiology
- Newly diagnosed B-cell acute lymphoblastic leukemia demonstrating localized bone marrow infiltration exclusively in the lower extremities
- Rapid Communication
- Biological properties of valve materials using RGD and EC
-
A single oral administration of flavanols enhances short
-term memory in mice along with increased brain-derived neurotrophic factor - Repeat influenza incidence across two consecutive influenza seasons
- Letter to the Editor
- Role of enhanced external counterpulsation in long COVID
- Expression of Concern
- Expression of concern “A ceRNA network mediated by LINC00475 in papillary thyroid carcinoma”
- Expression of concern “Notoginsenoside R1 alleviates spinal cord injury through the miR-301a/KLF7 axis to activate Wnt/β-catenin pathway”
- Expression of concern “circ_0020123 promotes cell proliferation and migration in lung adenocarcinoma via PDZD8”
- Corrigendum
- Corrigendum to “Empagliflozin improves aortic injury in obese mice by regulating fatty acid metabolism”
- Corrigendum to “Comparing the therapeutic efficacy of endoscopic minimally invasive surgery and traditional surgery for early-stage breast cancer: A meta-analysis”
- Corrigendum to “The progress of autoimmune hepatitis research and future challenges”
- Retraction
- Retraction of “miR-654-5p promotes gastric cancer progression via the GPRIN1/NF-κB pathway”
- Retraction of: “LncRNA CASC15 inhibition relieves renal fibrosis in diabetic nephropathy through downregulating SP-A by sponging to miR-424”
- Retraction of: “SCARA5 inhibits oral squamous cell carcinoma via inactivating the STAT3 and PI3K/AKT signaling pathways”
- Special Issue Advancements in oncology: bridging clinical and experimental research - Part II
- Unveiling novel biomarkers for platinum chemoresistance in ovarian cancer
- Lathyrol affects the expression of AR and PSA and inhibits the malignant behavior of RCC cells
- The era of increasing cancer survivorship: Trends in fertility preservation, medico-legal implications, and ethical challenges
- Bone scintigraphy and positron emission tomography in the early diagnosis of MRONJ
- Meta-analysis of clinical efficacy and safety of immunotherapy combined with chemotherapy in non-small cell lung cancer
- Special Issue Computational Intelligence Methodologies Meets Recurrent Cancers - Part IV
- Exploration of mRNA-modifying METTL3 oncogene as momentous prognostic biomarker responsible for colorectal cancer development
- Special Issue The evolving saga of RNAs from bench to bedside - Part III
- Interaction and verification of ferroptosis-related RNAs Rela and Stat3 in promoting sepsis-associated acute kidney injury
- The mRNA MOXD1: Link to oxidative stress and prognostic significance in gastric cancer
- Special Issue Exploring the biological mechanism of human diseases based on MultiOmics Technology - Part II
- Dynamic changes in lactate-related genes in microglia and their role in immune cell interactions after ischemic stroke
- A prognostic model correlated with fatty acid metabolism in Ewing’s sarcoma based on bioinformatics analysis
- Red cell distribution width predicts early kidney injury: A NHANES cross-sectional study
- Special Issue Diabetes mellitus: pathophysiology, complications & treatment
- Nutritional risk assessment and nutritional support in children with congenital diabetes during surgery
- Correlation of the differential expressions of RANK, RANKL, and OPG with obesity in the elderly population in Xinjiang
- A discussion on the application of fluorescence micro-optical sectioning tomography in the research of cognitive dysfunction in diabetes
- A review of brain research on T2DM-related cognitive dysfunction
- Metformin and estrogen modulation in LABC with T2DM: A 36-month randomized trial
- Special Issue Innovative Biomarker Discovery and Precision Medicine in Cancer Diagnostics
- CircASH1L-mediated tumor progression in triple-negative breast cancer: PI3K/AKT pathway mechanisms

