Abstract
Objective
This study examines the efficacy of ultrasound (US)-guided paravertebral nerve block (PVB) with and without MRI fusion for chronic back pain management.
Methods
A retrospective analysis of 20 patients, split into US–MRI fusion-guided (IF group, n = 10) and traditional US-guided (U group, n = 10) PVB, was conducted. Pain intensity, gabapentin dosage, procedure duration, and treatment efficacy were compared using numerical rating scale (NRS) scores.
Results
An hour after receiving treatment, the IF group showed a marked reduction in NRS scores (2.2 ± 0.9), significantly lower than those observed in the U group (2.5 ± 1.0; p < 0.05). Nonetheless, the difference in average NRS scores between the groups was not statistically significant 7 days post-treatment (IF group, 3.5 ± 0.8; U group, 3.4 ± 1.3; p > 0.05). The U group reported four instances of transient dizziness and diminished limb muscle strength, lasting between 30 and 90 min, which naturally resolved without intervention. No significant adverse effects were noted in the IF group.
Conclusions
Integrating US with MRI for PVB guidance emerges as a groundbreaking and efficacious strategy in chronic back pain treatment, showcasing significant improvements in safety and initial pain alleviation compared to the conventional use of US guidance alone.
1 Introduction
Chronic pain, persisting for over 3 months, significantly diminishes the quality of life for sufferers [1]. The technique of paravertebral nerve block (PVB) guided by ultrasound (US) is a prevalent approach for managing chronic pain, offering prompt pain relief and notable improvement in functional impairments [2]. Nonetheless, this method encounters several obstacles. US imagery is prone to creating shadows over calcified tissues, leading to potential signal disruptions to bone structures [3]. Moreover, in cases involving obese individuals or patients with localized swelling, US’s ability to provide clear imagery is compromised, hindering accurate intraoperative distinction [4]. The advent of US image fusion navigation technology, which facilitates the merging of various images for real-time guidance, enhances contrast and leverages the strengths of different imaging modalities to elevate the precision, efficiency, and safety of both diagnostic and therapeutic procedures. Magnetic resonance imaging (MRI) boasts superior capabilities in delineating spatial and soft tissue contrasts, including fat, muscle, and fascia, without the drawbacks of bone artifact interference, thus offering a more accurate depiction of lesions and adjacent normal anatomical features [5]. Image fusion technology has found extensive applications in diverse medical fields such as tumor physical therapy, stereotactic radiosurgery, image-guided navigation systems, and picture archiving and communication systems. Yet, the integration of US-MRI fusion for directing PVB in chronic pain management remains unexplored.
In light of this, our study introduces and examines the US-MRI fusion-guided PVB technique as a novel intervention for chronic pain treatment. We assessed its feasibility, efficacy, and safety by comparing therapeutic outcomes, adverse reaction rates, and procedural times against those observed with traditional US-guided PVB.
2 Methods
2.1 Participants and setting
This study received the endorsement of the hospital’s ethics committee, and prior to their inclusion, all participants consented in writing, ensuring their full awareness and agreement to partake. We strictly adhered to confidentiality protocols, safeguarding patient privacy and anonymizing identifiable information throughout the research process.
The investigation incorporated 20 patients who received treatment at the Southwest Hospital of Army Medical University (Third Military Medical University), China, between May 2019 and January 2020, selected based on predefined eligibility criteria. The inclusion parameters were as follows: (1) individuals aged between 20 and 75; (2) patients with a confirmed diagnosis of chronic pain who had not achieved adequate pain relief from standard medical treatments and were candidates for PVB therapy; (3) a numerical rating scale (NRS) score of 6 or higher; and (4) the completion of computed tomography (CT) and MRI prior to the nerve block procedure. The exclusion criteria encompassed (1) significant cardiac, pulmonary, or renal impairments; (2) diabetics with uncontrolled blood sugar levels (fasting glucose > 8 mmol/L, 2 h postprandial glucose > 10 mmol/L); (3) infection at the puncture site or a systemic infection; (4) coagulopathy; (5) any contraindication to nerve block procedures; and (6) contraindications to undergoing MRI scans.
2.2 Method of grouping
In this study, 20 patients fulfilling the inclusion criteria were initially considered. To minimize potential biases and confounders, propensity score matching (PSM) was employed to ensure comparability between the experimental (Imaging Fusion; IF) and control (US; U) groups [6,7]. A logistic regression model was used to generate a propensity score for each participant, incorporating the following covariates: gender, age, duration of disease, initial NRS scores, body mass index (BMI), disease type (lumbar disc herniation, radiculopathy, postherpetic neuralgia), and other relevant clinical characteristics.
Patients were matched with the IF group on a one-to-one basis using nearest-neighbor matching with a caliper width of 0.05 standard deviation. After matching, the balance of covariates between the groups was assessed using standardized mean difference (SMD), with SMD <0.1 indicating good balance. As a result, ten patients were successfully matched to form the control group (US; U), maintaining identical compositions in terms of gender and disease type.
2.3 Procedures
2.3.1 US-guided PVB
In the control group (US; U), the US was utilized to identify the nerve root, the nerve root artery, and adjacent vessels close to the nerve root’s edge, facilitating the planning of the injection path based on the anatomical structures surrounding the target area. A 50 mm, 23-gauge needle was then carefully inserted from the posterior aspect, with the needle’s tip positioned on the dorsal side of the nerve. This approach was meticulously designed to prevent potential harm to the nearby artery and to maintain a safe distance from the radicular artery. Following precise location verification, a compounded medicinal concoction was administered. This solution comprised 100 mg of lidocaine hydrochloride (2%, produced by Southwest Pharmaceutical), 50 mg of ropivacaine hydrochloride (1%, Naropin®, AstraZeneca), and 20 mg of triamcinolone acetonide (40 mg/mL, Transton®, Kunming JIDA), all diluted into a 15 mL mixture with 0.9% saline [8].
A total of 6 mL of this blended medicinal mixture was injected into each targeted nerve root. The success of the needle placement was judged by the spread and diffusion of the drug solution around the nerve root, serving as a guide for accurate puncturing. Throughout the injection, the spread of the solution was dynamically monitored, allowing for real-time adjustments to the needle’s position to ensure optimal delivery.
2.3.2 MRI scanning scheme
Utilizing a Siemens Trio 3.0 Tesla scanner, the examination of the lumbosacral vertebrae spanned from the upper margin of the L1 vertebra down to the lower boundary of S5, employing both the basic and body coils for scanning. Subsequent to this, coronal views of the lumbosacral nerves were captured utilizing a 3D-SPACE (Sampling Perfection with Application optimized Contrasts using different flip angle Evolutions) sequence. This sequence was strategically positioned based on sagittal scans, extending from the frontal edge of the vertebral body to the spinous processes of the lumbar spine. The 3D-SPACE sequence was characterized by specific technical parameters, including a field of view (FOV) of 420 mm × 420 mm, a matrix size of 184 × 184, a repetition time (TR) of 3,800 ms, an echo time (TE) of 293 ms, an inversion time (TI) of 170 ms, a slice thickness of 1.0 mm with no interval between slices, employing a single slab with a total of 80 slices, a number of signal averages (NSA) set to 2, the phase encoding direction being right to left (RL), and a signal-to-noise ratio (SNR) fixed at 1.00. The acquired 3D imaging data were then processed on a local post-processing workstation, enabling enhancements through maximum intensity projection (MIP) and multi-planar reconstruction (MPR) techniques.
2.3.3 US-MRI fusion-guided PVB
In the Imaging Fusion (IF) group, the process began with acquiring preoperative MRI scans, which were then integrated into the control unit of a multi-image fusion interventional navigation system. The procedural steps were as follows:
High-resolution MRI scans were conducted using a 3.0T MRI system (MAGNETOM Skyra 3.0T, Siemens, Amberg, Germany), with scanning parameters tailored to the specific characteristics of the target tissues, resulting in 1.5 mm-thick MRI slices.
The MRI data, formatted in DICOM (Digital Imaging and Communications in Medicine), were uploaded to the core system of a multi-image fusion interventional navigation device (Mindray, model RE7, China).
The connection of the magnetic transmitter facilitated the activation of the image fusion mode. Image registration was achieved by aligning the MRI images with the ultrasonic probe’s imagery and the adjustable screen, utilizing surface markers, bone landmarks, nerves, and other anatomical features as references for accurate matching (Figure 1).
The intended therapeutic target was pinpointed on the MRI images, guiding the formulation of a puncture trajectory based on the anatomical structures adjacent to the target (Figure 2).
Following the predetermined puncture path, the insertion was performed under US guidance, with the needle directed towards the target, aided by a puncture stand for precision.
Once the needle was accurately positioned, ensuring no blood, fluid, or gas was aspirated, the therapeutic medication was administered. The spread of the therapeutic agent was monitored in real-time via US, observing its diffusion around the target area (Figure 3).
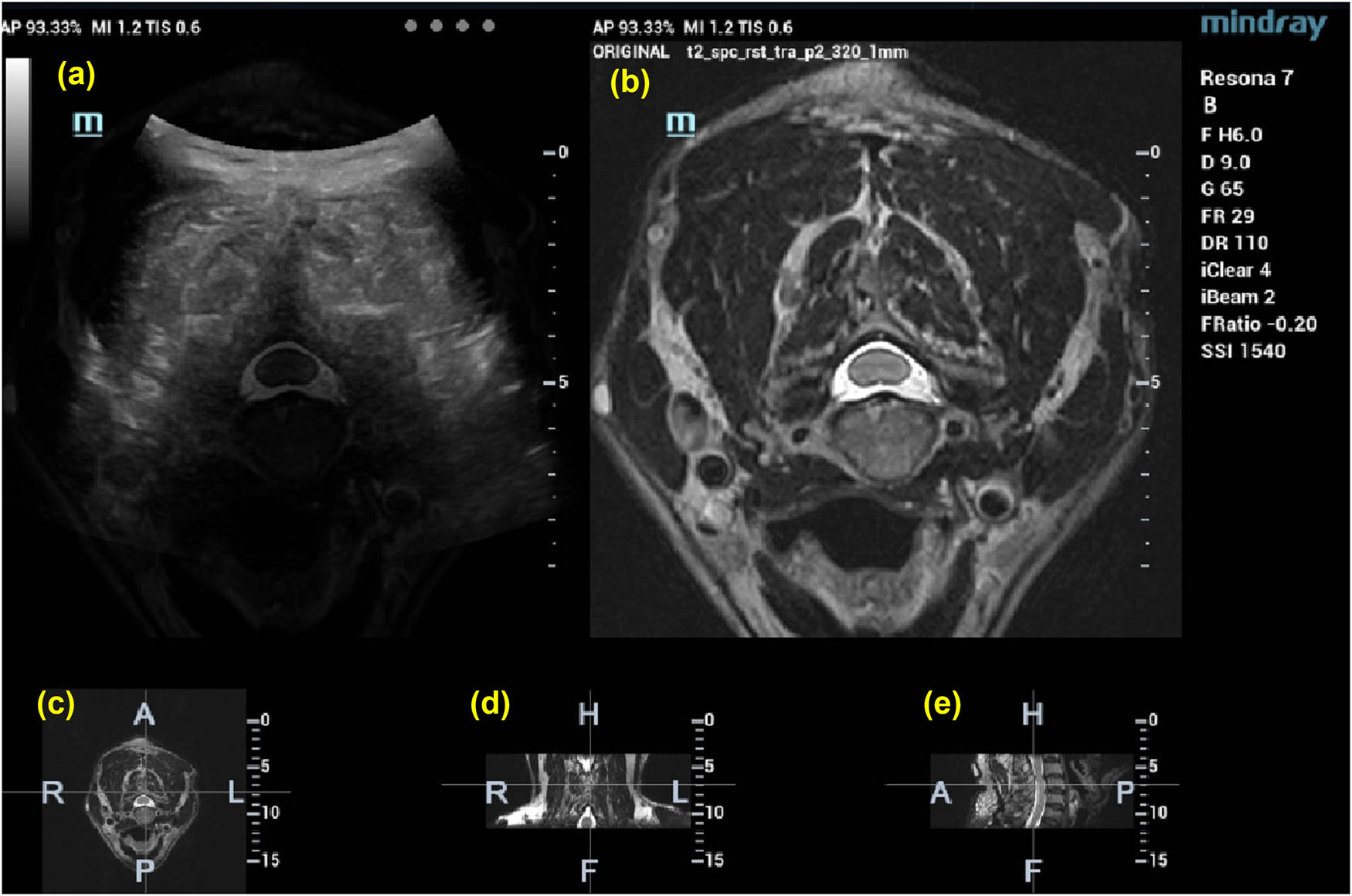
Images of cervical vertebrae after US-MRI fusion: (a) US-MRI fusion images, (b) MRI images, (c) cross section, (d) coronal section, and (e) sagittal section.
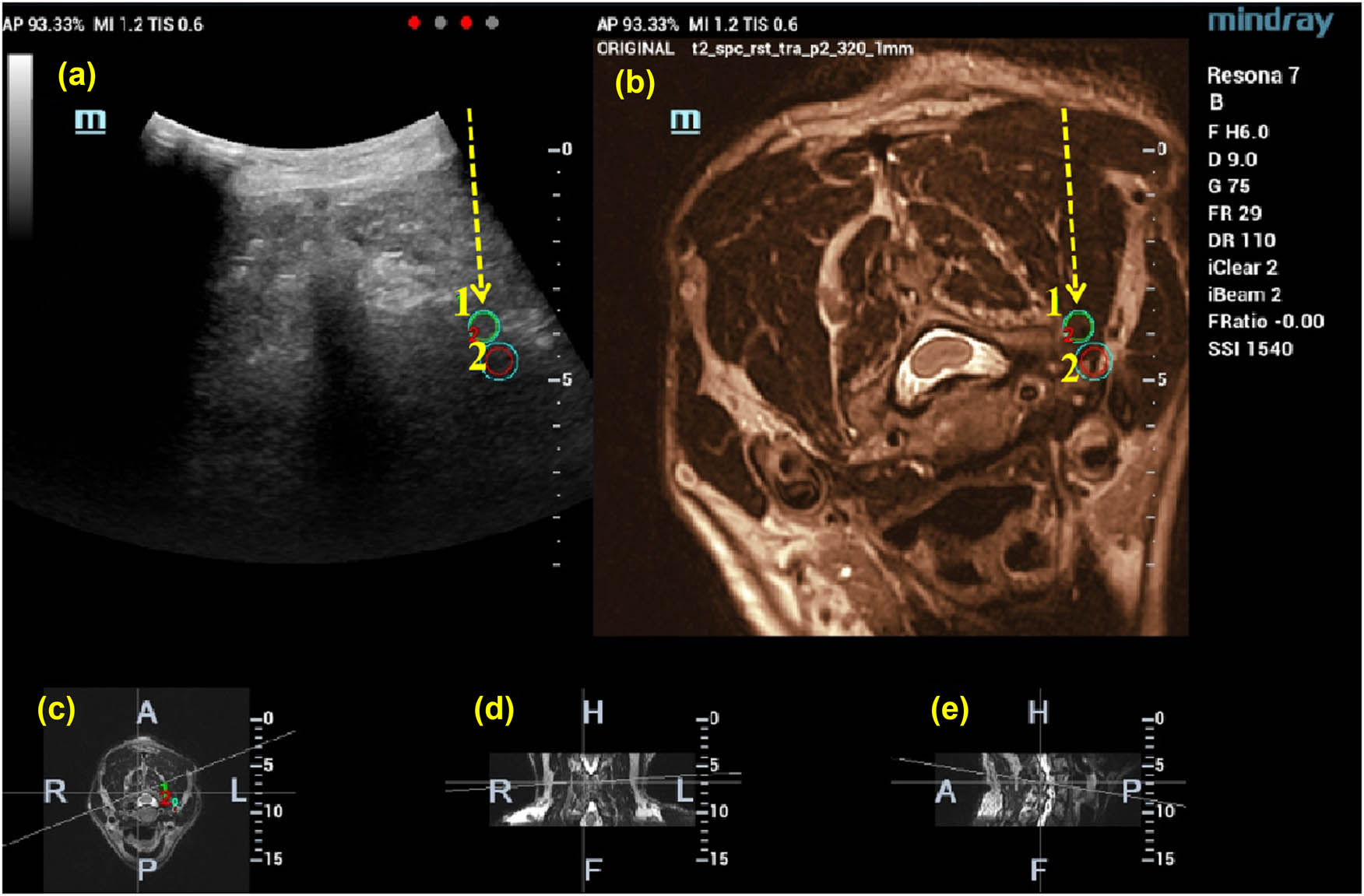
The therapeutic target is marked on the MRI image, and the location of the target is also displayed on the fused image at the same time (1, 2). Then, the puncture path is designed according to the MRI and US images (shown by the yellow arrow). (a) US-MRI fusion images, with green circles indicating the target puncture points, (b)MRI images, (c) cross section, (d) coronal section, and (e) sagittal section.
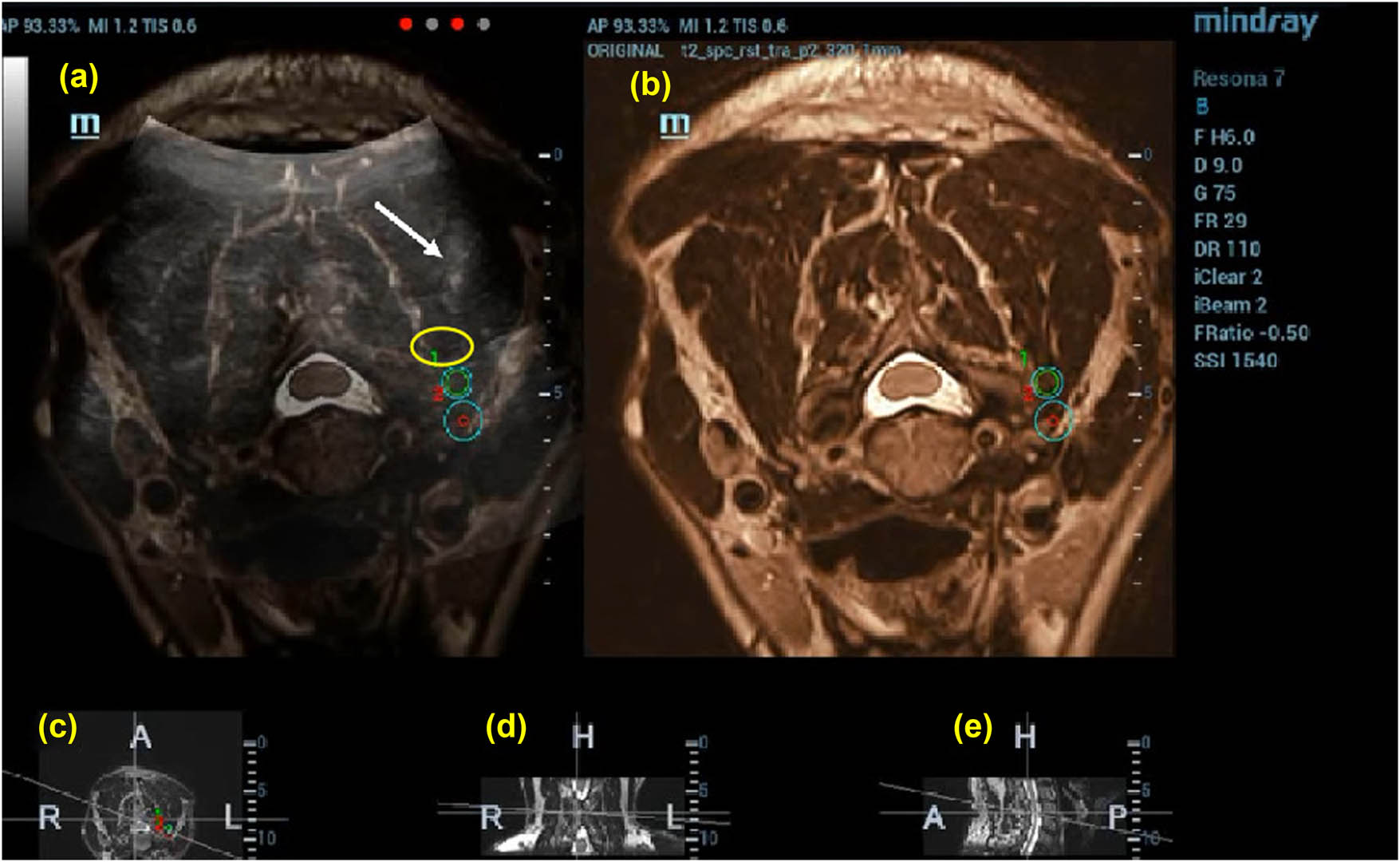
Puncture to preset target 1 guided by US (50%)-MRI (50%) image. The drug solution is injected after the puncture is guided by US (50%)-nuclear magnetic resonance (50%) image; the white arrow indicates the location of the puncture needle and the yellow circle indicates the solutions diffusion range. (a) US-MRI fusion images, with green circles indicating the target puncture points, (b)MRI images, (c) cross section, (d) coronal section, and (e) sagittal section.
2.3.4 Demographic and clinical characteristics
Baseline demographic and clinical characteristics were collected, including age, sex, disease categories, site of pain, and disease course.
2.4 Measures
2.4.1 Pain intensity
The degree of pain was quantified using the NRS, where patients rated the most intense pain experienced within the 24 h preceding the evaluation. Pain levels were divided into four categories: no pain (0), mild pain (1–3), moderate pain (4–6), and severe pain (≥7) [9].
2.4.2 Treatment effect
The effectiveness of the pain management strategy was determined by the NRS Weighted Value (NRS-WV), with outcomes categorized into four levels: cured (NRS-WV ≥ 75%), significant improvement (50% ≤ NRS-WV < 75%), improved (25% ≤ NRS-WV < 50%), and no effect (NRS-WV < 25%).
2.4.3 Operation time
The duration of the procedure was meticulously recorded, encompassing the time taken for target localization, the search for the target point via US, and the administration of the drug.
2.4.4 Average daily dose of gabapentin
The mean daily dosage of gabapentin was calculated for the week preceding and following the treatment, providing insights into the medication usage patterns.
2.5 Statistical analysis
Preliminary studies investigating the impact of US-guided paravertebral block (US-guided PVB) on NRS pain scores in patients with chronic pain demonstrated a median reduction of 4.6 points. Based on these findings, a cohort of 20 patients was determined to be sufficient to achieve 90% statistical power to detect a significant difference in pain scores pre- and post-treatment, utilizing a two-sided significance level of 0.05 and assuming a standard deviation (SD) of 2 in pain scores. Additionally, a power analysis conducted using PASS 15 software, focusing on the operation time data presented in Table 4, indicated that the current study possesses a statistical power of 100%. Consequently, the selected sample size is adequate to identify significant differences with high confidence, ensuring the validity and robustness of our findings. Experimental data are expressed as mean ± standard deviation (mean ± SD). To evaluate the significance of differences in post-treatment pain scores, efficacy rates of pain treatment, operation durations, and average daily doses of gabapentin between the two study groups, independent samples t-tests were employed. Following PSM, covariate balance between groups was assessed using the SMD of <0.1 considered indicative of negligible differences and effective matching. A P-value < 0.05 was regarded as statistically significant.
3 Results
3.1 Baseline data
The initial demographic and clinical profiles of participants are detailed in Table 1. Prior to treatment initiation, there was no significant disparity in the duration of the illness (4.3 ± 2.8 weeks for the US [U] group vs 4.4 ± 2.8 weeks for the Imaging Fusion [IF] group) or in the average NRS pain scores (7.1 ± 0.9 for the U group vs 7.0 ± 1.0 for the IF group), establishing a comparable baseline between the two cohorts (p > 0.05 for both indicators).
Baseline data after PSM
| Group | Sex (male/female) | Age (yr) | Disease course (week) | NRS | BMI (kg/m²) | Disease type | SMD |
|---|---|---|---|---|---|---|---|
| U (n = 10) | 6/4 | 46.8 ± 16.5 | 4.3 ± 2.8 | 7.1 ± 0.9 | 24.5 ± 3.2 | Lumbar disc herniation (4), radiculopathy (3), and postherpetic neuralgia (3) | 0.05 |
| IF (n = 10) | 6/4 | 46.6 ± 12.69 | 4.4 ± 2.8 | 7.0 ± 1.0 | 24.7 ± 3.1 | Lumbar disc herniation (4), radiculopathy (3), and postherpetic neuralgia (3) | 0.04 |
Values are presented as mean ± standard deviation. U group: control group; IF group: experimental group; NRS: numerical rating scale for pain intensity; BMI: body mass index; and SMD: standardized mean difference.
3.2 NRS scores
When comparing NRS pain scores post-treatment, the IF group demonstrated a notably lower average score (2.2 ± 0.9) 1 h after treatment compared to the U group (2.5 ± 1.0; p < 0.05) as presented in Table 2. However, there was no significant difference in the average NRS scores 7 days post-treatment between the groups (3.5 ± 0.8 for the IF group vs 3.4 ± 1.3 for the U group; p > 0.05), indicating a convergence in pain relief outcomes over time.
Comparison of NRS 1 h and 7 days after treatment
| Group | 1 h NRS | 7 days NRS |
|---|---|---|
| U | 2.5 ± 1.0* | 3.5 ± 0.8 |
| IF | 2.2 ± 0.9* | 3.4 ± 1.3 |
Values are mean ± SD, U group, IF group, numerical rating scale (NRS), *p < 0.05: comparison of U and IF groups.
3.3 Total effective rate of pain treatment
The comparison of the average NRS weighted value (NRS-WV) revealed no significant difference between the groups either 1 h (0.64 ± 0.16 for the U group vs 0.68 ± 0.14 for the IF group) or 7 days after treatment (0.51 ± 0.10 for the U group vs 0.50 ± 0.19 for the IF group; p > 0.05 for both), as shown in Table 3.
Comparison of NRS-WV
| Group | 1 h NRS-WV | 7 days NRS-WV |
|---|---|---|
| U | 0.6373 ± 0.1646 | 0.50616 ± 0.1036 |
| IF | 0.6778 ± 0.1445 | 0.50219 ± 0.1902 |
Values are mean ± SD, U group, IF group, numerical rating scale weighted value (NRS-WV).
3.4 Operation time
Operation durations, summarized in Table 4, showed a significant difference; the U group experienced a considerably shorter procedure time (754 ± 89.05 s) compared to the IF group (1516 ± 134.39 s; p < 0.05), highlighting the time efficiency of using US guidance alone.
Comparison of operation time
| Group | Operation time (s) |
|---|---|
| U | 754 ± 89.05145* |
| IF | 1516 ± 134.3859* |
Values are mean ± SD, control group (U group), experimental group (IF group), *p < 0.05: comparison of U and IF groups.
3.5 Average daily dosage of gabapentin
Table 5 outlines the gabapentin dosages before and after treatment. The 7-day pre-treatment average daily dosages were similar between the U group (1.38 ± 0.20) and the IF group (1.41 ± 0.23). Post-treatment, there was no significant difference in dosage changes between the groups (0.99 ± 0.41 for the U group vs 0.96 ± 0.67 for the IF group; all p > 0.05), indicating comparable medication adjustments.
Comparison of average daily dosage of gabapentin
| Group | Average daily dose of gabapentin within 7 days before treatment (g) | Average daily dose of gabapentin within 7 days after treatment (g) |
|---|---|---|
| U | 1.38 ± 0.1990 | 0.99 ± 0.4069 |
| IF | 1.41 ± 0.2343 | 0.96 ± 0.6681 |
Values are mean ± SD, control group (U group), and experimental group (IF group).
3.6 Incidence of adverse events
Post-treatment, four patients in the U group experienced transient symptoms of dizziness and decreased limb muscle strength, lasting between 30 and 90 min, which resolved spontaneously. The IF group reported no significant adverse effects, underscoring a potential advantage in safety with the use of imaging fusion guidance.
4 Discussion
PVB is heralded as a principal therapeutic approach for managing chronic pain [10]. US-guided PVB has been extensively validated in preceding research and stands on par with CT-guided techniques in terms of efficacy [11,12,13,14]. This method offers the advantage of continuous, real-time procedural guidance devoid of the risks associated with radiation exposure.
Nevertheless, the application of US guidance is not without its challenges. As highlighted by Chumnanvej et al., the technique’s visual field is significantly restricted due to the high acoustic impedance presented by bone, rendering US less effective for clear delineation of spinal anatomy in the lumbar area [15]. Consequently, certain minimally invasive pain management interventions cannot rely solely on US guidance and necessitate the adjunctive use of digital subtraction angiography or CT for comprehensive guidance. Furthermore, the aging process affects the echo intensity of muscle tissue under US, markedly increasing the whiteness and brightness of US images in older patients, thereby impairing tissue differentiation [16,17]. The calcification associated with aged, degenerated discs further complicates their distinction from bone via US [12]. Additionally, the presence of adipose tissue can diminish the clarity of US images, affecting both the precision and success rate of interventions and potentially leading to adverse outcomes [18]. These limitations underscore the “bottleneck” encountered in the advancement of pure US guidance technology, signaling a pressing need for innovative solutions to enhance its utility in clinical practice.
The utilization of MRI for the diagnosis and guidance in treating soft tissue and spinal bony lesions has been established as a feasible, effective, and safe method [19,20]. Key benefits of MRI include the absence of ionizing radiation, its capacity for high tissue contrast, and the flexibility of acquiring images in multiple planes [21]. Research conducted by Sequeiros et al. and Himes et al. has demonstrated the successful application of MRI guidance in treating spinal lesions, yielding promising outcomes [22,23]. However, reliance solely on MRI guidance introduces certain limitations, notably extending the duration of procedures due to the necessity for specialized puncture needles and the inability to provide real-time and dynamic guidance during interventions. Additionally, the bulky nature of MRI equipment and the complexity of its operation necessitate dedicated spaces and specialized technicians, significantly constraining the broader adoption of this technology.
In this forward-looking study, we scrutinized the disparities in both efficacy and safety of PVB when guided by US-MRI fusion versus traditional US guidance alone. The data revealed that the NRS scores for both groups significantly decreased 1 h and 7 days after treatment compared to pre-treatment scores. Notably, the NRS scores for patients who underwent PVB with US-MRI fusion guidance were significantly lower than those for patients receiving US-guided PVB 1 h post-injection, indicating that US-MRI fusion guidance surpasses pure US guidance in achieving short-term pain relief. This immediate analgesic effect is primarily attributable to the local anesthetic action in the injected solution, with the enhanced accuracy in needle placement near the nerve root under image fusion guidance likely contributing to the lower pain scores.
However, no significant difference was observed in NRS scores or the average daily consumption of gabapentin between the two groups after 7 days, as shown in Tables 1 and 5. The sustained therapeutic impact of the nerve block over this period predominantly stems from the long-lasting anti-inflammatory and analgesic effects facilitated by the gradual release and penetration of triamcinolone acetonide into the surrounding tissues. This similarity in long-term therapeutic outcomes suggests that despite the initial advantages of US-MRI fusion in terms of precision and immediate pain relief, both methods demonstrate comparable efficacy in managing chronic pain over a week, underscoring the potential of US-MRI fusion guidance as a valuable tool for enhancing the immediate effectiveness of PVB procedures without compromising long-term treatment outcomes.
In the cohort receiving US-guided PVB (US-guided PVB), four patients experienced adverse reactions post-treatment, including dizziness and a decline in lower limb muscle strength. These complications may be attributed to inadequate imaging quality of the paraspinal tissues, which compromised the efficacy of US guidance. The reduced imaging clarity could lead to inadvertent damage to surrounding blood vessels and tissues during multiple needle adjustments. Gofeld et al. [12] noted that the visibility of lumbar nerve roots and blood vessels depends on the depth and echogenicity of adjacent tissues, suggesting that nerves or blood vessels not clearly visualized might be inadvertently pierced by the needle, a finding that aligns with our observations. Additionally, during US-guided procedures, the nerve root may not be well visualized, increasing the risk of the needle tip damaging the nerve sheath or local anaesthetic infiltrating the subneural space, which could enhance motor nerve blockade and lead to reduced limb muscle strength.
Additionally, to further mitigate potential confounding factors between groups, we employed PSM. The matching process included covariates such as gender, age, disease duration, initial NRS scores, BMI, and disease type. The matching results indicated that after PSM, there were no significant differences in any covariates between the groups (SMD < 0.1, p > 0.05), ensuring comparability. This matching procedure enhances the credibility of our findings by reducing the impact of potential confounders on the study outcomes.
Remarkably, none of the patients who underwent US-MRI fusion-guided PVB reported adverse reactions akin to those seen with US guidance alone. This outcome underscores the capability of MRI to effectively bridge the gaps in US’s imaging of vascular and neural structures, thereby enhancing the treatment’s efficiency. The integration of MRI with US guidance evidently aids practitioners in more precisely navigating the needle, significantly reducing the likelihood of inadvertently puncturing blood vessels or nerves and, consequently, the occurrence of adverse events following the procedure. This suggests a considerable improvement in safety profiles for patients undergoing PVB with US-MRI fusion guidance, highlighting the method’s potential to refine procedural accuracy and minimize risk.
The method we have introduced, while promising, is not without its drawbacks. Initially, the process of target positioning and the duration of procedures under US-MRI fusion image guidance are considerably lengthier than those guided by US alone, which could potentially impact patient comfort and procedure throughput negatively. Additionally, the small sample size of our study limits the robustness and generalizability of our findings, necessitating further validation of the proposed method’s efficacy and safety within a larger patient cohort. Moreover, the brief follow-up period employed in our study precludes any assessment of the long-term comparative effectiveness of the two guidance techniques. To address these limitations, future research efforts will focus on expanding the participant base and extending the follow-up duration.
The integration of US and MRI technologies in our study has shown significant promise in enhancing the precision and safety of nerve block procedures. The combination leverages the real-time imaging capability of US with the superior tissue contrast of MRI, providing more accurate needle placement and reducing the risk of inadvertent damage to surrounding structures. This is particularly beneficial in complex anatomical areas where US alone may not provide sufficient visualization.
Moreover, the lower incidence of adverse reactions in the fusion imaging group suggests that the enhanced precision directly translates into improved patient safety. The ability to visualize and avoid critical structures more effectively reduces the likelihood of complications such as nerve damage and vascular injury. While the initial costs of US-MRI fusion technology are higher, the potential for reducing the incidence of adverse events and improving clinical outcomes may offer cost savings in the long term. Fewer complications mean less need for additional treatments and shorter recovery times, which could offset the higher upfront investment.
Our study specifically observed that at 1 h post-treatment, the pain scores in the US-MRI fusion group were superior to those in the US-guided group. This early indication of efficacy suggests that the fusion technique provides immediate benefits in pain management. Additionally, the incidence of adverse reactions was lower in the fusion group, reflecting better safety outcomes.
Furthermore, although this study achieved between-group comparability in baseline characteristics through PSM, we also considered other potential confounding factors, such as BMI. BMI may influence patients’ perception of pain as well as their response to PVB treatment. Therefore, future research should further investigate the potential impact of variables such as BMI on the efficacy of PVB therapy to ensure the comprehensiveness and accuracy of the findings.
Future research targeting areas where US guidance alone is challenging, such as the dorsal root ganglia and lumbar intervertebral discs, is expected to further demonstrate the advantages of fusion imaging technology. This ongoing work aims to expand the clinical applications of US-MRI fusion, potentially establishing it as a standard of care in more complex cases.
Acknowledgments
We would like to express our gratitude to Chao Zhang for his valuable contributions to patient recruitment and data collection during the research process.
-
Funding information: The authors acknowledge financial support from the Special Project for Undergraduate Students to Cultivate Scientific Research of Third Medical Military University (No. 31041337).
-
Author contributions: Ying Shi and Bo Li conceptualized and designed the study. Ying Shi recruited patients. Shuyao He was primarily responsible for writing the manuscript. Yaona Xu analyzed the data. Ying Shi and Bo Li are responsible for the overall content as guarantors. The final manuscript was read and approved by all writers.
-
Conflict of interest: The authors declare no conflicts of interest. Dr Bo Li serves as Editor for Open Medicine, but it did not affect the peer-review process.
-
Data availability statement: The original data could be obtained from the corresponding author.
References
[1] Hoy D, Brooks P, Blyth F. The epidemiology of low back pain. Best Pract Res Clin Rheumatol. 2010;24:769–81.10.1016/j.berh.2010.10.002Search in Google Scholar PubMed
[2] Will JS, Bury DC, Miller JA. Mechanical low back pain. Am Fam Phys. 2018;98:421–8.Search in Google Scholar
[3] Chen CP, Tang SF, Hsu TC, Tsai WC, Liu HP, Chen MJ, et al. Ultrasound guidance in caudal epidural needle placement. Anesthesiology. 2004;101:181–4.10.1097/00000542-200407000-00028Search in Google Scholar PubMed
[4] Evansa I, Logina I, Vanags I, Borgeat A. Ultrasound versus fluoroscopic-guided epidural steroid injections in patients with degenerative spinal diseases: A randomized study. Eur J Anaesthesiol. 2015;32:262–8.10.1097/EJA.0000000000000103Search in Google Scholar PubMed
[5] Carrino JA, Khurana B, Ready JE, Silverman SG, Winalski CS. Magnetic resonance imaging-guided percutaneous biopsy of musculoskeletal lesions. J Bone Jt Surg Am. 2007;89:2179–87.10.2106/JBJS.F.01230Search in Google Scholar PubMed
[6] Psaty BM, Siscovick DS. Minimizing bias due to confounding by indication in comparative effectiveness research: The importance of restriction. JAMA. 2010;304:897–8.10.1001/jama.2010.1205Search in Google Scholar PubMed
[7] Schober P, Vetter TR. Propensity score matching in observational research. Anesth Analg. 2020;130:1616–7.10.1213/ANE.0000000000004770Search in Google Scholar PubMed
[8] Jang JH, Lee WY, Kim JW, Cho KR, Nam SH, Park YB. Ultrasound-guided selective nerve root block versus fluoroscopy-guided interlaminar epidural block versus fluoroscopy-guided transforaminal epidural block for the treatment of radicular pain in the lower cervical spine: A retrospective comparative study. Pain Res Manag. 2020;2020:9103421.10.1155/2020/9103421Search in Google Scholar PubMed PubMed Central
[9] Li X-M, Xiao W-H, Yang P, Zhao H-X. Psychological distress and cancer pain: results from a controlled cross-sectional survey in China. Sci Rep. 2017;7:39397.10.1038/srep39397Search in Google Scholar PubMed PubMed Central
[10] American Society of Anesthesiologists Task Force on Chronic Pain Management, American Society of Regional Anesthesia and Pain Medicine. Practice guidelines for chronic pain management: An updated report by the American Society of Anesthesiologists Task Force on Chronic Pain Management and the American Society of Regional Anesthesia and Pain Medicine. Anesthesiology. 2010;112:810–33.10.1097/ALN.0b013e3181c43103Search in Google Scholar PubMed
[11] Cansever T, Kabatas S, Civelek E, Kircelli A, Yilmaz C, Musluman M, et al. Transforaminal epidural steroid injection via a preganglionic approach for the treatment of lumbar radicular pain. Turk Neurosurg. 2012;22:183–8.10.5137/1019-5149.JTN.5151-11.3Search in Google Scholar PubMed
[12] Gofeld M, Bristow SJ, Chiu SC, McQueen CK, Bollag L. Ultrasound-guided lumbar transforaminal injections: feasibility and validation study. Spine (Phila Pa 1976). 2012;37:808–12.10.1097/BRS.0b013e3182340096Search in Google Scholar PubMed
[13] Riew KD, Yin Y, Gilula L, Bridwell KH, Lenke LG, Lauryssen C, et al. The effect of nerve-root injections on the need for operative treatment of lumbar radicular pain. J Bone Jt Surg Am. 2000;82:1589–93.10.2106/00004623-200011000-00012Search in Google Scholar PubMed
[14] Rivera CE. Lumbar epidural steroid injections. Phys Med Rehabil Clin N Am. 2018;29:73–92.10.1016/j.pmr.2017.08.007Search in Google Scholar PubMed
[15] Chumnanvej S, Wetchagama N, Kounsongtham V. Accuracy of needle-tip localization by ultrasound guidance lumbar selective nerve root block: A prospective clinical study of 78 lumbar nerve roots block. J Med Assoc Thai. 2011;94:1451–6.Search in Google Scholar
[16] Maurits NM, Bollen AE, Windhausen A, De Jager AE, Van Der Hoeven JH. Muscle ultrasound analysis: normal values and differentiation between myopathies and neuropathies. Ultrasound Med Biol. 2003;29:215–25.10.1016/S0301-5629(02)00758-5Search in Google Scholar PubMed
[17] Karmakar MK, Li X, Ho M-H, Kwok WH, Chui PT. Real-time ultrasound-guided paramedian epidural access: evaluation of a novel in-plane technique. Br J Anaesth. 2009;102:845–54.10.1093/bja/aep079Search in Google Scholar PubMed
[18] Carvalho JC. Ultrasound-facilitated epidurals and spinals in obstetrics. Anesthesiol Clin. 2008;26:145–58.10.1016/j.anclin.2007.11.007Search in Google Scholar PubMed
[19] Svanbergsson G, Ingvarsson T, Arnardóttir RH. MRI for diagnosis of low back pain: Usability, association with symptoms and influence on treatment. Laeknabladid. 2017;103:17–22 (Icelandic).10.17992/lbl.2017.01.116Search in Google Scholar PubMed
[20] Pang H, Bow C, Cheung JPY, Zehra U, Borthakur A, Karppinen J, et al. The UTE disc sign on MRI: A novel imaging biomarker associated with degenerative spine changes, low back pain, and disability. Spine (Phila Pa 1976). 2018;43:503–11.10.1097/BRS.0000000000002369Search in Google Scholar PubMed PubMed Central
[21] Hovet S, Ren H, Xu S, Wood B, Tokuda J, Tse ZTH. MRI-powered biomedical devices. Minim Invasive Ther Allied Technol. 2018;27:191–202.10.1080/13645706.2017.1402188Search in Google Scholar PubMed PubMed Central
[22] Sequeiros RB, Ojala RO, Klemola R, Vaara TJ, Jyrkinen L, Tervonen OA. MRI-guided periradicular nerve root infiltration therapy in low-field (0.23-T) MRI system using optical instrument tracking. Eur Radiol. 2002;12:1331–7.10.1007/s00330-002-1397-zSearch in Google Scholar PubMed
[23] Himes NC, Chansakul T, Lee TC. Magnetic resonance imaging-guided spine interventions. Magn Reson Imaging Clin N Am. 2015;23:523–32.10.1016/j.mric.2015.05.007Search in Google Scholar PubMed PubMed Central
© 2025 the author(s), published by De Gruyter
This work is licensed under the Creative Commons Attribution 4.0 International License.
Articles in the same Issue
- Research Articles
- Network pharmacological analysis and in vitro testing of the rutin effects on triple-negative breast cancer
- Impact of diabetes on long-term survival in elderly liver cancer patients: A retrospective study
- Knockdown of CCNB1 alleviates high glucose-triggered trophoblast dysfunction during gestational diabetes via Wnt/β-catenin signaling pathway
- Risk factors for severe adverse drug reactions in hospitalized patients
- Analysis of the effect of ALA-PDT on macrophages in footpad model of mice infected with Fonsecaea monophora based on single-cell sequencing
- Development and validation of headspace gas chromatography with a flame ionization detector method for the determination of ethanol in the vitreous humor
- CMSP exerts anti-tumor effects on small cell lung cancer cells by inducing mitochondrial dysfunction and ferroptosis
- Predictive value of plasma sB7-H3 and YKL-40 in pediatric refractory Mycoplasma pneumoniae pneumonia
- Antiangiogenic potential of Elaeagnus umbellata extracts and molecular docking study by targeting VEGFR-2 pathway
- Comparison of the effectiveness of nurse-led preoperative counseling and postoperative follow-up care vs standard care for patients with gastric cancer
- Comparing the therapeutic efficacy of endoscopic minimally invasive surgery and traditional surgery for early-stage breast cancer: A meta-analysis
- Adhered macrophages as an additional marker of cardiomyocyte injury in biopsies of patients with dilated cardiomyopathy
- Association between statin administration and outcome in patients with sepsis: A retrospective study
- Exploration of the association between estimated glucose disposal rate and osteoarthritis in middle-aged and older adults: An analysis of NHANES data from 2011 to 2018
- A comparative analysis of the binary and multiclass classified chest X-ray images of pneumonia and COVID-19 with ML and DL models
- Lysophosphatidic acid 2 alleviates deep vein thrombosis via protective endothelial barrier function
- Transcription factor A, mitochondrial promotes lymph node metastasis and lymphangiogenesis in epithelial ovarian carcinoma
- Serum PM20D1 levels are associated with nutritional status and inflammatory factors in gastric cancer patients undergoing early enteral nutrition
- Hydromorphone reduced the incidence of emergence agitation after adenotonsillectomy in children with obstructive sleep apnea: A randomized, double-blind study
- Vitamin D replacement therapy may regulate sleep habits in patients with restless leg syndrome
- The first-line antihypertensive nitrendipine potentiated the therapeutic effect of oxaliplatin by downregulating CACNA1D in colorectal cancer
- Health literacy and health-related quality of life: The mediating role of irrational happiness
- Modulatory effects of Lycium barbarum polysaccharide on bone cell dynamics in osteoporosis
- Mechanism research on inhibition of gastric cancer in vitro by the extract of Pinellia ternata based on network pharmacology and cellular metabolomics
- Examination of the causal role of immune cells in non-alcoholic fatty liver disease by a bidirectional Mendelian randomization study
- Clinical analysis of ten cases of HIV infection combined with acute leukemia
- Investigating the cardioprotective potential of quercetin against tacrolimus-induced cardiotoxicity in Wistar rats: A mechanistic insights
- Clinical observation of probiotics combined with mesalazine and Yiyi Baitouweng Decoction retention enema in treating mild-to-moderate ulcerative colitis
- Diagnostic value of ratio of blood inflammation to coagulation markers in periprosthetic joint infection
- Sex-specific associations of sex hormone binding globulin and risk of bladder cancer
- Core muscle strength and stability-oriented breathing training reduces inter-recti distance in postpartum women
- The ERAS nursing care strategy for patients undergoing transsphenoidal endoscopic pituitary tumor resection: A randomized blinded controlled trial
- The serum IL-17A levels in patients with traumatic bowel rupture post-surgery and its predictive value for patient prognosis
- Impact of Kolb’s experiential learning theory-based nursing on caregiver burden and psychological state of caregivers of dementia patients
- Analysis of serum NLR combined with intraoperative margin condition to predict the prognosis of cervical HSIL patients undergoing LEEP surgery
- Commiphora gileadensis ameliorate infertility and erectile dysfunction in diabetic male mice
- The correlation between epithelial–mesenchymal transition classification and MMP2 expression of circulating tumor cells and prognosis of advanced or metastatic nasopharyngeal carcinoma
- Tetrahydropalmatine improves mitochondrial function in vascular smooth muscle cells of atherosclerosis in vitro by inhibiting Ras homolog gene family A/Rho-associated protein kinase-1 signaling pathway
- A cross-sectional study: Relationship between serum oxidative stress levels and arteriovenous fistula maturation in maintenance dialysis patients
- A comparative analysis of the impact of repeated administration of flavan 3-ol on brown, subcutaneous, and visceral adipose tissue
- Identifying early screening factors for depression in middle-aged and older adults: A cohort study
- Perform tumor-specific survival analysis for Merkel cell carcinoma patients undergoing surgical resection based on the SEER database by constructing a nomogram chart
- Unveiling the role of CXCL10 in pancreatic cancer progression: A novel prognostic indicator
- High-dose preoperative intraperitoneal erythropoietin and intravenous methylprednisolone in acute traumatic spinal cord injuries following decompression surgeries
- RAB39B: A novel biomarker for acute myeloid leukemia identified via multi-omics and functional validation
- Impact of peripheral conditioning on reperfusion injury following primary percutaneous coronary intervention in diabetic and non-diabetic STEMI patients
- Clinical efficacy of azacitidine in the treatment of middle- and high-risk myelodysplastic syndrome in middle-aged and elderly patients: A retrospective study
- The effect of ambulatory blood pressure load on mitral regurgitation in continuous ambulatory peritoneal dialysis patients
- Expression and clinical significance of ITGA3 in breast cancer
- Single-nucleus RNA sequencing reveals ARHGAP28 expression of podocytes as a biomarker in human diabetic nephropathy
- rSIG combined with NLR in the prognostic assessment of patients with multiple injuries
- Toxic metals and metalloids in collagen supplements of fish and jellyfish origin: Risk assessment for daily intake
- Exploring causal relationship between 41 inflammatory cytokines and marginal zone lymphoma: A bidirectional Mendelian randomization study
- Gender beliefs and legitimization of dating violence in adolescents
- Effect of serum IL-6, CRP, and MMP-9 levels on the efficacy of modified preperitoneal Kugel repair in patients with inguinal hernia
- Effect of smoking and smoking cessation on hematological parameters in polycythemic patients
- Pathogen surveillance and risk factors for pulmonary infection in patients with lung cancer: A retrospective single-center study
- Necroptosis of hippocampal neurons in paclitaxel chemotherapy-induced cognitive impairment mediates microglial activation via TLR4/MyD88 signaling pathway
- Celastrol suppresses neovascularization in rat aortic vascular endothelial cells stimulated by inflammatory tenocytes via modulating the NLRP3 pathway
- Cord-lamina angle and foraminal diameter as key predictors of C5 palsy after anterior cervical decompression and fusion surgery
- GATA1: A key biomarker for predicting the prognosis of patients with diffuse large B-cell lymphoma
- Influencing factors of false lumen thrombosis in type B aortic dissection: A single-center retrospective study
- MZB1 regulates the immune microenvironment and inhibits ovarian cancer cell migration
- Integrating experimental and network pharmacology to explore the pharmacological mechanisms of Dioscin against glioblastoma
- Trends in research on preterm birth in twin pregnancy based on bibliometrics
- Four-week IgE/baseline IgE ratio combined with tryptase predicts clinical outcome in omalizumab-treated children with moderate-to-severe asthma
- Single-cell transcriptomic analysis identifies a stress response Schwann cell subtype
- Acute pancreatitis risk in the diagnosis and management of inflammatory bowel disease: A critical focus
- Effect of subclinical esketamine on NLRP3 and cognitive dysfunction in elderly ischemic stroke patients
- Interleukin-37 mediates the anti-oral tumor activity in oral cancer through STAT3
- CA199 and CEA expression levels, and minimally invasive postoperative prognosis analysis in esophageal squamous carcinoma patients
- Efficacy of a novel drainage catheter in the treatment of CSF leak after posterior spine surgery: A retrospective cohort study
- Comprehensive biomedicine assessment of Apteranthes tuberculata extracts: Phytochemical analysis and multifaceted pharmacological evaluation in animal models
- Relation of time in range to severity of coronary artery disease in patients with type 2 diabetes: A cross-sectional study
- Dopamine attenuates ethanol-induced neuronal apoptosis by stimulating electrical activity in the developing rat retina
- Correlation between albumin levels during the third trimester and the risk of postpartum levator ani muscle rupture
- Factors associated with maternal attention and distraction during breastfeeding and childcare: A cross-sectional study in the west of Iran
- Mechanisms of hesperetin in treating metabolic dysfunction-associated steatosis liver disease via network pharmacology and in vitro experiments
- The law on oncological oblivion in the Italian and European context: How to best uphold the cancer patients’ rights to privacy and self-determination?
- The prognostic value of the neutrophil-to-lymphocyte ratio, platelet-to-lymphocyte ratio, and prognostic nutritional index for survival in patients with colorectal cancer
- Factors affecting the measurements of peripheral oxygen saturation values in healthy young adults
- Comparison and correlations between findings of hysteroscopy and vaginal color Doppler ultrasonography for detection of uterine abnormalities in patients with recurrent implantation failure
- The effects of different types of RAGT on balance function in stroke patients with low levels of independent walking in a convalescent rehabilitation hospital
- Causal relationship between asthma and ankylosing spondylitis: A bidirectional two-sample univariable and multivariable Mendelian randomization study
- Correlations of health literacy with individuals’ understanding and use of medications in Southern Taiwan
- Correlation of serum calprotectin with outcome of acute cerebral infarction
- Comparison of computed tomography and guided bronchoscopy in the diagnosis of pulmonary nodules: A systematic review and meta-analysis
- Curdione protects vascular endothelial cells and atherosclerosis via the regulation of DNMT1-mediated ERBB4 promoter methylation
- The identification of novel missense variant in ChAT gene in a patient with gestational diabetes denotes plausible genetic association
- Molecular genotyping of multi-system rare blood types in foreign blood donors based on DNA sequencing and its clinical significance
- Exploring the role of succinyl carnitine in the association between CD39⁺ CD4⁺ T cell and ulcerative colitis: A Mendelian randomization study
- Dexmedetomidine suppresses microglial activation in postoperative cognitive dysfunction via the mmu-miRNA-125/TRAF6 signaling axis
- Analysis of serum metabolomics in patients with different types of chronic heart failure
- Diagnostic value of hematological parameters in the early diagnosis of acute cholecystitis
- Pachymaran alleviates fat accumulation, hepatocyte degeneration, and injury in mice with nonalcoholic fatty liver disease
- Decrease in CD4 and CD8 lymphocytes are predictors of severe clinical picture and unfavorable outcome of the disease in patients with COVID-19
- METTL3 blocked the progression of diabetic retinopathy through m6A-modified SOX2
- The predictive significance of anti-RO-52 antibody in patients with interstitial pneumonia after treatment of malignant tumors
- Exploring cerebrospinal fluid metabolites, cognitive function, and brain atrophy: Insights from Mendelian randomization
- Development and validation of potential molecular subtypes and signatures of ocular sarcoidosis based on autophagy-related gene analysis
- Widespread venous thrombosis: Unveiling a complex case of Behçet’s disease with a literature perspective
- Uterine fibroid embolization: An analysis of clinical outcomes and impact on patients’ quality of life
- Discovery of lipid metabolism-related diagnostic biomarkers and construction of diagnostic model in steroid-induced osteonecrosis of femoral head
- Serum-derived exomiR-188-3p is a promising novel biomarker for early-stage ovarian cancer
- Enhancing chronic back pain management: A comparative study of ultrasound–MRI fusion guidance for paravertebral nerve block
- Peptide CCAT1-70aa promotes hepatocellular carcinoma proliferation and invasion via the MAPK/ERK pathway
- Electroacupuncture-induced reduction of myocardial ischemia–reperfusion injury via FTO-dependent m6A methylation modulation
- Hemorrhoids and cardiovascular disease: A bidirectional Mendelian randomization study
- Cell-free adipose extract inhibits hypertrophic scar formation through collagen remodeling and antiangiogenesis
- HALP score in Demodex blepharitis: A case–control study
- Assessment of SOX2 performance as a marker for circulating cancer stem-like cells (CCSCs) identification in advanced breast cancer patients using CytoTrack system
- Risk and prognosis for brain metastasis in primary metastatic cervical cancer patients: A population-based study
- Comparison of the two intestinal anastomosis methods in pediatric patients
- Factors influencing hematological toxicity and adverse effects of perioperative hyperthermic intraperitoneal vs intraperitoneal chemotherapy in gastrointestinal cancer
- Endotoxin tolerance inhibits NLRP3 inflammasome activation in macrophages of septic mice by restoring autophagic flux through TRIM26
- Lateral transperitoneal laparoscopic adrenalectomy: A single-centre experience of 21 procedures
- Petunidin attenuates lipopolysaccharide-induced retinal microglia inflammatory response in diabetic retinopathy by targeting OGT/NF-κB/LCN2 axis
- Procalcitonin and C-reactive protein as biomarkers for diagnosing and assessing the severity of acute cholecystitis
- Factors determining the number of sessions in successful extracorporeal shock wave lithotripsy patients
- Development of a nomogram for predicting cancer-specific survival in patients with renal pelvic cancer following surgery
- Inhibition of ATG7 promotes orthodontic tooth movement by regulating the RANKL/OPG ratio under compression force
- A machine learning-based prognostic model integrating mRNA stemness index, hypoxia, and glycolysis‑related biomarkers for colorectal cancer
- Glutathione attenuates sepsis-associated encephalopathy via dual modulation of NF-κB and PKA/CREB pathways
- FAHD1 prevents neuronal ferroptosis by modulating R-loop and the cGAS–STING pathway
- Association of placenta weight and morphology with term low birth weight: A case–control study
- Investigation of the pathogenic variants induced Sjogren’s syndrome in Turkish population
- Nucleotide metabolic abnormalities in post-COVID-19 condition and type 2 diabetes mellitus patients and their association with endocrine dysfunction
- TGF-β–Smad2/3 signaling in high-altitude pulmonary hypertension in rats: Role and mechanisms via macrophage M2 polarization
- Ultrasound-guided unilateral versus bilateral erector spinae plane block for postoperative analgesia of patients undergoing laparoscopic cholecystectomy
- Profiling gut microbiome dynamics in subacute thyroiditis: Implications for pathogenesis, diagnosis, and treatment
- Delta neutrophil index, CRP/albumin ratio, procalcitonin, immature granulocytes, and HALP score in acute appendicitis: Best performing biomarker?
- Anticancer activity mechanism of novelly synthesized and characterized benzofuran ring-linked 3-nitrophenyl chalcone derivative on colon cancer cells
- H2valdien3 arrests the cell cycle and induces apoptosis of gastric cancer
- Prognostic relevance of PRSS2 and its immune correlates in papillary thyroid carcinoma
- Association of SGLT2 inhibition with psychiatric disorders: A Mendelian randomization study
- Motivational interviewing for alcohol use reduction in Thai patients
- Luteolin alleviates oxygen-glucose deprivation/reoxygenation-induced neuron injury by regulating NLRP3/IL-1β signaling
- Polyphyllin II inhibits thyroid cancer cell growth by simultaneously inhibiting glycolysis and oxidative phosphorylation
- Relationship between the expression of copper death promoting factor SLC31A1 in papillary thyroid carcinoma and clinicopathological indicators and prognosis
- CSF2 polarized neutrophils and invaded renal cancer cells in vitro influence
- Proton pump inhibitors-induced thrombocytopenia: A systematic literature analysis of case reports
- The current status and influence factors of research ability among community nurses: A sequential qualitative–quantitative study
- OKAIN: A comprehensive oncology knowledge base for the interpretation of clinically actionable alterations
- The relationship between serum CA50, CA242, and SAA levels and clinical pathological characteristics and prognosis in patients with pancreatic cancer
- Identification and external validation of a prognostic signature based on hypoxia–glycolysis-related genes for kidney renal clear cell carcinoma
- Engineered RBC-derived nanovesicles functionalized with tumor-targeting ligands: A comparative study on breast cancer targeting efficiency and biocompatibility
- Relationship of resting echocardiography combined with serum micronutrients to the severity of low-gradient severe aortic stenosis
- Effect of vibration on pain during subcutaneous heparin injection: A randomized, single-blind, placebo-controlled trial
- The diagnostic performance of machine learning-based FFRCT for coronary artery disease: A meta-analysis
- Comparing biofeedback device vs diaphragmatic breathing for bloating relief: A randomized controlled trial
- Serum uric acid to albumin ratio and C-reactive protein as predictive biomarkers for chronic total occlusion and coronary collateral circulation quality
- Multiple organ scoring systems for predicting in-hospital mortality of sepsis patients in the intensive care unit
- Single-cell RNA sequencing data analysis of the inner ear in gentamicin-treated mice via intraperitoneal injection
- Suppression of cathepsin B attenuates myocardial injury via limiting cardiomyocyte apoptosis
- Influence of sevoflurane combined with propofol anesthesia on the anesthesia effect and adverse reactions in children with acute appendicitis
- Identification of hub genes related to acute kidney injury caused by sevoflurane anesthesia and endoplasmic reticulum stress
- Efficacy and safety of PD-1/PD-L1 inhibitors in pancreatic ductal adenocarcinoma: a systematic review and Meta-analysis of randomized controlled trials
- The value of diagnostic experience in O-RADS MRI score for ovarian-adnexal lesions
- Health education pathway for individuals with temporary enterostomies using patient journey mapping
- Serum TLR8 as a potential diagnostic biomarker of coronary heart disease
- Intraoperative temperature management and its effect on surgical outcomes in elderly patients undergoing lichtenstein unilateral inguinal hernia repair
- Immunohistochemical profiling and neuroepithelial heterogeneity in immature ovarian teratomas: a retrospective digital pathology-based study
- Associated risk factors and prevalence of human papillomavirus infection among females visiting tertiary care hospital: a cross-sectional study from Nepal
- Comparative evaluation of various disc elution methods for the detection of colistin-resistant gram-negative bacteria
- Effect of timing of cholecystectomy on weight loss after sleeve gastrectomy in morbidly obese individuals with cholelithiasis: a retrospective cohort study
- Causal association between ceramide levels and central precocious puberty: a mendelian randomization study
- Novel predictive model for colorectal liver metastases recurrence: a radiomics and clinical data approach
- Relationship between resident physicians’ perceived professional value and exposure to violence
- Multiple sclerosis and type 1 diabetes: a Mendelian randomization study of European ancestry
- Rapid pathogen identification in peritoneal dialysis effluent by MALDI-TOF MS following blood culture enrichment
- Comparison of open and percutaneous A1 pulley release in pediatric trigger thumb: a retrospective cohort study
- Impact of combined diaphragm-lung ultrasound assessment on postoperative respiratory function in patients under general anesthesia recovery
- Development and internal validation of a nomogram for predicting short-term prognosis in ICU patients with acute pyelonephritis
- The association between hypoxic burden and blood pressure in patients with obstructive sleep apnea
- Promotion of asthenozoospermia by C9orf72 through suppression of spermatogonia activity via fructose metabolism and mitophagy
- Review Articles
- The effects of enhanced external counter-pulsation on post-acute sequelae of COVID-19: A narrative review
- Diabetes-related cognitive impairment: Mechanisms, symptoms, and treatments
- Microscopic changes and gross morphology of placenta in women affected by gestational diabetes mellitus in dietary treatment: A systematic review
- Review of mechanisms and frontier applications in IL-17A-induced hypertension
- Research progress on the correlation between islet amyloid peptides and type 2 diabetes mellitus
- The safety and efficacy of BCG combined with mitomycin C compared with BCG monotherapy in patients with non-muscle-invasive bladder cancer: A systematic review and meta-analysis
- The application of augmented reality in robotic general surgery: A mini-review
- The effect of Greek mountain tea extract and wheat germ extract on peripheral blood flow and eicosanoid metabolism in mammals
- Neurogasobiology of migraine: Carbon monoxide, hydrogen sulfide, and nitric oxide as emerging pathophysiological trinacrium relevant to nociception regulation
- Plant polyphenols, terpenes, and terpenoids in oral health
- Laboratory medicine between technological innovation, rights safeguarding, and patient safety: A bioethical perspective
- End-of-life in cancer patients: Medicolegal implications and ethical challenges in Europe
- The maternal factors during pregnancy for intrauterine growth retardation: An umbrella review
- Intra-abdominal hypertension/abdominal compartment syndrome of pediatric patients in critical care settings
- PI3K/Akt pathway and neuroinflammation in sepsis-associated encephalopathy
- Screening of Group B Streptococcus in pregnancy: A systematic review for the laboratory detection
- Giant borderline ovarian tumours – review of the literature
- Leveraging artificial intelligence for collaborative care planning: Innovations and impacts in shared decision-making – A systematic review
- Cholera epidemiology analysis through the experience of the 1973 Naples epidemic
- Risk factors of frailty/sarcopenia in community older adults: Meta-analysis
- Supplement strategies for infertility in overweight women: Evidence and legal insights
- Scurvy, a not obsolete disorder: Clinical report in eight young children and literature review
- A meta-analysis of the effects of DBS on cognitive function in patients with advanced PD
- Protective role of selenium in sepsis: Mechanisms and potential therapeutic strategies
- Strategies for hyperkalemia management in dialysis patients: A systematic review
- C-reactive protein-to-albumin ratio in peripheral artery disease
- Research progress on autophagy and its roles in sepsis induced organ injury
- Neuronutrition in autism spectrum disorders
- Pumilio 2 in neural development, function, and specific neurological disorders
- Antibiotic prescribing patterns in general dental practice- a scoping review
- Clinical and medico-legal reflections on non-invasive prenatal testing
- Smartphone use and back pain: a narrative review of postural pathologies
- Targeting endothelial oxidative stress in hypertension
- Exploring links between acne and metabolic syndrome: a narrative review
- Case Reports
- Delayed graft function after renal transplantation
- Semaglutide treatment for type 2 diabetes in a patient with chronic myeloid leukemia: A case report and review of the literature
- Diverse electrophysiological demyelinating features in a late-onset glycogen storage disease type IIIa case
- Giant right atrial hemangioma presenting with ascites: A case report
- Laser excision of a large granular cell tumor of the vocal cord with subglottic extension: A case report
- EsoFLIP-assisted dilation for dysphagia in systemic sclerosis: Highlighting the role of multimodal esophageal evaluation
- Molecular hydrogen-rhodiola as an adjuvant therapy for ischemic stroke in internal carotid artery occlusion: A case report
- Coronary artery anomalies: A case of the “malignant” left coronary artery and its surgical management
- Combined VAT and retroperitoneoscopy for pleural empyema due to nephro-pleuric fistula in xanthogranulomatous pyelonephritis
- A rare case of Opalski syndrome with a suspected multiple sclerosis etiology
- Newly diagnosed B-cell acute lymphoblastic leukemia demonstrating localized bone marrow infiltration exclusively in the lower extremities
- Rapid Communication
- Biological properties of valve materials using RGD and EC
-
A single oral administration of flavanols enhances short
-term memory in mice along with increased brain-derived neurotrophic factor - Repeat influenza incidence across two consecutive influenza seasons
- Letter to the Editor
- Role of enhanced external counterpulsation in long COVID
- Expression of Concern
- Expression of concern “A ceRNA network mediated by LINC00475 in papillary thyroid carcinoma”
- Expression of concern “Notoginsenoside R1 alleviates spinal cord injury through the miR-301a/KLF7 axis to activate Wnt/β-catenin pathway”
- Expression of concern “circ_0020123 promotes cell proliferation and migration in lung adenocarcinoma via PDZD8”
- Corrigendum
- Corrigendum to “Empagliflozin improves aortic injury in obese mice by regulating fatty acid metabolism”
- Corrigendum to “Comparing the therapeutic efficacy of endoscopic minimally invasive surgery and traditional surgery for early-stage breast cancer: A meta-analysis”
- Corrigendum to “The progress of autoimmune hepatitis research and future challenges”
- Retraction
- Retraction of “miR-654-5p promotes gastric cancer progression via the GPRIN1/NF-κB pathway”
- Retraction of: “LncRNA CASC15 inhibition relieves renal fibrosis in diabetic nephropathy through downregulating SP-A by sponging to miR-424”
- Retraction of: “SCARA5 inhibits oral squamous cell carcinoma via inactivating the STAT3 and PI3K/AKT signaling pathways”
- Special Issue Advancements in oncology: bridging clinical and experimental research - Part II
- Unveiling novel biomarkers for platinum chemoresistance in ovarian cancer
- Lathyrol affects the expression of AR and PSA and inhibits the malignant behavior of RCC cells
- The era of increasing cancer survivorship: Trends in fertility preservation, medico-legal implications, and ethical challenges
- Bone scintigraphy and positron emission tomography in the early diagnosis of MRONJ
- Meta-analysis of clinical efficacy and safety of immunotherapy combined with chemotherapy in non-small cell lung cancer
- Special Issue Computational Intelligence Methodologies Meets Recurrent Cancers - Part IV
- Exploration of mRNA-modifying METTL3 oncogene as momentous prognostic biomarker responsible for colorectal cancer development
- Special Issue The evolving saga of RNAs from bench to bedside - Part III
- Interaction and verification of ferroptosis-related RNAs Rela and Stat3 in promoting sepsis-associated acute kidney injury
- The mRNA MOXD1: Link to oxidative stress and prognostic significance in gastric cancer
- Special Issue Exploring the biological mechanism of human diseases based on MultiOmics Technology - Part II
- Dynamic changes in lactate-related genes in microglia and their role in immune cell interactions after ischemic stroke
- A prognostic model correlated with fatty acid metabolism in Ewing’s sarcoma based on bioinformatics analysis
- Red cell distribution width predicts early kidney injury: A NHANES cross-sectional study
- Special Issue Diabetes mellitus: pathophysiology, complications & treatment
- Nutritional risk assessment and nutritional support in children with congenital diabetes during surgery
- Correlation of the differential expressions of RANK, RANKL, and OPG with obesity in the elderly population in Xinjiang
- A discussion on the application of fluorescence micro-optical sectioning tomography in the research of cognitive dysfunction in diabetes
- A review of brain research on T2DM-related cognitive dysfunction
- Metformin and estrogen modulation in LABC with T2DM: A 36-month randomized trial
- Special Issue Innovative Biomarker Discovery and Precision Medicine in Cancer Diagnostics
- CircASH1L-mediated tumor progression in triple-negative breast cancer: PI3K/AKT pathway mechanisms
Articles in the same Issue
- Research Articles
- Network pharmacological analysis and in vitro testing of the rutin effects on triple-negative breast cancer
- Impact of diabetes on long-term survival in elderly liver cancer patients: A retrospective study
- Knockdown of CCNB1 alleviates high glucose-triggered trophoblast dysfunction during gestational diabetes via Wnt/β-catenin signaling pathway
- Risk factors for severe adverse drug reactions in hospitalized patients
- Analysis of the effect of ALA-PDT on macrophages in footpad model of mice infected with Fonsecaea monophora based on single-cell sequencing
- Development and validation of headspace gas chromatography with a flame ionization detector method for the determination of ethanol in the vitreous humor
- CMSP exerts anti-tumor effects on small cell lung cancer cells by inducing mitochondrial dysfunction and ferroptosis
- Predictive value of plasma sB7-H3 and YKL-40 in pediatric refractory Mycoplasma pneumoniae pneumonia
- Antiangiogenic potential of Elaeagnus umbellata extracts and molecular docking study by targeting VEGFR-2 pathway
- Comparison of the effectiveness of nurse-led preoperative counseling and postoperative follow-up care vs standard care for patients with gastric cancer
- Comparing the therapeutic efficacy of endoscopic minimally invasive surgery and traditional surgery for early-stage breast cancer: A meta-analysis
- Adhered macrophages as an additional marker of cardiomyocyte injury in biopsies of patients with dilated cardiomyopathy
- Association between statin administration and outcome in patients with sepsis: A retrospective study
- Exploration of the association between estimated glucose disposal rate and osteoarthritis in middle-aged and older adults: An analysis of NHANES data from 2011 to 2018
- A comparative analysis of the binary and multiclass classified chest X-ray images of pneumonia and COVID-19 with ML and DL models
- Lysophosphatidic acid 2 alleviates deep vein thrombosis via protective endothelial barrier function
- Transcription factor A, mitochondrial promotes lymph node metastasis and lymphangiogenesis in epithelial ovarian carcinoma
- Serum PM20D1 levels are associated with nutritional status and inflammatory factors in gastric cancer patients undergoing early enteral nutrition
- Hydromorphone reduced the incidence of emergence agitation after adenotonsillectomy in children with obstructive sleep apnea: A randomized, double-blind study
- Vitamin D replacement therapy may regulate sleep habits in patients with restless leg syndrome
- The first-line antihypertensive nitrendipine potentiated the therapeutic effect of oxaliplatin by downregulating CACNA1D in colorectal cancer
- Health literacy and health-related quality of life: The mediating role of irrational happiness
- Modulatory effects of Lycium barbarum polysaccharide on bone cell dynamics in osteoporosis
- Mechanism research on inhibition of gastric cancer in vitro by the extract of Pinellia ternata based on network pharmacology and cellular metabolomics
- Examination of the causal role of immune cells in non-alcoholic fatty liver disease by a bidirectional Mendelian randomization study
- Clinical analysis of ten cases of HIV infection combined with acute leukemia
- Investigating the cardioprotective potential of quercetin against tacrolimus-induced cardiotoxicity in Wistar rats: A mechanistic insights
- Clinical observation of probiotics combined with mesalazine and Yiyi Baitouweng Decoction retention enema in treating mild-to-moderate ulcerative colitis
- Diagnostic value of ratio of blood inflammation to coagulation markers in periprosthetic joint infection
- Sex-specific associations of sex hormone binding globulin and risk of bladder cancer
- Core muscle strength and stability-oriented breathing training reduces inter-recti distance in postpartum women
- The ERAS nursing care strategy for patients undergoing transsphenoidal endoscopic pituitary tumor resection: A randomized blinded controlled trial
- The serum IL-17A levels in patients with traumatic bowel rupture post-surgery and its predictive value for patient prognosis
- Impact of Kolb’s experiential learning theory-based nursing on caregiver burden and psychological state of caregivers of dementia patients
- Analysis of serum NLR combined with intraoperative margin condition to predict the prognosis of cervical HSIL patients undergoing LEEP surgery
- Commiphora gileadensis ameliorate infertility and erectile dysfunction in diabetic male mice
- The correlation between epithelial–mesenchymal transition classification and MMP2 expression of circulating tumor cells and prognosis of advanced or metastatic nasopharyngeal carcinoma
- Tetrahydropalmatine improves mitochondrial function in vascular smooth muscle cells of atherosclerosis in vitro by inhibiting Ras homolog gene family A/Rho-associated protein kinase-1 signaling pathway
- A cross-sectional study: Relationship between serum oxidative stress levels and arteriovenous fistula maturation in maintenance dialysis patients
- A comparative analysis of the impact of repeated administration of flavan 3-ol on brown, subcutaneous, and visceral adipose tissue
- Identifying early screening factors for depression in middle-aged and older adults: A cohort study
- Perform tumor-specific survival analysis for Merkel cell carcinoma patients undergoing surgical resection based on the SEER database by constructing a nomogram chart
- Unveiling the role of CXCL10 in pancreatic cancer progression: A novel prognostic indicator
- High-dose preoperative intraperitoneal erythropoietin and intravenous methylprednisolone in acute traumatic spinal cord injuries following decompression surgeries
- RAB39B: A novel biomarker for acute myeloid leukemia identified via multi-omics and functional validation
- Impact of peripheral conditioning on reperfusion injury following primary percutaneous coronary intervention in diabetic and non-diabetic STEMI patients
- Clinical efficacy of azacitidine in the treatment of middle- and high-risk myelodysplastic syndrome in middle-aged and elderly patients: A retrospective study
- The effect of ambulatory blood pressure load on mitral regurgitation in continuous ambulatory peritoneal dialysis patients
- Expression and clinical significance of ITGA3 in breast cancer
- Single-nucleus RNA sequencing reveals ARHGAP28 expression of podocytes as a biomarker in human diabetic nephropathy
- rSIG combined with NLR in the prognostic assessment of patients with multiple injuries
- Toxic metals and metalloids in collagen supplements of fish and jellyfish origin: Risk assessment for daily intake
- Exploring causal relationship between 41 inflammatory cytokines and marginal zone lymphoma: A bidirectional Mendelian randomization study
- Gender beliefs and legitimization of dating violence in adolescents
- Effect of serum IL-6, CRP, and MMP-9 levels on the efficacy of modified preperitoneal Kugel repair in patients with inguinal hernia
- Effect of smoking and smoking cessation on hematological parameters in polycythemic patients
- Pathogen surveillance and risk factors for pulmonary infection in patients with lung cancer: A retrospective single-center study
- Necroptosis of hippocampal neurons in paclitaxel chemotherapy-induced cognitive impairment mediates microglial activation via TLR4/MyD88 signaling pathway
- Celastrol suppresses neovascularization in rat aortic vascular endothelial cells stimulated by inflammatory tenocytes via modulating the NLRP3 pathway
- Cord-lamina angle and foraminal diameter as key predictors of C5 palsy after anterior cervical decompression and fusion surgery
- GATA1: A key biomarker for predicting the prognosis of patients with diffuse large B-cell lymphoma
- Influencing factors of false lumen thrombosis in type B aortic dissection: A single-center retrospective study
- MZB1 regulates the immune microenvironment and inhibits ovarian cancer cell migration
- Integrating experimental and network pharmacology to explore the pharmacological mechanisms of Dioscin against glioblastoma
- Trends in research on preterm birth in twin pregnancy based on bibliometrics
- Four-week IgE/baseline IgE ratio combined with tryptase predicts clinical outcome in omalizumab-treated children with moderate-to-severe asthma
- Single-cell transcriptomic analysis identifies a stress response Schwann cell subtype
- Acute pancreatitis risk in the diagnosis and management of inflammatory bowel disease: A critical focus
- Effect of subclinical esketamine on NLRP3 and cognitive dysfunction in elderly ischemic stroke patients
- Interleukin-37 mediates the anti-oral tumor activity in oral cancer through STAT3
- CA199 and CEA expression levels, and minimally invasive postoperative prognosis analysis in esophageal squamous carcinoma patients
- Efficacy of a novel drainage catheter in the treatment of CSF leak after posterior spine surgery: A retrospective cohort study
- Comprehensive biomedicine assessment of Apteranthes tuberculata extracts: Phytochemical analysis and multifaceted pharmacological evaluation in animal models
- Relation of time in range to severity of coronary artery disease in patients with type 2 diabetes: A cross-sectional study
- Dopamine attenuates ethanol-induced neuronal apoptosis by stimulating electrical activity in the developing rat retina
- Correlation between albumin levels during the third trimester and the risk of postpartum levator ani muscle rupture
- Factors associated with maternal attention and distraction during breastfeeding and childcare: A cross-sectional study in the west of Iran
- Mechanisms of hesperetin in treating metabolic dysfunction-associated steatosis liver disease via network pharmacology and in vitro experiments
- The law on oncological oblivion in the Italian and European context: How to best uphold the cancer patients’ rights to privacy and self-determination?
- The prognostic value of the neutrophil-to-lymphocyte ratio, platelet-to-lymphocyte ratio, and prognostic nutritional index for survival in patients with colorectal cancer
- Factors affecting the measurements of peripheral oxygen saturation values in healthy young adults
- Comparison and correlations between findings of hysteroscopy and vaginal color Doppler ultrasonography for detection of uterine abnormalities in patients with recurrent implantation failure
- The effects of different types of RAGT on balance function in stroke patients with low levels of independent walking in a convalescent rehabilitation hospital
- Causal relationship between asthma and ankylosing spondylitis: A bidirectional two-sample univariable and multivariable Mendelian randomization study
- Correlations of health literacy with individuals’ understanding and use of medications in Southern Taiwan
- Correlation of serum calprotectin with outcome of acute cerebral infarction
- Comparison of computed tomography and guided bronchoscopy in the diagnosis of pulmonary nodules: A systematic review and meta-analysis
- Curdione protects vascular endothelial cells and atherosclerosis via the regulation of DNMT1-mediated ERBB4 promoter methylation
- The identification of novel missense variant in ChAT gene in a patient with gestational diabetes denotes plausible genetic association
- Molecular genotyping of multi-system rare blood types in foreign blood donors based on DNA sequencing and its clinical significance
- Exploring the role of succinyl carnitine in the association between CD39⁺ CD4⁺ T cell and ulcerative colitis: A Mendelian randomization study
- Dexmedetomidine suppresses microglial activation in postoperative cognitive dysfunction via the mmu-miRNA-125/TRAF6 signaling axis
- Analysis of serum metabolomics in patients with different types of chronic heart failure
- Diagnostic value of hematological parameters in the early diagnosis of acute cholecystitis
- Pachymaran alleviates fat accumulation, hepatocyte degeneration, and injury in mice with nonalcoholic fatty liver disease
- Decrease in CD4 and CD8 lymphocytes are predictors of severe clinical picture and unfavorable outcome of the disease in patients with COVID-19
- METTL3 blocked the progression of diabetic retinopathy through m6A-modified SOX2
- The predictive significance of anti-RO-52 antibody in patients with interstitial pneumonia after treatment of malignant tumors
- Exploring cerebrospinal fluid metabolites, cognitive function, and brain atrophy: Insights from Mendelian randomization
- Development and validation of potential molecular subtypes and signatures of ocular sarcoidosis based on autophagy-related gene analysis
- Widespread venous thrombosis: Unveiling a complex case of Behçet’s disease with a literature perspective
- Uterine fibroid embolization: An analysis of clinical outcomes and impact on patients’ quality of life
- Discovery of lipid metabolism-related diagnostic biomarkers and construction of diagnostic model in steroid-induced osteonecrosis of femoral head
- Serum-derived exomiR-188-3p is a promising novel biomarker for early-stage ovarian cancer
- Enhancing chronic back pain management: A comparative study of ultrasound–MRI fusion guidance for paravertebral nerve block
- Peptide CCAT1-70aa promotes hepatocellular carcinoma proliferation and invasion via the MAPK/ERK pathway
- Electroacupuncture-induced reduction of myocardial ischemia–reperfusion injury via FTO-dependent m6A methylation modulation
- Hemorrhoids and cardiovascular disease: A bidirectional Mendelian randomization study
- Cell-free adipose extract inhibits hypertrophic scar formation through collagen remodeling and antiangiogenesis
- HALP score in Demodex blepharitis: A case–control study
- Assessment of SOX2 performance as a marker for circulating cancer stem-like cells (CCSCs) identification in advanced breast cancer patients using CytoTrack system
- Risk and prognosis for brain metastasis in primary metastatic cervical cancer patients: A population-based study
- Comparison of the two intestinal anastomosis methods in pediatric patients
- Factors influencing hematological toxicity and adverse effects of perioperative hyperthermic intraperitoneal vs intraperitoneal chemotherapy in gastrointestinal cancer
- Endotoxin tolerance inhibits NLRP3 inflammasome activation in macrophages of septic mice by restoring autophagic flux through TRIM26
- Lateral transperitoneal laparoscopic adrenalectomy: A single-centre experience of 21 procedures
- Petunidin attenuates lipopolysaccharide-induced retinal microglia inflammatory response in diabetic retinopathy by targeting OGT/NF-κB/LCN2 axis
- Procalcitonin and C-reactive protein as biomarkers for diagnosing and assessing the severity of acute cholecystitis
- Factors determining the number of sessions in successful extracorporeal shock wave lithotripsy patients
- Development of a nomogram for predicting cancer-specific survival in patients with renal pelvic cancer following surgery
- Inhibition of ATG7 promotes orthodontic tooth movement by regulating the RANKL/OPG ratio under compression force
- A machine learning-based prognostic model integrating mRNA stemness index, hypoxia, and glycolysis‑related biomarkers for colorectal cancer
- Glutathione attenuates sepsis-associated encephalopathy via dual modulation of NF-κB and PKA/CREB pathways
- FAHD1 prevents neuronal ferroptosis by modulating R-loop and the cGAS–STING pathway
- Association of placenta weight and morphology with term low birth weight: A case–control study
- Investigation of the pathogenic variants induced Sjogren’s syndrome in Turkish population
- Nucleotide metabolic abnormalities in post-COVID-19 condition and type 2 diabetes mellitus patients and their association with endocrine dysfunction
- TGF-β–Smad2/3 signaling in high-altitude pulmonary hypertension in rats: Role and mechanisms via macrophage M2 polarization
- Ultrasound-guided unilateral versus bilateral erector spinae plane block for postoperative analgesia of patients undergoing laparoscopic cholecystectomy
- Profiling gut microbiome dynamics in subacute thyroiditis: Implications for pathogenesis, diagnosis, and treatment
- Delta neutrophil index, CRP/albumin ratio, procalcitonin, immature granulocytes, and HALP score in acute appendicitis: Best performing biomarker?
- Anticancer activity mechanism of novelly synthesized and characterized benzofuran ring-linked 3-nitrophenyl chalcone derivative on colon cancer cells
- H2valdien3 arrests the cell cycle and induces apoptosis of gastric cancer
- Prognostic relevance of PRSS2 and its immune correlates in papillary thyroid carcinoma
- Association of SGLT2 inhibition with psychiatric disorders: A Mendelian randomization study
- Motivational interviewing for alcohol use reduction in Thai patients
- Luteolin alleviates oxygen-glucose deprivation/reoxygenation-induced neuron injury by regulating NLRP3/IL-1β signaling
- Polyphyllin II inhibits thyroid cancer cell growth by simultaneously inhibiting glycolysis and oxidative phosphorylation
- Relationship between the expression of copper death promoting factor SLC31A1 in papillary thyroid carcinoma and clinicopathological indicators and prognosis
- CSF2 polarized neutrophils and invaded renal cancer cells in vitro influence
- Proton pump inhibitors-induced thrombocytopenia: A systematic literature analysis of case reports
- The current status and influence factors of research ability among community nurses: A sequential qualitative–quantitative study
- OKAIN: A comprehensive oncology knowledge base for the interpretation of clinically actionable alterations
- The relationship between serum CA50, CA242, and SAA levels and clinical pathological characteristics and prognosis in patients with pancreatic cancer
- Identification and external validation of a prognostic signature based on hypoxia–glycolysis-related genes for kidney renal clear cell carcinoma
- Engineered RBC-derived nanovesicles functionalized with tumor-targeting ligands: A comparative study on breast cancer targeting efficiency and biocompatibility
- Relationship of resting echocardiography combined with serum micronutrients to the severity of low-gradient severe aortic stenosis
- Effect of vibration on pain during subcutaneous heparin injection: A randomized, single-blind, placebo-controlled trial
- The diagnostic performance of machine learning-based FFRCT for coronary artery disease: A meta-analysis
- Comparing biofeedback device vs diaphragmatic breathing for bloating relief: A randomized controlled trial
- Serum uric acid to albumin ratio and C-reactive protein as predictive biomarkers for chronic total occlusion and coronary collateral circulation quality
- Multiple organ scoring systems for predicting in-hospital mortality of sepsis patients in the intensive care unit
- Single-cell RNA sequencing data analysis of the inner ear in gentamicin-treated mice via intraperitoneal injection
- Suppression of cathepsin B attenuates myocardial injury via limiting cardiomyocyte apoptosis
- Influence of sevoflurane combined with propofol anesthesia on the anesthesia effect and adverse reactions in children with acute appendicitis
- Identification of hub genes related to acute kidney injury caused by sevoflurane anesthesia and endoplasmic reticulum stress
- Efficacy and safety of PD-1/PD-L1 inhibitors in pancreatic ductal adenocarcinoma: a systematic review and Meta-analysis of randomized controlled trials
- The value of diagnostic experience in O-RADS MRI score for ovarian-adnexal lesions
- Health education pathway for individuals with temporary enterostomies using patient journey mapping
- Serum TLR8 as a potential diagnostic biomarker of coronary heart disease
- Intraoperative temperature management and its effect on surgical outcomes in elderly patients undergoing lichtenstein unilateral inguinal hernia repair
- Immunohistochemical profiling and neuroepithelial heterogeneity in immature ovarian teratomas: a retrospective digital pathology-based study
- Associated risk factors and prevalence of human papillomavirus infection among females visiting tertiary care hospital: a cross-sectional study from Nepal
- Comparative evaluation of various disc elution methods for the detection of colistin-resistant gram-negative bacteria
- Effect of timing of cholecystectomy on weight loss after sleeve gastrectomy in morbidly obese individuals with cholelithiasis: a retrospective cohort study
- Causal association between ceramide levels and central precocious puberty: a mendelian randomization study
- Novel predictive model for colorectal liver metastases recurrence: a radiomics and clinical data approach
- Relationship between resident physicians’ perceived professional value and exposure to violence
- Multiple sclerosis and type 1 diabetes: a Mendelian randomization study of European ancestry
- Rapid pathogen identification in peritoneal dialysis effluent by MALDI-TOF MS following blood culture enrichment
- Comparison of open and percutaneous A1 pulley release in pediatric trigger thumb: a retrospective cohort study
- Impact of combined diaphragm-lung ultrasound assessment on postoperative respiratory function in patients under general anesthesia recovery
- Development and internal validation of a nomogram for predicting short-term prognosis in ICU patients with acute pyelonephritis
- The association between hypoxic burden and blood pressure in patients with obstructive sleep apnea
- Promotion of asthenozoospermia by C9orf72 through suppression of spermatogonia activity via fructose metabolism and mitophagy
- Review Articles
- The effects of enhanced external counter-pulsation on post-acute sequelae of COVID-19: A narrative review
- Diabetes-related cognitive impairment: Mechanisms, symptoms, and treatments
- Microscopic changes and gross morphology of placenta in women affected by gestational diabetes mellitus in dietary treatment: A systematic review
- Review of mechanisms and frontier applications in IL-17A-induced hypertension
- Research progress on the correlation between islet amyloid peptides and type 2 diabetes mellitus
- The safety and efficacy of BCG combined with mitomycin C compared with BCG monotherapy in patients with non-muscle-invasive bladder cancer: A systematic review and meta-analysis
- The application of augmented reality in robotic general surgery: A mini-review
- The effect of Greek mountain tea extract and wheat germ extract on peripheral blood flow and eicosanoid metabolism in mammals
- Neurogasobiology of migraine: Carbon monoxide, hydrogen sulfide, and nitric oxide as emerging pathophysiological trinacrium relevant to nociception regulation
- Plant polyphenols, terpenes, and terpenoids in oral health
- Laboratory medicine between technological innovation, rights safeguarding, and patient safety: A bioethical perspective
- End-of-life in cancer patients: Medicolegal implications and ethical challenges in Europe
- The maternal factors during pregnancy for intrauterine growth retardation: An umbrella review
- Intra-abdominal hypertension/abdominal compartment syndrome of pediatric patients in critical care settings
- PI3K/Akt pathway and neuroinflammation in sepsis-associated encephalopathy
- Screening of Group B Streptococcus in pregnancy: A systematic review for the laboratory detection
- Giant borderline ovarian tumours – review of the literature
- Leveraging artificial intelligence for collaborative care planning: Innovations and impacts in shared decision-making – A systematic review
- Cholera epidemiology analysis through the experience of the 1973 Naples epidemic
- Risk factors of frailty/sarcopenia in community older adults: Meta-analysis
- Supplement strategies for infertility in overweight women: Evidence and legal insights
- Scurvy, a not obsolete disorder: Clinical report in eight young children and literature review
- A meta-analysis of the effects of DBS on cognitive function in patients with advanced PD
- Protective role of selenium in sepsis: Mechanisms and potential therapeutic strategies
- Strategies for hyperkalemia management in dialysis patients: A systematic review
- C-reactive protein-to-albumin ratio in peripheral artery disease
- Research progress on autophagy and its roles in sepsis induced organ injury
- Neuronutrition in autism spectrum disorders
- Pumilio 2 in neural development, function, and specific neurological disorders
- Antibiotic prescribing patterns in general dental practice- a scoping review
- Clinical and medico-legal reflections on non-invasive prenatal testing
- Smartphone use and back pain: a narrative review of postural pathologies
- Targeting endothelial oxidative stress in hypertension
- Exploring links between acne and metabolic syndrome: a narrative review
- Case Reports
- Delayed graft function after renal transplantation
- Semaglutide treatment for type 2 diabetes in a patient with chronic myeloid leukemia: A case report and review of the literature
- Diverse electrophysiological demyelinating features in a late-onset glycogen storage disease type IIIa case
- Giant right atrial hemangioma presenting with ascites: A case report
- Laser excision of a large granular cell tumor of the vocal cord with subglottic extension: A case report
- EsoFLIP-assisted dilation for dysphagia in systemic sclerosis: Highlighting the role of multimodal esophageal evaluation
- Molecular hydrogen-rhodiola as an adjuvant therapy for ischemic stroke in internal carotid artery occlusion: A case report
- Coronary artery anomalies: A case of the “malignant” left coronary artery and its surgical management
- Combined VAT and retroperitoneoscopy for pleural empyema due to nephro-pleuric fistula in xanthogranulomatous pyelonephritis
- A rare case of Opalski syndrome with a suspected multiple sclerosis etiology
- Newly diagnosed B-cell acute lymphoblastic leukemia demonstrating localized bone marrow infiltration exclusively in the lower extremities
- Rapid Communication
- Biological properties of valve materials using RGD and EC
-
A single oral administration of flavanols enhances short
-term memory in mice along with increased brain-derived neurotrophic factor - Repeat influenza incidence across two consecutive influenza seasons
- Letter to the Editor
- Role of enhanced external counterpulsation in long COVID
- Expression of Concern
- Expression of concern “A ceRNA network mediated by LINC00475 in papillary thyroid carcinoma”
- Expression of concern “Notoginsenoside R1 alleviates spinal cord injury through the miR-301a/KLF7 axis to activate Wnt/β-catenin pathway”
- Expression of concern “circ_0020123 promotes cell proliferation and migration in lung adenocarcinoma via PDZD8”
- Corrigendum
- Corrigendum to “Empagliflozin improves aortic injury in obese mice by regulating fatty acid metabolism”
- Corrigendum to “Comparing the therapeutic efficacy of endoscopic minimally invasive surgery and traditional surgery for early-stage breast cancer: A meta-analysis”
- Corrigendum to “The progress of autoimmune hepatitis research and future challenges”
- Retraction
- Retraction of “miR-654-5p promotes gastric cancer progression via the GPRIN1/NF-κB pathway”
- Retraction of: “LncRNA CASC15 inhibition relieves renal fibrosis in diabetic nephropathy through downregulating SP-A by sponging to miR-424”
- Retraction of: “SCARA5 inhibits oral squamous cell carcinoma via inactivating the STAT3 and PI3K/AKT signaling pathways”
- Special Issue Advancements in oncology: bridging clinical and experimental research - Part II
- Unveiling novel biomarkers for platinum chemoresistance in ovarian cancer
- Lathyrol affects the expression of AR and PSA and inhibits the malignant behavior of RCC cells
- The era of increasing cancer survivorship: Trends in fertility preservation, medico-legal implications, and ethical challenges
- Bone scintigraphy and positron emission tomography in the early diagnosis of MRONJ
- Meta-analysis of clinical efficacy and safety of immunotherapy combined with chemotherapy in non-small cell lung cancer
- Special Issue Computational Intelligence Methodologies Meets Recurrent Cancers - Part IV
- Exploration of mRNA-modifying METTL3 oncogene as momentous prognostic biomarker responsible for colorectal cancer development
- Special Issue The evolving saga of RNAs from bench to bedside - Part III
- Interaction and verification of ferroptosis-related RNAs Rela and Stat3 in promoting sepsis-associated acute kidney injury
- The mRNA MOXD1: Link to oxidative stress and prognostic significance in gastric cancer
- Special Issue Exploring the biological mechanism of human diseases based on MultiOmics Technology - Part II
- Dynamic changes in lactate-related genes in microglia and their role in immune cell interactions after ischemic stroke
- A prognostic model correlated with fatty acid metabolism in Ewing’s sarcoma based on bioinformatics analysis
- Red cell distribution width predicts early kidney injury: A NHANES cross-sectional study
- Special Issue Diabetes mellitus: pathophysiology, complications & treatment
- Nutritional risk assessment and nutritional support in children with congenital diabetes during surgery
- Correlation of the differential expressions of RANK, RANKL, and OPG with obesity in the elderly population in Xinjiang
- A discussion on the application of fluorescence micro-optical sectioning tomography in the research of cognitive dysfunction in diabetes
- A review of brain research on T2DM-related cognitive dysfunction
- Metformin and estrogen modulation in LABC with T2DM: A 36-month randomized trial
- Special Issue Innovative Biomarker Discovery and Precision Medicine in Cancer Diagnostics
- CircASH1L-mediated tumor progression in triple-negative breast cancer: PI3K/AKT pathway mechanisms

