Abstract
Introduction
Giant borderline ovarian tumours (GBOTs) are rare neoplasms that require meticulous management to prevent high-risk operative complications. The broader goal of this systematic review is to consolidate the existing knowledge on GBOTs by focusing on diagnostic approaches, differential diagnoses, and treatment strategies. Furthermore, the relationship between the clinical features of GBOTs and the types of diagnostic and therapeutic procedures implemented was determined.
Materials and methods
The publications were analysed for the following data: histopathological type of GBOT; patient’s age; dimensions, weight, and/or volume of the tumour; levels and types of tumour markers determined; types of imaging tests performed; type of treatment applied.
Results
Twenty-one articles describing the clinical situation of 22 patients met the inclusion criteria for the systematic review. The mean age of the patients included in the analysis was 46.68 years (SD: 19.1 years); the youngest patient was 12, and the oldest was 76 years of age. In the analysed literature, patients most often (81.8%) had the mucinous type of GBOT. In the vast majority of cases (86.36%), based on the analysed literature, the surgical treatment method for the patients was laparotomy. In more than half of the patients (54.55%), the uterus was removed during surgical treatment. In the analysed literature, the hysterectomy procedure was not performed in patients under 40 years of age. Based on the analysed literature, it was found that if the CA 125 concentration in the blood serum of patients with mucosal tumours exceeded 40 U/mL, laparoscopy was not performed and the patients were treated using an open approach.
Conclusions
GBOTs are rare neoplasms that require meticulous management to prevent high-risk operative complications. Despite the diagnostic and therapeutic challenges posed by the large size and potential complications of these tumours, with proper medical care, patients can achieve successful outcomes and a good prognosis.
1 Introduction
In an era of growing popularity of minimally invasive techniques in surgical gynaecology, giant borderline ovarian tumours (GBOTs) remain a niche in which classical surgical skills will undoubtedly remain essential. GBOTs are defined as ovarian masses of at least 20 cm in diameter. These tumours are relatively rare in the existing medical literature and present with a wide range of clinical manifestations [1]. BOTs typically occur in women who are about a decade younger than those diagnosed with epithelial ovarian cancer, with the majority of cases (approximately 75%) being detected at an early stage, particularly stage I, according to the International Federation of Gynaecology and Obstetrics (FIGO) [2]. GBOTs are characterised by slow growth and carry the potential to transform into malignant ovarian tumours [3]. Their large size and associated complications present unique diagnostic and therapeutic challenges, although advancements in imaging and healthcare have made the occurrence of such massive tumours increasingly rare [4]. The symptoms of GBOTs are similar to those of other ovarian tumours, including abdominal pain, bloating, and irregular menstrual cycles. Additionally, compressive symptoms or a visible abdominal mass is commonly observed [2]. Due to their size, these tumours can cause significant discomfort and hinder daily activities. The primary diagnostic tools are imaging techniques such as ultrasound (USG), computed tomography (CT), or magnetic resonance imaging (MRI). Diagnostics also include the evaluation of tumour markers. Surgical treatment generally consists of laparotomy with varying extents of organ removal, depending on the individual case [1].
The aim of this systematic review is to compile and evaluate the current knowledge on GBOTs, with particular focus on diagnostic methods, differential diagnosis, and treatment strategies. We emphasise the importance of preoperative assessment and a critical evaluation of surgical options. Although open laparotomy has traditionally been the standard approach – especially given the massive size of these tumours – minimally invasive techniques may be considered in a few carefully selected cases. Consequently, this review explores both the evolving role of laparoscopy and other minimally invasive methods, as well as the full range of surgical interventions available for managing large ovarian masses.
2 Materials and methods
This systematic review was conducted in accordance with the international standards and guidelines for systematic reviews (PRISMA – Preferred Reporting Items for Systematic Reviews and Meta-Analyses). The PRISMA 2020 checklist was applied in this study. A detailed review protocol is available from the author upon request. The review included publications from databases such as PubMed, Google Scholar, Scopus, and EBM Reviews (including the Cochrane Database of Systematic Reviews), covering articles published between 2000 and 2024. To increase precision, we incorporated Boolean operators (AND/OR) into our search strategy and used a targeted combination of keywords – “giant and borderline,” “borderline malignancy,” “ovarian tumour,” and “ovarian cyst” – to identify eligible studies. To ensure transparency and minimise selection bias, study selection, data extraction, and quality assessment were conducted independently by two reviewers; any disagreements were resolved through discussion and voting on disputed articles. If, following discussion, the reviewers reached unanimous agreement, the publication was included in the analysis. Searches were conducted on August 11, 2024. The Newcastle–Ottawa Scale was implemented to assess the quality of the included studies. The review was limited to publications in English or Polish and excluded repeated items and articles without full-text availability. The inclusion of publications in English and Polish was justified by the authors’ proficiency in these languages, which allowed for a thorough analysis of the content. The initial analysis primarily included peer-reviewed case reports, observational studies, and retrospective analyses. A secondary search entailed examining the reference lists of all the included articles. Certain publication types, such as editorials, comments, conference abstracts, abstracts, validation studies, and animal studies, were excluded from the analysis. Studies were excluded from the review if the diagnosis was other than a borderline tumour; the tumour size was less than 19 cm, weighed less than 1,000 g, or had a volume less than 500 mL; or the clinical data or results of the pathological examination were not reported. The inclusion and exclusion criteria for this study are summarised in Table 1, and a flow diagram illustrating the study selection process is presented in Figure 1. The publications were analysed for the following data: histopathological type of GBOT; patient’s age; dimensions, weight, and/or volume of the tumour; levels and types of tumour markers determined; types of imaging tests performed; and type of treatment applied.
Inclusion and exclusion criteria for the study
| Inclusion criteria | |
| Type of study | Peer-reviewed: Case reports, case series, and observational studies |
| Years | 2000–2024 |
| Language | English and Polish |
| Subject of study | Live humans |
| Clinical criteria | Borderline ovarian tumour (pathologically confirmed) and reported clinical data |
| Exclusion criteria | |
| Type of study | Editorials, comments, conference abstracts, abstracts, book chapters, and validation studies |
| Language | Other than English and Polish |
| Subject of study | Animals and autopsy |
| Clinical criteria | Size <20 cm or weight <1,000 g or volume <500 mL, not reported: Clinical data or pathological confirmation |
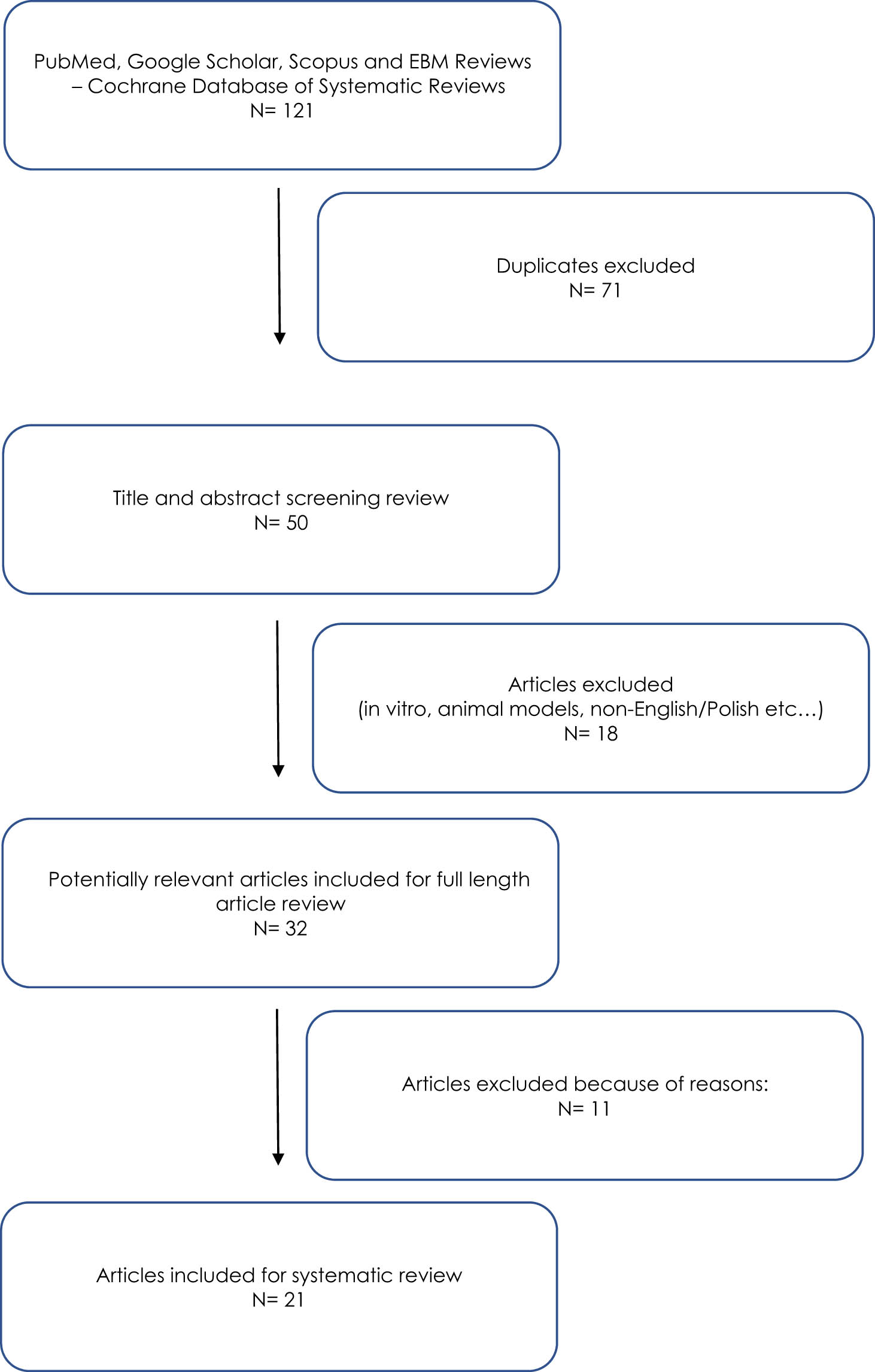
Flow diagram of the study selection process.
Statistical analyses were performed using the PQStat statistical package version 1.8.4.152. The scale results were compared using the Mann–Whitney U test, and a logistic regression model was also estimated. A test probability of p < 0.05 was considered significant, while a value of p < 0.01 was considered highly significant.
3 Results
After the first search of the databases (PubMed, Google Scholar, Scopus, and EBM Reviews, which included the Cochrane Database of Systematic Reviews) for the given keywords, 121 items were obtained. Duplicates were then excluded, leaving 50 publications. After the analysis of the abstracts of the selected publications, 32 items qualified for further analysis. Due to the lack of criteria allowing for qualification for the systematic review, another 11 publications were eliminated. Finally, 21 articles describing the clinical situation of 22 patients met the inclusion criteria for the systematic review. The clinical data obtained from the publications included in the systematic review are summarised in Table 2.
Clinical data obtained from publications included in the systematic review (BOT – borderline ovarian tumour, HA – abdominal hysterectomy, TLH – total laparoscopic hysterectomy, BSO – bilateral salpingo-oophorectomy, USO – unilateral salpingo-oophorectomy, CT – computed tomography, MRI – magnetic resonance imaging, USG – ultrasound examination, CA 125 – cancer antigen 125, CA 19-9 – cancer antigen 19-9, CEA – carcinoembryonic antigen, AFP – α-fetoprotein, ß-hCG – ß-human chorionic gonadotropin, and ND – no data)
| Author | No. of BOT CASES | Histological type of BOT | Max. dimensions/weight/volume | Age | Symptoms | Tumour markers | Diagnostics | Surgical treatment | |
|---|---|---|---|---|---|---|---|---|---|
| 1 | Mikos T | 1 | Mucinous/serous | 35 l | 59 | Dyspnoea abdominal distension | CA 125, 300 U/mL | USG and CT | Laparotomy and HA + BSO |
| 2 | Iwasaki M | 1 | Mucinous | 21 × 15.5 × 7 cm/1,120 g | 13 | Abdominal pain, abdominal distension, abdominal girth, and fever | CA 125, 184.0 U/mL; CA 19-9, 330.0 U/mL | USG and CT | Laparotomy, USO, and appendectomy |
| 3 | Cîrstoiu MM | 1 | Mucinous | 59 × 48 × 32 cm/30 kg | 44 | Abdominal pain, abdominal distension, constipation, and early satiety | CA 125, CA 19-9, CEA, and AFP – normal values | USG and CT | Laparotomy and HA + BSO |
| 4 | Lee HM | 1 | Mucinous | 19 × 15 × 8.5 cm/1,584 g | 13 | Abdominal distension | CA 125, 284 U/mL; CA 19-9, 2,581 U/mL | PET/CT | Laparotomy, unilateral USO, appendectomy, and omentectomy |
| 5 | Dougherty D | 1 | Mucinous/Brenner | 40 × 22 × 27 cm | 57 | Abdominal discomfort | CA 125, 249.4 U/mL; CEA, 6.1 ng/mL | CT | Laparotomy and HA + BSO |
| 6 | Pilone V | 1 | Mucinous | 60 × 50 × 40 cm/6,500 g (solid part) | 69 | Abdominal distension | CA 125, CEA, AFP, and CA 19-9 – normal values | CT | Laparotomy, HA + BSO, and partial omentectomy |
| 7 | Watanabe S | 1 | Mucinous | 42 × 22 × 20 cm/11,800 g | 12 | Abdominal distention and abdominal girth | CA 125, 96.3 U/mL; CEA, 117.5 ng/mL; AFP, 0.7 ng/mL; CA 19-9, 5029.0 U/mL; ß-hCG <0.003 units/mL | USG, MRI, and X-ray | Laparotomy and USO |
| 8 | Yazawa H | 1 | Endometrioid | 27 × 9 cm | 41 | Abdominal/back pain | CA 125, 150 U/mL; CA 19‐9, 220 IU/mL | MRI | Laparoscopy, TLH + BSO, partial omentectomy, and pelvic lymph node biopsy |
| 9 | Mulita F | 1 | Mucinous | 44 × 39 × 19 cm/15.4 kg | 59 | Abdominal distention, dyspnoea, and difficulty in ambulation | CA 19-9, >953 U/mL | ND | Laparotomy, HA + BSO, omentectomy, and appendectomy |
| 10 | Mitragkas P | 2 | 1. Mucinous; 2. mucinous | 1. 23.5 × 11 × 23.6 cm; 2. 24,7 cm | 1. 45; 2. 54 | 1. Constipation and early satiety; 2. Abdominal bloating and epigastrium pain | 1. All tumour markers were in normal range; 2. All tumour markers were in normal range | 1. USG and CT; 2. USG | 1. Laparotomy and USO; 2. Laparoscopy, TLH + BSO, and omentectomy |
| 11 | Deo A | 1 | Mucinous | 36 × 30 × 18 cm/32.5 kg | 76 | Massive ascites and breathlessness (NYHA III), abdominal distension, abdominal pain, weight loss, and constipation | CA 125, 53 U/mL; CA 19-9, 1,000 U/mL; CEA; ß-HCG; AFP – normal | USG and CT | Laparotomy – HA + BSO, biopsy (vaginal cuff, peritoneum, and omentum) |
| 12 | Halani D | 1 | Mucinous | 35 × 40 × 32 cm/24 kg | 53 | Abdominal pain | CA 125, 53.2 IU/mL; CA 19-9, 1,000 U/mL | CT | Laparotomy and HA + BSO |
| 13 | Yazawa R | 1 | Mucinous | >20 cm | 26 | ND | CA 125, 55.7 U/mL; CA 19-9, 177 U/mL; CEA, 16.6 ng/mL | CT and MRI | Laparotomy, USO, and appendectomy |
| 14 | Peiretti M | 1 | Mucinous | 47 × 36 × 33 cm | 52 | Abdominal distention, reflux, early satiety, constipation, difficulty in ambulation, and dyspnoea | CA 125, 33 U/mL; CEA, 0.97 ng/mL; CA 19-9, 19.2 U/mL; AFP, 1.1 ng/mL | USG and CT | Laparotomy, HA + BSO, intraoperative controlled drainage appendectomy, and abdominal wall reconstruction |
| 15 | Gharbia N | 1 | Mucinous | 27 × 12 × 26 cm | 30 | Abdominal pain and abdominal girth over the past fever | CA 125, 493 U/mL; CA 19-9, 273 U/mL | USG and MRI | Laparotomy, USO, omentectomy, and appendectomy |
| 16 | Onuzo CN | 1 | Mucinous | 50 cm | 24 | Abdominal discomfort | CA 125, 54.3 U/mL | USG and MRI | Laparotomy and USO |
| 17 | Bogliatto F | 1 | Mucinous | 34 cm | 60 | Abdominal pain | CA 125, CEA, AFP, and CA 19-9 – normal levels | USG and CT | Laparoscopy, intraoperative controlled drainage, and BSO |
| 18 | Stukan M | 1 | Mucinous | 50 × 45 × 26 cm | 49 | ND | CA 125, 140.4 U/mL | CT | Laparotomy and HA + BSO |
| 19 | Berbecar VT | 1 | Mucinous | 19 × 19 × 31 cm | 59 | Abdominal discomfort | ND | USG and CT | Laparotomy and USO |
| 20 | Rigo F | 1 | Serous | 26 × 33 × 20 cm/10 kg | 69 | Abdominal distension | CEA, 5.2 ng/mL; CA 19-9, 103 IU/mL; AFP, 0.8 IU/mL | CT | Laparotomy, HA + BSO, and appendectomy |
| 21 | Pence S | 1 | Mucinous | 35 × 25 × 35 cm | 63 | Septic shock | ND | ND | Laparotomy, BSO, and reparation of peptic ulcers |
The mean age of the patients included in the analysis was 46.68 years (SD 19.1 years); the youngest patient was 12 years of age, and the oldest was 76 years of age. In the analysed literature, patients most often (81.8%) had the mucinous type of GBOT. Moreover, patients up to 40 years of age had only the mucinous type of BOT. The tumours were analysed in terms of the largest dimension; the mean value was 36.16 cm, and the median was 35 cm. Half of the tumours were in the range of 27–44 cm, while the total range of results was 19–60 cm. The relationship between the maximum tumour size and age was examined, but no statistically significant relationship was found. In the analysed publications, the average tumour weight was 14,767 g, and the median was 11,800 g; the lightest tumour weighed was 1,120 g, and the heaviest was 32,500 g. All tumours in the cases analysed were limited to a single ovary. The average CA 125 level in the blood was 126.9 U/mL, with a median of 55 U/mL, and values ranged from 25 to 493 U/mL. We also looked at how CA 125 is related to age and found a nearly significant pattern (p = 0.0546): we observed a trend toward higher average and median CA 125 levels in patients ≤40 years (p = 0.0546) (Table 3). Based on the analysed literature, it was found that if the CA 125 concentration in the blood serum of patients with mucinous borderline tumours exceeded 40 U/mL, laparoscopy was not performed, and the patients were treated using an open approach. In the vast majority of cases (86.36%), based on the analysed literature, the surgical treatment method for the patients was laparotomy. In more than half of the patients (54.55%), the uterus was removed during surgical treatment. In the analysed literature, the hysterectomy procedure was not performed in patients under 40 years of age.
Relationship between the CA 125 concentration in blood serum and age; a relationship close to statistical significance was found (p = 0.0546) (SD – standard deviation, Q1 – first quartile, and Q3 – third quartile)
| CA 125 (U/mL) | |||
|---|---|---|---|
| ≤40 (years) | >40 (years) | ||
| Mean | 194.55 | 93.0833 | |
| SD | 170.7556 | 95.8221 | |
| Median | 140.15 | 43 | |
| Minimum | 54.3 | 25 | |
| Maximum | 493 | 300 | |
| Q1 | 65.85 | 29.5 | |
| Q3 | 259 | 142.8 | |
| Mann–Whitney U test | Z | 1.9220 | |
| p | 0.0546 | ||
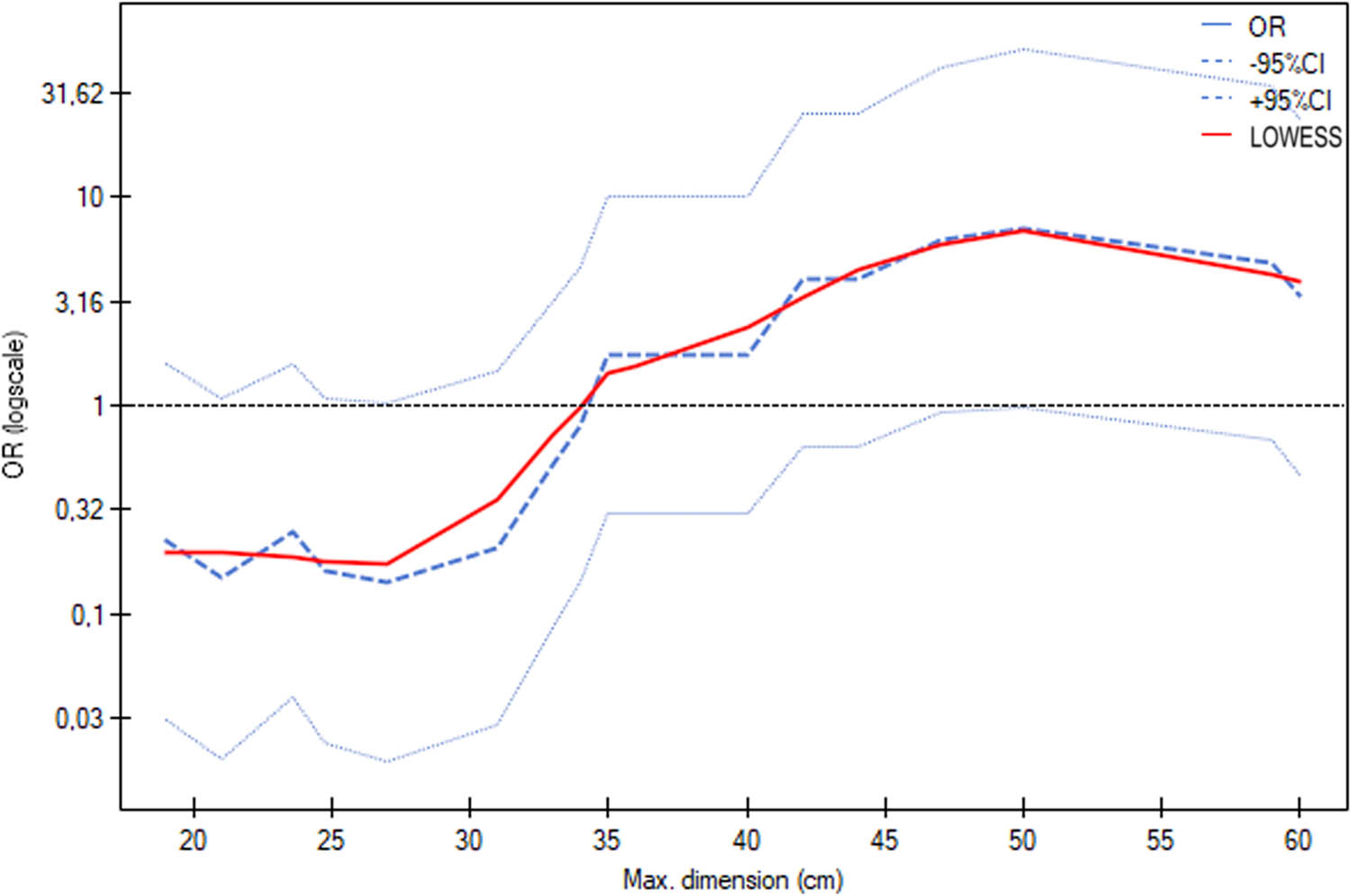
The relationship between age and the decision to perform hysterectomy was also examined, and in older patients, hysterectomy was statistically significantly more often performed (p = 0.0375) (Table 4 and Figure 2). The logistic regression model for the prediction of hysterectomy by age indicated a significant effect of age, as the odds ratio was 1.0923, with a 95% confidence interval from 1.0127 to 1.1781 (p = 0.0222). This means that each additional year of age was associated with a higher probability of undergoing hysterectomy, confirming a statistically significant effect of age (Figure 3). In five instances, fertility-sparing treatment was chosen due to the patient’s age. Appendectomy was performed in seven cases. The reviewed literature mostly did not report the duration of surgery or intraoperative blood loss.
Age in the group of the patients with and without hysterectomy
| Age (years) | |||
|---|---|---|---|
| Without hysterectomy | With hysterectomy | ||
| Mean | 34.5 | 56.8333 | |
| SD | 20.5656 | 10.4258 | |
| Median | 28 | 55.5 | |
| Minimum | 12 | 41 | |
| Maximum | 63 | 76 | |
| Q1 | 15.75 | 51.25 | |
| Q3 | 55.5 | 61.5 | |
| Mann–Whitney U test | Z | 2.0806 | |
| p | 0.0375 | ||
(SD – standard deviation, Q1 – first quartile, and Q3 – third quartile).
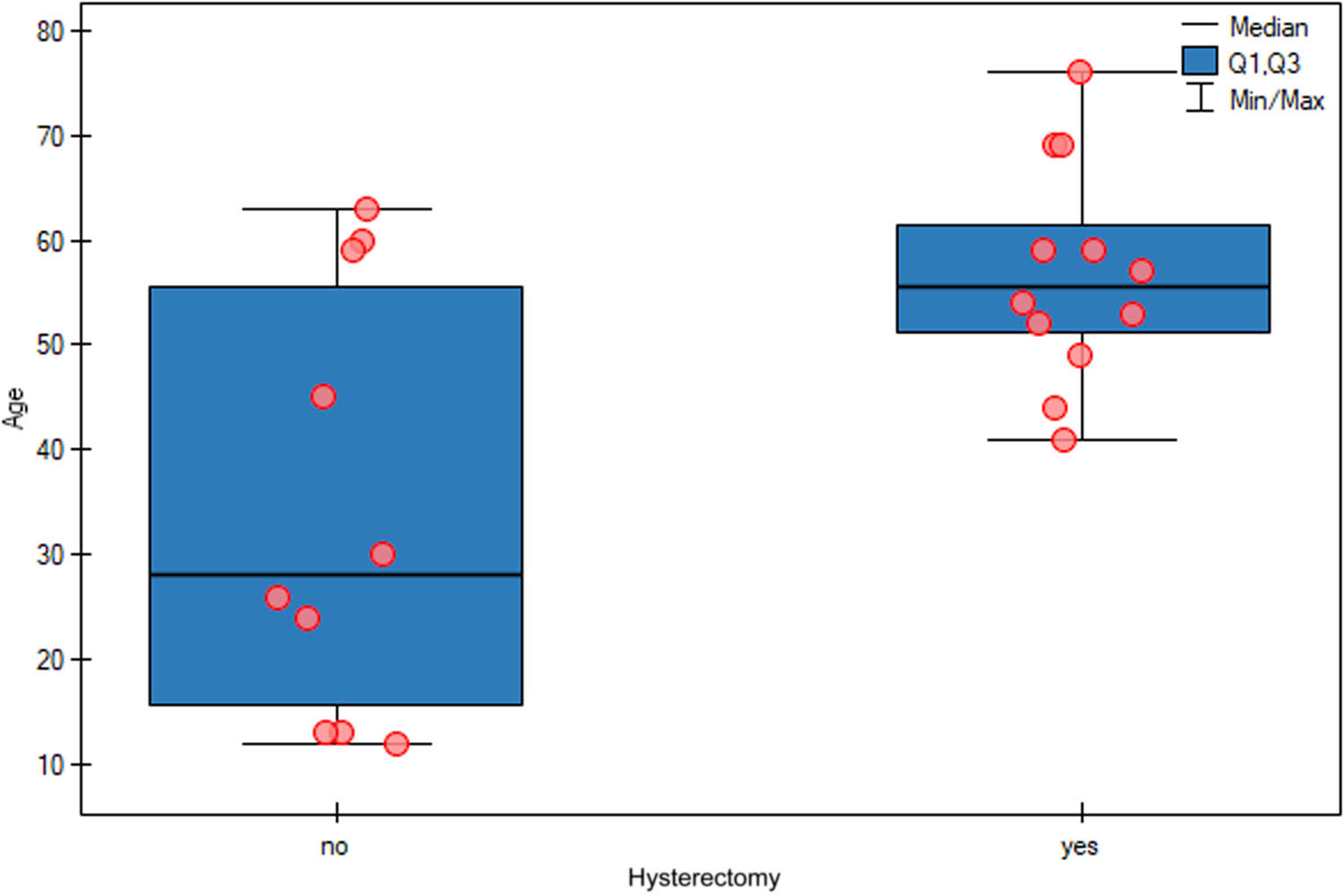
Relationship between age and the decision to perform hysterectomy. In older patients, hysterectomy was statistically significantly more often performed (p = 0.0375).

Logistic regression model of the prediction of hysterectomy by age indicates a significant effect of age, as the odds ratio is 1.0923 with a 95% confidence interval from 1.0127 to 1.1781 (p = 0.0222).
The relationship between the maximum tumour size and the decision to perform hysterectomy was also examined, and patients with larger tumours were statistically significantly more likely to undergo hysterectomy (p = 0.0344) (Table 5 and Figure 4). The logistic regression model for the prediction of hysterectomy based on the maximum tumour size did not indicate a significant effect of tumour size; however, the results were close to statistical significance, as the odds ratio was 1.1019, with a 95% confidence interval of 0.9987–1.2157 (p = 0.0530) (Figure 5).
Maximum tumour size in the group of patients with and without hysterectomy
| Maximum tumour size (cm) | |||
|---|---|---|---|
| Without hysterectomy | With hysterectomy | ||
| Mean | 30.36 | 41.4273 | |
| SD | 10.0977 | 11.8181 | |
| Median | 29 | 40 | |
| Minimum | 19 | 24.7 | |
| Maximum | 50 | 60 | |
| Q1 | 21.65 | 34 | |
| Q3 | 34.75 | 48.5 | |
| Mann–Whitney U test | Z | 2.1153 | |
| p | 0.0344 | ||
(SD – standard deviation, Q1 – first quartile, and Q3 – third quartile).
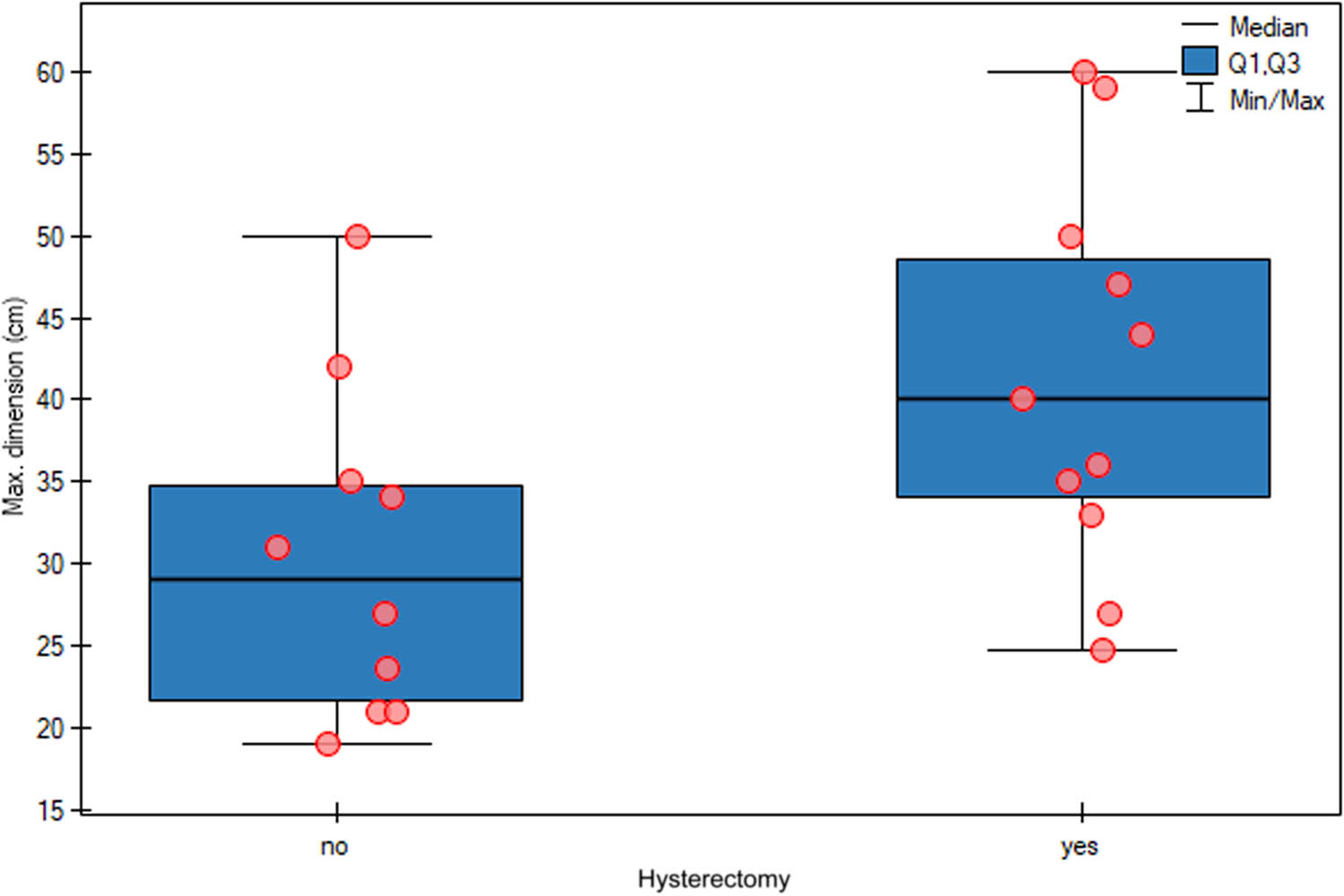
Relationship between the maximum tumour size and the decision to perform hysterectomy. Patients with larger tumours were statistically significantly more likely to undergo hysterectomy (p = 0.0344).
Logistic regression model for the prediction of hysterectomy based on the maximum tumour size does not indicate a significant effect of tumour size; however, the results are close to statistical significance as the odds ratio is 1.1019 with a 95% confidence interval of 0.9987 to 1.2157 (p = 0.0530).
Given the limited sample and borderline statistical significance for key predictors, our logistic regression findings should be interpreted as exploratory. They highlight potential associations worthy of further study but require confirmation in larger, more robust datasets.
4 Discussion
In this review, we found that GBOTs were primarily unilateral and mucinous in nature and most often managed via laparotomy. Elevated CA 125 levels were more commonly seen in patients aged 40 or younger, while the likelihood of hysterectomy increased significantly in older women and those with larger tumours. Fertility-sparing surgeries were employed relatively infrequently. Below, we present the key findings from our review in the context of selected literature sources.
Advancements in imaging technologies and the routine implementation of screenings have greatly enhanced the early detection of ovarian masses, as they have allowed for the identification of these tumours, while they are still asymptomatic and relatively small [5]. However, in rare cases, ovarian masses may remain undetected and grow significantly, often due to limitations of transvaginal USG, patient obesity, or restricted access to medical care. There is currently no universally accepted definition for categorising large or giant ovarian tumours; generally, a GBOT is defined as an ovarian mass with a diameter of at least 20 cm (Figure 6) [6].
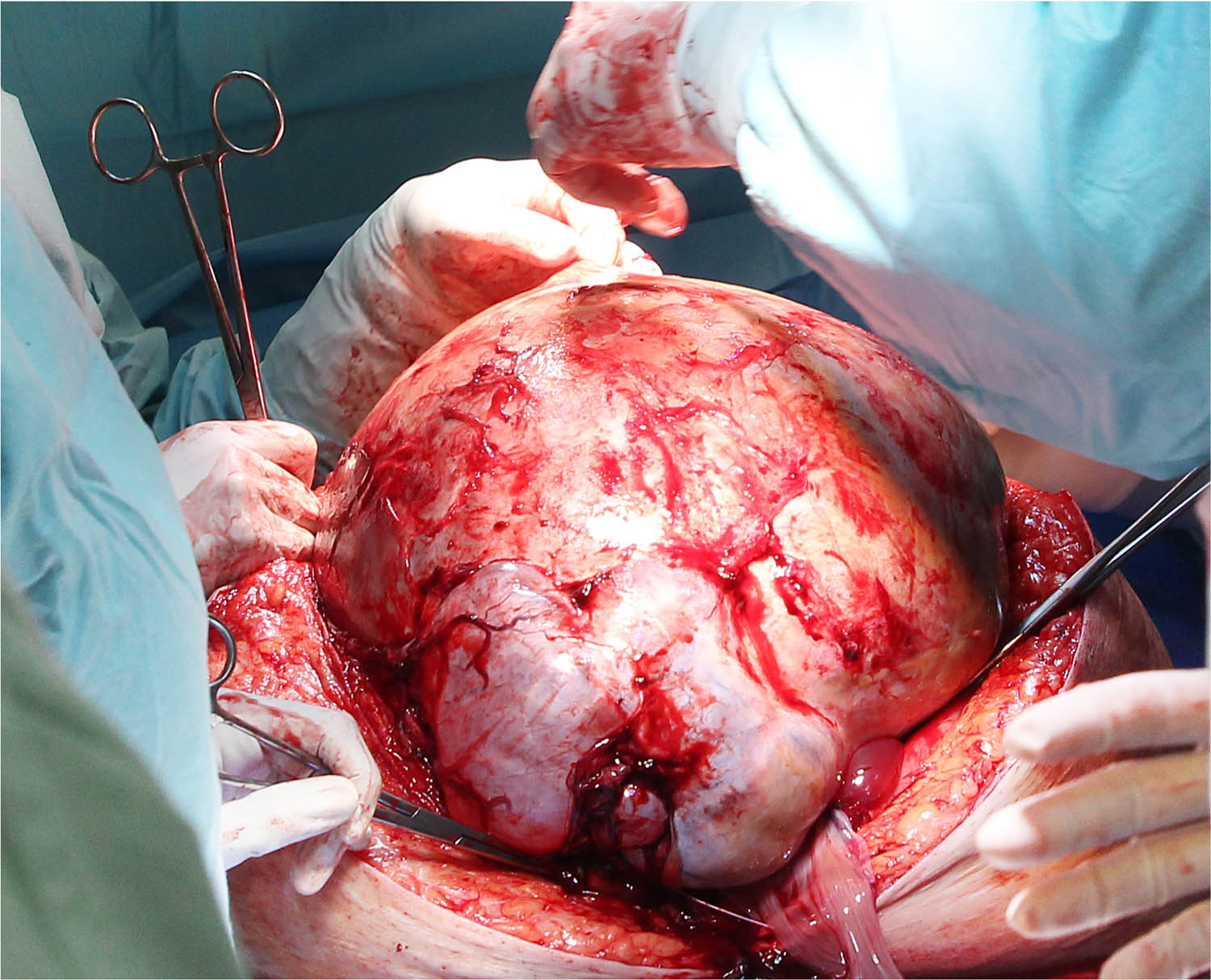
GBOT is defined as an ovarian mass with a diameter of at least 20 cm. Operative field view: A midline incision from the pubic symphysis to the xiphoid process, allowing for the safe exteriorisation of a giant ovarian tumour.
Mucinous tumours are typically unilateral, with bilateral cases occurring in only about 5% of the instances [7]. In the literature we analysed, all tumours were located in one of the ovaries, their average maximum dimension was 35 cm, and in terms of histopathology, the dominant type was mucinous. Ovarian cystic masses containing more than 10% borderline architecture are classified as BOTs; among these, mucinous BOTs (mBOTs) account for 45% of the cases [8]. Mucinous cystadenomas can grow into large masses and often remain undiagnosed until they reach giant sizes, typically being incidentally discovered during routine physical examinations or sonograms. Mucinous tumours are classified as benign (75%), borderline (10%), or malignant (15%); if left untreated, these tumours have the potential to progress into invasive mucinous carcinoma [1,9,10].
Based on our literature analysis, the most frequently reported symptoms in GBOTs include bloating, abdominal distension, fatigue, urinary symptoms, and pelvic or abdominal discomfort [11]. Gastrointestinal manifestations – such as abdominal pain, pressure, flatulence, and even constipation or diarrhoea – were also commonly documented, along with shortness of breath, particularly upon lying down or moving [12,13].
Diagnostics of GBOTs relies on a combination of clinical examination and advanced imaging modalities. Physical and pelvic examination may initially raise suspicion when a large adnexal mass is palpated, but definitive characterisation necessitates imaging. Transvaginal and abdominal USG serve as first-line tools: it excels at assessing lesion morphology, cystic versus solid components, septations, and distinguishing masses from ascites, thanks to its accessibility. However, its diagnostic accuracy is moderate – sensitivity around 77% and specificity roughly 83% for differentiating BOTs from benign lesions [14,15,16,17,18,19] – and limited by depth penetration in cases of giant masses. Consequently, computed tomography (CT) and magnetic resonance imaging (MRI) are recommended as supplementary modalities for comprehensive preoperative evaluation. CT provides valuable insights into tumour size, solid component characteristics, and potential metastases or lymphadenopathy and can aid in distinguishing BOTs from invasive epithelial ovarian cancers by analysing specific radiologic features such as small solid areas [15]. MRI offers superior soft-tissue contrast, enabling the detection of subtle intra-cystic nodules and papillary projections typical of borderline pathology, with MRI sensitivity and specificity reaching approximately 85 and 74%, respectively. In rare cases of GBOT, MRI and CT accurately define the lesion extent and adjacent structure involvement, guiding surgical planning [9,20].
When a GBOT is suspected, additional diagnostic tests, including tumour marker evaluations, are often conducted to assess the potential for malignancy. Suspicion of malignancy is primarily based on radiological findings and elevated levels of tumour markers, such as CA 125, human epididymis protein 4 (HE4), cancer antigen 19-9 (CA 19-9), carcinoembryonic antigen (CEA), ß-human chorionic gonadotropin (ß-hCG), α-fetoprotein (AFP), and lactate dehydrogenase [21,22]. The marker that is particularly important for distinguishing mucinous from serous tumours is CA 19-9. In some of the analysed studies, it was measured, and the levels reported in the publications were high; unfortunately, not all articles provided specific values. Another important marker for distinguishing benign from malignant lesions is HE4. When used alongside CA 125 in the risk of ovarian malignancy algorithm, it achieves a sensitivity of approximately 92% and a specificity around 75% in differentiating benign and malignant conditions [16]. In the literature we reviewed on GBOTs, HE4 was not routinely used. CA 125 is widely utilised to differentiate between malignant and benign pelvic masses, particularly in postmenopausal patients, where serum CA 125 levels above 200 U/mL have a 96% positive predictive value for malignancy [23]. However, in premenopausal patients, the specificity of CA 125 is lower due to its elevation in various benign conditions, such as endometriosis, and physiological changes in concentration during the menstrual cycle. In the publications concerning GBOTs included in our analysis, various tumour markers were used to expand preoperative diagnostics. CA 125 was measured in a majority of studies; therefore, we focused on it in our further analysis. We found a relationship close to statistical significance in patients under 40 years of age, as their CA 125 concentrations were higher compared to those in patients over 40 years. In the literature we analysed, no significant correlation between the tumour size and CA 125 levels was observed [11]. CA 125 also has a sensitivity of 50% for early-stage epithelial ovarian cancer. However, HE4 has demonstrated greater sensitivity than CA 125 in distinguishing benign from malignant conditions, making it a more effective biomarker in some cases [24]. Despite these diagnostic tools, the possibility of malignancy or borderline malignancy often remains uncertain until a final pathological diagnosis is made. In the literature we analysed, patients with mBOTs whose serum CA 125 concentrations exceeded the normal values were not qualified for surgery using minimally invasive techniques. Near-significant p-values must be interpreted with caution: in small samples, even moderate effect sizes may yield non-significant results, and conversely chance findings can appear significant. These small, heterogeneous samples greatly limit the external validity of findings and heighten concerns about publication bias, where positive or unusual cases are disproportionately published.
The differential diagnosis for giant ovarian cysts is extensive and covers both benign and malignant conditions of gynaecologic and non-gynaecologic origins. These can include a distended bladder, hydronephrosis, ascites, accentuated obesity, pregnancy, fibroids, and various intra-abdominal and adnexal masses [25,26,27]. Based on the cases we reviewed, the differential diagnosis commonly included benign and malignant lesions, non-epithelial tumours, and free fluid in the peritoneal cavity [28,29,30].
The management of GBOTs depends on several factors, including the patient’s age, menopausal status, fertility desires, nutritional status, access to medical facilities, and the surgeon’s expertise. Tumour size is a critical factor in determining clinical management, with surgical intervention often recommended for tumours larger than 10 cm, particularly when they cause symptoms. In cases where the tumour is particularly large, a staged surgical approach may be necessary. However, the significance of tumour size as a predictor of malignancy in ovarian tumours is still debated.
An examination of the pathological extent of BOTs is essential for appropriate intraoperative decision-making. In such cases, intraoperative frozen section analysis can help differentiate borderline tumours from invasive carcinomas, guiding the extent of surgical resection and fertility-sparing decisions. Although frozen section has moderate accuracy, sampling errors may occur, especially in large or heterogeneous tumours. Therefore, representative sampling of multiple tumour areas is crucial to minimize misdiagnosis [31]. Ultimately, integrating frozen section findings with careful gross inspection and preoperative imaging improves the likelihood of appropriate management of GBOTs.
The basic method of treating a patient with a GBOT is surgical treatment by laparotomy. This method allows for oncologically safe dissection of the tumour and its removal from the patient’s peritoneal cavity. Surgical treatment is determined based on the clinical stage of the tumour and the fertility plans of the patient. In patients with tumours confined to the ovary, corresponding to FIGO stage I, two surgical options are possible: hysterectomy with bilateral salpingo-oophorectomy can be performed if preservation of fertility is not a problem. However, if the patient wishes to preserve fertility, unilateral salpingo-oophorectomy can also be performed, leaving the ovary and uterus intact [2]. Uterine-sparing surgery in BOT patients is associated with a higher risk of recurrence, though studies show it does not increase the risk of death due to disease or death from any cause. Therefore, while uterine preservation may be considered to maintain fertility or avoid more complex surgery, women must be advised that it carries a greater likelihood of recurrence without compromising long-term survival [32]. A bilateral ovarian tumour, especially in women of childbearing age who wish to preserve fertility, presents a significant surgical challenge. In such cases, a successful two-step approach has been described in the literature, enabling accurate diagnosis of bilateral BOTs with peritoneal implants, fertility-sparing surgery, and preoperative oocyte retrieval with cryopreservation before cytoreductive intervention [33]. In the reviewed literature, more than half of the patients with GBOT underwent hysterectomy during surgery, a procedure significantly more common in those over 40 years of age and in cases with larger tumours. Moreover, hysterectomy was not performed in patients under 40 years of age.
A critical aspect of surgical treatment for malignant tumours and BOTs is ensuring complete removal of the lesion while avoiding rupture of the tumour capsule during surgery. Intraoperative rupture can lead to the intraperitoneal spread of tumour contents, which can increase the risk of disease progression and recurrence [34]. For open surgeries, it is crucial to make a sufficiently large incision and carefully free the lesion from adhesions. Adequate staging of BOTs requires meticulous inspection of the peritoneum and multiple peritoneal biopsies, while appendectomy – even in mucinous subtypes – is unnecessary unless the appendix appears macroscopically abnormal [35]. There is no supporting evidence for routine lymph node dissection in BOTs, and omission of comprehensive staging is linked to higher recurrence rates, though complete staging has not clearly demonstrated an overall survival benefit for FIGO stage I disease [36]. As hysterectomy appears to not impact survival outcomes of women with BOT, it might be avoided in the surgical staging [37].
Restaging surgery may only be justified for patients at elevated risk – such as those with serous tumours showing micropapillary features or when initial abdominal and pelvic exploration was incomplete – due to the associated morbidity and uncertain benefit. Complete removal of all visible peritoneal implants is essential both for accurate staging and therapeutic management of serous borderline ovarian tumours (sBOTs), particularly in cases exhibiting peritoneal disease, as routine lymphadenectomy has not demonstrated survival benefits in stage II/III sBOTs [36]. Fertility-sparing surgery in patients with peritoneal implants carries a higher risk of recurrence compared to stage I cases, but this elevated risk stems from the initial peritoneal spread rather than ovarian preservation itself [36].
Although laparotomy remains the predominant approach, emerging evidence supports a cautious expansion of minimally invasive techniques – especially laparoscopy – for large adnexal masses. In minimally invasive procedures, the tumour should be placed in a bag and removed through a small incision while maintaining oncological sterility [38]. Even large lesions up to 30 cm can be removed minimally invasively in a safe and effective manner. However, a cautious technique is essential: protected cyst aspiration and the use of specimen bags have been shown to significantly reduce the risk of tumour rupture during laparoscopy [39]. Similarly, five recent cases of giant cysts were managed via single-port laparoscopy with protective retrieval bags, achieving safe outcomes and excellent cosmetic results [40]. These evolving approaches – bag extraction, staged aspiration, and single-port methods – suggest that laparoscopy may be a feasible option in highly selected cases. That said, careful patient selection, meticulous technique, and oncologic safeguards remain paramount until larger prospective studies confirm the safety and long-term outcomes. An innovative approach, described by Kakinuma et al., involves the use of cyanoacrylate glue to secure the tumour within a sterile bag under laparoscopic guidance before extracting it through a small abdominal incision. This technique is particularly useful when malignancy cannot be ruled out and facilitates the removal of large tumours. However, its oncological safety in cases of BOTs would need to be confirmed through large randomised studies [41]. A similar scope of surgery in postmenopausal patients was performed in the publications we analysed. In the case of premenopausal patients, removal of the tumour alone or adnexa with the tumour was much more common. We also found that in the vast majority of cases, the decision was made to perform surgery by means of classic laparotomy with a midline incision; only in two cases it was decided to initiate treatment with minimally invasive techniques, which still required minilaparotomy to extract the tumour [42,43]. Moreover diagnostic laparoscopy – often combined with imaging (MRI, positron emission tomography [PET]-CT, and CT) and biomarkers like CA 125 and HE4 – has demonstrated high accuracy (up to 90%), with strong negative predictive value in ruling out unresectable disease and randomised trials, confirming its utility in optimising patient selection [42,43]. By enhancing preoperative assessment of intra- and extra-abdominal tumour burden, laparoscopy supports more personalised surgical planning and may safely guide decisions between primary debulking and neoadjuvant approaches [44].
The literature highlights the risk of complications in patients with giant ovarian tumours, which include life-threatening events, such as pulmonary and cardiac failure, pulmonary embolism, and sepsis [45]. These risks are heightened due to the challenges of managing massive ovarian tumours, which can cause severe hypotension, increased venous return, cardiac failure, respiratory complications, and intestinal distension. Postoperative complications often arise due to rapid changes in body circulation, including the development of pulmonary oedema [46]. One specific concern is hypotension syndrome, which is caused by the compression of large blood vessels when the patient is in a supine position; this condition can lead to sudden drops in intrathoracic and intracavitary pressure, resulting in haemodynamic disturbances. To mitigate these risks, a slow intraoperative drainage rate of 0.5–1 L/min and positioning the patient in a lateral decubitus position, rather than supine, is recommended to avoid vena cava compression and reduce the risk of cardiac arrest. In most cases reviewed in the literature, there were no intraoperative or early postoperative complications, which highlight the effectiveness of careful perioperative management. Implementation of Enhanced Recovery After Surgery (ERAS) protocols may significantly reduce the physiological stress of extensive laparotomy for ovarian tumours by promoting early feeding, mobilisation, and optimised pain control, thereby maintaining patients’ normal physiological state [47]. In patients undergoing open cytoreductive surgery for advanced ovarian masses, ERAS implementation has been associated with fewer postoperative complications and lower rates of Intensive Care Unit admission [48].
Ultimately, we found that the complexity of treating giant ovarian tumours necessitates a multidisciplinary approach, which is crucial for providing optimal patient care [49]. This approach involves collaboration among a medical oncologist, gynaecologic oncologist, radiologist, pathologist, and other specialists to develop personalised care plans. Multidisciplinary team meetings and continuous discussions of patient cases are thus essential for accurate diagnosis and determining the most effective treatment options [50,51]. The prognosis for patients with GBOTs varies based on factors such as tumour size and stage, patient age and overall health, and the success of treatment. FIGO classification is particularly important in determining the prognosis, guiding treatment decisions, and assessing outcomes [52,53].
5 Limitations of the study
The analysis is based on a small group of patients drawn from 21 studies, mostly of case reports and small observational studies with diverse designs and populations. Such small, heterogeneous samples severely limit the generalisability of findings, and raise concerns about publication bias – where positive or unusual cases are more likely to be reported. Although trends such as higher CA 125 levels in younger patients and an increased likelihood of hysterectomy with greater age or tumour size are intriguing, definitive conclusions require larger, prospective studies with standardised data collection protocols. An additional factor contributing to discrepancies may have been the limitation to publications in English and Polish, given that the authors were able to perform an in-depth analysis of their content.
6 Conclusions
GBOTs are rare neoplasms that require meticulous management to prevent high-risk operative complications. Despite the diagnostic and therapeutic challenges posed by the large size and potential complications of these tumours, with proper medical care, patients can achieve successful outcomes and good prognosis.
Abbreviations
- AFP
-
α-fetoprotein
- BOTs
-
borderline ovarian tumours
- BSO
-
bilateral salpingo-oophorectomy
- CA 125
-
cancer antigen 125
- CA 19-9
-
cancer antigen 19-9
- CEA
-
carcinoembryonic antigen
- CT
-
computed tomography
- CT
-
computed tomography
- FIGO
-
International Federation of Gynaecology and Obstetrics
- GBOTs
-
giant borderline ovarian tumours
- HA
-
abdominal hysterectomy
- LDH
-
lactate dehydrogenase
- mBOT
-
mucinous borderline ovarian tumour
- MRI
-
magnetic resonance imaging
- MRI
-
magnetic resonance imaging
- PET
-
positron emission tomography
- PRISMA
-
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- sBOT
-
serous borderline ovarian tumour
- ß-HCG
-
ß-human chorionic gonadotropin
- TLH
-
total laparoscopic hysterectomy
- USG
-
ultrasound
- USO
-
unilateral salpingo-oophorectomy
-
Funding information: The authors declare that no funds, grants, or other support was received.
-
Author contributions: PS: conceived and designed the analysis, collected the data, and wrote the article. KD: collected the data and wrote the article. PD: collected the data and wrote the article. MWS: contributed data and designed the analysis.
-
Conflict of interest: PS serves as an editor in Open Medicine, but it did not influence the peer-review process of the article.
-
Data availability statement: The data supporting the findings of this study are available from the corresponding author upon reasonable request.
References
[1] Gharbia N, Halouani A, Tekaya F, Slama SB, Triki A, Amor AB. Infected, giant borderline ovarian tumor: A case report. Int J Surg Case Rep. 2023;111:108873. 10.1016/j.ijscr.2023.108873, Epub 2023 Sep 26 . PMID: 37801963; PMCID: PMC10558306.Search in Google Scholar PubMed PubMed Central
[2] Fischerova D, Zikan M, Dundr P, Cibula D. Diagnosis, treatment, and follow-up of borderline ovarian tumors. Oncologist. 2012;17(12):1515–33. 10.1634/theoncologist.2012-0139, Epub 2012 Sep 28 . PMID: 23024155; PMCID: PMC3528384.Search in Google Scholar PubMed PubMed Central
[3] Pilone V, Tramontano S, Picarelli P, Monda A, Romano M, Renzulli M, et al. Giant mucinous ovarian borderline tumor. A good lesson from an asymptomatic case. Int J Surg Case Rep. 2018;50:25–7. 10.1016/j.ijscr.2018.07.016, Epub 2018 Jul 26. PMID: 30071377; PMCID: PMC6080572.Search in Google Scholar PubMed PubMed Central
[4] Moyon MA, León DA, Aguayo WG, Mecias AR, Moyon FX, Tufiño J, et al. Giant ovarian mucinous cystadenoma, a challenging situation in resource-limited countries. J Surg Case Rep. 2019;2019(12):rjz366. 10.1093/jscr/rjz366, PMID: 31832139; PMCID: PMC6900351.Search in Google Scholar PubMed PubMed Central
[5] Sahu SA, Shrivastava D. A comprehensive review of screening methods for ovarian masses: towards earlier detection. Cureus. 2023;15(11):e48534. 10.7759/cureus.48534, PMID: 38084173; PMCID: PMC10710762.Search in Google Scholar PubMed PubMed Central
[6] Sadlecki P, Dejewska K, Domieracka P, Walentowicz-Sadlecka M. Giant mucinous borderline ovarian tumor: challenges of diagnosis and treatment. Arch Gynecol Obstet. 2025;311(4):1205–7. 10.1007/s00404-024-07793-8, Epub 2024 Oct 23. PMID: 39441405; PMCID: PMC11985592.Search in Google Scholar PubMed PubMed Central
[7] Kluz T, Bogaczyk A, Wita-Popów B, Habało P, Kluz-Barłowska M. Giant ovarian tumor. Medicina (Kaunas). 2023;59(10):1833. 10.3390/medicina59101833, PMID: 37893550; PMCID: PMC10608514.Search in Google Scholar PubMed PubMed Central
[8] Sadlecki P, Walentowicz-Sadlecka M. Molecular landscape of borderline ovarian tumours: A systematic review. Open Med (Wars). 2024;19(1):20240976. 10.1515/med-2024-0976, PMID: 38859878; PMCID: PMC11163159.Search in Google Scholar PubMed PubMed Central
[9] Mitragkas P, Synekidou E, Hatzimisios K. Giant ovarian mucinous borderline tumors. A report of two cases and literature review. Maedica (Bucur). 2021;16(4):743–6. 10.26574/maedica.2020.16.4.743, PMID: 35261682; PMCID: PMC8897801.Search in Google Scholar PubMed PubMed Central
[10] Iwasaki M, Taira K, Kobayashi H, Saiga T. Ovarian mucinous cystadenoma of borderline malignancy in a premenarchal girl. J Pediatr Adolesc Gynecol. 2010;23(3):e119–23. 10.1016/j.jpag.2009.09.011, Epub 2009 Nov 5. PMID: 19896401.Search in Google Scholar PubMed
[11] Tjokroprawiro BA, Novitasari K, Ulhaq RA, Sulistya HA. Clinicopathological analysis of giant ovarian tumors. Eur J Obstet Gynecol Reprod Biol X. 2024;22:100318. 10.1016/j.eurox.2024.100318, PMID: 38881672; PMCID: PMC11176949.Search in Google Scholar PubMed PubMed Central
[12] Mulita F, Oikonomou N, Tchabashvili L, Liolis E, Kehagias I. A giant ovarian mucinous tumor in a 58-year-old postmenopausal patient with persistent abdominal pain and high serum levels of CA 19-9. Pan Afr Med J. 2020;37:76. 10.11604/pamj.2020.37.76.25932, PMID: 33244339; PMCID: PMC7680227.Search in Google Scholar PubMed PubMed Central
[13] Tanaka M, Yamanoi K, Kitamura S, Horikawa N, Chigusa Y, Horie A, et al. A 36 kg giant ovarian fibroma with Meigs syndrome: a case report and literature review of extremely giant ovarian tumor. Case Rep Obstet Gynecol. 2021;2021:1076855. 10.1155/2021/1076855, PMID: 34434586; PMCID: PMC8382553.Search in Google Scholar PubMed PubMed Central
[14] Borrelli GM, de Mattos LA, Andres MP, Gonçalves MO, Kho RM, Abrão MS. Role of imaging tools for the diagnosis of borderline ovarian tumors: a systematic review and meta-analysis. J Minim Invasive Gynecol. 2017;24(3):353–63. 10.1016/j.jmig.2016.12.012, Epub 2016 Dec 24. PMID: 28027973.Search in Google Scholar PubMed
[15] Moon MH, Park HS, Kim YJ, Yu MH, Park S, Jung SI. Computed tomography indicators for differentiating stage 1 borderline ovarian tumors from stage I malignant epithelial ovarian tumors. Diagnostics (Basel). 2023;13(3):480. 10.3390/diagnostics13030480, PMID: 36766584; PMCID: PMC9914279.Search in Google Scholar PubMed PubMed Central
[16] Van Gorp T, Cadron I, Despierre E, Daemen A, Leunen K, Amant F, et al. HE4 and CA125 as a diagnostic test in ovarian cancer: prospective validation of the Risk of Ovarian Malignancy Algorithm. Br J Cancer. 2011;104(5):863–70. 10.1038/sj.bjc.6606092, Epub 2011 Feb 8. PMID: 21304524; PMCID: PMC3048204.Search in Google Scholar PubMed PubMed Central
[17] Deo A, Shrivastava D, Shanoo A. Giant borderline mucinous cystadenoma: a distressing scenario. Cureus. 2022;14(4):e23968. 10.7759/cureus.23968, PMID: 35541292; PMCID: PMC9081803.Search in Google Scholar PubMed PubMed Central
[18] Halani D, Jaiswal A. Postmenopausal woman with 24 kilograms ovarian mucinous cystadenoma: a rare case report. Pan Afr Med J. 2023;44:42. 10.11604/pamj.2023.44.42.36942, PMID: 37070025; PMCID: PMC10105331.Search in Google Scholar PubMed PubMed Central
[19] Lee HM, So KA, Kim MK, Lee YK, Lee IH, Kim TJ, et al. A case report of a young girl with mucinous borderline tumor of the ovary. Obstet Gynecol Sci. 2016;59(4):333–6. 10.5468/ogs.2016.59.4.333Epub 2016 Jul 13, PMID: 27462604; PMCID: PMC4958683.Search in Google Scholar
[20] Menahem S, Shvartzman P. Giant ovarian cyst mimicking ascites. J Fam Pract. 1994;39(5):479–81, PMID: 7964546.Search in Google Scholar
[21] Desai S, Guddati AK. Carcinoembryonic antigen, carbohydrate antigen 19-9, cancer antigen 125, prostate-specific antigen and other cancer markers: a primer on commonly used cancer markers. World J Oncol. 2023;14(1):4–14. 10.14740/wjon1425, Epub 2023 Feb 26. PMID: 36895994; PMCID: PMC9990734.Search in Google Scholar PubMed PubMed Central
[22] Cîrstoiu MM, Sajin M, Secară DC, Munteanu O, Cîrstoiu FC. Giant ovarian mucinous cystadenoma with borderline areas: a case report. Rom J Morphol Embryol. 2014;55(4):1443–7, PMID: 25611279.Search in Google Scholar
[23] Behnamfar F, Esmaeilian F, Adibi A, Rouholamin S. Comparison of ultrasound and tumor marker CA125 in diagnosis of adnexal mass malignancies. Adv Biomed Res. 2022;11:18. 10.4103/abr.abr_164_20, PMID: 35386543; PMCID: PMC8977613.Search in Google Scholar PubMed PubMed Central
[24] Charkhchi P, Cybulski C, Gronwald J, Wong FO, Narod SA, Akbari MR. CA125 and ovarian cancer: a comprehensive review. Cancers (Basel). 2020;12(12):3730. 10.3390/cancers12123730, PMID: 33322519; PMCID: PMC7763876.Search in Google Scholar PubMed PubMed Central
[25] Giordano G, Berretta R, Silini E. Primary pure spindle cell carcinoma (sarcomatoid carcinoma) of the ovary: A case report with immunohistochemical study. Diagn Pathol. 2016;11(1):70. 10.1186/s13000-016-0521-3, PMID: 27491291; PMCID: PMC4974787.Search in Google Scholar PubMed PubMed Central
[26] Sanna E, Madeddu C, Melis L, Nemolato S, Macciò A. Laparoscopic management of a giant mucinous benign ovarian mass weighing 10150 grams: A case report. World J Clin Cases. 2020;8(16):3527–33. 10.12998/wjcc.v8.i16.3527, PMID: 32913859; PMCID: PMC7457110.Search in Google Scholar PubMed PubMed Central
[27] Barragán-Curiel AE, Murillo-Zepeda C, Castro-Perez KF, Alcalá-Aguirre FO, Diaz-Montoya LS, Ruiz-Félix OA, et al. Giant mature ovarian cystic teratoma in a pediatric patient: case report and literature review. Case Rep Oncol. 2023;16(1):1066–72. 10.1159/000534141, PMID: 37900852; PMCID: PMC10601794.Search in Google Scholar PubMed PubMed Central
[28] Kiseli M, Caglar GS, Cengiz SD, Karadag D, Yılmaz MB. Clinical diagnosis and complications of paratubal cysts: review of the literature and report of uncommon presentations. Arch Gynecol Obstet. 2012;285(6):1563–9. 10.1007/s00404-012-2304-8, Epub 2012 Apr 13. PMID: 22526447.Search in Google Scholar PubMed
[29] Mikos T, Tabakoudis GP, Pados G, Eugenidis NP, Assimakopoulos E. Failure of ultrasound to diagnose a giant ovarian cyst: a case report. Cases J. 2009;2:6909. 10.4076/1757-1626-2-6909, PMID: 19829881; PMCID: PMC274011.Search in Google Scholar PubMed PubMed Central
[30] Watanabe S, Nagashima S, Onagi C, Yamazaki N, Shimada S, Sakai M, et al. Treatment strategy for pediatric giant mucinous cystadenoma: A case report. Pediatr Rep. 2019;11(3):8190. 10.4081/pr.2019.8190, PMID: 31579185; PMCID: PMC6769354.Search in Google Scholar PubMed PubMed Central
[31] Buza N. Frozen section diagnosis of ovarian epithelial tumors: diagnostic pearls and pitfalls. Arch Pathol Lab Med. 2019;143(1):47–64. 10.5858/arpa.2018-0289-RA, PMID: 30785337.Search in Google Scholar PubMed
[32] Raimondo D, Raffone A, Zakhari A, Maletta M, Vizzielli G, Restaino S, et al. The impact of hysterectomy on oncological outcomes in patients with borderline ovarian tumors: A systematic review and meta-analysis. Gynecol Oncol. 2022;165(1):184–91. 10.1016/j.ygyno.2022.01.019, Epub 2022 Jan 26. PMID: 35090745.Search in Google Scholar PubMed
[33] Ronsini C, Restaino S, Budani MC, Porcelli G, Tiboni GM, Fanfani F. Fertility sparing treatment for bilateral borderline ovarian tumor: a case report and management strategy explication. Minerva Obstet Gynecol. 2023;75(6):583–7. 10.23736/S2724-606X.22.05115-6, Epub 2022 Oct 4. PMID: 36193828.Search in Google Scholar PubMed
[34] Yazawa R, Yazawa H, Fukuda K, Ohara M, Osuka F. Four cases of pseudomyxoma peritonei with ovarian tumors at our hospital. Fukushima J Med Sci. 2023;69(1):57–65. 10.5387/fms.2022-41, Epub 2023 Mar 30. PMID 36990788; PMCID: PMC10122967.Search in Google Scholar PubMed PubMed Central
[35] Kleppe M, Bruls J, Van Gorp T, Massuger L, Slangen BF, Van de Vijver KK, et al. Mucinous borderline tumours of the ovary and the appendix: a retrospective study and overview of the literature. Gynecol Oncol. 2014;133(2):155–8. 10.1016/j.ygyno.2014.02.013, Epub 2014 Feb 16. PMID: 24552756.Search in Google Scholar PubMed
[36] Colombo N, Sessa C, du Bois A, Ledermann J, McCluggage WG, McNeish I, et al. ESMO-ESGO Ovarian Cancer Consensus Conference Working Group. ESMO-ESGO consensus conference recommendations on ovarian cancer: pathology and molecular biology, early and advanced stages, borderline tumours and recurrent disease†. Ann Oncol. 2019;30(5):672–705. 10.1093/annonc/mdz062, PMID: 31046081.Search in Google Scholar PubMed
[37] Raimondo D, Raffone A, Scambia G, Maletta M, Lenzi J, Restaino S, et al. The impact of hysterectomy on oncological outcomes in postmenopausal patients with borderline ovarian tumors: A multicenter retrospective study. Front Oncol. 2022;12:1009341. 10.3389/fonc.2022.1009341, PMID: 36387131; PMCID: PMC964705.Search in Google Scholar PubMed PubMed Central
[38] Dubuisson J, Heersche S, Petignat P, Undurraga M. Laparoscopic management of giant ovarian cysts using the alexis laparoscopic system®: a case series. Front Surg. 2020;7:24. 10.3389/fsurg.2020.00024, PMID: 32435653; PMCID: PMC7218052.Search in Google Scholar PubMed PubMed Central
[39] El Hajj H, Hudry D, Gomez CM, Boscher A, Duchatelet M, Leblanc E, et al. Protected laparoscopic large ovarian cyst aspiration: a 5-step alternative to laparotomy. J Minim Invasive Gynecol. 2022;29(9):1038–9. 10.1016/j.jmig.2022.06.018, Epub 2022 Jun 23. PMID: 35753617.Search in Google Scholar PubMed
[40] Jiang L, Zhao X, Han Y, Liu K, Meng X. Giant ovarian cysts treated by single-port laparoscopic surgery: a case series. Front Oncol. 2021;11:796330. 10.3389/fonc.2021.796330, eCollection 2021.Search in Google Scholar PubMed PubMed Central
[41] Kakinuma T, Kakinuma K, Shinohara T, Shimizu A, Okamoto R, Kaneko A, et al. Efficacy and safety of an Aron Alpha method in managing giant ovarian tumors. Gynecol Oncol Rep. 2023;46:101167. 10.1016/j.gore.2023.101167, PMID: 37033210; PMCID: PMC10073634.Search in Google Scholar PubMed PubMed Central
[42] D’Augè TG, Giannini A, Cuccu I, De Angelis E, Di Donato V, Muzii L, et al. Laparoscopic prediction of primary cytoreducibility of epithelial ovarian cancer. Minerva Obstet Gynecol. 2024;76(6):548–57. 10.23736/S2724-606X.24.05452-6, Epub 2024 Oct 8. PMID: 39377288.Search in Google Scholar PubMed
[43] Yazawa H, Imaizumi K, Kato A, Takiguchi K. Extragonadal giant endometrial cyst with endometrioid borderline tumor. Gynecol Minim Invasive Ther. 2019;8(4):179–84. 10.4103/GMIT.GMIT_85_18, PMID: 31741845; PMCID: PMC6849104.Search in Google Scholar PubMed PubMed Central
[44] Bogliatto F, Crana F, Marino AA. Laparoscopic excision of giant mucinous ovarian borderline tumor. Is a safely approach? Arch Clin Med Case Rep. 2020;4:065–70.10.26502/acmcr.96550167Search in Google Scholar
[45] Amadasi A, Andreola S, Bianchi M, Boracchi M, Gentile G, Maciocco F, et al. Pulmonary thromboembolism secondary to pelvic thrombosis related to giant ovarian tumor. Autops Case Rep. 2019;9(1):e2018061. 10.4322/acr.2018.061, PMID: 30863733; PMCID: PMC6394364.Search in Google Scholar PubMed PubMed Central
[46] Cai S, Dai R, Mi J, Wang S, Jiang Y. Perioperative management of a patient with a giant ovarian tumor: A case report. Med (Baltim). 2020;99(41):e22625. 10.1097/MD.0000000000022625, PMID: 33031322; PMCID: PMC7544284.Search in Google Scholar PubMed PubMed Central
[47] Forte S, Ferrari FA, Majd HS, Cisotto F, Ferrari F. Enhanced recovery after surgery (ERAS) in gynecology: state of the art and the problem of barriers. Clin Exp Obstet Gynecol. 2023;50(1):14. 10.31083/j.ceog5001014.Search in Google Scholar
[48] Agarwal R, Rajanbabu A, Goel G, Madhusudanan L, UG U. A prospective study evaluating the impact of implementing the ERAS protocol on patients undergoing surgery for advanced ovarian cancer. Int J Gynecol Cancer. 2019;29(3):605–12. 10.1136/ijgc-2018-000043, Epub 2019 Jan 4. PMID: 30833445.Search in Google Scholar PubMed
[49] Stukan M, Dudziak M, Pawłowski M. Olbrzymi guz jajnika--opis przypadku i propozycja postepowania klincznego [Giant ovarian tumor--case report and proposal for clinical management]. Ginekol Pol. 2011;82(2):150–2Polish. PMID: 21574489.Search in Google Scholar
[50] Falzone L, Scandurra G, Lombardo V, Gattuso G, Lavoro A, Distefano AB, et al. A multidisciplinary approach remains the best strategy to improve and strengthen the management of ovarian cancer (Review). Int J Oncol. 2021;59(1):53. 10.3892/ijo.2021.5233, Epub 2021 Jun 16. PMID: 34132354; PMCID: PMC8208622.Search in Google Scholar PubMed PubMed Central
[51] Peiretti M, Mais V, D’Ancona G, Fais ML, Erdas E, Figus A, et al. Effective surgical management of a large serous ovarian cyst in a morbidly obese middle-aged woman: a case study and literature review. Am J Case Rep. 2023;24:e939697. 10.12659/AJCR.939697, PMID: 37342983; PMCID: PMC10290437.Search in Google Scholar PubMed PubMed Central
[52] Sun Y, Xu J, Jia X. The diagnosis, treatment, prognosis and molecular pathology of borderline ovarian tumors: current status and perspectives. Cancer Manag Res. 2020;12:3651–9. 10.2147/CMAR.S250394, PMID: 32547202; PMCID: PMC7246309.Search in Google Scholar PubMed PubMed Central
[53] Onuzo CN, Gordon AS, Amoatwo JKA, Kuti CK, Taylor P, Sefogah PE. A giant 25 litre volume ovarian cystic mucinous borderline ovarian tumour with intraepithelial carcinoma in a 24-year-old nulliparous woman: Case report. Int J Surg Case Rep. 2024;119:109732. 10.1016/j.ijscr.2024.109732, Epub 2024 May 8 . PMID: 38754159; PMCID: PMC11109311.Search in Google Scholar PubMed PubMed Central
© 2025 the author(s), published by De Gruyter
This work is licensed under the Creative Commons Attribution 4.0 International License.
Articles in the same Issue
- Research Articles
- Network pharmacological analysis and in vitro testing of the rutin effects on triple-negative breast cancer
- Impact of diabetes on long-term survival in elderly liver cancer patients: A retrospective study
- Knockdown of CCNB1 alleviates high glucose-triggered trophoblast dysfunction during gestational diabetes via Wnt/β-catenin signaling pathway
- Risk factors for severe adverse drug reactions in hospitalized patients
- Analysis of the effect of ALA-PDT on macrophages in footpad model of mice infected with Fonsecaea monophora based on single-cell sequencing
- Development and validation of headspace gas chromatography with a flame ionization detector method for the determination of ethanol in the vitreous humor
- CMSP exerts anti-tumor effects on small cell lung cancer cells by inducing mitochondrial dysfunction and ferroptosis
- Predictive value of plasma sB7-H3 and YKL-40 in pediatric refractory Mycoplasma pneumoniae pneumonia
- Antiangiogenic potential of Elaeagnus umbellata extracts and molecular docking study by targeting VEGFR-2 pathway
- Comparison of the effectiveness of nurse-led preoperative counseling and postoperative follow-up care vs standard care for patients with gastric cancer
- Comparing the therapeutic efficacy of endoscopic minimally invasive surgery and traditional surgery for early-stage breast cancer: A meta-analysis
- Adhered macrophages as an additional marker of cardiomyocyte injury in biopsies of patients with dilated cardiomyopathy
- Association between statin administration and outcome in patients with sepsis: A retrospective study
- Exploration of the association between estimated glucose disposal rate and osteoarthritis in middle-aged and older adults: An analysis of NHANES data from 2011 to 2018
- A comparative analysis of the binary and multiclass classified chest X-ray images of pneumonia and COVID-19 with ML and DL models
- Lysophosphatidic acid 2 alleviates deep vein thrombosis via protective endothelial barrier function
- Transcription factor A, mitochondrial promotes lymph node metastasis and lymphangiogenesis in epithelial ovarian carcinoma
- Serum PM20D1 levels are associated with nutritional status and inflammatory factors in gastric cancer patients undergoing early enteral nutrition
- Hydromorphone reduced the incidence of emergence agitation after adenotonsillectomy in children with obstructive sleep apnea: A randomized, double-blind study
- Vitamin D replacement therapy may regulate sleep habits in patients with restless leg syndrome
- The first-line antihypertensive nitrendipine potentiated the therapeutic effect of oxaliplatin by downregulating CACNA1D in colorectal cancer
- Health literacy and health-related quality of life: The mediating role of irrational happiness
- Modulatory effects of Lycium barbarum polysaccharide on bone cell dynamics in osteoporosis
- Mechanism research on inhibition of gastric cancer in vitro by the extract of Pinellia ternata based on network pharmacology and cellular metabolomics
- Examination of the causal role of immune cells in non-alcoholic fatty liver disease by a bidirectional Mendelian randomization study
- Clinical analysis of ten cases of HIV infection combined with acute leukemia
- Investigating the cardioprotective potential of quercetin against tacrolimus-induced cardiotoxicity in Wistar rats: A mechanistic insights
- Clinical observation of probiotics combined with mesalazine and Yiyi Baitouweng Decoction retention enema in treating mild-to-moderate ulcerative colitis
- Diagnostic value of ratio of blood inflammation to coagulation markers in periprosthetic joint infection
- Sex-specific associations of sex hormone binding globulin and risk of bladder cancer
- Core muscle strength and stability-oriented breathing training reduces inter-recti distance in postpartum women
- The ERAS nursing care strategy for patients undergoing transsphenoidal endoscopic pituitary tumor resection: A randomized blinded controlled trial
- The serum IL-17A levels in patients with traumatic bowel rupture post-surgery and its predictive value for patient prognosis
- Impact of Kolb’s experiential learning theory-based nursing on caregiver burden and psychological state of caregivers of dementia patients
- Analysis of serum NLR combined with intraoperative margin condition to predict the prognosis of cervical HSIL patients undergoing LEEP surgery
- Commiphora gileadensis ameliorate infertility and erectile dysfunction in diabetic male mice
- The correlation between epithelial–mesenchymal transition classification and MMP2 expression of circulating tumor cells and prognosis of advanced or metastatic nasopharyngeal carcinoma
- Tetrahydropalmatine improves mitochondrial function in vascular smooth muscle cells of atherosclerosis in vitro by inhibiting Ras homolog gene family A/Rho-associated protein kinase-1 signaling pathway
- A cross-sectional study: Relationship between serum oxidative stress levels and arteriovenous fistula maturation in maintenance dialysis patients
- A comparative analysis of the impact of repeated administration of flavan 3-ol on brown, subcutaneous, and visceral adipose tissue
- Identifying early screening factors for depression in middle-aged and older adults: A cohort study
- Perform tumor-specific survival analysis for Merkel cell carcinoma patients undergoing surgical resection based on the SEER database by constructing a nomogram chart
- Unveiling the role of CXCL10 in pancreatic cancer progression: A novel prognostic indicator
- High-dose preoperative intraperitoneal erythropoietin and intravenous methylprednisolone in acute traumatic spinal cord injuries following decompression surgeries
- RAB39B: A novel biomarker for acute myeloid leukemia identified via multi-omics and functional validation
- Impact of peripheral conditioning on reperfusion injury following primary percutaneous coronary intervention in diabetic and non-diabetic STEMI patients
- Clinical efficacy of azacitidine in the treatment of middle- and high-risk myelodysplastic syndrome in middle-aged and elderly patients: A retrospective study
- The effect of ambulatory blood pressure load on mitral regurgitation in continuous ambulatory peritoneal dialysis patients
- Expression and clinical significance of ITGA3 in breast cancer
- Single-nucleus RNA sequencing reveals ARHGAP28 expression of podocytes as a biomarker in human diabetic nephropathy
- rSIG combined with NLR in the prognostic assessment of patients with multiple injuries
- Toxic metals and metalloids in collagen supplements of fish and jellyfish origin: Risk assessment for daily intake
- Exploring causal relationship between 41 inflammatory cytokines and marginal zone lymphoma: A bidirectional Mendelian randomization study
- Gender beliefs and legitimization of dating violence in adolescents
- Effect of serum IL-6, CRP, and MMP-9 levels on the efficacy of modified preperitoneal Kugel repair in patients with inguinal hernia
- Effect of smoking and smoking cessation on hematological parameters in polycythemic patients
- Pathogen surveillance and risk factors for pulmonary infection in patients with lung cancer: A retrospective single-center study
- Necroptosis of hippocampal neurons in paclitaxel chemotherapy-induced cognitive impairment mediates microglial activation via TLR4/MyD88 signaling pathway
- Celastrol suppresses neovascularization in rat aortic vascular endothelial cells stimulated by inflammatory tenocytes via modulating the NLRP3 pathway
- Cord-lamina angle and foraminal diameter as key predictors of C5 palsy after anterior cervical decompression and fusion surgery
- GATA1: A key biomarker for predicting the prognosis of patients with diffuse large B-cell lymphoma
- Influencing factors of false lumen thrombosis in type B aortic dissection: A single-center retrospective study
- MZB1 regulates the immune microenvironment and inhibits ovarian cancer cell migration
- Integrating experimental and network pharmacology to explore the pharmacological mechanisms of Dioscin against glioblastoma
- Trends in research on preterm birth in twin pregnancy based on bibliometrics
- Four-week IgE/baseline IgE ratio combined with tryptase predicts clinical outcome in omalizumab-treated children with moderate-to-severe asthma
- Single-cell transcriptomic analysis identifies a stress response Schwann cell subtype
- Acute pancreatitis risk in the diagnosis and management of inflammatory bowel disease: A critical focus
- Effect of subclinical esketamine on NLRP3 and cognitive dysfunction in elderly ischemic stroke patients
- Interleukin-37 mediates the anti-oral tumor activity in oral cancer through STAT3
- CA199 and CEA expression levels, and minimally invasive postoperative prognosis analysis in esophageal squamous carcinoma patients
- Efficacy of a novel drainage catheter in the treatment of CSF leak after posterior spine surgery: A retrospective cohort study
- Comprehensive biomedicine assessment of Apteranthes tuberculata extracts: Phytochemical analysis and multifaceted pharmacological evaluation in animal models
- Relation of time in range to severity of coronary artery disease in patients with type 2 diabetes: A cross-sectional study
- Dopamine attenuates ethanol-induced neuronal apoptosis by stimulating electrical activity in the developing rat retina
- Correlation between albumin levels during the third trimester and the risk of postpartum levator ani muscle rupture
- Factors associated with maternal attention and distraction during breastfeeding and childcare: A cross-sectional study in the west of Iran
- Mechanisms of hesperetin in treating metabolic dysfunction-associated steatosis liver disease via network pharmacology and in vitro experiments
- The law on oncological oblivion in the Italian and European context: How to best uphold the cancer patients’ rights to privacy and self-determination?
- The prognostic value of the neutrophil-to-lymphocyte ratio, platelet-to-lymphocyte ratio, and prognostic nutritional index for survival in patients with colorectal cancer
- Factors affecting the measurements of peripheral oxygen saturation values in healthy young adults
- Comparison and correlations between findings of hysteroscopy and vaginal color Doppler ultrasonography for detection of uterine abnormalities in patients with recurrent implantation failure
- The effects of different types of RAGT on balance function in stroke patients with low levels of independent walking in a convalescent rehabilitation hospital
- Causal relationship between asthma and ankylosing spondylitis: A bidirectional two-sample univariable and multivariable Mendelian randomization study
- Correlations of health literacy with individuals’ understanding and use of medications in Southern Taiwan
- Correlation of serum calprotectin with outcome of acute cerebral infarction
- Comparison of computed tomography and guided bronchoscopy in the diagnosis of pulmonary nodules: A systematic review and meta-analysis
- Curdione protects vascular endothelial cells and atherosclerosis via the regulation of DNMT1-mediated ERBB4 promoter methylation
- The identification of novel missense variant in ChAT gene in a patient with gestational diabetes denotes plausible genetic association
- Molecular genotyping of multi-system rare blood types in foreign blood donors based on DNA sequencing and its clinical significance
- Exploring the role of succinyl carnitine in the association between CD39⁺ CD4⁺ T cell and ulcerative colitis: A Mendelian randomization study
- Dexmedetomidine suppresses microglial activation in postoperative cognitive dysfunction via the mmu-miRNA-125/TRAF6 signaling axis
- Analysis of serum metabolomics in patients with different types of chronic heart failure
- Diagnostic value of hematological parameters in the early diagnosis of acute cholecystitis
- Pachymaran alleviates fat accumulation, hepatocyte degeneration, and injury in mice with nonalcoholic fatty liver disease
- Decrease in CD4 and CD8 lymphocytes are predictors of severe clinical picture and unfavorable outcome of the disease in patients with COVID-19
- METTL3 blocked the progression of diabetic retinopathy through m6A-modified SOX2
- The predictive significance of anti-RO-52 antibody in patients with interstitial pneumonia after treatment of malignant tumors
- Exploring cerebrospinal fluid metabolites, cognitive function, and brain atrophy: Insights from Mendelian randomization
- Development and validation of potential molecular subtypes and signatures of ocular sarcoidosis based on autophagy-related gene analysis
- Widespread venous thrombosis: Unveiling a complex case of Behçet’s disease with a literature perspective
- Uterine fibroid embolization: An analysis of clinical outcomes and impact on patients’ quality of life
- Discovery of lipid metabolism-related diagnostic biomarkers and construction of diagnostic model in steroid-induced osteonecrosis of femoral head
- Serum-derived exomiR-188-3p is a promising novel biomarker for early-stage ovarian cancer
- Enhancing chronic back pain management: A comparative study of ultrasound–MRI fusion guidance for paravertebral nerve block
- Peptide CCAT1-70aa promotes hepatocellular carcinoma proliferation and invasion via the MAPK/ERK pathway
- Electroacupuncture-induced reduction of myocardial ischemia–reperfusion injury via FTO-dependent m6A methylation modulation
- Hemorrhoids and cardiovascular disease: A bidirectional Mendelian randomization study
- Cell-free adipose extract inhibits hypertrophic scar formation through collagen remodeling and antiangiogenesis
- HALP score in Demodex blepharitis: A case–control study
- Assessment of SOX2 performance as a marker for circulating cancer stem-like cells (CCSCs) identification in advanced breast cancer patients using CytoTrack system
- Risk and prognosis for brain metastasis in primary metastatic cervical cancer patients: A population-based study
- Comparison of the two intestinal anastomosis methods in pediatric patients
- Factors influencing hematological toxicity and adverse effects of perioperative hyperthermic intraperitoneal vs intraperitoneal chemotherapy in gastrointestinal cancer
- Endotoxin tolerance inhibits NLRP3 inflammasome activation in macrophages of septic mice by restoring autophagic flux through TRIM26
- Lateral transperitoneal laparoscopic adrenalectomy: A single-centre experience of 21 procedures
- Petunidin attenuates lipopolysaccharide-induced retinal microglia inflammatory response in diabetic retinopathy by targeting OGT/NF-κB/LCN2 axis
- Procalcitonin and C-reactive protein as biomarkers for diagnosing and assessing the severity of acute cholecystitis
- Factors determining the number of sessions in successful extracorporeal shock wave lithotripsy patients
- Development of a nomogram for predicting cancer-specific survival in patients with renal pelvic cancer following surgery
- Inhibition of ATG7 promotes orthodontic tooth movement by regulating the RANKL/OPG ratio under compression force
- A machine learning-based prognostic model integrating mRNA stemness index, hypoxia, and glycolysis‑related biomarkers for colorectal cancer
- Glutathione attenuates sepsis-associated encephalopathy via dual modulation of NF-κB and PKA/CREB pathways
- FAHD1 prevents neuronal ferroptosis by modulating R-loop and the cGAS–STING pathway
- Association of placenta weight and morphology with term low birth weight: A case–control study
- Investigation of the pathogenic variants induced Sjogren’s syndrome in Turkish population
- Nucleotide metabolic abnormalities in post-COVID-19 condition and type 2 diabetes mellitus patients and their association with endocrine dysfunction
- TGF-β–Smad2/3 signaling in high-altitude pulmonary hypertension in rats: Role and mechanisms via macrophage M2 polarization
- Ultrasound-guided unilateral versus bilateral erector spinae plane block for postoperative analgesia of patients undergoing laparoscopic cholecystectomy
- Profiling gut microbiome dynamics in subacute thyroiditis: Implications for pathogenesis, diagnosis, and treatment
- Delta neutrophil index, CRP/albumin ratio, procalcitonin, immature granulocytes, and HALP score in acute appendicitis: Best performing biomarker?
- Anticancer activity mechanism of novelly synthesized and characterized benzofuran ring-linked 3-nitrophenyl chalcone derivative on colon cancer cells
- H2valdien3 arrests the cell cycle and induces apoptosis of gastric cancer
- Prognostic relevance of PRSS2 and its immune correlates in papillary thyroid carcinoma
- Association of SGLT2 inhibition with psychiatric disorders: A Mendelian randomization study
- Motivational interviewing for alcohol use reduction in Thai patients
- Luteolin alleviates oxygen-glucose deprivation/reoxygenation-induced neuron injury by regulating NLRP3/IL-1β signaling
- Polyphyllin II inhibits thyroid cancer cell growth by simultaneously inhibiting glycolysis and oxidative phosphorylation
- Relationship between the expression of copper death promoting factor SLC31A1 in papillary thyroid carcinoma and clinicopathological indicators and prognosis
- CSF2 polarized neutrophils and invaded renal cancer cells in vitro influence
- Proton pump inhibitors-induced thrombocytopenia: A systematic literature analysis of case reports
- The current status and influence factors of research ability among community nurses: A sequential qualitative–quantitative study
- OKAIN: A comprehensive oncology knowledge base for the interpretation of clinically actionable alterations
- The relationship between serum CA50, CA242, and SAA levels and clinical pathological characteristics and prognosis in patients with pancreatic cancer
- Identification and external validation of a prognostic signature based on hypoxia–glycolysis-related genes for kidney renal clear cell carcinoma
- Engineered RBC-derived nanovesicles functionalized with tumor-targeting ligands: A comparative study on breast cancer targeting efficiency and biocompatibility
- Relationship of resting echocardiography combined with serum micronutrients to the severity of low-gradient severe aortic stenosis
- Effect of vibration on pain during subcutaneous heparin injection: A randomized, single-blind, placebo-controlled trial
- The diagnostic performance of machine learning-based FFRCT for coronary artery disease: A meta-analysis
- Comparing biofeedback device vs diaphragmatic breathing for bloating relief: A randomized controlled trial
- Serum uric acid to albumin ratio and C-reactive protein as predictive biomarkers for chronic total occlusion and coronary collateral circulation quality
- Multiple organ scoring systems for predicting in-hospital mortality of sepsis patients in the intensive care unit
- Single-cell RNA sequencing data analysis of the inner ear in gentamicin-treated mice via intraperitoneal injection
- Review Articles
- The effects of enhanced external counter-pulsation on post-acute sequelae of COVID-19: A narrative review
- Diabetes-related cognitive impairment: Mechanisms, symptoms, and treatments
- Microscopic changes and gross morphology of placenta in women affected by gestational diabetes mellitus in dietary treatment: A systematic review
- Review of mechanisms and frontier applications in IL-17A-induced hypertension
- Research progress on the correlation between islet amyloid peptides and type 2 diabetes mellitus
- The safety and efficacy of BCG combined with mitomycin C compared with BCG monotherapy in patients with non-muscle-invasive bladder cancer: A systematic review and meta-analysis
- The application of augmented reality in robotic general surgery: A mini-review
- The effect of Greek mountain tea extract and wheat germ extract on peripheral blood flow and eicosanoid metabolism in mammals
- Neurogasobiology of migraine: Carbon monoxide, hydrogen sulfide, and nitric oxide as emerging pathophysiological trinacrium relevant to nociception regulation
- Plant polyphenols, terpenes, and terpenoids in oral health
- Laboratory medicine between technological innovation, rights safeguarding, and patient safety: A bioethical perspective
- End-of-life in cancer patients: Medicolegal implications and ethical challenges in Europe
- The maternal factors during pregnancy for intrauterine growth retardation: An umbrella review
- Intra-abdominal hypertension/abdominal compartment syndrome of pediatric patients in critical care settings
- PI3K/Akt pathway and neuroinflammation in sepsis-associated encephalopathy
- Screening of Group B Streptococcus in pregnancy: A systematic review for the laboratory detection
- Giant borderline ovarian tumours – review of the literature
- Leveraging artificial intelligence for collaborative care planning: Innovations and impacts in shared decision-making – A systematic review
- Cholera epidemiology analysis through the experience of the 1973 Naples epidemic
- Risk factors of frailty/sarcopenia in community older adults: Meta-analysis
- Supplement strategies for infertility in overweight women: Evidence and legal insights
- Scurvy, a not obsolete disorder: Clinical report in eight young children and literature review
- A meta-analysis of the effects of DBS on cognitive function in patients with advanced PD
- Protective role of selenium in sepsis: Mechanisms and potential therapeutic strategies
- Strategies for hyperkalemia management in dialysis patients: A systematic review
- C-reactive protein-to-albumin ratio in peripheral artery disease
- Case Reports
- Delayed graft function after renal transplantation
- Semaglutide treatment for type 2 diabetes in a patient with chronic myeloid leukemia: A case report and review of the literature
- Diverse electrophysiological demyelinating features in a late-onset glycogen storage disease type IIIa case
- Giant right atrial hemangioma presenting with ascites: A case report
- Laser excision of a large granular cell tumor of the vocal cord with subglottic extension: A case report
- EsoFLIP-assisted dilation for dysphagia in systemic sclerosis: Highlighting the role of multimodal esophageal evaluation
- Molecular hydrogen-rhodiola as an adjuvant therapy for ischemic stroke in internal carotid artery occlusion: A case report
- Coronary artery anomalies: A case of the “malignant” left coronary artery and its surgical management
- Rapid Communication
- Biological properties of valve materials using RGD and EC
-
A single oral administration of flavanols enhances short
-term memory in mice along with increased brain-derived neurotrophic factor - Letter to the Editor
- Role of enhanced external counterpulsation in long COVID
- Expression of Concern
- Expression of concern “A ceRNA network mediated by LINC00475 in papillary thyroid carcinoma”
- Expression of concern “Notoginsenoside R1 alleviates spinal cord injury through the miR-301a/KLF7 axis to activate Wnt/β-catenin pathway”
- Expression of concern “circ_0020123 promotes cell proliferation and migration in lung adenocarcinoma via PDZD8”
- Corrigendum
- Corrigendum to “Empagliflozin improves aortic injury in obese mice by regulating fatty acid metabolism”
- Corrigendum to “Comparing the therapeutic efficacy of endoscopic minimally invasive surgery and traditional surgery for early-stage breast cancer: A meta-analysis”
- Corrigendum to “The progress of autoimmune hepatitis research and future challenges”
- Retraction
- Retraction of “miR-654-5p promotes gastric cancer progression via the GPRIN1/NF-κB pathway”
- Retraction of: “LncRNA CASC15 inhibition relieves renal fibrosis in diabetic nephropathy through downregulating SP-A by sponging to miR-424”
- Retraction of: “SCARA5 inhibits oral squamous cell carcinoma via inactivating the STAT3 and PI3K/AKT signaling pathways”
- Special Issue Advancements in oncology: bridging clinical and experimental research - Part II
- Unveiling novel biomarkers for platinum chemoresistance in ovarian cancer
- Lathyrol affects the expression of AR and PSA and inhibits the malignant behavior of RCC cells
- The era of increasing cancer survivorship: Trends in fertility preservation, medico-legal implications, and ethical challenges
- Bone scintigraphy and positron emission tomography in the early diagnosis of MRONJ
- Meta-analysis of clinical efficacy and safety of immunotherapy combined with chemotherapy in non-small cell lung cancer
- Special Issue Computational Intelligence Methodologies Meets Recurrent Cancers - Part IV
- Exploration of mRNA-modifying METTL3 oncogene as momentous prognostic biomarker responsible for colorectal cancer development
- Special Issue The evolving saga of RNAs from bench to bedside - Part III
- Interaction and verification of ferroptosis-related RNAs Rela and Stat3 in promoting sepsis-associated acute kidney injury
- The mRNA MOXD1: Link to oxidative stress and prognostic significance in gastric cancer
- Special Issue Exploring the biological mechanism of human diseases based on MultiOmics Technology - Part II
- Dynamic changes in lactate-related genes in microglia and their role in immune cell interactions after ischemic stroke
- A prognostic model correlated with fatty acid metabolism in Ewing’s sarcoma based on bioinformatics analysis
- Red cell distribution width predicts early kidney injury: A NHANES cross-sectional study
- Special Issue Diabetes mellitus: pathophysiology, complications & treatment
- Nutritional risk assessment and nutritional support in children with congenital diabetes during surgery
- Correlation of the differential expressions of RANK, RANKL, and OPG with obesity in the elderly population in Xinjiang
- A discussion on the application of fluorescence micro-optical sectioning tomography in the research of cognitive dysfunction in diabetes
- A review of brain research on T2DM-related cognitive dysfunction
- Metformin and estrogen modulation in LABC with T2DM: A 36-month randomized trial
- Special Issue Innovative Biomarker Discovery and Precision Medicine in Cancer Diagnostics
- CircASH1L-mediated tumor progression in triple-negative breast cancer: PI3K/AKT pathway mechanisms
Articles in the same Issue
- Research Articles
- Network pharmacological analysis and in vitro testing of the rutin effects on triple-negative breast cancer
- Impact of diabetes on long-term survival in elderly liver cancer patients: A retrospective study
- Knockdown of CCNB1 alleviates high glucose-triggered trophoblast dysfunction during gestational diabetes via Wnt/β-catenin signaling pathway
- Risk factors for severe adverse drug reactions in hospitalized patients
- Analysis of the effect of ALA-PDT on macrophages in footpad model of mice infected with Fonsecaea monophora based on single-cell sequencing
- Development and validation of headspace gas chromatography with a flame ionization detector method for the determination of ethanol in the vitreous humor
- CMSP exerts anti-tumor effects on small cell lung cancer cells by inducing mitochondrial dysfunction and ferroptosis
- Predictive value of plasma sB7-H3 and YKL-40 in pediatric refractory Mycoplasma pneumoniae pneumonia
- Antiangiogenic potential of Elaeagnus umbellata extracts and molecular docking study by targeting VEGFR-2 pathway
- Comparison of the effectiveness of nurse-led preoperative counseling and postoperative follow-up care vs standard care for patients with gastric cancer
- Comparing the therapeutic efficacy of endoscopic minimally invasive surgery and traditional surgery for early-stage breast cancer: A meta-analysis
- Adhered macrophages as an additional marker of cardiomyocyte injury in biopsies of patients with dilated cardiomyopathy
- Association between statin administration and outcome in patients with sepsis: A retrospective study
- Exploration of the association between estimated glucose disposal rate and osteoarthritis in middle-aged and older adults: An analysis of NHANES data from 2011 to 2018
- A comparative analysis of the binary and multiclass classified chest X-ray images of pneumonia and COVID-19 with ML and DL models
- Lysophosphatidic acid 2 alleviates deep vein thrombosis via protective endothelial barrier function
- Transcription factor A, mitochondrial promotes lymph node metastasis and lymphangiogenesis in epithelial ovarian carcinoma
- Serum PM20D1 levels are associated with nutritional status and inflammatory factors in gastric cancer patients undergoing early enteral nutrition
- Hydromorphone reduced the incidence of emergence agitation after adenotonsillectomy in children with obstructive sleep apnea: A randomized, double-blind study
- Vitamin D replacement therapy may regulate sleep habits in patients with restless leg syndrome
- The first-line antihypertensive nitrendipine potentiated the therapeutic effect of oxaliplatin by downregulating CACNA1D in colorectal cancer
- Health literacy and health-related quality of life: The mediating role of irrational happiness
- Modulatory effects of Lycium barbarum polysaccharide on bone cell dynamics in osteoporosis
- Mechanism research on inhibition of gastric cancer in vitro by the extract of Pinellia ternata based on network pharmacology and cellular metabolomics
- Examination of the causal role of immune cells in non-alcoholic fatty liver disease by a bidirectional Mendelian randomization study
- Clinical analysis of ten cases of HIV infection combined with acute leukemia
- Investigating the cardioprotective potential of quercetin against tacrolimus-induced cardiotoxicity in Wistar rats: A mechanistic insights
- Clinical observation of probiotics combined with mesalazine and Yiyi Baitouweng Decoction retention enema in treating mild-to-moderate ulcerative colitis
- Diagnostic value of ratio of blood inflammation to coagulation markers in periprosthetic joint infection
- Sex-specific associations of sex hormone binding globulin and risk of bladder cancer
- Core muscle strength and stability-oriented breathing training reduces inter-recti distance in postpartum women
- The ERAS nursing care strategy for patients undergoing transsphenoidal endoscopic pituitary tumor resection: A randomized blinded controlled trial
- The serum IL-17A levels in patients with traumatic bowel rupture post-surgery and its predictive value for patient prognosis
- Impact of Kolb’s experiential learning theory-based nursing on caregiver burden and psychological state of caregivers of dementia patients
- Analysis of serum NLR combined with intraoperative margin condition to predict the prognosis of cervical HSIL patients undergoing LEEP surgery
- Commiphora gileadensis ameliorate infertility and erectile dysfunction in diabetic male mice
- The correlation between epithelial–mesenchymal transition classification and MMP2 expression of circulating tumor cells and prognosis of advanced or metastatic nasopharyngeal carcinoma
- Tetrahydropalmatine improves mitochondrial function in vascular smooth muscle cells of atherosclerosis in vitro by inhibiting Ras homolog gene family A/Rho-associated protein kinase-1 signaling pathway
- A cross-sectional study: Relationship between serum oxidative stress levels and arteriovenous fistula maturation in maintenance dialysis patients
- A comparative analysis of the impact of repeated administration of flavan 3-ol on brown, subcutaneous, and visceral adipose tissue
- Identifying early screening factors for depression in middle-aged and older adults: A cohort study
- Perform tumor-specific survival analysis for Merkel cell carcinoma patients undergoing surgical resection based on the SEER database by constructing a nomogram chart
- Unveiling the role of CXCL10 in pancreatic cancer progression: A novel prognostic indicator
- High-dose preoperative intraperitoneal erythropoietin and intravenous methylprednisolone in acute traumatic spinal cord injuries following decompression surgeries
- RAB39B: A novel biomarker for acute myeloid leukemia identified via multi-omics and functional validation
- Impact of peripheral conditioning on reperfusion injury following primary percutaneous coronary intervention in diabetic and non-diabetic STEMI patients
- Clinical efficacy of azacitidine in the treatment of middle- and high-risk myelodysplastic syndrome in middle-aged and elderly patients: A retrospective study
- The effect of ambulatory blood pressure load on mitral regurgitation in continuous ambulatory peritoneal dialysis patients
- Expression and clinical significance of ITGA3 in breast cancer
- Single-nucleus RNA sequencing reveals ARHGAP28 expression of podocytes as a biomarker in human diabetic nephropathy
- rSIG combined with NLR in the prognostic assessment of patients with multiple injuries
- Toxic metals and metalloids in collagen supplements of fish and jellyfish origin: Risk assessment for daily intake
- Exploring causal relationship between 41 inflammatory cytokines and marginal zone lymphoma: A bidirectional Mendelian randomization study
- Gender beliefs and legitimization of dating violence in adolescents
- Effect of serum IL-6, CRP, and MMP-9 levels on the efficacy of modified preperitoneal Kugel repair in patients with inguinal hernia
- Effect of smoking and smoking cessation on hematological parameters in polycythemic patients
- Pathogen surveillance and risk factors for pulmonary infection in patients with lung cancer: A retrospective single-center study
- Necroptosis of hippocampal neurons in paclitaxel chemotherapy-induced cognitive impairment mediates microglial activation via TLR4/MyD88 signaling pathway
- Celastrol suppresses neovascularization in rat aortic vascular endothelial cells stimulated by inflammatory tenocytes via modulating the NLRP3 pathway
- Cord-lamina angle and foraminal diameter as key predictors of C5 palsy after anterior cervical decompression and fusion surgery
- GATA1: A key biomarker for predicting the prognosis of patients with diffuse large B-cell lymphoma
- Influencing factors of false lumen thrombosis in type B aortic dissection: A single-center retrospective study
- MZB1 regulates the immune microenvironment and inhibits ovarian cancer cell migration
- Integrating experimental and network pharmacology to explore the pharmacological mechanisms of Dioscin against glioblastoma
- Trends in research on preterm birth in twin pregnancy based on bibliometrics
- Four-week IgE/baseline IgE ratio combined with tryptase predicts clinical outcome in omalizumab-treated children with moderate-to-severe asthma
- Single-cell transcriptomic analysis identifies a stress response Schwann cell subtype
- Acute pancreatitis risk in the diagnosis and management of inflammatory bowel disease: A critical focus
- Effect of subclinical esketamine on NLRP3 and cognitive dysfunction in elderly ischemic stroke patients
- Interleukin-37 mediates the anti-oral tumor activity in oral cancer through STAT3
- CA199 and CEA expression levels, and minimally invasive postoperative prognosis analysis in esophageal squamous carcinoma patients
- Efficacy of a novel drainage catheter in the treatment of CSF leak after posterior spine surgery: A retrospective cohort study
- Comprehensive biomedicine assessment of Apteranthes tuberculata extracts: Phytochemical analysis and multifaceted pharmacological evaluation in animal models
- Relation of time in range to severity of coronary artery disease in patients with type 2 diabetes: A cross-sectional study
- Dopamine attenuates ethanol-induced neuronal apoptosis by stimulating electrical activity in the developing rat retina
- Correlation between albumin levels during the third trimester and the risk of postpartum levator ani muscle rupture
- Factors associated with maternal attention and distraction during breastfeeding and childcare: A cross-sectional study in the west of Iran
- Mechanisms of hesperetin in treating metabolic dysfunction-associated steatosis liver disease via network pharmacology and in vitro experiments
- The law on oncological oblivion in the Italian and European context: How to best uphold the cancer patients’ rights to privacy and self-determination?
- The prognostic value of the neutrophil-to-lymphocyte ratio, platelet-to-lymphocyte ratio, and prognostic nutritional index for survival in patients with colorectal cancer
- Factors affecting the measurements of peripheral oxygen saturation values in healthy young adults
- Comparison and correlations between findings of hysteroscopy and vaginal color Doppler ultrasonography for detection of uterine abnormalities in patients with recurrent implantation failure
- The effects of different types of RAGT on balance function in stroke patients with low levels of independent walking in a convalescent rehabilitation hospital
- Causal relationship between asthma and ankylosing spondylitis: A bidirectional two-sample univariable and multivariable Mendelian randomization study
- Correlations of health literacy with individuals’ understanding and use of medications in Southern Taiwan
- Correlation of serum calprotectin with outcome of acute cerebral infarction
- Comparison of computed tomography and guided bronchoscopy in the diagnosis of pulmonary nodules: A systematic review and meta-analysis
- Curdione protects vascular endothelial cells and atherosclerosis via the regulation of DNMT1-mediated ERBB4 promoter methylation
- The identification of novel missense variant in ChAT gene in a patient with gestational diabetes denotes plausible genetic association
- Molecular genotyping of multi-system rare blood types in foreign blood donors based on DNA sequencing and its clinical significance
- Exploring the role of succinyl carnitine in the association between CD39⁺ CD4⁺ T cell and ulcerative colitis: A Mendelian randomization study
- Dexmedetomidine suppresses microglial activation in postoperative cognitive dysfunction via the mmu-miRNA-125/TRAF6 signaling axis
- Analysis of serum metabolomics in patients with different types of chronic heart failure
- Diagnostic value of hematological parameters in the early diagnosis of acute cholecystitis
- Pachymaran alleviates fat accumulation, hepatocyte degeneration, and injury in mice with nonalcoholic fatty liver disease
- Decrease in CD4 and CD8 lymphocytes are predictors of severe clinical picture and unfavorable outcome of the disease in patients with COVID-19
- METTL3 blocked the progression of diabetic retinopathy through m6A-modified SOX2
- The predictive significance of anti-RO-52 antibody in patients with interstitial pneumonia after treatment of malignant tumors
- Exploring cerebrospinal fluid metabolites, cognitive function, and brain atrophy: Insights from Mendelian randomization
- Development and validation of potential molecular subtypes and signatures of ocular sarcoidosis based on autophagy-related gene analysis
- Widespread venous thrombosis: Unveiling a complex case of Behçet’s disease with a literature perspective
- Uterine fibroid embolization: An analysis of clinical outcomes and impact on patients’ quality of life
- Discovery of lipid metabolism-related diagnostic biomarkers and construction of diagnostic model in steroid-induced osteonecrosis of femoral head
- Serum-derived exomiR-188-3p is a promising novel biomarker for early-stage ovarian cancer
- Enhancing chronic back pain management: A comparative study of ultrasound–MRI fusion guidance for paravertebral nerve block
- Peptide CCAT1-70aa promotes hepatocellular carcinoma proliferation and invasion via the MAPK/ERK pathway
- Electroacupuncture-induced reduction of myocardial ischemia–reperfusion injury via FTO-dependent m6A methylation modulation
- Hemorrhoids and cardiovascular disease: A bidirectional Mendelian randomization study
- Cell-free adipose extract inhibits hypertrophic scar formation through collagen remodeling and antiangiogenesis
- HALP score in Demodex blepharitis: A case–control study
- Assessment of SOX2 performance as a marker for circulating cancer stem-like cells (CCSCs) identification in advanced breast cancer patients using CytoTrack system
- Risk and prognosis for brain metastasis in primary metastatic cervical cancer patients: A population-based study
- Comparison of the two intestinal anastomosis methods in pediatric patients
- Factors influencing hematological toxicity and adverse effects of perioperative hyperthermic intraperitoneal vs intraperitoneal chemotherapy in gastrointestinal cancer
- Endotoxin tolerance inhibits NLRP3 inflammasome activation in macrophages of septic mice by restoring autophagic flux through TRIM26
- Lateral transperitoneal laparoscopic adrenalectomy: A single-centre experience of 21 procedures
- Petunidin attenuates lipopolysaccharide-induced retinal microglia inflammatory response in diabetic retinopathy by targeting OGT/NF-κB/LCN2 axis
- Procalcitonin and C-reactive protein as biomarkers for diagnosing and assessing the severity of acute cholecystitis
- Factors determining the number of sessions in successful extracorporeal shock wave lithotripsy patients
- Development of a nomogram for predicting cancer-specific survival in patients with renal pelvic cancer following surgery
- Inhibition of ATG7 promotes orthodontic tooth movement by regulating the RANKL/OPG ratio under compression force
- A machine learning-based prognostic model integrating mRNA stemness index, hypoxia, and glycolysis‑related biomarkers for colorectal cancer
- Glutathione attenuates sepsis-associated encephalopathy via dual modulation of NF-κB and PKA/CREB pathways
- FAHD1 prevents neuronal ferroptosis by modulating R-loop and the cGAS–STING pathway
- Association of placenta weight and morphology with term low birth weight: A case–control study
- Investigation of the pathogenic variants induced Sjogren’s syndrome in Turkish population
- Nucleotide metabolic abnormalities in post-COVID-19 condition and type 2 diabetes mellitus patients and their association with endocrine dysfunction
- TGF-β–Smad2/3 signaling in high-altitude pulmonary hypertension in rats: Role and mechanisms via macrophage M2 polarization
- Ultrasound-guided unilateral versus bilateral erector spinae plane block for postoperative analgesia of patients undergoing laparoscopic cholecystectomy
- Profiling gut microbiome dynamics in subacute thyroiditis: Implications for pathogenesis, diagnosis, and treatment
- Delta neutrophil index, CRP/albumin ratio, procalcitonin, immature granulocytes, and HALP score in acute appendicitis: Best performing biomarker?
- Anticancer activity mechanism of novelly synthesized and characterized benzofuran ring-linked 3-nitrophenyl chalcone derivative on colon cancer cells
- H2valdien3 arrests the cell cycle and induces apoptosis of gastric cancer
- Prognostic relevance of PRSS2 and its immune correlates in papillary thyroid carcinoma
- Association of SGLT2 inhibition with psychiatric disorders: A Mendelian randomization study
- Motivational interviewing for alcohol use reduction in Thai patients
- Luteolin alleviates oxygen-glucose deprivation/reoxygenation-induced neuron injury by regulating NLRP3/IL-1β signaling
- Polyphyllin II inhibits thyroid cancer cell growth by simultaneously inhibiting glycolysis and oxidative phosphorylation
- Relationship between the expression of copper death promoting factor SLC31A1 in papillary thyroid carcinoma and clinicopathological indicators and prognosis
- CSF2 polarized neutrophils and invaded renal cancer cells in vitro influence
- Proton pump inhibitors-induced thrombocytopenia: A systematic literature analysis of case reports
- The current status and influence factors of research ability among community nurses: A sequential qualitative–quantitative study
- OKAIN: A comprehensive oncology knowledge base for the interpretation of clinically actionable alterations
- The relationship between serum CA50, CA242, and SAA levels and clinical pathological characteristics and prognosis in patients with pancreatic cancer
- Identification and external validation of a prognostic signature based on hypoxia–glycolysis-related genes for kidney renal clear cell carcinoma
- Engineered RBC-derived nanovesicles functionalized with tumor-targeting ligands: A comparative study on breast cancer targeting efficiency and biocompatibility
- Relationship of resting echocardiography combined with serum micronutrients to the severity of low-gradient severe aortic stenosis
- Effect of vibration on pain during subcutaneous heparin injection: A randomized, single-blind, placebo-controlled trial
- The diagnostic performance of machine learning-based FFRCT for coronary artery disease: A meta-analysis
- Comparing biofeedback device vs diaphragmatic breathing for bloating relief: A randomized controlled trial
- Serum uric acid to albumin ratio and C-reactive protein as predictive biomarkers for chronic total occlusion and coronary collateral circulation quality
- Multiple organ scoring systems for predicting in-hospital mortality of sepsis patients in the intensive care unit
- Single-cell RNA sequencing data analysis of the inner ear in gentamicin-treated mice via intraperitoneal injection
- Review Articles
- The effects of enhanced external counter-pulsation on post-acute sequelae of COVID-19: A narrative review
- Diabetes-related cognitive impairment: Mechanisms, symptoms, and treatments
- Microscopic changes and gross morphology of placenta in women affected by gestational diabetes mellitus in dietary treatment: A systematic review
- Review of mechanisms and frontier applications in IL-17A-induced hypertension
- Research progress on the correlation between islet amyloid peptides and type 2 diabetes mellitus
- The safety and efficacy of BCG combined with mitomycin C compared with BCG monotherapy in patients with non-muscle-invasive bladder cancer: A systematic review and meta-analysis
- The application of augmented reality in robotic general surgery: A mini-review
- The effect of Greek mountain tea extract and wheat germ extract on peripheral blood flow and eicosanoid metabolism in mammals
- Neurogasobiology of migraine: Carbon monoxide, hydrogen sulfide, and nitric oxide as emerging pathophysiological trinacrium relevant to nociception regulation
- Plant polyphenols, terpenes, and terpenoids in oral health
- Laboratory medicine between technological innovation, rights safeguarding, and patient safety: A bioethical perspective
- End-of-life in cancer patients: Medicolegal implications and ethical challenges in Europe
- The maternal factors during pregnancy for intrauterine growth retardation: An umbrella review
- Intra-abdominal hypertension/abdominal compartment syndrome of pediatric patients in critical care settings
- PI3K/Akt pathway and neuroinflammation in sepsis-associated encephalopathy
- Screening of Group B Streptococcus in pregnancy: A systematic review for the laboratory detection
- Giant borderline ovarian tumours – review of the literature
- Leveraging artificial intelligence for collaborative care planning: Innovations and impacts in shared decision-making – A systematic review
- Cholera epidemiology analysis through the experience of the 1973 Naples epidemic
- Risk factors of frailty/sarcopenia in community older adults: Meta-analysis
- Supplement strategies for infertility in overweight women: Evidence and legal insights
- Scurvy, a not obsolete disorder: Clinical report in eight young children and literature review
- A meta-analysis of the effects of DBS on cognitive function in patients with advanced PD
- Protective role of selenium in sepsis: Mechanisms and potential therapeutic strategies
- Strategies for hyperkalemia management in dialysis patients: A systematic review
- C-reactive protein-to-albumin ratio in peripheral artery disease
- Case Reports
- Delayed graft function after renal transplantation
- Semaglutide treatment for type 2 diabetes in a patient with chronic myeloid leukemia: A case report and review of the literature
- Diverse electrophysiological demyelinating features in a late-onset glycogen storage disease type IIIa case
- Giant right atrial hemangioma presenting with ascites: A case report
- Laser excision of a large granular cell tumor of the vocal cord with subglottic extension: A case report
- EsoFLIP-assisted dilation for dysphagia in systemic sclerosis: Highlighting the role of multimodal esophageal evaluation
- Molecular hydrogen-rhodiola as an adjuvant therapy for ischemic stroke in internal carotid artery occlusion: A case report
- Coronary artery anomalies: A case of the “malignant” left coronary artery and its surgical management
- Rapid Communication
- Biological properties of valve materials using RGD and EC
-
A single oral administration of flavanols enhances short
-term memory in mice along with increased brain-derived neurotrophic factor - Letter to the Editor
- Role of enhanced external counterpulsation in long COVID
- Expression of Concern
- Expression of concern “A ceRNA network mediated by LINC00475 in papillary thyroid carcinoma”
- Expression of concern “Notoginsenoside R1 alleviates spinal cord injury through the miR-301a/KLF7 axis to activate Wnt/β-catenin pathway”
- Expression of concern “circ_0020123 promotes cell proliferation and migration in lung adenocarcinoma via PDZD8”
- Corrigendum
- Corrigendum to “Empagliflozin improves aortic injury in obese mice by regulating fatty acid metabolism”
- Corrigendum to “Comparing the therapeutic efficacy of endoscopic minimally invasive surgery and traditional surgery for early-stage breast cancer: A meta-analysis”
- Corrigendum to “The progress of autoimmune hepatitis research and future challenges”
- Retraction
- Retraction of “miR-654-5p promotes gastric cancer progression via the GPRIN1/NF-κB pathway”
- Retraction of: “LncRNA CASC15 inhibition relieves renal fibrosis in diabetic nephropathy through downregulating SP-A by sponging to miR-424”
- Retraction of: “SCARA5 inhibits oral squamous cell carcinoma via inactivating the STAT3 and PI3K/AKT signaling pathways”
- Special Issue Advancements in oncology: bridging clinical and experimental research - Part II
- Unveiling novel biomarkers for platinum chemoresistance in ovarian cancer
- Lathyrol affects the expression of AR and PSA and inhibits the malignant behavior of RCC cells
- The era of increasing cancer survivorship: Trends in fertility preservation, medico-legal implications, and ethical challenges
- Bone scintigraphy and positron emission tomography in the early diagnosis of MRONJ
- Meta-analysis of clinical efficacy and safety of immunotherapy combined with chemotherapy in non-small cell lung cancer
- Special Issue Computational Intelligence Methodologies Meets Recurrent Cancers - Part IV
- Exploration of mRNA-modifying METTL3 oncogene as momentous prognostic biomarker responsible for colorectal cancer development
- Special Issue The evolving saga of RNAs from bench to bedside - Part III
- Interaction and verification of ferroptosis-related RNAs Rela and Stat3 in promoting sepsis-associated acute kidney injury
- The mRNA MOXD1: Link to oxidative stress and prognostic significance in gastric cancer
- Special Issue Exploring the biological mechanism of human diseases based on MultiOmics Technology - Part II
- Dynamic changes in lactate-related genes in microglia and their role in immune cell interactions after ischemic stroke
- A prognostic model correlated with fatty acid metabolism in Ewing’s sarcoma based on bioinformatics analysis
- Red cell distribution width predicts early kidney injury: A NHANES cross-sectional study
- Special Issue Diabetes mellitus: pathophysiology, complications & treatment
- Nutritional risk assessment and nutritional support in children with congenital diabetes during surgery
- Correlation of the differential expressions of RANK, RANKL, and OPG with obesity in the elderly population in Xinjiang
- A discussion on the application of fluorescence micro-optical sectioning tomography in the research of cognitive dysfunction in diabetes
- A review of brain research on T2DM-related cognitive dysfunction
- Metformin and estrogen modulation in LABC with T2DM: A 36-month randomized trial
- Special Issue Innovative Biomarker Discovery and Precision Medicine in Cancer Diagnostics
- CircASH1L-mediated tumor progression in triple-negative breast cancer: PI3K/AKT pathway mechanisms


