Abstract
Objective
This study aims to comprehensively evaluate the Charlson Comorbidity Index (CCI), Logistic Organ Dysfunction System (LODS) score, Acute Physiology Score III (APS III), Simplified Acute Physiology Score II (SAPS II), and Sequential Organ Failure Assessment (SOFA) in order to provide a more scientifically rigorous and effective tool for predicting mortality risk among sepsis patients in the Intensive Care Unit (ICU).
Methods
The demographic information and sepsis-related data were extracted from the MIMIC-IV database for patients admitted to the ICU with a diagnosis of sepsis. The predictive performance of CCI, LODS, APS III, SAPS II, and SOFA scoring systems in terms of ICU mortality was evaluated by comparing receiver operating characteristic (ROC) curves. Multivariate regression identified predictors, later validated with a nomogram. Finally, the dataset was divided into a training set and a validation set at a ratio of 7:3 to assess the clinical utility of the prediction model through ROC curves.
Results
The study enrolled a total of 17,226 patients with a median age of 67.65 (55.79, 78.82) years; among them, males accounted for 57.69%. Within this cohort, a total of 1,115 (6.47%) individuals succumbed during their admission to the ICU. The ROC curve demonstrated that both APS III and LODS score exhibited robust predictive value for ICU mortality. Multivariate regression analysis revealed that CCI, APS III score, LODS score, respiratory rate, body temperature, and race served as potential predictors. Combining these variables into a nomogram showed strong clinical utility, with AUCs of 0.803 (training set) and 0.797 (validation set).
Conclusions
Organ failure scores hold significant clinical relevance in predicting mortality among sepsis patients in the ICU. Augmenting predictive accuracy can be achieved by integrating the CCI, APS III score, LODS score, mean respiratory rate, and body temperature during the initial 24 h following ICU admission.
1 Introduction
Sepsis arises from an exaggerated immune response to infection, leading to tissue damage, organ dysfunction, and systemic inflammation [1]. The incidence and mortality rates of sepsis are increasing, presenting a significant challenge to global public health [2]. Sepsis accounts for 30–50% of Intensive Care Unit (ICU) fatalities, making it a leading cause of death in critical care [3,4,5,6].
In light of the significant mortality rate associated with sepsis, timely and accurate assessment of patients’ condition and risk of death is crucial for improving survival rates [7]. In clinical practice, physicians commonly utilize various scoring systems to evaluate the severity and prognosis of septic patients. These scoring systems include, but are not limited to, the Charlson Comorbidity Index (CCI) [8,9], Logistic Organ Dysfunction System (LODS) [10], Acute Physiology Score III (APS III) [11], Simplified Acute Physiology Score II (SAPS II) [12,13], and Sequential Organ Failure Assessment (SOFA) scoring systems [14]. Scoring systems, serving as a pivotal tool in quantifying the severity of a patient’s condition, assume an indispensable role in critical care medicine by employing physiological parameters, laboratory indexes, and other relevant clinical indicators to calculate a numerical value that predicts the patient’s risk of mortality [15,16,17]. Scoring systems prioritize different clinical aspects [18]. For example, the CCI primarily evaluates patients’ comorbidities [19], while the LODS and APS III focus more on the physiological condition of the patient [18,20]. In contrast, SAPS II and SOFA incorporate broader clinical parameters [20,21].
However, despite the pivotal role played by these scoring systems in predicting patient outcomes in sepsis, disparities exist in their respective levels of accuracy. Moreover, due to the intricate and dynamic nature of sepsis patients’ conditions, a singular scoring system often encounters challenges when attempting to comprehensively and accurately reflect their true state [22]. Consequently, the selection and utilization of these scoring systems as well as the integration of multiple system results have emerged as prominent issues within current clinical research for more precise assessment of mortality risk in sepsis patients. Recent studies have highlighted the prognostic value of various inflammatory markers in ICU patients. Mean platelet volume reflects platelet activation and correlates with disease severity and mortality [23]. The neutrophil-to-lymphocyte ratio serves as a marker of systemic inflammation linked to poor outcomes [24]. C-reactive protein (CRP), an acute-phase protein, is associated with inflammation and mortality risk [25]. Platelet distribution width, which measures platelet size variation, is linked to thrombotic risk and inflammation [26]. Despite the potential of these markers, existing scoring systems for predicting ICU mortality do not fully integrate them.
In conclusion, the objective of this study was to elucidate the prognostic value of each scoring system in assessing mortality risk among sepsis patients during their ICU stay. By conducting a comprehensive evaluation of the CCI, LODS, APS III, SAPS II, and SOFA scoring systems, while considering vital signs monitoring alongside multiple scoring systems, our aim is to provide a more scientifically robust and effective clinical prediction tool for evaluating the risk of mortality in sepsis.
2 Methods and methods
2.1 Study design
The data for this study were extracted from the Medical Information Mart for Intensive Care-IV (MIMIC-IV) database, encompassing comprehensive clinical information on a cohort of more than 190,000 patients and 450,000 hospitalizations admitted to Beth Israel Deaconess Medical Center (BIDMC) between 2008 and 2019 [24]. This extensive database comprises patient demographic details, laboratory test results, medication records, vital signs measurements, surgical procedures performed, disease diagnosis, drug management specifics, follow-up survival status updates, as well as other pertinent information. This study presents an analysis of a publicly available database, for which no approval from the Institutional Review Board of Jianhu County branch of Northern Jiangsu People’s Hospital was deemed necessary.
Patients admitted to the ICU for the first time with a diagnosis of sepsis were included with information from MIMIC-IV. The inclusion criteria were as follows: (1) Over 18 years of age and (2) diagnosis with sepsis. The exclusion criteria were defined as follows: patients who (1) with previous history of hospitalization, (2) duration of the ICU stay less than 24 h, and (3) with malignant tumors.
2.2 Date extraction
The diagnosis of sepsis was made in accordance with the sepsis-3 criteria [25]. The demographic information, encompassing age, gender, ethnicity, and body mass index (BMI), was extracted from the database utilizing Navicate Premium 16.0. The CCI, LODS, SOFA, APS III, SAPS II, GCS scores, and laboratory parameters including creatine were evaluated 24 h post admission to the ICU. For variables with multiple measurements, the mean value was used.
A patient was considered to have expired in the ICU if their time of death coincided with their discharge time from the ICU. If these times coincided, it was concluded that the patient deceased during their stay in the ICU; otherwise, they were considered to be alive.
2.3 Statistical analysis
Measurement data that followed a normal distribution were presented as Mean ± SD. For data with equal variances, a T-test was utilized to compare two groups. In cases where the measurement data did not conform to a normal distribution, quartiles and median values were used instead, and differences between any two groups were compared using the Mann–Whitney test. Count data were expressed in terms of frequencies and proportions, with group differences assessed through chi-square testing. Statistical significance was established when P < 0.05.
The predictive efficacy of each scoring system for ICU sepsis patients’ mortality was assessed using receiver operating characteristic (ROC) curve analysis. Potential predictors, including vital signs, laboratory parameters, and scores, were identified through regression analysis. The variables exhibiting a significance level of P < 0.05 in the univariate regression analysis were incorporated into the multivariate regression analysis and examined using the two-way stepwise regression method. A nomogram was employed to present the final combined score and baseline characteristics of the patients. Furthermore, a training set and validation set were created by dividing the dataset in a 7:3 ratio. The performance of the final model was validated using ROC curve analysis.
-
Ethical approval: This study is an analysis of a public database. Approval from the Institutional Review Board was not required.
-
Consent for publication: Not applicable.
3 Results
3.1 Clinical characteristics of patients with sepsis
The process of data extraction and screening was carried out following the workflow illustrated in Figure 1. A total of 24,816 adult patients were diagnosed with sepsis and admitted to the hospital for their initial presentation. After excluding 2,658 patients with a history of prior hospitalization, 3,051 patients with malignancy, and 1,881 patients who stayed in the ICU for less than 24 h, a total of 17,226 eligible patients were enrolled. Among them, 1,115 patients (6.47%) succumbed during their stay in the ICU. The enrolled patients had a median age of 67.65 (55.79, 78.82) years, with males accounting for 57.69% of the cohort. The baseline characteristics of the enrolled patients are presented in Table 1.
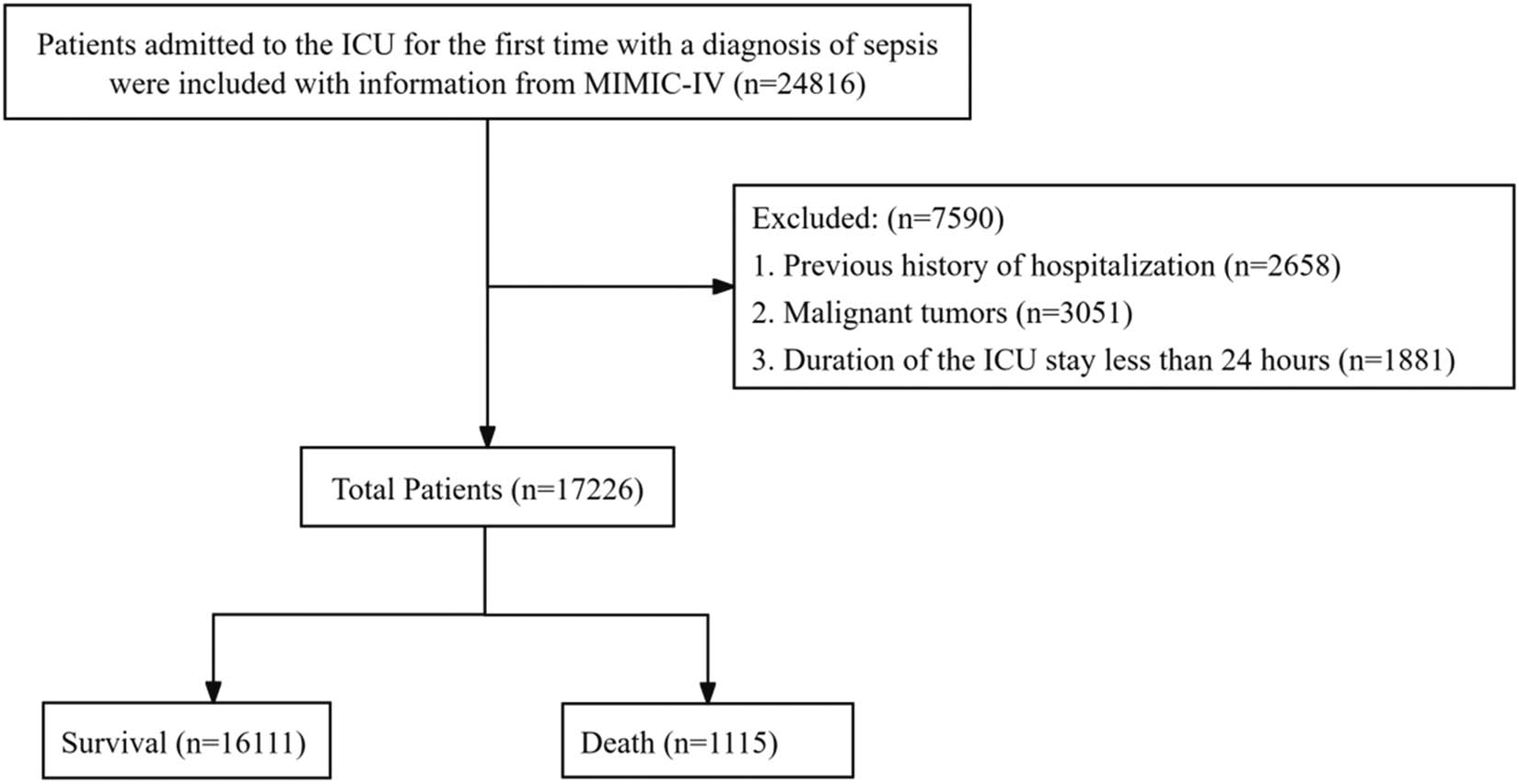
The process of information extraction and the screening criteria for sepsis patients.
Baseline data of the enrolled patients
| Variables | Total (n = 17,226) | Survival (n = 16,111) | Death (n = 1,115) | Statistic | P |
|---|---|---|---|---|---|
| Age, Years, M (Q 1, Q 3) | 67.65 (55.79, 78.82) | 67.51 (55.69, 78.64) | 70.16 (57.23, 81.64) | Z = −4.29 | <0.001 |
| Gender, n (%) | χ 2 = 4.59 | 0.032 | |||
| Female | 7,289 (42.31) | 6,783 (42.10) | 506 (45.38) | ||
| Male | 9,937 (57.69) | 9,328 (57.90) | 609 (54.62) | ||
| Race, n (%) | χ 2 = 236.70 | <0.001 | |||
| Asian | 438 (2.54) | 411 (2.55) | 27 (2.42) | ||
| Black | 1,306 (7.58) | 1,229 (7.63) | 77 (6.91) | ||
| White | 11,450 (66.47) | 10,867 (67.45) | 583 (52.29) | ||
| Hispanic/Latino | 550 (3.19) | 518 (3.22) | 32 (2.87) | ||
| Other | 744 (4.32) | 706 (4.38) | 38 (3.41) | ||
| Unknown | 2,738 (15.89) | 2,380 (14.77) | 358 (32.11) | ||
| BMI, kg/m2, M (Q 1, Q 3) | 28.30 (24.60, 33.10) | 28.40 (24.60, 33.10) | 27.90 (24.13, 32.90) | Z = 2.02 | 0.043 |
| SOFA, score, M (Q 1, Q 3) | 3.00 (2.00, 4.00) | 3.00 (2.00, 4.00) | 4.00 (2.00, 6.00) | Z = −12.29 | <0.001 |
| CCI, score, M (Q 1, Q 3) | 4.00 (3.00, 6.00) | 4.00 (3.00, 6.00) | 5.00 (3.00, 7.00) | Z = −9.43 | <0.001 |
| Creatinine, mg/dL, M(Q 1, Q 3) | 1.00 (0.70, 1.50) | 1.00 (0.70, 1.50) | 1.30 (0.90, 2.10) | Z = −13.90 | <0.001 |
| GCS, score, M (Q 1, Q 3) | 15.00 (15.00, 15.00) | 15.00 (15.00, 15.00) | 15.00 (15.00, 15.00) | Z = −0.81 | 0.415 |
| APS III, score, M (Q 1, Q 3) | 45.00 (33.00, 60.00) | 44.00 (32.00, 59.00) | 66.00 (50.00, 88.00) | Z = −28.63 | <0.001 |
| LODS, score, M (Q 1, Q 3) | 5.00 (3.00, 7.00) | 5.00 (3.00, 7.00) | 8.00 (6.00, 10.00) | Z = −29.01 | <0.001 |
| SAPS II, score, M (Q 1, Q 3) | 37.00 (30.00, 47.00) | 37.00 (29.00, 46.00) | 49.00 (39.00, 61.00) | Z = −26.20 | <0.001 |
| Heart Rate, bpm, M (Q 1, Q 3) | 84.62 (75.39, 96.26) | 84.42 (75.33, 95.92) | 87.68 (76.44, 102.18) | Z = −5.71 | <0.001 |
| SBP, mmHg, M (Q 1, Q 3) | 113.54 (105.64, 124.04) | 113.79 (105.90, 124.17) | 110.08 (102.32, 122.32) | Z = −7.72 | <0.001 |
| DBP, mmHg, M (Q 1, Q 3) | 60.20 (54.45, 66.95) | 60.23 (54.52, 66.85) | 59.56 (53.03, 68.30) | Z = 1.12 | 0.262 |
| Respiratory rate, insp/min, M (Q 1, Q 3) | 18.80 (16.65, 21.73) | 18.68 (16.58, 21.54) | 20.78 (18.21, 24.32) | Z = −16.17 | <0.001 |
| Temperature, °C, M (Q 1, Q 3) | 36.87 (36.59, 37.23) | 36.87 (36.60, 37.23) | 36.76 (36.32, 37.20) | Z = 8.40 | <0.001 |
| Diabetes with complication, n (%) | χ 2 = 0.18 | 0.675 | |||
| No | 15,636 (90.77) | 14,620 (90.75) | 1,016 (91.12) | ||
| Yes | 1,590 (9.23) | 1,491 (9.25) | 99 (8.88) | ||
| Mechanical ventilation, n (%) | χ 2 = 47.05 | <0.001 | |||
| No | 5,748 (37.51) | 5,454 (38.25) | 294 (27.68) | ||
| Yes | 9,574 (62.49) | 8,806 (61.75) | 768 (72.32) |
M: Median; Q 1: 1st Quartile; Q 3: 3rd Quartile. Z: Mann–Whitney test; χ 2: Chi square test. BMI: Body Mass Index; SOFA: Sequential Organ Failure Assessment; CCI: Charlson Comorbidity Index; GCS: Glasgow Coma Scale; APS III: Acute Physiology Score III; LODS: Logistic Organ Dysfunction Score; SAPS II: Simplified Acute Physiology Score II; SBP: systolic blood pressure; DBP: diastolic blood pressure.
The death group exhibited significantly higher levels of age, CCI, LODS, SOFA, APS III, SAPS II scores, GCS scores, creatine levels, heart rate within 24 h of admission to ICU compared to the survival group (P < 0.001). However, the deceased group exhibited a lower BMI and mean body temperature during the initial 24-h period in the ICU compared to the survivor group. Additionally, the proportion of females (P = 0.032) and patients receiving mechanical ventilation (P < 0.001) in the death group were higher compared to those in the survival group.
3.2 The effectiveness of five scoring systems in predicting ICU mortality
The ROC curve demonstrated that both APS III (AUC: 0.756, P < 0.001) and LODS (AUC: 0.758, P < 0.001) score exhibited robust predictive value for ICU mortality. The AUC (0.734, P < 0.001) of the SAPS II score exhibited a slightly lower value compared to that of the APS III and LODS scores (Figure 2). Additionally, the sensitivity and specificity for each scoring system were as follows: APS III (sensitivity: 76.1%, specificity: 68.4%), LODS (sensitivity: 75.8%, specificity: 69.2%), SAPS II (sensitivity: 71.3%, specificity: 65.7%), SOFA (sensitivity: 67.5%, specificity: 63.9%), and CCI (sensitivity: 59.2%, specificity: 60.1%). Calibration metrics also indicated that APS III and LODS showed better agreement between predicted and observed outcomes compared to the other scoring systems (Table S2).
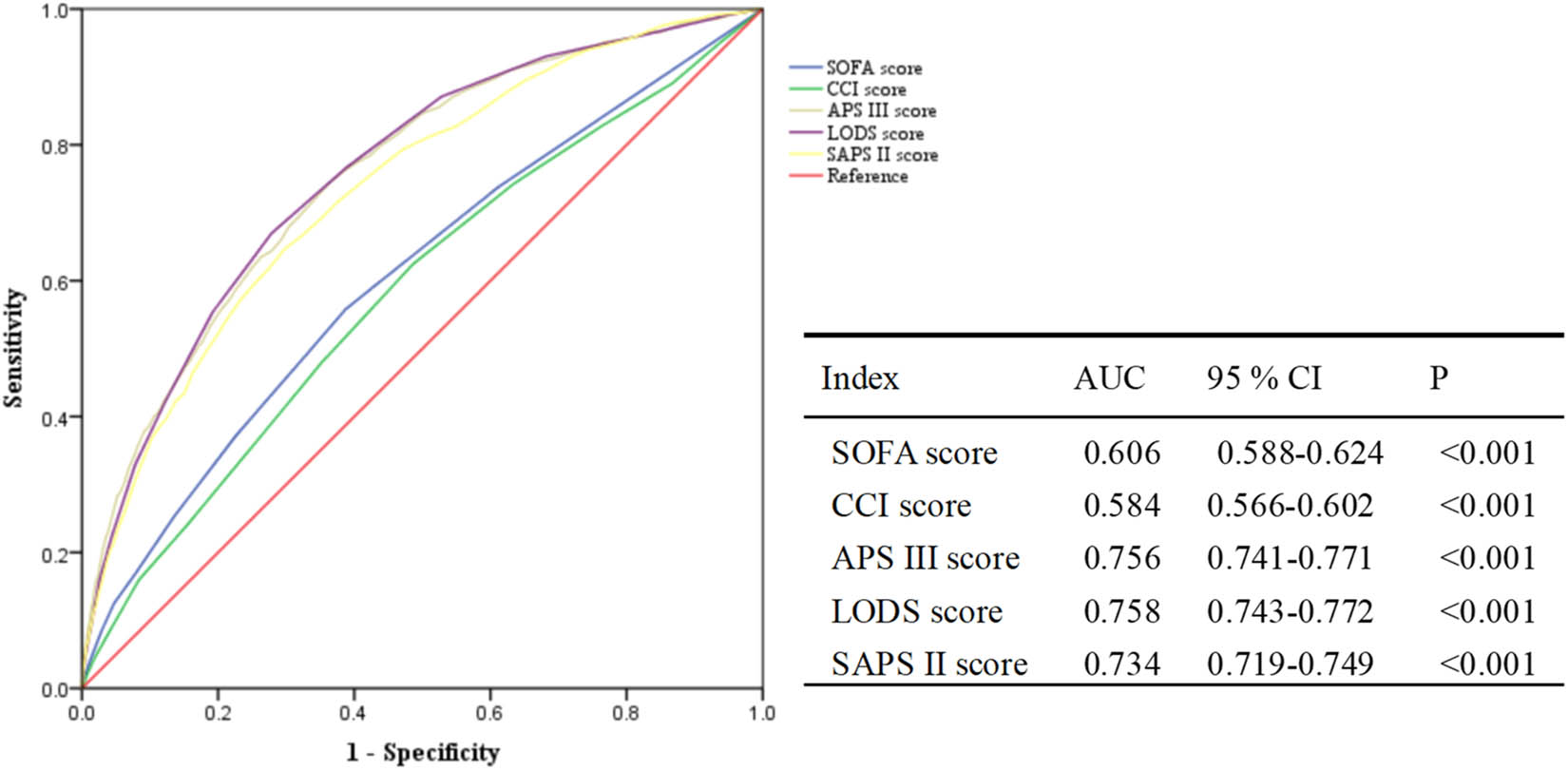
Prediction of mortality in septic ICU patients using multiple scoring systems. SOFA: Sequential Organ Failure Assessment; CCI: Charlson comorbidity index; APS III: Acute Physiology Score III; LODS: Logistic Organ Dysfunction Score; SAPS II: Simplified acute physiology score II; AUC: Area under the receiver operating characteristic curve; CI: confidence interval.
3.3 Regression analysis to identify potential factors
The potential predictors identified through univariate and multivariate regression analyses, with ICU mortality as the outcome, are presented in Table 2. Multivariate regression analysis revealed that CCI (OR = 1.10; 95% CI:(1.06, 1.14); P < 0.001), APS III score (OR = 1.01; 95% CI:(1.01, 1.02); P < 0.001), LODS score (OR = 1.14; 95% CI:(1.09, 1.20); P < 0.001), respiratory rate (OR = 1.07; 95% CI:(1.05, 1.10); P < 0.001), body temperature (OR = 0.75; 95% CI:(0.67, 0.85); P < 0.001), and unknown race (OR = 2.82; 95% CI:(2.27, 3.49); P < 0.001) served as potential predictors. The integration of these indicators into a nomogram demonstrated significant clinical relevance (Figure 3).
Screening of covariates as potential risk factors
| Variables | Univariate analysis | Multivariate analysis | ||||
|---|---|---|---|---|---|---|
| β | OR (95%CI) | P | β | OR (95%CI) | P | |
| Age, Years, M (Q 1, Q 3) | 0.01 | 1.01 (1.01, 1.01) | <0.001 | |||
| BMI, kg/m2, M (Q 1, Q 3) | −0.01 | 0.99 (0.98, 1.00) | 0.138 | |||
| SOFA, score, M (Q 1, Q 3) | 0.18 | 1.20 (1.16, 1.24) | <0.001 | |||
| CCI, score, M (Q 1, Q 3) | 0.11 | 1.12 (1.09, 1.15) | <0.001 | 0.09 | 1.10 (1.06, 1.14) | <0.001 |
| GCS, score, M (Q 1, Q 3) | 0.01 | 1.01 (0.97, 1.04) | 0.739 | |||
| APS III, score, M (Q 1, Q 3) | 0.04 | 1.04 (1.03, 1.04) | <0.001 | 0.01 | 1.01 (1.01, 1.02) | <0.001 |
| LODS, score, M (Q 1, Q 3) | 0.29 | 1.33 (1.30, 1.36) | <0.001 | 0.13 | 1.14 (1.09, 1.20) | <0.001 |
| SAPS II, score, M (Q 1, Q 3) | 0.06 | 1.06 (1.05, 1.06) | <0.001 | |||
| Heart Rate, bpm, M (Q 1, Q 3) | 0.01 | 1.01 (1.01, 1.02) | <0.001 | |||
| SBP, mmHg, M (Q 1, Q 3) | −0.01 | 0.99 (0.98, 0.99) | <0.001 | 0.01 | 1.01 (1.00, 1.01) | 0.102 |
| DBP, mmHg, M (Q 1, Q 3) | −0.00 | 1.00 (0.99, 1.00) | 0.481 | |||
| Respiratory rate, insp/min, M (Q 1, Q 3) | 0.11 | 1.12 (1.10, 1.13) | <0.001 | 0.07 | 1.07 (1.05, 1.10) | <0.001 |
| Temperature, °C, M (Q 1, Q 3) | −0.55 | 0.58 (0.52, 0.64) | <0.001 | −0.28 | 0.75 (0.67, 0.85) | <0.001 |
| Creatinine, mg/dL, M (Q 1, Q 3) | 0.10 | 1.11 (1.07, 1.14) | <0.001 | |||
| Gender | ||||||
| Male | Reference | |||||
| Female | 0.14 | 1.14 (0.99, 1.33) | 0.071 | |||
| Race | ||||||
| White | Reference | Reference | ||||
| Unknown | 1.06 | 2.90 (2.45, 3.42) | <0.001 | 1.04 | 2.82 (2.27, 3.49) | <0.001 |
| Hispanic/Latino | 0.03 | 1.03 (0.65, 1.64) | 0.891 | 0.21 | 1.24 (0.70, 2.18) | 0.460 |
| Black | 0.13 | 1.14 (0.85, 1.53) | 0.395 | 0.10 | 1.11 (0.75, 1.63) | 0.613 |
| Other | −0.11 | 0.90 (0.59, 1.36) | 0.615 | −0.12 | 0.89 (0.52, 1.51) | 0.668 |
| Asian | 0.09 | 1.09 (0.65, 1.82) | 0.746 | 0.04 | 1.04 (0.51, 2.14) | 0.907 |
| Diabetes with complication | ||||||
| No | Reference | |||||
| Yes | −0.06 | 0.94 (0.73, 1.21) | 0.634 | |||
| Mechanical ventilation | ||||||
| Yes | Reference | |||||
| No | −0.49 | 0.61 (0.52, 0.72) | <0.001 | |||
OR: odds ratio, CI: confidence interval. BMI: Body Mass Index; SOFA: Sequential Organ Failure Assessment; CCI: Charlson comorbidity index; GCS: Glasgow Coma Scale; APS III: Acute Physiology Score III; LODS: Logistic Organ Dysfunction Score; SAPS II: Simplified acute physiology score II; SBP: systolic blood pressure; DBP: diastolic blood pressure.
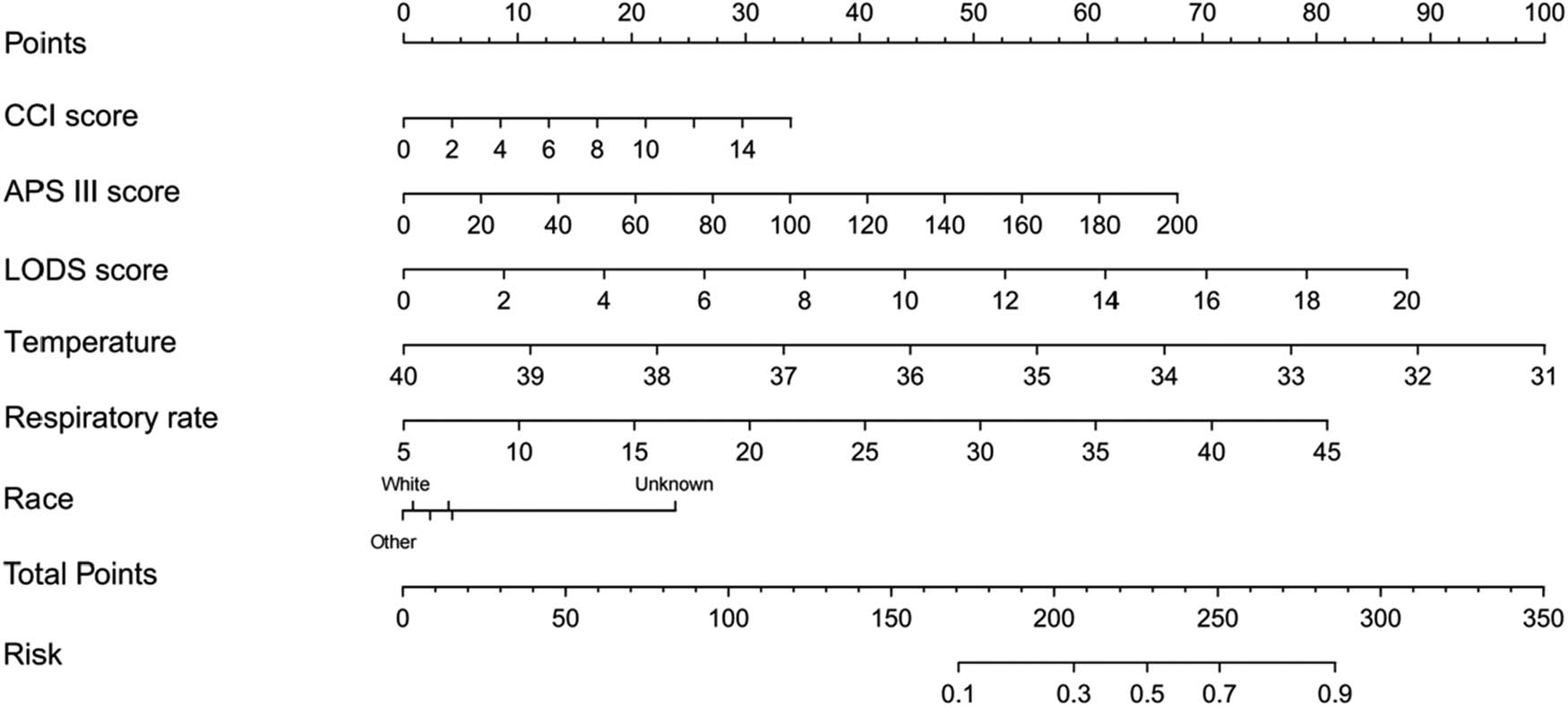
Nomogram for the prediction of death in the ICU. CCI: Charlson Comorbidity Index; APS III: Acute Physiology Score III; LODS: Logistic Organ Dysfunction Score.
3.4 Predictive performance assessed in training and validation sets
The training set comprised 12,058 patients, while the validation set included 5,168 patients. Table S1 presents a comparison of the characteristics between these two sets. The clinical data revealed no statistically significant disparities between the randomly allocated training set and the validation set.
The ROC curves achieved AUCs of 0.803 (training set) and 0.797 (validation set), indicating robust predictive performance. The training set demonstrated predictive sensitivities and specificities of 76.1 and 70.4%, respectively. In the validation set, corresponding sensitivities were observed to be 75.5 and 71.6% (Figure 4).
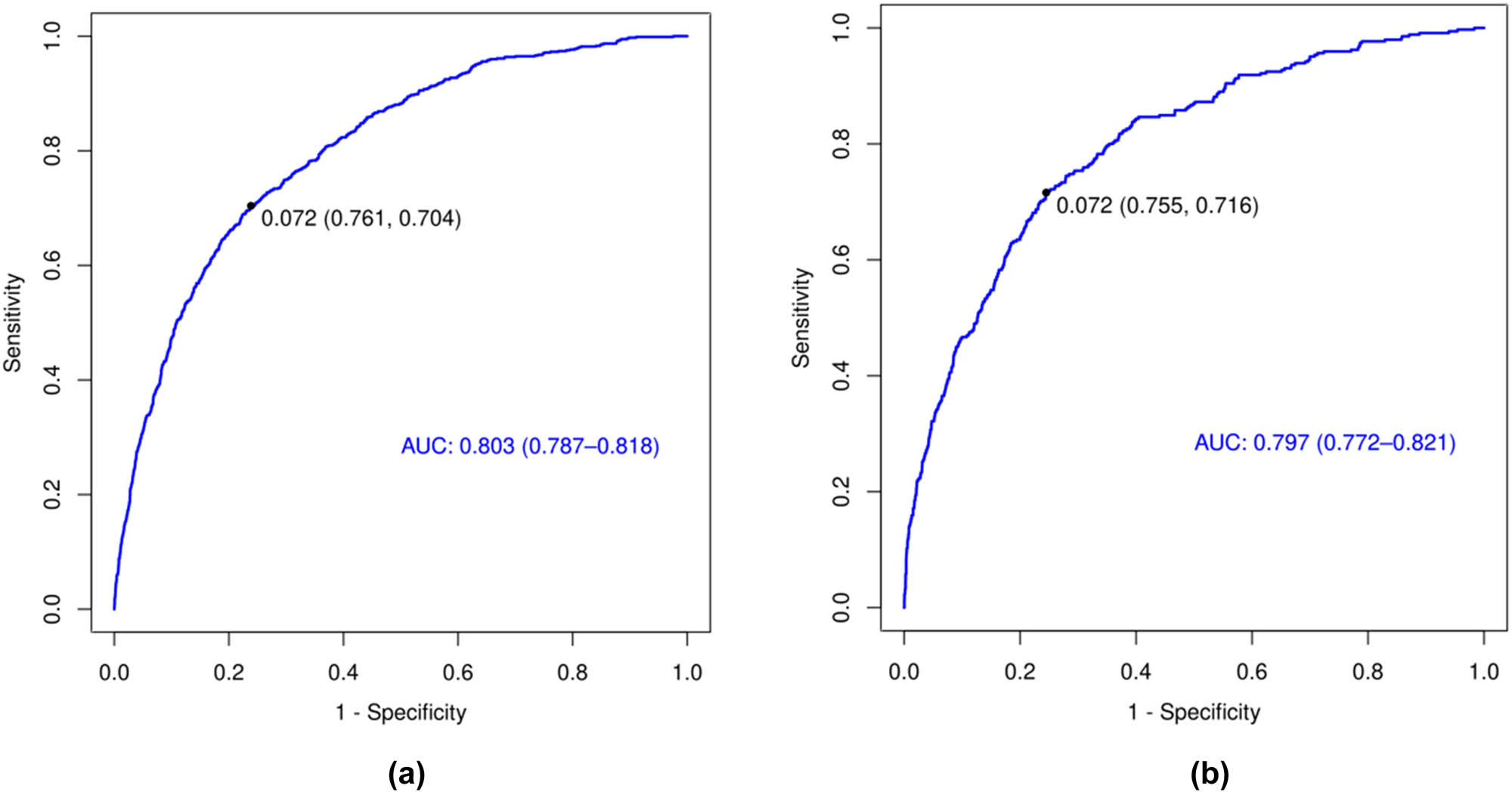
The performance of the prediction model in both the training and validation sets. (a) Evaluation of effectiveness in the training set; (b) assessment of performance in the validation set.
4 Discussion
The accurate prediction of mortality risk in sepsis has become imperative for optimizing patient survival, given its emergence as a predominant and lethal condition within the intensive care unit [26]. The objective of this study was to assess the efficacy of CCI, LODS, APS III, SAPS II, and SOFA scoring systems in predicting mortality among sepsis patients during their stay in the ICU. Retrospective analysis was conducted on clinical data from MIMIC-IV database to compare the predictive accuracy of these scoring systems. The findings of this investigation revealed variations in terms of accuracy among five scoring systems, indicating their prognostic capability for mortality prediction in septic patients. Notably, individual scoring systems such as APS III and LODS demonstrated significant predictive value. However, it is worth noting that a combination comprising CCI, APS III score, LODS score, average respiratory rate, and body temperature within 24 h after ICU admission along with race could further improve the accuracy of mortality risk predictions.
The APS III scoring system incorporates a range of physiological parameters, including blood pressure, body temperature, heart rate, respiratory rate, blood oxygen saturation, blood pH, serum electrolyte levels, and renal function indicators [27]. Each parameter is assigned a distinct score based on its correlation with the risk of mortality. By evaluating the APS III score of patients admitted to the ICU, physicians can promptly determine the severity of their condition and facilitate prognostication as well as evaluation of treatment response [28]. Additionally, the APS III score can serve as a valuable tool for assessing the effectiveness of various therapeutic interventions and guiding adjustments to clinical management plans [29]. The study also yielded consistent findings, demonstrating a remarkable predictive efficacy of a single APS III score in sepsis patients for ICU mortality with an AUC of 0.756.
The LODS scoring system encompasses six major organ systems, namely the respiratory, circulatory, hepatic, coagulation, nervous, and renal systems [30]. Each organ system’s dysfunction is accompanied by a corresponding scoring criterion. By measuring and evaluating the patient’s physiological parameters, the cumulative score can be computed to assess the extent of organ dysfunction [30,31]. The LODS scoring system has been shown to possess exceptional precision and reliability in predicting mortality risk among patients in the ICU, particularly those suffering from sepsis [32]. Similarly, in the present study, the prognostic efficacy of LODS on mortality in ICU septic patients was also substantial and superior to that of other scoring systems. When evaluating mortality in sepsis patients, the area under the curve (AUC) of the LODS score for predicting both 28-day and 90-day prognosis outperformed that of both SOFA and qSOFA scores [33]. Moreover, the admission of sepsis patients to the ICU is associated with an increased risk of in-hospital mortality, as evidenced by a higher LODS score [6].
The CCI scoring system consists of 19 major comorbid conditions, each assigned a weight ranging from 1 to 6 points based on its impact on the risk of mortality [34]. A higher cumulative score for a patient indicates an increased probability of death within the initial year. The CCI scoring system demonstrates certain predictive value in assessing mortality risk among patients [35]. The performance of CCI, however, was not satisfactory when solely evaluating mortality in septic patients during their stay in the ICU, aligning with findings from other studies [36]. The incorporation of CCI with other scoring systems enhances its efficacy in predicting both short-term and long-term mortality [36].
However, in this study, we did not observe a significant association between SAPS II and ICU mortality in septic patients. This may be attributed to the limited inclusion of comprehensive prognostic factors, such as immune and nutritional status of patients, within the current scoring system. Furthermore, potential changes in population demographics and treatment techniques could potentially compromise the predictive accuracy of the SAPS II scoring system, highlighting the necessity for periodic calibration and updates. Additionally, numerous studies have demonstrated that the SAPS II score exhibits a superior predictive value for mortality in ICU patients with non-septic shock compared to LODS [37,38]. The observed discrepancy in this study may be attributed to variations in the included covariates and the scoring system employed, which incorporates APS III and CCI. Zhu et al. employed six scoring systems to predict 28-day mortality in both general and specialized care units, with varying applicability across different types of ICU. For example, APS III or SAPS II can be utilized for predicting 28-day mortality in general ICUs, while the use of APS III or LODS is more effective in cardiovascular ICU for forecasting the risk of 28-day mortality [18]. The accuracy of predicting mortality risk in ICU patients with sepsis further improved by integrating multiple scoring systems with the physiological status of the patients in this study [39–41].
This study systematically compared and analyzed the value and efficacy of CCI, LODS, APS III, SAPS II, and SOFA scoring systems in predicting sepsis patient mortality within ICU settings. The findings demonstrate that although these scoring systems possess their individual strengths in prognosticating death risks among sepsis patients. Moreover, it is worth noting that a combination comprising CCI, APS III score, LODS score, average respiratory rate and body temperature within 24 h after ICU admission along with race could further improve the accuracy of mortality risk predictions. The inclusion of respiratory rate and temperature enhances the model by capturing dynamic physiological derangements not fully represented in static scoring systems like APS III. For example, hypothermia (<36°C) is strongly associated with immunosuppression and multi-organ failure in sepsis [42], while tachypnea may signal early respiratory compromise [43]. The inclusion of race as a predictor in our model requires careful interpretation. While race demonstrated statistical significance in predicting ICU mortality (P < 0.05), it is not a direct biological risk factor. Instead, race may serve as a surrogate for socioeconomic status, access to healthcare, or comorbidities that are associated with disparities in patient outcomes. For example, patients from certain racial backgrounds may experience barriers in accessing timely medical care or may have higher burdens of chronic diseases due to social determinants of health. These factors can indirectly influence mortality risk and thus contribute to the predictive power of race in our model. It is crucial to approach the use of race in predictive models with caution and to recognize the potential for confounding by these underlying social and economic factors. Future research should aim to disentangle the specific pathways through which race interacts with healthcare access and quality, socioeconomic status, and comorbidities to affect mortality outcomes. This would not only enhance the precision of predictive models but also inform interventions aimed at reducing healthcare disparities. While our nomogram leverages interpretable logistic regression, future studies should adopt ML techniques to refine variable selection and mitigate redundancy. For instance, LASSO regression could retain only non-overlapping predictors (e.g., APS III or respiratory rate), while tree-based methods (e.g., XGBoost) might identify novel interactions between scores and vital signs. Hybrid models combining ML-optimized features with clinician-friendly interfaces (e.g., SHAP values) could balance accuracy and interpretability. We propose that ML-driven approaches will be critical for advancing sepsis prediction models beyond the limitations of traditional scoring systems.
To translate our findings into practical clinical applications, we recommend integrating the nomogram into existing ICU protocols as a decision-support tool. The nomogram can serve as a valuable aid in identifying patients at high risk of mortality, allowing clinicians to prioritize resources and tailor interventions accordingly. For instance, patients with a predicted high mortality risk based on the nomogram could be monitored more closely, receive earlier intervention with evidence-based sepsis therapies, or be considered for enrollment in clinical trials exploring novel treatment approaches. Additionally, the nomogram can facilitate communication between healthcare providers and families by providing a data-driven prognosis, thereby supporting shared decision-making. It is important to note that while the nomogram offers a quantitative assessment, it should complement – rather than replace – clinical judgment. Future research could explore the implementation of such tools in electronic health record systems to streamline their use in busy ICU settings and further evaluate their impact on patient outcomes. The utilization of scoring systems not only facilitates physicians in making more precise risk assessments, but also provides guidance for clinical decision-making and resource allocation. For patients at high risk, physicians can potentially employ more aggressive treatment and intervention based on the scoring system results, thereby potentially reducing the patient’s mortality risk.
This study has certain limitations. First, the generalizability of our findings may be limited due to the use of data from the MIMIC-IV database, which is derived from a single US hospital system. Differences in patient demographics, such as age, comorbidities, and socioeconomic status, could influence the predictive performance of the scoring systems in other settings. Additionally, variations in sepsis management protocols, including differences in diagnostic criteria, treatment algorithms, and resource availability, may affect the applicability of our results. For example, healthcare systems with limited access to advanced monitoring equipment or specialized ICU care might observe different predictive accuracies for these scoring systems. Furthermore, cultural and regional differences in medical practice could also play a role in how these scoring systems perform in diverse populations. Future research should aim to validate these findings in multi-center datasets from different geographic regions to assess the generalizability of our conclusions across various healthcare settings. Additionally, it is important to consider that variations in adaptability and sensitivity among different scoring systems may exist due to differences in their original design and scoring elements. Furthermore, this study did not extensively explore the performance of these scoring systems in various sepsis subtypes or clinical scenarios. Therefore, future research could focus on comprehensively applying these scoring systems or developing new predictive models to further optimize risk assessment and management for patients with sepsis. The model did not account for dynamic interventions such as vasopressor use or fluid resuscitation, which may modulate mortality risk. For instance, delayed vasopressor initiation is associated with higher sepsis mortality, and fluid overload worsens outcomes in septic shock. Future studies should explore integrating these variables into longitudinal prediction models. Integrating biochemical markers such as lactate, procalcitonin, CRP, and IL-6 with clinical scoring systems could enhance predictive accuracy. These markers provide insights into critical pathological processes in sepsis. Future research should explore combining these markers with clinical data to improve risk stratification and guide clinical decision-making.
5 Conclusion
Organ failure scores hold significant clinical relevance in predicting mortality among sepsis patients in the ICU. Augmenting predictive accuracy can be achieved by integrating the CCI, APS III score, LODS score, mean respiratory rate, and body temperature during the initial 24 h following ICU admission.
Acknowledgments
Not Applicable.
-
Funding information: No funding source was identified for this study.
-
Author contributions: Xuan Zhou was responsible for the initial data extraction and preprocessing; Zhenen Zhang developed the algorithms for pattern recognition and anomaly detection within the medical data; Huimin Wang led the statistical analysis and interpretation of results; Pengfei Chen facilitated the integration of findings with existing medical knowledge, formulated the outline, and authored the paper.
-
Conflict of interest: The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
-
Data availability statement: All datasets used during the present study are publicly available in the MIMIC-IV v2.2 database (https://mimic. physionet.org).
References
[1] de Nooijer AH, Kotsaki A, Kranidioti E, Kox M, Pickkers P, Toonen EJM, et al. Complement activation in severely ill patients with sepsis: no relationship with inflammation and disease severity. Crit Care. 2023;27(1):63. 10.1186/s13054-023-04344-6. PMID: 36797757.Search in Google Scholar PubMed PubMed Central
[2] Fleischmann-Struzek C, Mikolajetz A, Schwarzkopf D, Cohen J, Hartog CS, Pletz M, et al. Challenges in assessing the burden of sepsis and understanding the inequalities of sepsis outcomes between National Health Systems: Secular trends in sepsis and infection incidence and mortality in Germany. Intensive Care Med. 2018;44(11):1826–35. 10.1007/s00134-018-5377-4. PMID: 30284637.Search in Google Scholar PubMed PubMed Central
[3] Thibaud P, Chow-Chine L, Gonzalez F, Bisbal M, Servan L, Sannini A, et al. Septic shock and biliary sepsis: 90-day mortality and associated risk factors. HPB. 2024;26(2):270–81. 10.1016/j.hpb.2023.10.012. PMID: 37940408.Search in Google Scholar PubMed
[4] Prescott HC, Harrison DA, Rowan KM, Shankar-Hari M, Wunsch H. Temporal trends in mortality of critically ill patients with sepsis in the United Kingdom, 1988–2019. Am J Resp Crit Care. 2024;209(5):507–16. 10.1164/rccm.202309-1636OC. PMID: 38259190.Search in Google Scholar PubMed
[5] Kuklin V, Sovershaev M, Bjerner J, Keith P, Scott LK, Thomas OMT, et al. Influence of therapeutic plasma exchange treatment on short-term mortality of critically ill adult patients with sepsis-induced organ dysfunction: A systematic review and meta-analysis. Crit Care. 2024;28(1):12. 10.1186/s13054-023-04795-x. PMID: 38178170.Search in Google Scholar PubMed PubMed Central
[6] Blanco J, Muriel-Bombín A, Sagredo V, Taboada F, Gandía F, Tamayo L, et al. Incidence, organ dysfunction and mortality in severe sepsis: A Spanish multicentre study. Crit Care. 2008;12(6):R158. 10.1186/cc7157. PMID: 19091069.Search in Google Scholar PubMed PubMed Central
[7] Liu S, He C, He W, Jiang T. Lactate-enhanced-qSOFA (LqSOFA) score is superior to the other four rapid scoring tools in predicting in-hospital mortality rate of the sepsis patients. Ann Transl Med. 2020;8(16):1013. 10.21037/atm-20-5410. PMID: 32953813.Search in Google Scholar PubMed PubMed Central
[8] Derin O, Şahin M, Dumlu R, Başgönül S, Bayrak AD, Arduç Ş, et al. Registry-based retrospective cohort study of mortality among adults admitted to intensive care units in istanbul with hospital acquired pseudomonas aeruginosa bloodstream-infection between 2014–2021. Antibiotics (Basel). 2024;13(1):90. 10.3390/antibiotics13010090. PMID: 38247649.Search in Google Scholar PubMed PubMed Central
[9] Torvik MA, Nymo SH, Nymo SH, Bjørnsen LP, Kvarenes HW, Ofstad EH. Patient characteristics in sepsis-related deaths: Prevalence of advanced frailty, comorbidity, and age in a Norwegian hospital trust. Infection. 2023;51(4):1103–15. 10.1007/s15010-023-02013-y. PMID: 36894755.Search in Google Scholar PubMed PubMed Central
[10] Cui L, Bao J, Yu C, Zhang C, Huang R, Liu L, et al. Development of a nomogram for predicting 90-day mortality in patients with sepsis-associated liver injury. Sci Rep. 2023;13(1):3662. 10.1038/s41598-023-30235-5. PMID: 36871054.Search in Google Scholar PubMed PubMed Central
[11] Yang J, Peng H, Luo Y, Zhu T, Xie L. Explainable ensemble machine learning model for prediction of 28-day mortality risk in patients with sepsis-associated acute kidney injury. Front Med (Lausanne). 2023;10:1165129. 10.3389/fmed.2023.1165129. PMID: 37275353.Search in Google Scholar PubMed PubMed Central
[12] Widyastuti Y, Jufan AY, Widodo U, Wisudarti CF, Fauzi RA, Ardiansyah F. A tertiary care center-based study of a novel ‘ICU mortality and prolonged stay risk scoring system’. Anaesth Pain Intensive Care. 2024;28(1):100–7. 10.35975/apic.v28i1.2382.Search in Google Scholar
[13] Boulet N, Boussere A, Mezzarobba M, Sofonea MT, Payen D, Lipman J, et al. Intensive care unit activity in France from the national database between 2013 and 2019: More critically ill patients, shorter stay and lower mortality rate. Anaesth Crit Care Pain Med. 2023;42(5):101228. 10.1016/j.accpm.2023.101228. PMID: 37031815.Search in Google Scholar PubMed
[14] Park SW, Yeo NY, Kang S, Ha T, Kim TH, Lee D, et al. Early prediction of mortality for septic patients visiting emergency room based on explainable machine learning: A real-world multicenter study. J Korean Med Sci. 2024;39(5):e53. 10.3346/jkms.2024.39.e53. PMID: 38317451.Search in Google Scholar PubMed PubMed Central
[15] Serafim R, Gomes JA, Salluh J, Póvoa P. A comparison of the quick-SOFA and systemic inflammatory response syndrome criteria for the diagnosis of sepsis and prediction of mortality: A systematic review and meta-analysis. Chest. 2018;153(3):646–55. 10.1016/j.chest.2017.12.015. PMID: 29289687.Search in Google Scholar PubMed
[16] Khwannimit B, Bhurayanontachai R, Vattanavanit V. Comparison of the performance of SOFA, qSOFA and SIRS for predicting mortality and organ failure among sepsis patients admitted to the intensive care unit in a middle-income country. J Crit Care. 2018;44:156–60. 10.1016/j.jcrc.2017.10.023. PMID: 29127841.Search in Google Scholar PubMed
[17] Finkelsztein EJ, Jones DS, Ma KC, Pabón MA, Delgado T, Nakahira K, et al. Comparison of qSOFA and SIRS for predicting adverse outcomes of patients with suspicion of sepsis outside the intensive care unit. Crit Care. 2017;21(1):73. 10.1186/s13054-017-1658-5. PMID: 28342442.Search in Google Scholar PubMed PubMed Central
[18] Zhu S, Chen H, Li X, Gulifeire T, Wang Y, Yang C, et al. Predictive value of six critical illness scores for 28-day death risk in comprehensive and specialized intensive care unit patients based on MIMIC-IV database. Zhonghua Wei Zhong Bing Ji Jiu Yi Xue. 2022;34(7):752–8. 10.3760/cma.j.cn121430-20220304-00205. PMID: 36100416.Search in Google Scholar PubMed
[19] Onur İD, Mutlu E, Sertesen E, Önder T, Duran AO, İnanç M. Evaluating the effectiveness of the Charlson Comorbidity Index in predicting immune checkpoint inhibitor-related adverse events. Immunotherapy-UK. 2024;16(5):295–303. 10.2217/imt-2023-0270. PMID: 38288692.Search in Google Scholar PubMed
[20] Pang K, Li L, Ouyang W, Liu X, Tang Y. Establishment of ICU mortality risk prediction models with machine learning algorithm using MIMIC-IV database. Diagnostics (Basel). 2022;12(5):1068. 10.3390/diagnostics12051068. PMID: 35626224.Search in Google Scholar PubMed PubMed Central
[21] Polok K, Fronczek J, Putowski Z, Czok M, Guidet B, Jung C, et al. Validity of the total SOFA score in patients ≥ 80 years old acutely admitted to intensive care units: a post-hoc analysis of the VIP2 prospective, international cohort study. Ann Intensive Care. 2023;13(1):98. 10.1186/s13613-023-01191-0. PMID: 37798561.Search in Google Scholar PubMed PubMed Central
[22] He Y, Xu J, Shang X, Fang X, Gao C, Sun D, et al. Clinical characteristics and risk factors associated with ICU-acquired infections in sepsis: A retrospective cohort study. Front Cell Infect Microbiol. 2022;12:962470. 10.3389/fcimb.2022.962470. PMID: 35967847.Search in Google Scholar PubMed PubMed Central
[23] Karagoz I, Aktas G, Yoldas H, Yildiz I, Ogun MN, Bilgi M, et al. Association between hemogram parameters and survival of critically ill patients. J Intensive Care Med. 2019;34(6):511–3.10.1177/0885066617703348Search in Google Scholar PubMed
[24] Karagöz İ, Özer B, Aktaş G. The predictors of outcome in patients that require management in intensive care units: A narrative review. Hitit Med J. 2024;6(3):367–78.10.52827/hititmedj.1443663Search in Google Scholar
[25] Karagoz I, Ozer B, Ital I, Turkoglu M, Disikirik A, Ozer S. C-reactive protein-to-serum albumin ratio as a marker of prognosis in adult intensive care population. Bratisl Lek Listy. 2023;124(4):277–9.10.4149/BLL_2023_042Search in Google Scholar PubMed
[26] Karagoz I. Does hemogram biomarkers predict mortality in intensive care population? Exp Biomed Res. 2019;2(4):163–8.10.30714/j-ebr.2019454854Search in Google Scholar
[27] Yao SL, Chen XW, Liu J, Chen XR, Zhou Y. Effect of mean heart rate on 30-day mortality in ischemic stroke with atrial fibrillation: Data from the MIMIC-IV database. Front Neurol. 2022-01-01;13:1017849. 10.3389/fneur.2022.1017849. PMID: 36388223.Search in Google Scholar PubMed PubMed Central
[28] Singer M, Deutschman CS, Seymour CW, Shankar-Hari M, Annane D, Bauer M, et al. The third international consensus definitions for sepsis and septic shock (Sepsis-3). JAMA-J Am Med Assoc. 2016;315(8):801–10. 10.1001/jama.2016.0287. PMID: 26903338.Search in Google Scholar PubMed PubMed Central
[29] Fleischmann-Struzek C, Mellhammar L, Rose N, Cassini A, Rudd KE, Schlattmann P, et al. Incidence and mortality of hospital- and ICU-treated sepsis: results from an updated and expanded systematic review and meta-analysis. Intens Care Med. 2020;46(8):1552–62. 10.1007/s00134-020-06151-x. PMID: 32572531.Search in Google Scholar PubMed PubMed Central
[30] Johnson AE, Kramer AA, Clifford GD. A new severity of illness scale using a subset of acute physiology and chronic health evaluation data elements shows comparable predictive accuracy. Crit Care Med. 2013;41(7):1711–8. 10.1097/CCM.0b013e31828a24fe. PMID: 23660729.Search in Google Scholar PubMed
[31] Arabi Y, Goraj R, McIntyre R, Al-Abdulkareem A. The predictive value of serial acute physiology score (APS) and simplified acute physiology score II (SAPS II) in post-operative liver transplant patients. Crit Care. 2000;4(Suppl 1):P240. 10.1186/cc959.Search in Google Scholar
[32] Haq A, Patil S, Parcells AL, Chamberlain RS. The simplified acute physiology score III is superior to the simplified acute physiology score II and acute physiology and chronic health evaluation II in predicting surgical and ICU mortality in the “Oldest Old”. Curr Gerontol Geriatr Res. 2014;2014:934852. 10.1155/2014/934852. PMID: 24696680.Search in Google Scholar PubMed PubMed Central
[33] Le Gall JR, Klar J, Lemeshow S, Saulnier F, Alberti C, Artigas A, et al. The logistic organ dysfunction system. A new way to assess organ dysfunction in the intensive care unit. ICU Scoring Group. JAMA-J Am Med Assoc. 1996;276(10):802–10. 10.1001/jama.276.10.802. PMID: 8769590.Search in Google Scholar PubMed
[34] Jang HN, Park HJ, Cho HS, Bae E, Lee TW, Chang SH, et al. The logistic organ dysfunction system score predicts the prognosis of patients with alcoholic ketoacidosis. Ren Fail. 2018;40(1):693–9. 10.1080/0886022X.2018.1491405. PMID: 30741615.Search in Google Scholar PubMed PubMed Central
[35] Yousefian M, Ghazi A, Amani F, Movaffagh B. Mortality rate in patients admitted to the ICU based on LODS, APACHE IV, TRIOS, SAPS II. J Adv Pharm Educ Res. 2022;12(1):56–62. 10.51847/cghzosuz9x.Search in Google Scholar
[36] Li Y, Yan C, Gan Z, Xi X, Tan Z, Li J, et al. Prognostic values of SOFA score, qSOFA score, and LODS score for patients with sepsis. Ann Palliat Med. 2020;9(3):1037–44. 10.21037/apm-20-984. PMID: 32498525.Search in Google Scholar PubMed
[37] Tang PL, Lin HS, Hsu CJ. Predicting in-hospital mortality for dementia patients after hip fracture surgery - A comparison between the Charlson Comorbidity Index (CCI) and the Elixhauser Comorbidity Index. J Orthop Sci. 2021;26(3):396–402. 10.1016/j.jos.2020.04.005. PMID: 32482586.Search in Google Scholar PubMed
[38] Yurkovich M, Avina-Zubieta JA, Thomas J, Gorenchtein M, Lacaille D. A systematic review identifies valid comorbidity indices derived from administrative health data. J Clin Epidemiol. 2015;68(1):3–14. 10.1016/j.jclinepi.2014.09.010. PMID: 25441702.Search in Google Scholar PubMed
[39] Zhu Y, Zhang R, Ye X, Liu H, Wei J. SAPS III is superior to SOFA for predicting 28-day mortality in sepsis patients based on Sepsis 3.0 criteria. Int J Infect Dis. 2022;114:135–41. 10.1016/j.ijid.2021.11.015. PMID: 34775116.Search in Google Scholar PubMed
[40] Zhao Y, Zhang B. Association between body temperature and all-cause mortality in patients with sepsis: Analysis of the MIMIC-IV database. Eur J Med Res. 2024;29(1):630.10.1186/s40001-024-02219-2Search in Google Scholar PubMed PubMed Central
[41] Puskarich MA, Nandi U, Long BG, Jones AE. Association between persistent tachycardia and tachypnea and in-hospital mortality among non-hypotensive emergency department patients admitted to the hospital. Clin Exp Emerg Med. 2017;4(1):2.10.15441/ceem.16.144Search in Google Scholar PubMed PubMed Central
[42] Christensen S, Johansen MB, Christiansen CF, Jensen R, Lemeshow S. Comparison of Charlson comorbidity index with SAPS and APACHE scores for prediction of mortality following intensive care. Clin Epidemiol. 2011;3:203–11. 10.2147/CLEP.S20247. PMID: 21750629.Search in Google Scholar PubMed PubMed Central
[43] Hu C, Hu B, Li Z, Yang X, Song H, Li J. Comparison of four scoring systems for predicting ICU mortality in patients with sepsis. Nan Fang Yi Ke Da Xue Xue Bao. 2020;40(4):513–8. 10.12122/j.issn.1673-4254.2020.04.10. PMID: 32895135.Search in Google Scholar PubMed PubMed Central
© 2025 the author(s), published by De Gruyter
This work is licensed under the Creative Commons Attribution 4.0 International License.
Articles in the same Issue
- Research Articles
- Network pharmacological analysis and in vitro testing of the rutin effects on triple-negative breast cancer
- Impact of diabetes on long-term survival in elderly liver cancer patients: A retrospective study
- Knockdown of CCNB1 alleviates high glucose-triggered trophoblast dysfunction during gestational diabetes via Wnt/β-catenin signaling pathway
- Risk factors for severe adverse drug reactions in hospitalized patients
- Analysis of the effect of ALA-PDT on macrophages in footpad model of mice infected with Fonsecaea monophora based on single-cell sequencing
- Development and validation of headspace gas chromatography with a flame ionization detector method for the determination of ethanol in the vitreous humor
- CMSP exerts anti-tumor effects on small cell lung cancer cells by inducing mitochondrial dysfunction and ferroptosis
- Predictive value of plasma sB7-H3 and YKL-40 in pediatric refractory Mycoplasma pneumoniae pneumonia
- Antiangiogenic potential of Elaeagnus umbellata extracts and molecular docking study by targeting VEGFR-2 pathway
- Comparison of the effectiveness of nurse-led preoperative counseling and postoperative follow-up care vs standard care for patients with gastric cancer
- Comparing the therapeutic efficacy of endoscopic minimally invasive surgery and traditional surgery for early-stage breast cancer: A meta-analysis
- Adhered macrophages as an additional marker of cardiomyocyte injury in biopsies of patients with dilated cardiomyopathy
- Association between statin administration and outcome in patients with sepsis: A retrospective study
- Exploration of the association between estimated glucose disposal rate and osteoarthritis in middle-aged and older adults: An analysis of NHANES data from 2011 to 2018
- A comparative analysis of the binary and multiclass classified chest X-ray images of pneumonia and COVID-19 with ML and DL models
- Lysophosphatidic acid 2 alleviates deep vein thrombosis via protective endothelial barrier function
- Transcription factor A, mitochondrial promotes lymph node metastasis and lymphangiogenesis in epithelial ovarian carcinoma
- Serum PM20D1 levels are associated with nutritional status and inflammatory factors in gastric cancer patients undergoing early enteral nutrition
- Hydromorphone reduced the incidence of emergence agitation after adenotonsillectomy in children with obstructive sleep apnea: A randomized, double-blind study
- Vitamin D replacement therapy may regulate sleep habits in patients with restless leg syndrome
- The first-line antihypertensive nitrendipine potentiated the therapeutic effect of oxaliplatin by downregulating CACNA1D in colorectal cancer
- Health literacy and health-related quality of life: The mediating role of irrational happiness
- Modulatory effects of Lycium barbarum polysaccharide on bone cell dynamics in osteoporosis
- Mechanism research on inhibition of gastric cancer in vitro by the extract of Pinellia ternata based on network pharmacology and cellular metabolomics
- Examination of the causal role of immune cells in non-alcoholic fatty liver disease by a bidirectional Mendelian randomization study
- Clinical analysis of ten cases of HIV infection combined with acute leukemia
- Investigating the cardioprotective potential of quercetin against tacrolimus-induced cardiotoxicity in Wistar rats: A mechanistic insights
- Clinical observation of probiotics combined with mesalazine and Yiyi Baitouweng Decoction retention enema in treating mild-to-moderate ulcerative colitis
- Diagnostic value of ratio of blood inflammation to coagulation markers in periprosthetic joint infection
- Sex-specific associations of sex hormone binding globulin and risk of bladder cancer
- Core muscle strength and stability-oriented breathing training reduces inter-recti distance in postpartum women
- The ERAS nursing care strategy for patients undergoing transsphenoidal endoscopic pituitary tumor resection: A randomized blinded controlled trial
- The serum IL-17A levels in patients with traumatic bowel rupture post-surgery and its predictive value for patient prognosis
- Impact of Kolb’s experiential learning theory-based nursing on caregiver burden and psychological state of caregivers of dementia patients
- Analysis of serum NLR combined with intraoperative margin condition to predict the prognosis of cervical HSIL patients undergoing LEEP surgery
- Commiphora gileadensis ameliorate infertility and erectile dysfunction in diabetic male mice
- The correlation between epithelial–mesenchymal transition classification and MMP2 expression of circulating tumor cells and prognosis of advanced or metastatic nasopharyngeal carcinoma
- Tetrahydropalmatine improves mitochondrial function in vascular smooth muscle cells of atherosclerosis in vitro by inhibiting Ras homolog gene family A/Rho-associated protein kinase-1 signaling pathway
- A cross-sectional study: Relationship between serum oxidative stress levels and arteriovenous fistula maturation in maintenance dialysis patients
- A comparative analysis of the impact of repeated administration of flavan 3-ol on brown, subcutaneous, and visceral adipose tissue
- Identifying early screening factors for depression in middle-aged and older adults: A cohort study
- Perform tumor-specific survival analysis for Merkel cell carcinoma patients undergoing surgical resection based on the SEER database by constructing a nomogram chart
- Unveiling the role of CXCL10 in pancreatic cancer progression: A novel prognostic indicator
- High-dose preoperative intraperitoneal erythropoietin and intravenous methylprednisolone in acute traumatic spinal cord injuries following decompression surgeries
- RAB39B: A novel biomarker for acute myeloid leukemia identified via multi-omics and functional validation
- Impact of peripheral conditioning on reperfusion injury following primary percutaneous coronary intervention in diabetic and non-diabetic STEMI patients
- Clinical efficacy of azacitidine in the treatment of middle- and high-risk myelodysplastic syndrome in middle-aged and elderly patients: A retrospective study
- The effect of ambulatory blood pressure load on mitral regurgitation in continuous ambulatory peritoneal dialysis patients
- Expression and clinical significance of ITGA3 in breast cancer
- Single-nucleus RNA sequencing reveals ARHGAP28 expression of podocytes as a biomarker in human diabetic nephropathy
- rSIG combined with NLR in the prognostic assessment of patients with multiple injuries
- Toxic metals and metalloids in collagen supplements of fish and jellyfish origin: Risk assessment for daily intake
- Exploring causal relationship between 41 inflammatory cytokines and marginal zone lymphoma: A bidirectional Mendelian randomization study
- Gender beliefs and legitimization of dating violence in adolescents
- Effect of serum IL-6, CRP, and MMP-9 levels on the efficacy of modified preperitoneal Kugel repair in patients with inguinal hernia
- Effect of smoking and smoking cessation on hematological parameters in polycythemic patients
- Pathogen surveillance and risk factors for pulmonary infection in patients with lung cancer: A retrospective single-center study
- Necroptosis of hippocampal neurons in paclitaxel chemotherapy-induced cognitive impairment mediates microglial activation via TLR4/MyD88 signaling pathway
- Celastrol suppresses neovascularization in rat aortic vascular endothelial cells stimulated by inflammatory tenocytes via modulating the NLRP3 pathway
- Cord-lamina angle and foraminal diameter as key predictors of C5 palsy after anterior cervical decompression and fusion surgery
- GATA1: A key biomarker for predicting the prognosis of patients with diffuse large B-cell lymphoma
- Influencing factors of false lumen thrombosis in type B aortic dissection: A single-center retrospective study
- MZB1 regulates the immune microenvironment and inhibits ovarian cancer cell migration
- Integrating experimental and network pharmacology to explore the pharmacological mechanisms of Dioscin against glioblastoma
- Trends in research on preterm birth in twin pregnancy based on bibliometrics
- Four-week IgE/baseline IgE ratio combined with tryptase predicts clinical outcome in omalizumab-treated children with moderate-to-severe asthma
- Single-cell transcriptomic analysis identifies a stress response Schwann cell subtype
- Acute pancreatitis risk in the diagnosis and management of inflammatory bowel disease: A critical focus
- Effect of subclinical esketamine on NLRP3 and cognitive dysfunction in elderly ischemic stroke patients
- Interleukin-37 mediates the anti-oral tumor activity in oral cancer through STAT3
- CA199 and CEA expression levels, and minimally invasive postoperative prognosis analysis in esophageal squamous carcinoma patients
- Efficacy of a novel drainage catheter in the treatment of CSF leak after posterior spine surgery: A retrospective cohort study
- Comprehensive biomedicine assessment of Apteranthes tuberculata extracts: Phytochemical analysis and multifaceted pharmacological evaluation in animal models
- Relation of time in range to severity of coronary artery disease in patients with type 2 diabetes: A cross-sectional study
- Dopamine attenuates ethanol-induced neuronal apoptosis by stimulating electrical activity in the developing rat retina
- Correlation between albumin levels during the third trimester and the risk of postpartum levator ani muscle rupture
- Factors associated with maternal attention and distraction during breastfeeding and childcare: A cross-sectional study in the west of Iran
- Mechanisms of hesperetin in treating metabolic dysfunction-associated steatosis liver disease via network pharmacology and in vitro experiments
- The law on oncological oblivion in the Italian and European context: How to best uphold the cancer patients’ rights to privacy and self-determination?
- The prognostic value of the neutrophil-to-lymphocyte ratio, platelet-to-lymphocyte ratio, and prognostic nutritional index for survival in patients with colorectal cancer
- Factors affecting the measurements of peripheral oxygen saturation values in healthy young adults
- Comparison and correlations between findings of hysteroscopy and vaginal color Doppler ultrasonography for detection of uterine abnormalities in patients with recurrent implantation failure
- The effects of different types of RAGT on balance function in stroke patients with low levels of independent walking in a convalescent rehabilitation hospital
- Causal relationship between asthma and ankylosing spondylitis: A bidirectional two-sample univariable and multivariable Mendelian randomization study
- Correlations of health literacy with individuals’ understanding and use of medications in Southern Taiwan
- Correlation of serum calprotectin with outcome of acute cerebral infarction
- Comparison of computed tomography and guided bronchoscopy in the diagnosis of pulmonary nodules: A systematic review and meta-analysis
- Curdione protects vascular endothelial cells and atherosclerosis via the regulation of DNMT1-mediated ERBB4 promoter methylation
- The identification of novel missense variant in ChAT gene in a patient with gestational diabetes denotes plausible genetic association
- Molecular genotyping of multi-system rare blood types in foreign blood donors based on DNA sequencing and its clinical significance
- Exploring the role of succinyl carnitine in the association between CD39⁺ CD4⁺ T cell and ulcerative colitis: A Mendelian randomization study
- Dexmedetomidine suppresses microglial activation in postoperative cognitive dysfunction via the mmu-miRNA-125/TRAF6 signaling axis
- Analysis of serum metabolomics in patients with different types of chronic heart failure
- Diagnostic value of hematological parameters in the early diagnosis of acute cholecystitis
- Pachymaran alleviates fat accumulation, hepatocyte degeneration, and injury in mice with nonalcoholic fatty liver disease
- Decrease in CD4 and CD8 lymphocytes are predictors of severe clinical picture and unfavorable outcome of the disease in patients with COVID-19
- METTL3 blocked the progression of diabetic retinopathy through m6A-modified SOX2
- The predictive significance of anti-RO-52 antibody in patients with interstitial pneumonia after treatment of malignant tumors
- Exploring cerebrospinal fluid metabolites, cognitive function, and brain atrophy: Insights from Mendelian randomization
- Development and validation of potential molecular subtypes and signatures of ocular sarcoidosis based on autophagy-related gene analysis
- Widespread venous thrombosis: Unveiling a complex case of Behçet’s disease with a literature perspective
- Uterine fibroid embolization: An analysis of clinical outcomes and impact on patients’ quality of life
- Discovery of lipid metabolism-related diagnostic biomarkers and construction of diagnostic model in steroid-induced osteonecrosis of femoral head
- Serum-derived exomiR-188-3p is a promising novel biomarker for early-stage ovarian cancer
- Enhancing chronic back pain management: A comparative study of ultrasound–MRI fusion guidance for paravertebral nerve block
- Peptide CCAT1-70aa promotes hepatocellular carcinoma proliferation and invasion via the MAPK/ERK pathway
- Electroacupuncture-induced reduction of myocardial ischemia–reperfusion injury via FTO-dependent m6A methylation modulation
- Hemorrhoids and cardiovascular disease: A bidirectional Mendelian randomization study
- Cell-free adipose extract inhibits hypertrophic scar formation through collagen remodeling and antiangiogenesis
- HALP score in Demodex blepharitis: A case–control study
- Assessment of SOX2 performance as a marker for circulating cancer stem-like cells (CCSCs) identification in advanced breast cancer patients using CytoTrack system
- Risk and prognosis for brain metastasis in primary metastatic cervical cancer patients: A population-based study
- Comparison of the two intestinal anastomosis methods in pediatric patients
- Factors influencing hematological toxicity and adverse effects of perioperative hyperthermic intraperitoneal vs intraperitoneal chemotherapy in gastrointestinal cancer
- Endotoxin tolerance inhibits NLRP3 inflammasome activation in macrophages of septic mice by restoring autophagic flux through TRIM26
- Lateral transperitoneal laparoscopic adrenalectomy: A single-centre experience of 21 procedures
- Petunidin attenuates lipopolysaccharide-induced retinal microglia inflammatory response in diabetic retinopathy by targeting OGT/NF-κB/LCN2 axis
- Procalcitonin and C-reactive protein as biomarkers for diagnosing and assessing the severity of acute cholecystitis
- Factors determining the number of sessions in successful extracorporeal shock wave lithotripsy patients
- Development of a nomogram for predicting cancer-specific survival in patients with renal pelvic cancer following surgery
- Inhibition of ATG7 promotes orthodontic tooth movement by regulating the RANKL/OPG ratio under compression force
- A machine learning-based prognostic model integrating mRNA stemness index, hypoxia, and glycolysis‑related biomarkers for colorectal cancer
- Glutathione attenuates sepsis-associated encephalopathy via dual modulation of NF-κB and PKA/CREB pathways
- FAHD1 prevents neuronal ferroptosis by modulating R-loop and the cGAS–STING pathway
- Association of placenta weight and morphology with term low birth weight: A case–control study
- Investigation of the pathogenic variants induced Sjogren’s syndrome in Turkish population
- Nucleotide metabolic abnormalities in post-COVID-19 condition and type 2 diabetes mellitus patients and their association with endocrine dysfunction
- TGF-β–Smad2/3 signaling in high-altitude pulmonary hypertension in rats: Role and mechanisms via macrophage M2 polarization
- Ultrasound-guided unilateral versus bilateral erector spinae plane block for postoperative analgesia of patients undergoing laparoscopic cholecystectomy
- Profiling gut microbiome dynamics in subacute thyroiditis: Implications for pathogenesis, diagnosis, and treatment
- Delta neutrophil index, CRP/albumin ratio, procalcitonin, immature granulocytes, and HALP score in acute appendicitis: Best performing biomarker?
- Anticancer activity mechanism of novelly synthesized and characterized benzofuran ring-linked 3-nitrophenyl chalcone derivative on colon cancer cells
- H2valdien3 arrests the cell cycle and induces apoptosis of gastric cancer
- Prognostic relevance of PRSS2 and its immune correlates in papillary thyroid carcinoma
- Association of SGLT2 inhibition with psychiatric disorders: A Mendelian randomization study
- Motivational interviewing for alcohol use reduction in Thai patients
- Luteolin alleviates oxygen-glucose deprivation/reoxygenation-induced neuron injury by regulating NLRP3/IL-1β signaling
- Polyphyllin II inhibits thyroid cancer cell growth by simultaneously inhibiting glycolysis and oxidative phosphorylation
- Relationship between the expression of copper death promoting factor SLC31A1 in papillary thyroid carcinoma and clinicopathological indicators and prognosis
- CSF2 polarized neutrophils and invaded renal cancer cells in vitro influence
- Proton pump inhibitors-induced thrombocytopenia: A systematic literature analysis of case reports
- The current status and influence factors of research ability among community nurses: A sequential qualitative–quantitative study
- OKAIN: A comprehensive oncology knowledge base for the interpretation of clinically actionable alterations
- The relationship between serum CA50, CA242, and SAA levels and clinical pathological characteristics and prognosis in patients with pancreatic cancer
- Identification and external validation of a prognostic signature based on hypoxia–glycolysis-related genes for kidney renal clear cell carcinoma
- Engineered RBC-derived nanovesicles functionalized with tumor-targeting ligands: A comparative study on breast cancer targeting efficiency and biocompatibility
- Relationship of resting echocardiography combined with serum micronutrients to the severity of low-gradient severe aortic stenosis
- Effect of vibration on pain during subcutaneous heparin injection: A randomized, single-blind, placebo-controlled trial
- The diagnostic performance of machine learning-based FFRCT for coronary artery disease: A meta-analysis
- Comparing biofeedback device vs diaphragmatic breathing for bloating relief: A randomized controlled trial
- Serum uric acid to albumin ratio and C-reactive protein as predictive biomarkers for chronic total occlusion and coronary collateral circulation quality
- Multiple organ scoring systems for predicting in-hospital mortality of sepsis patients in the intensive care unit
- Single-cell RNA sequencing data analysis of the inner ear in gentamicin-treated mice via intraperitoneal injection
- Review Articles
- The effects of enhanced external counter-pulsation on post-acute sequelae of COVID-19: A narrative review
- Diabetes-related cognitive impairment: Mechanisms, symptoms, and treatments
- Microscopic changes and gross morphology of placenta in women affected by gestational diabetes mellitus in dietary treatment: A systematic review
- Review of mechanisms and frontier applications in IL-17A-induced hypertension
- Research progress on the correlation between islet amyloid peptides and type 2 diabetes mellitus
- The safety and efficacy of BCG combined with mitomycin C compared with BCG monotherapy in patients with non-muscle-invasive bladder cancer: A systematic review and meta-analysis
- The application of augmented reality in robotic general surgery: A mini-review
- The effect of Greek mountain tea extract and wheat germ extract on peripheral blood flow and eicosanoid metabolism in mammals
- Neurogasobiology of migraine: Carbon monoxide, hydrogen sulfide, and nitric oxide as emerging pathophysiological trinacrium relevant to nociception regulation
- Plant polyphenols, terpenes, and terpenoids in oral health
- Laboratory medicine between technological innovation, rights safeguarding, and patient safety: A bioethical perspective
- End-of-life in cancer patients: Medicolegal implications and ethical challenges in Europe
- The maternal factors during pregnancy for intrauterine growth retardation: An umbrella review
- Intra-abdominal hypertension/abdominal compartment syndrome of pediatric patients in critical care settings
- PI3K/Akt pathway and neuroinflammation in sepsis-associated encephalopathy
- Screening of Group B Streptococcus in pregnancy: A systematic review for the laboratory detection
- Giant borderline ovarian tumours – review of the literature
- Leveraging artificial intelligence for collaborative care planning: Innovations and impacts in shared decision-making – A systematic review
- Cholera epidemiology analysis through the experience of the 1973 Naples epidemic
- Risk factors of frailty/sarcopenia in community older adults: Meta-analysis
- Supplement strategies for infertility in overweight women: Evidence and legal insights
- Scurvy, a not obsolete disorder: Clinical report in eight young children and literature review
- A meta-analysis of the effects of DBS on cognitive function in patients with advanced PD
- Protective role of selenium in sepsis: Mechanisms and potential therapeutic strategies
- Strategies for hyperkalemia management in dialysis patients: A systematic review
- C-reactive protein-to-albumin ratio in peripheral artery disease
- Case Reports
- Delayed graft function after renal transplantation
- Semaglutide treatment for type 2 diabetes in a patient with chronic myeloid leukemia: A case report and review of the literature
- Diverse electrophysiological demyelinating features in a late-onset glycogen storage disease type IIIa case
- Giant right atrial hemangioma presenting with ascites: A case report
- Laser excision of a large granular cell tumor of the vocal cord with subglottic extension: A case report
- EsoFLIP-assisted dilation for dysphagia in systemic sclerosis: Highlighting the role of multimodal esophageal evaluation
- Molecular hydrogen-rhodiola as an adjuvant therapy for ischemic stroke in internal carotid artery occlusion: A case report
- Coronary artery anomalies: A case of the “malignant” left coronary artery and its surgical management
- Rapid Communication
- Biological properties of valve materials using RGD and EC
-
A single oral administration of flavanols enhances short
-term memory in mice along with increased brain-derived neurotrophic factor - Letter to the Editor
- Role of enhanced external counterpulsation in long COVID
- Expression of Concern
- Expression of concern “A ceRNA network mediated by LINC00475 in papillary thyroid carcinoma”
- Expression of concern “Notoginsenoside R1 alleviates spinal cord injury through the miR-301a/KLF7 axis to activate Wnt/β-catenin pathway”
- Expression of concern “circ_0020123 promotes cell proliferation and migration in lung adenocarcinoma via PDZD8”
- Corrigendum
- Corrigendum to “Empagliflozin improves aortic injury in obese mice by regulating fatty acid metabolism”
- Corrigendum to “Comparing the therapeutic efficacy of endoscopic minimally invasive surgery and traditional surgery for early-stage breast cancer: A meta-analysis”
- Corrigendum to “The progress of autoimmune hepatitis research and future challenges”
- Retraction
- Retraction of “miR-654-5p promotes gastric cancer progression via the GPRIN1/NF-κB pathway”
- Retraction of: “LncRNA CASC15 inhibition relieves renal fibrosis in diabetic nephropathy through downregulating SP-A by sponging to miR-424”
- Retraction of: “SCARA5 inhibits oral squamous cell carcinoma via inactivating the STAT3 and PI3K/AKT signaling pathways”
- Special Issue Advancements in oncology: bridging clinical and experimental research - Part II
- Unveiling novel biomarkers for platinum chemoresistance in ovarian cancer
- Lathyrol affects the expression of AR and PSA and inhibits the malignant behavior of RCC cells
- The era of increasing cancer survivorship: Trends in fertility preservation, medico-legal implications, and ethical challenges
- Bone scintigraphy and positron emission tomography in the early diagnosis of MRONJ
- Meta-analysis of clinical efficacy and safety of immunotherapy combined with chemotherapy in non-small cell lung cancer
- Special Issue Computational Intelligence Methodologies Meets Recurrent Cancers - Part IV
- Exploration of mRNA-modifying METTL3 oncogene as momentous prognostic biomarker responsible for colorectal cancer development
- Special Issue The evolving saga of RNAs from bench to bedside - Part III
- Interaction and verification of ferroptosis-related RNAs Rela and Stat3 in promoting sepsis-associated acute kidney injury
- The mRNA MOXD1: Link to oxidative stress and prognostic significance in gastric cancer
- Special Issue Exploring the biological mechanism of human diseases based on MultiOmics Technology - Part II
- Dynamic changes in lactate-related genes in microglia and their role in immune cell interactions after ischemic stroke
- A prognostic model correlated with fatty acid metabolism in Ewing’s sarcoma based on bioinformatics analysis
- Red cell distribution width predicts early kidney injury: A NHANES cross-sectional study
- Special Issue Diabetes mellitus: pathophysiology, complications & treatment
- Nutritional risk assessment and nutritional support in children with congenital diabetes during surgery
- Correlation of the differential expressions of RANK, RANKL, and OPG with obesity in the elderly population in Xinjiang
- A discussion on the application of fluorescence micro-optical sectioning tomography in the research of cognitive dysfunction in diabetes
- A review of brain research on T2DM-related cognitive dysfunction
- Metformin and estrogen modulation in LABC with T2DM: A 36-month randomized trial
- Special Issue Innovative Biomarker Discovery and Precision Medicine in Cancer Diagnostics
- CircASH1L-mediated tumor progression in triple-negative breast cancer: PI3K/AKT pathway mechanisms
Articles in the same Issue
- Research Articles
- Network pharmacological analysis and in vitro testing of the rutin effects on triple-negative breast cancer
- Impact of diabetes on long-term survival in elderly liver cancer patients: A retrospective study
- Knockdown of CCNB1 alleviates high glucose-triggered trophoblast dysfunction during gestational diabetes via Wnt/β-catenin signaling pathway
- Risk factors for severe adverse drug reactions in hospitalized patients
- Analysis of the effect of ALA-PDT on macrophages in footpad model of mice infected with Fonsecaea monophora based on single-cell sequencing
- Development and validation of headspace gas chromatography with a flame ionization detector method for the determination of ethanol in the vitreous humor
- CMSP exerts anti-tumor effects on small cell lung cancer cells by inducing mitochondrial dysfunction and ferroptosis
- Predictive value of plasma sB7-H3 and YKL-40 in pediatric refractory Mycoplasma pneumoniae pneumonia
- Antiangiogenic potential of Elaeagnus umbellata extracts and molecular docking study by targeting VEGFR-2 pathway
- Comparison of the effectiveness of nurse-led preoperative counseling and postoperative follow-up care vs standard care for patients with gastric cancer
- Comparing the therapeutic efficacy of endoscopic minimally invasive surgery and traditional surgery for early-stage breast cancer: A meta-analysis
- Adhered macrophages as an additional marker of cardiomyocyte injury in biopsies of patients with dilated cardiomyopathy
- Association between statin administration and outcome in patients with sepsis: A retrospective study
- Exploration of the association between estimated glucose disposal rate and osteoarthritis in middle-aged and older adults: An analysis of NHANES data from 2011 to 2018
- A comparative analysis of the binary and multiclass classified chest X-ray images of pneumonia and COVID-19 with ML and DL models
- Lysophosphatidic acid 2 alleviates deep vein thrombosis via protective endothelial barrier function
- Transcription factor A, mitochondrial promotes lymph node metastasis and lymphangiogenesis in epithelial ovarian carcinoma
- Serum PM20D1 levels are associated with nutritional status and inflammatory factors in gastric cancer patients undergoing early enteral nutrition
- Hydromorphone reduced the incidence of emergence agitation after adenotonsillectomy in children with obstructive sleep apnea: A randomized, double-blind study
- Vitamin D replacement therapy may regulate sleep habits in patients with restless leg syndrome
- The first-line antihypertensive nitrendipine potentiated the therapeutic effect of oxaliplatin by downregulating CACNA1D in colorectal cancer
- Health literacy and health-related quality of life: The mediating role of irrational happiness
- Modulatory effects of Lycium barbarum polysaccharide on bone cell dynamics in osteoporosis
- Mechanism research on inhibition of gastric cancer in vitro by the extract of Pinellia ternata based on network pharmacology and cellular metabolomics
- Examination of the causal role of immune cells in non-alcoholic fatty liver disease by a bidirectional Mendelian randomization study
- Clinical analysis of ten cases of HIV infection combined with acute leukemia
- Investigating the cardioprotective potential of quercetin against tacrolimus-induced cardiotoxicity in Wistar rats: A mechanistic insights
- Clinical observation of probiotics combined with mesalazine and Yiyi Baitouweng Decoction retention enema in treating mild-to-moderate ulcerative colitis
- Diagnostic value of ratio of blood inflammation to coagulation markers in periprosthetic joint infection
- Sex-specific associations of sex hormone binding globulin and risk of bladder cancer
- Core muscle strength and stability-oriented breathing training reduces inter-recti distance in postpartum women
- The ERAS nursing care strategy for patients undergoing transsphenoidal endoscopic pituitary tumor resection: A randomized blinded controlled trial
- The serum IL-17A levels in patients with traumatic bowel rupture post-surgery and its predictive value for patient prognosis
- Impact of Kolb’s experiential learning theory-based nursing on caregiver burden and psychological state of caregivers of dementia patients
- Analysis of serum NLR combined with intraoperative margin condition to predict the prognosis of cervical HSIL patients undergoing LEEP surgery
- Commiphora gileadensis ameliorate infertility and erectile dysfunction in diabetic male mice
- The correlation between epithelial–mesenchymal transition classification and MMP2 expression of circulating tumor cells and prognosis of advanced or metastatic nasopharyngeal carcinoma
- Tetrahydropalmatine improves mitochondrial function in vascular smooth muscle cells of atherosclerosis in vitro by inhibiting Ras homolog gene family A/Rho-associated protein kinase-1 signaling pathway
- A cross-sectional study: Relationship between serum oxidative stress levels and arteriovenous fistula maturation in maintenance dialysis patients
- A comparative analysis of the impact of repeated administration of flavan 3-ol on brown, subcutaneous, and visceral adipose tissue
- Identifying early screening factors for depression in middle-aged and older adults: A cohort study
- Perform tumor-specific survival analysis for Merkel cell carcinoma patients undergoing surgical resection based on the SEER database by constructing a nomogram chart
- Unveiling the role of CXCL10 in pancreatic cancer progression: A novel prognostic indicator
- High-dose preoperative intraperitoneal erythropoietin and intravenous methylprednisolone in acute traumatic spinal cord injuries following decompression surgeries
- RAB39B: A novel biomarker for acute myeloid leukemia identified via multi-omics and functional validation
- Impact of peripheral conditioning on reperfusion injury following primary percutaneous coronary intervention in diabetic and non-diabetic STEMI patients
- Clinical efficacy of azacitidine in the treatment of middle- and high-risk myelodysplastic syndrome in middle-aged and elderly patients: A retrospective study
- The effect of ambulatory blood pressure load on mitral regurgitation in continuous ambulatory peritoneal dialysis patients
- Expression and clinical significance of ITGA3 in breast cancer
- Single-nucleus RNA sequencing reveals ARHGAP28 expression of podocytes as a biomarker in human diabetic nephropathy
- rSIG combined with NLR in the prognostic assessment of patients with multiple injuries
- Toxic metals and metalloids in collagen supplements of fish and jellyfish origin: Risk assessment for daily intake
- Exploring causal relationship between 41 inflammatory cytokines and marginal zone lymphoma: A bidirectional Mendelian randomization study
- Gender beliefs and legitimization of dating violence in adolescents
- Effect of serum IL-6, CRP, and MMP-9 levels on the efficacy of modified preperitoneal Kugel repair in patients with inguinal hernia
- Effect of smoking and smoking cessation on hematological parameters in polycythemic patients
- Pathogen surveillance and risk factors for pulmonary infection in patients with lung cancer: A retrospective single-center study
- Necroptosis of hippocampal neurons in paclitaxel chemotherapy-induced cognitive impairment mediates microglial activation via TLR4/MyD88 signaling pathway
- Celastrol suppresses neovascularization in rat aortic vascular endothelial cells stimulated by inflammatory tenocytes via modulating the NLRP3 pathway
- Cord-lamina angle and foraminal diameter as key predictors of C5 palsy after anterior cervical decompression and fusion surgery
- GATA1: A key biomarker for predicting the prognosis of patients with diffuse large B-cell lymphoma
- Influencing factors of false lumen thrombosis in type B aortic dissection: A single-center retrospective study
- MZB1 regulates the immune microenvironment and inhibits ovarian cancer cell migration
- Integrating experimental and network pharmacology to explore the pharmacological mechanisms of Dioscin against glioblastoma
- Trends in research on preterm birth in twin pregnancy based on bibliometrics
- Four-week IgE/baseline IgE ratio combined with tryptase predicts clinical outcome in omalizumab-treated children with moderate-to-severe asthma
- Single-cell transcriptomic analysis identifies a stress response Schwann cell subtype
- Acute pancreatitis risk in the diagnosis and management of inflammatory bowel disease: A critical focus
- Effect of subclinical esketamine on NLRP3 and cognitive dysfunction in elderly ischemic stroke patients
- Interleukin-37 mediates the anti-oral tumor activity in oral cancer through STAT3
- CA199 and CEA expression levels, and minimally invasive postoperative prognosis analysis in esophageal squamous carcinoma patients
- Efficacy of a novel drainage catheter in the treatment of CSF leak after posterior spine surgery: A retrospective cohort study
- Comprehensive biomedicine assessment of Apteranthes tuberculata extracts: Phytochemical analysis and multifaceted pharmacological evaluation in animal models
- Relation of time in range to severity of coronary artery disease in patients with type 2 diabetes: A cross-sectional study
- Dopamine attenuates ethanol-induced neuronal apoptosis by stimulating electrical activity in the developing rat retina
- Correlation between albumin levels during the third trimester and the risk of postpartum levator ani muscle rupture
- Factors associated with maternal attention and distraction during breastfeeding and childcare: A cross-sectional study in the west of Iran
- Mechanisms of hesperetin in treating metabolic dysfunction-associated steatosis liver disease via network pharmacology and in vitro experiments
- The law on oncological oblivion in the Italian and European context: How to best uphold the cancer patients’ rights to privacy and self-determination?
- The prognostic value of the neutrophil-to-lymphocyte ratio, platelet-to-lymphocyte ratio, and prognostic nutritional index for survival in patients with colorectal cancer
- Factors affecting the measurements of peripheral oxygen saturation values in healthy young adults
- Comparison and correlations between findings of hysteroscopy and vaginal color Doppler ultrasonography for detection of uterine abnormalities in patients with recurrent implantation failure
- The effects of different types of RAGT on balance function in stroke patients with low levels of independent walking in a convalescent rehabilitation hospital
- Causal relationship between asthma and ankylosing spondylitis: A bidirectional two-sample univariable and multivariable Mendelian randomization study
- Correlations of health literacy with individuals’ understanding and use of medications in Southern Taiwan
- Correlation of serum calprotectin with outcome of acute cerebral infarction
- Comparison of computed tomography and guided bronchoscopy in the diagnosis of pulmonary nodules: A systematic review and meta-analysis
- Curdione protects vascular endothelial cells and atherosclerosis via the regulation of DNMT1-mediated ERBB4 promoter methylation
- The identification of novel missense variant in ChAT gene in a patient with gestational diabetes denotes plausible genetic association
- Molecular genotyping of multi-system rare blood types in foreign blood donors based on DNA sequencing and its clinical significance
- Exploring the role of succinyl carnitine in the association between CD39⁺ CD4⁺ T cell and ulcerative colitis: A Mendelian randomization study
- Dexmedetomidine suppresses microglial activation in postoperative cognitive dysfunction via the mmu-miRNA-125/TRAF6 signaling axis
- Analysis of serum metabolomics in patients with different types of chronic heart failure
- Diagnostic value of hematological parameters in the early diagnosis of acute cholecystitis
- Pachymaran alleviates fat accumulation, hepatocyte degeneration, and injury in mice with nonalcoholic fatty liver disease
- Decrease in CD4 and CD8 lymphocytes are predictors of severe clinical picture and unfavorable outcome of the disease in patients with COVID-19
- METTL3 blocked the progression of diabetic retinopathy through m6A-modified SOX2
- The predictive significance of anti-RO-52 antibody in patients with interstitial pneumonia after treatment of malignant tumors
- Exploring cerebrospinal fluid metabolites, cognitive function, and brain atrophy: Insights from Mendelian randomization
- Development and validation of potential molecular subtypes and signatures of ocular sarcoidosis based on autophagy-related gene analysis
- Widespread venous thrombosis: Unveiling a complex case of Behçet’s disease with a literature perspective
- Uterine fibroid embolization: An analysis of clinical outcomes and impact on patients’ quality of life
- Discovery of lipid metabolism-related diagnostic biomarkers and construction of diagnostic model in steroid-induced osteonecrosis of femoral head
- Serum-derived exomiR-188-3p is a promising novel biomarker for early-stage ovarian cancer
- Enhancing chronic back pain management: A comparative study of ultrasound–MRI fusion guidance for paravertebral nerve block
- Peptide CCAT1-70aa promotes hepatocellular carcinoma proliferation and invasion via the MAPK/ERK pathway
- Electroacupuncture-induced reduction of myocardial ischemia–reperfusion injury via FTO-dependent m6A methylation modulation
- Hemorrhoids and cardiovascular disease: A bidirectional Mendelian randomization study
- Cell-free adipose extract inhibits hypertrophic scar formation through collagen remodeling and antiangiogenesis
- HALP score in Demodex blepharitis: A case–control study
- Assessment of SOX2 performance as a marker for circulating cancer stem-like cells (CCSCs) identification in advanced breast cancer patients using CytoTrack system
- Risk and prognosis for brain metastasis in primary metastatic cervical cancer patients: A population-based study
- Comparison of the two intestinal anastomosis methods in pediatric patients
- Factors influencing hematological toxicity and adverse effects of perioperative hyperthermic intraperitoneal vs intraperitoneal chemotherapy in gastrointestinal cancer
- Endotoxin tolerance inhibits NLRP3 inflammasome activation in macrophages of septic mice by restoring autophagic flux through TRIM26
- Lateral transperitoneal laparoscopic adrenalectomy: A single-centre experience of 21 procedures
- Petunidin attenuates lipopolysaccharide-induced retinal microglia inflammatory response in diabetic retinopathy by targeting OGT/NF-κB/LCN2 axis
- Procalcitonin and C-reactive protein as biomarkers for diagnosing and assessing the severity of acute cholecystitis
- Factors determining the number of sessions in successful extracorporeal shock wave lithotripsy patients
- Development of a nomogram for predicting cancer-specific survival in patients with renal pelvic cancer following surgery
- Inhibition of ATG7 promotes orthodontic tooth movement by regulating the RANKL/OPG ratio under compression force
- A machine learning-based prognostic model integrating mRNA stemness index, hypoxia, and glycolysis‑related biomarkers for colorectal cancer
- Glutathione attenuates sepsis-associated encephalopathy via dual modulation of NF-κB and PKA/CREB pathways
- FAHD1 prevents neuronal ferroptosis by modulating R-loop and the cGAS–STING pathway
- Association of placenta weight and morphology with term low birth weight: A case–control study
- Investigation of the pathogenic variants induced Sjogren’s syndrome in Turkish population
- Nucleotide metabolic abnormalities in post-COVID-19 condition and type 2 diabetes mellitus patients and their association with endocrine dysfunction
- TGF-β–Smad2/3 signaling in high-altitude pulmonary hypertension in rats: Role and mechanisms via macrophage M2 polarization
- Ultrasound-guided unilateral versus bilateral erector spinae plane block for postoperative analgesia of patients undergoing laparoscopic cholecystectomy
- Profiling gut microbiome dynamics in subacute thyroiditis: Implications for pathogenesis, diagnosis, and treatment
- Delta neutrophil index, CRP/albumin ratio, procalcitonin, immature granulocytes, and HALP score in acute appendicitis: Best performing biomarker?
- Anticancer activity mechanism of novelly synthesized and characterized benzofuran ring-linked 3-nitrophenyl chalcone derivative on colon cancer cells
- H2valdien3 arrests the cell cycle and induces apoptosis of gastric cancer
- Prognostic relevance of PRSS2 and its immune correlates in papillary thyroid carcinoma
- Association of SGLT2 inhibition with psychiatric disorders: A Mendelian randomization study
- Motivational interviewing for alcohol use reduction in Thai patients
- Luteolin alleviates oxygen-glucose deprivation/reoxygenation-induced neuron injury by regulating NLRP3/IL-1β signaling
- Polyphyllin II inhibits thyroid cancer cell growth by simultaneously inhibiting glycolysis and oxidative phosphorylation
- Relationship between the expression of copper death promoting factor SLC31A1 in papillary thyroid carcinoma and clinicopathological indicators and prognosis
- CSF2 polarized neutrophils and invaded renal cancer cells in vitro influence
- Proton pump inhibitors-induced thrombocytopenia: A systematic literature analysis of case reports
- The current status and influence factors of research ability among community nurses: A sequential qualitative–quantitative study
- OKAIN: A comprehensive oncology knowledge base for the interpretation of clinically actionable alterations
- The relationship between serum CA50, CA242, and SAA levels and clinical pathological characteristics and prognosis in patients with pancreatic cancer
- Identification and external validation of a prognostic signature based on hypoxia–glycolysis-related genes for kidney renal clear cell carcinoma
- Engineered RBC-derived nanovesicles functionalized with tumor-targeting ligands: A comparative study on breast cancer targeting efficiency and biocompatibility
- Relationship of resting echocardiography combined with serum micronutrients to the severity of low-gradient severe aortic stenosis
- Effect of vibration on pain during subcutaneous heparin injection: A randomized, single-blind, placebo-controlled trial
- The diagnostic performance of machine learning-based FFRCT for coronary artery disease: A meta-analysis
- Comparing biofeedback device vs diaphragmatic breathing for bloating relief: A randomized controlled trial
- Serum uric acid to albumin ratio and C-reactive protein as predictive biomarkers for chronic total occlusion and coronary collateral circulation quality
- Multiple organ scoring systems for predicting in-hospital mortality of sepsis patients in the intensive care unit
- Single-cell RNA sequencing data analysis of the inner ear in gentamicin-treated mice via intraperitoneal injection
- Review Articles
- The effects of enhanced external counter-pulsation on post-acute sequelae of COVID-19: A narrative review
- Diabetes-related cognitive impairment: Mechanisms, symptoms, and treatments
- Microscopic changes and gross morphology of placenta in women affected by gestational diabetes mellitus in dietary treatment: A systematic review
- Review of mechanisms and frontier applications in IL-17A-induced hypertension
- Research progress on the correlation between islet amyloid peptides and type 2 diabetes mellitus
- The safety and efficacy of BCG combined with mitomycin C compared with BCG monotherapy in patients with non-muscle-invasive bladder cancer: A systematic review and meta-analysis
- The application of augmented reality in robotic general surgery: A mini-review
- The effect of Greek mountain tea extract and wheat germ extract on peripheral blood flow and eicosanoid metabolism in mammals
- Neurogasobiology of migraine: Carbon monoxide, hydrogen sulfide, and nitric oxide as emerging pathophysiological trinacrium relevant to nociception regulation
- Plant polyphenols, terpenes, and terpenoids in oral health
- Laboratory medicine between technological innovation, rights safeguarding, and patient safety: A bioethical perspective
- End-of-life in cancer patients: Medicolegal implications and ethical challenges in Europe
- The maternal factors during pregnancy for intrauterine growth retardation: An umbrella review
- Intra-abdominal hypertension/abdominal compartment syndrome of pediatric patients in critical care settings
- PI3K/Akt pathway and neuroinflammation in sepsis-associated encephalopathy
- Screening of Group B Streptococcus in pregnancy: A systematic review for the laboratory detection
- Giant borderline ovarian tumours – review of the literature
- Leveraging artificial intelligence for collaborative care planning: Innovations and impacts in shared decision-making – A systematic review
- Cholera epidemiology analysis through the experience of the 1973 Naples epidemic
- Risk factors of frailty/sarcopenia in community older adults: Meta-analysis
- Supplement strategies for infertility in overweight women: Evidence and legal insights
- Scurvy, a not obsolete disorder: Clinical report in eight young children and literature review
- A meta-analysis of the effects of DBS on cognitive function in patients with advanced PD
- Protective role of selenium in sepsis: Mechanisms and potential therapeutic strategies
- Strategies for hyperkalemia management in dialysis patients: A systematic review
- C-reactive protein-to-albumin ratio in peripheral artery disease
- Case Reports
- Delayed graft function after renal transplantation
- Semaglutide treatment for type 2 diabetes in a patient with chronic myeloid leukemia: A case report and review of the literature
- Diverse electrophysiological demyelinating features in a late-onset glycogen storage disease type IIIa case
- Giant right atrial hemangioma presenting with ascites: A case report
- Laser excision of a large granular cell tumor of the vocal cord with subglottic extension: A case report
- EsoFLIP-assisted dilation for dysphagia in systemic sclerosis: Highlighting the role of multimodal esophageal evaluation
- Molecular hydrogen-rhodiola as an adjuvant therapy for ischemic stroke in internal carotid artery occlusion: A case report
- Coronary artery anomalies: A case of the “malignant” left coronary artery and its surgical management
- Rapid Communication
- Biological properties of valve materials using RGD and EC
-
A single oral administration of flavanols enhances short
-term memory in mice along with increased brain-derived neurotrophic factor - Letter to the Editor
- Role of enhanced external counterpulsation in long COVID
- Expression of Concern
- Expression of concern “A ceRNA network mediated by LINC00475 in papillary thyroid carcinoma”
- Expression of concern “Notoginsenoside R1 alleviates spinal cord injury through the miR-301a/KLF7 axis to activate Wnt/β-catenin pathway”
- Expression of concern “circ_0020123 promotes cell proliferation and migration in lung adenocarcinoma via PDZD8”
- Corrigendum
- Corrigendum to “Empagliflozin improves aortic injury in obese mice by regulating fatty acid metabolism”
- Corrigendum to “Comparing the therapeutic efficacy of endoscopic minimally invasive surgery and traditional surgery for early-stage breast cancer: A meta-analysis”
- Corrigendum to “The progress of autoimmune hepatitis research and future challenges”
- Retraction
- Retraction of “miR-654-5p promotes gastric cancer progression via the GPRIN1/NF-κB pathway”
- Retraction of: “LncRNA CASC15 inhibition relieves renal fibrosis in diabetic nephropathy through downregulating SP-A by sponging to miR-424”
- Retraction of: “SCARA5 inhibits oral squamous cell carcinoma via inactivating the STAT3 and PI3K/AKT signaling pathways”
- Special Issue Advancements in oncology: bridging clinical and experimental research - Part II
- Unveiling novel biomarkers for platinum chemoresistance in ovarian cancer
- Lathyrol affects the expression of AR and PSA and inhibits the malignant behavior of RCC cells
- The era of increasing cancer survivorship: Trends in fertility preservation, medico-legal implications, and ethical challenges
- Bone scintigraphy and positron emission tomography in the early diagnosis of MRONJ
- Meta-analysis of clinical efficacy and safety of immunotherapy combined with chemotherapy in non-small cell lung cancer
- Special Issue Computational Intelligence Methodologies Meets Recurrent Cancers - Part IV
- Exploration of mRNA-modifying METTL3 oncogene as momentous prognostic biomarker responsible for colorectal cancer development
- Special Issue The evolving saga of RNAs from bench to bedside - Part III
- Interaction and verification of ferroptosis-related RNAs Rela and Stat3 in promoting sepsis-associated acute kidney injury
- The mRNA MOXD1: Link to oxidative stress and prognostic significance in gastric cancer
- Special Issue Exploring the biological mechanism of human diseases based on MultiOmics Technology - Part II
- Dynamic changes in lactate-related genes in microglia and their role in immune cell interactions after ischemic stroke
- A prognostic model correlated with fatty acid metabolism in Ewing’s sarcoma based on bioinformatics analysis
- Red cell distribution width predicts early kidney injury: A NHANES cross-sectional study
- Special Issue Diabetes mellitus: pathophysiology, complications & treatment
- Nutritional risk assessment and nutritional support in children with congenital diabetes during surgery
- Correlation of the differential expressions of RANK, RANKL, and OPG with obesity in the elderly population in Xinjiang
- A discussion on the application of fluorescence micro-optical sectioning tomography in the research of cognitive dysfunction in diabetes
- A review of brain research on T2DM-related cognitive dysfunction
- Metformin and estrogen modulation in LABC with T2DM: A 36-month randomized trial
- Special Issue Innovative Biomarker Discovery and Precision Medicine in Cancer Diagnostics
- CircASH1L-mediated tumor progression in triple-negative breast cancer: PI3K/AKT pathway mechanisms


