Left atrial appendage closure in conjunction with radiofrequency ablation: Effects on left atrial functioning in patients with paroxysmal atrial fibrillation
-
Jing Lv
Abstract
Objective
In the present study, we investigated the impact of left atrial appendage closure (LAAC) following catheter ablation (CA) on the left atrial structure and functioning of patients with paroxysmal atrial fibrillation (AF).
Methods
Patients with paroxysmal AF were enrolled in this single-center prospective cohort study between April 2015 and July 2021; 353 patients received CA alone, while 93 patients received CA in combination with Watchman LAAC. We used age, gender, CHA2DS2-VASc, and HAS-BLED scores as well as other demographic variables to perform propensity score matching. Patients with paroxysmal AF were randomly assigned to the CA combined with Watchman LAAC group (combined treatment group) and the simple CA group, with 89 patients in each group. The left atrial structure, reserve, ventricular diastole, and pump functions and their changes in patients were assessed using routine Doppler echocardiography and 2D speckle tracking echocardiography over the course of a 1-year follow-up.
Results
At 1-week follow-up, the reserve, ventricular diastole, and pump functions of the left atrium (LA) increased in both groups; these functions were gradually restored at the 1- to 3-month follow-up; they were close to or returned to their pre-operative levels at the 3-month follow-up; and no significant differences were found compared with the pre-operative levels at the 12-month follow-up. In the first 3 months, the reserve (Ƹ, SRs) and pump functions (SRa) in the combined treatment group decreased significantly when compared with the simple CA group, and the differences were statistically significant.
Conclusion
Patients with paroxysmal AF may experience a short term, partial effect of LAAC on LA reserve and pump functions, which are gradually restored and the effect disappears by 12 months.
1 Introduction
As a leading cause of both stroke and heart failure, atrial fibrillation (AF) is a serious issue affecting the modern world [1,2]. Patients with AF have a number of alternatives for stroke prevention; one of the options is left atrial appendage closure (LAAC), which has been shown to be as effective as, if not more successful than Warfarin and novel oral anticoagulants in avoiding ischemic stroke [3,4]. Thus, AF ablation plus LAAC (termed “one-stop surgery”) can safely and effectively restore sinus rhythm in the treatment of heart failure and prevention of stroke [5]. Under normal conditions, the left atrial appendage (LAA) performs both mechanical and endocrine roles; however, AF causes a dramatic loss in the mechanical performance of LAA, with the rate of decline differing between paroxysmal and persistent AF [6–8]. Morphology of the LAA can significantly affect pathophysiological properties of the LAA, choice of closure technique, the course of the procedure, its results, and complications. Presented morphometrical data should be considered during planning and when performing procedures targeted to LAAC, as significant differences in the anatomy of the LAA may be encountered in patients with AF. The study of Słodowska et al. confirmed that substantial morphometrical differences in LAA orifice are found, which is significantly larger and more oval in patients with AF compared to healthy controls. Although no difference in LAA body type and size is observed, the LAA ejection fraction is significantly lower in AF patients [9]. Consequently, the effect of LAAC on the left atrial structure and functions of AF patients, especially those with different types of AF is still unclear.
According to our previous studies, research on the left atrial functions of patients with persistent AF confirmed that additional LAAC had an impact on the reserve and ventricular diastole functions of left atrium (LA) within 3 months [10], with no effect on the improvement of the LA functions after catheter ablation (CA) within a year. However, no research has systematically discussed the impact of the one-stop surgery on the LA functions of patients with paroxysmal AF. In light of the substantial disparities in the LAA functions between paroxysmal AF and persistent AF, it is hypothesized that LAAC has different effects on the LA functions of patients with paroxysmal AF and with persistent AF. LAAC provides excellent results in patients with AF. LAAC is recommended for the treatment of patients with AF in whom oral anticoagulation is contraindicated and the number of procedures is increasing every year [11]. Moreover, the indications for LAAC may be expanded in the future based on the encouraging results of some clinical trials [12,13]. This study uses patients with AF treated with radiofrequency ablation alone as a control group to explore whether additional LAAC on top of CA has an impact on the left atrial function in patients with paroxysmal AF. This may provide some references for clinicians to understand the concept of a one-stop surgery, and also offer more insights into selecting the best treatment strategy for LAAC therapy.
2 Methods
2.1 Study population
In this single-center prospective cohort study, patients with paroxysmal non-valvular AF (NVAF) were selected and hospitalized in the Cardiology Department I of the Second Hospital of Hebe Medical University from April 2015 to July 2021. Paroxysmal AF is defined as AF that terminates spontaneously or with intervention within 7 days of onset. In this study, 93 patients with paroxysmal AF who were treated by CA combined with Watchman LAAC were included in the combined treatment group. This study exclusively employs endocardial LAAC for all cases. Inclusion criteria were (1) patients aged >18 years, (2) patients with symptomatic NVAF intractable with antiarrhythmic drugs, (3) patients with a high stroke risk (CHA2DS2-VASc score ≥2 points for male and ≥3 points for females), (4) patients with the HAS-BLED score ≥3 points or major hemorrhage events during anticoagulation treatment (severe organ hemorrhage such as cerebral hemorrhage), with a higher hemorrhage risk predicted, and (5) LAAC was preferred instead of long-term oral anticoagulants. Exclusion criteria included: (1) patients with LA or LAA thrombosis, (2) patients with LA enlargement (≥55 mm), (3) patients with severe valvular heart disease, (4) patients with serious sequelae after severe disabling ischemic stroke on the basis of NVAF, and (5) patients with life expectancy <1 year. In the corresponding period, 353 additional patients with paroxysmal AF who only received CA were included in the control group. Inclusion criteria were patients aged ≥18 years, with symptomatic NVAF intractable with antiarrhythmic drugs. Exclusion criteria were the same as those for the combined treatment group. Propensity score matching (PSM) extension was used at a 1:1 ratio in terms of the age, gender, CHA2DS2-VASc score, and HAS-BLED score, and 89 patients were included in the combined treatment group and the simple CA group each. The research flowchart is shown in Figure 1.

Flowchart of the study procedure. LA, left atrial; LAAC, left atrial appendage closure; AF, atrial fibrillation; treatment group; combined treatment group; control group; simple CA group.
-
Ethical approval: This study was conducted in accordance with the declaration of Helsinki. This study was conducted with approval from the Ethics Committee of The Second Hospital of Hebei Medical University (No. 2022-R134).
-
Informed consent: A written informed consent was obtained from all participants.
2.2 Procedure
One to two days before the procedure, a transesophageal echocardiography (TEE) is performed to exclude the presence of thrombi in the LA and LAA, and to evaluate the type (chicken wing type, cauliflower type, and arrowhead type), size, and depth of the LAA, as well as to measure the emptying velocity of the LAA. A pulmonary vein enhancement CT scan is conducted to assess the anterior–posterior diameter, left–right diameter, superior–inferior diameter of the LA, and the cross-sectional short axis of both pulmonary veins.
2.3 CA procedure
All procedures were performed while patients were under conscious sedation and local anesthesia. CA was performed in all cases with wide antral circumferential until the entrance and exit block was demonstrated for each pulmonary vein. With a three-dimensional electroanatomical mapping system (CARTO R@ 3; Biosense Webster, Irvine, CA, USA), the ablation catheter (Thermocool SMARTTOUCH; Biosense Webster) was inserted into the LA to perform radiofrequency ablation. The mapping catheter was used to record pulmonary vein potentials (Lasso® NAV Eco; Biosense Webster). Circumferential ablation in both the left and right pulmonary veins was confirmed. No additional ablation lines or complex fractionated atrial electrogram ablation was performed in this study. Sinus rhythm was restored by either ablation or electric cardioversion.
2.4 LAAC procedure
Occluder devices for the LAA were implanted under fluoroscopic or TEE guidance in the combined treatment group as soon as pulmonary vein isolation (PVI) was completed. After CA, the LAA was occluded with the use of occluder devices (Watchman; Boston Scientific, Marlborough, MA, USA). All patients undergoing LAAC procedures received up to 1,500 mL of 0.9% normal saline intravenous infusion to ensure the filling of the LAA. The process of Watchman implantation is shown in Figure 2. Angiography of the LAA was performed to measure the ostial width and depth. Oversizing by 10–20% of the diameter of the LAA was recommended in order to choose an appropriate device size, and the device was released in the proper position after stability testing. Before releasing the occluder device, we ensured that no or minimal (<5 mm) residual flow remained and that adjacent structures (such as the mitral annulus and circumflex coronary artery) were not compressed.
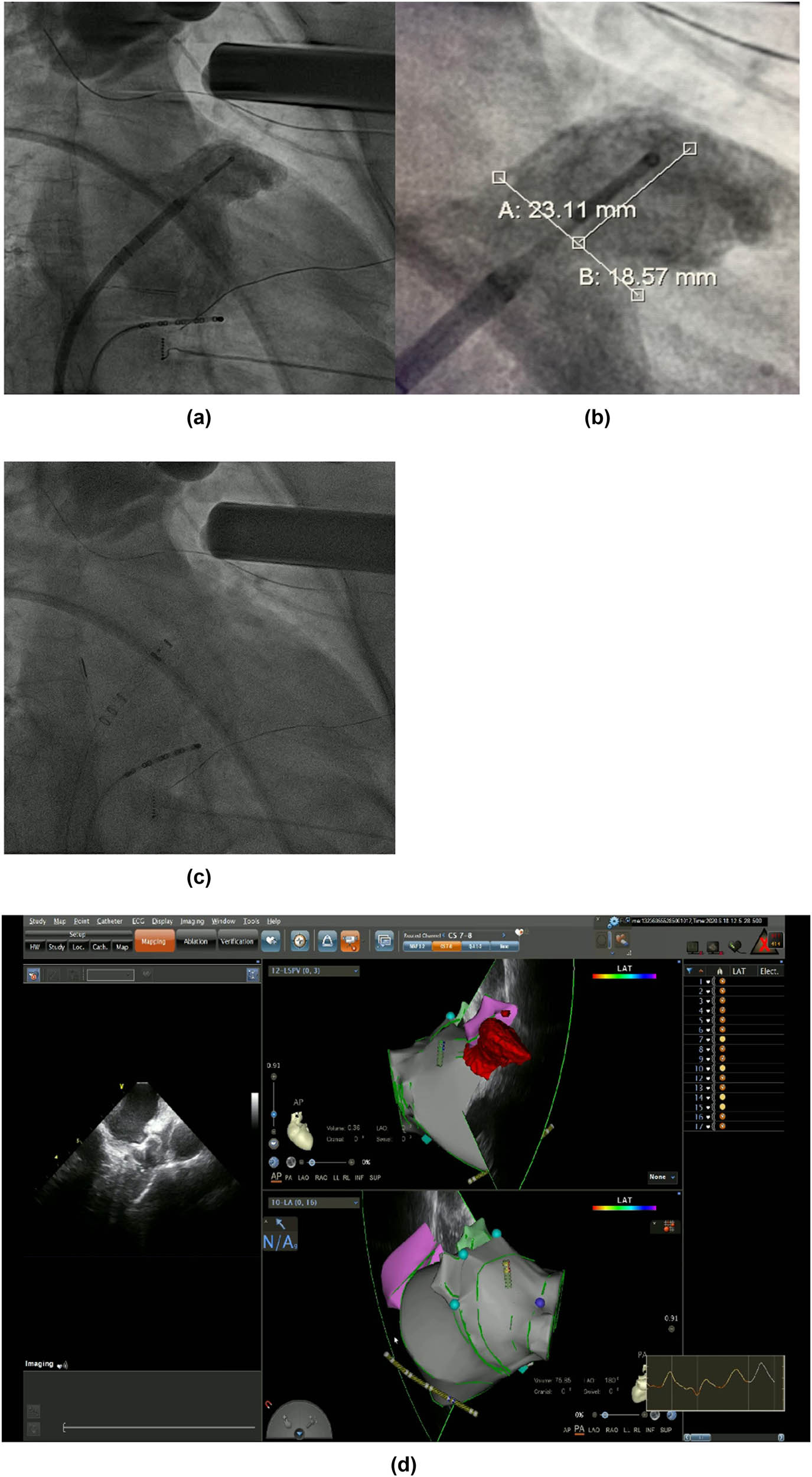
LAAC with WATCHMAN device. (a) and (b) Angiography of the LAA was performed to measure the ostial width and depth. (c) Fluoroscopic view after delivery of the WATCHMAN device in the proper position. (d) Peri-device leakage and compression were detected by TEE post-implantation.
2.5 Echocardiographic examination
The left atrial functions were determined using echocardiography (iE33 system, equipped with the X3-1 probe; Philips Medical Systems, Eindhoven, Netherlands) at baseline, 1 week, and 1, 3, and 12 months after surgery.
All patients at follow-up had sinus rhythm when 2D transthoracic echocardiography (2D-TTE) and speckle tracking echocardiography (2D-STE) was conducted. The LA volumes at three time points during the cardiac cycle were measured on the 2D-TTE: (1) at the diastasis before the bicuspid valve opened (maximum LA volume [LAVmax]), (2) the end-systolic frame before the bicuspid valve closed (minimum LA volume [LAVmin]), (3) the time of the P-wave on the echocardiography, or the last frame before the bicuspid valve opened (before atrial systole [LAVpreA]), and (4) the left atrial diameter (LAD) at the end of systole was measured on the parasternal long-axis view.
An experienced senior sonographer completed the measurement using speckle tracking technique on the Philips Qlab CMQ software based on 2D echocardiography. Three reference points were placed on the 2-chamber view, namely the anterior atrial wall, the side of the bicuspid ring free wall, and the top of atrium; three reference points were placed on the 4-chamber view, namely the side of the bicuspid ring septum, the side of the bicuspid ring free wall, and the top of atrium; three cardiac cycles were manually tracked to obtain a stable strain rate curve, and the LA sampling observation point was placed on the image of LAVmax to obtain the total LA strain (Ƹ) and LA strain rate curve. This measurement method was confirmed in our previous study [12,14]. The curve consists of an upward waveform – ventricular systolic strain rate (SRs) and two downward waveforms – early ventricular diastolic strain rate (SRe) and atrial systolic strain rate (SRa), where Ƹ and SRs reflect the atrial reserve function, SRe reflects the atrial ventricular diastole function, and SRa reflects the atria pump function.
2.6 Arrhythmia recurrence assessment
All patients were treated with antiarrhythmic drugs and anticoagulants for 3 months after surgery. Regular dosing of blood pressure medications was maintained, and no additional medications were prescribed. If no thrombus ≥5 mm related to the device or residual shunt around the device was found in the TEE examination at 3 months, patients receiving the combined treatment were advised to receive the dual antiplatelet treatment (aspirin [100 mg/day] ± clopidogrel [75 mg/day]) for another 3 months while orally taking aspirin until 1 year after surgery. Patients underwent 24 h dynamic electrocardiogram monitoring at 3 and 12 months after surgery to assess the presence of atrial arrhythmia. AF, atrial flutter, or atrial tachycardia that occurred 3 months after ablation and lasted ≥30 s were considered recurrence of AF.
2.7 Statistical analysis
Statistical analysis was conducted using SPSS Statistics, version 25 (IBM, Armonk, NY, USA). The Kolmogorov–Smirnov test was applied to determine whether the data followed a normal distribution. Normally distributed data are expressed as the mean ± standard deviation, while non-normally distributed data are presented as medians with interquartile ranges. Counting data are expressed as percentages (%). Student’s t-test (normality) or Mann–Whitney U test (non-normality) and chi-squared test were used to compare the baseline parameters between the two groups of patients. Continuous data of different indices after the operation were assessed with analysis of variance for repeated measures. To compare LA function between the two groups, we used the least significant difference test. A P-value of <0.05 was considered statistically significant. PSM analysis (1:1 matching) using age, sex, CHA2DS2-VASc score, and HAS-BLED score was performed to control for selection bias within a caliper of 0.05 on the propensity-score using SPSS 23 software.
3 Results
3.1 Baseline data
Among the 178 patients in this study, 89 patients underwent PVI combined with Watchman LAAC (combined treatment group) successfully, and 89 patients in the control group underwent CA only (simple CA group). Clinical features are shown in Table 1. There were no statistical differences in the age, gender, BMI, CHA 2 DS 2-VASc, HAS-BLED score, complications, drugs, and LAA type before ablation between the combined treatment group and the matched AF ablation group (P > 0.05). Results are shown in Table 1.
Baseline characteristics of the population
| Treatment group | Control group | P-value | |
|---|---|---|---|
| Age (years) | 64.17 ± 7.56 | 65.60 ± 8.15 | 0.23 |
| Sex, male, n (%) | 52 (58) | 44 (49) | 0.23 |
| Smoke, n (%) | 19 (21) | 15 (17) | 0.45 |
| Alcohol, n (%) | 10 (11) | 12 (14) | 0.65 |
| Hypertension, n (%) | 62 (70) | 68 (76) | 0.31 |
| Coronary artery disease, n (%) | 44 (49) | 45 (51) | 0.88 |
| Diabetes mellitus, n (%) | 24 (27) | 28 (32) | 0.51 |
| Congestive heart failure, n (%) | 41 (46) | 32 (36) | 0.17 |
| II | 31 (35) | 28 (32) | 0.63 |
| III | 9 (10) | 4 (5) | 0.15 |
| IV | 1 (1) | 0 (1) | 0.32 |
| Stroke, n (%) | 50 (56) | 46 (52) | 0.55 |
| Bleeding, n (%) | 2 (2) | 2 (2) | 1 |
| BMI | 25.76 ± 2.97 | 26.05 ± 4.06 | 0.59 |
| serum creatinine | 72.26 ± 20.28 | 72.84 ± 22.99 | 0.87 |
| CHA2DS2-VASc score | 4.16 ± 1.56 | 4.20 ± 1.69 | 0.84 |
| HAS-BLED score | 2.96 ± 0.92 | 3.10 ± 0.72 | 0.30 |
| Drugs before ablation, n (%) | |||
| AAD | 12 (13) | 10 (11) | 0.65 |
| Beta-blocker | 32 (36) | 36 (40) | 0.54 |
| ACEI or ARB | 27 (30) | 25 (28) | 0.74 |
| Aldosterone receptor antagonists | 6 (7) | 5 (6) | 0.76 |
| Other diuretics | 8 (9) | 6 (7) | 0.58 |
| LAA type, n (%) | |||
| Chicken wing type | 40 (45) | 38 (43) | 0.76 |
| Cauliflower type | 32 (36) | 35 (39) | 0.64 |
| Arrowhead type | 17 (19) | 16 (18) | 0.85 |
Data are shown as mean ± SD or n (%). BMI, body mass index; AAD, antiarrhythmic drugs; ACEI, angiotensin converting enzyme inhibitor; ARB, angiotensin-2 receptor blockade.
3.2 Intra-group comparison of left atrial functions between the two groups
Among a total of 178 patients, 37 patients were excluded due to AF or atrial flutter on echocardiography at follow-up, the remaining 141 patients (69 in the combined treatment group and 72 in the simple CA group) were included in the analysis of LA structure, Ƹ, and SR.
LAD, LAVmax, LAVpreA, and LAVmin values in the combined treatment group and simple CA group increased at 1 week compared with that before surgery, and gradually decreased from 1 month, and these parameters were similar to or slightly below the baseline levels at 12 months after ablation. There were no statistical differences in these parameters in all groups when compared with those before surgery. Results are shown in Table 2 and Figure 3.
Evolution of LA function after the LAAC combined with CA and simple CA group assessed volumetric indices
| Variables | Groups | Baseline | 1 W | 1 M | 3 M | 12 M | P-value |
|---|---|---|---|---|---|---|---|
| LA D | Treatment group | 36.80 ± 4.61 | 37.54 ± 4.41 | 36.83 ± 4.20 | 36.18 ± 4.29 | 36.20 ± 4.33 | 0.003 |
| P for time | 0.341 | 0.975 | 0.412 | 0.432 | |||
| Control group | 35.93 ± 4.55 | 36.90 ± 4.41 | 36.11 ± 4.11 | 35.49 ± 4.23 | 35.29 ± 3.59 | 0.001 | |
| P for time | 0.196 | 0.802 | 0.547 | 0.354 | |||
| LAVmax | Treatment group | 60.05 ± 15.63 | 64.39 ± 14.58 | 60.95 ± 13.78 | 58.30 ± 15.32 | 55.48 ± 15.69 | <0.001 |
| P for time | 0.101 | 0.724 | 0.519 | 0.097 | |||
| Control group | 59.22 ± 17.07 | 61.61 ± 18.47 | 58.69 ± 18.69 | 57.15 ± 15.26 | 55.07 ± 13.45 | 0.011 | |
| P for time | 0.422 | 0.860 | 0.444 | 0.107 | |||
| LAVpreA | Treatment group | 48.91 ± 24.03 | 51.42 ± 17.02 | 48.49 ± 17.02 | 46.70 ± 16.20 | 44.44 ± 16.88 | 0.021 |
| P for time | 0.486 | 0.909 | 0.535 | 0.216 | |||
| Control group | 45.41 ± 15.78 | 47.18 ± 15.95 | 44.48 ± 15.64 | 42.26 ± 14.53 | 41.73 ± 12.98 | 0.104 | |
| P for time | 0.519 | 0.730 | 0.224 | 0.135 | |||
| LAVmin | Treatment group | 30.36 ± 14.10 | 34.73 ± 13.23 | 31.26 ± 11.85 | 29.02 ± 13.26 | 28.08 ± 15.41 | 0.001 |
| P for time | 0.069 | 0.694 | 0.572 | 0.375 | |||
| Control group | 28.64 ± 13.81 | 31.32 ± 13.50 | 28.19 ± 11.81 | 27.00 ± 10.01 | 26.27 ± 9.56 | 0.008 | |
| P for time | 0.241 | 0.836 | 0.416 | 0.235 |
Data are shown as mean ± S. P for time is the P value of the relevant parameters compared with their baseline values at a single follow-up time point.
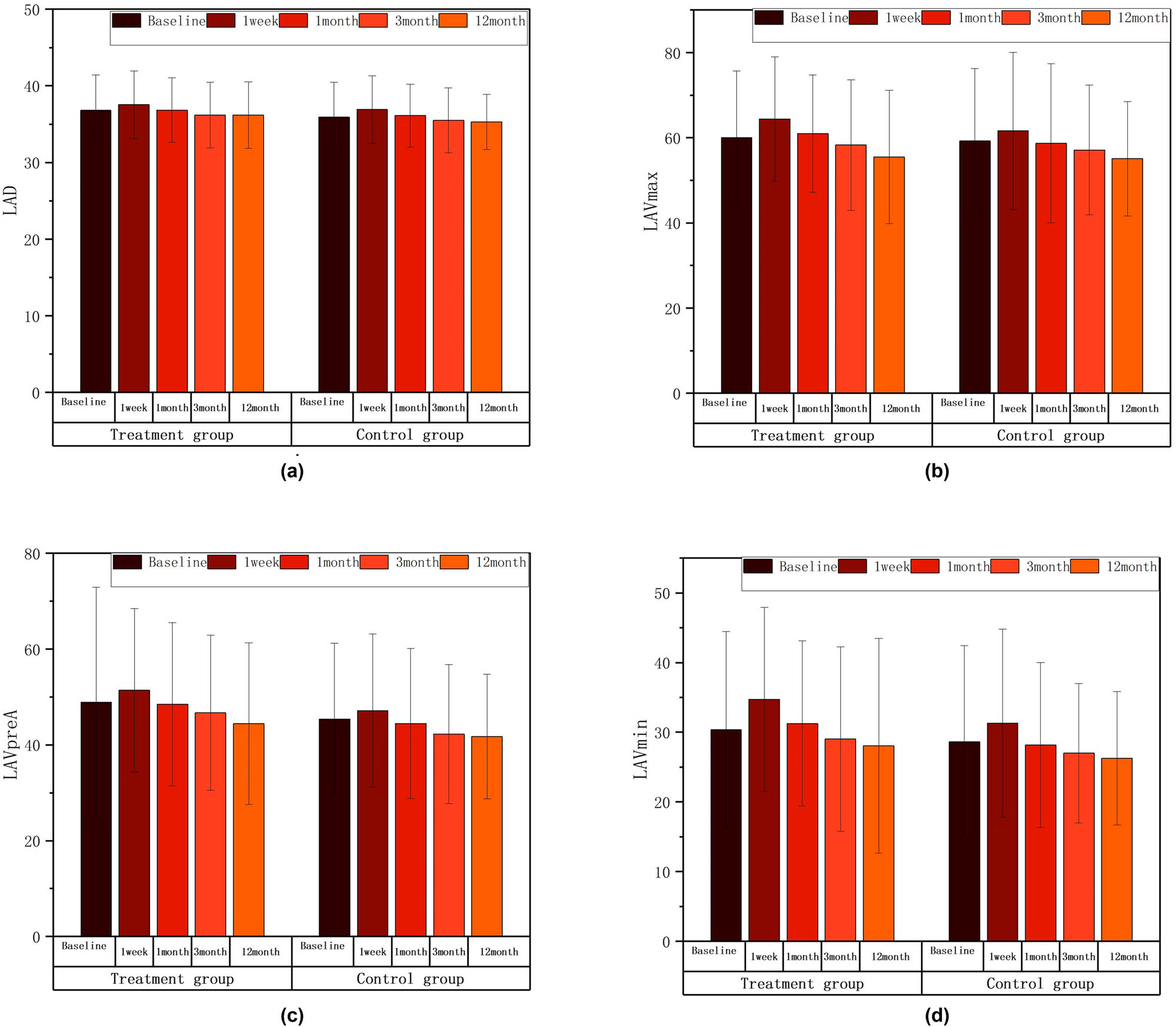
LAD, LAVmax, LAVpreA, LAVmin intra-group comparison diagram; ∗P < 0.05; ∗∗P < 0.01; ∗∗∗P < 0.001 compared with the baseline level. There were no statistical differences in these parameters in all groups when compared with those before surgery. The postoperative comparison of parameters representing left atrial structure, such as LAD (a), LAVmax (b), LAVpreA (c), and LAVmin (d), did not show any statistically significant differences when compared to the preoperative values in both groups.
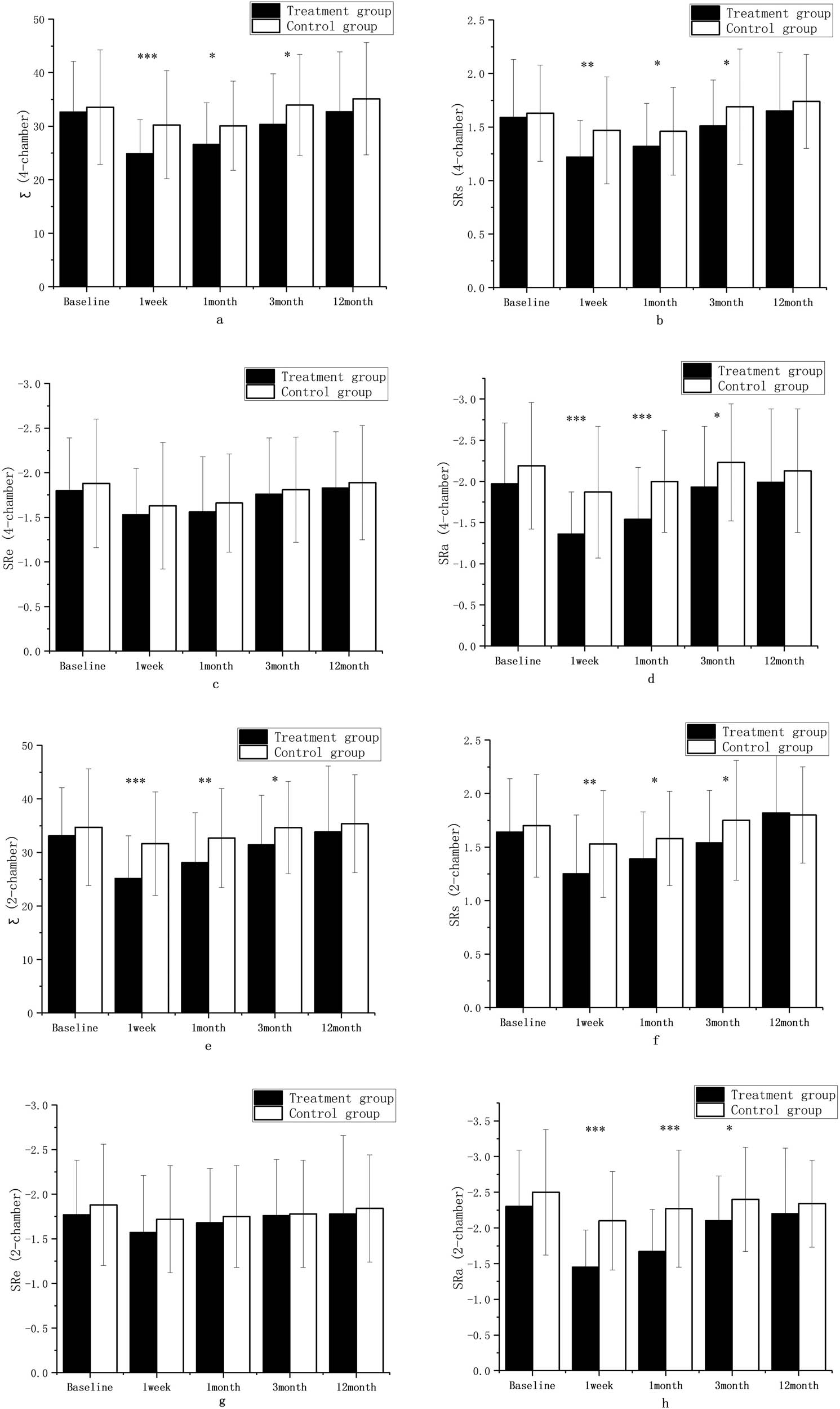
The values of Ƹ, SRs, SRe, and SRa in the 2-chamber and 4-chamber views in the two groups decreased at 1 week compared with that before surgery, and gradually increased from 1–3 months to 12 months with a consistent trend in the two groups, and these parameters were similar to or slightly below the baseline levels at 12 months after ablation. Compared with those before surgery, Ƹ (4-chamber), SRs (4-chamber), the absolute value of SRa (4-chamber), Ƹ (2-chamber), SRs (2-chamber), and the absolute value of SRa (2-chamber) in the combined treatment group significantly decreased at 1 week (P < 0.001), the absolute value of SRe (4-chamber) in the combined treatment group and the absolute value of SRa (2-chamber) in the simple CA group significantly decreased at 1 week (P < 0.01), and SRs (4-chamber), the absolute values of SRe (4-chamber), the absolute values of SRa (4-chamber), and SRs (2-chamber) in the simple CA group decreased at 1 week (P < 0.05). Compared with those before surgery, Ƹ (4-chamber), the absolute value of SRa (4-chamber), and the absolute value of SRa (2-chamber) in the combined treatment group significantly decreased at 1 month (P < 0.001); Ƹ (2-chamber) in the combined treatment group and SRs (2-chamber) in the simple CA group significantly decreased at 1 month (P < 0.01); SRs (4-chamber) and the absolute value of SRe (4-chamber) in the combined treatment group and Ƹ (4-chamber), SRs (4-chamber), and the absolute value of SRe (4-chamber) in the simple CA group significantly decreased at 1 month (P < 0.05). There were no statistical differences in the Ƹ, SRs, SRe, and SRa values on 2-chamber and 4-chamber views between the two groups at 3 and 12 months when compared with those before surgery. Results are shown in Table 3 and Figure 4.
Evolution of LA function after the LAAC combined with CA and simple CA group assessed strain indices
| Variables | Groups | Baseline | 1 W | 1 M | 3 M | 12 M | P-value |
|---|---|---|---|---|---|---|---|
| Ƹ (4-chamber) | Treatment group | 32.67 ± 9.41 | 24.85 ± 6.35 | 26.57 ± 7.81 | 30.35 ± 9.45 | 32.71 ± 11.20 | <0.001 |
| P for time | <0.001 | <0.001 | 0.151 | 0.980 | |||
| Control group | 33.56 ± 10.72 | 30.25 ± 10.09 | 30.07 ± 8.33 | 33.93 ± 9.46 | 35.13 ± 10.47 | <0.001 | |
| P for time | 0.059 | 0.031 | 0.824 | 0.376 | |||
| SRs (4-chamber) | Treatment group | 1.59 ± 0.54 | 1.22 ± 0.34 | 1.32 ± 0.40 | 1.51 ± 0.43 | 1.65 ± 0.55 | <0.001 |
| P for time | <0.001 | 0.01 | 0.336 | 0.519 | |||
| Control group | 1.63 ± 0.45 | 1.47 ± 0.50 | 1.46 ± 0.41 | 1.69 ± 0.54 | 1.74 ± 0.44 | <0.001 | |
| P for time | 0.040 | 0.020 | 0.482 | 0.151 | |||
| SRe (4-chamber) | Treatment group | −1.80 ± 0.59 | −1.53 ± 0.52 | −1.56 ± 0.62 | −1.76 ± 0.63 | −1.83 ± 0.63 | <0.001 |
| P for time | 0.037 | 0.047 | 0.538 | 0.922 | |||
| Control group | −1.88 ± 0.72 | −1.63 ± 0.71 | −1.66 ± 0.55 | −1.81 ± 0.59 | −1.89 ± 0.64 | 0.001 | |
| P for time | 0.003 | 0.002 | 0.32 | 0.90 | |||
| SRa (4-chamber) | Treatment group | −1.97 ± 0.74 | −1.36 ± 0.51 | −1.54 ± 0.63 | −1.93 ± 0.74 | −1.99 ± 0.89 | <0.001 |
| P for time | <0.001 | <0.001 | 0.738 | 0.895 | |||
| Control group | −2.19 ± 0.77 | −1.87 ± 0.80 | −2.00 ± 0.62 | −2.23 ± 0.71 | −2.13 ± 0.75 | 0.001 | |
| P for time | 0.016 | 0.106 | 0.729 | 0.641 | |||
| Ƹ (2-chamber) | Treatment group | 33.09 ± 9.01 | 25.14 ± 7.95 | 28.10 ± 9.32 | 31.45 ± 9.23 | 33.83 ± 12.30 | <0.001 |
| P for time | <0.001 | 0.002 | 0.293 | 0.688 | |||
| Control group | 34.72 ± 10.89 | 31.65 ± 9.68 | 32.68 ± 9.25 | 34.64 ± 8.65 | 35.35 ± 9.15 | 0.012 | |
| P for time | 0.076 | 0.227 | 0.960 | 0.710 | |||
| SRs (2-chamber) | Treatment group | 1.64 ± 0.50 | 1.25 ± 0.55 | 1.39 ± 0.44 | 1.54 ± 0.49 | 1.82 ± 0.60 | <0.001 |
| P for time | <0.001 | 0.02 | 0.203 | 0.072 | |||
| Control group | 1.70 ± 0.48 | 1.53 ± 0.50 | 1.58 ± 0.44 | 1.75 ± 0.56 | 1.80 ± 0.45 | <0.001 | |
| P for time | 0.046 | 0.136 | 0.538 | 0.179 | |||
| SRe (2-chamber) | Treatment group | −1.77 ± 0.61 | −1.57 ± 0.64 | −1.68 ± 0.61 | −1.76 ± 0.63 | −1.78 ± 0.88 | 0.004 |
| P for time | 0.064 | 0. 357 | 0.931 | 0.962 | |||
| Control group | −1.88 ± 0.68 | −1.72 ± 0.60 | −1.75 ± 0.57 | −1.78 ± 0.60 | −1.84 ± 0.60 | 0.213 | |
| P for time | 0.143 | 0.235 | 0.363 | 0.706 | |||
| SRa (2-chamber) | Treatment group | −2.30 ± 0.79 | −1.45 ± 0.52 | −1.67 ± 0.59 | −2.10 ± 0.63 | −2.20 ± 0.92 | <0.001 |
| P for time | <0.001 | <0.001 | 0.104 | 0.505 | |||
| Control group | −2.50 ± 0.88 | −2.10 ± 0.69 | −2.27 ± 0.82 | −2.40 ± 0.73 | −2.34 ± 0.61 | <0.001 | |
| P for time | 0.003 | 0.111 | 0.455 | 0.227 |
Data are shown as mean ± S. P for time is the P value of the relevant parameters compared with their baseline values at a single follow-up time point.
![Figure 4
Reserve (SRs [2-chamber (f), 4-chamber (b)]), ventricular diastole (SRe [2-chamber (g), 4-chamber (c)]), and pump (Ƹ [2-chamber (e), 4-chamber (a)], SRa [2-chamber (h), 4-chamber (d)]) functions of the LA intra-group comparison diagram; ∗P < 0.05; ∗∗P < 0.01; ∗∗∗P < 0.001 compared with the baseline level.](/document/doi/10.1515/med-2024-0951/asset/graphic/j_med-2024-0951_fig_004.jpg)
Reserve (SRs [2-chamber (f), 4-chamber (b)]), ventricular diastole (SRe [2-chamber (g), 4-chamber (c)]), and pump (Ƹ [2-chamber (e), 4-chamber (a)], SRa [2-chamber (h), 4-chamber (d)]) functions of the LA intra-group comparison diagram; ∗P < 0.05; ∗∗P < 0.01; ∗∗∗P < 0.001 compared with the baseline level.
3.3 Comparison of left atrial functions between two groups
There was consistency in the changes of the structural function (LAD, LAVmax, LAVpreA, LAVmin), the reserve function (Ƹ, SRs), the ventricular diastole function (SRe), and the pump function (SRa) of LA in patients in the combined treatment group and simple CA group over time. Results are shown in Figures 5 and 6.
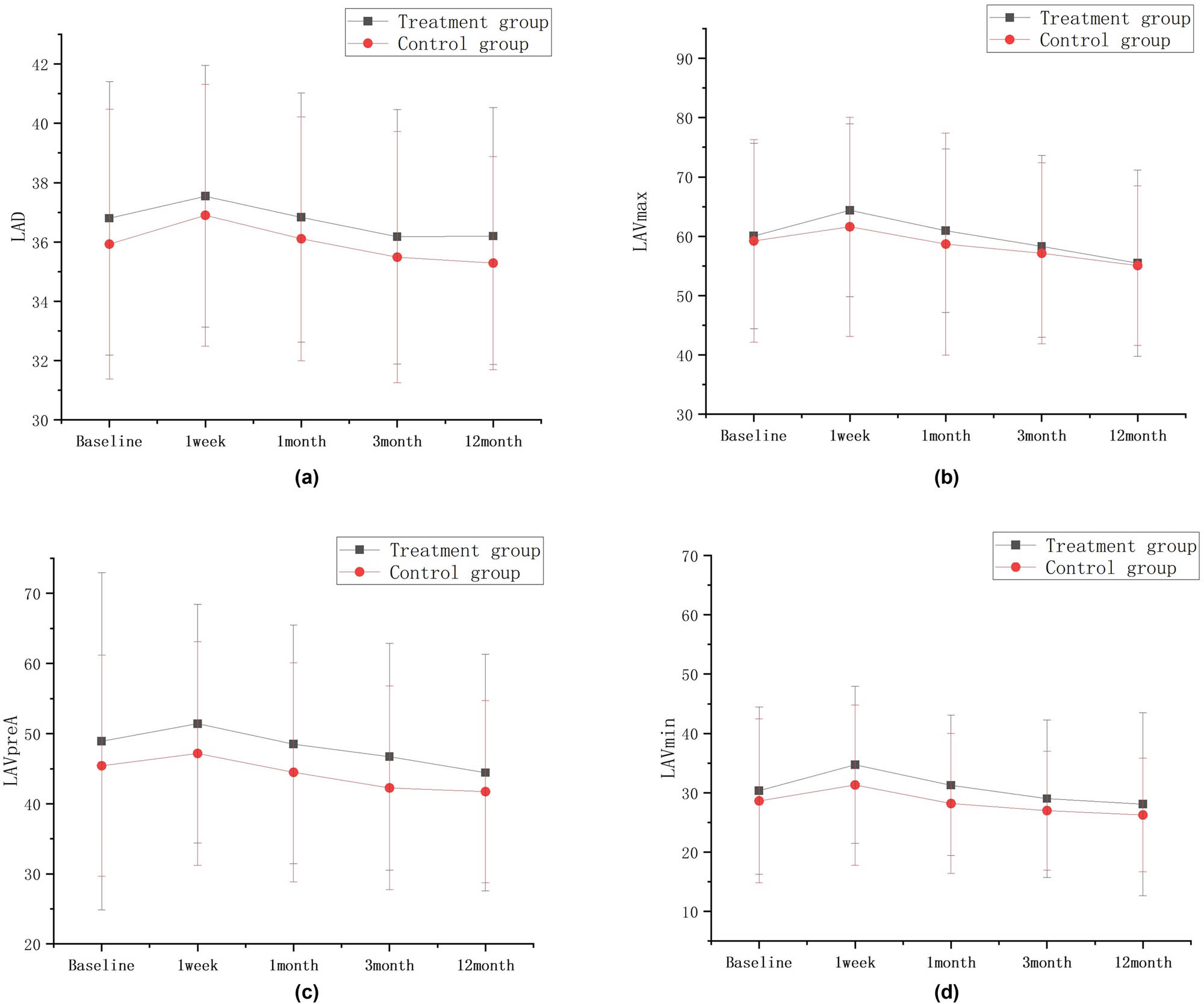
Left atrial structure LAD (a), LAVmax (b), LAVpreA (c), and LAVmin (d) trend chart.
![Figure 6
Reserve (SRs [2-chamber (f), 4-chamber (b)]), ventricular diastole (SRe [2-chamber (g), 4-chamber (c)]), and pump (Ƹ [2-chamber (e), 4-chamber (a)], SRa 2-chamber (h), 4-chamber (d)]) functions of the LA trend chart.](/document/doi/10.1515/med-2024-0951/asset/graphic/j_med-2024-0951_fig_006.jpg)
Reserve (SRs [2-chamber (f), 4-chamber (b)]), ventricular diastole (SRe [2-chamber (g), 4-chamber (c)]), and pump (Ƹ [2-chamber (e), 4-chamber (a)], SRa 2-chamber (h), 4-chamber (d)]) functions of the LA trend chart.
The structural functions of LA structure between the two groups (LAD, LAVmax, LAVpreA, LAVmin) and channel function (SRe (4-chamber), SRe (2-chamber) were not statistically significant between the two groups at each time point. The atrial catheter function (ventricular diastole function) (Ƹ [4-chamber], Ƹ [2-chamber], SRs [4-chamber], SRs [2-chamber]) and atrial pump function (SRa [4-chamber], SRa [2-chamber]) during the follow-up at 1 week, 1 month, and 3 months were significantly different between the two groups, and the values were lower in the combined treatment group than in the simple CA group. There were no statistical differences in the reserve function (Ƹ [4-chamber], SRs [4-chamber], Ƹ [2-chamber], SRs [2-chamber]), and the pump function (SRa [4-chamber], SRa [2-chamber]) between the two groups at the 12-month follow-up. Results are shown in Figures 7 and 8.
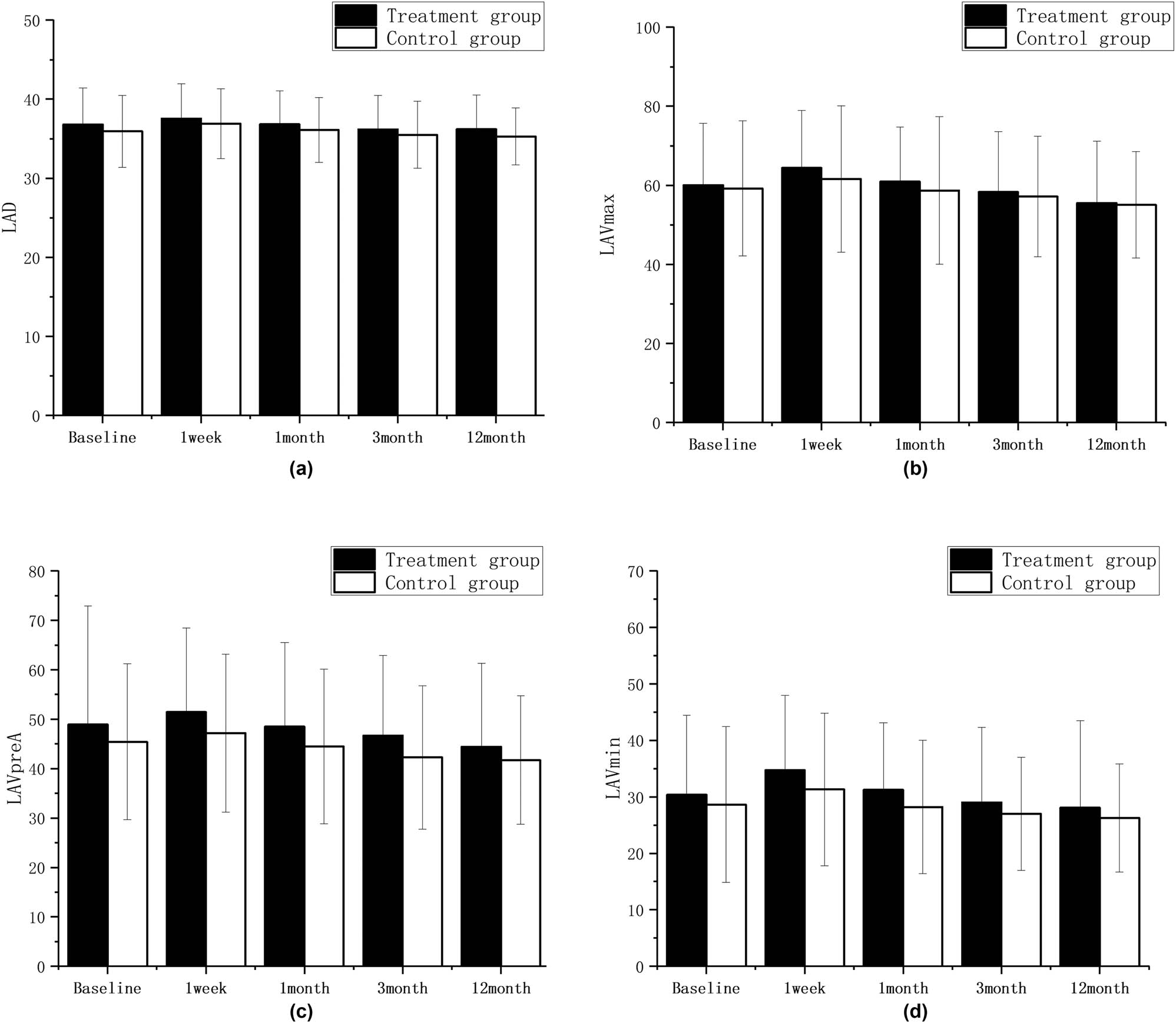
LAD (a), LAVmax (b), LAVpreA (c), and LAVmin (d) comparison diagram between groups; ∗P < 0.05; ∗∗P < 0.01; ∗∗∗P < 0.001 vs control group.
Ƹ (4-chamber) (a), SRs(4-chamber) (b), SRe (4-chamber) (c), SRa (4-chamber) (d), Ƹ (2-chamber) (e), SRs (2-chamber) (f), SRe (2-chamber) (g), SRa (2-chamber) (h) comparison diagram between groups; ∗P < 0.05; ∗∗P < 0.01; ∗∗∗P < 0.001 vs control group.
3.4 Clinical outcome
All surgeries were successful, and all implants were well sealed (residual shunt <5 mm) in the combined treatment group. Three patients in the combined treatment group and one patient in the simple CA group developed pericardial effusion during the surgery; however, they recovered normally after percutaneous drainage. During the 3-month follow-up, one patient in the combined treatment group was found to have erythrocyte spontaneous contrast in the LA using TEE, and one patient with recurrent AF in the simple CA group developed ischemic stroke at 6 months. In the combined treatment group, one patient developed severe cerebral hemorrhage at 3 months, one patient had gingival bleeding at 9 months, and one patient had pseudoaneurysm at 1 month, and no bleeding death was reported. In the simple CA group, one patient developed a small amount of hemoptysis during surgery, one patient had hematoma of the groin 10 days after surgery, and one patient with cerebral hemorrhage 2 months after AF ablation recovered after conservative treatment. All patients underwent pulmonary vein isolation to restore sinus rhythm. During the 12-month follow-up, no device dislocation occurred; 20 patients (23%) in the combined treatment group and 17 patients (19%) in the simple CA group developed recurrent AF or atrial flutter. There was no statistical difference between the two groups.
4 Discussion
In a retrospective, observational matched pair study [14], LAAC did not impair the left atrial systolic function or the left atrial ejection fraction, compared with patients with untreated LAA, while the echocardiography at follow-up showed that the reserve and ventricular diastole functions of LA were significantly impaired in both groups. Dar et al. [15] and Murtaza et al. [16] studied patients implanted with Lariat and Watchman occluders using Doppler imaging and STE and found no improvement in the reserve and ventricular diastole functions of LA after LAAC. The results of some studies suggest that LAAC causes no significant changes in the LA and left heart functions although LAA accounts for 10% or so of the total volume of LA [17]. Other studies also support the contention that there is no negative effect on the heart function after LAA excision [18]. The study includes both endocardial and epicardial LAAC, which can impact the assessment of left atrial function. However, the effect of LAAC on the left atrial function in patients with different types of AF have not been reported as yet.
In our study, among the two groups of patients, the most common LAA type was the chicken wing type, followed by the cauliflower type, with the arrowhead type being less common. This distribution aligns with previous research findings [19]. Known for the pathological connection to AF, the LAA is the most common source of thromboembolism in patients with AF and may be an arrhythmogenic source for the maintenance of AF. Potential interventions of the LAA for stroke prevention have recently been developed through better understanding its anatomy and physiology. LAAC is an alternative to the use of life-long anticoagulation in selected NVAF cases. Among participants with AF who had undergone cardiac surgery, most of whom continued to receive ongoing antithrombotic therapy, the risk of ischemic stroke or systemic embolism was lower with concomitant LAAC performed during the surgery than without it [20]. However, the LAA is structurally complex and has considerable morphological variations among individuals, and it can be challenging to generalize the device for all patients. Continued technological developments including occlusion/ligation through epicardial, endocardial, or surgical approaches, as well as operator expertise regarding LAA anatomy, physiology, and pathophysiology, should improve interventional outcomes. The absence of trials comparing each LAAC modality, as with the novel anticoagulant therapy, makes it difficult to decide which therapy is superior for patients. Since each LAAC technique offers unique benefits and risks, patient selection must be individualized. Anatomical recognition of the location of the LAA ostium, definition and management of device leaks, and management of LAA with variant anatomy remain important topics to be addressed [21]. The neck of the LAA is a smooth-walled, truncated cone-shaped channel located between its pectinated component and the body of the LA. Notably, the current research found that there are no statistically significant differences or correlations regarding the LAA type and the LAA neck morphometry. Precise definition and morphometrical details of the LAA neck that were introduced in previous study may influence the effectiveness and safety of LAA exclusion procedures [22]. LAAC can be performed via epicardial access or endocardial access with an occlusion device. Endocardial and epicardial LAAC techniques shows comparable implantation outcomes and safety profile and stroke prevention in patients with AF [23]. The number of LAAC is systematically increasing worldwide. Unfortunately, LAAC, like any invasive procedure, carries a risk of complications. One of the worst, but rare, complications of LAAC is coronary artery damage. The study showed that most dangerous distances (30.2%) occurred in the LAA landing zone dimension. The data showed that landing zones more distal from the orifice of the LAA are safer in terms of the circumflex artery damage. Therefore, LAAC should always be performed with caution, to avoid iatrogenic complications [24].
In this study, changes in the reserve, ventricular diastole, and pump functions of LA over time were consistent in the two groups – the functions decreased at 1 week and gradually recovered at 1 month, and there were no significant differences when compared with the values before surgery at the 12-month follow-up. The reasons may be that the heat effect of CA may cause damage and necrosis to cardiac muscle tissue in LA, which leads to edema and scar tissue formation, followed by secondary conduction dysfunction that leads to non-uniform contraction of atrial muscle tissue, transient increase of LAD, and transient decrease of LA ejection fraction; finally, transient decline in LA functions and atrial stunning occur. However, these changes in LA functions are reversible and recoverable. An aberrant state of LA electro-mechanical connection was produced by atrial stunning 1 week after surgery, and it was gradually restored within 3 months [25]. Our previous studies indicated that patients with paroxysmal AF in the three groups showed significant decrease in the total LA strain (εP), LA reserve function strain (SRP), LA ventricular diastole function strain (SRE), and LA pump function strain (SRA) on the 2-chamber and 4-chamber views at 7 days after ablation [26], which suggested left atrial stunning; these parameters gradually recovered within 4 weeks to 3 months after ablation, and were completely restored to the baseline levels within 9 months after ablation. Our findings of the changes in the left atrial functions are in line with the results of previous studies [26,27,28]. Given that thromboembolic events are linked to atrial stasis, we emphasized the significance of appropriate anticoagulant therapy in both groups 3 months after surgery.
The results of our previous studies suggested that patients with persistent AF in the combined treatment group and the simple CA group started to show significant improvement in the left atrial functions at 1 week, which continued till 3 months and maintained till 12 months [10]. In this study, the difference was that the left atrial functions of patients with paroxysmal AF in the two groups significantly decreased at 1 week and 1 month after the surgery when compared with the baseline levels, and were gradually restored to the preoperative levels at 3 months and remained at 12 months. The discrepancy between studies may be due, in large part, to the fact that various forms of AF have varying impacts on hemodynamics following one-stop surgery [10]. Prior to surgery, the left atrial function of most patients with paroxysmal AF was significantly higher than that of patients with persistent AF. Patients with paroxysmal AF tended to have more normal left atrial function at baseline, suggesting that there was less room for improvement in left atrial function following ablation. Patients who have persistent AF, on the other hand, experience the opposite. Left atrial enlargement is evident in patients with persistent AF prior to surgery, and left atrial function is typically below normal at baseline; however, left atrial function improves more significantly after ablation. The different responses of left atrial functions to ablation can be explained as follows. AF ablation on atrial myocardium has an inherently detrimental effect on LA functions, and the atrial function impairment may last 2–3 months while leading to LA reverse remodeling by reducing the AF burden [29]. This beneficial effect is most obvious in patients with persistent AF with high AF burden and impaired baseline functions [30]. Thus, the effect of AF ablation on LA function depends on the balance of these detrimental and beneficial effects. Several studies have revealed that patients with persistent AF who recovered their sinus rhythm after successful CA, developed significant LA reverse remodeling in the long term [31–33]. A further comparative study showed that patients with persistent AF had significant improvement in the left atrial functions than those with paroxysmal AF after ablation [28].
On the other hand, additional LAAC influenced the reserve and ventricular diastole functions of LA within 3 months among patients with persistent AF who underwent one-stop surgery, while the results of our study showed that the reserve and pump (contraction) functions of LA were affected by LAAC within the first 3 months. The reasons for this may be that with faster LAA emptying and better LA and LAA contraction functions in patients with paroxysmal AF than in those with persistent AF, the paroxysmal AF contraction functions may be affected more severely in early LAAC. Previous studies have indicated that patients with paroxysmal AF have better LA and LAA contraction functions, and LAAC leads to a dramatic decrease in LA compliance in the short term, followed by the increase in the size and pressure of LA and decrease in the cardiac output, resulting in decrease in the LA reserve function, which may influence the reserve and contraction functions of LA in the short and medium term.
Our study’s strength lies in its ability to elucidate the effect of LAAC on the left atrial functions after eliminating the effect of CA by comparing patients in the one-stop surgery group with those in the simple CA group. During the 3-month follow-up, and especially at 1 week and 1 month, patients in the combined treatment group had significantly decreased reserve function (Ƹ, SRs) and pump function (SRa) of LA compared with the simple CA group, and the difference was statistically significant at 3 months; there was no difference in the left atrial functions after 3 months. The causes may be as follows. First, LAA has some important functions with its unique anatomical and physiological properties, and these functions and their contribution to cardiac hemodynamics have been confirmed. Besides, due to the higher compliance than LA and an important role in the presence of LA pressure and/or volume overload [34], LAA may affect the LA reserve and contraction functions in the short term after LAAC. The mechanical properties of the LAA are determined by its contractile characteristics, playing a role in hemodynamic function by regulating left atrial pressure. As a part of the LA, the LAA possesses a certain capacity and is structurally more pliable than the rest of the LA. When there is an overload in volume or pressure within the LA, the LAA can expand to become an important reservoir, alleviating pressure in the LA and ensuring adequate blood filling of the left ventricle [35]. Second, LAA has little contribution to the stroke volume, thus LAAC is of little significance in the Frank–Starlin mechanism. The Frank–Starlin mechanism describes the relationship between the increased length of myocardial fiber and its mechanical property, showing an essential therapeutic and prognostic value in the evaluation of left atrial functions. Previous studies indicated that the Frank–Starling mechanism was also found in the LA [36]. The LA is the reservoir, ventricular diastole, and booster pump that returns blood from the lungs to the heart. In previous studies, as the LA preload increased, the LA contractility increased to a certain extent and then decreased, which indicated that there was a Frank–Starlin mechanism. Using 2D/3D TEE (TTE and 2D STI), Coisne et al. [37] found that the reserve and contraction functions of LA, such as LA volume index, LA reserve volume, LAEF, and LA strain, were improved after one-stop surgery. This may be attributed to the Frank–Staring compensatory mechanism rather than the changes in the intrinsic myocardial properties. Our study used patients with AF treated solely with radiofrequency ablation as the control group. We found that the additional LAAC on top of CA had a short-term impact on the left atrial reservoir and pump function in patients with paroxysmal AF, which gradually returned to normal.
5 Limitations
There are limitations to this study. Due to the low number of patients treated with LAAC at our center, a single control group was unavailable to directly indicate the efficacy of LAAC on LA functions. We observed no significant changes in the volume and strain parameters at 12 months when compared with that before surgery, thus only long-term data can reveal whether the result is persistent or transient. Therefore, these deficiencies should be considered and further investigated. Study was not randomized, inclusion criteria differed in important parts and lack of some data which was declared to be measured may lead to data bias. Additionally, it is suspected that the population was ethnically homogenous. Additionally, only one type of LAAC procedure was used.
6 Conclusion
The left atrial functions decreased in the two groups at 1 week and 1 month, but they were close to or restored to the preoperative levels at 3 months. When compared with the simple CA group, patients in the combined treatment group showed a significant decrease in the reserve function and pump functions of the LA within the first 3 months; however, there were no statistical differences at 12 months between the two groups, suggesting that LAAC may have partial short-term impact on LA reserve function and pump function of patients with paroxysmal AF; these functions were later restored gradually, and were not affected at 12 months.
-
Funding information: This study was supported by the Natural Science Foundation of Hebei Province (No. H2020206081).
-
Author contributions: Conception and design of the research: Jing Lv, Ruiqin Xie, Jing Yang, and Ling You; acquisition of data: Rui Wang, Chao Yang, Yan Zhang, Qian Liu, and Jinting Liu; analysis and interpretation of the data: Rui Wang, Chao Yang, Qian Liu, Lei Yin, and Jinting Liu; statistical analysis: Yan Zhang and Lei Yin; obtaining financing: Ruiqin Xie; writing of the manuscript: Jing Lv and Ruiqin Xie; critical revision of the manuscript for intellectual content: Ruiqin Xie, Jing Yang, and Ling You. All authors read and approved the final draft.
-
Conflict of interest: All authors have contributed significantly to the manuscript and declare that the work is original and has not been submitted or published elsewhere. None of the authors have any financial disclosure or conflict of interest.
-
Data availability statement: The datasets used and/or analyzed during the current study available from the corresponding author on reasonable request.
References
[1] Chieng D, Ling LH, Kaye DM. Reply: Heart failure with atrial fibrillation: who will benefit the most from atrial fibrillation ablation? JACC Heart Fail. 2023;12:1770. 10.1016/j.jchf.2023.09.017.Suche in Google Scholar PubMed
[2] Smith EE, Yaghi S, Sposato LA, Fisher M. Atrial fibrillation detection and load: knowledge gaps related to stroke prevention. Stroke. 2024;55:205–13. 10.1161/STROKEAHA.123.043665.Suche in Google Scholar PubMed
[3] Osmancik P, Herman D, Neuzil P, Hala P, Taborsky M, Kala P, et al. 4-year outcomes after left atrial appendage closure versus nonwarfarin oral anticoagulation for atrial fibrillation. J Am Coll Cardiol. 2022;79:1–14. 10.1016/j.jacc.2021.10.023. Epub 2021 Nov 5.Suche in Google Scholar PubMed
[4] Turagam MK, Osmancik P, Neuzil P, Dukkipati SR, Reddy VY. Left atrial appendage closure versus oral anticoagulants in atrial fibrillation: a meta-analysis of randomized trials. J Am Coll Cardiol. 2020;76:2795–7. 10.1016/j.jacc.2020.08.089.Suche in Google Scholar PubMed
[5] Phillips KP, Romanov A, Artemenko S, Folkeringa RJ, Szili-Torok T, Senatore G, et al. Combining left atrial appendage closure and catheter ablation for atrial fibrillation: 2-year outcomes from a multinational registry. Europace. 2020;22:225–31. 10.1093/europace/euz286.Suche in Google Scholar PubMed
[6] Schweizer J, Arnold M, König IR, Bicvic A, Westphal LP, Schütz V, et al. Measurement of midregional pro-atrial natriuretic peptide to discover atrial fibrillation in patients with ischemic stroke. J Am Coll Cardiol. 2022;79:1369–81. 10.1016/j.jacc.2022.01.042.Suche in Google Scholar PubMed
[7] Yang Z, Subati T, Kim K, Murphy MB, Dougherty OP, Christopher IL, et al. Natriuretic peptide oligomers cause proarrhythmic metabolic and electrophysiological effects in atrial myocytes. Circ Arrhythmia Electrophysiol. 2022;15:e010636. 10.1161/CIRCEP.121.010636.Suche in Google Scholar PubMed PubMed Central
[8] Kouibaran FR, Sabatino M, Barozzi C, Diemberger I. Atrial natriuretic peptides as a bridge between atrial fibrillation, heart failure, and amyloidosis of the atria. Int J Mol Sci. 2023;24:6470. 10.3390/ijms24076470.Suche in Google Scholar PubMed PubMed Central
[9] Słodowska KM, Batko J, Hołda JP, Dudkiewicz D, Koziej M, Litwinowicz R, et al. Morphometrical features of left atrial appendage in the atrial fibrillation patients subjected to left atrial appendage closure. Folia Morphol. 2023;82:814–21. 10.5603/FM.a2022.0080.Suche in Google Scholar PubMed
[10] Yang J, Liu Y, Feng L, Liu M, You L, Liu Y, et al. Effect of left atrial appendage closure in combination with catheter ablation on left atrial function for persistent atrial fibrillation. Front Cardiovasc Med. 2021;8:666465. 10.3389/fcvm.2021.666465.Suche in Google Scholar PubMed PubMed Central
[11] Hindricks G, Potpara T, Dagres N, Arbelo E, Bax JJ, Blomström-Lundqvist C, et al. 2020 ESC guidelines for the diagnosis and management of atrial fibrillation developed in collaboration with the European Association for Cardio-Thoracic Surgery (EACTS): the Task Force for the diagnosis and management of atrial fibrillation of the European Society of Cardiology (ESC) developed with the special contribution of the European Heart Rhythm Association (EHRA) of the ESC. Eur Heart J. 2021;42:373–498.10.1093/eurheartj/ehab648Suche in Google Scholar PubMed
[12] Litwinowicz R, Bartus M, Malec-Litwinowicz M, Michalski M, Banaszkiewicz K, Kapelak B, et al. Left atrial appendage occlusion for secondary stroke prevention in patients with atrial fibrillation: long-term results. Cerebrovasc Dis. 2019;47:188–95.10.1159/000500850Suche in Google Scholar PubMed
[13] Litwinowicz R, Bartus M, Ceranowicz P, Brzezinski M, Kapelak B, Lakkireddy D, et al. Left atrial appendage occlusion for stroke prevention in diabetes mellitus patients with atrial fibrillation: long-term results. J Diabetes. 2019;11:75–82.10.1111/1753-0407.12824Suche in Google Scholar PubMed
[14] De Maat GE, Benussi S, Hummel YM, Krul S, Pozzoli A, Driessen AH, et al. Surgical left atrial appendage exclusion does not impair left atrial contraction function: a pilot study. Biomed Res Int. 2015;2015:318901. 10.1155/2015/318901.Suche in Google Scholar PubMed PubMed Central
[15] Dar T, Afzal MR, Yarlagadda B, Kutty S, Shang Q, Gunda S, et al. Mechanical function of the left atrium is improved with epicardial ligation of the left atrial appendage: insights from the LAFIT-LARIAT registry. Heart Rhythm. 2018;15:955–9. 10.1016/j.hrthm.2018.02.022.Suche in Google Scholar PubMed
[16] Murtaza G, Vuddanda V, Akella K, Rocca DG, Sharma S, Li L, et al. Impact of left atrial appendage occlusion on left atrial function – the LAFIT Watchman study. J Interv Card Electrophysiol. 2020;58:163–7. 10.1007/s10840-019-00674-0.Suche in Google Scholar PubMed
[17] Asmarats L, Bernier M, O’Hara G, Paradis JM, O’Connor K, Beaudoin J, et al. Hemodynamic impact of percutaneous left atrial appendage closure in patients with paroxysmal atrial fibrillation. J Interv Card Electrophysiol. 2018;53:151–7. 10.1007/s10840-018-0387-2.Suche in Google Scholar PubMed
[18] Inoue T, Suematsu Y. Left atrial appendage resection can be performed minimally invasively with good clinical and echocardiographic outcomes without any severe risk. Eur J Cardiothorac Surg. 2018;54:78–83. 10.1093/ejcts/ezx506.Suche in Google Scholar PubMed
[19] Słodowska K, Szczepanek E, Dudkiewicz D, Hołda J, Bolechała F, Strona M, et al. Morphology of the left atrial appendage: introduction of a new simplified shape-based classification system. Heart Lung Circ. 2021;30:1014–22. 10.1016/j.hlc.2020.12.006.Suche in Google Scholar PubMed
[20] Whitlock RP, Belley-Cote EP, Paparella D, Healey JS, Brady K, Sharma M, et al. Left atrial appendage occlusion during cardiac surgery to prevent stroke. N Engl J Med. 2021;384:2081–91. 10.1056/NEJMoa2101897.Suche in Google Scholar PubMed
[21] Naksuk N, Padmanabhan D, Yogeswaran V, Asirvatham SJ. Left atrial appendage. JACC: Clin Electrophysiol. 2016;2:403–12. 10.1016/j.jacep.2016.06.006.Suche in Google Scholar PubMed
[22] Batko J, Jakiel R, Krawczyk–Ożóg A, Litwinowicz R, Hołda J, Bartuś S, et al. Definition and anatomical description of the left atrial appendage neck. Clin Anat. 2023;37:201–9. 10.1002/ca.24125.Suche in Google Scholar PubMed
[23] Litwinowicz R, Burysz M, Mazur P, Kapelak B, Bartus M, Lakkireddy D, et al. Endocardial versus epicardial left atrial appendage exclusion for stroke prevention in patients with atrial fibrillation: midterm follow‐up. J Cardiovasc Electrophysiol. 2020;32:93–101. 10.1111/jce.14802.Suche in Google Scholar PubMed
[24] Batko J, Rams D, Filip G, Bartoszcze A, Kapelak B, Bartuś K, et al. Left atrial appendage morphology and course of the circumflex artery: anatomical implications for left atrial appendage occlusion procedures. Innov: Technol Tech Cardiothorac Vasc Surg. 2022;17:424–9. 10.1177/15569845221128569.Suche in Google Scholar PubMed
[25] Zhang Y, Sun H, Li M, Luo M, Xu F, Shao Y, et al. Impact of stand-alone minimally invasive radiofrequency ablation with left atrial appendectomy on left atrial function assessed by echocardiography. Quant Imaging Med Surg. 2020;10:970–8. 10.21037/qims.2020.03.01.Suche in Google Scholar PubMed PubMed Central
[26] You L, Yao L, Zhou B, Jin L, Yin H, Wu J, et al. Effects of different ablation strategies on long-term left atrial function in patients with paroxysmal atrial fibrillation: a single-blind randomized controlled trial. Sci Rep. 2019;9:7695. 10.1038/s41598-019-44168-5.Suche in Google Scholar PubMed PubMed Central
[27] Yin GL, Xie RQ, You L, Yin HN, Sun YC, Wu JL, et al. Left atrial function, inflammation, and prothrombotic response after radiofrequency ablation for atrial fibrillation. J Chin Med Assoc. 2018;81:409–15. 10.1016/j.jcma.2017.12.001.Suche in Google Scholar PubMed
[28] Liu Y, Liu Q, Yang Y, Zhang C, Yin H, Wu J, et al. Effect of radiofrequency catheter ablation on left atrial structure and function in patients with different types of atrial fibrillation. Sci Rep. 2022;12:9511. 10.1038/s41598-022-13725-w.Suche in Google Scholar PubMed PubMed Central
[29] Angelini E, Sieweke JT, Berliner D, Biber S, Hohmann S, Oldhafer M, et al. Echocardiographic parameters indicating left atrial reverse remodeling after catheter ablation for atrial fibrillation. Front Cardiovasc Med. 2023;18:1270422. 10.3389/fcvm.2023.1270422.Suche in Google Scholar PubMed PubMed Central
[30] Hirose K, Nakanishi K, Daimon M, Iwama K, Yoshida Y, Mukai Y, et al. Association of atrial fibrillation progression with left atrial functional reserve and its reversibility. J Am Heart Assoc. 2024;13:e032215. 10.1161/JAHA.123.032215.Suche in Google Scholar PubMed PubMed Central
[31] Khan HR, Yakupoglu HY, Hans IK, Haldar S, Bahrami T, Clague J, et al. Left atrial function predicts atrial arrhythmia recurrence following ablation of long-standing persistent atrial fibrillation. Circ Cardiovasc Imaging. 2023;16:e015352. 10.1161/CIRCIMAGING.123.015352.Suche in Google Scholar PubMed PubMed Central
[32] Kriatselis C, Unruh T, Kaufmann J, Gerds-Li JH, Kelle S, Gebker R, et al. Long-term left atrial remodeling after ablation of persistent atrial fibrillation: 7-year follow-up by cardiovascular magnetic resonance imaging. J Interv Card Electrophysiol. 2020;58:21–7.10.1007/s10840-019-00584-1Suche in Google Scholar PubMed
[33] Assaf AY, Noujaim C, Mekhael M, Younes H, Chouman N, Dhore-Patil A, et al. Early remodeling of the left atrium following catheter ablation of atrial fibrillation: Insights from DECAAFII. JACC Clin Electrophysiol. 2023;9:2253–62. 10.1016/j.jacep.2023.07.025.Suche in Google Scholar PubMed
[34] Spencer RJ, DeJong P, Fahmy P, Lempereur M, Tsang MY, Gin KG, et al. Changes in left atrial appendage dimensions following volume loading during percutaneous left atrial appendage closure. JACC Cardiovasc Interv. 2015;8:1935–41.10.1016/j.jcin.2015.07.035Suche in Google Scholar PubMed
[35] Karim N, Ho SY, Nicol E, Li W, Zemrak F, Markides V, et al. The left atrial appendage in humans:structure, physiology, and pathogenesis. Europace. 2020;22:5–18.10.1093/europace/euz212Suche in Google Scholar PubMed
[36] Khokhlova A, Myachina T, Butova X, Volzhaninov D, Berg V, Kochurova A, et al. Differing effects of estrogen deficiency on the contractile function of atrial and ventricular myocardium. Biochem Biophys Res Commun. 2021;541:30–5. 10.1016/j.bbrc.2020.12.102.Suche in Google Scholar PubMed
[37] Coisne A, Pilato R, Brigadeau F, Klug D, Marquie C, Souissi Z, et al. Percutaneous left atrial appendage closure improves left atrial mechanical function through Frank–Starling mechanism. Heart Rhythm. 2017;14:710–6.10.1016/j.hrthm.2017.01.042Suche in Google Scholar PubMed
© 2024 the author(s), published by De Gruyter
This work is licensed under the Creative Commons Attribution 4.0 International License.
Artikel in diesem Heft
- Research Articles
- EDNRB inhibits the growth and migration of prostate cancer cells by activating the cGMP-PKG pathway
- STK11 (LKB1) mutation suppresses ferroptosis in lung adenocarcinoma by facilitating monounsaturated fatty acid synthesis
- Association of SOX6 gene polymorphisms with Kashin-Beck disease risk in the Chinese Han population
- The pyroptosis-related signature predicts prognosis and influences the tumor immune microenvironment in dedifferentiated liposarcoma
- METTL3 attenuates ferroptosis sensitivity in lung cancer via modulating TFRC
- Identification and validation of molecular subtypes and prognostic signature for stage I and stage II gastric cancer based on neutrophil extracellular traps
- Novel lumbar plexus block versus femoral nerve block for analgesia and motor recovery after total knee arthroplasty
- Correlation between ABCB1 and OLIG2 polymorphisms and the severity and prognosis of patients with cerebral infarction
- Study on the radiotherapy effect and serum neutral granulocyte lymphocyte ratio and inflammatory factor expression of nasopharyngeal carcinoma
- Transcriptome analysis of effects of Tecrl deficiency on cardiometabolic and calcium regulation in cardiac tissue
- Aflatoxin B1 induces infertility, fetal deformities, and potential therapies
- Serum levels of HMW adiponectin and its receptors are associated with cytokine levels and clinical characteristics in chronic obstructive pulmonary disease
- METTL3-mediated methylation of CYP2C19 mRNA may aggravate clopidogrel resistance in ischemic stroke patients
- Understand how machine learning impact lung cancer research from 2010 to 2021: A bibliometric analysis
- Pressure ulcers in German hospitals: Analysis of reimbursement and length of stay
- Metformin plus L-carnitine enhances brown/beige adipose tissue activity via Nrf2/HO-1 signaling to reduce lipid accumulation and inflammation in murine obesity
- Downregulation of carbonic anhydrase IX expression in mouse xenograft nasopharyngeal carcinoma model via doxorubicin nanobubble combined with ultrasound
- Feasibility of 3-dimensional printed models in simulated training and teaching of transcatheter aortic valve replacement
- miR-335-3p improves type II diabetes mellitus by IGF-1 regulating macrophage polarization
- The analyses of human MCPH1 DNA repair machinery and genetic variations
- Activation of Piezo1 increases the sensitivity of breast cancer to hyperthermia therapy
- Comprehensive analysis based on the disulfidptosis-related genes identifies hub genes and immune infiltration for pancreatic adenocarcinoma
- Changes of serum CA125 and PGE2 before and after high-intensity focused ultrasound combined with GnRH-a in treatment of patients with adenomyosis
- The clinical value of the hepatic venous pressure gradient in patients undergoing hepatic resection for hepatocellular carcinoma with or without liver cirrhosis
- Development and validation of a novel model to predict pulmonary embolism in cardiology suspected patients: A 10-year retrospective analysis
- Downregulation of lncRNA XLOC_032768 in diabetic patients predicts the occurrence of diabetic nephropathy
- Circ_0051428 targeting miR-885-3p/MMP2 axis enhances the malignancy of cervical cancer
- Effectiveness of ginkgo diterpene lactone meglumine on cognitive function in patients with acute ischemic stroke
- The construction of a novel prognostic prediction model for glioma based on GWAS-identified prognostic-related risk loci
- Evaluating the impact of childhood BMI on the risk of coronavirus disease 2019: A Mendelian randomization study
- Lactate dehydrogenase to albumin ratio is associated with in-hospital mortality in patients with acute heart failure: Data from the MIMIC-III database
- CD36-mediated podocyte lipotoxicity promotes foot process effacement
- Efficacy of etonogestrel subcutaneous implants versus the levonorgestrel-releasing intrauterine system in the conservative treatment of adenomyosis
- FLRT2 mediates chondrogenesis of nasal septal cartilage and mandibular condyle cartilage
- Challenges in treating primary immune thrombocytopenia patients undergoing COVID-19 vaccination: A retrospective study
- Let-7 family regulates HaCaT cell proliferation and apoptosis via the ΔNp63/PI3K/AKT pathway
- Phospholipid transfer protein ameliorates sepsis-induced cardiac dysfunction through NLRP3 inflammasome inhibition
- Postoperative cognitive dysfunction in elderly patients with colorectal cancer: A randomized controlled study comparing goal-directed and conventional fluid therapy
- Long-pulsed ultrasound-mediated microbubble thrombolysis in a rat model of microvascular obstruction
- High SEC61A1 expression predicts poor outcome of acute myeloid leukemia
- Comparison of polymerase chain reaction and next-generation sequencing with conventional urine culture for the diagnosis of urinary tract infections: A meta-analysis
- Secreted frizzled-related protein 5 protects against renal fibrosis by inhibiting Wnt/β-catenin pathway
- Pan-cancer and single-cell analysis of actin cytoskeleton genes related to disulfidptosis
- Overexpression of miR-532-5p restrains oxidative stress response of chondrocytes in nontraumatic osteonecrosis of the femoral head by inhibiting ABL1
- Autologous liver transplantation for unresectable hepatobiliary malignancies in enhanced recovery after surgery model
- Clinical analysis of incomplete rupture of the uterus secondary to previous cesarean section
- Abnormal sleep duration is associated with sarcopenia in older Chinese people: A large retrospective cross-sectional study
- No genetic causality between obesity and benign paroxysmal vertigo: A two-sample Mendelian randomization study
- Identification and validation of autophagy-related genes in SSc
- Long non-coding RNA SRA1 suppresses radiotherapy resistance in esophageal squamous cell carcinoma by modulating glycolytic reprogramming
- Evaluation of quality of life in patients with schizophrenia: An inpatient social welfare institution-based cross-sectional study
- The possible role of oxidative stress marker glutathione in the assessment of cognitive impairment in multiple sclerosis
- Compilation of a self-management assessment scale for postoperative patients with aortic dissection
- Left atrial appendage closure in conjunction with radiofrequency ablation: Effects on left atrial functioning in patients with paroxysmal atrial fibrillation
- Effect of anterior femoral cortical notch grade on postoperative function and complications during TKA surgery: A multicenter, retrospective study
- Clinical characteristics and assessment of risk factors in patients with influenza A-induced severe pneumonia after the prevalence of SARS-CoV-2
- Analgesia nociception index is an indicator of laparoscopic trocar insertion-induced transient nociceptive stimuli
- High STAT4 expression correlates with poor prognosis in acute myeloid leukemia and facilitates disease progression by upregulating VEGFA expression
- Factors influencing cardiovascular system-related post-COVID-19 sequelae: A single-center cohort study
- HOXD10 regulates intestinal permeability and inhibits inflammation of dextran sulfate sodium-induced ulcerative colitis through the inactivation of the Rho/ROCK/MMPs axis
- Mesenchymal stem cell-derived exosomal miR-26a induces ferroptosis, suppresses hepatic stellate cell activation, and ameliorates liver fibrosis by modulating SLC7A11
- Endovascular thrombectomy versus intravenous thrombolysis for primary distal, medium vessel occlusion in acute ischemic stroke
- ANO6 (TMEM16F) inhibits gastrointestinal stromal tumor growth and induces ferroptosis
- Prognostic value of EIF5A2 in solid tumors: A meta-analysis and bioinformatics analysis
- The role of enhanced expression of Cx43 in patients with ulcerative colitis
- Choosing a COVID-19 vaccination site might be driven by anxiety and body vigilance
- Role of ICAM-1 in triple-negative breast cancer
- Cost-effectiveness of ambroxol in the treatment of Gaucher disease type 2
- HLA-DRB5 promotes immune thrombocytopenia via activating CD8+ T cells
- Efficacy and factors of myofascial release therapy combined with electrical and magnetic stimulation in the treatment of chronic pelvic pain syndrome
- Efficacy of tacrolimus monotherapy in primary membranous nephropathy
- Mechanisms of Tripterygium wilfordii Hook F on treating rheumatoid arthritis explored by network pharmacology analysis and molecular docking
- FBXO45 levels regulated ferroptosis renal tubular epithelial cells in a model of diabetic nephropathy by PLK1
- Optimizing anesthesia strategies to NSCLC patients in VATS procedures: Insights from drug requirements and patient recovery patterns
- Alpha-lipoic acid upregulates the PPARγ/NRF2/GPX4 signal pathway to inhibit ferroptosis in the pathogenesis of unexplained recurrent pregnancy loss
- Correlation between fat-soluble vitamin levels and inflammatory factors in paediatric community-acquired pneumonia: A prospective study
- CD1d affects the proliferation, migration, and apoptosis of human papillary thyroid carcinoma TPC-1 cells via regulating MAPK/NF-κB signaling pathway
- miR-let-7a inhibits sympathetic nerve remodeling after myocardial infarction by downregulating the expression of nerve growth factor
- Immune response analysis of solid organ transplantation recipients inoculated with inactivated COVID-19 vaccine: A retrospective analysis
- The H2Valdien derivatives regulate the epithelial–mesenchymal transition of hepatoma carcinoma cells through the Hedgehog signaling pathway
- Clinical efficacy of dexamethasone combined with isoniazid in the treatment of tuberculous meningitis and its effect on peripheral blood T cell subsets
- Comparison of short-segment and long-segment fixation in treatment of degenerative scoliosis and analysis of factors associated with adjacent spondylolisthesis
- Lycopene inhibits pyroptosis of endothelial progenitor cells induced by ox-LDL through the AMPK/mTOR/NLRP3 pathway
- Methylation regulation for FUNDC1 stability in childhood leukemia was up-regulated and facilitates metastasis and reduces ferroptosis of leukemia through mitochondrial damage by FBXL2
- Correlation of single-fiber electromyography studies and functional status in patients with amyotrophic lateral sclerosis
- Risk factors of postoperative airway obstruction complications in children with oral floor mass
- Expression levels and clinical significance of serum miR-19a/CCL20 in patients with acute cerebral infarction
- Physical activity and mental health trends in Korean adolescents: Analyzing the impact of the COVID-19 pandemic from 2018 to 2022
- Evaluating anemia in HIV-infected patients using chest CT
- Ponticulus posticus and skeletal malocclusion: A pilot study in a Southern Italian pre-orthodontic court
- Causal association of circulating immune cells and lymphoma: A Mendelian randomization study
- Assessment of the renal function and fibrosis indexes of conventional western medicine with Chinese medicine for dredging collaterals on treating renal fibrosis: A systematic review and meta-analysis
- Comprehensive landscape of integrator complex subunits and their association with prognosis and tumor microenvironment in gastric cancer
- New target-HMGCR inhibitors for the treatment of primary sclerosing cholangitis: A drug Mendelian randomization study
- Population pharmacokinetics of meropenem in critically ill patients
- Comparison of the ability of newly inflammatory markers to predict complicated appendicitis
- Comparative morphology of the cruciate ligaments: A radiological study
- Immune landscape of hepatocellular carcinoma: The central role of TP53-inducible glycolysis and apoptosis regulator
- Serum SIRT3 levels in epilepsy patients and its association with clinical outcomes and severity: A prospective observational study
- SHP-1 mediates cigarette smoke extract-induced epithelial–mesenchymal transformation and inflammation in 16HBE cells
- Acute hyper-hypoxia accelerates the development of depression in mice via the IL-6/PGC1α/MFN2 signaling pathway
- The GJB3 correlates with the prognosis, immune cell infiltration, and therapeutic responses in lung adenocarcinoma
- Physical fitness and blood parameters outcomes of breast cancer survivor in a low-intensity circuit resistance exercise program
- Exploring anesthetic-induced gene expression changes and immune cell dynamics in atrial tissue post-coronary artery bypass graft surgery
- Empagliflozin improves aortic injury in obese mice by regulating fatty acid metabolism
- Analysis of the risk factors of the radiation-induced encephalopathy in nasopharyngeal carcinoma: A retrospective cohort study
- Reproductive outcomes in women with BRCA 1/2 germline mutations: A retrospective observational study and literature review
- Evaluation of upper airway ultrasonographic measurements in predicting difficult intubation: A cross-section of the Turkish population
- Prognostic and diagnostic value of circulating IGFBP2 in pancreatic cancer
- Postural stability after operative reconstruction of the AFTL in chronic ankle instability comparing three different surgical techniques
- Research trends related to emergence agitation in the post-anaesthesia care unit from 2001 to 2023: A bibliometric analysis
- Frequency and clinicopathological correlation of gastrointestinal polyps: A six-year single center experience
- ACSL4 mediates inflammatory bowel disease and contributes to LPS-induced intestinal epithelial cell dysfunction by activating ferroptosis and inflammation
- Affibody-based molecular probe 99mTc-(HE)3ZHER2:V2 for non-invasive HER2 detection in ovarian and breast cancer xenografts
- Effectiveness of nutritional support for clinical outcomes in gastric cancer patients: A meta-analysis of randomized controlled trials
- The relationship between IFN-γ, IL-10, IL-6 cytokines, and severity of the condition with serum zinc and Fe in children infected with Mycoplasma pneumoniae
- Paraquat disrupts the blood–brain barrier by increasing IL-6 expression and oxidative stress through the activation of PI3K/AKT signaling pathway
- Sleep quality associate with the increased prevalence of cognitive impairment in coronary artery disease patients: A retrospective case–control study
- Dioscin protects against chronic prostatitis through the TLR4/NF-κB pathway
- Association of polymorphisms in FBN1, MYH11, and TGF-β signaling-related genes with susceptibility of sporadic thoracic aortic aneurysm and dissection in the Zhejiang Han population
- Application value of multi-parameter magnetic resonance image-transrectal ultrasound cognitive fusion in prostate biopsy
- Laboratory variables‐based artificial neural network models for predicting fatty liver disease: A retrospective study
- Decreased BIRC5-206 promotes epithelial–mesenchymal transition in nasopharyngeal carcinoma through sponging miR-145-5p
- Sepsis induces the cardiomyocyte apoptosis and cardiac dysfunction through activation of YAP1/Serpine1/caspase-3 pathway
- Assessment of iron metabolism and iron deficiency in incident patients on incident continuous ambulatory peritoneal dialysis
- Tibial periosteum flap combined with autologous bone grafting in the treatment of Gustilo-IIIB/IIIC open tibial fractures
- The application of intravenous general anesthesia under nasopharyngeal airway assisted ventilation undergoing ureteroscopic holmium laser lithotripsy: A prospective, single-center, controlled trial
- Long intergenic noncoding RNA for IGF2BP2 stability suppresses gastric cancer cell apoptosis by inhibiting the maturation of microRNA-34a
- Role of FOXM1 and AURKB in regulating keratinocyte function in psoriasis
- Parental control attitudes over their pre-school children’s diet
- The role of auto-HSCT in extranodal natural killer/T cell lymphoma
- Significance of negative cervical cytology and positive HPV in the diagnosis of cervical lesions by colposcopy
- Echinacoside inhibits PASMCs calcium overload to prevent hypoxic pulmonary artery remodeling by regulating TRPC1/4/6 and calmodulin
- ADAR1 plays a protective role in proximal tubular cells under high glucose conditions by attenuating the PI3K/AKT/mTOR signaling pathway
- The risk of cancer among insulin glargine users in Lithuania: A retrospective population-based study
- The unusual location of primary hydatid cyst: A case series study
- Intraoperative changes in electrophysiological monitoring can be used to predict clinical outcomes in patients with spinal cavernous malformation
- Obesity and risk of placenta accreta spectrum: A meta-analysis
- Shikonin alleviates asthma phenotypes in mice via an airway epithelial STAT3-dependent mechanism
- NSUN6 and HTR7 disturbed the stability of carotid atherosclerotic plaques by regulating the immune responses of macrophages
- The effect of COVID-19 lockdown on admission rates in Maternity Hospital
- Temporal muscle thickness is not a prognostic predictor in patients with high-grade glioma, an experience at two centers in China
- Luteolin alleviates cerebral ischemia/reperfusion injury by regulating cell pyroptosis
- Therapeutic role of respiratory exercise in patients with tuberculous pleurisy
- Effects of CFTR-ENaC on spinal cord edema after spinal cord injury
- Irisin-regulated lncRNAs and their potential regulatory functions in chondrogenic differentiation of human mesenchymal stem cells
- DMD mutations in pediatric patients with phenotypes of Duchenne/Becker muscular dystrophy
- Combination of C-reactive protein and fibrinogen-to-albumin ratio as a novel predictor of all-cause mortality in heart failure patients
- Significant role and the underly mechanism of cullin-1 in chronic obstructive pulmonary disease
- Ferroptosis-related prognostic model of mantle cell lymphoma
- Observation of choking reaction and other related indexes in elderly painless fiberoptic bronchoscopy with transnasal high-flow humidification oxygen therapy
- A bibliometric analysis of Prader-Willi syndrome from 2002 to 2022
- The causal effects of childhood sunburn occasions on melanoma: A univariable and multivariable Mendelian randomization study
- Oxidative stress regulates glycogen synthase kinase-3 in lymphocytes of diabetes mellitus patients complicated with cerebral infarction
- Role of COX6C and NDUFB3 in septic shock and stroke
- Trends in disease burden of type 2 diabetes, stroke, and hypertensive heart disease attributable to high BMI in China: 1990–2019
- Purinergic P2X7 receptor mediates hyperoxia-induced injury in pulmonary microvascular endothelial cells via NLRP3-mediated pyroptotic pathway
- Investigating the role of oviductal mucosa–endometrial co-culture in modulating factors relevant to embryo implantation
- Analgesic effect of external oblique intercostal block in laparoscopic cholecystectomy: A retrospective study
- Elevated serum miR-142-5p correlates with ischemic lesions and both NSE and S100β in ischemic stroke patients
- Correlation between the mechanism of arteriopathy in IgA nephropathy and blood stasis syndrome: A cohort study
- Risk factors for progressive kyphosis after percutaneous kyphoplasty in osteoporotic vertebral compression fracture
- Predictive role of neuron-specific enolase and S100-β in early neurological deterioration and unfavorable prognosis in patients with ischemic stroke
- The potential risk factors of postoperative cognitive dysfunction for endovascular therapy in acute ischemic stroke with general anesthesia
- Fluoxetine inhibited RANKL-induced osteoclastic differentiation in vitro
- Detection of serum FOXM1 and IGF2 in patients with ARDS and their correlation with disease and prognosis
- Rhein promotes skin wound healing by activating the PI3K/AKT signaling pathway
- Differences in mortality risk by levels of physical activity among persons with disabilities in South Korea
- Review Articles
- Cutaneous signs of selected cardiovascular disorders: A narrative review
- XRCC1 and hOGG1 polymorphisms and endometrial carcinoma: A meta-analysis
- A narrative review on adverse drug reactions of COVID-19 treatments on the kidney
- Emerging role and function of SPDL1 in human health and diseases
- Adverse reactions of piperacillin: A literature review of case reports
- Molecular mechanism and intervention measures of microvascular complications in diabetes
- Regulation of mesenchymal stem cell differentiation by autophagy
- Molecular landscape of borderline ovarian tumours: A systematic review
- Advances in synthetic lethality modalities for glioblastoma multiforme
- Investigating hormesis, aging, and neurodegeneration: From bench to clinics
- Frankincense: A neuronutrient to approach Parkinson’s disease treatment
- Sox9: A potential regulator of cancer stem cells in osteosarcoma
- Early detection of cardiovascular risk markers through non-invasive ultrasound methodologies in periodontitis patients
- Advanced neuroimaging and criminal interrogation in lie detection
- Maternal factors for neural tube defects in offspring: An umbrella review
- The chemoprotective hormetic effects of rosmarinic acid
- CBD’s potential impact on Parkinson’s disease: An updated overview
- Progress in cytokine research for ARDS: A comprehensive review
- Utilizing reactive oxygen species-scavenging nanoparticles for targeting oxidative stress in the treatment of ischemic stroke: A review
- NRXN1-related disorders, attempt to better define clinical assessment
- Lidocaine infusion for the treatment of complex regional pain syndrome: Case series and literature review
- Trends and future directions of autophagy in osteosarcoma: A bibliometric analysis
- Iron in ventricular remodeling and aneurysms post-myocardial infarction
- Case Reports
- Sirolimus potentiated angioedema: A case report and review of the literature
- Identification of mixed anaerobic infections after inguinal hernia repair based on metagenomic next-generation sequencing: A case report
- Successful treatment with bortezomib in combination with dexamethasone in a middle-aged male with idiopathic multicentric Castleman’s disease: A case report
- Complete heart block associated with hepatitis A infection in a female child with fatal outcome
- Elevation of D-dimer in eosinophilic gastrointestinal diseases in the absence of venous thrombosis: A case series and literature review
- Four years of natural progressive course: A rare case report of juvenile Xp11.2 translocations renal cell carcinoma with TFE3 gene fusion
- Advancing prenatal diagnosis: Echocardiographic detection of Scimitar syndrome in China – A case series
- Outcomes and complications of hemodialysis in patients with renal cancer following bilateral nephrectomy
- Anti-HMGCR myopathy mimicking facioscapulohumeral muscular dystrophy
- Recurrent opportunistic infections in a HIV-negative patient with combined C6 and NFKB1 mutations: A case report, pedigree analysis, and literature review
- Letter to the Editor
- Letter to the Editor: Total parenteral nutrition-induced Wernicke’s encephalopathy after oncologic gastrointestinal surgery
- Erratum
- Erratum to “Bladder-embedded ectopic intrauterine device with calculus”
- Retraction
- Retraction of “XRCC1 and hOGG1 polymorphisms and endometrial carcinoma: A meta-analysis”
- Corrigendum
- Corrigendum to “Investigating hormesis, aging, and neurodegeneration: From bench to clinics”
- Corrigendum to “Frankincense: A neuronutrient to approach Parkinson’s disease treatment”
- Special Issue The evolving saga of RNAs from bench to bedside - Part II
- Machine-learning-based prediction of a diagnostic model using autophagy-related genes based on RNA sequencing for patients with papillary thyroid carcinoma
- Unlocking the future of hepatocellular carcinoma treatment: A comprehensive analysis of disulfidptosis-related lncRNAs for prognosis and drug screening
- Elevated mRNA level indicates FSIP1 promotes EMT and gastric cancer progression by regulating fibroblasts in tumor microenvironment
- Special Issue Advancements in oncology: bridging clinical and experimental research - Part I
- Ultrasound-guided transperineal vs transrectal prostate biopsy: A meta-analysis of diagnostic accuracy and complication rates
- Assessment of diagnostic value of unilateral systematic biopsy combined with targeted biopsy in detecting clinically significant prostate cancer
- SENP7 inhibits glioblastoma metastasis and invasion by dissociating SUMO2/3 binding to specific target proteins
- MARK1 suppress malignant progression of hepatocellular carcinoma and improves sorafenib resistance through negatively regulating POTEE
- Analysis of postoperative complications in bladder cancer patients
- Carboplatin combined with arsenic trioxide versus carboplatin combined with docetaxel treatment for LACC: A randomized, open-label, phase II clinical study
- Special Issue Exploring the biological mechanism of human diseases based on MultiOmics Technology - Part I
- Comprehensive pan-cancer investigation of carnosine dipeptidase 1 and its prospective prognostic significance in hepatocellular carcinoma
- Identification of signatures associated with microsatellite instability and immune characteristics to predict the prognostic risk of colon cancer
- Single-cell analysis identified key macrophage subpopulations associated with atherosclerosis
Artikel in diesem Heft
- Research Articles
- EDNRB inhibits the growth and migration of prostate cancer cells by activating the cGMP-PKG pathway
- STK11 (LKB1) mutation suppresses ferroptosis in lung adenocarcinoma by facilitating monounsaturated fatty acid synthesis
- Association of SOX6 gene polymorphisms with Kashin-Beck disease risk in the Chinese Han population
- The pyroptosis-related signature predicts prognosis and influences the tumor immune microenvironment in dedifferentiated liposarcoma
- METTL3 attenuates ferroptosis sensitivity in lung cancer via modulating TFRC
- Identification and validation of molecular subtypes and prognostic signature for stage I and stage II gastric cancer based on neutrophil extracellular traps
- Novel lumbar plexus block versus femoral nerve block for analgesia and motor recovery after total knee arthroplasty
- Correlation between ABCB1 and OLIG2 polymorphisms and the severity and prognosis of patients with cerebral infarction
- Study on the radiotherapy effect and serum neutral granulocyte lymphocyte ratio and inflammatory factor expression of nasopharyngeal carcinoma
- Transcriptome analysis of effects of Tecrl deficiency on cardiometabolic and calcium regulation in cardiac tissue
- Aflatoxin B1 induces infertility, fetal deformities, and potential therapies
- Serum levels of HMW adiponectin and its receptors are associated with cytokine levels and clinical characteristics in chronic obstructive pulmonary disease
- METTL3-mediated methylation of CYP2C19 mRNA may aggravate clopidogrel resistance in ischemic stroke patients
- Understand how machine learning impact lung cancer research from 2010 to 2021: A bibliometric analysis
- Pressure ulcers in German hospitals: Analysis of reimbursement and length of stay
- Metformin plus L-carnitine enhances brown/beige adipose tissue activity via Nrf2/HO-1 signaling to reduce lipid accumulation and inflammation in murine obesity
- Downregulation of carbonic anhydrase IX expression in mouse xenograft nasopharyngeal carcinoma model via doxorubicin nanobubble combined with ultrasound
- Feasibility of 3-dimensional printed models in simulated training and teaching of transcatheter aortic valve replacement
- miR-335-3p improves type II diabetes mellitus by IGF-1 regulating macrophage polarization
- The analyses of human MCPH1 DNA repair machinery and genetic variations
- Activation of Piezo1 increases the sensitivity of breast cancer to hyperthermia therapy
- Comprehensive analysis based on the disulfidptosis-related genes identifies hub genes and immune infiltration for pancreatic adenocarcinoma
- Changes of serum CA125 and PGE2 before and after high-intensity focused ultrasound combined with GnRH-a in treatment of patients with adenomyosis
- The clinical value of the hepatic venous pressure gradient in patients undergoing hepatic resection for hepatocellular carcinoma with or without liver cirrhosis
- Development and validation of a novel model to predict pulmonary embolism in cardiology suspected patients: A 10-year retrospective analysis
- Downregulation of lncRNA XLOC_032768 in diabetic patients predicts the occurrence of diabetic nephropathy
- Circ_0051428 targeting miR-885-3p/MMP2 axis enhances the malignancy of cervical cancer
- Effectiveness of ginkgo diterpene lactone meglumine on cognitive function in patients with acute ischemic stroke
- The construction of a novel prognostic prediction model for glioma based on GWAS-identified prognostic-related risk loci
- Evaluating the impact of childhood BMI on the risk of coronavirus disease 2019: A Mendelian randomization study
- Lactate dehydrogenase to albumin ratio is associated with in-hospital mortality in patients with acute heart failure: Data from the MIMIC-III database
- CD36-mediated podocyte lipotoxicity promotes foot process effacement
- Efficacy of etonogestrel subcutaneous implants versus the levonorgestrel-releasing intrauterine system in the conservative treatment of adenomyosis
- FLRT2 mediates chondrogenesis of nasal septal cartilage and mandibular condyle cartilage
- Challenges in treating primary immune thrombocytopenia patients undergoing COVID-19 vaccination: A retrospective study
- Let-7 family regulates HaCaT cell proliferation and apoptosis via the ΔNp63/PI3K/AKT pathway
- Phospholipid transfer protein ameliorates sepsis-induced cardiac dysfunction through NLRP3 inflammasome inhibition
- Postoperative cognitive dysfunction in elderly patients with colorectal cancer: A randomized controlled study comparing goal-directed and conventional fluid therapy
- Long-pulsed ultrasound-mediated microbubble thrombolysis in a rat model of microvascular obstruction
- High SEC61A1 expression predicts poor outcome of acute myeloid leukemia
- Comparison of polymerase chain reaction and next-generation sequencing with conventional urine culture for the diagnosis of urinary tract infections: A meta-analysis
- Secreted frizzled-related protein 5 protects against renal fibrosis by inhibiting Wnt/β-catenin pathway
- Pan-cancer and single-cell analysis of actin cytoskeleton genes related to disulfidptosis
- Overexpression of miR-532-5p restrains oxidative stress response of chondrocytes in nontraumatic osteonecrosis of the femoral head by inhibiting ABL1
- Autologous liver transplantation for unresectable hepatobiliary malignancies in enhanced recovery after surgery model
- Clinical analysis of incomplete rupture of the uterus secondary to previous cesarean section
- Abnormal sleep duration is associated with sarcopenia in older Chinese people: A large retrospective cross-sectional study
- No genetic causality between obesity and benign paroxysmal vertigo: A two-sample Mendelian randomization study
- Identification and validation of autophagy-related genes in SSc
- Long non-coding RNA SRA1 suppresses radiotherapy resistance in esophageal squamous cell carcinoma by modulating glycolytic reprogramming
- Evaluation of quality of life in patients with schizophrenia: An inpatient social welfare institution-based cross-sectional study
- The possible role of oxidative stress marker glutathione in the assessment of cognitive impairment in multiple sclerosis
- Compilation of a self-management assessment scale for postoperative patients with aortic dissection
- Left atrial appendage closure in conjunction with radiofrequency ablation: Effects on left atrial functioning in patients with paroxysmal atrial fibrillation
- Effect of anterior femoral cortical notch grade on postoperative function and complications during TKA surgery: A multicenter, retrospective study
- Clinical characteristics and assessment of risk factors in patients with influenza A-induced severe pneumonia after the prevalence of SARS-CoV-2
- Analgesia nociception index is an indicator of laparoscopic trocar insertion-induced transient nociceptive stimuli
- High STAT4 expression correlates with poor prognosis in acute myeloid leukemia and facilitates disease progression by upregulating VEGFA expression
- Factors influencing cardiovascular system-related post-COVID-19 sequelae: A single-center cohort study
- HOXD10 regulates intestinal permeability and inhibits inflammation of dextran sulfate sodium-induced ulcerative colitis through the inactivation of the Rho/ROCK/MMPs axis
- Mesenchymal stem cell-derived exosomal miR-26a induces ferroptosis, suppresses hepatic stellate cell activation, and ameliorates liver fibrosis by modulating SLC7A11
- Endovascular thrombectomy versus intravenous thrombolysis for primary distal, medium vessel occlusion in acute ischemic stroke
- ANO6 (TMEM16F) inhibits gastrointestinal stromal tumor growth and induces ferroptosis
- Prognostic value of EIF5A2 in solid tumors: A meta-analysis and bioinformatics analysis
- The role of enhanced expression of Cx43 in patients with ulcerative colitis
- Choosing a COVID-19 vaccination site might be driven by anxiety and body vigilance
- Role of ICAM-1 in triple-negative breast cancer
- Cost-effectiveness of ambroxol in the treatment of Gaucher disease type 2
- HLA-DRB5 promotes immune thrombocytopenia via activating CD8+ T cells
- Efficacy and factors of myofascial release therapy combined with electrical and magnetic stimulation in the treatment of chronic pelvic pain syndrome
- Efficacy of tacrolimus monotherapy in primary membranous nephropathy
- Mechanisms of Tripterygium wilfordii Hook F on treating rheumatoid arthritis explored by network pharmacology analysis and molecular docking
- FBXO45 levels regulated ferroptosis renal tubular epithelial cells in a model of diabetic nephropathy by PLK1
- Optimizing anesthesia strategies to NSCLC patients in VATS procedures: Insights from drug requirements and patient recovery patterns
- Alpha-lipoic acid upregulates the PPARγ/NRF2/GPX4 signal pathway to inhibit ferroptosis in the pathogenesis of unexplained recurrent pregnancy loss
- Correlation between fat-soluble vitamin levels and inflammatory factors in paediatric community-acquired pneumonia: A prospective study
- CD1d affects the proliferation, migration, and apoptosis of human papillary thyroid carcinoma TPC-1 cells via regulating MAPK/NF-κB signaling pathway
- miR-let-7a inhibits sympathetic nerve remodeling after myocardial infarction by downregulating the expression of nerve growth factor
- Immune response analysis of solid organ transplantation recipients inoculated with inactivated COVID-19 vaccine: A retrospective analysis
- The H2Valdien derivatives regulate the epithelial–mesenchymal transition of hepatoma carcinoma cells through the Hedgehog signaling pathway
- Clinical efficacy of dexamethasone combined with isoniazid in the treatment of tuberculous meningitis and its effect on peripheral blood T cell subsets
- Comparison of short-segment and long-segment fixation in treatment of degenerative scoliosis and analysis of factors associated with adjacent spondylolisthesis
- Lycopene inhibits pyroptosis of endothelial progenitor cells induced by ox-LDL through the AMPK/mTOR/NLRP3 pathway
- Methylation regulation for FUNDC1 stability in childhood leukemia was up-regulated and facilitates metastasis and reduces ferroptosis of leukemia through mitochondrial damage by FBXL2
- Correlation of single-fiber electromyography studies and functional status in patients with amyotrophic lateral sclerosis
- Risk factors of postoperative airway obstruction complications in children with oral floor mass
- Expression levels and clinical significance of serum miR-19a/CCL20 in patients with acute cerebral infarction
- Physical activity and mental health trends in Korean adolescents: Analyzing the impact of the COVID-19 pandemic from 2018 to 2022
- Evaluating anemia in HIV-infected patients using chest CT
- Ponticulus posticus and skeletal malocclusion: A pilot study in a Southern Italian pre-orthodontic court
- Causal association of circulating immune cells and lymphoma: A Mendelian randomization study
- Assessment of the renal function and fibrosis indexes of conventional western medicine with Chinese medicine for dredging collaterals on treating renal fibrosis: A systematic review and meta-analysis
- Comprehensive landscape of integrator complex subunits and their association with prognosis and tumor microenvironment in gastric cancer
- New target-HMGCR inhibitors for the treatment of primary sclerosing cholangitis: A drug Mendelian randomization study
- Population pharmacokinetics of meropenem in critically ill patients
- Comparison of the ability of newly inflammatory markers to predict complicated appendicitis
- Comparative morphology of the cruciate ligaments: A radiological study
- Immune landscape of hepatocellular carcinoma: The central role of TP53-inducible glycolysis and apoptosis regulator
- Serum SIRT3 levels in epilepsy patients and its association with clinical outcomes and severity: A prospective observational study
- SHP-1 mediates cigarette smoke extract-induced epithelial–mesenchymal transformation and inflammation in 16HBE cells
- Acute hyper-hypoxia accelerates the development of depression in mice via the IL-6/PGC1α/MFN2 signaling pathway
- The GJB3 correlates with the prognosis, immune cell infiltration, and therapeutic responses in lung adenocarcinoma
- Physical fitness and blood parameters outcomes of breast cancer survivor in a low-intensity circuit resistance exercise program
- Exploring anesthetic-induced gene expression changes and immune cell dynamics in atrial tissue post-coronary artery bypass graft surgery
- Empagliflozin improves aortic injury in obese mice by regulating fatty acid metabolism
- Analysis of the risk factors of the radiation-induced encephalopathy in nasopharyngeal carcinoma: A retrospective cohort study
- Reproductive outcomes in women with BRCA 1/2 germline mutations: A retrospective observational study and literature review
- Evaluation of upper airway ultrasonographic measurements in predicting difficult intubation: A cross-section of the Turkish population
- Prognostic and diagnostic value of circulating IGFBP2 in pancreatic cancer
- Postural stability after operative reconstruction of the AFTL in chronic ankle instability comparing three different surgical techniques
- Research trends related to emergence agitation in the post-anaesthesia care unit from 2001 to 2023: A bibliometric analysis
- Frequency and clinicopathological correlation of gastrointestinal polyps: A six-year single center experience
- ACSL4 mediates inflammatory bowel disease and contributes to LPS-induced intestinal epithelial cell dysfunction by activating ferroptosis and inflammation
- Affibody-based molecular probe 99mTc-(HE)3ZHER2:V2 for non-invasive HER2 detection in ovarian and breast cancer xenografts
- Effectiveness of nutritional support for clinical outcomes in gastric cancer patients: A meta-analysis of randomized controlled trials
- The relationship between IFN-γ, IL-10, IL-6 cytokines, and severity of the condition with serum zinc and Fe in children infected with Mycoplasma pneumoniae
- Paraquat disrupts the blood–brain barrier by increasing IL-6 expression and oxidative stress through the activation of PI3K/AKT signaling pathway
- Sleep quality associate with the increased prevalence of cognitive impairment in coronary artery disease patients: A retrospective case–control study
- Dioscin protects against chronic prostatitis through the TLR4/NF-κB pathway
- Association of polymorphisms in FBN1, MYH11, and TGF-β signaling-related genes with susceptibility of sporadic thoracic aortic aneurysm and dissection in the Zhejiang Han population
- Application value of multi-parameter magnetic resonance image-transrectal ultrasound cognitive fusion in prostate biopsy
- Laboratory variables‐based artificial neural network models for predicting fatty liver disease: A retrospective study
- Decreased BIRC5-206 promotes epithelial–mesenchymal transition in nasopharyngeal carcinoma through sponging miR-145-5p
- Sepsis induces the cardiomyocyte apoptosis and cardiac dysfunction through activation of YAP1/Serpine1/caspase-3 pathway
- Assessment of iron metabolism and iron deficiency in incident patients on incident continuous ambulatory peritoneal dialysis
- Tibial periosteum flap combined with autologous bone grafting in the treatment of Gustilo-IIIB/IIIC open tibial fractures
- The application of intravenous general anesthesia under nasopharyngeal airway assisted ventilation undergoing ureteroscopic holmium laser lithotripsy: A prospective, single-center, controlled trial
- Long intergenic noncoding RNA for IGF2BP2 stability suppresses gastric cancer cell apoptosis by inhibiting the maturation of microRNA-34a
- Role of FOXM1 and AURKB in regulating keratinocyte function in psoriasis
- Parental control attitudes over their pre-school children’s diet
- The role of auto-HSCT in extranodal natural killer/T cell lymphoma
- Significance of negative cervical cytology and positive HPV in the diagnosis of cervical lesions by colposcopy
- Echinacoside inhibits PASMCs calcium overload to prevent hypoxic pulmonary artery remodeling by regulating TRPC1/4/6 and calmodulin
- ADAR1 plays a protective role in proximal tubular cells under high glucose conditions by attenuating the PI3K/AKT/mTOR signaling pathway
- The risk of cancer among insulin glargine users in Lithuania: A retrospective population-based study
- The unusual location of primary hydatid cyst: A case series study
- Intraoperative changes in electrophysiological monitoring can be used to predict clinical outcomes in patients with spinal cavernous malformation
- Obesity and risk of placenta accreta spectrum: A meta-analysis
- Shikonin alleviates asthma phenotypes in mice via an airway epithelial STAT3-dependent mechanism
- NSUN6 and HTR7 disturbed the stability of carotid atherosclerotic plaques by regulating the immune responses of macrophages
- The effect of COVID-19 lockdown on admission rates in Maternity Hospital
- Temporal muscle thickness is not a prognostic predictor in patients with high-grade glioma, an experience at two centers in China
- Luteolin alleviates cerebral ischemia/reperfusion injury by regulating cell pyroptosis
- Therapeutic role of respiratory exercise in patients with tuberculous pleurisy
- Effects of CFTR-ENaC on spinal cord edema after spinal cord injury
- Irisin-regulated lncRNAs and their potential regulatory functions in chondrogenic differentiation of human mesenchymal stem cells
- DMD mutations in pediatric patients with phenotypes of Duchenne/Becker muscular dystrophy
- Combination of C-reactive protein and fibrinogen-to-albumin ratio as a novel predictor of all-cause mortality in heart failure patients
- Significant role and the underly mechanism of cullin-1 in chronic obstructive pulmonary disease
- Ferroptosis-related prognostic model of mantle cell lymphoma
- Observation of choking reaction and other related indexes in elderly painless fiberoptic bronchoscopy with transnasal high-flow humidification oxygen therapy
- A bibliometric analysis of Prader-Willi syndrome from 2002 to 2022
- The causal effects of childhood sunburn occasions on melanoma: A univariable and multivariable Mendelian randomization study
- Oxidative stress regulates glycogen synthase kinase-3 in lymphocytes of diabetes mellitus patients complicated with cerebral infarction
- Role of COX6C and NDUFB3 in septic shock and stroke
- Trends in disease burden of type 2 diabetes, stroke, and hypertensive heart disease attributable to high BMI in China: 1990–2019
- Purinergic P2X7 receptor mediates hyperoxia-induced injury in pulmonary microvascular endothelial cells via NLRP3-mediated pyroptotic pathway
- Investigating the role of oviductal mucosa–endometrial co-culture in modulating factors relevant to embryo implantation
- Analgesic effect of external oblique intercostal block in laparoscopic cholecystectomy: A retrospective study
- Elevated serum miR-142-5p correlates with ischemic lesions and both NSE and S100β in ischemic stroke patients
- Correlation between the mechanism of arteriopathy in IgA nephropathy and blood stasis syndrome: A cohort study
- Risk factors for progressive kyphosis after percutaneous kyphoplasty in osteoporotic vertebral compression fracture
- Predictive role of neuron-specific enolase and S100-β in early neurological deterioration and unfavorable prognosis in patients with ischemic stroke
- The potential risk factors of postoperative cognitive dysfunction for endovascular therapy in acute ischemic stroke with general anesthesia
- Fluoxetine inhibited RANKL-induced osteoclastic differentiation in vitro
- Detection of serum FOXM1 and IGF2 in patients with ARDS and their correlation with disease and prognosis
- Rhein promotes skin wound healing by activating the PI3K/AKT signaling pathway
- Differences in mortality risk by levels of physical activity among persons with disabilities in South Korea
- Review Articles
- Cutaneous signs of selected cardiovascular disorders: A narrative review
- XRCC1 and hOGG1 polymorphisms and endometrial carcinoma: A meta-analysis
- A narrative review on adverse drug reactions of COVID-19 treatments on the kidney
- Emerging role and function of SPDL1 in human health and diseases
- Adverse reactions of piperacillin: A literature review of case reports
- Molecular mechanism and intervention measures of microvascular complications in diabetes
- Regulation of mesenchymal stem cell differentiation by autophagy
- Molecular landscape of borderline ovarian tumours: A systematic review
- Advances in synthetic lethality modalities for glioblastoma multiforme
- Investigating hormesis, aging, and neurodegeneration: From bench to clinics
- Frankincense: A neuronutrient to approach Parkinson’s disease treatment
- Sox9: A potential regulator of cancer stem cells in osteosarcoma
- Early detection of cardiovascular risk markers through non-invasive ultrasound methodologies in periodontitis patients
- Advanced neuroimaging and criminal interrogation in lie detection
- Maternal factors for neural tube defects in offspring: An umbrella review
- The chemoprotective hormetic effects of rosmarinic acid
- CBD’s potential impact on Parkinson’s disease: An updated overview
- Progress in cytokine research for ARDS: A comprehensive review
- Utilizing reactive oxygen species-scavenging nanoparticles for targeting oxidative stress in the treatment of ischemic stroke: A review
- NRXN1-related disorders, attempt to better define clinical assessment
- Lidocaine infusion for the treatment of complex regional pain syndrome: Case series and literature review
- Trends and future directions of autophagy in osteosarcoma: A bibliometric analysis
- Iron in ventricular remodeling and aneurysms post-myocardial infarction
- Case Reports
- Sirolimus potentiated angioedema: A case report and review of the literature
- Identification of mixed anaerobic infections after inguinal hernia repair based on metagenomic next-generation sequencing: A case report
- Successful treatment with bortezomib in combination with dexamethasone in a middle-aged male with idiopathic multicentric Castleman’s disease: A case report
- Complete heart block associated with hepatitis A infection in a female child with fatal outcome
- Elevation of D-dimer in eosinophilic gastrointestinal diseases in the absence of venous thrombosis: A case series and literature review
- Four years of natural progressive course: A rare case report of juvenile Xp11.2 translocations renal cell carcinoma with TFE3 gene fusion
- Advancing prenatal diagnosis: Echocardiographic detection of Scimitar syndrome in China – A case series
- Outcomes and complications of hemodialysis in patients with renal cancer following bilateral nephrectomy
- Anti-HMGCR myopathy mimicking facioscapulohumeral muscular dystrophy
- Recurrent opportunistic infections in a HIV-negative patient with combined C6 and NFKB1 mutations: A case report, pedigree analysis, and literature review
- Letter to the Editor
- Letter to the Editor: Total parenteral nutrition-induced Wernicke’s encephalopathy after oncologic gastrointestinal surgery
- Erratum
- Erratum to “Bladder-embedded ectopic intrauterine device with calculus”
- Retraction
- Retraction of “XRCC1 and hOGG1 polymorphisms and endometrial carcinoma: A meta-analysis”
- Corrigendum
- Corrigendum to “Investigating hormesis, aging, and neurodegeneration: From bench to clinics”
- Corrigendum to “Frankincense: A neuronutrient to approach Parkinson’s disease treatment”
- Special Issue The evolving saga of RNAs from bench to bedside - Part II
- Machine-learning-based prediction of a diagnostic model using autophagy-related genes based on RNA sequencing for patients with papillary thyroid carcinoma
- Unlocking the future of hepatocellular carcinoma treatment: A comprehensive analysis of disulfidptosis-related lncRNAs for prognosis and drug screening
- Elevated mRNA level indicates FSIP1 promotes EMT and gastric cancer progression by regulating fibroblasts in tumor microenvironment
- Special Issue Advancements in oncology: bridging clinical and experimental research - Part I
- Ultrasound-guided transperineal vs transrectal prostate biopsy: A meta-analysis of diagnostic accuracy and complication rates
- Assessment of diagnostic value of unilateral systematic biopsy combined with targeted biopsy in detecting clinically significant prostate cancer
- SENP7 inhibits glioblastoma metastasis and invasion by dissociating SUMO2/3 binding to specific target proteins
- MARK1 suppress malignant progression of hepatocellular carcinoma and improves sorafenib resistance through negatively regulating POTEE
- Analysis of postoperative complications in bladder cancer patients
- Carboplatin combined with arsenic trioxide versus carboplatin combined with docetaxel treatment for LACC: A randomized, open-label, phase II clinical study
- Special Issue Exploring the biological mechanism of human diseases based on MultiOmics Technology - Part I
- Comprehensive pan-cancer investigation of carnosine dipeptidase 1 and its prospective prognostic significance in hepatocellular carcinoma
- Identification of signatures associated with microsatellite instability and immune characteristics to predict the prognostic risk of colon cancer
- Single-cell analysis identified key macrophage subpopulations associated with atherosclerosis

