Atherogenic index of plasma and coronary artery disease: A systematic review
-
Juan R. Ulloque-Badaracco
, Percy Herrera-Añazco
Abstract
Various studies suggest that the atherogenic index of plasma (AIP) is associated with the risk of coronary artery disease (CAD) in different clinical scenarios. This review aimed to synthesize evidence of the association between AIP values and CAD. A literature search was carried out on four databases, namely, PubMed, Scopus, Web of Science, and Ovid-Medline. A handsearch was performed on preprint repositories (MedRxiv and Research Square). The effect measurements were expressed as odds ratios (OR) with their corresponding 95% confidence intervals (CI). For the quantitative synthesis, we employed a random-effects model. We analyzed 14 articles (with 40,902 participants) from seven different countries. The quantitative analysis revealed that an increase in one unit of AIP was associated with higher odds of developing CAD (OR 2.11; 95% CI 1.65–2.69; P < 0.001; I 2 = 98%). We conducted subgroup analyses of Chinese (OR 1.89; 95% CI 1.40–2.56; P < 0.001) and non-Chinese studies (OR 2.51; 95% CI 1.42–4.42; P < 0.001). The sensitivity analysis by risk of bias continued to demonstrate an association, and the heterogeneity remained unchanged (OR 1.75; 95% CI 1.33–2.31; P < 0.001; I 2 = 98%). Higher AIP values were associated with higher odds of developing CAD.
1 Introduction
Coronary artery disease (CAD), also referred to as coronary heart disease (CHD) or ischemic heart disease, is a disease with a high prevalence and is one of the leading causes of death worldwide [1,2,3]. In the last few decades, as preventive and treatment measures have strengthened and improved, the incidence and mortality of this pathology have decreased in developed countries [4,5,6,7]. However, the global prevalence is expected to increase to 1,845 cases per 100,000 population by 2030 [1].
Cardiac risk stratification is necessary to improve preventive and therapeutic interventions [8]. Biomarkers are an essential component in this task, either as part of prediction models or on their own. In recent years, multiple CAD risk biomarkers have been identified and investigated, including C-reactive protein [9], lipoprotein-associated phospholipase A2 [10], and fibrinogen [11], among others. The atherogenic index of plasma (AIP) is a novel biomarker consisting of the logarithmically transformed ratio of triglycerides to high-density lipoprotein (HDL)-cholesterol in molar concentrations. Unlike biomarkers such as serum amyloid alpha [12] or matrix metalloproteinases [13], AIP is an easily accessible biomarker because only a standard lipid profile is required for its calculation [14].
Hypertriglyceridemia and low HDL levels are independent markers of CHD [15,16]. Therefore, the AIP combines these two lipid parameters into a single biomarker to boost its predictive capabilities.
Thus, several studies have suggested that AIP acts as a marker associated with cardiovascular diseases in patients with various pathologies [17,18,19,20,21,22]. This association is related to a surrogate involvement of endothelial vascular damage, such as carotid intima-media thickening, compromised atrial coronary anatomical, or clinical conditions, e.g., stroke and acute coronary syndromes, as a manifestation of CAD. However, to the best of our knowledge, the evidence of the association between AIP and CAD has not been systematized. Thus, this review aimed to synthesize such evidence.
2 Methods
2.1 Study design, registration, and report guideline
We conducted this systematic review in accordance with the guidelines of the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) statement [23]. The summarized version of the protocol was registered in the International Prospective Register of Systematic Reviews with code CRD42021289308 (see PRISMA checklist in Table S1).
2.2 Data sources and searches
We conducted a literature search on articles that evaluated the association between AIP and CAD on October 15, 2021. Four databases were searched: PubMed, Scopus, Web of Science, and Ovid-Medline. A handsearch was also performed on preprint repositories (MedRxiv and Research Square) (see Supplementary Appendix 1).
2.3 Study selection and data extraction
The articles collected from the aforementioned databases were exported to the Rayyan data management software [24], and duplicate studies were eliminated. Four reviewers independently screened each study (A.C.-A., E.A.A.-B., E.A.H.-B., and J.R.U.-B.) by analyzing the titles and abstracts according to the selection criteria. We included (1) case–control and cohort studies that (2) evaluated the association between AIP and CAD in (3) adults (≥18 years old). We excluded articles that were (1) case reports, (2) studies conducted on animals, (3) scoping reviews, (4) narrative reviews, and (5) systematic reviews.
Once this phase was completed, each of the articles was read in full-text, and we determined whether they met the previously established selection criteria. A study was excluded if it failed to comply with the selection criteria. If an article did not contain the required information, an attempt was made to contact the corresponding author of the said article. A secondary bibliographic search was conducted on the articles that reached the full-text review phase.
In case of disagreements on the inclusion or exclusion of an article, a third reviewer was consulted. Finally, information of the selected articles was extracted and collated in a standardized Excel 2016 document. The extracted data included author name, country, year of publication, study sample, study design, population characteristics (age, gender, etc.), exposure (AIP mean or median of the whole sample and according to sample stratification), and crude/adjusted association measures (odds ratio [OR], relative risk [RR], and hazard ratio). Outcome definitions are presented in Table S2.
2.4 Assessment of study quality and publication bias
Four authors (A.C.-A., V.A.V.-C., M.D.M.-R., and F.E.S.-V.) evaluated the included studies independently using the Newcastle–Ottawa Scale [24]. The studies were stratified into three levels of methodological quality according to the number of stars: low risk of bias (≥6 stars), moderate risk of bias (4–5 stars), and high risk of bias (<4 stars). In addition, funnel plots and Begg’s test were conducted to assess publication bias; P-values > 0.1 were considered indicative of no publication bias.
2.5 Data synthesis and analysis
The quantitative analysis was conducted using the RevMan 5.4 statistical program (Cochrane Collaboration, Copenhagen, Denmark). The OR and their corresponding 95% confidence intervals (CI) were the only effect measures used; thus, we transformed standardized mean differences to ln[OR] using the Chinn method. RR was converted into OR [25,26]. Variables expressed as median and interquartile range were converted to means and standard deviation using Hozo’s method [27]. We assessed statistical heterogeneity by calculating the I 2-statistic, where values >60% were considered to indicate severe heterogeneity. A Cochran’s Q test was also conducted, where a P-value < 0.05 was considered statistically significant. A random-effects model was used for the meta-analysis as we anticipated heterogeneity among studies. In the subgroup analysis, we conducted a comparison between associations according to country (Chinese vs non-Chinese studies), study design, CAD definition, and gender (women vs mixed). In the sensitivity analysis, we excluded studies with a high risk of bias. We also analyzed all studies after transforming OR to RR. In addition, we performed a meta-regression, reported as bubble plots, in order to search for heterogeneity sources, due to differences in the clinical and methodological characteristics of the individual studies. Assessed variables were study design, study location, CAD definition, and gender.
3 Results
3.1 Study selection
The search strategy yielded 975 records. After removing 610 duplicates, 365 articles finally remained. After evaluating the titles and abstracts, we excluded 322 more studies. Then, a full-text review was performed on the remaining 43 articles, which led to the exclusion of 29 more articles. In the end, 14 articles were included in the qualitative analysis and meta-analysis [20,28,29,30,31,32,33,34,35,36,37,38,39,40]. This process is documented in a PRISMA flow diagram (Figure 1).
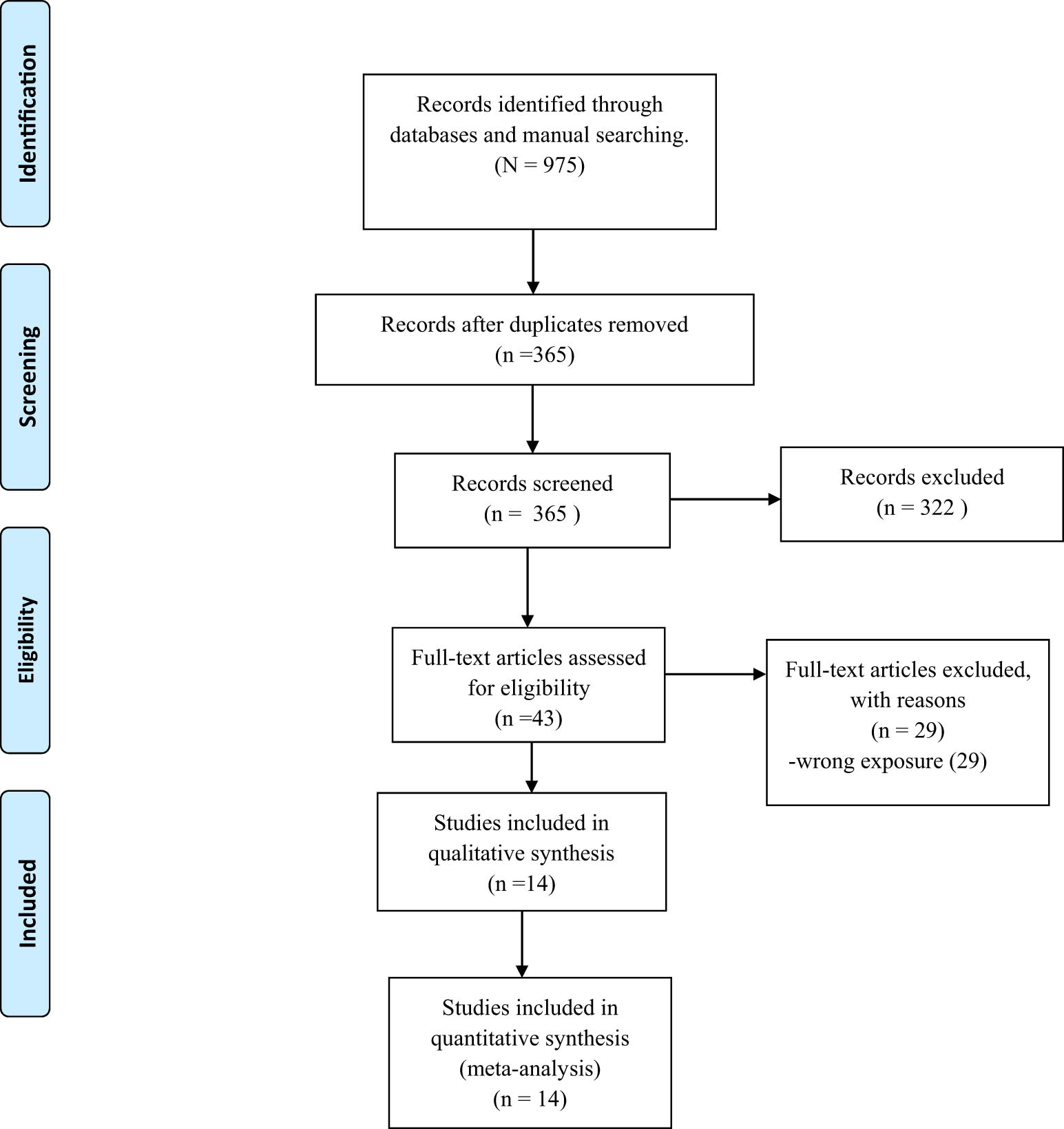
PRISMA flow diagram.
3.2 Study characteristics
The characteristics of each study are presented in detail in Table 1. Most of the articles (8 out of 14) were case–control studies, and six were cohort studies. The distribution of the studies by country was as follows: China (7), India (1), Turkey (2), Egypt (1), South Korea (1), Slovakia (1), and the USA (1). In total, there were 40,902 participants with samples ranging from 80 to 11,164 participants. The gender distribution was as follows: 17,026 were male, and 23,876 were female. The study by Celik et al. reported an optimal cutoff value of AIP for CAD of 0.541 and an area under the curve of 0.617 [30].
Clinical characteristics of the included studies
| Author | Year | Country | Participants (male/female) | Median/mean age (Interquartile range\standard deviation (SD)) | Study design | AIP mean (SD) in CAD patients | AIP mean (SD) in non-CAD patients | SMD between CAD and non-CAD patients | OR (95% CI), P-value (crude) | OR (95% CI), P-value (adjusted) |
|---|---|---|---|---|---|---|---|---|---|---|
| Onat et al. | 2010 | Turkey | 2,676 (1,294/1,392) | 49 (13) | Cohort | NR | NR | NR | NR | 1.34 (1.11–1.61), P < 0.001a |
| Raj-Sedhai et al. | 2018 | USA | 313 (169/144) | 63 (12) | Cohort | 0.39 (0.03) | 0.35 (0.02) | 1.51 [1.25, 1.76] | NR | NR |
| Al-Shaer et al. | 2021 | Egypt | 140 (NR/NR) | NR | Case–control | 0.20 (0.27) | 0.1 (0.27) | 0.37 [0.03, 0.70] | NR | NR |
| Celik et al. | 2019 | Turkey | 280 (154/126) | 64 (10) | Case–control | 0.62 (0.30) | 0.48 (0.28) | 0.48 [0.24, 0.72] | NR | NR |
| Wang et al. | 2021 | China | 3,600 (2,243/1,357) | 60 (10) | Cohort | NR | NR | NR | 2.6 (2.381–2.8348), P < 0.001 | NR |
| Won et al. | 2020 | South Korea | 6,928 (3,977/2,951) | 52 (10) | Cohort | NR | NR | NR | 1.1 (1.07–1.13), P < 0.001 | NR |
| Guo et al. | 2020 | China | 4,644 (0/4,644) | 64 (8) | Case–control | 0.15 (0.28) | 0.10 (0.28) | 0.18 [0.12, 0.24] | NR | NR |
| Wu et al. | 2018 | China | 696 (0/696) | 61 (7) | Case–control | 0.20 (0.27) | 0.10 (0.27) | 0.37 [0.03, 0.70] | NR | NR |
| Cai et al. | 2017 | China | 5,387 (3,242/2,145) | 62 (9) | Case–control | 0.17 (0.30) | 0.12 (0.31) | 0.16 [0.11, 0.22] | NR | NR |
| Pridavkova et al. | 2015 | Slovakia | 80 (43/37) | NR | Cohort | 0.22 (0.29) | 0.17 (0.34) | 0.16 [−0.29, 0.61] | NR | NR |
| Shanker et al. | 2016 | India | 11,164 (7,379/3,515) | 53 (8) | Cohort | NR | NR | NR | 1.80 (1.54–2.1), P < 0.001 | NR |
| Dai et al. | 2012 | China | 238 (0/238) | 65 (7) | Case–control | 0.61 (0.14) | 0.53 (0.09) | 0.67 [0.41, 0.93] | NR | NR |
| Zhou et al. | 2021 | China | 3,278 (2,473/805) | 59 (10) | Case–control | 0.37 (0.23) | 0.25 (0.26) | 0.50 [0.42, 0.57] | NR | NR |
| Gaojun et al. | 2019 | China | 1,478 (1,373/1,05) | 33 (30–35) | Case–control | 0.35 (0.30) | 0.21 (0.33) | 0.45 [0.34, 0.57] | NR | NR |
a: Adjusted to age and serum C-reactive protein. NR: Not reported.
3.3 Assessment of study quality and publication bias
Table S3 presents the results of the methodological quality assessment. In summary, 10 and 4 studies were classified as having a low and moderate risk of bias, respectively.
3.4 AIP and risk of CAD
The quantitative analysis revealed that patients with higher AIP values were associated with higher odds of developing CAD (OR 2.11; 95% CI 1.65–2.69; P < 0.001) (Figure 2a) with severe heterogeneity (I 2 = 98%). Statistically significant associations with high heterogeneity were observed in all subgroup analyses by study location (Figure 2b), study design (Figure 2c), definition of CAD (Figure 2d), and gender (Figure 2e). Sensitivity analyses were conducted. In one analysis, only studies with a low risk of bias (Figure 2f) were included (OR 1.75; CI 95% 1.33–2.31; P < 0.001; I 2 = 98%), whereas in the other, all OR values were transformed to RR (RR 1.29; CI 95% 1.17–1.42; P < 0.001; I 2 = 99%); however, the association with high heterogeneity remained in both cases (Figure 2g).
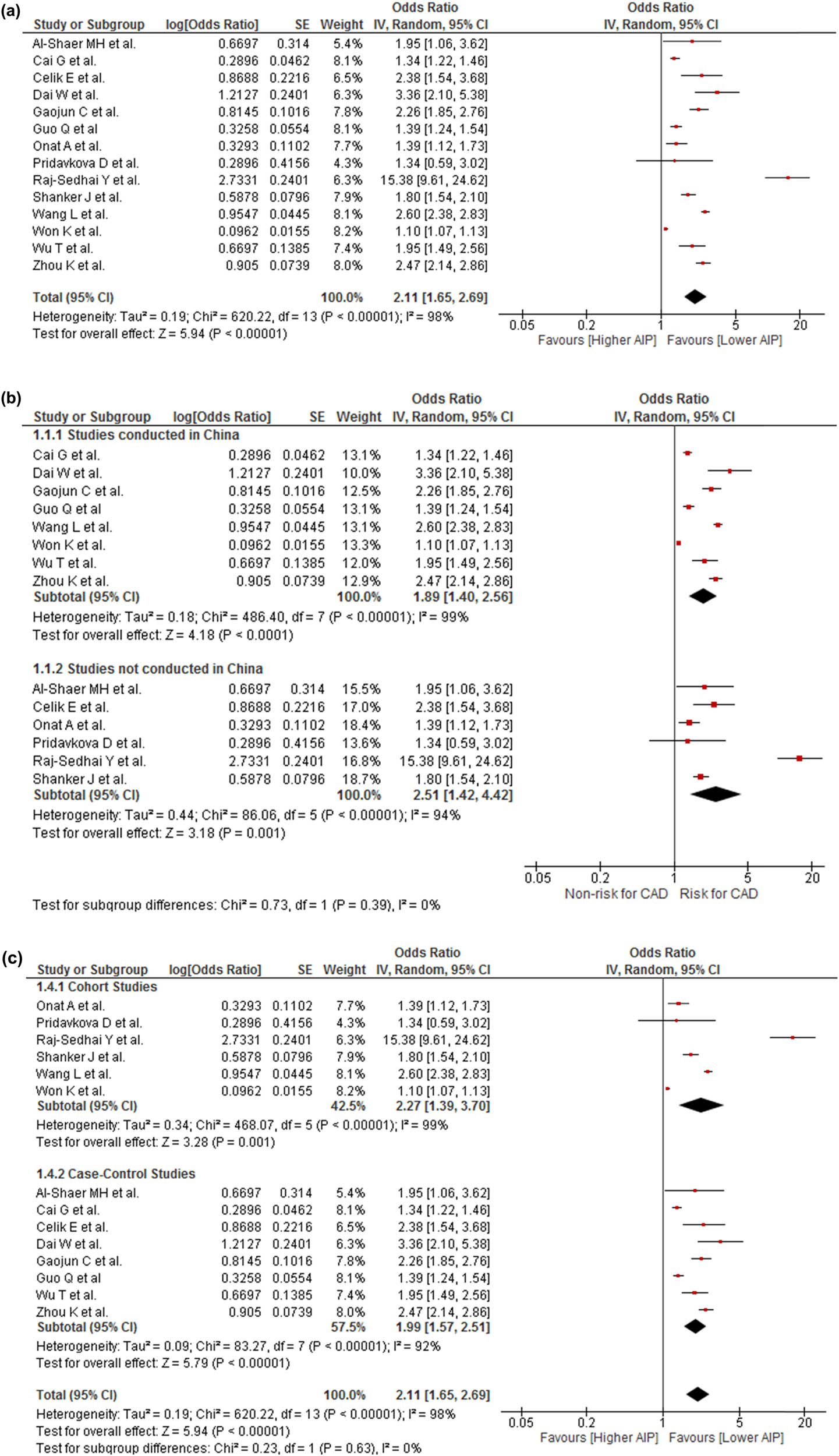
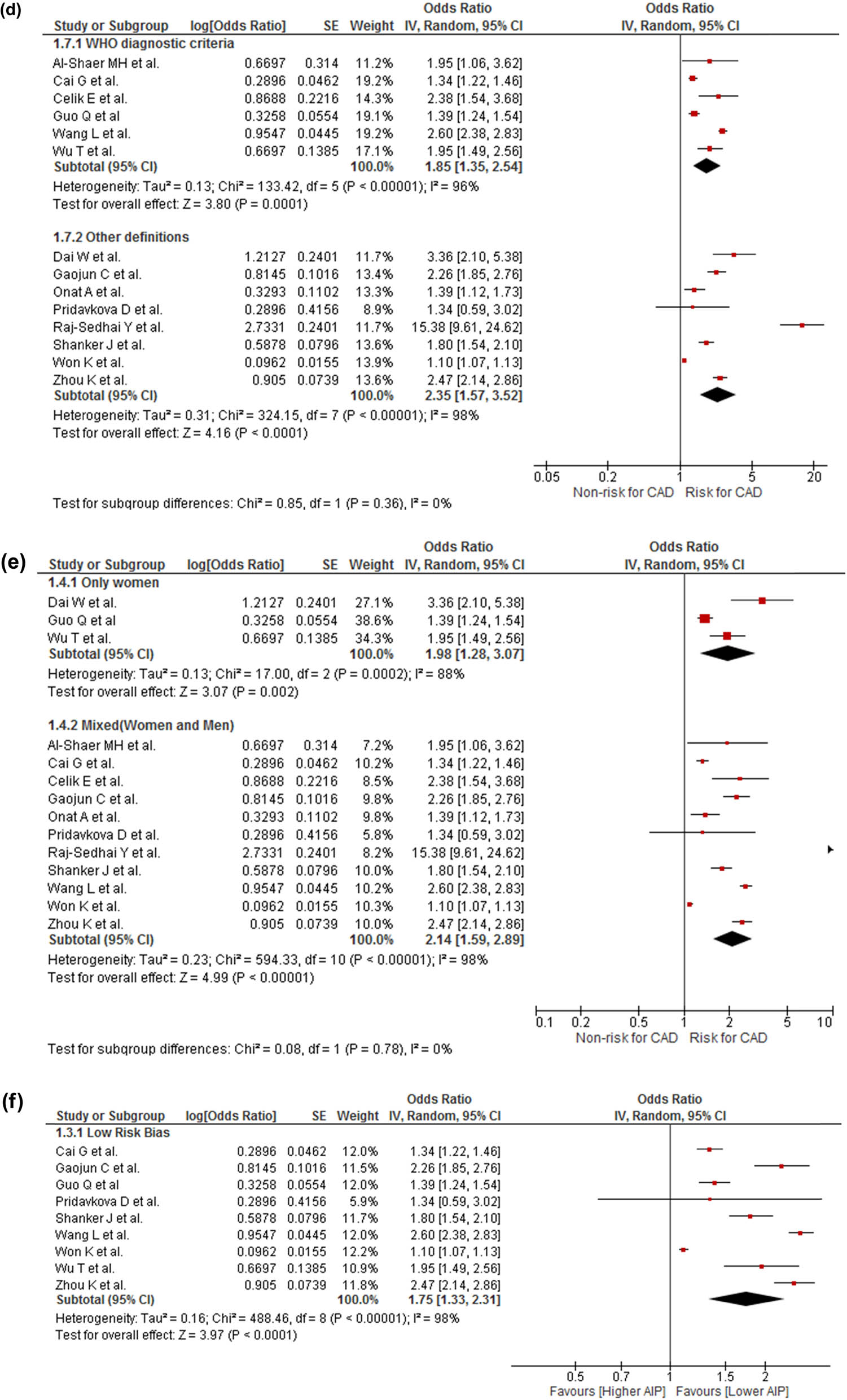
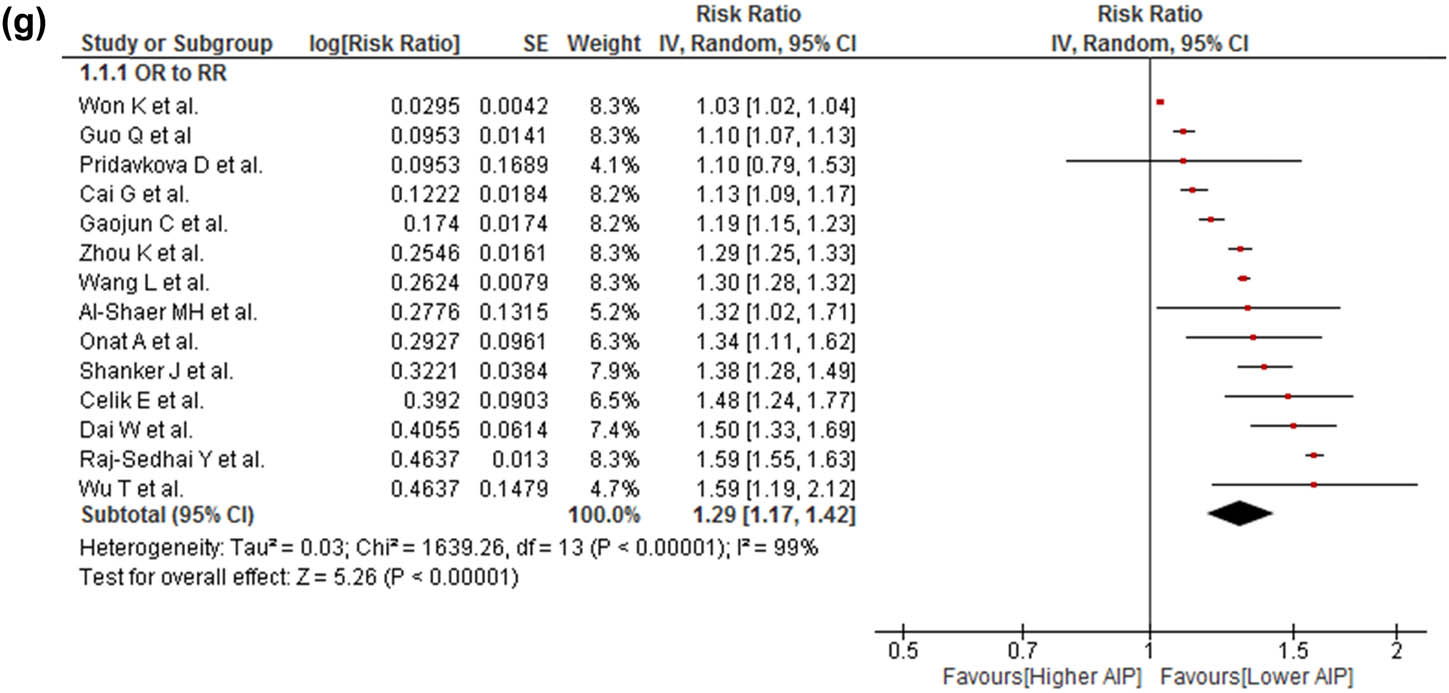
(a) Association of AIP and risk for CAD. (b) Subgroup analysis according to the origin country of the association between AIP and risk for CAD. (c) Subgroup analysis according to the study design of the association between AIP and risk for CAD. (d) Subgroup analysis according to CAD definition of the association between AIP and risk for CAD. (e) Subgroup analysis according to the gender of the association between AIP and risk for CAD. (f) Sensitivity analysis according to the risk of bias of the association between AIP and risk for CAD. (g) Sensitivity analysis according to the transformation from OR to RR.
3.5 Meta-regression
No significantly associated coefficient was observed in study location (P = 0.974) (Figure S1), study design (P = 0.959) (Figure S2), CAD definition (P = 0.614) (Figure S3), or gender (P = 0.958) (Figure S4).
3.6 Publication bias
There was no indication of small-study effects (Begg’s test, P = 0.956), and the funnel plots did not show asymmetry (Figure S5).
4 Discussion
From our systematic review and meta-analysis, we obtained sufficient evidence to consider AIP as a marker of CAD risk in the general population.
Multiple studies suggested the value of AIP as a predictor of fatty liver [41], hidradenitis suppurativa [42], osteomyelitis in patients with diabetic foot [43], obesity [44], diabetes [45], and an estimate-reduced glomerular filtration rate [46]. These associations are related to oxitdative stress [47], insulin resistance and hyperinsulinemia [45], and mechanisms associated with atherosclerosis [43,44], which are common risk factors for cardiovascular disease.
AIP is positively correlated with the fractional esterification rate of HDL, especially with small dense low-density lipoprotein (sdLDL), whose expression in AIP reflects the complex interactions of lipoprotein metabolism and is useful in predicting plasma atherogenicity [48]. sdLDL has atherogenic properties, such as reduced clearance from the bloodstream, enhanced oxidation compared with other lipoproteins, enhanced binding to endothelial proteoglycans, enhanced penetration across the endothelial barrier, and increased uptake by macrophage receptors [49]. These properties increase the formation of foam cells and are the initial stages of atherogenesis [50]. These factors could explain the results of different studies indicating an association between AIP and CAD [51,52,53], which varies depending on the value of this marker. In this way, Dobiásová suggested that AIP values between −0.3 and 0.1 were associated with low cardiovascular risk and AIP values from 0.1 to more than 0.24 were associated with high cardiovascular risk [14].
For the aforementioned reasons, our finding of an association between high AIP values and increased CAD risk is not surprising. In addition to the aforementioned factors, factors associated with specific CAD conditions could also explain our results. In this context, some studies have found an association between AIP and arterial stiffness in normotensive patients [54], which is a risk factor for CAD [55]. Choudhary et al., in a study conducted on subjects without antihypertensive or lipid-lowering therapy, found that AIP was related to pulse wave velocity but not to aortic or radial blood pressure, cardiac output, or systemic vascular resistance [54] Similarly, other studies associated AIP with the progression of coronary calcification, a known surrogate marker of CAD [56]. Two studies from Korea found a significant correlation between AIP and coronary calcification progression in subjects without cardiovascular disease [57], although AIP was not an independent predictor [57].
Contrarily, in a multinational study in seven countries from 2003 to 2015, this association was independent of traditional risk factors [58]. Similarly, AIP was also a predictor of subclinical CAD. A study of patients with or without chronic kidney disease found that AIP was associated with advanced subclinical CAD after adjustment for age older than 60 years, male sex, hypertension, diabetes mellitus, dyslipidemia, obesity, and proteinuria [59].
Finally, some studies demonstrated an association between AIP and the evolution of patients with acute coronary syndromes and myocardial infarction. For example, a Turkish study found that AIP was independently associated with the absence of reflow in patients with ST-elevated myocardial infarction following the primary percutaneous coronary intervention [52]. Surprisingly, a study in Jakarta found that patients hospitalized following myocardial infarction with AIP values <0.24 had almost four times higher mortality than those who did not have [60]. Although the authors did not find an explanation for their results, they suggested the role of the patients’ diet as a possible reason.
The meta-analysis conducted by Wu et al. [61] found that high AIP values are associated with an increased risk of AIP; however, this meta-analysis has many inconsistencies, such as the incorrect grouping of values in the overall meta-analysis, as they placed AIP values according to gender, which should have been done in a subgroup analysis according to the participants’ gender. Another error in this manuscript is the lack of explanation of how the AIP values were obtained for the subgroup analysis according to the patients’ health status because there is no such information in the primary studies they used.
Despite the evidence suggesting an association between AIP and CAD, this is a systematic review and meta-analysis that systematize the available evidence. We also conducted sensitivity analyses considering the biases of the studies and the place of origin of the studies, which provided robustness to our results. The findings obtained allow us to suggest the use of AIP as a potential low-cost marker of CAD that will allow health personnel to prioritize management strategies and could even be used as part of predictive scores, replacing markers such as triglycerides. Similarly, the usefulness of this marker is independent of the age of the patients [39,62], although, concerning gender, some studies suggested that, at least in young patients, its predictive value is mainly in males [39], which should be verified in subsequent studies. However, despite the fact that AIP is a marker that is calculated using parameters that are easy to obtain in clinical practice and that our results indicate its usefulness, the studies included in our systematic review are flawed and have small sample sizes. In this sense, despite being promising, more studies with better design are needed before adopting it in usual clinical practice.
Our systematic review has some limitations that must be acknowledged. First, there is evidence of high statistical heterogeneity due to the clinical and methodological differences between the analyzed studies. Second, most studies have not controlled the AIP values for confounding variables that impact the proposed outcome. Sociodemographic lifestyles and comorbidity variables should be considered in future studies to avoid confounding bias. Despite this, the direction of the effect is consistent in most of the reported studies. Third, most studies were conducted in Asia, with few or no studies found in other continents. Therefore, it is important to analyze the AIP value in CAD risk in these populations to establish its usefulness. Fourth, no definitive cutoff points have been reported to set the sensitivity and specificity of the AIP in CAD; thus, it is necessary to address it in future research in various contexts and populations. Finally, our findings indicate that high AIP values are associated with a greater possibility of suffering from CAD; however, with the obtained evidence, we consider that AIP is a risk marker and not a causal risk factor because the causes of lipid alterations are mediated by genetic and environmental factors. The AIP in altered ranges would be the expression of this multicausality and, therefore, a biomarker of the pathophysiological process leading to the appearance of CAD.
5 Conclusion
This systematic review and meta-analysis demonstrated that patients with higher AIP values have higher odds of developing CAD. However, additional primary studies are warranted to define an optimal cutoff point of AIP to predict CAD.
Acknowledgments
None.
-
Funding information: The authors state that there is no funding involved.
-
Author contributions: J.R.U.-B.: conceptualization, methodology, investigation, formal analysis, and writing – original draft. A.H.-B.: methodology, investigation, formal analysis, and writing – original draft. A.A.-B.: methodology, investigation, formal analysis, and writing – original draft. M.D.M.-R.: methodology, investigation, formal analysis, and writing – original draft. A.C.-A.: methodology, investigation, formal analysis, and writing – original draft. F.E.S.-V.: methodology, investigation, formal analysis, and writing – original draft. A.V.-C.: methodology, investigation, formal analysis, and writing – original draft. V.A.B.-Z.: conceptualization, methodology, writing – review and editing, visualization, and supervision. P.H.-A.: investigation, writing – original draft, visualization, and supervision. G.V.-R.: investigation, writing – original draft, visualization, and supervision. A.V.-H.: conceptualization, methodology, writing – review and editing, visualization, and supervision. All authors have accepted responsibility for the entire content of this manuscript and approved its submission.
-
Conflict of interest: The authors state there is no conflict of interest.
-
Data availability statement: All data generated or analyzed during this study are included in this published article (and its supplementary information files).
References
[1] Khan MA, Hashim MJ, Mustafa H, Baniyas MY, Suwaidi SKBM, Al AlKatheeri R, et al. Global epidemiology of ischemic heart disease: results from the global burden of disease study. Cureus. 2020;12:e9349. 10.7759/CUREUS.9349.Suche in Google Scholar
[2] Virani SS, Alonso CA, Aparicio HJ, Benjamin EJ, Bittencourt MS, Callaway CW, et al. Heart disease and stroke statistics – 2021 update a report from the American Heart Association. Circulation. 2021;143:e254–743. 10.1161/CIR.0000000000000950.Suche in Google Scholar PubMed
[3] Virani SS, Alonso A, Benjamin EJ, Bittencourt MS, Callaway CW, Carson AP, et al. Heart disease and stroke statistics – 2020 update: a report from the American Heart Association. Circulation. 2020;141:e139–596. 10.1161/CIR.0000000000000757.Suche in Google Scholar PubMed
[4] Sanchis-Gomar F, Perez-Quilis C, Leischik R, Lucia A. Epidemiology of coronary heart disease and acute coronary syndrome. Ann Transl Med. 2016;4:256. 10.21037/ATM.2016.06.33.Suche in Google Scholar PubMed PubMed Central
[5] Luepker RV. Falling coronary heart disease rates: a better explanation. Circulation. 2016;133:8–11. 10.1161/CIRCULATIONAHA.115.019862.Suche in Google Scholar PubMed PubMed Central
[6] Bhatnagar P, Wickramasinghe K, Wilkins E, Townsend N. Trends in the epidemiology of cardiovascular disease in the UK. Heart. 2016;102:1945–52. 10.1136/HEARTJNL-2016-309573.Suche in Google Scholar
[7] Mensah GA, Wei GS, Sorlie PD, Fine LJ, Rosenberg Y, Kaufmann PG, et al. Decline in cardiovascular mortality: possible causes and implications. Circulation Res. 2017;120:366–80. 10.1161/CIRCRESAHA.116.309115.Suche in Google Scholar PubMed PubMed Central
[8] Kullo IJ. Novel biomarkers of coronary artery disease risk. Mayo clinic cardiology: concise textbook. 4th ed. New York: Oxford University Press; 2013. 10.1093/MED/9780199915712.003.1166.Suche in Google Scholar
[9] Casas JP, Shah T, Hingorani AD, Danesh J, Pepys MB. C-reactive protein and coronary heart disease: a critical review. J Intern Med. 2008;264:295–314. 10.1111/J.1365-2796.2008.02015.X.Suche in Google Scholar
[10] Khuseyinova N, Imhof A, Rothenbacher D, Trischler G, Kuelb S, Scharnagl H, et al. Association between Lp-PLA2 and coronary artery disease: focus on its relationship with lipoproteins and markers of inflammation and hemostasis. Atherosclerosis. 2005;182:181–8. 10.1016/J.ATHEROSCLEROSIS.2004.10.046.Suche in Google Scholar
[11] Morange PE, Bickel C, Nicaud V, Schnabel R, Rupprecht HJ, Peetz D, et al. Haemostatic factors and the risk of cardiovascular death in patients with coronary artery disease: the AtheroGene study. Arteriosclerosis Thrombosis, Vasc Biol. 2006;26:2793–9. 10.1161/01.ATV.0000249406.92992.0d.Suche in Google Scholar PubMed
[12] Johnson BD, Kip KE, Marroquin OC, Ridker PM, Kelsey SF, Shaw LJ, et al. Serum amyloid A as a predictor of coronary artery disease and cardiovascular outcome in women: the National Heart, Lung, and Blood Institute-Sponsored Women’s Ischemia Syndrome Evaluation (WISE). Circulation. 2004;109:726–32. 10.1161/01.CIR.0000115516.54550.B1.Suche in Google Scholar PubMed
[13] Hassanzadeh-Makoui R, Razi B, Aslani S, Imani D, Tabaee SS. The association between Matrix Metallo-proteinases-9 (MMP-9) gene family polymorphisms and risk of Coronary Artery Disease (CAD): a systematic review and meta-analysis. BMC Cardiovascular Disord. 2020;20:1–15. 10.1186/s12872-020-01510-4.Suche in Google Scholar PubMed PubMed Central
[14] Dobiásová M. Atherogenic impact of lecithin-cholesterol acyltransferase and its relation to cholesterol esterification rate in HDL (FERHDL) and AIP [log(TG/HDL-C)] biomarkers: the butterfly effect? Physiol Res. 2017;66:193–203.10.33549/physiolres.933621Suche in Google Scholar PubMed
[15] Han SH, Nicholls SJ, Sakuma I, Zhao D, Koh KK. Hypertriglyceridemia and cardiovascular diseases: revisited. Korean Circul J. 2016;46:135–44. 10.4070/KCJ.2016.46.2.135.Suche in Google Scholar PubMed PubMed Central
[16] Miller M, Kwiterovich PO. Isolated low HDL-cholesterol as an important risk factor for coronary heart disease. Eur Heart J. 1990;11:9–14. 10.1161/01.ATV.17.1.107.Suche in Google Scholar
[17] James SR, Ray L, Ravichandran K, Nanda SK. High atherogenic index of plasma in subclinical hypothyroidism: implications in assessment of cardiovascular disease risk. Indian J Endocrinol Metab. 2016;20:656–61. 10.4103/2230-8210.190550.Suche in Google Scholar PubMed PubMed Central
[18] Tagoe EA, Dwamena-Akoto E, Nsaful J, Aikins AR, Clegg-Lamptey JN, Quaye O. High atherogenic index of plasma and cardiovascular risk factors among Ghanaian breast cancer patients. Exp Biol Med (Maywood). 2020;245:1648–55. 10.1177/1535370220940992.Suche in Google Scholar PubMed PubMed Central
[19] Onen S, Taymur I. Evidence for the atherogenic index of plasma as a potential biomarker for cardiovascular disease in schizophrenia. J Psychopharmacol. 2021;35:1120–6. 10.1177/02698811211026450.Suche in Google Scholar PubMed
[20] Wang L, Chen F, Xiaoqi C, Yujun C, Zijie L. Atherogenic index of plasma is an independent risk factor for coronary artery disease and a higher SYNTAX score. Angiology. 2021;72:181–6. 10.1177/0003319720949804.Suche in Google Scholar PubMed
[21] Al Shawaf E, Al-Ozairi E, Al-Asfar F, Mohammad A, Al-Beloushi S, Devarajan S, et al. Atherogenic index of plasma (AIP) a tool to assess changes in cardiovascular disease risk post laparoscopic sleeve gastrectomy. J Diabetes Res. 2020;2020:1–9. 10.1155/2020/2091341.Suche in Google Scholar PubMed PubMed Central
[22] Guo Q, Zhou S, Feng X, Yang J, Qiao J, Zhao Y, et al. The sensibility of the new blood lipid indicator—atherogenic index of plasma (AIP) in menopausal women with coronary artery disease. Lipids in Health and Disease. 2020;19:1–8. 10.1186/S12944-020-01208-8.Suche in Google Scholar
[23] Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JPA, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ. 2009;339:b2700. 10.1136/BMJ.B2700.Suche in Google Scholar PubMed PubMed Central
[24] Wells G, Shea B, O’Connell D, Peterson J, Welch V, Losos M, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. 2014. http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp.Suche in Google Scholar
[25] Zhang J, Yu KF. What’s the relative risk? A method of correcting the odds ratio in cohort studies of common outcomes. JAMA. 1998;280:1690–1. 10.1001/JAMA.280.19.1690.Suche in Google Scholar PubMed
[26] Shor E, Roelfs D, Vang ZM. The “Hispanic mortality paradox” revisited: meta-analysis and meta-regression of life-course differentials in Latin American and Caribbean immigrants’ mortality. Soc Sci Med. 2017;186:20–33. 10.1016/J.SOCSCIMED.2017.05.049.Suche in Google Scholar PubMed
[27] Hozo SP, Djulbegovic B, Hozo I. Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Methodol. 2005;5(1):1–10. 10.1186/1471-2288-5-13.Suche in Google Scholar PubMed PubMed Central
[28] Onat A, Can G, Kaya H, Hergenç G. “Atherogenic index of plasma” (log10 triglyceride/high-density lipoprotein−cholesterol) predicts high blood pressure, diabetes, and vascular events. J Clin Lipidol. 2010;4:89–98. 10.1016/J.JACL.2010.02.005.Suche in Google Scholar PubMed
[29] Al-Shaer MH, Elzaky MM, Farag ESM, Saad MOM. In type 2 diabetes mellitus patients, the atherogenic index of plasma as a marker of coronary artery diseases. Indian J Clin Cardiol. 2021;1:263246362110313. 10.1177/26324636211031362.Suche in Google Scholar
[30] Çelik E, Çora AR, Karadem KB. The effect of untraditional lipid parameters in the development of coronary artery disease: Atherogenic index of plasma, atherogenic coefficient and lipoprotein combined index. J Saudi Heart Assoc. 2021;33:244–50. 10.37616/2212-5043.1266.Suche in Google Scholar PubMed PubMed Central
[31] Won KB, Jang MH, Park EJ, Park HB, Heo R, Han D, et al. Atherogenic index of plasma and the risk of advanced subclinical coronary artery disease beyond traditional risk factors: an observational cohort study. Clin Cardiol. 2020;43:1398–404. 10.1002/CLC.23450.Suche in Google Scholar PubMed PubMed Central
[32] Guo Q, Zhou S, Feng X, Yang J, Qiao J, Zhao Y, et al. The sensibility of the new blood lipid indicator-atherogenic index of plasma (AIP) in menopausal women with coronary artery disease. Lipids Health and Disease. 2020:19;1–8. 10.1186%2Fs12944-020-01208-8.Suche in Google Scholar
[33] Wu TT, Gao Y, Zheng YY, Ma YT, Xie X. Atherogenic index of plasma (AIP): a novel predictive indicator for the coronary artery disease in postmenopausal women. Lipids Health Dis. 2018;17:1–7. 10.1186/S12944-018-0828-Z.Suche in Google Scholar
[34] Cai G, Shi G, Xue S, Lu W. The atherogenic index of plasma is a strong and independent predictor for coronary artery disease in the Chinese Han population. Med (U S). 2017;96:1–6. 10.1097/MD.0000000000008058.Suche in Google Scholar PubMed PubMed Central
[35] Shanker J, Kakkar VV. Contribution of classical and emerging risk factors to coronary artery disease in Asian Indians. Int J Cardiol. 2016;214:97–106. 10.1016/J.IJCARD.2016.03.012.Suche in Google Scholar
[36] Priídavkovaá D, Kantárová D, Lišková R, Červeň P, Kovář F, Mokáň M. The role of epicardial fat and obesity parameters in the prediction of coronary heart disease. Vnitr Lek. 2016;62:256–62.Suche in Google Scholar
[37] Dai W, Li Y, Zheng H. Estradiol/testosterone imbalance: impact on coronary heart disease risk factors in postmenopausal women. Cardiology. 2012;121:249–54. 10.1159/000337274.Suche in Google Scholar PubMed
[38] Zhou K, Qin Z, Tian J, Cui K, Yan Y, Lyu S. The atherogenic index of plasma: a powerful and reliable predictor for coronary artery disease in patients with type 2 diabetes. Angiology. 2021;72:934–41. 10.1177/00033197211012129.Suche in Google Scholar PubMed
[39] Cai G, Liu W, Lv S, Wang X, Guo Y, Yan Z, et al. Gender-specific associations between atherogenic index of plasma and the presence and severity of acute coronary syndrome in very young adults: a hospital-based observational study. Lipids Health Dis. 2019;18:1–9. 10.1186/s12944-019-1043-2.Suche in Google Scholar PubMed PubMed Central
[40] Sedhai YR, Basnyat S, Konda P, Koirala A, Prasai P, Raza M, et al. Atherogenic index of plasma is a marker of plaque vulnerability in coronary artery disease. Chest. 2018;154:85A–6A. 10.1016/J.CHEST.2018.08.077.Suche in Google Scholar
[41] Xie F, Zhou H, Wang Y. Atherogenic index of plasma is a novel and strong predictor associated with fatty liver: a cross-sectional study in the Chinese Han population. Lipids Health Dis. 2019;18:1–6. 10.1186/s12944-019-1112-6.Suche in Google Scholar PubMed PubMed Central
[42] Hernández JL, Baldeón C, López-Sundh AE, Ocejo-Vinyals JG, Blanco R, González-López MA. Atherogenic index of plasma is associated with the severity of hidradenitis suppurativa: a case-control study. Lipids Health Dis. 2020;19:1–6. 10.1186/S12944-020-01377-6.Suche in Google Scholar
[43] Nie X, Gao L, Wang L, Wang J. Atherogenic index of plasma: a potential biomarker for clinical diagnosis of diabetic foot osteomyelitis. Surg Infect (Larchmt). 2020;21:9–14. 10.1089/SUR.2019.020.Suche in Google Scholar
[44] Shen SW, Lu Y, Li F, Yang CJ, Feng YB, Li HW, et al. Atherogenic index of plasma is an effective index for estimating abdominal obesity. Lipids Health Dis. 2018;17:1–6. 10.1186/S12944-018-0656-1.Suche in Google Scholar PubMed PubMed Central
[45] Zhu XW, Deng FY, Lei SF. Meta-analysis of atherogenic index of plasma and other lipid parameters in relation to risk of type 2 diabetes mellitus. Prim Care Diabetes. 2015;9:60–7. 10.1016/J.PCD.2014.03.007.Suche in Google Scholar
[46] Zhou Y, Shang X. Usefulness of atherogenic index of plasma for estimating reduced eGFR risk: insights from the national health and nutrition examination survey. Postgrad Med. 2021;133:278–85. 10.1080/00325481.2020.1838138.Suche in Google Scholar PubMed
[47] Kubong LN, Nya Biapa PC, Chetcha B, Yanou-Njintang N, Moor Ama VJ, Pieme CA. Relationship between higher atherogenic index of plasma and oxidative stress of a group of patients living with sickle cell anemia in Cameroon. Adv Hematol. 2020;2020. 10.1155/2020/9864371.Suche in Google Scholar PubMed PubMed Central
[48] Kammar-García A, López-Moreno P, Hernández-Hernández ME, Ortíz-Bueno AM, Martínez-Montaño MLC. Atherogenic index of plasma as a marker of cardiovascular risk factors in Mexicans aged 18 to 22 years. Proc (Bayl Univ Med Cent). 2020;34:22–7. 10.1080/08998280.2020.1799479.Suche in Google Scholar PubMed PubMed Central
[49] Garg R, Knox N, Prasad S, Zinzuwadia S, Rech MA. The atherogenic index of plasma is independently associated with symptomatic carotid artery stenosis. J Stroke Cerebrovasc Dis. 2020;29:105351. 10.1016/J.JVS.2010.03.047.Suche in Google Scholar
[50] Sigala F, Kotsinas A, Savari P, Filis K, Markantonis S, Iliodromitis EK, et al. Oxidized LDL in human carotid plaques is related to symptomatic carotid disease and lesion instability. J Vasc Surg. 2010;52:704–13. 10.1016/J.JVS.2010.03.047.Suche in Google Scholar
[51] Fu L, Zhou Y, Sun J, Zhu Z, Xing Z, Zhou S, et al. Atherogenic index of plasma is associated with major adverse cardiovascular events in patients with type 2 diabetes mellitus. Cardiovas Diabetol. 2021;201:1–11. 10.1186/s12933-021-01393-5.Suche in Google Scholar PubMed PubMed Central
[52] Süleymanoğlu M, Rencüzoğulları İ, Karabağ Y, Çağdaş M, Yesin M, Gümüşdağ A, et al. The relationship between atherogenic index of plasma and no-reflow in patients with acute ST-segment elevation myocardial infarction who underwent primary percutaneous coronary intervention. Int J Cardiovas Imaging. 2020;36:789–96. 10.1007/S10554-019-01766-8.Suche in Google Scholar
[53] Bo MS, Cheah WL, Lwin S, Moe Nwe T, Win TT, Aung M. Understanding the relationship between atherogenic index of plasma and cardiovascular disease risk factors among staff of an university in Malaysia. J Nutr Metab. 2018;2018:1–6. 10.1155/2018/7027624.Suche in Google Scholar PubMed PubMed Central
[54] Choudhary MK, Eräranta A, Koskela J, Tikkakoski AJ, Nevalainen PI, Kähönen M, et al. Atherogenic index of plasma is related to arterial stiffness but not to blood pressure in normotensive and never-treated hypertensive subjects. Blood Press. 2019;28:157–67. 10.1080/08037051.2019.1583060.Suche in Google Scholar PubMed
[55] Ikonomidis I, Makavos G, Lekakis J. Arterial stiffness and coronary artery disease. Curr OpCardiology. 2015;30:422–31. 10.1097/HCO.0000000000000179.Suche in Google Scholar PubMed
[56] Kaur M, Rahimi R, Razali F, Mohd Noor N, Omar E, Abdul Manaf Z, et al. Association of coronary artery calcium score with calcification and degree of stenosis: an autopsy study. Malaysian J Pathol. 2019;41:177–83. http://www.mjpath.org.my/2019/v41n2/coronary-artery-calcium.pdf.Suche in Google Scholar
[57] Nam JS, Kim MK, Nam JY, Park K, Kang S, Ahn CW, et al. Association between atherogenic index of plasma and coronary artery calcification progression in Korean adults. Lipids Health Dis. 2020;19:1–7. 10.1186/S12944-020-01317-4.Suche in Google Scholar
[58] Won KB, Heo R, Park HB, Lee BK, Lin FY, Hadamitzky M, et al. Atherogenic index of plasma and the risk of rapid progression of coronary atherosclerosis beyond traditional risk factors. Atherosclerosis. 2021;324:46–51. 10.1016/J.ATHEROSCLEROSIS.2021.03.009.Suche in Google Scholar PubMed
[59] Won KB, Jang MH, Park EJ, Park HB, Heo R, Han D, et al. Atherogenic index of plasma and the risk of advanced subclinical coronary artery disease beyond traditional risk factors: an observational cohort study. Clin Cardiol. 2020;43:1398–404. 10.1002/CLC.23450.Suche in Google Scholar PubMed PubMed Central
[60] Hartopo AB, Arso IA, Setianto BY Low plasma atherogenic index associated with poor prognosis in hospitalized patients with acute myocardial infarction. Indonesian J Intern Med 2016;48:106–13. http://www.inaactamedica.org/archives/2016/27550879.pdf.Suche in Google Scholar
[61] Wu J, Zhou Q, Wei Z, Wei J, Cui M. Atherogenic index of plasma and coronary artery disease in the adult population: a meta-analysis. Front Cardiovas Med. 2021;0:1927. 10.3389/FCVM.2021.817441.Suche in Google Scholar
[62] Huang H, Yu X, Li L, Shi G, Li F, Xiao J, et al. Atherogenic index of plasma is related to coronary atherosclerotic disease in elderly individuals: a cross-sectional study. Lipids Health Dis. 2021;20:1–9. 10.1186/S12944-021-01496-8.Suche in Google Scholar
© 2022 the author(s), published by De Gruyter
This work is licensed under the Creative Commons Attribution 4.0 International License.
Artikel in diesem Heft
- Research Articles
- AMBRA1 attenuates the proliferation of uveal melanoma cells
- A ceRNA network mediated by LINC00475 in papillary thyroid carcinoma
- Differences in complications between hepatitis B-related cirrhosis and alcohol-related cirrhosis
- Effect of gestational diabetes mellitus on lipid profile: A systematic review and meta-analysis
- Long noncoding RNA NR2F1-AS1 stimulates the tumorigenic behavior of non-small cell lung cancer cells by sponging miR-363-3p to increase SOX4
- Promising novel biomarkers and candidate small-molecule drugs for lung adenocarcinoma: Evidence from bioinformatics analysis of high-throughput data
- Plasmapheresis: Is it a potential alternative treatment for chronic urticaria?
- The biomarkers of key miRNAs and gene targets associated with extranodal NK/T-cell lymphoma
- Gene signature to predict prognostic survival of hepatocellular carcinoma
- Effects of miRNA-199a-5p on cell proliferation and apoptosis of uterine leiomyoma by targeting MED12
- Does diabetes affect paraneoplastic thrombocytosis in colorectal cancer?
- Is there any effect on imprinted genes H19, PEG3, and SNRPN during AOA?
- Leptin and PCSK9 concentrations are associated with vascular endothelial cytokines in patients with stable coronary heart disease
- Pericentric inversion of chromosome 6 and male fertility problems
- Staple line reinforcement with nebulized cyanoacrylate glue in laparoscopic sleeve gastrectomy: A propensity score-matched study
- Retrospective analysis of crescent score in clinical prognosis of IgA nephropathy
- Expression of DNM3 is associated with good outcome in colorectal cancer
- Activation of SphK2 contributes to adipocyte-induced EOC cell proliferation
- CRRT influences PICCO measurements in febrile critically ill patients
- SLCO4A1-AS1 mediates pancreatic cancer development via miR-4673/KIF21B axis
- lncRNA ACTA2-AS1 inhibits malignant phenotypes of gastric cancer cells
- circ_AKT3 knockdown suppresses cisplatin resistance in gastric cancer
- Prognostic value of nicotinamide N-methyltransferase in human cancers: Evidence from a meta-analysis and database validation
- GPC2 deficiency inhibits cell growth and metastasis in colon adenocarcinoma
- A pan-cancer analysis of the oncogenic role of Holliday junction recognition protein in human tumors
- Radiation increases COL1A1, COL3A1, and COL1A2 expression in breast cancer
- Association between preventable risk factors and metabolic syndrome
- miR-29c-5p knockdown reduces inflammation and blood–brain barrier disruption by upregulating LRP6
- Cardiac contractility modulation ameliorates myocardial metabolic remodeling in a rabbit model of chronic heart failure through activation of AMPK and PPAR-α pathway
- Quercitrin protects human bronchial epithelial cells from oxidative damage
- Smurf2 suppresses the metastasis of hepatocellular carcinoma via ubiquitin degradation of Smad2
- circRNA_0001679/miR-338-3p/DUSP16 axis aggravates acute lung injury
- Sonoclot’s usefulness in prediction of cardiopulmonary arrest prognosis: A proof of concept study
- Four drug metabolism-related subgroups of pancreatic adenocarcinoma in prognosis, immune infiltration, and gene mutation
- Decreased expression of miR-195 mediated by hypermethylation promotes osteosarcoma
- LMO3 promotes proliferation and metastasis of papillary thyroid carcinoma cells by regulating LIMK1-mediated cofilin and the β-catenin pathway
- Cx43 upregulation in HUVECs under stretch via TGF-β1 and cytoskeletal network
- Evaluation of menstrual irregularities after COVID-19 vaccination: Results of the MECOVAC survey
- Histopathologic findings on removed stomach after sleeve gastrectomy. Do they influence the outcome?
- Analysis of the expression and prognostic value of MT1-MMP, β1-integrin and YAP1 in glioma
- Optimal diagnosis of the skin cancer using a hybrid deep neural network and grasshopper optimization algorithm
- miR-223-3p alleviates TGF-β-induced epithelial-mesenchymal transition and extracellular matrix deposition by targeting SP3 in endometrial epithelial cells
- Clinical value of SIRT1 as a prognostic biomarker in esophageal squamous cell carcinoma, a systematic meta-analysis
- circ_0020123 promotes cell proliferation and migration in lung adenocarcinoma via PDZD8
- miR-22-5p regulates the self-renewal of spermatogonial stem cells by targeting EZH2
- hsa-miR-340-5p inhibits epithelial–mesenchymal transition in endometriosis by targeting MAP3K2 and inactivating MAPK/ERK signaling
- circ_0085296 inhibits the biological functions of trophoblast cells to promote the progression of preeclampsia via the miR-942-5p/THBS2 network
- TCD hemodynamics findings in the subacute phase of anterior circulation stroke patients treated with mechanical thrombectomy
- Development of a risk-stratification scoring system for predicting risk of breast cancer based on non-alcoholic fatty liver disease, non-alcoholic fatty pancreas disease, and uric acid
- Tollip promotes hepatocellular carcinoma progression via PI3K/AKT pathway
- circ_0062491 alleviates periodontitis via the miR-142-5p/IGF1 axis
- Human amniotic fluid as a source of stem cells
- lncRNA NONRATT013819.2 promotes transforming growth factor-β1-induced myofibroblastic transition of hepatic stellate cells by miR24-3p/lox
- NORAD modulates miR-30c-5p-LDHA to protect lung endothelial cells damage
- Idiopathic pulmonary fibrosis telemedicine management during COVID-19 outbreak
- Risk factors for adverse drug reactions associated with clopidogrel therapy
- Serum zinc associated with immunity and inflammatory markers in Covid-19
- The relationship between night shift work and breast cancer incidence: A systematic review and meta-analysis of observational studies
- LncRNA expression in idiopathic achalasia: New insight and preliminary exploration into pathogenesis
- Notoginsenoside R1 alleviates spinal cord injury through the miR-301a/KLF7 axis to activate Wnt/β-catenin pathway
- Moscatilin suppresses the inflammation from macrophages and T cells
- Zoledronate promotes ECM degradation and apoptosis via Wnt/β-catenin
- Epithelial-mesenchymal transition-related genes in coronary artery disease
- The effect evaluation of traditional vaginal surgery and transvaginal mesh surgery for severe pelvic organ prolapse: 5 years follow-up
- Repeated partial splenic artery embolization for hypersplenism improves platelet count
- Low expression of miR-27b in serum exosomes of non-small cell lung cancer facilitates its progression by affecting EGFR
- Exosomal hsa_circ_0000519 modulates the NSCLC cell growth and metastasis via miR-1258/RHOV axis
- miR-455-5p enhances 5-fluorouracil sensitivity in colorectal cancer cells by targeting PIK3R1 and DEPDC1
- The effect of tranexamic acid on the reduction of intraoperative and postoperative blood loss and thromboembolic risk in patients with hip fracture
- Isocitrate dehydrogenase 1 mutation in cholangiocarcinoma impairs tumor progression by sensitizing cells to ferroptosis
- Artemisinin protects against cerebral ischemia and reperfusion injury via inhibiting the NF-κB pathway
- A 16-gene signature associated with homologous recombination deficiency for prognosis prediction in patients with triple-negative breast cancer
- Lidocaine ameliorates chronic constriction injury-induced neuropathic pain through regulating M1/M2 microglia polarization
- MicroRNA 322-5p reduced neuronal inflammation via the TLR4/TRAF6/NF-κB axis in a rat epilepsy model
- miR-1273h-5p suppresses CXCL12 expression and inhibits gastric cancer cell invasion and metastasis
- Clinical characteristics of pneumonia patients of long course of illness infected with SARS-CoV-2
- circRNF20 aggravates the malignancy of retinoblastoma depending on the regulation of miR-132-3p/PAX6 axis
- Linezolid for resistant Gram-positive bacterial infections in children under 12 years: A meta-analysis
- Rack1 regulates pro-inflammatory cytokines by NF-κB in diabetic nephropathy
- Comprehensive analysis of molecular mechanism and a novel prognostic signature based on small nuclear RNA biomarkers in gastric cancer patients
- Smog and risk of maternal and fetal birth outcomes: A retrospective study in Baoding, China
- Let-7i-3p inhibits the cell cycle, proliferation, invasion, and migration of colorectal cancer cells via downregulating CCND1
- β2-Adrenergic receptor expression in subchondral bone of patients with varus knee osteoarthritis
- Possible impact of COVID-19 pandemic and lockdown on suicide behavior among patients in Southeast Serbia
- In vitro antimicrobial activity of ozonated oil in liposome eyedrop against multidrug-resistant bacteria
- Potential biomarkers for inflammatory response in acute lung injury
- A low serum uric acid concentration predicts a poor prognosis in adult patients with candidemia
- Antitumor activity of recombinant oncolytic vaccinia virus with human IL2
- ALKBH5 inhibits TNF-α-induced apoptosis of HUVECs through Bcl-2 pathway
- Risk prediction of cardiovascular disease using machine learning classifiers
- Value of ultrasonography parameters in diagnosing polycystic ovary syndrome
- Bioinformatics analysis reveals three key genes and four survival genes associated with youth-onset NSCLC
- Identification of autophagy-related biomarkers in patients with pulmonary arterial hypertension based on bioinformatics analysis
- Protective effects of glaucocalyxin A on the airway of asthmatic mice
- Overexpression of miR-100-5p inhibits papillary thyroid cancer progression via targeting FZD8
- Bioinformatics-based analysis of SUMOylation-related genes in hepatocellular carcinoma reveals a role of upregulated SAE1 in promoting cell proliferation
- Effectiveness and clinical benefits of new anti-diabetic drugs: A real life experience
- Identification of osteoporosis based on gene biomarkers using support vector machine
- Tanshinone IIA reverses oxaliplatin resistance in colorectal cancer through microRNA-30b-5p/AVEN axis
- miR-212-5p inhibits nasopharyngeal carcinoma progression by targeting METTL3
- Association of ST-T changes with all-cause mortality among patients with peripheral T-cell lymphomas
- LINC00665/miRNAs axis-mediated collagen type XI alpha 1 correlates with immune infiltration and malignant phenotypes in lung adenocarcinoma
- The perinatal factors that influence the excretion of fecal calprotectin in premature-born children
- Effect of femoral head necrosis cystic area on femoral head collapse and stress distribution in femoral head: A clinical and finite element study
- Does the use of 3D-printed cones give a chance to postpone the use of megaprostheses in patients with large bone defects in the knee joint?
- lncRNA HAGLR modulates myocardial ischemia–reperfusion injury in mice through regulating miR-133a-3p/MAPK1 axis
- Protective effect of ghrelin on intestinal I/R injury in rats
- In vivo knee kinematics of an innovative prosthesis design
- Relationship between the height of fibular head and the incidence and severity of knee osteoarthritis
- lncRNA WT1-AS attenuates hypoxia/ischemia-induced neuronal injury during cerebral ischemic stroke via miR-186-5p/XIAP axis
- Correlation of cardiac troponin T and APACHE III score with all-cause in-hospital mortality in critically ill patients with acute pulmonary embolism
- LncRNA LINC01857 reduces metastasis and angiogenesis in breast cancer cells via regulating miR-2052/CENPQ axis
- Endothelial cell-specific molecule 1 (ESM1) promoted by transcription factor SPI1 acts as an oncogene to modulate the malignant phenotype of endometrial cancer
- SELENBP1 inhibits progression of colorectal cancer by suppressing epithelial–mesenchymal transition
- Visfatin is negatively associated with coronary artery lesions in subjects with impaired fasting glucose
- Treatment and outcomes of mechanical complications of acute myocardial infarction during the Covid-19 era: A comparison with the pre-Covid-19 period. A systematic review and meta-analysis
- Neonatal stroke surveillance study protocol in the United Kingdom and Republic of Ireland
- Oncogenic role of TWF2 in human tumors: A pan-cancer analysis
- Mean corpuscular hemoglobin predicts the length of hospital stay independent of severity classification in patients with acute pancreatitis
- Association of gallstone and polymorphisms of UGT1A1*27 and UGT1A1*28 in patients with hepatitis B virus-related liver failure
- TGF-β1 upregulates Sar1a expression and induces procollagen-I secretion in hypertrophic scarring fibroblasts
- Antisense lncRNA PCNA-AS1 promotes esophageal squamous cell carcinoma progression through the miR-2467-3p/PCNA axis
- NK-cell dysfunction of acute myeloid leukemia in relation to the renin–angiotensin system and neurotransmitter genes
- The effect of dilution with glucose and prolonged injection time on dexamethasone-induced perineal irritation – A randomized controlled trial
- miR-146-5p restrains calcification of vascular smooth muscle cells by suppressing TRAF6
- Role of lncRNA MIAT/miR-361-3p/CCAR2 in prostate cancer cells
- lncRNA NORAD promotes lung cancer progression by competitively binding to miR-28-3p with E2F2
- Noninvasive diagnosis of AIH/PBC overlap syndrome based on prediction models
- lncRNA FAM230B is highly expressed in colorectal cancer and suppresses the maturation of miR-1182 to increase cell proliferation
- circ-LIMK1 regulates cisplatin resistance in lung adenocarcinoma by targeting miR-512-5p/HMGA1 axis
- LncRNA SNHG3 promoted cell proliferation, migration, and metastasis of esophageal squamous cell carcinoma via regulating miR-151a-3p/PFN2 axis
- Risk perception and affective state on work exhaustion in obstetrics during the COVID-19 pandemic
- lncRNA-AC130710/miR-129-5p/mGluR1 axis promote migration and invasion by activating PKCα-MAPK signal pathway in melanoma
- SNRPB promotes cell cycle progression in thyroid carcinoma via inhibiting p53
- Xylooligosaccharides and aerobic training regulate metabolism and behavior in rats with streptozotocin-induced type 1 diabetes
- Serpin family A member 1 is an oncogene in glioma and its translation is enhanced by NAD(P)H quinone dehydrogenase 1 through RNA-binding activity
- Silencing of CPSF7 inhibits the proliferation, migration, and invasion of lung adenocarcinoma cells by blocking the AKT/mTOR signaling pathway
- Ultrasound-guided lumbar plexus block versus transversus abdominis plane block for analgesia in children with hip dislocation: A double-blind, randomized trial
- Relationship of plasma MBP and 8-oxo-dG with brain damage in preterm
- Identification of a novel necroptosis-associated miRNA signature for predicting the prognosis in head and neck squamous cell carcinoma
- Delayed femoral vein ligation reduces operative time and blood loss during hip disarticulation in patients with extremity tumors
- The expression of ASAP3 and NOTCH3 and the clinicopathological characteristics of adult glioma patients
- Longitudinal analysis of factors related to Helicobacter pylori infection in Chinese adults
- HOXA10 enhances cell proliferation and suppresses apoptosis in esophageal cancer via activating p38/ERK signaling pathway
- Meta-analysis of early-life antibiotic use and allergic rhinitis
- Marital status and its correlation with age, race, and gender in prognosis of tonsil squamous cell carcinomas
- HPV16 E6E7 up-regulates KIF2A expression by activating JNK/c-Jun signal, is beneficial to migration and invasion of cervical cancer cells
- Amino acid profiles in the tissue and serum of patients with liver cancer
- Pain in critically ill COVID-19 patients: An Italian retrospective study
- Immunohistochemical distribution of Bcl-2 and p53 apoptotic markers in acetamiprid-induced nephrotoxicity
- Estradiol pretreatment in GnRH antagonist protocol for IVF/ICSI treatment
- Long non-coding RNAs LINC00689 inhibits the apoptosis of human nucleus pulposus cells via miR-3127-5p/ATG7 axis-mediated autophagy
- The relationship between oxygen therapy, drug therapy, and COVID-19 mortality
- Monitoring hypertensive disorders in pregnancy to prevent preeclampsia in pregnant women of advanced maternal age: Trial mimicking with retrospective data
- SETD1A promotes the proliferation and glycolysis of nasopharyngeal carcinoma cells by activating the PI3K/Akt pathway
- The role of Shunaoxin pills in the treatment of chronic cerebral hypoperfusion and its main pharmacodynamic components
- TET3 governs malignant behaviors and unfavorable prognosis of esophageal squamous cell carcinoma by activating the PI3K/AKT/GSK3β/β-catenin pathway
- Associations between morphokinetic parameters of temporary-arrest embryos and the clinical prognosis in FET cycles
- Long noncoding RNA WT1-AS regulates trophoblast proliferation, migration, and invasion via the microRNA-186-5p/CADM2 axis
- The incidence of bronchiectasis in chronic obstructive pulmonary disease
- Integrated bioinformatics analysis shows integrin alpha 3 is a prognostic biomarker for pancreatic cancer
- Inhibition of miR-21 improves pulmonary vascular responses in bronchopulmonary dysplasia by targeting the DDAH1/ADMA/NO pathway
- Comparison of hospitalized patients with severe pneumonia caused by COVID-19 and influenza A (H7N9 and H1N1): A retrospective study from a designated hospital
- lncRNA ZFAS1 promotes intervertebral disc degeneration by upregulating AAK1
- Pathological characteristics of liver injury induced by N,N-dimethylformamide: From humans to animal models
- lncRNA ELFN1-AS1 enhances the progression of colon cancer by targeting miR-4270 to upregulate AURKB
- DARS-AS1 modulates cell proliferation and migration of gastric cancer cells by regulating miR-330-3p/NAT10 axis
- Dezocine inhibits cell proliferation, migration, and invasion by targeting CRABP2 in ovarian cancer
- MGST1 alleviates the oxidative stress of trophoblast cells induced by hypoxia/reoxygenation and promotes cell proliferation, migration, and invasion by activating the PI3K/AKT/mTOR pathway
- Bifidobacterium lactis Probio-M8 ameliorated the symptoms of type 2 diabetes mellitus mice by changing ileum FXR-CYP7A1
- circRNA DENND1B inhibits tumorigenicity of clear cell renal cell carcinoma via miR-122-5p/TIMP2 axis
- EphA3 targeted by miR-3666 contributes to melanoma malignancy via activating ERK1/2 and p38 MAPK pathways
- Pacemakers and methylprednisolone pulse therapy in immune-related myocarditis concomitant with complete heart block
- miRNA-130a-3p targets sphingosine-1-phosphate receptor 1 to activate the microglial and astrocytes and to promote neural injury under the high glucose condition
- Review Articles
- Current management of cancer pain in Italy: Expert opinion paper
- Hearing loss and brain disorders: A review of multiple pathologies
- The rationale for using low-molecular weight heparin in the therapy of symptomatic COVID-19 patients
- Amyotrophic lateral sclerosis and delayed onset muscle soreness in light of the impaired blink and stretch reflexes – watch out for Piezo2
- Interleukin-35 in autoimmune dermatoses: Current concepts
- Recent discoveries in microbiota dysbiosis, cholangiocytic factors, and models for studying the pathogenesis of primary sclerosing cholangitis
- Advantages of ketamine in pediatric anesthesia
- Congenital adrenal hyperplasia. Role of dentist in early diagnosis
- Migraine management: Non-pharmacological points for patients and health care professionals
- Atherogenic index of plasma and coronary artery disease: A systematic review
- Physiological and modulatory role of thioredoxins in the cellular function
- Case Reports
- Intrauterine Bakri balloon tamponade plus cervical cerclage for the prevention and treatment of postpartum haemorrhage in late pregnancy complicated with acute aortic dissection: Case series
- A case of successful pembrolizumab monotherapy in a patient with advanced lung adenocarcinoma: Use of multiple biomarkers in combination for clinical practice
- Unusual neurological manifestations of bilateral medial medullary infarction: A case report
- Atypical symptoms of malignant hyperthermia: A rare causative mutation in the RYR1 gene
- A case report of dermatomyositis with the missed diagnosis of non-small cell lung cancer and concurrence of pulmonary tuberculosis
- A rare case of endometrial polyp complicated with uterine inversion: A case report and clinical management
- Spontaneous rupturing of splenic artery aneurysm: Another reason for fatal syncope and shock (Case report and literature review)
- Fungal infection mimicking COVID-19 infection – A case report
- Concurrent aspergillosis and cystic pulmonary metastases in a patient with tongue squamous cell carcinoma
- Paraganglioma-induced inverted takotsubo-like cardiomyopathy leading to cardiogenic shock successfully treated with extracorporeal membrane oxygenation
- Lineage switch from lymphoma to myeloid neoplasms: First case series from a single institution
- Trismus during tracheal extubation as a complication of general anaesthesia – A case report
- Simultaneous treatment of a pubovesical fistula and lymph node metastasis secondary to multimodal treatment for prostate cancer: Case report and review of the literature
- Two case reports of skin vasculitis following the COVID-19 immunization
- Ureteroiliac fistula after oncological surgery: Case report and review of the literature
- Synchronous triple primary malignant tumours in the bladder, prostate, and lung harbouring TP53 and MEK1 mutations accompanied with severe cardiovascular diseases: A case report
- Huge mucinous cystic neoplasms with adhesion to the left colon: A case report and literature review
- Commentary
- Commentary on “Clinicopathological features of programmed cell death-ligand 1 expression in patients with oral squamous cell carcinoma”
- Rapid Communication
- COVID-19 fear, post-traumatic stress, growth, and the role of resilience
- Erratum
- Erratum to “Tollip promotes hepatocellular carcinoma progression via PI3K/AKT pathway”
- Erratum to “Effect of femoral head necrosis cystic area on femoral head collapse and stress distribution in femoral head: A clinical and finite element study”
- Erratum to “lncRNA NORAD promotes lung cancer progression by competitively binding to miR-28-3p with E2F2”
- Retraction
- Expression and role of ABIN1 in sepsis: In vitro and in vivo studies
- Retraction to “miR-519d downregulates LEP expression to inhibit preeclampsia development”
- Special Issue Computational Intelligence Methodologies Meets Recurrent Cancers - Part II
- Usefulness of close surveillance for rectal cancer patients after neoadjuvant chemoradiotherapy
Artikel in diesem Heft
- Research Articles
- AMBRA1 attenuates the proliferation of uveal melanoma cells
- A ceRNA network mediated by LINC00475 in papillary thyroid carcinoma
- Differences in complications between hepatitis B-related cirrhosis and alcohol-related cirrhosis
- Effect of gestational diabetes mellitus on lipid profile: A systematic review and meta-analysis
- Long noncoding RNA NR2F1-AS1 stimulates the tumorigenic behavior of non-small cell lung cancer cells by sponging miR-363-3p to increase SOX4
- Promising novel biomarkers and candidate small-molecule drugs for lung adenocarcinoma: Evidence from bioinformatics analysis of high-throughput data
- Plasmapheresis: Is it a potential alternative treatment for chronic urticaria?
- The biomarkers of key miRNAs and gene targets associated with extranodal NK/T-cell lymphoma
- Gene signature to predict prognostic survival of hepatocellular carcinoma
- Effects of miRNA-199a-5p on cell proliferation and apoptosis of uterine leiomyoma by targeting MED12
- Does diabetes affect paraneoplastic thrombocytosis in colorectal cancer?
- Is there any effect on imprinted genes H19, PEG3, and SNRPN during AOA?
- Leptin and PCSK9 concentrations are associated with vascular endothelial cytokines in patients with stable coronary heart disease
- Pericentric inversion of chromosome 6 and male fertility problems
- Staple line reinforcement with nebulized cyanoacrylate glue in laparoscopic sleeve gastrectomy: A propensity score-matched study
- Retrospective analysis of crescent score in clinical prognosis of IgA nephropathy
- Expression of DNM3 is associated with good outcome in colorectal cancer
- Activation of SphK2 contributes to adipocyte-induced EOC cell proliferation
- CRRT influences PICCO measurements in febrile critically ill patients
- SLCO4A1-AS1 mediates pancreatic cancer development via miR-4673/KIF21B axis
- lncRNA ACTA2-AS1 inhibits malignant phenotypes of gastric cancer cells
- circ_AKT3 knockdown suppresses cisplatin resistance in gastric cancer
- Prognostic value of nicotinamide N-methyltransferase in human cancers: Evidence from a meta-analysis and database validation
- GPC2 deficiency inhibits cell growth and metastasis in colon adenocarcinoma
- A pan-cancer analysis of the oncogenic role of Holliday junction recognition protein in human tumors
- Radiation increases COL1A1, COL3A1, and COL1A2 expression in breast cancer
- Association between preventable risk factors and metabolic syndrome
- miR-29c-5p knockdown reduces inflammation and blood–brain barrier disruption by upregulating LRP6
- Cardiac contractility modulation ameliorates myocardial metabolic remodeling in a rabbit model of chronic heart failure through activation of AMPK and PPAR-α pathway
- Quercitrin protects human bronchial epithelial cells from oxidative damage
- Smurf2 suppresses the metastasis of hepatocellular carcinoma via ubiquitin degradation of Smad2
- circRNA_0001679/miR-338-3p/DUSP16 axis aggravates acute lung injury
- Sonoclot’s usefulness in prediction of cardiopulmonary arrest prognosis: A proof of concept study
- Four drug metabolism-related subgroups of pancreatic adenocarcinoma in prognosis, immune infiltration, and gene mutation
- Decreased expression of miR-195 mediated by hypermethylation promotes osteosarcoma
- LMO3 promotes proliferation and metastasis of papillary thyroid carcinoma cells by regulating LIMK1-mediated cofilin and the β-catenin pathway
- Cx43 upregulation in HUVECs under stretch via TGF-β1 and cytoskeletal network
- Evaluation of menstrual irregularities after COVID-19 vaccination: Results of the MECOVAC survey
- Histopathologic findings on removed stomach after sleeve gastrectomy. Do they influence the outcome?
- Analysis of the expression and prognostic value of MT1-MMP, β1-integrin and YAP1 in glioma
- Optimal diagnosis of the skin cancer using a hybrid deep neural network and grasshopper optimization algorithm
- miR-223-3p alleviates TGF-β-induced epithelial-mesenchymal transition and extracellular matrix deposition by targeting SP3 in endometrial epithelial cells
- Clinical value of SIRT1 as a prognostic biomarker in esophageal squamous cell carcinoma, a systematic meta-analysis
- circ_0020123 promotes cell proliferation and migration in lung adenocarcinoma via PDZD8
- miR-22-5p regulates the self-renewal of spermatogonial stem cells by targeting EZH2
- hsa-miR-340-5p inhibits epithelial–mesenchymal transition in endometriosis by targeting MAP3K2 and inactivating MAPK/ERK signaling
- circ_0085296 inhibits the biological functions of trophoblast cells to promote the progression of preeclampsia via the miR-942-5p/THBS2 network
- TCD hemodynamics findings in the subacute phase of anterior circulation stroke patients treated with mechanical thrombectomy
- Development of a risk-stratification scoring system for predicting risk of breast cancer based on non-alcoholic fatty liver disease, non-alcoholic fatty pancreas disease, and uric acid
- Tollip promotes hepatocellular carcinoma progression via PI3K/AKT pathway
- circ_0062491 alleviates periodontitis via the miR-142-5p/IGF1 axis
- Human amniotic fluid as a source of stem cells
- lncRNA NONRATT013819.2 promotes transforming growth factor-β1-induced myofibroblastic transition of hepatic stellate cells by miR24-3p/lox
- NORAD modulates miR-30c-5p-LDHA to protect lung endothelial cells damage
- Idiopathic pulmonary fibrosis telemedicine management during COVID-19 outbreak
- Risk factors for adverse drug reactions associated with clopidogrel therapy
- Serum zinc associated with immunity and inflammatory markers in Covid-19
- The relationship between night shift work and breast cancer incidence: A systematic review and meta-analysis of observational studies
- LncRNA expression in idiopathic achalasia: New insight and preliminary exploration into pathogenesis
- Notoginsenoside R1 alleviates spinal cord injury through the miR-301a/KLF7 axis to activate Wnt/β-catenin pathway
- Moscatilin suppresses the inflammation from macrophages and T cells
- Zoledronate promotes ECM degradation and apoptosis via Wnt/β-catenin
- Epithelial-mesenchymal transition-related genes in coronary artery disease
- The effect evaluation of traditional vaginal surgery and transvaginal mesh surgery for severe pelvic organ prolapse: 5 years follow-up
- Repeated partial splenic artery embolization for hypersplenism improves platelet count
- Low expression of miR-27b in serum exosomes of non-small cell lung cancer facilitates its progression by affecting EGFR
- Exosomal hsa_circ_0000519 modulates the NSCLC cell growth and metastasis via miR-1258/RHOV axis
- miR-455-5p enhances 5-fluorouracil sensitivity in colorectal cancer cells by targeting PIK3R1 and DEPDC1
- The effect of tranexamic acid on the reduction of intraoperative and postoperative blood loss and thromboembolic risk in patients with hip fracture
- Isocitrate dehydrogenase 1 mutation in cholangiocarcinoma impairs tumor progression by sensitizing cells to ferroptosis
- Artemisinin protects against cerebral ischemia and reperfusion injury via inhibiting the NF-κB pathway
- A 16-gene signature associated with homologous recombination deficiency for prognosis prediction in patients with triple-negative breast cancer
- Lidocaine ameliorates chronic constriction injury-induced neuropathic pain through regulating M1/M2 microglia polarization
- MicroRNA 322-5p reduced neuronal inflammation via the TLR4/TRAF6/NF-κB axis in a rat epilepsy model
- miR-1273h-5p suppresses CXCL12 expression and inhibits gastric cancer cell invasion and metastasis
- Clinical characteristics of pneumonia patients of long course of illness infected with SARS-CoV-2
- circRNF20 aggravates the malignancy of retinoblastoma depending on the regulation of miR-132-3p/PAX6 axis
- Linezolid for resistant Gram-positive bacterial infections in children under 12 years: A meta-analysis
- Rack1 regulates pro-inflammatory cytokines by NF-κB in diabetic nephropathy
- Comprehensive analysis of molecular mechanism and a novel prognostic signature based on small nuclear RNA biomarkers in gastric cancer patients
- Smog and risk of maternal and fetal birth outcomes: A retrospective study in Baoding, China
- Let-7i-3p inhibits the cell cycle, proliferation, invasion, and migration of colorectal cancer cells via downregulating CCND1
- β2-Adrenergic receptor expression in subchondral bone of patients with varus knee osteoarthritis
- Possible impact of COVID-19 pandemic and lockdown on suicide behavior among patients in Southeast Serbia
- In vitro antimicrobial activity of ozonated oil in liposome eyedrop against multidrug-resistant bacteria
- Potential biomarkers for inflammatory response in acute lung injury
- A low serum uric acid concentration predicts a poor prognosis in adult patients with candidemia
- Antitumor activity of recombinant oncolytic vaccinia virus with human IL2
- ALKBH5 inhibits TNF-α-induced apoptosis of HUVECs through Bcl-2 pathway
- Risk prediction of cardiovascular disease using machine learning classifiers
- Value of ultrasonography parameters in diagnosing polycystic ovary syndrome
- Bioinformatics analysis reveals three key genes and four survival genes associated with youth-onset NSCLC
- Identification of autophagy-related biomarkers in patients with pulmonary arterial hypertension based on bioinformatics analysis
- Protective effects of glaucocalyxin A on the airway of asthmatic mice
- Overexpression of miR-100-5p inhibits papillary thyroid cancer progression via targeting FZD8
- Bioinformatics-based analysis of SUMOylation-related genes in hepatocellular carcinoma reveals a role of upregulated SAE1 in promoting cell proliferation
- Effectiveness and clinical benefits of new anti-diabetic drugs: A real life experience
- Identification of osteoporosis based on gene biomarkers using support vector machine
- Tanshinone IIA reverses oxaliplatin resistance in colorectal cancer through microRNA-30b-5p/AVEN axis
- miR-212-5p inhibits nasopharyngeal carcinoma progression by targeting METTL3
- Association of ST-T changes with all-cause mortality among patients with peripheral T-cell lymphomas
- LINC00665/miRNAs axis-mediated collagen type XI alpha 1 correlates with immune infiltration and malignant phenotypes in lung adenocarcinoma
- The perinatal factors that influence the excretion of fecal calprotectin in premature-born children
- Effect of femoral head necrosis cystic area on femoral head collapse and stress distribution in femoral head: A clinical and finite element study
- Does the use of 3D-printed cones give a chance to postpone the use of megaprostheses in patients with large bone defects in the knee joint?
- lncRNA HAGLR modulates myocardial ischemia–reperfusion injury in mice through regulating miR-133a-3p/MAPK1 axis
- Protective effect of ghrelin on intestinal I/R injury in rats
- In vivo knee kinematics of an innovative prosthesis design
- Relationship between the height of fibular head and the incidence and severity of knee osteoarthritis
- lncRNA WT1-AS attenuates hypoxia/ischemia-induced neuronal injury during cerebral ischemic stroke via miR-186-5p/XIAP axis
- Correlation of cardiac troponin T and APACHE III score with all-cause in-hospital mortality in critically ill patients with acute pulmonary embolism
- LncRNA LINC01857 reduces metastasis and angiogenesis in breast cancer cells via regulating miR-2052/CENPQ axis
- Endothelial cell-specific molecule 1 (ESM1) promoted by transcription factor SPI1 acts as an oncogene to modulate the malignant phenotype of endometrial cancer
- SELENBP1 inhibits progression of colorectal cancer by suppressing epithelial–mesenchymal transition
- Visfatin is negatively associated with coronary artery lesions in subjects with impaired fasting glucose
- Treatment and outcomes of mechanical complications of acute myocardial infarction during the Covid-19 era: A comparison with the pre-Covid-19 period. A systematic review and meta-analysis
- Neonatal stroke surveillance study protocol in the United Kingdom and Republic of Ireland
- Oncogenic role of TWF2 in human tumors: A pan-cancer analysis
- Mean corpuscular hemoglobin predicts the length of hospital stay independent of severity classification in patients with acute pancreatitis
- Association of gallstone and polymorphisms of UGT1A1*27 and UGT1A1*28 in patients with hepatitis B virus-related liver failure
- TGF-β1 upregulates Sar1a expression and induces procollagen-I secretion in hypertrophic scarring fibroblasts
- Antisense lncRNA PCNA-AS1 promotes esophageal squamous cell carcinoma progression through the miR-2467-3p/PCNA axis
- NK-cell dysfunction of acute myeloid leukemia in relation to the renin–angiotensin system and neurotransmitter genes
- The effect of dilution with glucose and prolonged injection time on dexamethasone-induced perineal irritation – A randomized controlled trial
- miR-146-5p restrains calcification of vascular smooth muscle cells by suppressing TRAF6
- Role of lncRNA MIAT/miR-361-3p/CCAR2 in prostate cancer cells
- lncRNA NORAD promotes lung cancer progression by competitively binding to miR-28-3p with E2F2
- Noninvasive diagnosis of AIH/PBC overlap syndrome based on prediction models
- lncRNA FAM230B is highly expressed in colorectal cancer and suppresses the maturation of miR-1182 to increase cell proliferation
- circ-LIMK1 regulates cisplatin resistance in lung adenocarcinoma by targeting miR-512-5p/HMGA1 axis
- LncRNA SNHG3 promoted cell proliferation, migration, and metastasis of esophageal squamous cell carcinoma via regulating miR-151a-3p/PFN2 axis
- Risk perception and affective state on work exhaustion in obstetrics during the COVID-19 pandemic
- lncRNA-AC130710/miR-129-5p/mGluR1 axis promote migration and invasion by activating PKCα-MAPK signal pathway in melanoma
- SNRPB promotes cell cycle progression in thyroid carcinoma via inhibiting p53
- Xylooligosaccharides and aerobic training regulate metabolism and behavior in rats with streptozotocin-induced type 1 diabetes
- Serpin family A member 1 is an oncogene in glioma and its translation is enhanced by NAD(P)H quinone dehydrogenase 1 through RNA-binding activity
- Silencing of CPSF7 inhibits the proliferation, migration, and invasion of lung adenocarcinoma cells by blocking the AKT/mTOR signaling pathway
- Ultrasound-guided lumbar plexus block versus transversus abdominis plane block for analgesia in children with hip dislocation: A double-blind, randomized trial
- Relationship of plasma MBP and 8-oxo-dG with brain damage in preterm
- Identification of a novel necroptosis-associated miRNA signature for predicting the prognosis in head and neck squamous cell carcinoma
- Delayed femoral vein ligation reduces operative time and blood loss during hip disarticulation in patients with extremity tumors
- The expression of ASAP3 and NOTCH3 and the clinicopathological characteristics of adult glioma patients
- Longitudinal analysis of factors related to Helicobacter pylori infection in Chinese adults
- HOXA10 enhances cell proliferation and suppresses apoptosis in esophageal cancer via activating p38/ERK signaling pathway
- Meta-analysis of early-life antibiotic use and allergic rhinitis
- Marital status and its correlation with age, race, and gender in prognosis of tonsil squamous cell carcinomas
- HPV16 E6E7 up-regulates KIF2A expression by activating JNK/c-Jun signal, is beneficial to migration and invasion of cervical cancer cells
- Amino acid profiles in the tissue and serum of patients with liver cancer
- Pain in critically ill COVID-19 patients: An Italian retrospective study
- Immunohistochemical distribution of Bcl-2 and p53 apoptotic markers in acetamiprid-induced nephrotoxicity
- Estradiol pretreatment in GnRH antagonist protocol for IVF/ICSI treatment
- Long non-coding RNAs LINC00689 inhibits the apoptosis of human nucleus pulposus cells via miR-3127-5p/ATG7 axis-mediated autophagy
- The relationship between oxygen therapy, drug therapy, and COVID-19 mortality
- Monitoring hypertensive disorders in pregnancy to prevent preeclampsia in pregnant women of advanced maternal age: Trial mimicking with retrospective data
- SETD1A promotes the proliferation and glycolysis of nasopharyngeal carcinoma cells by activating the PI3K/Akt pathway
- The role of Shunaoxin pills in the treatment of chronic cerebral hypoperfusion and its main pharmacodynamic components
- TET3 governs malignant behaviors and unfavorable prognosis of esophageal squamous cell carcinoma by activating the PI3K/AKT/GSK3β/β-catenin pathway
- Associations between morphokinetic parameters of temporary-arrest embryos and the clinical prognosis in FET cycles
- Long noncoding RNA WT1-AS regulates trophoblast proliferation, migration, and invasion via the microRNA-186-5p/CADM2 axis
- The incidence of bronchiectasis in chronic obstructive pulmonary disease
- Integrated bioinformatics analysis shows integrin alpha 3 is a prognostic biomarker for pancreatic cancer
- Inhibition of miR-21 improves pulmonary vascular responses in bronchopulmonary dysplasia by targeting the DDAH1/ADMA/NO pathway
- Comparison of hospitalized patients with severe pneumonia caused by COVID-19 and influenza A (H7N9 and H1N1): A retrospective study from a designated hospital
- lncRNA ZFAS1 promotes intervertebral disc degeneration by upregulating AAK1
- Pathological characteristics of liver injury induced by N,N-dimethylformamide: From humans to animal models
- lncRNA ELFN1-AS1 enhances the progression of colon cancer by targeting miR-4270 to upregulate AURKB
- DARS-AS1 modulates cell proliferation and migration of gastric cancer cells by regulating miR-330-3p/NAT10 axis
- Dezocine inhibits cell proliferation, migration, and invasion by targeting CRABP2 in ovarian cancer
- MGST1 alleviates the oxidative stress of trophoblast cells induced by hypoxia/reoxygenation and promotes cell proliferation, migration, and invasion by activating the PI3K/AKT/mTOR pathway
- Bifidobacterium lactis Probio-M8 ameliorated the symptoms of type 2 diabetes mellitus mice by changing ileum FXR-CYP7A1
- circRNA DENND1B inhibits tumorigenicity of clear cell renal cell carcinoma via miR-122-5p/TIMP2 axis
- EphA3 targeted by miR-3666 contributes to melanoma malignancy via activating ERK1/2 and p38 MAPK pathways
- Pacemakers and methylprednisolone pulse therapy in immune-related myocarditis concomitant with complete heart block
- miRNA-130a-3p targets sphingosine-1-phosphate receptor 1 to activate the microglial and astrocytes and to promote neural injury under the high glucose condition
- Review Articles
- Current management of cancer pain in Italy: Expert opinion paper
- Hearing loss and brain disorders: A review of multiple pathologies
- The rationale for using low-molecular weight heparin in the therapy of symptomatic COVID-19 patients
- Amyotrophic lateral sclerosis and delayed onset muscle soreness in light of the impaired blink and stretch reflexes – watch out for Piezo2
- Interleukin-35 in autoimmune dermatoses: Current concepts
- Recent discoveries in microbiota dysbiosis, cholangiocytic factors, and models for studying the pathogenesis of primary sclerosing cholangitis
- Advantages of ketamine in pediatric anesthesia
- Congenital adrenal hyperplasia. Role of dentist in early diagnosis
- Migraine management: Non-pharmacological points for patients and health care professionals
- Atherogenic index of plasma and coronary artery disease: A systematic review
- Physiological and modulatory role of thioredoxins in the cellular function
- Case Reports
- Intrauterine Bakri balloon tamponade plus cervical cerclage for the prevention and treatment of postpartum haemorrhage in late pregnancy complicated with acute aortic dissection: Case series
- A case of successful pembrolizumab monotherapy in a patient with advanced lung adenocarcinoma: Use of multiple biomarkers in combination for clinical practice
- Unusual neurological manifestations of bilateral medial medullary infarction: A case report
- Atypical symptoms of malignant hyperthermia: A rare causative mutation in the RYR1 gene
- A case report of dermatomyositis with the missed diagnosis of non-small cell lung cancer and concurrence of pulmonary tuberculosis
- A rare case of endometrial polyp complicated with uterine inversion: A case report and clinical management
- Spontaneous rupturing of splenic artery aneurysm: Another reason for fatal syncope and shock (Case report and literature review)
- Fungal infection mimicking COVID-19 infection – A case report
- Concurrent aspergillosis and cystic pulmonary metastases in a patient with tongue squamous cell carcinoma
- Paraganglioma-induced inverted takotsubo-like cardiomyopathy leading to cardiogenic shock successfully treated with extracorporeal membrane oxygenation
- Lineage switch from lymphoma to myeloid neoplasms: First case series from a single institution
- Trismus during tracheal extubation as a complication of general anaesthesia – A case report
- Simultaneous treatment of a pubovesical fistula and lymph node metastasis secondary to multimodal treatment for prostate cancer: Case report and review of the literature
- Two case reports of skin vasculitis following the COVID-19 immunization
- Ureteroiliac fistula after oncological surgery: Case report and review of the literature
- Synchronous triple primary malignant tumours in the bladder, prostate, and lung harbouring TP53 and MEK1 mutations accompanied with severe cardiovascular diseases: A case report
- Huge mucinous cystic neoplasms with adhesion to the left colon: A case report and literature review
- Commentary
- Commentary on “Clinicopathological features of programmed cell death-ligand 1 expression in patients with oral squamous cell carcinoma”
- Rapid Communication
- COVID-19 fear, post-traumatic stress, growth, and the role of resilience
- Erratum
- Erratum to “Tollip promotes hepatocellular carcinoma progression via PI3K/AKT pathway”
- Erratum to “Effect of femoral head necrosis cystic area on femoral head collapse and stress distribution in femoral head: A clinical and finite element study”
- Erratum to “lncRNA NORAD promotes lung cancer progression by competitively binding to miR-28-3p with E2F2”
- Retraction
- Expression and role of ABIN1 in sepsis: In vitro and in vivo studies
- Retraction to “miR-519d downregulates LEP expression to inhibit preeclampsia development”
- Special Issue Computational Intelligence Methodologies Meets Recurrent Cancers - Part II
- Usefulness of close surveillance for rectal cancer patients after neoadjuvant chemoradiotherapy


