Abstract
Blood–brain barrier participates in the pathological process of ischemic stroke. MicroRNA-29c-5p was highly expressed in clinical samples from patients with ischemic stroke. In this study, oxygen-glucose deprivation (OGD) treatment of astrocytes enhanced the permeability of brain microvascular endothelial cells (BMECs), and the miR-29c-5p expression was elevated in clinical samples from patients with ischemic stroke. For the function of miR-29c-5p in ischemic stroke, the miR-29c-5p knockdown decreased the permeability and the tight junction protein (TJP) destruction of BMECs and ameliorated the inflammation induced by OGD-treated astrocytes. Mechanistically, miR-29c-5p interacted with lipoprotein receptor-related protein 6 (LRP6) and negatively regulated the LRP6 expression in astrocytes. Moreover, the rescue assays indicated that the interference with miR-29c-5p ameliorated the TJP destruction of BMECs and inflammation caused by OGD-treated astrocytes by increasing the LRP6 expression. Together, miR-29c-5p knockdown decreased the high permeability and the TJP destruction of BMECs and ameliorated the inflammation induced by OGD-treated astrocytes by elevating LRP6 expression.
1 Introduction
Ischemic stroke is a central nervous system disease with high morbidity and mortality worldwide [1]. One of the pathophysiological features of ischemic stroke is the destruction of blood–brain barrier (BBB) [2]. BBB is formed by the tight junctions and adhesion of endothelial cells, and it acts as a functional barrier between the blood and the brain, which provides an optimal environment for neural network [3]. Considering the critical function of BBB dysfunction in the pathophysiology of ischemic stroke [4,5], maintaining BBB function and integrity are expected to alleviate brain injury after ischemic stroke. However, the mechanisms that regulate the BBB function after ischemic stroke have not been fully established.
Brain microvascular endothelial cells (BMECs) and astrocytes are major components of BBB [6]. In brain injury, BMECs and astrocytes support the formation of a neurovascular unit, a complex structural and functional unit that protects the BBB [7,8]. As the most abundant cell type in the central nervous system, astrocytes exert pivotal functions in maintaining normal brain function [9]. BMECs exert a critical role in BBB function through a highly selective barrier, in which tight junction proteins (TJPs) such as claudin-5, occludin, and zonula occluden-1 (ZO-1) are vital proteins regulating BBB integrity [10,11]. Under physiological and pathological conditions, BMECs–astrocyte interactions and signal transduction are critical for BBB integrity [12]. Thus, uncovering the underlying mechanism of BMECs–astrocyte interaction is essential for protecting BBB function after ischemic stroke.
MicroRNAs (miRNAs) are small noncoding RNAs that regulate mRNA degradation or translation by binding to the 3′-untranslated region (UTR) of target mRNAs [13]. MiRNAs participate in regulating various cellular behaviors, mainly including cell proliferation, differentiation, and metabolism [14,15]. Recently, increasing miRNAs have been confirmed to be abnormally expressed in ischemic stroke and to mediate the occurrence and development of ischemic stroke. For instance, Zuo et al. found that miR-132 alleviates brain injury by protecting the BBB in mice, suggesting that miR-132 might be a novel therapeutic target for BBB protection in ischemic stroke [16]; Zhang et al. indicated that miR-182 protects the integrity of the BBB during cerebral ischemia by repressing endothelial apoptosis, implying that miR-182 might be a potential target for the treatment of BBB disruption during cerebral ischemia [17]. Notably, another study confirmed that in an in vitro BBB model induced by the coculture of BMECs and astrocytes, miR-9-5p alleviates BBB injury and neuroinflammatory response and promotes neurological function recovery [18]. Thus, the discovery of novel miRNAs involved in the BMECs–astrocyte interaction is beneficial to better reveal the regulatory mechanism of BBB function after ischemic stroke.
The low-density lipoprotein receptor-related protein (LRP) signaling pathway participates in several processes, such as cerebral vascular remodeling and cerebral ischemia [19]. LRP6 is a single-span transmembrane protein and is involved in the regulation of various disease processes, including ischemic stroke [20]. As has been reported, the mutations in LRP6 are associated with the risk of ischemic stroke [21]; LRP6 protects the brain from ischemic injury, suggesting that LRP6 might provide a novel therapeutic approach for ischemic stroke [22]. In this study, the abnormal expressions of the miR-181 and miR-29 families in cerebral ischemia astrocytes were verified in the clinical samples from patients with ischemic stroke. Furthermore, the results authenticated that only miR-29c-5p was markedly overexpressed. Based on this finding, we selected miR-29c-5p as the mainly studied miRNA. Meanwhile, we found the binding sites between miR-29c-5p and LRP6 through TargetScan and Metascape databases. On this basis, we used various molecular techniques to conduct in-depth studies on its role and mechanism in the BBB after ischemic stroke, aiming to provide novel potential biomarkers for the clinical treatment of ischemic stroke.
2 Materials and methods
2.1 Clinical samples
Twenty patients with ischemic stroke and the matched healthy controls were included in this research. All of them were diagnosed based on a detailed stroke history and a physical examination using a professional clinical care provider. After obtaining informed consent from the patient or family members, the blood samples from the patients were collected for subsequent research. This study was approved by the Ethics Committee of Haian Hospital of Traditional Chinese Medicine.
2.2 Quantitative real-time PCR (qRT-PCR)
The expressions of miR-29c-5p, miR-29a-5p, miR-181-5p, and LRP6 in the blood samples of patients with ischemic stroke, and the LRP6 expression in astrocytes were determined using qRT-PCR. In brief, Trizol reagent (ThermoFisher Scientific, WA, USA) was used to extract the total RNAs, and the concentrations of RNAs were quantified by a NanoDrop spectrophotometer (Nanodrop Technologies, USA). To measure the LRP6 expression, High-Capacity cDNA Reverse Transcription Kit (Thermo Fisher Scientific) was used. To assess the expressions of miR-29c-5p, miR-29a-5p, and miR-181-5p, TaqMan MicroRNA Reverse Transcription Kit (Thermo Fisher Scientific) was used. Subsequently, the real-time PCR was conducted on a 7500 Real-Time PCR system (Applied Biosystems, USA) with TaqMan Universal PCR Master Mix (Thermo Fisher Scientific). The expressions of miR-29c-5p, miR-29a-5p, and miR-181-5p were normalized to U6, and the LRP6 expression was normalized to GAPDH. The relative expression of the above molecules was determined by the 2−ΔΔCT method. All the primer sequences are exhibited in Table 1.
The sequences of all primers used in qRT-PCR
| Gene name | Primer sequence (5′–3′) |
|---|---|
| miR-29c-5p | Forward: TAGTAGTGGTTGTTTGTTTTTTTGA |
| Reverse: CCACTCTACTAAAAACTCCATCTCC | |
| miR-29a-5p | Forward: GCGGCGGACTGATTTCTTTTGGT |
| Reverse: ATCCAGTGCAGGGTCCGAGG | |
| miR-181-5p | Forward: ACACTCCAGCTGGGAACATTCAACGCTGTCGG |
| Reverse: TGGTGTCGTGGAGTCGA | |
| LRP6 | Forward: TCAACCCAGAGCTATTGCCTT |
| Reverse: TAACCACTGCCTGCCGATTT | |
| U6 | Forward: GCTTCGGCAGCACATATACTAAAAT |
| Reverse: CGCTTCACGAATTTGCGTGTCAT | |
| GAPDH | Forward: CTCTGACTTCAACAGCGAC |
| Reverse: CGTTGTCATACCAGGAAATGAG |
2.3 Isolation and identification of primary astrocytes
Primary astrocytes were obtained from neonatal 1-day-old C57BL/6 mice [23,24]. In detail, the cortex was isolated from the mouse brain, and the meninges were removed. Subsequently, the cortex was digested at 37°C with 0.25 mg/mL trypsin and 0.1 mg/mL DNase for 20 min. The resuspended cells were collected and placed in a growth medium supplemented with high-glucose Dulbecco’s Modified Eagle’s Medium (DMEM, Thermo Fisher Scientific) with 10% fetal bovine serum (FBS, Thermo Fisher Scientific) and 1% penicillin–streptomycin, and then placed in a polylysine-coated flask and grown at 37°C, in the presence of 5% CO2. The plastic flask was then placed on a shaker and gently shaken at 260 rpm to separate the microglia. The remaining adherent astrocytes were identified using immunofluorescence staining, and glial fibrillary acidic protein (GFAP) was used as a molecular marker, and more than 95% of the cells were positive for GFAP.
2.4 Cell culture and different treatments
Primary BMECs (5 × 105 cells) were purchased from Procell (Wuhan, China). The cells were put in 90% high-glucose DMEM containing 10% FBS and cultured at 37°C, in the presence of 5% CO2.
After washing the astrocytes twice with PBS, the cells were placed in oxygen-glucose deprivation (OGD) medium (glucose-free and serum-free DMEM with 10 μM hemin) and cultured in hypoxia (5% CO2 + 0.4% O2 + 95% N2) at 37°C for 4 h.
To initiate the coculture system of BMECs and astrocytes, primary astrocytes isolated from normal mice were treated with OGD for 3 h. Subsequently, BMECs were transferred to a medium containing primary astrocytes for coculture for 24 h [25].
2.5 Transepithelial electrical resistance (TEER) analysis
A Millicell-ERS instrument (Millipore, MA, USA) was used to detect the TEER values of BMECs. In detail, the isolated primary astrocytes (1 × 104 cells) were grown on six-well plates for 2 days. Then, the coculture inserts were placed at room temperature for 25 min. Subsequently, we detected the values of TEER immediately after changing the medium. Before calculating the final resistance, the background resistance was subtracted and the TEER value was expressed as Ω cm2.
2.6 Analysis of the penetration rate of sodium fluorescein (NaF)
To assess the barrier formation, we measured the exclusion of NaF daily for 4 days. In brief, we added 5 µM NaF (Sigma-Aldrich, Buchs, Switzerland) to the apical chamber and then added 1 mL standard medium to the basal chamber. After incubating for 2 h, we measured the NaF in basolateral samples by a microplate reader (Berthold Technologies GmbH, excitation 485 nm, emission 528 nm).
2.7 Cell transfection
miR-29a-5p inhibitor, negative control (NC)-inhibitor, miR-29a-5p mimic, NC-mimic, si-LRP6, and si-NC were synthesized from GenePharma (Shanghai, China).
The cell transfection was conducted using Lipofectamine 2000 (Thermo Fisher Scientific). In particular, the astrocytes (3 × 105 cells) were grown in six-well plates for 24 h. Subsequently, the miR-29a-5p inhibitor, miR-29a-5p mimic, si-LRP6, and their corresponding controls were transfected into astrocytes using Lipofectamine 2000. Forty-eight hours after transfection, we collected the astrocytes for subsequent studies.
2.8 Western blot assay
BMECs and primary astrocytes with different treatments were harvested and radioimmunoprecipitation assay (RIPA) lysis buffer (Thermo Fisher Scientific) was used to isolate the total proteins. The same amount of protein samples were separated using 10% sodium dodecyl sulfonate-polyacrylamide gel electrophoresis and transferred onto membranes (Millipore, Massachusetts, USA). Then, the membranes were incubated with 5% skim milk for 1 h. The membranes were further incubated with anti-GFAP (Abcam, 1:10,000 dilution, ab7260), anti-GLP-1R (Abcam, 1:1,000 dilution, ab218532), anti-claudin-5 (Abcam, 1:1,000 dilution, ab131259), anti-occludin (Abcam, 1:1,000 dilution, ab216327), anti-ZO-1 (Abcam, 1:1,000 dilution, ab276131), anti-VEGF-A (Abcam, 1:1,000 dilution, ab214424), anti-MMP-9 (Abcam, 1:1,000 dilution, ab76003) and anti-β-actin (Abcam, 1 µg/mL, ab8226) at 4°C overnight. Then, the membranes were further incubated with the secondary antibodies (Abcam, 1:2,000 dilution, ab205718). Ultimately, the signal of protein level was visualized by an enhanced chemiluminescent reagent (Thermo Fisher Scientific), and the images were analyzed by using Image-Pro Plus 5.1 Image Analysis Software (Media Cybernetics, MD, USA).
2.9 Lactate dehydrogenase (LDH) release assay
Referring to the standard procedure from reagent manufacturers, LDH release assay was performed using an LDH Cytotoxicity Assay Kit (Abcam, Cambridge, UK). BMECs with different treatments (3 × 103 cells) were put in 96-well plates and cultured for 24 h. The cells were lysed using 0.2% Triton X-100 (Solarbio, Beijing, China). After centrifugation, the supernatants were collected and coincubated with LDH reaction solution. Subsequently, a microplate reader (Bio-Rad Co., Hercules, CA, USA) was conducted to detect the optical density (OD) value at 490 nm. The content of LDH in cell lysates was determined to assess the cellular injury.
2.10 Immunofluorescence staining assay
Based on the previously reported methods [26], the immunofluorescence staining was conducted to assess the expressions of TJPs claudin5, occludin, and ZO-1. The primary antibodies were anti-claudin5 (Abcam, Assay dependent, ab15106), anti-occludin (Abcam, 1:100 dilution, ab216327), anti-ZO-1 (Abcam, 1:100 dilution, ab221547), anti-VEGFA (Abcam, 1 µg/mL, ab39250), and anti-MMP-9 (Abcam, 1:500 dilution, ab76003). The secondary antibodies were Alexa Flur 488 mouse anti-rabbit IgG and tetraethyl rhodamine isothiocyanate goat anti-rabbit IgG. The nuclei were stained using 4′,6-Diamidino-2-phenylindole staining solution (Sigma-Aldrich). Ultimately, Vectra® Polaris™ Automated Quantitative Pathology Imaging System (PerkinElmer, USA) was used to analyze all images.
2.11 Enzyme-linked immunosorbent assay (ELISA)
The contents of inflammatory cytokines interleukin-1β (IL-1β), interleukin-6 (IL-6), Tumor Necrosis Factor Alpha (TNF-α), and Transforming growth factor β (TGF-β) in the cell culture supernatant of astrocytes were quantified by using ELISA. Briefly, astrocytes (3 × 103 cells) were put in 96-well plates. The ELISA kit (ThermoFisher Scientific) was conducted to detect the concentrations of IL-1β, IL-6, TNF-α, and TGF-β in the cell culture supernatant of astrocytes based on the instructions of the manufacturer. The OD at 450 nm was measured.
2.12 Dual-luciferase reporter gene assay
Before the cell transfection, the astrocytes were grown in six-well plates and cultured to 80% fusion. The pmirGLO reporter vector containing a wild type (WT) or mutant type (Mut) miR-29a-5p binding sites in the 3′-UTR of LRP6, and named LRP6 WT or LRP6 Mut, was synthesized by Ribobio (Guangdong, China). miR-29a-5p mimic and the above recombinant vector were cotransfected into astrocytes using Lipofectamine 2000. Forty-eight hours after the transfection, the dual-luciferase reporter assay system (Thermo Fisher Scientific) was used to measure the relative luciferase activity.
2.13 Statistical analysis
All data were presented as the mean ± standard deviation. When the differences between the control and experimental groups were assessed, an unpaired Student’s t-test was carried out; when the differences among more than two groups were assessed, one-way analysis of variance (ANOVA) followed by Tukey’s post-test was conducted. P < 0.05 was considered significant.
-
Ethics approval and consent to participate: The experimental protocol was established, according to the ethical guidelines of the Helsinki Declaration and was approved by the Ethics Committee of Haian Hospital of Traditional Chinese Medicine.
3 Results
3.1 OGD treatment of astrocytes increases the permeability of BMECs
BBB is essential for maintaining normal brain activity and is composed of BMECs arranged in blood vessels, and BMECs form a barrier to regulate the transportation of cells between the blood and the brain [27]. Moreover, the coculture of BMECs and astrocytes is commonly used as the in vitro model of BBB [18]. In this study, we isolated primary astrocytes from mice and identified them by immunofluorescence staining assay. GFAP was used as a molecular marker, and more than 95% of the cells were positive for GFAP (Figure 1a). Subsequently, the primary astrocytes treated with OGD were cocultured with BMECs. TEER analysis revealed that compared to the control group, OGD treatment increased the TEER of BMECs (Figure 1b). Similarly, compared to the control group, OGD treatment enhanced the ability of NaF to penetrate BMECs (Figure 1c). In general, OGD treatment of astrocytes enhanced the permeability of BMECs.

Influence of the OGD treatment of astrocytes on the permeability of BMECs. The primary astrocytes were isolated, and the primary astrocytes were treated with OGD for 3 h and then cocultured with primary brain microvascular epithelial cells (BMECs) for 24 h. (a) An immunofluorescence staining assay was performed to verify the isolated primary astrocytes (scale bar: 100 µm). (b) The TEER value of BMECs was determined using the Millicell-ERS instrument (Millipore, MA, USA). (c) Analysis of the penetration rate of NaF. OGD: oxygen-glucose deprivation, TEER: transepithelial electrical resistance, and NaF: sodium fluorescein. Data are presented as an average of three independent assays. **P < 0.01, ***P < 0.001 vs control.
3.2 Low expression of miR-29c-5p reduces the high permeability of BMECs caused by OGD-treated astrocytes
We further detected the expressions of miR-29c-5p, miR-29a-5p, and miR-181-5p in the blood samples of patients with ischemic stroke, and the results indicated that only the miR-29c-5p was elevated, suggesting that miR-29c-5p might be related to the occurrence of ischemic stroke (Figure S1). Thus, miR-29c-5p was selected as the main miRNA for our subsequent studies.
Furthermore, we sought to explore whether miR-29c-5p mediated the high permeability of BMECs caused by OGD-treated astrocytes. Astrocytes transfected with miR-29c-5p inhibitor or NC-inhibitor were treated with OGD and then cocultured with BMECs. We detected the protein levels of astrocyte activation markers GFAP and glucagon-like peptide-1 receptor (GLP-1R) and found that compared to the NC-inhibitor group, the GFAP and GLP-1R protein levels were decreased in the miR-29c-5p inhibitor group (Figure 2a). Meanwhile, the TEER value in the miR-29c-5p inhibitor group was much lower than that in the NC-inhibitor group (Figure 2b). Similar to this finding, the ability of NaF to penetrate BMECs was weakened in the miR-29c-5p inhibitor group compared to the NC-inhibitor group (Figure 2c). Cell injury can be assessed through the LDH release assay [28]. As shown in Figure 2d, compared with the NC-inhibitor group, there was no remarkable change in the LDH release of BMECs in the miR-29c-5p inhibitor group. Together, the above results clarified that the miR-29c-5p knockdown decreased the high permeability of BMECs induced by OGD-treated astrocytes.

Effect of miR-29c-5p on the high permeability of BMECs caused by OGD-treated astrocytes. Astrocytes transfected with miR-29c-5p inhibitor or NC-inhibitor were treated with OGD for 3 h and then cocultured with BMECs for 24 h. (a) Western blot was performed to analyze the protein levels of astrocyte activation markers GFAP and GLP-1R. (b) Analysis of the TEER value of BMECs. (c) Detection of the ability of NaF to penetrate BMECs. (d) LDH release assay was performed to assess the injury of BMECs. NC: negative control, GLP-1R: glucagon-like peptide-1 receptor, and LDH: lactate dehydrogenase. Data are presented as an average of three independent assays. *P < 0.05, ***P < 0.001 vs NC-inhibitor.
3.3 miR-29c-5p knockdown ameliorates TJP destruction of BMECs induced by OGD-treated astrocytes
Earlier studies indicate that one of the biochemical features of BBB injury is the decreased expression of TJPs, mainly including claudin-5, occludin, and ZO-1 [2,29]. Astrocytes transfected with miR-29c-5p inhibitor or NC-inhibitor were treated with OGD and then cocultured with BMECs. Western blot analysis authenticated that claudin-5, occludin, and ZO-1 were upregulated after the miR-29c-5p knockdown (Figure 3a). Immunofluorescence staining assay further confirmed that claudin-5, occludin, and ZO-1 expressions were increased in the miR-29c-5p inhibitor group (Figure 3b). In general, the interference with miR-29c-5p relieved the TJP destruction of BMECs caused by OGD-treated astrocytes.
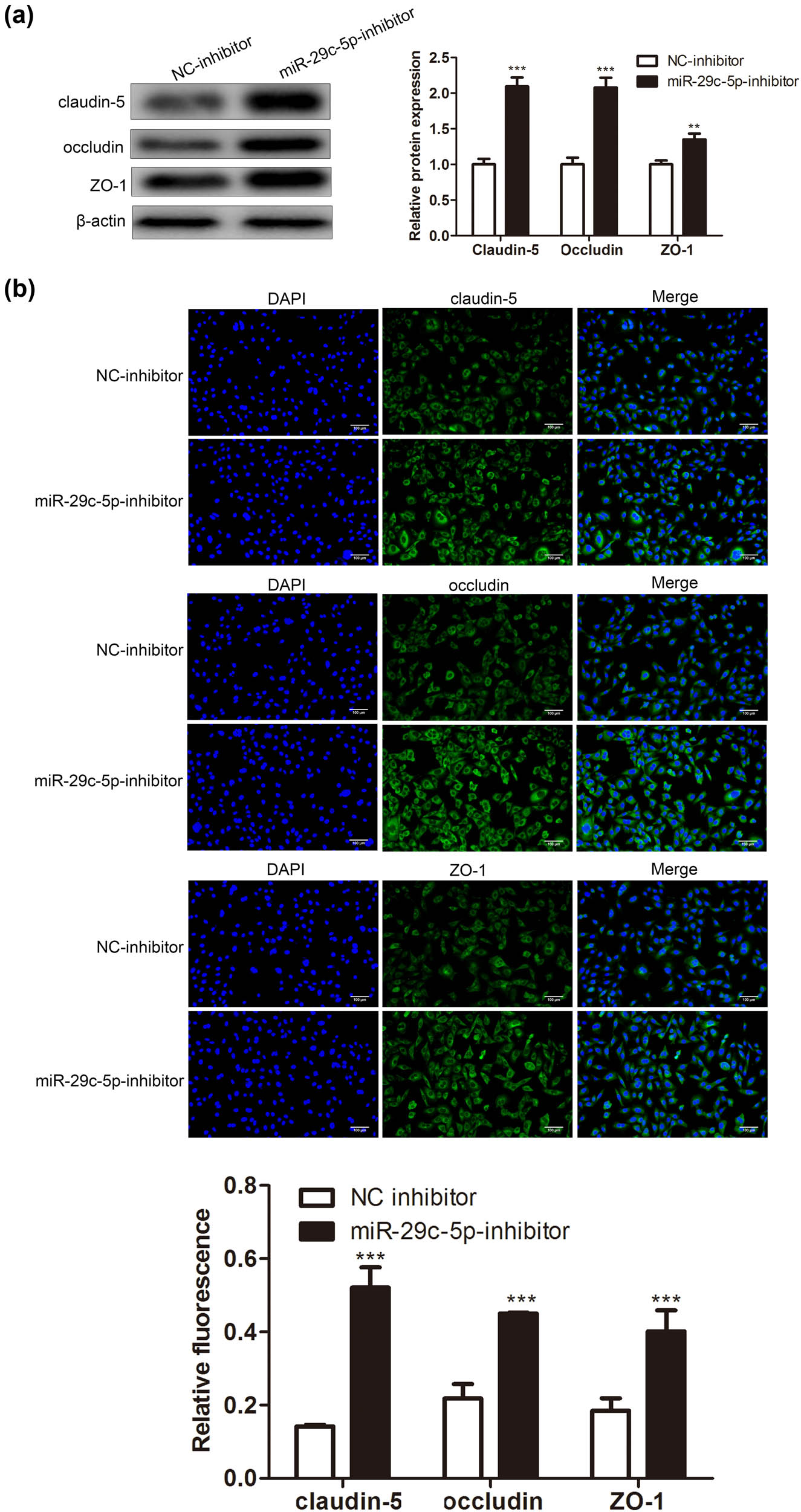
Influence of miR-29c-5p on the TJP destruction of BMECs caused by OGD-treated astrocytes. Astrocytes transfected with miR-29c-5p inhibitor or NC-inhibitor were treated with OGD for 3 h, and the cells were cocultured with BMECs for 24 h. (a) The protein levels of TJPs claudin-5, occludin, and ZO-1 were determined using Western blot. (b) Immunofluorescence staining assay was applied to quantify the claudin-5, occludin, and ZO-1 expressions (scale bar: 100 µm). Data are presented as an average of three independent assays. **P < 0.01, ***P < 0.001 vs NC-inhibitor.
3.4 Interference with miR-29c-5p relieves inflammation induced by OGD-treated astrocytes
Based on the above findings, we attempted to clarify whether miR-29c-5p mediated the inflammation induced by OGD-treated astrocytes. As exhibited in Figure 4a, the miR-29c-5p knockdown reduced the concentrations of IL-1β, IL-6, TNF-α, and TGF-β. Inflammatory factors such as vascular endothelial growth factor (VEGF-A) and matrix metalloproteinase-9 (MMP-9) directly or indirectly aggravate BBB [30,31]. As shown in Figure 4b, compared with the NC-inhibitor group, the protein levels of VEGF-A and MMP-9 were decreased in the miR-29c-5p inhibitor group. Furthermore, the immunofluorescence results showed the same trend (Figure 4c). Together, the miR-29c-5p knockdown reduced the inflammation caused by OGD-treated astrocytes.

Effect of miR-29c-5p on the inflammation caused by OGD-treated astrocytes. Astrocytes transfected with miR-29c-5p inhibitor or NC-inhibitor were treated with OGD for 3 h. (a) ELISA was performed to test the concentrations of inflammatory cytokines IL-1β, IL-6, TNF-α, and TGF-β in cell culture supernatant of astrocytes. (b) The protein levels of inflammatory factors VEGF-A and MMP-9 were tested using Western blot. (c) An immunofluorescence assay was performed to assess the expressions of VEGF-A and MMP-9 (scale bar: 100 µm). Data are presented as an average of three independent assays. **P < 0.01, ***P < 0.001 vs NC-inhibitor.
3.5 MiR-29c-5p targets LRP6
Recent studies have confirmed that the activation of the Wnt/β-catenin signaling by protective astrocytes repairs BBB injury [32], and miRNAs exert regulatory functions by targeting the 3′-UTR of mRNAs [33]. Thus, we applied bioinformatic databases (TargetScan and Metascape) to predict the possible downstream regulatory targets of miR-29c-5p and screened out the targets that participated in the regulation of the Wnt pathway. The results showed that there were binding sites between miR-29c-5p and LRP6 (Figure 5a and b). To verify this combination, we performed the dual-luciferase reporter gene assay, and the results confirmed that the transfection of miR-29c-5p mimic reduced the relative luciferase activity of LRP6 WT, and had no obvious changes on the relative luciferase activity of LRP6 MUT, implying that there was an interaction between miR-29c-5p and LRP6 (Figure 5c). Subsequently, we transfected miR-29c-5p mimic into astrocytes to investigate the regulation of miR-29c-5p on the LRP6 expression. The results authenticated that the transfection of miR-29c-5p mimic decreased the LRP6 expression (Figure 5d). Meanwhile, the LRP6 expression was evaluated, and the data confirmed that LRP6 was lowly expressed in the blood samples of patients with ischemic stroke (Figure 5e). To sum up, miR-29c-5p bound to LRP6 and negatively regulated the expression of LRP6 in astrocytes.

Verification of the interaction between miR-29c-5p and LRP6: (a and b) Bioinformatic databases, TargetScan and Metascape, were applied to predict the possible downstream regulatory targets of miR-29c-5p and screen out the targets that participated in regulating the Wnt pathway. (c) The binding of miR-29c-5p to LRP6 was proved by dual-luciferase reporter gene assay. (d) miR-29c-5p mimic or NC-mimic was transfected into astrocytes. QRT-PCR was carried out to quantify the LRP6 expression. (e) A total of 20 patients with ischemic stroke and 20 matched healthy controls were included, and the blood samples were isolated from them. The expression of LRP6 was analyzed by qRT-PCR. Data are presented as an average of three independent assays. ***P < 0.001 vs NC mimic.
3.6 Rescue assay investigates the function of the miR-29c-5p/LRP6 axis in the TJP destruction of BMECs and inflammation caused by OGD-treated astrocytes
We further investigated whether miR-29c-5p regulated the inflammation and TJP destruction of BMECs induced by OGD-treated astrocytes via LRP6. Astrocytes transfected with miR-29c-5p inhibitor and/or si-LRP6 were treated with OGD. As shown in Figure 6a, the interference with miR-29c-5p reduced the concentrations of IL-1β, IL-6, TNF-α, and TGF-β, and this reduction was compensated by the interference with LRP6. Similarly, the miR-29c-5p knockdown downregulated the protein levels of VEGF-A and MMP-9, whereas the LRP6 knockdown partially reversed this trend (Figure 6b). Furthermore, astrocytes transfected with miR-29c-5p inhibitor and si-LRP6 were treated with OGD and then cocultured with BMECs. From the results of Western blot, we found that the transfection of miR-29c-5p inhibitor downregulated the GFAP and GLP-1R protein levels, and this downregulation was partially reversed by the transfection of si-LRP6 (Figure 6c). Moreover, the interference with miR-29c-5p increased the protein levels of claudin-5, occludin, and ZO-1, whereas the interference with LRP6 partially reversed this increase (Figure 6d). Overall, the interference with miR-29c-5p ameliorated the inflammation and TJP destruction of BMECs induced by OGD-treated astrocytes by increasing LRP6.

Verification of the regulatory function of the miR-29c-5p/LRP6 axis in the TJP destruction of BMECs and inflammation caused by OGD-treated astrocytes: (a) Astrocytes transfected with miR-29c-5p inhibitor and si-LRP6 were treated with OGD for 3 h. The concentrations of IL-1β, IL-6, TNF-α, and TGF-β in the cell culture supernatant of astrocytes were measured by ELISA. (b) Western blot was carried out to test the protein levels of VEGF-A and MMP-9. (c) Astrocytes transfected with miR-29c-5p inhibitor and si-LRP6 were treated with OGD for 3 h and then cocultured with BMECs for 24 h. The protein levels of GFAP and GLP-1R were quantified using Western blot. (d) Analysis of the claudin-5, occludin, and ZO-1 protein levels using Western blot. Data are presented as an average of three independent assays. ***P < 0.001 vs NC-inhibitor + Si-NC. # P < 0.05, ## P < 0.01, ### P < 0.001 vs miR-29c-5p inhibitor + si-NC.
4 Discussion
The previous study demonstrates that the miR-181 and miR-29 families are abnormally expressed in cerebral ischemia astrocytes [34]. Based on this, this study further verified the expressions of miR-181 family and miR-29 family in clinical blood samples from patients with ischemic stroke and authenticated that only miR-29c-5p was remarkably overexpressed. Thus, we focused on the mechanism of miR-29c-5p in ischemic stroke in the current study. Here, we demonstrated that the interference with miR-29c-5p decreased the high permeability and the TJP destruction of BMECs and the inflammation induced by OGD-treated astrocytes. Mechanism research results confirmed that miR-29c-5p interacted with LRP6 and negatively regulated LRP6 expression in astrocytes. Moreover, the rescue assays indicated that the interference with miR-29c-5p ameliorated the TJP destruction of BMECs and inflammation caused by OGD-treated astrocytes by upregulating LRP6 expression. Thus, our study might provide a novel regulatory axis for ischemic stroke: miR-29c-5p/LRP6.
Accumulated evidence suggest that BBB dysfunction is the pathogenesis of many neurological diseases, including ischemic stroke [35]. Various factors contribute to BBB dysfunction, including the major components of BBB: BMECs and astrocytes [6,36]. As reported, an in vitro BBB model composed of BMECs and primary culture of astrocytes has been used to elucidate the mechanisms of BBB and to develop novel therapeutic strategies [12]. Similarly, we obtained primary astrocytes from normal C57BL/6 mice and established a coculture system of BMECs and OGD-treated astrocytes. Our study confirmed that OGD treatment of astrocytes enhanced the permeability of BMECs. Based on this finding, we would continue investigating the potential mechanism of BMECs–astrocyte interaction under the pathological condition of BBB dysfunction after ischemic stroke.
Increasing studies illustrate that those different mechanisms, including miRNAs, are related to the pathogenesis of BBB dysfunction after ischemic stroke. For instance, Chen et al. identified a double-negative feedback loop: let-7i/TGF-βR1 in ischemic stroke, providing a potential therapeutic target for ischemic stroke [37]; Ma et al. indicated that the deletion of miR-15a/16-1 gene in endothelial cells represses BBB dysfunction after ischemic stroke, suggesting that miR-15a/16-1 mediates BBB dysfunction to alleviate ischemic stroke [38]. Similarly, our study illustrated that miR-29c-5p was elevated in clinical blood samples from patients with ischemic stroke, implying that miR-29c-5p might be related to the occurrence and development of ischemic stroke. Our functional study further clarified that the miR-29c-5p knockdown reduced the high permeability and the TJP destruction of BMECs and the inflammation induced by OGD-treated astrocytes.
As an essential member of the LRP family, LRP6 has been proved to exert an important regulatory function in the occurrence of ischemic stroke [21,39]. Interestingly, our research found that there were binding sites between miR-29c-5p and LRP6 through TargetScan and Metascape databases. Based on these findings, we further confirmed that miR-29c-5p bound to LRP6, and the expression of LRP6 in astrocytes was negatively regulated by miR-29c-5p, and LRP6 was lowly expressed in clinical blood samples from patients with ischemic stroke. Meanwhile, the rescue assays illustrated that the interference with miR-29c-5p ameliorated the TJP destruction of BMECs and inflammation caused by OGD-treated astrocytes by elevating LRP6.
In summary, our results provided evidence that miR-29c-5p improved the TJP destruction of BMECs and inflammation caused by OGD-treated astrocytes by upregulating LRP6. This study might provide a novel regulatory axis for ischemic stroke: miR-29c-5p/LRP6. Besides, there might also be other targets for miR-29C-5p, and we would continue to explore in-depth to further enrich the content of this study.
Acknowledgments
Not applicable.
-
Funding information: This work was supported by the 2020 Nantong Science and technology plan project (MSZ20084).
-
Author contributions: Yueqin Ding conceived and designed the study. Qijun Dai, JianSun, and Tianyi Dai performed the literature search and data extraction. Peipei Jiang, Qin Xu, and Pei Xu drafted the manuscript. All authors read and approved the final manuscript.
-
Competing interests: The authors declare that they have no conflicts of interest.
-
Consent for publication: The authors agree to the publication of the article in the journal.
-
Data availability statement: The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
[1] Qin C, Zhou LQ, Ma XT, Hu ZW, Yang S, Chen M, et al. Dual functions of microglia in ischemic stroke. Neurosci Bull. 2019;35(5):921–33.10.1007/s12264-019-00388-3Search in Google Scholar PubMed PubMed Central
[2] Abdullahi W, Tripathi D, Ronaldson PT. Blood-brain barrier dysfunction in ischemic stroke: targeting tight junctions and transporters for vascular protection. Am J Physiol Cell Physiol. 2018;315(3):C343–56.10.1152/ajpcell.00095.2018Search in Google Scholar PubMed PubMed Central
[3] Schoknecht K, David Y, Heinemann U. The blood-brain barrier-gatekeeper to neuronal homeostasis: clinical implications in the setting of stroke. SemCell Developmental Biol. 2015;38:35–42.10.1016/j.semcdb.2014.10.004Search in Google Scholar PubMed
[4] Shah K, Abbruscato T. The role of blood-brain barrier transporters in pathophysiology and pharmacotherapy of stroke. Curr Pharm Des. 2014;20(10):1510–22.10.2174/13816128113199990465Search in Google Scholar PubMed
[5] Jiang X, Andjelkovic AV, Zhu L, Yang T, Bennett MVL, Chen J, et al. Blood-brain barrier dysfunction and recovery after ischemic stroke. Prog Neurobiol. 2018;163–164:144–71.10.1016/j.pneurobio.2017.10.001Search in Google Scholar PubMed PubMed Central
[6] Srivastava K, Shao B, Bayraktutan U. PKC-β exacerbates in vitro brain barrier damage in hyperglycemic settings via regulation of RhoA/Rho-kinase/MLC2 pathway. J Cereb Blood Flow Metabolism: Off J Int Soc Cereb Blood Flow Metab. 2013;33(12):1928–36.10.1038/jcbfm.2013.151Search in Google Scholar PubMed PubMed Central
[7] Liu LR, Liu JC, Bao JS, Bai QQ, Wang GQ. Interaction of microglia and astrocytes in the neurovascular unit. Front immunology. 2020;11:1024.10.3389/fimmu.2020.01024Search in Google Scholar PubMed PubMed Central
[8] Lok J, Wang XS, Xing CH, Maki TK, Wu LM, Guo SZ, et al. Targeting the neurovascular unit in brain trauma. CNS Neurosci Therapeutics. 2015;21(4):304–8.10.1111/cns.12359Search in Google Scholar PubMed PubMed Central
[9] Liu Z, Chopp M. Astrocytes, therapeutic targets for neuroprotection and neurorestoration in ischemic stroke. Prog Neurobiol. 2016;144:103–20.10.1016/j.pneurobio.2015.09.008Search in Google Scholar PubMed PubMed Central
[10] Strazielle N, Ghersi-Egea JF. Physiology of blood-brain interfaces in relation to brain disposition of small compounds and macromolecules. Mol Pharmaceutics. 2013;10(5):1473–91.10.1021/mp300518eSearch in Google Scholar PubMed
[11] Pan Q, He C, Liu H, Liao X, Dai B, Chen Y, et al. Microvascular endothelial cells-derived microvesicles imply in ischemic stroke by modulating astrocyte and blood brain barrier function and cerebral blood flow. Mol Brain. 2016;9(1):63.10.1186/s13041-016-0243-1Search in Google Scholar PubMed PubMed Central
[12] Li C, Wang X, Cheng F, Du X, Yan J, Zhai C, et al. Geniposide protects against hypoxia/reperfusion-induced blood-brain barrier impairment by increasing tight junction protein expression and decreasing inflammation, oxidative stress, and apoptosis in an in vitro system. Eur J Pharmacology. 2019;854:224–31.10.1016/j.ejphar.2019.04.021Search in Google Scholar PubMed
[13] Saliminejad K, Khorram Khorshid HR, Soleymani Fard S, Ghaffari SH. An overview of microRNAs: Biology, functions, therapeutics, and analysis methods. J Cell Physiol. 2019;234(5):5451–65.10.1002/jcp.27486Search in Google Scholar PubMed
[14] Wang F, Liang R, Tandon N, Matthews ER, Shrestha S, Yang J, et al. H19X-encoded miR-424(322)/-503 cluster: emerging roles in cell differentiation, proliferation, plasticity and metabolism. Cell Mol Life Sciences: CMLS. 2019;76(5):903–20.10.1007/s00018-018-2971-0Search in Google Scholar PubMed PubMed Central
[15] Engin AB. MicroRNA and adipogenesis. Adv Exp Med Biol. 2017;960:489–509.10.1007/978-3-319-48382-5_21Search in Google Scholar PubMed
[16] Zuo X, Lu J, Manaenko A, Qi X, Tang J, Mei Q, et al. MicroRNA-132 attenuates cerebral injury by protecting blood-brain-barrier in MCAO mice. Exp Neurol. 2019;316:12–9.10.1016/j.expneurol.2019.03.017Search in Google Scholar PubMed
[17] Zhang T, Tian C, Wu J, Zhang Y, Wang J, Kong Q, et al. MicroRNA-182 exacerbates blood-brain barrier (BBB) disruption by downregulating the mTOR/FOXO1 pathway in cerebral ischemia. FASEB Journal: Off Publ Federation Am Societies Exp Biol. 2020;34(10):13762–75.10.1096/fj.201903092RSearch in Google Scholar PubMed
[18] Wu J, He J, Tian X, Luo Y, Zhong J, Zhang H, et al. microRNA-9-5p alleviates blood-brain barrier damage and neuroinflammation after traumatic brain injury. J neurochemistry. 2020;153(6):710–26.10.1111/jnc.14963Search in Google Scholar PubMed PubMed Central
[19] Chang L, Hu L, Wei C, Zhang H, Liu S. Chinese medicine Tongxinluo capsule protects against blood-brain barrier disruption after ischemic stroke by inhibiting the low-density lipoprotein receptor-related protein 1 pathway in mice. J Stroke Cerebrovasc Diseases: Off J Natl Stroke Assoc. 2020;29(9):105071.10.1016/j.jstrokecerebrovasdis.2020.105071Search in Google Scholar PubMed
[20] Acebron SP, Niehrs C. β-Catenin-independent roles of Wnt/LRP6 signaling. Trends Cell Biol. 2016;26(12):956–67.10.1016/j.tcb.2016.07.009Search in Google Scholar PubMed
[21] Harriott AM, Heckman MG, Rayaprolu S, Soto-Ortolaza AI, Diehl NN, Kanekiyo T, et al. Low density lipoprotein receptor related protein 1 and 6 gene variants and ischaemic stroke risk. Eur J Neurol. 2015;22(8):1235–41.10.1111/ene.12735Search in Google Scholar PubMed PubMed Central
[22] Abe T, Zhou P, Jackman K, Capone C, Casolla B, Hochrainer K, et al. Lipoprotein receptor-related protein-6 protects the brain from ischemic injury. Stroke. 2013;44(8):2284–91.10.1161/STROKEAHA.113.001320Search in Google Scholar PubMed PubMed Central
[23] Arai K, Lo EH. Astrocytes protect oligodendrocyte precursor cells via MEK/ERK and PI3K/Akt signaling. J Neurosci Res. 2010;88(4):758–63.10.1002/jnr.22256Search in Google Scholar PubMed PubMed Central
[24] Kim SK, Yang H, Pascual JM, De Vivo DC. Valproic acid enhances glucose transport in the cultured brain astrocytes of glucose transporter 1 heterozygous mice. J Child Neurol. 2013;28(1):70–6.10.1177/0883073812440044Search in Google Scholar PubMed
[25] Hollmann EK, Bailey AK, Potharazu AV, Neely MD, Bowman AB, Lippmann ES. Accelerated differentiation of human induced pluripotent stem cells to blood-brain barrier endothelial cells. Fluids Barriers CNS. 2017;14(1):9.10.1186/s12987-017-0059-0Search in Google Scholar PubMed PubMed Central
[26] Wang F, Li R, Tu P, Chen J, Zeng K, Jiang Y. Total glycosides of cistanche deserticola promote neurological function recovery by inducing neurovascular regeneration via Nrf-2/Keap-1 pathway in MCAO/R Rats. Front Pharmacology. 2020;11:236.10.3389/fphar.2020.00236Search in Google Scholar PubMed PubMed Central
[27] Canfield SG, Stebbins MJ, Morales BS, Asai SW, Vatine GD, Svendsen CN, et al. An isogenic blood-brain barrier model comprising brain endothelial cells, astrocytes, and neurons derived from human induced pluripotent stem cells. J neurochemistry. 2017;140(6):874–88.10.1111/jnc.13923Search in Google Scholar PubMed PubMed Central
[28] Hu S, Wu Y, Zhao B, Hu H, Zhu B, Sun Z, et al. Panax notoginseng saponins protect cerebral microvascular endothelial cells against oxygen-glucose deprivation/reperfusion-induced barrier dysfunction via activation of PI3K/Akt/Nrf2 antioxidant signaling pathway. Molecules (Basel, Switzerland). 2018;23(11):2781–98.10.3390/molecules23112781Search in Google Scholar PubMed PubMed Central
[29] Jiao H, Wang Z, Liu Y, Wang P, Xue Y. Specific role of tight junction proteins claudin-5, occludin, and ZO-1 of the blood-brain barrier in a focal cerebral ischemic insult. J Mol Neuroscience: MN. 2011;44(2):130–9.10.1007/s12031-011-9496-4Search in Google Scholar PubMed
[30] Argaw AT, Asp L, Zhang J, Navrazhina K, Pham T, Mariani JN, et al. Astrocyte-derived VEGF-A drives blood-brain barrier disruption in CNS inflammatory disease. J Clin investigation. 2012;122(7):2454–68.10.1172/JCI60842Search in Google Scholar PubMed PubMed Central
[31] Wiese S, Karus M, Faissner A. Astrocytes as a source for extracellular matrix molecules and cytokines. Front Pharmacology. 2012;3:120.10.3389/fphar.2012.00120Search in Google Scholar PubMed PubMed Central
[32] Song S, Huang H, Guan X, Fiesler V, Bhuiyan MIH, Liu R, et al. Activation of endothelial Wnt/β-catenin signaling by protective astrocytes repairs BBB damage in ischemic stroke. Prog Neurobiol. 2021;199:101963.10.1016/j.pneurobio.2020.101963Search in Google Scholar PubMed PubMed Central
[33] Xi T, Jin F, Zhu Y, Wang J, Tang L, Wang Y, et al. miR-27a-3p protects against blood-brain barrier disruption and brain injury after intracerebral hemorrhage by targeting endothelial aquaporin-11. J Biol Chem. 2018;293(52):20041–50.10.1074/jbc.RA118.001858Search in Google Scholar PubMed PubMed Central
[34] Ouyang YB, Xu L, Liu S, Giffard RG. Role of astrocytes in delayed neuronal death: GLT-1 and its novel regulation by MicroRNAs. Adv Neurobiol. 2014;11:171–88.10.1007/978-3-319-08894-5_9Search in Google Scholar PubMed PubMed Central
[35] Zhao Z, Nelson AR, Betsholtz C, Zlokovic BV. Establishment and dysfunction of the blood-brain barrier. Cell. 2015;163(5):1064–78.10.1016/j.cell.2015.10.067Search in Google Scholar PubMed PubMed Central
[36] Xia YP, He QW, Li YN, Chen SC, Huang M, Wang Y, et al. Recombinant human sonic hedgehog protein regulates the expression of ZO-1 and occludin by activating angiopoietin-1 in stroke damage. PLoS one. 2013;8(7):e68891.10.1371/journal.pone.0068891Search in Google Scholar PubMed PubMed Central
[37] Chen D, Li L, Wang Y, Xu R, Peng S, Zhou L, et al. Ischemia-reperfusion injury of brain induces endothelial-mesenchymal transition and vascular fibrosis via activating let-7i/TGF-βR1 double-negative feedback loop. FASEB J: Off Publ Federation Am Societies Exp Biol. 2020;34(5):7178–91.10.1096/fj.202000201RSearch in Google Scholar PubMed
[38] Ma F, Sun P, Zhang X, Hamblin MH, Yin KJ. Endothelium-targeted deletion of the miR-15a/16-1 cluster ameliorates blood-brain barrier dysfunction in ischemic stroke. Sci Signal. 2020;13(626):eaay5686.10.1126/scisignal.aay5686Search in Google Scholar PubMed PubMed Central
[39] Ren H, Luo JQ, Ouyang F, Cheng L, Chen XP, Zhou HH, et al. WNT3A rs752107(C > T) polymorphism is associated with an increased risk of essential hypertension and related cardiovascular diseases. Front Cardiovascular Med. 2021;8:675222.10.3389/fcvm.2021.675222Search in Google Scholar PubMed PubMed Central
© 2022 Qijun Dai et al., published by De Gruyter
This work is licensed under the Creative Commons Attribution 4.0 International License.
Articles in the same Issue
- Research Articles
- AMBRA1 attenuates the proliferation of uveal melanoma cells
- A ceRNA network mediated by LINC00475 in papillary thyroid carcinoma
- Differences in complications between hepatitis B-related cirrhosis and alcohol-related cirrhosis
- Effect of gestational diabetes mellitus on lipid profile: A systematic review and meta-analysis
- Long noncoding RNA NR2F1-AS1 stimulates the tumorigenic behavior of non-small cell lung cancer cells by sponging miR-363-3p to increase SOX4
- Promising novel biomarkers and candidate small-molecule drugs for lung adenocarcinoma: Evidence from bioinformatics analysis of high-throughput data
- Plasmapheresis: Is it a potential alternative treatment for chronic urticaria?
- The biomarkers of key miRNAs and gene targets associated with extranodal NK/T-cell lymphoma
- Gene signature to predict prognostic survival of hepatocellular carcinoma
- Effects of miRNA-199a-5p on cell proliferation and apoptosis of uterine leiomyoma by targeting MED12
- Does diabetes affect paraneoplastic thrombocytosis in colorectal cancer?
- Is there any effect on imprinted genes H19, PEG3, and SNRPN during AOA?
- Leptin and PCSK9 concentrations are associated with vascular endothelial cytokines in patients with stable coronary heart disease
- Pericentric inversion of chromosome 6 and male fertility problems
- Staple line reinforcement with nebulized cyanoacrylate glue in laparoscopic sleeve gastrectomy: A propensity score-matched study
- Retrospective analysis of crescent score in clinical prognosis of IgA nephropathy
- Expression of DNM3 is associated with good outcome in colorectal cancer
- Activation of SphK2 contributes to adipocyte-induced EOC cell proliferation
- CRRT influences PICCO measurements in febrile critically ill patients
- SLCO4A1-AS1 mediates pancreatic cancer development via miR-4673/KIF21B axis
- lncRNA ACTA2-AS1 inhibits malignant phenotypes of gastric cancer cells
- circ_AKT3 knockdown suppresses cisplatin resistance in gastric cancer
- Prognostic value of nicotinamide N-methyltransferase in human cancers: Evidence from a meta-analysis and database validation
- GPC2 deficiency inhibits cell growth and metastasis in colon adenocarcinoma
- A pan-cancer analysis of the oncogenic role of Holliday junction recognition protein in human tumors
- Radiation increases COL1A1, COL3A1, and COL1A2 expression in breast cancer
- Association between preventable risk factors and metabolic syndrome
- miR-29c-5p knockdown reduces inflammation and blood–brain barrier disruption by upregulating LRP6
- Cardiac contractility modulation ameliorates myocardial metabolic remodeling in a rabbit model of chronic heart failure through activation of AMPK and PPAR-α pathway
- Quercitrin protects human bronchial epithelial cells from oxidative damage
- Smurf2 suppresses the metastasis of hepatocellular carcinoma via ubiquitin degradation of Smad2
- circRNA_0001679/miR-338-3p/DUSP16 axis aggravates acute lung injury
- Sonoclot’s usefulness in prediction of cardiopulmonary arrest prognosis: A proof of concept study
- Four drug metabolism-related subgroups of pancreatic adenocarcinoma in prognosis, immune infiltration, and gene mutation
- Decreased expression of miR-195 mediated by hypermethylation promotes osteosarcoma
- LMO3 promotes proliferation and metastasis of papillary thyroid carcinoma cells by regulating LIMK1-mediated cofilin and the β-catenin pathway
- Cx43 upregulation in HUVECs under stretch via TGF-β1 and cytoskeletal network
- Evaluation of menstrual irregularities after COVID-19 vaccination: Results of the MECOVAC survey
- Histopathologic findings on removed stomach after sleeve gastrectomy. Do they influence the outcome?
- Analysis of the expression and prognostic value of MT1-MMP, β1-integrin and YAP1 in glioma
- Optimal diagnosis of the skin cancer using a hybrid deep neural network and grasshopper optimization algorithm
- miR-223-3p alleviates TGF-β-induced epithelial-mesenchymal transition and extracellular matrix deposition by targeting SP3 in endometrial epithelial cells
- Clinical value of SIRT1 as a prognostic biomarker in esophageal squamous cell carcinoma, a systematic meta-analysis
- circ_0020123 promotes cell proliferation and migration in lung adenocarcinoma via PDZD8
- miR-22-5p regulates the self-renewal of spermatogonial stem cells by targeting EZH2
- hsa-miR-340-5p inhibits epithelial–mesenchymal transition in endometriosis by targeting MAP3K2 and inactivating MAPK/ERK signaling
- circ_0085296 inhibits the biological functions of trophoblast cells to promote the progression of preeclampsia via the miR-942-5p/THBS2 network
- TCD hemodynamics findings in the subacute phase of anterior circulation stroke patients treated with mechanical thrombectomy
- Development of a risk-stratification scoring system for predicting risk of breast cancer based on non-alcoholic fatty liver disease, non-alcoholic fatty pancreas disease, and uric acid
- Tollip promotes hepatocellular carcinoma progression via PI3K/AKT pathway
- circ_0062491 alleviates periodontitis via the miR-142-5p/IGF1 axis
- Human amniotic fluid as a source of stem cells
- lncRNA NONRATT013819.2 promotes transforming growth factor-β1-induced myofibroblastic transition of hepatic stellate cells by miR24-3p/lox
- NORAD modulates miR-30c-5p-LDHA to protect lung endothelial cells damage
- Idiopathic pulmonary fibrosis telemedicine management during COVID-19 outbreak
- Risk factors for adverse drug reactions associated with clopidogrel therapy
- Serum zinc associated with immunity and inflammatory markers in Covid-19
- The relationship between night shift work and breast cancer incidence: A systematic review and meta-analysis of observational studies
- LncRNA expression in idiopathic achalasia: New insight and preliminary exploration into pathogenesis
- Notoginsenoside R1 alleviates spinal cord injury through the miR-301a/KLF7 axis to activate Wnt/β-catenin pathway
- Moscatilin suppresses the inflammation from macrophages and T cells
- Zoledronate promotes ECM degradation and apoptosis via Wnt/β-catenin
- Epithelial-mesenchymal transition-related genes in coronary artery disease
- The effect evaluation of traditional vaginal surgery and transvaginal mesh surgery for severe pelvic organ prolapse: 5 years follow-up
- Repeated partial splenic artery embolization for hypersplenism improves platelet count
- Low expression of miR-27b in serum exosomes of non-small cell lung cancer facilitates its progression by affecting EGFR
- Exosomal hsa_circ_0000519 modulates the NSCLC cell growth and metastasis via miR-1258/RHOV axis
- miR-455-5p enhances 5-fluorouracil sensitivity in colorectal cancer cells by targeting PIK3R1 and DEPDC1
- The effect of tranexamic acid on the reduction of intraoperative and postoperative blood loss and thromboembolic risk in patients with hip fracture
- Isocitrate dehydrogenase 1 mutation in cholangiocarcinoma impairs tumor progression by sensitizing cells to ferroptosis
- Artemisinin protects against cerebral ischemia and reperfusion injury via inhibiting the NF-κB pathway
- A 16-gene signature associated with homologous recombination deficiency for prognosis prediction in patients with triple-negative breast cancer
- Lidocaine ameliorates chronic constriction injury-induced neuropathic pain through regulating M1/M2 microglia polarization
- MicroRNA 322-5p reduced neuronal inflammation via the TLR4/TRAF6/NF-κB axis in a rat epilepsy model
- miR-1273h-5p suppresses CXCL12 expression and inhibits gastric cancer cell invasion and metastasis
- Clinical characteristics of pneumonia patients of long course of illness infected with SARS-CoV-2
- circRNF20 aggravates the malignancy of retinoblastoma depending on the regulation of miR-132-3p/PAX6 axis
- Linezolid for resistant Gram-positive bacterial infections in children under 12 years: A meta-analysis
- Rack1 regulates pro-inflammatory cytokines by NF-κB in diabetic nephropathy
- Comprehensive analysis of molecular mechanism and a novel prognostic signature based on small nuclear RNA biomarkers in gastric cancer patients
- Smog and risk of maternal and fetal birth outcomes: A retrospective study in Baoding, China
- Let-7i-3p inhibits the cell cycle, proliferation, invasion, and migration of colorectal cancer cells via downregulating CCND1
- β2-Adrenergic receptor expression in subchondral bone of patients with varus knee osteoarthritis
- Possible impact of COVID-19 pandemic and lockdown on suicide behavior among patients in Southeast Serbia
- In vitro antimicrobial activity of ozonated oil in liposome eyedrop against multidrug-resistant bacteria
- Potential biomarkers for inflammatory response in acute lung injury
- A low serum uric acid concentration predicts a poor prognosis in adult patients with candidemia
- Antitumor activity of recombinant oncolytic vaccinia virus with human IL2
- ALKBH5 inhibits TNF-α-induced apoptosis of HUVECs through Bcl-2 pathway
- Risk prediction of cardiovascular disease using machine learning classifiers
- Value of ultrasonography parameters in diagnosing polycystic ovary syndrome
- Bioinformatics analysis reveals three key genes and four survival genes associated with youth-onset NSCLC
- Identification of autophagy-related biomarkers in patients with pulmonary arterial hypertension based on bioinformatics analysis
- Protective effects of glaucocalyxin A on the airway of asthmatic mice
- Overexpression of miR-100-5p inhibits papillary thyroid cancer progression via targeting FZD8
- Bioinformatics-based analysis of SUMOylation-related genes in hepatocellular carcinoma reveals a role of upregulated SAE1 in promoting cell proliferation
- Effectiveness and clinical benefits of new anti-diabetic drugs: A real life experience
- Identification of osteoporosis based on gene biomarkers using support vector machine
- Tanshinone IIA reverses oxaliplatin resistance in colorectal cancer through microRNA-30b-5p/AVEN axis
- miR-212-5p inhibits nasopharyngeal carcinoma progression by targeting METTL3
- Association of ST-T changes with all-cause mortality among patients with peripheral T-cell lymphomas
- LINC00665/miRNAs axis-mediated collagen type XI alpha 1 correlates with immune infiltration and malignant phenotypes in lung adenocarcinoma
- The perinatal factors that influence the excretion of fecal calprotectin in premature-born children
- Effect of femoral head necrosis cystic area on femoral head collapse and stress distribution in femoral head: A clinical and finite element study
- Does the use of 3D-printed cones give a chance to postpone the use of megaprostheses in patients with large bone defects in the knee joint?
- lncRNA HAGLR modulates myocardial ischemia–reperfusion injury in mice through regulating miR-133a-3p/MAPK1 axis
- Protective effect of ghrelin on intestinal I/R injury in rats
- In vivo knee kinematics of an innovative prosthesis design
- Relationship between the height of fibular head and the incidence and severity of knee osteoarthritis
- lncRNA WT1-AS attenuates hypoxia/ischemia-induced neuronal injury during cerebral ischemic stroke via miR-186-5p/XIAP axis
- Correlation of cardiac troponin T and APACHE III score with all-cause in-hospital mortality in critically ill patients with acute pulmonary embolism
- LncRNA LINC01857 reduces metastasis and angiogenesis in breast cancer cells via regulating miR-2052/CENPQ axis
- Endothelial cell-specific molecule 1 (ESM1) promoted by transcription factor SPI1 acts as an oncogene to modulate the malignant phenotype of endometrial cancer
- SELENBP1 inhibits progression of colorectal cancer by suppressing epithelial–mesenchymal transition
- Visfatin is negatively associated with coronary artery lesions in subjects with impaired fasting glucose
- Treatment and outcomes of mechanical complications of acute myocardial infarction during the Covid-19 era: A comparison with the pre-Covid-19 period. A systematic review and meta-analysis
- Neonatal stroke surveillance study protocol in the United Kingdom and Republic of Ireland
- Oncogenic role of TWF2 in human tumors: A pan-cancer analysis
- Mean corpuscular hemoglobin predicts the length of hospital stay independent of severity classification in patients with acute pancreatitis
- Association of gallstone and polymorphisms of UGT1A1*27 and UGT1A1*28 in patients with hepatitis B virus-related liver failure
- TGF-β1 upregulates Sar1a expression and induces procollagen-I secretion in hypertrophic scarring fibroblasts
- Antisense lncRNA PCNA-AS1 promotes esophageal squamous cell carcinoma progression through the miR-2467-3p/PCNA axis
- NK-cell dysfunction of acute myeloid leukemia in relation to the renin–angiotensin system and neurotransmitter genes
- The effect of dilution with glucose and prolonged injection time on dexamethasone-induced perineal irritation – A randomized controlled trial
- miR-146-5p restrains calcification of vascular smooth muscle cells by suppressing TRAF6
- Role of lncRNA MIAT/miR-361-3p/CCAR2 in prostate cancer cells
- lncRNA NORAD promotes lung cancer progression by competitively binding to miR-28-3p with E2F2
- Noninvasive diagnosis of AIH/PBC overlap syndrome based on prediction models
- lncRNA FAM230B is highly expressed in colorectal cancer and suppresses the maturation of miR-1182 to increase cell proliferation
- circ-LIMK1 regulates cisplatin resistance in lung adenocarcinoma by targeting miR-512-5p/HMGA1 axis
- LncRNA SNHG3 promoted cell proliferation, migration, and metastasis of esophageal squamous cell carcinoma via regulating miR-151a-3p/PFN2 axis
- Risk perception and affective state on work exhaustion in obstetrics during the COVID-19 pandemic
- lncRNA-AC130710/miR-129-5p/mGluR1 axis promote migration and invasion by activating PKCα-MAPK signal pathway in melanoma
- SNRPB promotes cell cycle progression in thyroid carcinoma via inhibiting p53
- Xylooligosaccharides and aerobic training regulate metabolism and behavior in rats with streptozotocin-induced type 1 diabetes
- Serpin family A member 1 is an oncogene in glioma and its translation is enhanced by NAD(P)H quinone dehydrogenase 1 through RNA-binding activity
- Silencing of CPSF7 inhibits the proliferation, migration, and invasion of lung adenocarcinoma cells by blocking the AKT/mTOR signaling pathway
- Ultrasound-guided lumbar plexus block versus transversus abdominis plane block for analgesia in children with hip dislocation: A double-blind, randomized trial
- Relationship of plasma MBP and 8-oxo-dG with brain damage in preterm
- Identification of a novel necroptosis-associated miRNA signature for predicting the prognosis in head and neck squamous cell carcinoma
- Delayed femoral vein ligation reduces operative time and blood loss during hip disarticulation in patients with extremity tumors
- The expression of ASAP3 and NOTCH3 and the clinicopathological characteristics of adult glioma patients
- Longitudinal analysis of factors related to Helicobacter pylori infection in Chinese adults
- HOXA10 enhances cell proliferation and suppresses apoptosis in esophageal cancer via activating p38/ERK signaling pathway
- Meta-analysis of early-life antibiotic use and allergic rhinitis
- Marital status and its correlation with age, race, and gender in prognosis of tonsil squamous cell carcinomas
- HPV16 E6E7 up-regulates KIF2A expression by activating JNK/c-Jun signal, is beneficial to migration and invasion of cervical cancer cells
- Amino acid profiles in the tissue and serum of patients with liver cancer
- Pain in critically ill COVID-19 patients: An Italian retrospective study
- Immunohistochemical distribution of Bcl-2 and p53 apoptotic markers in acetamiprid-induced nephrotoxicity
- Estradiol pretreatment in GnRH antagonist protocol for IVF/ICSI treatment
- Long non-coding RNAs LINC00689 inhibits the apoptosis of human nucleus pulposus cells via miR-3127-5p/ATG7 axis-mediated autophagy
- The relationship between oxygen therapy, drug therapy, and COVID-19 mortality
- Monitoring hypertensive disorders in pregnancy to prevent preeclampsia in pregnant women of advanced maternal age: Trial mimicking with retrospective data
- SETD1A promotes the proliferation and glycolysis of nasopharyngeal carcinoma cells by activating the PI3K/Akt pathway
- The role of Shunaoxin pills in the treatment of chronic cerebral hypoperfusion and its main pharmacodynamic components
- TET3 governs malignant behaviors and unfavorable prognosis of esophageal squamous cell carcinoma by activating the PI3K/AKT/GSK3β/β-catenin pathway
- Associations between morphokinetic parameters of temporary-arrest embryos and the clinical prognosis in FET cycles
- Long noncoding RNA WT1-AS regulates trophoblast proliferation, migration, and invasion via the microRNA-186-5p/CADM2 axis
- The incidence of bronchiectasis in chronic obstructive pulmonary disease
- Integrated bioinformatics analysis shows integrin alpha 3 is a prognostic biomarker for pancreatic cancer
- Inhibition of miR-21 improves pulmonary vascular responses in bronchopulmonary dysplasia by targeting the DDAH1/ADMA/NO pathway
- Comparison of hospitalized patients with severe pneumonia caused by COVID-19 and influenza A (H7N9 and H1N1): A retrospective study from a designated hospital
- lncRNA ZFAS1 promotes intervertebral disc degeneration by upregulating AAK1
- Pathological characteristics of liver injury induced by N,N-dimethylformamide: From humans to animal models
- lncRNA ELFN1-AS1 enhances the progression of colon cancer by targeting miR-4270 to upregulate AURKB
- DARS-AS1 modulates cell proliferation and migration of gastric cancer cells by regulating miR-330-3p/NAT10 axis
- Dezocine inhibits cell proliferation, migration, and invasion by targeting CRABP2 in ovarian cancer
- MGST1 alleviates the oxidative stress of trophoblast cells induced by hypoxia/reoxygenation and promotes cell proliferation, migration, and invasion by activating the PI3K/AKT/mTOR pathway
- Bifidobacterium lactis Probio-M8 ameliorated the symptoms of type 2 diabetes mellitus mice by changing ileum FXR-CYP7A1
- circRNA DENND1B inhibits tumorigenicity of clear cell renal cell carcinoma via miR-122-5p/TIMP2 axis
- EphA3 targeted by miR-3666 contributes to melanoma malignancy via activating ERK1/2 and p38 MAPK pathways
- Pacemakers and methylprednisolone pulse therapy in immune-related myocarditis concomitant with complete heart block
- miRNA-130a-3p targets sphingosine-1-phosphate receptor 1 to activate the microglial and astrocytes and to promote neural injury under the high glucose condition
- Review Articles
- Current management of cancer pain in Italy: Expert opinion paper
- Hearing loss and brain disorders: A review of multiple pathologies
- The rationale for using low-molecular weight heparin in the therapy of symptomatic COVID-19 patients
- Amyotrophic lateral sclerosis and delayed onset muscle soreness in light of the impaired blink and stretch reflexes – watch out for Piezo2
- Interleukin-35 in autoimmune dermatoses: Current concepts
- Recent discoveries in microbiota dysbiosis, cholangiocytic factors, and models for studying the pathogenesis of primary sclerosing cholangitis
- Advantages of ketamine in pediatric anesthesia
- Congenital adrenal hyperplasia. Role of dentist in early diagnosis
- Migraine management: Non-pharmacological points for patients and health care professionals
- Atherogenic index of plasma and coronary artery disease: A systematic review
- Physiological and modulatory role of thioredoxins in the cellular function
- Case Reports
- Intrauterine Bakri balloon tamponade plus cervical cerclage for the prevention and treatment of postpartum haemorrhage in late pregnancy complicated with acute aortic dissection: Case series
- A case of successful pembrolizumab monotherapy in a patient with advanced lung adenocarcinoma: Use of multiple biomarkers in combination for clinical practice
- Unusual neurological manifestations of bilateral medial medullary infarction: A case report
- Atypical symptoms of malignant hyperthermia: A rare causative mutation in the RYR1 gene
- A case report of dermatomyositis with the missed diagnosis of non-small cell lung cancer and concurrence of pulmonary tuberculosis
- A rare case of endometrial polyp complicated with uterine inversion: A case report and clinical management
- Spontaneous rupturing of splenic artery aneurysm: Another reason for fatal syncope and shock (Case report and literature review)
- Fungal infection mimicking COVID-19 infection – A case report
- Concurrent aspergillosis and cystic pulmonary metastases in a patient with tongue squamous cell carcinoma
- Paraganglioma-induced inverted takotsubo-like cardiomyopathy leading to cardiogenic shock successfully treated with extracorporeal membrane oxygenation
- Lineage switch from lymphoma to myeloid neoplasms: First case series from a single institution
- Trismus during tracheal extubation as a complication of general anaesthesia – A case report
- Simultaneous treatment of a pubovesical fistula and lymph node metastasis secondary to multimodal treatment for prostate cancer: Case report and review of the literature
- Two case reports of skin vasculitis following the COVID-19 immunization
- Ureteroiliac fistula after oncological surgery: Case report and review of the literature
- Synchronous triple primary malignant tumours in the bladder, prostate, and lung harbouring TP53 and MEK1 mutations accompanied with severe cardiovascular diseases: A case report
- Huge mucinous cystic neoplasms with adhesion to the left colon: A case report and literature review
- Commentary
- Commentary on “Clinicopathological features of programmed cell death-ligand 1 expression in patients with oral squamous cell carcinoma”
- Rapid Communication
- COVID-19 fear, post-traumatic stress, growth, and the role of resilience
- Erratum
- Erratum to “Tollip promotes hepatocellular carcinoma progression via PI3K/AKT pathway”
- Erratum to “Effect of femoral head necrosis cystic area on femoral head collapse and stress distribution in femoral head: A clinical and finite element study”
- Erratum to “lncRNA NORAD promotes lung cancer progression by competitively binding to miR-28-3p with E2F2”
- Retraction
- Expression and role of ABIN1 in sepsis: In vitro and in vivo studies
- Retraction to “miR-519d downregulates LEP expression to inhibit preeclampsia development”
- Special Issue Computational Intelligence Methodologies Meets Recurrent Cancers - Part II
- Usefulness of close surveillance for rectal cancer patients after neoadjuvant chemoradiotherapy
Articles in the same Issue
- Research Articles
- AMBRA1 attenuates the proliferation of uveal melanoma cells
- A ceRNA network mediated by LINC00475 in papillary thyroid carcinoma
- Differences in complications between hepatitis B-related cirrhosis and alcohol-related cirrhosis
- Effect of gestational diabetes mellitus on lipid profile: A systematic review and meta-analysis
- Long noncoding RNA NR2F1-AS1 stimulates the tumorigenic behavior of non-small cell lung cancer cells by sponging miR-363-3p to increase SOX4
- Promising novel biomarkers and candidate small-molecule drugs for lung adenocarcinoma: Evidence from bioinformatics analysis of high-throughput data
- Plasmapheresis: Is it a potential alternative treatment for chronic urticaria?
- The biomarkers of key miRNAs and gene targets associated with extranodal NK/T-cell lymphoma
- Gene signature to predict prognostic survival of hepatocellular carcinoma
- Effects of miRNA-199a-5p on cell proliferation and apoptosis of uterine leiomyoma by targeting MED12
- Does diabetes affect paraneoplastic thrombocytosis in colorectal cancer?
- Is there any effect on imprinted genes H19, PEG3, and SNRPN during AOA?
- Leptin and PCSK9 concentrations are associated with vascular endothelial cytokines in patients with stable coronary heart disease
- Pericentric inversion of chromosome 6 and male fertility problems
- Staple line reinforcement with nebulized cyanoacrylate glue in laparoscopic sleeve gastrectomy: A propensity score-matched study
- Retrospective analysis of crescent score in clinical prognosis of IgA nephropathy
- Expression of DNM3 is associated with good outcome in colorectal cancer
- Activation of SphK2 contributes to adipocyte-induced EOC cell proliferation
- CRRT influences PICCO measurements in febrile critically ill patients
- SLCO4A1-AS1 mediates pancreatic cancer development via miR-4673/KIF21B axis
- lncRNA ACTA2-AS1 inhibits malignant phenotypes of gastric cancer cells
- circ_AKT3 knockdown suppresses cisplatin resistance in gastric cancer
- Prognostic value of nicotinamide N-methyltransferase in human cancers: Evidence from a meta-analysis and database validation
- GPC2 deficiency inhibits cell growth and metastasis in colon adenocarcinoma
- A pan-cancer analysis of the oncogenic role of Holliday junction recognition protein in human tumors
- Radiation increases COL1A1, COL3A1, and COL1A2 expression in breast cancer
- Association between preventable risk factors and metabolic syndrome
- miR-29c-5p knockdown reduces inflammation and blood–brain barrier disruption by upregulating LRP6
- Cardiac contractility modulation ameliorates myocardial metabolic remodeling in a rabbit model of chronic heart failure through activation of AMPK and PPAR-α pathway
- Quercitrin protects human bronchial epithelial cells from oxidative damage
- Smurf2 suppresses the metastasis of hepatocellular carcinoma via ubiquitin degradation of Smad2
- circRNA_0001679/miR-338-3p/DUSP16 axis aggravates acute lung injury
- Sonoclot’s usefulness in prediction of cardiopulmonary arrest prognosis: A proof of concept study
- Four drug metabolism-related subgroups of pancreatic adenocarcinoma in prognosis, immune infiltration, and gene mutation
- Decreased expression of miR-195 mediated by hypermethylation promotes osteosarcoma
- LMO3 promotes proliferation and metastasis of papillary thyroid carcinoma cells by regulating LIMK1-mediated cofilin and the β-catenin pathway
- Cx43 upregulation in HUVECs under stretch via TGF-β1 and cytoskeletal network
- Evaluation of menstrual irregularities after COVID-19 vaccination: Results of the MECOVAC survey
- Histopathologic findings on removed stomach after sleeve gastrectomy. Do they influence the outcome?
- Analysis of the expression and prognostic value of MT1-MMP, β1-integrin and YAP1 in glioma
- Optimal diagnosis of the skin cancer using a hybrid deep neural network and grasshopper optimization algorithm
- miR-223-3p alleviates TGF-β-induced epithelial-mesenchymal transition and extracellular matrix deposition by targeting SP3 in endometrial epithelial cells
- Clinical value of SIRT1 as a prognostic biomarker in esophageal squamous cell carcinoma, a systematic meta-analysis
- circ_0020123 promotes cell proliferation and migration in lung adenocarcinoma via PDZD8
- miR-22-5p regulates the self-renewal of spermatogonial stem cells by targeting EZH2
- hsa-miR-340-5p inhibits epithelial–mesenchymal transition in endometriosis by targeting MAP3K2 and inactivating MAPK/ERK signaling
- circ_0085296 inhibits the biological functions of trophoblast cells to promote the progression of preeclampsia via the miR-942-5p/THBS2 network
- TCD hemodynamics findings in the subacute phase of anterior circulation stroke patients treated with mechanical thrombectomy
- Development of a risk-stratification scoring system for predicting risk of breast cancer based on non-alcoholic fatty liver disease, non-alcoholic fatty pancreas disease, and uric acid
- Tollip promotes hepatocellular carcinoma progression via PI3K/AKT pathway
- circ_0062491 alleviates periodontitis via the miR-142-5p/IGF1 axis
- Human amniotic fluid as a source of stem cells
- lncRNA NONRATT013819.2 promotes transforming growth factor-β1-induced myofibroblastic transition of hepatic stellate cells by miR24-3p/lox
- NORAD modulates miR-30c-5p-LDHA to protect lung endothelial cells damage
- Idiopathic pulmonary fibrosis telemedicine management during COVID-19 outbreak
- Risk factors for adverse drug reactions associated with clopidogrel therapy
- Serum zinc associated with immunity and inflammatory markers in Covid-19
- The relationship between night shift work and breast cancer incidence: A systematic review and meta-analysis of observational studies
- LncRNA expression in idiopathic achalasia: New insight and preliminary exploration into pathogenesis
- Notoginsenoside R1 alleviates spinal cord injury through the miR-301a/KLF7 axis to activate Wnt/β-catenin pathway
- Moscatilin suppresses the inflammation from macrophages and T cells
- Zoledronate promotes ECM degradation and apoptosis via Wnt/β-catenin
- Epithelial-mesenchymal transition-related genes in coronary artery disease
- The effect evaluation of traditional vaginal surgery and transvaginal mesh surgery for severe pelvic organ prolapse: 5 years follow-up
- Repeated partial splenic artery embolization for hypersplenism improves platelet count
- Low expression of miR-27b in serum exosomes of non-small cell lung cancer facilitates its progression by affecting EGFR
- Exosomal hsa_circ_0000519 modulates the NSCLC cell growth and metastasis via miR-1258/RHOV axis
- miR-455-5p enhances 5-fluorouracil sensitivity in colorectal cancer cells by targeting PIK3R1 and DEPDC1
- The effect of tranexamic acid on the reduction of intraoperative and postoperative blood loss and thromboembolic risk in patients with hip fracture
- Isocitrate dehydrogenase 1 mutation in cholangiocarcinoma impairs tumor progression by sensitizing cells to ferroptosis
- Artemisinin protects against cerebral ischemia and reperfusion injury via inhibiting the NF-κB pathway
- A 16-gene signature associated with homologous recombination deficiency for prognosis prediction in patients with triple-negative breast cancer
- Lidocaine ameliorates chronic constriction injury-induced neuropathic pain through regulating M1/M2 microglia polarization
- MicroRNA 322-5p reduced neuronal inflammation via the TLR4/TRAF6/NF-κB axis in a rat epilepsy model
- miR-1273h-5p suppresses CXCL12 expression and inhibits gastric cancer cell invasion and metastasis
- Clinical characteristics of pneumonia patients of long course of illness infected with SARS-CoV-2
- circRNF20 aggravates the malignancy of retinoblastoma depending on the regulation of miR-132-3p/PAX6 axis
- Linezolid for resistant Gram-positive bacterial infections in children under 12 years: A meta-analysis
- Rack1 regulates pro-inflammatory cytokines by NF-κB in diabetic nephropathy
- Comprehensive analysis of molecular mechanism and a novel prognostic signature based on small nuclear RNA biomarkers in gastric cancer patients
- Smog and risk of maternal and fetal birth outcomes: A retrospective study in Baoding, China
- Let-7i-3p inhibits the cell cycle, proliferation, invasion, and migration of colorectal cancer cells via downregulating CCND1
- β2-Adrenergic receptor expression in subchondral bone of patients with varus knee osteoarthritis
- Possible impact of COVID-19 pandemic and lockdown on suicide behavior among patients in Southeast Serbia
- In vitro antimicrobial activity of ozonated oil in liposome eyedrop against multidrug-resistant bacteria
- Potential biomarkers for inflammatory response in acute lung injury
- A low serum uric acid concentration predicts a poor prognosis in adult patients with candidemia
- Antitumor activity of recombinant oncolytic vaccinia virus with human IL2
- ALKBH5 inhibits TNF-α-induced apoptosis of HUVECs through Bcl-2 pathway
- Risk prediction of cardiovascular disease using machine learning classifiers
- Value of ultrasonography parameters in diagnosing polycystic ovary syndrome
- Bioinformatics analysis reveals three key genes and four survival genes associated with youth-onset NSCLC
- Identification of autophagy-related biomarkers in patients with pulmonary arterial hypertension based on bioinformatics analysis
- Protective effects of glaucocalyxin A on the airway of asthmatic mice
- Overexpression of miR-100-5p inhibits papillary thyroid cancer progression via targeting FZD8
- Bioinformatics-based analysis of SUMOylation-related genes in hepatocellular carcinoma reveals a role of upregulated SAE1 in promoting cell proliferation
- Effectiveness and clinical benefits of new anti-diabetic drugs: A real life experience
- Identification of osteoporosis based on gene biomarkers using support vector machine
- Tanshinone IIA reverses oxaliplatin resistance in colorectal cancer through microRNA-30b-5p/AVEN axis
- miR-212-5p inhibits nasopharyngeal carcinoma progression by targeting METTL3
- Association of ST-T changes with all-cause mortality among patients with peripheral T-cell lymphomas
- LINC00665/miRNAs axis-mediated collagen type XI alpha 1 correlates with immune infiltration and malignant phenotypes in lung adenocarcinoma
- The perinatal factors that influence the excretion of fecal calprotectin in premature-born children
- Effect of femoral head necrosis cystic area on femoral head collapse and stress distribution in femoral head: A clinical and finite element study
- Does the use of 3D-printed cones give a chance to postpone the use of megaprostheses in patients with large bone defects in the knee joint?
- lncRNA HAGLR modulates myocardial ischemia–reperfusion injury in mice through regulating miR-133a-3p/MAPK1 axis
- Protective effect of ghrelin on intestinal I/R injury in rats
- In vivo knee kinematics of an innovative prosthesis design
- Relationship between the height of fibular head and the incidence and severity of knee osteoarthritis
- lncRNA WT1-AS attenuates hypoxia/ischemia-induced neuronal injury during cerebral ischemic stroke via miR-186-5p/XIAP axis
- Correlation of cardiac troponin T and APACHE III score with all-cause in-hospital mortality in critically ill patients with acute pulmonary embolism
- LncRNA LINC01857 reduces metastasis and angiogenesis in breast cancer cells via regulating miR-2052/CENPQ axis
- Endothelial cell-specific molecule 1 (ESM1) promoted by transcription factor SPI1 acts as an oncogene to modulate the malignant phenotype of endometrial cancer
- SELENBP1 inhibits progression of colorectal cancer by suppressing epithelial–mesenchymal transition
- Visfatin is negatively associated with coronary artery lesions in subjects with impaired fasting glucose
- Treatment and outcomes of mechanical complications of acute myocardial infarction during the Covid-19 era: A comparison with the pre-Covid-19 period. A systematic review and meta-analysis
- Neonatal stroke surveillance study protocol in the United Kingdom and Republic of Ireland
- Oncogenic role of TWF2 in human tumors: A pan-cancer analysis
- Mean corpuscular hemoglobin predicts the length of hospital stay independent of severity classification in patients with acute pancreatitis
- Association of gallstone and polymorphisms of UGT1A1*27 and UGT1A1*28 in patients with hepatitis B virus-related liver failure
- TGF-β1 upregulates Sar1a expression and induces procollagen-I secretion in hypertrophic scarring fibroblasts
- Antisense lncRNA PCNA-AS1 promotes esophageal squamous cell carcinoma progression through the miR-2467-3p/PCNA axis
- NK-cell dysfunction of acute myeloid leukemia in relation to the renin–angiotensin system and neurotransmitter genes
- The effect of dilution with glucose and prolonged injection time on dexamethasone-induced perineal irritation – A randomized controlled trial
- miR-146-5p restrains calcification of vascular smooth muscle cells by suppressing TRAF6
- Role of lncRNA MIAT/miR-361-3p/CCAR2 in prostate cancer cells
- lncRNA NORAD promotes lung cancer progression by competitively binding to miR-28-3p with E2F2
- Noninvasive diagnosis of AIH/PBC overlap syndrome based on prediction models
- lncRNA FAM230B is highly expressed in colorectal cancer and suppresses the maturation of miR-1182 to increase cell proliferation
- circ-LIMK1 regulates cisplatin resistance in lung adenocarcinoma by targeting miR-512-5p/HMGA1 axis
- LncRNA SNHG3 promoted cell proliferation, migration, and metastasis of esophageal squamous cell carcinoma via regulating miR-151a-3p/PFN2 axis
- Risk perception and affective state on work exhaustion in obstetrics during the COVID-19 pandemic
- lncRNA-AC130710/miR-129-5p/mGluR1 axis promote migration and invasion by activating PKCα-MAPK signal pathway in melanoma
- SNRPB promotes cell cycle progression in thyroid carcinoma via inhibiting p53
- Xylooligosaccharides and aerobic training regulate metabolism and behavior in rats with streptozotocin-induced type 1 diabetes
- Serpin family A member 1 is an oncogene in glioma and its translation is enhanced by NAD(P)H quinone dehydrogenase 1 through RNA-binding activity
- Silencing of CPSF7 inhibits the proliferation, migration, and invasion of lung adenocarcinoma cells by blocking the AKT/mTOR signaling pathway
- Ultrasound-guided lumbar plexus block versus transversus abdominis plane block for analgesia in children with hip dislocation: A double-blind, randomized trial
- Relationship of plasma MBP and 8-oxo-dG with brain damage in preterm
- Identification of a novel necroptosis-associated miRNA signature for predicting the prognosis in head and neck squamous cell carcinoma
- Delayed femoral vein ligation reduces operative time and blood loss during hip disarticulation in patients with extremity tumors
- The expression of ASAP3 and NOTCH3 and the clinicopathological characteristics of adult glioma patients
- Longitudinal analysis of factors related to Helicobacter pylori infection in Chinese adults
- HOXA10 enhances cell proliferation and suppresses apoptosis in esophageal cancer via activating p38/ERK signaling pathway
- Meta-analysis of early-life antibiotic use and allergic rhinitis
- Marital status and its correlation with age, race, and gender in prognosis of tonsil squamous cell carcinomas
- HPV16 E6E7 up-regulates KIF2A expression by activating JNK/c-Jun signal, is beneficial to migration and invasion of cervical cancer cells
- Amino acid profiles in the tissue and serum of patients with liver cancer
- Pain in critically ill COVID-19 patients: An Italian retrospective study
- Immunohistochemical distribution of Bcl-2 and p53 apoptotic markers in acetamiprid-induced nephrotoxicity
- Estradiol pretreatment in GnRH antagonist protocol for IVF/ICSI treatment
- Long non-coding RNAs LINC00689 inhibits the apoptosis of human nucleus pulposus cells via miR-3127-5p/ATG7 axis-mediated autophagy
- The relationship between oxygen therapy, drug therapy, and COVID-19 mortality
- Monitoring hypertensive disorders in pregnancy to prevent preeclampsia in pregnant women of advanced maternal age: Trial mimicking with retrospective data
- SETD1A promotes the proliferation and glycolysis of nasopharyngeal carcinoma cells by activating the PI3K/Akt pathway
- The role of Shunaoxin pills in the treatment of chronic cerebral hypoperfusion and its main pharmacodynamic components
- TET3 governs malignant behaviors and unfavorable prognosis of esophageal squamous cell carcinoma by activating the PI3K/AKT/GSK3β/β-catenin pathway
- Associations between morphokinetic parameters of temporary-arrest embryos and the clinical prognosis in FET cycles
- Long noncoding RNA WT1-AS regulates trophoblast proliferation, migration, and invasion via the microRNA-186-5p/CADM2 axis
- The incidence of bronchiectasis in chronic obstructive pulmonary disease
- Integrated bioinformatics analysis shows integrin alpha 3 is a prognostic biomarker for pancreatic cancer
- Inhibition of miR-21 improves pulmonary vascular responses in bronchopulmonary dysplasia by targeting the DDAH1/ADMA/NO pathway
- Comparison of hospitalized patients with severe pneumonia caused by COVID-19 and influenza A (H7N9 and H1N1): A retrospective study from a designated hospital
- lncRNA ZFAS1 promotes intervertebral disc degeneration by upregulating AAK1
- Pathological characteristics of liver injury induced by N,N-dimethylformamide: From humans to animal models
- lncRNA ELFN1-AS1 enhances the progression of colon cancer by targeting miR-4270 to upregulate AURKB
- DARS-AS1 modulates cell proliferation and migration of gastric cancer cells by regulating miR-330-3p/NAT10 axis
- Dezocine inhibits cell proliferation, migration, and invasion by targeting CRABP2 in ovarian cancer
- MGST1 alleviates the oxidative stress of trophoblast cells induced by hypoxia/reoxygenation and promotes cell proliferation, migration, and invasion by activating the PI3K/AKT/mTOR pathway
- Bifidobacterium lactis Probio-M8 ameliorated the symptoms of type 2 diabetes mellitus mice by changing ileum FXR-CYP7A1
- circRNA DENND1B inhibits tumorigenicity of clear cell renal cell carcinoma via miR-122-5p/TIMP2 axis
- EphA3 targeted by miR-3666 contributes to melanoma malignancy via activating ERK1/2 and p38 MAPK pathways
- Pacemakers and methylprednisolone pulse therapy in immune-related myocarditis concomitant with complete heart block
- miRNA-130a-3p targets sphingosine-1-phosphate receptor 1 to activate the microglial and astrocytes and to promote neural injury under the high glucose condition
- Review Articles
- Current management of cancer pain in Italy: Expert opinion paper
- Hearing loss and brain disorders: A review of multiple pathologies
- The rationale for using low-molecular weight heparin in the therapy of symptomatic COVID-19 patients
- Amyotrophic lateral sclerosis and delayed onset muscle soreness in light of the impaired blink and stretch reflexes – watch out for Piezo2
- Interleukin-35 in autoimmune dermatoses: Current concepts
- Recent discoveries in microbiota dysbiosis, cholangiocytic factors, and models for studying the pathogenesis of primary sclerosing cholangitis
- Advantages of ketamine in pediatric anesthesia
- Congenital adrenal hyperplasia. Role of dentist in early diagnosis
- Migraine management: Non-pharmacological points for patients and health care professionals
- Atherogenic index of plasma and coronary artery disease: A systematic review
- Physiological and modulatory role of thioredoxins in the cellular function
- Case Reports
- Intrauterine Bakri balloon tamponade plus cervical cerclage for the prevention and treatment of postpartum haemorrhage in late pregnancy complicated with acute aortic dissection: Case series
- A case of successful pembrolizumab monotherapy in a patient with advanced lung adenocarcinoma: Use of multiple biomarkers in combination for clinical practice
- Unusual neurological manifestations of bilateral medial medullary infarction: A case report
- Atypical symptoms of malignant hyperthermia: A rare causative mutation in the RYR1 gene
- A case report of dermatomyositis with the missed diagnosis of non-small cell lung cancer and concurrence of pulmonary tuberculosis
- A rare case of endometrial polyp complicated with uterine inversion: A case report and clinical management
- Spontaneous rupturing of splenic artery aneurysm: Another reason for fatal syncope and shock (Case report and literature review)
- Fungal infection mimicking COVID-19 infection – A case report
- Concurrent aspergillosis and cystic pulmonary metastases in a patient with tongue squamous cell carcinoma
- Paraganglioma-induced inverted takotsubo-like cardiomyopathy leading to cardiogenic shock successfully treated with extracorporeal membrane oxygenation
- Lineage switch from lymphoma to myeloid neoplasms: First case series from a single institution
- Trismus during tracheal extubation as a complication of general anaesthesia – A case report
- Simultaneous treatment of a pubovesical fistula and lymph node metastasis secondary to multimodal treatment for prostate cancer: Case report and review of the literature
- Two case reports of skin vasculitis following the COVID-19 immunization
- Ureteroiliac fistula after oncological surgery: Case report and review of the literature
- Synchronous triple primary malignant tumours in the bladder, prostate, and lung harbouring TP53 and MEK1 mutations accompanied with severe cardiovascular diseases: A case report
- Huge mucinous cystic neoplasms with adhesion to the left colon: A case report and literature review
- Commentary
- Commentary on “Clinicopathological features of programmed cell death-ligand 1 expression in patients with oral squamous cell carcinoma”
- Rapid Communication
- COVID-19 fear, post-traumatic stress, growth, and the role of resilience
- Erratum
- Erratum to “Tollip promotes hepatocellular carcinoma progression via PI3K/AKT pathway”
- Erratum to “Effect of femoral head necrosis cystic area on femoral head collapse and stress distribution in femoral head: A clinical and finite element study”
- Erratum to “lncRNA NORAD promotes lung cancer progression by competitively binding to miR-28-3p with E2F2”
- Retraction
- Expression and role of ABIN1 in sepsis: In vitro and in vivo studies
- Retraction to “miR-519d downregulates LEP expression to inhibit preeclampsia development”
- Special Issue Computational Intelligence Methodologies Meets Recurrent Cancers - Part II
- Usefulness of close surveillance for rectal cancer patients after neoadjuvant chemoradiotherapy

