Abstract
Several studies reported that the expression of SIRT1 was associated with the clinical features of patients with esophageal squamous cell carcinoma (ESCC), but the function remains inconsistent. We conducted this study to illustrate the clinical value of SIRT1 expression in the early diagnosis and prediction of prognosis of ESCC. In this study, PubMed, Embase, and Web of Science were searched by two independent researchers and STATA14.0 software was used to conduct meta-analysis. The odds ratio with 95% confidence interval was used to estimate the pooled effect. Egger’s test and Begg’s funnel were used to assess publication bias. Sensitivity analysis was used to evaluate the reliability and stability of meta-analysis results. According to the inclusion and exclusion criteria, six studies were enrolled, including 811 cases of ESCC. Results of the meta-analysis indicated that SIRT1 was overexpressed in ESCC and the SIRT1 expression was closely related to the clinicopathological features of ESCC, such as tumor infiltration, tumor node metastasis (TNM) stage, and lymph node metastasis. In the survival analysis, high expression of SIRT1 represented a poor prognosis in ESCC patients. Our study demonstrated that SIRT1 was overexpressed in ESCC, and it might be a potential biomarker for progress of ESCC.
1 Introduction
Esophageal carcinoma is the eighth most common type of cancer worldwide and constitutes the sixth leading cause of cancer [1] accounting for over 600,000 new cases and 540,000 cancer deaths annually, which is 3.1% of all global new cancer cases and 5.5% of all cancer deaths [2]. The incident cases of esophageal carcinoma are expected to increase by roughly 35% from 2018 to 2030 worldwide and the estimated number of deaths are expected to increase by roughly 37% during this same timeframe [3]. In China, more than 90% of esophageal cancers are SCC (squamous cell carcinoma). Despite major advances in the fields of surgery, radiotherapy, and chemotherapy, the effectiveness of related treatments for ESCC (esophageal squamous cell carcinoma) is still very low. Due to its aggressive characteristics, the prognosis of ESCC is very poor, and the five-year survival rate is only 15–25% [4]. Early diagnosis of ESCC remains the best way to improve cure and survival rates [5]. Therefore, it is critical to explore effective biomarkers for early diagnosis of ESCC and predicting tumor progression and prognosis, which will significantly reduce mortality, especially in advanced or metastatic ESCC patients.
Sirtuins (SIRTs) are a conservative family of proteins. There are seven different subtypes (SIRT1–7), which mainly regulate the expression of multiple genes through acetylation of proteins and participate in the pathogenesis of many chronic diseases such as diabetes, cardiovascular diseases, and cancer. SIRT1 is a histone deacetylase and an important component of cell self-protection. It is located on the human chromosome 10q21.3 and is highly conserved, playing an important role in tissue and cell growth, aging, and apoptosis [6].
The mechanism of SIRT1 expression with the occurrence and progress of ESCC is still unclear. Several studies reported a relationship between SIRT1 and ESCC, but the results are inconsistent. He et al. [7], Zhang et al. [8], and Ma et al. [9] demonstrated that there was no significant difference of SIRT1 expression between infiltration (T1 + T2) and infiltration (T3 + T4) of ESCC. However, Yan et al. [10] and Chen et al. [11] reported that the SIRT1 expression was significantly lower in infiltration (T1 + T2) than that in infiltration (T3 + T4) of ESCC. Such inconsistent results were also observed in the TNM stage, lymph node metastasis, and other clinicopathological features of ESCC. Because of the inconsistent results of published studies and small sample size, the conclusion is unreliable according to a single clinical randomized controlled study. Therefore, we conducted this meta-analysis including all of the eligible studies to obtain a pooled effect to evaluate the association between SIRT1 expression and clinicopathological features of ESCC, providing basis for early diagnosis, treatment, and evaluation of progression and prognosis of ESCC.
2 Materials and methods
This meta-analysis was based on the preferred reporting items for systematic reviews and meta-analysis (PRISMA) guidelines [12].
2.1 Studies searching strategy
Published studies about SIRT1 expression and ESCC were searched in PubMed, Embase, and Web of Science by two independent researchers (up to July 2021). The following strategy and keywords were used for study searching, “SIRT1” or “Sirtuin1” and “Esophageal cancer” or “Esophageal tumor” or “Esophageal carcinoma”. Furthermore, “carcinoma” was replaced by “Esophageal squamous cell carcinoma” to identify any missing studies. The reference lists of retrieved studies were also manually reviewed to identify additional potentially relevant studies. No limitation on country, race, and language was added when studies were searched.
2.2 Inclusion and exclusion criteria
The included studies must meet the following criteria: (1) the studies explored the relationship between SIRT1 expression and ESCC, providing a clear detection and analysis method. (2) The studies provided the criteria for defining high and low expression of SIRT1 in ESCC tissues clearly. (3) Data of SIRT1 expression and clinicopathological features, such as differentiation, infiltration, and TNM clinical stage in ESCC can be obtained or calculated. (4) Repetitive data of articles published by the same research team in different journals, the largest sample size, or the latest published articles were included. The exclusion involved: (1) secondary research such as review, meta-analysis and case reports, and meeting papers. (2) Cell or animal research studies. (3) Studies with insufficient information or contradictions in data. (4) Duplicated studies.
2.3 Data extraction and quality assessment
2.3.1 Data extraction
A prespecified, standardized data extraction form was used for data extracting, two researchers independently completed the data extraction and screening. Any disagreements were resolved by discussion to achieve a consensus. The extracted data mainly included the first author’s name, year of publication, number of cases and controls, testing method of SIRT1 expression, and clinicopathological features of ESCC.
2.3.2 Variables
The clinicopathological features of ESCC included tumor size, differentiation, infiltration, TNM clinical stage, and lymph node metastasis. The tumor size of ESCC was grouped ≤5 cm and >5 cm. The tumor differentiation was grouped high, medium, and low in the included studies, and high and medium were combined into one group when the pooled effect was calculated. Tumor infiltration was grouped T1, T2, T3, and T4 in the included studies, and T1 and T2 were combined into one group and T3 and T4 to another group when the pooled effect was calculated. The clinical stage was grouped stage I, II, III, and IV in the included studies, and I and II were combined into one group and III and IV to another group when the pooled effect was calculated. The tumor lymph node metastasis was grouped as negative and positive. The HR of overall survival time was collected or infered through Kaplan-Meier curve.
2.3.3 Quality assessment
The Newcastle-Ottawa Scale (NOS) was used to evaluate the quality of included studies. The scores ranged from 0 to 9, and the studies with 6 or more was regarded as high quality [13].
2.4 Statistical analysis
STATA 14.0 software was used to conduct statistical analysis. The relationship between SIRT1 expression and clinicopathological features or overall survival time of ESCC was conducted by pooled odds ratio (OR) or hazard ratio (HR) and 95% confidence interval (CI). The statistical significance of the OR or HR was analyzed by the Z-test and the corresponding P value. The heterogeneity test was performed by the I 2 test and the corresponding P value; when I 2 ≥ 50% and P ≤ 0.05, it meant there was significant heterogeneity among the included studies, and the random effects model was used; when I 2 < 50% and P > 0.05, it meant there was no significant heterogeneity among the included studies and the fixed effects model was used. Publication bias was tested through Egger’s test and Begg’s funnel. Sensitivity analysis was used to evaluate the reliability and stability of meta-analysis results. Two-tailed P ≤ 0.05 was regarded as statistically significant.
3 Results
3.1 Characteristics of the included studies
According to the inclusion and exclusion criteria, six studies were enrolled, including 811 cases of ESCC. Only one study reported SIRT1 expression in ESCC and control. Six studies reported the relationship between SIRT1 expression and differentiation in ESCC. Five studies reported the relationship between SIRT1 expression and infiltration in ESCC. Six studies reported the relationship between SIRT1 expression and the TNM clinical stage in ESCC. Four studies reported the relationship between SIRT1 expression and lymph node metastasis in ESCC. Six studies reported the relationship between SIRT1 expression and the overall survival time in ESCC. Six studies reported the relationship between SIRT1 and tumor size, age, and gender in ESCC (Table 1). All the studies inspected SIRT1 expression with immunohistochemistry. The flow diagram of study searching and screening is shown in Figure 1.
Characteristics of included studies
| Study | Year | Case | Control | Clinicopathological features | NOS score |
|---|---|---|---|---|---|
| He et al. [7] | 2015 | 86 | — | 1, 2, 3, 4, 5, 6, 7, 8 | 6 |
| Zhang et al. [8] | 2013 | 176 | 32 | 1, 2, 3, 4, 5, 6, 7, 8 | 8 |
| Ma et al. [9] | 2018 | 155 | — | 1, 2, 4, 5, 6, 7, 8 | 7 |
| Yan et al. [10] | 2020 | 93 | — | 1, 2, 3, 4, 5, 6, 7, 8 | 6 |
| Chen et al. [11] | 2014 | 206 | — | 1, 2, 3, 4, 5, 6, 8 | 7 |
| Han et al. [14] | 2018 | 95 | — | 1, 2, 3, 4, 6, 8 | 6 |
1, Age; 2, gender; 3, tumor size; 4, differentiation; 5, infiltration; 6, TNM stage; and 7, lymph node metastasis; 8, overall survival time.

Flow diagram.
3.2 The expression of SIRT1 in ESCC
Because only one study was enrolled about the expression of SIRT1 in ESCC and control, meta-analysis could not be conducted. The result of this study indicated that SIRT1 was overexpressed in ESCC patients than in the control, which was consistent with the data in The Cancer Genome Atlas (TCGA) database (http://gepia2.cancer-pku.cn) (Figure 2).

SIRT1 expression in ESCC and normal tissues in the TCGA database.
3.3 Relationship between SIRT1 expression and clinicopathological features of ESCC
3.3.1 Relationship between SIRT1 expression and differentiation of ESCC
Six studies including 776 cases were enrolled about SIRT1 expression and differentiation of ESCC. The cases with positive SIRT1 expression were 181 among 360 cases in medium and high differentiation of ESCC, with a positive rate of 50.28%. The cases with positive SIRT1 expression were 246 among 416 cases in low differentiation of ESCC, with a positive rate of 59.13%. The heterogeneity test indicated that no significant heterogeneity was observed among the included studies (I 2 = 26.4%, P = 0.24), and the fixed effects model was used to calculate the pooled effect variable. The SIRT1 expression was a little lower in medium and high differentiation than that in low differentiation of ESCC (OR = 1.01, 95% CI: 0.72–1.43), but the difference was not statistically significant (Z = 0.09, P = 0.93), (Figure 3). No significant publication bias was observed (t = 1.73, P = 0.16).

Forest figure of relationship between the expression of SIRT1 and differentiation of ESCC.
3.3.2 Relationship between SIRT1 expression and infiltration of ESCC
Five studies including 716 cases were enrolled about SIRT1 expression and infiltration of ESCC. The cases with positive SIRT1 expression were 130 among 301 cases in tumor infiltration (T1 + T2) of ESCC, with a positive rate of 43.19%. The cases with positive SIRT1 expression were 252 among 415 cases in tumor infiltration (T3 + T4) of ESCC, with a positive rate of 60.72%. The heterogeneity test indicated that heterogeneity was observed among the included studies (I 2 = 58.1%, P = 0.05), and the random effects model was used to calculate the pooled effect variable. The SIRT1 expression was significantly lower in infiltration (T1 + T2) than that in infiltration (T3 + T4) of ESCC (OR = 0.47, 95% CI: 0.27–0.82), the difference was statistically significant (Z = 2.67, P < 0.05), (Figure 4). No significant publication bias was observed (t = 0.51, P = 0.66).

Forest figure of relationship between the expression of SIRT1 and infiltration of ESCC.
3.3.3 Relationship between SIRT1 expression and the TNM stage of ESCC
Six studies including 811 cases were enrolled about SIRT1 expression and the TNM stage of ESCC. The cases with positive SIRT1 expression were 176 among 359 cases in the tumor stage (I + II) of ESCC, with a positive rate of 49.03%. The cases with positive SIRT1 expression were 269 among 452 cases in the tumor stage (III + IV) of ESCC, with a positive rate of 59.51%. The heterogeneity test indicated that no significant heterogeneity was observed among the included studies (I 2 = 19.9%, P = 0.28), and the fixed effects model was used to calculate the pooled effect variable. The SIRT1 expression was lower in the tumor stage (I + II) than that in stage (III + IV) of ESCC (OR = 0.45, 95% CI: 0.32–0.63), and the difference was statistically significant (Z = 4.72, P < 0.05), (Figure 5). No significant publication bias was observed (t = 2.42, P = 0.07).

Forest figure of relationship between the expression of SIRT1 and the TNM stage of ESCC.
3.3.4 Relationship between SIRT1 expression and lymph node metastasis of ESCC
Four studies including 510 cases were enrolled about SIRT1 expression and lymph node metastasis of ESCC. The cases with positive SIRT1 expression were 117 among 239 cases without tumor lymph node metastasis of ESCC, with a positive rate of 48.95%, The cases with positive SIRT1 expression were 170 among 271 cases with tumor lymph node metastasis of ESCC, with a positive rate of 62.73%. The heterogeneity test indicated that heterogeneity was observed among the included studies (I 2 = 37.1%, P = 0.19), and the fixed effects model was used to calculate the pooled effect variable. The result indicated that SIRT1 expression was lower in ESCC without lymph node metastasis than that with tumor lymph node metastasis (OR = 0.47, 95% CI: 0.31–0.69), and the difference was statistically significant (Z = 3.76, P < 0.05) (Figure 6). No significant publication bias was observed (t = 2.10, P = 0.17).
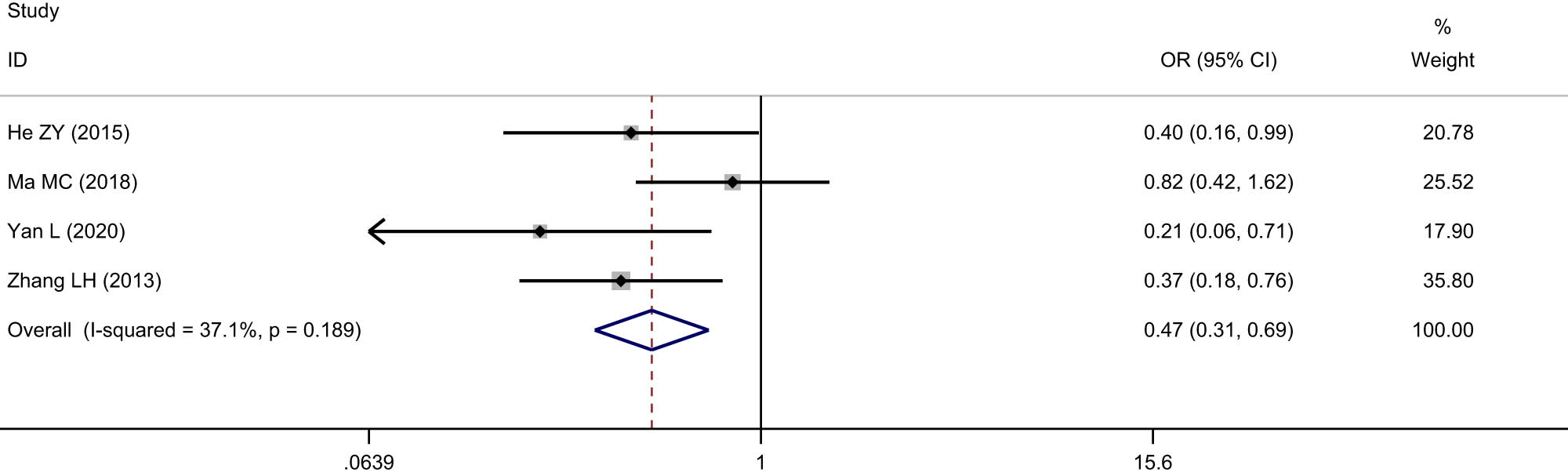
Forest figure of relationship between the expression of SIRT1 and lymph node metastasis of ESCC.
3.3.5 Relationship between SIRT1 expression and tumor size, age, and gender of ESCC
Five studies including 656 cases reported relationship between SIRT1 expression and tumor size in ESCC. No significant difference of SIRT1 expression was observed between tumor size (≤5 cm) and tumor size (>5 cm) (OR = 1.14, 95% CI: 0.78–1.66). Six studies including 811 cases reported relationship between SIRT1 expression and age and gender in ESCC. No significant difference of SIRT1 expression was observed between age (≤60 cm) and age (>60 cm) (OR = 1.24, 95% CI: 0.92–1.67) and was also observed in males and females (OR = 1.07, 95% CI: 0.74–1.54) (Table 2).
Meta-analysis of SIRT1 expression and tumor size, age, and gender of ESCC
| Variables | Included studies | SIRT1 expression | Heterogeneity | Publication bias | ||||
|---|---|---|---|---|---|---|---|---|
| OR (95% CI) | Z | P | I 2 | P | t | P | ||
| Tumor size | 5 | 1.14 (0.78–1.66) | 0.67 | 0.50 | 0.0% | 0.81 | 3.78 | 0.03 |
| Age | 6 | 1.24 (0.92–1.67) | 1.39 | 0.16 | 0.0% | 0.99 | 4.54 | 0.01 |
| Gender | 6 | 1.07 (0.74–1.54) | 0.35 | 0.72 | 0.0% | 0.42 | 1.40 | 0.23 |
3.3.6 Relationship between SIRT1 and overall survival of ESCC
Six studies including 811 cases reported the relationship between the overexpression of SIRT1 and the overall survival time of ESCC patients after surgery. The result indicated that the overall survival time of ESCC patients with positive SIRT1 expression was significantly lower than that in patients with negative SIRT1 expression after surgery (HR = 1.92, 95% CI: 1.52–2.44), and the difference was statistically significant (Z = 5.43, P < 0.05) (Figure 7), suggesting that SIRT1 is closely related to the prognosis of ESCC. The heterogeneity test indicated that no heterogeneity was observed among the included studies (I 2 = 0.0%, P = 0.95). No publication bias was observed (t = 2.11, P = 0.10).

Relationship between SIRT1 and overall survival of ESCC.
3.4 Publication bias and sensitivity analysis
Publication bias was tested through Egger’s test and Begg’s funnel. No significant publication bias was observed in the analysis of SIRT1 expression and differentiation, infiltration, TNM stage, lymph node metastasis, and the overall survival time in ESCC (P > 0.05). But some publication bias was observed in the analysis of SIRT1 expression and tumor size and age in ESCC (P < 0.05).
The results of sensitivity analysis indicated that our meta-analysis was stable.
4 Discussion
SIRT1 is one of the SIRTs, which participates in a large number of biological processes including DNA repair, apoptosis and inflammation [15], aging [16], and autophagy. It plays a crucial role in protection against various human diseases, including metabolic syndromes, cardiovascular diseases, and tumorigenesis. A lot of studies indicated that SIRT1 could serve as a candidate biomarker of human cancer. However, as a crucial regulator, the function of SIRT1 in ESCC has not been well understood.
Our study demonstrated that SIRT1 overexpressed in ESCC compared with normal control. To explore the status of SIRT1 expression in the progress and prognosis of ESCC, we analyzed the relationship between SIRT1 and differentiation, infiltration, TNM stage, lymph node metastasis, and the overall survival time of ESCC. According to the results of our meta-analysis, the pooled effect indicated that SIRT1 overexpressed in tumor infiltration (T3 + T4), TNM stage (III + IV), and positive cases lymph node metastasis of ESCC (P < 0.05). No significant correlation was found between SIRT1 expression and tumor differentiation, tumor size, age, and gender in cases of ESCC (P > 0.05). Our result also indicated that the overall survival time of ESCC patients with positive SIRT1 expression was significantly lower than that of patients with negative SIRT1 expression after surgery (HR = 1.92), which meant that SIRT1 might be a cancer promoting factor. In our meta-analysis, heterogeneity among the included studies was also analyzed, and the sample size and study quality might be the main sources of heterogeneity.
Our study confirmed that the expression of SIRT1 was closely related to ESCC, and the expression of SIRT1 might be a potential biomarker to identify the progress and prognosis of ESCC. At present, the mechanisms of SIRT1 in tumorigenesis and development are still unclear. The mechanisms are mainly as follows: (1) SIRT1 effects metabolism of tumor cells. The activity of SIRT1 is often coupled with homeostasis and metabolism. Chen et al. [17] reported that SIRT1 promoted GLUT1 expression and progression in bladder cancer via regulation of glucose uptake. Simmons et al. [18] found that SIRT1 influenced pathways that provided an alternative means of deriving energy (such as fatty acid oxidation and gluconeogenesis) when a cell encountered nutritive stress and could therefore lead to altered lipid metabolism in various pathophysiological contexts. The survival function of SIRT1 may reflect abnormal cancer metabolism and identifies SIRT1 as a target for anticancer therapy. (2) SIRT1 engenders an error in repairing damaged DNA. SIRT1 can interact with distinct proteins from the main DNA repair mechanisms and DNA damage response (DDR) pathways recruiting them to DNA damage foci or activating the proteins involved in DNA repair by deacetylating them. These processes help the cells to live without damaged DNA but also prone to errors, leading to mutations and abnormal epigenetic marks [19]. The relationship between the function of SIRT1 on DNA repairment and tumorigenesis is not fully understood. Studies to elucidate these pathways will provide a breakthrough in cancer biology. (3) SIRT1 plays a role in tumor promoting by affecting cell proliferation, metastasis, and apoptosis. Garten et al. [20] reported that overexpression of SIRT1 significantly decreased sorafenib-induced apoptosis, which could be an underlying mechanism of resistance to sorafenib treatment in hepatocellular carcinoma (HCC). Zhang et al. [21] found that SIRT1 functioned as a tumor suppressor encouraging gastric cancer progression through the activation of STAT3/MMP-13 signaling, inhibited proliferation, and metastasis of gastric cancer. The function of promoting the proliferation and metastasis of SIRT1 was also observed in pancreatic cancer [22], colorectal cancer [23], lung cancer [24], and other cancers. Effects on immune responses [25], autophagy [26,27], and inflammation [28] were also observed in published studies to illustrate the mechanism of SIRT1 on cancer cell proliferation, metastasis, and apoptosis.
Although efforts had been made, our studies still had some limitations. (1) Due to the limitations of published studies, the population included in this study is mainly the Han Chinese population, and some bias might exist in the analysis. (2) Due to limitation of included studies, the sample size was relatively small. (3) Due to different criteria for judging the positive or negative expression of SIRT1, the included studies had some heterogeneity. (4) Since the included studies were all case-control studies, it was difficult to determine whether SIRT1 was the cause or result of ESCC. (5) Because some included articles did not report detailed survival data, we could only use the Kaplan–Meier curve in the survival analysis to infer the corresponding results, which might overestimate or underestimate the real survival data. Hence, our results of this meta-analysis should be verified by additional larger sample size and well-designed clinical randomized controlled studies in different races, and larger sample size cohort study will also be conducted to verify whether SIRT1 overexpression was the cause or result of ESCC.
5 Conclusion
We confirmed that SIRT1 was overexpressed in ESCC, and the expression of SIRT1 was closely related to the invasion, metastasis, and prognosis of ESCC. SIRT1 might be a potential biomarker to identify the progress and prognosis in ESCC.
-
Funding information: This work was supported by the project of Huai-an Science and Technology (HAB202134). The funders had roles in study design, data collection, analysis, and decision to publish the manuscript.
-
Author contributions: PC conceived and designed the research, YJZ collected the data, YLZ analyzed the data, YLZ and YG wrote and edited the manuscript. All the authors read and approved the final version of manuscript.
-
Conflict of interest: The authors have no conflicts of interest to disclose.
-
Data availability statement: All datasets presented in this study are included in the article/supplementary material.
References
[1] Uhlenhopp DJ, Then EO, Sunkara T, Gaduputi V. Epidemiology of esophageal cancer: update in global trends, etiology and risk factors. Clin J Gastroenterol. 2020;13(6):1010–21.10.1007/s12328-020-01237-xSuche in Google Scholar PubMed
[2] Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71(3):209–49.10.3322/caac.21660Suche in Google Scholar PubMed
[3] Ferlay J, Ervik M, Lam F. Global cancer observatory: cancer tomorrow. Lyon, France: International Agency for Research on Cancer; 2018. https://gco.iarc.fr/tomorrow accessed 15 March 2020.Suche in Google Scholar
[4] Meng X, Chen X, Lu P, Ma W, Yue D, Song L, et al. miR-202 promotes cell apoptosis in esophageal squamous cell carcinoma by targeting HSF2. Oncol Res. 2017;25(2):215–23.10.3727/096504016X14732772150541Suche in Google Scholar PubMed PubMed Central
[5] Lopes AB, Fagundes RB. Esophageal squamous cell carcinoma precursor lesions and early diagnosis. World J Gastrointest Endosc. 2012;4:9–16.10.4253/wjge.v4.i1.9Suche in Google Scholar PubMed PubMed Central
[6] Qiu G, Li X, Che X, Wei C, He S, Lu J, et al. SIRT1 is a regulator of autophagy: Implications in gastric cancer progression and treatment. FEBS Lett. 2015;589(16):2034–42.10.1016/j.febslet.2015.05.042Suche in Google Scholar PubMed
[7] He Z, Yi J, Jin L, Pan B, Chen L, Song H. Overexpression of Sirtuin-1 is associated with poor clinical outcome in esophageal squamous cell carcinoma. Tumour Biol. 2016;37(6):7139–48.10.1007/s13277-015-4459-ySuche in Google Scholar PubMed
[8] Zhang LH, Huang Q, Fan XS, Wu HY, Yang J, Feng AN. Clinicopathological significance of SIRT1 and p300/CBP expression in gastroesophageal junction (GEJ) cancer and the correlation with E-cadherin and MLH1. Pathol Res Pract. 2013;209(10):611–7.10.1016/j.prp.2013.03.012Suche in Google Scholar PubMed
[9] Ma MC, Chiu TJ, Lu HI, Huang WT, Lo CM, Tien WY, et al. SIRT1 overexpression is an independent prognosticator for patients with esophageal squamous cell carcinoma. J Cardiothorac Surg. 2018;13(1):25.10.1186/s13019-018-0718-5Suche in Google Scholar PubMed PubMed Central
[10] Yan L, Zhao Q, Liu L, Jin N, Wang S, Zhan X. Expression of SIRT1 and surviving correlates with poor prognosis in esophageal squamous cell carcinoma. Medicine (Baltimore). 2020;99(34):e21645.10.1097/MD.0000000000021645Suche in Google Scholar PubMed PubMed Central
[11] Chen GQ, Tian H, Yue WM, Li L, Li SH, Qi L, et al. SIRT1 expression is associated with lymphangiogenesis, lymphovascular invasion and prognosis in pN0 esophageal squamous cell carcinoma. Cell Biosci. 2014;4:48.10.1186/2045-3701-4-48Suche in Google Scholar PubMed PubMed Central
[12] Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7):1000097.10.1371/journal.pmed.1000097Suche in Google Scholar PubMed PubMed Central
[13] Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. 2010;25(9):603–5.10.1007/s10654-010-9491-zSuche in Google Scholar PubMed
[14] Han F, Zhang S, Liang J, Qiu W. Clinicopathological and predictive significance of SIRT1 and peroxisome proliferator-activated receptor gamma in esophageal squamous cell carcinoma: the correlation with EGFR and survivin. Pathol Res Pract. 2018;214(5):686–90.10.1016/j.prp.2018.03.018Suche in Google Scholar PubMed
[15] Lamichane S, Baek SH, Kim YJ, Park JH, Dahal Lamichane B, Jang WB, et al. MHY2233 attenuates replicative cellular senescence in human endothelial progenitor cells via SIRT1 signaling. Oxid Med Cell Longev. 2019;2019:6492029.10.1155/2019/6492029Suche in Google Scholar PubMed PubMed Central
[16] Mendelsohn AR, Larrick JW. The NAD +/PARP1/SIRT1 axis in aging. Rejuvenation Res. 2017;20(3):244–7.10.1089/rej.2017.1980Suche in Google Scholar PubMed
[17] Chen J, Cao L, Li Z, Li Y. SIRT1 promotes GLUT1 expression and bladder cancer progression via regulation of glucose uptake. Hum Cell. 2019;32(2):193–201.10.1007/s13577-019-00237-5Suche in Google Scholar PubMed
[18] Simmons Jr GE, Pruitt WM, Pruitt K. Diverse roles of SIRT1 in cancer biology and lipid metabolism. Int J Mol Sci. 2015;16(1):950–65.10.3390/ijms16010950Suche in Google Scholar PubMed PubMed Central
[19] Alves-Fernandes DK, Jasiulionis MG. The role of SIRT1 on DNA damage response and epigenetic alterations in cancer. Int J Mol Sci. 2019;20(13):3153.10.3390/ijms20133153Suche in Google Scholar PubMed PubMed Central
[20] Garten A, Grohmann T, Kluckova K, Lavery GG, Kiess W, Penke M. Sorafenib-induced apoptosis in hepatocellular carcinoma is reversed by SIRT1. Int J Mol Sci. 2019;20(16):4048.10.3390/ijms20164048Suche in Google Scholar PubMed PubMed Central
[21] Zhang S, Yang Y, Huang S, Deng C, Zhou S, Yang J, et al. SIRT1 inhibits gastric cancer proliferation and metastasis via STAT3/MMP-13 signaling. J Cell Physiol. 2019;234(9):15395–406.10.1002/jcp.28186Suche in Google Scholar PubMed
[22] Jin J, Chu Z, Ma P, Meng Y, Yang Y. SIRT1 promotes the proliferation and metastasis of human pancreatic cancer cells. Tumour Biol. 2017;39(3):1010428317691180.10.1177/1010428317691180Suche in Google Scholar PubMed
[23] Yu L, Dong L, Li H, Liu Z, Luo Z, Duan G, et al. Ubiquitination- mediated degradation of SIRT1 by SMURF2 suppresses CRC cell proliferation and tumorigenesis. Oncogene. 2020;39(22):4450–64.10.1038/s41388-020-1298-0Suche in Google Scholar PubMed
[24] Ji K, Sun X, Liu Y, Du L, Wang Y, He N, et al. Regulation of apoptosis and radiation sensitization in lung cancer cells via the Sirt1/NF-κB/Smac pathway. Cell Physiol Biochem. 2018;48(1):304–16.10.1159/000491730Suche in Google Scholar PubMed
[25] Yu Q, Dong L, Li Y, Liu G. SIRT1 and HIF1α signaling in metabolism and immune responses. Cancer Lett. 2018;418:20–6.10.1016/j.canlet.2017.12.035Suche in Google Scholar PubMed
[26] Xu C, Wang L, Fozouni P, Evjen G, Chandra V, Jiang J, et al. SIRT1 is downregulated by autophagy in senescence and ageing. Nat Cell Biol. 2020t;22(10):1170–9.10.1038/s41556-020-00579-5Suche in Google Scholar PubMed PubMed Central
[27] Luo G, Jian Z, Zhu Y, Zhu Y, Chen B, Ma R, et al. Sirt1 promotes autophagy and inhibits apoptosis to protect cardiomyocytes from hypoxic stress. Int J Mol Med. 2019;43(5):2033–43.10.3892/ijmm.2019.4125Suche in Google Scholar PubMed PubMed Central
[28] Yang H, Bi Y, Xue L, Wang J, Lu Y, Zhang Z, et al. Multifaceted modulation of SIRT1 in cancer and inflammation. Crit Rev Oncog. 2015;20(1–2):49–64.10.1615/CritRevOncog.2014012374Suche in Google Scholar
© 2022 Yu-ling Zhang et al., published by De Gruyter
This work is licensed under the Creative Commons Attribution 4.0 International License.
Artikel in diesem Heft
- Research Articles
- AMBRA1 attenuates the proliferation of uveal melanoma cells
- A ceRNA network mediated by LINC00475 in papillary thyroid carcinoma
- Differences in complications between hepatitis B-related cirrhosis and alcohol-related cirrhosis
- Effect of gestational diabetes mellitus on lipid profile: A systematic review and meta-analysis
- Long noncoding RNA NR2F1-AS1 stimulates the tumorigenic behavior of non-small cell lung cancer cells by sponging miR-363-3p to increase SOX4
- Promising novel biomarkers and candidate small-molecule drugs for lung adenocarcinoma: Evidence from bioinformatics analysis of high-throughput data
- Plasmapheresis: Is it a potential alternative treatment for chronic urticaria?
- The biomarkers of key miRNAs and gene targets associated with extranodal NK/T-cell lymphoma
- Gene signature to predict prognostic survival of hepatocellular carcinoma
- Effects of miRNA-199a-5p on cell proliferation and apoptosis of uterine leiomyoma by targeting MED12
- Does diabetes affect paraneoplastic thrombocytosis in colorectal cancer?
- Is there any effect on imprinted genes H19, PEG3, and SNRPN during AOA?
- Leptin and PCSK9 concentrations are associated with vascular endothelial cytokines in patients with stable coronary heart disease
- Pericentric inversion of chromosome 6 and male fertility problems
- Staple line reinforcement with nebulized cyanoacrylate glue in laparoscopic sleeve gastrectomy: A propensity score-matched study
- Retrospective analysis of crescent score in clinical prognosis of IgA nephropathy
- Expression of DNM3 is associated with good outcome in colorectal cancer
- Activation of SphK2 contributes to adipocyte-induced EOC cell proliferation
- CRRT influences PICCO measurements in febrile critically ill patients
- SLCO4A1-AS1 mediates pancreatic cancer development via miR-4673/KIF21B axis
- lncRNA ACTA2-AS1 inhibits malignant phenotypes of gastric cancer cells
- circ_AKT3 knockdown suppresses cisplatin resistance in gastric cancer
- Prognostic value of nicotinamide N-methyltransferase in human cancers: Evidence from a meta-analysis and database validation
- GPC2 deficiency inhibits cell growth and metastasis in colon adenocarcinoma
- A pan-cancer analysis of the oncogenic role of Holliday junction recognition protein in human tumors
- Radiation increases COL1A1, COL3A1, and COL1A2 expression in breast cancer
- Association between preventable risk factors and metabolic syndrome
- miR-29c-5p knockdown reduces inflammation and blood–brain barrier disruption by upregulating LRP6
- Cardiac contractility modulation ameliorates myocardial metabolic remodeling in a rabbit model of chronic heart failure through activation of AMPK and PPAR-α pathway
- Quercitrin protects human bronchial epithelial cells from oxidative damage
- Smurf2 suppresses the metastasis of hepatocellular carcinoma via ubiquitin degradation of Smad2
- circRNA_0001679/miR-338-3p/DUSP16 axis aggravates acute lung injury
- Sonoclot’s usefulness in prediction of cardiopulmonary arrest prognosis: A proof of concept study
- Four drug metabolism-related subgroups of pancreatic adenocarcinoma in prognosis, immune infiltration, and gene mutation
- Decreased expression of miR-195 mediated by hypermethylation promotes osteosarcoma
- LMO3 promotes proliferation and metastasis of papillary thyroid carcinoma cells by regulating LIMK1-mediated cofilin and the β-catenin pathway
- Cx43 upregulation in HUVECs under stretch via TGF-β1 and cytoskeletal network
- Evaluation of menstrual irregularities after COVID-19 vaccination: Results of the MECOVAC survey
- Histopathologic findings on removed stomach after sleeve gastrectomy. Do they influence the outcome?
- Analysis of the expression and prognostic value of MT1-MMP, β1-integrin and YAP1 in glioma
- Optimal diagnosis of the skin cancer using a hybrid deep neural network and grasshopper optimization algorithm
- miR-223-3p alleviates TGF-β-induced epithelial-mesenchymal transition and extracellular matrix deposition by targeting SP3 in endometrial epithelial cells
- Clinical value of SIRT1 as a prognostic biomarker in esophageal squamous cell carcinoma, a systematic meta-analysis
- circ_0020123 promotes cell proliferation and migration in lung adenocarcinoma via PDZD8
- miR-22-5p regulates the self-renewal of spermatogonial stem cells by targeting EZH2
- hsa-miR-340-5p inhibits epithelial–mesenchymal transition in endometriosis by targeting MAP3K2 and inactivating MAPK/ERK signaling
- circ_0085296 inhibits the biological functions of trophoblast cells to promote the progression of preeclampsia via the miR-942-5p/THBS2 network
- TCD hemodynamics findings in the subacute phase of anterior circulation stroke patients treated with mechanical thrombectomy
- Development of a risk-stratification scoring system for predicting risk of breast cancer based on non-alcoholic fatty liver disease, non-alcoholic fatty pancreas disease, and uric acid
- Tollip promotes hepatocellular carcinoma progression via PI3K/AKT pathway
- circ_0062491 alleviates periodontitis via the miR-142-5p/IGF1 axis
- Human amniotic fluid as a source of stem cells
- lncRNA NONRATT013819.2 promotes transforming growth factor-β1-induced myofibroblastic transition of hepatic stellate cells by miR24-3p/lox
- NORAD modulates miR-30c-5p-LDHA to protect lung endothelial cells damage
- Idiopathic pulmonary fibrosis telemedicine management during COVID-19 outbreak
- Risk factors for adverse drug reactions associated with clopidogrel therapy
- Serum zinc associated with immunity and inflammatory markers in Covid-19
- The relationship between night shift work and breast cancer incidence: A systematic review and meta-analysis of observational studies
- LncRNA expression in idiopathic achalasia: New insight and preliminary exploration into pathogenesis
- Notoginsenoside R1 alleviates spinal cord injury through the miR-301a/KLF7 axis to activate Wnt/β-catenin pathway
- Moscatilin suppresses the inflammation from macrophages and T cells
- Zoledronate promotes ECM degradation and apoptosis via Wnt/β-catenin
- Epithelial-mesenchymal transition-related genes in coronary artery disease
- The effect evaluation of traditional vaginal surgery and transvaginal mesh surgery for severe pelvic organ prolapse: 5 years follow-up
- Repeated partial splenic artery embolization for hypersplenism improves platelet count
- Low expression of miR-27b in serum exosomes of non-small cell lung cancer facilitates its progression by affecting EGFR
- Exosomal hsa_circ_0000519 modulates the NSCLC cell growth and metastasis via miR-1258/RHOV axis
- miR-455-5p enhances 5-fluorouracil sensitivity in colorectal cancer cells by targeting PIK3R1 and DEPDC1
- The effect of tranexamic acid on the reduction of intraoperative and postoperative blood loss and thromboembolic risk in patients with hip fracture
- Isocitrate dehydrogenase 1 mutation in cholangiocarcinoma impairs tumor progression by sensitizing cells to ferroptosis
- Artemisinin protects against cerebral ischemia and reperfusion injury via inhibiting the NF-κB pathway
- A 16-gene signature associated with homologous recombination deficiency for prognosis prediction in patients with triple-negative breast cancer
- Lidocaine ameliorates chronic constriction injury-induced neuropathic pain through regulating M1/M2 microglia polarization
- MicroRNA 322-5p reduced neuronal inflammation via the TLR4/TRAF6/NF-κB axis in a rat epilepsy model
- miR-1273h-5p suppresses CXCL12 expression and inhibits gastric cancer cell invasion and metastasis
- Clinical characteristics of pneumonia patients of long course of illness infected with SARS-CoV-2
- circRNF20 aggravates the malignancy of retinoblastoma depending on the regulation of miR-132-3p/PAX6 axis
- Linezolid for resistant Gram-positive bacterial infections in children under 12 years: A meta-analysis
- Rack1 regulates pro-inflammatory cytokines by NF-κB in diabetic nephropathy
- Comprehensive analysis of molecular mechanism and a novel prognostic signature based on small nuclear RNA biomarkers in gastric cancer patients
- Smog and risk of maternal and fetal birth outcomes: A retrospective study in Baoding, China
- Let-7i-3p inhibits the cell cycle, proliferation, invasion, and migration of colorectal cancer cells via downregulating CCND1
- β2-Adrenergic receptor expression in subchondral bone of patients with varus knee osteoarthritis
- Possible impact of COVID-19 pandemic and lockdown on suicide behavior among patients in Southeast Serbia
- In vitro antimicrobial activity of ozonated oil in liposome eyedrop against multidrug-resistant bacteria
- Potential biomarkers for inflammatory response in acute lung injury
- A low serum uric acid concentration predicts a poor prognosis in adult patients with candidemia
- Antitumor activity of recombinant oncolytic vaccinia virus with human IL2
- ALKBH5 inhibits TNF-α-induced apoptosis of HUVECs through Bcl-2 pathway
- Risk prediction of cardiovascular disease using machine learning classifiers
- Value of ultrasonography parameters in diagnosing polycystic ovary syndrome
- Bioinformatics analysis reveals three key genes and four survival genes associated with youth-onset NSCLC
- Identification of autophagy-related biomarkers in patients with pulmonary arterial hypertension based on bioinformatics analysis
- Protective effects of glaucocalyxin A on the airway of asthmatic mice
- Overexpression of miR-100-5p inhibits papillary thyroid cancer progression via targeting FZD8
- Bioinformatics-based analysis of SUMOylation-related genes in hepatocellular carcinoma reveals a role of upregulated SAE1 in promoting cell proliferation
- Effectiveness and clinical benefits of new anti-diabetic drugs: A real life experience
- Identification of osteoporosis based on gene biomarkers using support vector machine
- Tanshinone IIA reverses oxaliplatin resistance in colorectal cancer through microRNA-30b-5p/AVEN axis
- miR-212-5p inhibits nasopharyngeal carcinoma progression by targeting METTL3
- Association of ST-T changes with all-cause mortality among patients with peripheral T-cell lymphomas
- LINC00665/miRNAs axis-mediated collagen type XI alpha 1 correlates with immune infiltration and malignant phenotypes in lung adenocarcinoma
- The perinatal factors that influence the excretion of fecal calprotectin in premature-born children
- Effect of femoral head necrosis cystic area on femoral head collapse and stress distribution in femoral head: A clinical and finite element study
- Does the use of 3D-printed cones give a chance to postpone the use of megaprostheses in patients with large bone defects in the knee joint?
- lncRNA HAGLR modulates myocardial ischemia–reperfusion injury in mice through regulating miR-133a-3p/MAPK1 axis
- Protective effect of ghrelin on intestinal I/R injury in rats
- In vivo knee kinematics of an innovative prosthesis design
- Relationship between the height of fibular head and the incidence and severity of knee osteoarthritis
- lncRNA WT1-AS attenuates hypoxia/ischemia-induced neuronal injury during cerebral ischemic stroke via miR-186-5p/XIAP axis
- Correlation of cardiac troponin T and APACHE III score with all-cause in-hospital mortality in critically ill patients with acute pulmonary embolism
- LncRNA LINC01857 reduces metastasis and angiogenesis in breast cancer cells via regulating miR-2052/CENPQ axis
- Endothelial cell-specific molecule 1 (ESM1) promoted by transcription factor SPI1 acts as an oncogene to modulate the malignant phenotype of endometrial cancer
- SELENBP1 inhibits progression of colorectal cancer by suppressing epithelial–mesenchymal transition
- Visfatin is negatively associated with coronary artery lesions in subjects with impaired fasting glucose
- Treatment and outcomes of mechanical complications of acute myocardial infarction during the Covid-19 era: A comparison with the pre-Covid-19 period. A systematic review and meta-analysis
- Neonatal stroke surveillance study protocol in the United Kingdom and Republic of Ireland
- Oncogenic role of TWF2 in human tumors: A pan-cancer analysis
- Mean corpuscular hemoglobin predicts the length of hospital stay independent of severity classification in patients with acute pancreatitis
- Association of gallstone and polymorphisms of UGT1A1*27 and UGT1A1*28 in patients with hepatitis B virus-related liver failure
- TGF-β1 upregulates Sar1a expression and induces procollagen-I secretion in hypertrophic scarring fibroblasts
- Antisense lncRNA PCNA-AS1 promotes esophageal squamous cell carcinoma progression through the miR-2467-3p/PCNA axis
- NK-cell dysfunction of acute myeloid leukemia in relation to the renin–angiotensin system and neurotransmitter genes
- The effect of dilution with glucose and prolonged injection time on dexamethasone-induced perineal irritation – A randomized controlled trial
- miR-146-5p restrains calcification of vascular smooth muscle cells by suppressing TRAF6
- Role of lncRNA MIAT/miR-361-3p/CCAR2 in prostate cancer cells
- lncRNA NORAD promotes lung cancer progression by competitively binding to miR-28-3p with E2F2
- Noninvasive diagnosis of AIH/PBC overlap syndrome based on prediction models
- lncRNA FAM230B is highly expressed in colorectal cancer and suppresses the maturation of miR-1182 to increase cell proliferation
- circ-LIMK1 regulates cisplatin resistance in lung adenocarcinoma by targeting miR-512-5p/HMGA1 axis
- LncRNA SNHG3 promoted cell proliferation, migration, and metastasis of esophageal squamous cell carcinoma via regulating miR-151a-3p/PFN2 axis
- Risk perception and affective state on work exhaustion in obstetrics during the COVID-19 pandemic
- lncRNA-AC130710/miR-129-5p/mGluR1 axis promote migration and invasion by activating PKCα-MAPK signal pathway in melanoma
- SNRPB promotes cell cycle progression in thyroid carcinoma via inhibiting p53
- Xylooligosaccharides and aerobic training regulate metabolism and behavior in rats with streptozotocin-induced type 1 diabetes
- Serpin family A member 1 is an oncogene in glioma and its translation is enhanced by NAD(P)H quinone dehydrogenase 1 through RNA-binding activity
- Silencing of CPSF7 inhibits the proliferation, migration, and invasion of lung adenocarcinoma cells by blocking the AKT/mTOR signaling pathway
- Ultrasound-guided lumbar plexus block versus transversus abdominis plane block for analgesia in children with hip dislocation: A double-blind, randomized trial
- Relationship of plasma MBP and 8-oxo-dG with brain damage in preterm
- Identification of a novel necroptosis-associated miRNA signature for predicting the prognosis in head and neck squamous cell carcinoma
- Delayed femoral vein ligation reduces operative time and blood loss during hip disarticulation in patients with extremity tumors
- The expression of ASAP3 and NOTCH3 and the clinicopathological characteristics of adult glioma patients
- Longitudinal analysis of factors related to Helicobacter pylori infection in Chinese adults
- HOXA10 enhances cell proliferation and suppresses apoptosis in esophageal cancer via activating p38/ERK signaling pathway
- Meta-analysis of early-life antibiotic use and allergic rhinitis
- Marital status and its correlation with age, race, and gender in prognosis of tonsil squamous cell carcinomas
- HPV16 E6E7 up-regulates KIF2A expression by activating JNK/c-Jun signal, is beneficial to migration and invasion of cervical cancer cells
- Amino acid profiles in the tissue and serum of patients with liver cancer
- Pain in critically ill COVID-19 patients: An Italian retrospective study
- Immunohistochemical distribution of Bcl-2 and p53 apoptotic markers in acetamiprid-induced nephrotoxicity
- Estradiol pretreatment in GnRH antagonist protocol for IVF/ICSI treatment
- Long non-coding RNAs LINC00689 inhibits the apoptosis of human nucleus pulposus cells via miR-3127-5p/ATG7 axis-mediated autophagy
- The relationship between oxygen therapy, drug therapy, and COVID-19 mortality
- Monitoring hypertensive disorders in pregnancy to prevent preeclampsia in pregnant women of advanced maternal age: Trial mimicking with retrospective data
- SETD1A promotes the proliferation and glycolysis of nasopharyngeal carcinoma cells by activating the PI3K/Akt pathway
- The role of Shunaoxin pills in the treatment of chronic cerebral hypoperfusion and its main pharmacodynamic components
- TET3 governs malignant behaviors and unfavorable prognosis of esophageal squamous cell carcinoma by activating the PI3K/AKT/GSK3β/β-catenin pathway
- Associations between morphokinetic parameters of temporary-arrest embryos and the clinical prognosis in FET cycles
- Long noncoding RNA WT1-AS regulates trophoblast proliferation, migration, and invasion via the microRNA-186-5p/CADM2 axis
- The incidence of bronchiectasis in chronic obstructive pulmonary disease
- Integrated bioinformatics analysis shows integrin alpha 3 is a prognostic biomarker for pancreatic cancer
- Inhibition of miR-21 improves pulmonary vascular responses in bronchopulmonary dysplasia by targeting the DDAH1/ADMA/NO pathway
- Comparison of hospitalized patients with severe pneumonia caused by COVID-19 and influenza A (H7N9 and H1N1): A retrospective study from a designated hospital
- lncRNA ZFAS1 promotes intervertebral disc degeneration by upregulating AAK1
- Pathological characteristics of liver injury induced by N,N-dimethylformamide: From humans to animal models
- lncRNA ELFN1-AS1 enhances the progression of colon cancer by targeting miR-4270 to upregulate AURKB
- DARS-AS1 modulates cell proliferation and migration of gastric cancer cells by regulating miR-330-3p/NAT10 axis
- Dezocine inhibits cell proliferation, migration, and invasion by targeting CRABP2 in ovarian cancer
- MGST1 alleviates the oxidative stress of trophoblast cells induced by hypoxia/reoxygenation and promotes cell proliferation, migration, and invasion by activating the PI3K/AKT/mTOR pathway
- Bifidobacterium lactis Probio-M8 ameliorated the symptoms of type 2 diabetes mellitus mice by changing ileum FXR-CYP7A1
- circRNA DENND1B inhibits tumorigenicity of clear cell renal cell carcinoma via miR-122-5p/TIMP2 axis
- EphA3 targeted by miR-3666 contributes to melanoma malignancy via activating ERK1/2 and p38 MAPK pathways
- Pacemakers and methylprednisolone pulse therapy in immune-related myocarditis concomitant with complete heart block
- miRNA-130a-3p targets sphingosine-1-phosphate receptor 1 to activate the microglial and astrocytes and to promote neural injury under the high glucose condition
- Review Articles
- Current management of cancer pain in Italy: Expert opinion paper
- Hearing loss and brain disorders: A review of multiple pathologies
- The rationale for using low-molecular weight heparin in the therapy of symptomatic COVID-19 patients
- Amyotrophic lateral sclerosis and delayed onset muscle soreness in light of the impaired blink and stretch reflexes – watch out for Piezo2
- Interleukin-35 in autoimmune dermatoses: Current concepts
- Recent discoveries in microbiota dysbiosis, cholangiocytic factors, and models for studying the pathogenesis of primary sclerosing cholangitis
- Advantages of ketamine in pediatric anesthesia
- Congenital adrenal hyperplasia. Role of dentist in early diagnosis
- Migraine management: Non-pharmacological points for patients and health care professionals
- Atherogenic index of plasma and coronary artery disease: A systematic review
- Physiological and modulatory role of thioredoxins in the cellular function
- Case Reports
- Intrauterine Bakri balloon tamponade plus cervical cerclage for the prevention and treatment of postpartum haemorrhage in late pregnancy complicated with acute aortic dissection: Case series
- A case of successful pembrolizumab monotherapy in a patient with advanced lung adenocarcinoma: Use of multiple biomarkers in combination for clinical practice
- Unusual neurological manifestations of bilateral medial medullary infarction: A case report
- Atypical symptoms of malignant hyperthermia: A rare causative mutation in the RYR1 gene
- A case report of dermatomyositis with the missed diagnosis of non-small cell lung cancer and concurrence of pulmonary tuberculosis
- A rare case of endometrial polyp complicated with uterine inversion: A case report and clinical management
- Spontaneous rupturing of splenic artery aneurysm: Another reason for fatal syncope and shock (Case report and literature review)
- Fungal infection mimicking COVID-19 infection – A case report
- Concurrent aspergillosis and cystic pulmonary metastases in a patient with tongue squamous cell carcinoma
- Paraganglioma-induced inverted takotsubo-like cardiomyopathy leading to cardiogenic shock successfully treated with extracorporeal membrane oxygenation
- Lineage switch from lymphoma to myeloid neoplasms: First case series from a single institution
- Trismus during tracheal extubation as a complication of general anaesthesia – A case report
- Simultaneous treatment of a pubovesical fistula and lymph node metastasis secondary to multimodal treatment for prostate cancer: Case report and review of the literature
- Two case reports of skin vasculitis following the COVID-19 immunization
- Ureteroiliac fistula after oncological surgery: Case report and review of the literature
- Synchronous triple primary malignant tumours in the bladder, prostate, and lung harbouring TP53 and MEK1 mutations accompanied with severe cardiovascular diseases: A case report
- Huge mucinous cystic neoplasms with adhesion to the left colon: A case report and literature review
- Commentary
- Commentary on “Clinicopathological features of programmed cell death-ligand 1 expression in patients with oral squamous cell carcinoma”
- Rapid Communication
- COVID-19 fear, post-traumatic stress, growth, and the role of resilience
- Erratum
- Erratum to “Tollip promotes hepatocellular carcinoma progression via PI3K/AKT pathway”
- Erratum to “Effect of femoral head necrosis cystic area on femoral head collapse and stress distribution in femoral head: A clinical and finite element study”
- Erratum to “lncRNA NORAD promotes lung cancer progression by competitively binding to miR-28-3p with E2F2”
- Retraction
- Expression and role of ABIN1 in sepsis: In vitro and in vivo studies
- Retraction to “miR-519d downregulates LEP expression to inhibit preeclampsia development”
- Special Issue Computational Intelligence Methodologies Meets Recurrent Cancers - Part II
- Usefulness of close surveillance for rectal cancer patients after neoadjuvant chemoradiotherapy
Artikel in diesem Heft
- Research Articles
- AMBRA1 attenuates the proliferation of uveal melanoma cells
- A ceRNA network mediated by LINC00475 in papillary thyroid carcinoma
- Differences in complications between hepatitis B-related cirrhosis and alcohol-related cirrhosis
- Effect of gestational diabetes mellitus on lipid profile: A systematic review and meta-analysis
- Long noncoding RNA NR2F1-AS1 stimulates the tumorigenic behavior of non-small cell lung cancer cells by sponging miR-363-3p to increase SOX4
- Promising novel biomarkers and candidate small-molecule drugs for lung adenocarcinoma: Evidence from bioinformatics analysis of high-throughput data
- Plasmapheresis: Is it a potential alternative treatment for chronic urticaria?
- The biomarkers of key miRNAs and gene targets associated with extranodal NK/T-cell lymphoma
- Gene signature to predict prognostic survival of hepatocellular carcinoma
- Effects of miRNA-199a-5p on cell proliferation and apoptosis of uterine leiomyoma by targeting MED12
- Does diabetes affect paraneoplastic thrombocytosis in colorectal cancer?
- Is there any effect on imprinted genes H19, PEG3, and SNRPN during AOA?
- Leptin and PCSK9 concentrations are associated with vascular endothelial cytokines in patients with stable coronary heart disease
- Pericentric inversion of chromosome 6 and male fertility problems
- Staple line reinforcement with nebulized cyanoacrylate glue in laparoscopic sleeve gastrectomy: A propensity score-matched study
- Retrospective analysis of crescent score in clinical prognosis of IgA nephropathy
- Expression of DNM3 is associated with good outcome in colorectal cancer
- Activation of SphK2 contributes to adipocyte-induced EOC cell proliferation
- CRRT influences PICCO measurements in febrile critically ill patients
- SLCO4A1-AS1 mediates pancreatic cancer development via miR-4673/KIF21B axis
- lncRNA ACTA2-AS1 inhibits malignant phenotypes of gastric cancer cells
- circ_AKT3 knockdown suppresses cisplatin resistance in gastric cancer
- Prognostic value of nicotinamide N-methyltransferase in human cancers: Evidence from a meta-analysis and database validation
- GPC2 deficiency inhibits cell growth and metastasis in colon adenocarcinoma
- A pan-cancer analysis of the oncogenic role of Holliday junction recognition protein in human tumors
- Radiation increases COL1A1, COL3A1, and COL1A2 expression in breast cancer
- Association between preventable risk factors and metabolic syndrome
- miR-29c-5p knockdown reduces inflammation and blood–brain barrier disruption by upregulating LRP6
- Cardiac contractility modulation ameliorates myocardial metabolic remodeling in a rabbit model of chronic heart failure through activation of AMPK and PPAR-α pathway
- Quercitrin protects human bronchial epithelial cells from oxidative damage
- Smurf2 suppresses the metastasis of hepatocellular carcinoma via ubiquitin degradation of Smad2
- circRNA_0001679/miR-338-3p/DUSP16 axis aggravates acute lung injury
- Sonoclot’s usefulness in prediction of cardiopulmonary arrest prognosis: A proof of concept study
- Four drug metabolism-related subgroups of pancreatic adenocarcinoma in prognosis, immune infiltration, and gene mutation
- Decreased expression of miR-195 mediated by hypermethylation promotes osteosarcoma
- LMO3 promotes proliferation and metastasis of papillary thyroid carcinoma cells by regulating LIMK1-mediated cofilin and the β-catenin pathway
- Cx43 upregulation in HUVECs under stretch via TGF-β1 and cytoskeletal network
- Evaluation of menstrual irregularities after COVID-19 vaccination: Results of the MECOVAC survey
- Histopathologic findings on removed stomach after sleeve gastrectomy. Do they influence the outcome?
- Analysis of the expression and prognostic value of MT1-MMP, β1-integrin and YAP1 in glioma
- Optimal diagnosis of the skin cancer using a hybrid deep neural network and grasshopper optimization algorithm
- miR-223-3p alleviates TGF-β-induced epithelial-mesenchymal transition and extracellular matrix deposition by targeting SP3 in endometrial epithelial cells
- Clinical value of SIRT1 as a prognostic biomarker in esophageal squamous cell carcinoma, a systematic meta-analysis
- circ_0020123 promotes cell proliferation and migration in lung adenocarcinoma via PDZD8
- miR-22-5p regulates the self-renewal of spermatogonial stem cells by targeting EZH2
- hsa-miR-340-5p inhibits epithelial–mesenchymal transition in endometriosis by targeting MAP3K2 and inactivating MAPK/ERK signaling
- circ_0085296 inhibits the biological functions of trophoblast cells to promote the progression of preeclampsia via the miR-942-5p/THBS2 network
- TCD hemodynamics findings in the subacute phase of anterior circulation stroke patients treated with mechanical thrombectomy
- Development of a risk-stratification scoring system for predicting risk of breast cancer based on non-alcoholic fatty liver disease, non-alcoholic fatty pancreas disease, and uric acid
- Tollip promotes hepatocellular carcinoma progression via PI3K/AKT pathway
- circ_0062491 alleviates periodontitis via the miR-142-5p/IGF1 axis
- Human amniotic fluid as a source of stem cells
- lncRNA NONRATT013819.2 promotes transforming growth factor-β1-induced myofibroblastic transition of hepatic stellate cells by miR24-3p/lox
- NORAD modulates miR-30c-5p-LDHA to protect lung endothelial cells damage
- Idiopathic pulmonary fibrosis telemedicine management during COVID-19 outbreak
- Risk factors for adverse drug reactions associated with clopidogrel therapy
- Serum zinc associated with immunity and inflammatory markers in Covid-19
- The relationship between night shift work and breast cancer incidence: A systematic review and meta-analysis of observational studies
- LncRNA expression in idiopathic achalasia: New insight and preliminary exploration into pathogenesis
- Notoginsenoside R1 alleviates spinal cord injury through the miR-301a/KLF7 axis to activate Wnt/β-catenin pathway
- Moscatilin suppresses the inflammation from macrophages and T cells
- Zoledronate promotes ECM degradation and apoptosis via Wnt/β-catenin
- Epithelial-mesenchymal transition-related genes in coronary artery disease
- The effect evaluation of traditional vaginal surgery and transvaginal mesh surgery for severe pelvic organ prolapse: 5 years follow-up
- Repeated partial splenic artery embolization for hypersplenism improves platelet count
- Low expression of miR-27b in serum exosomes of non-small cell lung cancer facilitates its progression by affecting EGFR
- Exosomal hsa_circ_0000519 modulates the NSCLC cell growth and metastasis via miR-1258/RHOV axis
- miR-455-5p enhances 5-fluorouracil sensitivity in colorectal cancer cells by targeting PIK3R1 and DEPDC1
- The effect of tranexamic acid on the reduction of intraoperative and postoperative blood loss and thromboembolic risk in patients with hip fracture
- Isocitrate dehydrogenase 1 mutation in cholangiocarcinoma impairs tumor progression by sensitizing cells to ferroptosis
- Artemisinin protects against cerebral ischemia and reperfusion injury via inhibiting the NF-κB pathway
- A 16-gene signature associated with homologous recombination deficiency for prognosis prediction in patients with triple-negative breast cancer
- Lidocaine ameliorates chronic constriction injury-induced neuropathic pain through regulating M1/M2 microglia polarization
- MicroRNA 322-5p reduced neuronal inflammation via the TLR4/TRAF6/NF-κB axis in a rat epilepsy model
- miR-1273h-5p suppresses CXCL12 expression and inhibits gastric cancer cell invasion and metastasis
- Clinical characteristics of pneumonia patients of long course of illness infected with SARS-CoV-2
- circRNF20 aggravates the malignancy of retinoblastoma depending on the regulation of miR-132-3p/PAX6 axis
- Linezolid for resistant Gram-positive bacterial infections in children under 12 years: A meta-analysis
- Rack1 regulates pro-inflammatory cytokines by NF-κB in diabetic nephropathy
- Comprehensive analysis of molecular mechanism and a novel prognostic signature based on small nuclear RNA biomarkers in gastric cancer patients
- Smog and risk of maternal and fetal birth outcomes: A retrospective study in Baoding, China
- Let-7i-3p inhibits the cell cycle, proliferation, invasion, and migration of colorectal cancer cells via downregulating CCND1
- β2-Adrenergic receptor expression in subchondral bone of patients with varus knee osteoarthritis
- Possible impact of COVID-19 pandemic and lockdown on suicide behavior among patients in Southeast Serbia
- In vitro antimicrobial activity of ozonated oil in liposome eyedrop against multidrug-resistant bacteria
- Potential biomarkers for inflammatory response in acute lung injury
- A low serum uric acid concentration predicts a poor prognosis in adult patients with candidemia
- Antitumor activity of recombinant oncolytic vaccinia virus with human IL2
- ALKBH5 inhibits TNF-α-induced apoptosis of HUVECs through Bcl-2 pathway
- Risk prediction of cardiovascular disease using machine learning classifiers
- Value of ultrasonography parameters in diagnosing polycystic ovary syndrome
- Bioinformatics analysis reveals three key genes and four survival genes associated with youth-onset NSCLC
- Identification of autophagy-related biomarkers in patients with pulmonary arterial hypertension based on bioinformatics analysis
- Protective effects of glaucocalyxin A on the airway of asthmatic mice
- Overexpression of miR-100-5p inhibits papillary thyroid cancer progression via targeting FZD8
- Bioinformatics-based analysis of SUMOylation-related genes in hepatocellular carcinoma reveals a role of upregulated SAE1 in promoting cell proliferation
- Effectiveness and clinical benefits of new anti-diabetic drugs: A real life experience
- Identification of osteoporosis based on gene biomarkers using support vector machine
- Tanshinone IIA reverses oxaliplatin resistance in colorectal cancer through microRNA-30b-5p/AVEN axis
- miR-212-5p inhibits nasopharyngeal carcinoma progression by targeting METTL3
- Association of ST-T changes with all-cause mortality among patients with peripheral T-cell lymphomas
- LINC00665/miRNAs axis-mediated collagen type XI alpha 1 correlates with immune infiltration and malignant phenotypes in lung adenocarcinoma
- The perinatal factors that influence the excretion of fecal calprotectin in premature-born children
- Effect of femoral head necrosis cystic area on femoral head collapse and stress distribution in femoral head: A clinical and finite element study
- Does the use of 3D-printed cones give a chance to postpone the use of megaprostheses in patients with large bone defects in the knee joint?
- lncRNA HAGLR modulates myocardial ischemia–reperfusion injury in mice through regulating miR-133a-3p/MAPK1 axis
- Protective effect of ghrelin on intestinal I/R injury in rats
- In vivo knee kinematics of an innovative prosthesis design
- Relationship between the height of fibular head and the incidence and severity of knee osteoarthritis
- lncRNA WT1-AS attenuates hypoxia/ischemia-induced neuronal injury during cerebral ischemic stroke via miR-186-5p/XIAP axis
- Correlation of cardiac troponin T and APACHE III score with all-cause in-hospital mortality in critically ill patients with acute pulmonary embolism
- LncRNA LINC01857 reduces metastasis and angiogenesis in breast cancer cells via regulating miR-2052/CENPQ axis
- Endothelial cell-specific molecule 1 (ESM1) promoted by transcription factor SPI1 acts as an oncogene to modulate the malignant phenotype of endometrial cancer
- SELENBP1 inhibits progression of colorectal cancer by suppressing epithelial–mesenchymal transition
- Visfatin is negatively associated with coronary artery lesions in subjects with impaired fasting glucose
- Treatment and outcomes of mechanical complications of acute myocardial infarction during the Covid-19 era: A comparison with the pre-Covid-19 period. A systematic review and meta-analysis
- Neonatal stroke surveillance study protocol in the United Kingdom and Republic of Ireland
- Oncogenic role of TWF2 in human tumors: A pan-cancer analysis
- Mean corpuscular hemoglobin predicts the length of hospital stay independent of severity classification in patients with acute pancreatitis
- Association of gallstone and polymorphisms of UGT1A1*27 and UGT1A1*28 in patients with hepatitis B virus-related liver failure
- TGF-β1 upregulates Sar1a expression and induces procollagen-I secretion in hypertrophic scarring fibroblasts
- Antisense lncRNA PCNA-AS1 promotes esophageal squamous cell carcinoma progression through the miR-2467-3p/PCNA axis
- NK-cell dysfunction of acute myeloid leukemia in relation to the renin–angiotensin system and neurotransmitter genes
- The effect of dilution with glucose and prolonged injection time on dexamethasone-induced perineal irritation – A randomized controlled trial
- miR-146-5p restrains calcification of vascular smooth muscle cells by suppressing TRAF6
- Role of lncRNA MIAT/miR-361-3p/CCAR2 in prostate cancer cells
- lncRNA NORAD promotes lung cancer progression by competitively binding to miR-28-3p with E2F2
- Noninvasive diagnosis of AIH/PBC overlap syndrome based on prediction models
- lncRNA FAM230B is highly expressed in colorectal cancer and suppresses the maturation of miR-1182 to increase cell proliferation
- circ-LIMK1 regulates cisplatin resistance in lung adenocarcinoma by targeting miR-512-5p/HMGA1 axis
- LncRNA SNHG3 promoted cell proliferation, migration, and metastasis of esophageal squamous cell carcinoma via regulating miR-151a-3p/PFN2 axis
- Risk perception and affective state on work exhaustion in obstetrics during the COVID-19 pandemic
- lncRNA-AC130710/miR-129-5p/mGluR1 axis promote migration and invasion by activating PKCα-MAPK signal pathway in melanoma
- SNRPB promotes cell cycle progression in thyroid carcinoma via inhibiting p53
- Xylooligosaccharides and aerobic training regulate metabolism and behavior in rats with streptozotocin-induced type 1 diabetes
- Serpin family A member 1 is an oncogene in glioma and its translation is enhanced by NAD(P)H quinone dehydrogenase 1 through RNA-binding activity
- Silencing of CPSF7 inhibits the proliferation, migration, and invasion of lung adenocarcinoma cells by blocking the AKT/mTOR signaling pathway
- Ultrasound-guided lumbar plexus block versus transversus abdominis plane block for analgesia in children with hip dislocation: A double-blind, randomized trial
- Relationship of plasma MBP and 8-oxo-dG with brain damage in preterm
- Identification of a novel necroptosis-associated miRNA signature for predicting the prognosis in head and neck squamous cell carcinoma
- Delayed femoral vein ligation reduces operative time and blood loss during hip disarticulation in patients with extremity tumors
- The expression of ASAP3 and NOTCH3 and the clinicopathological characteristics of adult glioma patients
- Longitudinal analysis of factors related to Helicobacter pylori infection in Chinese adults
- HOXA10 enhances cell proliferation and suppresses apoptosis in esophageal cancer via activating p38/ERK signaling pathway
- Meta-analysis of early-life antibiotic use and allergic rhinitis
- Marital status and its correlation with age, race, and gender in prognosis of tonsil squamous cell carcinomas
- HPV16 E6E7 up-regulates KIF2A expression by activating JNK/c-Jun signal, is beneficial to migration and invasion of cervical cancer cells
- Amino acid profiles in the tissue and serum of patients with liver cancer
- Pain in critically ill COVID-19 patients: An Italian retrospective study
- Immunohistochemical distribution of Bcl-2 and p53 apoptotic markers in acetamiprid-induced nephrotoxicity
- Estradiol pretreatment in GnRH antagonist protocol for IVF/ICSI treatment
- Long non-coding RNAs LINC00689 inhibits the apoptosis of human nucleus pulposus cells via miR-3127-5p/ATG7 axis-mediated autophagy
- The relationship between oxygen therapy, drug therapy, and COVID-19 mortality
- Monitoring hypertensive disorders in pregnancy to prevent preeclampsia in pregnant women of advanced maternal age: Trial mimicking with retrospective data
- SETD1A promotes the proliferation and glycolysis of nasopharyngeal carcinoma cells by activating the PI3K/Akt pathway
- The role of Shunaoxin pills in the treatment of chronic cerebral hypoperfusion and its main pharmacodynamic components
- TET3 governs malignant behaviors and unfavorable prognosis of esophageal squamous cell carcinoma by activating the PI3K/AKT/GSK3β/β-catenin pathway
- Associations between morphokinetic parameters of temporary-arrest embryos and the clinical prognosis in FET cycles
- Long noncoding RNA WT1-AS regulates trophoblast proliferation, migration, and invasion via the microRNA-186-5p/CADM2 axis
- The incidence of bronchiectasis in chronic obstructive pulmonary disease
- Integrated bioinformatics analysis shows integrin alpha 3 is a prognostic biomarker for pancreatic cancer
- Inhibition of miR-21 improves pulmonary vascular responses in bronchopulmonary dysplasia by targeting the DDAH1/ADMA/NO pathway
- Comparison of hospitalized patients with severe pneumonia caused by COVID-19 and influenza A (H7N9 and H1N1): A retrospective study from a designated hospital
- lncRNA ZFAS1 promotes intervertebral disc degeneration by upregulating AAK1
- Pathological characteristics of liver injury induced by N,N-dimethylformamide: From humans to animal models
- lncRNA ELFN1-AS1 enhances the progression of colon cancer by targeting miR-4270 to upregulate AURKB
- DARS-AS1 modulates cell proliferation and migration of gastric cancer cells by regulating miR-330-3p/NAT10 axis
- Dezocine inhibits cell proliferation, migration, and invasion by targeting CRABP2 in ovarian cancer
- MGST1 alleviates the oxidative stress of trophoblast cells induced by hypoxia/reoxygenation and promotes cell proliferation, migration, and invasion by activating the PI3K/AKT/mTOR pathway
- Bifidobacterium lactis Probio-M8 ameliorated the symptoms of type 2 diabetes mellitus mice by changing ileum FXR-CYP7A1
- circRNA DENND1B inhibits tumorigenicity of clear cell renal cell carcinoma via miR-122-5p/TIMP2 axis
- EphA3 targeted by miR-3666 contributes to melanoma malignancy via activating ERK1/2 and p38 MAPK pathways
- Pacemakers and methylprednisolone pulse therapy in immune-related myocarditis concomitant with complete heart block
- miRNA-130a-3p targets sphingosine-1-phosphate receptor 1 to activate the microglial and astrocytes and to promote neural injury under the high glucose condition
- Review Articles
- Current management of cancer pain in Italy: Expert opinion paper
- Hearing loss and brain disorders: A review of multiple pathologies
- The rationale for using low-molecular weight heparin in the therapy of symptomatic COVID-19 patients
- Amyotrophic lateral sclerosis and delayed onset muscle soreness in light of the impaired blink and stretch reflexes – watch out for Piezo2
- Interleukin-35 in autoimmune dermatoses: Current concepts
- Recent discoveries in microbiota dysbiosis, cholangiocytic factors, and models for studying the pathogenesis of primary sclerosing cholangitis
- Advantages of ketamine in pediatric anesthesia
- Congenital adrenal hyperplasia. Role of dentist in early diagnosis
- Migraine management: Non-pharmacological points for patients and health care professionals
- Atherogenic index of plasma and coronary artery disease: A systematic review
- Physiological and modulatory role of thioredoxins in the cellular function
- Case Reports
- Intrauterine Bakri balloon tamponade plus cervical cerclage for the prevention and treatment of postpartum haemorrhage in late pregnancy complicated with acute aortic dissection: Case series
- A case of successful pembrolizumab monotherapy in a patient with advanced lung adenocarcinoma: Use of multiple biomarkers in combination for clinical practice
- Unusual neurological manifestations of bilateral medial medullary infarction: A case report
- Atypical symptoms of malignant hyperthermia: A rare causative mutation in the RYR1 gene
- A case report of dermatomyositis with the missed diagnosis of non-small cell lung cancer and concurrence of pulmonary tuberculosis
- A rare case of endometrial polyp complicated with uterine inversion: A case report and clinical management
- Spontaneous rupturing of splenic artery aneurysm: Another reason for fatal syncope and shock (Case report and literature review)
- Fungal infection mimicking COVID-19 infection – A case report
- Concurrent aspergillosis and cystic pulmonary metastases in a patient with tongue squamous cell carcinoma
- Paraganglioma-induced inverted takotsubo-like cardiomyopathy leading to cardiogenic shock successfully treated with extracorporeal membrane oxygenation
- Lineage switch from lymphoma to myeloid neoplasms: First case series from a single institution
- Trismus during tracheal extubation as a complication of general anaesthesia – A case report
- Simultaneous treatment of a pubovesical fistula and lymph node metastasis secondary to multimodal treatment for prostate cancer: Case report and review of the literature
- Two case reports of skin vasculitis following the COVID-19 immunization
- Ureteroiliac fistula after oncological surgery: Case report and review of the literature
- Synchronous triple primary malignant tumours in the bladder, prostate, and lung harbouring TP53 and MEK1 mutations accompanied with severe cardiovascular diseases: A case report
- Huge mucinous cystic neoplasms with adhesion to the left colon: A case report and literature review
- Commentary
- Commentary on “Clinicopathological features of programmed cell death-ligand 1 expression in patients with oral squamous cell carcinoma”
- Rapid Communication
- COVID-19 fear, post-traumatic stress, growth, and the role of resilience
- Erratum
- Erratum to “Tollip promotes hepatocellular carcinoma progression via PI3K/AKT pathway”
- Erratum to “Effect of femoral head necrosis cystic area on femoral head collapse and stress distribution in femoral head: A clinical and finite element study”
- Erratum to “lncRNA NORAD promotes lung cancer progression by competitively binding to miR-28-3p with E2F2”
- Retraction
- Expression and role of ABIN1 in sepsis: In vitro and in vivo studies
- Retraction to “miR-519d downregulates LEP expression to inhibit preeclampsia development”
- Special Issue Computational Intelligence Methodologies Meets Recurrent Cancers - Part II
- Usefulness of close surveillance for rectal cancer patients after neoadjuvant chemoradiotherapy

