Abstract
Transcutaneous electrical stimulation is a common treatment option for patients suffering from spinal cord injury or stroke. Two major difficulties arise when employing electrical stimulation in patients: Accurate stimulation electrode placement and configuration of optimal stimulation parameters. Optimizing the stimulation parameters has the advantage to reduce muscle fatigue after repetitive stimulation. Here we present a newly developed system which is able to automatically find the optimal individual stimulation intensity by varying the pulse length. The effectiveness is measured with flex sensors. By adapting the stimulation parameters, the effect of muscle fatigue can be compensated, allowing for a more stable movement upon stimulation over time.
1 Introduction
Functional electrical stimulation (FES) has been used to help patients who suffer from stroke or spinal chord injury for many years now [1]. FES is able to support patients in activities of daily living, like walking or grasping [2]. Performing electrical stimulation in most cases arises two core questions: Where the optimal placement of the stimulation electrodes is and which stimulation intensity should be applied [3]. Addressing the former question, prior studies have investigated the optimal electrode placement by using electrode arrays [4]. Addressing the latter is an equivalently complex question, as parameters vary from patient to patient. Providing neither too strong, nor too weak stimulation intensity is crucial, as too weak stimulation leads to an insufficiently opened hand or incorrect step while walking. Too strong stimulation exhaust the muscles quickly without any further benefit, leading to muscle fatigue [5].
Here we present a newly developed system which is able to increase the intensity of stimulation in a stepwise manner until the optimal point is reached. We demonstrate it’s use in a chronic stroke patient with hand paresis, focusing the opening of the hand. In order to cancel out fatigue, we regulate the intensity, allowing a stable opening of the affected hand.
2 System design
Figure 1 shows the typical stimulation sequence for the hand opening. At first stimulation is too weak and causes no reaction. After the intensity is increased, the hand starts to open and soon the maximal extension is reached. Increasing the intensity even more would lead to an inefficient stimulation, as the hand is not opened significantly further, so lowering the intensity, leading back to the point of optimal stimulation, has to be done. The stimulation intensity is then kept constant until the user decides to stop the stimulation or the hand starts closing due to fatigue. To keep the hand open at a constant level, the intensity has to be increased.
The whole system is divided into three parts. The first part consists of the implementation of a program on the stimulator (here Motionstim8), controlling stimulation intensity. The second part compromises the feedback system to analyze stimulation response and measure the efficiency of the stimulation applied. The third part covers the software implementation of the overall control system on the used micro-controller board.
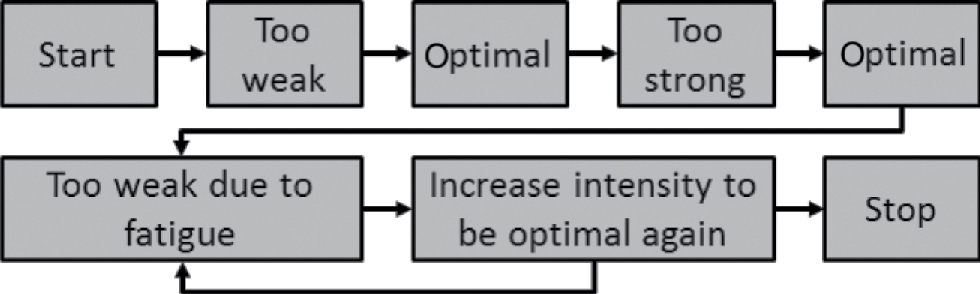
Flow diagram of stimulation status during a typical grasping motion.
2.1 Stimulator program
We used the commercially available stimulator Motionstim8 (Medel GmbH, Hamburg, Germany). The advantage of the Motionstim8 is the accessibility of four digital inputs, which can be used to control the stimulator to a certain degree. As the amplitude is fixed and can only be changed manually, the pulse length was used to control the intensity of the stimulation. The available Motionsoft software was used to program the course of stimulation. It is able to handle four inputs and up to 30 state machine states. Figure 2 shows the implementation of the state machine for the controllable stimulation intensity program.
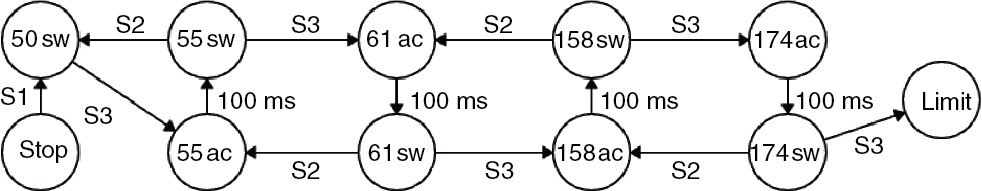
State Machine of Motionstim8 implementation.
The secure start point, which is needed to prevent unwanted stimulation, is program stage 00-stop, where the stimulation is deactivated. The following state can only be arrived as long as a low signal is applied to input 1, therefore acting as a security switch for interruption or lost connection. The state 01-50-switch activates continuous stimulation with a pulse width of 50 μs and is also ready to switch to a higher intensity state if necessary, which can be controlled with input 3, letting the state machine move to the next state, 02-55-active.
In the second stimulation intensity state the applied pulse width is 55 μs. After a delay of 100 ms to prevent unintended fast switching, the stimulator moves over to the third stage 03-55-switch, which acts accordingly to 03-55-switch, also allowing to switch to a lower intensity state with input 2.
Each following stimulation intensity is implemented the same way as the intensity with a pulse width of 55 μs, containing an active state and a switching state. For N stimulation intensities this leads to a total number of 2*(N − 1) + 3 states. As the Motionstim8 is able to handle up to 30 states, a total of 14 different pulse widths, 50 μs to 174 μs in steps of 10% each, have been implemented.
Reaching a pulse width of 174 μs and trying to increase again leads the stimulator into a warning state and gives the user feedback that the maximum intensity is reached. Stimulation is then deactivated and the stimulation amplitude has to be increased manually to maintain correct control.
2.2 Feedback system
To control the efficiency of the electrical stimulation, it is necessary to measure the degree of hand opening during the stimulation. For this reason, hand movement was measured using flex sensors. They were attached to a wristband and kept close to the fingers with ring attachments as seen in Figure 3. The system has two sensors that are monitored, one for the index finger and one for the ring finger.
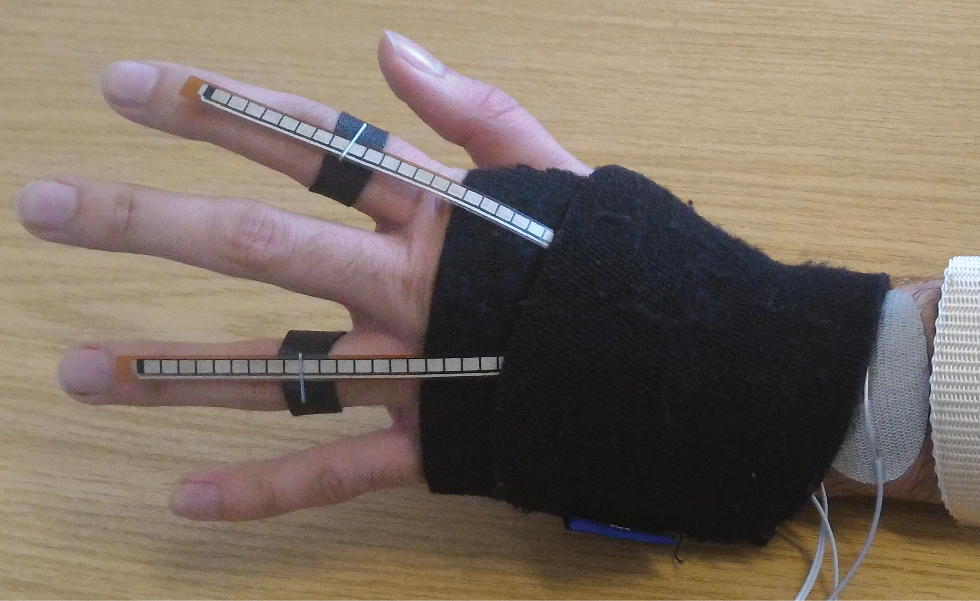
flex sensors with wristband and attachment rings for hand movement characterization of a stroke patient.
2.3 Micro-controller implementation
To decide whether or not a stimulation is efficient, an Arduino Uno micro-controller board was used to calculate the efficiency and filter the sensor values using a median filter. The flex sensors were connected, using a voltage divider, to the analog input pins of the Arduino, thus enabling the Arduino to characterize the hand opening of the stimulated hand.
The Arduino implementation is loop based. Each loops duration is 10 ms in total and has the same order of instructions, as described in the following:
Check current sensor values
Transmit detailed data via USB
Check control state machine (see Figure 4)
Wait until total time of 10 ms has passed
The code for checking the sensor values as well as recording and sending the data were placed outside of the state machine, hence allowing better timing control. In addition the device can also be used as a pure monitoring device without using the control algorithm.
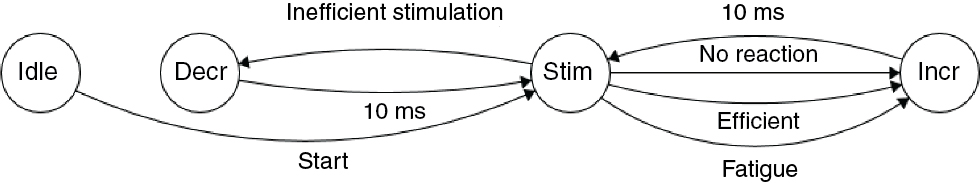
Arduino state machine for stimulation control.
As shown in Figure 4, the state machine for stimulation control is divided into four main states Idle, Stimulation, Increase and Decrease.
Idle – In Idle state, the stimulation is disabled, setting output 1 to high, therefore keeping the Motionstim8 in 00-stop. In addition, the system determines the current sensor level. This is done to be able to determine an adapting starting point in order to calculate the degree of hand opening. Idle state is left when a stimulation shall be started as triggered by the user.
Stimulation – The state Stimulation handles the continuous stimulation of the hand and checks whether the intensity has to be increased or decreased. As seen in Figure 4, there are three reasons to increase stimulation intensity and one reason to decrease stimulation intensity. They correspond to the three increments of stimulation intensity shown in Figure 1. Increase intensity until there is either a reaction, until stimulation becomes inefficient or to cancel out fatigue.
Firstly, if the stimulation intensity is too weak and no reaction occurred, the intensity has to be increased, leaving the state and moving over to Increase. This usually happens in the first stages of stimulation intensity, prior to reaching the threshold of successful stimulation. The second reason for increasing the intensity occurs as soon as the hand starts too open and the movement is strong enough to be determined as effective, respectively a dramatic change of sensor values. This is true if the degree of hand opening exceeds approximately 10% of the maximum hand opening degree. Thirdly, when the hand starts to close due to muscle fatigue, the intensity has to be increased again. This decision is based on a comparison between the degree of hand opening during the optimal stimulation point and the current sensor level.
The decrement of stimulation intensity is used to get back from overshooting the optimal stimulation point as shown in Figure 1. This happens as soon as a stimulation is marked as inefficient. In practice this means that the hand is already open and an increasing intensity cannot open the hand even more, therefore wasting energy and stressing the patient. The state is then changed to Decrease.
Increase – In order to deliver a low output signal on output 3 that can be detected by the Motionstim8, the Increase state keeps the output at a constant low level for 10 ms. This is extremely important for reliable operation, as both systems, Arduino and Motionstim8, are not synchronized. After the delay the state switches back to Stimulation. During Increase the output of the stimulator is still active, stimulation and control are not interrupted by short pauses.
Decrease – This state behaves in the same way as Increase. In Decrease output 2 is set to low instead of output 3, compared to Increase.
It should be noted that the Motionstim8 prioritizes lower number inputs, e.g. input 1 has a higher priority than input 2. Therefore stopping the stimulation before decreasing the intensity is prioritized and the increase of intensity is treated with the lowest priority.
3 System demonstration
The developed system was tested on ten healthy subjects and one stroke patient. Two different test scenarios were performed. The first test characterizes a single hand opening and keeps the hand open for two minutes straight. This reflects the case of a closing hand due to fatigue and forces the control system to increase the intensity. As shown in Figure 5, the initial increasing intensity is performed until the optimal stage is reached, surpassed by one stage to ensure that the optimum is really reached and then lowered back to the optimal level. In addition to that a decrease of hand opening due to fatigue triggers another increment of the intensity, as intended.
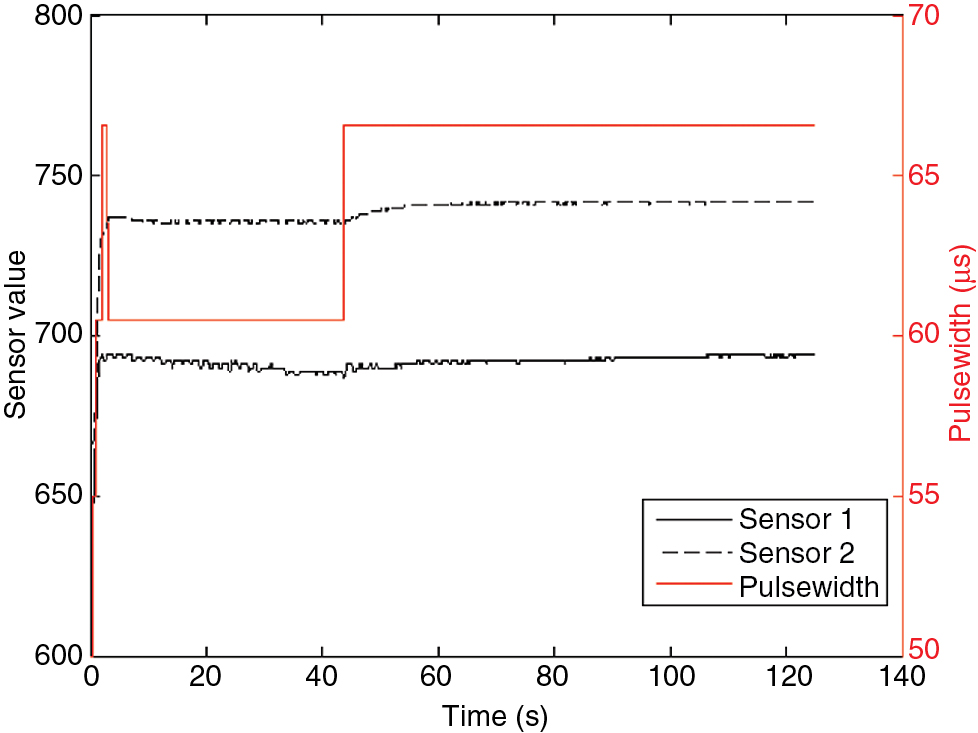
Continuous stimulation with initial intensity ramping and correction due to fatigue cancellation of one test subject.
The second test scenario consists of several opening and closing motions of the hand in a short interval, mimicking grasping motions. As shown in Figure 6, six adjacent grasping motions were successfully performed. Even though they vary in intensity, each single motion is approximately equal, with the same degree of hand opening.
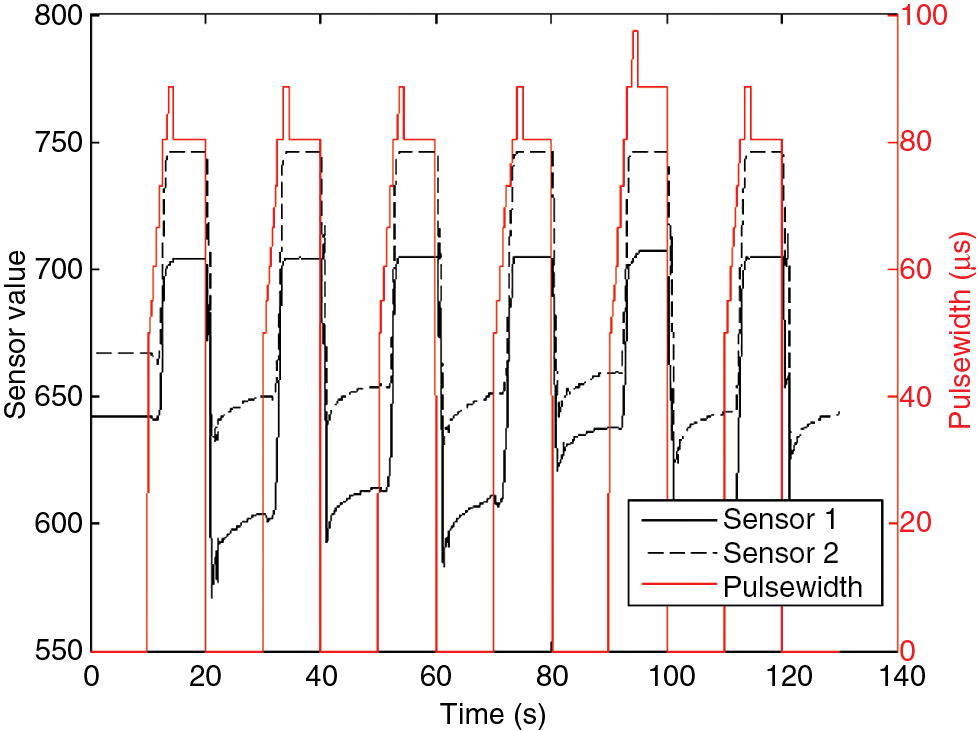
Repeating grasping motions with varying needed intensities and approximately same hand opening of one test subject.
4 Discussion and conclusion
The developed system is able to open the hand as intended, thereby reacting to different influences like changing starting point, fatigue or different intensities needed. As the system is currently only evaluating one of the flex sensors, one future improvement would be to include the second sensor value into the threshold comparison.
Another improvement would be to use the end value of a prior hand-opening sequence in order to determine more accurate thresholds and decrease ramp up time to the needed intensity. Hence prior values could be used as an approximate target for every new stimulation. In addition, the threshold values for optimal stimulation could then be adjusted, as current values are now solely based on experience and an approximation of 10% of an opened hand.
Author’s Statement
Research funding: This work was supported by a grant from the Federal Ministry of Education and Research (BMBF, ESiMED [16 M3201]). Conflict of interest: Authors state no conflict of interest. Material and Methods: Informed consent: Informed consent has been obtained from all individuals included in this study. Ethical approval: The research related to human use complies with all the relevant national regulations, institutional policies and was performed in accordance with the tenets of the Helsinki Declaration, and has been approved by the authors’ institutional review board or equivalent committee.
References
[1] Quandt F, Hummel FC. The influence of functional electrical stimulation on hand motor recovery in stroke patients: a review. Exp Transl Stroke Med. 2014;6:1–7.10.1186/2040-7378-6-9Search in Google Scholar
[2] Doucet BM, Lam A, Griffin L. Neuromuscular electrical stimulation for skeletal muscle function. Yale J Biol Med. 2012;85:201–15.Search in Google Scholar
[3] Gobbo M, Maffiuletti NA, Orizio C, Minetto MA. Muscle motor point identification is essential for optimizing neuromuscular electrical stimulation use. J Neuroeng Rehabil. 2014;11:1–6.10.1186/1743-0003-11-17Search in Google Scholar
[4] Heller BW, Clarke AJ, Good TR, Healey TJ, Nair S, Pratt EJ, et al. Automated setup of functional electrical stimulation for drop foot using a novel 64 channel prototype stimulator and electrode array: results from a gait-lab based study. Med Eng Phys. 2013;35:74–81.10.1016/j.medengphy.2012.03.012Search in Google Scholar
[5] Jones DA, Bigland-Ritchie B, Edwards RHT. Excitation frequency and muscle fatigue: mechanical responses during voluntary and stimulated contractions. Exp Neurol. 1979;64;401–13.10.1016/0014-4886(79)90279-6Search in Google Scholar
©2016 Aljoscha Reinert et al., licensee De Gruyter.
This work is licensed under the Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 License.
Articles in the same Issue
- Synthesis and characterization of PIL/pNIPAAm hybrid hydrogels
- Novel blood protein based scaffolds for cardiovascular tissue engineering
- Cell adhesion and viability of human endothelial cells on electrospun polymer scaffolds
- Effects of heat treatment and welding process on superelastic behaviour and microstructure of micro electron beam welded NiTi
- Long-term stable modifications of silicone elastomer for improved hemocompatibility
- The effect of thermal treatment on the mechanical properties of PLLA tubular specimens
- Biocompatible wear-resistant thick ceramic coating
- Protection of active implant electronics with organosilicon open air plasma coating for plastic overmolding
- Examination of dielectric strength of thin Parylene C films under various conditions
- Open air plasma deposited antimicrobial SiOx/TiOx composite films for biomedical applications
- Systemic analysis about residual chloroform in PLLA films
- A macrophage model of osseointegration
- Towards in silico prognosis using big data
- Technical concept and evaluation of a novel shoulder simulator with adaptive muscle force generation and free motion
- Usability evaluation of a locomotor therapy device considering different strategies
- Hypoxia-on-a-chip
- Integration of a semi-automatic in-vitro RFA procedure into an experimental setup
- Fabrication of MEMS-based 3D-μECoG-MEAs
- High speed digital interfacing for a neural data acquisition system
- Bionic forceps for the handling of sensitive tissue
- Experimental studies on 3D printing of barium titanate ceramics for medical applications
- Patient specific root-analogue dental implants – additive manufacturing and finite element analysis
- 3D printing – a key technology for tailored biomedical cell culture lab ware
- 3D printing of hydrogels in a temperature controlled environment with high spatial resolution
- Biocompatibility of photopolymers for additive manufacturing
- Biochemical piezoresistive sensors based on pH- and glucose-sensitive hydrogels for medical applications
- Novel wireless measurement system of pressure dedicated to in vivo studies
- Portable auricular device for real-time swallow and chew detection
- Detection of miRNA using a surface plasmon resonance biosensor and antibody amplification
- Simulation and evaluation of stimulation scenarios for targeted vestibular nerve excitation
- Deep brain stimulation: increasing efficiency by alternative waveforms
- Prediction of immediately occurring microsleep events from brain electric signals
- Determining cardiac vagal threshold from short term heart rate complexity
- Classification of cardiac excitation patterns during atrial fibrillation
- An algorithm to automatically determine the cycle length coverage to identify rotational activity during atrial fibrillation – a simulation study
- Deriving respiration from high resolution 12-channel-ECG during cycling exercise
- Reducing of gradient induced artifacts on the ECG signal during MRI examinations using Wilcoxon filter
- Automatic detection and mapping of double potentials in intracardiac electrograms
- Modeling the pelvic region for non-invasive pelvic intraoperative neuromonitoring
- Postprocessing algorithm for automated analysis of pelvic intraoperative neuromonitoring signals
- Best practice: surgeon driven application in pelvic operations
- Vasomotor assessment by camera-based photoplethysmography
- Classification of morphologic changes in photoplethysmographic waveforms
- Novel computation of pulse transit time from multi-channel PPG signals by wavelet transform
- Efficient design of FIR filter based low-pass differentiators for biomedical signal processing
- Nonlinear causal influences assessed by mutual compression entropy
- Comparative study of methods for solving the correspondence problem in EMD applications
- fNIRS for future use in auditory diagnostics
- Semi-automated detection of fractional shortening in zebrafish embryo heart videos
- Blood pressure measurement on the cheek
- Derivation of the respiratory rate from directly and indirectly measured respiratory signals using autocorrelation
- Left cardiac atrioventricular delay and inter-ventricular delay in cardiac resynchronization therapy responder and non-responder
- An automatic systolic peak detector of blood pressure waveforms using 4th order cumulants
- Real-time QRS detection using integrated variance for ECG gated cardiac MRI
- Preprocessing of unipolar signals acquired by a novel intracardiac mapping system
- In-vitro experiments to characterize ventricular electromechanics
- Continuous non-invasive monitoring of blood pressure in the operating room: a cuffless optical technology at the fingertip
- Application of microwave sensor technology in cardiovascular disease for plaque detection
- Artificial blood circulatory and special Ultrasound Doppler probes for detecting and sizing gaseous embolism
- Detection of microsleep events in a car driving simulation study using electrocardiographic features
- A method to determine the kink resistance of stents and stent delivery systems according to international standards
- Comparison of stented bifurcation and straight vessel 3D-simulation with a prior simulated velocity profile inlet
- Transient Euler-Lagrange/DEM simulation of stent thrombosis
- Automated control of the laser welding process of heart valve scaffolds
- Automation of a test bench for accessing the bendability of electrospun vascular grafts
- Influence of storage conditions on the release of growth factors in platelet-rich blood derivatives
- Cryopreservation of cells using defined serum-free cryoprotective agents
- New bioreactor vessel for tissue engineering of human nasal septal chondrocytes
- Determination of the membrane hydraulic permeability of MSCs
- Climate retainment in carbon dioxide incubators
- Multiple factors influencing OR ventilation system effectiveness
- Evaluation of an app-based stress protocol
- Medication process in Styrian hospitals
- Control tower to surgical theater
- Development of a skull phantom for the assessment of implant X-ray visibility
- Surgical navigation with QR codes
- Investigation of the pressure gradient of embolic protection devices
- Computer assistance in femoral derotation osteotomy: a bottom-up approach
- Automatic depth scanning system for 3D infrared thermography
- A service for monitoring the quality of intraoperative cone beam CT images
- Resectoscope with an easy to use twist mechanism for improved handling
- In vitro simulation of distribution processes following intramuscular injection
- Adjusting inkjet printhead parameters to deposit drugs into micro-sized reservoirs
- A flexible standalone system with integrated sensor feedback for multi-pad electrode FES of the hand
- Smart control for functional electrical stimulation with optimal pulse intensity
- Tactile display on the remaining hand for unilateral hand amputees
- Effects of sustained electrical stimulation on spasticity assessed by the pendulum test
- An improved tracking framework for ultrasound probe localization in image-guided radiosurgery
- Improvement of a subviral particle tracker by the use of a LAP-Kalman-algorithm
- Learning discriminative classification models for grading anal intraepithelial neoplasia
- Regularization of EIT reconstruction based on multi-scales wavelet transforms
- Assessing MRI susceptibility artefact through an indicator of image distortion
- EyeGuidance – a computer controlled system to guide eye movements
- A framework for feedback-based segmentation of 3D image stacks
- Doppler optical coherence tomography as a promising tool for detecting fluid in the human middle ear
- 3D Local in vivo Environment (LivE) imaging for single cell protein analysis of bone tissue
- Inside-Out access strategy using new trans-vascular catheter approach
- US/MRI fusion with new optical tracking and marker approach for interventional procedures inside the MRI suite
- Impact of different registration methods in MEG source analysis
- 3D segmentation of thyroid ultrasound images using active contours
- Designing a compact MRI motion phantom
- Cerebral cortex classification by conditional random fields applied to intraoperative thermal imaging
- Classification of indirect immunofluorescence images using thresholded local binary count features
- Analysis of muscle fatigue conditions using time-frequency images and GLCM features
- Numerical evaluation of image parameters of ETR-1
- Fabrication of a compliant phantom of the human aortic arch for use in Particle Image Velocimetry (PIV) experimentation
- Effect of the number of electrodes on the reconstructed lung shape in electrical impedance tomography
- Hardware dependencies of GPU-accelerated beamformer performances for microwave breast cancer detection
- Computer assisted assessment of progressing osteoradionecrosis of the jaw for clinical diagnosis and treatment
- Evaluation of reconstruction parameters of electrical impedance tomography on aorta detection during saline bolus injection
- Evaluation of open-source software for the lung segmentation
- Automatic determination of lung features of CF patients in CT scans
- Image analysis of self-organized multicellular patterns
- Effect of key parameters on synthesis of superparamagnetic nanoparticles (SPIONs)
- Radiopacity assessment of neurovascular implants
- Development of a desiccant based dielectric for monitoring humidity conditions in miniaturized hermetic implantable packages
- Development of an artifact-free aneurysm clip
- Enhancing the regeneration of bone defects by alkalizing the peri-implant zone – an in vitro approach
- Rapid prototyping of replica knee implants for in vitro testing
- Protecting ultra- and hyperhydrophilic implant surfaces in dry state from loss of wettability
- Advanced wettability analysis of implant surfaces
- Patient-specific hip prostheses designed by surgeons
- Plasma treatment on novel carbon fiber reinforced PEEK cages to enhance bioactivity
- Wear of a total intervertebral disc prosthesis
- Digital health and digital biomarkers – enabling value chains on health data
- Usability in the lifecycle of medical software development
- Influence of different test gases in a non-destructive 100% quality control system for medical devices
- Device development guided by user satisfaction survey on auricular vagus nerve stimulation
- Empirical assessment of the time course of innovation in biomedical engineering: first results of a comparative approach
- Effect of left atrial hypertrophy on P-wave morphology in a computational model
- Simulation of intracardiac electrograms around acute ablation lesions
- Parametrization of activation based cardiac electrophysiology models using bidomain model simulations
- Assessment of nasal resistance using computational fluid dynamics
- Resistance in a non-linear autoregressive model of pulmonary mechanics
- Inspiratory and expiratory elastance in a non-linear autoregressive model of pulmonary mechanics
- Determination of regional lung function in cystic fibrosis using electrical impedance tomography
- Development of parietal bone surrogates for parietal graft lift training
- Numerical simulation of mechanically stimulated bone remodelling
- Conversion of engineering stresses to Cauchy stresses in tensile and compression tests of thermoplastic polymers
- Numerical examinations of simplified spondylodesis models concerning energy absorption in magnetic resonance imaging
- Principle study on the signal connection at transabdominal fetal pulse oximetry
- Influence of Siluron® insertion on model drug distribution in the simulated vitreous body
- Evaluating different approaches to identify a three parameter gas exchange model
- Effects of fibrosis on the extracellular potential based on 3D reconstructions from histological sections of heart tissue
- From imaging to hemodynamics – how reconstruction kernels influence the blood flow predictions in intracranial aneurysms
- Flow optimised design of a novel point-of-care diagnostic device for the detection of disease specific biomarkers
- Improved FPGA controlled artificial vascular system for plethysmographic measurements
- Minimally spaced electrode positions for multi-functional chest sensors: ECG and respiratory signal estimation
- Automated detection of alveolar arches for nasoalveolar molding in cleft lip and palate treatment
- Control scheme selection in human-machine- interfaces by analysis of activity signals
- Event-based sampling for reducing communication load in realtime human motion analysis by wireless inertial sensor networks
- Automatic pairing of inertial sensors to lower limb segments – a plug-and-play approach
- Contactless respiratory monitoring system for magnetic resonance imaging applications using a laser range sensor
- Interactive monitoring system for visual respiratory biofeedback
- Development of a low-cost senor based aid for visually impaired people
- Patient assistive system for the shoulder joint
- A passive beating heart setup for interventional cardiology training
Articles in the same Issue
- Synthesis and characterization of PIL/pNIPAAm hybrid hydrogels
- Novel blood protein based scaffolds for cardiovascular tissue engineering
- Cell adhesion and viability of human endothelial cells on electrospun polymer scaffolds
- Effects of heat treatment and welding process on superelastic behaviour and microstructure of micro electron beam welded NiTi
- Long-term stable modifications of silicone elastomer for improved hemocompatibility
- The effect of thermal treatment on the mechanical properties of PLLA tubular specimens
- Biocompatible wear-resistant thick ceramic coating
- Protection of active implant electronics with organosilicon open air plasma coating for plastic overmolding
- Examination of dielectric strength of thin Parylene C films under various conditions
- Open air plasma deposited antimicrobial SiOx/TiOx composite films for biomedical applications
- Systemic analysis about residual chloroform in PLLA films
- A macrophage model of osseointegration
- Towards in silico prognosis using big data
- Technical concept and evaluation of a novel shoulder simulator with adaptive muscle force generation and free motion
- Usability evaluation of a locomotor therapy device considering different strategies
- Hypoxia-on-a-chip
- Integration of a semi-automatic in-vitro RFA procedure into an experimental setup
- Fabrication of MEMS-based 3D-μECoG-MEAs
- High speed digital interfacing for a neural data acquisition system
- Bionic forceps for the handling of sensitive tissue
- Experimental studies on 3D printing of barium titanate ceramics for medical applications
- Patient specific root-analogue dental implants – additive manufacturing and finite element analysis
- 3D printing – a key technology for tailored biomedical cell culture lab ware
- 3D printing of hydrogels in a temperature controlled environment with high spatial resolution
- Biocompatibility of photopolymers for additive manufacturing
- Biochemical piezoresistive sensors based on pH- and glucose-sensitive hydrogels for medical applications
- Novel wireless measurement system of pressure dedicated to in vivo studies
- Portable auricular device for real-time swallow and chew detection
- Detection of miRNA using a surface plasmon resonance biosensor and antibody amplification
- Simulation and evaluation of stimulation scenarios for targeted vestibular nerve excitation
- Deep brain stimulation: increasing efficiency by alternative waveforms
- Prediction of immediately occurring microsleep events from brain electric signals
- Determining cardiac vagal threshold from short term heart rate complexity
- Classification of cardiac excitation patterns during atrial fibrillation
- An algorithm to automatically determine the cycle length coverage to identify rotational activity during atrial fibrillation – a simulation study
- Deriving respiration from high resolution 12-channel-ECG during cycling exercise
- Reducing of gradient induced artifacts on the ECG signal during MRI examinations using Wilcoxon filter
- Automatic detection and mapping of double potentials in intracardiac electrograms
- Modeling the pelvic region for non-invasive pelvic intraoperative neuromonitoring
- Postprocessing algorithm for automated analysis of pelvic intraoperative neuromonitoring signals
- Best practice: surgeon driven application in pelvic operations
- Vasomotor assessment by camera-based photoplethysmography
- Classification of morphologic changes in photoplethysmographic waveforms
- Novel computation of pulse transit time from multi-channel PPG signals by wavelet transform
- Efficient design of FIR filter based low-pass differentiators for biomedical signal processing
- Nonlinear causal influences assessed by mutual compression entropy
- Comparative study of methods for solving the correspondence problem in EMD applications
- fNIRS for future use in auditory diagnostics
- Semi-automated detection of fractional shortening in zebrafish embryo heart videos
- Blood pressure measurement on the cheek
- Derivation of the respiratory rate from directly and indirectly measured respiratory signals using autocorrelation
- Left cardiac atrioventricular delay and inter-ventricular delay in cardiac resynchronization therapy responder and non-responder
- An automatic systolic peak detector of blood pressure waveforms using 4th order cumulants
- Real-time QRS detection using integrated variance for ECG gated cardiac MRI
- Preprocessing of unipolar signals acquired by a novel intracardiac mapping system
- In-vitro experiments to characterize ventricular electromechanics
- Continuous non-invasive monitoring of blood pressure in the operating room: a cuffless optical technology at the fingertip
- Application of microwave sensor technology in cardiovascular disease for plaque detection
- Artificial blood circulatory and special Ultrasound Doppler probes for detecting and sizing gaseous embolism
- Detection of microsleep events in a car driving simulation study using electrocardiographic features
- A method to determine the kink resistance of stents and stent delivery systems according to international standards
- Comparison of stented bifurcation and straight vessel 3D-simulation with a prior simulated velocity profile inlet
- Transient Euler-Lagrange/DEM simulation of stent thrombosis
- Automated control of the laser welding process of heart valve scaffolds
- Automation of a test bench for accessing the bendability of electrospun vascular grafts
- Influence of storage conditions on the release of growth factors in platelet-rich blood derivatives
- Cryopreservation of cells using defined serum-free cryoprotective agents
- New bioreactor vessel for tissue engineering of human nasal septal chondrocytes
- Determination of the membrane hydraulic permeability of MSCs
- Climate retainment in carbon dioxide incubators
- Multiple factors influencing OR ventilation system effectiveness
- Evaluation of an app-based stress protocol
- Medication process in Styrian hospitals
- Control tower to surgical theater
- Development of a skull phantom for the assessment of implant X-ray visibility
- Surgical navigation with QR codes
- Investigation of the pressure gradient of embolic protection devices
- Computer assistance in femoral derotation osteotomy: a bottom-up approach
- Automatic depth scanning system for 3D infrared thermography
- A service for monitoring the quality of intraoperative cone beam CT images
- Resectoscope with an easy to use twist mechanism for improved handling
- In vitro simulation of distribution processes following intramuscular injection
- Adjusting inkjet printhead parameters to deposit drugs into micro-sized reservoirs
- A flexible standalone system with integrated sensor feedback for multi-pad electrode FES of the hand
- Smart control for functional electrical stimulation with optimal pulse intensity
- Tactile display on the remaining hand for unilateral hand amputees
- Effects of sustained electrical stimulation on spasticity assessed by the pendulum test
- An improved tracking framework for ultrasound probe localization in image-guided radiosurgery
- Improvement of a subviral particle tracker by the use of a LAP-Kalman-algorithm
- Learning discriminative classification models for grading anal intraepithelial neoplasia
- Regularization of EIT reconstruction based on multi-scales wavelet transforms
- Assessing MRI susceptibility artefact through an indicator of image distortion
- EyeGuidance – a computer controlled system to guide eye movements
- A framework for feedback-based segmentation of 3D image stacks
- Doppler optical coherence tomography as a promising tool for detecting fluid in the human middle ear
- 3D Local in vivo Environment (LivE) imaging for single cell protein analysis of bone tissue
- Inside-Out access strategy using new trans-vascular catheter approach
- US/MRI fusion with new optical tracking and marker approach for interventional procedures inside the MRI suite
- Impact of different registration methods in MEG source analysis
- 3D segmentation of thyroid ultrasound images using active contours
- Designing a compact MRI motion phantom
- Cerebral cortex classification by conditional random fields applied to intraoperative thermal imaging
- Classification of indirect immunofluorescence images using thresholded local binary count features
- Analysis of muscle fatigue conditions using time-frequency images and GLCM features
- Numerical evaluation of image parameters of ETR-1
- Fabrication of a compliant phantom of the human aortic arch for use in Particle Image Velocimetry (PIV) experimentation
- Effect of the number of electrodes on the reconstructed lung shape in electrical impedance tomography
- Hardware dependencies of GPU-accelerated beamformer performances for microwave breast cancer detection
- Computer assisted assessment of progressing osteoradionecrosis of the jaw for clinical diagnosis and treatment
- Evaluation of reconstruction parameters of electrical impedance tomography on aorta detection during saline bolus injection
- Evaluation of open-source software for the lung segmentation
- Automatic determination of lung features of CF patients in CT scans
- Image analysis of self-organized multicellular patterns
- Effect of key parameters on synthesis of superparamagnetic nanoparticles (SPIONs)
- Radiopacity assessment of neurovascular implants
- Development of a desiccant based dielectric for monitoring humidity conditions in miniaturized hermetic implantable packages
- Development of an artifact-free aneurysm clip
- Enhancing the regeneration of bone defects by alkalizing the peri-implant zone – an in vitro approach
- Rapid prototyping of replica knee implants for in vitro testing
- Protecting ultra- and hyperhydrophilic implant surfaces in dry state from loss of wettability
- Advanced wettability analysis of implant surfaces
- Patient-specific hip prostheses designed by surgeons
- Plasma treatment on novel carbon fiber reinforced PEEK cages to enhance bioactivity
- Wear of a total intervertebral disc prosthesis
- Digital health and digital biomarkers – enabling value chains on health data
- Usability in the lifecycle of medical software development
- Influence of different test gases in a non-destructive 100% quality control system for medical devices
- Device development guided by user satisfaction survey on auricular vagus nerve stimulation
- Empirical assessment of the time course of innovation in biomedical engineering: first results of a comparative approach
- Effect of left atrial hypertrophy on P-wave morphology in a computational model
- Simulation of intracardiac electrograms around acute ablation lesions
- Parametrization of activation based cardiac electrophysiology models using bidomain model simulations
- Assessment of nasal resistance using computational fluid dynamics
- Resistance in a non-linear autoregressive model of pulmonary mechanics
- Inspiratory and expiratory elastance in a non-linear autoregressive model of pulmonary mechanics
- Determination of regional lung function in cystic fibrosis using electrical impedance tomography
- Development of parietal bone surrogates for parietal graft lift training
- Numerical simulation of mechanically stimulated bone remodelling
- Conversion of engineering stresses to Cauchy stresses in tensile and compression tests of thermoplastic polymers
- Numerical examinations of simplified spondylodesis models concerning energy absorption in magnetic resonance imaging
- Principle study on the signal connection at transabdominal fetal pulse oximetry
- Influence of Siluron® insertion on model drug distribution in the simulated vitreous body
- Evaluating different approaches to identify a three parameter gas exchange model
- Effects of fibrosis on the extracellular potential based on 3D reconstructions from histological sections of heart tissue
- From imaging to hemodynamics – how reconstruction kernels influence the blood flow predictions in intracranial aneurysms
- Flow optimised design of a novel point-of-care diagnostic device for the detection of disease specific biomarkers
- Improved FPGA controlled artificial vascular system for plethysmographic measurements
- Minimally spaced electrode positions for multi-functional chest sensors: ECG and respiratory signal estimation
- Automated detection of alveolar arches for nasoalveolar molding in cleft lip and palate treatment
- Control scheme selection in human-machine- interfaces by analysis of activity signals
- Event-based sampling for reducing communication load in realtime human motion analysis by wireless inertial sensor networks
- Automatic pairing of inertial sensors to lower limb segments – a plug-and-play approach
- Contactless respiratory monitoring system for magnetic resonance imaging applications using a laser range sensor
- Interactive monitoring system for visual respiratory biofeedback
- Development of a low-cost senor based aid for visually impaired people
- Patient assistive system for the shoulder joint
- A passive beating heart setup for interventional cardiology training

