Abstract
Our aim was to evaluate lung injury due to oxidative stress and antioxidant activity levels in an infrarenal ischemia–reperfusion model and to compare prevention effects of single and combined use of propofol and remifentanil. In this study, a total of 40 adult Wistar Albino rats were randomly divided into five groups of eight rats as SHAM, physiological saline, intraperitoneal propofol, remifentanil, and propofol and remifentanil groups. Blood and tissue samples were obtained after 80 min of reperfusion. The malondialdehyde (MDA) level, a measure of lipid peroxidation, was measured in lung tissue samples and red blood cells; additionally, total oxidant status and total antioxidant capacity of lung tissues were measured and histopathological examination was performed. Distant organ (lung) injury developed due to lower extremity ischemia–reperfusion was created by infrarenal aortic clamping. The lipid peroxidation product MDA and total oxidant levels were increased, but there was insufficient antioxidant protection both in the lung tissues and red blood cells. While propofol prevented this injury consistent with its proposed antioxidant properties; no protective effect of remifentanil was observed. On the contrary, it showed oxidative stress increasing effect. This study concluded that the antioxidant effect of propofol was suppressed by remifentanil in the case of combined use.
1 Introduction
It has been shown that ischemia–reperfusion (I/R) injury is not only limited to the tissue exposed to ischemia but the other distant organs are also affected by some mediators and toxic products like oxygen radicals, cytokines, complement proteins, prostaglandins and thromboxane released to the systemic circulation [1,2,3]. One of the distant organs mostly affected by I/R injury is the lungs. Lung injury that occurs following I/R leads to significant postoperative mortality and morbidity. In the case of lung injury caused by I/R, the findings are hypoxemia, pulmonary hypertension, reduced lung compliance and nonhydrostatic pulmonary edema and the severity of the disease may vary from a temporary subclinical condition to a serious condition, resulting in acute respiratory distress syndrome (ARDS) [4,5,6,7].
Various studies have shown the protective effects of antioxidant compounds against distant organ injury developing after acute I/R injury. Although there have been a large number of drugs or substances that have been studied for their antioxidant effects and are being used for that purpose, anesthetic substances have a different and important place among them [8,9,10,11,12,13,14,15]. One of these anesthetic substances that have been greatly emphasized is propofol. Due to its structural characteristics, it has free radical scavenging properties. As propofol is highly lipid-soluble, it particularly accumulates on lipophilic membranes, which are very sensitive to oxidative injury, and may increase or prevent the decrease in antioxidant capacity [16,17,18,19].
Remifentanil is the only opioid metabolized to its inactive metabolites by nonspecific plasma and tissue esterases. It is widely distributed in plasma, red blood cells and interstitial structures. Myocardial protective effects of remifentanil against I/R injury have been reported in several studies [20,21,22].
Our aim was to evaluate distal organ lung injury in terms of oxidative stress and antioxidant activity levels in an infrarenal ischemia–reperfusion (I/R) model and to compare the antioxidant and lung injury prevention effects of single and combined use of propofol and remifentanil as preconditioning.
2 Materials and methods
The study was performed in Erciyes University Experimental Research and Application Center in accordance with the “Guiding Principles for Research Involving Animals and Human Beings,” by the approval of the Institutional Animal Care and Use Committee of Erciyes University (Approval number: 11/62). In this study, 40 male Wistar albino rats, 5 months old, weighing 200 ± 40 g were used. During the experiments, all rats were kept in a 10 h light/14 h dark cycle, at a room temperature of 24 ± 2°C, and were fed with standard pellet and tap water.
Rats were divided randomly into five experiment groups, each containing 8 rats. Group 1 (SHAM) rats underwent laparotomy, closed, and after 100 min their tissue and blood samples were obtained; they were not treated with any substances during the experiment. Following laparotomy, Group 2 (PS) rats were infused with physiological saline, in the same amount of drug volume that the other groups received. While Group 3 (PRO) and Group 4 (REM) rats received 50 mg kg−1 h−1 propofol and 20 μg kg−1 min−1 remifentanil, respectively; Group 5 (PRO + REM) rats received 20 μg kg−1 min−1 remifentanil and 50 mg kg−1 h−1 propofol infusion starting 10 min before ischemia and continued for 30 min during ischemia. After 60 min of reperfusion, their tissue and blood samples were obtained.
2.1 Ischemia–reperfusion model
On the day of the study, the rats were weighed and anesthetized using intraperitoneal 1.6 mg kg−1 urethane. Following anesthesia, the abdomen of rats was dissected and the infrarenal abdominal aorta was explored; by placing an atraumatic vascular clamp, ischemia was achieved. In order to prevent fluid and heat loss, the abdominal region of the rat was closed using gauze soaked with warm physiological saline under a heating lamp and the body temperature of the rats was kept at 37 ± 1°C. The drugs were given intraperitoneally using an infusion pump; the infusion was started 10 min before ischemia and continued during ischemia. After 30 min of ischemia, the clamp was removed; restoring blood flow and perfusion were re-established at the distal tissues. After 60 min of reperfusion, intracardiac blood samples and lung tissue samples were obtained for histopathological and biochemical evaluations.
The lung tissue samples were washed with physiological saline and were divided into two parts: the part separated for histological examination was put in 10% formaldehyde, and the other part, the lung tissue sample, was stored at −70°C for biochemical measurements. In blood samples, hemorheological parameters were tested within 2 h, the remaining blood was centrifuged at 2,500 rpm for 10 min to separate plasma and red blood cells (RBC). RBC were washed three times with physiological saline and both RBC and plasma were stored at −20°C for biochemical measurements.
2.2 Biochemical measurements
The measurement of malondialdehyde (MDA), a product of lipid peroxidation, is based on the spectrophotometric reaction of MDA with thiobarbituric acid (TBA), forming a pink colored complex showing maximum absorbance at 532 nm wavelength [23].
The method developed by Ohkawa et al. was used in the assessment of MDA levels in lung tissue samples [24]. The supernatant obtained by centrifugation of tissue homogenates (1/10 w/v) was used: 0.1 mL of supernatants was put into a glass tube with a stopper, and 0.1 mL of sodium dodecyl sulfate (SDS), 0.75 mL of acetic acid, 0.75 mL of TBA and 0.3 mL of distilled water were added and the mixture was stirred. The tightly closed tubes were brewed in a boiling water bath for 60 min. Then, 0.5 mL of distilled water and 2.5 mL of n-butanol/pyridine mixture were added to the tubes, and the tubes were cooled with tap water and mixed with a vortex. Following extraction, the absorbance of the pink-colored organic phase that was formed on the upper part of the tubes, which were centrifuged at 4°C at 4,000 rpm for 15 min, was measured with a spectrophotometer at 532 nm (Unicam Helios Beta), against blind control that was formed with distilled water in the same way. Quantitation was done using a standard curve. Tissue MDA levels were calculated (nmol/ml) per milligram protein (nmol MDA/mg protein).
In lung tissue homogenates, total oxidative stress (TOS), total antioxidant capacity (TAC) and oxidative stress index (OSI) were measured using commercial kits (Rel Assay Kit Diagnostics® Gaziantep, Turkey) by Erel’s specific fully automated measurement method [25,26]. The total oxidative stress measurement method is based on the oxidation of bivalent ferrous iron to trivalent ferric iron by the oxidants present in the sample. In an acidic medium, ferric iron ions form a colored complex with xylenol and are read spectrophotometrically at a wavelength of 660 nm.
The experiment is calibrated by H2O2, and the values are expressed as μmol Trolox equivalent/mg protein. The total antioxidant capacity method is based on the measurement of the characteristic color formed by total antioxidants of the sample with more stable 2,2′-azino-bis (3-ethylbenz-thiazoline-6-sulfonic acid) (ABTS) radicals at 530 nm and is expressed as mmol Trolox equivalent/mg protein. The oxidative stress index was calculated by the following formula: OSI = [(TOS, μmol Trolox equivalent units/mg protein)/(TAC, mmol Trolox equivalent units/mg protein)].
2.3 Histological methods
The collected tissue samples from the right inferior lobe were fixed in 10% neutral formalin solution for 72 h at room temperature. The fixed tissues were examined under a light microscope, and paraffin blocks were formed. The prepared blocks were cut using a microtome (Leica SM 2000, Germany), and 4–5 μm thick sections were mounted on polylysine-coated slides. The sections were stained using hematoxylin–eosin to assess the structural changes, examined under light microscopy, and assessed in terms of histopathological parameters.
2.4 Statistical analysis
Shapiro–Wilk test was used to test normality, and one-way ANOVA test was performed for inter-group comparisons. If there is a significant difference, post-hoc Scheffe test was used to reveal the group that made the difference. Data are presented as mean ± SD.
All analysis was done using SPSS Statistics 20.0 (IBM-SPSS Inc., Chicago, IL) software program. A p value <0.05 was accepted as the significance level.
3 Results
3.1 Erythrocyte and lung tissue MDA values
The levels of MDA, an oxidative stress indicator and lipid peroxidation product, in lung tissue samples and RBC are presented in Table 1.
MDA levels in lung tissues and RBC
| Groups | Erythrocyte MDA (nmol/g Hb) | Lung MDA (nmol/mg protein) |
|---|---|---|
| SHAM (n = 8) | 78.09 ± 2.50† | 2.66 ± 0.29† |
| PS (n = 8) | 225.69 ± 5.67* | 6.62 ± 0.28* |
| PROP (n = 8) | 190.33 ± 4.21*†† | 2.88 ± 0.13†** |
| REM (n = 8) | 371.44 ± 35.06*† | 7.89 ± 0.38*† |
| PROP + REM (n = 8) | 257.44 ± 10.91* | 4.39 ± 0.27*† |
Values are presented as mean ± standard deviation.
*p < 0.0001 in comparison to the SHAM group, **p < 0.005 in comparison to the SHAM group.
† p < 0.0001 in comparison to the PS group, †† p < 0.005 in comparison to the PS group.
The lung tissue and erythrocyte MDA levels of all I/R-treated groups were significantly higher than that of the SHAM group, while the greatest increase was seen in the remifentanil group (p < 0.0001). Erythrocyte and lung MDA levels were significantly lower in the propofol group compared to the saline group, but both values were observed significantly higher in the REM group (p < 0.0001). On the other hand, while the lung MDA level was lower in the PROP + REM group than in the PS group, there was no significant difference between the erythrocyte MDA levels.
3.2 Total oxidant (TOS) and antioxidant capacity (TAC) levels in lung tissues
Total oxidative stress and total antioxidant capacity of the lung tissues are presented in Table 2.
Total oxidative stress (TOS) and total antioxidant capacity (TAC) of lung tissues
| Groups | Lung tissue TOS (µmol Trolox equivalent U/g protein) | Lung tissue TAC (mmol Trolox equivalent U/g protein) | OSI (AU) |
|---|---|---|---|
| SHAM (n = 8) | 6.46 ± 0.28† | 2.63 ± 0.23† | 2.46 ± 0.15 † |
| PS (n = 8) | 10.53 ± 0.24* | 1.57 ± 0.16* | 6.75 ± 0.74* |
| PRO (n = 8) | 7.48 ± 0.15**† | 4.15 ± 0.27*† | 1.80 ± 0.10† |
| REM (n = 8) | 10.63 ± 0.93* | 2.53 ± 0.22† | 4.24 ± 0.63* |
| PRO + REM (n = 8) | 8.91 ± 0.29*† | 3.01 ± 0.10*† | 2.95 ± 0.09† |
Values are presented as mean ± standard deviation.
OSI: oxidative stress index; AU: arbitrary unit, *p < 0.0001 in comparison to the SHAM group, **p < 0.004 in comparison to the SHAM group, † p < 0.0001 in comparison to the PS group.
Total oxidative stress (TOS) and total antioxidant capacity (TAC) of lung tissue samples are expressed in mmol per gram protein. Total oxidative stress and total antioxidant capacity measured in lung tissue samples showed parallelism with the MDA results. While the TOS levels were significantly higher in all I/R-treated groups compared to the SHAM group, the TAC level was lower in the PS group, higher in the PRO and PRO + REM groups (p < 0.0001), and no significant difference was observed in the REM group. On the other hand, while TOS levels did not differ in the REM group compared to the PS group, they were significantly lower in the other two groups (p < 0.0001).
TAC levels were found to be significantly higher in all three drug-administered I/R groups than in the PS group (p < 0.0001).
3.3 Oxidative stress index (OSI) values in lung tissue samples
The ratio of total oxidants to antioxidants in lung tissue samples (TOS/TAC) was expressed as the oxidative stress index. When OSI was compared between the groups, the highest OSI value was in the PS group. According to the Scheffe test, all inter-group comparisons were found to be statistically significant (F = 150.82, p < 0.0001), except SHAM and PRO (p = 0.09) and SHAM and PRO + REM (p = 0.33) groups.
3.4 Histopathological findings
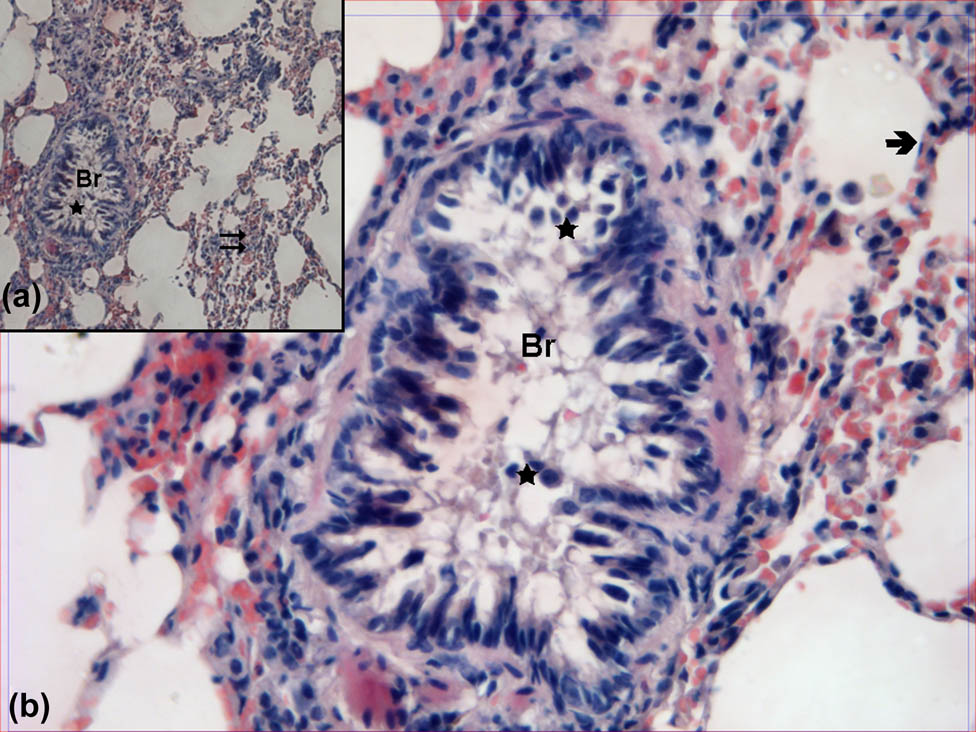
In the evaluation of hematoxylin–eosin-stained lung samples obtained from the control group, the bronchi, bronchioles, alveoli and interalveolar septa showed normal structure both by ×100 and ×400 magnification (Figure 1).
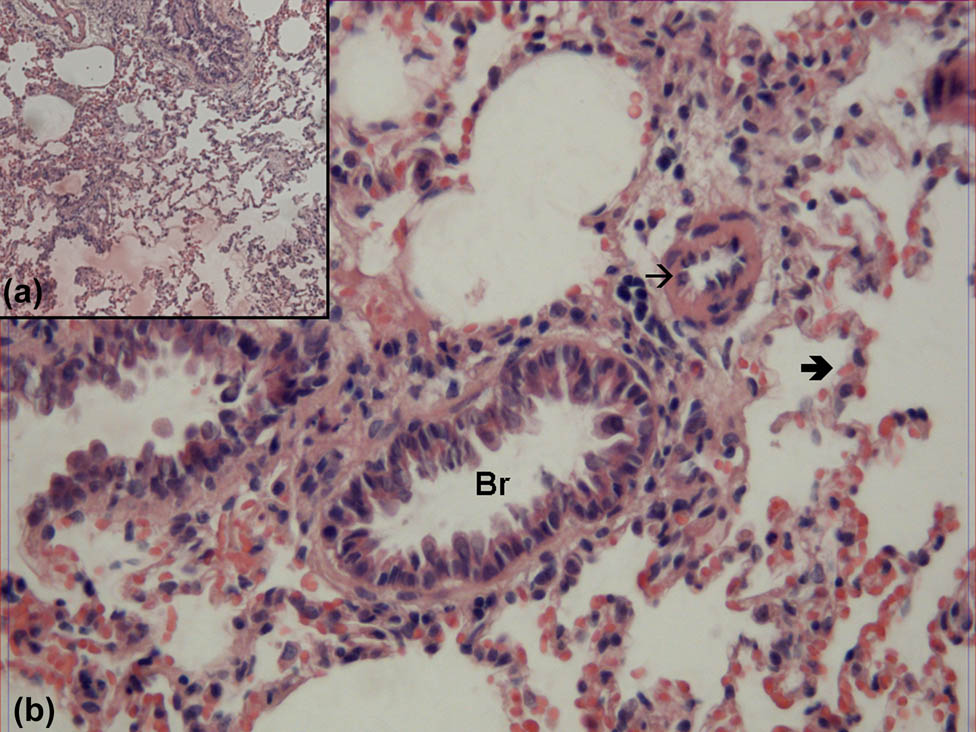
Hematoxylin–eosin-stained lung samples obtained from the SHAM group. Br: bronchioles,  : alveoli, →: vessel (hematoxylin–eosin, A: ×100, B: ×400).
: alveoli, →: vessel (hematoxylin–eosin, A: ×100, B: ×400).
The cell debris composed of epithelial cells was observed in the bronchiole lumen of tissue samples obtained from the PS group. In high magnification imaging, it was seen that while the structure was protected in some areas, the epithelial layer was disrupted in some areas and some epithelial cells with pyknotic nuclei fall into the lumen. Alveoli and interalveoler septa were also thickened (Figure 2).
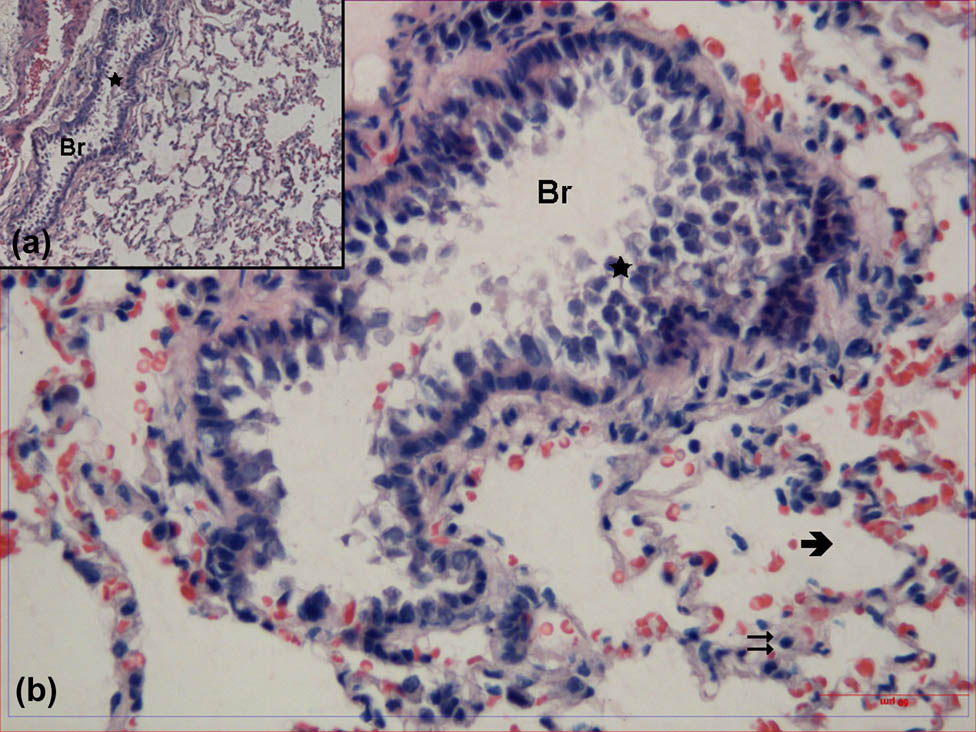
Hematoxylin–eosin-stained lung tissue samples obtained from the group treated with physiological saline. Br: bronchioles,  : alveoli,
: alveoli,  : interalveolar septa,
: interalveolar septa,  : cell debris (hematoxylin–eosin, A: ×100, B: ×400).
: cell debris (hematoxylin–eosin, A: ×100, B: ×400).
In the samples obtained from the propofol-treated group, epithelization was quite normal in the bronchioles. It was observed that epithelial debris in bronchiole lumens was less significant compared to the PS group by high magnification. The thickness of the interalveoler septum was normal and the wall structure was similar to that of the SHAM group (Figure 3).
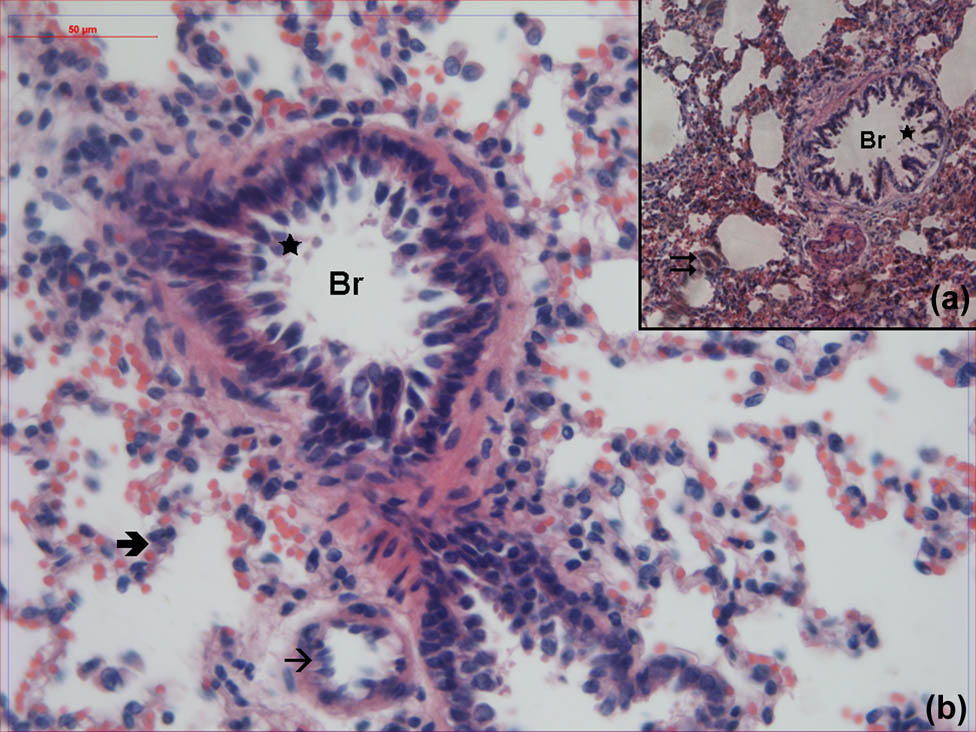
Hematoxylin–eosin-stained lung samples obtained from the propofol-treated group. Br: bronchioles,  : alveoli,
: alveoli,  : interalveolar septa,
: interalveolar septa,  : cell debris, →: vessel (hematoxylin–eosin, A: ×100, B: ×400).
: cell debris, →: vessel (hematoxylin–eosin, A: ×100, B: ×400).
When the lung samples obtained from the REM group were evaluated, it was observed that the epithelial cell debris in the lumen of the bronchioles was more significant and the interalveoler septum was thickened (Figure 4).
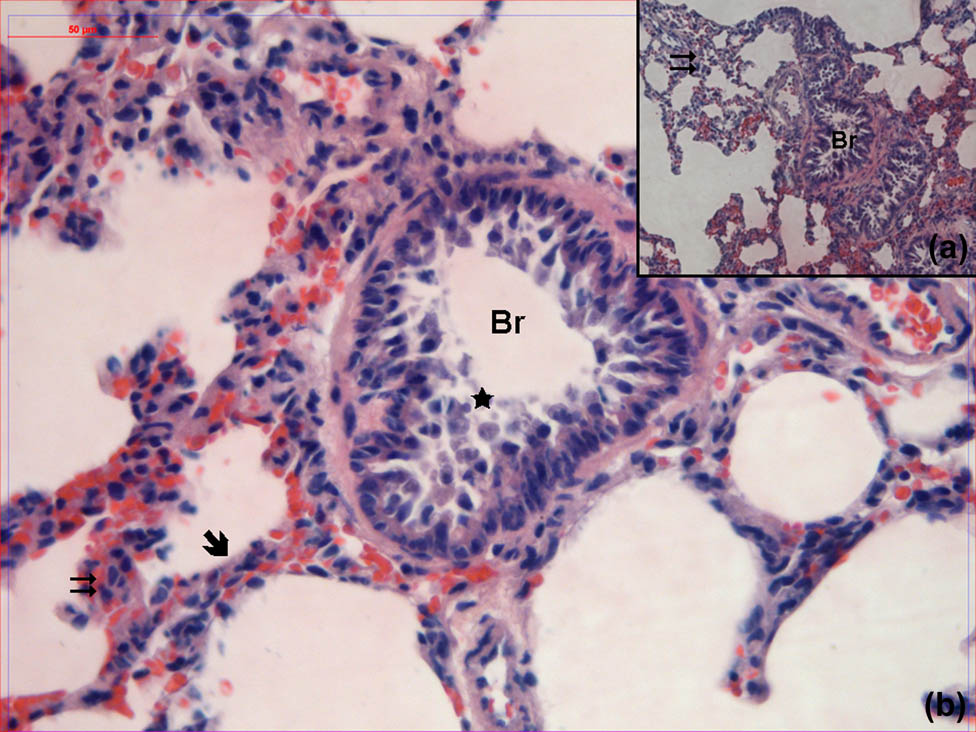
Hematoxylin–eosin-stained lung samples obtained from the group treated with remifentanil. Br: bronchioles,  : alveoli,
: alveoli,  : interalveolar septa,
: interalveolar septa,  : cell debris (hematoxylin–eosin, A: ×100, B: ×400).
: cell debris (hematoxylin–eosin, A: ×100, B: ×400).
In the examination of the tissue samples obtained from the PRO + REM group, it was observed that the cell debris in the bronchiole lumens was extremely significant. Although alveoli showed normal structure in some areas, interalveolar septa were partially thickened (Figure 5).
Hematoxylin–eosin-stained lung samples obtained from the group treated with remifentanil plus propofol. Br: bronchioles,  : alveoli,
: alveoli,  : interalveolar septa,
: interalveolar septa,  : cell debris (hematoxylin–eosin, A: ×100, B: ×400).
: cell debris (hematoxylin–eosin, A: ×100, B: ×400).
4 Discussion
In our study, experimental ischemia–reperfusion was created with infrarenal abdominal aortic occlusion in rats, and the lungs that were most affected by distant organ damage due to their rich microcapillary system were selected to be examined; MDA, TOS and TAS levels were measured as indicators of oxidative damage. Increased erythrocyte and lung MDA levels in all groups underwent I/R compared to the SHAM group, indicating that pulmonary oxidative injury develops as a result of infrarenal aortic ischemia–reperfusion.
Histological findings also showed a parallel trend to MDA results. While the lung samples obtained from the SHAM group showed a normal structure, the partial destruction of epithelization, cell debris, thickening of alveoli and interalveoler septa were observed in the samples obtained from the PS group are the results of lung tissue injury after ischemia–reperfusion.
Intraperitoneal infusions of propofol, remifentanil and propofol plus remifentanil were started 10 min before ischemia and were continued during ischemia. The application of drugs in this way may also be considered as preconditioning. It has been proposed that antioxidant substances show their effects by preventing the increase in pulmonary microvascular permeability, neutrophil adhesion and accumulation or by binding to free oxygen radicals, thus showing their protective effects against distant organ injury that develop after I/R [10,11,27,28,29] In our study, positive results could only be achieved by propofol, and remifentanil showed no preventive effects on the injury.
It was demonstrated in our study that the lung tissue MDA levels increased in all I/R-treated groups compared to the SHAM group, and ischemia–reperfusion injury was significantly prevented in the propofol-treated group, while combined use of propofol and remifentanil partially prevented I/R injury. The highest level of MDA was observed in the remifentanil group. Remifentanil infusion failed to prevent lungs against lower extremity ischemia–reperfusion injury; on the contrary, the level of oxidative injury was further increased in that group.
Therefore, our study shows that propofol is also effective in preventing distant organ lung injury in rats with infrarenal aortic ischemia. Propofol infusion was started before ischemia at a subanesthetic dose and continued during ischemia in our study. In this regard, it differs from the other ischemia–reperfusion injury prevention models. In a study emphasizing this issue, it was reported that propofol administration as induction was not very effective in terms of protection, but continuous infusion during the operation could reduce the damage [30]. This finding confirms our results.
As well known, due to the weak analgesic effect of propofol, it is used together with tranquilizers, sedatives or various analgesics. One of these combinations is the use of propofol as a hypnotic and remifentanil as an analgesic due to their short duration of action. Therefore, we compared whether remifentanil alone or in combination with propofol infusion is effective in preventing ischemia–reperfusion injury with the effect of propofol alone. Remifentanil is a short-acting opioid that metabolizes to its inactive metabolites by nonspecific plasma and tissue esterases. It is widely distributed in plasma, RBCs and interstitial structures. It has been proposed that remifentanil can suppress the cellular immune response in sepsis and may be protective for lungs, which are one of the earliest affected organs [31]. Some researchers found that opioid analgesics may significantly reduce cytokine response, and propofol and remifentanil suppress TNF-α and IL-6 induction, thus affecting neutrophil migration and adhesion molecule expression [19,32] Recently, studies on the protective effects of remifentanil against intestinal, hepatic and myocardial I/R injury have been reported [33,34]. These studies show that remifentanil prevents I/R damage in the local target organ.
In our study, while propofol alone had a very high antioxidant effect against the lung tissue I/R damage, remifentanil had no protective effect. We observed that remifentanil did not prevent lung injury as a distant organ in infrarenal I/R. In our previous study, Erkılıç et al. [35] compared the protective effects of remifentanil and dexmedetomidine (DEX) on renal I/R injury. We have demonstrated that neutrophil gelatinase-associated lipocalin (NGAL) levels and histopathological findings reflected protection by DEX against renal I/R injury while remifentanil was not as effective as DEX.
In our study, it was observed that the antioxidant effect of propofol was suppressed by remifentanil in the PROP + REM group animals. Observations obtained as a result of the examination of histological sections also support our biochemical findings. Indeed, the cell debris consisting of epithelial cells in the bronchiolitis lumen was prominent and the interalveolar septum thickness increased in the remifentanil group.
As a result of ischemia–reperfusion, along with the injuries in both local and distant organs, RBC in the blood circulation are also affected. As RBC are cells carrying oxygen to the tissues, they are among the main structures exposed to oxidative stress, hence, free oxygen radicals. These oxygen radicals may lead to lipid peroxidation, and changes in enzymes, other proteins, and, especially, the hemoglobin molecule [36]. All these changes negatively affect the oxygen transport functions of RBC. This situation would certainly affect the other tissue and organs, not in the ischemic region.
Therefore, in our study, along with oxidative injury in the lungs, RBC MDA levels that could contribute to the injury were measured. The RBC MDA levels were expressed as nmol per gram hemoglobin and show parallelism to values measured in lung tissues. The erythrocyte MDA levels were higher in I/R-treated groups in comparison to that in the SHAM group. The highest MDA levels were again found in the remifentanil and propofol plus remifentanil groups. The lowest MDA levels among the three groups that were treated with anesthetic substance infusion were observed in propofol-treated rats. Another in vitro study proposed that propofol shows protective effects against oxidative injury in RBC, partially protects their mechanic or rheological properties, and therefore, may be beneficial in decreasing surgical procedure injury [37].
Oxidative stress-related rheological changes in RBC negatively affect their functions, and thus, the blood flow and oxygenation of various tissues and organs. The reason for the single or combined use of different anesthetics is their different effect mechanisms and increased protective effect against oxidative injury; in this way, alternative protocols can be developed in the selection of anesthetic substances in surgical procedures. However, as our study demonstrated, combined use of some anesthetics may not be an appropriate choice. In our study, besides showing no protective effects against oxidative injury, remifentanil seems to increase oxidative injury in the red blood cells. This might both be due to its vulnerability to being metabolized by circulation enzymes because of its ester bond and its binding to proteins [38]. To our knowledge, there are no studies on whether remifentanil is bound by RBC or affected by them or not.
5 Conclusion
In conclusion, distant organ lung injury is developed by lower extremity ischemia–reperfusion by infrarenal aortic clamping. The lipid peroxidation product MDA and total oxidant levels increase both in lung tissues and red blood cells, and antioxidant protection remains insufficient. While propofol infusion at subanesthetic doses prevents this injury by showing an antioxidant effect, remifentanil shows no protective effect; on the contrary, it shows oxidative stress increasing effect. It was also observed in the histological examination that propofol decreased negative effects of I/R on tissues, while remifentanil was not effective as propofol. In the group that was treated with both agents, remifentanil maintained its effects and perhaps suppressed the positive effects of propofol. Although these two anesthetic substances with different anesthetic structures and properties have been preferred to be used together, it was concluded that in the case of combined use of both agents the antioxidant effects of propofol are suppressed. Therefore, in oxidative stress-associated cases such as abdominal or lower extremity surgeries, it should be kept in mind that I/R may cause distant organ lung injury, and there is a need for new studies to investigate the effect of remifentanil on I/R damage on distant organs, especially on lung injury.
-
Funding information: The authors state no funding involved.
-
Author contributions: Three authors contributed equally to this work as a co-first author.
-
Conflict of interest: The authors state no conflict of interest.
-
Data availability statement: The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
[1] Kalogeris T, Baines CP, Krenz M, Korthuis RJ. Ischemia/reperfusion. Compr Physiol. 2016;7(1):113–70.10.1002/cphy.c160006Suche in Google Scholar PubMed PubMed Central
[2] Halladin NL, Ekeløf S, Alamili M, Bendzen K, Lykkesfeldt J, Rosenberg J, et al. Lower limb ischaemia and reperfusion injury in healthy volunteers measured by oxidative and inflammatory biomarkers. Perfusion. 2015;30(1):64–70.10.1177/0267659114530769Suche in Google Scholar PubMed
[3] Leurcharusmee P, Sawaddiruk P, Punjasawadwong Y, Chattipakorn N, Chattipakorn SC. The possible pathophysiological outcomes and mechanisms of tourniquet-induced ischemia–reperfusion injury during total knee arthroplasty. Oxid Med Cell Longev. 2018;2018:8087598.10.1155/2018/8087598Suche in Google Scholar PubMed PubMed Central
[4] Cui Y, Wang Y, Li G, Ma W, Zhou X, Wang J, et al. The Nox1/Nox4 inhibitor attenuates acute lung injury induced by ischemia–reperfusion in mice. PLoS One. 2018;13(12):e0209444.10.1371/journal.pone.0209444Suche in Google Scholar PubMed PubMed Central
[5] Fard N, Saffari A, Emami G, Hofer S, Kauczor HU, Mehrabi A. Acute respiratory distress syndrome induction by pulmonary ischemia–reperfusion injury in large animal models. J Surg Res. 2014;189(2):274–84.10.1016/j.jss.2014.02.034Suche in Google Scholar PubMed
[6] Thomaz Neto FJ, Koike MK, Abrahão Mde S, Carillo Neto F, Pereira RK, Machado JL, et al. Ischemic preconditioning attenuates remote pulmonary inflammatory infiltration of diabetic rats with an intestinal and hepatic ischemia–reperfusion injury. Acta Cir Bras. 2013;28(3):174–8.10.1590/S0102-86502013000300003Suche in Google Scholar PubMed
[7] Chen LN1, Yang XH, Nissen DH, Chen YY, Wang LJ, Wang JH, et al. Dysregulated renin-angiotensin system contributes to acute lung injury caused by hind-limb ischemia–reperfusion in mice. Shock. 2013 Nov;40(5):420–9.10.1097/SHK.0b013e3182a6953eSuche in Google Scholar PubMed
[8] Karaca Ö, Pinar HU, Özgür AF, Kulaksizoğlu S, Doğan R. The effect of pregabalin on tourniquet-induced ischemia–reperfusion injury: a prospective randomized study. Turk J Med Sci. 2019;49(6):1693–700.Suche in Google Scholar
[9] Kao MC, Jan WC, Tsai PS, Wang TY, Huang CJ. Magnesium sulfate mitigates lung injury induced by bilateral lower limb ischemia–reperfusion in rats. J Surg Res. 2011;171(1):e97–e106.10.1016/j.jss.2011.03.028Suche in Google Scholar PubMed
[10] Takhtfooladi HA, Hesaraki S, Razmara F, Takhtfooladi MA, Hajizadeh H. Effects of N-acetylcysteine and pentoxifylline on remote lung injury in a rat model of hind-limb ischemia/reperfusion injury. J Bras Pneumol. 2016;42(1):9–14.10.1590/S1806-37562016000000183Suche in Google Scholar PubMed PubMed Central
[11] Tuncay A, Sivgin V, Ozdemirkan A, Sezen SC, Boyunaga H, Kucuk A, et al. The effect of cerium oxide on lung tissue in lower extremity ischemia reperfusion injury in sevoflurane administered rats. Int J Nanomedicine. 2020;15:7481–9.10.2147/IJN.S263001Suche in Google Scholar PubMed PubMed Central
[12] Erturk E. Ischemia–reperfusion injury and volatile anesthetics. Biomed Res Int. 2014;2014:526301.10.1155/2014/526301Suche in Google Scholar PubMed PubMed Central
[13] Yamada T, Nagata H, Kosugi S, Suzuki T, Morisaki H, Kotake Y. Interaction between anesthetic conditioning and ischemic preconditioning on metabolic function after hepatic ischemia–reperfusion in rabbits. J Anesth. 2018;32(4):599–607.10.1007/s00540-018-2523-7Suche in Google Scholar PubMed
[14] Zhang Y, Chen Z, Feng N, Tang J, Zhao X, Liu C, et al. Protective effect of propofol preconditioning on ischemia–reperfusion injury in human hepatocyte. J Thorac Dis. 2017;9(3):702–10.10.21037/jtd.2017.02.80Suche in Google Scholar PubMed PubMed Central
[15] Lemoine S, Tritapepe L, Hanouz JL, Puddu PE. The mechanisms of cardio-protective effects of desflurane and sevoflurane at the time of reperfusion: anaesthetic post-conditioning potentially translatable to humans? Br J Anaesth. 2016;116(4):456–75.10.1093/bja/aev451Suche in Google Scholar PubMed
[16] Álvarez P, Tapia L, Mardones LA, Pedemonte JC, Farías JG, Castillo RL. Cellular mechanisms against ischemia reperfusion injury induced by the use of anesthetic pharmacological agents. Chem Biol Interact. 2014 Jul 25;218:89–98.10.1016/j.cbi.2014.04.019Suche in Google Scholar PubMed
[17] Liu Y, Du X, Zhang S, Liu X, Xu G. Propofol alleviates hepatic ischemia/reperfusion injury via the activation of the Sirt1 pathway. Int J Clin Exp Pathol. 2017 Nov 1;10(11):10959–68.Suche in Google Scholar
[18] Halladin NL, Zahle FV, Rosenberg J, Gögenur I. Interventions to reduce tourniquet-related ischaemic damage in orthopaedic surgery: a qualitative systematic review of randomised trials. Anaesthesia. 2014;69(9):1033–50.10.1111/anae.12664Suche in Google Scholar PubMed
[19] Roh GU, Song Y, Park J, Ki YM, Han DW. Effects of propofol on the inflammatory response during robot-assisted laparoscopic radical prostatectomy: a prospective randomized controlled study. Sci Rep. 2019;9(1):5242.10.1038/s41598-019-41708-xSuche in Google Scholar PubMed PubMed Central
[20] Wong GT, Huang Z, Ji S, Irwin MG. Remifentanil reduces the release of biochemical markers of myocardial damage after coronary artery bypass surgery: a randomized trial. J CardiothoracVascAnesth. 2010;24:790–6.10.1053/j.jvca.2009.09.012Suche in Google Scholar PubMed
[21] Sheng M, Zhang G, Wang J, Yang Q, Zhao H, Cheng X, et al. Remifentanil induces cardio protection against ischemia/reperfusion injury by inhibiting endoplasmic reticulum stress through the maintenance of zinc homeostasis. Anesth Analg. 2018 Jul;127(1):267–76.10.1213/ANE.0000000000003414Suche in Google Scholar PubMed
[22] Tanaka K, Kersten JR, Riess ML. Opioid-induced cardioprotection. Curr Pharm Des. 2014;20(36):5696–705.10.2174/1381612820666140204120311Suche in Google Scholar PubMed PubMed Central
[23] Yagi K. Assay for blood plasma or serum. In: Colowick SP, Kaplan NO, editors. Methods enzymol, vol. 105. New York, San Fransisco, London: Academic Press, Inc.; 1984. p. 328–31.10.1016/S0076-6879(84)05042-4Suche in Google Scholar
[24] Ohkawa H, Ohishi N, Yagi K. Assay for lipid peroxides in animal tissues by thiobarbituric acid reaction. Anal Biochem. 1979;95:351–8.10.1016/0003-2697(79)90738-3Suche in Google Scholar
[25] Erel O. A novel automated method to measure total antioxidant response against potent free radical reactions. Clin Biochem. 2004;37(2):112–9.10.1016/j.clinbiochem.2003.10.014Suche in Google Scholar PubMed
[26] Erel Ö. A new automated colorimetric method for measuring total oxidant status. ClinBiochem. 2005;38:1103–11.10.1016/j.clinbiochem.2005.08.008Suche in Google Scholar PubMed
[27] Liang S, Wang Y, Liu Y. Dexmedetomidine alleviates lung ischemia–reperfusion injury in rats by activating PI3K/Akt pathway. Eur Rev Med Pharmacol Sci. 2019 Jan;23(1):370–7.Suche in Google Scholar
[28] Vasileiou I, Kalimeris K, Nomikos T, Xanthopoulou MN, Perrea D, Agrogiannis G, et al. Propofol prevents lung injury following intestinal ischemia–reperfusion. J Surg Res. 2012 Jan;172(1):146–52.10.1016/j.jss.2010.07.034Suche in Google Scholar PubMed
[29] Dwaich KH, Al-Amran FG, Al-Sheibani BI, Al-Aubaidy HA. Melatonin effects on myocardial ischemia–reperfusion injury: Impact on the outcome in patients undergoing coronary artery bypass grafting surgery. Int J Cardiol. 2016;221:977–86.10.1016/j.ijcard.2016.07.108Suche in Google Scholar PubMed
[30] Turan R, Yagmurdur H, Kavutcu M, Dikmen B. Propofol and tourniquet induced ischaemia reperfusion injury in lower extremity operations. Eur J Anaesthesiol. 2007;24:185–9.10.1017/S0265021506001347Suche in Google Scholar PubMed
[31] Zongze Z, Jia Z, Chang C, Kai C, Yanlin W. Protective effects of remifentanil on septic mice. Mol Biol Rep. 2010;37:2803–8.10.1007/s11033-009-9828-4Suche in Google Scholar PubMed
[32] Qu ZJ, Qu ZJ, Zhou HB, Xu CS, Zhang DZ, Wang G. Protective effect of remifentanil on myocardial ischemia–reperfusion injury through Fas apoptosis signaling pathway. Eur Rev Med Pharmacol Sci. 2019 Jul;23(13):5980–6.Suche in Google Scholar
[33] Liu X, Pan Z, Su D, Yang Z, Zheng B, Wang X, et al. Remifentanil ameliorates liver ischemia–reperfusion injury through inhibition of interleukin-18 signaling. Transplantation. 2015;99(10):2109–17.10.1097/TP.0000000000000737Suche in Google Scholar PubMed
[34] Cho SS, Rudloff I, Berger PJ, Irwin MG, Nold MF, Cheng W, et al. Remifentanil ameliorates intestinal ischemia–reperfusion injury. BMC Gastroenterol. 2013 Apr 22;13:69.10.1186/1471-230X-13-69Suche in Google Scholar PubMed PubMed Central
[35] Erkılıç E, Kesimci E, Alaybeyoğlu F, Kılınç I, Tural R, Yazgan A, et al. Does remifentanil attenuate renal ischemia–reperfusion injury better than dexmedetomidine in rat kidney? Drug Des Devel Ther. 2017;11:677–83.10.2147/DDDT.S126701Suche in Google Scholar PubMed PubMed Central
[36] Mester A, Magyar Z, Sogor V, Tanczos B, Stark Y, Cherniavsky K, et al. Intestinal ischemia–reperfusion leads to early systemic micro-rheological and multiorgan microcirculatory alterations in the rat. Clin Hemorheol Microcirc. 2018;68(1):35–44.10.3233/CH-170278Suche in Google Scholar PubMed
[37] Tsuchiya M, Asada A, Kasahara E, Sato EF, Shindo M, Inoue M. Antioxidant protection of propofol and its recycling in erythrocyte membranes. Am J Respir Crit Care Med. 2002;165:54–60.10.1164/ajrccm.165.1.2010134Suche in Google Scholar PubMed
[38] Mei B, Wang T, Wang Y, Xia Z, Irwin MG, Wong GT. High dose remifentanil increases myocardial oxidative stress and compromises remifentanil infarct-sparing effects in rats. Eur J Pharmacol. 2013;718(1–3):484–92.10.1016/j.ejphar.2013.07.030Suche in Google Scholar PubMed
© 2021 Orhan Kanbak et al., published by De Gruyter
This work is licensed under the Creative Commons Attribution 4.0 International License.
Artikel in diesem Heft
- Research Articles
- Identification of ZG16B as a prognostic biomarker in breast cancer
- Behçet’s disease with latent Mycobacterium tuberculosis infection
- Erratum
- Erratum to “Suffering from Cerebral Small Vessel Disease with and without Metabolic Syndrome”
- Research Articles
- GPR37 promotes the malignancy of lung adenocarcinoma via TGF-β/Smad pathway
- Expression and role of ABIN1 in sepsis: In vitro and in vivo studies
- Additional baricitinib loading dose improves clinical outcome in COVID-19
- The co-treatment of rosuvastatin with dapagliflozin synergistically inhibited apoptosis via activating the PI3K/AKt/mTOR signaling pathway in myocardial ischemia/reperfusion injury rats
- SLC12A8 plays a key role in bladder cancer progression and EMT
- LncRNA ATXN8OS enhances tamoxifen resistance in breast cancer
- Case Report
- Serratia marcescens as a cause of unfavorable outcome in the twin pregnancy
- Spleno-adrenal fusion mimicking an adrenal metastasis of a renal cell carcinoma: A case report and embryological background
- Research Articles
- TRIM25 contributes to the malignancy of acute myeloid leukemia and is negatively regulated by microRNA-137
- CircRNA circ_0004370 promotes cell proliferation, migration, and invasion and inhibits cell apoptosis of esophageal cancer via miR-1301-3p/COL1A1 axis
- LncRNA XIST regulates atherosclerosis progression in ox-LDL-induced HUVECs
- Potential role of IFN-γ and IL-5 in sepsis prediction of preterm neonates
- Rapid Communication
- COVID-19 vaccine: Call for employees in international transportation industries and international travelers as the first priority in global distribution
- Case Report
- Rare squamous cell carcinoma of the kidney with concurrent xanthogranulomatous pyelonephritis: A case report and review of the literature
- An infertile female delivered a baby after removal of primary renal carcinoid tumor
- Research Articles
- Hypertension, BMI, and cardiovascular and cerebrovascular diseases
- Case Report
- Coexistence of bilateral macular edema and pale optic disc in the patient with Cohen syndrome
- Research Articles
- Correlation between kinematic sagittal parameters of the cervical lordosis or head posture and disc degeneration in patients with posterior neck pain
- Review Articles
- Hepatoid adenocarcinoma of the lung: An analysis of the Surveillance, Epidemiology, and End Results (SEER) database
- Research Articles
- Thermography in the diagnosis of carpal tunnel syndrome
- Pemetrexed-based first-line chemotherapy had particularly prominent objective response rate for advanced NSCLC: A network meta-analysis
- Comparison of single and double autologous stem cell transplantation in multiple myeloma patients
- The influence of smoking in minimally invasive spinal fusion surgery
- Impact of body mass index on left atrial dimension in HOCM patients
- Expression and clinical significance of CMTM1 in hepatocellular carcinoma
- miR-142-5p promotes cervical cancer progression by targeting LMX1A through Wnt/β-catenin pathway
- Comparison of multiple flatfoot indicators in 5–8-year-old children
- Early MRI imaging and follow-up study in cerebral amyloid angiopathy
- Intestinal fatty acid-binding protein as a biomarker for the diagnosis of strangulated intestinal obstruction: A meta-analysis
- miR-128-3p inhibits apoptosis and inflammation in LPS-induced sepsis by targeting TGFBR2
- Dynamic perfusion CT – A promising tool to diagnose pancreatic ductal adenocarcinoma
- Biomechanical evaluation of self-cinching stitch techniques in rotator cuff repair: The single-loop and double-loop knot stitches
- Review Articles
- The ambiguous role of mannose-binding lectin (MBL) in human immunity
- Case Report
- Membranous nephropathy with pulmonary cryptococcosis with improved 1-year follow-up results: A case report
- Fertility problems in males carrying an inversion of chromosome 10
- Acute myeloid leukemia with leukemic pleural effusion and high levels of pleural adenosine deaminase: A case report and review of literature
- Metastatic renal Ewing’s sarcoma in adult woman: Case report and review of the literature
- Burkitt-like lymphoma with 11q aberration in a patient with AIDS and a patient without AIDS: Two cases reports and literature review
- Skull hemophilia pseudotumor: A case report
- Judicious use of low-dosage corticosteroids for non-severe COVID-19: A case report
- Adult-onset citrullinaemia type II with liver cirrhosis: A rare cause of hyperammonaemia
- Clinicopathologic features of Good’s syndrome: Two cases and literature review
- Fatal immune-related hepatitis with intrahepatic cholestasis and pneumonia associated with camrelizumab: A case report and literature review
- Research Articles
- Effects of hydroxyethyl starch and gelatin on the risk of acute kidney injury following orthotopic liver transplantation: A multicenter retrospective comparative clinical study
- Significance of nucleic acid positive anal swab in COVID-19 patients
- circAPLP2 promotes colorectal cancer progression by upregulating HELLS by targeting miR-335-5p
- Ratios between circulating myeloid cells and lymphocytes are associated with mortality in severe COVID-19 patients
- Risk factors of left atrial appendage thrombus in patients with non-valvular atrial fibrillation
- Clinical features of hypertensive patients with COVID-19 compared with a normotensive group: Single-center experience in China
- Surgical myocardial revascularization outcomes in Kawasaki disease: systematic review and meta-analysis
- Decreased chromobox homologue 7 expression is associated with epithelial–mesenchymal transition and poor prognosis in cervical cancer
- FGF16 regulated by miR-520b enhances the cell proliferation of lung cancer
- Platelet-rich fibrin: Basics of biological actions and protocol modifications
- Accurate diagnosis of prostate cancer using logistic regression
- miR-377 inhibition enhances the survival of trophoblast cells via upregulation of FNDC5 in gestational diabetes mellitus
- Prognostic significance of TRIM28 expression in patients with breast carcinoma
- Integrative bioinformatics analysis of KPNA2 in six major human cancers
- Exosomal-mediated transfer of OIP5-AS1 enhanced cell chemoresistance to trastuzumab in breast cancer via up-regulating HMGB3 by sponging miR-381-3p
- A four-lncRNA signature for predicting prognosis of recurrence patients with gastric cancer
- Knockdown of circ_0003204 alleviates oxidative low-density lipoprotein-induced human umbilical vein endothelial cells injury: Circulating RNAs could explain atherosclerosis disease progression
- Propofol postpones colorectal cancer development through circ_0026344/miR-645/Akt/mTOR signal pathway
- Knockdown of lncRNA TapSAKI alleviates LPS-induced injury in HK-2 cells through the miR-205/IRF3 pathway
- COVID-19 severity in relation to sociodemographics and vitamin D use
- Clinical analysis of 11 cases of nocardiosis
- Cis-regulatory elements in conserved non-coding sequences of nuclear receptor genes indicate for crosstalk between endocrine systems
- Four long noncoding RNAs act as biomarkers in lung adenocarcinoma
- Real-world evidence of cytomegalovirus reactivation in non-Hodgkin lymphomas treated with bendamustine-containing regimens
- Relation between IL-8 level and obstructive sleep apnea syndrome
- circAGFG1 sponges miR-28-5p to promote non-small-cell lung cancer progression through modulating HIF-1α level
- Nomogram prediction model for renal anaemia in IgA nephropathy patients
- Effect of antibiotic use on the efficacy of nivolumab in the treatment of advanced/metastatic non-small cell lung cancer: A meta-analysis
- NDRG2 inhibition facilitates angiogenesis of hepatocellular carcinoma
- A nomogram for predicting metabolic steatohepatitis: The combination of NAMPT, RALGDS, GADD45B, FOSL2, RTP3, and RASD1
- Clinical and prognostic features of MMP-2 and VEGF in AEG patients
- The value of miR-510 in the prognosis and development of colon cancer
- Functional implications of PABPC1 in the development of ovarian cancer
- Prognostic value of preoperative inflammation-based predictors in patients with bladder carcinoma after radical cystectomy
- Sublingual immunotherapy increases Treg/Th17 ratio in allergic rhinitis
- Prediction of improvement after anterior cruciate ligament reconstruction
- Effluent Osteopontin levels reflect the peritoneal solute transport rate
- circ_0038467 promotes PM2.5-induced bronchial epithelial cell dysfunction
- Significance of miR-141 and miR-340 in cervical squamous cell carcinoma
- Association between hair cortisol concentration and metabolic syndrome
- Microvessel density as a prognostic indicator of prostate cancer: A systematic review and meta-analysis
- Characteristics of BCR–ABL gene variants in patients of chronic myeloid leukemia
- Knee alterations in rheumatoid arthritis: Comparison of US and MRI
- Long non-coding RNA TUG1 aggravates cerebral ischemia and reperfusion injury by sponging miR-493-3p/miR-410-3p
- lncRNA MALAT1 regulated ATAD2 to facilitate retinoblastoma progression via miR-655-3p
- Development and validation of a nomogram for predicting severity in patients with hemorrhagic fever with renal syndrome: A retrospective study
- Analysis of COVID-19 outbreak origin in China in 2019 using differentiation method for unusual epidemiological events
- Laparoscopic versus open major liver resection for hepatocellular carcinoma: A case-matched analysis of short- and long-term outcomes
- Travelers’ vaccines and their adverse events in Nara, Japan
- Association between Tfh and PGA in children with Henoch–Schönlein purpura
- Can exchange transfusion be replaced by double-LED phototherapy?
- circ_0005962 functions as an oncogene to aggravate NSCLC progression
- Circular RNA VANGL1 knockdown suppressed viability, promoted apoptosis, and increased doxorubicin sensitivity through targeting miR-145-5p to regulate SOX4 in bladder cancer cells
- Serum intact fibroblast growth factor 23 in healthy paediatric population
- Algorithm of rational approach to reconstruction in Fournier’s disease
- A meta-analysis of exosome in the treatment of spinal cord injury
- Src-1 and SP2 promote the proliferation and epithelial–mesenchymal transition of nasopharyngeal carcinoma
- Dexmedetomidine may decrease the bupivacaine toxicity to heart
- Hypoxia stimulates the migration and invasion of osteosarcoma via up-regulating the NUSAP1 expression
- Long noncoding RNA XIST knockdown relieves the injury of microglia cells after spinal cord injury by sponging miR-219-5p
- External fixation via the anterior inferior iliac spine for proximal femoral fractures in young patients
- miR-128-3p reduced acute lung injury induced by sepsis via targeting PEL12
- HAGLR promotes neuron differentiation through the miR-130a-3p-MeCP2 axis
- Phosphoglycerate mutase 2 is elevated in serum of patients with heart failure and correlates with the disease severity and patient’s prognosis
- Cell population data in identifying active tuberculosis and community-acquired pneumonia
- Prognostic value of microRNA-4521 in non-small cell lung cancer and its regulatory effect on tumor progression
- Mean platelet volume and red blood cell distribution width is associated with prognosis in premature neonates with sepsis
- 3D-printed porous scaffold promotes osteogenic differentiation of hADMSCs
- Association of gene polymorphisms with women urinary incontinence
- Influence of COVID-19 pandemic on stress levels of urologic patients
- miR-496 inhibits proliferation via LYN and AKT pathway in gastric cancer
- miR-519d downregulates LEP expression to inhibit preeclampsia development
- Comparison of single- and triple-port VATS for lung cancer: A meta-analysis
- Fluorescent light energy modulates healing in skin grafted mouse model
- Silencing CDK6-AS1 inhibits LPS-induced inflammatory damage in HK-2 cells
- Predictive effect of DCE-MRI and DWI in brain metastases from NSCLC
- Severe postoperative hyperbilirubinemia in congenital heart disease
- Baicalin improves podocyte injury in rats with diabetic nephropathy by inhibiting PI3K/Akt/mTOR signaling pathway
- Clinical factors predicting ureteral stent failure in patients with external ureteral compression
- Novel H2S donor proglumide-ADT-OH protects HUVECs from ox-LDL-induced injury through NF-κB and JAK/SATA pathway
- Triple-Endobutton and clavicular hook: A propensity score matching analysis
- Long noncoding RNA MIAT inhibits the progression of diabetic nephropathy and the activation of NF-κB pathway in high glucose-treated renal tubular epithelial cells by the miR-182-5p/GPRC5A axis
- Serum exosomal miR-122-5p, GAS, and PGR in the non-invasive diagnosis of CAG
- miR-513b-5p inhibits the proliferation and promotes apoptosis of retinoblastoma cells by targeting TRIB1
- Fer exacerbates renal fibrosis and can be targeted by miR-29c-3p
- The diagnostic and prognostic value of miR-92a in gastric cancer: A systematic review and meta-analysis
- Prognostic value of α2δ1 in hypopharyngeal carcinoma: A retrospective study
- No significant benefit of moderate-dose vitamin C on severe COVID-19 cases
- circ_0000467 promotes the proliferation, metastasis, and angiogenesis in colorectal cancer cells through regulating KLF12 expression by sponging miR-4766-5p
- Downregulation of RAB7 and Caveolin-1 increases MMP-2 activity in renal tubular epithelial cells under hypoxic conditions
- Educational program for orthopedic surgeons’ influences for osteoporosis
- Expression and function analysis of CRABP2 and FABP5, and their ratio in esophageal squamous cell carcinoma
- GJA1 promotes hepatocellular carcinoma progression by mediating TGF-β-induced activation and the epithelial–mesenchymal transition of hepatic stellate cells
- lncRNA-ZFAS1 promotes the progression of endometrial carcinoma by targeting miR-34b to regulate VEGFA expression
- Anticoagulation is the answer in treating noncritical COVID-19 patients
- Effect of late-onset hemorrhagic cystitis on PFS after haplo-PBSCT
- Comparison of Dako HercepTest and Ventana PATHWAY anti-HER2 (4B5) tests and their correlation with silver in situ hybridization in lung adenocarcinoma
- VSTM1 regulates monocyte/macrophage function via the NF-κB signaling pathway
- Comparison of vaginal birth outcomes in midwifery-led versus physician-led setting: A propensity score-matched analysis
- Treatment of osteoporosis with teriparatide: The Slovenian experience
- New targets of morphine postconditioning protection of the myocardium in ischemia/reperfusion injury: Involvement of HSP90/Akt and C5a/NF-κB
- Superenhancer–transcription factor regulatory network in malignant tumors
- β-Cell function is associated with osteosarcopenia in middle-aged and older nonobese patients with type 2 diabetes: A cross-sectional study
- Clinical features of atypical tuberculosis mimicking bacterial pneumonia
- Proteoglycan-depleted regions of annular injury promote nerve ingrowth in a rabbit disc degeneration model
- Effect of electromagnetic field on abortion: A systematic review and meta-analysis
- miR-150-5p affects AS plaque with ASMC proliferation and migration by STAT1
- MALAT1 promotes malignant pleural mesothelioma by sponging miR-141-3p
- Effects of remifentanil and propofol on distant organ lung injury in an ischemia–reperfusion model
- miR-654-5p promotes gastric cancer progression via the GPRIN1/NF-κB pathway
- Identification of LIG1 and LIG3 as prognostic biomarkers in breast cancer
- MitoQ inhibits hepatic stellate cell activation and liver fibrosis by enhancing PINK1/parkin-mediated mitophagy
- Dissecting role of founder mutation p.V727M in GNE in Indian HIBM cohort
- circATP2A2 promotes osteosarcoma progression by upregulating MYH9
- Prognostic role of oxytocin receptor in colon adenocarcinoma
- Review Articles
- The function of non-coding RNAs in idiopathic pulmonary fibrosis
- Efficacy and safety of therapeutic plasma exchange in stiff person syndrome
- Role of cesarean section in the development of neonatal gut microbiota: A systematic review
- Small cell lung cancer transformation during antitumor therapies: A systematic review
- Research progress of gut microbiota and frailty syndrome
- Recommendations for outpatient activity in COVID-19 pandemic
- Rapid Communication
- Disparity in clinical characteristics between 2019 novel coronavirus pneumonia and leptospirosis
- Use of microspheres in embolization for unruptured renal angiomyolipomas
- COVID-19 cases with delayed absorption of lung lesion
- A triple combination of treatments on moderate COVID-19
- Social networks and eating disorders during the Covid-19 pandemic
- Letter
- COVID-19, WHO guidelines, pedagogy, and respite
- Inflammatory factors in alveolar lavage fluid from severe COVID-19 pneumonia: PCT and IL-6 in epithelial lining fluid
- COVID-19: Lessons from Norway tragedy must be considered in vaccine rollout planning in least developed/developing countries
- What is the role of plasma cell in the lamina propria of terminal ileum in Good’s syndrome patient?
- Case Report
- Rivaroxaban triggered multifocal intratumoral hemorrhage of the cabozantinib-treated diffuse brain metastases: A case report and review of literature
- CTU findings of duplex kidney in kidney: A rare duplicated renal malformation
- Synchronous primary malignancy of colon cancer and mantle cell lymphoma: A case report
- Sonazoid-enhanced ultrasonography and pathologic characters of CD68 positive cell in primary hepatic perivascular epithelioid cell tumors: A case report and literature review
- Persistent SARS-CoV-2-positive over 4 months in a COVID-19 patient with CHB
- Pulmonary parenchymal involvement caused by Tropheryma whipplei
- Mediastinal mixed germ cell tumor: A case report and literature review
- Ovarian female adnexal tumor of probable Wolffian origin – Case report
- Rare paratesticular aggressive angiomyxoma mimicking an epididymal tumor in an 82-year-old man: Case report
- Perimenopausal giant hydatidiform mole complicated with preeclampsia and hyperthyroidism: A case report and literature review
- Primary orbital ganglioneuroblastoma: A case report
- Primary aortic intimal sarcoma masquerading as intramural hematoma
- Sustained false-positive results for hepatitis A virus immunoglobulin M: A case report and literature review
- Peritoneal loose body presenting as a hepatic mass: A case report and review of the literature
- Chondroblastoma of mandibular condyle: Case report and literature review
- Trauma-induced complete pacemaker lead fracture 8 months prior to hospitalization: A case report
- Primary intradural extramedullary extraosseous Ewing’s sarcoma/peripheral primitive neuroectodermal tumor (PIEES/PNET) of the thoracolumbar spine: A case report and literature review
- Computer-assisted preoperative planning of reduction of and osteosynthesis of scapular fracture: A case report
- High quality of 58-month life in lung cancer patient with brain metastases sequentially treated with gefitinib and osimertinib
- Rapid response of locally advanced oral squamous cell carcinoma to apatinib: A case report
- Retrieval of intrarenal coiled and ruptured guidewire by retrograde intrarenal surgery: A case report and literature review
- Usage of intermingled skin allografts and autografts in a senior patient with major burn injury
- Retraction
- Retraction on “Dihydromyricetin attenuates inflammation through TLR4/NF-kappa B pathway”
- Special Issue Computational Intelligence Methodologies Meets Recurrent Cancers - Part I
- An artificial immune system with bootstrap sampling for the diagnosis of recurrent endometrial cancers
- Breast cancer recurrence prediction with ensemble methods and cost-sensitive learning
Artikel in diesem Heft
- Research Articles
- Identification of ZG16B as a prognostic biomarker in breast cancer
- Behçet’s disease with latent Mycobacterium tuberculosis infection
- Erratum
- Erratum to “Suffering from Cerebral Small Vessel Disease with and without Metabolic Syndrome”
- Research Articles
- GPR37 promotes the malignancy of lung adenocarcinoma via TGF-β/Smad pathway
- Expression and role of ABIN1 in sepsis: In vitro and in vivo studies
- Additional baricitinib loading dose improves clinical outcome in COVID-19
- The co-treatment of rosuvastatin with dapagliflozin synergistically inhibited apoptosis via activating the PI3K/AKt/mTOR signaling pathway in myocardial ischemia/reperfusion injury rats
- SLC12A8 plays a key role in bladder cancer progression and EMT
- LncRNA ATXN8OS enhances tamoxifen resistance in breast cancer
- Case Report
- Serratia marcescens as a cause of unfavorable outcome in the twin pregnancy
- Spleno-adrenal fusion mimicking an adrenal metastasis of a renal cell carcinoma: A case report and embryological background
- Research Articles
- TRIM25 contributes to the malignancy of acute myeloid leukemia and is negatively regulated by microRNA-137
- CircRNA circ_0004370 promotes cell proliferation, migration, and invasion and inhibits cell apoptosis of esophageal cancer via miR-1301-3p/COL1A1 axis
- LncRNA XIST regulates atherosclerosis progression in ox-LDL-induced HUVECs
- Potential role of IFN-γ and IL-5 in sepsis prediction of preterm neonates
- Rapid Communication
- COVID-19 vaccine: Call for employees in international transportation industries and international travelers as the first priority in global distribution
- Case Report
- Rare squamous cell carcinoma of the kidney with concurrent xanthogranulomatous pyelonephritis: A case report and review of the literature
- An infertile female delivered a baby after removal of primary renal carcinoid tumor
- Research Articles
- Hypertension, BMI, and cardiovascular and cerebrovascular diseases
- Case Report
- Coexistence of bilateral macular edema and pale optic disc in the patient with Cohen syndrome
- Research Articles
- Correlation between kinematic sagittal parameters of the cervical lordosis or head posture and disc degeneration in patients with posterior neck pain
- Review Articles
- Hepatoid adenocarcinoma of the lung: An analysis of the Surveillance, Epidemiology, and End Results (SEER) database
- Research Articles
- Thermography in the diagnosis of carpal tunnel syndrome
- Pemetrexed-based first-line chemotherapy had particularly prominent objective response rate for advanced NSCLC: A network meta-analysis
- Comparison of single and double autologous stem cell transplantation in multiple myeloma patients
- The influence of smoking in minimally invasive spinal fusion surgery
- Impact of body mass index on left atrial dimension in HOCM patients
- Expression and clinical significance of CMTM1 in hepatocellular carcinoma
- miR-142-5p promotes cervical cancer progression by targeting LMX1A through Wnt/β-catenin pathway
- Comparison of multiple flatfoot indicators in 5–8-year-old children
- Early MRI imaging and follow-up study in cerebral amyloid angiopathy
- Intestinal fatty acid-binding protein as a biomarker for the diagnosis of strangulated intestinal obstruction: A meta-analysis
- miR-128-3p inhibits apoptosis and inflammation in LPS-induced sepsis by targeting TGFBR2
- Dynamic perfusion CT – A promising tool to diagnose pancreatic ductal adenocarcinoma
- Biomechanical evaluation of self-cinching stitch techniques in rotator cuff repair: The single-loop and double-loop knot stitches
- Review Articles
- The ambiguous role of mannose-binding lectin (MBL) in human immunity
- Case Report
- Membranous nephropathy with pulmonary cryptococcosis with improved 1-year follow-up results: A case report
- Fertility problems in males carrying an inversion of chromosome 10
- Acute myeloid leukemia with leukemic pleural effusion and high levels of pleural adenosine deaminase: A case report and review of literature
- Metastatic renal Ewing’s sarcoma in adult woman: Case report and review of the literature
- Burkitt-like lymphoma with 11q aberration in a patient with AIDS and a patient without AIDS: Two cases reports and literature review
- Skull hemophilia pseudotumor: A case report
- Judicious use of low-dosage corticosteroids for non-severe COVID-19: A case report
- Adult-onset citrullinaemia type II with liver cirrhosis: A rare cause of hyperammonaemia
- Clinicopathologic features of Good’s syndrome: Two cases and literature review
- Fatal immune-related hepatitis with intrahepatic cholestasis and pneumonia associated with camrelizumab: A case report and literature review
- Research Articles
- Effects of hydroxyethyl starch and gelatin on the risk of acute kidney injury following orthotopic liver transplantation: A multicenter retrospective comparative clinical study
- Significance of nucleic acid positive anal swab in COVID-19 patients
- circAPLP2 promotes colorectal cancer progression by upregulating HELLS by targeting miR-335-5p
- Ratios between circulating myeloid cells and lymphocytes are associated with mortality in severe COVID-19 patients
- Risk factors of left atrial appendage thrombus in patients with non-valvular atrial fibrillation
- Clinical features of hypertensive patients with COVID-19 compared with a normotensive group: Single-center experience in China
- Surgical myocardial revascularization outcomes in Kawasaki disease: systematic review and meta-analysis
- Decreased chromobox homologue 7 expression is associated with epithelial–mesenchymal transition and poor prognosis in cervical cancer
- FGF16 regulated by miR-520b enhances the cell proliferation of lung cancer
- Platelet-rich fibrin: Basics of biological actions and protocol modifications
- Accurate diagnosis of prostate cancer using logistic regression
- miR-377 inhibition enhances the survival of trophoblast cells via upregulation of FNDC5 in gestational diabetes mellitus
- Prognostic significance of TRIM28 expression in patients with breast carcinoma
- Integrative bioinformatics analysis of KPNA2 in six major human cancers
- Exosomal-mediated transfer of OIP5-AS1 enhanced cell chemoresistance to trastuzumab in breast cancer via up-regulating HMGB3 by sponging miR-381-3p
- A four-lncRNA signature for predicting prognosis of recurrence patients with gastric cancer
- Knockdown of circ_0003204 alleviates oxidative low-density lipoprotein-induced human umbilical vein endothelial cells injury: Circulating RNAs could explain atherosclerosis disease progression
- Propofol postpones colorectal cancer development through circ_0026344/miR-645/Akt/mTOR signal pathway
- Knockdown of lncRNA TapSAKI alleviates LPS-induced injury in HK-2 cells through the miR-205/IRF3 pathway
- COVID-19 severity in relation to sociodemographics and vitamin D use
- Clinical analysis of 11 cases of nocardiosis
- Cis-regulatory elements in conserved non-coding sequences of nuclear receptor genes indicate for crosstalk between endocrine systems
- Four long noncoding RNAs act as biomarkers in lung adenocarcinoma
- Real-world evidence of cytomegalovirus reactivation in non-Hodgkin lymphomas treated with bendamustine-containing regimens
- Relation between IL-8 level and obstructive sleep apnea syndrome
- circAGFG1 sponges miR-28-5p to promote non-small-cell lung cancer progression through modulating HIF-1α level
- Nomogram prediction model for renal anaemia in IgA nephropathy patients
- Effect of antibiotic use on the efficacy of nivolumab in the treatment of advanced/metastatic non-small cell lung cancer: A meta-analysis
- NDRG2 inhibition facilitates angiogenesis of hepatocellular carcinoma
- A nomogram for predicting metabolic steatohepatitis: The combination of NAMPT, RALGDS, GADD45B, FOSL2, RTP3, and RASD1
- Clinical and prognostic features of MMP-2 and VEGF in AEG patients
- The value of miR-510 in the prognosis and development of colon cancer
- Functional implications of PABPC1 in the development of ovarian cancer
- Prognostic value of preoperative inflammation-based predictors in patients with bladder carcinoma after radical cystectomy
- Sublingual immunotherapy increases Treg/Th17 ratio in allergic rhinitis
- Prediction of improvement after anterior cruciate ligament reconstruction
- Effluent Osteopontin levels reflect the peritoneal solute transport rate
- circ_0038467 promotes PM2.5-induced bronchial epithelial cell dysfunction
- Significance of miR-141 and miR-340 in cervical squamous cell carcinoma
- Association between hair cortisol concentration and metabolic syndrome
- Microvessel density as a prognostic indicator of prostate cancer: A systematic review and meta-analysis
- Characteristics of BCR–ABL gene variants in patients of chronic myeloid leukemia
- Knee alterations in rheumatoid arthritis: Comparison of US and MRI
- Long non-coding RNA TUG1 aggravates cerebral ischemia and reperfusion injury by sponging miR-493-3p/miR-410-3p
- lncRNA MALAT1 regulated ATAD2 to facilitate retinoblastoma progression via miR-655-3p
- Development and validation of a nomogram for predicting severity in patients with hemorrhagic fever with renal syndrome: A retrospective study
- Analysis of COVID-19 outbreak origin in China in 2019 using differentiation method for unusual epidemiological events
- Laparoscopic versus open major liver resection for hepatocellular carcinoma: A case-matched analysis of short- and long-term outcomes
- Travelers’ vaccines and their adverse events in Nara, Japan
- Association between Tfh and PGA in children with Henoch–Schönlein purpura
- Can exchange transfusion be replaced by double-LED phototherapy?
- circ_0005962 functions as an oncogene to aggravate NSCLC progression
- Circular RNA VANGL1 knockdown suppressed viability, promoted apoptosis, and increased doxorubicin sensitivity through targeting miR-145-5p to regulate SOX4 in bladder cancer cells
- Serum intact fibroblast growth factor 23 in healthy paediatric population
- Algorithm of rational approach to reconstruction in Fournier’s disease
- A meta-analysis of exosome in the treatment of spinal cord injury
- Src-1 and SP2 promote the proliferation and epithelial–mesenchymal transition of nasopharyngeal carcinoma
- Dexmedetomidine may decrease the bupivacaine toxicity to heart
- Hypoxia stimulates the migration and invasion of osteosarcoma via up-regulating the NUSAP1 expression
- Long noncoding RNA XIST knockdown relieves the injury of microglia cells after spinal cord injury by sponging miR-219-5p
- External fixation via the anterior inferior iliac spine for proximal femoral fractures in young patients
- miR-128-3p reduced acute lung injury induced by sepsis via targeting PEL12
- HAGLR promotes neuron differentiation through the miR-130a-3p-MeCP2 axis
- Phosphoglycerate mutase 2 is elevated in serum of patients with heart failure and correlates with the disease severity and patient’s prognosis
- Cell population data in identifying active tuberculosis and community-acquired pneumonia
- Prognostic value of microRNA-4521 in non-small cell lung cancer and its regulatory effect on tumor progression
- Mean platelet volume and red blood cell distribution width is associated with prognosis in premature neonates with sepsis
- 3D-printed porous scaffold promotes osteogenic differentiation of hADMSCs
- Association of gene polymorphisms with women urinary incontinence
- Influence of COVID-19 pandemic on stress levels of urologic patients
- miR-496 inhibits proliferation via LYN and AKT pathway in gastric cancer
- miR-519d downregulates LEP expression to inhibit preeclampsia development
- Comparison of single- and triple-port VATS for lung cancer: A meta-analysis
- Fluorescent light energy modulates healing in skin grafted mouse model
- Silencing CDK6-AS1 inhibits LPS-induced inflammatory damage in HK-2 cells
- Predictive effect of DCE-MRI and DWI in brain metastases from NSCLC
- Severe postoperative hyperbilirubinemia in congenital heart disease
- Baicalin improves podocyte injury in rats with diabetic nephropathy by inhibiting PI3K/Akt/mTOR signaling pathway
- Clinical factors predicting ureteral stent failure in patients with external ureteral compression
- Novel H2S donor proglumide-ADT-OH protects HUVECs from ox-LDL-induced injury through NF-κB and JAK/SATA pathway
- Triple-Endobutton and clavicular hook: A propensity score matching analysis
- Long noncoding RNA MIAT inhibits the progression of diabetic nephropathy and the activation of NF-κB pathway in high glucose-treated renal tubular epithelial cells by the miR-182-5p/GPRC5A axis
- Serum exosomal miR-122-5p, GAS, and PGR in the non-invasive diagnosis of CAG
- miR-513b-5p inhibits the proliferation and promotes apoptosis of retinoblastoma cells by targeting TRIB1
- Fer exacerbates renal fibrosis and can be targeted by miR-29c-3p
- The diagnostic and prognostic value of miR-92a in gastric cancer: A systematic review and meta-analysis
- Prognostic value of α2δ1 in hypopharyngeal carcinoma: A retrospective study
- No significant benefit of moderate-dose vitamin C on severe COVID-19 cases
- circ_0000467 promotes the proliferation, metastasis, and angiogenesis in colorectal cancer cells through regulating KLF12 expression by sponging miR-4766-5p
- Downregulation of RAB7 and Caveolin-1 increases MMP-2 activity in renal tubular epithelial cells under hypoxic conditions
- Educational program for orthopedic surgeons’ influences for osteoporosis
- Expression and function analysis of CRABP2 and FABP5, and their ratio in esophageal squamous cell carcinoma
- GJA1 promotes hepatocellular carcinoma progression by mediating TGF-β-induced activation and the epithelial–mesenchymal transition of hepatic stellate cells
- lncRNA-ZFAS1 promotes the progression of endometrial carcinoma by targeting miR-34b to regulate VEGFA expression
- Anticoagulation is the answer in treating noncritical COVID-19 patients
- Effect of late-onset hemorrhagic cystitis on PFS after haplo-PBSCT
- Comparison of Dako HercepTest and Ventana PATHWAY anti-HER2 (4B5) tests and their correlation with silver in situ hybridization in lung adenocarcinoma
- VSTM1 regulates monocyte/macrophage function via the NF-κB signaling pathway
- Comparison of vaginal birth outcomes in midwifery-led versus physician-led setting: A propensity score-matched analysis
- Treatment of osteoporosis with teriparatide: The Slovenian experience
- New targets of morphine postconditioning protection of the myocardium in ischemia/reperfusion injury: Involvement of HSP90/Akt and C5a/NF-κB
- Superenhancer–transcription factor regulatory network in malignant tumors
- β-Cell function is associated with osteosarcopenia in middle-aged and older nonobese patients with type 2 diabetes: A cross-sectional study
- Clinical features of atypical tuberculosis mimicking bacterial pneumonia
- Proteoglycan-depleted regions of annular injury promote nerve ingrowth in a rabbit disc degeneration model
- Effect of electromagnetic field on abortion: A systematic review and meta-analysis
- miR-150-5p affects AS plaque with ASMC proliferation and migration by STAT1
- MALAT1 promotes malignant pleural mesothelioma by sponging miR-141-3p
- Effects of remifentanil and propofol on distant organ lung injury in an ischemia–reperfusion model
- miR-654-5p promotes gastric cancer progression via the GPRIN1/NF-κB pathway
- Identification of LIG1 and LIG3 as prognostic biomarkers in breast cancer
- MitoQ inhibits hepatic stellate cell activation and liver fibrosis by enhancing PINK1/parkin-mediated mitophagy
- Dissecting role of founder mutation p.V727M in GNE in Indian HIBM cohort
- circATP2A2 promotes osteosarcoma progression by upregulating MYH9
- Prognostic role of oxytocin receptor in colon adenocarcinoma
- Review Articles
- The function of non-coding RNAs in idiopathic pulmonary fibrosis
- Efficacy and safety of therapeutic plasma exchange in stiff person syndrome
- Role of cesarean section in the development of neonatal gut microbiota: A systematic review
- Small cell lung cancer transformation during antitumor therapies: A systematic review
- Research progress of gut microbiota and frailty syndrome
- Recommendations for outpatient activity in COVID-19 pandemic
- Rapid Communication
- Disparity in clinical characteristics between 2019 novel coronavirus pneumonia and leptospirosis
- Use of microspheres in embolization for unruptured renal angiomyolipomas
- COVID-19 cases with delayed absorption of lung lesion
- A triple combination of treatments on moderate COVID-19
- Social networks and eating disorders during the Covid-19 pandemic
- Letter
- COVID-19, WHO guidelines, pedagogy, and respite
- Inflammatory factors in alveolar lavage fluid from severe COVID-19 pneumonia: PCT and IL-6 in epithelial lining fluid
- COVID-19: Lessons from Norway tragedy must be considered in vaccine rollout planning in least developed/developing countries
- What is the role of plasma cell in the lamina propria of terminal ileum in Good’s syndrome patient?
- Case Report
- Rivaroxaban triggered multifocal intratumoral hemorrhage of the cabozantinib-treated diffuse brain metastases: A case report and review of literature
- CTU findings of duplex kidney in kidney: A rare duplicated renal malformation
- Synchronous primary malignancy of colon cancer and mantle cell lymphoma: A case report
- Sonazoid-enhanced ultrasonography and pathologic characters of CD68 positive cell in primary hepatic perivascular epithelioid cell tumors: A case report and literature review
- Persistent SARS-CoV-2-positive over 4 months in a COVID-19 patient with CHB
- Pulmonary parenchymal involvement caused by Tropheryma whipplei
- Mediastinal mixed germ cell tumor: A case report and literature review
- Ovarian female adnexal tumor of probable Wolffian origin – Case report
- Rare paratesticular aggressive angiomyxoma mimicking an epididymal tumor in an 82-year-old man: Case report
- Perimenopausal giant hydatidiform mole complicated with preeclampsia and hyperthyroidism: A case report and literature review
- Primary orbital ganglioneuroblastoma: A case report
- Primary aortic intimal sarcoma masquerading as intramural hematoma
- Sustained false-positive results for hepatitis A virus immunoglobulin M: A case report and literature review
- Peritoneal loose body presenting as a hepatic mass: A case report and review of the literature
- Chondroblastoma of mandibular condyle: Case report and literature review
- Trauma-induced complete pacemaker lead fracture 8 months prior to hospitalization: A case report
- Primary intradural extramedullary extraosseous Ewing’s sarcoma/peripheral primitive neuroectodermal tumor (PIEES/PNET) of the thoracolumbar spine: A case report and literature review
- Computer-assisted preoperative planning of reduction of and osteosynthesis of scapular fracture: A case report
- High quality of 58-month life in lung cancer patient with brain metastases sequentially treated with gefitinib and osimertinib
- Rapid response of locally advanced oral squamous cell carcinoma to apatinib: A case report
- Retrieval of intrarenal coiled and ruptured guidewire by retrograde intrarenal surgery: A case report and literature review
- Usage of intermingled skin allografts and autografts in a senior patient with major burn injury
- Retraction
- Retraction on “Dihydromyricetin attenuates inflammation through TLR4/NF-kappa B pathway”
- Special Issue Computational Intelligence Methodologies Meets Recurrent Cancers - Part I
- An artificial immune system with bootstrap sampling for the diagnosis of recurrent endometrial cancers
- Breast cancer recurrence prediction with ensemble methods and cost-sensitive learning

