Abstract
Lung cancer is the most common cause of cancer-related death. Non-small cell lung cancer (NSCLC) and small cell lung cancer (SCLC) are the two major histological categories of lung cancers. Drug resistance is a great challenge for cancer treatment, and histological transformation from NSCLC to SCLC is one of the mechanisms underlying drug resistance in NSCLC patients. SCLC-transformed patients show combined characteristics of NSCLC and SCLC; however, they lack timely diagnoses and effective treatment strategies. Thus, we reviewed the clinical characteristics of SCLC transformation patients with a literature search to enhance clinical consciousness, diagnosis, and personalized treatment for patients with it.
1 Introduction
Lung cancer has the highest mortality rate among all cancer types, and it is classified into two major categories: non-small cell lung cancer (NSCLC) occurs in approximately 85% of cases, while small cell lung cancer (SCLC) accounts for the remaining 15% [1]. Adenocarcinoma and squamous cell carcinoma are the main pathological types of NSCLC, accounting for more than 70% of all cases [2]. Despite the multiple choices of antitumor therapies, the 5-year overall survival (OS) remains poor, ranging from 4 to 17%, with differences in staging and pathology [3,4]. In 2006, the first SCLC transformation was reported in a 45-year old woman who was diagnosed with adenocarcinoma and received targeted therapy, radiotherapy, and chemotherapy before re-biopsy. However, despite the combination therapy of gefitinib and etoposide after transformation, the patient did not have a good survival [5]. Since then, the histological transformation from NSCLC to SCLC has become an increasingly noticeable form of resistance in recent years. Previous studies have shown that the incidence of SCLC transformation in patients with epidermal growth factor receptor-tyrosine kinase inhibitor (EGFR-TKI) resistance was approximately 14%, and further studies showed that SCLC transformation also occurred after other types of resistance [6,7]. However, the clinical consciousness of histological transformation is suboptimal, and the treatments are still controversial. Thus, this review aimed to explore the occurrence, diagnosis, and treatment strategies of SCLC transformation using a literature search to demonstrate the clinical characteristics of patients with SCLC transformation.
2 Methods
We searched the PubMed database for studies published until February 2020. The search keywords included “NSCLC,” “SCLC,” “adenocarcinoma,” “squamous cell carcinoma,” and “transformation.” Two investigators independently searched for and screened the literature. The included studies focused on patients who underwent transformation from NSCLC to SCLC. Clinical cases, retrospective studies, and clinical trials were eligible, and the included studies were published in English. The exclusion criteria included basic research, studies focused on other types of cancer, non-English articles, and review articles. A total of 451 published studies were found, of which 90 studies were left after screening abstracts. Seventy studies were finally included after a further screening of the full texts. The retrieval flow chart is shown in Figure 1.
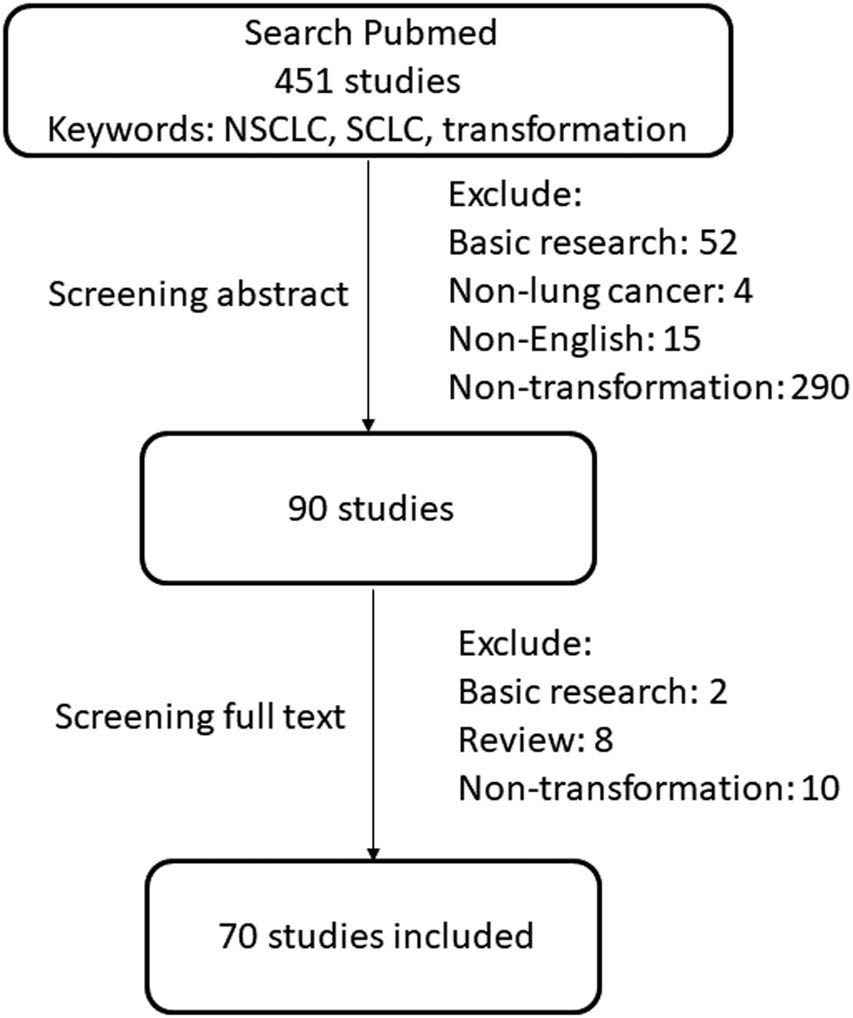
The retrieval flow chart.
Among the 70 studies, most were published in Asian countries (45 studies, 64.3%). Despite 132 transformed SCLC patients without specific information in five retrospective studies (summarized in Table 1), 65 studies with 104 patients were included in the following analysis, where we summarized the clinical characteristics of patients with transformed SCLC.
Characteristics of five retrospective studies
| Patients | Year | Country | Pathologic types | Prognosis | References | |
|---|---|---|---|---|---|---|
| 1 | 46 | 2018 | US | 30 Adenocarcinoma | mOS: 304 days | [58] |
| 16 Squamous cell carcinoma | ||||||
| 2 | 3 | 2019 | Korea | Adenocarcinoma | — | [59] |
| 3 | 4 | 2019 | France | Adenocarcinoma | — | [60] |
| 4 | 58 | 2018 | US | Adenocarcinoma | mOS: 10.9 months | [42] |
| 5 | 21 | 2017 | Korea | Adenocarcinoma | — | [26] |
mOS: median overall survival.
3 Clinical characteristics of patients with SCLC transformation
3.1 Clinical characteristics before transformation
The clinical characteristics of the patients are summarized in Figure 2. Of the 86 patients with reported gender information, 50 (58.1%) were women and 36 (42%) were men. Transformation mostly occurred in patients aged 61–70 years (26 patients, 29.5%), followed by the 51–60 years group (24 patients, 27.3%) and 41−50 years group (22 patients, 25%). Among the 80 patients with a history of smoking, 33 (41.3%) were previous or current smokers, while 47 (58.8%) were nonsmokers. Five patients were diagnosed with preexisting disease, and three patients had a history of other types of cancer.
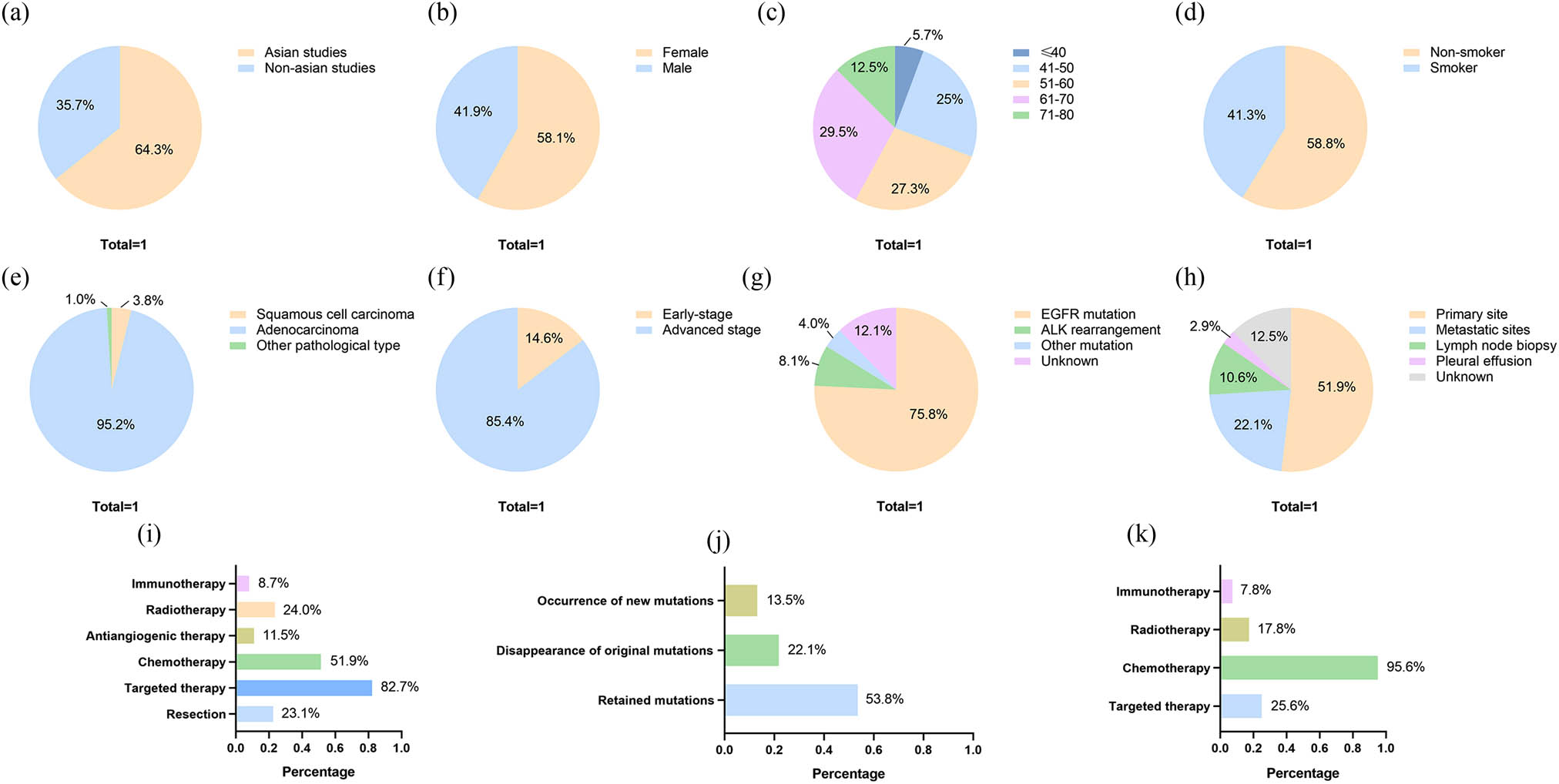
Clinical characteristics of patients. (a) Published countries of studies. (b) Gender information of patients. (c) Age of patients. (d) Smoking history of patients. (e) Pathological type of patients. (f) Stage information of patients. (g) Mutations of patients with adenocarcinoma. (h) Re-biopsy sites of patients. (i) Treatments before transformation. (j) Mutations in re-biopsy. (k) Treatments after transformation.
Eighty-two patients were diagnosed based on TNM stage information, 70 patients (85.4%) were diagnosed with locally advanced or metastatic NSCLC, while 12 patients (14.6%) were diagnosed with early stage NSCLC. Histologically, the main pathological type was adenocarcinoma (99 patients, 95.2%), and four patients (3.8%) were diagnosed with squamous cell carcinoma. Among the 99 adenocarcinoma patients, epidermal growth factor receptor (EGFR) mutations were detected in 75 patients (75.8%), and ALK rearrangement was found in eight patients (8.1%). In addition, three patients had K-RAS mutations, and one patient had PD-L1 positive NSCLC.
Based on the pathological types and gene mutations, the majority of patients were administered targeted therapy (86 patients, 82.7%) or chemotherapy (54 patients, 51.9%). Besides, 25 patients (24.0%) received radiotherapy, 24 patients (23.1%) underwent resection at the primary site, 12 patients (11.5%) received antiangiogenic therapy, and nine patients (8.7%) received immunotherapy.
3.2 Clinical characteristics after transformation
Re-biopsy is necessary for the detection of SCLC transformation. Apart from the 13 patients (12.5%) without a description of the method of re-biopsy, most of the patients (54 patients, 51.9%) underwent re-biopsy at the primary site, 23 patients (22.1%) were diagnosed with transformation through a biopsy at the metastatic sites, 11 patients were diagnosed (10.6%) through lymph node biopsy, and three patients (2.9%) had cytological evidence of pleural effusion. Considering that gene mutations can guide treatment decisions, a second mutation test was also significant. Fifty-six patients (53.8%) were found to have retained mutations during re-biopsy similar to those for the initial diagnosis. The original mutations could not be found in 23 patients (22.1%), and new mutations were observed in 14 patients (13.5%), five of whom were found to have the Thr790Met mutation. In some cases, the disappearance of the original mutation occurs simultaneously with the appearance of a new mutation. For example, it has been reported that a patient showed the disappearance of the original exon 19 mutation and a new L858R and Thr790Met mutation during re-biopsy at the same time [8]. Another patient was found to have reduced expression of programmed cell death ligand 1 (PD-L1) from 30% to less than 1% [9]. In addition, 19 patients were reported to have changes in tumor biomarkers; 14 patients were found to have an increase in neuron-specific enolase (NSE) and eight patients had an increase in prn-gastrin-releasing peptide (Pro-GRP).
Regarding the treatments for SCLC transformation, treatment strategies after diagnosis with transformation were reported for 90 patients. Almost all patients (86 patients, 95.6%) received chemotherapy (mainly platinum and etoposide), which is widely recognized as a sensitive therapy for SCLC. Twenty-three patients (25.6%) underwent targeted therapy according to the results of the gene mutations, 16 patients (17.8%) received radiotherapy, and seven patients (7.8%) received immunotherapy.
4 Enhanced awareness and individualized treatment
4.1 Explore potential mechanism
Currently, there are two major hypotheses on the mechanism of transformation from NSCLC to SCLC. The first hypothesis suggested that both NSCLC and SCLC components coexisted in tumor tissues, and only a part of them were detected during the initial biopsy, which gradually became dominant after treatment for NSCLC. Some patients were initially diagnosed with combined NSCLC and SCLC without receiving any antitumor treatment, which supports this hypothesis [10]. However, SCLC transformation was also observed in patients who underwent tumor resection with abundant histopathological tissue. In addition, SCLC patients without timely treatment progressed rapidly and had a poor prognosis, and their progression-free survival (PFS) was significantly reduced, which was also contrary to the hypothesis [11].
The second hypothesis was the theory for the transformation from NSCLC to SCLC, in which tumor stem cells would differentiate into NSCLC cells before undergoing SCLC transformation during the process of proliferation under the influence of external factors, such as EGFR-TKI treatment. Studies have demonstrated that epigenetic regulation is associated with changes in cell fate; transdifferentiation is a type of cell lineage plasticity, while mechanistic exploration has not been fully elucidated [12]. Current studies have shown that tumor cells first enter a reversible slow-growing drug-tolerant state, called “drug-tolerant persisters (DTPs),” and sensitivity can be regained after removing external stimuli [13,14,15]. DTPs can further acquire permanent resistance through reprogramming, which is associated with epigenetic changes, transcription factors, key signaling pathways, and complex tumor microenvironments [16,17]. Takagi et al. reported a 70-year-old woman diagnosed with a mixed component of SCLC and adenocarcinoma, with a rare mutation, L861Q, in both parts, which suggested that SCLC and NSCLC were more likely from the same progenitor [18]. In addition, more than half of the patients retained their original mutations after transformation according to our statistics, which also supported the second hypothesis.
The transformation of SCLC was also demonstrated at the molecular level in processes including retinoblastoma 1 gene (RB1) deletion and tumor protein p53 gene (TP53) inactivation [19]. The deletion of RB1 can cause the inhibition of entry into the S-phase of cell cycles, which plays an important role in the tumorigenesis of SCLC [12]. RB1 deletions result in an expression deficiency of retinoblastoma protein, which is one of the significant differences between SCLC and NSCLC [20,21]. TP53 is a tumor suppressor gene, and the inactivation of TP53 leads to an abnormal regulatory effect on cell growth, apoptosis, and DNA repair, which plays an important role in tumor formation [22,23]. Previous studies have shown that TP53-deficient and RB1-deficient cells are involved in the lineage plasticity and neuroendocrine differentiation process, but further evidence is needed to confirm whether there is a causal relationship between these molecular changes and pathological phenotypic changes [24,25]. Currently, complete inactivation of RB1 and TP53 is widely accepted as a predictive biomarker for SCLC transformation [26]. Clinicians should pay more attention to monitoring SCLC transformation during the treatment of NSCLC patients with an inactivated RB1 or P53, and the assessment of RB1 and TP53 status should be performed when the disease progresses, which may unravel a potential SCLC transformation [27]. In addition, other immunohistochemical characteristics of SCLC, including synaptophysin, chromogranin, and CD56, were also found after transformation, which is worthy of further attention [7].
4.2 Raise consciousness of transformation
According to the basic clinical characteristics of the current study, it was found that the transformation to SCLC from NSCLC mainly occurred in patients with EGFR-mutant advanced adenocarcinoma with a greater tendency of female Asian patients without a smoking history. The proportion was similar to that of EGFR mutations, which emerged mainly in Asian patients and mostly in adenocarcinoma, women, and never-smokers [4]. SCLC transformation is widely accepted as one of the drug resistance mechanisms of targeted therapy, and previous studies have mainly focused on the transformation of adenocarcinoma; only a few studies have reported patients with squamous cell carcinoma [7]. A possible reason is that alveolar type II cells can differentiate into both EGFR-mutant adenocarcinoma and SCLC, which may contribute to a higher likelihood of SCLC transformation in patients with EGFR-mutant adenocarcinomas [11]. Another possible reason is the high frequency of gene mutations and subsequent resistance to antitumor therapies in patients with adenocarcinoma. Consequently, adenocarcinoma patients with gene mutations were more likely to have re-biopsies and to be diagnosed with SCLC transformation. However, transformation occurred not only in patients with EGFR mutations, but also in patients with ALK rearrangement and other uncommon mutations, and SCLC transformation was also found in patients with wild-type mutations and squamous cell carcinomas [28,29,30]. Thus, the bias associated with clinical practice cannot be ignored. For patients with wild-type mutations or squamous cell carcinomas, re-biopsy should also be considered to detect transformation when the disease progresses.
Subsequently, the transformation of SCLC may occur after various treatment strategies, including different generations of targeted therapies, as well as other antitumor therapies, including chemotherapy, radiotherapy, antiangiogenic therapy, and immunotherapy [31]. When hyper-progressive disease occurs during immunotherapy, SCLC transformation should also not be overlooked, as it may be a cause of resistance to immunotherapy [32]. Thus, despite paying attention to the mechanism of drug resistance after targeted therapy when progressive disease occurs, clinicians should also be aware of transformed SCLC arising after other antitumor therapies. Further studies can explore the potential of SCLC transformation among various NSCLC subsets and patients after different treatment therapies.
Meanwhile, SCLC transformation should be distinguished from combined small cell lung cancer (C-SCLC), which is defined as a subtype of SCLC with an incidence of approximately 2–23% of SCLC [33,34]. Although the potential mechanisms are still unclear, current research suggests that the most common pathological type is squamous cell carcinoma and large cell neuroendocrine carcinoma [35]. C-SCLC was more likely to be found in older men with a long smoking history, which is similar to the incidence of SCLC [36,37].
4.3 Strengthen the early diagnostic capacity
Since the majority of patients were preliminarily diagnosed with advanced disease, and disease progression also reduced the likelihood of resection, re-biopsy was necessary for the diagnosis of transformation. In addition to re-biopsy of primary sites, re-biopsies from lymph nodes and metastatic sites could also be conducive to the detection and diagnosis of transformation, and the detection of pleural effusion was also an auxiliary diagnostic method. It was also necessary to carry out gene mutation detection in the re-biopsied tissues. Considering that nearly half of the patients retained mutations, both the disappearance of original mutations and new mutations may occur. Thus, timely detection can facilitate better treatment strategies when drug resistance or unexpected treatment response occurs.
Moreover, patients with SCLC transformation may have multiple tumor lesions with different pathological types. For instance, a non-smoking 76-year-old woman was diagnosed with clinical stage IIIB NSCLC; after chemotherapy and radiotherapy, multiple lung metastases were found 15 months later, and she received targeted therapy until death. At autopsy, nine metastatic lesions were found with different pathological types, including six SCLCs, two NSCLCs, and one retroperitoneal lymph node with combined histology. Furthermore, an EGFR exon 19 deletion mutation was found in all lesions, while the T790M mutation was only found in adenocarcinoma lesions [38]. Therefore, the transformation may be partial and multiple, and the diversity of transformation should not be overlooked, especially for metastatic lesions. This emphasizes the significance of biopsy and suggests a supplemental role of next-generation sequencing (NGS) for ctDNA.
In addition, data showed that some patients had increased tumor biomarkers associated with SCLC, and the most common tumor biomarkers were NSE and Pro-GRP. Although the sensitivity and specificity of tumor biomarkers should be further investigated, considering the simplicity and dynamics of detection, they may provide an early clue for re-biopsy and serve as an auxiliary diagnostic method for SCLC transformation. Thus, in addition to regular imaging evaluations, the monitoring of tumor biomarkers during treatment should also be applied in clinical practice. An elevated NSE or Pro-GRP may be considered for its potential to facilitate transformation.
4.4 Proceed active personalized treatment
The prognosis and survival period varied among patients, and most patients who underwent transformation had been treated with multiline treatments. The overall prognosis was poor, and it was associated with the physical condition of the patients. A systematic review that included 39 adenocarcinoma patients showed a median duration of 19 months from the initial diagnosis to SCLC transformation, and a median survival duration of 6 months after the transformed SCLC diagnosis [39]. To improve the prognosis of patients, both the prevention of transformation and personalized treatment after transformation were significant. Effective strategies to prevent transformation include intermittent treatment, combination therapy, and the inhibition of molecular pathways regulating cell lineage plasticity; however, specific treatment regimens and mechanisms still require further exploration [16].
For personalized treatment after transformation, epigenetics showed that transformed SCLC was more similar to SCLC than NSCLC based on their mRNA expressions and drug sensitivities [40]. Previous studies have also shown that chemotherapy, which is sensitive to classic SCLC (platinum and etoposide), may be the best treatment option for transformed SCLC, and taxanes also showed high response rates [41,42]. However, some transformed SCLC may partially retain the characteristics of NSCLC, and treatments for NSCLC and SCLC differ substantially. Despite the generally recognized SCLC-sensitive chemotherapy, treatment strategies should be decided after thorough considerations, and specific individualized treatments should be administered, considering the pathological and gene mutation results of re-biopsies. For instance, a SCLC-transformed patient with both exon 19 deletion and Thr790Met mutation received a combination of chemotherapy and osimertinib and achieved obvious clinical responses [43]. Another patient with an initial EGFR L858R mutation received alternating therapy of chemotherapy (carboplatin and irinotecan) and osimertinib for one year after SCLC transformation. The serum level of the tumor biomarkers showed that osimertinib led to a decrease in sialyl Lewis X (SLX), while the pro-GRP levels declined after administration of chemotherapy [44]. A 76-year-old female patient with EGFR L858R-mutant adenocarcinoma was diagnosed with SCLC transformation with consistent L858R mutation and received chemotherapy (cisplatin and etoposide) as the subsequent treatment for 5 months, after which she underwent both chemotherapy and immunotherapy (amrubicin, nivolumab, and irinotecan); however, further progression was observed after 6 months, and a second re-biopsy revealed both L858R and T790M mutations, which led to the administration of osimertinib, and a partial response was achieved and lasted for 3 months [45]. In addition, some of the SCLC-transformed patients experienced further gene mutations and histologic changes, and it was reported that NSCLC could be dominant again during treatment [46,47,48,49]. Therefore, treatment strategies should be selected according to the individual characteristics of patients. Considering that the histopathological types and gene mutations may change during the process of treatment for transformation, continuous monitoring and repeated re-biopsy are of significance for treatment decisions.
Moreover, clinical trials have shown that immune checkpoint inhibitors can improve the prognosis of patients with NSCLC and SCLC [50,51,52,53]. However, it has also been suggested that the application of EGFR-TKIs may reduce the expression of PD-L1 [9,54]. A previous retrospective study demonstrated that patients with transformed SCLC from EGFR-mutant adenocarcinomas had a poor response to checkpoint inhibitors [42]. Several cases have reported patients administered immunotherapy after SCLC transformation in clinical practice. Three cases reported patients with EGFR-mutant adenocarcinoma receiving immunotherapy (nivolumab) following other treatments and disease progression after SCLC transformation; however, immunotherapy did not show much efficacy [9,45,55]. Two patients with squamous cell NSCLC who were previously treated with nivolumab also received nivolumab after SCLC transformation; however, one patient experienced disease progression after 1 month, while the other was lost to follow-up [29]. A 62‑year‑old male patient with ALK rearrangement adenocarcinoma received subsequent combined immunotherapy and chemotherapy (amrubicin, irinotecan, and nivolumab) after SCLC transformation following targeted therapy and chemotherapy, which also showed a poor response [56]. A 75-year-old female patient with advanced KRAS G12C-mutant lung adenocarcinoma had previously received 33 cycles of nivolumab as second-line therapy. After SCLC transformation, she received chemotherapy (carboplatin and etoposide), immunotherapy (nivolumab and ipilimumab), and chemotherapy (irinotecan) in sequence and achieved a further 16-month survival [57]. Therefore, further investigations to determine whether immunotherapy or combined immunotherapy is promising for patients with SCLC transformation are recommended, and the levels of expression of PD-L1 should be monitored.
5 Conclusion
In conclusion, the transformation from NSCLC to SCLC should be further researched as a specific phenotype, as it has distinct characteristics from those of NSCLC and SCLC. Clinicians should be aware of the significance of re-biopsy and the dynamic monitoring of relevant biomarkers. Precision medicine is necessary for transformed patients based on individualized characteristics.
-
Author contributions: The manuscript has been read and approved by all the authors, all journal requirements for authorship have been met, and each author believes that the manuscript represents honest work.
-
Conflict of interest: All authors have completed the ICMJE uniform disclosure form. The authors declare no conflict of interest.
-
Data availability statement: All data generated or analyzed during this study are included in this published article.
References
[1] Pikor LA, Ramnarine VR, Lam S, Lam WL. Genetic alterations defining NSCLC subtypes and their therapeutic implications. Lung Cancer. 2013;82(2):179–89.10.1016/j.lungcan.2013.07.025Search in Google Scholar
[2] Travis WD, Brambilla E, Nicholson AG, Yatabe Y, Austin JHM, Beasley MB, et al. The 2015 world health organization classification of lung tumors: impact of genetic, clinical and radiologic advances since the 2004 classification. J Thorac Oncol. 2015;10(9):1243–60.10.1097/JTO.0000000000000630Search in Google Scholar
[3] Arbour KC, Riely GJ. Systemic therapy for locally advanced and metastatic non-small cell lung cancer: a review. Jama. 2019;322(8):764–74.10.1001/jama.2019.11058Search in Google Scholar
[4] Hirsch FR, Scagliotti GV, Mulshine JL, Kwon R, Curran WJ Jr, Wu YL, et al. Lung cancer: current therapies and new targeted treatments. Lancet. 2017;389(10066):299–311.10.1016/S0140-6736(16)30958-8Search in Google Scholar
[5] Zakowski MF, Ladanyi M, Kris MG. EGFR mutations in small-cell lung cancers in patients who have never smoked. N Engl J Med. 2006;355(2):213–5.10.1056/NEJMc053610Search in Google Scholar PubMed
[6] Shao Y, Zhong DS. Histological transformation after acquired resistance to epidermal growth factor tyrosine kinase inhibitors. Int J Clin Oncol. 2018;23(2):235–42.10.1007/s10147-017-1211-1Search in Google Scholar PubMed
[7] Hobeika C, Rached G, Eid R, Haddad F, Chucri S, Kourie HR, et al. ALK-rearranged adenocarcinoma transformed to small-cell lung cancer: a new entity with specific prognosis and treatment. Per Med. 2018;15(2):111–5.10.2217/pme-2017-0069Search in Google Scholar PubMed
[8] Norkowski E, Ghigna MR, Lacroix L, Le Chevalier T, Fadel É, Dartevelle P, et al. Small-cell carcinoma in the setting of pulmonary adenocarcinoma: new insights in the era of molecular pathology. J Thorac Oncol. 2013;8(10):1265–71.10.1097/JTO.0b013e3182a407faSearch in Google Scholar PubMed
[9] Nishikawa S, Tambo Y, Ninomiya H, Oguri T, Kawashima Y, Takano N, et al. A case treated with nivolumab after small cell lung cancer transformation of mutant EGFR non-small cell lung cancer. Ann Oncol. 2016;27(12):2300–2.10.1093/annonc/mdw431Search in Google Scholar PubMed
[10] Lu HY, Mao WM, Cheng QY, Chen B, Cai JF, Wang XJ, et al. Mutation status of epidermal growth factor receptor and clinical features of patients with combined small cell lung cancer who received surgical treatment. Oncol Lett. 2012;3(6):1288–92.10.3892/ol.2012.666Search in Google Scholar PubMed PubMed Central
[11] Oser MG, Niederst MJ, Sequist LV, Engelman JA. Transformation from non-small-cell lung cancer to small-cell lung cancer: molecular drivers and cells of origin. Lancet Oncol. 2015;16(4):e165–72.10.1016/S1470-2045(14)71180-5Search in Google Scholar
[12] Rudin CM, Brambilla E, Faivre-Finn C, Sage J. Small-cell lung cancer. Nat Rev Dis Primers. 2021 Jan 14;7(1):3.10.1038/s41572-020-00235-0Search in Google Scholar PubMed PubMed Central
[13] Hata AN, Niederst MJ, Archibald HL, Gomez-Caraballo M, Siddiqui FM, Mulvey HE, et al. Tumor cells can follow distinct evolutionary paths to become resistant to epidermal growth factor receptor inhibition. Nat Med. 2016 Mar;22(3):262–9.10.1038/nm.4040Search in Google Scholar PubMed PubMed Central
[14] Sharma SV, Lee DY, Li B, Quinlan MP, Takahashi F, Maheswaran S, et al. A chromatin-mediated reversible drug-tolerant state in cancer cell subpopulations. Cell. 2010 Apr 2;141(1):69–80.10.1016/j.cell.2010.02.027Search in Google Scholar PubMed PubMed Central
[15] Shaffer SM, Dunagin MC, Torborg SR, Torre EA, Emert B, Krepler C, et al. Rare cell variability and drug-induced reprogramming as a mode of cancer drug resistance. Nature. 2017 Jun 15;546(7658):431–5.10.1038/nature22794Search in Google Scholar PubMed PubMed Central
[16] Boumahdi S, de Sauvage FJ. The great escape: tumour cell plasticity in resistance to targeted therapy. Nat Rev Drug Discov. 2020 Jan;19(1):39–56.10.1038/s41573-019-0044-1Search in Google Scholar PubMed
[17] Quintanal-Villalonga Á, Chan JM, Yu HA, Pe’er D, Sawyers CL, Sen T, et al. Lineage plasticity in cancer: a shared pathway of therapeutic resistance. Nat Rev Clin Oncol. 2020 Jun;17(6):360–71.10.1038/s41571-020-0340-zSearch in Google Scholar PubMed PubMed Central
[18] Takagi Y, Nakahara Y, Hosomi Y, Hishima T. Small-cell lung cancer with a rare epidermal growth factor receptor gene mutation showing “wax-and-wane” transformation. BMC Cancer. 2013;13:529.10.1186/1471-2407-13-529Search in Google Scholar PubMed PubMed Central
[19] George J, Lim JS, Jang SJ, Cun Y, Ozretić L, Kong G, et al. Comprehensive genomic profiles of small cell lung cancer. Nature. 2015 Aug 6;524(7563):47–53.10.1038/nature14664Search in Google Scholar PubMed PubMed Central
[20] Hamilton G, Rath B, Ulsperger E. How to target small cell lung cancer. Oncoscience. 2015;2(8):684–92.10.18632/oncoscience.212Search in Google Scholar PubMed PubMed Central
[21] Park KS, Liang MC, Raiser DM, Zamponi R, Roach RR, Curtis SJ, et al. Characterization of the cell of origin for small cell lung cancer. Cell Cycle. 2011;10(16):2806–15.10.4161/cc.10.16.17012Search in Google Scholar PubMed PubMed Central
[22] George J, Lim JS, Jang SJ, Cun Y, Ozretić L, Kong G, et al. Comprehensive genomic profiles of small cell lung cancer. Nature. 2015;524(7563):47–53.10.1038/nature14664Search in Google Scholar PubMed PubMed Central
[23] Almodovar K, Iams WT, Meador CB, Zhao Z, York S, Horn L, et al. Longitudinal cell-free DNA analysis in patients with small cell lung cancer reveals dynamic insights into treatment efficacy and disease relapse. J Thorac Oncol. 2018;13(1):112–23.10.1016/j.jtho.2017.09.1951Search in Google Scholar PubMed PubMed Central
[24] Dick FA, Goodrich DW, Sage J, Dyson NJ. Non-canonical functions of the RB protein in cancer. Nat Rev Cancer. 2018 Jul;18(7):442–51.10.1038/s41568-018-0008-5Search in Google Scholar PubMed PubMed Central
[25] Ku SY, Rosario S, Wang Y, Mu P, Seshadri M, Goodrich ZW, et al. Rb1 and Trp53 cooperate to suppress prostate cancer lineage plasticity, metastasis, and antiandrogen resistance. Science. 2017 Jan 6;355(6320):78–83.10.1126/science.aah4199Search in Google Scholar PubMed PubMed Central
[26] Lee JK, Lee J, Kim S, Kim S, Youk J, Park S, et al. Clonal history and genetic predictors of transformation into small-cell carcinomas from lung adenocarcinomas. J Clin Oncol. 2017;35(26):3065–74.10.1200/JCO.2016.71.9096Search in Google Scholar PubMed
[27] Sutherland KD, Proost N, Brouns I, Adriaensen D, Song JY, Berns A. Cell of origin of small cell lung cancer: inactivation of Trp53 and Rb1 in distinct cell types of adult mouse lung. Cancer Cell. 2011;19(6):754–64.10.1016/j.ccr.2011.04.019Search in Google Scholar PubMed
[28] O’Leary CG, Corrigan L, Martin P, Horgan A, O’Connor M, Calvert P. Epidermal growth factor receptor mutated oligometastatic adeno-squamous lung cancer transformation to small cell lung cancer. Oxf Med Case Reports. 2018;2018(10):omy078.10.1093/omcr/omy078Search in Google Scholar PubMed PubMed Central
[29] Bar J, Ofek E, Barshack I, Gottfried T, Zadok O, Kamer I, et al. Transformation to small cell lung cancer as a mechanism of resistance to immunotherapy in non-small cell lung cancer. Lung Cancer. 2019;138:109–15.10.1016/j.lungcan.2019.09.025Search in Google Scholar PubMed
[30] Abdallah N, Nagasaka M, Abdulfatah E, Shi D, Wozniak AJ, Sukari A. Non-small cell to small cell lung cancer on PD-1 inhibitors: two cases on potential histologic transformation. Lung Cancer (Auckl). 2018;9:85–90.10.2147/LCTT.S173724Search in Google Scholar PubMed PubMed Central
[31] Imakita T, Fujita K, Kanai O, Terashima T, Mio T. Small cell lung cancer transformation during immunotherapy with nivolumab: a case report. Respir Med Case Rep. 2017;21:52–5.10.1016/j.rmcr.2017.03.019Search in Google Scholar PubMed PubMed Central
[32] Okeya K, Kawagishi Y, Muranaka E, Izumida T, Tsuji H, Takeda S. Hyperprogressive disease in lung cancer with transformation of adenocarcinoma to small-cell carcinoma during pembrolizumab therapy. Intern Med. 2019;58(22):3295–8.10.2169/internalmedicine.2892-19Search in Google Scholar PubMed PubMed Central
[33] Travis WD. Update on small cell carcinoma and its differentiation from squamous cell carcinoma and other non-small cell carcinomas. Mod Pathol. 2012;25(Suppl 1):S18–30.10.1038/modpathol.2011.150Search in Google Scholar PubMed
[34] Shao N, Cai Q. High pretreatment neutrophil-lymphocyte ratio predicts recurrence and poor prognosis for combined small cell lung cancer. Clin Transl Oncol. 2015;17(10):772–8.10.1007/s12094-015-1289-8Search in Google Scholar PubMed
[35] Babakoohi S, Fu P, Yang M, Linden PA, Dowlati A. Combined SCLC clinical and pathologic characteristics. Clin Lung Cancer. 2013;14(2):113–9.10.1016/j.cllc.2012.07.002Search in Google Scholar PubMed
[36] Hassan WA, Takebayashi SI, Abdalla MOA, Fujino K, Kudoh S, Motooka Y, et al. Correlation between histone acetylation and expression of Notch1 in human lung carcinoma and its possible role in combined small-cell lung carcinoma. Lab Invest. 2017;97(8):913–21.10.1038/labinvest.2017.36Search in Google Scholar PubMed
[37] Cerami E, Gao J, Dogrusoz U, Gross BE, Sumer SO, Aksoy BA, et al. The cBio cancer genomics portal: an open platform for exploring multidimensional cancer genomics data. Cancer Discov. 2012;2(5):401–4.10.1158/2159-8290.CD-12-0095Search in Google Scholar PubMed PubMed Central
[38] Suda K, Murakami I, Sakai K, Mizuuchi H, Shimizu S, Sato K, et al. Small cell lung cancer transformation and T790M mutation: complimentary roles in acquired resistance to kinase inhibitors in lung cancer. Sci Rep. 2015;5:14447.10.1038/srep14447Search in Google Scholar PubMed PubMed Central
[39] Roca E, Gurizzan C, Amoroso V, Vermi W, Ferrari V, Berruti A. Outcome of patients with lung adenocarcinoma with transformation to small-cell lung cancer following tyrosine kinase inhibitors treatment: a systematic review and pooled analysis. Cancer Treat Rev. 2017;59:117–22.10.1016/j.ctrv.2017.07.007Search in Google Scholar PubMed
[40] Dorantes-Heredia R, Ruiz-Morales JM, Cano-Garcia F. Histopathological transformation to small-cell lung carcinoma in non-small cell lung carcinoma tumors. Transl Lung Cancer Res. 2016;5(4):401–12.10.21037/tlcr.2016.07.10Search in Google Scholar PubMed PubMed Central
[41] Shao Y, Zhong DS. Histological transformation after acquired resistance to epidermal growth factor tyrosine kinase inhibitors. Int J Clin Oncol. 2018;23(2):235–42.10.1007/s10147-017-1211-1Search in Google Scholar PubMed
[42] Marcoux N, Gettinger SN, O’Kane G, Arbour KC, Neal JW, Husain H, et al. EGFR-Mutant adenocarcinomas that transform to small-cell lung cancer and other neuroendocrine carcinomas: clinical outcomes. J Clin Oncol. 2019;37(4):278–85.10.1200/JCO.18.01585Search in Google Scholar PubMed PubMed Central
[43] Tang K, Jiang N, Kuang Y, He Q, Li S, Luo J, et al. Overcoming T790M mutant small cell lung cancer with the third-generation EGFR-TKI osimertinib. Thoracic Cancer. 2019;10(2):359–64.10.1111/1759-7714.12927Search in Google Scholar PubMed PubMed Central
[44] Hirakawa H, Komiya K, Nakashima C, Ogusu S, Nakamura T, Tanaka M, et al. A case of osimertinib-resistant lung adenocarcinoma responded effectively to alternating therapy. Ann Transl Med. 2018;6(23):464.10.21037/atm.2018.11.25Search in Google Scholar PubMed PubMed Central
[45] Sonoda T, Nishikawa S, Sakakibara R, Saiki M, Ariyasu R, Koyama J, et al. EGFR T790M mutation after chemotherapy for small cell lung cancer transformation of EGFR-positive non-small cell lung cancer. Respir Med Case Rep. 2018;24:19–21.10.1016/j.rmcr.2018.03.009Search in Google Scholar PubMed PubMed Central
[46] Sequist LV, Waltman BA, Dias-Santagata D, Digumarthy S, Turke AB, Fidias P, et al. Genotypic and histological evolution of lung cancers acquiring resistance to EGFR inhibitors. Sci Transl Med. 2011;3(75):75ra26.10.1126/scitranslmed.3002003Search in Google Scholar PubMed PubMed Central
[47] Morinaga R, Okamoto I, Furuta K, Kawano Y, Sekijima M, Dote K, et al. Sequential occurrence of non-small cell and small cell lung cancer with the same EGFR mutation. Lung Cancer. 2007;58(3):411–3.10.1016/j.lungcan.2007.05.014Search in Google Scholar PubMed
[48] Iacono D, Osman GA, Migliorino MR, Grillo L, Remotti D, Nunnari J, et al. Intrapatient molecular and histologic heterogeneity after first-generation or second-generation TKI therapy of NSCLC patients: potential clinical impact on subsequent third-generation TKI treatment. Am J Clin Oncol. 2019;42(11):845–50.10.1097/COC.0000000000000615Search in Google Scholar PubMed
[49] Xie Z, Gu Y, Lin X, Ouyang M, Qin Y, Zhang J, et al. Unexpected favorable outcome to etoposide and cisplatin in a small cell lung cancer transformed patient: a case report. Cancer Biol Ther. 2019;20(9):1172–5.10.1080/15384047.2019.1617561Search in Google Scholar PubMed PubMed Central
[50] Chung HC, Piha-Paul SA, Lopez-Martin J, Schellens JHM, Kao S, Miller WH Jr, et al. Pembrolizumab after two or more lines of previous therapy in patients with recurrent or metastatic SCLC: results from the KEYNOTE-028 and KEYNOTE-158 studies. J Thorac Oncol. 2019;15(4):618–27.10.1016/j.jtho.2019.12.109Search in Google Scholar PubMed
[51] Gadgeel SM, Pennell NA, Fidler MJ, Halmos B, Bonomi P, Stevenson J, et al. Phase II study of maintenance pembrolizumab in patients with extensive-stage small cell lung cancer (SCLC). J Thorac Oncol. 2018;13(9):1393–9.10.1016/j.jtho.2018.05.002Search in Google Scholar PubMed PubMed Central
[52] Gandhi L, Rodríguez-Abreu D, Gadgeel S, Esteban E, Felip E, De Angelis F, et al. Pembrolizumab plus chemotherapy in metastatic non-small-cell lung cancer. N Engl J Med. 2018;378(22):2078–92.10.1056/NEJMoa1801005Search in Google Scholar PubMed
[53] Vokes EE, Ready N, Felip E, Horn L, Burgio MA, Antonia SJ, et al. Nivolumab versus docetaxel in previously treated advanced non-small-cell lung cancer (CheckMate 017 and CheckMate 057): 3-year update and outcomes in patients with liver metastases. Ann Oncol. 2018;29(4):959–65.10.1093/annonc/mdy041Search in Google Scholar PubMed
[54] Chen N, Fang W, Zhan J, Hong S, Tang Y, Kang S, et al. Upregulation of PD-L1 by EGFR activation mediates the immune escape in EGFR-driven NSCLC: implication for optional immune targeted therapy for NSCLC patients with EGFR mutation. J Thorac Oncol. 2015;10(6):910–23.10.1097/JTO.0000000000000500Search in Google Scholar PubMed
[55] Tokaca N, Wotherspoon A, Nicholson AG, Fotiadis N, Thompson L, Popat S. Lack of response to nivolumab in a patient with EGFR-mutant non-small cell lung cancer adenocarcinoma sub-type transformed to small cell lung cancer. Lung Cancer. 2017;111:65–8.10.1016/j.lungcan.2017.07.012Search in Google Scholar PubMed
[56] Oya Y, Yoshida T, Uemura T, Murakami Y, Inaba Y, Hida T. Serum ProGRP and NSE levels predicting small cell lung cancer transformation in a patient with ALK rearrangement-positive non-small cell lung cancer: a case report. Oncol Lett. 2018;16(4):4219–22.10.3892/ol.2018.9158Search in Google Scholar PubMed PubMed Central
[57] Iams WT, Beckermann KE, Almodovar K, Hernandez J, Vnencak-Jones C, Lim LP, et al. Small cell lung cancer transformation as a mechanism of resistance to PD-1 therapy in KRAS-mutant lung adenocarcinoma: a report of two cases. J Thorac Oncol. 2019;14(3):e45–8.10.1016/j.jtho.2018.11.031Search in Google Scholar PubMed PubMed Central
[58] Ahmed T, Vial MR, Ost D, Stewart J, Hasan MA, Grosu HB. Non-small cell lung cancer transdifferentiation into small cell lung cancer: a case series. Lung Cancer. 2018;122:220–3.10.1016/j.lungcan.2018.06.024Search in Google Scholar PubMed
[59] Lee K, Kim Y, Jung HA, Lee SH, Ahn JS, Ahn MJ, et al. Repeat biopsy procedures and T790M rates after afatinib, gefitinib, or erlotinib therapy in patients with lung cancer. Lung Cancer. 2019;130:87–92.10.1016/j.lungcan.2019.01.012Search in Google Scholar PubMed
[60] Mehlman C, Cadranel J, Rousseau-Bussac G, Lacave R, Pujals A, Girard N, et al. Resistance mechanisms to osimertinib in EGFR-mutated advanced non-small-cell lung cancer: a multicentric retrospective French study. Lung Cancer. 2019;137:149–56.10.1016/j.lungcan.2019.09.019Search in Google Scholar PubMed
© 2021 Xing Chai et al., published by De Gruyter
This work is licensed under the Creative Commons Attribution 4.0 International License.
Articles in the same Issue
- Research Articles
- Identification of ZG16B as a prognostic biomarker in breast cancer
- Behçet’s disease with latent Mycobacterium tuberculosis infection
- Erratum
- Erratum to “Suffering from Cerebral Small Vessel Disease with and without Metabolic Syndrome”
- Research Articles
- GPR37 promotes the malignancy of lung adenocarcinoma via TGF-β/Smad pathway
- Expression and role of ABIN1 in sepsis: In vitro and in vivo studies
- Additional baricitinib loading dose improves clinical outcome in COVID-19
- The co-treatment of rosuvastatin with dapagliflozin synergistically inhibited apoptosis via activating the PI3K/AKt/mTOR signaling pathway in myocardial ischemia/reperfusion injury rats
- SLC12A8 plays a key role in bladder cancer progression and EMT
- LncRNA ATXN8OS enhances tamoxifen resistance in breast cancer
- Case Report
- Serratia marcescens as a cause of unfavorable outcome in the twin pregnancy
- Spleno-adrenal fusion mimicking an adrenal metastasis of a renal cell carcinoma: A case report and embryological background
- Research Articles
- TRIM25 contributes to the malignancy of acute myeloid leukemia and is negatively regulated by microRNA-137
- CircRNA circ_0004370 promotes cell proliferation, migration, and invasion and inhibits cell apoptosis of esophageal cancer via miR-1301-3p/COL1A1 axis
- LncRNA XIST regulates atherosclerosis progression in ox-LDL-induced HUVECs
- Potential role of IFN-γ and IL-5 in sepsis prediction of preterm neonates
- Rapid Communication
- COVID-19 vaccine: Call for employees in international transportation industries and international travelers as the first priority in global distribution
- Case Report
- Rare squamous cell carcinoma of the kidney with concurrent xanthogranulomatous pyelonephritis: A case report and review of the literature
- An infertile female delivered a baby after removal of primary renal carcinoid tumor
- Research Articles
- Hypertension, BMI, and cardiovascular and cerebrovascular diseases
- Case Report
- Coexistence of bilateral macular edema and pale optic disc in the patient with Cohen syndrome
- Research Articles
- Correlation between kinematic sagittal parameters of the cervical lordosis or head posture and disc degeneration in patients with posterior neck pain
- Review Articles
- Hepatoid adenocarcinoma of the lung: An analysis of the Surveillance, Epidemiology, and End Results (SEER) database
- Research Articles
- Thermography in the diagnosis of carpal tunnel syndrome
- Pemetrexed-based first-line chemotherapy had particularly prominent objective response rate for advanced NSCLC: A network meta-analysis
- Comparison of single and double autologous stem cell transplantation in multiple myeloma patients
- The influence of smoking in minimally invasive spinal fusion surgery
- Impact of body mass index on left atrial dimension in HOCM patients
- Expression and clinical significance of CMTM1 in hepatocellular carcinoma
- miR-142-5p promotes cervical cancer progression by targeting LMX1A through Wnt/β-catenin pathway
- Comparison of multiple flatfoot indicators in 5–8-year-old children
- Early MRI imaging and follow-up study in cerebral amyloid angiopathy
- Intestinal fatty acid-binding protein as a biomarker for the diagnosis of strangulated intestinal obstruction: A meta-analysis
- miR-128-3p inhibits apoptosis and inflammation in LPS-induced sepsis by targeting TGFBR2
- Dynamic perfusion CT – A promising tool to diagnose pancreatic ductal adenocarcinoma
- Biomechanical evaluation of self-cinching stitch techniques in rotator cuff repair: The single-loop and double-loop knot stitches
- Review Articles
- The ambiguous role of mannose-binding lectin (MBL) in human immunity
- Case Report
- Membranous nephropathy with pulmonary cryptococcosis with improved 1-year follow-up results: A case report
- Fertility problems in males carrying an inversion of chromosome 10
- Acute myeloid leukemia with leukemic pleural effusion and high levels of pleural adenosine deaminase: A case report and review of literature
- Metastatic renal Ewing’s sarcoma in adult woman: Case report and review of the literature
- Burkitt-like lymphoma with 11q aberration in a patient with AIDS and a patient without AIDS: Two cases reports and literature review
- Skull hemophilia pseudotumor: A case report
- Judicious use of low-dosage corticosteroids for non-severe COVID-19: A case report
- Adult-onset citrullinaemia type II with liver cirrhosis: A rare cause of hyperammonaemia
- Clinicopathologic features of Good’s syndrome: Two cases and literature review
- Fatal immune-related hepatitis with intrahepatic cholestasis and pneumonia associated with camrelizumab: A case report and literature review
- Research Articles
- Effects of hydroxyethyl starch and gelatin on the risk of acute kidney injury following orthotopic liver transplantation: A multicenter retrospective comparative clinical study
- Significance of nucleic acid positive anal swab in COVID-19 patients
- circAPLP2 promotes colorectal cancer progression by upregulating HELLS by targeting miR-335-5p
- Ratios between circulating myeloid cells and lymphocytes are associated with mortality in severe COVID-19 patients
- Risk factors of left atrial appendage thrombus in patients with non-valvular atrial fibrillation
- Clinical features of hypertensive patients with COVID-19 compared with a normotensive group: Single-center experience in China
- Surgical myocardial revascularization outcomes in Kawasaki disease: systematic review and meta-analysis
- Decreased chromobox homologue 7 expression is associated with epithelial–mesenchymal transition and poor prognosis in cervical cancer
- FGF16 regulated by miR-520b enhances the cell proliferation of lung cancer
- Platelet-rich fibrin: Basics of biological actions and protocol modifications
- Accurate diagnosis of prostate cancer using logistic regression
- miR-377 inhibition enhances the survival of trophoblast cells via upregulation of FNDC5 in gestational diabetes mellitus
- Prognostic significance of TRIM28 expression in patients with breast carcinoma
- Integrative bioinformatics analysis of KPNA2 in six major human cancers
- Exosomal-mediated transfer of OIP5-AS1 enhanced cell chemoresistance to trastuzumab in breast cancer via up-regulating HMGB3 by sponging miR-381-3p
- A four-lncRNA signature for predicting prognosis of recurrence patients with gastric cancer
- Knockdown of circ_0003204 alleviates oxidative low-density lipoprotein-induced human umbilical vein endothelial cells injury: Circulating RNAs could explain atherosclerosis disease progression
- Propofol postpones colorectal cancer development through circ_0026344/miR-645/Akt/mTOR signal pathway
- Knockdown of lncRNA TapSAKI alleviates LPS-induced injury in HK-2 cells through the miR-205/IRF3 pathway
- COVID-19 severity in relation to sociodemographics and vitamin D use
- Clinical analysis of 11 cases of nocardiosis
- Cis-regulatory elements in conserved non-coding sequences of nuclear receptor genes indicate for crosstalk between endocrine systems
- Four long noncoding RNAs act as biomarkers in lung adenocarcinoma
- Real-world evidence of cytomegalovirus reactivation in non-Hodgkin lymphomas treated with bendamustine-containing regimens
- Relation between IL-8 level and obstructive sleep apnea syndrome
- circAGFG1 sponges miR-28-5p to promote non-small-cell lung cancer progression through modulating HIF-1α level
- Nomogram prediction model for renal anaemia in IgA nephropathy patients
- Effect of antibiotic use on the efficacy of nivolumab in the treatment of advanced/metastatic non-small cell lung cancer: A meta-analysis
- NDRG2 inhibition facilitates angiogenesis of hepatocellular carcinoma
- A nomogram for predicting metabolic steatohepatitis: The combination of NAMPT, RALGDS, GADD45B, FOSL2, RTP3, and RASD1
- Clinical and prognostic features of MMP-2 and VEGF in AEG patients
- The value of miR-510 in the prognosis and development of colon cancer
- Functional implications of PABPC1 in the development of ovarian cancer
- Prognostic value of preoperative inflammation-based predictors in patients with bladder carcinoma after radical cystectomy
- Sublingual immunotherapy increases Treg/Th17 ratio in allergic rhinitis
- Prediction of improvement after anterior cruciate ligament reconstruction
- Effluent Osteopontin levels reflect the peritoneal solute transport rate
- circ_0038467 promotes PM2.5-induced bronchial epithelial cell dysfunction
- Significance of miR-141 and miR-340 in cervical squamous cell carcinoma
- Association between hair cortisol concentration and metabolic syndrome
- Microvessel density as a prognostic indicator of prostate cancer: A systematic review and meta-analysis
- Characteristics of BCR–ABL gene variants in patients of chronic myeloid leukemia
- Knee alterations in rheumatoid arthritis: Comparison of US and MRI
- Long non-coding RNA TUG1 aggravates cerebral ischemia and reperfusion injury by sponging miR-493-3p/miR-410-3p
- lncRNA MALAT1 regulated ATAD2 to facilitate retinoblastoma progression via miR-655-3p
- Development and validation of a nomogram for predicting severity in patients with hemorrhagic fever with renal syndrome: A retrospective study
- Analysis of COVID-19 outbreak origin in China in 2019 using differentiation method for unusual epidemiological events
- Laparoscopic versus open major liver resection for hepatocellular carcinoma: A case-matched analysis of short- and long-term outcomes
- Travelers’ vaccines and their adverse events in Nara, Japan
- Association between Tfh and PGA in children with Henoch–Schönlein purpura
- Can exchange transfusion be replaced by double-LED phototherapy?
- circ_0005962 functions as an oncogene to aggravate NSCLC progression
- Circular RNA VANGL1 knockdown suppressed viability, promoted apoptosis, and increased doxorubicin sensitivity through targeting miR-145-5p to regulate SOX4 in bladder cancer cells
- Serum intact fibroblast growth factor 23 in healthy paediatric population
- Algorithm of rational approach to reconstruction in Fournier’s disease
- A meta-analysis of exosome in the treatment of spinal cord injury
- Src-1 and SP2 promote the proliferation and epithelial–mesenchymal transition of nasopharyngeal carcinoma
- Dexmedetomidine may decrease the bupivacaine toxicity to heart
- Hypoxia stimulates the migration and invasion of osteosarcoma via up-regulating the NUSAP1 expression
- Long noncoding RNA XIST knockdown relieves the injury of microglia cells after spinal cord injury by sponging miR-219-5p
- External fixation via the anterior inferior iliac spine for proximal femoral fractures in young patients
- miR-128-3p reduced acute lung injury induced by sepsis via targeting PEL12
- HAGLR promotes neuron differentiation through the miR-130a-3p-MeCP2 axis
- Phosphoglycerate mutase 2 is elevated in serum of patients with heart failure and correlates with the disease severity and patient’s prognosis
- Cell population data in identifying active tuberculosis and community-acquired pneumonia
- Prognostic value of microRNA-4521 in non-small cell lung cancer and its regulatory effect on tumor progression
- Mean platelet volume and red blood cell distribution width is associated with prognosis in premature neonates with sepsis
- 3D-printed porous scaffold promotes osteogenic differentiation of hADMSCs
- Association of gene polymorphisms with women urinary incontinence
- Influence of COVID-19 pandemic on stress levels of urologic patients
- miR-496 inhibits proliferation via LYN and AKT pathway in gastric cancer
- miR-519d downregulates LEP expression to inhibit preeclampsia development
- Comparison of single- and triple-port VATS for lung cancer: A meta-analysis
- Fluorescent light energy modulates healing in skin grafted mouse model
- Silencing CDK6-AS1 inhibits LPS-induced inflammatory damage in HK-2 cells
- Predictive effect of DCE-MRI and DWI in brain metastases from NSCLC
- Severe postoperative hyperbilirubinemia in congenital heart disease
- Baicalin improves podocyte injury in rats with diabetic nephropathy by inhibiting PI3K/Akt/mTOR signaling pathway
- Clinical factors predicting ureteral stent failure in patients with external ureteral compression
- Novel H2S donor proglumide-ADT-OH protects HUVECs from ox-LDL-induced injury through NF-κB and JAK/SATA pathway
- Triple-Endobutton and clavicular hook: A propensity score matching analysis
- Long noncoding RNA MIAT inhibits the progression of diabetic nephropathy and the activation of NF-κB pathway in high glucose-treated renal tubular epithelial cells by the miR-182-5p/GPRC5A axis
- Serum exosomal miR-122-5p, GAS, and PGR in the non-invasive diagnosis of CAG
- miR-513b-5p inhibits the proliferation and promotes apoptosis of retinoblastoma cells by targeting TRIB1
- Fer exacerbates renal fibrosis and can be targeted by miR-29c-3p
- The diagnostic and prognostic value of miR-92a in gastric cancer: A systematic review and meta-analysis
- Prognostic value of α2δ1 in hypopharyngeal carcinoma: A retrospective study
- No significant benefit of moderate-dose vitamin C on severe COVID-19 cases
- circ_0000467 promotes the proliferation, metastasis, and angiogenesis in colorectal cancer cells through regulating KLF12 expression by sponging miR-4766-5p
- Downregulation of RAB7 and Caveolin-1 increases MMP-2 activity in renal tubular epithelial cells under hypoxic conditions
- Educational program for orthopedic surgeons’ influences for osteoporosis
- Expression and function analysis of CRABP2 and FABP5, and their ratio in esophageal squamous cell carcinoma
- GJA1 promotes hepatocellular carcinoma progression by mediating TGF-β-induced activation and the epithelial–mesenchymal transition of hepatic stellate cells
- lncRNA-ZFAS1 promotes the progression of endometrial carcinoma by targeting miR-34b to regulate VEGFA expression
- Anticoagulation is the answer in treating noncritical COVID-19 patients
- Effect of late-onset hemorrhagic cystitis on PFS after haplo-PBSCT
- Comparison of Dako HercepTest and Ventana PATHWAY anti-HER2 (4B5) tests and their correlation with silver in situ hybridization in lung adenocarcinoma
- VSTM1 regulates monocyte/macrophage function via the NF-κB signaling pathway
- Comparison of vaginal birth outcomes in midwifery-led versus physician-led setting: A propensity score-matched analysis
- Treatment of osteoporosis with teriparatide: The Slovenian experience
- New targets of morphine postconditioning protection of the myocardium in ischemia/reperfusion injury: Involvement of HSP90/Akt and C5a/NF-κB
- Superenhancer–transcription factor regulatory network in malignant tumors
- β-Cell function is associated with osteosarcopenia in middle-aged and older nonobese patients with type 2 diabetes: A cross-sectional study
- Clinical features of atypical tuberculosis mimicking bacterial pneumonia
- Proteoglycan-depleted regions of annular injury promote nerve ingrowth in a rabbit disc degeneration model
- Effect of electromagnetic field on abortion: A systematic review and meta-analysis
- miR-150-5p affects AS plaque with ASMC proliferation and migration by STAT1
- MALAT1 promotes malignant pleural mesothelioma by sponging miR-141-3p
- Effects of remifentanil and propofol on distant organ lung injury in an ischemia–reperfusion model
- miR-654-5p promotes gastric cancer progression via the GPRIN1/NF-κB pathway
- Identification of LIG1 and LIG3 as prognostic biomarkers in breast cancer
- MitoQ inhibits hepatic stellate cell activation and liver fibrosis by enhancing PINK1/parkin-mediated mitophagy
- Dissecting role of founder mutation p.V727M in GNE in Indian HIBM cohort
- circATP2A2 promotes osteosarcoma progression by upregulating MYH9
- Prognostic role of oxytocin receptor in colon adenocarcinoma
- Review Articles
- The function of non-coding RNAs in idiopathic pulmonary fibrosis
- Efficacy and safety of therapeutic plasma exchange in stiff person syndrome
- Role of cesarean section in the development of neonatal gut microbiota: A systematic review
- Small cell lung cancer transformation during antitumor therapies: A systematic review
- Research progress of gut microbiota and frailty syndrome
- Recommendations for outpatient activity in COVID-19 pandemic
- Rapid Communication
- Disparity in clinical characteristics between 2019 novel coronavirus pneumonia and leptospirosis
- Use of microspheres in embolization for unruptured renal angiomyolipomas
- COVID-19 cases with delayed absorption of lung lesion
- A triple combination of treatments on moderate COVID-19
- Social networks and eating disorders during the Covid-19 pandemic
- Letter
- COVID-19, WHO guidelines, pedagogy, and respite
- Inflammatory factors in alveolar lavage fluid from severe COVID-19 pneumonia: PCT and IL-6 in epithelial lining fluid
- COVID-19: Lessons from Norway tragedy must be considered in vaccine rollout planning in least developed/developing countries
- What is the role of plasma cell in the lamina propria of terminal ileum in Good’s syndrome patient?
- Case Report
- Rivaroxaban triggered multifocal intratumoral hemorrhage of the cabozantinib-treated diffuse brain metastases: A case report and review of literature
- CTU findings of duplex kidney in kidney: A rare duplicated renal malformation
- Synchronous primary malignancy of colon cancer and mantle cell lymphoma: A case report
- Sonazoid-enhanced ultrasonography and pathologic characters of CD68 positive cell in primary hepatic perivascular epithelioid cell tumors: A case report and literature review
- Persistent SARS-CoV-2-positive over 4 months in a COVID-19 patient with CHB
- Pulmonary parenchymal involvement caused by Tropheryma whipplei
- Mediastinal mixed germ cell tumor: A case report and literature review
- Ovarian female adnexal tumor of probable Wolffian origin – Case report
- Rare paratesticular aggressive angiomyxoma mimicking an epididymal tumor in an 82-year-old man: Case report
- Perimenopausal giant hydatidiform mole complicated with preeclampsia and hyperthyroidism: A case report and literature review
- Primary orbital ganglioneuroblastoma: A case report
- Primary aortic intimal sarcoma masquerading as intramural hematoma
- Sustained false-positive results for hepatitis A virus immunoglobulin M: A case report and literature review
- Peritoneal loose body presenting as a hepatic mass: A case report and review of the literature
- Chondroblastoma of mandibular condyle: Case report and literature review
- Trauma-induced complete pacemaker lead fracture 8 months prior to hospitalization: A case report
- Primary intradural extramedullary extraosseous Ewing’s sarcoma/peripheral primitive neuroectodermal tumor (PIEES/PNET) of the thoracolumbar spine: A case report and literature review
- Computer-assisted preoperative planning of reduction of and osteosynthesis of scapular fracture: A case report
- High quality of 58-month life in lung cancer patient with brain metastases sequentially treated with gefitinib and osimertinib
- Rapid response of locally advanced oral squamous cell carcinoma to apatinib: A case report
- Retrieval of intrarenal coiled and ruptured guidewire by retrograde intrarenal surgery: A case report and literature review
- Usage of intermingled skin allografts and autografts in a senior patient with major burn injury
- Retraction
- Retraction on “Dihydromyricetin attenuates inflammation through TLR4/NF-kappa B pathway”
- Special Issue Computational Intelligence Methodologies Meets Recurrent Cancers - Part I
- An artificial immune system with bootstrap sampling for the diagnosis of recurrent endometrial cancers
- Breast cancer recurrence prediction with ensemble methods and cost-sensitive learning
Articles in the same Issue
- Research Articles
- Identification of ZG16B as a prognostic biomarker in breast cancer
- Behçet’s disease with latent Mycobacterium tuberculosis infection
- Erratum
- Erratum to “Suffering from Cerebral Small Vessel Disease with and without Metabolic Syndrome”
- Research Articles
- GPR37 promotes the malignancy of lung adenocarcinoma via TGF-β/Smad pathway
- Expression and role of ABIN1 in sepsis: In vitro and in vivo studies
- Additional baricitinib loading dose improves clinical outcome in COVID-19
- The co-treatment of rosuvastatin with dapagliflozin synergistically inhibited apoptosis via activating the PI3K/AKt/mTOR signaling pathway in myocardial ischemia/reperfusion injury rats
- SLC12A8 plays a key role in bladder cancer progression and EMT
- LncRNA ATXN8OS enhances tamoxifen resistance in breast cancer
- Case Report
- Serratia marcescens as a cause of unfavorable outcome in the twin pregnancy
- Spleno-adrenal fusion mimicking an adrenal metastasis of a renal cell carcinoma: A case report and embryological background
- Research Articles
- TRIM25 contributes to the malignancy of acute myeloid leukemia and is negatively regulated by microRNA-137
- CircRNA circ_0004370 promotes cell proliferation, migration, and invasion and inhibits cell apoptosis of esophageal cancer via miR-1301-3p/COL1A1 axis
- LncRNA XIST regulates atherosclerosis progression in ox-LDL-induced HUVECs
- Potential role of IFN-γ and IL-5 in sepsis prediction of preterm neonates
- Rapid Communication
- COVID-19 vaccine: Call for employees in international transportation industries and international travelers as the first priority in global distribution
- Case Report
- Rare squamous cell carcinoma of the kidney with concurrent xanthogranulomatous pyelonephritis: A case report and review of the literature
- An infertile female delivered a baby after removal of primary renal carcinoid tumor
- Research Articles
- Hypertension, BMI, and cardiovascular and cerebrovascular diseases
- Case Report
- Coexistence of bilateral macular edema and pale optic disc in the patient with Cohen syndrome
- Research Articles
- Correlation between kinematic sagittal parameters of the cervical lordosis or head posture and disc degeneration in patients with posterior neck pain
- Review Articles
- Hepatoid adenocarcinoma of the lung: An analysis of the Surveillance, Epidemiology, and End Results (SEER) database
- Research Articles
- Thermography in the diagnosis of carpal tunnel syndrome
- Pemetrexed-based first-line chemotherapy had particularly prominent objective response rate for advanced NSCLC: A network meta-analysis
- Comparison of single and double autologous stem cell transplantation in multiple myeloma patients
- The influence of smoking in minimally invasive spinal fusion surgery
- Impact of body mass index on left atrial dimension in HOCM patients
- Expression and clinical significance of CMTM1 in hepatocellular carcinoma
- miR-142-5p promotes cervical cancer progression by targeting LMX1A through Wnt/β-catenin pathway
- Comparison of multiple flatfoot indicators in 5–8-year-old children
- Early MRI imaging and follow-up study in cerebral amyloid angiopathy
- Intestinal fatty acid-binding protein as a biomarker for the diagnosis of strangulated intestinal obstruction: A meta-analysis
- miR-128-3p inhibits apoptosis and inflammation in LPS-induced sepsis by targeting TGFBR2
- Dynamic perfusion CT – A promising tool to diagnose pancreatic ductal adenocarcinoma
- Biomechanical evaluation of self-cinching stitch techniques in rotator cuff repair: The single-loop and double-loop knot stitches
- Review Articles
- The ambiguous role of mannose-binding lectin (MBL) in human immunity
- Case Report
- Membranous nephropathy with pulmonary cryptococcosis with improved 1-year follow-up results: A case report
- Fertility problems in males carrying an inversion of chromosome 10
- Acute myeloid leukemia with leukemic pleural effusion and high levels of pleural adenosine deaminase: A case report and review of literature
- Metastatic renal Ewing’s sarcoma in adult woman: Case report and review of the literature
- Burkitt-like lymphoma with 11q aberration in a patient with AIDS and a patient without AIDS: Two cases reports and literature review
- Skull hemophilia pseudotumor: A case report
- Judicious use of low-dosage corticosteroids for non-severe COVID-19: A case report
- Adult-onset citrullinaemia type II with liver cirrhosis: A rare cause of hyperammonaemia
- Clinicopathologic features of Good’s syndrome: Two cases and literature review
- Fatal immune-related hepatitis with intrahepatic cholestasis and pneumonia associated with camrelizumab: A case report and literature review
- Research Articles
- Effects of hydroxyethyl starch and gelatin on the risk of acute kidney injury following orthotopic liver transplantation: A multicenter retrospective comparative clinical study
- Significance of nucleic acid positive anal swab in COVID-19 patients
- circAPLP2 promotes colorectal cancer progression by upregulating HELLS by targeting miR-335-5p
- Ratios between circulating myeloid cells and lymphocytes are associated with mortality in severe COVID-19 patients
- Risk factors of left atrial appendage thrombus in patients with non-valvular atrial fibrillation
- Clinical features of hypertensive patients with COVID-19 compared with a normotensive group: Single-center experience in China
- Surgical myocardial revascularization outcomes in Kawasaki disease: systematic review and meta-analysis
- Decreased chromobox homologue 7 expression is associated with epithelial–mesenchymal transition and poor prognosis in cervical cancer
- FGF16 regulated by miR-520b enhances the cell proliferation of lung cancer
- Platelet-rich fibrin: Basics of biological actions and protocol modifications
- Accurate diagnosis of prostate cancer using logistic regression
- miR-377 inhibition enhances the survival of trophoblast cells via upregulation of FNDC5 in gestational diabetes mellitus
- Prognostic significance of TRIM28 expression in patients with breast carcinoma
- Integrative bioinformatics analysis of KPNA2 in six major human cancers
- Exosomal-mediated transfer of OIP5-AS1 enhanced cell chemoresistance to trastuzumab in breast cancer via up-regulating HMGB3 by sponging miR-381-3p
- A four-lncRNA signature for predicting prognosis of recurrence patients with gastric cancer
- Knockdown of circ_0003204 alleviates oxidative low-density lipoprotein-induced human umbilical vein endothelial cells injury: Circulating RNAs could explain atherosclerosis disease progression
- Propofol postpones colorectal cancer development through circ_0026344/miR-645/Akt/mTOR signal pathway
- Knockdown of lncRNA TapSAKI alleviates LPS-induced injury in HK-2 cells through the miR-205/IRF3 pathway
- COVID-19 severity in relation to sociodemographics and vitamin D use
- Clinical analysis of 11 cases of nocardiosis
- Cis-regulatory elements in conserved non-coding sequences of nuclear receptor genes indicate for crosstalk between endocrine systems
- Four long noncoding RNAs act as biomarkers in lung adenocarcinoma
- Real-world evidence of cytomegalovirus reactivation in non-Hodgkin lymphomas treated with bendamustine-containing regimens
- Relation between IL-8 level and obstructive sleep apnea syndrome
- circAGFG1 sponges miR-28-5p to promote non-small-cell lung cancer progression through modulating HIF-1α level
- Nomogram prediction model for renal anaemia in IgA nephropathy patients
- Effect of antibiotic use on the efficacy of nivolumab in the treatment of advanced/metastatic non-small cell lung cancer: A meta-analysis
- NDRG2 inhibition facilitates angiogenesis of hepatocellular carcinoma
- A nomogram for predicting metabolic steatohepatitis: The combination of NAMPT, RALGDS, GADD45B, FOSL2, RTP3, and RASD1
- Clinical and prognostic features of MMP-2 and VEGF in AEG patients
- The value of miR-510 in the prognosis and development of colon cancer
- Functional implications of PABPC1 in the development of ovarian cancer
- Prognostic value of preoperative inflammation-based predictors in patients with bladder carcinoma after radical cystectomy
- Sublingual immunotherapy increases Treg/Th17 ratio in allergic rhinitis
- Prediction of improvement after anterior cruciate ligament reconstruction
- Effluent Osteopontin levels reflect the peritoneal solute transport rate
- circ_0038467 promotes PM2.5-induced bronchial epithelial cell dysfunction
- Significance of miR-141 and miR-340 in cervical squamous cell carcinoma
- Association between hair cortisol concentration and metabolic syndrome
- Microvessel density as a prognostic indicator of prostate cancer: A systematic review and meta-analysis
- Characteristics of BCR–ABL gene variants in patients of chronic myeloid leukemia
- Knee alterations in rheumatoid arthritis: Comparison of US and MRI
- Long non-coding RNA TUG1 aggravates cerebral ischemia and reperfusion injury by sponging miR-493-3p/miR-410-3p
- lncRNA MALAT1 regulated ATAD2 to facilitate retinoblastoma progression via miR-655-3p
- Development and validation of a nomogram for predicting severity in patients with hemorrhagic fever with renal syndrome: A retrospective study
- Analysis of COVID-19 outbreak origin in China in 2019 using differentiation method for unusual epidemiological events
- Laparoscopic versus open major liver resection for hepatocellular carcinoma: A case-matched analysis of short- and long-term outcomes
- Travelers’ vaccines and their adverse events in Nara, Japan
- Association between Tfh and PGA in children with Henoch–Schönlein purpura
- Can exchange transfusion be replaced by double-LED phototherapy?
- circ_0005962 functions as an oncogene to aggravate NSCLC progression
- Circular RNA VANGL1 knockdown suppressed viability, promoted apoptosis, and increased doxorubicin sensitivity through targeting miR-145-5p to regulate SOX4 in bladder cancer cells
- Serum intact fibroblast growth factor 23 in healthy paediatric population
- Algorithm of rational approach to reconstruction in Fournier’s disease
- A meta-analysis of exosome in the treatment of spinal cord injury
- Src-1 and SP2 promote the proliferation and epithelial–mesenchymal transition of nasopharyngeal carcinoma
- Dexmedetomidine may decrease the bupivacaine toxicity to heart
- Hypoxia stimulates the migration and invasion of osteosarcoma via up-regulating the NUSAP1 expression
- Long noncoding RNA XIST knockdown relieves the injury of microglia cells after spinal cord injury by sponging miR-219-5p
- External fixation via the anterior inferior iliac spine for proximal femoral fractures in young patients
- miR-128-3p reduced acute lung injury induced by sepsis via targeting PEL12
- HAGLR promotes neuron differentiation through the miR-130a-3p-MeCP2 axis
- Phosphoglycerate mutase 2 is elevated in serum of patients with heart failure and correlates with the disease severity and patient’s prognosis
- Cell population data in identifying active tuberculosis and community-acquired pneumonia
- Prognostic value of microRNA-4521 in non-small cell lung cancer and its regulatory effect on tumor progression
- Mean platelet volume and red blood cell distribution width is associated with prognosis in premature neonates with sepsis
- 3D-printed porous scaffold promotes osteogenic differentiation of hADMSCs
- Association of gene polymorphisms with women urinary incontinence
- Influence of COVID-19 pandemic on stress levels of urologic patients
- miR-496 inhibits proliferation via LYN and AKT pathway in gastric cancer
- miR-519d downregulates LEP expression to inhibit preeclampsia development
- Comparison of single- and triple-port VATS for lung cancer: A meta-analysis
- Fluorescent light energy modulates healing in skin grafted mouse model
- Silencing CDK6-AS1 inhibits LPS-induced inflammatory damage in HK-2 cells
- Predictive effect of DCE-MRI and DWI in brain metastases from NSCLC
- Severe postoperative hyperbilirubinemia in congenital heart disease
- Baicalin improves podocyte injury in rats with diabetic nephropathy by inhibiting PI3K/Akt/mTOR signaling pathway
- Clinical factors predicting ureteral stent failure in patients with external ureteral compression
- Novel H2S donor proglumide-ADT-OH protects HUVECs from ox-LDL-induced injury through NF-κB and JAK/SATA pathway
- Triple-Endobutton and clavicular hook: A propensity score matching analysis
- Long noncoding RNA MIAT inhibits the progression of diabetic nephropathy and the activation of NF-κB pathway in high glucose-treated renal tubular epithelial cells by the miR-182-5p/GPRC5A axis
- Serum exosomal miR-122-5p, GAS, and PGR in the non-invasive diagnosis of CAG
- miR-513b-5p inhibits the proliferation and promotes apoptosis of retinoblastoma cells by targeting TRIB1
- Fer exacerbates renal fibrosis and can be targeted by miR-29c-3p
- The diagnostic and prognostic value of miR-92a in gastric cancer: A systematic review and meta-analysis
- Prognostic value of α2δ1 in hypopharyngeal carcinoma: A retrospective study
- No significant benefit of moderate-dose vitamin C on severe COVID-19 cases
- circ_0000467 promotes the proliferation, metastasis, and angiogenesis in colorectal cancer cells through regulating KLF12 expression by sponging miR-4766-5p
- Downregulation of RAB7 and Caveolin-1 increases MMP-2 activity in renal tubular epithelial cells under hypoxic conditions
- Educational program for orthopedic surgeons’ influences for osteoporosis
- Expression and function analysis of CRABP2 and FABP5, and their ratio in esophageal squamous cell carcinoma
- GJA1 promotes hepatocellular carcinoma progression by mediating TGF-β-induced activation and the epithelial–mesenchymal transition of hepatic stellate cells
- lncRNA-ZFAS1 promotes the progression of endometrial carcinoma by targeting miR-34b to regulate VEGFA expression
- Anticoagulation is the answer in treating noncritical COVID-19 patients
- Effect of late-onset hemorrhagic cystitis on PFS after haplo-PBSCT
- Comparison of Dako HercepTest and Ventana PATHWAY anti-HER2 (4B5) tests and their correlation with silver in situ hybridization in lung adenocarcinoma
- VSTM1 regulates monocyte/macrophage function via the NF-κB signaling pathway
- Comparison of vaginal birth outcomes in midwifery-led versus physician-led setting: A propensity score-matched analysis
- Treatment of osteoporosis with teriparatide: The Slovenian experience
- New targets of morphine postconditioning protection of the myocardium in ischemia/reperfusion injury: Involvement of HSP90/Akt and C5a/NF-κB
- Superenhancer–transcription factor regulatory network in malignant tumors
- β-Cell function is associated with osteosarcopenia in middle-aged and older nonobese patients with type 2 diabetes: A cross-sectional study
- Clinical features of atypical tuberculosis mimicking bacterial pneumonia
- Proteoglycan-depleted regions of annular injury promote nerve ingrowth in a rabbit disc degeneration model
- Effect of electromagnetic field on abortion: A systematic review and meta-analysis
- miR-150-5p affects AS plaque with ASMC proliferation and migration by STAT1
- MALAT1 promotes malignant pleural mesothelioma by sponging miR-141-3p
- Effects of remifentanil and propofol on distant organ lung injury in an ischemia–reperfusion model
- miR-654-5p promotes gastric cancer progression via the GPRIN1/NF-κB pathway
- Identification of LIG1 and LIG3 as prognostic biomarkers in breast cancer
- MitoQ inhibits hepatic stellate cell activation and liver fibrosis by enhancing PINK1/parkin-mediated mitophagy
- Dissecting role of founder mutation p.V727M in GNE in Indian HIBM cohort
- circATP2A2 promotes osteosarcoma progression by upregulating MYH9
- Prognostic role of oxytocin receptor in colon adenocarcinoma
- Review Articles
- The function of non-coding RNAs in idiopathic pulmonary fibrosis
- Efficacy and safety of therapeutic plasma exchange in stiff person syndrome
- Role of cesarean section in the development of neonatal gut microbiota: A systematic review
- Small cell lung cancer transformation during antitumor therapies: A systematic review
- Research progress of gut microbiota and frailty syndrome
- Recommendations for outpatient activity in COVID-19 pandemic
- Rapid Communication
- Disparity in clinical characteristics between 2019 novel coronavirus pneumonia and leptospirosis
- Use of microspheres in embolization for unruptured renal angiomyolipomas
- COVID-19 cases with delayed absorption of lung lesion
- A triple combination of treatments on moderate COVID-19
- Social networks and eating disorders during the Covid-19 pandemic
- Letter
- COVID-19, WHO guidelines, pedagogy, and respite
- Inflammatory factors in alveolar lavage fluid from severe COVID-19 pneumonia: PCT and IL-6 in epithelial lining fluid
- COVID-19: Lessons from Norway tragedy must be considered in vaccine rollout planning in least developed/developing countries
- What is the role of plasma cell in the lamina propria of terminal ileum in Good’s syndrome patient?
- Case Report
- Rivaroxaban triggered multifocal intratumoral hemorrhage of the cabozantinib-treated diffuse brain metastases: A case report and review of literature
- CTU findings of duplex kidney in kidney: A rare duplicated renal malformation
- Synchronous primary malignancy of colon cancer and mantle cell lymphoma: A case report
- Sonazoid-enhanced ultrasonography and pathologic characters of CD68 positive cell in primary hepatic perivascular epithelioid cell tumors: A case report and literature review
- Persistent SARS-CoV-2-positive over 4 months in a COVID-19 patient with CHB
- Pulmonary parenchymal involvement caused by Tropheryma whipplei
- Mediastinal mixed germ cell tumor: A case report and literature review
- Ovarian female adnexal tumor of probable Wolffian origin – Case report
- Rare paratesticular aggressive angiomyxoma mimicking an epididymal tumor in an 82-year-old man: Case report
- Perimenopausal giant hydatidiform mole complicated with preeclampsia and hyperthyroidism: A case report and literature review
- Primary orbital ganglioneuroblastoma: A case report
- Primary aortic intimal sarcoma masquerading as intramural hematoma
- Sustained false-positive results for hepatitis A virus immunoglobulin M: A case report and literature review
- Peritoneal loose body presenting as a hepatic mass: A case report and review of the literature
- Chondroblastoma of mandibular condyle: Case report and literature review
- Trauma-induced complete pacemaker lead fracture 8 months prior to hospitalization: A case report
- Primary intradural extramedullary extraosseous Ewing’s sarcoma/peripheral primitive neuroectodermal tumor (PIEES/PNET) of the thoracolumbar spine: A case report and literature review
- Computer-assisted preoperative planning of reduction of and osteosynthesis of scapular fracture: A case report
- High quality of 58-month life in lung cancer patient with brain metastases sequentially treated with gefitinib and osimertinib
- Rapid response of locally advanced oral squamous cell carcinoma to apatinib: A case report
- Retrieval of intrarenal coiled and ruptured guidewire by retrograde intrarenal surgery: A case report and literature review
- Usage of intermingled skin allografts and autografts in a senior patient with major burn injury
- Retraction
- Retraction on “Dihydromyricetin attenuates inflammation through TLR4/NF-kappa B pathway”
- Special Issue Computational Intelligence Methodologies Meets Recurrent Cancers - Part I
- An artificial immune system with bootstrap sampling for the diagnosis of recurrent endometrial cancers
- Breast cancer recurrence prediction with ensemble methods and cost-sensitive learning

