Evaluation of prognostic markers in patients infected with SARS-CoV-2
-
Dipendra Kumar Mandal
, Mandira Chhusyabaga
Abstract
Prognostic markers are the biomarkers used to measure the disease progression and patient outcome regardless of treatment in coronavirus disease 2019 (COVID-19). This study aimed to analyze laboratory parameters as prognostic markers for the early identification of disease severity. In this study, 165 patients attending Sukraraj Tropical and Infectious Disease Hospital with COVID-19 were enrolled and divided into severe and non-severe groups. The demographic data, underlying co-morbidities, and laboratory findings were analyzed and compared between severe and non-severe cases. The correlation between the disease criticality and laboratory parameters was analyzed. Cut-off values of parameters for severe patients were speculated through the receiver operating characteristics (ROC) curve, and regression analysis was performed to determine the risk factors. Patients with severe COVID-19 infection had significantly higher absolute neutrophil count, neutrophil–lymphocyte ratio (NLR), platelet–lymphocyte ratio (PLR), ferritin, positive carbohydrate reactive protein (CRP), glucose, urea, creatinine, and aspartate aminotransferase, while lower absolute lymphocyte count, absolute eosinophil count (AEC), and red blood cell count in comparison to non-severe infection. ROC analysis gave a cut-off value (sensitivity, specificity) of age, AEC, NLR, PLR, and ferritin as 47.5 years (70.2, 64.7%), 335 cells/mm3 (74, 67%) 3.3 (68.4, 63.7%), 129 (77.2, 51%), and 241 ng/mL (74.0%, 65.0%) respectively. Risk factor analysis showed higher age, low AEC, high ferritin, and positive CRP as independent risk factors associated with severe COVID-19 infection. Hematological and inflammatory markers, including novel NLR and PLR, should be assessed to aid clinicians in the early identification of severe cases, prioritization of cases, and effective management to decrease the mortality of COVID-19 patients.
1 Introduction
Coronaviruses are enveloped, positive sense, single-stranded RNA viruses with a comparatively larger genome (30 kb), which belong to the order Nidovirales family Coronaviridae and subfamily Coronavirinae [1]. In late 2019, the very first case of coronavirus disease 2019 (COVID-19) caused by Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) was reported from Wuhan, China, and due to its alarming level of transmission and severity to public health, World health organization declared a global pandemic on March 11, 2020 [2].
COVID-19 infection could start with flu-like symptoms; although it could be asymptomatic, about 15% of the patients are complicated with disease severity [3]. COVID-19 patients typically present with fever, myalgia, respiratory symptoms such as nonproductive cough and dyspnea, decreased lymphocyte counts, and radiographic evidence of bilateral interstitial pneumonia; clinical presentation ranges from mild to critical case, requiring intensive care unit (ICU) admission [4]. COVID-19-associated mortality varies broadly according to geographical areas, patient demographic characteristics, and other comorbidities [5,6,7,8,9].
The major finding of immunopathology in COVID-19 is the cytokine storm. The rapid replication of the virus in epithelial and endothelial cells results in the development of significant numbers of proinflammatory cytokines and chemokine that eventually leads to acute respiratory distress syndrome (ARDS) and multiple organ failure (MOF) [10]. Critical cases quickly progress to complications like ARDS, septic shock, metabolic acidosis, coagulopathy, and MOF [11,12].
Based on clinical symptoms and laboratory findings, the patient can be classified as a mild, moderate, severe, and critical case [13,14]. Among them, 81% account for mild/moderate cases, while 14 and 5% for severe and critical cases [15,16]. Almost 20% of hospitalized patients require an ICU admission, with a mortality rate (61.5%) [12,17].
Different hematological parameters (complete blood count, erythrocyte sedimentation rate, coagulation profile, D-dimer), biochemical parameters: liver function test (LFT), renal function test (RFT), electrolytes, cardiac enzymes, procalcitonin, lactate dehydrogenase, and inflammatory markers: carbohydrate reactive protein (CRP), ferritin as prognostic markers can be used to measure the disease progression to severity and patient outcome regardless of treatment [18].
Neutrophil-to-lymphocyte ratio (NLR) and platelet-to-lymphocyte ratio (PLR) are the established inflammatory markers and are readily calculated with hemograms, an inexpensive tool for the early stratification of risk groups and treatment. The diagnostic and prognostic value of NLR is established in cardiovascular disease (CVD), thyroiditis [19], functional bowel conditions [20], and COVID-19 infection [21]. PLR is another novel marker of inflammation, and elevated PLR has been reported in thyroid conditions [22], cancer [23], diabetes mellitus (DM) [24], and irritable bowel disease [20]. CRP is an inflammatory marker increased in inflammatory conditions such as thyroiditis [25], hepatitis C [26], and type 2 DM [27].
Thus, this study aims to identify the role of these biomarkers as a predictor of severity and clinical outcomes during disease, which could help in the early identification of the risk group patients and better patient management.
2 Methods
This laboratory-based cross-sectional study was conducted for the period of 3 months (November 2020 to January 2021) in Sukraraj Tropical and Infectious Disease Hospital (STIDH), Kathmandu, Nepal, in collaboration with Manmohan Memorial Institute of Health Sciences (MMIHS), Kathmandu, Nepal.
2.1 Inclusion and exclusion criteria
COVID-19-infected patients confirmed with positive reverse transcriptase polymerase chain reaction (RT-PCR) and presented with clinical symptoms were included in the study, while a repeated sample from the same patient and asymptomatic patients were excluded from the study.
All 165 patients who fulfilled with above-mentioned inclusion criteria were taken with informed & written consent and recorded with their demographic data, co-morbidities, and laboratory parameters using standard performance.
-
Informed consent: Informed consent has been obtained from all individuals included in this study.
-
Ethical approval: The research related to human use has been complied with all the relevant national regulations, and institutional policies and in accordance with the tenets of the Helsinki Declaration, and has been approved and has been approved by the Institution Review Committee of Manmohan Memorial Institute of Health Sciences (IRC MMIHS), Kathmandu, Nepal (letter of approval Ref No: MMIHS-IRC 484).
2.2 Experimental protocol
Venous blood samples were collected following standard operating procedures. In addition, whole blood was collected in K2 EDTA vacutainer (BD Vacutainer, USA), Gel and clot activator tube (Hebei Xinle Sci & Tech Co. Ltd, China), and Sodium citrate vacutainer (BD Vacutainer, USA), which was used for hematological parameters, and serum was separated for inflammatory markers and biochemical analysis.
Whole blood samples were analyzed for hematological parameters such as complete blood cell count (CBC) including hemoglobin (Hb), red blood cell count (RBC), hematocrit (Hct), white blood cell count (WBC), absolute neutrophil count (ANC), absolute lymphocyte count (ALC), absolute monocyte count (AMC), absolute eosinophil count (AEC), absolute basophil count (ABC), Platelets, mean cell volume (MCV), mean cell hemoglobin (MCH), mean cell hemoglobin concentration (MCHC) using a coulter counter (Sysmex XN-330, Asia Green, Singapore) in the Department of Hematology, STIDH. NLR and PLR were calculated manually using the data obtained from the coulter counter. In addition, ferritin was estimated quantitatively by nephelometer (mispa-i2, Kerala, India) as per the instructions provided by the reagent manufacturer (AGAPPE DIAGNOSTICS LTD, Kerala, India), and qualitative CRP was performed by following the manufacturer’s guideline (Omega diagnostics, UK).
Random blood sugar, LFT including alanine transferase (ALT), aspartate transferase (AST), alkaline phosphatase (ALP), total bilirubin, direct bilirubin, and RFT including urea, creatinine, sodium, and potassium were estimated. All the parameters were analyzed using a fully automated random access clinical chemistry analyzer XL-200 (ERBA, Mannheim, Germany) in the Department of Biochemistry, STIDH.
Diagnosis and clinical classification of COVID-19 according to the new coronavirus pneumonia diagnosis and treatment plan (trial version 7) developed by the National Health Commission of the People’s Republic of China are as follows: (1) mild, minor symptoms and imaging show no pneumonia; (2) moderate, with fever, respiratory tract symptoms and imaging show pneumonia; (3) severe, meet any of the following: (a) respiratory distress, respiratory rate ≥ 30 beats/min; (b) oxygen saturation ≤ 93%; (c) arterial blood oxygen partial pressure ≤ 300 mmHg, pulmonary imaging showed that the lesion progressed more than 50% within 24–48 h. (4) critical, one of the following conditions: (a) respiratory failure occurs and requires mechanical ventilation, (b) Shock occurs and (c) ICU admission is required for combined organ failure [28].
2.3 Statistical analysis
Data were collected in Microsoft Excel 2013 and analyzed using SPSS version 20.0 (IBM Corp., Armonk, NY, USA). The normal distribution was analyzed using the Shapiro-Wilk test. Independent sample t-test for normally distributed variable and expressed as mean ± SD, and Mann–Whitney U test for non-normally distributed variable expressed as median (Q 1–Q 3) were used to analyze the differences in laboratory parameters between severe and non-severe patients. Categorical variables were presented as numbers (percentage) and compared using the Chi-square test. Receiver-operating characteristics (ROC) curve analysis was used to determine the optimum cut-off points of the parameters. Similarly, a risk estimate was obtained for the severity of the disease. Univariate analysis was done to obtain the association of risk factors for disease severity. Further, the associated covariates were entered in stepwise multivariate risk analysis for adjusted odds ratio using a binary logistic regression model.
3 Results
A total of 165 COVID-19 patients were enrolled, among which 114 (31%) had a severe infection while 51 (69%) had a non-severe infection. Higher age was significantly associated with disease severity (p < 0.001). Male and female participants were 124 (75.2) and 41 (24.6%), respectively (Tables 1 and 2).
Characteristics of the patients with COVID-19
| Variable | Total | Non-severe | Severe | p-Value |
|---|---|---|---|---|
| N = 165 | N = 51 | N = 114 | ||
| n (%) | n (%) | n (%) | ||
| Age in years | ||||
| (Mean ± SD) | 53.5 ± 16.5 | 44.4 ± 14.3 | 57.5 ± 15.3 | <0.001 a |
| <30 | 15 (9.1) | 11 (21.6) | 4 (3.5) | |
| 30–49 | 54 (32.7) | 22 (43.1) | 32 (28) | |
| 50–69 | 64 (38.8) | 16 (31.4) | 48 (42.1) | |
| 70–89 | 31 (18.8) | 2 (15.7) | 29 (25.4) | |
| >89 | 1 (0.6) | 0 (0) | 1 (0.9) | |
| Gender | ||||
| Male | 124 (75.2) | 38(74.5) | 86 (75.4) | 0.898b |
| Female | 41 (24.6) | 13(25.5) | 28 (24.6) |
p < 0.05 was considered statistically significant.
a p-value calculated using an independent sample t test.
b p-value calculated using the chi-square test.
Hematological and inflammatory markers of a patient with COVID-19
| Disease severity | ||||
|---|---|---|---|---|
| Laboratory parameters | Total | Non-severe | Severe | p-Value |
| Median (IQR) | N = 165 | N = 51 | N = 114 | |
| Hb (gm/dL) | 13.2 (12–14.4) | 13.4 (12–15) | 13.1 (12.2–14.2) | 0.23 |
| RBC (millions/cumm) | 4.5 (4.1–5) | 4.8 (4.2–5.2) | 4.5 (4.1–1.9) | 0.037* |
| Hct (%) | 39 (15, 36–42) | 40 (15, 35–42) | 39 (15, 36–41) | 0.40 |
| WBC (×106/mL) | 6.7 (4.9–9.6) | 5.8 (4.6–8.6) | 7.2 (5–10.1) | 0.07 |
| ANC (×106/mL) | 5.2 (3–7.9) | 4.3 (2.5–6) | 5.7 (3.6–8.6) | 0.004* |
| ALC (×106/mL) | 1.1 (0.8–1.5) | 1.4 (1, 2) | 1 (0.7–1.4) | 0.001* |
| AMC (×106/mL) | 0.3 (0.2–0.5) | 0.3 (0.2–0.5) | 0.29 (0.16–0.44) | 0.097 |
| AEC (×106/mL) | 0 (0–7.1) | 5.3 (0–10.9) | 0 (0–4.2) | <0.001* |
| Platelets (×106/mL) | 205 (154–269) | 210 (165–240) | 203.5 (153.3–282) | 0.518 |
| MCV (fL) | 85 (83–89) | 85 (82–89) | 86 (83–89) | 0.18 |
| MCH (pg/cell) | 29 (27–30) | 29 (28–30) | 29 (27–30) | 0.54 |
| MCHC (g/dL) | 34 (33, 34) | 34 (33–35) | 33 (33, 34) | 0.29 |
| NLR | 4.8 (2.2–9.1) | 2.8 (1.6–4.6) | 6.1 (2.7–11) | <0.001* |
| PLR | 192 (112–285) | 129 (94–231) | 213 (135–307.5) | <0.001* |
| Ferritin (ng/mL) | 350 (146.5–538.5) | 171 (88–367) | 440 (205–630) | <0.001* |
Abbreviations: ANC, absolute neutrophil count; ALC, absolute lymphocyte count; AMC, absolute monocyte count; AEC, absolute eosinophil count; MCV mean cell volume; MCH, mean cell hemoglobin; MCHC, mean cell hemoglobin concentration; NLR, neutrophil/lymphocyte ratio; and PLR, platelet/lymphocyte ratio.
Based on the clinical report, 84 (50.9%) individuals were presented with at least one complication or co-morbidities in our study. Co-morbidities like hypertension (33.3%) and DM (15.8%) were predominant, followed by hypothyroidism, COPD, CVD, pulmonary disease, and others (Figure 1).
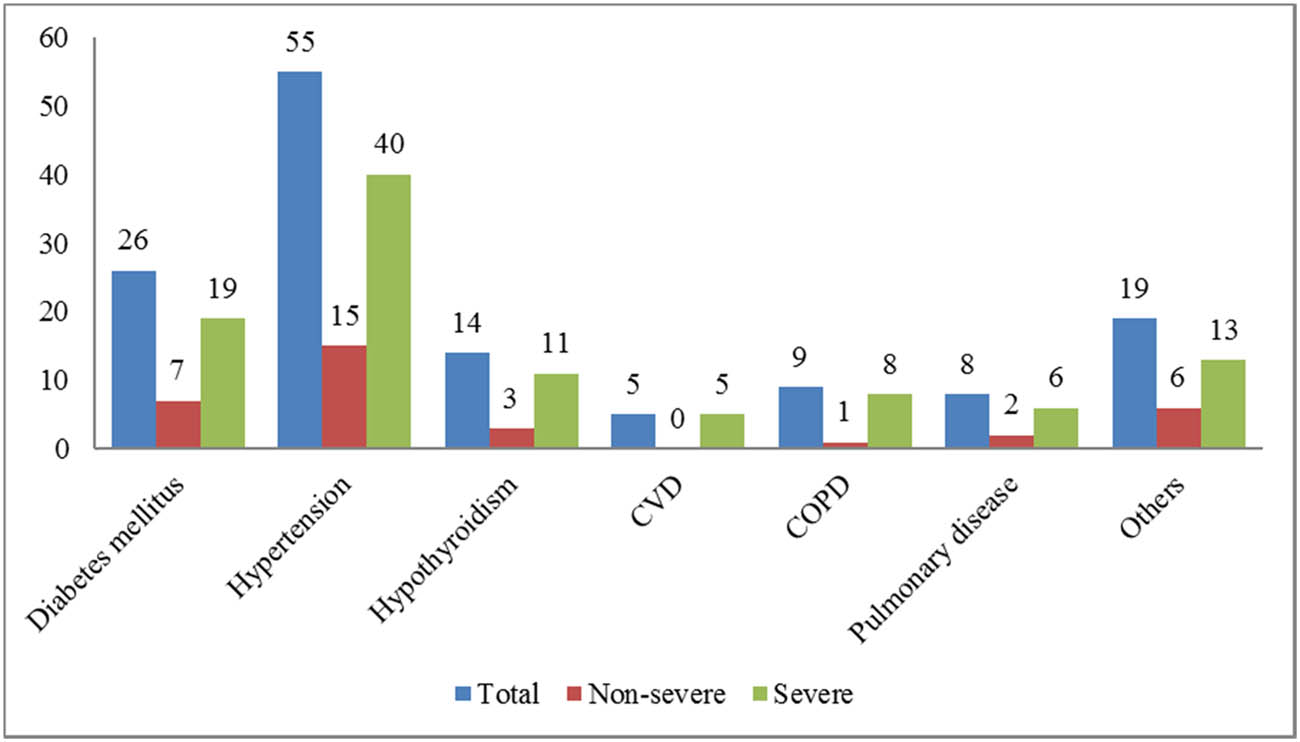
Distribution of co-morbidities among COVID-19 patients; CVD, cardiovascular disease; COPD, chronic obstructive pulmonary disease.
ANC (p = 0.004), NLR (p < 0.001), PLR (p < 0.001), and ferritin (p < 0.001) were significantly higher in severe cases in comparison to non-severe cases while ALC (p = 0.001), AEC (p < 0.001), and RBC (p = 0.037) were significantly lower in severe cases as compared to non-severe cases (Table 3). Similarly, positive CRP was significantly higher in severe cases than in non-severe cases (p < 0.001) (Figure 2). Furthermore, we observed that severe patients showed significantly increased glucose (p = 0.046), urea (p = 0.001), creatinine (p = 0.013), and AST (p = 0.030) levels than non-severe (Table 3 and Figure 3).
Biochemical findings of a patient with COVID-19 on admission to hospital
| Disease severity | ||||
|---|---|---|---|---|
| Biochemical parameters | Total | Non-severe | Severe | p-Value |
| Median (IQR) | N = 165 | N = 51 | N = 114 | |
| Glucose (g/dL) | 136 (115–185) | 133 (106–180) | 141 (120–192) | 0.046* |
| Urea (mg/dL) | 27 (18–39.5) | 21 (15–33) | 29.5 (20–50.25) | 0.001* |
| Creatinine (mg/dL) | 0.8 (0.7–0.95) | 0.8 (0.6–0.8) | 0.8 (0.7–1) | 0.013* |
| Sodium (mEq/L) | 136 (133–138) | 135 (133–138) | 136 (133–138) | 0.442 |
| Potassium (mEq/L) | 4 (3.7–4.35) | 4 (3.7–4.4) | 4 (3.7–4.3) | 0.660 |
| Total bilirubin (mg/dL) | 0.8 (0.7–0.9) | 0.8 (0.7–0.8) | 0.8 (0.7–0.9) | 0.139 |
| Direct bilirubin (mg/dL) | 0.2 (0.2–0.2) | 0.2 (0.2–0.3) | 0.2 (0.2–0.3) | 0.163 |
| ALP (U/L) | 95 (67–118) | 94 (67–118) | 98 (67–118) | 0.764 |
| ALT (U/L) | 45 (15, 28–58, 60–75) | 40 (23.5–69) | 47 (15, 31–58, 60–78) | 0.066 |
| AST (U/L) | 53 (32–73.5) | 40 (15, 23–58, 60–69) | 54.5 (34–81.25) | 0.030* |
| AST/ALT | 1.09 (0.84–1.46) | 1.07 (0.82–1.47) | 1.11 (0.84–1.47) | 0.615 |
Abbreviations: ALP, alkaline phosphatase; ALT, alanine aminotransferase; and AST, aspartate aminotransferase.
The bold letter signifies the statistically significant.
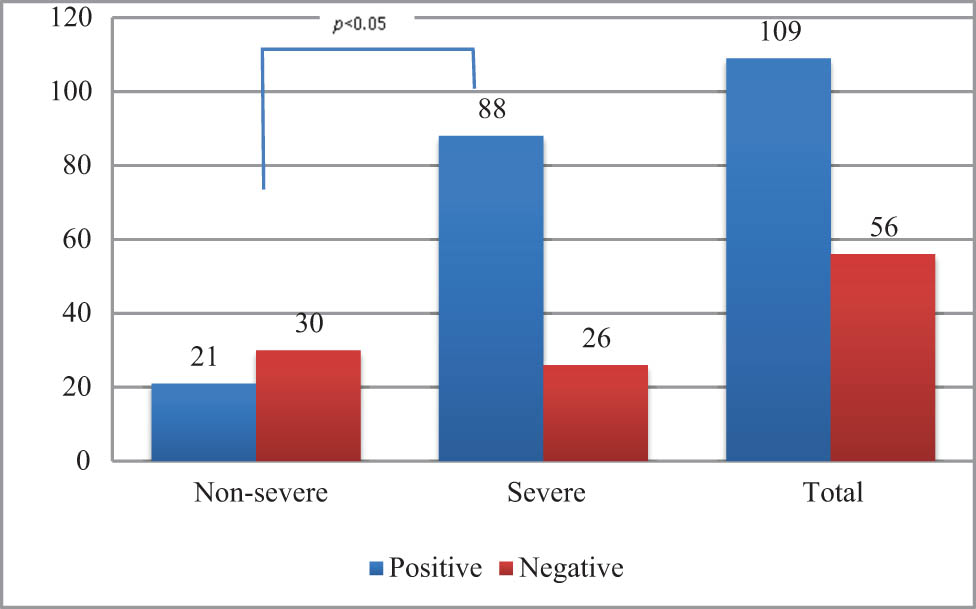
Distribution of CRP among COVID-19 patients.
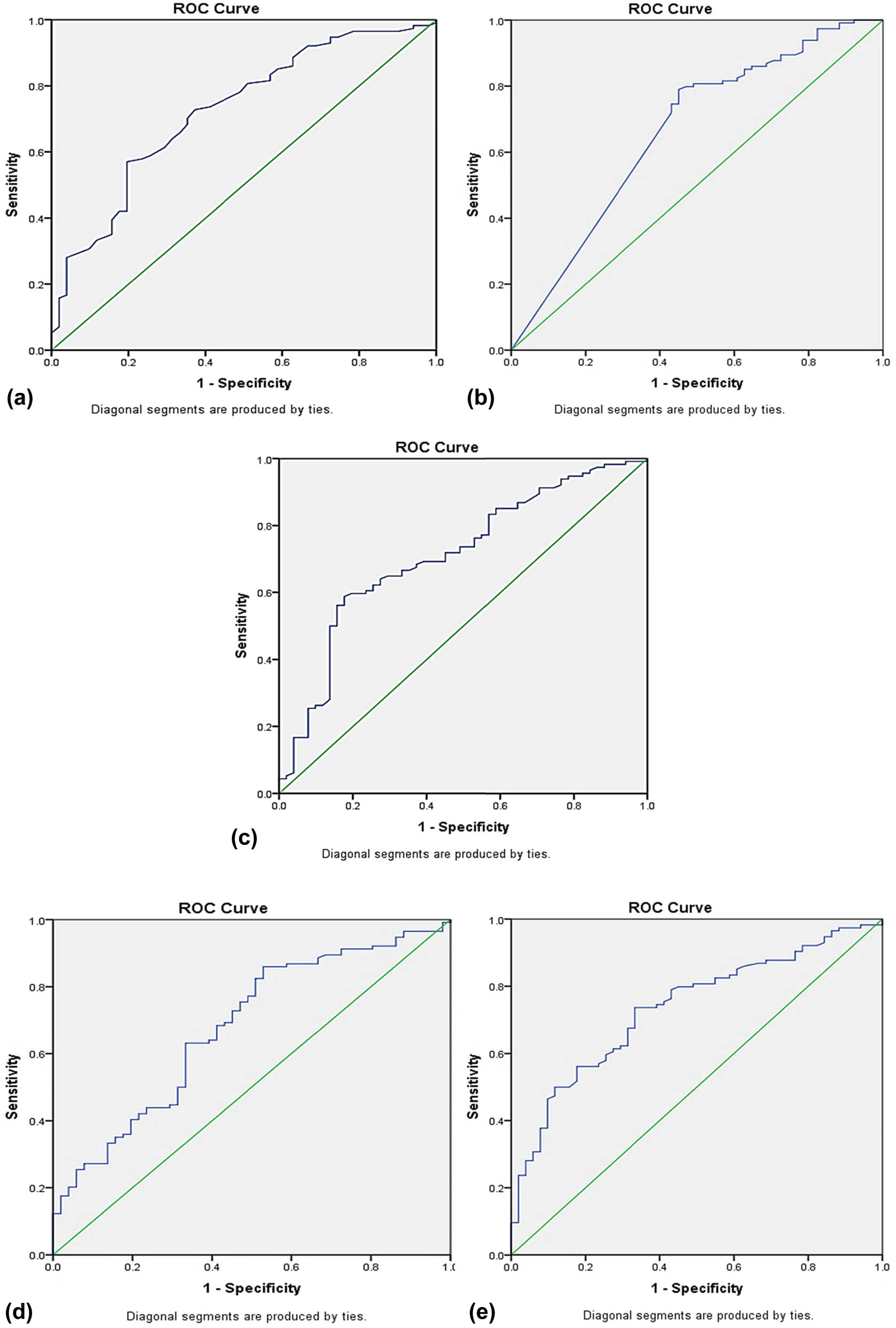
ROC curves of indicators on basis of COVID-19 severity: (a) age, (b) AEC, (c) NLR, (d) PLR, (e) ferritin.
The crude odd ratio (Model I) of risk factors associated with COVID-19 infection was calculated using bivariate logistic regression analysis. Higher age, positive CRP, high ferritin, low ALC, NLR, PLR, high urea, and AST were individual risks associated with severe COVID-19 infection. The significant results obtained from Model I were adjusted in Model II and Model III, and multivariate regression analysis [odds ratio (OR) (95% confidence interval (CI))] was performed that showed higher age [3.611 (1.641–7.947)], positive CRP [2.930 (1.256–6.837)], high ferritin [2.754 (1.184–6.408)], low AEC [3.415 (1.544–7.552)] were independent risk factors associated with severe COVID-19 infection (Tables 4 and 5).
Logistic regression analysis of variables associated with severity of COVID-19
| Test parameter | Model I | p-Value | Model II | p-Value | Model III | p-Value |
|---|---|---|---|---|---|---|
| Age | 3.818 | 0.001* | 3.202 | 0.008* | (1.641–7.947) | 0.001* |
| (>53 years) | (1.876–7.771) | (1.364–7.516) | ||||
| Gender | 1.051 | 0.898 | — | — | — | — |
| (Male) | (0.491–2.248) | |||||
| Co-morbidities | 1.116 | 0.745 | — | — | — | — |
| (0.576–2.160) | ||||||
| ANC | 2.245 | 0.078 | — | - | — | - |
| (High) | (0.913–5.521) | |||||
| ALC | 2.824 | 0.006* | 1.173 | 0.773 | — | — |
| (Low) | (1.341–5.944) | (0.380–3.457) | ||||
| AEC | 3.568 | 0.001* | 2.702 | 0.027* | 3.415 | 0.002* |
| (Low) | (1.782–7.144) | (1.122–6.510) | (1.544–7.552) | |||
| NLR (>3.3) | 3.649 | 0.001* | 0.774 | 0.654 | — | — |
| (1.828–7.286) | (0.253–2.366) | |||||
| PLR (>129) | 3.351 | 0.001* | 1.749 | 0.445 | — | — |
| (1.607–6.738) | (0.541–4.040) | |||||
| Ferritin (High) | 4.340 (2.516–8.738) | 0.001* | 2.508 | 0.049* | 2.754 | 0.019* |
| (0.980–6.420) | (1.184–6.408) | |||||
| CRP | 4.835 | 0.001* | 2.810 | 0.021* | 2.930 | 0.023* |
| (Positive) | (2.380–9.823) | (1.173–6.734) | (1.256–6.837) | |||
| Glucose (High) | 1.833 | 0.081 | — | — | — | — |
| (0.927–3.625) | ||||||
| Urea | 9.151 | 0.003* | 4.897 | 0.066 | — | — |
| (High) | (2.098–39.912) | (0.898–26.704) | ||||
| AST (High) | 2.092 | 0.034* | 1.510 | 0.345 | — | — |
| (1.059–4.131) | (0.642–3.554) |
Odds ratios were given at 95% CI, and p < 0.05 was considered statistically significant.
The bold letter signifies the statistically significant.
ROC curve for the severity of COVID-19
| Test parameters | AUC | 95% CI | p-Value | Cut-off value | Sensitivity% | Specificity% |
|---|---|---|---|---|---|---|
| Age (Years) | 0.724 | (0.641–0.807) | 0.001* | 47.5 | 70.2 | 64.7 |
| AEC (cells/mm3) | 0.661 | (0.567–0.755) | 0.001* | 35.5 | 74 | 67 |
| NLR | 0.710 | (0.625–0.795) | 0.001* | 3.3 | 68.4 | 63.7 |
| PLR | 0.678 | (0.590–0.767) | 0.001* | 129 | 77.2 | 51 |
| Ferritin (ng/mL) | 0.735 | (0.656–0.813) | 0.001* | 241 | 74 | 65 |
The bold letter signifies the statistically significant.
We tested the potential of significant prognostic markers (Age, NLR, PLR, Ferritin, and AEC) using AUROC curve analysis. The highest area under curve (AUC) (0.735) of ferritin was observed with an optimal cut-off value of 241 ng/mL, sensitivity and specificity of 74.0 and 65.0%, respectively, while the lowest AUC (0.661) of AEC with a cut-off of 35.5 cells/mm3, sensitivity 74.0%, and specificity 67%. Similarly, at the cut-off of 47.5 years, age had AUC, sensitivity, and specificity of 0.724, 70.2, and 64.7%, respectively. NLR had AUC, cut-off, sensitivity, and specificity of 0.710, 3.3, 68.4, and 63.7%, respectively. Finally, the sensitivity and specificity of PLR were 77.2 and 51% at cut-off 129 with 0.678 AUC.
4 Discussion
Prognostic markers used to measure the disease severity are considered useful in the patients’ stratification into severe and non-severe groups. However, although most cases are mild to moderate with a better prognosis, the mortality rate was markedly higher in patients developing into severe cases. Therefore, the early identification of critical cases must reduce the mortality rate and improve the recovery rate by the early appropriate clinical intervention [29].
In our study, the mean ages of the study patients were 53.3 ± 16.5 years, which is similar to the study conducted by Chen et al. (55.5 years) [30], while older than that reported by Huang et al. (49 years) [29]. Most of the severe patients were older, with a mean age of 57.5 years than non-severe patients with a mean age of 44.4 years, which is in accordance with a study that suggested age may be a risk factor for poor outcome [30]. Moreover, the ROC curve for age was administered in our study, and the best cut-off point of age was 47.5 years which is similar to that of Yang et al. (49.5 years) [15], while younger than that of Wang et al. (52 years) [4]. Increasing age was found to be an independent risk factor for COVID-19 severity. Similar to our study, in a retrospective analysis of COVID-19 patients, multivariable regression showed an association of disease severity with older age (OR 1.10, 95% CI 1.03–1.17; p = 0.0043) [31]. In general, aged people are more prone to severity than younger people, which may be due to more health issues and underlying diseases in this population [32].
RBC was significantly associated with disease severity which may be due to pro-inflammatory cytokines released during COVID-19 infection resulting in blunt erythropoiesis [33]. However, in contrast to our study, other studies showed that RBC was not affected in COVID-19 patients [5,29,34,35].
In a study by Khalid and Ali Jaffar, leukocytosis was significant among COVID-19 patients [36]. Furthermore, a study of 140 hospitalized patients in Wuhan showed significantly higher leucocyte counts in severe cases than in milder forms [37]. The observed leukocytosis is contributed by the elevation of neutrophils as other WBC populations seem to decrease in severe cases of COVID-19 [38]. Similarly, our study demonstrated more neutrophils and fewer lymphocytes in severe cases compared to those in non-severe patients, similar to Xu et al. [5]. In addition, ANC was significantly higher in severe cases than in non-severe cases in our study, which corresponds well with other studies [29,32,37,39].
Absolute lymphocytopenia is primarily seen in COVID-19 patients, but significant lymphocytopenia is a cardinal marker of enhanced disease severity and indicator of mortality, which has been consistently depicted by several published reports and supported by our study [12,29,37,38]. During hospitalization, non-survivors established more advanced lymphocytopenia than recovered patients [32]. The significance of lymphocytopenia as a hematological symptom of COVID-19 infection has become evident from several studies, including that of Yang et al. showing 72.3% with lymphocytopenia [15], which is in concordance with our study (52.7%). Similarly, ALC was significantly lower in severe groups than in non-severe groups, supported by different studies [12,36]. Reasons for lymphocytopenia with disease severity may be due to the intensification of the inflammatory process (cytokine storm syndrome), direct infections of lymphocytes, and destruction of lymphoid organs, which is supported by the infection of T cells through receptor-dependent S protein-mediated membrane fusion which results in depletion of the cytotoxic capacity of lymphocytes [40–42].
Accordingly, eosinopenia has been reported in more than half (52.9–78.8%) of COVID-19 patients [37,39], which is in correspondence with our findings (65.5%). Similarly, AEC decreased significantly in severe as compared to that in non-severe cases, which is supported by Cai et al. [12]. Possible reasons for eosinopenia include viral attacking bone marrow and blocking eosinophil entrance to peripheral circulation [43]. In addition, AUC was found to be 0.717, which is similar to those of Li et al. (0.717) [43] and Seyit et al. (0.696) [44]. Similarly, our study supported the OR for eosinophil was found to be 3.41, which is supported by Li et al. (3.51) [43]. So, eosinophil, a routine parameter with other parameters, could be used to identify the highly suspected cases from mixed patients.
According to Liu et al., an increase in neutrophil count indicates the intensity of inflammatory response while lymphopenia suggests immune system disruption; therefore, high NLR may be a potential marker for risk factors [45]. NLR has also been a novel marker in other conditions, including thyroid nodules in patients with increased NLR in the preoperative period in case of underlying malignant nodular disease [46]. Our study depicted increased NLR among severe cases compared to not severe cases, similar to other studies [36,47,48]. Recent publications have suggested a high prognostic value of NLR for the prediction of disease severity with AUC 0.94 [12], 0.615 [44], and 0.689 [49], which supported our study that NLR was statistically significant between severe and non-severe groups with 0.710 AUC. Our cut-off value of NLR (3.3) was similar to Yang et al. [15], which showed a superior prognostic possibility of clinical symptoms to convert from mild to severe and similar to that of Liu et al., which gives 3.13. As per the regression analysis in our study performed, OR for NLR was 3.649, which was higher than that of Zhu et al. (1.090) [49] and Seyit et al. (1.274) [44]. Chinese retrospective study reported NLR, along with SARS-CoV-2 IgG used as a simple tool for the severity of COVID-19 infection and to predict clinical outcomes [29].
Increased PLR in COVID-19 patients is due to increased platelet activation and relative lymphocytopenia due to apoptosis of lymphocytes. The high PLR result in our study is consistent with a study [36]. The high PLR rate among COVID patients based on the length of hospital stay is also associated with the prognosis of the disease, which is also depicted by our study and several other studies [15,37,41,50]. Inflammation plays a key role in COVID-19 pathophysiology, with cytokine storm as a hallmark condition in severe disease and poor prognosis, whereas PLR is an established inflammatory marker [51,52]. Similarly, the PLR ratio was found to be 129 in our study, which is greater than that of the study performed by Seyit et al. [44], with a cut-off of 102.8, sensitivity of 70%, and specificity of 52%. In addition, we showed PLR as a risk factor for disease severity with COR 3.351, which is supported by a study with AOR 1.009 [44].
In our study, inflammatory markers, including ferritin and CRP, show a significant increase as indicated by Khalid and Ali Jaffar suggesting its association with disease severity and poor outcome, which may be associated with elevated hepcidin levels due to inflammatory reaction [36]. As per Kell and Pretorius ferritin levels greater than 600 ng/dL indicate cellular damage [53]. In our study, AUC for ferritin was found to be 0.735 with a cut-off of 241 ng/mL and an independent risk factor for the disease severity with AOR 2.754, which is supported by other findings [54]. It may be due to the extreme immune activation of cytokine storms in severe patients, leading to upregulation of serum ferritin levels [55]. CRP is an acute phase protein synthesized by hepatocytes, with increased levels parallel to the severity of inflammation [43]. In our study, 66.1% showed positive CRP with a higher population among severe cases (77.2%) than among non-severe cases (41.2%) in response to proinflammatory cytokines. According to Tan et al., CRP significantly increases among severe cases and predicts early severe cases [56]. Our study found positive CRP as an independent risk factor for disease severity with OR 2.930.
In this study, biochemical parameters such as glucose, urea, creatinine, and AST had significant differences between severe and non-severe cases. Glucose is significantly higher in severe cases than in non-severe cases, similar to that of Gao et al. [57]. Creatinine was a significantly higher concentration in severe cases, supported by a study by Huang et al. [29]. In addition, 55.7 and 64.8% of patients showed elevated ALT and AST, respectively, as reported by Guan et al., which might show virus-mediated liver impairment. According to Zhang et al., any immune-mediated inflammation in particular cytokine storm and pneumonia-associated hypoxia may lead to liver damage in severe COVID-19 patients [58].
With the evaluation of the trends and variations of CBC and inflammatory parameters among severe and non-severe COVID-19 patients, it can be concluded that the use of readily available, inexpensive tests could be helpful for the diagnosis, prognosis, stratification, and prioritization of treatment in the unavailability of the standard test like RT-PCR, and CT- scan in the developing countries lacking the infrastructures and manpower with a heavy burden of the diseases.
This study has several limitations. First, some inflammatory factors and immunological indexes cannot be detected and compared due to the limitation of experimental conditions. Second, this is a cross-sectional study with participants from a single center rather than multiple centers.
5 Conclusion
In comparison to non-severe COVID-19, severe COVID-19 was associated with increased markers of the innate immune response such as neutrophil count, NLR, CRP, and serum ferritin; decreased markers of the adaptive immune response such as lymphocyte, and increased markers of significant organ damage including AST, urea, and creatinine. Moreover, age, AEC, CRP, and ferritin were independent risk factors for assessing the severity of COVID-19. Therefore, with the following parameters such as age > 47.5 years, NLR > 3.3, PLR > 129, ferritin > 241 ng/mL, and AEC < 35.5 cells/cumm, the progress of COVID-19 to the severe stage should be closely observed and managed accordingly.
Additionally, hematological and inflammatory parameters can aid clinicians in determining the severity of disease that can help prioritize cases and provide prompt treatment reducing the mortality rate.
Acknowledgment
We thank all the patients participating in this study. Furthermore, our special thanks go to all the laboratory staff, management, and officials of STIDH and MMIHS for providing the opportunity to carry out this research work.
-
Funding information: Authors state no funding is involved.
-
Author contributions: D.K.M., M.P.B. – primary and corresponding author who designed the study methodology. MC., B.R.B. – literature review, prepare the laboratory protocols, perform the laboratory investigations, and collect data. M.C., B.R.B., S.A. & S.P. – analyzed the data and, prepared the article for submission, performed proofreading of the article. D.M., M.P.B., S.K.B., and S.B.M. – supervision and project administration. A.B., S.K.S., and R.N. – filling the consent forms, sample collection, and drafting the manuscript. All authors contributed to drafting and critically revising the study and agree to be accountable for all aspects of the work.
-
Conflict of interest: Authors state no conflict of interest.
-
Data availability statement: The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
[1] Fehr AR, Perlman S. Coronaviruses: an overview of their replication and pathogenesis. Methods Mol Biol (Clifton, NJ). 2015;1282:1–23.10.1007/978-1-4939-2438-7_1Suche in Google Scholar
[2] Dhakal S, Karki S. Early epidemiological features of COVID-19 in Nepal and public health response. Front Med (Lausanne). 2020;7:524.10.3389/fmed.2020.00524Suche in Google Scholar
[3] Aktas G. A comprehensive review on rational and effective treatment strategies against an invisible enemy; SARS Cov-2 infection. Exp Biomed Res. 2020;3:293–311.10.30714/j-ebr.2020463629Suche in Google Scholar
[4] Wang D, Li R, Wang J, Jiang Q, Gao C, Yang J, et al. Correlation analysis between disease severity and clinical and biochemical characteristics of 143 cases of COVID-19 in Wuhan, China: a descriptive study. 2020;20(1):519.10.1186/s12879-020-05242-wSuche in Google Scholar
[5] Xu XW, Wu XX, Jiang XG, Xu KJ, Ying LJ, Ma CL, et al. Clinical findings in a group of patients infected with the 2019 novel coronavirus (SARS-Cov-2) outside of Wuhan, China: retrospective case series. BMJ (Clin Res Ed). 2020;368:m606.10.1136/bmj.m606Suche in Google Scholar
[6] Chan JF, Zhang AJ, Yuan S, Poon VK, Chan CC, Lee AC, et al. Simulation of the clinical and pathological manifestations of coronavirus disease 2019 (COVID-19) in a golden syrian hamster model: implications for disease pathogenesis and transmissibility. Clin Infect Dis. 2020;71(9):2428–46.10.1093/cid/ciaa325Suche in Google Scholar
[7] Rothe C, Schunk M, Sothmann P, Bretzel G, Froeschl G, Wallrauch C, et al. Transmission of 2019-nCoV infection from an asymptomatic contact in Germany. N Engl J Med. 2020;382(10):970–1.10.1056/NEJMc2001468Suche in Google Scholar
[8] Qin C, Zhou L, Hu Z, Zhang S, Yang S, Tao Y, et al. Dysregulation of immune response in patients with coronavirus 2019 (COVID-19) in Wuhan, China. Clin Infect Diseases Off Publ Infect Dis Soc Am. 2020;71(15):762–8.10.1093/cid/ciaa248Suche in Google Scholar
[9] Yang X, Yu Y, Xu J, Shu H, Xia J, Liu H, et al. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Respir Med. 2020;8(5):475–81.10.1016/S2213-2600(20)30079-5Suche in Google Scholar
[10] Yuki K, Fujiogi M, Koutsogiannaki S. COVID-19 pathophysiology: A review. Clin Immunol. 2020;215:108427.10.1016/j.clim.2020.108427Suche in Google Scholar PubMed PubMed Central
[11] Yang W, Cao Q, Qin L, Wang X, Cheng Z, Pan A, et al. Clinical characteristics and imaging manifestations of the 2019 novel coronavirus disease (COVID-19):A multi-center study in Wenzhou city, Zhejiang, China. J Infect. 2020;80(4):388–93.10.1016/j.jinf.2020.02.016Suche in Google Scholar PubMed PubMed Central
[12] Cai Q, Huang D, Ou P, Yu H, Zhu Z, Xia Z, et al. COVID-19 in a designated infectious diseases hospital outside Hubei Province, China. Allergy. 2020;75(7):1742–52.10.1111/all.14309Suche in Google Scholar PubMed
[13] Li X, Xu S, Yu M, Wang K, Tao Y, Zhou Y, et al. Risk factors for severity and mortality in adult COVID-19 inpatients in Wuhan. J Allergy Clin Immunol. 2020;146(1):110–8.10.1016/j.jaci.2020.04.006Suche in Google Scholar PubMed PubMed Central
[14] Liu Y, Yang Y, Zhang C, Huang F, Wang F, Yuan J, et al. Clinical and biochemical indexes from 2019-nCoV infected patients linked to viral loads and lung injury. Sci China Life Sci. 2020;63(3):364–74.10.1007/s11427-020-1643-8Suche in Google Scholar PubMed PubMed Central
[15] Yang AP, Liu JP, Tao WQ, Li HM. The diagnostic and predictive role of NLR, d-NLR and PLR in COVID-19 patients. Int Immunopharmacol. 2020;84:106504.10.1016/j.intimp.2020.106504Suche in Google Scholar PubMed PubMed Central
[16] Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in china: summary of a report of 72,314 cases from the chinese center for disease control and prevention. JAMA. 2020;323(13):1239–42.10.1001/jama.2020.2648Suche in Google Scholar PubMed
[17] Rodriguez-Morales AJ, Cardona-Ospina JA, Gutiérrez-Ocampo E, Villamizar-Peña R, Holguin-Rivera Y, Escalera-Antezana JP, et al. Clinical, laboratory and imaging features of COVID-19: A systematic review and meta-analysis. Travel Med Infect Dis. 2020;34:101623.10.1016/j.tmaid.2020.101623Suche in Google Scholar PubMed PubMed Central
[18] Lippi G, Plebani M, Henry BM. Thrombocytopenia is associated with severe coronavirus disease 2019 (COVID-19) infections: A meta-analysis. Clin Chim Acta Int J Clin Chem. 2020;506:145–8.10.1016/j.cca.2020.03.022Suche in Google Scholar PubMed PubMed Central
[19] Aktas G, Sit M, Dikbas O, Erkol H, Altinordu R, Erkus E, et al. Elevated neutrophil-to-lymphocyte ratio in the diagnosis of Hashimoto’s thyroiditis. Rev da Assoc Med Brasileira (1992). 2017;63(12):1065–8.10.1590/1806-9282.63.12.1065Suche in Google Scholar PubMed
[20] Aktas G, Duman T, Atak B, Kurtkulagi O, Bilgin S, Basaran E, et al. Irritable bowel syndrome is associated with novel inflammatory markers derived from hemogram parameters. Family Med Prim Care Rev. 2020;22:107–10.10.5114/fmpcr.2020.95311Suche in Google Scholar
[21] Aktas G. Hematological predictors of novel coronavirus infection. Rev da Assoc Méd Brasileira. 2021;67:1–2.10.1590/1806-9282.67.suppl1.20200678Suche in Google Scholar
[22] Afsin H, Aktas G. Platelet to lymphocyte and neutrophil to lymphocyte Ratios are useful in differentiation of thyroid conditions with normal and increased uptake. Ethiopian. J Health Dev. 2021;35(3):149–53.Suche in Google Scholar
[23] Atak BM, Kahveci GB, Bilgin S, Kurtkulagi O, Kosekli MA. Platelet to lymphocyte ratio in differentiation of benign and malignant thyroid nodules. Exp Biomed Res. 2021;4(2):148–53.10.30714/j-ebr.2021267978Suche in Google Scholar
[24] Atak B, Aktas G, Duman TT, Erkus E, Kocak MZ, Savli H. O controle diabético poderia ser predicado por Platelet para a relação de linfócitos no hemograma. Rev da Assoc Méd Brasileira. 2019;65:38–42.10.1590/1806-9282.65.1.38Suche in Google Scholar
[25] Demirkol ME, Aktas G. C-reactive protein to LymphocytE count ratio could be a reliable mArkeR of thyroiditis; the CLEAR-T study. Precis Med Sci. 2022;11(1):31–4.10.1002/prm2.12065Suche in Google Scholar
[26] Demirkol ME, Aktas G. C-reactive protein to lymphocyte count ratio is a promising novel marker in hepatitis C infection: the clear hep-c study. Rev Assoc Med Brasileira (1992). 2022;68(6):838–41.10.1590/1806-9282.20220236Suche in Google Scholar
[27] Bilgin S, Kurtkulagi O, Atak Tel BM, Duman TT, Kahveci G, Khalid A, et al. Does C-reactive protein to serum albumin ratio correlate with diabEtic nephropathy in patients with Type 2 dIabetes MEllitus? The CARE TIME study. Prim Care Diabetes. 2021;15(6):1071–4.10.1016/j.pcd.2021.08.015Suche in Google Scholar
[28] Commission NH. Medicine NAoTC. Diagnosis and treatment protocol for novel coronavirus pneumonia (Trial Version 7). Chin Med J (Engl). 2020;133(9):1087–95.10.1097/CM9.0000000000000819Suche in Google Scholar
[29] Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. lancet. 2020;395(10223):497–506.10.1016/S0140-6736(20)30183-5Suche in Google Scholar
[30] Chen G, Wu D, Guo W, Cao Y, Huang D, Wang H, et al. Clinical and immunological features of severe and moderate coronavirus disease 2019. J Clin investigation. 2020;130(5):2620–9.10.1172/JCI137244Suche in Google Scholar
[31] Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. lancet. 2020;395(10229):1054–62.10.1016/S0140-6736(20)30566-3Suche in Google Scholar
[32] Wang D, Hu B, Hu C, Zhu F, Liu X, Zhang J, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. Jama. 2020;323(11):1061–9.10.1001/jama.2020.1585Suche in Google Scholar PubMed PubMed Central
[33] Nemeth E, Ganz T. Anemia of inflammation. Hematol/Oncol Clin North Am. 2014;28(4):671–81. vi.10.1016/j.hoc.2014.04.005Suche in Google Scholar PubMed PubMed Central
[34] Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He JX, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382(18):1708–20.10.1056/NEJMoa2002032Suche in Google Scholar PubMed PubMed Central
[35] Chang D, Lin M, Wei L, Xie L, Zhu G, Dela Cruz CS, et al. Epidemiologic and clinical characteristics of novel coronavirus infections involving 13 patients outside Wuhan, China. Jama. 2020;323(11):1092–3.10.1001/jama.2020.1623Suche in Google Scholar PubMed PubMed Central
[36] Khalid A, Ali Jaffar M. Hematological and biochemical parameters as diagnostic and prognostic markers in SARS-COV-2 infected patients of Pakistan: a retrospective comparative analysis. Hematol (Amsterdam, Netherlands). 2021;26(1):529–42.10.1080/16078454.2021.1950898Suche in Google Scholar PubMed
[37] Liu J, Li S, Liu J, Liang B, Wang X, Wang H, et al. Longitudinal characteristics of lymphocyte responses and cytokine profiles in the peripheral blood of SARS-CoV-2 infected patients. EBioMedicine. 2020;55:102763.10.1016/j.ebiom.2020.102763Suche in Google Scholar PubMed PubMed Central
[38] Henry BM, de Oliveira MHS, Benoit S, Plebani M, Lippi G. Hematologic, biochemical and immune biomarker abnormalities associated with severe illness and mortality in coronavirus disease 2019 (COVID-19): a meta-analysis. Clin Chem Lab Med. 2020;58(7):1021–8.10.1515/cclm-2020-0369Suche in Google Scholar PubMed
[39] Li Q, Ding X, Xia G, Geng Z, Chen F, Wang L, et al. A simple laboratory parameter facilitates early identification of COVID-19 patients. medRxiv. 2020;2020.02.13.20022830.10.1101/2020.02.13.20022830Suche in Google Scholar
[40] Hoffmann M, Kleine-Weber H, Schroeder S, Krüger N, Herrler T, Erichsen S, et al. SARS-CoV-2 cell entry depends on ACE2 and TMPRSS2 and is blocked by a clinically proven protease inhibitor. Cell. 2020;181(2):271–80.e8.10.1016/j.cell.2020.02.052Suche in Google Scholar PubMed PubMed Central
[41] Sun S, Cai X, Wang H, He G, Lin Y, Lu B, et al. Abnormalities of peripheral blood system in patients with COVID-19 in Wenzhou, China. Clinica Chim Acta Int J Clin Chem. 2020;507:174–80.10.1016/j.cca.2020.04.024Suche in Google Scholar PubMed PubMed Central
[42] Zheng M, Gao Y, Wang G, Song G, Liu S, Sun D, et al. Functional exhaustion of antiviral lymphocytes in COVID-19 patients. Cell Mol Immunol. 2020;17(5):533–5.10.1038/s41423-020-0402-2Suche in Google Scholar PubMed PubMed Central
[43] Li Q, Ding X, Xia G, Chen H-G, Chen F, Geng Z, et al. Eosinopenia and elevated C-reactive protein facilitate triage of COVID-19 patients in fever clinic: a retrospective case-control study. Eclinical Med. 2020;23:100375.10.1016/j.eclinm.2020.100375Suche in Google Scholar PubMed PubMed Central
[44] Seyit M, Avci E, Nar R, Senol H, Yilmaz A, Ozen M, et al. Neutrophil to lymphocyte ratio, lymphocyte to monocyte ratio and platelet to lymphocyte ratio to predict the severity of COVID-19. Am J Emerg Med. 2021;40:110–4.10.1016/j.ajem.2020.11.058Suche in Google Scholar PubMed PubMed Central
[45] Liu J, Liu Y, Xiang P, Pu L, Xiong H, Li C, et al. Neutrophil-to-lymphocyte ratio predicts critical illness patients with 2019 coronavirus disease in the early stage. J Transl Med. 2020;18(1):1–12.10.1186/s12967-020-02374-0Suche in Google Scholar PubMed PubMed Central
[46] Chan AS, Rout A. Use of Neutrophil-to-Lymphocyte and Platelet-to-Lymphocyte Ratios in COVID-19. J Clin Med Res. 2020;12(7):448–53.10.14740/jocmr4240Suche in Google Scholar PubMed PubMed Central
[47] Ghahramani S, Tabrizi R, Lankarani KB, Kashani SMA, Rezaei S, Zeidi N, et al. Laboratory features of severe vs. non-severe COVID-19 patients in Asian populations: a systematic review and meta-analysis. Eur J Med Res. 2020;25(1):30.10.1186/s40001-020-00432-3Suche in Google Scholar PubMed PubMed Central
[48] Lagunas-Rangel FA. Neutrophil-to-lymphocyte ratio and lymphocyte-to-C-reactive protein ratio in patients with severe coronavirus disease 2019 (COVID-19): A meta-analysis. J Med Virol. 2020;92(10):1733–4.10.1002/jmv.25819Suche in Google Scholar PubMed PubMed Central
[49] Zhu Z, Cai T, Fan L, Lou K, Hua X, Huang Z, et al. Clinical value of immune-inflammatory parameters to assess the severity of coronavirus disease 2019. Int J Infect Dis. 2020;95:332–9.10.1016/j.ijid.2020.04.041Suche in Google Scholar PubMed PubMed Central
[50] Gong J, Ou J, Qiu X, Jie Y, Chen Y, Yuan L, et al. A tool for early prediction of severe coronavirus disease 2019 (COVID-19): a multicenter study using the risk nomogram in Wuhan and Guangdong, China. Clin Infect Diseases Off Publ Infect Dis Soc Am. 2020;71(15):833–40.10.1093/cid/ciaa443Suche in Google Scholar PubMed PubMed Central
[51] Merad M, Martin JC. Author correction: pathological inflammation in patients with COVID-19: a key role for monocytes and macrophages. Nat Rev Immunol. 2020;20(7):448.10.1038/s41577-020-0353-ySuche in Google Scholar PubMed PubMed Central
[52] Akboga MK, Canpolat U, Yuksel M, Yayla C, Yilmaz S, Turak O, et al. Platelet to lymphocyte ratio as a novel indicator of inflammation is correlated with the severity of metabolic syndrome: A single center large-scale study. Platelets. 2016;27(2):178–83.10.3109/09537104.2015.1064518Suche in Google Scholar
[53] Kell DB, Pretorius E. Serum ferritin is an important inflammatory disease marker, as it is mainly a leakage product from damaged cells. Metallomics Integr Biometal Sci. 2014;6(4):748–73.10.1039/C3MT00347GSuche in Google Scholar
[54] Chen T, Wu D, Chen H, Yan W, Yang D, Chen G, et al. Clinical characteristics of 113 deceased patients with coronavirus disease 2019: retrospective study. BMJ (Clin Res ed). 2020;368:m1091.10.1136/bmj.m1091Suche in Google Scholar
[55] Kernan KF, Carcillo JA. Hyperferritinemia and inflammation. Int Immunol. 2017;29(9):401–9.10.1093/intimm/dxx031Suche in Google Scholar
[56] Tan C, Huang Y, Shi F, Tan K, Ma Q, Chen Y, et al. C-reactive protein correlates with computed tomographic findings and predicts severe COVID-19 early. J Med Virol. 2020;92(7):856–62.10.1002/jmv.25871Suche in Google Scholar
[57] Gao Y, Li T, Han M, Li X, Wu D, Xu Y, et al. Diagnostic utility of clinical laboratory data determinations for patients with the severe COVID-19. J Med Virol. 2020;92(7):791–6.10.1002/jmv.25770Suche in Google Scholar
[58] Zhang C, Shi L, Wang FS. Liver injury in COVID-19: management and challenges. Lancet Gastroenterol Hepatol. 2020;5(5):428–30.10.1016/S2468-1253(20)30057-1Suche in Google Scholar
© 2022 Dipendra Kumar Mandal et al., published by De Gruyter
This work is licensed under the Creative Commons Attribution 4.0 International License.
Artikel in diesem Heft
- Biomedical Sciences
- Effects of direct oral anticoagulants dabigatran and rivaroxaban on the blood coagulation function in rabbits
- The mother of all battles: Viruses vs humans. Can humans avoid extinction in 50–100 years?
- Knockdown of G1P3 inhibits cell proliferation and enhances the cytotoxicity of dexamethasone in acute lymphoblastic leukemia
- LINC00665 regulates hepatocellular carcinoma by modulating mRNA via the m6A enzyme
- Association study of CLDN14 variations in patients with kidney stones
- Concanavalin A-induced autoimmune hepatitis model in mice: Mechanisms and future outlook
- Regulation of miR-30b in cancer development, apoptosis, and drug resistance
- Informatic analysis of the pulmonary microecology in non-cystic fibrosis bronchiectasis at three different stages
- Swimming attenuates tumor growth in CT-26 tumor-bearing mice and suppresses angiogenesis by mediating the HIF-1α/VEGFA pathway
- Characterization of intestinal microbiota and serum metabolites in patients with mild hepatic encephalopathy
- Functional conservation and divergence in plant-specific GRF gene family revealed by sequences and expression analysis
- Application of the FLP/LoxP-FRT recombination system to switch the eGFP expression in a model prokaryote
- Biomedical evaluation of antioxidant properties of lamb meat enriched with iodine and selenium
- Intravenous infusion of the exosomes derived from human umbilical cord mesenchymal stem cells enhance neurological recovery after traumatic brain injury via suppressing the NF-κB pathway
- Effect of dietary pattern on pregnant women with gestational diabetes mellitus and its clinical significance
- Potential regulatory mechanism of TNF-α/TNFR1/ANXA1 in glioma cells and its role in glioma cell proliferation
- Effect of the genetic mutant G71R in uridine diphosphate-glucuronosyltransferase 1A1 on the conjugation of bilirubin
- Quercetin inhibits cytotoxicity of PC12 cells induced by amyloid-beta 25–35 via stimulating estrogen receptor α, activating ERK1/2, and inhibiting apoptosis
- Nutrition intervention in the management of novel coronavirus pneumonia patients
- circ-CFH promotes the development of HCC by regulating cell proliferation, apoptosis, migration, invasion, and glycolysis through the miR-377-3p/RNF38 axis
- Bmi-1 directly upregulates glucose transporter 1 in human gastric adenocarcinoma
- Lacunar infarction aggravates the cognitive deficit in the elderly with white matter lesion
- Hydroxysafflor yellow A improved retinopathy via Nrf2/HO-1 pathway in rats
- Comparison of axon extension: PTFE versus PLA formed by a 3D printer
- Elevated IL-35 level and iTr35 subset increase the bacterial burden and lung lesions in Mycobacterium tuberculosis-infected mice
- A case report of CAT gene and HNF1β gene variations in a patient with early-onset diabetes
- Study on the mechanism of inhibiting patulin production by fengycin
- SOX4 promotes high-glucose-induced inflammation and angiogenesis of retinal endothelial cells by activating NF-κB signaling pathway
- Relationship between blood clots and COVID-19 vaccines: A literature review
- Analysis of genetic characteristics of 436 children with dysplasia and detailed analysis of rare karyotype
- Bioinformatics network analyses of growth differentiation factor 11
- NR4A1 inhibits the epithelial–mesenchymal transition of hepatic stellate cells: Involvement of TGF-β–Smad2/3/4–ZEB signaling
- Expression of Zeb1 in the differentiation of mouse embryonic stem cell
- Study on the genetic damage caused by cadmium sulfide quantum dots in human lymphocytes
- Association between single-nucleotide polymorphisms of NKX2.5 and congenital heart disease in Chinese population: A meta-analysis
- Assessment of the anesthetic effect of modified pentothal sodium solution on Sprague-Dawley rats
- Genetic susceptibility to high myopia in Han Chinese population
- Potential biomarkers and molecular mechanisms in preeclampsia progression
- Silencing circular RNA-friend leukemia virus integration 1 restrained malignancy of CC cells and oxaliplatin resistance by disturbing dyskeratosis congenita 1
- Endostar plus pembrolizumab combined with a platinum-based dual chemotherapy regime for advanced pulmonary large-cell neuroendocrine carcinoma as a first-line treatment: A case report
- The significance of PAK4 in signaling and clinicopathology: A review
- Sorafenib inhibits ovarian cancer cell proliferation and mobility and induces radiosensitivity by targeting the tumor cell epithelial–mesenchymal transition
- Characterization of rabbit polyclonal antibody against camel recombinant nanobodies
- Active legumain promotes invasion and migration of neuroblastoma by regulating epithelial-mesenchymal transition
- Effect of cell receptors in the pathogenesis of osteoarthritis: Current insights
- MT-12 inhibits the proliferation of bladder cells in vitro and in vivo by enhancing autophagy through mitochondrial dysfunction
- Study of hsa_circRNA_000121 and hsa_circRNA_004183 in papillary thyroid microcarcinoma
- BuyangHuanwu Decoction attenuates cerebral vasospasm caused by subarachnoid hemorrhage in rats via PI3K/AKT/eNOS axis
- Effects of the interaction of Notch and TLR4 pathways on inflammation and heart function in septic heart
- Monosodium iodoacetate-induced subchondral bone microstructure and inflammatory changes in an animal model of osteoarthritis
- A rare presentation of type II Abernethy malformation and nephrotic syndrome: Case report and review
- Rapid death due to pulmonary epithelioid haemangioendothelioma in several weeks: A case report
- Hepatoprotective role of peroxisome proliferator-activated receptor-α in non-cancerous hepatic tissues following transcatheter arterial embolization
- Correlation between peripheral blood lymphocyte subpopulations and primary systemic lupus erythematosus
- A novel SLC8A1-ALK fusion in lung adenocarcinoma confers sensitivity to alectinib: A case report
- β-Hydroxybutyrate upregulates FGF21 expression through inhibition of histone deacetylases in hepatocytes
- Identification of metabolic genes for the prediction of prognosis and tumor microenvironment infiltration in early-stage non-small cell lung cancer
- BTBD10 inhibits glioma tumorigenesis by downregulating cyclin D1 and p-Akt
- Mucormycosis co-infection in COVID-19 patients: An update
- Metagenomic next-generation sequencing in diagnosing Pneumocystis jirovecii pneumonia: A case report
- Long non-coding RNA HOXB-AS1 is a prognostic marker and promotes hepatocellular carcinoma cells’ proliferation and invasion
- Preparation and evaluation of LA-PEG-SPION, a targeted MRI contrast agent for liver cancer
- Proteomic analysis of the liver regulating lipid metabolism in Chaohu ducks using two-dimensional electrophoresis
- Nasopharyngeal tuberculosis: A case report
- Characterization and evaluation of anti-Salmonella enteritidis activity of indigenous probiotic lactobacilli in mice
- Aberrant pulmonary immune response of obese mice to periodontal infection
- Bacteriospermia – A formidable player in male subfertility
- In silico and in vivo analysis of TIPE1 expression in diffuse large B cell lymphoma
- Effects of KCa channels on biological behavior of trophoblasts
- Interleukin-17A influences the vulnerability rather than the size of established atherosclerotic plaques in apolipoprotein E-deficient mice
- Multiple organ failure and death caused by Staphylococcus aureus hip infection: A case report
- Prognostic signature related to the immune environment of oral squamous cell carcinoma
- Primary and metastatic squamous cell carcinoma of the thyroid gland: Two case reports
- Neuroprotective effects of crocin and crocin-loaded niosomes against the paraquat-induced oxidative brain damage in rats
- Role of MMP-2 and CD147 in kidney fibrosis
- Geometric basis of action potential of skeletal muscle cells and neurons
- Babesia microti-induced fulminant sepsis in an immunocompromised host: A case report and the case-specific literature review
- Role of cerebellar cortex in associative learning and memory in guinea pigs
- Application of metagenomic next-generation sequencing technique for diagnosing a specific case of necrotizing meningoencephalitis caused by human herpesvirus 2
- Case report: Quadruple primary malignant neoplasms including esophageal, ureteral, and lung in an elderly male
- Long non-coding RNA NEAT1 promotes angiogenesis in hepatoma carcinoma via the miR-125a-5p/VEGF pathway
- Osteogenic differentiation of periodontal membrane stem cells in inflammatory environments
- Knockdown of SHMT2 enhances the sensitivity of gastric cancer cells to radiotherapy through the Wnt/β-catenin pathway
- Continuous renal replacement therapy combined with double filtration plasmapheresis in the treatment of severe lupus complicated by serious bacterial infections in children: A case report
- Simultaneous triple primary malignancies, including bladder cancer, lymphoma, and lung cancer, in an elderly male: A case report
- Preclinical immunogenicity assessment of a cell-based inactivated whole-virion H5N1 influenza vaccine
- One case of iodine-125 therapy – A new minimally invasive treatment of intrahepatic cholangiocarcinoma
- S1P promotes corneal trigeminal neuron differentiation and corneal nerve repair via upregulating nerve growth factor expression in a mouse model
- Early cancer detection by a targeted methylation assay of circulating tumor DNA in plasma
- Calcifying nanoparticles initiate the calcification process of mesenchymal stem cells in vitro through the activation of the TGF-β1/Smad signaling pathway and promote the decay of echinococcosis
- Evaluation of prognostic markers in patients infected with SARS-CoV-2
- N6-Methyladenosine-related alternative splicing events play a role in bladder cancer
- Characterization of the structural, oxidative, and immunological features of testis tissue from Zucker diabetic fatty rats
- Effects of glucose and osmotic pressure on the proliferation and cell cycle of human chorionic trophoblast cells
- Investigation of genotype diversity of 7,804 norovirus sequences in humans and animals of China
- Characteristics and karyotype analysis of a patient with turner syndrome complicated with multiple-site tumors: A case report
- Aggravated renal fibrosis is positively associated with the activation of HMGB1-TLR2/4 signaling in STZ-induced diabetic mice
- Distribution characteristics of SARS-CoV-2 IgM/IgG in false-positive results detected by chemiluminescent immunoassay
- SRPX2 attenuated oxygen–glucose deprivation and reperfusion-induced injury in cardiomyocytes via alleviating endoplasmic reticulum stress-induced apoptosis through targeting PI3K/Akt/mTOR axis
- Aquaporin-8 overexpression is involved in vascular structure and function changes in placentas of gestational diabetes mellitus patients
- Relationship between CRP gene polymorphisms and ischemic stroke risk: A systematic review and meta-analysis
- Effects of growth hormone on lipid metabolism and sexual development in pubertal obese male rats
- Cloning and identification of the CTLA-4IgV gene and functional application of vaccine in Xinjiang sheep
- Antitumor activity of RUNX3: Upregulation of E-cadherin and downregulation of the epithelial–mesenchymal transition in clear-cell renal cell carcinoma
- PHF8 promotes osteogenic differentiation of BMSCs in old rat with osteoporosis by regulating Wnt/β-catenin pathway
- A review of the current state of the computer-aided diagnosis (CAD) systems for breast cancer diagnosis
- Bilateral dacryoadenitis in adult-onset Still’s disease: A case report
- A novel association between Bmi-1 protein expression and the SUVmax obtained by 18F-FDG PET/CT in patients with gastric adenocarcinoma
- The role of erythrocytes and erythroid progenitor cells in tumors
- Relationship between platelet activation markers and spontaneous abortion: A meta-analysis
- Abnormal methylation caused by folic acid deficiency in neural tube defects
- Silencing TLR4 using an ultrasound-targeted microbubble destruction-based shRNA system reduces ischemia-induced seizures in hyperglycemic rats
- Plant Sciences
- Seasonal succession of bacterial communities in cultured Caulerpa lentillifera detected by high-throughput sequencing
- Cloning and prokaryotic expression of WRKY48 from Caragana intermedia
- Novel Brassica hybrids with different resistance to Leptosphaeria maculans reveal unbalanced rDNA signal patterns
- Application of exogenous auxin and gibberellin regulates the bolting of lettuce (Lactuca sativa L.)
- Phytoremediation of pollutants from wastewater: A concise review
- Genome-wide identification and characterization of NBS-encoding genes in the sweet potato wild ancestor Ipomoea trifida (H.B.K.)
- Alleviative effects of magnetic Fe3O4 nanoparticles on the physiological toxicity of 3-nitrophenol to rice (Oryza sativa L.) seedlings
- Selection and functional identification of Dof genes expressed in response to nitrogen in Populus simonii × Populus nigra
- Study on pecan seed germination influenced by seed endocarp
- Identification of active compounds in Ophiopogonis Radix from different geographical origins by UPLC-Q/TOF-MS combined with GC-MS approaches
- The entire chloroplast genome sequence of Asparagus cochinchinensis and genetic comparison to Asparagus species
- Genome-wide identification of MAPK family genes and their response to abiotic stresses in tea plant (Camellia sinensis)
- Selection and validation of reference genes for RT-qPCR analysis of different organs at various development stages in Caragana intermedia
- Cloning and expression analysis of SERK1 gene in Diospyros lotus
- Integrated metabolomic and transcriptomic profiling revealed coping mechanisms of the edible and medicinal homologous plant Plantago asiatica L. cadmium resistance
- A missense variant in NCF1 is associated with susceptibility to unexplained recurrent spontaneous abortion
- Assessment of drought tolerance indices in faba bean genotypes under different irrigation regimes
- The entire chloroplast genome sequence of Asparagus setaceus (Kunth) Jessop: Genome structure, gene composition, and phylogenetic analysis in Asparagaceae
- Food Science
- Dietary food additive monosodium glutamate with or without high-lipid diet induces spleen anomaly: A mechanistic approach on rat model
- Binge eating disorder during COVID-19
- Potential of honey against the onset of autoimmune diabetes and its associated nephropathy, pancreatitis, and retinopathy in type 1 diabetic animal model
- FTO gene expression in diet-induced obesity is downregulated by Solanum fruit supplementation
- Physical activity enhances fecal lactobacilli in rats chronically drinking sweetened cola beverage
- Supercritical CO2 extraction, chemical composition, and antioxidant effects of Coreopsis tinctoria Nutt. oleoresin
- Functional constituents of plant-based foods boost immunity against acute and chronic disorders
- Effect of selenium and methods of protein extraction on the proteomic profile of Saccharomyces yeast
- Microbial diversity of milk ghee in southern Gansu and its effect on the formation of ghee flavor compounds
- Ecology and Environmental Sciences
- Effects of heavy metals on bacterial community surrounding Bijiashan mining area located in northwest China
- Microorganism community composition analysis coupling with 15N tracer experiments reveals the nitrification rate and N2O emissions in low pH soils in Southern China
- Genetic diversity and population structure of Cinnamomum balansae Lecomte inferred by microsatellites
- Preliminary screening of microplastic contamination in different marine fish species of Taif market, Saudi Arabia
- Plant volatile organic compounds attractive to Lygus pratensis
- Effects of organic materials on soil bacterial community structure in long-term continuous cropping of tomato in greenhouse
- Effects of soil treated fungicide fluopimomide on tomato (Solanum lycopersicum L.) disease control and plant growth
- Prevalence of Yersinia pestis among rodents captured in a semi-arid tropical ecosystem of south-western Zimbabwe
- Effects of irrigation and nitrogen fertilization on mitigating salt-induced Na+ toxicity and sustaining sea rice growth
- Bioengineering and Biotechnology
- Poly-l-lysine-caused cell adhesion induces pyroptosis in THP-1 monocytes
- Development of alkaline phosphatase-scFv and its use for one-step enzyme-linked immunosorbent assay for His-tagged protein detection
- Development and validation of a predictive model for immune-related genes in patients with tongue squamous cell carcinoma
- Agriculture
- Effects of chemical-based fertilizer replacement with biochar-based fertilizer on albic soil nutrient content and maize yield
- Genome-wide identification and expression analysis of CPP-like gene family in Triticum aestivum L. under different hormone and stress conditions
- Agronomic and economic performance of mung bean (Vigna radiata L.) varieties in response to rates of blended NPS fertilizer in Kindo Koysha district, Southern Ethiopia
- Influence of furrow irrigation regime on the yield and water consumption indicators of winter wheat based on a multi-level fuzzy comprehensive evaluation
- Discovery of exercise-related genes and pathway analysis based on comparative genomes of Mongolian originated Abaga and Wushen horse
- Lessons from integrated seasonal forecast-crop modelling in Africa: A systematic review
- Evolution trend of soil fertility in tobacco-planting area of Chenzhou, Hunan Province, China
- Animal Sciences
- Morphological and molecular characterization of Tatera indica Hardwicke 1807 (Rodentia: Muridae) from Pothwar, Pakistan
- Research on meat quality of Qianhua Mutton Merino sheep and Small-tail Han sheep
- SI: A Scientific Memoir
- Suggestions on leading an academic research laboratory group
- My scientific genealogy and the Toronto ACDC Laboratory, 1988–2022
- Erratum
- Erratum to “Changes of immune cells in patients with hepatocellular carcinoma treated by radiofrequency ablation and hepatectomy, a pilot study”
- Erratum to “A two-microRNA signature predicts the progression of male thyroid cancer”
- Retraction
- Retraction of “Lidocaine has antitumor effect on hepatocellular carcinoma via the circ_DYNC1H1/miR-520a-3p/USP14 axis”
Artikel in diesem Heft
- Biomedical Sciences
- Effects of direct oral anticoagulants dabigatran and rivaroxaban on the blood coagulation function in rabbits
- The mother of all battles: Viruses vs humans. Can humans avoid extinction in 50–100 years?
- Knockdown of G1P3 inhibits cell proliferation and enhances the cytotoxicity of dexamethasone in acute lymphoblastic leukemia
- LINC00665 regulates hepatocellular carcinoma by modulating mRNA via the m6A enzyme
- Association study of CLDN14 variations in patients with kidney stones
- Concanavalin A-induced autoimmune hepatitis model in mice: Mechanisms and future outlook
- Regulation of miR-30b in cancer development, apoptosis, and drug resistance
- Informatic analysis of the pulmonary microecology in non-cystic fibrosis bronchiectasis at three different stages
- Swimming attenuates tumor growth in CT-26 tumor-bearing mice and suppresses angiogenesis by mediating the HIF-1α/VEGFA pathway
- Characterization of intestinal microbiota and serum metabolites in patients with mild hepatic encephalopathy
- Functional conservation and divergence in plant-specific GRF gene family revealed by sequences and expression analysis
- Application of the FLP/LoxP-FRT recombination system to switch the eGFP expression in a model prokaryote
- Biomedical evaluation of antioxidant properties of lamb meat enriched with iodine and selenium
- Intravenous infusion of the exosomes derived from human umbilical cord mesenchymal stem cells enhance neurological recovery after traumatic brain injury via suppressing the NF-κB pathway
- Effect of dietary pattern on pregnant women with gestational diabetes mellitus and its clinical significance
- Potential regulatory mechanism of TNF-α/TNFR1/ANXA1 in glioma cells and its role in glioma cell proliferation
- Effect of the genetic mutant G71R in uridine diphosphate-glucuronosyltransferase 1A1 on the conjugation of bilirubin
- Quercetin inhibits cytotoxicity of PC12 cells induced by amyloid-beta 25–35 via stimulating estrogen receptor α, activating ERK1/2, and inhibiting apoptosis
- Nutrition intervention in the management of novel coronavirus pneumonia patients
- circ-CFH promotes the development of HCC by regulating cell proliferation, apoptosis, migration, invasion, and glycolysis through the miR-377-3p/RNF38 axis
- Bmi-1 directly upregulates glucose transporter 1 in human gastric adenocarcinoma
- Lacunar infarction aggravates the cognitive deficit in the elderly with white matter lesion
- Hydroxysafflor yellow A improved retinopathy via Nrf2/HO-1 pathway in rats
- Comparison of axon extension: PTFE versus PLA formed by a 3D printer
- Elevated IL-35 level and iTr35 subset increase the bacterial burden and lung lesions in Mycobacterium tuberculosis-infected mice
- A case report of CAT gene and HNF1β gene variations in a patient with early-onset diabetes
- Study on the mechanism of inhibiting patulin production by fengycin
- SOX4 promotes high-glucose-induced inflammation and angiogenesis of retinal endothelial cells by activating NF-κB signaling pathway
- Relationship between blood clots and COVID-19 vaccines: A literature review
- Analysis of genetic characteristics of 436 children with dysplasia and detailed analysis of rare karyotype
- Bioinformatics network analyses of growth differentiation factor 11
- NR4A1 inhibits the epithelial–mesenchymal transition of hepatic stellate cells: Involvement of TGF-β–Smad2/3/4–ZEB signaling
- Expression of Zeb1 in the differentiation of mouse embryonic stem cell
- Study on the genetic damage caused by cadmium sulfide quantum dots in human lymphocytes
- Association between single-nucleotide polymorphisms of NKX2.5 and congenital heart disease in Chinese population: A meta-analysis
- Assessment of the anesthetic effect of modified pentothal sodium solution on Sprague-Dawley rats
- Genetic susceptibility to high myopia in Han Chinese population
- Potential biomarkers and molecular mechanisms in preeclampsia progression
- Silencing circular RNA-friend leukemia virus integration 1 restrained malignancy of CC cells and oxaliplatin resistance by disturbing dyskeratosis congenita 1
- Endostar plus pembrolizumab combined with a platinum-based dual chemotherapy regime for advanced pulmonary large-cell neuroendocrine carcinoma as a first-line treatment: A case report
- The significance of PAK4 in signaling and clinicopathology: A review
- Sorafenib inhibits ovarian cancer cell proliferation and mobility and induces radiosensitivity by targeting the tumor cell epithelial–mesenchymal transition
- Characterization of rabbit polyclonal antibody against camel recombinant nanobodies
- Active legumain promotes invasion and migration of neuroblastoma by regulating epithelial-mesenchymal transition
- Effect of cell receptors in the pathogenesis of osteoarthritis: Current insights
- MT-12 inhibits the proliferation of bladder cells in vitro and in vivo by enhancing autophagy through mitochondrial dysfunction
- Study of hsa_circRNA_000121 and hsa_circRNA_004183 in papillary thyroid microcarcinoma
- BuyangHuanwu Decoction attenuates cerebral vasospasm caused by subarachnoid hemorrhage in rats via PI3K/AKT/eNOS axis
- Effects of the interaction of Notch and TLR4 pathways on inflammation and heart function in septic heart
- Monosodium iodoacetate-induced subchondral bone microstructure and inflammatory changes in an animal model of osteoarthritis
- A rare presentation of type II Abernethy malformation and nephrotic syndrome: Case report and review
- Rapid death due to pulmonary epithelioid haemangioendothelioma in several weeks: A case report
- Hepatoprotective role of peroxisome proliferator-activated receptor-α in non-cancerous hepatic tissues following transcatheter arterial embolization
- Correlation between peripheral blood lymphocyte subpopulations and primary systemic lupus erythematosus
- A novel SLC8A1-ALK fusion in lung adenocarcinoma confers sensitivity to alectinib: A case report
- β-Hydroxybutyrate upregulates FGF21 expression through inhibition of histone deacetylases in hepatocytes
- Identification of metabolic genes for the prediction of prognosis and tumor microenvironment infiltration in early-stage non-small cell lung cancer
- BTBD10 inhibits glioma tumorigenesis by downregulating cyclin D1 and p-Akt
- Mucormycosis co-infection in COVID-19 patients: An update
- Metagenomic next-generation sequencing in diagnosing Pneumocystis jirovecii pneumonia: A case report
- Long non-coding RNA HOXB-AS1 is a prognostic marker and promotes hepatocellular carcinoma cells’ proliferation and invasion
- Preparation and evaluation of LA-PEG-SPION, a targeted MRI contrast agent for liver cancer
- Proteomic analysis of the liver regulating lipid metabolism in Chaohu ducks using two-dimensional electrophoresis
- Nasopharyngeal tuberculosis: A case report
- Characterization and evaluation of anti-Salmonella enteritidis activity of indigenous probiotic lactobacilli in mice
- Aberrant pulmonary immune response of obese mice to periodontal infection
- Bacteriospermia – A formidable player in male subfertility
- In silico and in vivo analysis of TIPE1 expression in diffuse large B cell lymphoma
- Effects of KCa channels on biological behavior of trophoblasts
- Interleukin-17A influences the vulnerability rather than the size of established atherosclerotic plaques in apolipoprotein E-deficient mice
- Multiple organ failure and death caused by Staphylococcus aureus hip infection: A case report
- Prognostic signature related to the immune environment of oral squamous cell carcinoma
- Primary and metastatic squamous cell carcinoma of the thyroid gland: Two case reports
- Neuroprotective effects of crocin and crocin-loaded niosomes against the paraquat-induced oxidative brain damage in rats
- Role of MMP-2 and CD147 in kidney fibrosis
- Geometric basis of action potential of skeletal muscle cells and neurons
- Babesia microti-induced fulminant sepsis in an immunocompromised host: A case report and the case-specific literature review
- Role of cerebellar cortex in associative learning and memory in guinea pigs
- Application of metagenomic next-generation sequencing technique for diagnosing a specific case of necrotizing meningoencephalitis caused by human herpesvirus 2
- Case report: Quadruple primary malignant neoplasms including esophageal, ureteral, and lung in an elderly male
- Long non-coding RNA NEAT1 promotes angiogenesis in hepatoma carcinoma via the miR-125a-5p/VEGF pathway
- Osteogenic differentiation of periodontal membrane stem cells in inflammatory environments
- Knockdown of SHMT2 enhances the sensitivity of gastric cancer cells to radiotherapy through the Wnt/β-catenin pathway
- Continuous renal replacement therapy combined with double filtration plasmapheresis in the treatment of severe lupus complicated by serious bacterial infections in children: A case report
- Simultaneous triple primary malignancies, including bladder cancer, lymphoma, and lung cancer, in an elderly male: A case report
- Preclinical immunogenicity assessment of a cell-based inactivated whole-virion H5N1 influenza vaccine
- One case of iodine-125 therapy – A new minimally invasive treatment of intrahepatic cholangiocarcinoma
- S1P promotes corneal trigeminal neuron differentiation and corneal nerve repair via upregulating nerve growth factor expression in a mouse model
- Early cancer detection by a targeted methylation assay of circulating tumor DNA in plasma
- Calcifying nanoparticles initiate the calcification process of mesenchymal stem cells in vitro through the activation of the TGF-β1/Smad signaling pathway and promote the decay of echinococcosis
- Evaluation of prognostic markers in patients infected with SARS-CoV-2
- N6-Methyladenosine-related alternative splicing events play a role in bladder cancer
- Characterization of the structural, oxidative, and immunological features of testis tissue from Zucker diabetic fatty rats
- Effects of glucose and osmotic pressure on the proliferation and cell cycle of human chorionic trophoblast cells
- Investigation of genotype diversity of 7,804 norovirus sequences in humans and animals of China
- Characteristics and karyotype analysis of a patient with turner syndrome complicated with multiple-site tumors: A case report
- Aggravated renal fibrosis is positively associated with the activation of HMGB1-TLR2/4 signaling in STZ-induced diabetic mice
- Distribution characteristics of SARS-CoV-2 IgM/IgG in false-positive results detected by chemiluminescent immunoassay
- SRPX2 attenuated oxygen–glucose deprivation and reperfusion-induced injury in cardiomyocytes via alleviating endoplasmic reticulum stress-induced apoptosis through targeting PI3K/Akt/mTOR axis
- Aquaporin-8 overexpression is involved in vascular structure and function changes in placentas of gestational diabetes mellitus patients
- Relationship between CRP gene polymorphisms and ischemic stroke risk: A systematic review and meta-analysis
- Effects of growth hormone on lipid metabolism and sexual development in pubertal obese male rats
- Cloning and identification of the CTLA-4IgV gene and functional application of vaccine in Xinjiang sheep
- Antitumor activity of RUNX3: Upregulation of E-cadherin and downregulation of the epithelial–mesenchymal transition in clear-cell renal cell carcinoma
- PHF8 promotes osteogenic differentiation of BMSCs in old rat with osteoporosis by regulating Wnt/β-catenin pathway
- A review of the current state of the computer-aided diagnosis (CAD) systems for breast cancer diagnosis
- Bilateral dacryoadenitis in adult-onset Still’s disease: A case report
- A novel association between Bmi-1 protein expression and the SUVmax obtained by 18F-FDG PET/CT in patients with gastric adenocarcinoma
- The role of erythrocytes and erythroid progenitor cells in tumors
- Relationship between platelet activation markers and spontaneous abortion: A meta-analysis
- Abnormal methylation caused by folic acid deficiency in neural tube defects
- Silencing TLR4 using an ultrasound-targeted microbubble destruction-based shRNA system reduces ischemia-induced seizures in hyperglycemic rats
- Plant Sciences
- Seasonal succession of bacterial communities in cultured Caulerpa lentillifera detected by high-throughput sequencing
- Cloning and prokaryotic expression of WRKY48 from Caragana intermedia
- Novel Brassica hybrids with different resistance to Leptosphaeria maculans reveal unbalanced rDNA signal patterns
- Application of exogenous auxin and gibberellin regulates the bolting of lettuce (Lactuca sativa L.)
- Phytoremediation of pollutants from wastewater: A concise review
- Genome-wide identification and characterization of NBS-encoding genes in the sweet potato wild ancestor Ipomoea trifida (H.B.K.)
- Alleviative effects of magnetic Fe3O4 nanoparticles on the physiological toxicity of 3-nitrophenol to rice (Oryza sativa L.) seedlings
- Selection and functional identification of Dof genes expressed in response to nitrogen in Populus simonii × Populus nigra
- Study on pecan seed germination influenced by seed endocarp
- Identification of active compounds in Ophiopogonis Radix from different geographical origins by UPLC-Q/TOF-MS combined with GC-MS approaches
- The entire chloroplast genome sequence of Asparagus cochinchinensis and genetic comparison to Asparagus species
- Genome-wide identification of MAPK family genes and their response to abiotic stresses in tea plant (Camellia sinensis)
- Selection and validation of reference genes for RT-qPCR analysis of different organs at various development stages in Caragana intermedia
- Cloning and expression analysis of SERK1 gene in Diospyros lotus
- Integrated metabolomic and transcriptomic profiling revealed coping mechanisms of the edible and medicinal homologous plant Plantago asiatica L. cadmium resistance
- A missense variant in NCF1 is associated with susceptibility to unexplained recurrent spontaneous abortion
- Assessment of drought tolerance indices in faba bean genotypes under different irrigation regimes
- The entire chloroplast genome sequence of Asparagus setaceus (Kunth) Jessop: Genome structure, gene composition, and phylogenetic analysis in Asparagaceae
- Food Science
- Dietary food additive monosodium glutamate with or without high-lipid diet induces spleen anomaly: A mechanistic approach on rat model
- Binge eating disorder during COVID-19
- Potential of honey against the onset of autoimmune diabetes and its associated nephropathy, pancreatitis, and retinopathy in type 1 diabetic animal model
- FTO gene expression in diet-induced obesity is downregulated by Solanum fruit supplementation
- Physical activity enhances fecal lactobacilli in rats chronically drinking sweetened cola beverage
- Supercritical CO2 extraction, chemical composition, and antioxidant effects of Coreopsis tinctoria Nutt. oleoresin
- Functional constituents of plant-based foods boost immunity against acute and chronic disorders
- Effect of selenium and methods of protein extraction on the proteomic profile of Saccharomyces yeast
- Microbial diversity of milk ghee in southern Gansu and its effect on the formation of ghee flavor compounds
- Ecology and Environmental Sciences
- Effects of heavy metals on bacterial community surrounding Bijiashan mining area located in northwest China
- Microorganism community composition analysis coupling with 15N tracer experiments reveals the nitrification rate and N2O emissions in low pH soils in Southern China
- Genetic diversity and population structure of Cinnamomum balansae Lecomte inferred by microsatellites
- Preliminary screening of microplastic contamination in different marine fish species of Taif market, Saudi Arabia
- Plant volatile organic compounds attractive to Lygus pratensis
- Effects of organic materials on soil bacterial community structure in long-term continuous cropping of tomato in greenhouse
- Effects of soil treated fungicide fluopimomide on tomato (Solanum lycopersicum L.) disease control and plant growth
- Prevalence of Yersinia pestis among rodents captured in a semi-arid tropical ecosystem of south-western Zimbabwe
- Effects of irrigation and nitrogen fertilization on mitigating salt-induced Na+ toxicity and sustaining sea rice growth
- Bioengineering and Biotechnology
- Poly-l-lysine-caused cell adhesion induces pyroptosis in THP-1 monocytes
- Development of alkaline phosphatase-scFv and its use for one-step enzyme-linked immunosorbent assay for His-tagged protein detection
- Development and validation of a predictive model for immune-related genes in patients with tongue squamous cell carcinoma
- Agriculture
- Effects of chemical-based fertilizer replacement with biochar-based fertilizer on albic soil nutrient content and maize yield
- Genome-wide identification and expression analysis of CPP-like gene family in Triticum aestivum L. under different hormone and stress conditions
- Agronomic and economic performance of mung bean (Vigna radiata L.) varieties in response to rates of blended NPS fertilizer in Kindo Koysha district, Southern Ethiopia
- Influence of furrow irrigation regime on the yield and water consumption indicators of winter wheat based on a multi-level fuzzy comprehensive evaluation
- Discovery of exercise-related genes and pathway analysis based on comparative genomes of Mongolian originated Abaga and Wushen horse
- Lessons from integrated seasonal forecast-crop modelling in Africa: A systematic review
- Evolution trend of soil fertility in tobacco-planting area of Chenzhou, Hunan Province, China
- Animal Sciences
- Morphological and molecular characterization of Tatera indica Hardwicke 1807 (Rodentia: Muridae) from Pothwar, Pakistan
- Research on meat quality of Qianhua Mutton Merino sheep and Small-tail Han sheep
- SI: A Scientific Memoir
- Suggestions on leading an academic research laboratory group
- My scientific genealogy and the Toronto ACDC Laboratory, 1988–2022
- Erratum
- Erratum to “Changes of immune cells in patients with hepatocellular carcinoma treated by radiofrequency ablation and hepatectomy, a pilot study”
- Erratum to “A two-microRNA signature predicts the progression of male thyroid cancer”
- Retraction
- Retraction of “Lidocaine has antitumor effect on hepatocellular carcinoma via the circ_DYNC1H1/miR-520a-3p/USP14 axis”


