Abstract
Background
Proximal femur fracture surgeries have become increasingly prevalent, presenting unique challenges for postoperative pain management due to patient demographics and comorbidities. Erector spinae plane block (ESPB) has emerged as a relatively safe alternative to paravertebral block (PVB). Our aim was to compare ultrasound-guided continuous ESPB with continuous PVB for postoperative analgesia in patients undergoing proximal femur surgeries under spinal anesthesia.
Methods
A prospective randomized interventional study was conducted on 60 patients between 18 and 60 years of age undergoing proximal femur surgeries under spinal anesthesia with American Society of Anesthesiologists physical status I and II between January 2019 and April 2020. Patients were randomly assigned to receive either ultrasound-guided continuous ESPB (Group E, n = 30) or ultrasound-guided continuous PVB (Group P, n = 30) using a computer-generated randomization table. The mean maximum visual analog scale (VAS) score, VAS score in the first 24 h, the time of rescue analgesia, and total requirement of rescue analgesia were assessed.
Results
The maximum VAS score within the first 24 h was numerically higher in Group P but statistically insignificant (p-value 0.279). VAS scores at 0, 1, 2, 6, and 18 h postoperatively were comparable in both groups. However, at the 24-h mark, the VAS score between Group E and Group P was statistically significant (p-value 0.018) but not clinically relevant. The mean paracetamol and tramadol requirements were comparable between the two groups.
Conclusion
Continuous ESPB is as effective as continuous PVB for postoperative analgesia in proximal femur surgeries. The enhanced safety profile of erector spinae block underscores its significance in postoperative pain management.
1 Introduction
Surgical procedures often result in post-operative pain due to tissue damage and the release of inflammatory mediators. Effective pain management is crucial to minimize detrimental effects on patient outcomes. Hip and proximal femur surgeries, which are common for osteoporosis and trauma-related injuries, particularly affect elderly individuals with a high incidence rate of approximately 129 per 100,000 [1].
The complex nerve supply in the hip region contributes to both superficial and deep pain post-surgery. The hip joint is richly supplied by branches of femoral (L2–4), obturator (L2–4) sciatic nerves, and superior gluteal nerve (L4, L5, and S1) [2]. The skin incision of the posterolateral approach to the hip joint goes through the superior lateral gluteal region and the proximal part of the lateral thigh. This area is innervated by the lateral femoral cutaneous nerve from the lumbar plexus (L2–L3), the lateral cutaneous branch of ilio-hypogastric nerve (T12 and L1), and the subcostal nerve (T12 thoracic nerve) [3].
Given the limitations and complications associated with pharmacological pain relief methods, regional analgesia, including peripheral nerve blocks, is increasingly favored. Recent years have seen a rise in the use of regional analgesic techniques for proximal femur surgeries, with a particular focus on peripheral nerve blocks due to their safety profile [4,5,6]. Paravertebral block (PVB) and erector spinae plane blocks (ESPB) are emerging as promising options in postoperative pain management in proximal femur surgeries. However, there is a paucity of studies comparing the ultrasound-guided continuous PVB and ultrasound-guided continuous ESPB for postoperative analgesia in proximal femur surgeries. In this study, we aimed to address this gap in the literature.
2 Materials and methods
This prospective, randomized comparative study was conducted in a tertiary care hospital in India from January 2019 to April 2020, after receiving Institutional Ethical Committee clearance. The study was registered in the Clinical Trials Registry India (CTRI/2019/03/017975, date: 7/3/2019). The objective was to compare ultrasound-guided continuous ESPB and PVB for postoperative analgesia in patients undergoing proximal femur surgeries. All patients provided written informed consent.
Continuous L2 PVB for postoperative analgesia after direct anterior total hip arthroplasty: a case series was studied by Ardon et al. [7]. The study observed mean maximum pain on postoperative day 0 in PVB was 5.4 ± 3.0. Taking these values as a reference, and assuming a mean difference of 2.5, the minimum required sample size with 80% power of study and 5% level of significance is 23 patients in each study group. To reduce the margin of error, a total sample size of 60 (30 patients per group) was taken. The 15 pilot studies were only done to ascertain the feasibility of the study and the timing and dosage of a block. The study was single blinded due to the resource limitation of the center. The patients remained unaware of the specific block they received. The same anesthesiologist performed the block in all the cases after having performed 20 blocks of each type.
A computer-generated random table system assigned patients to either of the following groups:
Group E (n = 30): ultrasound-guided continuous ESPB.
Group P (n = 30): ultrasound-guided continuous PVB.
Inclusion criteria encompassed patients aged 18–60 years, of any gender, undergoing proximal femur surgeries under spinal anesthesia with American Society of Anesthesiologists (ASA) grades I and II. Exclusion criteria included contraindications to regional anesthesia, known allergies to local anesthetics, bleeding disorders, anticoagulant use, severe kidney or liver disease, lack of proper comprehension due to dementia, and pregnant or lactating females.
All 60 patients underwent thorough pre-anesthetic evaluations and relevant investigations. Patients fasted in accordance with guidelines, and the study’s purpose, advantages, and potential side effects of both techniques were explained to them before obtaining written informed consent. Linear visual analog scale (VAS) for determining the intensity of pain was explained to the patient. Premedication included Tab. Alprazolam 0.25 mg, Tab. Ranitidine 150 mg, and Tab. Metoclopramide 40 mg orally the night before surgery and 2 h prior to surgery.
Upon arrival at operation theatre, standard monitors were attached before giving regional anesthesia. Basal parameters like heart rate (HR), blood pressure (BP) – systolic, diastolic, and mean, oxygen saturation, and electrocardiography were recorded. An intravenous line was secured, and ringer lactate infusion was started. Emergency resuscitation equipment were kept ready.
In Group E (n = 30), patients were positioned in a sitting position with meticulous aseptic measures. The erector spinae muscles were identified, superficial to the tip of L2 transverse process, using a linear ultrasound transducer. Following administration of local anesthesia with 2% lignocaine, an 18-G, 10-cm Touhy’s needle was carefully inserted using an in-plane approach, placing the tip within the fascial plane on the deep (anterior aspect) of erector spinae muscles. Once the needle’s correct placement was confirmed by the visible spread of fluid, gently lifting the erector spinae muscle off the bony shadow of the L2 transverse process, a catheter was threaded through the Touhy’s needle Figure 1.
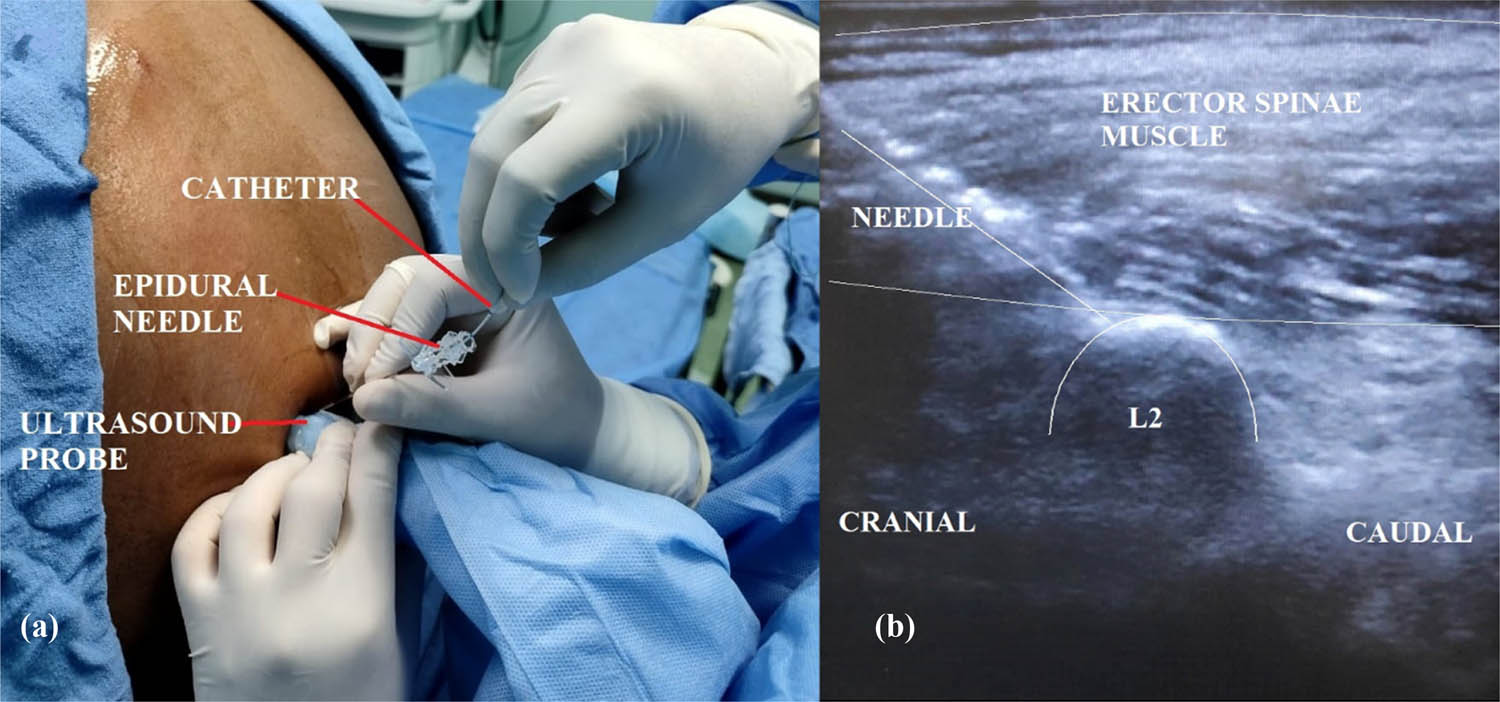
(a) Ultrasound-guided erector spinae block with catheter insertion in a sitting position. (b) Ultrasound image of erector spinae block showing needle, L2 vertebrae, and erector spinae muscle.
For Group P (n = 30), a similar stringent aseptic protocol was followed. Patients were positioned in a sitting position, paravertebral space at L2 vertebrae was located under ultrasound guidance, and 18-G Tuohy’s needle was inserted. After confirming the site using the hydro location technique, a catheter was threaded through the Tuohy’s needle and precisely placed within the paravertebral space Figure 2.
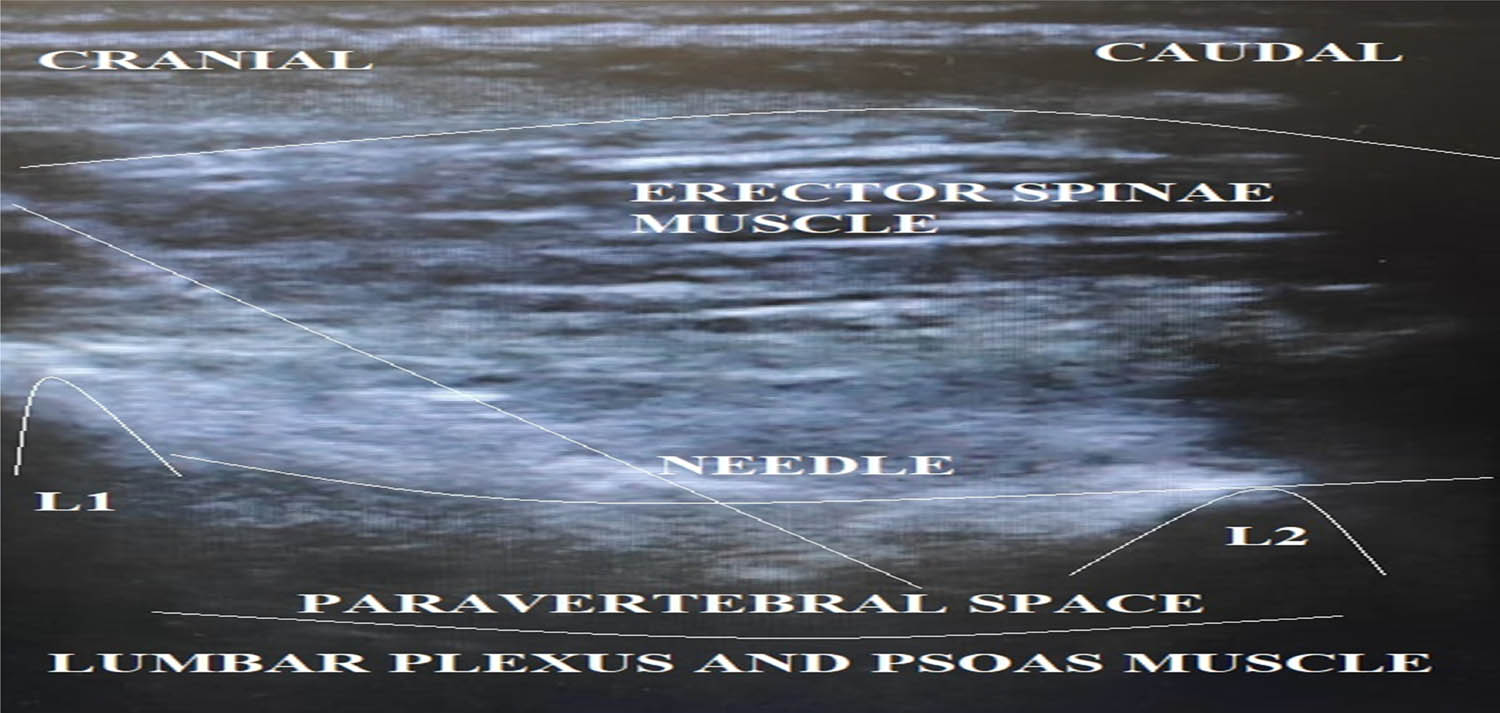
Ultrasound image of PVB showing needle, L1 and L2 vertebrae, and paravertebral space.
Following the catheter placement, patients underwent surgery after receiving a subarachnoid block (SAB) with hyperbaric 0.5% bupivacaine (2.5 ml) and fentanyl (15 µg). The adequacy of SAB was verified by assessing the level of sensory blockade, typically through assessing analgesia to pinprick. Continuous monitoring included recording HR, SPO2, non-invasive BP, blood loss, and urine output. Patients received inhalational oxygen via venturi mask and intravenous fluids tailored to their deficit and body weight, considering blood loss. Any bradycardia was treated with IV atropine sulfate (20 μg/kg), while hypotension was addressed with IV fluid boluses and IV mephentermine. Any other complications were managed following standard operating procedures and documented accordingly.
During surgery, the level of sensory block was continually monitored. When the sensory block receded to the T10 level, 25 ml of 0.5% ropivacaine was administered through the catheter. This was followed by the initiation of a continuous infusion of 0.25% ropivacaine at a rate of 5 ml per hour postoperatively for 24 h in both study groups.
Patients were closely monitored in the recovery room for 2 h before being transferred to the ward. Postoperatively, pain intensity was assessed using the VAS immediately after surgery, at 1, 2, 6, 18, and 24 h post-surgery. Patients received intravenous Paracetamol (1 g) when the VAS score at rest fell within the range of 4–7. If the pain persisted, inj. Tramadol (100 mg IV) was administered. Patient satisfaction was assessed 24 h after surgery.
The primary objective of the study was to compare the mean maximum VAS score. The secondary objective involved comparing VAS scores in both groups during the first 24 h, assessing the time of rescue analgesia, and evaluating the total requirement for rescue analgesics within 24 h.
Data obtained from the study was entered into a Microsoft Excel spreadsheet, and statistical analysis was conducted using appropriate software. Categorical variables were presented in terms of numbers and percentages (%), while continuous variables were expressed as mean ± SD and median. The normality of data was assessed using the Kolmogorov-Smirnov test. When the data sets were found to be non-normally distributed, quantitative variables were compared using an unpaired t-test/Mann–Whitney test. Qualitative variables were compared using the Chi-square test/Fisher’s exact test. A p-value of <0.05 was considered statistically significant.
3 Results
Out of 72 patients approached, 60 were eligible for the final analysis (of 70, 2 declined, 6 were ASA III, 2 patients received general anesthesia and 2 had catheter-related issues) Figure 3.
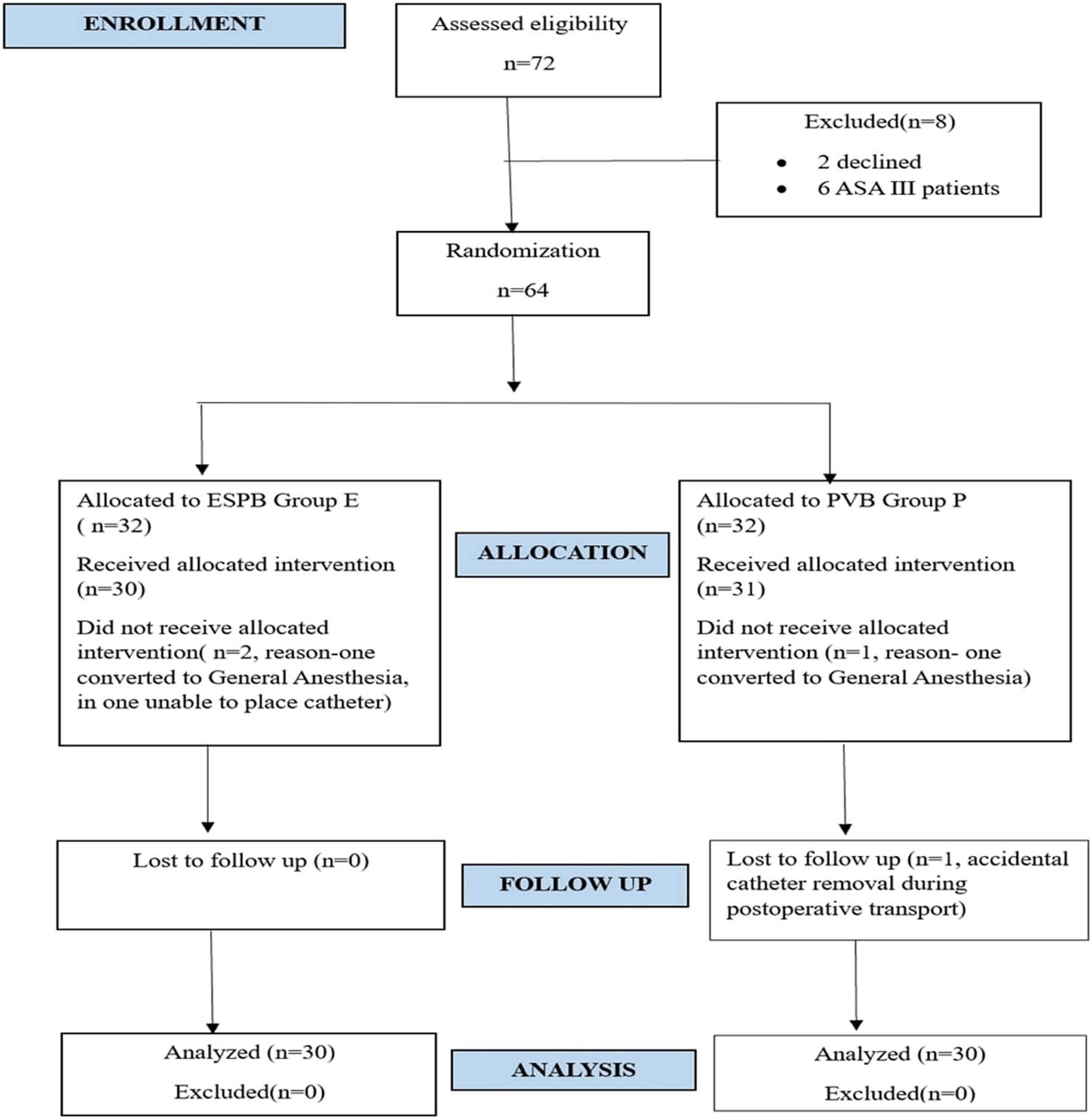
Consort diagram of the study.
The mean age of participants in Group E was 39.63 years, and in Group P was 40.4 years, with both groups consisting of 80% male and 20% female participants. Both groups were comparable with respect to patient demographics and anthropometric parameters (Table 1).
Demographic and anthropometric comparison between Group E and Group P
| Variables | Group E (n = 30) | Group P (n = 30) | p value |
|---|---|---|---|
| Age (years) – mean ± SD | 39.63 ± 12.23 | 40.4 ± 12.14 | 0.716 |
| Gender – male – n% | 80% | 80% | 1 |
| Gender – female – n% | 20% | 20% | 1 |
| Weight (kg) – mean ± SD | 63.7 ± 8.69 | 67.17 ± 6.43 | 0.11 |
| Height (cm) – mean ± SD | 166.63 ± 5.49 | 169.07 ± 5.53 | 0.092 |
| BMI (kg/m2) – mean ± SD | 23.08 ± 3.38 | 23.49 ± 1.79 | 0.568 |
| ASA grade I – n% | 66.67% | 63.33% | 0.787 |
| ASA grade II – n% | 33.33% | 36.67% | 0.787 |
BMI – body mass index; ASA grade – American Society of Anesthesiologists physical status grading.
We included intertrochanteric fracture femur, subtrochanteric fracture femur, and fracture neck of femur in our study (Table 2).
Types of proximal femur surgeries performed in both groups
| Group P | Group E | |
|---|---|---|
| Intertrochanteric fracture femur | 7 | 14 |
| Subtrochanteric fracture femur | 11 | 7 |
| Fracture neck of femur | 12 | 9 |
The different proximal femur surgeries that were performed in both the groups are given in Table 3. In Group P, 15 patients underwent proximal femur nailing (PFN), 11 had cannulated cancellous screw (CCS) fixation, 3 had dynamic hip screw (DHS) fixation, and 1 patient had dynamic condylar screw fixation. In Group E, 19 patients received PFN, 8 had CCS fixation, 1 underwent DHS fixation, 1 had a valgus osteotomy, and 1 had plating.
Different surgeries performed in both groups
| Group P | Group E | |
|---|---|---|
| PFN | 15 | 19 |
| CCS fixation | 11 | 8 |
| DHS fixation | 3 | 1 |
| Valgus osteotomy | 1 | |
| Plating | 1 | |
| DCS fixation | 1 |
PFN – proximal femur nailing; CCS – cannulated cancellous screw; DHS – dynamic hip screw; DCS – dynamic condylar screw.
We did not observe any difference in the efficacy between the two block groups with the different types of surgery performed.
In the majority of patients in both groups, the time between spinal and block (in hours) fell within the 1- to 3-h range, accounting for 76.67% in E and 83.33% in P. For those exceeding 3 h, 23.33% were in Group E, and 16.67% in Group P, showing no significant distinction. The time distribution was normal, allowing for parametric testing. Additionally, there was no significant variation in the mean time between spinal and block for Group E (2.51 ± 0.63) and Group P (2.75 ± 0.77) [p value 0.18, t test]. We did not observe any difference in the time taken to perform the block as it was not our objective.
Mean maximum VAS refers to the mean of the maximum VAS recorded in the 24 h in the particular study group. Apart from this, VAS was also recorded at 0, 1, 2, 6, 18, and 24 h and compared. VAS scores recorded at 0, 1, 2, 6, and 18 h post-surgery exhibited no significant differences between Groups E and P. However, at 24 h, a statistically significant difference in VAS scores emerged (p value 0.018, Mann–Whitney test) (Table 4). Group E exhibited a VAS score of 2.33, while Group P scored 1.77 at the 24-h mark. While statistically significant, we feel that it will not change our treatment practically. The difference may be due to PVB being anatomically closer to the nerve roots. Due to the resource limitation of our center, only static VAS scoring was performed. We recognize the limitation of our study for not being able to compare dynamic VAS scoring.
Comparison of visual analog scale between Groups E and P
| Visual analog scale (h) | Group E (n = 30) mean (SD) | Group P (n = 30) mean (SD) | p value |
|---|---|---|---|
| At 0 | 1.47 (0.68) | 1.33 (0.55) | 0.369 |
| At 1 | 2.4 (0.72) | 2.2 (0.89) | 0.299 |
| At 2 | 2.67 (1.06) | 2.57 (0.94) | 0.797 |
| At 6 | 2.93 (1.41) | 3.03 (1.07) | 0.488 |
| At 18 | 2.77 (0.86) | 2.6 (0.86) | 0.382 |
| At 24 | 2.33 (0.99) | 1.77 (0.68) | 0.018 |
The mean maximum VAS score in the first 24 h for Group E was 4.77 ± 1.33, while for Group P, it was 5.1 ± 0.76, with a total mean of 4.93 ± 1.09. The median VAS scores were identical in both groups, at 5, with interquartile ranges indicating slight variations (4–5 for Group E and 5–5 for Group P). The range of scores spanned from 0 to 7 in Group E and 3 to 7 in Group P, with the overall range being 0 to 7. The Mann–Whitney test yielded a p-value of 0.279, suggesting no statistically significant difference in the mean maximum VAS scores between the two groups.
The time to first analgesia showed no significant difference between Groups E (3.71 h) and P (3.72 h), with a p-value of 0.98 (Mann–Whitney Test). Most patients in both groups required rescue analgesia within 24 h (Group E: 93.33%, Group P: 96.67%). There was no statistical difference in the distribution of rescue analgesia requirements between the groups (p value 1, Fisher exact test).
The mean paracetamol requirement was comparable between both groups (Group E: 1.13 g, Group P: 1.17 g) with no statistical difference (p value 0.814, Mann–Whitney Test). The mean tramadol requirement was also similar (Group E: 86.67 mg, Group P: 96.67 mg) with no significant difference (p value 0.391, Mann–Whitney test). Patient satisfaction was 100% in both groups, and no complications were observed.
4 Discussion
This study marks the first-ever prospective, randomized comparison of ultrasound-guided continuous ESPB with continuous PVB for postoperative analgesia in proximal femur surgeries. The key findings confirm that both techniques are equally effective, which has significant implications for clinical practice and future research in this field.
The introduction of ESPB by Forero et al. [8] in 2016 has introduced a promising technique for postoperative analgesia. Its use for post-operative analgesia for hip surgeries was first demonstrated by Tulgar et al. [9] in 2017. The advantages of ESPB lie in its superficial anatomy, reducing the risk of complications and allowing for straightforward landmark visualization. The non-inferiority of ultrasound-guided continuous ESPB compared to PVB in our study suggests that it can be a safe and effective alternative for patients undergoing proximal femur fracture surgery.
Comparative studies between the ESPB and the PVB have provided valuable insights into their efficacy, safety, and applicability in various surgical contexts. One study by Moorthy et al. [10] concluded that the ESPB provided better overall Quality of Recovery-15 (QoR-15) scores at 24 and 48 h postoperatively compared to the PVB in patients undergoing video-assisted thoracoscopic surgery. However, there were no significant differences between the two techniques in terms of pain levels, opioid consumption, or chronic postsurgical pain at 3 months. Another study by Yang et al. [11] found that bilateral ultrasound-guided ESPB and PVB provided comparable quality of postoperative recovery (QoR-15 scores) in obese patients undergoing laparoscopic sleeve gastrectomy. Additionally, there were no significant differences between the two groups in terms of pain scores, opioid consumption, or other recovery-related outcomes. One meta-analysis by Weng et al. [12] concluded that the ESPB provides superior analgesia compared to systemic analgesics within 24 h after breast surgery. Additionally, ESPB offers similar analgesic effectiveness to the PVB, making it a viable alternative for postoperative pain management in breast surgery. Forero et al. [8] reported that the ESP block could be a suitable alternative to the PVB for abdominal surgeries, providing effective analgesia with a simpler technique and lower risk. These studies suggest that while both blocks are effective, the ESP block might be preferred in certain surgical contexts due to its simplicity and lower risk of complications.
Several studies have compared the ESPB with other blocks in hip surgeries. For instance, Tulgar et al. [13] conducted a prospective feasibility study comparing lumbar erector spinae block and transmuscular quadratus lumborum block for postoperative analgesia in patients undergoing hip and femur operations. They found improved analgesic effects compared to standard intravenous analgesia, though it is important to note that their cases were performed under general anesthesia, unlike our study which utilized spinal anesthesia. Furthermore, they employed single-shot blocks, while our study employed continuous blocks, which may explain the differing requirements for rescue analgesia.
Chen et al. [14] conducted a study comparing continuous lumbar erector spinae block with continuous lumbar plexus block in revision hip arthroplasty and found no significant differences in opioid consumption and pain scores similar to our study. However, our study’s prospective nature and exclusive use of spinal anesthesia distinguish it from Chen et al., s retrospective analysis, which involved varied modes of intraoperative anesthesia and postoperative analgesia plans.
Townsend et al. [15] conducted a randomized controlled study comparing 24-h opioid requirements between lumbar erector spinae block and spinal anesthesia alone for total hip arthroplasty. They found that the erector spinae block reduced opioid utilization in the first 8 h but not beyond. In contrast, our study addressed this limitation by using continuous local anesthetic infusion.
A recent study by Flaviano et al. [16] compared the ESPB and fascia iliaca block after total hip arthroplasty. While the fascia iliaca block exhibited more reliable sensory effects, there was no statistical difference in postoperative opioid requirements. The advantage of the ESPB was evident in preserved quadriceps motor strength postoperatively, particularly beneficial for early patient mobilization.
Surange and Mohan [17] compared continuous PVB with continuous epidural block for postoperative hip surgeries. Both blocks effectively controlled postoperative pain, similar to our findings. Their use of the loss of resistance technique contrasted with our use of ultrasound-guided catheter insertion. Notably, they did not assess postoperative opioid requirements, as our study did.
Wardhan et al. [18] compared continuous L2 PVB with continuous lumbar plexus block for postoperative analgesia in patients undergoing minimal access hip arthroplasty. Their results demonstrated that postoperative pain scores were similar between the two groups, mirroring our findings.
In our study, we performed the blocks under real-time ultrasound guidance. There was no incidence of any block-related complication in our study. However, we cannot comment on the rare complications that may happen as the number of cases performed is less. For this, a large no of cases needs to be performed to uncover the rare complications. We refer to the theoretical benefit that is thought to be the advantage of the ESPB as it has a bony endpoint, preventing deeper structures from any accidental injury and the spread of drug limiting the autonomic response [19].
The primary strength of our study lies in its non-inferiority design, which establishes that continuous lumbar erector spinae block is comparable to continuous PVB in managing postoperative pain in proximal femur surgeries. Our study stands out as the first-ever comparison between these two continuous block techniques using a structured approach to evaluate maximum VAS score, 24-h mean VAS score, and the need for rescue analgesia in both groups.
However, our study has limitations, including the subjective nature of pain perception and the potential variation among patients. The occurrence of postoperative fever in three out of the 60 recruited patients confounded total paracetamol requirements and pain scores. Our study was single-blinded, and the relatively small sample size due to a short recruitment duration may introduce bias. Another limitation of our study is that we did not account for multiplicity, which may explain why the VAS at 24 h showed statistical significance. Variability in the surgical procedures performed could also affect pain requirements
5 Conclusion
Our study demonstrates that continuous ESP block is equally effective in managing postoperative pain in patients undergoing proximal femur fracture surgery compared to PVB. This technique proves to be a safe, easy, and effective addition to our arsenal for postoperative pain management following proximal femur fracture surgery. Further studies are needed to compare the two blocks using standardized surgical techniques and to evaluate the optimal volume and concentration of local anesthetics.
-
Research ethics: Research involving human subjects complied with all relevant national regulations, institutional policies and is in accordance with the tenets of the Helsinki Declaration (as amended in 2013), and has been approved by the authors' Institutional Review Board IEC/VMMC/SJH/Thesis/October/2018-146.
-
Informed consent: Informed consent was obtained from all individuals included in this study, or their legal guardians or wards.
-
Author contributions: The authors have accepted responsibility for the entire content of this manuscript and approved its submission. The individual author contributions are: Aditya Mehrotra – concept, design, definition of intellectual content, literature search, clinical studies, data acquisition and analysis, statistical analysis, manuscript preparation; Madhu Dayal – concept, design, definition of intellectual content, clinical studies, manuscript review; Sushmita Bairagi – guarantor, concept, design, definition of intellectual content, literature search, clinical studies, manuscript preparation, editing and manuscript review.
-
Competing interests: The authors state no conflict of interest.
-
Research funding: None declared.
-
Data availability: The raw data can be obtained on request from the corresponding author.
-
Artificial intelligence/machine learning tools: Not applicable.
References
[1] Dhanwal DK, Siwach R, Dixit V, Mithal A, Jameson K, Cooper C. Incidence of hip fracture in Rohtak district, North India. Arch Osteoporos. 2013;8(0):135. 10.1007/s11657-013-0135-2.Suche in Google Scholar PubMed PubMed Central
[2] Birnbaum K, Prescher A, Hessler S, Heller KD. The sensory innervation of the hip joint – an anatomical study. Surg Radiol Anat. 1997;19(6):371–5. 10.1007/BF01628504.Suche in Google Scholar PubMed
[3] Snell RS. 10 the lower limb. In: Snell RS, Horvath K., editors. Clinical anatomy by regions. 8th edn. Lippincott Williams & Wilkins: Phildelphia; 2008. p. 549–666.Suche in Google Scholar
[4] Modig J, Borg T, Karlström G, Maripuu E, Sahlstedt B. Thromboembolism after total hip replacement: role of epidural and general anesthesia. Anesth Analg. 1983 Feb;62(2):174–80.10.1213/00000539-198302000-00010Suche in Google Scholar
[5] McKenzie PJ, Wishart HY, Gray I, Smith G. Effects of anaesthetic technique on deep vein thrombosis. A comparison of subarachnoid and general anaesthesia. Br J Anaesth. 1985 Sep;57(9):853–7. 10.1093/bja/57.9.853.Suche in Google Scholar PubMed
[6] Mingus ML. Recovery advantages of regional anesthesia compared with general anesthesia: adult patients. J Clin Anesth. 1995 Nov;7(7):628–33. 10.1016/0952-8180(95)00157-3.Suche in Google Scholar PubMed
[7] Ardon AE, Reed RR, McClain RL, Kalava A, Lee J, Redmond J, et al. Continuous L2 paravertebral block for postoperative analgesia after direct anterior total hip arthroplasty: a case series. J Anesth. 2017;24:35–42.Suche in Google Scholar
[8] Forero M, Adhikary SD, Lopez H, Tsui C, Chin KJ. The erector spinae plane block: a novel analgesic technique in thoracic neuropathic pain. Reg Anesth Pain Med. 2016 Sep-Oct;41(5):621–7. 10.1097/AAP.0000000000000451.Suche in Google Scholar PubMed
[9] Tulgar S, Senturk O. Ultrasound guided erector spinae plane block at L-4 transverse process level provides effective postoperative analgesia for total hip arthroplasty. J Clin Anesth. 2018 Feb;44:68. 10.1016/j.jclinane.2017.11.006.Suche in Google Scholar PubMed
[10] Moorthy A, Ní Eochagáin A, Dempsey E, Wall V, Marsh H, Murphy T, et al. Postoperative recovery with continuous erector spinae plane block or video-assisted paravertebral block after minimally invasive thoracic surgery: a prospective, randomised controlled trial. Br J Anaesth. 2023 Jan;130(1):e137–47. 10.1016/j.bja.2022.07.051.Suche in Google Scholar PubMed
[11] Yang G, Wang P, Yin Y, Qu H, Zhao X, Jin X, et al. Erector spinae plane block versus paravertebral block on postoperative quality of recovery in obese patients undergoing laparoscopic sleeve gastrectomy: a randomized controlled trial. PeerJ. 2024;12:e17431. 10.7717/peerj.17431.Suche in Google Scholar PubMed PubMed Central
[12] Weng WT, Wang CJ, Li CY, Wen HW, Liu YC. Erector spinae plane block similar to paravertebral block for perioperative pain control in breast surgery: a meta-analysis study. Pain Physician. 2021 May;24(3):203–13.10.36076/ppj.2021/24/203Suche in Google Scholar
[13] Tulgar S, Kose HC, Selvi O, Senturk O, Thomas DT, Ermis MN, et al. Comparison of ultrasound-guided lumbar erector spinae plane block and transmuscular quadratus lumborum block for postoperative analgesia in hip and proximal femur surgery: a prospective randomized feasibility study. Anesth Essays Res. 2018 Oct–Dec;12(4):825–31. 10.4103/aer.AER_142_18.Suche in Google Scholar PubMed PubMed Central
[14] Chen A, Kolodzie K, Schultz A, Hansen EN, Braehler M. Continuous lumbar plexus block vs continuous lumbar erector spinae plane block for postoperative pain control after revision total hip arthroplasty. Arthroplast Today. 2021 Apr;9:29–34. 10.1016/j.artd.2021.03.016.Suche in Google Scholar PubMed PubMed Central
[15] Townsend D, Siddique N, Kimura A, Chein Y, Kamara E, Pope J, et al. Lumbar erector spinae plane block for total hip arthroplasty comparing 24-hour opioid requirements: a randomized controlled study. Anesthesiol Res Pract. 2022 Oct;2022:9826638. 10.1155/2022/9826638.Suche in Google Scholar PubMed PubMed Central
[16] Flaviano E, Bettinelli S, Assandri M, Muhammad H, Benigni A, Cappelleri G, et al. Erector spinae plane versus fascia iliaca block after total hip arthroplasty: a randomized clinical trial comparing analgesic effectiveness and motor block. Korean J Anesthesiol. 2023 Aug;76(4):326–35. 10.4097/kja.22669.Suche in Google Scholar PubMed PubMed Central
[17] Surange PN, Mohan CVR. Comparative evaluation of continuous lumbar paravertebral versus continuous epidural block for post-operative pain relief in hip surgeries. Anesth Pain Med. 2012;1(3):178–83. 10.5812/kowsar.22287523.3348.Suche in Google Scholar PubMed PubMed Central
[18] Wardhan R, Auroux AS, Ben-David B, Chelly JE. Is L2 paravertebral block comparable to lumbar plexus block for postoperative analgesia after total hip arthroplasty? Clin Orthop Relat Res. 2014 May;472(5):1475–81. 10.1007/s11999-013-3393-9.Suche in Google Scholar PubMed PubMed Central
[19] El-Boghdadly K, Pawa A. The erector spinae plane block: plane and simple. Anaesthesia. 2017 Apr;72(4):434–8. 10.1111/anae.13830.Suche in Google Scholar PubMed
© 2024 the author(s), published by De Gruyter
This work is licensed under the Creative Commons Attribution 4.0 International License.
Artikel in diesem Heft
- Editorial Comment
- From pain to relief: Exploring the consistency of exercise-induced hypoalgesia
- Christmas greetings 2024 from the Editor-in-Chief
- Original Articles
- The Scandinavian Society for the Study of Pain 2022 Postgraduate Course and Annual Scientific (SASP 2022) Meeting 12th to 14th October at Rigshospitalet, Copenhagen
- Comparison of ultrasound-guided continuous erector spinae plane block versus continuous paravertebral block for postoperative analgesia in patients undergoing proximal femur surgeries
- Clinical Pain Researches
- The effect of tourniquet use on postoperative opioid consumption after ankle fracture surgery – a retrospective cohort study
- Changes in pain, daily occupations, lifestyle, and health following an occupational therapy lifestyle intervention: a secondary analysis from a feasibility study in patients with chronic high-impact pain
- Tonic cuff pressure pain sensitivity in chronic pain patients and its relation to self-reported physical activity
- Reliability, construct validity, and factorial structure of a Swedish version of the medical outcomes study social support survey (MOS-SSS) in patients with chronic pain
- Hurdles and potentials when implementing internet-delivered Acceptance and commitment therapy for chronic pain: a retrospective appraisal using the Quality implementation framework
- Exploring the outcome “days with bothersome pain” and its association with pain intensity, disability, and quality of life
- Fatigue and cognitive fatigability in patients with chronic pain
- The Swedish version of the pain self-efficacy questionnaire short form, PSEQ-2SV: Cultural adaptation and psychometric evaluation in a population of patients with musculoskeletal disorders
- Pain coping and catastrophizing in youth with and without cerebral palsy
- Neuropathic pain after surgery – A clinical validation study and assessment of accuracy measures of the 5-item NeuPPS scale
- Translation, contextual adaptation, and reliability of the Danish Concept of Pain Inventory (COPI-Adult (DK)) – A self-reported outcome measure
- Cosmetic surgery and associated chronic postsurgical pain: A cross-sectional study from Norway
- The association of hemodynamic parameters and clinical demographic variables with acute postoperative pain in female oncological breast surgery patients: A retrospective cohort study
- Healthcare professionals’ experiences of interdisciplinary collaboration in pain centres – A qualitative study
- Effects of deep brain stimulation and verbal suggestions on pain in Parkinson’s disease
- Painful differences between different pain scale assessments: The outcome of assessed pain is a matter of the choices of scale and statistics
- Prevalence and characteristics of fibromyalgia according to three fibromyalgia diagnostic criteria: A secondary analysis study
- Sex moderates the association between quantitative sensory testing and acute and chronic pain after total knee/hip arthroplasty
- Tramadol-paracetamol for postoperative pain after spine surgery – A randomized, double-blind, placebo-controlled study
- Cancer-related pain experienced in daily life is difficult to communicate and to manage – for patients and for professionals
- Making sense of pain in inflammatory bowel disease (IBD): A qualitative study
- Patient-reported pain, satisfaction, adverse effects, and deviations from ambulatory surgery pain medication
- Does pain influence cognitive performance in patients with mild traumatic brain injury?
- Hypocapnia in women with fibromyalgia
- Application of ultrasound-guided thoracic paravertebral block or intercostal nerve block for acute herpes zoster and prevention of post-herpetic neuralgia: A case–control retrospective trial
- Translation and examination of construct validity of the Danish version of the Tampa Scale for Kinesiophobia
- A positive scratch collapse test in anterior cutaneous nerve entrapment syndrome indicates its neuropathic character
- ADHD-pain: Characteristics of chronic pain and association with muscular dysregulation in adults with ADHD
- The relationship between changes in pain intensity and functional disability in persistent disabling low back pain during a course of cognitive functional therapy
- Intrathecal pain treatment for severe pain in patients with terminal cancer: A retrospective analysis of treatment-related complications and side effects
- Psychometric evaluation of the Danish version of the Pain Self-Efficacy Questionnaire in patients with subacute and chronic low back pain
- Dimensionality, reliability, and validity of the Finnish version of the pain catastrophizing scale in chronic low back pain
- To speak or not to speak? A secondary data analysis to further explore the context-insensitive avoidance scale
- Pain catastrophizing levels differentiate between common diseases with pain: HIV, fibromyalgia, complex regional pain syndrome, and breast cancer survivors
- Prevalence of substance use disorder diagnoses in patients with chronic pain receiving reimbursed opioids: An epidemiological study of four Norwegian health registries
- Pain perception while listening to thrash heavy metal vs relaxing music at a heavy metal festival – the CoPainHell study – a factorial randomized non-blinded crossover trial
- Observational Studies
- Cutaneous nerve biopsy in patients with symptoms of small fiber neuropathy: a retrospective study
- The incidence of post cholecystectomy pain (PCP) syndrome at 12 months following laparoscopic cholecystectomy: a prospective evaluation in 200 patients
- Associations between psychological flexibility and daily functioning in endometriosis-related pain
- Relationship between perfectionism, overactivity, pain severity, and pain interference in individuals with chronic pain: A cross-lagged panel model analysis
- Access to psychological treatment for chronic cancer-related pain in Sweden
- Validation of the Danish version of the knowledge and attitudes survey regarding pain
- Associations between cognitive test scores and pain tolerance: The Tromsø study
- Healthcare experiences of fibromyalgia patients and their associations with satisfaction and pain relief. A patient survey
- Video interpretation in a medical spine clinic: A descriptive study of a diverse population and intervention
- Role of history of traumatic life experiences in current psychosomatic manifestations
- Social determinants of health in adults with whiplash associated disorders
- Which patients with chronic low back pain respond favorably to multidisciplinary rehabilitation? A secondary analysis of a randomized controlled trial
- A preliminary examination of the effects of childhood abuse and resilience on pain and physical functioning in patients with knee osteoarthritis
- Differences in risk factors for flare-ups in patients with lumbar radicular pain may depend on the definition of flare
- Real-world evidence evaluation on consumer experience and prescription journey of diclofenac gel in Sweden
- Patient characteristics in relation to opioid exposure in a chronic non-cancer pain population
- Topical Reviews
- Bridging the translational gap: adenosine as a modulator of neuropathic pain in preclinical models and humans
- What do we know about Indigenous Peoples with low back pain around the world? A topical review
- The “future” pain clinician: Competencies needed to provide psychologically informed care
- Systematic Reviews
- Pain management for persistent pain post radiotherapy in head and neck cancers: systematic review
- High-frequency, high-intensity transcutaneous electrical nerve stimulation compared with opioids for pain relief after gynecological surgery: a systematic review and meta-analysis
- Reliability and measurement error of exercise-induced hypoalgesia in pain-free adults and adults with musculoskeletal pain: A systematic review
- Noninvasive transcranial brain stimulation in central post-stroke pain: A systematic review
- Short Communications
- Are we missing the opioid consumption in low- and middle-income countries?
- Association between self-reported pain severity and characteristics of United States adults (age ≥50 years) who used opioids
- Could generative artificial intelligence replace fieldwork in pain research?
- Skin conductance algesimeter is unreliable during sudden perioperative temperature increases
- Original Experimental
- Confirmatory study of the usefulness of quantum molecular resonance and microdissectomy for the treatment of lumbar radiculopathy in a prospective cohort at 6 months follow-up
- Pain catastrophizing in the elderly: An experimental pain study
- Improving general practice management of patients with chronic musculoskeletal pain: Interdisciplinarity, coherence, and concerns
- Concurrent validity of dynamic bedside quantitative sensory testing paradigms in breast cancer survivors with persistent pain
- Transcranial direct current stimulation is more effective than pregabalin in controlling nociceptive and anxiety-like behaviors in a rat fibromyalgia-like model
- Paradox pain sensitivity using cuff pressure or algometer testing in patients with hemophilia
- Physical activity with person-centered guidance supported by a digital platform or with telephone follow-up for persons with chronic widespread pain: Health economic considerations along a randomized controlled trial
- Measuring pain intensity through physical interaction in an experimental model of cold-induced pain: A method comparison study
- Pharmacological treatment of pain in Swedish nursing homes: Prevalence and associations with cognitive impairment and depressive mood
- Neck and shoulder pain and inflammatory biomarkers in plasma among forklift truck operators – A case–control study
- The effect of social exclusion on pain perception and heart rate variability in healthy controls and somatoform pain patients
- Revisiting opioid toxicity: Cellular effects of six commonly used opioids
- Letter to the Editor
- Post cholecystectomy pain syndrome: Letter to Editor
- Response to the Letter by Prof Bordoni
- Response – Reliability and measurement error of exercise-induced hypoalgesia
- Is the skin conductance algesimeter index influenced by temperature?
- Skin conductance algesimeter is unreliable during sudden perioperative temperature increase
- Corrigendum
- Corrigendum to “Chronic post-thoracotomy pain after lung cancer surgery: a prospective study of preoperative risk factors”
- Obituary
- A Significant Voice in Pain Research Björn Gerdle in Memoriam (1953–2024)
Artikel in diesem Heft
- Editorial Comment
- From pain to relief: Exploring the consistency of exercise-induced hypoalgesia
- Christmas greetings 2024 from the Editor-in-Chief
- Original Articles
- The Scandinavian Society for the Study of Pain 2022 Postgraduate Course and Annual Scientific (SASP 2022) Meeting 12th to 14th October at Rigshospitalet, Copenhagen
- Comparison of ultrasound-guided continuous erector spinae plane block versus continuous paravertebral block for postoperative analgesia in patients undergoing proximal femur surgeries
- Clinical Pain Researches
- The effect of tourniquet use on postoperative opioid consumption after ankle fracture surgery – a retrospective cohort study
- Changes in pain, daily occupations, lifestyle, and health following an occupational therapy lifestyle intervention: a secondary analysis from a feasibility study in patients with chronic high-impact pain
- Tonic cuff pressure pain sensitivity in chronic pain patients and its relation to self-reported physical activity
- Reliability, construct validity, and factorial structure of a Swedish version of the medical outcomes study social support survey (MOS-SSS) in patients with chronic pain
- Hurdles and potentials when implementing internet-delivered Acceptance and commitment therapy for chronic pain: a retrospective appraisal using the Quality implementation framework
- Exploring the outcome “days with bothersome pain” and its association with pain intensity, disability, and quality of life
- Fatigue and cognitive fatigability in patients with chronic pain
- The Swedish version of the pain self-efficacy questionnaire short form, PSEQ-2SV: Cultural adaptation and psychometric evaluation in a population of patients with musculoskeletal disorders
- Pain coping and catastrophizing in youth with and without cerebral palsy
- Neuropathic pain after surgery – A clinical validation study and assessment of accuracy measures of the 5-item NeuPPS scale
- Translation, contextual adaptation, and reliability of the Danish Concept of Pain Inventory (COPI-Adult (DK)) – A self-reported outcome measure
- Cosmetic surgery and associated chronic postsurgical pain: A cross-sectional study from Norway
- The association of hemodynamic parameters and clinical demographic variables with acute postoperative pain in female oncological breast surgery patients: A retrospective cohort study
- Healthcare professionals’ experiences of interdisciplinary collaboration in pain centres – A qualitative study
- Effects of deep brain stimulation and verbal suggestions on pain in Parkinson’s disease
- Painful differences between different pain scale assessments: The outcome of assessed pain is a matter of the choices of scale and statistics
- Prevalence and characteristics of fibromyalgia according to three fibromyalgia diagnostic criteria: A secondary analysis study
- Sex moderates the association between quantitative sensory testing and acute and chronic pain after total knee/hip arthroplasty
- Tramadol-paracetamol for postoperative pain after spine surgery – A randomized, double-blind, placebo-controlled study
- Cancer-related pain experienced in daily life is difficult to communicate and to manage – for patients and for professionals
- Making sense of pain in inflammatory bowel disease (IBD): A qualitative study
- Patient-reported pain, satisfaction, adverse effects, and deviations from ambulatory surgery pain medication
- Does pain influence cognitive performance in patients with mild traumatic brain injury?
- Hypocapnia in women with fibromyalgia
- Application of ultrasound-guided thoracic paravertebral block or intercostal nerve block for acute herpes zoster and prevention of post-herpetic neuralgia: A case–control retrospective trial
- Translation and examination of construct validity of the Danish version of the Tampa Scale for Kinesiophobia
- A positive scratch collapse test in anterior cutaneous nerve entrapment syndrome indicates its neuropathic character
- ADHD-pain: Characteristics of chronic pain and association with muscular dysregulation in adults with ADHD
- The relationship between changes in pain intensity and functional disability in persistent disabling low back pain during a course of cognitive functional therapy
- Intrathecal pain treatment for severe pain in patients with terminal cancer: A retrospective analysis of treatment-related complications and side effects
- Psychometric evaluation of the Danish version of the Pain Self-Efficacy Questionnaire in patients with subacute and chronic low back pain
- Dimensionality, reliability, and validity of the Finnish version of the pain catastrophizing scale in chronic low back pain
- To speak or not to speak? A secondary data analysis to further explore the context-insensitive avoidance scale
- Pain catastrophizing levels differentiate between common diseases with pain: HIV, fibromyalgia, complex regional pain syndrome, and breast cancer survivors
- Prevalence of substance use disorder diagnoses in patients with chronic pain receiving reimbursed opioids: An epidemiological study of four Norwegian health registries
- Pain perception while listening to thrash heavy metal vs relaxing music at a heavy metal festival – the CoPainHell study – a factorial randomized non-blinded crossover trial
- Observational Studies
- Cutaneous nerve biopsy in patients with symptoms of small fiber neuropathy: a retrospective study
- The incidence of post cholecystectomy pain (PCP) syndrome at 12 months following laparoscopic cholecystectomy: a prospective evaluation in 200 patients
- Associations between psychological flexibility and daily functioning in endometriosis-related pain
- Relationship between perfectionism, overactivity, pain severity, and pain interference in individuals with chronic pain: A cross-lagged panel model analysis
- Access to psychological treatment for chronic cancer-related pain in Sweden
- Validation of the Danish version of the knowledge and attitudes survey regarding pain
- Associations between cognitive test scores and pain tolerance: The Tromsø study
- Healthcare experiences of fibromyalgia patients and their associations with satisfaction and pain relief. A patient survey
- Video interpretation in a medical spine clinic: A descriptive study of a diverse population and intervention
- Role of history of traumatic life experiences in current psychosomatic manifestations
- Social determinants of health in adults with whiplash associated disorders
- Which patients with chronic low back pain respond favorably to multidisciplinary rehabilitation? A secondary analysis of a randomized controlled trial
- A preliminary examination of the effects of childhood abuse and resilience on pain and physical functioning in patients with knee osteoarthritis
- Differences in risk factors for flare-ups in patients with lumbar radicular pain may depend on the definition of flare
- Real-world evidence evaluation on consumer experience and prescription journey of diclofenac gel in Sweden
- Patient characteristics in relation to opioid exposure in a chronic non-cancer pain population
- Topical Reviews
- Bridging the translational gap: adenosine as a modulator of neuropathic pain in preclinical models and humans
- What do we know about Indigenous Peoples with low back pain around the world? A topical review
- The “future” pain clinician: Competencies needed to provide psychologically informed care
- Systematic Reviews
- Pain management for persistent pain post radiotherapy in head and neck cancers: systematic review
- High-frequency, high-intensity transcutaneous electrical nerve stimulation compared with opioids for pain relief after gynecological surgery: a systematic review and meta-analysis
- Reliability and measurement error of exercise-induced hypoalgesia in pain-free adults and adults with musculoskeletal pain: A systematic review
- Noninvasive transcranial brain stimulation in central post-stroke pain: A systematic review
- Short Communications
- Are we missing the opioid consumption in low- and middle-income countries?
- Association between self-reported pain severity and characteristics of United States adults (age ≥50 years) who used opioids
- Could generative artificial intelligence replace fieldwork in pain research?
- Skin conductance algesimeter is unreliable during sudden perioperative temperature increases
- Original Experimental
- Confirmatory study of the usefulness of quantum molecular resonance and microdissectomy for the treatment of lumbar radiculopathy in a prospective cohort at 6 months follow-up
- Pain catastrophizing in the elderly: An experimental pain study
- Improving general practice management of patients with chronic musculoskeletal pain: Interdisciplinarity, coherence, and concerns
- Concurrent validity of dynamic bedside quantitative sensory testing paradigms in breast cancer survivors with persistent pain
- Transcranial direct current stimulation is more effective than pregabalin in controlling nociceptive and anxiety-like behaviors in a rat fibromyalgia-like model
- Paradox pain sensitivity using cuff pressure or algometer testing in patients with hemophilia
- Physical activity with person-centered guidance supported by a digital platform or with telephone follow-up for persons with chronic widespread pain: Health economic considerations along a randomized controlled trial
- Measuring pain intensity through physical interaction in an experimental model of cold-induced pain: A method comparison study
- Pharmacological treatment of pain in Swedish nursing homes: Prevalence and associations with cognitive impairment and depressive mood
- Neck and shoulder pain and inflammatory biomarkers in plasma among forklift truck operators – A case–control study
- The effect of social exclusion on pain perception and heart rate variability in healthy controls and somatoform pain patients
- Revisiting opioid toxicity: Cellular effects of six commonly used opioids
- Letter to the Editor
- Post cholecystectomy pain syndrome: Letter to Editor
- Response to the Letter by Prof Bordoni
- Response – Reliability and measurement error of exercise-induced hypoalgesia
- Is the skin conductance algesimeter index influenced by temperature?
- Skin conductance algesimeter is unreliable during sudden perioperative temperature increase
- Corrigendum
- Corrigendum to “Chronic post-thoracotomy pain after lung cancer surgery: a prospective study of preoperative risk factors”
- Obituary
- A Significant Voice in Pain Research Björn Gerdle in Memoriam (1953–2024)


