Abstract
Objectives
Although the relationship between traumatic experiences (TEs) and psychosomatic manifestations (pain, somatization, somatosensory amplification [SSA], and alexithymia) has been widely described, very few studies have investigated how these variables correlate with each other and with a history of TEs. The aim of this study was to investigate whether and how current psychosomatic manifestations are correlated with major and minor adult- and childhood TEs.
Methods
One hundred and forty-six patients (91 with pain) from the Pisa Gift Institute for Integrative Medicine Psychosomatics Lab., Italy, were assessed for pain, history of TEs (divided into major and minor based on whether or not they meet the DSM-5 Criterion A for post-traumatic stress disorder), alexithymia, somatization, and SSA.
Results
TEs were positively correlated with age, the sensorial dimension and intensity of pain, somatization, psychopathology index, SSA, and alexithymia. Using the somatization score (controlled for age) as a covariate, the previous correlations between psychosomatic dimensions and TEs lost their statistical significance: SSA (total TEs: from r = 0.30, p = 0.000 to r = −0.04, p = 0.652); alexithymia (total TEs: from r = 0.28, p = 0.001 to r = 0.04, p = 0.663); sensorial dimension of pain (total TEs: from r = 0.30, p = 0.015 to r = 0.12, p = 0.373); and pain intensity (total TEs: from r = 0.38, p = 0.004 to r = −0.15, p = 0.317). Interestingly, the tendency to report more intense pain was mainly predicted by minor TEs in childhood (β = 0.28; p = 0.030).
Conclusions
The number of lifetime TEs is positively correlated with the sensorial dimension and intensity of pain but not its affective and cognitive dimensions. However, the former relationship depends on the presence of somatization. The intensity of pain is associated with minor rather than major TEs, especially when they occur in childhood.
1 Introduction
According to the recent WHO World Mental Health survey, the prevalence of traumatic experiences (TEs), defined as self-reported exposure to stressful events, is estimated to be 82.7% in the United States and 69.7% across all participating countries, with 30.5% of adults having experienced almost four TEs [1]. TEs can lead to the development of post-traumatic stress disorder (PTSD) and other mental disorders, including anxiety, depression, and substance-use disorders [2]. A single TE exposure is also linked to an increased risk of physical diseases like chronic pain, which further increases as more TEs are experienced [3].
For the purposes of diagnosing PTSD, TEs included in the DSM-5 Criterion A are by definition “major,” involving “death, threatened death, actual or threatened serious injury, or actual or threatened sexual violence” [4]. To this might be added life-altering events such as involuntary separation from/as a child. Due to the severity of their impact, major TEs are those most explored in the pain literature [5], but other TEs should not be overlooked [6]. To this end, Giannantonio proposed a systematization of traumas, which includes a group of minor traumas (adoption, divorce, economic problems, physical/emotional neglect, miscarriage, non-sudden death, observations of a sexual nature), distinguishing between TEs that occurred in childhood (before the age of 18) and adulthood [7]. Such a system would be useful in clearing some of the confusion in the classification of trauma in the literature. For example, in a study by Haviland et al. highlighting the relationship between assault/sexual abuse and fibromyalgia, emotional neglect (which had no relationship with fibromyalgia) was included in the major trauma group [8], despite it being absent from DSM-5 Criterion A. As mentioned, Giannantonio classed emotional neglect as a minor trauma [7]. This lack of clarity may have a detrimental impact on psychological research in general. For example, although the relationship between somatization and TEs has been widely described in the scientific literature [9,10,11,12], how somatization is related to major versus minor trauma, and to what extent, currently remains uncertain.
In line with Lipowski, for this study, we defined somatization as the tendency to experience and communicate psychological distress in the form of somatic symptoms and to seek medical help for them [13]. The tendency to experience intense, noxious, and disturbing somatic sensations (somatosensory amplification [SSA]) [14] and alexithymia (the difficulty in identifying and distinguishing between feelings and bodily sensations, difficulty in describing feelings, and outward-oriented thinking) [15] appear to be two of the most influential factors on the process of somatization [16], the former enhancing somatization symptoms and the latter contributing to its cognitive dimension, attributing negative implications to normal somatic sensations [16].
According to the literature, the level of SSA (measured using the somatosensory amplification scale [SSAS]) is increased in fibromyalgia [17], and high SSA is associated with a low pressure-pain threshold in healthy individuals [18]. It also seems to be associated with oral hypervigilance and oral behaviours that predispose an individual to temporomandibular disorders [19]. It has also been shown, using a questionnaire investigating major TEs, that subjects with somatoform disorders report a greater number of TEs than healthy controls, and that there is a positive correlation between major TEs and SSA [12].
As for the aetiopathogenesis of fibromyalgia, TEs (such as physical or sexual violence) are widely considered to be involved, even though the only available evidence comes from case series or reports, and the results to date have been inconsistent [20]. Similarly, emotional and physical abuse in childhood and an unsupportive family have been implicated in the relationship between somatization and TEs [21], and somatization features may stem from intergenerational transmission of maternal PTSD [22]. In contrast, the relationship between TEs and somatization appears to be little affected by the presence of alexithymia [22], which, instead, is observed more clearly in the relationship between trauma and conversion disorder [23,24]. The relationship between TEs and psychosomatic manifestations such as SSA and alexithymia has also been widely described [12,25], but very few studies have investigated how these variables interact with each other and how this relationship relates to a history of TEs [26,24].
Although several studies support a relationship between TEs and somatic symptoms, there are few that have provided significant evidence on the types of TEs that affect the distortion of body perception. Hence, the aim of this study was to investigate whether and how current psychosomatic manifestations, i.e. somatization, pain, SSA, and alexithymia, are correlated with major and minor adult- and childhood TEs.
2 Methods
2.1 Participants
This study is based on retrospective data from 146 patients seeking assessment and treatment for psychological suffering collected at the Pisa Gift Institute for Integrative Medicine Psychosomatics Lab., Italy, between 2021 and 2023. The total sample was divided into pain (91 patients) and pain-free (55 patients). The group with pain was distinguished from the group without pain based on the presence/absence of pain, investigated through relevant screening questions on a case report form (CRF), including “Have you had pain in the last 2 years?” and through the Italian Pain Questionnaire (IPQ) [27]. All patients were identified as alphanumeric codes in the stored data to guarantee their anonymity, and all signed informed consent. This was an observational study conducted in accordance with the Ethical Principles for Medical Research Involving Human Subjects outlined in the Helsinki Declaration. This article adheres to the STROBE statement guidelines for reporting observational research [28].
2.2 Measures
2.2.1 Sociodemographic variables
Data on patients’ age, gender, education, and civil and social status (based on monthly income), as well as general information on their pain (time of onset, persistence, location, and temporal trend), were collected for each patient on a CRF.
2.2.2 Pain
The IPQ [27], the Italian adaptation of the McGill Pain Questionnaire [29], is a self-report questionnaire consisting of 42 pain descriptors distributed across 16 subclasses under the following four main classes or dimensions: sensory (the sensory qualities of pain), affective (unpleasantness of pain experience), evaluative (pain intensity and subjective evaluation of pain experience), and mixed (the mixed sensory, affective and evaluative aspects of pain). In our study, IPQ dimensions were calculated on the basis of the PRIrc (pain rating index rank coefficient) ordinal coefficient score between 0 and 1. Scores for each dimension: sensorial (PRIrcS), affective (PRIrcA), evaluative (PRIrcE), and mixed (PRIrcM) were calculated, as was the total (PRIrcT, the sum of all the four dimensions). The internal consistency (Cronbach’s α) of our data was as follows: total IPQ = 0.90 and sensory dimension = 0.94.
In line with a previous study [30], the intensity of current pain was assessed using a numerical rating scale (NRS), a self-assessment tool consisting of a horizontal line with numbers at each end, respectively, corresponding to “no pain” (a score of 0) and the “maximum pain imaginable” (a score of 10), which is not included in the IPQ.
2.2.3 History of TEs
The “Inventory of Stressful and Traumatic Life Events” [7], the Italian adaptation of the Life Stressor Checklist-Revised [31], is a self-report questionnaire made up of 29 questions exploring stressful/traumatic events. The questionnaire elicits information on TEs, distinguishing between childhood and adult trauma. Subjects presenting one or more events listed in DSM 5 Criterion A for PTSD [4] were taken as having experienced “Major Trauma,” while other TEs, not listed in DSM 5 Criterion A, were defined as having experienced “Minor Trauma.” The internal consistency (Cronbach’s α) of our data for the total TEs was 0.79.
2.2.4 Alexithymia
Toronto Alexithymia Scale-20 (TAS-20) [15] is a self-report questionnaire composed of 20 items investigating: difficulty in identifying and distinguishing between feelings and bodily sensations (F1), difficulty in describing feelings (F2), and outward-oriented thinking (F3). A total score is also provided. For a diagnosis of alexithymia, the total score must reach at least 61 [15]. The internal consistency (Cronbach’s α) of our data for total TAS-20 was 0.65.
2.2.5 Somatization
The Symptom Checklist-90 Revised (SCL-90 R) [32] is a self-report questionnaire used to measure psychopathology. It consists of 90 items grouped into nine symptom dimensions, namely somatization, obsession-compulsion, interpersonal sensitivity, depression, anxiety, hostility, phobic anxiety, paranoia, and psychoticism. Three global indices are also provided: the Global Severity Index (GSI), the Positive Symptom Total (PST), and the Positive Symptom Distress Index (PSDI). The internal consistency (Cronbach’s α) of our data for the somatization dimension was 0.95.
2.2.6 SSA
The somatosensory amplification scale (SSAS) [14] is a self-report scale that quantifies the propensity of a subject to SSA, i.e. the tendency to experience intense, noxious, and disturbing somatic sensations. It consists of ten items scored on a 0–4 Likert scale, with high scores indicating a greater tendency to somatic amplification. The internal consistency (Cronbach’s α) was 0.72 [14].
2.3 Statistical analysis
All the data were analysed using the IBM Statistical Package for Social Sciences, version 26.0, and the significance level was set at p < 0.05. The Kolmogorov–Smirnov test was used to confirm the Gaussian distribution of the data. The total sample was subdivided on the basis of the self-reported presence of pain over the preceding 2 years into pain-free and pain groups, and the differences between groups in sociodemographic variables, number of TEs, somatization, alexithymia, and psychopathological dimensions were investigated using the t-test for continuous variables, and the chi-squared test with Fisher’s exact test for categorical variables. The effect sizes were calculated with the tx2/(df)0.5 formula for the t-test, and are expressed as phi (φ; small = 0.10, medium = 0.30, large = 0.50) for chi-squared [33]. To investigate any relationships between TEs, alexithymia, and pain, Pearson’s partial correlation analyses were performed. To interpret effect size according to Cohen’s d [34], an r correlation coefficient of 0.10 was considered a weak or small association; an r of 0.30 a moderate correlation; and an r of 0.50 a greater or strong correlation.
To investigate TEs as a predictor of psychosomatic manifestations (somatization, pain, SSA, alexithymia), multiple regression analyses using the stepwise forward model were performed. The elements of the linear regression represented are the following: the coefficient of determination (or R2), which measures the ability of the model to predict the result (an R2 of 1 indicates that the model explains all of the variability in the outcome); the t-test, which tests the significance of single regression parameters; the standardized coefficient (or β), which reveals the relative relevance of each variable and thereby enables identification of which factors have the highest and lowest relative predictive validity; the p value, which indicates a statistically significant association between the predictor variables and the outcome variable; and the confidence interval (CI), which will be used to determine statistical significance: when the CI does not contain 0, there is a statistically significant difference [35].
3 Results
3.1 Differences between pain-free and pain groups
The total sample was divided into pain-free (55 patients) and pain (91 patients) groups. As shown in Table 1, the two groups differed in terms of age, with the pain-free group being younger (t = −4.185, p = 0.000). Married and divorced people were more prevalent in the pain than in the pain-free group, and the only widowed people were in the pain group (χ 2 = 8.55, p = 0.036, φ = 0.25). No differences in gender, education, or social status were found between the two groups.
Differences in socio-demographic variables, TE subtypes, somatization, psychopathology, SSA, and alexithymia between the pain-free and pain groups
| Pain-free group | Pain group | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| N (%) | M (sD) | N (%) | M (sD) | χ2 | t | p | φ/d | ||
| Total sample size | 55 (37.67) | 91 (62.33) | |||||||
| Age | 27.54 (8.72) | 36.80 (14.80) | −4.18 | 0.000 | 0.76 | ||||
| Gender | Males | 22 (40.00) | 29 (31.90) | 0.99 | 0.372 | 0.08 | |||
| Females | 33 (60.00) | 62 (68.10) | |||||||
| Education (years) | 17.27 (2.82) | 16.57 (3.14) | 1.32 | 0.190 | 0.23 | ||||
| Civil status | Single | 45 (91.84) | 62 (71.26) | 8.55 | 0.036 | 0.25 | |||
| Married | 3 (6.12) | 17 (19.54) | |||||||
| Divorced | 1 (2.04) | 7 (8.05) | |||||||
| Widowed | 0 (0.00) | 1 (1.15) | |||||||
| Social status | High | 2 (4.16) | 0 (0.00) | 4.00 | 0.135 | 0.17 | |||
| Medium | 40 (83.34) | 77 (91.67) | |||||||
| Low | 6 (12.50) | 7 (8.33) | |||||||
| No TEs | 3 (75.00) | 1 (25.00) | 2.40 | 0.153 | 0.13 | ||||
| No. total TEs | 3.20 (2.31) | 4.16 (2.84) | −2.13 | 0.035 | 0.37 | ||||
| No. major TEs | 1.55 (1.40) | 1.98 (1.73) | −1.57 | 0.118 | 0.27 | ||||
| No. minor TEs | 1.45 (1.21) | 1.95 (1.36) | −2.19 | 0.030 | 0.38 | ||||
| No. child. TEs | 1.38 (1.75) | 1.54 (1.59) | −0.56 | 0.579 | 0.09 | ||||
| Subtypes of child. TEs | Major | 0.42 (0.50) | 0.51 (0.50) | −1.02 | 0.126 | 0.18 | |||
| Minor | 0.42 (0.50) | 0.48 (0.50) | −0.76 | 0.153 | 0.12 | ||||
| No. adult. TEs | 1.62 (1.53) | 2.16 (1.77) | −1.90 | 0.059 | 0.32 | ||||
| SCL-90 R | Somatization | 0.67 (0.74) | 1.06 (0.70) | −3.12 | 0.002 | 0.54 | |||
| Obsession-Compulsion | 0.87 (0.87) | 1.22 (0.86) | −2.32 | 0.022 | 0.40 | ||||
| Interpersonal sensitivity | 0.80 (0.87) | 0.95 (0.82) | −1.02 | 0.310 | 0.17 | ||||
| Depression | 1 (1.02) | 1.33 (0.91) | −2.00 | 0.047 | 1.27 | ||||
| Anxiety | 0.85 (0.89) | 1.06 (0.83) | −1.46 | 0.150 | 0.24 | ||||
| Hostility | 0.59 (0.71) | 0.66 (0.58) | −0.60 | 0.550 | 0.10 | ||||
| Phobic anxiety | 0.40 (0.66) | 0.42 (0.56) | −0.20 | 0.840 | 0.03 | ||||
| Paranoid ideation | 0.77 (0.82) | 0.83 (0.71) | −0.44 | 0.660 | 0.07 | ||||
| Psychoticism | 0.50 (0.63) | 0.58 (0.56) | −0.83 | 0.410 | 0.13 | ||||
| GSI | 0.74 (0.75) | 0.96 (0.62) | −1.90 | 0.060 | 0.31 | ||||
| Total | 35.39 (22.59) | 43.49 (21.46) | −2.13 | 0.035 | 0.36 | ||||
| PSDI | 1.60 (0.65) | 1.80 (0.54) | −1.91 | 0.055 | 0.33 | ||||
| SSAS | 5.80 (6.79) | 11.65 (8.30) | −4.22 | 0.000 | 0.77 | ||||
| TAS-20 | F1 | 13.12 (5.64) | 15.21 (7.20) | −1.79 | 0.076 | 0.32 | |||
| F2 | 12.17 (4.45) | 12.16 (5.36) | 0.01 | 0.991 | 0.00 | ||||
| F3 | 15.67 (4.73) | 16.36 (4.48) | −0.86 | 0.394 | 0.14 | ||||
| Total | 40.94 (11.49) | 43.73 (13.32) | −1.25 | 0.212 | 0.22 | ||||
TEs = traumatic experiences; SCL-90 R = SymptomCheck-List-90 Revised; GSI = Global Severity Index; PSDI = Positive Symptom Distress Index; SSAS = Somatosensory Amplification Scale; TAS-20 = Toronto Alexithymia Scale-20; t = unpaired t value; χ 2 = chi-squared value; p < 0.05; φ = phi (small = 0.10, medium = 0.30, large = 0.50); d (Cohen’s d effect size): 0.20 = small effect, 0.50 = moderate effect, and 0.80 = large effect. Statistically significant values are in bold.
Significant differences between the two groups were found in the number of total and minor TEs (t = −2.127, p = 0.036; t = −2.196, p = 0.030, respectively), which were both higher in the pain group, as shown in Table 1. The pain group also had higher scores than the pain-free group for the SCL-90 R dimension somatization, obsession-compulsion, and depression (t = −3.119, p = 0.002; t = −2.320, p = 0.022; t = −2.000, p = 0.047, respectively). SSAS scores were also higher in the pain group than in the pain-free group (t = −4.216, p = 0.000). No differences in alexithymia dimensions (TAS-20) were found between the two groups.
From Table 1, an SD value greater than some average scores can be observed. This could be attributed to the sample size, as highlighted in the limitations discussed below.
3.2 Correlations between TE subtypes, age, psychopathology, alexithymia, somatization, SSA, and pain
Figure 1 (heatmap) reports bivariate linear correlations between TEs and psychosomatic variables for the whole sample. Variables with no significant correlation with TE subtypes, including the remaining TAS-20 factors and SCL-90 R dimensions, are not included in the heatmap.
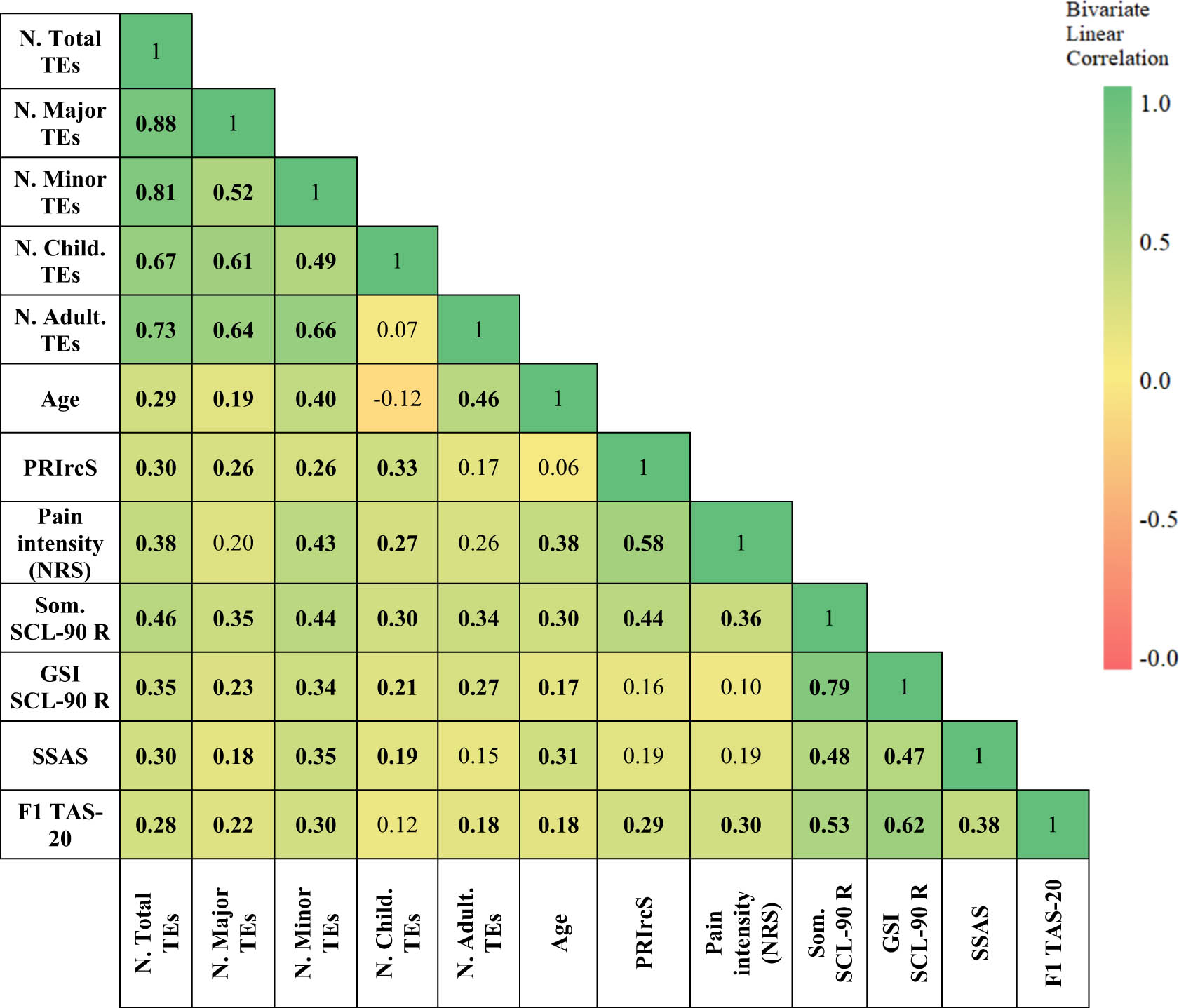
Linear correlations between TE subtypes, age, alexithymia, somatization, SSA, and pain in the total sample. Colours of the heatmap ranges from red to green to illustrate the effect size: green indicates a stronger effect size (r > 0.50) of the correlation, yellow a medium effect (range of r = 0.30–0.50), and red a weak effect (<0.30). TEs = traumatic experiences; PRIrcS = sensorial dimension of pain; NRS = Numeric Rating Scale; Som. SCL-90 R = somatization dimension on SCL-90 R (Symptom Checklist-90 Revised); GSI SCL-90 R = Global Severity Index (Symptom Checklist 90-Revised); SSAS = Somatosensory Amplification Scale; F1 TAS-20 = Factor 1 on TAS-20 (Toronto Alexithymia Scale-20).
Linear correlation analysis showed that all TE subtypes were positively correlated with age (total TEs: r = 0.29, p = 0.000), and both the sensorial dimension (PRIrcS, total TEs: r = 0.30, p = 0.015) and intensity of pain (NRS, total TEs: r = 0.38, p = 0.004), as well as somatization (total TEs: r = 0.46, p = 0.000), the SCL-90 R GSI (total TEs: r = 0.35, p = 0.000), SSAS (total TEs: r = 0.30, p = 0.000), and alexithymia, in particular the difficulty in identifying and distinguishing between feelings and bodily sensations (TAS-20 F1, total TEs: r = 0.28, p = 0.001). Only the number of TEs experienced in adulthood did not correlate significantly with PRIrcS (r = 0.17, p = 0.154) or NRS (r = 0.26, p = 0.054). With the exception of the PRIrcS (which was only correlated with age), all psychosomatic dimensions correlated with both age and each other. The strongest effect sizes were found between TAS-20 F1 and SCL-90 R somatization (r = 0.53, p = 0.000), and between SSAS and SCL-90 R somatization (r = 0.48, p = 0.000).
3.3 Role of each variable in the relationships between TE subtypes, alexithymia, somatization, SSA, and pain
Since there was a difference in the mean age of the two groups of subjects studied (Table 1) and since age was found to correlate with most of the variables investigated (Figure 1), all the correlations among the psychosomatic variables explored were adjusted for age. Even when adjusted for age, the somatization dimension seems to be closely linked to the number of TEs in childhood, as shown in Table 2, r = 0.36; p = 0.000, with a medium effect size when the partial correlation analysis was controlled for age. The correlation between SCL90 somatization and the number of TEs in childhood remained significant even when SSAS (r = 0.38; p = 0.000), TAS-20 F1 (r = 0.28, p = 0.001), PRIrcS (r = 0.32, p = 0.012), and NRS (r = 0.40, p = 0.005) were added to the correction effect adjustment.
Partial correlations between TE subtypes and psychosomatic variables
| Controlling for | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Variables | df | Age | Age + Som. SCL-90 R | Age + GSI SCL-90 R | Age + SSAS | Age + F1 TAS-20 | Age + PRIicS | Age + NRS | |
| Som. SCL-90 R | No. total TEs | 136 | 0.40*** | 0.26** | 0.38*** | 0.32*** | 0.36** | 0.45** | |
| No. major TEs | 136 | 0.33*** | 0.25** | 0.35*** | 0.29** | 0.32* | 0.40** | ||
| No. minor TEs | 136 | 0.31*** | 0.18* | 0.25** | 0.19* | 0.27* | 0.33* | ||
| No. child. TEs | 136 | 0.36*** | 0.28** | 0.38*** | 0.28** | 0.32* | 0.40** | ||
| No. adult. TEs | 136 | 0.21* | 0.09 | 0.19* | 0.23* | 0.23 | 0.30* | ||
| SSAS | No. total TEs | 131 | 0.22* | 0.04 | 0.06 | 0.09 | 0.35** | 0.25 | |
| No. major TEs | 131 | 0.12 | −0.05 | −0.01 | 0.02 | 0.29* | 0.21 | ||
| No. minor TEs | 131 | 0.24** | 0.11 | 0.13 | 0.10 | 0.3* | 0.22 | ||
| No. child. TEs | 131 | 0.24** | 0.07 | 0.13 | 0.10 | 0.42** | 0.31* | ||
| No. adult. TEs | 131 | −0.01 | −0.11 | −0.14 | −0.04 | 0.13 | 0.1 | ||
| F1 TAS-20 | No. total TEs | 134 | 0.23** | 0.04 | 0.11 | 0.23* | 0.22 | 0.28* | |
| No. major TEs | 134 | 0.18* | 0.00 | 0.07 | 0.18* | 0.15 | 0.21 | ||
| No. minor TEs | 134 | 0.26** | 0.12 | 0.16 | 0.25** | 0.31* | 0.32* | ||
| No. child. TEs | 134 | 0.14 | −0.01 | 0.09 | 0.12 | 0.05 | 0.12 | ||
| No. adult. TEs | 134 | 0.11 | −0.04 | −0.06 | 0.15 | 0.14 | 0.15 | ||
| PRIrcS | No. total TEs | 64 | 0.29* | 0.12 | 0.24 | 0.23 | 0.24 | 0.20 | |
| No. major TEs | 64 | 0.25* | 0.09 | 0.21 | 0.22 | 0.23 | 0.22 | ||
| No. minor TEs | 64 | 0.26* | 0.12 | 0.22 | 0.17 | 0.17 | 0.10 | ||
| No. child. TEs | 64 | 0.34** | 0.19 | 0.33* | 0.34** | 0.34** | 0.25 | ||
| No. adult. TEs | 64 | 0.17 | 0.05 | 0.12 | 0.06 | 0.11 | 0.13 | ||
| Pain intensity (NRS) | No. total TEs | 52 | 0.28* | 0.15 | 0.22 | 0.29* | 0.29* | 0.11 | |
| No. major TEs | 52 | 0.11 | −0.03 | 0.06 | 0.21 | 0.21 | −0.04 | ||
| No. minor TEs | 52 | 0.31* | 0.22 | 0.28 | 0.29* | 0.25 | 0.20 | ||
| No. child. TEs | 52 | 0.34* | 0.27 | 0.35* | 0.38** | 0.35* | 0.14 | ||
| No. adult. TEs | 52 | 0.10 | −0.01 | 0.04 | 0.12 | 0.15 | 0.00 | ||
TEs = traumatic experiences; SCL-90 R Som. = somatization dimension on SCL-90 R; SSAS = Somatosensory Amplification Scale; TAS-20 F1 = TAS-20 Factor 1; PRIrcS = sensorial dimension of pain; NRS = Numeric Rating Scale; *p < 0.05, **p < 0.01, ***p = 0.000.
After the somatization dimension was used as a controlling variable in the partial correlation, all correlations among TE subtypes and psychosomatic dimensions previously found to be statistically significant were no longer so (Table 2). Somatization appears to play a relevant role in the correlation between pain, particularly in its sensory dimension and intensity, and all types of TEs. Indeed, as shown in Table 2, the correlations between PRIrcS and NRS and all subtypes of TEs lost their statistical significance when controlled for SCL-90 R somatization.
SSA (SSAS) and alexithymia (TAS-20 F1) also appear to influence the correlations between the intensity and sensory dimension of pain with all types of TEs investigated, except for childhood trauma (r = 0.34, p = 0.009; r = 0.34, p = 0.007 for the sensory dimension and r = 0.38, p = 0.007; r = 0.35, p = 0.014 for the intensity of pain). When controlled for SSAS and TAS-20 F1, the correlations between all TEs (with the exception of childhood trauma) and the sensorial dimension and intensity of pain lost their statistical significance. As a whole, this indicates a significant correlation between the number of TEs in childhood and the degree of somatization, which is not influenced by SSA, pain, or alexithymia. However, SSA and alexithymia do influence each other in their respective correlations with childhood trauma.
3.4 Predicting the effect of TE subtypes on psychosomatic manifestations
Stepwise forward multiple linear regression analysis using psychosomatic manifestations as dependent variables was used to test whether TE subtypes significantly predicted psychosomatic manifestations (Table 3). For all dependent variables, one model is sufficient to predict variables, with the exception of the relationship between pain intensity (NRS) and types of childhood trauma. Minor TEs were found to be an important predictor of pain intensity, not only in general but also considering them in childhood. As shown in Table 3, model 2 revealed that the predictors of pain intensity are lifetime minor TEs and minor childhood TEs. Minor TEs rather than major TEs represent the most important predictor in adulthood of somatic amplification, the inability to recognize emotions and the intensity of pain.
Stepwise forward multiple regression model with TE subtypes predicting somatization (Som. SCL-90 R), somatosensory amplification (SSAS), TAS-20 Factor 1 (TAS-20 F1), sensorial dimension (PRIrcS), and intensity (NRS) of pain
| Model | Predictors | Dependent | Adjusted R square | t | β | p | Low | 95% CI |
|---|---|---|---|---|---|---|---|---|
| High | ||||||||
| 1 | No. total TEs | Som. SCL-90 R | 0.20 | 4.49 | 0.46 | 0.000 | 0.08 | 0.16 |
| 1 | No. minor TEs | SSAS | 0.11 | 5.12 | 0.34 | 0.000 | 1.13 | 3.11 |
| 1 | No. minor TEs | F1 TAS-20 | 0.08 | 13.08 | 0.30 | 0.000 | 0.68 | 2.31 |
| 1 | No. child. TEs | PRIrcS | 0.09 | 6.57 | 0.33 | 0.007 | 0.01 | 0.06 |
| 1 | No. minor TEs | Pain intensity (NRS) | 0.17 | 3.04 | 0.43 | 0.001 | 0.44 | 0.70 |
| 2 | No. minor TEs | Pain intensity (NRS) | 0.22 | 2.70 | 0.34 | 0.009 | 0.22 | 1.49 |
| No. min. child. TEs | 0.22 | 2.23 | 0.28 | 0.030 | 0.94 | 4.71 |
TEs = traumatic experiences; Som. SCL-90 R = somatization dimension on SCL-90 R; SSAS = somatosensory Amplification Scale; F1 TAS-20 = TAS-20 Factor 1; NRS = Numeric Rating Scale; PRIrcS = sensorial dimension of pain; 95 CI = confidence interval of 95%.
4 Discussion
This study was designed to investigate the influence of the severity of trauma and when it occurred on both pain and somatization in adulthood. Results of sociodemographic variables (Table 1) indicate that there is no gender difference between the pain and pain-free groups. This result does not seem to be in line with what is reported in the literature, as the subjects with pain are mostly female [36,37]. However, our pain-free group was mostly represented by psychiatric subjects with depressive and anxiety disorders. It is known that these disorders mostly affect females [4], so it is possible that the lack of difference between the two groups depends on the type of sample investigated. The level of education in both our groups was medium or high, and there was no difference between the two groups. The literature reports a higher incidence of chronic pain in subjects with a low social status [36,37], but it is not clear how much this corresponds to the level of education. This also applies to a control sample with psychiatric disorders. Furthermore, it should be underlined that the subjects with pain investigated in this study do not necessarily suffer from chronic pain.
In our study, the group with pain was older than the group without pain, although with a lower average than what is reported in the literature (41–60 years) [36,37]. This result may be due to the composition of the pain group, which did not necessarily include subjects with chronic pain. Nonetheless, we found that age was a significant variable (Figure 1), with our results indicating that with increasing age, there is an increase in both the intensity of pain and somatization. Although the literature reports differences in age and education level between subjects exposed to TEs and those not exposed, especially as regards major traumas (e.g. violence, accidents, and natural disasters) [1], the feature of our sample is that most subjects in our sample had experienced trauma, with only four subjects reporting no TEs. Therefore, our data provide no information relating to subjects without TEs. Although, generally speaking, this might be considered a limitation, in the specific case, it cannot, given the objective of the study.
Our results show that subjects who report pain have a greater tendency towards somatization. This confirms previous findings [13] and indicates that the tendency towards somatization contributes to variations in physiological body perception (interoception), implicated in the transformation of pain from recurrent to chronic [38]. Indeed, pain is one of the most important expressions of somatization, and there seems to be an association between pain in childhood or adolescence and an abnormal response to stress in adulthood [39]. It appears, therefore, that there is a strong link between pain, somatization, and stress response forged in childhood. According to our results, the psychosomatic dimension in adulthood most strongly associated with a history of TEs is somatization (investigated using the SCL-90 R). As shown in Figure 1, its correlations with all TE subtypes are strong, and the number of TEs overall was a predictor for somatization in adults (Table 3).
The presence of somatization in adulthood affects the relationship between TEs and all other aspects of somatization, including pain (Table 2). Furthermore, the age of exposure and the severity of trauma seem to influence the intensity and sensorial component of pain (Table 3). However, the main finding in study is that it is minor rather than major TEs that affect pain and the psychosomatic dimension. This is interesting because most previous research has highlighted the role of major trauma, especially PTSD [40,41,42]. That being said, most of the studies in the literature have investigated the relationship between trauma and chronic pain, and it is, therefore, possible that the difference lies precisely in this; perhaps minor traumas in childhood predict the presence of pain in adults, but only major traumas predispose to chronic pain.
Whatever the case, the results of this investigation make it clear that limited research into minor trauma is a huge gap in the literature. In the attempt to bridge this gap, our study is one of the very few to investigate minor trauma in subjects with pain. It reveals that the tendency to somatization seems to correlate strongly, and independently of age, with both major and minor traumas, whether the exposure was in childhood or adulthood. However, it is minor trauma that seems to be more predictive of the link between pain and the individual subcomponents of somatization, specifically somatic amplification and alexithymia, in particular the aspects pertaining to lack of recognition of emotions, in line with Wise and Mann theory that alexithymia and SSA contribute to the process of somatization [16].
Although, according to the ICD-11 classification [43], alexithymia seems more closely linked to primary rather than secondary chronic pain, our results confirm the weak relationship between TEs and alexithymia that we have previously reported [12], though it should be noted that in this study Cronbach’s alpha for the total TAS was relatively low. That being said, the inability to recognize and be aware of emotions (TAS-20 Factor 1) seems to be a dimension of alexithymia that is linked to the presence of pain, as revealed in our previous studies conducted on primary school children [44]. Furthermore, it supports the hypothesis that the elaboration of trauma is focused on the body and the information that spreads from it.
We encourage more research in this area, as there have been very few studies to explore the effect of minor trauma on pain and somatization. Traumatic everyday events can also affect temporality, trust and perceptual awareness, as well documented by Craig [45], and it would be interesting to explore in more depth the links emerging between these variables.
5 Limitations
The main limitation of this study was the sample size, which may explain the weakness of the correlations and the reliability of some questionnaires found. Like previous studies, ours was also cross-sectional, retrospective, and observational; the results would certainly be more meaningful if the study had been conducted longitudinally. As mentioned above, the sample of this study was younger and better educated than reported by clinical studies for the chronic pain population. At present, we cannot rule out that a different age and/or a different level of education may affect the results obtained. That being said, it is important to note that our sample had pain, not specifically chronic pain. Considering the literature, it might have been more useful to investigate chronic pain, rather than pain in general. Although this may be thought of as a limitation, it may also represent a strength further to the investigation of predictors of the onset of chronic pain. Indeed, our results indicate that TEs predispose a person to somatization and pain, even if it is not chronic.
The lack of difference in gender between pain-free and pain groups might also be a limitation. However, as we have reported previously, subjects without pain often suffer from anxiety and/or depression, which mainly affect females.
The use of self-report tools is also a weakness, as it is associated with various biases – in particular, social desirability – that can affect results. The mid-level Cronbach for some tools used, such as the questionnaire that investigates TEs, encourages us to look for more reliable and validated tools in Italy, which guarantees us a more accurate investigation.
On the other hand, a strength of this study is the investigation of the relationship between trauma and somatization, breaking down the two conditions into their individual subparts, as each of them contributes to a greater or lesser extent to generating what is the complexity, or “gestalt,” of the suffering of an individual with psychosomatic problems.
6 Conclusions
Interestingly, the presence of pain in adulthood appears to be associated with minor rather than major TEs, especially if experienced during childhood. This relationship appears to be mediated by somatization, a psychosomatic variable with a strong association with all types of traumatic events. In short, our results indicate that the more pronounced the history of minor daily childhood trauma, the adult is more prone to somatization, and the more severe their pain and the somatic components thereof.
Acknowledgements
The authors thank Professor Giancarlo Carli for supervision in the clinical and research field of pain and Aplysia APS for supporting the development of psychosomatic research in the field of pain.
-
Research ethics: As it is a retrospective study, no Ethics Committee approval was necessary. The study adheres to the STROBE statement guidelines for observational research.
-
Informed consent: Informed consent was obtained from all individuals included in this study.
-
Author contributions: All authors accept responsibility for the entire content of this manuscript and have approved its submission. Melania Boni contributed to data collection and assisted with writing and preparing the manuscript. Simone Violi contributed to the data collection. Antonella Ciaramella conceived and designed the study, contributed to the data analysis, and assisted with writing.
-
Competing interests: The authors state no conflict of interest.
-
Research funding: None declared.
-
Data availability: Not applicable.
References
[1] Kessler RC, Aguilar-Gaxiola S, Alonso J, Benjet C, Bromet EJ, Cardoso G, et al. Trauma and PTSD in the WHO world mental health surveys. Eur J Psychotraumatol. 2017 Oct 27;8(sup 5):1353383. 10.1080/20008198.2017.1353383. PMID: 29075426; PMCID: PMC5632781.Search in Google Scholar PubMed PubMed Central
[2] Degenhardt L, Bharat C, Glantz MD, Bromet EJ, Alonso J, Bruffaerts R, et al. WHO World Mental Health Survey collaborators. The associations between traumatic experiences and subsequent onset of a substance use disorder: Findings from the World Health Organization World Mental Health surveys. Drug Alcohol Depend. 2022 Nov 1;240:109574. 10.1016/j.drugalcdep.2022.109574. Epub 2022 Jul 16. PMID: 36150948.Search in Google Scholar PubMed
[3] Scott KM, Koenen KC, Aguilar-Gaxiola S, Alonso J, Angermeyer MC, Benjet C, et al. Associations between lifetime traumatic events and subsequent chronic physical conditions: a cross-national, cross-sectional study. PLoS One. 2013 Nov 19;8(11):e80573. 10.1371/journal.pone.0080573. PMID: 24348911; PMCID: PMC3864645.Search in Google Scholar PubMed PubMed Central
[4] Diagnostic and Statistical Manual of Mental Disorders: DSM-5. 5th edn. Arlington, VA: American Psychiatric Association; 2013.Search in Google Scholar
[5] Berger M, Piralic-Spitzl S, Aigner M. Trauma and post-traumatic stress disorder in transcultural patients with chronic pain. Neuropsychiatrie. 2014;28(4):185–91. 10.1007/s40211-014-0122-x. PMID: 25274146.Search in Google Scholar PubMed
[6] Slavich GM, Irwin MR. From stress to inflammation and major depressive disorder: a social signal transduction theory of depression. Psychol Bull. 2014 May;140(3):774–815. 10.1037/a0035302. Epub 2014 Jan 13. PMID: 24417575; PMCID: PMC4006295.Search in Google Scholar PubMed PubMed Central
[7] Giannantonio M. Psicotraumatologia. Fondamenti e strumenti operativi. Torino: Centro Scientifico Editore; 2009.Search in Google Scholar
[8] Haviland MG, Morton KR, Oda K, Fraser GE. Traumatic experiences, major life stressors, and self-reporting a physician-given fibromyalgia diagnosis. Psychiatry Res. 2010 May 30;177(3):335–41. 10.1016/j.psychres.2009.08.017. Epub 2010 Apr 10. PMID: 20382432; PMCID: PMC2868959.Search in Google Scholar PubMed PubMed Central
[9] van der Kolk BA, Pelcovitz D, Roth S, Mandel FS, McFarlane A, Herman JL. Dissociation, somatization, and affect dysregulation: the complexity of adaptation of trauma. Am J Psychiatry. 1996 Jul;153(7 Suppl):83–93. 10.1176/ajp.153.7.83. PMID: 8659645.Search in Google Scholar PubMed
[10] Aragona M, Catino E, Pucci D, Carrer S, Colosimo F, Lafuente M, et al. The relationship between somatization and post-traumatic symptoms among immigrants receiving primary care services. J Trauma Stress. 2010 Oct;23(5):615–22. 10.1002/jts.20571. PMID: 20931663.Search in Google Scholar PubMed
[11] Sadeghi S, Dolatshahi B, Pourshahbaz A, Zarei M, Kami M. Relationship between traumatic experiences and somatic symptoms severity in students. PCP. 2017;5(3):211–6.10.18869/acadpub.jpcp.5.3.211Search in Google Scholar
[12] Ciaramella A. The influence of trauma on autobiographical memory in the assessment of somatoform disorders according to DSM IV criteria. Psychiatr Q. 2018 Dec;89(4):991–1005. 10.1007/s11126-018-9597-0. PMID: 30136256.Search in Google Scholar PubMed
[13] Lipowski ZJ. Somatization: The experience and communication of psychological distress as somatic symptoms. Psychother Psychosom. 1987;47(3–4):160–7. 10.1159/000288013. PMID: 3333284.Search in Google Scholar PubMed
[14] Barsky AJ, Goodson JD, Lane RS, Cleary PD. The amplification of somatic symptoms. Psychosom Med. 1988 Sep-Oct;50(5):510–9. 10.1097/00006842-198809000-00007. PMID: 3186894.Search in Google Scholar PubMed
[15] Bagby RM, Parker JD, Taylor GJ. The twenty-item Toronto Alexithymia Scale--I. Item selection and cross-validation of the factor structure. J Psychosom Res. 1994 Jan;38(1):23–32. 10.1016/0022-3999(94)90005-1. PMID: 8126686.Search in Google Scholar PubMed
[16] Wise TN, Mann LS. The relationship between somatosensory amplification, alexithymia, and neuroticism. J Psychosom Res. 1994 Aug;38(6):515–21. 10.1016/0022-3999(94)90048-5. PMID: 7990059.Search in Google Scholar PubMed
[17] Ciaramella A, Silvestri S, Pozzolini V, Federici M, Carli G. A retrospective observational study comparing somatosensory amplification in fibromyalgia, chronic pain, psychiatric disorders and healthy subjects. Scand J Pain. 2020 Nov;21(2):317–29. 10.1515/sjpain-2020-0103. PMID: 34387956.Search in Google Scholar PubMed
[18] Spano VE, Imbriglio TV, Ho KCJ, Chow JCF, Cioffi I. Increased somatosensory amplification is associated with decreased pressure pain thresholds at both trigeminal and extra-trigeminal locations in healthy individuals. J Oral Rehabil. 2021 Jan;48(1):10–7. 10.1111/joor.13101. Epub 2020 Oct 7. PMID: 32979854.Search in Google Scholar PubMed
[19] Chow JC, Cioffi I. Effects of trait anxiety, somatosensory amplification, and facial pain on self-reported oral behaviors. Clin Oral Invest. 2019;23:1653–61. 10.1007/s00784-018-2600-1.Search in Google Scholar PubMed
[20] Wolfe F, Häuser W, Walitt BT, Katz RS, Rasker JJ, Russell AS. Fibromyalgia and physical trauma: the concepts we invent. J Rheumatol. 2014 Sep;41(9):1737–45. 10.3899/jrheum.140268. Epub 2014 Aug 1. PMID: 25086080.Search in Google Scholar PubMed
[21] Brown RJ, Schrag A, Trimble MR. Dissociation, childhood interpersonal trauma, and family functioning in patients with somatization disorder. Am J Psychiatry. 2005 May;162(5):899–905. 10.1176/appi.ajp.162.5.899. PMID: 15863791.Search in Google Scholar PubMed
[22] Glaus J, Moser DA, Rusconi Serpa S, Jouabli S, Turri F, Plessen KJ, et al. Families with violence exposure and the intergenerational transmission of somatization. Front Psychiatry. 2022 Feb;13:820652. 10.3389/fpsyt.2022.820652. PMID: 35280182; PMCID: PMC8904725.Search in Google Scholar PubMed PubMed Central
[23] Roelofs K, Keijsers GP, Hoogduin KA, Näring GW, Moene FC. Childhood abuse in patients with conversion disorder. Am J Psychiatry. 2002 Nov;159(11):1908–13. 10.1176/appi.ajp.159.11.1908. PMID: 12411227.Search in Google Scholar PubMed
[24] Farooq A, Yousaf A. Childhood trauma and alexithymia in patients with conversion disorder. J Coll Phys Surg Pak. 2016 Jul;26(7):606–10. PMID: 27504555.Search in Google Scholar
[25] Goldsmith RE, Freyd JJ. Awareness for emotional abuse. J Emotional Abuse. 2005;5(1):95–123. 10.1300/J135v05n01_04.Search in Google Scholar
[26] Güleç MY, Altintaş M, İnanç L, Bezgin CH, Koca EK, Güleç H. Effects of childhood trauma on somatization in major depressive disorder: The role of alexithymia. J Affect Disord. 2013 Mar;146(1):137–41. 10.1016/j.jad.2012.06.033. Epub 2012 Aug 9. PMID: 22884234.Search in Google Scholar PubMed
[27] De Benedittis G, Massel R, Nobili R, Pieri A. The Italian pain questionnaire. Pain. 1988 Apr;33(1):53–62. 10.1016/0304-3959(88)90203-5. PMID: 3380551.Search in Google Scholar PubMed
[28] von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. STROBE InitiativeThe strengthening the reporting of observational studies in epidemiology (STROBE) statement: Guidelines for reporting observational studies. Lancet. 2007 Oct 20;370(9596):1453–7. 10.1016/S0140-6736(07)61602-X. PMID: 18064739.Search in Google Scholar PubMed
[29] Melzack R. The McGill pain questionnaire: Major properties and scoring methods. Pain. 1975 Sep;1(3):277–99. 10.1016/0304-3959(75)90044-5. PMID: 1235985.Search in Google Scholar PubMed
[30] McCormack HM, Horne DJ, Sheather S. Clinical applications of visual analogue scales: A critical review. Psychol Med. 1988 Nov;18(4):1007–19. 10.1017/s0033291700009934. PMID: 3078045.Search in Google Scholar PubMed
[31] Wolfe J, Kimerling R. Gender issues in the assessment of post-traumatic stress disorder. In: Wilson JP, Keane TM, editors. Assessing psychological trauma and PTSD. The Guilford Press; 1997. p. 192–238.Search in Google Scholar
[32] Derogatis Leonard R. Scl-90-R: Symptom checklist-90-R: Administration scoring & procedures manual. 3rd edn. National Computer Systems; 1994.Search in Google Scholar
[33] Pautz N, Olivier B, Steyn F. The use of nonparametric effect sizes in single study musculoskeletal physiotherapy research: A practical primer. Phys Ther Sport. 2018 Sep;33:117–24. 10.1016/j.ptsp.2018.07.009. Epub 2018 Jul 29. PMID: 30077090.Search in Google Scholar PubMed
[34] Cohen J. Statistical power analysis for the behavioral sciences. 2nd edn. Mahwah, New Jersey, United States: L. Erlbaum Associates; 1988.Search in Google Scholar
[35] Olsen AA, McLaughlin JE, Harpe SE. Using multiple linear regression in pharmacy education scholarship. Curr Pharm Teach Learn. 2020 Oct;12(10):1258–68. 10.1016/j.cptl.2020.05.017. Epub 2020 Jun 12. PMID: 32739064.Search in Google Scholar PubMed
[36] Breivik H, Collett B, Ventafridda V, Cohen R, Gallacher D. Survey of chronic pain in Europe: prevalence, impact on daily life, and treatment. Eur J Pain. 2006 May;10(4):287–333. 10.1016/j.ejpain.2005.06.009. Epub 2005 Aug 10. PMID: 16095934.Search in Google Scholar PubMed
[37] Goudman L, De Smedt A, Linderoth B, Eldabe S, Witkam R, Henssen D, et al. Identifying goals in patients with chronic pain: A European survey. Eur J Pain. 2021 Oct;25(9):1959–70. 10.1002/ejp.1814. Epub 2021 Jun 20. PMID: 34048121.Search in Google Scholar PubMed
[38] Ciaramella A, Pozzolini V, Scatena E, Carli G. Can interoceptive sensitivity provide information on the difference in the perceptual mechanisms of recurrent and chronic pain? Part I. A retrospective clinical study related to multidimensional pain assessment. Scand J Pain. 2022 Sep 23;23(2):308–17. 10.1515/sjpain-2022-0040. PMID: 36131533.Search in Google Scholar PubMed
[39] Gold JI, Kant AJ, Kim SH. The impact of unintentional pediatric trauma: a review of pain, acute stress, and post-traumatic stress. J Pediatr Nurs. 2008 Apr;23(2):81–91. 10.1016/j.pedn.2007.08.005. PMID: 18339334.Search in Google Scholar PubMed
[40] Demyttenaere K, Bruffaerts R, Lee S, Posada-Villa J, Kovess V, Angermeyer MC, et al. Mental disorders among persons with chronic back or neck pain: results from the World Mental Health Surveys. Pain. 2007 Jun;129(3):332–42. 10.1016/j.pain.2007.01.022. Epub 2007 Mar 9. PMID: 17350169.Search in Google Scholar PubMed
[41] McWilliams LA, Cox BJ, Enns MW. Mood and anxiety disorders associated with chronic pain: an examination in a nationally representative sample. Pain. 2003 Nov;106(1–2):127–33. 10.1016/s0304-3959(03)00301-4. PMID: 14581119.Search in Google Scholar PubMed
[42] Sledjeski EM, Speisman B, Dierker LC. Does number of lifetime traumas explain the relationship between PTSD and chronic medical conditions? Answers from the National Comorbidity Survey-Replication (NCS-R). J Behav Med. 2008 Aug;31(4):341–9. 10.1007/s10865-008-9158-3. Epub 2008 Jun 14. PMID: 18553129; PMCID: PMC2659854.Search in Google Scholar PubMed PubMed Central
[43] Treede RD, Rief W, Barke A, Aziz Q, Bennett MI, Benoliel R, et al. Chronic pain as a symptom or a disease: the IASP Classification of Chronic Pain for the International Classification of Diseases (ICD-11). Pain. 2019 Jan;160(1):19–27. 10.1097/j.pain.0000000000001384. PMID: 30586067.Search in Google Scholar PubMed
[44] Rossi M, Bruno G, Chiusalupi M, Ciaramella A. Relationship between pain, somatisation, and emotional awareness in primary school children. Pain Res Treat. 2018 Nov;2018:4316234. 10.1155/2018/4316234. PMID: 30538863; PMCID: PMC6260528.Search in Google Scholar PubMed PubMed Central
[45] Craig AD(Bud). How do you feel?: An interoceptive moment with your neurobiological self. Princeton, New Jersey, United States: Princeton University Press; 2015.10.1515/9781400852727Search in Google Scholar
© 2024 the author(s), published by De Gruyter
This work is licensed under the Creative Commons Attribution 4.0 International License.
Articles in the same Issue
- Editorial Comment
- From pain to relief: Exploring the consistency of exercise-induced hypoalgesia
- Christmas greetings 2024 from the Editor-in-Chief
- Original Articles
- The Scandinavian Society for the Study of Pain 2022 Postgraduate Course and Annual Scientific (SASP 2022) Meeting 12th to 14th October at Rigshospitalet, Copenhagen
- Comparison of ultrasound-guided continuous erector spinae plane block versus continuous paravertebral block for postoperative analgesia in patients undergoing proximal femur surgeries
- Clinical Pain Researches
- The effect of tourniquet use on postoperative opioid consumption after ankle fracture surgery – a retrospective cohort study
- Changes in pain, daily occupations, lifestyle, and health following an occupational therapy lifestyle intervention: a secondary analysis from a feasibility study in patients with chronic high-impact pain
- Tonic cuff pressure pain sensitivity in chronic pain patients and its relation to self-reported physical activity
- Reliability, construct validity, and factorial structure of a Swedish version of the medical outcomes study social support survey (MOS-SSS) in patients with chronic pain
- Hurdles and potentials when implementing internet-delivered Acceptance and commitment therapy for chronic pain: a retrospective appraisal using the Quality implementation framework
- Exploring the outcome “days with bothersome pain” and its association with pain intensity, disability, and quality of life
- Fatigue and cognitive fatigability in patients with chronic pain
- The Swedish version of the pain self-efficacy questionnaire short form, PSEQ-2SV: Cultural adaptation and psychometric evaluation in a population of patients with musculoskeletal disorders
- Pain coping and catastrophizing in youth with and without cerebral palsy
- Neuropathic pain after surgery – A clinical validation study and assessment of accuracy measures of the 5-item NeuPPS scale
- Translation, contextual adaptation, and reliability of the Danish Concept of Pain Inventory (COPI-Adult (DK)) – A self-reported outcome measure
- Cosmetic surgery and associated chronic postsurgical pain: A cross-sectional study from Norway
- The association of hemodynamic parameters and clinical demographic variables with acute postoperative pain in female oncological breast surgery patients: A retrospective cohort study
- Healthcare professionals’ experiences of interdisciplinary collaboration in pain centres – A qualitative study
- Effects of deep brain stimulation and verbal suggestions on pain in Parkinson’s disease
- Painful differences between different pain scale assessments: The outcome of assessed pain is a matter of the choices of scale and statistics
- Prevalence and characteristics of fibromyalgia according to three fibromyalgia diagnostic criteria: A secondary analysis study
- Sex moderates the association between quantitative sensory testing and acute and chronic pain after total knee/hip arthroplasty
- Tramadol-paracetamol for postoperative pain after spine surgery – A randomized, double-blind, placebo-controlled study
- Cancer-related pain experienced in daily life is difficult to communicate and to manage – for patients and for professionals
- Making sense of pain in inflammatory bowel disease (IBD): A qualitative study
- Patient-reported pain, satisfaction, adverse effects, and deviations from ambulatory surgery pain medication
- Does pain influence cognitive performance in patients with mild traumatic brain injury?
- Hypocapnia in women with fibromyalgia
- Application of ultrasound-guided thoracic paravertebral block or intercostal nerve block for acute herpes zoster and prevention of post-herpetic neuralgia: A case–control retrospective trial
- Translation and examination of construct validity of the Danish version of the Tampa Scale for Kinesiophobia
- A positive scratch collapse test in anterior cutaneous nerve entrapment syndrome indicates its neuropathic character
- ADHD-pain: Characteristics of chronic pain and association with muscular dysregulation in adults with ADHD
- The relationship between changes in pain intensity and functional disability in persistent disabling low back pain during a course of cognitive functional therapy
- Intrathecal pain treatment for severe pain in patients with terminal cancer: A retrospective analysis of treatment-related complications and side effects
- Psychometric evaluation of the Danish version of the Pain Self-Efficacy Questionnaire in patients with subacute and chronic low back pain
- Dimensionality, reliability, and validity of the Finnish version of the pain catastrophizing scale in chronic low back pain
- To speak or not to speak? A secondary data analysis to further explore the context-insensitive avoidance scale
- Pain catastrophizing levels differentiate between common diseases with pain: HIV, fibromyalgia, complex regional pain syndrome, and breast cancer survivors
- Prevalence of substance use disorder diagnoses in patients with chronic pain receiving reimbursed opioids: An epidemiological study of four Norwegian health registries
- Pain perception while listening to thrash heavy metal vs relaxing music at a heavy metal festival – the CoPainHell study – a factorial randomized non-blinded crossover trial
- Observational Studies
- Cutaneous nerve biopsy in patients with symptoms of small fiber neuropathy: a retrospective study
- The incidence of post cholecystectomy pain (PCP) syndrome at 12 months following laparoscopic cholecystectomy: a prospective evaluation in 200 patients
- Associations between psychological flexibility and daily functioning in endometriosis-related pain
- Relationship between perfectionism, overactivity, pain severity, and pain interference in individuals with chronic pain: A cross-lagged panel model analysis
- Access to psychological treatment for chronic cancer-related pain in Sweden
- Validation of the Danish version of the knowledge and attitudes survey regarding pain
- Associations between cognitive test scores and pain tolerance: The Tromsø study
- Healthcare experiences of fibromyalgia patients and their associations with satisfaction and pain relief. A patient survey
- Video interpretation in a medical spine clinic: A descriptive study of a diverse population and intervention
- Role of history of traumatic life experiences in current psychosomatic manifestations
- Social determinants of health in adults with whiplash associated disorders
- Which patients with chronic low back pain respond favorably to multidisciplinary rehabilitation? A secondary analysis of a randomized controlled trial
- A preliminary examination of the effects of childhood abuse and resilience on pain and physical functioning in patients with knee osteoarthritis
- Differences in risk factors for flare-ups in patients with lumbar radicular pain may depend on the definition of flare
- Real-world evidence evaluation on consumer experience and prescription journey of diclofenac gel in Sweden
- Patient characteristics in relation to opioid exposure in a chronic non-cancer pain population
- Topical Reviews
- Bridging the translational gap: adenosine as a modulator of neuropathic pain in preclinical models and humans
- What do we know about Indigenous Peoples with low back pain around the world? A topical review
- The “future” pain clinician: Competencies needed to provide psychologically informed care
- Systematic Reviews
- Pain management for persistent pain post radiotherapy in head and neck cancers: systematic review
- High-frequency, high-intensity transcutaneous electrical nerve stimulation compared with opioids for pain relief after gynecological surgery: a systematic review and meta-analysis
- Reliability and measurement error of exercise-induced hypoalgesia in pain-free adults and adults with musculoskeletal pain: A systematic review
- Noninvasive transcranial brain stimulation in central post-stroke pain: A systematic review
- Short Communications
- Are we missing the opioid consumption in low- and middle-income countries?
- Association between self-reported pain severity and characteristics of United States adults (age ≥50 years) who used opioids
- Could generative artificial intelligence replace fieldwork in pain research?
- Skin conductance algesimeter is unreliable during sudden perioperative temperature increases
- Original Experimental
- Confirmatory study of the usefulness of quantum molecular resonance and microdissectomy for the treatment of lumbar radiculopathy in a prospective cohort at 6 months follow-up
- Pain catastrophizing in the elderly: An experimental pain study
- Improving general practice management of patients with chronic musculoskeletal pain: Interdisciplinarity, coherence, and concerns
- Concurrent validity of dynamic bedside quantitative sensory testing paradigms in breast cancer survivors with persistent pain
- Transcranial direct current stimulation is more effective than pregabalin in controlling nociceptive and anxiety-like behaviors in a rat fibromyalgia-like model
- Paradox pain sensitivity using cuff pressure or algometer testing in patients with hemophilia
- Physical activity with person-centered guidance supported by a digital platform or with telephone follow-up for persons with chronic widespread pain: Health economic considerations along a randomized controlled trial
- Measuring pain intensity through physical interaction in an experimental model of cold-induced pain: A method comparison study
- Pharmacological treatment of pain in Swedish nursing homes: Prevalence and associations with cognitive impairment and depressive mood
- Neck and shoulder pain and inflammatory biomarkers in plasma among forklift truck operators – A case–control study
- The effect of social exclusion on pain perception and heart rate variability in healthy controls and somatoform pain patients
- Revisiting opioid toxicity: Cellular effects of six commonly used opioids
- Letter to the Editor
- Post cholecystectomy pain syndrome: Letter to Editor
- Response to the Letter by Prof Bordoni
- Response – Reliability and measurement error of exercise-induced hypoalgesia
- Is the skin conductance algesimeter index influenced by temperature?
- Skin conductance algesimeter is unreliable during sudden perioperative temperature increase
- Corrigendum
- Corrigendum to “Chronic post-thoracotomy pain after lung cancer surgery: a prospective study of preoperative risk factors”
- Obituary
- A Significant Voice in Pain Research Björn Gerdle in Memoriam (1953–2024)
Articles in the same Issue
- Editorial Comment
- From pain to relief: Exploring the consistency of exercise-induced hypoalgesia
- Christmas greetings 2024 from the Editor-in-Chief
- Original Articles
- The Scandinavian Society for the Study of Pain 2022 Postgraduate Course and Annual Scientific (SASP 2022) Meeting 12th to 14th October at Rigshospitalet, Copenhagen
- Comparison of ultrasound-guided continuous erector spinae plane block versus continuous paravertebral block for postoperative analgesia in patients undergoing proximal femur surgeries
- Clinical Pain Researches
- The effect of tourniquet use on postoperative opioid consumption after ankle fracture surgery – a retrospective cohort study
- Changes in pain, daily occupations, lifestyle, and health following an occupational therapy lifestyle intervention: a secondary analysis from a feasibility study in patients with chronic high-impact pain
- Tonic cuff pressure pain sensitivity in chronic pain patients and its relation to self-reported physical activity
- Reliability, construct validity, and factorial structure of a Swedish version of the medical outcomes study social support survey (MOS-SSS) in patients with chronic pain
- Hurdles and potentials when implementing internet-delivered Acceptance and commitment therapy for chronic pain: a retrospective appraisal using the Quality implementation framework
- Exploring the outcome “days with bothersome pain” and its association with pain intensity, disability, and quality of life
- Fatigue and cognitive fatigability in patients with chronic pain
- The Swedish version of the pain self-efficacy questionnaire short form, PSEQ-2SV: Cultural adaptation and psychometric evaluation in a population of patients with musculoskeletal disorders
- Pain coping and catastrophizing in youth with and without cerebral palsy
- Neuropathic pain after surgery – A clinical validation study and assessment of accuracy measures of the 5-item NeuPPS scale
- Translation, contextual adaptation, and reliability of the Danish Concept of Pain Inventory (COPI-Adult (DK)) – A self-reported outcome measure
- Cosmetic surgery and associated chronic postsurgical pain: A cross-sectional study from Norway
- The association of hemodynamic parameters and clinical demographic variables with acute postoperative pain in female oncological breast surgery patients: A retrospective cohort study
- Healthcare professionals’ experiences of interdisciplinary collaboration in pain centres – A qualitative study
- Effects of deep brain stimulation and verbal suggestions on pain in Parkinson’s disease
- Painful differences between different pain scale assessments: The outcome of assessed pain is a matter of the choices of scale and statistics
- Prevalence and characteristics of fibromyalgia according to three fibromyalgia diagnostic criteria: A secondary analysis study
- Sex moderates the association between quantitative sensory testing and acute and chronic pain after total knee/hip arthroplasty
- Tramadol-paracetamol for postoperative pain after spine surgery – A randomized, double-blind, placebo-controlled study
- Cancer-related pain experienced in daily life is difficult to communicate and to manage – for patients and for professionals
- Making sense of pain in inflammatory bowel disease (IBD): A qualitative study
- Patient-reported pain, satisfaction, adverse effects, and deviations from ambulatory surgery pain medication
- Does pain influence cognitive performance in patients with mild traumatic brain injury?
- Hypocapnia in women with fibromyalgia
- Application of ultrasound-guided thoracic paravertebral block or intercostal nerve block for acute herpes zoster and prevention of post-herpetic neuralgia: A case–control retrospective trial
- Translation and examination of construct validity of the Danish version of the Tampa Scale for Kinesiophobia
- A positive scratch collapse test in anterior cutaneous nerve entrapment syndrome indicates its neuropathic character
- ADHD-pain: Characteristics of chronic pain and association with muscular dysregulation in adults with ADHD
- The relationship between changes in pain intensity and functional disability in persistent disabling low back pain during a course of cognitive functional therapy
- Intrathecal pain treatment for severe pain in patients with terminal cancer: A retrospective analysis of treatment-related complications and side effects
- Psychometric evaluation of the Danish version of the Pain Self-Efficacy Questionnaire in patients with subacute and chronic low back pain
- Dimensionality, reliability, and validity of the Finnish version of the pain catastrophizing scale in chronic low back pain
- To speak or not to speak? A secondary data analysis to further explore the context-insensitive avoidance scale
- Pain catastrophizing levels differentiate between common diseases with pain: HIV, fibromyalgia, complex regional pain syndrome, and breast cancer survivors
- Prevalence of substance use disorder diagnoses in patients with chronic pain receiving reimbursed opioids: An epidemiological study of four Norwegian health registries
- Pain perception while listening to thrash heavy metal vs relaxing music at a heavy metal festival – the CoPainHell study – a factorial randomized non-blinded crossover trial
- Observational Studies
- Cutaneous nerve biopsy in patients with symptoms of small fiber neuropathy: a retrospective study
- The incidence of post cholecystectomy pain (PCP) syndrome at 12 months following laparoscopic cholecystectomy: a prospective evaluation in 200 patients
- Associations between psychological flexibility and daily functioning in endometriosis-related pain
- Relationship between perfectionism, overactivity, pain severity, and pain interference in individuals with chronic pain: A cross-lagged panel model analysis
- Access to psychological treatment for chronic cancer-related pain in Sweden
- Validation of the Danish version of the knowledge and attitudes survey regarding pain
- Associations between cognitive test scores and pain tolerance: The Tromsø study
- Healthcare experiences of fibromyalgia patients and their associations with satisfaction and pain relief. A patient survey
- Video interpretation in a medical spine clinic: A descriptive study of a diverse population and intervention
- Role of history of traumatic life experiences in current psychosomatic manifestations
- Social determinants of health in adults with whiplash associated disorders
- Which patients with chronic low back pain respond favorably to multidisciplinary rehabilitation? A secondary analysis of a randomized controlled trial
- A preliminary examination of the effects of childhood abuse and resilience on pain and physical functioning in patients with knee osteoarthritis
- Differences in risk factors for flare-ups in patients with lumbar radicular pain may depend on the definition of flare
- Real-world evidence evaluation on consumer experience and prescription journey of diclofenac gel in Sweden
- Patient characteristics in relation to opioid exposure in a chronic non-cancer pain population
- Topical Reviews
- Bridging the translational gap: adenosine as a modulator of neuropathic pain in preclinical models and humans
- What do we know about Indigenous Peoples with low back pain around the world? A topical review
- The “future” pain clinician: Competencies needed to provide psychologically informed care
- Systematic Reviews
- Pain management for persistent pain post radiotherapy in head and neck cancers: systematic review
- High-frequency, high-intensity transcutaneous electrical nerve stimulation compared with opioids for pain relief after gynecological surgery: a systematic review and meta-analysis
- Reliability and measurement error of exercise-induced hypoalgesia in pain-free adults and adults with musculoskeletal pain: A systematic review
- Noninvasive transcranial brain stimulation in central post-stroke pain: A systematic review
- Short Communications
- Are we missing the opioid consumption in low- and middle-income countries?
- Association between self-reported pain severity and characteristics of United States adults (age ≥50 years) who used opioids
- Could generative artificial intelligence replace fieldwork in pain research?
- Skin conductance algesimeter is unreliable during sudden perioperative temperature increases
- Original Experimental
- Confirmatory study of the usefulness of quantum molecular resonance and microdissectomy for the treatment of lumbar radiculopathy in a prospective cohort at 6 months follow-up
- Pain catastrophizing in the elderly: An experimental pain study
- Improving general practice management of patients with chronic musculoskeletal pain: Interdisciplinarity, coherence, and concerns
- Concurrent validity of dynamic bedside quantitative sensory testing paradigms in breast cancer survivors with persistent pain
- Transcranial direct current stimulation is more effective than pregabalin in controlling nociceptive and anxiety-like behaviors in a rat fibromyalgia-like model
- Paradox pain sensitivity using cuff pressure or algometer testing in patients with hemophilia
- Physical activity with person-centered guidance supported by a digital platform or with telephone follow-up for persons with chronic widespread pain: Health economic considerations along a randomized controlled trial
- Measuring pain intensity through physical interaction in an experimental model of cold-induced pain: A method comparison study
- Pharmacological treatment of pain in Swedish nursing homes: Prevalence and associations with cognitive impairment and depressive mood
- Neck and shoulder pain and inflammatory biomarkers in plasma among forklift truck operators – A case–control study
- The effect of social exclusion on pain perception and heart rate variability in healthy controls and somatoform pain patients
- Revisiting opioid toxicity: Cellular effects of six commonly used opioids
- Letter to the Editor
- Post cholecystectomy pain syndrome: Letter to Editor
- Response to the Letter by Prof Bordoni
- Response – Reliability and measurement error of exercise-induced hypoalgesia
- Is the skin conductance algesimeter index influenced by temperature?
- Skin conductance algesimeter is unreliable during sudden perioperative temperature increase
- Corrigendum
- Corrigendum to “Chronic post-thoracotomy pain after lung cancer surgery: a prospective study of preoperative risk factors”
- Obituary
- A Significant Voice in Pain Research Björn Gerdle in Memoriam (1953–2024)

