Abstract
Objectives
Pain assessment in anesthetized and non-communicative patients remains a challenge. Clinical signs such as tachycardia, hypertension, sweat and tears, have a low specificity for pain and should therefore ideally be replaced by more specific monitoring techniques. Skin conductance variability has been demonstrated to establish a patients’ sensitivity to pain, but may be influenced by temperature changes that leads to profuse sweating. The aim of this pilot study was to test skin conductance changes during sudden temperature changes due to hyperthermic intraperitoneal chemotherapy (HIPEC) perfusation.
Methods
We investigated skin conductance algesimeter (SCA) in ten consecutive patients undergoing cytoreductive surgery and HIPEC. Results from the SCA was compared to other standard physiological variables at seven time points during the surgical procedure, in particular during the period with hyperthermic intraabdominal perfusion leading to an increase in the patients core temperature.
Results
Nine out of ten patients had an increase in the SCA measurements during the HIPEC phase correlating the increase in temperature.
Conclusion
SCA is unreliable to detect increased pain sensation during sudden perioperative temperature changes in adult patients.
1 Introduction
General anesthesia consists of hypnosis, analgesia, and areflexia. The administration of hypnotic agents is used to prevent awareness, the analgesics to prevent autonomic and somatic responses, and muscle relaxants to prevent reflex movements [1]. Different commercial devices have been developed to monitor depth of anesthesia, like bispectral index spectroscopy (BIS) [2], auditory evoked potential [3], and state entropy [4]. These are based on analyses of the electroencephalography signal [5] and seem to be more related to the hypnotic state of the patient than to anti-nociception perceived as pain or physiological stress induced by noxious stimuli. Nevertheless, pain assessment in anesthetized and non-communicative patients remains a problem. Use of clinical signs such as tachycardia, hypertension, sweat, and tears, has a low specificity for pain and should therefore ideally be replaced by a more specific monitoring technique [6]. At least four methods are commercially available [7]: pupillometry [8], analgesia/nociception index [9,10], surgical pleth index [11], and the skin conductance algesimeter (SCA) [12–15]. These techniques assess nociception and anti-nociception through the balance between activity of the sympathetic and parasympathetic nervous system.
The SCA is a non-invasive electronic conductance meter for detecting skin conductance changes on palmar and plantar skin sites to determine a patients sensitivity to pain [16,17]. The SCA device is a class II A medical device. It is IP-protected and CE-certified. The SCA reflects the sympathetic nervous system, influenced by changes in emotions. Release of acetylcholine acts on muscarinic receptors, causing a subsequent burst of sweat and increased skin conductance. The SCA reacts immediately and is not influenced by hemodynamic variability or neuromuscular blockade. Skin conductance measured in the palmar region reflect the emotional part of the autonomous nervous system [12,13,15]. SCA registration ≥0.20 peaks per second have been shown to indicate moderate or severe pain in the postoperative setting. Skin conductance variability to assess pain has, however, shown varying results. Furthermore, skin conductance variability may be influenced by temperature changes that leads to profuse sweating [18].
Cytoreductive surgery-hyperthermic intraperitoneal chemotherapy (CRS-HIPEC) [19] is a national service for Norway located at the Norwegian Radium Hospital for treatment of peritoneal metastasis in certain intraabdominal cancers. Macroscopic cancerous tumours are surgically removed, and then heated chemotherapy drugs are applied intraperitonally in the abdomen to eliminate the remaining cancerous cells lining the peritoneum and remaining free tumour clusters. During the hyperthermic intraperitoneal chemotherapy (HIPEC) phase, the patients usually develop raised core body temperature up to 40.5°C due to the hyperthermic perfusate (with a temperature of 43–44.0°C) resulting in a median temperature of 42.0°C inside the abdominal cavity. Although different procedures to control patient temperature are used, raised patient temperatures are expected. Raised temperature can lead to excessive sweating. Excessive sweating can influence SCA [18,20].
The aim of this pilot study was to test SCA during the hyperthermic perfusate period, and whether this method is influenced by the patient temperature changes and not variations in noxious stimuli during general anesthesia.
2 Methods
We investigated SCA in ten consecutive HIPEC patients in this pilot study. A SCA from MedStorm Innovation AS was used as described by the manufacturer. Electrodes were attached on the palm of hand and the pain sensor attached to the wrist of the patient. The algesimeter collected, measured, and calculated data from the sensor and transferred the results by Bluetooth Low Energy connectivity to a tablet for display. The measured conductive peaks per second are reflected in the SCA index. The index is expressed numerically from 1 to 10, 1 being low probability of pain and 10 gives high probability of pain. SCA measurements were performed at seven different time points (Figure 1). To compare the results from the SCA with other physiological variables, measurements of oesophageal temperature, arterial blood pressure, pulse, minimal alveolar concentration (MAC) of inhalation agents, BIS, epidural infusions, remifentanil infusion (if used), and accumulated fentanyl at seven time points during the surgical procedure were recorded. These physiological variables and medication dosing are routinely used and registered during CRS-HIPEC at the Norwegian Radium Hospital.
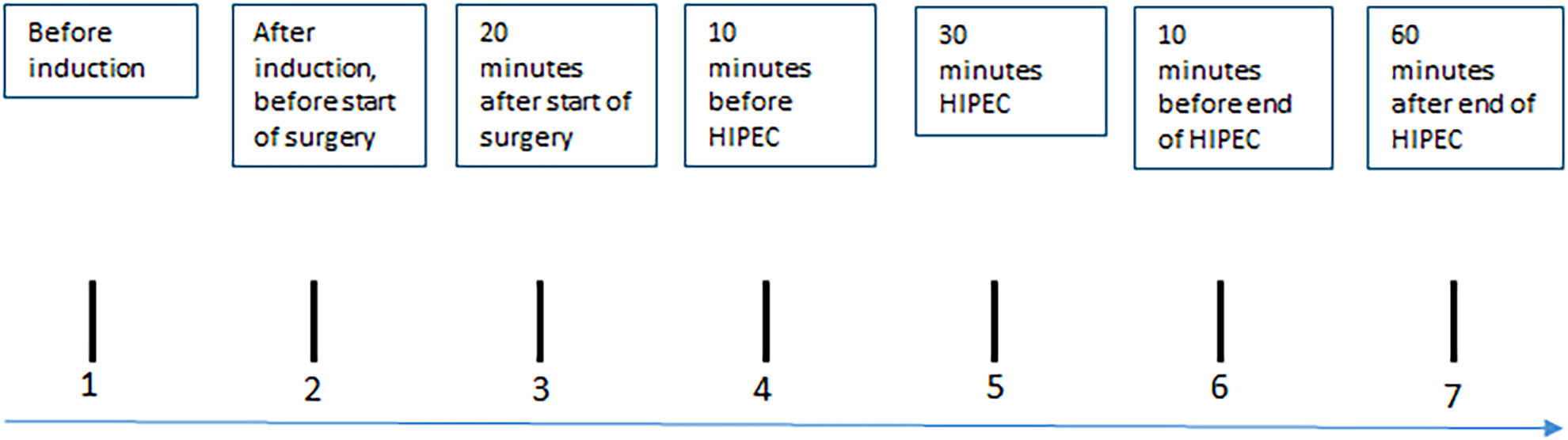
Flow diagram with time points for SCA measurements, oesophageal temperature, and other physiological variables.
General anaesthesia was induced with fentanyl and propofol. Muscle relaxation was obtained with rocuronium bromide with incremental doses guided by neuromuscular monitoring. Anaesthesia was maintained with fentanyl, remifentanil, and desflurane. All patients had a thoracic epidural catheter inserted before the start of anaesthesia, and all patients had a continuous epidural infusion with a standard solution (bupivacaine 1 mg/mL, fentanyl 2 µg/mL, and adrenaline 2 µg/mL) activated before the start of surgery and maintained throughout the procedure. All patients received a bolus before the start of epidural infusion. Rate of epidural infusion was not standardized, but was adjusted according to vital parameters at the discretion of the attending anaesthesiologist.
The study was approved by the local representative for the Norwegian Data Protection Authority (case number 23/05469).
3 Results
Six female and four male patients were included. Medium weight was 68 kg (quartiles: 58, 81) and median age was 65 years (quartiles: 63, 67). All patients had an increase in temperature during the HIPEC procedure (median increase from 36.2 to 38.4°C (Figure 2 and Table 1). Nine out of ten patients had an increase in SCA measurements during the HIPEC procedure (Figure 3 and Table 1) with a median SCA signal of 8 during maximum temperature increase. There were no clinical signs indicating that the patients had an increased pain sensation during the HIPEC procedure (Table 1). None of the patients received additional bolus or change in the rate of epidural infusions, nor did they receive additional opioids during the HIPEC procedure. At time point 6 (10 min before end of HIPEC) we registered a median accumulated fentanyl dose of 375 mcg (quartiles: 350, 440), a median accumulated remifentanil dose of 0.6 mcg (quartiles: 0.0, 25.9), a median accumulated epidural infusion volume of 70 mL (quartiles: 56, 81), and a MAC of 0.9 (quartiles: 0.8, 1.0).

Oesophageal temperature changes (°C) at different time points during surgery and HIPEC.
SCA measruements and physiological variables
| Time point 1 | Time point 2 | Time point 3 | Time point 4 | Time point 5 | Time point 6 | Time point 7 | |
|---|---|---|---|---|---|---|---|
| SCA | 2 (1, 6) | 0 (0, 0) | 0 (0, 5) | 0 (0, 7) | 0 (0, 0) | 8 (3, 10) | 0 (0, 3) |
| Oesophageal temperature | 36.2 (35.9, 36.4) | 36.1 (35.7, 36.4) | 36.4 (36.2, 36.6) | 37.6 (37.3, 37.7) | 38.4 (38.0, 38.5) | 37.9 (37.7, 37.9) | |
| MAP | 71 (64, 76) | 72 (65, 101) | 75 (71, 85) | 66 (63, 69) | 66 (63, 73) | 70 (65, 73) | |
| Pulse | 77 (59, 75) | 75 (65, 84) | 77 (65, 83) | 77 (66, 80) | 84 (70, 88) | 84 (73, 90) | |
| BIS | 37 (31, 48) | 35 (31, 41) | 40 (30, 50) | 44 (30, 54) | 40 (33, 47) | 38 (34, 53) | |
| MAC | 0.9 (0.8, 1.0) | 1.0 (0.9, 1.0) | 1.0 (0.9, 1.0) | 1.0 (0.9, 1.0) | 1.0 (0.9, 1.0) | 0.9 (0.3, 1.0) |
SCA measurements and different physiological variables at specific time points according to protocol. Median values with 25 and 75 percentiles in parenthesis. SCA = skin conductance algesimeter; MAP = mean arterial pressure; BIS = bispectral index; MAC = minimum alveolar concentration.
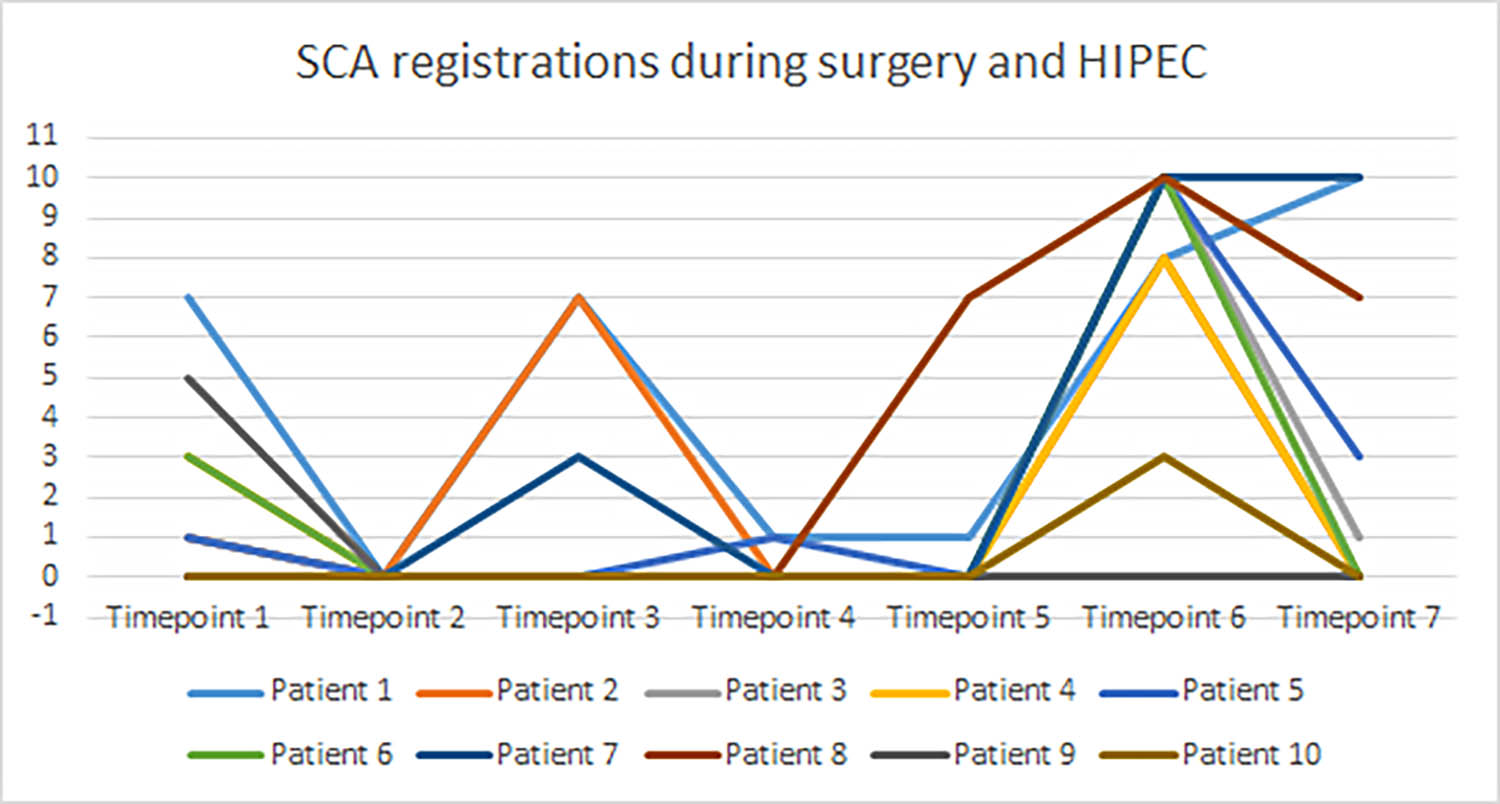
SCA measurements at different time points during surger and HIPEC.
4 Discussion
Nine out of ten patients had an increase in the SCA measurements during the HIPEC phase correlating the increase in temperature.
During the HIPEC procedure, catheters and suction drains are placed into the abdominal cavity and connected to a perfusion machine in a closed circuit system. To increase the effect of chemotherapy drugs, the solution is heated up to 43–44°C attempting to have median 42°C in the outflow abdominal catheter. The perfusion is maintained for 90 min and as a consequence, the patient core temperature increases. During this phase, the patients are not exposed to surgical stimuli.
Since the patients were not exposed to surgical pain stimuli during the HIPEC phase (besides the abdominal perfusion of heated chemotherapy drugs), while maintaining a stable anaesthesia level, we suspect that the increase in the SCA measurements were caused by the increase in core and skin temperature. It can be argued that the abdominal perfusion of chemotherapy can cause peritoneal inflammation and thus pain [21]. However, peritoneal inflammatory pain and neuropathic pain components will probably take some time to develop [21]. Furthermore, all patients received continuous thoracic epidural analgesia to reduce nociception from the abdomen which has been demonstrated to give adequate analgesic effect in patients with CRS-HIPEC [22]. In addition, there was no increase in blood pressure and only a minor increase in heart rate (probably due to increase in temperature [23]) during the HIPEC phase (Table 1).
Thermoregulation is a homeostatic process that maintains a steady internal body temperature despite changes in external conditions. The body responds by dissipating heat by activating sympathetic cholinergic fibers innervating sweat glands, leading to increased sweat and heat loss [24].
Abnormal temperature regulation and defects in sweat production in the body can indicate a dysfunction in the autonomic nervous system in a number of clinical conditions including hyperhidrosis, small fiber and autonomic neuropathies, multiple system atrophy, Parkinson disease with autonomic dysfunction, and pure autonomic failure [24].
Excessive sweating has also been observed following intrathecal morphine administration [25].
Whether increased sweating in the clinical situations mentioned above also effects SCA measurements remains to be seen.
Since the use of clinical signs such as tachycardia, hypertension, sweat, tears, and pupillary reactions, has a low specificity for pain, different monitoring techniques have been developed [1,7]. Accurate real-time acquisition and analysis of patients’ response to surgically induced nociception would provide an efficient way to continuously assess the response of analgesics in order to suppress nociception and avoid under or over-dose of anesthetics. If 100% reliable, such a monitoring device would represent a “holy grail” in personalized drug administration [26]. Today, these monitoring devices all have some limitations. According to Banerjee and MacDougall [1], there appeared to be no statistically significant difference between nociception monitoring and standard monitoring with respect to intraoperative adverse events, postoperative opioid or analgesic consumption, postoperative pain, and postoperative adverse events. Thus, it is important to be aware of flaws and imperfections in each apparatus, as pointed out in this report regarding SCA in HIPEC patients during temperature increase.
5 Conclusion
With this pilot study we have demonstrated that SCA is unreliable during sudden perioperative temperature changes in adult patients. From our data, we cannot conclude that skin conductance changes are influenced by changes in temperature in other clinical conditions or in other age groups.
-
Research ethics: The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). Research data were part of a quality assurance project and thus exempted from REC (Regional Ethics Committee) approval in agreement with national and local research guidelines. The study was approved by the local representative of the Norwegian Data Protection Authority (case number 23/050469).
-
Informed consent: Not applicable.
-
Author contributions: All authors have contributed in writing and have approved the final manuscript.
-
Competing interests: Ulf E. Kongsgaard is section editor for Scandinavian Journal of Pain (Clinical sciences: cancer-related pain). The authors declare no conflict of interest.
-
Research funding: This study had internal funding only.
-
Data availability: The raw data can be obtained on request from the corresponding author.
-
Artificial intelligence/Machine learning tools: Not applicable.
References
[1] Banerjee S, MacDougall D. CADTH rapid response reports, in nociception monitoring for general anesthesia: A review of clinical effectiveness, Cost-effectiveness, and guidelines. 2018, Canadian Agency for Drugs and Technologies in Health Health Nociception Monitoring for General Anesthesia. https://pubmed.ncbi.nlm.nih.gov/30855764/. Assessed 25 September 2023.Search in Google Scholar
[2] Bard JW. The BIS monitor: a review and technology assessment. AANA J. 2001;69(6):477–83.Search in Google Scholar
[3] De Cosmo G, Aceto P, Clemente A, Congedo E. Auditory evoked potentials. Minerva Anestesiol. 2004;70(5):293–7.Search in Google Scholar
[4] Shepherd J, Jones J, Frampton G, Bryant J, Baxter L, Cooper K. Clinical effectiveness and cost-effectiveness of depth of anaesthesia monitoring (E-entropy, bispectral index and narcotrend): a systematic review and economic evaluation. Health Technol Assess. 2013;17(34):1–264.10.3310/hta17340Search in Google Scholar PubMed PubMed Central
[5] Roche D, Mahon P. Depth of anesthesia monitoring. Anesthesiol Clin. 2021;39(3):477–92.10.1016/j.anclin.2021.04.004Search in Google Scholar PubMed
[6] Ben-Israel N, Kliger M, Zuckerman G, Katz Y, Edry R. Monitoring the nociception level: a multi-parameter approach. J Clin Monit Comput. 2013;27(6):659–68.10.1007/s10877-013-9487-9Search in Google Scholar PubMed
[7] Ledowski T. Objective monitoring of nociception: a review of current commercial solutions. Br J Anaesth. 2019;123(2):e312–21.10.1016/j.bja.2019.03.024Search in Google Scholar PubMed PubMed Central
[8] Kim JH, Jwa EK, Choung Y, Yeon HJ, Kim SY, Kim E. Comparison of pupillometry with surgical pleth index monitoring on perioperative opioid consumption and nociception during propofol-remifentanil anesthesia: a prospective randomized controlled trial. Anesth Analg. 2020;131(5):1589–98.10.1213/ANE.0000000000004958Search in Google Scholar PubMed
[9] Edry R, Recea V, Dikust Y, Sessler DI. Preliminary intraoperative validation of the nociception level index: a noninvasive nociception monitor. Anesthesiology. 2016;125(1):193–203.10.1097/ALN.0000000000001130Search in Google Scholar PubMed
[10] Gélinas C, Shahiri T S, Richard-Lalonde M, Laporta D, Morin JF, Boitor M, et al. Exploration of a multi-parameter technology for pain assessment in postoperative patients after cardiac surgery in the intensive care unit: the nociception level index (NOL)(TM). J Pain Res. 2021;14:3723–31.10.2147/JPR.S332845Search in Google Scholar PubMed PubMed Central
[11] Guo J, Zhu W, Shi Q, Bao F, Xu J. Effect of surgical pleth index-guided analgesia versus conventional analgesia techniques on fentanyl consumption under multimodal analgesia in laparoscopic cholecystectomy: a prospective, randomized and controlled study. BMC Anesthesiol. 2021;21(1):167.10.1186/s12871-021-01366-xSearch in Google Scholar PubMed PubMed Central
[12] Storm H. Changes in skin conductance as a tool to monitor nociceptive stimulation and pain. Curr Opin Anaesthesiol. 2008;21(6):796–804.10.1097/ACO.0b013e3283183fe4Search in Google Scholar PubMed
[13] Storm H, Støen R, Klepstad P, Skorpen F, Qvigstad E, Raeder J. Nociceptive stimuli responses at different levels of general anaesthesia and genetic variability. Acta Anaesthesiol Scand. 2013;57(1):89–99.10.1111/aas.12017Search in Google Scholar PubMed
[14] Gjerstad AC, Storm H, Hagen R, Huiku M, Qvigstad E, Raeder J. Comparison of skin conductance with entropy during intubation, tetanic stimulation and emergence from general anaesthesia. Acta Anaesthesiol Scand. 2007;51(1):8–15.10.1111/j.1399-6576.2006.01189.xSearch in Google Scholar PubMed
[15] Storm H, Shafiei M, Myre K, Raeder J. Palmar skin conductance compared to a developed stress score and to noxious and awakening stimuli on patients in anaesthesia. Acta Anaesthesiol Scand. 2005;49(6):798–803.10.1111/j.1399-6576.2005.00665.xSearch in Google Scholar PubMed
[16] Storm H, Myre K, Rostrup M, Stokland O, Lien MD, Raeder JC. Skin conductance correlates with perioperative stress. Acta Anaesthesiol Scand. 2002;46(7):887–95.10.1034/j.1399-6576.2002.460721.xSearch in Google Scholar PubMed
[17] Storm H, Fremming A, Odegaard S, Martinsen OG, Morkrid L. The development of a software program for analyzing spontaneous and externally elicited skin conductance changes in infants and adults. Clin Neurophysiol. 2000;111(10):1889–98.10.1016/S1388-2457(00)00421-1Search in Google Scholar PubMed
[18] Valkenburg AJ, Niehof SP, van Dijk M, Verhaar EJ, Tibboel D. Skin conductance peaks could result from changes in vital parameters unrelated to pain. Pediatr Res. 2012;71(4 Pt 1):375–9.10.1038/pr.2011.72Search in Google Scholar PubMed
[19] Morano WF, Khalili M, Chi DS, Bowne WB, Esquivel J. Clinical studies in CRS and HIPEC: trials, tribulations, and future directions – a systematic review. J Surg Oncol. 2018;117(2):245–59.10.1002/jso.24813Search in Google Scholar PubMed PubMed Central
[20] Ogawa T, Terada E, Kobyayashi M, Takagi K. Variations of the electric conductivity of the skin in relation to sweating. Jpn J Physiol. 1965;15:14–309.10.2170/jjphysiol.15.296Search in Google Scholar
[21] Wang X, Li T. Postoperative pain pathophysiology and treatment strategies after CRS + HIPEC for peritoneal cancer. World J Surg Oncol. 2020;18(1):62.10.1186/s12957-020-01842-7Search in Google Scholar PubMed PubMed Central
[22] Piccioni F, Casiraghi C, Fumagalli L, Kusamura S, Baratti D, Deraco M, et al. Epidural analgesia for cytoreductive surgery with peritonectomy and heated intraperitoneal chemotherapy. Int J Surg. 2015;16(Pt A):99–106.10.1016/j.ijsu.2015.02.025Search in Google Scholar PubMed
[23] Kim MH, Yoo YC, Bai SJ, Lee KY, Kim N, Lee KY. Physiologic and hemodynamic changes in patients undergoing open abdominal cytoreductive surgery with hyperthermic intraperitoneal chemotherapy. J Int Med Res. 2021;49(1):300060520983263.10.1177/0300060520983263Search in Google Scholar PubMed PubMed Central
[24] Osilla EV, Marsidi JL, Schumway KR, Sharma S. Physiology, temperature regulation. In StatPearls. Treasure Island (FL), USA; 2023. https://www.ncbi.nlm.nih.gov/books/NBK507838/Assessed 25 September 2023.Search in Google Scholar
[25] Ferraz S, Caria T, Da Silva AV, Candeias MJ, Cenicante T. Persistent hypothermia and excessive sweating following intrathecal morphine administration in a teenage boy: a case report. Anesth Pain Med. 2018;8(1):e66724.10.5812/aapm.66724Search in Google Scholar PubMed PubMed Central
[26] De Jonckheere J, Bonhomme V, Jeanne M, Boselli E, Gruenewald M, Logier R, et al. Physiological signal processing for individualized anti-nociception management during general anesthesia: a review. Yearb Med Inf. 2015;10(1):95–101.10.15265/IY-2015-004Search in Google Scholar PubMed PubMed Central
© 2024 the author(s), published by De Gruyter
This work is licensed under the Creative Commons Attribution 4.0 International License.
Articles in the same Issue
- Editorial Comment
- From pain to relief: Exploring the consistency of exercise-induced hypoalgesia
- Christmas greetings 2024 from the Editor-in-Chief
- Original Articles
- The Scandinavian Society for the Study of Pain 2022 Postgraduate Course and Annual Scientific (SASP 2022) Meeting 12th to 14th October at Rigshospitalet, Copenhagen
- Comparison of ultrasound-guided continuous erector spinae plane block versus continuous paravertebral block for postoperative analgesia in patients undergoing proximal femur surgeries
- Clinical Pain Researches
- The effect of tourniquet use on postoperative opioid consumption after ankle fracture surgery – a retrospective cohort study
- Changes in pain, daily occupations, lifestyle, and health following an occupational therapy lifestyle intervention: a secondary analysis from a feasibility study in patients with chronic high-impact pain
- Tonic cuff pressure pain sensitivity in chronic pain patients and its relation to self-reported physical activity
- Reliability, construct validity, and factorial structure of a Swedish version of the medical outcomes study social support survey (MOS-SSS) in patients with chronic pain
- Hurdles and potentials when implementing internet-delivered Acceptance and commitment therapy for chronic pain: a retrospective appraisal using the Quality implementation framework
- Exploring the outcome “days with bothersome pain” and its association with pain intensity, disability, and quality of life
- Fatigue and cognitive fatigability in patients with chronic pain
- The Swedish version of the pain self-efficacy questionnaire short form, PSEQ-2SV: Cultural adaptation and psychometric evaluation in a population of patients with musculoskeletal disorders
- Pain coping and catastrophizing in youth with and without cerebral palsy
- Neuropathic pain after surgery – A clinical validation study and assessment of accuracy measures of the 5-item NeuPPS scale
- Translation, contextual adaptation, and reliability of the Danish Concept of Pain Inventory (COPI-Adult (DK)) – A self-reported outcome measure
- Cosmetic surgery and associated chronic postsurgical pain: A cross-sectional study from Norway
- The association of hemodynamic parameters and clinical demographic variables with acute postoperative pain in female oncological breast surgery patients: A retrospective cohort study
- Healthcare professionals’ experiences of interdisciplinary collaboration in pain centres – A qualitative study
- Effects of deep brain stimulation and verbal suggestions on pain in Parkinson’s disease
- Painful differences between different pain scale assessments: The outcome of assessed pain is a matter of the choices of scale and statistics
- Prevalence and characteristics of fibromyalgia according to three fibromyalgia diagnostic criteria: A secondary analysis study
- Sex moderates the association between quantitative sensory testing and acute and chronic pain after total knee/hip arthroplasty
- Tramadol-paracetamol for postoperative pain after spine surgery – A randomized, double-blind, placebo-controlled study
- Cancer-related pain experienced in daily life is difficult to communicate and to manage – for patients and for professionals
- Making sense of pain in inflammatory bowel disease (IBD): A qualitative study
- Patient-reported pain, satisfaction, adverse effects, and deviations from ambulatory surgery pain medication
- Does pain influence cognitive performance in patients with mild traumatic brain injury?
- Hypocapnia in women with fibromyalgia
- Application of ultrasound-guided thoracic paravertebral block or intercostal nerve block for acute herpes zoster and prevention of post-herpetic neuralgia: A case–control retrospective trial
- Translation and examination of construct validity of the Danish version of the Tampa Scale for Kinesiophobia
- A positive scratch collapse test in anterior cutaneous nerve entrapment syndrome indicates its neuropathic character
- ADHD-pain: Characteristics of chronic pain and association with muscular dysregulation in adults with ADHD
- The relationship between changes in pain intensity and functional disability in persistent disabling low back pain during a course of cognitive functional therapy
- Intrathecal pain treatment for severe pain in patients with terminal cancer: A retrospective analysis of treatment-related complications and side effects
- Psychometric evaluation of the Danish version of the Pain Self-Efficacy Questionnaire in patients with subacute and chronic low back pain
- Dimensionality, reliability, and validity of the Finnish version of the pain catastrophizing scale in chronic low back pain
- To speak or not to speak? A secondary data analysis to further explore the context-insensitive avoidance scale
- Pain catastrophizing levels differentiate between common diseases with pain: HIV, fibromyalgia, complex regional pain syndrome, and breast cancer survivors
- Prevalence of substance use disorder diagnoses in patients with chronic pain receiving reimbursed opioids: An epidemiological study of four Norwegian health registries
- Pain perception while listening to thrash heavy metal vs relaxing music at a heavy metal festival – the CoPainHell study – a factorial randomized non-blinded crossover trial
- Observational Studies
- Cutaneous nerve biopsy in patients with symptoms of small fiber neuropathy: a retrospective study
- The incidence of post cholecystectomy pain (PCP) syndrome at 12 months following laparoscopic cholecystectomy: a prospective evaluation in 200 patients
- Associations between psychological flexibility and daily functioning in endometriosis-related pain
- Relationship between perfectionism, overactivity, pain severity, and pain interference in individuals with chronic pain: A cross-lagged panel model analysis
- Access to psychological treatment for chronic cancer-related pain in Sweden
- Validation of the Danish version of the knowledge and attitudes survey regarding pain
- Associations between cognitive test scores and pain tolerance: The Tromsø study
- Healthcare experiences of fibromyalgia patients and their associations with satisfaction and pain relief. A patient survey
- Video interpretation in a medical spine clinic: A descriptive study of a diverse population and intervention
- Role of history of traumatic life experiences in current psychosomatic manifestations
- Social determinants of health in adults with whiplash associated disorders
- Which patients with chronic low back pain respond favorably to multidisciplinary rehabilitation? A secondary analysis of a randomized controlled trial
- A preliminary examination of the effects of childhood abuse and resilience on pain and physical functioning in patients with knee osteoarthritis
- Differences in risk factors for flare-ups in patients with lumbar radicular pain may depend on the definition of flare
- Real-world evidence evaluation on consumer experience and prescription journey of diclofenac gel in Sweden
- Patient characteristics in relation to opioid exposure in a chronic non-cancer pain population
- Topical Reviews
- Bridging the translational gap: adenosine as a modulator of neuropathic pain in preclinical models and humans
- What do we know about Indigenous Peoples with low back pain around the world? A topical review
- The “future” pain clinician: Competencies needed to provide psychologically informed care
- Systematic Reviews
- Pain management for persistent pain post radiotherapy in head and neck cancers: systematic review
- High-frequency, high-intensity transcutaneous electrical nerve stimulation compared with opioids for pain relief after gynecological surgery: a systematic review and meta-analysis
- Reliability and measurement error of exercise-induced hypoalgesia in pain-free adults and adults with musculoskeletal pain: A systematic review
- Noninvasive transcranial brain stimulation in central post-stroke pain: A systematic review
- Short Communications
- Are we missing the opioid consumption in low- and middle-income countries?
- Association between self-reported pain severity and characteristics of United States adults (age ≥50 years) who used opioids
- Could generative artificial intelligence replace fieldwork in pain research?
- Skin conductance algesimeter is unreliable during sudden perioperative temperature increases
- Original Experimental
- Confirmatory study of the usefulness of quantum molecular resonance and microdissectomy for the treatment of lumbar radiculopathy in a prospective cohort at 6 months follow-up
- Pain catastrophizing in the elderly: An experimental pain study
- Improving general practice management of patients with chronic musculoskeletal pain: Interdisciplinarity, coherence, and concerns
- Concurrent validity of dynamic bedside quantitative sensory testing paradigms in breast cancer survivors with persistent pain
- Transcranial direct current stimulation is more effective than pregabalin in controlling nociceptive and anxiety-like behaviors in a rat fibromyalgia-like model
- Paradox pain sensitivity using cuff pressure or algometer testing in patients with hemophilia
- Physical activity with person-centered guidance supported by a digital platform or with telephone follow-up for persons with chronic widespread pain: Health economic considerations along a randomized controlled trial
- Measuring pain intensity through physical interaction in an experimental model of cold-induced pain: A method comparison study
- Pharmacological treatment of pain in Swedish nursing homes: Prevalence and associations with cognitive impairment and depressive mood
- Neck and shoulder pain and inflammatory biomarkers in plasma among forklift truck operators – A case–control study
- The effect of social exclusion on pain perception and heart rate variability in healthy controls and somatoform pain patients
- Revisiting opioid toxicity: Cellular effects of six commonly used opioids
- Letter to the Editor
- Post cholecystectomy pain syndrome: Letter to Editor
- Response to the Letter by Prof Bordoni
- Response – Reliability and measurement error of exercise-induced hypoalgesia
- Is the skin conductance algesimeter index influenced by temperature?
- Skin conductance algesimeter is unreliable during sudden perioperative temperature increase
- Corrigendum
- Corrigendum to “Chronic post-thoracotomy pain after lung cancer surgery: a prospective study of preoperative risk factors”
- Obituary
- A Significant Voice in Pain Research Björn Gerdle in Memoriam (1953–2024)
Articles in the same Issue
- Editorial Comment
- From pain to relief: Exploring the consistency of exercise-induced hypoalgesia
- Christmas greetings 2024 from the Editor-in-Chief
- Original Articles
- The Scandinavian Society for the Study of Pain 2022 Postgraduate Course and Annual Scientific (SASP 2022) Meeting 12th to 14th October at Rigshospitalet, Copenhagen
- Comparison of ultrasound-guided continuous erector spinae plane block versus continuous paravertebral block for postoperative analgesia in patients undergoing proximal femur surgeries
- Clinical Pain Researches
- The effect of tourniquet use on postoperative opioid consumption after ankle fracture surgery – a retrospective cohort study
- Changes in pain, daily occupations, lifestyle, and health following an occupational therapy lifestyle intervention: a secondary analysis from a feasibility study in patients with chronic high-impact pain
- Tonic cuff pressure pain sensitivity in chronic pain patients and its relation to self-reported physical activity
- Reliability, construct validity, and factorial structure of a Swedish version of the medical outcomes study social support survey (MOS-SSS) in patients with chronic pain
- Hurdles and potentials when implementing internet-delivered Acceptance and commitment therapy for chronic pain: a retrospective appraisal using the Quality implementation framework
- Exploring the outcome “days with bothersome pain” and its association with pain intensity, disability, and quality of life
- Fatigue and cognitive fatigability in patients with chronic pain
- The Swedish version of the pain self-efficacy questionnaire short form, PSEQ-2SV: Cultural adaptation and psychometric evaluation in a population of patients with musculoskeletal disorders
- Pain coping and catastrophizing in youth with and without cerebral palsy
- Neuropathic pain after surgery – A clinical validation study and assessment of accuracy measures of the 5-item NeuPPS scale
- Translation, contextual adaptation, and reliability of the Danish Concept of Pain Inventory (COPI-Adult (DK)) – A self-reported outcome measure
- Cosmetic surgery and associated chronic postsurgical pain: A cross-sectional study from Norway
- The association of hemodynamic parameters and clinical demographic variables with acute postoperative pain in female oncological breast surgery patients: A retrospective cohort study
- Healthcare professionals’ experiences of interdisciplinary collaboration in pain centres – A qualitative study
- Effects of deep brain stimulation and verbal suggestions on pain in Parkinson’s disease
- Painful differences between different pain scale assessments: The outcome of assessed pain is a matter of the choices of scale and statistics
- Prevalence and characteristics of fibromyalgia according to three fibromyalgia diagnostic criteria: A secondary analysis study
- Sex moderates the association between quantitative sensory testing and acute and chronic pain after total knee/hip arthroplasty
- Tramadol-paracetamol for postoperative pain after spine surgery – A randomized, double-blind, placebo-controlled study
- Cancer-related pain experienced in daily life is difficult to communicate and to manage – for patients and for professionals
- Making sense of pain in inflammatory bowel disease (IBD): A qualitative study
- Patient-reported pain, satisfaction, adverse effects, and deviations from ambulatory surgery pain medication
- Does pain influence cognitive performance in patients with mild traumatic brain injury?
- Hypocapnia in women with fibromyalgia
- Application of ultrasound-guided thoracic paravertebral block or intercostal nerve block for acute herpes zoster and prevention of post-herpetic neuralgia: A case–control retrospective trial
- Translation and examination of construct validity of the Danish version of the Tampa Scale for Kinesiophobia
- A positive scratch collapse test in anterior cutaneous nerve entrapment syndrome indicates its neuropathic character
- ADHD-pain: Characteristics of chronic pain and association with muscular dysregulation in adults with ADHD
- The relationship between changes in pain intensity and functional disability in persistent disabling low back pain during a course of cognitive functional therapy
- Intrathecal pain treatment for severe pain in patients with terminal cancer: A retrospective analysis of treatment-related complications and side effects
- Psychometric evaluation of the Danish version of the Pain Self-Efficacy Questionnaire in patients with subacute and chronic low back pain
- Dimensionality, reliability, and validity of the Finnish version of the pain catastrophizing scale in chronic low back pain
- To speak or not to speak? A secondary data analysis to further explore the context-insensitive avoidance scale
- Pain catastrophizing levels differentiate between common diseases with pain: HIV, fibromyalgia, complex regional pain syndrome, and breast cancer survivors
- Prevalence of substance use disorder diagnoses in patients with chronic pain receiving reimbursed opioids: An epidemiological study of four Norwegian health registries
- Pain perception while listening to thrash heavy metal vs relaxing music at a heavy metal festival – the CoPainHell study – a factorial randomized non-blinded crossover trial
- Observational Studies
- Cutaneous nerve biopsy in patients with symptoms of small fiber neuropathy: a retrospective study
- The incidence of post cholecystectomy pain (PCP) syndrome at 12 months following laparoscopic cholecystectomy: a prospective evaluation in 200 patients
- Associations between psychological flexibility and daily functioning in endometriosis-related pain
- Relationship between perfectionism, overactivity, pain severity, and pain interference in individuals with chronic pain: A cross-lagged panel model analysis
- Access to psychological treatment for chronic cancer-related pain in Sweden
- Validation of the Danish version of the knowledge and attitudes survey regarding pain
- Associations between cognitive test scores and pain tolerance: The Tromsø study
- Healthcare experiences of fibromyalgia patients and their associations with satisfaction and pain relief. A patient survey
- Video interpretation in a medical spine clinic: A descriptive study of a diverse population and intervention
- Role of history of traumatic life experiences in current psychosomatic manifestations
- Social determinants of health in adults with whiplash associated disorders
- Which patients with chronic low back pain respond favorably to multidisciplinary rehabilitation? A secondary analysis of a randomized controlled trial
- A preliminary examination of the effects of childhood abuse and resilience on pain and physical functioning in patients with knee osteoarthritis
- Differences in risk factors for flare-ups in patients with lumbar radicular pain may depend on the definition of flare
- Real-world evidence evaluation on consumer experience and prescription journey of diclofenac gel in Sweden
- Patient characteristics in relation to opioid exposure in a chronic non-cancer pain population
- Topical Reviews
- Bridging the translational gap: adenosine as a modulator of neuropathic pain in preclinical models and humans
- What do we know about Indigenous Peoples with low back pain around the world? A topical review
- The “future” pain clinician: Competencies needed to provide psychologically informed care
- Systematic Reviews
- Pain management for persistent pain post radiotherapy in head and neck cancers: systematic review
- High-frequency, high-intensity transcutaneous electrical nerve stimulation compared with opioids for pain relief after gynecological surgery: a systematic review and meta-analysis
- Reliability and measurement error of exercise-induced hypoalgesia in pain-free adults and adults with musculoskeletal pain: A systematic review
- Noninvasive transcranial brain stimulation in central post-stroke pain: A systematic review
- Short Communications
- Are we missing the opioid consumption in low- and middle-income countries?
- Association between self-reported pain severity and characteristics of United States adults (age ≥50 years) who used opioids
- Could generative artificial intelligence replace fieldwork in pain research?
- Skin conductance algesimeter is unreliable during sudden perioperative temperature increases
- Original Experimental
- Confirmatory study of the usefulness of quantum molecular resonance and microdissectomy for the treatment of lumbar radiculopathy in a prospective cohort at 6 months follow-up
- Pain catastrophizing in the elderly: An experimental pain study
- Improving general practice management of patients with chronic musculoskeletal pain: Interdisciplinarity, coherence, and concerns
- Concurrent validity of dynamic bedside quantitative sensory testing paradigms in breast cancer survivors with persistent pain
- Transcranial direct current stimulation is more effective than pregabalin in controlling nociceptive and anxiety-like behaviors in a rat fibromyalgia-like model
- Paradox pain sensitivity using cuff pressure or algometer testing in patients with hemophilia
- Physical activity with person-centered guidance supported by a digital platform or with telephone follow-up for persons with chronic widespread pain: Health economic considerations along a randomized controlled trial
- Measuring pain intensity through physical interaction in an experimental model of cold-induced pain: A method comparison study
- Pharmacological treatment of pain in Swedish nursing homes: Prevalence and associations with cognitive impairment and depressive mood
- Neck and shoulder pain and inflammatory biomarkers in plasma among forklift truck operators – A case–control study
- The effect of social exclusion on pain perception and heart rate variability in healthy controls and somatoform pain patients
- Revisiting opioid toxicity: Cellular effects of six commonly used opioids
- Letter to the Editor
- Post cholecystectomy pain syndrome: Letter to Editor
- Response to the Letter by Prof Bordoni
- Response – Reliability and measurement error of exercise-induced hypoalgesia
- Is the skin conductance algesimeter index influenced by temperature?
- Skin conductance algesimeter is unreliable during sudden perioperative temperature increase
- Corrigendum
- Corrigendum to “Chronic post-thoracotomy pain after lung cancer surgery: a prospective study of preoperative risk factors”
- Obituary
- A Significant Voice in Pain Research Björn Gerdle in Memoriam (1953–2024)

