Abstract
Objectives
There is an ongoing opioid crisis in the United States where the illicit and non-medical use of prescription opioids is associated with an increasing number of overdose deaths. Few studies have investigated opioid-induced effects on cell viability, and comparative studies are limited. Here, we examine the toxicity of six commonly used opioids: methadone, morphine, oxycodone, hydromorphone, ketobemidone, and fentanyl with respect to mitochondrial and membrane function in vitro.
Methods
The opioids were tested in four different cell cultures: primary cortical cell cultures, human neuroblastoma SH-SY5Y cells, and both differentiated and undifferentiated neuroblastoma/glioma hybrid NG108-15 cells. The mitochondrial activity was assessed using 3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide (MTT) assay and the membrane integrity was assessed by measuring the leakage of lactate dehydrogenase. To compare the different opioids, the toxic dose (TD50) was calculated.
Results
The results displayed a similar trend of opioid-reduced cell viability in all four cell cultures. The most toxic opioid was methadone, followed by fentanyl, while morphine was overall ranked as the least toxic opioid displaying little to no negative impact on cell viability. The remaining opioids varied in rank between the different cell types.
Conclusion
This in vitro study highlights opioid-dependent variations in toxicity across all four tested cell types, with methadone emerging as the most potent opioid.
Abbreviations
- dbcAMP
-
Dibutyryl cAMP
- DMEM
-
Dulbecco’s modified Eagle’s medium
- FBS
-
Fetal bovine serum
- TD50
-
Toxic dose 50%
- LDH
-
Lactate dehydrogenase
- MOR
-
Mu-opioid receptor
- MTT
-
3-(4,5-Dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide
- NBM
-
Neurobasal medium
- NMDA
-
N-methyl-d-aspartate
- PCC
-
Primary cortical cell
- RT
-
Room temperature
- TX
-
Triton-X 100
1 Introduction
Inappropriate prescription of opioids, as reported from several countries, is described as one of the main reasons for the dramatically increased opioid use and prescription-opioid-related mortality [1]. The actual recommendation from the International Association of Pain (IASP) is to use opioids in chronic pain patients sparsely and only in exceptional cases, in restricted doses, and only over a short period of time [2]. In the United States, the overall prevalence of overdose deaths increased from 8.2 to 32.6 deaths per 100,000 standard population from 2002 to 2022 [3]. There are also worrying trends seen in the Scandinavian countries, as oxycodone prescription has increased in Denmark, Norway, and Sweden [4,5], with recent data from Sweden showing a slight increase in oxycodone-related deaths [6].
The toxic effects associated with clinically used opioids generally involve effects associated with a negative impact on cell function, cell survival, cognition, and the immune system. For instance, acute treatment with morphine induces apoptosis in primary hippocampal cells from mice [7], and in NG108-15 cells, a mouse/rat hybrid neuroblastoma/glioma cell line [8]. Similar effects of methadone are also reported, where acute treatment with high concentrations of methadone causes cell death in both human-derived neuronal SH-SY5Y cells [9] and in primary cortical rat cells [10,11], possibly through an N-methyl-d-aspartate (NMDA) receptor-mediated pathway [11]. Furthermore, we have previously demonstrated that 100 µM of both methadone and fentanyl negatively affect mitochondrial viability as early as 90 min after exposure [12]. In addition, there is evidence that chronic treatment with morphine inhibits neurogenesis in rat hippocampus [13], induces apoptosis in the spinal cord of rats [14], and alters the volumetric size of different regions in the brain [15]. These effects on the brain may impact higher cognitive function, such as learning and memory, which several studies with methadone have demonstrated [16,17,18,19,20]. Similarly, opioid-induced cell death of immune cells may lead to a suppressed immune system, which is generally observed in patients treated with opioids [21,22].
However, evidence supporting the claim that opioids may impact cognitive function or cell viability is scarce and few comparative studies using different opioids exist. The present study therefore aims to explore the effects on cell viability in a comparative in vitro approach following a 24-h acute treatment of six commonly used opioids; methadone, morphine, oxycodone, hydromorphone, ketobemidone, and fentanyl, in four different neuronal cell cultures.
2 Materials and methods
The following cell cultures, with varying characteristics to represent a greater variability among cells, were used: primary rat cell cultures, undifferentiated and differentiated mouse/rat NG108-15 cells, and human undifferentiated SH-SY5Y cells. All cultures were incubated at 37°C with 5% CO₂ in a humidified incubator, and 96-well plates were precoated with 50 µg/mL poly-d-lysine (Sigma Aldrich).
2.1 Primary cortical cell (PCC) cultures
All animal experiments were approved by the Uppsala Animal Ethics Committee (5.8.18-18550/2018) according to Swedish guidelines regarding animal experiments (Animal Welfare Act SFS1998:56) and the European Communities directive (86/609/EEC).
Mixed PCCs were harvested from embryonic day 17 fetuses from pregnant Wistar rats (Charles River, Sulzfeld, Germany) as described elsewhere [23]. Briefly, cortical tissue was dissected and digested using 0.2 mg/mL trypsin (Sigma-Aldrich) for 10 min at 37°C. Tissues were centrifuged at 3,200 rpm for 3 min and trypsin was inhibited using 0.52 mg/mL trypsin inhibitor (Sigma-Aldrich) prior to mechanical dissociation. The cell pellet was resuspended in neurobasal medium (NBM; Thermo Fisher Scientific, Waltham, USA) containing 0.5 mM GlutaMAX™ (Thermo-Fisher Scientific), 2% (v/v) B27 (Thermo-Fisher Scientific), 100 U/mL penicillin/streptomycin (Thermo-Fisher Scientific), and 10% (v/v) fetal bovine serum (FBS; Thermo-Fisher Scientific). Cells were counted using Countess™II Automated Cell Counter (Thermo-Fisher Scientific) and seeded at 1 × 105 cells per well in 96-well plates. Media was replaced the next day with serum-free NBM + 2% B27. Cells grew for 7 days in vitro with a partial media change on day 4. The cultures contained approximately 84% neurons (beta-III tubulin-positive).
2.2 NG108-15 and SH-SY5Y cell lines
The NG108-15 cell line (kind gift from Dr. Malin Jarvius, Uppsala University) is a hybrid mix of mouse neuroblastoma and rat glioma [24] and the SH-SY5Y cell line (kind gift from Dr. Anne-Lie Svensson, Uppsala University) is derived from human neuroblastoma. Both of these cell lines share properties similar to neuronal cell cultures. NG108-15 cells were cultured in Dulbecco’s modified Eagle’s medium (DMEM, Thermo-Fisher Scientific) supplemented with 10% (v/v) FBS, 100 U/mL penicillin/streptomycin, and 2% (v/v) Gibco® HAT supplement (Thermo-Fisher Scientific) containing 5 mM sodium hypoxanthine, 20 µM aminopterin, and 0.8 µM thymidine. SH-SY5Y cells were cultured in a minimum essential medium (Thermo-Fisher Scientific) supplemented with 10% FBS and 100 U/mL penicillin/streptomycin. Media changes were performed every 2–3 days and cells were subcultured at approximately 80% confluency using 0.25% trypsin-EDTA (Thermo-Fisher Scientific). Prior to the start of the experiment, undifferentiated NG108-15 and SH-SY5Y cells were seeded to a 96-well plate at a density of 1.5 × 104 cells per well. The plates were placed in an incubator overnight to ensure proper adhesion to the wells. Additional 96-well plates with NG108-15 cells were cultured in differentiation media containing DMEM supplemented with 2% (v/v) FBS, 100 U/mL penicillin/streptomycin, and 1 mM dibutyryl cAMP (dbcAMP, Sigma-Aldrich) for 3 days. All experiments were performed within 10 passages.
2.3 Immunocytochemistry
For immunocytochemistry, cells were seeded to black 96-well plates. The cells were fixed with 4% paraformaldehyde for 15 min at room temperature (RT), permeabilized with Tween-20, and blocked using normal donkey serum (Sigma-Aldrich). To examine the mu-opioid receptor (MOR) expression in PCC, NG108-15, and SH-SY5Y cells, 1:100 of the rabbit anti-MOR (Abcam, Cambridge, USA) was added to the cells and incubated for one hour at RT. A fluorescent-conjugated secondary antibody (Alexa488, Sigma-Aldrich) was added and incubated for another hour in RT, protected from light. Lastly, cells were counterstained using nuclei marker 4′,6-diamidino-2-phenylindole (DAPI; Sigma-Aldrich). Images were acquired using ImageXpress (Molecular Devices, San Jose, USA) at 20× magnification. To evaluate MOR expression, control wells containing only the fluorescent-conjugated secondary antibody were added and images were visually compared.
2.4 Opioid treatment
The opioids methadone (Sigma-Aldrich), morphine (Apoteket AB, Stockholm, Sweden), oxycodone (Sigma-Aldrich), hydromorphone (Sigma-Aldrich), ketobemidone (Apoteket AB), and fentanyl (Sigma-Aldrich) were added to the cells at 1, 10, 100, and 1,000 µM in triplicates for 24 h. Control cells were treated with media only. As a positive control for cytotoxicity, 1% Triton X-100 (TX) was added in triplicates to ensure full functionality of the cell viability assays.
2.5 Mitochondrial function assay
The mitochondrial function was assessed using the 3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide (MTT) assay. Briefly, MTT is metabolized to a purple formazan product in active mitochondria and acts as a marker for mitochondrial function. After 24 h of opioid treatment, 1 mg/mL MTT (Sigma-Aldrich) was added to each well and incubated for 30 min prior to lysing the cells with dimethyl sulfoxide. The absorbance of the formazan product was quantified using a plate reader (FLUOstar Omega, Ortenberg, Germany) at 570 nm.
2.6 Membrane integrity assay
The membrane integrity was assessed using the lactate dehydrogenase (LDH) assay. Briefly, LDH is a cytosolic enzyme that is released from cells during membrane damage and therefore acts as a marker for membrane integrity. After 24 h of opioid treatment, 50 µL media from each well was transferred to a new empty 96-well plate. A cytotoxicity detection kit (Sigma-Aldrich) was prepared according to instructions from the manufacturer, added to each well, and incubated for 30 min at RT, protected from light. The reaction mix metabolizes LDH to a red formazan product, correlating to the amount of LDH present in cell media. To quantify the levels of membrane integrity, the absorbance of the red formazan product was detected at 492 nm using a plate reader.
2.7 Statistical analysis
Statistical analysis was conducted in GraphPad Prism (v.9.3.1). PCCs harvested from one individual rat, and cells from one NG108-15 or SH-SY5Y passage were each considered one culture (n = 1). Results were normalized to the percent of control to account for culture variability. Data were analyzed by non-linear regression to obtain a best-fit value of the toxic dose 50% (TD50) for each opioid, the dose causing severe dysfunction in 50% of the cell population. Data are presented as mean log TD50 ± standard deviation and mean TD50 in table format, and graph data points are presented as mean ± standard error of the mean (SEM). The calculated TD50 values were used to rank the toxicity of the different opioids.
3 Results
3.1 Immunocytochemistry
In all tested cell types, PCC cultures, NG108-15, and SH-SY5Y cell line, a clear MOR intensity was detected in the cell cytoplasm (Figure 1). These results confirm that the MOR is expressed in all tested cell types.
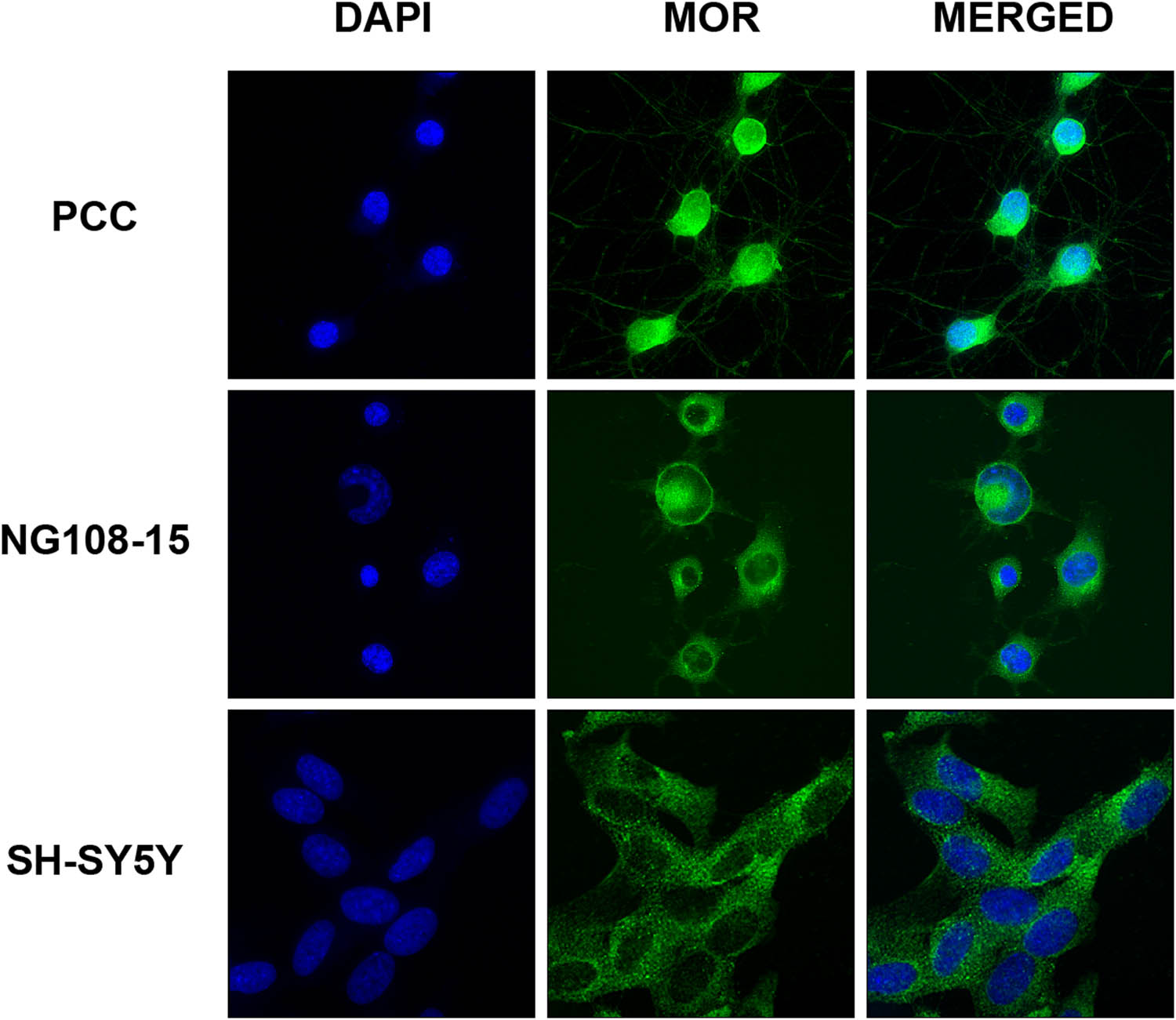
MOR immunocytochemistry. PCC cultures, NG108-15, and SH-SY5Y cells were exposed to a primary antibody targeting the MOR and visualized using a fluorescent-conjugated secondary antibody (Alexa 488). Cells were counterstained with the nuclei marker DAPI. Images were acquired using ImageXpress (Molecular Devices) mounted with a 20× objective and display a clear expression of the MOR in the cell cytoplasm in all tested cell types.
3.2 Mitochondrial function
The results of the calculated best-fit TD50 value from each opioid treatment and cell type (as assessed using the MTT assay) are presented in Table 1. For PCC cultures, undifferentiated and differentiated NG108-15 cells, and the SH-SY5Y cells, methadone treatment had the lowest calculated TD50 in comparison to the other opioids. Fentanyl treatment had the second lowest TD50 value followed by ketobemidone or oxycodone, depending on cell type. Morphine had the highest TD50 values of all the opioids in PCC cultures, differentiated NG108-15 cells, and SH-SY5Y cells and can be considered to induce little to no damage to the mitochondrial function. For undifferentiated NG108-15 cells, oxycodone had the highest TD50 value, although very similar to morphine. The nonlinear regression curves of the two opioids with the highest TD50 values (methadone and fentanyl), as well as the opioid with the lowest TD50 (morphine), are illustrated in Figure 2 while graphs of the other opioids (ketobemidone, oxycodone, and hydromorphone) are illustrated in Figure S1, Supplementary material.
Calculated best-fit values of mean log TD50 ± standard deviation and mean TD50 after nonlinear regression analysis of 3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide (MTT) metabolism in percentage of control (n = 4–5) after 24 h opioid treatment with methadone, fentanyl, oxycodone, hydromorphone, ketobemidone, and morphine in PCC, undifferentiated and differentiated NG108-15 cells, and SH-SY5Y cells
| Cell type | Opioid | Mean log TD50 ± SD | Mean TD50 |
|---|---|---|---|
| PCC cultures | Methadone | −3.76 ± 0.05 | 174 µM |
| Fentanyl | −3.54 ± 0.10 | 292 µM | |
| Oxycodone | −2.95 ± 0.13 | 1116 µM* | |
| Ketobemidone | −2.88 ± 0.13 | 1311 µM* | |
| Morphine | −2.27 ± 0.56 | 5382 µM* | |
| Hydromorphone | N/A** | N/A** | |
| Undifferentiated | Methadone | −4.25 ± 0.13 | 56 µM |
| NG108-15 | Fentanyl | −3.94 ± 0.10 | 115 µM |
| Ketobemidone | −3.52 ± 0.13 | 300 µM | |
| Hydromorphone | −3.15 ± 0.10 | 701 µM | |
| Morphine | −2.94 ± 0.08 | 1142 µM* | |
| Oxycodone | −2.94 ± 0.11 | 1158 µM* | |
| Differentiated | Methadone | −4.55 ± 0.09 | 28 µM |
| NG108-15 | Fentanyl | −4.03 ± 0.16 | 94 µM |
| Ketobemidone | −3.72 ± 0.11 | 189 µM | |
| Oxycodone | −3.27 ± 0.20 | 538 µM | |
| Hydromorphone | −3.09 ± 0.15 | 806 µM | |
| Morphine | −2.19 ± 0.88 | 6490 µM* | |
| Undifferentiated | Methadone | −4.18 ± 0.10 | 66 µM |
| SH-SY5Y | Fentanyl | −3.67 ± 0.10 | 213 µM |
| Ketobemidone | −3.52 ± 0.15 | 300 µM | |
| Oxycodone | −3.46 ± 0.14 | 350 µM | |
| Hydromorphone | −3.13 ± 0.09 | 735 µM | |
| Morphine | −2.99 ± 0.12 | 1016 µM* |
*Calculated theoretical value, mean TD50 exceeds highest concentration used.
**Calculated TD50 is not applicable due to ambiguous curve fit.

The effect of opioid treatment on mitochondrial activity. The level of 3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide (MTT) metabolism after 24 h treatment with the opioids methadone, fentanyl, and morphine in concentrations 1, 10, 100, and 1,000 µM was determined in (a) PCC cultures, (b) undifferentiated NG108-15 cells, (c) differentiated NG108-15 cells, and (d) undifferentiated SY-SY5Y cells. Data were normalized to percentage of control and nonlinear regression analysis was performed to determine the best-fit TD50 value for each opioid treatment. The nonlinear fit is shown in red and measured data points are shown in black as mean ± SEM from 4 to 5 different cultures (n = 4–5).
3.3 Membrane integrity
The opioid treatments induced low cytotoxicity and the nonlinear regression curves were ambiguous, and as a result, the TD50 values calculated from this assay were not applicable. Thus, the data from this assay are not included in the ranking of opioids and no further statistical analysis was performed. For a calculated mean percentage of cytotoxicity for control, 100 and 1,000 µM, see Table S1, Supplementary material.
4 Discussion
This study reveals differences in opioid-induced cell viability among methadone, morphine, oxycodone, hydromorphone, ketobemidone, and fentanyl. Both mitochondrial function and membrane integrity were assessed as markers for cell viability. Interestingly, the membrane integrity assay showed lower levels of cytotoxicity than the mitochondrial activity assay, and no stable TD50 value could be calculated. This suggests that acute opioid exposure more effectively reduces mitochondrial function compared to membrane integrity. There was a toxic effect of methadone at higher concentrations, but it was difficult to compare methadone with the different opioids.
Methadone treatment induced a higher degree of toxicity when compared to all the other opioids studied. In the mitochondrial function assay, the calculated TD50 value for methadone was the lowest in all four tested cell types, followed by fentanyl as the second lowest. The ranking of the other opioids (hydromorphone, morphine, ketobemidone, oxycodone) varied between the different cell types, but the highest TD50 value was found for oxycodone in undifferentiated NG108-15 and for morphine in the other three cell types. The overall ranking of the ability to decrease mitochondrial function in all different cell types was methadone > fentanyl > ketobemidone > oxycodone > hydromorphone > morphine. Since the four tested cell cultures originate from either rat, mouse, or human, and a similar toxicity profile was observed across the four cell cultures for the different opioids, this indicates that these opioid-induced effects occur in cells of both rodent and human origin.
All of the opioids in the present study display affinity to the MOR [25,26], which was confirmed in this study to be expressed in NG108-15, SH-SY5Y, and PCC cultures using immunocytochemistry. However, the MOR binding K i -values do not correlate with the degree of induced toxicity between the treatments. The affinity ranking, as described by Volpe and coworkers (excluding ketobemidone), is as follows: hydromorphone (0.3654 nM) > morphine (1.168 nM) > fentanyl (1.346 nM) > methadone (3.378 nM) > oxycodone (25.87 nM) [25]. The affinity K i -values for ketobemidone were not reported in this study but it is known that ketobemidone has a lower binding affinity for the MOR than morphine [27]. Interestingly, both morphine and hydromorphone display high affinity to the MOR but induce little to no effect on cell viability. This suggests that the cause of the opioid-induced toxicity demonstrated in the present study is not mediated via the MOR, but rather through other signaling pathways. The delta- or kappa-opioid receptor may be involved, but similar to the MOR, both morphine and hydromorphone display high affinity to these opioid receptors as well, in comparison to the other opioids [28,29,30].
Interestingly, methadone and ketobemidone, two of the most toxic opioids in this study, differ from the other opioids in regard to binding properties, as they are non-competitive antagonists to the NMDA receptor with K i -values of 0.85 and 26 µM, respectively [31]. It is likely that these opioids induce cell damage via the NMDA receptor when used in higher concentrations. We have previously reported that the opioid receptor antagonist naloxone is unable to prevent methadone-induced mitochondrial dysfunction and that the methadone-induced damage is associated with upregulated mRNA expression of NMDA receptor subunits [11] indicating that methadone-induced toxicity is linked to the NMDA receptor. Furthermore, activation of the NMDA receptor is suggested to be associated with opioid dependence and neuronal toxicity as prolonged treatment with morphine induces apoptosis via activation of the NMDA receptor in opioid-tolerant mice [14]. It is possible that regulation of the NMDA receptor plays a key role in opioid-induced effects on cell viability, as seen from the high doses of methadone treatment in this study, and that this can occur in opioid-tolerant patients consuming opioids long-term.
The results from the present study further confirm the in vitro toxicity profile of various opioids. Methadone has previously been shown to induce mitochondrial and membrane damage [10], induce necrosis [9], and upregulate pro-apoptotic proteins [16]. A recent study demonstrated impaired memory function as well as increased astrogliosis and decreased number of neurons in the hippocampus of male rats treated with methadone [32]. Thus, decreased cellular function may be one contributing factor to the reported methadone-induced cognitive dysfunction as seen in both rodents and humans [16,17,18,19]. Additionally, previous literature suggest that fentanyl induces cellular toxicity and decreases cell viability [33,34,35] which is further confirmed in this study. There are few studies describing the cell viability effects of oxycodone, hydromorphone, and ketobemidone. However, oxycodone has been reported to reduce cell viability in the human neuroblastoma cell line SH-SY5Y [36]. On the contrary, a recent study demonstrated that oxycodone did not affect mitochondrial function [37], and furthermore, using human hepatoma cells, oxycodone treatment did not impact membrane integrity [38]. A similar ambiguity with regard to oxycodone was seen in this study as the opioid seems to be more toxic in the human SH-SY5Y cells compared to the other cell types. A previous comparative study using morphine, fentanyl, and hydromorphone, among others, revealed a similar outcome as the present study whereas fentanyl was more effective in inducing cytotoxicity compared with morphine and hydromorphone [39]. To the best of our knowledge, there have been no published reports on the effects of ketobemidone on cell viability, most likely because this opioid is not commonly used outside the Scandinavian countries. However, there are reports that ketobemidone exerts immunomodulating effects as the opioid has been shown to inhibit chemokines associated with inflammation [40].
The main advantage of the present pre-clinical study is the comparison of various opioids tested in four cell types with different origins, including human and rat. Methadone was associated with the highest degree of toxicity, independent of the cell type used. The cell cultures used in the present study seem to have different vulnerabilities to opioid-induced toxicity, as the TD50 values obtained vary based on the type of cell culture used. Overall, the TD50 values, as calculated from the mitochondrial function assay, were lower in the cell lines, NG108-15 and SH-SY5Y, in comparison to the PCC cultures. This is likely due to the greater variation in the proportions of different cell types in PCC cultures, in contrast to the uniform cell types present in the cell lines. This is not surprising given that PCC cultures are more biologically relevant in comparison to cell lines as they also contain other cell types that are normally present in the brain. As both the NG108-15 and SH-SY5Y cells originate from neuroblastoma, this indicates that neurons are more sensitive to opioid-induced damage compared to other cell types present in the PCC cultures. Using different types of cell cultures and high opioid concentrations enabled us to detect differences between the opioid treatments and it is possible that some of these effects occur in the brain following the chronic use of opioids in humans.
The present study contains data that are limiting the interpretation of the results, particularly in relation to clinical relevancy. For instance, the TD50 values demonstrated in the present study are considered to be very high and it is unlikely that these concentrations correspond to the opioid levels in the brain following oral or parental administration in a clinical setting. For instance, the C max of methadone in the plasma of patients overdosing on methadone has been reported to reach as high as 4,000 ng/mL, which corresponds to approximately 12 µM [41]. However, it is important to consider that the effects observed in the present study result from an acute 24-h opioid treatment. The obtained TD50 values would likely be lower if the opioids were administered repeatedly for a longer time. It is difficult to maintain cells for long-term in vitro, and therefore difficult to mimic the opioid administration of a traditional chronic user without compromising the general health of the cultured cells, which in turn also would impact the outcome of the results. Thus, these results need to be further evaluated in vivo to confirm the clinical relevance. Another important aspect to consider is that the human-derived cell line SH-SY5Y in the present study was used in a non-differentiated state and thus, the clinical significance of the results from the SH-SY5Y cells needs to be evaluated accordingly. However, as the same trend with regard to opioid-induced toxicity was observed in the PCC cultures and differentiated NG108-15 cells, which are more physiologically relevant, it is likely that these effects occur also in differentiated SH-SY5Y cells.
In conclusion, the present in vitro study reveals opioid-dependent differences in toxicity which is confirmed in all four tested cell types. Methadone was the most potent opioid with regard to opioid-induced mitochondrial damage, followed by fentanyl and ketobemidone. The impact of morphine and hydromorphone on cell viability was less pronounced and thus the least toxic to the cell cultures. Oxycodone was also ranked as one of the least toxic opioids in the assays examined. The results from this comparative study warrant further investigation in vivo as aside from the problems associated with addiction and mortality, opioids may impact higher cognitive functions in long-term opioid users.
Acknowledgements
We thank Anatole Nöstl for providing valuable insights and comments to our work.
-
Research ethics: All animal experiments were approved by the Uppsala Animal Ethics Committee (Dnr 5.8.18-18550/2018) according to Swedish guidelines regarding animal experiments (Animal Welfare Act SFS1998:56) and the European Communities directive (86/609/EEC).
-
Informed consent: Not applicable.
-
Author contributions: The authors have accepted responsibility for the entire content of this manuscript and approved its submission. Conceptualization: E.N., A.G., and M.H.; methodology: F.S., E.N., S.Z., A.G., and J.B.; software: F.S., E.N.; validation: F.S., E.N., A.G., and M.H.; formal analysis: F.S., E.N., and J.B.; investigation: F.S. and E.N.; resources: M.H.; data curation: F.S. and E.N.; writing – original draft preparation: E.N. and L.K.; writing – review and editing: F.S., E.N., S.Z., L.K., J.B., F.N., A.G., and M.H.; visualization: E.N.; supervision: A.G., F.N., and M.H.; project administration: E.N. and M.H.; funding acquisition: M.H., A.G.
-
Competing interests: The authors state no conflict of interest.
-
Previous presentation of study data at scientific meetings: Part of the study data was presented at the International Narcotics Research Conference (INRC) 2019, New York, USA.
-
Ethical permit: Uppsala Animal Ethics Committee permitted the study (no. 5.8.18-18550/2018).
-
Research funding: This work was supported by the Kjell and Märta Beijer Foundation, the Swedish Research Council (grant number 9459), and the Swedish Brain Foundation.
-
Data availability: The raw data can be obtained on request from the corresponding author.
-
Artificial intelligence/Machine learning tools: Not applicable.
-
Supplementary Material: This article contains supplementary material (followed by the link to the article online).
References
[1] Jalal H, Buchanich JM, Roberts MS, Balmert LC, Zhang K, Burke DS. Changing dynamics of the drug overdose epidemic in the United States from 1979 through 2016. Science. 2018 Sep;361(6408):eaau1184. 10.1126/science.aau1184.Search in Google Scholar PubMed PubMed Central
[2] International Association for the Study of Pain. Opioids for pain management [Internet]. iasp-pain.org; 2018 [cited 2023 Oct 16]. https://www.iasp-pain.org/advocacy/iasp-statements/opioids-for-pain-management/.Search in Google Scholar
[3] Spencer M, Garnett M, Miniño A. Drug overdose deaths in the United States, 2002–2022 [Internet]. National Center for Health Statistics (U.S.); 2023 Dec. [cited 2024 Oct 3]. 10.15620/cdc:135849.Search in Google Scholar
[4] Muller AE, Clausen T, Sjøgren P, Odsbu I, Skurtveit S. Prescribed opioid analgesic use developments in three Nordic countries, 2006–2017. Scand J Pain. 2019 Apr;19(2):345–53. 10.1515/sjpain-2018-0307.Search in Google Scholar PubMed
[5] Swedish National Board of Health and Welfare. Statistical database, Pharmaceuticals [Internet]. Socialstyrelsen.se; 2024 [cited 2024 Oct 03]. https://sdb.socialstyrelsen.se/if_lak/val.aspx.Search in Google Scholar
[6] Fugelstad A, Ågren G, Ramstedt M, Thiblin I, Hjelmström P. Oxycodone-related deaths in Sweden 2006-2018. Drug Alcohol Depend. 2022 May;234:109402. 10.1016/j.drugalcdep.2022.109402.Search in Google Scholar PubMed
[7] Svensson AL, Bucht N, Hallberg M, Nyberg F. Reversal of opiate-induced apoptosis by human recombinant growth hormone in murine foetus primary hippocampal neuronal cell cultures. Proc Natl Acad Sci U S A. 2008 May 20;105(20):7304–8. 10.1073/pnas.0802531105.Search in Google Scholar PubMed PubMed Central
[8] Polanco MJ, Alguacil LF, González-Martín C. Pro-apoptotic properties of morphine in neuroblastoma × glioma NG108-15 hybrid cells: modulation by yohimbine. J Appl Toxicol. 2014 Jan;34(1):19–24. 10.1002/jat.2817.Search in Google Scholar PubMed
[9] Perez-Alvarez S, Cuenca-Lopez MD, de Mera RMMF, Puerta E, Karachitos A, Bednarczyk P, et al. Methadone induces necrotic-like cell death in SH-SY5Y cells by an impairment of mitochondrial ATP synthesis. Biochim Biophys Acta. 2010 Nov;1802(11):1036–47. 10.1016/j.bbadis.2010.07.024.Search in Google Scholar PubMed
[10] Nylander E, Zelleroth S, Nyberg F, Grönbladh A, Hallberg M. The protective and restorative effects of growth hormone and insulin-like growth factor-1 on methadone-induced toxicity in vitro. Int J Mol Sci. 2018 Nov;19(11):3627. 10.3390/ijms19113627.Search in Google Scholar PubMed PubMed Central
[11] Nylander E, Grönbladh A, Zelleroth S, Diwakarla S, Nyberg F, Hallberg M. Growth hormone is protective against acute methadone-induced toxicity by modulating the NMDA receptor complex. Neuroscience. 2016 Dec;339:538–47. 10.1016/j.neuroscience.2016.10.019.Search in Google Scholar PubMed
[12] Nylander E, Zelleroth S, Nyberg F, Grönbladh A, Hallberg M. The effects of morphine, methadone, and fentanyl on mitochondria: A live cell imaging study. Brain Res Bull. 2021 Jun;171:126–34. 10.1016/j.brainresbull.2021.03.009.Search in Google Scholar PubMed
[13] Eisch AJ, Barrot M, Schad CA, Self DW, Nestler EJ. Opiates inhibit neurogenesis in the adult rat hippocampus. Proc Natl Acad Sci U S A. 2000 Jun;97(13):7579–84. 10.1073/pnas.120552597.Search in Google Scholar PubMed PubMed Central
[14] Mao J, Sung B, Ji RR, Lim G. Neuronal apoptosis associated with morphine tolerance: evidence for an opioid-induced neurotoxic mechanism. J Neurosci J Soc Neurosci. 2002 Sep;22(17):7650–61. 10.1523/JNEUROSCI.22-17-07650.2002.Search in Google Scholar PubMed PubMed Central
[15] Younger JW, Chu LF, D’Arcy NT, Trott KE, Jastrzab LE, Mackey SC. Prescription opioid analgesics rapidly change the human brain. Pain. 2011 Aug;152(8):1803–10. 10.1016/j.pain.2011.03.028.Search in Google Scholar PubMed PubMed Central
[16] Tramullas M, Martínez-Cué C, Hurlé MA. Chronic methadone treatment and repeated withdrawal impair cognition and increase the expression of apoptosis-related proteins in mouse brain. Psychopharmacology (Berl). 2007 Jul;193(1):107–20. 10.1007/s00213-007-0751-x.Search in Google Scholar PubMed
[17] Andersen JM, Olaussen CF, Ripel A, Mørland J. Long-term methadone treatment impairs novelty preference in rats both when present and absent in brain tissue. Pharmacol Biochem Behav. 2011 May;98(3):412–6. 10.1016/j.pbb.2011.02.017.Search in Google Scholar PubMed
[18] Hepner IJ, Homewood J, Taylor AJ. Methadone disrupts performance on the working memory version of the Morris water task. Physiol Behav. 2002 May;76(1):41–9. 10.1016/s0031-9384(02)00695-9.Search in Google Scholar PubMed
[19] Schiltenwolf M, Akbar M, Hug A, Pfüller U, Gantz S, Neubauer E, et al. Evidence of specific cognitive deficits in patients with chronic low back pain under long-term substitution treatment of opioids. Pain Physician. 2014;17(1):9–20.10.36076/ppj.2014/17/9Search in Google Scholar
[20] Turner AD, Sullivan T, Drury K, Hall TA, Williams CN, Guilliams KP, et al. Cognitive dysfunction after analgesia and sedation: Out of the operating room and into the pediatric intensive care unit. Front Behav Neurosci. 2021;15:713668. 10.3389/fnbeh.2021.713668.Search in Google Scholar PubMed PubMed Central
[21] Plein LM, Rittner HL. Opioids and the immune system – friend or foe. Br J Pharmacol. 2018 Jul;175(14):2717–25. 10.1111/bph.13750.Search in Google Scholar PubMed PubMed Central
[22] Wiese AD, Griffin MR, Schaffner W, Stein CM, Greevy RA, Mitchel EF, et al. Long-acting opioid use and the risk of serious infections: A retrospective cohort study. Clin Infect Dis. 2019 May;68(11):1862–9. 10.1093/cid/ciy809.Search in Google Scholar PubMed PubMed Central
[23] Diwakarla S, Nylander E, Grönbladh A, Vanga SR, Khan YS, Gutiérrez-de-Terán H, et al. Binding to and inhibition of insulin-regulated aminopeptidase by macrocyclic disulfides enhances spine density. Mol Pharmacol. 2016 Apr;89(4):413–24. 10.1124/mol.115.102533.Search in Google Scholar PubMed
[24] Hamprecht B, Glaser T, Reiser G, Bayer E, Propst F. Culture and characteristics of hormone-responsive neuroblastoma X glioma hybrid cells. Methods Enzymol. 1985;109:316–41. 10.1016/0076-6879(85)09096-6.Search in Google Scholar PubMed
[25] Volpe DA, McMahon Tobin GA, Mellon RD, Katki AG, Parker RJ, Colatsky T, et al. Uniform assessment and ranking of opioid μ receptor binding constants for selected opioid drugs. Regul Toxicol Pharmacol. 2011 Apr;59(3):385–90. 10.1016/j.yrtph.2010.12.007.Search in Google Scholar PubMed
[26] Vandeputte MM, Persson M, Walther D, Vikingsson S, Kronstrand R, Baumann MH, et al. Characterization of recent non-fentanyl synthetic opioids via three different in vitro µ-opioid receptor activation assays. Arch Toxicol. 2022 Mar;96(3):877–97. 10.1007/s00204-021-03207-9.Search in Google Scholar PubMed
[27] Christensen CB. The opioid receptor binding profiles of ketobemidone and morphine. Pharmacol Toxicol. 1993 Dec;73(6):344–5. 10.1111/j.1600-0773.1993.tb01363.x.Search in Google Scholar PubMed
[28] Raynor K, Kong H, Chen Y, Yasuda K, Yu L, Bell GI, et al. Pharmacological characterization of the cloned kappa-, delta-, and mu-opioid receptors. Mol Pharmacol. 1994 Feb;45(2):330–4.Search in Google Scholar
[29] Codd EE, Shank RP, Schupsky JJ, Raffa RB. Serotonin and norepinephrine uptake inhibiting activity of centrally acting analgesics: structural determinants and role in antinociception. J Pharmacol Exp Ther. 1995 Sep;274(3):1263–70.Search in Google Scholar
[30] Maguire PA, Perez JJ, Tsai NF, Rodriguez L, Beatty MF, Villar HO, et al. Molecular mechanism of delta-selectivity of indole analogs of nonpeptide opioids. Mol Pharmacol. 1993 Dec;44(6):1246–51.Search in Google Scholar
[31] Ebert B, Andersen S, Krogsgaard-Larsen P. Ketobemidone, methadone and pethidine are non-competitive N-methyl-D-aspartate (NMDA) antagonists in the rat cortex and spinal cord. Neurosci Lett. 1995 Mar;187(3):165–8. 10.1016/0304-3940(95)11364-3.Search in Google Scholar PubMed
[32] Navaei F, Fathabadi FF, Moghaddam MH, Fathi M, Vakili K, Abdollahifar MA, et al. Chronic exposure to methadone impairs memory, induces microgliosis, astrogliosis and neuroinflammation in the hippocampus of adult male rats. J Chem Neuroanat. 2022 Nov;125:102139. 10.1016/j.jchemneu.2022.102139.Search in Google Scholar PubMed
[33] Vilela SMF, Santos DJSL, Félix L, Almeida JM, Antunes L, Peixoto F. Are fentanyl and remifentanil safe opioids for rat brain mitochondrial bioenergetics? Mitochondrion. 2009 Jul;9(4):247–53. 10.1016/j.mito.2009.03.002.Search in Google Scholar PubMed
[34] Ficklscherer A, Sievers B, Redeker J, Gülecyüz MF, Paulus A, Pietschmann MF, et al. Comparison of ropivacaine and fentanyl toxicity in human fibroblasts. Arch Med Sci. 2013 Jun;9(3):576–80. 10.5114/aoms.2013.35339.Search in Google Scholar PubMed PubMed Central
[35] Taghizadehghalehjoughi A, Naldan ME, Yeni Y, Genc S, Hacimuftuoglu A, Isik M, et al. Effect of fentanyl and remifentanil on neuron damage and oxidative stress during induction neurotoxicity. J Cell Mol Med. 2024 Feb;28(4):e18118. 10.1111/jcmm.18118.Search in Google Scholar PubMed PubMed Central
[36] Kokki M, Pesonen M, Vehviläinen P, Litmala O, Pasanen M, Kokki H. Cytotoxicity of oxycodone and morphine in human neuroblastoma and mouse motoneuronal cells: A comparative approach. Drugs RD. 2016 Jun;16(2):155–63. 10.1007/s40268-016-0125-0.Search in Google Scholar PubMed PubMed Central
[37] Lima LS, da Costa NdS, Galiciolli MEA, Pereira ME, Almeida W, Margarete Cestari M, et al. Assessment of neurotoxic effects of oxycodone and naloxone in SH-SY5Y cell line. Int J Mol Sci. 2023 Jan;24(2):1424. 10.3390/ijms24021424.Search in Google Scholar PubMed PubMed Central
[38] Jairaj M, Watson DG, Grant MH, Skellern GG. The toxicity of opiates and their metabolites in HepG2 cells. Chem Biol Interact. 2003 Oct;146(2):121–9. 10.1016/s0009-2797(03)00091-7.Search in Google Scholar PubMed
[39] Nassiri MR, Flynn GL, Shipman C. Inhibition of cell growth and DNA, RNA, and protein synthesis in vitro by fentanyl, sufentanil, and opiate analgesics. Pharmacol Toxicol. 1991 Jul;69(1):17–21. 10.1111/j.1600-0773.1991.tb00402.x.Search in Google Scholar PubMed
[40] Bastami S, Norling C, Trinks C, Holmlund B, Walz TM, Ahlner J, et al. Inhibitory effect of opiates on LPS mediated release of TNF and IL-8. Acta Oncol Stockh Swed. 2013 Jun;52(5):1022–33. 10.3109/0284186X.2012.737932.Search in Google Scholar PubMed
[41] Errico S, Bedocchi D, Drommi M, Barranco R, Bonsignore A, Ventura F. Forensic pathological study of methadone-related deaths in the Genoa (Italy) district: A six-year study. J Forensic Leg Med. 2021 Apr;79:102149. 10.1016/j.jflm.2021.102149.Search in Google Scholar PubMed
© 2024 the author(s), published by De Gruyter
This work is licensed under the Creative Commons Attribution 4.0 International License.
Articles in the same Issue
- Editorial Comment
- From pain to relief: Exploring the consistency of exercise-induced hypoalgesia
- Christmas greetings 2024 from the Editor-in-Chief
- Original Articles
- The Scandinavian Society for the Study of Pain 2022 Postgraduate Course and Annual Scientific (SASP 2022) Meeting 12th to 14th October at Rigshospitalet, Copenhagen
- Comparison of ultrasound-guided continuous erector spinae plane block versus continuous paravertebral block for postoperative analgesia in patients undergoing proximal femur surgeries
- Clinical Pain Researches
- The effect of tourniquet use on postoperative opioid consumption after ankle fracture surgery – a retrospective cohort study
- Changes in pain, daily occupations, lifestyle, and health following an occupational therapy lifestyle intervention: a secondary analysis from a feasibility study in patients with chronic high-impact pain
- Tonic cuff pressure pain sensitivity in chronic pain patients and its relation to self-reported physical activity
- Reliability, construct validity, and factorial structure of a Swedish version of the medical outcomes study social support survey (MOS-SSS) in patients with chronic pain
- Hurdles and potentials when implementing internet-delivered Acceptance and commitment therapy for chronic pain: a retrospective appraisal using the Quality implementation framework
- Exploring the outcome “days with bothersome pain” and its association with pain intensity, disability, and quality of life
- Fatigue and cognitive fatigability in patients with chronic pain
- The Swedish version of the pain self-efficacy questionnaire short form, PSEQ-2SV: Cultural adaptation and psychometric evaluation in a population of patients with musculoskeletal disorders
- Pain coping and catastrophizing in youth with and without cerebral palsy
- Neuropathic pain after surgery – A clinical validation study and assessment of accuracy measures of the 5-item NeuPPS scale
- Translation, contextual adaptation, and reliability of the Danish Concept of Pain Inventory (COPI-Adult (DK)) – A self-reported outcome measure
- Cosmetic surgery and associated chronic postsurgical pain: A cross-sectional study from Norway
- The association of hemodynamic parameters and clinical demographic variables with acute postoperative pain in female oncological breast surgery patients: A retrospective cohort study
- Healthcare professionals’ experiences of interdisciplinary collaboration in pain centres – A qualitative study
- Effects of deep brain stimulation and verbal suggestions on pain in Parkinson’s disease
- Painful differences between different pain scale assessments: The outcome of assessed pain is a matter of the choices of scale and statistics
- Prevalence and characteristics of fibromyalgia according to three fibromyalgia diagnostic criteria: A secondary analysis study
- Sex moderates the association between quantitative sensory testing and acute and chronic pain after total knee/hip arthroplasty
- Tramadol-paracetamol for postoperative pain after spine surgery – A randomized, double-blind, placebo-controlled study
- Cancer-related pain experienced in daily life is difficult to communicate and to manage – for patients and for professionals
- Making sense of pain in inflammatory bowel disease (IBD): A qualitative study
- Patient-reported pain, satisfaction, adverse effects, and deviations from ambulatory surgery pain medication
- Does pain influence cognitive performance in patients with mild traumatic brain injury?
- Hypocapnia in women with fibromyalgia
- Application of ultrasound-guided thoracic paravertebral block or intercostal nerve block for acute herpes zoster and prevention of post-herpetic neuralgia: A case–control retrospective trial
- Translation and examination of construct validity of the Danish version of the Tampa Scale for Kinesiophobia
- A positive scratch collapse test in anterior cutaneous nerve entrapment syndrome indicates its neuropathic character
- ADHD-pain: Characteristics of chronic pain and association with muscular dysregulation in adults with ADHD
- The relationship between changes in pain intensity and functional disability in persistent disabling low back pain during a course of cognitive functional therapy
- Intrathecal pain treatment for severe pain in patients with terminal cancer: A retrospective analysis of treatment-related complications and side effects
- Psychometric evaluation of the Danish version of the Pain Self-Efficacy Questionnaire in patients with subacute and chronic low back pain
- Dimensionality, reliability, and validity of the Finnish version of the pain catastrophizing scale in chronic low back pain
- To speak or not to speak? A secondary data analysis to further explore the context-insensitive avoidance scale
- Pain catastrophizing levels differentiate between common diseases with pain: HIV, fibromyalgia, complex regional pain syndrome, and breast cancer survivors
- Prevalence of substance use disorder diagnoses in patients with chronic pain receiving reimbursed opioids: An epidemiological study of four Norwegian health registries
- Pain perception while listening to thrash heavy metal vs relaxing music at a heavy metal festival – the CoPainHell study – a factorial randomized non-blinded crossover trial
- Observational Studies
- Cutaneous nerve biopsy in patients with symptoms of small fiber neuropathy: a retrospective study
- The incidence of post cholecystectomy pain (PCP) syndrome at 12 months following laparoscopic cholecystectomy: a prospective evaluation in 200 patients
- Associations between psychological flexibility and daily functioning in endometriosis-related pain
- Relationship between perfectionism, overactivity, pain severity, and pain interference in individuals with chronic pain: A cross-lagged panel model analysis
- Access to psychological treatment for chronic cancer-related pain in Sweden
- Validation of the Danish version of the knowledge and attitudes survey regarding pain
- Associations between cognitive test scores and pain tolerance: The Tromsø study
- Healthcare experiences of fibromyalgia patients and their associations with satisfaction and pain relief. A patient survey
- Video interpretation in a medical spine clinic: A descriptive study of a diverse population and intervention
- Role of history of traumatic life experiences in current psychosomatic manifestations
- Social determinants of health in adults with whiplash associated disorders
- Which patients with chronic low back pain respond favorably to multidisciplinary rehabilitation? A secondary analysis of a randomized controlled trial
- A preliminary examination of the effects of childhood abuse and resilience on pain and physical functioning in patients with knee osteoarthritis
- Differences in risk factors for flare-ups in patients with lumbar radicular pain may depend on the definition of flare
- Real-world evidence evaluation on consumer experience and prescription journey of diclofenac gel in Sweden
- Patient characteristics in relation to opioid exposure in a chronic non-cancer pain population
- Topical Reviews
- Bridging the translational gap: adenosine as a modulator of neuropathic pain in preclinical models and humans
- What do we know about Indigenous Peoples with low back pain around the world? A topical review
- The “future” pain clinician: Competencies needed to provide psychologically informed care
- Systematic Reviews
- Pain management for persistent pain post radiotherapy in head and neck cancers: systematic review
- High-frequency, high-intensity transcutaneous electrical nerve stimulation compared with opioids for pain relief after gynecological surgery: a systematic review and meta-analysis
- Reliability and measurement error of exercise-induced hypoalgesia in pain-free adults and adults with musculoskeletal pain: A systematic review
- Noninvasive transcranial brain stimulation in central post-stroke pain: A systematic review
- Short Communications
- Are we missing the opioid consumption in low- and middle-income countries?
- Association between self-reported pain severity and characteristics of United States adults (age ≥50 years) who used opioids
- Could generative artificial intelligence replace fieldwork in pain research?
- Skin conductance algesimeter is unreliable during sudden perioperative temperature increases
- Original Experimental
- Confirmatory study of the usefulness of quantum molecular resonance and microdissectomy for the treatment of lumbar radiculopathy in a prospective cohort at 6 months follow-up
- Pain catastrophizing in the elderly: An experimental pain study
- Improving general practice management of patients with chronic musculoskeletal pain: Interdisciplinarity, coherence, and concerns
- Concurrent validity of dynamic bedside quantitative sensory testing paradigms in breast cancer survivors with persistent pain
- Transcranial direct current stimulation is more effective than pregabalin in controlling nociceptive and anxiety-like behaviors in a rat fibromyalgia-like model
- Paradox pain sensitivity using cuff pressure or algometer testing in patients with hemophilia
- Physical activity with person-centered guidance supported by a digital platform or with telephone follow-up for persons with chronic widespread pain: Health economic considerations along a randomized controlled trial
- Measuring pain intensity through physical interaction in an experimental model of cold-induced pain: A method comparison study
- Pharmacological treatment of pain in Swedish nursing homes: Prevalence and associations with cognitive impairment and depressive mood
- Neck and shoulder pain and inflammatory biomarkers in plasma among forklift truck operators – A case–control study
- The effect of social exclusion on pain perception and heart rate variability in healthy controls and somatoform pain patients
- Revisiting opioid toxicity: Cellular effects of six commonly used opioids
- Letter to the Editor
- Post cholecystectomy pain syndrome: Letter to Editor
- Response to the Letter by Prof Bordoni
- Response – Reliability and measurement error of exercise-induced hypoalgesia
- Is the skin conductance algesimeter index influenced by temperature?
- Skin conductance algesimeter is unreliable during sudden perioperative temperature increase
- Corrigendum
- Corrigendum to “Chronic post-thoracotomy pain after lung cancer surgery: a prospective study of preoperative risk factors”
- Obituary
- A Significant Voice in Pain Research Björn Gerdle in Memoriam (1953–2024)
Articles in the same Issue
- Editorial Comment
- From pain to relief: Exploring the consistency of exercise-induced hypoalgesia
- Christmas greetings 2024 from the Editor-in-Chief
- Original Articles
- The Scandinavian Society for the Study of Pain 2022 Postgraduate Course and Annual Scientific (SASP 2022) Meeting 12th to 14th October at Rigshospitalet, Copenhagen
- Comparison of ultrasound-guided continuous erector spinae plane block versus continuous paravertebral block for postoperative analgesia in patients undergoing proximal femur surgeries
- Clinical Pain Researches
- The effect of tourniquet use on postoperative opioid consumption after ankle fracture surgery – a retrospective cohort study
- Changes in pain, daily occupations, lifestyle, and health following an occupational therapy lifestyle intervention: a secondary analysis from a feasibility study in patients with chronic high-impact pain
- Tonic cuff pressure pain sensitivity in chronic pain patients and its relation to self-reported physical activity
- Reliability, construct validity, and factorial structure of a Swedish version of the medical outcomes study social support survey (MOS-SSS) in patients with chronic pain
- Hurdles and potentials when implementing internet-delivered Acceptance and commitment therapy for chronic pain: a retrospective appraisal using the Quality implementation framework
- Exploring the outcome “days with bothersome pain” and its association with pain intensity, disability, and quality of life
- Fatigue and cognitive fatigability in patients with chronic pain
- The Swedish version of the pain self-efficacy questionnaire short form, PSEQ-2SV: Cultural adaptation and psychometric evaluation in a population of patients with musculoskeletal disorders
- Pain coping and catastrophizing in youth with and without cerebral palsy
- Neuropathic pain after surgery – A clinical validation study and assessment of accuracy measures of the 5-item NeuPPS scale
- Translation, contextual adaptation, and reliability of the Danish Concept of Pain Inventory (COPI-Adult (DK)) – A self-reported outcome measure
- Cosmetic surgery and associated chronic postsurgical pain: A cross-sectional study from Norway
- The association of hemodynamic parameters and clinical demographic variables with acute postoperative pain in female oncological breast surgery patients: A retrospective cohort study
- Healthcare professionals’ experiences of interdisciplinary collaboration in pain centres – A qualitative study
- Effects of deep brain stimulation and verbal suggestions on pain in Parkinson’s disease
- Painful differences between different pain scale assessments: The outcome of assessed pain is a matter of the choices of scale and statistics
- Prevalence and characteristics of fibromyalgia according to three fibromyalgia diagnostic criteria: A secondary analysis study
- Sex moderates the association between quantitative sensory testing and acute and chronic pain after total knee/hip arthroplasty
- Tramadol-paracetamol for postoperative pain after spine surgery – A randomized, double-blind, placebo-controlled study
- Cancer-related pain experienced in daily life is difficult to communicate and to manage – for patients and for professionals
- Making sense of pain in inflammatory bowel disease (IBD): A qualitative study
- Patient-reported pain, satisfaction, adverse effects, and deviations from ambulatory surgery pain medication
- Does pain influence cognitive performance in patients with mild traumatic brain injury?
- Hypocapnia in women with fibromyalgia
- Application of ultrasound-guided thoracic paravertebral block or intercostal nerve block for acute herpes zoster and prevention of post-herpetic neuralgia: A case–control retrospective trial
- Translation and examination of construct validity of the Danish version of the Tampa Scale for Kinesiophobia
- A positive scratch collapse test in anterior cutaneous nerve entrapment syndrome indicates its neuropathic character
- ADHD-pain: Characteristics of chronic pain and association with muscular dysregulation in adults with ADHD
- The relationship between changes in pain intensity and functional disability in persistent disabling low back pain during a course of cognitive functional therapy
- Intrathecal pain treatment for severe pain in patients with terminal cancer: A retrospective analysis of treatment-related complications and side effects
- Psychometric evaluation of the Danish version of the Pain Self-Efficacy Questionnaire in patients with subacute and chronic low back pain
- Dimensionality, reliability, and validity of the Finnish version of the pain catastrophizing scale in chronic low back pain
- To speak or not to speak? A secondary data analysis to further explore the context-insensitive avoidance scale
- Pain catastrophizing levels differentiate between common diseases with pain: HIV, fibromyalgia, complex regional pain syndrome, and breast cancer survivors
- Prevalence of substance use disorder diagnoses in patients with chronic pain receiving reimbursed opioids: An epidemiological study of four Norwegian health registries
- Pain perception while listening to thrash heavy metal vs relaxing music at a heavy metal festival – the CoPainHell study – a factorial randomized non-blinded crossover trial
- Observational Studies
- Cutaneous nerve biopsy in patients with symptoms of small fiber neuropathy: a retrospective study
- The incidence of post cholecystectomy pain (PCP) syndrome at 12 months following laparoscopic cholecystectomy: a prospective evaluation in 200 patients
- Associations between psychological flexibility and daily functioning in endometriosis-related pain
- Relationship between perfectionism, overactivity, pain severity, and pain interference in individuals with chronic pain: A cross-lagged panel model analysis
- Access to psychological treatment for chronic cancer-related pain in Sweden
- Validation of the Danish version of the knowledge and attitudes survey regarding pain
- Associations between cognitive test scores and pain tolerance: The Tromsø study
- Healthcare experiences of fibromyalgia patients and their associations with satisfaction and pain relief. A patient survey
- Video interpretation in a medical spine clinic: A descriptive study of a diverse population and intervention
- Role of history of traumatic life experiences in current psychosomatic manifestations
- Social determinants of health in adults with whiplash associated disorders
- Which patients with chronic low back pain respond favorably to multidisciplinary rehabilitation? A secondary analysis of a randomized controlled trial
- A preliminary examination of the effects of childhood abuse and resilience on pain and physical functioning in patients with knee osteoarthritis
- Differences in risk factors for flare-ups in patients with lumbar radicular pain may depend on the definition of flare
- Real-world evidence evaluation on consumer experience and prescription journey of diclofenac gel in Sweden
- Patient characteristics in relation to opioid exposure in a chronic non-cancer pain population
- Topical Reviews
- Bridging the translational gap: adenosine as a modulator of neuropathic pain in preclinical models and humans
- What do we know about Indigenous Peoples with low back pain around the world? A topical review
- The “future” pain clinician: Competencies needed to provide psychologically informed care
- Systematic Reviews
- Pain management for persistent pain post radiotherapy in head and neck cancers: systematic review
- High-frequency, high-intensity transcutaneous electrical nerve stimulation compared with opioids for pain relief after gynecological surgery: a systematic review and meta-analysis
- Reliability and measurement error of exercise-induced hypoalgesia in pain-free adults and adults with musculoskeletal pain: A systematic review
- Noninvasive transcranial brain stimulation in central post-stroke pain: A systematic review
- Short Communications
- Are we missing the opioid consumption in low- and middle-income countries?
- Association between self-reported pain severity and characteristics of United States adults (age ≥50 years) who used opioids
- Could generative artificial intelligence replace fieldwork in pain research?
- Skin conductance algesimeter is unreliable during sudden perioperative temperature increases
- Original Experimental
- Confirmatory study of the usefulness of quantum molecular resonance and microdissectomy for the treatment of lumbar radiculopathy in a prospective cohort at 6 months follow-up
- Pain catastrophizing in the elderly: An experimental pain study
- Improving general practice management of patients with chronic musculoskeletal pain: Interdisciplinarity, coherence, and concerns
- Concurrent validity of dynamic bedside quantitative sensory testing paradigms in breast cancer survivors with persistent pain
- Transcranial direct current stimulation is more effective than pregabalin in controlling nociceptive and anxiety-like behaviors in a rat fibromyalgia-like model
- Paradox pain sensitivity using cuff pressure or algometer testing in patients with hemophilia
- Physical activity with person-centered guidance supported by a digital platform or with telephone follow-up for persons with chronic widespread pain: Health economic considerations along a randomized controlled trial
- Measuring pain intensity through physical interaction in an experimental model of cold-induced pain: A method comparison study
- Pharmacological treatment of pain in Swedish nursing homes: Prevalence and associations with cognitive impairment and depressive mood
- Neck and shoulder pain and inflammatory biomarkers in plasma among forklift truck operators – A case–control study
- The effect of social exclusion on pain perception and heart rate variability in healthy controls and somatoform pain patients
- Revisiting opioid toxicity: Cellular effects of six commonly used opioids
- Letter to the Editor
- Post cholecystectomy pain syndrome: Letter to Editor
- Response to the Letter by Prof Bordoni
- Response – Reliability and measurement error of exercise-induced hypoalgesia
- Is the skin conductance algesimeter index influenced by temperature?
- Skin conductance algesimeter is unreliable during sudden perioperative temperature increase
- Corrigendum
- Corrigendum to “Chronic post-thoracotomy pain after lung cancer surgery: a prospective study of preoperative risk factors”
- Obituary
- A Significant Voice in Pain Research Björn Gerdle in Memoriam (1953–2024)

