Abstract
Background
Low back pain (LBP) represents a worldwide burden with rising disability, especially in low- and middle-income countries. Indigenous Peoples are exposed to many risk factors for LBP and seem to have overall worse health and higher mortality compared to non-Indigenous. This article aims to provide a topical overview of LBP in Indigenous Peoples.
Methods
A comprehensive search was done using the keywords “Indigenous” and “back pain.” Secondly, a cross-reference search of the citations list of the included articles was conducted.
Results
LBP is a prevalent, disabling health condition among Indigenous Peoples that impacts activities of daily living, emotional well-being, and cultural identity. Indigenous Peoples face numerous and unique barriers to obtain Western health care. LBP in Indigenous Peoples is partly iatrogenic and available health care lacks a culturally secure setting. In combination with racism and discrimination by health care providers, this leads to miscommunication, frustration, and poor outcome in Indigenous patients around the world.
Conclusion
Contextual considerations and interpretation of findings within the appropriate cultural context are needed in future research and treatment of LBP in Indigenous Peoples. However, our literature analysis exhibits disproportionate representation with the scarcity of studies of Indigenous Peoples of Asia and Africa. Addressing this gap in the literature could provide significant scientific value. Indigenous Peoples should not be forgotten in reducing the global burden for LBP.
1 Introduction
Low back pain (LBP) is a debilitating health condition prevalent in all ages and geographical areas and affects most people at least once in their life [1]. In 2016, The Global Burden of Disease study estimated that more than half a billion people worldwide suffered from LBP, making it the leading cause of years lived with disability [2]. Lifetime prevalence of LBP ranges from 49 to 70% with a high recurrence rate of 85% [2]. LBP places a heavy burden on the individual, society, and health care systems in terms of medical costs, functional disability, and workdays lost [1]. Globally, LBP-related disability is rising with the most pronounced increases in low- and middle-income countries (LMICs) [1]. Furthermore, consequences of LBP in LMICs are more severe due to healthcare systems that focus more on infectious diseases. Moreover, they are not accommodated to cope with the growing burden of more chronic health issues as LBP [1].
Although the impact of LBP between high-income countries and LMICs is different, several universal risk factors for LBP have been identified such as poor mental health, previous episodes of LBP, and chronic co-morbid conditions like diabetes [3]. In addition, physical risk factors such as heavy lifting, repetitive twisting, and bending have also been reported [4]. These risk factors are prevalent among Indigenous Peoples due to traditional agriculture and fishing in rural areas or physical demanding manual labor jobs in urban areas [5,6].
There are about 476 million Indigenous Peoples living worldwide and they account for most of the world’s cultural diversity [7,8]. Historically, many Indigenous Peoples have suffered from the inhumane processes of colonization and its consequences. Even today, many Indigenous Peoples are often socially marginalized and impoverished facing threats to their very existence [7,8].
Research has shown that not all people within societies (including the Indigenous) receive the same opportunities for health care [9,10,11]. Access to health care is strongly influenced by financial status because economic factors prevail in many healthcare systems around the world [9,11,12]. Indigenous Peoples are estimated to make up about one-third of the world’s poorest people living in rural areas [7,8]. International studies provided insights into public health, revealing disparities for Indigenous communities in relation to the general population [6]. Indigenous Peoples have overall worse health, higher mortality, lower literacy, and higher incidence of poverty compared to non-Indigenous communities [6].
In 2018, The Lancet published a call for action about the rising burden of LBP worldwide, partly attributable to poor health care [1,13,14]. Within this series, the growing burden in LMIC has been addressed. However, a comprehensive overview about LBP in Indigenous Peoples is lacking in the existing literature. Therefore, the aim of this article was to give a topical review of current knowledge of LBP in Indigenous Peoples. A narrative approach was used to obtain a broad perspective and identify potential gaps on the topic in the available literature not only to stimulate future research but also to initiate action.
2 Methods
2.1 Literature review
First, a comprehensive search was conducted in July 2022 using three electronic databases (Web of Science, PubMed, and SCOPUS). The main keywords used in this search were “Indigenous” and “back pain”. Synonyms of the main keywords, including endemic and local Indigenous groups, were also searched. Second, a cross-reference search of the bibliographies of the selected articles was conducted.
Screening of titles and abstracts was done for all identified literature. If the title of the study included ‘LBP’ and ‘Indigenous’ (or synonyms), the study was included. If Indigenous (or synonym) and broader terms were used in the title such as rheumatic diseases or (back) pain were present in the title or abstract, the full text was screened to check if relevant information was present about LBP. If so, the study was included. Other inclusion criteria were published in peer-reviewed journals, adult population, and full text available in English language. Letters, commentaries, unpublished manuscripts, dissertations, government reports, conference proceedings, meeting abstracts, and lecturers were excluded.
Definition of the term ‘Indigenous’ is a contested subject and outside the scope of this article [15]. Due to the great diversity of the Indigenous Peoples, agreeing on a single definition is likely not realistic. Furthermore, political, social, and legal perspectives have an influence on national level in defining Indigenous Peoples [15]. Depending on these perspectives, some communities do not want to be recognized as Indigenous Peoples. For this review, all included studies were checked on their definition of “Indigenous,” having at least six out of the seven characteristics identified by the United Nations Permanent Forum on Indigenous Issues [16]. If not or unclear, they were excluded.
Figure 1 provides a flow-chart of the study selection and an overview of all the included studies, keywords, methods, and country or region can be found in Table 1. Manually two references with respect to Sami Indigenous Peoples were added bringing the total to 29 included papers.
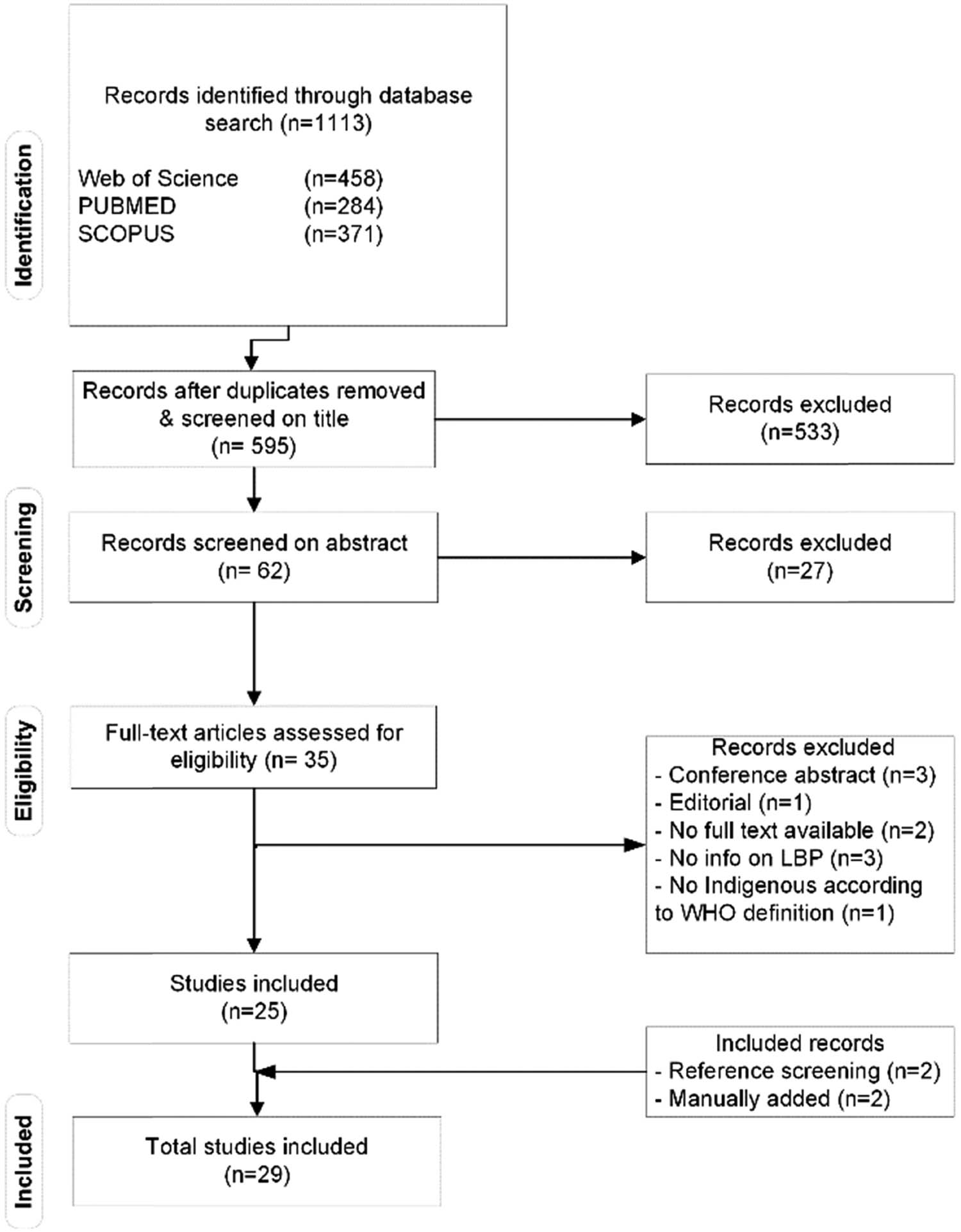
Flow chart of study selection.
Overview of all included articles in the literature review
| Year | Authors | Article title | Keywords | Methodology | Country or region |
|---|---|---|---|---|---|
| 1996 | Honeyman, P. T. | Effects of culture on back pain in Australian Aboriginals |
|
Mixed method | Australia |
| 2004 | Vindigni, D. | Prevalence of musculoskeletal conditions, associated pain and disability and the barriers to managing these conditions in a rural, Australian Aboriginal community. |
|
Quantitative/COPCORD | Australia |
| 2005 | Vindigni, D. | Low back pain risk factors in a large rural Australian Aboriginal community. An opportunity for managing co-morbidities? |
|
Quantitative | Australia |
| 2003 | Daerga, L. | Work-related musculoskeletal pain among reindeer herding Sami in Sweden – a pilot study on causes and prevention |
|
Quantitative | Europe |
| 2006 | Deyo, R. A. | Back pain prevalence and Visit rates: Estimates from U.S. national surveys, 2002 |
|
Quantitative | United States |
| 2008 | Sjölander, P. | Musculoskeletal symptoms and perceived work strain among reindeer herders in Sweden |
|
Quantitative | Sweden |
| 2011 | Jimenez, N. | A review of the experience, Epidemiology, and management of pain among American Indian, Alaska Native, and Aboriginal Canadian Peoples |
|
Review | United States/Canada |
| 2012 | Lin, I.B. | “I am absolutely shattered”: The impact of chronic low back pain on Australian Aboriginal people |
|
Qualitative | Australia |
| 2013 | Lin, I. B. | Disabling chronic low back pain as an iatrogenic disorder: a qualitative study in Aboriginal Australians |
|
Qualitative | Australia |
| 2014 | Lin, I. B. | “I can sit and talk to her”: Aboriginal people, chronic low back pain and healthcare practitioner communication |
|
Qualitative | Australia |
| 2015 | Strong, J. | Quiet about pain: Experiences of Aboriginal people in two rural communities |
|
Qualitative | Australia |
| 2015 | Peláez-Ballestas, I. | Prevalence and factors associated with musculoskeletal disorders and rheumatic diseases in indigenous Maya-Yucateco people: a cross-sectional community-based study |
|
Quantitative/COPCORD | Mexico |
| 2015 | Julián-Santiago, F. | Epidemiology of rheumatic diseases in Mixtec and Chontal Indigenous communities in Mexico: a cross-sectional community-based study |
|
Quantitative/COPCORD | Mexico |
| 2016 | Granados, Y. | Prevalence of musculoskeletal disorders and rheumatic disease in the Warao, Kari'ña, and Chaima indigenous populations of Monagas State, Venezuela |
|
Quantitative/COPCORD | Venezuela |
| 2016 | Quintana, R. | Prevalence of musculoskeletal disorders and rheumatic diseases in the indigenous Qom population of Rosario, Argentina |
|
Quantitative/COPCORD | Argentina |
| 2016 | Incayawar, M. | Exploring pain in the Andes-learning from the Quichua (Inca) people experience |
|
Qualitative | Ecuador |
| 2016 | Del Río Nájera, D. | Prevalence of rheumatic diseases in Raramuri people in Chihuahua, Mexico: a community-based study |
|
Quantitative/COPCORD | Mexico |
| 2017 | Lin, I. B. | Addressing disparities in low back pain care by developing culturally appropriate information for Aboriginal Australians: “My back on track, my future” |
|
Qualitative | Australia |
| 2017 | Lin I. B. | Unmet Needs of Aboriginal Australians with Musculoskeletal Pain: A Mixed-Method Systematic Review. |
|
Qualitative | Australia |
| 2018 | Peláez-Ballestas, I. | Epidemiology and socioeconomic impact of the rheumatic diseases on indigenous people: an invisible syndemic public health problem |
|
Quantitative | Venezuela and Mexico |
| 2019 | Arthur, L. | A systematic review of western medicine’s understanding of pain experience, expression, assessment, and management for Australian Aboriginal and Torres Strait Islander Peoples |
|
Systematic Review | Australia |
| 2020 | Strozzi, A. | Syndemic and syndemogenesis of low back pain in Latin-American population: a network and cluster analysis |
|
Quantitative | Latin-America |
| 2020 | Juárez, V. | Prevalence of musculoskeletal disorders and rheumatic diseases in an Argentinean indigenous Wichi community |
|
Quantitative/COPCORD | Argentina |
| 2020 | Mullerpatan, R. | Burden of spine among rural and tribal population in Raigad District of Maharashtra State of India |
|
Mixed method | India |
| 2020 | Guevara, S. V. | Prevalence of Rheumatic Diseases and Quality of Life in the Saraguro Indigenous People, Ecuador: A Cross-sectional Community-Based Study |
|
Quantitative/COPCORD | Ecuador |
| 2021 | Barbosa de Moraes, E. | Pain Management of Amazon Indigenous Peoples: A Community-Based Study |
|
Quantitative | Brazil |
| 2021 | Ho-A-Tham, N. | Low back pain prevalence, beliefs and treatment-seeking behaviour in multi-ethnic Suriname |
|
Quantitative/COPCORD | Suriname |
| 2022 | Minaur, N. | Rheumatic disease in an Australian Aboriginal community in North Queensland, Australia. A WHO-ILAR COPCORD survey |
|
Quantitative/COPCORD | Australia |
| 2022 | Ottesen, T. D. | The Unmet Need for Orthopedic Services among American Indian and Alaska Native Communities in the United States |
|
Review | United States |
3 Results
3.1 Prevalence of LBP in Indigenous Peoples
Prevalence of LBP in different Indigenous communities is summarized in Table 2. Point prevalence for LBP ranged from 10% in three tribal villages in India to 72% in Aboriginals in Australia [17,18,19,20,22]. Seven-day prevalence of LBP was reported for 12 different Indigenous Peoples ranging between 1.5 and 45.7% [12,21,23,24,25,26 27].
Prevalence of LBP in different Indigenous communities
| Indigenous communities | Prevalence LBP (%) | Prevalence type1 | Country | Reference paper |
|---|---|---|---|---|
| Europe | ||||
| Sami | 45.7 | 7D | Sweden | Sjölander, 2008 |
| Sami | 45.2 | 7D | Sweden | Daerga, 2003 |
| North America | ||||
| Yucatec Maya | 10.0 | 7D–C | Mexico | Peláez-Ballestas, 2018 |
| Mixteca Alta | 16.7 | 7D–C | Mexico | Peláez-Ballestas, 2018 |
| Chontal | 10.4 | 7D–C | Mexico | Peláez-Ballestas, 2018 |
| Raramuri | 1.5 | 7D–C | Mexico | Peláez-Ballestas, 2018 |
| American Indians/Alaska Native | 35.0 | 3M | United States | Deyo, 2006 |
| South America | ||||
| Qom (Tobas) | 19.8 | 7D–C | Argentina | Peláez-Ballestas, 2018 |
| Wichi | 13.1 | 7D–C | Argentina | Julián-Santiago, 2020 |
| Warao | 13.2 | 7D–C | Venezuela | Peláez-Ballestas, 2018 |
| Karina | 7.2 | 7D–C | Venezuela | Peláez-Ballestas, 2018 |
| Chaima | 9.8 | 7D–C | Venezuela | Peláez-Ballestas, 2018 |
| Saraguro | 9.3 | 7D–C | Ecuador | Guevara, 2020 |
| Rural indigenous Brazil | 45.3 | PP | Brazil | Barbosa de Moraes, 2021 |
| Indigenous and Creole | 13.3 | PP | Suriname | Ho-A-Tham, 2021 |
| Oceania | ||||
| Aboriginals | 41.0 | PP | Australia | Honeyman et al., 1996 |
| Aboriginals | 72.0 | PP | Australia | Vindigni, 2005 |
| Aboriginals | 39.0 | 7D | Australia | Vindigni, 2004 |
| Aboriginals | 4.3 | 7D–C | Australia | Minaur, 2022 |
| Asia | ||||
| 3 tribal villages in India | 10.0 | PP | India | Mullerpatan, 2020 |
1 7D–C = 7-day prevalence using COPCORD protocol; 7D = 7-day prevalence; PP = point prevalence; 3M = 3-month prevalence.
3.2 Impact of LBP
In Australia, Aboriginals experienced long-term LBP but reported no disability due to LBP [19]. Honeyman et al. concluded that LBP was not a health issue and Aboriginals were buffered from (chronic) LBP due to their cultural beliefs [19]. However, more recent qualitative research has rejected this concept concluding that in Aboriginals, LBP is a highly disabling health concern, negatively affecting activities of daily living (ADL) and emotional and cultural well-being [28].
In three tribal villages in India, 95% of the participants reported having difficulty to perform at least one or more ADL due to LBP using a self-developed questionnaire [20]. Participants continued their ADL (such as field work and household activities), even though these activities aggravated their pain because they could not afford absence from work [20]. Similar findings were reported in Indigenous communities in Brazil where LBP had an impact on mood, sleep, and ADL [17]. Daily pain was somewhat accepted as part of the traditional Indigenous way of living and Indigenous Peoples minimized their pain [17,20].
3.3 Western health care in Indigenous Peoples
3.3.1 Pain and Western healthcare perception
3.3.1.1 Cultural beliefs
Pain is a universal, complex experience impacted by a wide variety of factors including beliefs, attitudes, and behavior. Orhan et al. concluded that various populations and ethnicities present differences in coping strategies, beliefs, and pain attitudes [29]. Aboriginals do not make their LBP publicly known due to cultural beliefs [28]. Vindigni et al. found that 33% of Aboriginals did not seek medical treatment for musculoskeletal conditions (of which LBP was the most prevalent condition) as they ‘learnt to live with it’ [21]. Studies done in the Quichuas in the Andes and Indigenous communities in the Amazon found that ignoring the pain was the most favored coping strategy [17,30].
Worldwide evidence shows LBP is partly iatrogenic and negative beliefs about LBP from health care practitioners (HCP) (e.g., LBP is caused by weak core) can harm patients [13]. Lin et al. found that biomedical, negative belief about LBP and its future consequences were present among Aboriginals in Australia due to interactions with Western HCP [31]. These negative beliefs have a negative, long-lasting impact on disability due to LBP [14]. This finding may be a consequence of greater exposure to biomedical beliefs, possibly in combination with erosion of cultural beliefs as previous research showed that LBP was not viewed as a health issue in Aboriginals [19].
3.3.1.2 Mistrust in Western healthcare
Mistrust of Western health care was seen in Indigenous Peoples in both the Americas and Australia [9,21,31,32]. Lack of trust in modern health care was caused by previous negative care experiences including stigmatization by the HCP, lack of empowerment in treatment decision-making, and perception that HCP fail to acknowledge their cultural identity and experience to understand pain [33,34].
3.3.2 Access to Western health care
Limited access to adequate Western health care due to financial constraints is a worldwide problem affecting almost half of the world’s population, especially many Indigenous communities [10,35]. In this review, the barriers for Indigenous Peoples with LBP were discussed along the journey of an Indigenous individual to Western health care as presented in Figure 2.
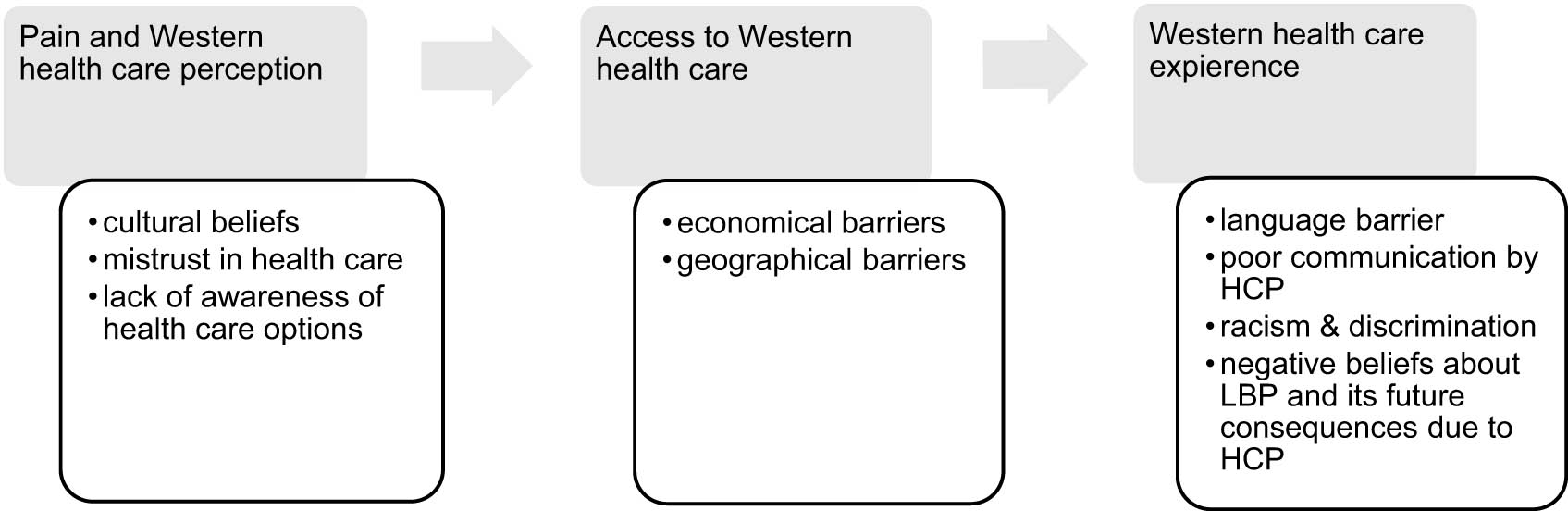
Western health care in Indigenous Peoples.
When an Indigenous person decides to seek Western medical care, many barriers for accessing health care exist [9,36]. Not in all countries a universal health care system is present. In South America, only 3% of the people reported having a complete social insurance, i.e., insurance that covers all necessary health-related expenses [12]. Furthermore, the cost of treatment is not affordable for many Indigenous Peoples [20,32,37].
Difficulty accessing adequate Western health care due to the geographical location of the communities is an important problem reported in multiple studies [9,10,20,21,32,37,38]. The most reported barriers were lack of (public) transport, high travel costs, and long travel time to adequate health care. For Indigenous individuals living in very remote villages in the Amazon, this barrier is obvious and hard to overcome [17]. Interestingly, also urban communities such as American Natives living 3 h from a hospital by car reported similar barriers [36]. Most of these natives live in poverty, without means of transportation to clinical appointments as public transport and ambulances are not available on all reservations [9]. Similar findings were reported by studies in Mexico, Venezuela, and India [20,32,37,39].
3.3.3 Western healthcare experience
When Indigenous managed to access Western health care for their LBP, the experience was often negative [31,32,34]. Communication with HCP is difficult as a limited number of HCP speak an Indigenous language, resulting in discrimination against patients who only speak an Indigenous language [17,32]. According to Aboriginals, poor communication by the HCP is one of the biggest factors contributing to inadequate care for LBP [33]. Indigenous Peoples reported having difficulties making themselves understood toward the HCP, even though they are fluent in English [33]. Information provided by the HCP was often unclear. Moreover Aboriginals reported being too embarrassed to ask for clarification (including medical jargon) [33]. Similar findings were reported in South America [5,17,32,40]. Commonly used clinical tools such as abstract scales are not all applicable to Indigenous patients [5,17,36,41]. For example, Indigenous Peoples express difficulties in reducing their pain intensity to a numerical scale [36,42]. Furthermore, negative stereotypes and racial views were present in HCP toward Indigenous patients [9,32,33,36].
4 Discussion
LBP is estimated to have a point prevalence of about 7.5% worldwide [2]. All five studies in our review reporting on point prevalence found higher prevalence rates compared to the global average [17,18,19,20,21].
Research on Indigenous populations and their experience with LBP is limited. Furthermore, the literature suffers from a disproportional representation of Indigenous communities. Specifically, about 40% of all articles were conducted in Australia, while they represent only 3% of the world’s Indigenous Peoples [39]. By contrast, only one study from Asia and no studies from Africa were included, while it is estimated that about 75% of the world’s Indigenous Peoples live in Asia and many Indigenous communities are present in Africa [43]. The recognition of Indigenous Peoples in Asia and Africa has been a complex and contentious issue influenced by social, economic, and political factors [15]. Empirical research and concerted efforts are still needed to address this issue. One of the limitations of this study is that all conclusions are mostly drawn from Indigenous Peoples in the Americas and Australia. Nonetheless, this review has identified a clear gap in research on these underrepresented Indigenous communities that could offer great scientific value if addressed.
This review highlights the need for more contextual considerations in the future for research and treatment of LBP in Indigenous Peoples. Not all measurement tools, treatment options, and methodologies used are applicable in Indigenous Peoples [28,36,42]. Both treatment and research approaches should be sensitive to the unique cultural, social, and economic context. Findings should be interpreted within the appropriate cultural context.
First, the use of Indigenous identity in studies often does not go beyond labeling based on ethnicity without further analysis of the psychosocial, economic, and cultural factors that may influence LBP outcomes. Considering the significant role of these factors in the prevalence and risk factors for LBP, using Indigenous Identity as a proxy variable could provide valuable insights.
Second, quantitative questionnaires lack cultural validity, and many have abstract scales that are hard to interpret for many Indigenous Peoples [5,17,36,41,42]. This limitation is particularly evident in this review when examining disability in Indigenous populations. LBP burden in Indigenous Peoples, even though quantitative questionnaires were not able to detect this previously [19,28]. Many Indigenous Peoples reported that they had no choice but to continue their ADL due to the socio-economic situation, possibly resulting in under representation of the true impact of LBP [17,20,28]. Disability may not carry the same meaning or even be a consideration in some Indigenous Peoples [28]. In 2011, Jimenez et al. made a recommendation for the development of culturally appropriate measurement tools as they identified the challenges with utilizing quantitative methods in Indigenous Peoples [36]. Only the WHO International League of Associations of Rheumatology Community Oriented Program for Control of Rheumatic Diseases protocol has done some in-depth research on cultural validity and adapted their questionnaire which has been used in some studies [5,32,37,40,42]. However, the authors of this article state that this development of more culturally appropriate measurement tools for LBP is a necessity and possesses substantial scientific value in quantitative research in Indigenous Peoples. Furthermore, some tools could prove to be useful in objectifying improvement in the treatment of LBP as well.
Alternatively, Lin et al. suggested that qualitative methods within a culturally rigorous framework could be more suitable to assess the impact of LBP [28]. Qualitative methods have more close engagement with Indigenous Peoples and attempt to understand the data through the perspective of Indigenous cultural lens if done correctly [28].
Third, a culturally adapted and safe setting in health care for Indigenous Peoples is frequently lacking and communication of the HCP is often poor, leading to miscommunications and negative health experience in Indigenous Peoples [31–34]. Worldwide, a gap exists between current evidence and intervention for LBP, even in high-income countries. Overuse of imaging for diagnostics, (opioid) medications, and surgery for treatment are a major problem as they are in conflict with current guidelines [14,44].
Exposure to HCP with a biomedical approach can have negative consequences for (Indigenous) patients as LBP is partly iatrogenic [31]. Current guidelines recommend that HCP should have an active approach focusing on psychosocial factors, education, and improving function to help patients with LBP [14]. Good communication and understanding between HCP and patients are cornerstones in the management of LBP and have an important influence on the outcome of the treatment [14]. Indigenous individuals with LBP need to be able to discuss their pain and associated factors in a safe and culturally appropriate setting [34,45,46]. Within healthcare systems, a culturally adapted and safe setting for Indigenous Peoples is frequently lacking and communication of the HCP is often poor with discrimination and racism being present around the world [9,32,36]. An HCP presented with an Indigenous patient often needs a way to overcome mistrust in health care systems and avoid miscommunications. Attention to language use as well as implementing a cultural form of conversation (e.g., ‘yarning’ in Aboriginal culture) could be beneficial [33,47]. This could help to build a relationship between HCP and their patients, which is an important factor in treatment satisfaction for Indigenous. Towle et al. suggested taking the time to listen to the patient and knowledge of the history of Indigenous Peoples can also enhance the communication [48].
Indigenous leaders and communities globally have emphasized the importance of training HCP in culturally safe care for Indigenous Peoples. In the past, these programs have been successful in mitigating racism and raising awareness [46,49,50]. However, more legislations and guidelines need to be implemented around the world to bring structural changes [51]. Despite some countries having white papers that stipulate equal accessible health care for all and legal entitlement for Indigenous patients to use their traditional language in healthcare interactions, many challenges to equal culturally safe care still exist [52].
Other initiatives such as development of culturally appropriate information for Aboriginals with LBP in line with the current guidelines could be beneficial [53]. As results seem promising, this could strengthen positive beliefs about LBP and reduce the need for access to physical and Western health care. The authors suggest that more similar initiatives should be taken in providing culturally adapted information on LBP management to Indigenous Peoples worldwide.
5 Conclusions
LBP is a burden among Indigenous Peoples impacting different aspects of their lives including their cultural identity. Obtaining Western healthcare presents unique challenges for Indigenous Peoples. Quality of health care is often unacceptable due to poor communication by HCP, ignorance of their patients’ culture, racism, and discrimination. While certain healthcare systems are actively striving for greater inclusivity for Indigenous Peoples, a considerable journey lies ahead.
The current literature lacks proportional representation of Indigenous Peoples, indicating a significant gap in the literature. Increased recognition, collaboration, and engagement with these underrepresented Indigenous Peoples are necessary to address this gap. Doing so has the potential to provide valuable scientific insights into these Indigenous Peoples and contribute to improving their health and well-being. It is time to act!
This article emphasizes the importance of contextual factors in both research and treatment in Indigenous Peoples due to their unique cultural identity. Many widely used measurement tools, treatment options, and methodologies lack cultural validity and are not applicable in Indigenous Peoples. The development of culturally valid measurement tools has important scientific merit and is essential for the advancements of research in Indigenous Peoples.
-
Research ethics: Not applicable.
-
Informed consent: Not applicable.
-
Author contributions: All authors have accepted responsibility for the entire content of this manuscript and approved its submission.
-
Competing interests: This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors. The authors have no conflicts of interest.
-
Research funding: Authors state that no funding was involved.
-
Data availability: Not applicable.
References
[1] Hartvigsen J, Hancock MJ, Kongsted A, Louw Q, Ferreira ML, Genevay S, et al. What low back pain is and why we need to pay attention. Lancet. 2018;391:2356–67. 10.1016/S0140-6736(18)30480-X.Search in Google Scholar PubMed
[2] Wu A, March L, Zheng X, Huang J, Wang X, Zhao J, et al. Global low back pain prevalence and years lived with disability from 1990 to 2017: Estimates from the Global Burden of Disease Study 2017. Ann Transl Med. 2020;8:299. 10.21037/atm.2020.02.175.Search in Google Scholar PubMed PubMed Central
[3] Taylor JB, Goode AP, George SZ, Cook CE. Incidence and risk factors for first-time incident low back pain: A systematic review and meta-analysis. Spine J. 2014;14:2299–319. 10.1016/j.spinee.2014.01.026.Search in Google Scholar PubMed
[4] Parreira P, Maher CG, Steffens D, Hancock MJ, Ferreira ML. Risk factors for low back pain and sciatica: an umbrella review. Spine J. 2018;18:1715–21. 10.1016/j.spinee.2018.05.018.Search in Google Scholar PubMed
[5] Del Río Nájera D, Santana N, Peláez-Ballestas I, González-Chávez SA, Quiñonez-Flores CM, Pacheco-Tena C. Prevalence of rheumatic diseases in Raramuri people in Chihuahua, Mexico: a community-based study. Clin Rheumatol. 2016;35:43–52. 10.1007/s10067-016-3225-x.Search in Google Scholar PubMed PubMed Central
[6] Anderson I, Robson B, Connolly M, Al-Yaman F, Bjertness E, King A, et al. Indigenous and tribal peoples’ health (The Lancet–Lowitja Institute Global Collaboration): a population study. Lancet. 2016;388:131–57. 10.1016/S0140-6736(16)00345-7.Search in Google Scholar PubMed
[7] United Nations. 10 things to know about indigenous peoples by United Nations Development Program| UNDP – Exposure; 2019.Search in Google Scholar
[8] United Nations. Department of Economic and Social Affairs. Permanent Forum on Indigenous Issues (United Nations), United Nations. Statistical Division. State of the world’s indigenous peoples 1st Volume; 2009.Search in Google Scholar
[9] Ottesen TD, Amick M, Kapadia A, Ziatyk EQ, Joe JR, Sequist TD, et al. The unmet need for orthopaedic services among American Indian and Alaska Native Communities in the United States. J Bone Jt Surg. 2022;104:E47. 10.2106/JBJS.21.00512.Search in Google Scholar PubMed
[10] Strozzi AG, Peláez-Ballestas I, Granados Y, Burgos-Vargas R, Quintana R, Londoño J, et al. Syndemic and syndemogenesis of low back pain in Latin-American population: a network and cluster analysis. Clin Rheumatol. 2020;39:2715–26. 10.1007/s10067-020-05047-x.Search in Google Scholar PubMed
[11] Green C, Todd KH, Lebovits A, Francis M. Disparities in pain: Ethical issues. Pain Med. 2006;7:530–3. 10.1111/j.1526-4637.2006.00244.x.Search in Google Scholar PubMed
[12] Peláez-Ballestas I, Granados Y, Quintana R, Loyola-Sánchez A, Julián-Santiago F, Rosillo C, et al. Epidemiology and socioeconomic impact of the rheumatic diseases on indigenous people: An invisible syndemic public health problem. Ann Rheumatic Dis. 2018;77(10):1397–404. 10.1136/annrheumdis-2018-213625.Search in Google Scholar PubMed
[13] Buchbinder R, van Tulder M, Öberg B, Costa LM, Woolf A, Schoene M, et al. Low back pain: A call for action. Lancet. 2018;391:2384–8. 10.1016/S0140-6736(18)30488-4.Search in Google Scholar PubMed
[14] Foster NE, Anema JR, Cherkin D, Chou R, Cohen SP, Gross DP, et al. Prevention and treatment of low back pain: evidence, challenges, and promising directions. Lancet. 2018;391:2368–83. 10.1016/S0140-6736(18)30489-6.Search in Google Scholar PubMed
[15] Bartlett JG, Madariaga-Vignudo L, O’Neil JD, Kuhnlein HV. Identifying indigenous peoples for health research in a global context: a review of perspectives and challenges. Int J Circumpolar Health. 2007;66:287–307. 10.3402/ijch.v66i4.18270.Search in Google Scholar PubMed
[16] UN Permanent Forum on Indigenous Issues. Who are indigenous peoples? 2002. https://www.un.org/esa/socdev/unpfii/documents/5session_factsheet1.pdf (accessed November 16, 2022).Search in Google Scholar
[17] Barbosa de Moraes EB, Dal Fabbro DR, de Oliveira LB, Leão ER. Pain management of amazon indigenous peoples: A community-based study. J Pain Res. 2021;14:1969–80. 10.2147/JPR.S298219.Search in Google Scholar PubMed PubMed Central
[18] Ho-A-Tham N, Ting-A-Kee B, Struyf N, Vanlandewijck Y, Dankaerts W. Low back pain prevalence, beliefs and treatment-seeking behaviour in multi-ethnic Suriname. Rheumatol Adv Pract. 2021;5(3):rkab074. 10.1093/rap/rkab074.Search in Google Scholar PubMed PubMed Central
[19] Honeyman PT, Jacobs EA. Effects of culture on back pain in Australian aboriginals. Spine. 1996;21:841–3. 10.1097/00007632-199604010-00013.Search in Google Scholar PubMed
[20] Mullerpatan R, Nahar S, Singh Y, Cote P, Nordin M. Burden of spine pain among rural and tribal populations in Raigad District of Maharashtra State of India. Eur Spine J. 2021;30:1004–10. 10.1007/s00586-020-06585-3.Search in Google Scholar PubMed
[21] Vindigni D, Griffen D, Perkins J, Da Costa C, Parkinson L. Prevalence of musculoskeletal conditions, associated pain and disability and the barriers to managing these conditions in a rural, Australian Aboriginal community. Rural Remote Health. 2004;4:230.10.22605/RRH230Search in Google Scholar
[22] Vindigni D, Walker BF, Jamison JR, Da Costa C, Parkinson L, Blunden S. Low back pain risk factors in a large rural Australian Aboriginal community. An opportunity managing co-morbidities? Chiropr Osteopathy. 2005;13:1–12. 10.1186/1746-1340-13-21.Search in Google Scholar PubMed PubMed Central
[23] Guevara SV, Feicán EA, Peláez I, Valdiviezo WA, Montaleza MA, Molina GM, et al. Prevalence of rheumatic diseases and quality of life in the saraguro indigenous people, Ecuador: A cross-sectional community-based study. J Clin Rheumatol. 2020;26:S139–47. 10.1097/RHU.0000000000001131.Search in Google Scholar PubMed
[24] Juárez V, Quintana R, Elena Crespo M, Aciar M, Buschiazzo E, Cucchiaro NL, et al. Prevalence of musculoskeletal disorders and rheumatic diseases in an Argentinean indigenous Wichi community. Clin Rheumatol. 2021;40:75–83. 10.1007/s10067-020-05130-3/Published.Search in Google Scholar
[25] Minaur N, Sawyers S, Parker J, Darmawan J. Rheumatic disease in an Australian Aboriginal community in North Queensland, Australia. A WHO-ILAR COPCORD survey. J Rheumatol. 2004;31:965–72.Search in Google Scholar
[26] Daerga L, Edin-Liljegren A, Sjölander P. Work-related musculoskeletal pain among reindeer herding Sami in Sweden - a pilot study on causes and prevention. Int J Circumpolar Health. 2004;63:343–8. 10.3402/ijch.v63i0.17932.Search in Google Scholar PubMed
[27] Sjolander P, Daerga L, Edin-Liljegren A, Jacobsson L. Musculoskeletal symptoms and perceived work strain among reindeer herders in Sweden. Occup Med. 2008;58:572–9. 10.1093/occmed/kqn153.Search in Google Scholar PubMed
[28] Lin IB, O’Sullivan PB, Coffin JA, Mak DB, Toussaint S, Straker LM. “I am absolutely shattered”: The impact of chronic low back pain on Australian Aboriginal people. Eur J Pain. 2012;16:1331–41. 10.1002/j.1532-2149.2012.00128.x.Search in Google Scholar PubMed
[29] Orhan C, Meeus M, Looveren EV, Cagnie B, Mukhtar NB, Lenoir D. Systematic review are pain beliefs, cognitions, and behaviors influenced by race, ethnicity, and culture in patients with chronic musculoskeletal pain: A systematic review. Pain Physician. 2018;21:541–58.10.36076/ppj.2018.6.541Search in Google Scholar
[30] Incayawar M, Saucier JF. Exploring pain in the Andes – learning from the Quichua (Inca) people experience. Postgrad Med. 2015;127:368–75. 10.1080/00325481.2015.1015395.Search in Google Scholar PubMed
[31] Lin IB, O’Sullivan PB, Coffin JA, Mak DB, Toussaint S, Straker LM. Disabling chronic low back pain as an iatrogenic disorder: A qualitative study in Aboriginal Australians. BMJ Open. 2013;3:e002654. 10.1136/bmjopen-2013-002654.Search in Google Scholar PubMed PubMed Central
[32] Peláez-Ballestas I, Alvarez-Nemegyei J, Loyola-Sánchez A, Escudero ML. Prevalence and factors associated with musculoskeletal disorders and rheumatic diseases in indigenous Maya-Yucateco people: a cross-sectional community-based study. Clin Rheumatol. 2016;35:15–23. 10.1007/s10067-015-3085-9.Search in Google Scholar PubMed PubMed Central
[33] Lin IB, O’Sullivan PB, Coffin JA, Toussaint S, Straker L. I can sit and talk to her, aboriginal people cLBP and healthcare practitioner communication. Aust Fam Physician. 2014;5:320–4.Search in Google Scholar
[34] Strong J, Nielsen M, Williams M, Huggins J, Sussex R. Quiet about pain: Experiences of Aboriginal people in two rural communities. Australian J Rural Health. 2015;23:181–4. 10.1111/ajr.12185.Search in Google Scholar PubMed
[35] World Health Organization and International Bank for Reconstruction and Development/The world Bank. Tracking universal health coverage: 2017 Global Monitoring Report; 2017.Search in Google Scholar
[36] Jimenez N, Garroutte E, Kundu A, Morales L, Buchwald D. A review of the experience, epidemiology, and management of pain among American Indian, Alaska Native, and Aboriginal Canadian peoples. J Pain. 2011;12:511–22. 10.1016/j.jpain.2010.12.002.Search in Google Scholar PubMed PubMed Central
[37] Granados Y, Rosillo C, Cedeño L, Martínez Y, Sánchez G, López G, et al. Prevalence of musculoskeletal disorders and rheumatic disease in the Warao, Kari’ña, and Chaima indigenous populations of Monagas State, Venezuela. Clin Rheumatol. 2016;35:53–61. 10.1007/s10067-016-3194-0.Search in Google Scholar PubMed PubMed Central
[38] Alvarez-Nemegyei J, Peláez-Ballestas I, Goñi M, Julián-Santiago F, García-García C, Quintana R, et al. Prevalence of rheumatic regional pain syndromes in Latin-American indigenous groups: a census study based on COPCORD methodology and syndrome-specific diagnostic criteria. Clin Rheumatol. 2016;35:63–70. 10.1007/s10067-016-3188-y.Search in Google Scholar PubMed PubMed Central
[39] Australian Bureau of Statistics. National Aboriginal and Torres Strait Islander Social Survey, 2014-15. Cat. No. 4714.0. ABS 2016; 2016.Search in Google Scholar
[40] Julián-Santiago F, García-García C, García-Olivera I, Goycochea-Robles MV, Pelaez-Ballestas I. Epidemiology of rheumatic diseases in Mixtec and Chontal indigenous communities in Mexico: A cross-sectional community-based study. Clin Rheumatol. 2016;35:35–42. 10.1007/s10067-015-3148-y.Search in Google Scholar PubMed PubMed Central
[41] Arthur L, Rolan P. A systematic review of western medicine’s understanding of pain experience, expression, assessment, and management for Australian Aboriginal and Torres Strait Islander Peoples. Pain Rep. 2019;4(6):e764. 10.1097/PR9.0000000000000764.Search in Google Scholar PubMed PubMed Central
[42] Peláez-Ballestas I, Granados Y, Silvestre A, Alvarez-Nemegyei J, Valls E, Quintana R, et al. Culture-sensitive adaptation and validation of the Community-Oriented Program for the Control of Rheumatic Diseases methodology for rheumatic disease in Latin American indigenous populations. Rheumatol Int. 2014;34:1299–309. 10.1007/s00296-014-2997-z.Search in Google Scholar PubMed
[43] Barsh R. The world’s indigenous Peoples. Lethbridge, MB: Department of Native American Studies, University of Lethbridge; 1999. p. 1–12.Search in Google Scholar
[44] O’Sullivan P. It’s time for change with the management of non-specific chronic low back pain. Br J Sports Med. 2012;46:224–7. 10.1136/bjsm.2010.081638.Search in Google Scholar PubMed
[45] Lærum E, Indahl A, Skouen JS. What is “the good back-consultation”? A combined qualitative and quantitative study of chronic low back pain patients’ interaction with and perceptions of consultations with specialists. J Rehabilitation Med. 2006;38:255–62. 10.1080/16501970600613461.Search in Google Scholar PubMed
[46] Graham S, Muir NM, Formsma JW, Smylie J. First nations, Inuit and Métis Peoples Living in Urban Areas of Canada and their access to healthcare: A systematic review. IJERPH. 2023;20:5956. 10.3390/ijerph20115956.Search in Google Scholar PubMed PubMed Central
[47] Lin IB, Green C, Bessarab D. “Yarn with me”: Applying clinical yarning to improve clinician-patient communication in Aboriginal health care. Australian J Prim Health. 2016;22:377–82. 10.1071/PY16051.Search in Google Scholar PubMed
[48] Towle A, Godolphin W, Alexander T. Doctor-patient communications in the Aboriginal community: Towards the development of educational programs. Patient Educ Counseling. 2006;62:340–6. 10.1016/j.pec.2006.06.006.Search in Google Scholar PubMed
[49] McDermott D, Bond C, Harding L, Jones R, Kaholokula JK, Kamaka M, et al. Having the hard conversations: strengthening pedagogical effectiveness by working with student and institutional resistance to Indigenous health curriculum. Canberra, ACT: Australian Government Department of Education; 2020.Search in Google Scholar
[50] Yaphe S, Richer F, Martin C. Cultural safety training for health professionals working with indigenous populations in Montreal, Québec. IJIH. 2019;14:60–84. 10.32799/ijih.v14i1.30861.Search in Google Scholar
[51] Wilson D, Ronde SDL, Brascoupé S, Nicole Apale A, Barney L, Guthrie B, et al. Health professionals working with first nations, Inuit, and Métis consensus guideline. J Obstet Gynaecol Can. 2013;35:550–3. 10.1016/S1701-2163(15)30915-4.Search in Google Scholar PubMed
[52] Engnes JI, Sivertsen N, Bongo BA, Mehus G. Sámi language in Norwegian health care: ‘He speaks good enough Norwegian, I don’t see why he needs an interpreter. Scand Caring Sci. 2022;36:275–84. 10.1111/scs.12986.Search in Google Scholar PubMed
[53] Lin IB, Ryder K, Coffin JA, Green C, Dalgety E, Scott B, et al. Addressing disparities in low back pain care by developing culturally appropriate information for Aboriginal Australians: “My back on track, my future. Pain Med. 2017;18:2070–80. 10.1093/pm/pnw314.Search in Google Scholar PubMed
© 2024 the author(s), published by De Gruyter
This work is licensed under the Creative Commons Attribution 4.0 International License.
Articles in the same Issue
- Editorial Comment
- From pain to relief: Exploring the consistency of exercise-induced hypoalgesia
- Christmas greetings 2024 from the Editor-in-Chief
- Original Articles
- The Scandinavian Society for the Study of Pain 2022 Postgraduate Course and Annual Scientific (SASP 2022) Meeting 12th to 14th October at Rigshospitalet, Copenhagen
- Comparison of ultrasound-guided continuous erector spinae plane block versus continuous paravertebral block for postoperative analgesia in patients undergoing proximal femur surgeries
- Clinical Pain Researches
- The effect of tourniquet use on postoperative opioid consumption after ankle fracture surgery – a retrospective cohort study
- Changes in pain, daily occupations, lifestyle, and health following an occupational therapy lifestyle intervention: a secondary analysis from a feasibility study in patients with chronic high-impact pain
- Tonic cuff pressure pain sensitivity in chronic pain patients and its relation to self-reported physical activity
- Reliability, construct validity, and factorial structure of a Swedish version of the medical outcomes study social support survey (MOS-SSS) in patients with chronic pain
- Hurdles and potentials when implementing internet-delivered Acceptance and commitment therapy for chronic pain: a retrospective appraisal using the Quality implementation framework
- Exploring the outcome “days with bothersome pain” and its association with pain intensity, disability, and quality of life
- Fatigue and cognitive fatigability in patients with chronic pain
- The Swedish version of the pain self-efficacy questionnaire short form, PSEQ-2SV: Cultural adaptation and psychometric evaluation in a population of patients with musculoskeletal disorders
- Pain coping and catastrophizing in youth with and without cerebral palsy
- Neuropathic pain after surgery – A clinical validation study and assessment of accuracy measures of the 5-item NeuPPS scale
- Translation, contextual adaptation, and reliability of the Danish Concept of Pain Inventory (COPI-Adult (DK)) – A self-reported outcome measure
- Cosmetic surgery and associated chronic postsurgical pain: A cross-sectional study from Norway
- The association of hemodynamic parameters and clinical demographic variables with acute postoperative pain in female oncological breast surgery patients: A retrospective cohort study
- Healthcare professionals’ experiences of interdisciplinary collaboration in pain centres – A qualitative study
- Effects of deep brain stimulation and verbal suggestions on pain in Parkinson’s disease
- Painful differences between different pain scale assessments: The outcome of assessed pain is a matter of the choices of scale and statistics
- Prevalence and characteristics of fibromyalgia according to three fibromyalgia diagnostic criteria: A secondary analysis study
- Sex moderates the association between quantitative sensory testing and acute and chronic pain after total knee/hip arthroplasty
- Tramadol-paracetamol for postoperative pain after spine surgery – A randomized, double-blind, placebo-controlled study
- Cancer-related pain experienced in daily life is difficult to communicate and to manage – for patients and for professionals
- Making sense of pain in inflammatory bowel disease (IBD): A qualitative study
- Patient-reported pain, satisfaction, adverse effects, and deviations from ambulatory surgery pain medication
- Does pain influence cognitive performance in patients with mild traumatic brain injury?
- Hypocapnia in women with fibromyalgia
- Application of ultrasound-guided thoracic paravertebral block or intercostal nerve block for acute herpes zoster and prevention of post-herpetic neuralgia: A case–control retrospective trial
- Translation and examination of construct validity of the Danish version of the Tampa Scale for Kinesiophobia
- A positive scratch collapse test in anterior cutaneous nerve entrapment syndrome indicates its neuropathic character
- ADHD-pain: Characteristics of chronic pain and association with muscular dysregulation in adults with ADHD
- The relationship between changes in pain intensity and functional disability in persistent disabling low back pain during a course of cognitive functional therapy
- Intrathecal pain treatment for severe pain in patients with terminal cancer: A retrospective analysis of treatment-related complications and side effects
- Psychometric evaluation of the Danish version of the Pain Self-Efficacy Questionnaire in patients with subacute and chronic low back pain
- Dimensionality, reliability, and validity of the Finnish version of the pain catastrophizing scale in chronic low back pain
- To speak or not to speak? A secondary data analysis to further explore the context-insensitive avoidance scale
- Pain catastrophizing levels differentiate between common diseases with pain: HIV, fibromyalgia, complex regional pain syndrome, and breast cancer survivors
- Prevalence of substance use disorder diagnoses in patients with chronic pain receiving reimbursed opioids: An epidemiological study of four Norwegian health registries
- Pain perception while listening to thrash heavy metal vs relaxing music at a heavy metal festival – the CoPainHell study – a factorial randomized non-blinded crossover trial
- Observational Studies
- Cutaneous nerve biopsy in patients with symptoms of small fiber neuropathy: a retrospective study
- The incidence of post cholecystectomy pain (PCP) syndrome at 12 months following laparoscopic cholecystectomy: a prospective evaluation in 200 patients
- Associations between psychological flexibility and daily functioning in endometriosis-related pain
- Relationship between perfectionism, overactivity, pain severity, and pain interference in individuals with chronic pain: A cross-lagged panel model analysis
- Access to psychological treatment for chronic cancer-related pain in Sweden
- Validation of the Danish version of the knowledge and attitudes survey regarding pain
- Associations between cognitive test scores and pain tolerance: The Tromsø study
- Healthcare experiences of fibromyalgia patients and their associations with satisfaction and pain relief. A patient survey
- Video interpretation in a medical spine clinic: A descriptive study of a diverse population and intervention
- Role of history of traumatic life experiences in current psychosomatic manifestations
- Social determinants of health in adults with whiplash associated disorders
- Which patients with chronic low back pain respond favorably to multidisciplinary rehabilitation? A secondary analysis of a randomized controlled trial
- A preliminary examination of the effects of childhood abuse and resilience on pain and physical functioning in patients with knee osteoarthritis
- Differences in risk factors for flare-ups in patients with lumbar radicular pain may depend on the definition of flare
- Real-world evidence evaluation on consumer experience and prescription journey of diclofenac gel in Sweden
- Patient characteristics in relation to opioid exposure in a chronic non-cancer pain population
- Topical Reviews
- Bridging the translational gap: adenosine as a modulator of neuropathic pain in preclinical models and humans
- What do we know about Indigenous Peoples with low back pain around the world? A topical review
- The “future” pain clinician: Competencies needed to provide psychologically informed care
- Systematic Reviews
- Pain management for persistent pain post radiotherapy in head and neck cancers: systematic review
- High-frequency, high-intensity transcutaneous electrical nerve stimulation compared with opioids for pain relief after gynecological surgery: a systematic review and meta-analysis
- Reliability and measurement error of exercise-induced hypoalgesia in pain-free adults and adults with musculoskeletal pain: A systematic review
- Noninvasive transcranial brain stimulation in central post-stroke pain: A systematic review
- Short Communications
- Are we missing the opioid consumption in low- and middle-income countries?
- Association between self-reported pain severity and characteristics of United States adults (age ≥50 years) who used opioids
- Could generative artificial intelligence replace fieldwork in pain research?
- Skin conductance algesimeter is unreliable during sudden perioperative temperature increases
- Original Experimental
- Confirmatory study of the usefulness of quantum molecular resonance and microdissectomy for the treatment of lumbar radiculopathy in a prospective cohort at 6 months follow-up
- Pain catastrophizing in the elderly: An experimental pain study
- Improving general practice management of patients with chronic musculoskeletal pain: Interdisciplinarity, coherence, and concerns
- Concurrent validity of dynamic bedside quantitative sensory testing paradigms in breast cancer survivors with persistent pain
- Transcranial direct current stimulation is more effective than pregabalin in controlling nociceptive and anxiety-like behaviors in a rat fibromyalgia-like model
- Paradox pain sensitivity using cuff pressure or algometer testing in patients with hemophilia
- Physical activity with person-centered guidance supported by a digital platform or with telephone follow-up for persons with chronic widespread pain: Health economic considerations along a randomized controlled trial
- Measuring pain intensity through physical interaction in an experimental model of cold-induced pain: A method comparison study
- Pharmacological treatment of pain in Swedish nursing homes: Prevalence and associations with cognitive impairment and depressive mood
- Neck and shoulder pain and inflammatory biomarkers in plasma among forklift truck operators – A case–control study
- The effect of social exclusion on pain perception and heart rate variability in healthy controls and somatoform pain patients
- Revisiting opioid toxicity: Cellular effects of six commonly used opioids
- Letter to the Editor
- Post cholecystectomy pain syndrome: Letter to Editor
- Response to the Letter by Prof Bordoni
- Response – Reliability and measurement error of exercise-induced hypoalgesia
- Is the skin conductance algesimeter index influenced by temperature?
- Skin conductance algesimeter is unreliable during sudden perioperative temperature increase
- Corrigendum
- Corrigendum to “Chronic post-thoracotomy pain after lung cancer surgery: a prospective study of preoperative risk factors”
- Obituary
- A Significant Voice in Pain Research Björn Gerdle in Memoriam (1953–2024)
Articles in the same Issue
- Editorial Comment
- From pain to relief: Exploring the consistency of exercise-induced hypoalgesia
- Christmas greetings 2024 from the Editor-in-Chief
- Original Articles
- The Scandinavian Society for the Study of Pain 2022 Postgraduate Course and Annual Scientific (SASP 2022) Meeting 12th to 14th October at Rigshospitalet, Copenhagen
- Comparison of ultrasound-guided continuous erector spinae plane block versus continuous paravertebral block for postoperative analgesia in patients undergoing proximal femur surgeries
- Clinical Pain Researches
- The effect of tourniquet use on postoperative opioid consumption after ankle fracture surgery – a retrospective cohort study
- Changes in pain, daily occupations, lifestyle, and health following an occupational therapy lifestyle intervention: a secondary analysis from a feasibility study in patients with chronic high-impact pain
- Tonic cuff pressure pain sensitivity in chronic pain patients and its relation to self-reported physical activity
- Reliability, construct validity, and factorial structure of a Swedish version of the medical outcomes study social support survey (MOS-SSS) in patients with chronic pain
- Hurdles and potentials when implementing internet-delivered Acceptance and commitment therapy for chronic pain: a retrospective appraisal using the Quality implementation framework
- Exploring the outcome “days with bothersome pain” and its association with pain intensity, disability, and quality of life
- Fatigue and cognitive fatigability in patients with chronic pain
- The Swedish version of the pain self-efficacy questionnaire short form, PSEQ-2SV: Cultural adaptation and psychometric evaluation in a population of patients with musculoskeletal disorders
- Pain coping and catastrophizing in youth with and without cerebral palsy
- Neuropathic pain after surgery – A clinical validation study and assessment of accuracy measures of the 5-item NeuPPS scale
- Translation, contextual adaptation, and reliability of the Danish Concept of Pain Inventory (COPI-Adult (DK)) – A self-reported outcome measure
- Cosmetic surgery and associated chronic postsurgical pain: A cross-sectional study from Norway
- The association of hemodynamic parameters and clinical demographic variables with acute postoperative pain in female oncological breast surgery patients: A retrospective cohort study
- Healthcare professionals’ experiences of interdisciplinary collaboration in pain centres – A qualitative study
- Effects of deep brain stimulation and verbal suggestions on pain in Parkinson’s disease
- Painful differences between different pain scale assessments: The outcome of assessed pain is a matter of the choices of scale and statistics
- Prevalence and characteristics of fibromyalgia according to three fibromyalgia diagnostic criteria: A secondary analysis study
- Sex moderates the association between quantitative sensory testing and acute and chronic pain after total knee/hip arthroplasty
- Tramadol-paracetamol for postoperative pain after spine surgery – A randomized, double-blind, placebo-controlled study
- Cancer-related pain experienced in daily life is difficult to communicate and to manage – for patients and for professionals
- Making sense of pain in inflammatory bowel disease (IBD): A qualitative study
- Patient-reported pain, satisfaction, adverse effects, and deviations from ambulatory surgery pain medication
- Does pain influence cognitive performance in patients with mild traumatic brain injury?
- Hypocapnia in women with fibromyalgia
- Application of ultrasound-guided thoracic paravertebral block or intercostal nerve block for acute herpes zoster and prevention of post-herpetic neuralgia: A case–control retrospective trial
- Translation and examination of construct validity of the Danish version of the Tampa Scale for Kinesiophobia
- A positive scratch collapse test in anterior cutaneous nerve entrapment syndrome indicates its neuropathic character
- ADHD-pain: Characteristics of chronic pain and association with muscular dysregulation in adults with ADHD
- The relationship between changes in pain intensity and functional disability in persistent disabling low back pain during a course of cognitive functional therapy
- Intrathecal pain treatment for severe pain in patients with terminal cancer: A retrospective analysis of treatment-related complications and side effects
- Psychometric evaluation of the Danish version of the Pain Self-Efficacy Questionnaire in patients with subacute and chronic low back pain
- Dimensionality, reliability, and validity of the Finnish version of the pain catastrophizing scale in chronic low back pain
- To speak or not to speak? A secondary data analysis to further explore the context-insensitive avoidance scale
- Pain catastrophizing levels differentiate between common diseases with pain: HIV, fibromyalgia, complex regional pain syndrome, and breast cancer survivors
- Prevalence of substance use disorder diagnoses in patients with chronic pain receiving reimbursed opioids: An epidemiological study of four Norwegian health registries
- Pain perception while listening to thrash heavy metal vs relaxing music at a heavy metal festival – the CoPainHell study – a factorial randomized non-blinded crossover trial
- Observational Studies
- Cutaneous nerve biopsy in patients with symptoms of small fiber neuropathy: a retrospective study
- The incidence of post cholecystectomy pain (PCP) syndrome at 12 months following laparoscopic cholecystectomy: a prospective evaluation in 200 patients
- Associations between psychological flexibility and daily functioning in endometriosis-related pain
- Relationship between perfectionism, overactivity, pain severity, and pain interference in individuals with chronic pain: A cross-lagged panel model analysis
- Access to psychological treatment for chronic cancer-related pain in Sweden
- Validation of the Danish version of the knowledge and attitudes survey regarding pain
- Associations between cognitive test scores and pain tolerance: The Tromsø study
- Healthcare experiences of fibromyalgia patients and their associations with satisfaction and pain relief. A patient survey
- Video interpretation in a medical spine clinic: A descriptive study of a diverse population and intervention
- Role of history of traumatic life experiences in current psychosomatic manifestations
- Social determinants of health in adults with whiplash associated disorders
- Which patients with chronic low back pain respond favorably to multidisciplinary rehabilitation? A secondary analysis of a randomized controlled trial
- A preliminary examination of the effects of childhood abuse and resilience on pain and physical functioning in patients with knee osteoarthritis
- Differences in risk factors for flare-ups in patients with lumbar radicular pain may depend on the definition of flare
- Real-world evidence evaluation on consumer experience and prescription journey of diclofenac gel in Sweden
- Patient characteristics in relation to opioid exposure in a chronic non-cancer pain population
- Topical Reviews
- Bridging the translational gap: adenosine as a modulator of neuropathic pain in preclinical models and humans
- What do we know about Indigenous Peoples with low back pain around the world? A topical review
- The “future” pain clinician: Competencies needed to provide psychologically informed care
- Systematic Reviews
- Pain management for persistent pain post radiotherapy in head and neck cancers: systematic review
- High-frequency, high-intensity transcutaneous electrical nerve stimulation compared with opioids for pain relief after gynecological surgery: a systematic review and meta-analysis
- Reliability and measurement error of exercise-induced hypoalgesia in pain-free adults and adults with musculoskeletal pain: A systematic review
- Noninvasive transcranial brain stimulation in central post-stroke pain: A systematic review
- Short Communications
- Are we missing the opioid consumption in low- and middle-income countries?
- Association between self-reported pain severity and characteristics of United States adults (age ≥50 years) who used opioids
- Could generative artificial intelligence replace fieldwork in pain research?
- Skin conductance algesimeter is unreliable during sudden perioperative temperature increases
- Original Experimental
- Confirmatory study of the usefulness of quantum molecular resonance and microdissectomy for the treatment of lumbar radiculopathy in a prospective cohort at 6 months follow-up
- Pain catastrophizing in the elderly: An experimental pain study
- Improving general practice management of patients with chronic musculoskeletal pain: Interdisciplinarity, coherence, and concerns
- Concurrent validity of dynamic bedside quantitative sensory testing paradigms in breast cancer survivors with persistent pain
- Transcranial direct current stimulation is more effective than pregabalin in controlling nociceptive and anxiety-like behaviors in a rat fibromyalgia-like model
- Paradox pain sensitivity using cuff pressure or algometer testing in patients with hemophilia
- Physical activity with person-centered guidance supported by a digital platform or with telephone follow-up for persons with chronic widespread pain: Health economic considerations along a randomized controlled trial
- Measuring pain intensity through physical interaction in an experimental model of cold-induced pain: A method comparison study
- Pharmacological treatment of pain in Swedish nursing homes: Prevalence and associations with cognitive impairment and depressive mood
- Neck and shoulder pain and inflammatory biomarkers in plasma among forklift truck operators – A case–control study
- The effect of social exclusion on pain perception and heart rate variability in healthy controls and somatoform pain patients
- Revisiting opioid toxicity: Cellular effects of six commonly used opioids
- Letter to the Editor
- Post cholecystectomy pain syndrome: Letter to Editor
- Response to the Letter by Prof Bordoni
- Response – Reliability and measurement error of exercise-induced hypoalgesia
- Is the skin conductance algesimeter index influenced by temperature?
- Skin conductance algesimeter is unreliable during sudden perioperative temperature increase
- Corrigendum
- Corrigendum to “Chronic post-thoracotomy pain after lung cancer surgery: a prospective study of preoperative risk factors”
- Obituary
- A Significant Voice in Pain Research Björn Gerdle in Memoriam (1953–2024)


