Abstract
This study evaluates the efficacy and safety of bevacizumab (BEV) in the treatment of non-small cell lung cancer (NSCLC) patients with brain metastases (BM) by performing meta-analyses of response and survival indices. Seventeen studies were included. BEV treatment was associated with a lower new BM incidence (hazard ratio: 0.30 [95% confidence interval (CI): 0.14, 0.46]) during follow-up. Disease control rate (DCR) of BEV-treated patients with BM was 91% [95% CI: 85, 95]. However, intracranial DCR was relatively higher (94% [95% CI: 87, 98]) than extracranial DCR (86% [95% CI: 74, 96]). DCR of NSCLC patients with BM was significantly better with BEV than with control therapies (odds ratio: 2.71 [95% CI: 1.26, 5.86], P = 0.01). Progression-free survival (PFS) of BEV-treated patients with and without BM was 7.1 months [95% CI: 6.2, 8.0] and 7.4 months [95% CI: 6.3, 8.4], respectively. Intracranial PFS of BEV-treated patients with BM was 8.0 months [95% CI: 6.0, 10.0]. Overall survival of BEV-treated NSCLC patients with and without BM was 13.5 months [95% CI: 11.4, 15.6] and 12.5 months [95% CI: 10.2, 14.8], respectively. The incidence of bleeding/hemorrhage in the central nervous system was 1% with BEV treatment.
1 Introduction
Non-small cell lung cancer (NSCLC) comprises 80–85% of all types of lung cancer and is a leading cause of cancer-related mortality among men and women worldwide [1]. Of all NSCLC cases, 60–70% are diagnosed with stage IIIB or IV for which the prognosis is poor [2]. Active or passive smoking, alcohol use, air pollution, occupational exposure, and cancer susceptibility genes are important risk factors for NSCLC [3]. The 5-year survival of NSCLC patients after diagnosis is only 15% [3]. Age, stage of cancer, performance status, mediastinal lymph node status at diagnosis, comorbidity, leukocyte and neutrophil count, delay of management, and antitumor treatment are important determinants of the prognosis [4,5]. Brain metastasis (BM) is a common consequence of lung cancer, with an incidence of approximately 10% at initial diagnosis and up to 40% during the progression of disease [6,7].
Conventionally, chemotherapy and radiotherapy are the mainstays of treatment for BM. The median progression-free survival (PFS) of NSCLC patients with BM is approximately 8–9 months after stereotactic radiosurgery or whole-brain radiation therapy and chemotherapy [8,9]. With the development of targeted therapies, clinical and survival outcomes of NSCLC patients have been improved. Among tyrosine kinase inhibitors (TKIs), osimertinib as first-line treatment significantly improves PFS compared with first-generation TKIs (19 versus 10 months) in NSCLC patients [10]. Although patients can benefit from such therapies, some limitations still exist such as drug resistance to epidermal growth factor receptor and anaplastic lymphoma kinase inhibitors, the impaired ability of drugs to cross the blood–brain barrier, and impaired neurocognitive function caused by the whole-brain radiation therapy [11]. Therefore, advanced treatment options are needed for NSCLC patients.
Bevacizumab (BEV), a recombinant humanized monoclonal antibody against vascular endothelial growth factor (VEGF), has exhibited efficacy in several cancer types. This antibody can inhibit tumor growth by competing with VEGF for VEGF receptors. Several trials are conducted to evaluate the efficacy and safety of BEV, which are also well reviewed. A meta-analysis of 24 randomized controlled trials found that BEV treatment improved the overall survival (OS) and PFS in patients with metastatic solid tumors but was associated with a statistically higher incidence of fatal adverse events (AEs) overall and an increased risk of fatal pulmonary hemorrhage in patients with lung cancer [12]. However, a meta-analysis of cancer patients with BM found that BEV treatment was not associated with a significantly increased risk of intracerebral hemorrhage [13].
The meta-analyses of patients with advanced NSCLC have also shown that BEV treatment with chemotherapy was able to significantly prolong OS and PFS and was well tolerated [14,15]. However, clinical potentials of BEV for NSCLC patients with BM are not clear. The aim of this study was to systematically review the studies that have evaluated the efficacy and safety of BEV in NSCLC patients with BM to perform meta-analyses of important indices to gain a refined evidence of the efficacy and safety of BEV in the treatment of NSCLC patients with BM.
2 Methods
2.1 Search strategy
Electronic databases (Cochrane Library, Clinical Trials, CNKI, Embase, Google Scholar, Ovid SP, and PubMed) were searched for relevant articles published before January 2020. The following terms were used for the search: bevacizumab, Avastin, non-small cell lung cancer, brain, central nervous system, CNS, metastases, efficacy, safety, response, and survival. After identifying the relevant articles, we also checked the reference lists of the included studies to find additional relevant studies.
2.2 Eligibility criteria
Inclusion criteria were that the study (1) recruited adult NSCLC patients (tissue or cell diagnosed) with BM (diagnosed with computed tomography or magnetic resonance imaging) who were treated with BEV alone or in combination with other therapies; (2) recruited adult NSCLC patients without BM and treated them with BEV to examine the incidence of BM during study period; and (3) reported quantitative data of efficacy and safety, especially the disease control rate (DCR), the overall response rate (ORR), PFS, OS, and the incidence of AEs. Exclusion criteria were that the study: (1) did not differentiate the outcomes by BM, (2) used BEV for brain lesions other than BM from NSCLC, (3) had a follow-up completion rate of less than 60%, and (4) published as case reports.
2.3 Data extraction and study quality assessment
The following data were extracted from research articles of the qualified studies: study design and conduct variables; demographic information and clinical and pathological characteristics of the patients; performance status and mutational characteristics of the patients; treatments and dosage schedules; treatment history; outcome data, especially for PFS, OS, DCR, ORR, treatment-related mortality, grade 3 or 4 AEs; and associational data. Three reviewers identified the eligible articles independently by the following eligibility criteria. Any disagreement was resolved with mutual discussions or by involving a senior colleague. Data extraction was also carried out by 3 reviewers independently and then outputs were unified by arriving at consensus when any disagreement arose. Study quality assessment was performed with the Newcastle-Ottawa Scale for observational studies.
2.4 Statistical analyses
The hazard ratios (HRs) reported by the individual studies were pooled under random effects model to achieve HR estimates of (1) the survival of BEV-treated versus control NSCLC patients with BM, (2) the survival of BEV-treated NSCLC patients with BM versus without BM, and (3) the incidence versus no incidence of BM during the study in patients who were without BM at study start.
A meta-analysis of the odds ratios (ORs) was performed to determine the significance of difference in the DCR and ORR between the BEV and control treatments in the NSCLC patients with BM using binomial data reported by the individual studies. In a separate meta-analysis, the median PFS and OS rates reported by the individual studies were pooled under random effects model by subgrouping the patients with and without BM.
The meta-analyses of the proportions with Freeman–Tukey double arcsine transformation were performed to achieve the complete remission, partial remission, stable disease, progressive disease, ORR, DCR, 1-year OS, and the incidence of bleeding or hemorrhage in the central nervous system (CNS) rates by subgrouping the outcomes with regard to intracranial and extracranial or BM and no BM outcomes. The clinical significance of the outcomes was decided based on the overall/subgroup effect sizes and their corresponding 95% confidence intervals (CIs).
Publication bias assessment was performed with Begg’s funnel plot asymmetry test. The statistical analyses were performed with Stata software (Stata Corporation, Texas, USA) or with the Cochrane Review Manager software.
3 Results
3.1 Characteristics of the included studies
Seventeen studies [16–32] were selected based on the eligibility criteria (Figure 1). Fifteen studies had 7,212 NSCLC patients with BM at baseline, of which 1,548 were treated with BEV in combination with one or more therapies including chemotherapy, radiotherapy, stereotactic radiosurgery, and TKIs, and 5,664 patients served as controls who were treated with one or more of the above-mentioned therapies without BEV. Two studies recruited patients without BM at baseline (806 BEV-treated and 396 control patients) and followed them for the incidence of BM through follow-up. No significant publication bias was detected by Begg’s test (P = 0.245; Figure S1).
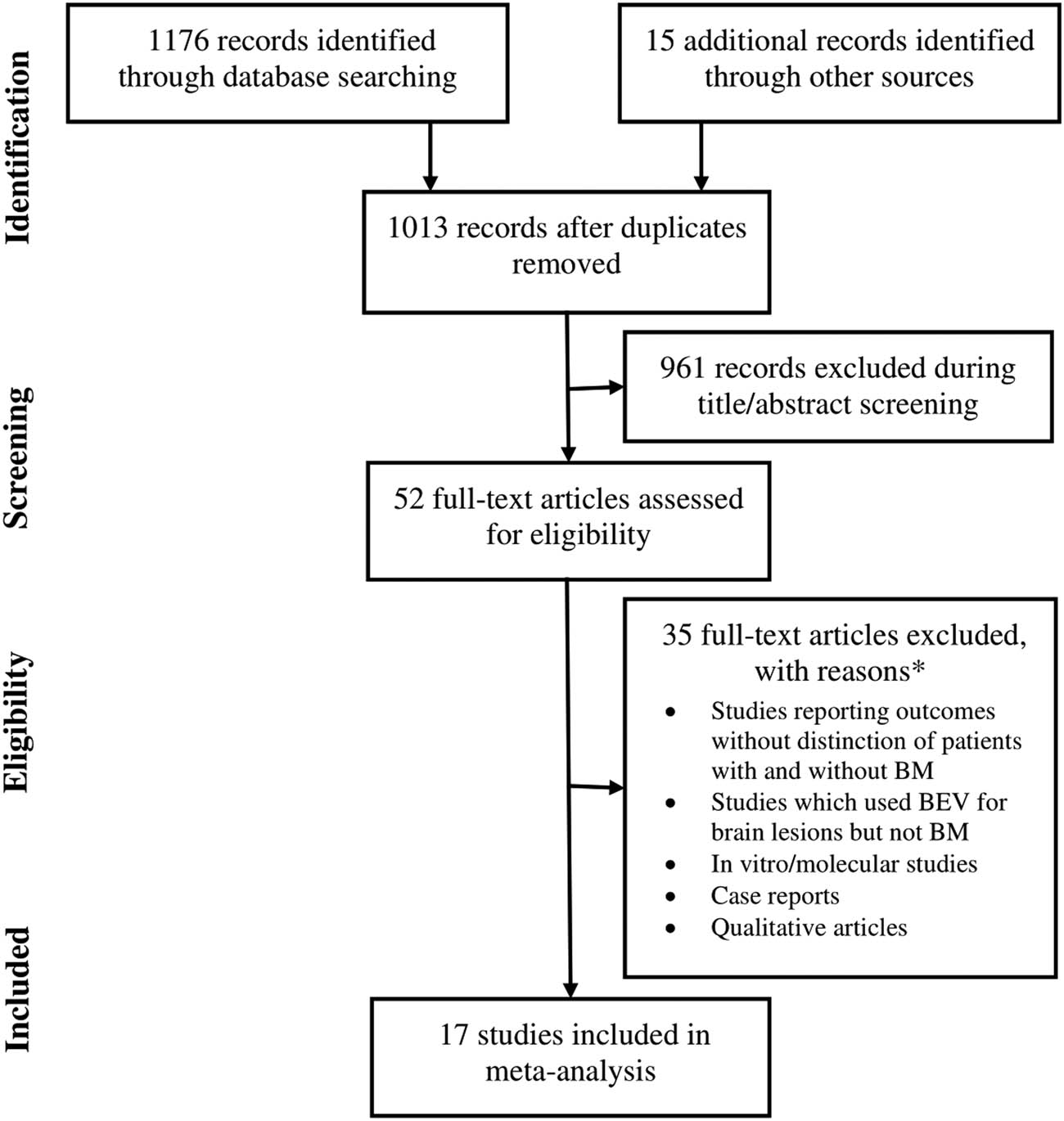
A flowchart of the study screening and selection process.
Important characteristics of the included studies are presented in Table S1, and study design and treatment features are presented in Table S2. Adenocarcinoma was predominant histological subtype of NSCLC, which was found in 87% [95% CI: 81, 92] of the patients, whereas large cell carcinoma was found in 10% [95% CI: 4, 17] of the patients. Most of the patients had an Eastern Ontario Oncology Group performance status of 0 or 1 (93% [95% CI: 84, 98]). The percentage of smokers (current or past) was 52% [95% CI: 38, 65]. In general, the quality of the included studies was above moderate. An assessment with New Castle–Ottawa scales is presented in Table S3.
3.2 Prevention of BM incidence
In two studies that recruited NSCLC patients without BM at baseline, in comparison with chemotherapy alone, BEV treatment with chemotherapy was associated with low BM incidence in the NSCLC patients without BM at the start of study (HR: 0.30 [95% CI: 0.14, 0.46]; Figure 2).
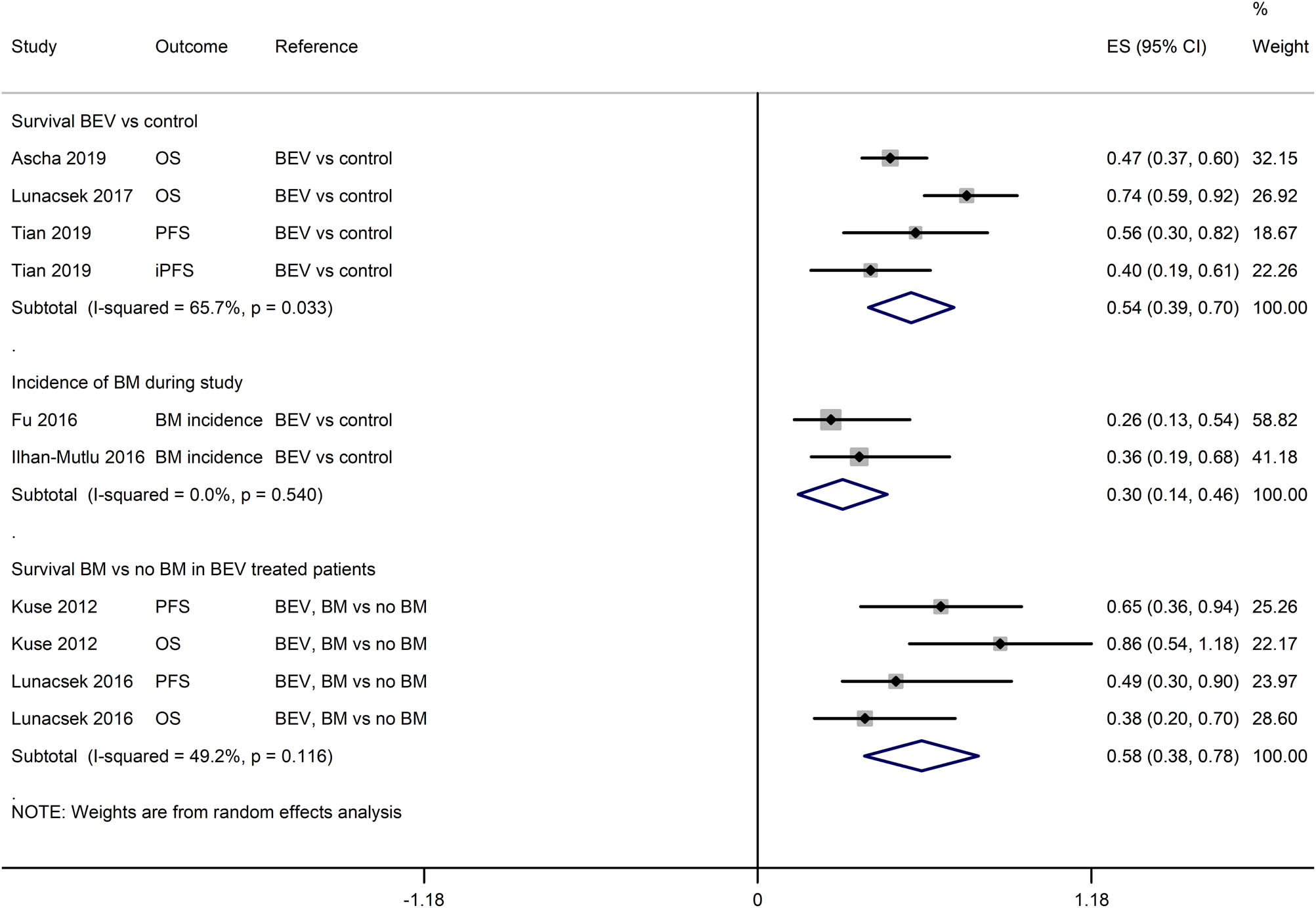
A forest graph showing the pooled HRs (effect size and 95% CI) regarding the incidence of new BM or survival to show BEV efficacy in preventing BM and survival outcomes.
3.3 Response rates
In a pooled analysis, the overall DCR in the NSCLC patients with BM was 91% [95% CI: 85, 95]. However, the intracranial DCR was higher (94% [95% CI: 87, 98] than the extracranial DCR (86% [95% CI: 74, 96]) (Figure 3). In the NSCLC patients with BM, the ORR and DCR of the BEV-treated regimen were significantly better than those of the control treatments (OR: 2.03 [1.28, 3.20]; P = 0.002 for the ORR; and OR: 2.87 [1.32, 6.23]; P = 0.008 for the DCR; Figure 4). Correspondingly, the intracranial versus extracranial response rates of BEV-treated NSCLC patients with BM were 6% [95% CI: 0, 17] versus 0% [95% CI: 0, 4] for complete remission, 42% [95% CI: 33, 51] versus 47% [95% CI: 26, 68] for partial remission, 35% [95% CI: 26, 44] versus 28% [95% CI: 17, 40] for stable disease, and 5% [95% CI: 0, 13] versus 12% [95% CI: 3, 26] for progressive disease (Figures S2–S5).
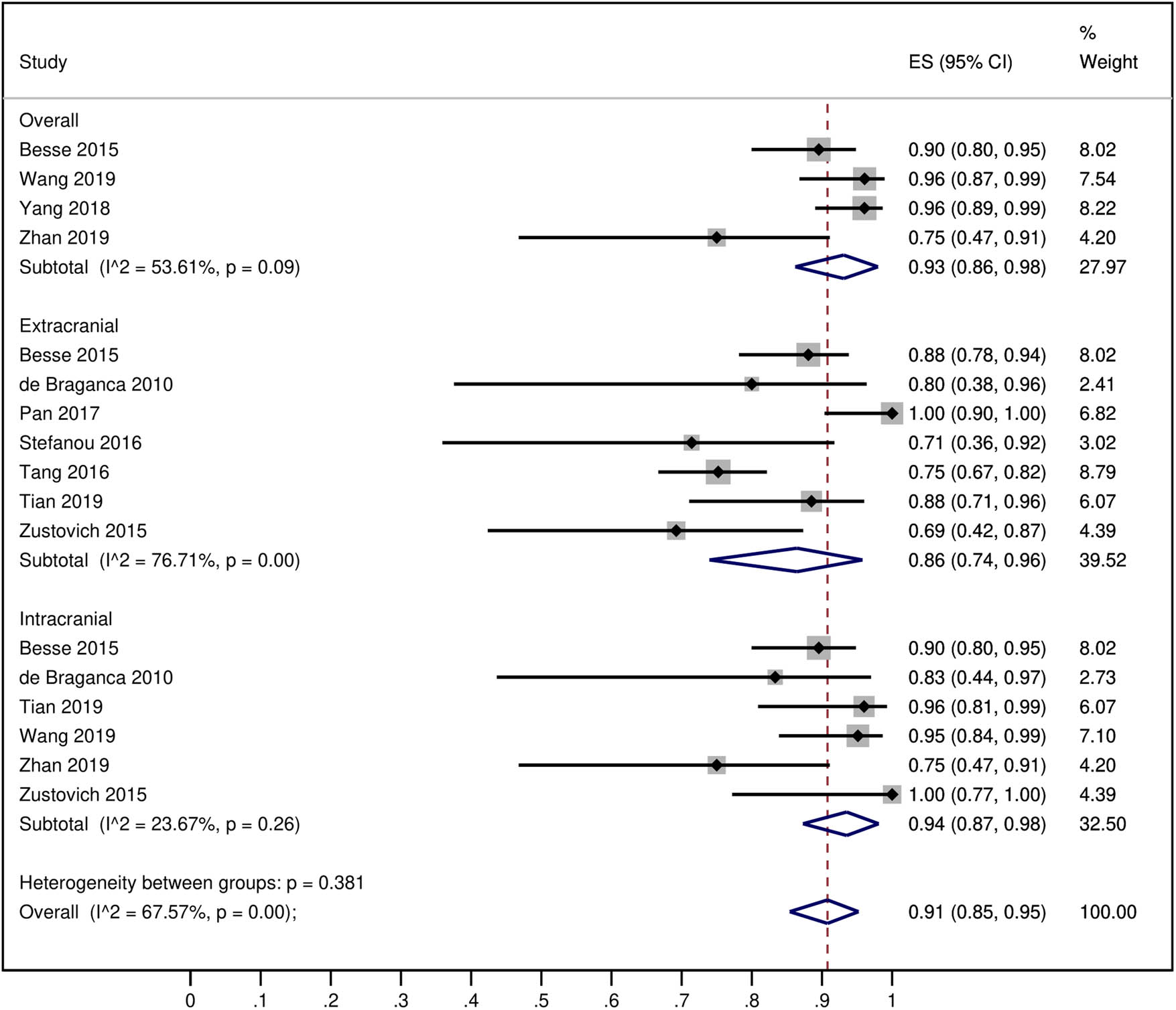
A forest graph showing the pooled DCRs of the BEV-treated NSCLC patients with the intracranial and extracranial subgroups. Subgroup “overall” represents the DCR of studies that reported DCR rates without distinguishing intracranial and extracranial DCRs.
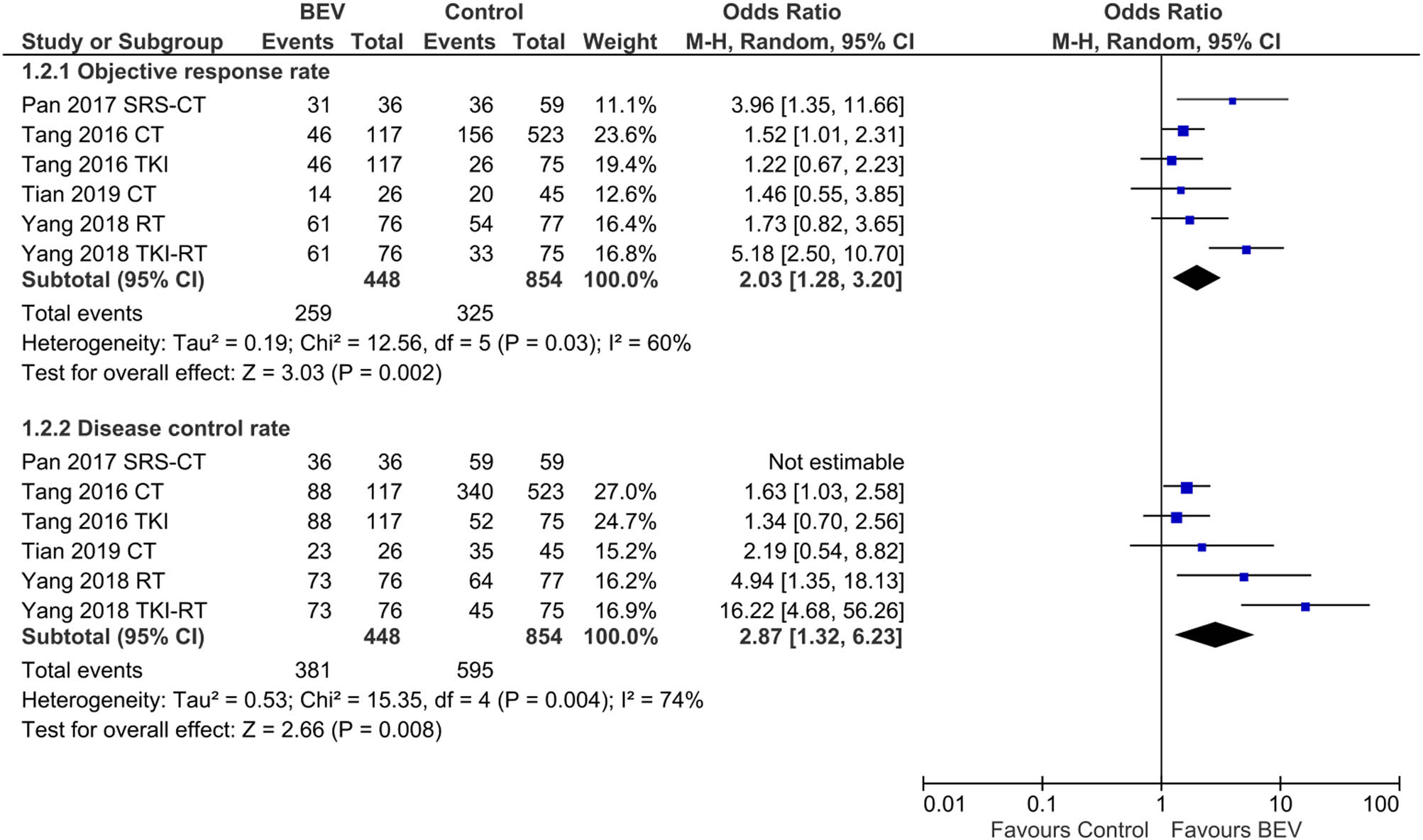
A forest graph showing the outcomes of the meta-analysis of the ORs between the BEV-treated and control patients in the ORR and DCR. Abbreviations in study identities: CT, chemotherapy; RT, radiotherapy; SRS, stereotactic radiosurgery; TKI, tyrosine kinase inhibitor.
3.4 Survival
The PFS of the BEV-treated NSCLC patients with and without BM was 7.10 months [95% CI: 6.17, 8.03] and 7.37 months [95% CI: 6.30, 8.43], respectively, whereas the intracranial PFS of the BEV-treated NSCLC patients with BM was 7.98 months [95% CI: 5.95, 10.0] (Figure 5). The OS of the BEV-treated NSCLC patients with and without BM was 13.49 months [95% CI: 11.35, 15.62] and 12.49 months [95% CI: 10.22, 14.76], respectively (Figure S6). The 1-year OS in the NSCLC patients with BM was 66% [95% CI: 56, 74] (Figure S7). The pooled analyses of HRs reported by the individual studies indicated that the BEV treatment was associated with better survival in comparison with the control treatments in the NSCLC patients with BM (HR: 0.54 [95% CI: 0.39, 0.70]). Moreover, the BEV treatment was also associated with better survival in NSCLC patients with BM in comparison with NSCLC patients without BM (HR: 0.58 [95% CI: 0.38, 0.78]; Figure 2).
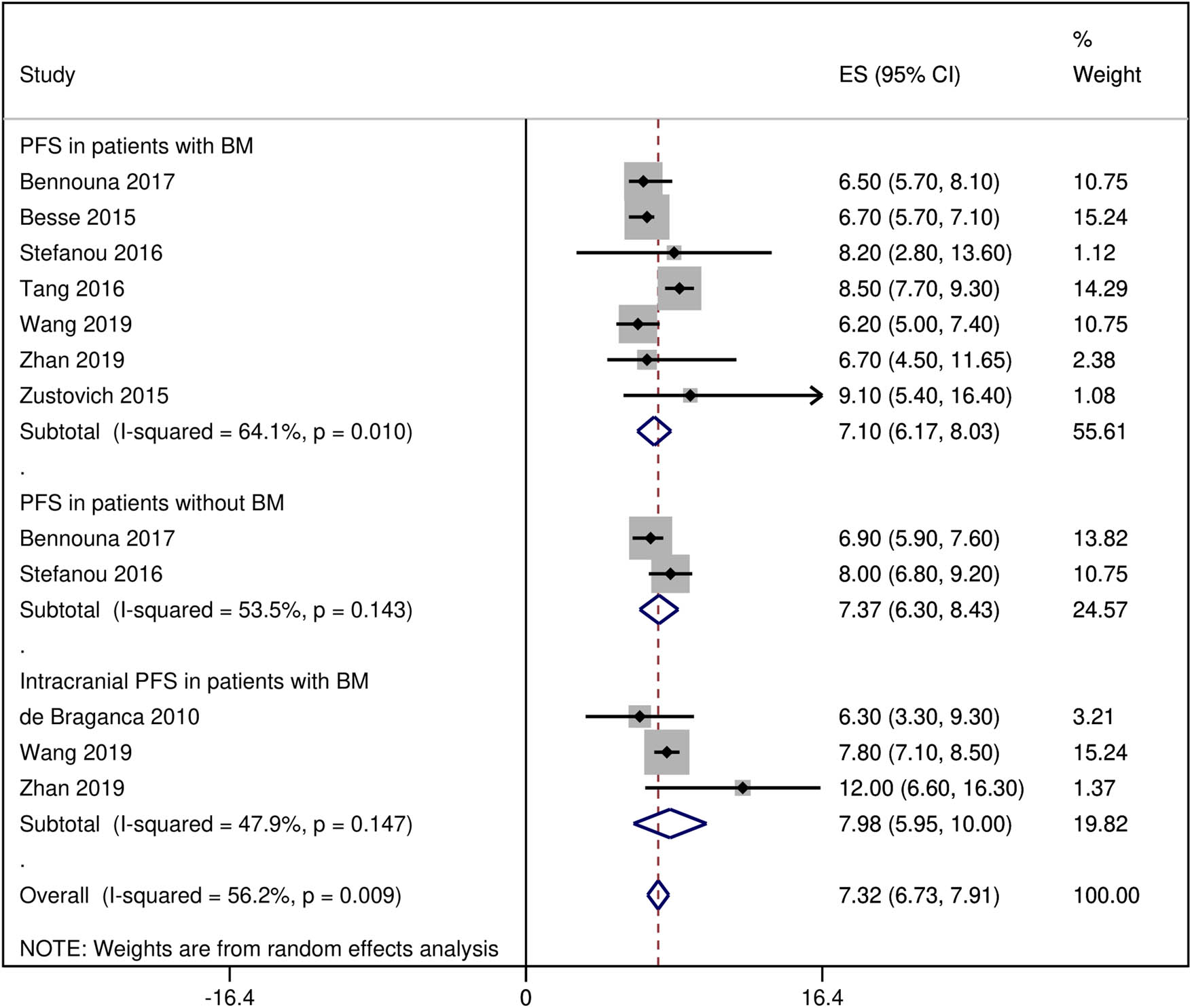
A forest graph showing the pooled overall and subgroup PFS rates of BEV-treated patients.
3.5 CNS bleeding
A meta-analysis of the studies that reported bleeding/hemorrhage in the CNS estimated the incidence at 1% [0, 3] with the BEV treatment as combinational regimen in the NSCLC patients with BM (Figure S8).
4 Discussion
This meta-analysis found that BEV treatment was associated with better efficacy in NSCLC patients with BM in comparison with control therapies; BEV efficacy was also better in patients with BM than in patients without BM; and BEV has preventive potentials for new BM incidence during the study follow-up. The incidence of intracranial hemorrhage was low (1%) in this population of NSCLC patients.
BM is one of the common complications of advanced NSCLC as more than 50% of NSCLC patients eventually develop BM [33]. BEV obstructs the VEGF pathway and has been shown to inhibit the growth of tumor cells by promoting tumor vascular degradation and normalizing existing tumor blood vessels [34,35]. Clinically, BEV-based treatments have become new therapeutic options for NSCLC patients with BM. However, only a few prospective studies have been made on BM from NSCLC, and debate continues about whether patients with BM can benefit from a BEV-based therapy.
The results of this meta-analysis show that as a first-line or maintenance therapy, BEV reduced the risk of a new incidence of BM from NSCLC by approximately 70% compared with chemotherapy or placebo. Blood circulation is a major path for tumor metastasis. As a VEGF inhibitor, BEV inhibits the growth of human tumor xenografts [36,37] and normalizes tumor blood vessels [35]. Therefore, we speculate that the possible mechanism of action of BEV is to prevent tumor cells from entering the blood vessels, which then reduces the incidence of BM.
BEV may normalize tumor blood vessels, which may result in a more efficient delivery and action of chemotherapies [35]. Pan et al. have reported that stereotactic radiotherapy combined with BEV to treat BM from pulmonary adenocarcinoma can achieve higher near-term tumor remission and perilesional edema control rates [24]. Furthermore, a study on mice showed that BEV not only inhibited angiogenesis but also enhanced the cytotoxicity of cisplatin and promoted apoptosis of tumor cells as a chemosensitizer [38]. It has also been found that low-dose BEV can also be used to treat brain edema due to radiotherapy [39].
Generally, the side effects of BEV therapy include hemorrhage/bleeding, wound healing complications, gastrointestinal perforation, arterial thromboembolism, congestive heart failure, hypertension, proteinuria/nephrotic syndrome, infusion-related hypersensitivity reactions, and reversible posterior leukoencephalopathy syndrome [40,41]. A meta-analysis of eight studies found that BEV treatment was not associated with a significant increase in intracerebral hemorrhage in cancer patients with BM [13]. In this study, the CNS bleeding rate with BEV treatment in NSCLC patients was 1%, which suggests that the risk of intracerebral hemorrhage is low with BEV treatment.
However, bleeding potential of BEV should not be overlooked altogether, as some studies have shown considerable bleeding events with BEV treatment. In a phase IV trial (SAiL) of the 2,212 non-squamous NSCLC patients treated with BEV, 38.2% had a bleeding event, of which 87% were resolved but 10% led to BEV discontinuation. The incidence of grade ≥3 pulmonary hemorrhage and intracerebral hemorrhage was 0.7% and 0.1%, respectively, in a previous study [42]. A meta-analysis also found that BEV treatment was associated with an increased risk of fatal pulmonary hemorrhage (relative risk 5.65 [95% CI: 1.26, 25.26]) in patients with lung cancer [12].
The meta-analysis of several indices reflecting the efficacy of BEV in the NSCLC patients with BM is the major strength of this study. Moreover, a reliable estimate of the incidence of CNS hemorrhage in the NSCLC patients with BM is also reported for the first time herein. However, some limitations of this study should also be noted: (1) no studies could be found from the literature to evaluate BEV versus other therapies with regard to survival, so a comparative account with regard to survival could not be made; (2) because of the observational design of the included studies, several types of biases could affect the outcomes; (3) in the pooled analyses, the subgroups were not balanced and hence ad hoc outcomes depending on future studies should be considered; and (4) the course of treatment was not uniform in all the studies. Therefore, a large, multicenter, randomized controlled trial is needed to verify further the safety and efficacy of BEV in the treatment of NSCLC patients with BM.
5 Conclusion
Our meta-analysis has shown that in NSCLC patients with BM, the ORR and DCR were significantly better with BEV-treatment than with contemporary therapies. The DCR and PFS of the BEV-treated patients were better for intracranial than for extracranial disease. Based on data from two studies, it was found that BEV reduced the risk of new BM incidence by 70%, which shows that it may have preventive potentials for BM. The risk of intracranial hemorrhage with BEV treatment was low.
Abbreviations
- AEs
adverse events
- BEV
bevacizumab
- BM
brain metastasis
- CNS
central nervous system
- CNKI
China National Knowledge Infrastructure
- DCR
disease control rate
- HR
hazard ratio
- NSCLC
non-small cell lung cancer
- OR
odds ratio
- ORR
objective response rate
- OS
overall survival
- PFS
progression-free survival
- TKI
tyrosine kinase inhibitor
- VEGF
vascular endothelial growth factor
Acknowledgments
The study was supported by the Scientific Research Program of Hebei Provincial Health Department (20150368).
Conflict of interest: All authors declare that they have no competing interests.
References
[1] Ettinger DS, Akerley W, Borghaei H, Chang AC, Cheney RT, Chirieac LR, et al. Non-small cell lung cancer, version 2.2013. J Natl Compr Canc Netw. 2013;11(6):645–53.10.6004/jnccn.2013.0084Search in Google Scholar
[2] Kitagawa C, Mori M, Ichiki M, Sukoh N, Kada A, Saito AM, et al. Gefitinib plus bevacizumab vs. gefitinib alone for EGFR mutant non-squamous non-small cell lung cancer. In Vivo. 2019;33(2):477–82.10.21873/invivo.11498Search in Google Scholar
[3] Molina JR, Yang P, Cassivi SD, Schild SE, Adjei AA. Non-small cell lung cancer: epidemiology, risk factors, treatment, and survivorship. Mayo Clin Proc. 2008;83(5):584–94.10.1016/S0025-6196(11)60735-0Search in Google Scholar
[4] Paesmans M, Sculier JP, Libert P, Bureau G, Dabouis G, Thiriaux J, et al. Prognostic factors for survival in advanced non-small-cell lung cancer: univariate and multivariate analyses including recursive partitioning and amalgamation algorithms in 1,052 patients. The European Lung Cancer Working Party. J Clin Oncol. 1995;13(5):1221–30.10.1200/JCO.1995.13.5.1221Search in Google Scholar PubMed
[5] Kwas H, Guermazi E, Khattab A, Hrizi C, Zendah I, Ghedira H. Prognostic factors of advanced stage non-small-cell lung cancer. Rev Pneumol Clin. 2017;73(4):180–7.10.1016/j.pneumo.2017.05.002Search in Google Scholar PubMed
[6] Waqar SN, Samson PP, Robinson CG, Bradley J, Devarakonda S, Du L, et al. Non-small-cell lung cancer with brain metastasis at presentation. Clin lung cancer. 2018;19(4):e373–9. 10.1016/j.cllc.2018.01.007Search in Google Scholar PubMed PubMed Central
[7] Carolan H, Sun AY, Bezjak A, Yi QL, Payne D, Kane G, et al. Does the incidence and outcome of brain metastases in locally advanced non-small cell lung cancer justify prophylactic cranial irradiation or early detection? Lung Cancer. 2005;49(1):109–15.10.1016/j.lungcan.2004.12.004Search in Google Scholar PubMed
[8] Arrieta O, Villarreal-Garza C, Zamora J, Blake-Cerda M, de la Mata MD, Zavala DG, et al. Long-term survival in patients with non-small cell lung cancer and synchronous brain metastasis treated with whole-brain radiotherapy and thoracic chemoradiation. Radiat Oncol. 2011;6:166. 10.1186/1748-717X-6-166Search in Google Scholar PubMed PubMed Central
[9] Won YK, Lee JY, Kang YN, Jang JS, Kang JH, Jung SL. Stereotactic radiosurgery for brain metastasis in non-small cell lung cancer. Radiat Oncol J. 2015;33(3):207–16.10.3857/roj.2015.33.3.207Search in Google Scholar PubMed PubMed Central
[10] Ohe Y, Imamura F, Nogami N, Okamoto I, Kurata T, Kato T, et al. Osimertinib versus standard-of-care EGFR-TKI as first-line treatment for EGFRm advanced NSCLC: FLAURA Japanese subset. Jpn J Clin Oncol. 2019;49(1):29–36.10.1093/jjco/hyy179Search in Google Scholar PubMed PubMed Central
[11] Ulahannan D, Khalifa J, Faivre-Finn C, Lee SM. Emerging treatment paradigms for brain metastasis in non-small-cell lung cancer: an overview of the current landscape and challenges ahead. Ann Oncol. 2017;28:2923–31.10.1093/annonc/mdx481Search in Google Scholar PubMed
[12] Amit L, Ben-Aharon I, Vidal L, Leibovici L, Stemmer S. The impact of Bevacizumab (Avastin) on survival in metastatic solid tumors-a meta-analysis and systematic review. PLoS One. 2013;8(1):e51780. 10.1371/journal.pone.0051780.Search in Google Scholar PubMed PubMed Central
[13] Yang L, Chen CJ, Guo XL, Wu X, Lv B, Wang H, et al. Bevacizumab and risk of intracranial hemorrhage in patients with brain metastases: a meta-analysis. J Neurooncol. 2018;137(1):49–56.10.1007/s11060-017-2693-4Search in Google Scholar PubMed PubMed Central
[14] Lima AB, Macedo LT, Sasse AD. Addition of bevacizumab to chemotherapy in advanced non-small cell lung cancer: a systematic review and meta-analysis. PLoS One. 2011;6(8):e22681. 10.1371/journal.pone.0022681.Search in Google Scholar PubMed PubMed Central
[15] Soria JC, Mauguen A, Reck M, Sandler AB, Saijo N, Johnson DH, et al. Systematic review and meta-analysis of randomised, phase II/III trials adding bevacizumab to platinum-based chemotherapy as first-line treatment in patients with advanced non-small-cell lung cancer. Ann Oncol. 2013;24(1):20–30.10.1093/annonc/mds590Search in Google Scholar PubMed
[16] Ascha MS, Wang JF, Kumthekar P, Sloan AE, Kruchko C, Barnholtz-Sloan JS. Bevacizumab for the treatment of non-small cell lung cancer patients with synchronous brain metastases. Sci Rep. 2019;9(1):17792. 10.1038/s41598-019-54513-3.Search in Google Scholar PubMed PubMed Central
[17] Bennouna J, Falchero L, Schott R, Bonnetain F, Coudert M, Ben Hadj Yahia B, et al. Bevacizumab in combination with platinum-based chemotherapy in patients with advanced non-squamous non-small cell lung cancer with or without brain metastases: a French Cohort Study (EOLE). Oncology. 2018;94(1):55–64.10.1159/000480702Search in Google Scholar PubMed
[18] Besse B, Le Moulec S, Mazières J, Senellart H, Barlesi F, Chouaid C, et al. Bevacizumab in patients with nonsquamous non-small cell lung cancer and asymptomatic, untreated brain metastases (BRAIN): a nonrandomized, phase II Study. Clin Cancer Res. 2015;21(8):1896–903.10.1158/1078-0432.CCR-14-2082Search in Google Scholar PubMed
[19] De Braganca KC, Janjigian YY, Azzoli CG, Kris MG, Pietanza MC, Nolan CP, et al. Efficacy and safety of bevacizumab in active brain metastases from non-small cell lung cancer. J Neurooncol. 2010;100(3):443–7.10.1007/s11060-010-0200-2Search in Google Scholar PubMed PubMed Central
[20] Fu Y, Hu J, Du N, Jiao S, Li F, Li X, et al. Bevacizumab plus chemotherapy versus chemotherapy alone for preventing brain metastasis derived from advanced lung cancer. J Chemother. 2016;28(3):218–24.10.1179/1973947815Y.0000000045Search in Google Scholar PubMed
[21] Ilhan-Mutlu A, Osswald M, Liao Y, Gömmel M, Reck M, Miles D, et al. Bevacizumab prevents brain metastases formation in lung adenocarcinoma. Mol Cancer Ther. 2016;15(4):702–10.10.1158/1535-7163.MCT-15-0582Search in Google Scholar PubMed
[22] Kuse N, Yoshimori K, Ueyama M, Hirukawa I, Nakagawa Y, Aoki M, et al. Safety of bevacizumab-containing chemotherapy in non-small-cell lung cancer patients with brain metastases. Ann Cancer Res Ther. 2012;20:47–51.10.4993/acrt.20.47Search in Google Scholar
[23] Lunacsek OE, Ravelo A, Coutinho AD, Hazard SJ, Green MR, Willey J, et al. First-line treatment with bevacizumab and platinum doublet combination in non-squamous non-small cell lung cancer: a retrospective cohort study in the US oncology community practices. Drugs Real World Outcomes. 2016;3(3):333–43.10.1007/s40801-016-0090-5Search in Google Scholar PubMed PubMed Central
[24] Pan M, Li Y, Qiu S, Guo Y, Chen L, Shao X, et al. Efficacy and safety of stereotactic radiotherapy combined with bevacizumab for brain metastases of lung adenocarcinoma. Chin J Radiation Oncol. 2017;26:880–3.Search in Google Scholar
[25] Socinski MA, Langer CJ, Huang JE, Kolb MM, Compton P, Wang L, et al. Safety of bevacizumab in patients with non-small-cell lung cancer and brain metastases. J Clin Oncol. 2009;27(31):5255–61.10.1200/JCO.2009.22.0616Search in Google Scholar PubMed
[26] Stefanou D, Stamatopoulou S, Sakellaropoulou A, Akakios G, Gkiaouraki M, Gkeka D, et al. Bevacizumab, pemetrexed and carboplatin in first-line treatment of non-small cell lung cancer patients: focus on patients with brain metastases. Oncol Lett. 2016;12(6):4635–42.10.3892/ol.2016.5268Search in Google Scholar PubMed PubMed Central
[27] Tang N, Guo J, Zhang Q, Wang Y, Wang Z. Greater efficacy of chemotherapy plus bevacizumab compared to chemo- and targeted therapy alone on non-small cell lung cancer patients with brain metastasis. Oncotarget. 2016;7:3635–44.10.18632/oncotarget.6184Search in Google Scholar PubMed PubMed Central
[28] Tian Y, Zhai X, Tian H, Jing W, Zhu H, Yu J. Bevacizumab in combination with pemetrexed and platinum significantly improved the clinical outcome of patients with advanced adenocarcinoma NSCLC and brain metastases. Cancer Manage Res. 2019;11:10083–92.10.2147/CMAR.S222910Search in Google Scholar PubMed PubMed Central
[29] Wang Z, Yang JJ, Tu HY, Yan HH, Wu YL. Retrospective study on bevacizumab in the treatment of non-small cell lung cancer with brain metastases. Int J Clin Oncol. 2020;25:267–73. 10.1007/s10147-019-01552-5.Search in Google Scholar PubMed
[30] Yang RF, Yu B, Zhang RQ, Wang XH, Li C, Wang P, et al. Bevacizumab and gefitinib enhanced whole-brain radiation therapy for brain metastases due to non-small-cell lung cancer. Braz J Med Biol Res. 2017;51(1):e6073. 10.1590/1414-431X20176073.Search in Google Scholar PubMed PubMed Central
[31] Zhan Q, Miao F, Huang R, Zhou X, Ge M, Liang X. Efficacy and safety of bevacizumab combined with chemotherapy in symptomatic brain metastases from lung adenocarcinoma: a retrospective analysis. J Thoracic Dis. 2019;11(11):4725–34.10.21037/jtd.2019.10.49Search in Google Scholar PubMed PubMed Central
[32] Zustovich F, Ferro A, Lombardi G, Farina P, Zagonel V. Bevacizumab-based therapy for patients with brain metastases from non-small-cell lung cancer: preliminary results. Chemotherapy. 2014;60:294–99.10.1159/000376605Search in Google Scholar PubMed
[33] Hendriks LEL, Henon C, Auclin E, Mezquita L, Ferrara R, Audigier-Valette C, et al. Outcome of patients with non-small cell lung cancer and brain metastases treated with checkpoint inhibitors. J Thorac Oncol. 2019;14(7):1244–54.10.1016/j.jtho.2019.02.009Search in Google Scholar PubMed
[34] Willett CG, Boucher Y, di Tomaso E, Duda DG, Munn LL, Tong RT, et al. Direct evidence that the VEGF-specific antibody bevacizumab has antivascular effects in human rectal cancer. Nat Med. 2004;10(2):145–7.10.1038/nm988Search in Google Scholar PubMed PubMed Central
[35] Jain RK. Normalization of tumor vasculature: an emerging concept in antiangiogenic therapy. Science. 2005;307:58–62.10.1126/science.1104819Search in Google Scholar PubMed
[36] Ferrara N, Gerber HP, LeCouter J. The biology of VEGF and its receptors. Nature Med. 2003;9:669–76.10.1038/nm0603-669Search in Google Scholar PubMed
[37] Borgstrom P, Gold DP, Hillan KJ, Ferrara N. Importance of VEGF for breast cancer angiogenesis in vivo implications from intravital microscopy of combination treatments with an anti-VEGF neutralizing monoclonal antibody and doxorubicin. Anticancer Res. 1999;19:4203–14.Search in Google Scholar
[38] Wang Y, Dong L, Bi Q, Ge X, Zhang X, Wu D, et al. Beyond antiangiogenesis: intratumorally injected bevacizumab plays a cisplatin-sensitizing role in squamous cell carcinomas in mice. Chemotherapy. 2011;57(3):244–52.10.1159/000326485Search in Google Scholar PubMed
[39] Yano H, Nakayama N, Morimitsu K, Futamura M, Ohe N, Miwa K, et al. Changes in protein level in the cerebrospinal fluid of a patient with cerebral radiation necrosis treated with bevacizumab. Clin Med Insights Oncol. 2014;8:153–7.10.4137/CMO.S19823Search in Google Scholar PubMed PubMed Central
[40] Gressett SM, Shah SR. Intricacies of bevacizumab-induced toxicities and their management. Ann Pharmacother. 2009;43:490–501.10.1345/aph.1L426Search in Google Scholar PubMed
[41] Shamloo BK, Chhabra P, Freedman AN, Potosky A, Malin J, Weiss Smith S. Novel adverse events of bevacizumab in the US FDA adverse event reporting system database: a disproportionality analysis. Drug Saf. 2012;35(6):507–18.10.2165/11597600-000000000-00000Search in Google Scholar PubMed
[42] Dansin E, Cinieri S, Garrido P, Griesinger F, Isla D, Koehler M, et al. MO19390 (SAiL): bleeding events in a phase IV study of first-line bevacizumab with chemotherapy in patients with advanced non-squamous NSCLC. Lung Cancer. 2012;76(3):373–9.10.1016/j.lungcan.2011.11.020Search in Google Scholar PubMed
© 2020 Ping Liang et al., published by De Gruyter
This work is licensed under the Creative Commons Attribution 4.0 International License.
Articles in the same Issue
- Research Article
- MicroRNA-451b participates in coronary heart disease by targeting VEGFA
- Case Report
- A combination therapy for Kawasaki disease with severe complications: a case report
- Vitamin E for prevention of biofilm-caused Healthcare-associated infections
- Research Article
- Differential diagnosis: retroperitoneal fibrosis and oncological diseases
- Optimization of the Convolutional Neural Networks for Automatic Detection of Skin Cancer
- NEAT1 promotes LPS-induced inflammatory injury in macrophages by regulating miR-17-5p/TLR4
- Plasma matrix metalloproteinase-9 and tissue inhibitor of matrix metalloproteinase-1 as prognostic biomarkers in critically ill patients
- Effects of extracorporeal magnetic stimulation in fecal incontinence
- Case Report
- Mixed germ cell tumor of the endometrium: a case report and literature review
- Bowel perforation after ventriculoperitoneal-shunt placement: case report and review of the literature
- Research Article
- Prognostic value of lncRNA HOTAIR in colorectal cancer : a meta-analysis
- Case Report
- Treatment of insulinomas by laparoscopic radiofrequency ablation: case reports and literature review
- Research Article
- The characteristics and nomogram for primary lung papillary adenocarcinoma
- Undiagnosed pheochromocytoma presenting as a pancreatic tumor: A case report
- Bioinformatics Analysis of the Expression of ATP binding cassette subfamily C member 3 (ABCC3) in Human Glioma
- Diagnostic value of recombinant heparin-binding hemagglutinin adhesin protein in spinal tuberculosis
- Primary cutaneous DLBCL non-GCB type: challenges of a rare case
- LINC00152 knock-down suppresses esophageal cancer by EGFR signaling pathway
- Case Report
- Life-threatening anaemia in patient with hereditary haemorrhagic telangiectasia (Rendu-Osler-Weber syndrome)
- Research Article
- QTc interval predicts disturbed circadian blood pressure variation
- Shoulder ultrasound in the diagnosis of the suprascapular neuropathy in athletes
- The number of negative lymph nodes is positively associated with survival in esophageal squamous cell carcinoma patients in China
- Differentiation of pontine infarction by size
- RAF1 expression is correlated with HAF, a parameter of liver computed tomographic perfusion, and may predict the early therapeutic response to sorafenib in advanced hepatocellular carcinoma patients
- LncRNA ZEB1-AS1 regulates colorectal cancer cells by miR-205/YAP1 axis
- Tissue coagulation in laser hemorrhoidoplasty – an experimental study
- Classification of pathological types of lung cancer from CT images by deep residual neural networks with transfer learning strategy
- Enhanced Recovery after Surgery for Lung Cancer Patients
- Case Report
- Streptococcus pneumoniae-associated thrombotic microangiopathy in an immunosuppressed adult
- Research Article
- The characterization of Enterococcus genus: resistance mechanisms and inflammatory bowel disease
- Case Report
- Inflammatory fibroid polyp: an unusual cause of abdominal pain in the upper gastrointestinal tract A case report
- Research Article
- microRNA-204-5p participates in atherosclerosis via targeting MMP-9
- LncRNA LINC00152 promotes laryngeal cancer progression by sponging miR-613
- Can keratin scaffolds be used for creating three-dimensional cell cultures?
- miRNA-186 improves sepsis induced renal injury via PTEN/PI3K/AKT/P53 pathway
- Case Report
- Delayed bowel perforation after routine distal loopogram prior to ileostomy closure
- Research Article
- Diagnostic accuracy of MALDI-TOF mass spectrometry for the direct identification of clinical pathogens from urine
- The R219K polymorphism of the ATP binding cassette subfamily A member 1 gene and susceptibility to ischemic stroke in Chinese population
- miR-92 regulates the proliferation, migration, invasion and apoptosis of glioma cells by targeting neogenin
- Clinicopathological features of programmed cell death-ligand 1 expression in patients with oral squamous cell carcinoma
- NF2 inhibits proliferation and cancer stemness in breast cancer
- Body composition indices and cardiovascular risk in type 2 diabetes. CV biomarkers are not related to body composition
- S100A6 promotes proliferation and migration of HepG2 cells via increased ubiquitin-dependent degradation of p53
- Review Article
- Focus on localized laryngeal amyloidosis: management of five cases
- Research Article
- NEAT1 aggravates sepsis-induced acute kidney injury by sponging miR-22-3p
- Pericentric inversion in chromosome 1 and male infertility
- Increased atherogenic index in the general hearing loss population
- Prognostic role of SIRT6 in gastrointestinal cancers: a meta-analysis
- The complexity of molecular processes in osteoarthritis of the knee joint
- Interleukin-6 gene −572 G > C polymorphism and myocardial infarction risk
- Case Report
- Severe anaphylactic reaction to cisatracurium during anesthesia with cross-reactivity to atracurium
- Research Article
- Rehabilitation training improves nerve injuries by affecting Notch1 and SYN
- Case Report
- Myocardial amyloidosis following multiple myeloma in a 38-year-old female patient: A case report
- Research Article
- Identification of the hub genes RUNX2 and FN1 in gastric cancer
- miR-101-3p sensitizes non-small cell lung cancer cells to irradiation
- Distinct functions and prognostic values of RORs in gastric cancer
- Clinical impact of post-mortem genetic testing in cardiac death and cardiomyopathy
- Efficacy of pembrolizumab for advanced/metastatic melanoma: a meta-analysis
- Review Article
- The role of osteoprotegerin in the development, progression and management of abdominal aortic aneurysms
- Research Article
- Identification of key microRNAs of plasma extracellular vesicles and their diagnostic and prognostic significance in melanoma
- miR-30a-3p participates in the development of asthma by targeting CCR3
- microRNA-491-5p protects against atherosclerosis by targeting matrix metallopeptidase-9
- Bladder-embedded ectopic intrauterine device with calculus
- Case Report
- Mycobacterial identification on homogenised biopsy facilitates the early diagnosis and treatment of laryngeal tuberculosis
- Research Article
- The will of young minors in the terminal stage of sickness: A case report
- Extended perfusion protocol for MS lesion quantification
- Identification of four genes associated with cutaneous metastatic melanoma
- Case Report
- Thalidomide-induced serious RR interval prolongation (longest interval >5.0 s) in multiple myeloma patient with rectal cancer: A case report
- Research Article
- Voluntary exercise and cardiac remodeling in a myocardial infarction model
- Electromyography as an intraoperative test to assess the quality of nerve anastomosis – experimental study on rats
- Case Report
- CT findings of severe novel coronavirus disease (COVID-19): A case report of Heilongjiang Province, China
- Commentary
- Directed differentiation into insulin-producing cells using microRNA manipulation
- Research Article
- Culture-negative infective endocarditis (CNIE): impact on postoperative mortality
- Extracorporeal shock wave therapy for the treatment of chronic pelvic pain syndrome
- Plasma microRNAs in human left ventricular reverse remodelling
- Bevacizumab for non-small cell lung cancer patients with brain metastasis: A meta-analysis
- Risk factors for cerebral vasospasm in patients with aneurysmal subarachnoid hemorrhage
- Problems and solutions of personal protective equipment doffing in COVID-19
- Evaluation of COVID-19 based on ACE2 expression in normal and cancer patients
- Review Article
- Gastroenterological complications in kidney transplant patients
- Research Article
- CXCL13 concentration in latent syphilis patients with treatment failure
- A novel age-biomarker-clinical history prognostic index for heart failure with reduced left ventricular ejection fraction
- Case Report
- Clinicopathological analysis of composite lymphoma: A two-case report and literature review
- Trastuzumab-induced thrombocytopenia after eight cycles of trastuzumab treatment
- Research Article
- Inhibition of vitamin D analog eldecalcitol on hepatoma in vitro and in vivo
- CCTs as new biomarkers for the prognosis of head and neck squamous cancer
- Effect of glucagon-like peptide-1 receptor agonists on adipokine level of nonalcoholic fatty liver disease in rats fed high-fat diet
- 72 hour Holter monitoring, 7 day Holter monitoring, and 30 day intermittent patient-activated heart rhythm recording in detecting arrhythmias in cryptogenic stroke patients free from arrhythmia in a screening 24 h Holter
- FOXK2 downregulation suppresses EMT in hepatocellular carcinoma
- Case Report
- Total parenteral nutrition-induced Wernicke’s encephalopathy after oncologic gastrointestinal surgery
- Research Article
- Clinical prediction for outcomes of patients with acute-on-chronic liver failure associated with HBV infection: A new model establishment
- Case Report
- Combination of chest CT and clinical features for diagnosis of 2019 novel coronavirus pneumonia
- Research Article
- Clinical significance and potential mechanisms of miR-223-3p and miR-204-5p in squamous cell carcinoma of head and neck: a study based on TCGA and GEO
- Review Article
- Hemoperitoneum caused by spontaneous rupture of hepatocellular carcinoma in noncirrhotic liver. A case report and systematic review
- Research Article
- Voltage-dependent anion channels mediated apoptosis in refractory epilepsy
- Prognostic factors in stage I gastric cancer: A retrospective analysis
- Circulating irisin is linked to bone mineral density in geriatric Chinese men
- Case Report
- A family study of congenital dysfibrinogenemia caused by a novel mutation in the FGA gene: A case report
- Research Article
- CBCT for estimation of the cemento-enamel junction and crestal bone of anterior teeth
- Case Report
- Successful de-escalation antibiotic therapy using cephamycins for sepsis caused by extended-spectrum beta-lactamase-producing Enterobacteriaceae bacteremia: A sequential 25-case series
- Research Article
- Influence factors of extra-articular manifestations in rheumatoid arthritis
- Assessment of knowledge of use of electronic cigarette and its harmful effects among young adults
- Predictive factors of progression to severe COVID-19
- Procedural sedation and analgesia for percutaneous trans-hepatic biliary drainage: Randomized clinical trial for comparison of two different concepts
- Acute chemoradiotherapy toxicity in cervical cancer patients
- IGF-1 regulates the growth of fibroblasts and extracellular matrix deposition in pelvic organ prolapse
- NANOG regulates the proliferation of PCSCs via the TGF-β1/SMAD pathway
- An immune-relevant signature of nine genes as a prognostic biomarker in patients with gastric carcinoma
- Computer-aided diagnosis of skin cancer based on soft computing techniques
- MiR-1225-5p acts as tumor suppressor in glioblastoma via targeting FNDC3B
- miR-300/FA2H affects gastric cancer cell proliferation and apoptosis
- Hybrid treatment of fibroadipose vascular anomaly: A case report
- Surgical treatment for common hepatic aneurysm. Original one-step technique
- Neuropsychiatric symptoms, quality of life and caregivers’ burden in dementia
- Predictor of postoperative dyspnea for Pierre Robin Sequence infants
- Long non-coding RNA FOXD2-AS1 promotes cell proliferation, metastasis and EMT in glioma by sponging miR-506-5p
- Analysis of expression and prognosis of KLK7 in ovarian cancer
- Circular RNA circ_SETD2 represses breast cancer progression via modulating the miR-155-5p/SCUBE2 axis
- Glial cell induced neural differentiation of bone marrow stromal cells
- Case Report
- Moraxella lacunata infection accompanied by acute glomerulonephritis
- Research Article
- Diagnosis of complication in lung transplantation by TBLB + ROSE + mNGS
- Case Report
- Endometrial cancer in a renal transplant recipient: A case report
- Research Article
- Downregulation of lncRNA FGF12-AS2 suppresses the tumorigenesis of NSCLC via sponging miR-188-3p
- Case Report
- Splenic abscess caused by Streptococcus anginosus bacteremia secondary to urinary tract infection: a case report and literature review
- Research Article
- Advances in the role of miRNAs in the occurrence and development of osteosarcoma
- Rheumatoid arthritis increases the risk of pleural empyema
- Effect of miRNA-200b on the proliferation and apoptosis of cervical cancer cells by targeting RhoA
- LncRNA NEAT1 promotes gastric cancer progression via miR-1294/AKT1 axis
- Key pathways in prostate cancer with SPOP mutation identified by bioinformatic analysis
- Comparison of low-molecular-weight heparins in thromboprophylaxis of major orthopaedic surgery – randomized, prospective pilot study
- Case Report
- A case of SLE with COVID-19 and multiple infections
- Research Article
- Circular RNA hsa_circ_0007121 regulates proliferation, migration, invasion, and epithelial–mesenchymal transition of trophoblast cells by miR-182-5p/PGF axis in preeclampsia
- SRPX2 boosts pancreatic cancer chemoresistance by activating PI3K/AKT axis
- Case Report
- A case report of cervical pregnancy after in vitro fertilization complicated by tuberculosis and a literature review
- Review Article
- Serrated lesions of the colon and rectum: Emergent epidemiological data and molecular pathways
- Research Article
- Biological properties and therapeutic effects of plant-derived nanovesicles
- Case Report
- Clinical characterization of chromosome 5q21.1–21.3 microduplication: A case report
- Research Article
- Serum calcium levels correlates with coronary artery disease outcomes
- Rapunzel syndrome with cholangitis and pancreatitis – A rare case report
- Review Article
- A review of current progress in triple-negative breast cancer therapy
- Case Report
- Peritoneal-cutaneous fistula successfully treated at home: A case report and literature review
- Research Article
- Trim24 prompts tumor progression via inducing EMT in renal cell carcinoma
- Degradation of connexin 50 protein causes waterclefts in human lens
- GABRD promotes progression and predicts poor prognosis in colorectal cancer
- The lncRNA UBE2R2-AS1 suppresses cervical cancer cell growth in vitro
- LncRNA FOXD3-AS1/miR-135a-5p function in nasopharyngeal carcinoma cells
- MicroRNA-182-5p relieves murine allergic rhinitis via TLR4/NF-κB pathway
Articles in the same Issue
- Research Article
- MicroRNA-451b participates in coronary heart disease by targeting VEGFA
- Case Report
- A combination therapy for Kawasaki disease with severe complications: a case report
- Vitamin E for prevention of biofilm-caused Healthcare-associated infections
- Research Article
- Differential diagnosis: retroperitoneal fibrosis and oncological diseases
- Optimization of the Convolutional Neural Networks for Automatic Detection of Skin Cancer
- NEAT1 promotes LPS-induced inflammatory injury in macrophages by regulating miR-17-5p/TLR4
- Plasma matrix metalloproteinase-9 and tissue inhibitor of matrix metalloproteinase-1 as prognostic biomarkers in critically ill patients
- Effects of extracorporeal magnetic stimulation in fecal incontinence
- Case Report
- Mixed germ cell tumor of the endometrium: a case report and literature review
- Bowel perforation after ventriculoperitoneal-shunt placement: case report and review of the literature
- Research Article
- Prognostic value of lncRNA HOTAIR in colorectal cancer : a meta-analysis
- Case Report
- Treatment of insulinomas by laparoscopic radiofrequency ablation: case reports and literature review
- Research Article
- The characteristics and nomogram for primary lung papillary adenocarcinoma
- Undiagnosed pheochromocytoma presenting as a pancreatic tumor: A case report
- Bioinformatics Analysis of the Expression of ATP binding cassette subfamily C member 3 (ABCC3) in Human Glioma
- Diagnostic value of recombinant heparin-binding hemagglutinin adhesin protein in spinal tuberculosis
- Primary cutaneous DLBCL non-GCB type: challenges of a rare case
- LINC00152 knock-down suppresses esophageal cancer by EGFR signaling pathway
- Case Report
- Life-threatening anaemia in patient with hereditary haemorrhagic telangiectasia (Rendu-Osler-Weber syndrome)
- Research Article
- QTc interval predicts disturbed circadian blood pressure variation
- Shoulder ultrasound in the diagnosis of the suprascapular neuropathy in athletes
- The number of negative lymph nodes is positively associated with survival in esophageal squamous cell carcinoma patients in China
- Differentiation of pontine infarction by size
- RAF1 expression is correlated with HAF, a parameter of liver computed tomographic perfusion, and may predict the early therapeutic response to sorafenib in advanced hepatocellular carcinoma patients
- LncRNA ZEB1-AS1 regulates colorectal cancer cells by miR-205/YAP1 axis
- Tissue coagulation in laser hemorrhoidoplasty – an experimental study
- Classification of pathological types of lung cancer from CT images by deep residual neural networks with transfer learning strategy
- Enhanced Recovery after Surgery for Lung Cancer Patients
- Case Report
- Streptococcus pneumoniae-associated thrombotic microangiopathy in an immunosuppressed adult
- Research Article
- The characterization of Enterococcus genus: resistance mechanisms and inflammatory bowel disease
- Case Report
- Inflammatory fibroid polyp: an unusual cause of abdominal pain in the upper gastrointestinal tract A case report
- Research Article
- microRNA-204-5p participates in atherosclerosis via targeting MMP-9
- LncRNA LINC00152 promotes laryngeal cancer progression by sponging miR-613
- Can keratin scaffolds be used for creating three-dimensional cell cultures?
- miRNA-186 improves sepsis induced renal injury via PTEN/PI3K/AKT/P53 pathway
- Case Report
- Delayed bowel perforation after routine distal loopogram prior to ileostomy closure
- Research Article
- Diagnostic accuracy of MALDI-TOF mass spectrometry for the direct identification of clinical pathogens from urine
- The R219K polymorphism of the ATP binding cassette subfamily A member 1 gene and susceptibility to ischemic stroke in Chinese population
- miR-92 regulates the proliferation, migration, invasion and apoptosis of glioma cells by targeting neogenin
- Clinicopathological features of programmed cell death-ligand 1 expression in patients with oral squamous cell carcinoma
- NF2 inhibits proliferation and cancer stemness in breast cancer
- Body composition indices and cardiovascular risk in type 2 diabetes. CV biomarkers are not related to body composition
- S100A6 promotes proliferation and migration of HepG2 cells via increased ubiquitin-dependent degradation of p53
- Review Article
- Focus on localized laryngeal amyloidosis: management of five cases
- Research Article
- NEAT1 aggravates sepsis-induced acute kidney injury by sponging miR-22-3p
- Pericentric inversion in chromosome 1 and male infertility
- Increased atherogenic index in the general hearing loss population
- Prognostic role of SIRT6 in gastrointestinal cancers: a meta-analysis
- The complexity of molecular processes in osteoarthritis of the knee joint
- Interleukin-6 gene −572 G > C polymorphism and myocardial infarction risk
- Case Report
- Severe anaphylactic reaction to cisatracurium during anesthesia with cross-reactivity to atracurium
- Research Article
- Rehabilitation training improves nerve injuries by affecting Notch1 and SYN
- Case Report
- Myocardial amyloidosis following multiple myeloma in a 38-year-old female patient: A case report
- Research Article
- Identification of the hub genes RUNX2 and FN1 in gastric cancer
- miR-101-3p sensitizes non-small cell lung cancer cells to irradiation
- Distinct functions and prognostic values of RORs in gastric cancer
- Clinical impact of post-mortem genetic testing in cardiac death and cardiomyopathy
- Efficacy of pembrolizumab for advanced/metastatic melanoma: a meta-analysis
- Review Article
- The role of osteoprotegerin in the development, progression and management of abdominal aortic aneurysms
- Research Article
- Identification of key microRNAs of plasma extracellular vesicles and their diagnostic and prognostic significance in melanoma
- miR-30a-3p participates in the development of asthma by targeting CCR3
- microRNA-491-5p protects against atherosclerosis by targeting matrix metallopeptidase-9
- Bladder-embedded ectopic intrauterine device with calculus
- Case Report
- Mycobacterial identification on homogenised biopsy facilitates the early diagnosis and treatment of laryngeal tuberculosis
- Research Article
- The will of young minors in the terminal stage of sickness: A case report
- Extended perfusion protocol for MS lesion quantification
- Identification of four genes associated with cutaneous metastatic melanoma
- Case Report
- Thalidomide-induced serious RR interval prolongation (longest interval >5.0 s) in multiple myeloma patient with rectal cancer: A case report
- Research Article
- Voluntary exercise and cardiac remodeling in a myocardial infarction model
- Electromyography as an intraoperative test to assess the quality of nerve anastomosis – experimental study on rats
- Case Report
- CT findings of severe novel coronavirus disease (COVID-19): A case report of Heilongjiang Province, China
- Commentary
- Directed differentiation into insulin-producing cells using microRNA manipulation
- Research Article
- Culture-negative infective endocarditis (CNIE): impact on postoperative mortality
- Extracorporeal shock wave therapy for the treatment of chronic pelvic pain syndrome
- Plasma microRNAs in human left ventricular reverse remodelling
- Bevacizumab for non-small cell lung cancer patients with brain metastasis: A meta-analysis
- Risk factors for cerebral vasospasm in patients with aneurysmal subarachnoid hemorrhage
- Problems and solutions of personal protective equipment doffing in COVID-19
- Evaluation of COVID-19 based on ACE2 expression in normal and cancer patients
- Review Article
- Gastroenterological complications in kidney transplant patients
- Research Article
- CXCL13 concentration in latent syphilis patients with treatment failure
- A novel age-biomarker-clinical history prognostic index for heart failure with reduced left ventricular ejection fraction
- Case Report
- Clinicopathological analysis of composite lymphoma: A two-case report and literature review
- Trastuzumab-induced thrombocytopenia after eight cycles of trastuzumab treatment
- Research Article
- Inhibition of vitamin D analog eldecalcitol on hepatoma in vitro and in vivo
- CCTs as new biomarkers for the prognosis of head and neck squamous cancer
- Effect of glucagon-like peptide-1 receptor agonists on adipokine level of nonalcoholic fatty liver disease in rats fed high-fat diet
- 72 hour Holter monitoring, 7 day Holter monitoring, and 30 day intermittent patient-activated heart rhythm recording in detecting arrhythmias in cryptogenic stroke patients free from arrhythmia in a screening 24 h Holter
- FOXK2 downregulation suppresses EMT in hepatocellular carcinoma
- Case Report
- Total parenteral nutrition-induced Wernicke’s encephalopathy after oncologic gastrointestinal surgery
- Research Article
- Clinical prediction for outcomes of patients with acute-on-chronic liver failure associated with HBV infection: A new model establishment
- Case Report
- Combination of chest CT and clinical features for diagnosis of 2019 novel coronavirus pneumonia
- Research Article
- Clinical significance and potential mechanisms of miR-223-3p and miR-204-5p in squamous cell carcinoma of head and neck: a study based on TCGA and GEO
- Review Article
- Hemoperitoneum caused by spontaneous rupture of hepatocellular carcinoma in noncirrhotic liver. A case report and systematic review
- Research Article
- Voltage-dependent anion channels mediated apoptosis in refractory epilepsy
- Prognostic factors in stage I gastric cancer: A retrospective analysis
- Circulating irisin is linked to bone mineral density in geriatric Chinese men
- Case Report
- A family study of congenital dysfibrinogenemia caused by a novel mutation in the FGA gene: A case report
- Research Article
- CBCT for estimation of the cemento-enamel junction and crestal bone of anterior teeth
- Case Report
- Successful de-escalation antibiotic therapy using cephamycins for sepsis caused by extended-spectrum beta-lactamase-producing Enterobacteriaceae bacteremia: A sequential 25-case series
- Research Article
- Influence factors of extra-articular manifestations in rheumatoid arthritis
- Assessment of knowledge of use of electronic cigarette and its harmful effects among young adults
- Predictive factors of progression to severe COVID-19
- Procedural sedation and analgesia for percutaneous trans-hepatic biliary drainage: Randomized clinical trial for comparison of two different concepts
- Acute chemoradiotherapy toxicity in cervical cancer patients
- IGF-1 regulates the growth of fibroblasts and extracellular matrix deposition in pelvic organ prolapse
- NANOG regulates the proliferation of PCSCs via the TGF-β1/SMAD pathway
- An immune-relevant signature of nine genes as a prognostic biomarker in patients with gastric carcinoma
- Computer-aided diagnosis of skin cancer based on soft computing techniques
- MiR-1225-5p acts as tumor suppressor in glioblastoma via targeting FNDC3B
- miR-300/FA2H affects gastric cancer cell proliferation and apoptosis
- Hybrid treatment of fibroadipose vascular anomaly: A case report
- Surgical treatment for common hepatic aneurysm. Original one-step technique
- Neuropsychiatric symptoms, quality of life and caregivers’ burden in dementia
- Predictor of postoperative dyspnea for Pierre Robin Sequence infants
- Long non-coding RNA FOXD2-AS1 promotes cell proliferation, metastasis and EMT in glioma by sponging miR-506-5p
- Analysis of expression and prognosis of KLK7 in ovarian cancer
- Circular RNA circ_SETD2 represses breast cancer progression via modulating the miR-155-5p/SCUBE2 axis
- Glial cell induced neural differentiation of bone marrow stromal cells
- Case Report
- Moraxella lacunata infection accompanied by acute glomerulonephritis
- Research Article
- Diagnosis of complication in lung transplantation by TBLB + ROSE + mNGS
- Case Report
- Endometrial cancer in a renal transplant recipient: A case report
- Research Article
- Downregulation of lncRNA FGF12-AS2 suppresses the tumorigenesis of NSCLC via sponging miR-188-3p
- Case Report
- Splenic abscess caused by Streptococcus anginosus bacteremia secondary to urinary tract infection: a case report and literature review
- Research Article
- Advances in the role of miRNAs in the occurrence and development of osteosarcoma
- Rheumatoid arthritis increases the risk of pleural empyema
- Effect of miRNA-200b on the proliferation and apoptosis of cervical cancer cells by targeting RhoA
- LncRNA NEAT1 promotes gastric cancer progression via miR-1294/AKT1 axis
- Key pathways in prostate cancer with SPOP mutation identified by bioinformatic analysis
- Comparison of low-molecular-weight heparins in thromboprophylaxis of major orthopaedic surgery – randomized, prospective pilot study
- Case Report
- A case of SLE with COVID-19 and multiple infections
- Research Article
- Circular RNA hsa_circ_0007121 regulates proliferation, migration, invasion, and epithelial–mesenchymal transition of trophoblast cells by miR-182-5p/PGF axis in preeclampsia
- SRPX2 boosts pancreatic cancer chemoresistance by activating PI3K/AKT axis
- Case Report
- A case report of cervical pregnancy after in vitro fertilization complicated by tuberculosis and a literature review
- Review Article
- Serrated lesions of the colon and rectum: Emergent epidemiological data and molecular pathways
- Research Article
- Biological properties and therapeutic effects of plant-derived nanovesicles
- Case Report
- Clinical characterization of chromosome 5q21.1–21.3 microduplication: A case report
- Research Article
- Serum calcium levels correlates with coronary artery disease outcomes
- Rapunzel syndrome with cholangitis and pancreatitis – A rare case report
- Review Article
- A review of current progress in triple-negative breast cancer therapy
- Case Report
- Peritoneal-cutaneous fistula successfully treated at home: A case report and literature review
- Research Article
- Trim24 prompts tumor progression via inducing EMT in renal cell carcinoma
- Degradation of connexin 50 protein causes waterclefts in human lens
- GABRD promotes progression and predicts poor prognosis in colorectal cancer
- The lncRNA UBE2R2-AS1 suppresses cervical cancer cell growth in vitro
- LncRNA FOXD3-AS1/miR-135a-5p function in nasopharyngeal carcinoma cells
- MicroRNA-182-5p relieves murine allergic rhinitis via TLR4/NF-κB pathway

