Abstract
Objectives
The objective was to determine whether specific physical activity (PA) or psychological stress factors are associated with different definitions of flare-ups (pain-defined flares [PDFs]: periods of increased pain lasting at least 2 h, when pain intensity is distinctly worse than it has been recently; and non-pain-defined flares [NPDFs]: obviously uncomfortable feelings, such as fatigue, loss of function, or emotional/psychosocial fluctuations, without major fluctuations in pain intensity based on 11-point scales) among people with lumbar radicular pain.
Methods
This was a case-crossover study. Participants with acute or subacute lumbar radicular pain completed serial face-to-face or online assessments for 6 weeks at 3-day intervals to determine whether they experienced sciatica flare-ups (PDF/NPDF) after specific types of PA or psychological stresses.
Results
A total of 152 participants were enroled. There were 597 PDF and 323 NPDF case periods and 800 control periods. The odds of PDFs were increased by prolonged walking and standing, and the odds of NPDFs were increased by prolonged sitting, mental distress, and depressed mood. According to the multivariable analyses, prolonged sitting (OR: 3.0, 95% CI: 1.7–5.5), prolonged walking (OR: 6.2, 95% CI: 3.9–9.9), and prolonged standing (OR: 5.6, 95% CI: 3.3–9.5) were significantly associated with the odds of PDFs, and prolonged sitting (OR: 3.4, 95% CI: 1.8–6.2), mental distress (OR: 6.7, 95% CI: 2.5–17.5), and depressed mood (OR: 5.8, 95% CI: 2.6–12.8) associated with the odds of NPDFs.
Conclusions
Prolonged sitting, walking, and standing triggered the occurrence of PDF. Prolonged sitting, mental distress, and depressed mood triggered the occurrence of NPDF.
1 Introduction
Low back pain (LBP) with or without radicular pain (also known as sciatica) is a fairly common health problem and a common cause of work disability [1–6]. Lumbar radicular pain is usually caused by compression or irritation of one of the lumbosacral nerve roots and is a common symptom of lumbar disc herniation. LBP has historically been classified as acute, subacute, or chronic. However, contemporary research highlights that LBP is often present as persistent and fluctuating, or episodic, and it rarely resolves completely without recurrence [7]. As a result, research has examined the trajectories of LBP, including fluctuations such as “flare-ups,” episodes, and recurrences [8–10]. LBP flare-ups have been defined as “periods of increased pain lasting at least 2 h, when the pain intensity is distinctly worse than it has been recently” [11,12]. There are different definitions of flare-ups, including “a worsening condition lasting from hours to weeks that is difficult to tolerate and generally impacts usual activities and/or emotions” [12,13]. Flare-ups are therefore characterized not only by an increase in pain but also by other factors, such as fatigue, loss of function, and psychosocial changes.
A variety of environmental and individual characteristics have been reported to increase the risk of LBP. A better understanding of the risk factors for flare-ups of LBP may provide important insights into the prevention and management of this condition. Numerous previous studies of risk factors associated with LBP and sciatica have been published. Suri et al. reported that prolonged sitting (>6 h) was a trigger for LBP flare-ups in adults with acute LBP. In contrast, activities involving physical exertion were not associated with an increased transient risk of flare-ups [14]. In older men with LBP and sciatica, even if LBP is associated with anatomical abnormalities, such as osteoporotic fractures, metastases, spinal stenosis, degenerative spondylolisthesis, and scoliosis, nonanatomical factors, such as age, social factors, obesity, and lifestyle factors, also seem to influence the subjective experience of pain [15–17]. Costa et al. reported that participants considered biomedical factors to be the main triggers of their LBP flare-ups, but some also cited nonbiomedical triggers. The most frequently reported reasons for experiencing flare-ups were active movements and static postures [9]. A recent study identified different risk factors for LBP flare-ups using different definitions, such as pain-defined flares (PDFs) or self-reported flares (SRFs) [12]. Poor sleep quality, fatigue, leisure time physical activity (PA), and fear of PA increased the risk for PDFs. Risk factors differed when the SRF definition was used.
To date, no studies have explored the risk factors for flare-ups in patients with lumbar radicular pain depending on how flare-ups is defined, such as PDFs and non-pain-defined flares (NPDFs). The aims of this study were to describe (i) the risk factors associated with flare-ups in people with lumbar radicular pain and (ii) the differences between risk factors for flare-ups using two different definitions: PDFs or NPDFs.
2 Methods
2.1 Study design
We used a case-crossover design to explore the risk factors for flare-ups in patients with lumbar radicular pain depending on the definition used (PDFs or NPDFs). Case-crossover studies involve each person functioning as their own control, eliminating between-person confounding by measured and unmeasured characteristics that remain constant over time [18]. This study design examines the transient effects of a brief exposure on the onset of an acute outcome. By design, each sciatica participant served as his or her own control, and so factors that were less likely to change within a short duration, such as age, sex, weight, socioeconomic status, lifestyle habits, and comorbidities, were automatically controlled for.
Two definitions of flare-ups (PDF and NPDF) were used. PDFs were defined as “periods of increased pain lasting at least 2 h, when the pain intensity is distinctly worse than it has been recently.” NPDFs were defined as obviously uncomfortable feelings, such as fatigue, loss of function, or emotional/psychosocial fluctuations, without major fluctuation in pain intensity based on 11-point scales (Table S1, Supplementary Material). The first question (Select the number that best describes the PAIN you felt due to your lumbar radicular pain) is to respond to the PDF, and questions 2 (Select the number that best describes the DIFFICULTY you had in doing physical activities, such as walking, dressing, or preparing meals, etc., due to your lumbar radicular pain), 3 (Select the number that best describes the FATIGUE you felt due to your lumbar radicular pain), or 4 (Select the number that best describes the DEPRESSED MOOD you had due to your lumbar radicular pain) determine the NPDF. A >2-point increase over the usual intensity on an 11-point scale for radicular pain, difficulty, fatigue, or depressed mood was classified as a large fluctuation. The case period was defined as the 24 h prior to a PDF/NPDF. Similarly, the control period was defined as the 24 h that preceded a day with no flare-ups.
2.2 Participants
This descriptive study aimed to investigate the risk factors for flare-ups (PDF/NPDF). The incidence of PDF is approximately 2/3, while the incidence of NPDF is around 1/3 based on our clinical experience. The sample size estimation was based on the precision (width) of the 95% confidence intervals (CIs) of the proportions of expected events, and calculated using power analysis via SPSS software. The inclusion criteria were (i) patients with lumbar radicular pain, defined as pain radiating into the leg below the gluteal fold, also known as LBP with radicular pain, and lumbar MRI-confirmed disc herniation resulting in nerve root compression who developed sciatica; (ii) patients aged 18 years and older; and (iii) patients with a new episode of LBP with a radicular pain of duration ≤3 months, preceded by at least 1 month without LBP. The exclusion criteria were as follows: (i) clinical suspicion due to “red flag” conditions, including infection, fracture, or neoplasm; (ii) LBP without radicular pain; and (iii) previous spinal surgery, recent low back trauma, pregnancy, or severe active medical comorbidities. Participants reported their age, sex, employment status, and LBP history at their initial LBP consultation. Pain intensity was measured using an 11-point numerical rating scale (NRS) ranging from 0 (no pain) to 10 (worst imaginable pain). Participants completed the Oswestry Disability Index (ODI), the Fear-Avoidance Beliefs Questionnaire, and the PA subscale. This study was approved by the Ethics Committee of Chongqing Medical University (Decision number: 2021750). All study protocols and procedures were conducted in accordance with the Declaration of Helsinki.
2.3 Exposure assessment
The participants completed face-to-face interviews or online surveys. The participants reported whether they had PDFs or NPDFs, and whether they had engaged in specific types of PA exposures during the past 24 h prior to a PDF/NPDF or a day with no flare-ups, including prolonged sitting (>1 h), prolonged standing (>1 h), prolonged walking (>half an hour), manual handling of objects (10 kg), driving (>1 h), frequent bending, frequent twisting, frequent lifting (≥1/2 of the day as frequent) [16], mental distress, depressed mood, and dissatisfaction with life. To avoid confusion in the risk factor analysis, we did not include both PDF and NPDF on the same day in same participant. Subsequent surveys reassessed triggers and flare-ups at 3-day intervals after the first survey, for a maximum of 15 surveys completed during the 6-week follow-up. All participants received standard medical care for acute LBP with radicular pain as per clinical practice guidelines.
2.4 Statistical analysis
Only participants with both case and control periods were included in the analysis. Participant characteristics were reported using descriptive statistics. Continuous variables were expressed as mean (standard deviations [SDs]), and categorical variables are expressed as numbers and percentages. Comparisons of categorical variables (sex, BMI, history of prior LBP history, history of prior lumbar radicular pain, and employment status) were conducted using the χ 2 test or Fisher’s exact test, as appropriate. Numerical data (age, duration of symptoms, NRS score, ODI score, and fear avoidance belief questionnaire score) were analysed using an unpaired t-test or the Mann–Whitney U-test, as appropriate. We calculated crude odds ratios (ORs) and 95% CIs for associations between triggers over the past 24 h and the risk of PDFs and NPDFs, respectively, using univariate analysis. Next, based on the univariate analysis, factors with statistical significance and approximate significance were included in the multivariate conditional logistic regression analyses.
In addition, we performed sensitivity analyses by treating recurrent flare events within each person as a cluster, constructing the conditional likelihood on a person/flare level, and restricting analyses to the first reported flare-up for each participant.
Data were analysed using IBM® SPSS® statistics software, version 24 (IBM SPSS Statistics for Mac, version 24.0., IBM Corp., Armonk, NY, USA). A p-value <0.05 was considered to indicate statistical significance.
3 Results
This case-crossover study included 152 participants recruited from the outpatient clinic or who were admitted to the Department of Rehabilitation Medicine, the Affiliated Hospital of Chongqing Medical University between August 2022 and May 2023 (Figure 1). The characteristics of the study sample (n = 178) are presented in Table 1. The mean (SD) age of the participants was 49(15.5) years, and 49% of the participants were male. Participants who were included in the case-crossover analysis (n = 152) had similar characteristics to those who were not included. Of the 1,831 surveys (1,108 face-to-face surveys by 152 participants, 723 online surveys by 114 participants) completed by participants in the case-crossover analysis, a total of 1,031 flare-up days were identified, and 111 flare periods were excluded for having both PDF and NPDF on the same day in same participant. This left 920 case periods, being 597 PDF and 323 NPDF case periods, and 800 control periods during the 6-week follow-up, with an average of 12 completed surveys per participant.
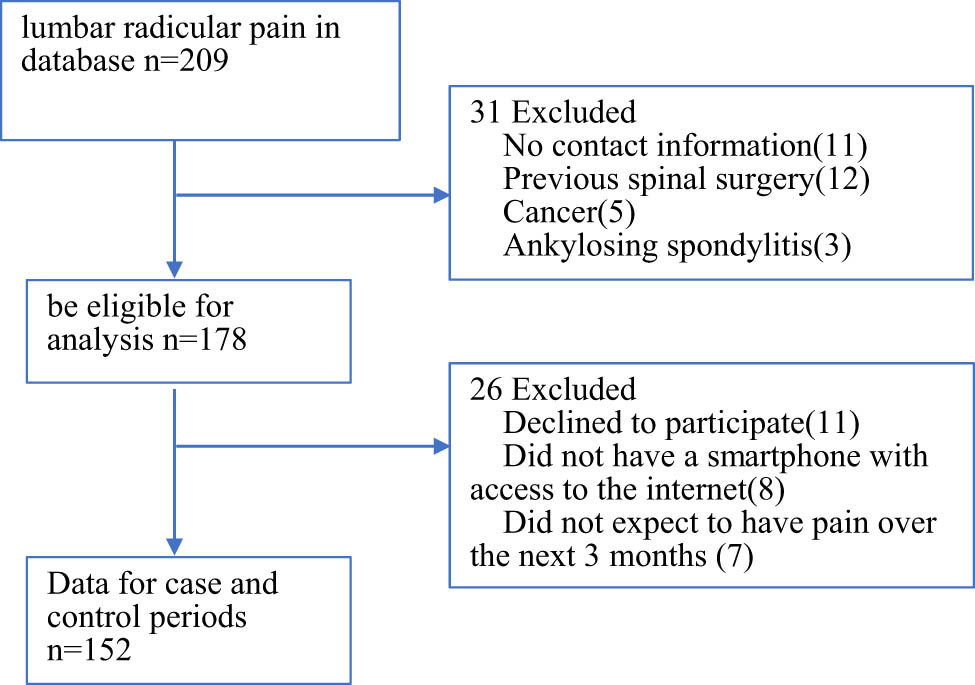
Flow diagram for the inclusion and exclusion of patients with lumbar radicular pain.
Characteristics of acute and subacute participants with lumbar radicular pain
| Eligible participants (n = 178) | Included in case-crossover analysis (n = 152) | Not included in case-crossover analysis (n = 26) | |
|---|---|---|---|
| Mean (standard deviation) or n (%) | |||
| Age, year | 48.9(15.3) | 47.5(15.9) | 49.4(14.8) |
| Sex (% male) | 87(48.9%) | 81(53.3%) | 15(57.7%) |
| <25 kg/m2 | 143(80.3%) | 125(82.2%) | 21(80.8%) |
| ≥25 kg/m2 | 35(19.7%) | 27(17.8%) | 5(19.2%) |
| Duration of symptoms, days | 16(15.0) | 14(15.3) | 15(16.6) |
| Prior low back pain history (%) | 163(91.6%) | 141(92.8%) | 25(96.1%) |
| Prior lumbar radicular pain history (%) | 63(35.4%) | 46(30.3%) | 7(26.9%) |
| Full- or part-time employment | 126(70.8%) | 95(62.5%) | 17(65.4%) |
| Retired | 24(13.5%) | 25(16.4%) | 4(15.4%) |
| Unemployed | 15(8.4%) | 24(15.8%) | 2(7.7%) |
| Disabled | 13(7.3%) | 8(5.3%) | 3(11.5%) |
| NRS (0–10) | 6.9(2.5) | 7.2(2.4) | 7.5(2.3) |
| ODI (0–100) | 59(26) | 61(23) | 65(25) |
| Fear avoidance beliefs questionnaire, PA subscale | 13.9(4.9) | 14.8(4.6) | 14.0(5.1) |
BMI: body mass index; NRS: numerical rating scale; ODI: Oswestry Disability Index; PA: physical activity.
3.1 Risk factors for PDF
The absolute number of triggers reported during flare periods was low for many of the triggers studied (Table 2). Prolonged walking (>half an hour) and prolonged standing (>1 h) in the past 24 h were activities that were significantly associated with PDFs, conferring a fourfold and threefold increased risk of flare-up compared to not walking and standing for prolonged periods (OR: 4.0, 95% CI: 2.6–6.1; OR: 3.0, 95% CI: 1.8–4.8, respectively). For most physical activities involving physical exertion (except for walking and standing), the frequency of triggers reported during flare periods was similar to that reported during control periods. Variables related to psychological stress were not associated with PDF (Table 2). According to the multivariable logistic analyses, prolonged sitting (OR: 3.0, 95% CI: 1.7–5.5), prolonged walking (OR: 6.2, 95% CI: 3.9–9.9), and prolonged standing (OR: 5.6, 95% CI: 3.3–9.5) were independently and significantly associated with PDF risk (Table 2).
Analyses of associations between potential risk of PDF during an acute and subacute lumbar radicular pain
| No. (%) of PDF periods (n = 597) | No. (%) of control periods (n = 800) | Univariate | Multivariate | |
|---|---|---|---|---|
| ORs (95% CI) | ORs (95% CI) | |||
| Physical activities | ||||
| Prolonged sitting (>1 h) | 84(14.1%) | 76(9.5%) | 1.6(0.9–2.7) | 3.0(1.7–5.5) |
| Prolonged walking (>half an hour) | 242(40.5%) | 117(14.6%) | 4.0(2.6–6.1) | 6.2(3.9–9.9) |
| Prolonged standing (>1 h) | 154(25.8%) | 84(10.5%) | 3.0(1.8–4.8) | 5.6(3.3–9.5) |
| Manual handling of objects <10 kg | 19(3.2%) | 16(2.0%) | 1.5(0.5–4.8) | |
| Manual handling of objects ≥10 kg | 14(2.3%) | 16(2.0%) | 1.1(0.3–3.7) | |
| Time driving (for >1 h) | 11(1.8%) | 14(1.8%) | 1.1(0.3–4.0) | |
| Frequent bending | 8(1.3%) | 11(1.4%) | 1.0(0.2–4.5) | |
| Frequent twisting | 16(2.7%) | 14(1.8%) | 1.6(0.5–5.4) | |
| Frequent lifting | 19(3.2%) | 22(2.8%) | 1.2(0.4–3.3) | |
| Psychological stress | ||||
| Mental distress | 21(3.5%) | 19(2.4%) | 1.6(0.6–4.3) | |
| Depressed mood | 27(4.5%) | 33(4.1%) | 1.1(0.5–2.6) | 0.9(0.3–2.3) |
| Dissatisfaction with life | 14(2.3%) | 27(3.4%) | 0.7(0.2–2.0) | |
PDF: pain-defined flare-ups.
The bold values mean potential risk with statistically significant associations with PDF.
3.2 Risk factors for NPDF
The ORs (95% CIs) of each variable for the case and control days preceding an NPDF or nonflare day are presented in Table 3. Prolonged sitting (>1 h) (OR: 2.4, 95% CI: 1.3–4.4), mental distress (OR: 5.0, 95% CI: 2.0–13.0), and depressed mood (OR: 4.2, 95% CI: 2.0–9.0) in the past 24 h were significantly associated with NPDFs, conferring a twofold, fivefold, and fourfold increased risk of NPDFs. For all physical activities involving physical exertion except for sitting, the frequency of triggers reported during flare periods was similar to that reported during control periods. Variables related to psychological stress were significantly associated with NPDFs except for dissatisfaction with life. According to multivariable logistic analyses, prolonged sitting (OR: 3.4, 95% CI: 1.8–6.2), mental distress (OR: 6.7, 95% CI: 2.5–17.5), and depressed mood (OR: 5.8, 95% CI: 2.6–12.8) were independently and significantly associated with NPDF risk (Table 3).
Analyses of associations between potential risk of NPDF during an acute and subacute lumbar radicular pain
| No. (%) of NPDF periods (n = 323) | No. (%) of control periods (n = 800) | Univariate | Multivariate | |
|---|---|---|---|---|
| ORs (95% CI) | ORs (95% CI) | |||
| Physical activities | ||||
| Prolonged sitting (>1 h) | 65(20.1%) | 76(9.5%) | 2.4(1.3–4.4) | 3.4(1.8–6.2) |
| Prolonged walking (>half an hour) | 49(15.2%) | 117(14.6%) | 1.0(0.6–1.9) | |
| Prolonged standing (>1 h) | 41(12.7%) | 84(10.5%) | 1.2(0.6–2.3) | 1.5(0.8–3.0) |
| Manual handling of objects <10 kg | 14(4.3%) | 16(2.0%) | 2.1(0.6–7.1) | |
| Manual handling of objects ≥10 kg | 16(5.0%) | 16(2.0%) | 2.6(0.8–8.1) | |
| Time driving (for >1 h) | 14(4.3%) | 14(1.8%) | 2.5(0.7–9.0) | |
| Frequent bending | 8(2.5%) | 11(1.4%) | 1.9(0.4–8.5) | |
| frequent twisting | 16(5.0%) | 14(1.8%) | 3.1(0.9–10.3) | |
| Frequent lifting | 14(4.3%) | 22(2.8%) | 1.6(0.5–4.9) | |
| Psychological stress | ||||
| Mental distress | 35(10.8%) | 19(2.4%) | 5.0(2.0–13.0) | 6.7(2.5–17.5) |
| Depressed mood | 49(15.2%) | 33(4.1%) | 4.2(2.0–9.0) | 5.8(2.6–12.8) |
| Dissatisfaction with life | 22(6.8%) | 27(3.4%) | 2.1(0.8–5.3) | |
NPDF: non-pain-defined flare-ups.
The bold values mean potential risk with statistically significant associations with NPDF.
The sensitivity analyses yielded results that were not materially different from those of the primary analyses, although the precision of the risk estimates decreased in the analyses restricted to the first flare-ups, as expected owing to the smaller number of flare events included (online Supplementary material).
4 Discussion
Our study demonstrated that there are different risk factors for flare-ups in patients with lumbar radicular pain depending on whether the flare is defined as a PDF or an NPDF. Prolonged sitting (>1 h), prolonged walking (>half an hour), and prolonged standing (>1 h) triggered PDFs. However, prolonged sitting (>1 h), mental distress, and depressed mood triggered NPDFs. Therefore, prolonged sitting triggered both PDFs and NPDFs.
Parreira et al. previously performed an overview of risk factors evaluated for their association with LBP and sciatica [19]. Their results showed that exposure to a range of factors pertaining to the individual, poor general health, physical or psychological stress significantly increased the risk of LBP and sciatica. The associations between PA and psychological stress and lumbar radicular pain were also noted in an earlier study [20]. The findings of this study are consistent with these earlier reports and demonstrate that PA and stress or depression trigger LBP and sciatica flare-ups. Similar to Costa’s findings relating to risk factors for low back pain flares [12], this study revealed that risk factors for flare-ups vary depending on the different definitions of flare. These findings built upon earlier work by further demonstrating that prolonged sitting (>1 h), prolonged walking (>half an hour), and prolonged standing (>1 h) triggered PDFs, and prolonged sitting (>1 h), mental distress, and depressed mood triggered NPDFs for patients with lumbar radicular pain who developed sciatica.
The categories of risk factors for flare-ups in patients with sciatica in the present study, such as PA and psychological stress, are similar to the categories of risk factors for low back pain reported by Parreira et al. [19]. While PA categories consisted of sitting (>2 h), prolonged standing (>2 h), and prolonged walking (>2 h) for low back pain patients according to Parreira’s review, the duration of PA in the present study was shorter, and PA consisted of sitting (>1 h), prolonged standing (>1 h), and prolonged walking (>half an hour). This means that there are significant differences in the intensity of PA between patients with the low back pain only and those with sciatica, with patients with lumbar radicular pain who develop sciatica requiring less intense PA to induce flares than patients with low back pain alone. In other words, shorter periods of PA can induce and aggravate sciatica.
The similarities and differences in the risk factors for flare-ups in lumbar radicular pain patients are noteworthy given that different definitions of flare-ups (PDFs or NPDFs) were used. Prolonged sitting (>1 h) is a common risk factor for both PDFs and NPDFs. Although other physical activities (manual handling of objects, driving, and frequent lifting) were not significantly associated with flare-ups in our study, it is possible that participants with sciatica rarely engage in such heavy PA, biasing effect estimates toward the null and decreasing our ability to detect associations. The majority of patients with lumbar radicular pain may perform only basic activities of daily living. Mental distress and depressed mood represent important and complex risk factors for NPDF-related lumbar radicular pain. A common theory holds that depression is a psychiatric disorder with various symptoms and is often accompanied by unexplained painful somatic symptoms [21]. As argued by Torta and Munari, depression may reduce the pain threshold and sensitize pain perception [22].
The data of risk factors for flare-ups in patients with lumbar radicular pain in this study were collected by face-to-face interviews or online survey. The majority of our participants (114/152) could complete the survey by both face-to-face and online methods, and a few participants (38/152) by only face-to-face interview. Significantly older and more dumpphone users were found in the only face-to-face surveys compared both face-to-face and online surveys. Overall, assessments of face-to-face validity were similar to online.
This study presents novel information about differences in risk factors for flare-ups in patients with lumbar radicular pain, depending on the different definitions of flare-ups used; this information may be useful for clinicians. First, prolonged sitting (>1 h) is a common risk factor for both PDFs and NPDFs in individuals with sciatica. Prolonged sitting may increase flare-ups in sciatica patients, particularly NPDFs. Second, clinicians should be aware that increases in flare-ups of radicular pain (PDF) may be related to PA, such as prolonged standing (>1 h) and prolonged walking (>half an hour), consistent with the characteristics of low back pain with radicular pain. Finally, the findings that mental distress and depressed mood are major risk factors for NPDFs, could influence clinicians’ decisions to pay attention to patients’ emotional states and provide timely psychological support in time for sciatica patients with lumbar radicular pain. In short, a better understanding of these risk factors provides a logical rationale for the development of more effective prevention strategies.
This study has several limitations. First, although the case-crossover design is an epidemiologic technique with distinct strengths for assessing the change in the risk of an acute event during a brief interval after exposure to a transient risk factor, there are some limitations of this study design. Such as incomplete data on exposures, overestimating exposures immediately prior to the outcome, and underestimating exposures during control intervals [23]. Second, the duration of our flare-up survey period, which spanned more than 3 days, was excessively long and may compromise the authenticity of determining the cause of the incident. Flare-ups reported more than a few hours (more than 3–4 h) after flare onset are problematic because when reporting such flares, participants often mistakenly report the consequences of a flare (things they have done or experienced because of the flare) as they happened before the flare. Future studies examining pain fluctuations should incorporate a longitudinal design to better characterize the quantitative changes in pain intensity typical of flare-ups, and to identify flare-ups prospectively, thereby avoiding the possible biases of retrospective flare-up assessments used in the present study. Last, although we excluded for having both PDF and NPDF on the same day in same participant, we examined the occurrence of either only PDFs or only NPDFs in terms of the participants’ respective risk factors. However, there may be an inherent logical connection between PDFs and NPDFs, or a vicious cycle between PDFs and NPDFs. Indeed, increased pain intensity can lead to functional limitations and depressed mood. For example, a PDF on a previous day may lead to an NPDF the next day. In fact, increased pain intensity can result in functional limitations and a depressed mood. This can create major problems in pain research. Future research should better clarify the differences and connections between PDFs and NPDFs.
5 Conclusions
This study of participants with acute lumbar radicular pain revealed that prolonged sitting (>1 h), prolonged walking (>half an hour), and prolonged standing (>1 h) increased risk for PDFs, and prolonged sitting (>1 h), mental distress, and depressed mood increased the risk for NPDFs.
Acknowledgements
This work was supported by grant 2021MSXM281 from Chongqing Health Commission & Science and Technology Commission.
-
Research ethics: The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). This study was approved by the Ethics Committee of Chongqing Medical University (Decision number: 2021750).
-
Informed consent: Informed consent was obtained from all individuals included in this study, or their legal guardians or wards.
-
Author contributions: The authors have accepted responsibility for the entire content of this manuscript and approved its submission. Wang Dawu and Yi Weiwei designed the study; Wang Dawu and Li Kaiting wrote the main manuscript text; Chen Dawei prepared Figure 1 and Supplementary tables; Tao Yuzhang prepared Table 1–3. All authors reviewed the manuscript.
-
Competing interests: The authors state no conflict of interest.
-
Research funding: This work was supported by grant 2021MSXM281 from Chongqing Health Commission & Science and Technology Commission.
-
Data availability: The raw data can be obtained on request from the corresponding author.
-
Artificial intelligence/Machine learning tools: Not applicable.
-
Supplementary Material: This article contains supplementary material (followed by the link to the article online).
References
[1] Hartvigsen J, Hancock MJ, Kongsted A, Louw Q, Ferreira ML, Genevay S, et al. What low back pain is and why we need to pay attention. Lancet. 2018;391(10137):2356–67.10.1016/S0140-6736(18)30480-XSearch in Google Scholar PubMed
[2] Will JS, Bury DC, Miller JA. Mechanical low back pain. Am Fam Physician. 2018;98(7):421–8.Search in Google Scholar
[3] Dincer F, Kesikburun S, Ozdemir O, Yaşar E, Munoz S, Valero R, et al. The approach of physiatrists to low back pain across Europe. J Back Musculoskelet Rehabil. 2019;32(1):131–9.10.3233/BMR-171001Search in Google Scholar PubMed
[4] Heliövaara M, Impivaara O, Sievers K, Melkas T, Knekt P, Korpi J, et al. Lumbar disc syndrome in Finland. J Epidemiol Community Health. 1987;41:251–8.10.1136/jech.41.3.251Search in Google Scholar PubMed PubMed Central
[5] Zimmer JM, Fauser D, Golla A, Wienke A, Schmitt N, Bethge M, et al. Barriers to applying for medical rehabilitation: a time-to-event analysis of employees with severe back pain in Germany. J Rehabil Med. 2022 Mar;54:jrm00274.10.2340/jrm.v53.1408Search in Google Scholar PubMed PubMed Central
[6] Aartun E, Iben AX, Silvano MI, Yngve RØ, Hondras M, Kretz L, et al. Contextualizing the lived experiences of patients with low back pain from different countries according to the ICF framework. J Rehabil Med. 2021;53(5):jrm00189.10.2340/16501977-2819Search in Google Scholar PubMed PubMed Central
[7] Axén I, Leboeuf-Yde C. Trajectories of low back pain. Best Pract Res Clin Rheumatol. 2013;27(5):601–12.10.1016/j.berh.2013.10.004Search in Google Scholar PubMed
[8] Kongsted A, Kent P, Axen I, Downie AS, Dunn KM. What have we learned from ten years of trajectory research in low back pain? BMC Musculoskelet Disord. 2016;17:220.10.1186/s12891-016-1071-2Search in Google Scholar PubMed PubMed Central
[9] Costa N, Hodges PW, Ferreira ML, Makovey J, Setchell J. What triggers an LBP flare? A content analysis of individuals’ perspectives. Pain Med. 2020;21(1):13–20.10.1093/pm/pnz021Search in Google Scholar PubMed
[10] de Vet HC, Heymans MW, Dunn KM, Pope DP, van der Beek AJ, Macfarlane GJ, et al. Episodes of low back pain: a proposal for uniform definitions to be used in research. Spine (Phila PA 1976). 2002;27(21):2409–16.10.1097/00007632-200211010-00016Search in Google Scholar
[11] VonKorff M. Studying the natural history of back pain. Spine (Phila PA 1976). 1994;19(18 Suppl):2041S–6S.10.1097/00007632-199409151-00005Search in Google Scholar PubMed
[12] Costa N, Smits E, Kasza J, Salomoni S, Ferreira M, Sullivan M, et al. ISSLS PRIZE IN CLINICAL SCIENCE 2021: What are the risk factors for low back pain flares and does this depend on how flare is defined? Eur Spine J. 2021;30(5):1089–97.10.1007/s00586-021-06730-6Search in Google Scholar
[13] Costa N, Ferreira ML, Setchell J, Makovey J, Dekroo T, Downie A, et al. A Definition of “flare” in low back pain: a multiphase process involving perspectives of individuals with low back pain and expert consensus. J Pain. 2019;20(11):1267–75.10.1016/j.jpain.2019.03.009Search in Google Scholar
[14] Suri P, Rainville J, de Schepper E, Martha J, Hartigan C, Hunter DJ. Do physical activities trigger flare-ups during an acute low back pain episode? A longitudinal case-crossover feasibility study. Spine (Phila PA 1976). 2018;43(6):427–33.10.1097/BRS.0000000000002326Search in Google Scholar
[15] Kherad M, Rosengren BE, Hasserius R, Nilsson JÅ, Redlund-Johnell I, Ohlsson C, et al. Risk factors for low back pain and sciatica in elderly men - the MrOS Sweden study. Age Ageing. 2017;46(1):64–71.10.1093/ageing/afw152Search in Google Scholar
[16] Matsudaira K, Kawaguchi M, Isomura T, Arisaka M, Fujii T, Takeshita K, et al. Identification of risk factors for new-onset sciatica in Japanese workers: findings from the Japan epidemiological research of occupation-related back pain study. Spine (Phila PA 1976). 2013;38(26):E1691–700.10.1097/BRS.0000000000000003Search in Google Scholar
[17] Shiri R, Falah-Hassani K, Heliövaara M, Solovieva S, Amiri S, Lallukka T, et al. Risk factors for low back pain: a population-based longitudinal study. Arthritis Care Res (Hoboken). 2019;71(2):290–9.10.1002/acr.23710Search in Google Scholar
[18] Schneeweiss S, Stürmer T, Maclure M. Case-crossover and case-time-control designs as alternatives in pharmacoepidemiologic research. Pharmacoepidemiol Drug Saf. 1997;6(Suppl 3):S51–9.10.1002/(SICI)1099-1557(199710)6:3+<S51::AID-PDS301>3.0.CO;2-SSearch in Google Scholar
[19] Parreira P, Maher CG, Steffens D, Hancock MJ, Ferreira ML. Risk factors for low back pain and sciatica: an umbrella review. Spine J. 2018;18(9):1715–21.10.1016/j.spinee.2018.05.018Search in Google Scholar
[20] Younes M, Béjia I, Aguir Z, Letaief M, Hassen-Zrour S, Touzi M, et al. Prevalence and risk factors of disk-related sciatica in an urban population in Tunisia. Jt Bone Spine. 2006;73(5):538–42.10.1016/j.jbspin.2005.10.022Search in Google Scholar
[21] Nekovarova T, Yamamotova A, Vales K, Stuchlik A, Fricova J, Rokyta R. Common mechanisms of pain and depression: are antidepressants also analgesics? Front Behav Neurosci. 2014;8:99. Published 2014 Mar 25.10.3389/fnbeh.2014.00099Search in Google Scholar
[22] Torta RG, Munari J. Symptom cluster: depression and pain. Surg Oncol. 2010;19(3):155–9.10.1016/j.suronc.2009.11.007Search in Google Scholar PubMed
[23] Redelmeier DA, Tibshirani RJ. Interpretation and bias in case-crossover studies. J Clin Epidemiol. 1997;50(11):1281–7.10.1016/S0895-4356(97)00196-0Search in Google Scholar
© 2024 the author(s), published by De Gruyter
This work is licensed under the Creative Commons Attribution 4.0 International License.
Articles in the same Issue
- Editorial Comment
- From pain to relief: Exploring the consistency of exercise-induced hypoalgesia
- Christmas greetings 2024 from the Editor-in-Chief
- Original Articles
- The Scandinavian Society for the Study of Pain 2022 Postgraduate Course and Annual Scientific (SASP 2022) Meeting 12th to 14th October at Rigshospitalet, Copenhagen
- Comparison of ultrasound-guided continuous erector spinae plane block versus continuous paravertebral block for postoperative analgesia in patients undergoing proximal femur surgeries
- Clinical Pain Researches
- The effect of tourniquet use on postoperative opioid consumption after ankle fracture surgery – a retrospective cohort study
- Changes in pain, daily occupations, lifestyle, and health following an occupational therapy lifestyle intervention: a secondary analysis from a feasibility study in patients with chronic high-impact pain
- Tonic cuff pressure pain sensitivity in chronic pain patients and its relation to self-reported physical activity
- Reliability, construct validity, and factorial structure of a Swedish version of the medical outcomes study social support survey (MOS-SSS) in patients with chronic pain
- Hurdles and potentials when implementing internet-delivered Acceptance and commitment therapy for chronic pain: a retrospective appraisal using the Quality implementation framework
- Exploring the outcome “days with bothersome pain” and its association with pain intensity, disability, and quality of life
- Fatigue and cognitive fatigability in patients with chronic pain
- The Swedish version of the pain self-efficacy questionnaire short form, PSEQ-2SV: Cultural adaptation and psychometric evaluation in a population of patients with musculoskeletal disorders
- Pain coping and catastrophizing in youth with and without cerebral palsy
- Neuropathic pain after surgery – A clinical validation study and assessment of accuracy measures of the 5-item NeuPPS scale
- Translation, contextual adaptation, and reliability of the Danish Concept of Pain Inventory (COPI-Adult (DK)) – A self-reported outcome measure
- Cosmetic surgery and associated chronic postsurgical pain: A cross-sectional study from Norway
- The association of hemodynamic parameters and clinical demographic variables with acute postoperative pain in female oncological breast surgery patients: A retrospective cohort study
- Healthcare professionals’ experiences of interdisciplinary collaboration in pain centres – A qualitative study
- Effects of deep brain stimulation and verbal suggestions on pain in Parkinson’s disease
- Painful differences between different pain scale assessments: The outcome of assessed pain is a matter of the choices of scale and statistics
- Prevalence and characteristics of fibromyalgia according to three fibromyalgia diagnostic criteria: A secondary analysis study
- Sex moderates the association between quantitative sensory testing and acute and chronic pain after total knee/hip arthroplasty
- Tramadol-paracetamol for postoperative pain after spine surgery – A randomized, double-blind, placebo-controlled study
- Cancer-related pain experienced in daily life is difficult to communicate and to manage – for patients and for professionals
- Making sense of pain in inflammatory bowel disease (IBD): A qualitative study
- Patient-reported pain, satisfaction, adverse effects, and deviations from ambulatory surgery pain medication
- Does pain influence cognitive performance in patients with mild traumatic brain injury?
- Hypocapnia in women with fibromyalgia
- Application of ultrasound-guided thoracic paravertebral block or intercostal nerve block for acute herpes zoster and prevention of post-herpetic neuralgia: A case–control retrospective trial
- Translation and examination of construct validity of the Danish version of the Tampa Scale for Kinesiophobia
- A positive scratch collapse test in anterior cutaneous nerve entrapment syndrome indicates its neuropathic character
- ADHD-pain: Characteristics of chronic pain and association with muscular dysregulation in adults with ADHD
- The relationship between changes in pain intensity and functional disability in persistent disabling low back pain during a course of cognitive functional therapy
- Intrathecal pain treatment for severe pain in patients with terminal cancer: A retrospective analysis of treatment-related complications and side effects
- Psychometric evaluation of the Danish version of the Pain Self-Efficacy Questionnaire in patients with subacute and chronic low back pain
- Dimensionality, reliability, and validity of the Finnish version of the pain catastrophizing scale in chronic low back pain
- To speak or not to speak? A secondary data analysis to further explore the context-insensitive avoidance scale
- Pain catastrophizing levels differentiate between common diseases with pain: HIV, fibromyalgia, complex regional pain syndrome, and breast cancer survivors
- Prevalence of substance use disorder diagnoses in patients with chronic pain receiving reimbursed opioids: An epidemiological study of four Norwegian health registries
- Pain perception while listening to thrash heavy metal vs relaxing music at a heavy metal festival – the CoPainHell study – a factorial randomized non-blinded crossover trial
- Observational Studies
- Cutaneous nerve biopsy in patients with symptoms of small fiber neuropathy: a retrospective study
- The incidence of post cholecystectomy pain (PCP) syndrome at 12 months following laparoscopic cholecystectomy: a prospective evaluation in 200 patients
- Associations between psychological flexibility and daily functioning in endometriosis-related pain
- Relationship between perfectionism, overactivity, pain severity, and pain interference in individuals with chronic pain: A cross-lagged panel model analysis
- Access to psychological treatment for chronic cancer-related pain in Sweden
- Validation of the Danish version of the knowledge and attitudes survey regarding pain
- Associations between cognitive test scores and pain tolerance: The Tromsø study
- Healthcare experiences of fibromyalgia patients and their associations with satisfaction and pain relief. A patient survey
- Video interpretation in a medical spine clinic: A descriptive study of a diverse population and intervention
- Role of history of traumatic life experiences in current psychosomatic manifestations
- Social determinants of health in adults with whiplash associated disorders
- Which patients with chronic low back pain respond favorably to multidisciplinary rehabilitation? A secondary analysis of a randomized controlled trial
- A preliminary examination of the effects of childhood abuse and resilience on pain and physical functioning in patients with knee osteoarthritis
- Differences in risk factors for flare-ups in patients with lumbar radicular pain may depend on the definition of flare
- Real-world evidence evaluation on consumer experience and prescription journey of diclofenac gel in Sweden
- Patient characteristics in relation to opioid exposure in a chronic non-cancer pain population
- Topical Reviews
- Bridging the translational gap: adenosine as a modulator of neuropathic pain in preclinical models and humans
- What do we know about Indigenous Peoples with low back pain around the world? A topical review
- The “future” pain clinician: Competencies needed to provide psychologically informed care
- Systematic Reviews
- Pain management for persistent pain post radiotherapy in head and neck cancers: systematic review
- High-frequency, high-intensity transcutaneous electrical nerve stimulation compared with opioids for pain relief after gynecological surgery: a systematic review and meta-analysis
- Reliability and measurement error of exercise-induced hypoalgesia in pain-free adults and adults with musculoskeletal pain: A systematic review
- Noninvasive transcranial brain stimulation in central post-stroke pain: A systematic review
- Short Communications
- Are we missing the opioid consumption in low- and middle-income countries?
- Association between self-reported pain severity and characteristics of United States adults (age ≥50 years) who used opioids
- Could generative artificial intelligence replace fieldwork in pain research?
- Skin conductance algesimeter is unreliable during sudden perioperative temperature increases
- Original Experimental
- Confirmatory study of the usefulness of quantum molecular resonance and microdissectomy for the treatment of lumbar radiculopathy in a prospective cohort at 6 months follow-up
- Pain catastrophizing in the elderly: An experimental pain study
- Improving general practice management of patients with chronic musculoskeletal pain: Interdisciplinarity, coherence, and concerns
- Concurrent validity of dynamic bedside quantitative sensory testing paradigms in breast cancer survivors with persistent pain
- Transcranial direct current stimulation is more effective than pregabalin in controlling nociceptive and anxiety-like behaviors in a rat fibromyalgia-like model
- Paradox pain sensitivity using cuff pressure or algometer testing in patients with hemophilia
- Physical activity with person-centered guidance supported by a digital platform or with telephone follow-up for persons with chronic widespread pain: Health economic considerations along a randomized controlled trial
- Measuring pain intensity through physical interaction in an experimental model of cold-induced pain: A method comparison study
- Pharmacological treatment of pain in Swedish nursing homes: Prevalence and associations with cognitive impairment and depressive mood
- Neck and shoulder pain and inflammatory biomarkers in plasma among forklift truck operators – A case–control study
- The effect of social exclusion on pain perception and heart rate variability in healthy controls and somatoform pain patients
- Revisiting opioid toxicity: Cellular effects of six commonly used opioids
- Letter to the Editor
- Post cholecystectomy pain syndrome: Letter to Editor
- Response to the Letter by Prof Bordoni
- Response – Reliability and measurement error of exercise-induced hypoalgesia
- Is the skin conductance algesimeter index influenced by temperature?
- Skin conductance algesimeter is unreliable during sudden perioperative temperature increase
- Corrigendum
- Corrigendum to “Chronic post-thoracotomy pain after lung cancer surgery: a prospective study of preoperative risk factors”
- Obituary
- A Significant Voice in Pain Research Björn Gerdle in Memoriam (1953–2024)
Articles in the same Issue
- Editorial Comment
- From pain to relief: Exploring the consistency of exercise-induced hypoalgesia
- Christmas greetings 2024 from the Editor-in-Chief
- Original Articles
- The Scandinavian Society for the Study of Pain 2022 Postgraduate Course and Annual Scientific (SASP 2022) Meeting 12th to 14th October at Rigshospitalet, Copenhagen
- Comparison of ultrasound-guided continuous erector spinae plane block versus continuous paravertebral block for postoperative analgesia in patients undergoing proximal femur surgeries
- Clinical Pain Researches
- The effect of tourniquet use on postoperative opioid consumption after ankle fracture surgery – a retrospective cohort study
- Changes in pain, daily occupations, lifestyle, and health following an occupational therapy lifestyle intervention: a secondary analysis from a feasibility study in patients with chronic high-impact pain
- Tonic cuff pressure pain sensitivity in chronic pain patients and its relation to self-reported physical activity
- Reliability, construct validity, and factorial structure of a Swedish version of the medical outcomes study social support survey (MOS-SSS) in patients with chronic pain
- Hurdles and potentials when implementing internet-delivered Acceptance and commitment therapy for chronic pain: a retrospective appraisal using the Quality implementation framework
- Exploring the outcome “days with bothersome pain” and its association with pain intensity, disability, and quality of life
- Fatigue and cognitive fatigability in patients with chronic pain
- The Swedish version of the pain self-efficacy questionnaire short form, PSEQ-2SV: Cultural adaptation and psychometric evaluation in a population of patients with musculoskeletal disorders
- Pain coping and catastrophizing in youth with and without cerebral palsy
- Neuropathic pain after surgery – A clinical validation study and assessment of accuracy measures of the 5-item NeuPPS scale
- Translation, contextual adaptation, and reliability of the Danish Concept of Pain Inventory (COPI-Adult (DK)) – A self-reported outcome measure
- Cosmetic surgery and associated chronic postsurgical pain: A cross-sectional study from Norway
- The association of hemodynamic parameters and clinical demographic variables with acute postoperative pain in female oncological breast surgery patients: A retrospective cohort study
- Healthcare professionals’ experiences of interdisciplinary collaboration in pain centres – A qualitative study
- Effects of deep brain stimulation and verbal suggestions on pain in Parkinson’s disease
- Painful differences between different pain scale assessments: The outcome of assessed pain is a matter of the choices of scale and statistics
- Prevalence and characteristics of fibromyalgia according to three fibromyalgia diagnostic criteria: A secondary analysis study
- Sex moderates the association between quantitative sensory testing and acute and chronic pain after total knee/hip arthroplasty
- Tramadol-paracetamol for postoperative pain after spine surgery – A randomized, double-blind, placebo-controlled study
- Cancer-related pain experienced in daily life is difficult to communicate and to manage – for patients and for professionals
- Making sense of pain in inflammatory bowel disease (IBD): A qualitative study
- Patient-reported pain, satisfaction, adverse effects, and deviations from ambulatory surgery pain medication
- Does pain influence cognitive performance in patients with mild traumatic brain injury?
- Hypocapnia in women with fibromyalgia
- Application of ultrasound-guided thoracic paravertebral block or intercostal nerve block for acute herpes zoster and prevention of post-herpetic neuralgia: A case–control retrospective trial
- Translation and examination of construct validity of the Danish version of the Tampa Scale for Kinesiophobia
- A positive scratch collapse test in anterior cutaneous nerve entrapment syndrome indicates its neuropathic character
- ADHD-pain: Characteristics of chronic pain and association with muscular dysregulation in adults with ADHD
- The relationship between changes in pain intensity and functional disability in persistent disabling low back pain during a course of cognitive functional therapy
- Intrathecal pain treatment for severe pain in patients with terminal cancer: A retrospective analysis of treatment-related complications and side effects
- Psychometric evaluation of the Danish version of the Pain Self-Efficacy Questionnaire in patients with subacute and chronic low back pain
- Dimensionality, reliability, and validity of the Finnish version of the pain catastrophizing scale in chronic low back pain
- To speak or not to speak? A secondary data analysis to further explore the context-insensitive avoidance scale
- Pain catastrophizing levels differentiate between common diseases with pain: HIV, fibromyalgia, complex regional pain syndrome, and breast cancer survivors
- Prevalence of substance use disorder diagnoses in patients with chronic pain receiving reimbursed opioids: An epidemiological study of four Norwegian health registries
- Pain perception while listening to thrash heavy metal vs relaxing music at a heavy metal festival – the CoPainHell study – a factorial randomized non-blinded crossover trial
- Observational Studies
- Cutaneous nerve biopsy in patients with symptoms of small fiber neuropathy: a retrospective study
- The incidence of post cholecystectomy pain (PCP) syndrome at 12 months following laparoscopic cholecystectomy: a prospective evaluation in 200 patients
- Associations between psychological flexibility and daily functioning in endometriosis-related pain
- Relationship between perfectionism, overactivity, pain severity, and pain interference in individuals with chronic pain: A cross-lagged panel model analysis
- Access to psychological treatment for chronic cancer-related pain in Sweden
- Validation of the Danish version of the knowledge and attitudes survey regarding pain
- Associations between cognitive test scores and pain tolerance: The Tromsø study
- Healthcare experiences of fibromyalgia patients and their associations with satisfaction and pain relief. A patient survey
- Video interpretation in a medical spine clinic: A descriptive study of a diverse population and intervention
- Role of history of traumatic life experiences in current psychosomatic manifestations
- Social determinants of health in adults with whiplash associated disorders
- Which patients with chronic low back pain respond favorably to multidisciplinary rehabilitation? A secondary analysis of a randomized controlled trial
- A preliminary examination of the effects of childhood abuse and resilience on pain and physical functioning in patients with knee osteoarthritis
- Differences in risk factors for flare-ups in patients with lumbar radicular pain may depend on the definition of flare
- Real-world evidence evaluation on consumer experience and prescription journey of diclofenac gel in Sweden
- Patient characteristics in relation to opioid exposure in a chronic non-cancer pain population
- Topical Reviews
- Bridging the translational gap: adenosine as a modulator of neuropathic pain in preclinical models and humans
- What do we know about Indigenous Peoples with low back pain around the world? A topical review
- The “future” pain clinician: Competencies needed to provide psychologically informed care
- Systematic Reviews
- Pain management for persistent pain post radiotherapy in head and neck cancers: systematic review
- High-frequency, high-intensity transcutaneous electrical nerve stimulation compared with opioids for pain relief after gynecological surgery: a systematic review and meta-analysis
- Reliability and measurement error of exercise-induced hypoalgesia in pain-free adults and adults with musculoskeletal pain: A systematic review
- Noninvasive transcranial brain stimulation in central post-stroke pain: A systematic review
- Short Communications
- Are we missing the opioid consumption in low- and middle-income countries?
- Association between self-reported pain severity and characteristics of United States adults (age ≥50 years) who used opioids
- Could generative artificial intelligence replace fieldwork in pain research?
- Skin conductance algesimeter is unreliable during sudden perioperative temperature increases
- Original Experimental
- Confirmatory study of the usefulness of quantum molecular resonance and microdissectomy for the treatment of lumbar radiculopathy in a prospective cohort at 6 months follow-up
- Pain catastrophizing in the elderly: An experimental pain study
- Improving general practice management of patients with chronic musculoskeletal pain: Interdisciplinarity, coherence, and concerns
- Concurrent validity of dynamic bedside quantitative sensory testing paradigms in breast cancer survivors with persistent pain
- Transcranial direct current stimulation is more effective than pregabalin in controlling nociceptive and anxiety-like behaviors in a rat fibromyalgia-like model
- Paradox pain sensitivity using cuff pressure or algometer testing in patients with hemophilia
- Physical activity with person-centered guidance supported by a digital platform or with telephone follow-up for persons with chronic widespread pain: Health economic considerations along a randomized controlled trial
- Measuring pain intensity through physical interaction in an experimental model of cold-induced pain: A method comparison study
- Pharmacological treatment of pain in Swedish nursing homes: Prevalence and associations with cognitive impairment and depressive mood
- Neck and shoulder pain and inflammatory biomarkers in plasma among forklift truck operators – A case–control study
- The effect of social exclusion on pain perception and heart rate variability in healthy controls and somatoform pain patients
- Revisiting opioid toxicity: Cellular effects of six commonly used opioids
- Letter to the Editor
- Post cholecystectomy pain syndrome: Letter to Editor
- Response to the Letter by Prof Bordoni
- Response – Reliability and measurement error of exercise-induced hypoalgesia
- Is the skin conductance algesimeter index influenced by temperature?
- Skin conductance algesimeter is unreliable during sudden perioperative temperature increase
- Corrigendum
- Corrigendum to “Chronic post-thoracotomy pain after lung cancer surgery: a prospective study of preoperative risk factors”
- Obituary
- A Significant Voice in Pain Research Björn Gerdle in Memoriam (1953–2024)

