Abstract
Objectives:
Pain catastrophizing in the aging population has not been studied in great detail. Existing investigations have reported conflicting results on the effects of age on pain catastrophizing in relation to pain responses. This study investigated the relationship between pain catastrophizing, and its individual components (rumination, magnification, and helplessness), and the responses to standardized experimental pain stimuli in old and young, healthy adults.
Methods:
Sixty-six volunteers (32 old: 65–87, 18 females; 34 young: 20–35, 17 females) participated in the study. Pain catastrophizing including the components of rumination, magnification, and helplessness was assessed with the pain catastrophizing scale (PCS). Experimental pain was induced by applying predefined pressure stimulations to the trapezius muscle. Pain intensity and unpleasantness were assessed using numerical rating scales. Pain catastrophizing levels and pain responses were statistically compared between the two age groups.
Results:
Elderly individuals reported significantly (p = 0.028) lower scores of pain catastrophizing (Med = 5; interquartile range [IQR] = 14) than younger individuals; this difference was driven by the significantly lower components of rumination (Med = 2; IQR = 4; p = 0.017) and helplessness (Med = 2; IQR = 7; p = 0.049). A larger proportion of young (57.8%) rated pain catastrophizing at high levels, with scores above the 75th percentile (Med = 20). Additionally, elderly reported the lowest pain intensity (Med = 5; p = 0.034) and pain unpleasantness (Med = 4.5; p = 0.011) responses to the experimental pressure stimuli. In the elderly group, pain unpleasantness was positively and significantly associated with pain catastrophizing (r s = 0.416, p = 0.021), rumination (r s = 0.42, p = 0.019), and helplessness (r s = 0.434, p = 0.015), respectively. No associations were found in the young group.
Conclusions:
Elderly reported lower PCSs than young adults. Rumination and helplessness were reduced in the elderly group. The elderly population showed positive correlations between catastrophizing levels and pain unpleasantness to standardized pressure pain stimuli. Results supported the view that elderly possess resilience over specific domains of pain catastrophizing that could counteract pain perception due to physiological decline.
1 Introduction
The effect of aging on pain perception remains controversial. Some clinical and experimental studies have reported higher pain sensitivity in elderly [1,2], whereas others have shown reduced pain sensitivity, pain complaints, and emotional reactivity in elderly individuals when compared with younger ones [3,4,5,6]. Although elderly individuals are more vulnerable to adverse health outcomes such as declining in physiological functioning and developing painful chronic conditions, the aging process per se does not necessarily lead to chronic pain [7]. Differences in prevalence of chronic pain could be attributed to several social, psychological, and biological variables and the copresence of co-morbid factors, which, in turn, can impact pain perception and modulation. Cognitive decline among the aging population poses a specific problem when pain conditions are assessed.
Aging is a complex dynamic process due to various physical and psychological changes [8]. Studies have found that elderly are more psychologically resilient than younger individuals. In fact, there is a slight decrease in self-reported negative affect, lower rates of anxiety, and major depression as compared with younger and middle-aged adults [9,10].
Among psychological factors, pain catastrophizing has been identified as a significant risk marker for adverse pain and health outcomes [11,12,13]. High pain catastrophizing is associated with enhanced pain sensitivity, increased pain severity, emotional distress and suffering, increased disability, and worse outcomes after surgery [14,15,16,17,18]. Additionally, catastrophizing has been suggested to be a predictor for developing chronic pain or chronification of acute pain in pain-free individuals [19].
Pain catastrophizing may decrease with age. However, the relationship between pain catastrophizing and pain perception in elderly individuals is unclear and may depend on individual factors and the type of pain experienced. Additionally, this relationship has been mainly reported by observational studies [20,21]. Some studies have reported that age moderates the relationship between pain catastrophizing and pain severity, indicating that young individuals with recurrent acute pain catastrophize more than elderly individuals with persistent and disabling chronic pain [22]. On the contrary, pain catastrophizing is found to be more strongly associated with pain intensity among older people, whereas pain intensity among younger people is more related to emotional responses to pain [23]. A longitudinal study showed that the effects of pain catastrophizing in worsening pain perception disappear when controlling for age, suggesting that elderly individuals might use different coping strategies [24].
Pain catastrophizing is a multifaceted construct constituted by several interrelated psychological dimensions [11,13]. Most commonly, it has been accepted to incorporate the tendency to repetitive negative thoughts about pain (rumination), the exaggeration on the perceived pain-related threat (magnification), and the sense of inability to effectively cope with pain (helplessness) [25]. Although existing research on the differential effect of these dimensions of pain catastrophizing on pain is scarce, the few studies revealed key contributions of the single domains of catastrophizing over pain-related outcomes [26,27]. Helplessness has shown to predict pain levels, perceived interference in life, affective distress, and depression; magnification has been associated with physical health and functioning [26,28,29], whereas rumination has been associated with lower pain tolerance [27]. So far, no studies on age-related differences investigating separate domains of pain catastrophizing are available. However, psychological literature, which examined these constructs separately and directly compared young and old adults, found that older individuals reported less ruminative thinking than young ones [30,31], and that reduced helplessness can predict resilience in both young and elderly individuals [32].
Pain catastrophizing has often been investigated as single construct; however, examining the construct as whole limits the analysis of its dimensions and their impact on pain-related outcomes [11,26]. Instead, an identification of how specific components of pain catastrophizing contribute to age difference in pain can be used to identify risk or resilience factors that can be informative regarding treatment approaches for proper psychological pain-related management.
The aim of the present experimental study was to investigate the relationship between pain catastrophizing together with its subdimensions (rumination, magnification, and helplessness) and pain responses to standardized experimental pressure stimuli in elderly and young individuals. Based on previous findings, we hypothesized that the elderly would have the lowest pain catastrophizing scores (PCSs) and the lowest pain sensitivity. Additionally, we hypothesized that each single dimension of catastrophizing will have different relationships with age and pain sensitivity.
2 Methods
2.1 Subjects
Sixty-six healthy young and elderly volunteers participated in the study, 34 young: 20–35 (24 ± 3.2 years, 17 F) and 32 elderly: 65–87 (74 ± 6.2 years, 18 F). Sample size was determined using an a priori calculation estimating type 1 error at 5% (alpha = 0.05) and type 2 error at 15% (85% power), with a conservative effect size moderate-to-large (d = 0.5–0.8).
Participants were recruited via posted advertisements and signed informed consent. They were screened with an interview prior to participation to exclude conditions that could affect their ability to follow instructions, answer the questionnaire, and report pain perception. In the interview, the participants were also assessed with the Mini Mental State Examination (MMSE) to ensure that their cognitive capabilities were intact. Individuals that scored >28 on MMSE were included in the study. Additionally, the following exclusion criteria were determined: if the participant reported the presence of severe ongoing pain, diabetes, signs of rheumatic or arthritic disease, especially on the neck and shoulders, and mental conditions such as anxiety and depression. All participants were pain-free, and none had taken any analgesic or sedative for at least 48 h prior to the experiment.
The study protocol was approved by the local ethical committee (N-20130071; N-20210065), and it was in accordance with all relevant national regulations, institutional policies, and followed the Helsinki Declaration and IASP’s guidelines for pain research in humans. The study was part of a larger study on assessing pain in dementia as a part of the EU-COST action TD1005. The subjects in this study were recruited as healthy controls in the primary study.
2.2 Apparatus
2.2.1 Pressure stimuli
An electronic hand-held pressure algometer (Somedic AB, Stockholm, Sweden) was used to produce noxious mechanical pressure. A force gauge fitted with a rubber disk with a surface of 1 cm2 was used in this study.
2.2.2 Experimental pain testing
Pressure stimuli of varying intensities were used and applied by using the electronic hand-held pressure algometer. Three different pressure intensities were used (50, 200, and 400 kPa) that have been shown to elicit “no pain,” “slight pain,” and “moderate pain,” respectively. Each pressure stimulus was applied on the upper border of the trapezius muscle in ascending order. Stimuli were applied to the right and left trapezius muscle resulting in six pressure stimuli at the two location sites (left and right) at three different intensities. The pressure was increased steadily for 2 s until the desired intensity was reached and kept constant for 5 s. A similar protocol was used in previous studies [33,34].
2.2.3 Numerical rating scale (NRS)
Participants’ pain intensity and unpleasantness ratings were assessed immediately after each pressure stimulus using an NRS posted in front of the participants. The intensity rating scale ranged from 0 (no pain) to 10 (the worst pain imaginable). The unpleasantness rating scale ranged from 0 (no unpleasant) to 10 (unbearable unpleasant). Before the experiment started, the experimenter introduced the two rating scales to the subject and explained the conceptual distinction between the intensity and unpleasantness dimensions of pain. Instructions were like the ones used by previous authors [35,36].
2.2.4 PCS
The PCS is composed of 13 items answered on a 5-point Likert-type scale. Total score lies between 0 and 52, and a higher score reflects higher levels of pain catastrophizing. Scores above 30 indicate a cut-off point for clinical significance. The scale comprises three subscales: rumination, magnification, and helplessness. These subscales are composed of four items (score range: 0–16) for rumination, three items (score range: 0–12) for magnification, and six items (score range: 0–24) for helplessness [25]. Reliability data report adequate to excellent internal validity scores (coefficient alpha for total PCS = 0.87–0.93, rumination = 0.87–0.91, magnification = 0.66–0.75, and helplessness = 0.78–0.87, respectively) [37].
The PCS was administered before the pain measures and was used as an index of individual characteristics. The participants were instructed to answer the questions by reflecting on their thoughts and feelings about past pain experiences.
2.3 Procedure
The experiment took place in a quiet and climate-controlled room, where the subjects were seated in a comfortable chair. The subjects filled in the PCS and were familiarized with the experimental procedure. Before the test started, subjects were trained until they understood the procedure and could follow the instructions.
Six pressures were applied on the trapezius muscle starting from the lowest intensity on the dominant and non-dominant side of the body in an alternated order: 50 kPa (dominant) – 50 kPa (non-dominant) – 200 kPa (dominant) – 200 kPa (non-dominant) – 400 kPa (dominant) – 400 kPa (non-dominant). Randomization for starting with the dominant/non-dominant side of the body was applied across subjects and individually assessed.
After each stimulation, subjects were instructed to rate the pain intensity and unpleasantness of the pressure stimulation.
2.4 Data analysis
Data were checked for normality using Shapiro–Wilk tests and calculating data frequency in histograms and Q–Q plots. Data were non-normally distributed; consequently, non-parametric tests were used in the following analyses.
Mann–Whitney U-tests were used to compare pain catastrophizing and subscales of rumination, magnification, helplessness, and NRS pain intensity and unpleasantness between young and elderly. Effect size estimations were calculated using the following formula:
Spearman’s r correlations were used to evaluate the relationship between NRS pain intensities, unpleasantness responses, and pain catastrophizing measures in the elderly and young groups. The significance of these correlations was assessed using the bias-corrected and accelerated method, which is effective in controlling type 1 errors associated with multiple comparisons. The 95% confidence interval (CI) using bootstrap resampling (1,000 sample, bias-corrected confidence limits) was computed for each correlation. Significant coefficients with an associated CI that did not include zero were considered statistically significant.
Box plots were used for descriptive statistics, where results were presented as the median, range, and interquartile range (IQR).
Data were statistically analyzed using SPSS version 28.0. A significant level of 0.05 was used. One elderly subject was excluded from the analyses since the PCS was incomplete.
3 Results
3.1 Distribution of pain catastrophizing between young and elderly
The distribution of pain catastrophizing total score and subscale scores resulted in the following for (1) the young group: PCS tot (Med = 10; IQR = 8.8; 95% CI = 8.8–13.7), rumination (Med = 4; IQR = 6; 95% CI = 3.5–5.6), magnification (Med = 2; IQR = 3; 95% CI = 1.2–2.6), helplessness (Med = 4; IQR = 5.3; 95% CI = 3.8–6.0), and (2) the elderly group: PCS tot (Med = 5; IQR = 14; 95% CI = 4.8–11.0), rumination (Med = 2; IQR = 4; 95% CI = 1.5–5.6), magnification (Med = 2; IQR = 2; 95% CI = 0.9–2.0), and helplessness (Med = 2; IQR = 7; 95% CI = 2.1–5.3).
In addition, 19 subjects (24% of the sample) reported PCSs above the 75th percentile, corresponding to PCSs of ≥15 (Med = 20). A larger percentage of these individuals was young, 57.8%, whereas a smaller percentage, 42%, was elderly, with a larger percentage of men, 68.3%, as compared with women, 31.5%. Notably, in the elderly group, men were significantly older than women (EM, Med = 76.5; EW, Med = 71; U = 190; N = 31; P < 0.005).
Mann–Whitney U-tests showed that elderly individuals reported significantly lower pain catastrophizing total scores than young individuals (U = 360.5, N1 = 34, N2 = 31, Z = −2.193, r = −0.27, p = 0.028, two-tailed asymptotic). Additionally, comparisons within the subscale scores showed that elderly individuals had significantly lower ruminations (U = 347.5, N1 = 34, N2 = 31, Z = 2.390, r = −0.29, p = 0.017, two-tailed asymptotic) and helplessness scores (U = 378.0, N1 = 34, N2 = 31, Z = −1.970, r = −0.24, p = 0.049, two-tailed asymptotic) than young individuals. No significant difference was observed in the magnification dimension (U = 469.5, N1 = 34, N2 = 31, Z = −0.784, r = −0.09, p = 0.433) (Figure 1).
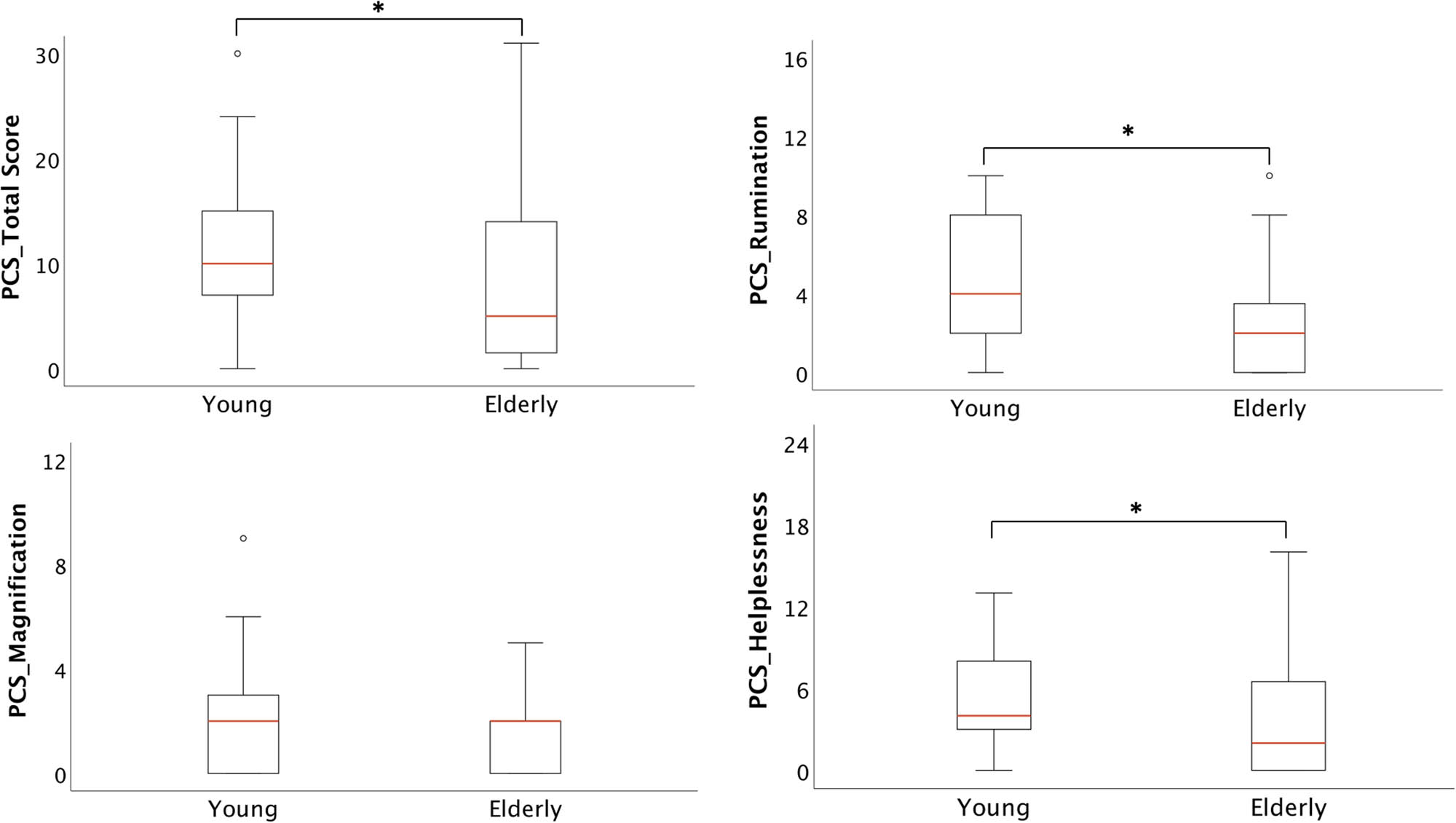
Significant lower pain catastrophizing total scores (p = 0.028*), rumination (p = 0.017*), and helplessness (p = 0.049*) scores were observed in elderly individuals when compared with young ones. Outliers are presented as ° in the figure.
3.2 Pressure stimuli 50, 200, and 400 kPa: NRS intensities and unpleasantness
The different pressure stimulations resulted in the following: 400 kPa moderately pain intensity (dominant Med = 6; IQR = 4.13; no-dominant Med = 6; IQR = 7.5) and unpleasant pain (dominant Med = 5; IQR = 4.13; no-dominant Med = 5; IQR = 2.5) perceptions; 200 kPa slightly pain intensity (dominant Med = 4; IQR = 5; no-dominant Med = 5; IQR = 3.7) and unpleasant pain (dominant Med = 3; IQR = 4.5; no-dominant Med = 4; IQR = 4.5) perceptions; and 50 kPa no-pain intensity (dominant Med = 0.5; IQR = 1; no-dominant Med = 0.5; IQR = 1) and unpleasant pain (dominant Med = 0.0; IQR = 0.5; no-dominant Med = 0.0; IQR = 0.5) perceptions. No statistical difference was observed between the dominant and non-dominant sites. Since pressures of 400 kPa could elicit moderate pain stimulations, these were further analyzed.
Mann–Whitney U-tests showed that elderly individuals (Med = 5) reported significantly lower NRS intensity pain scores (U = 366, N1 = 34, N2 = 31, Z = −2.122, r = −0.26, p = 0.034, two-tailed asymptotic), and lower NRS unpleasantness pain scores (Med = 4.5) (U = 334, N1 = 34, N2 = 31, Z = −2.546, r = −0.31, p = 0.011, two-tailed asymptotic), than young individuals (Med = 6.3, NRS intensity; Med = 5.5, NRS unpleasantness), respectively (Figure 2).

Significant lower pain intensity (p = 0.034*) and unpleasantness (p = 0.011*) NRS scores were observed in elderly individuals when compared with young ones.
3.3 Correlations between NRS pain responses and pain catastrophizing levels
Correlations were evaluated between NRS pain intensities and unpleasantness responses and total score of pain catastrophizing, rumination, magnification, and helplessness scores in elderly and young groups. No significant correlations were observed in the young group. In the elderly group, significant, positive correlations were observed between NRS pain unpleasantness scores and total PCSs (r s = 0.416, p = 0.020, two-tailed), rumination (r s = 0.420, p = 0.019, two-tailed), and helplessness (r s = 0.434, p = 0.015, two-tailed). No significant correlations were observed with magnification and between all sub-scales of PCSs and NRS pain intensities.
4 Discussion
This study showed significantly lower scores of pain catastrophizing in elderly individuals compared to young ones. This difference was driven by rumination and helplessness, which were significantly lower in the elderly. Additionally, a larger percentage of young individuals rated pain catastrophizing at high levels, with scores above the 75th percentile. Elderly individuals also reported the lowest pain intensity and pain unpleasantness to experimental pressure stimuli. In the elderly group, pain catastrophizing, rumination, and helplessness were positively associated with pain unpleasantness scores.
4.1 Different emotional regulatory strategies in elderly individuals
The study supported the view that older adults are less bothered or emotionally affected by pain and might use pain-related coping strategies associated with psychosocial well-being more effectively. The results were also in line with empirical evidence from large-scale studies showing that elderly, non-demented, individuals are in a better mood than their younger counterparts [10,39] and have fewer negative emotional experiences and greater emotional control [40,41]. Different types of explanations exist, for example, an improved resilience due to more experience with life-related stressors, enhanced use of coping strategies, or simply the acceptance of pain as part of the aging process [3,42,43]. Greater pain acceptance or reluctance to express pain has been often related to stoic attitudes toward pain and have been reported in older adults [44]. However, a recent study that compared stoic attitudes between young and elderly during an acute experimental pain induction have not found any significant difference among the groups [45].
The suggestion that elderly make a more effective use of pain-related coping strategies has been corroborated by studies showing that older people appear to use active [46,47] and adaptive coping strategies regardless of the overall pain intensity [42] and diverse use of emotion regulation strategies [48]. Today, it is acknowledged that pain catastrophizing is a complex phenomenon resulting in several interrelated processes, and it can be accounted as an emotional regulatory process [11].
Studies focusing on emotional regulatory strategies have found that reappraisal strategies (reframing the way one thinks about pain to reduce its emotional impact) partially mediate the relationship between the affective dimensions of pain and catastrophizing. Older women used reappraisal strategies more than younger women, whereas older men reported a lower use of reappraisal [48] and a larger use of suppression strategies (intentionally avoiding thoughts and feelings related to pain) than women. This is consistent with the idea that men tend to avoid emotional reactivity [49]. Additionally, distress, anxiety, and negative lifestyles mediated the relationship between catastrophizing and pain-related outcomes in older adults [20].
The present study also examined the contribution of the individual dimensions of pain catastrophizing between young and elderly. Rumination and helplessness were both reduced in the elderly as compared with the young ones. Previous psychological studies have shown that helplessness leads to a deterioration in motivation, cognition, and affect [50,51], and in elderly, the symptoms of helplessness have been associated with the risk of developing addictive behaviors [52]. Research on patients with rheumatological diseases revealed that helplessness is associated with a number of negative outcomes, such as poorer quality of life, functional disability, more severe symptoms, pain, fatigue, and higher distress [29,53,54]. Additionally, helplessness influenced patient’s attitudes toward illness and interfered negatively with treatment compliance [55,56]. Conversely, a reduced sense of helplessness enabled engagement in meaningful activities for copying with pain [57]. In elderly, the self-perception to control over health-related issues is fundamental for maintaining physical and psychological well-being [58]. Similarly, studies investigating the influence of rumination over health showed that individuals with high levels of rumination, and who continued to think about stressful events, had a slower recovery of heart rate and higher levels of cortisol [59]. Less rumination is observed in older individuals above the age of 63 when compared with other age groups [30], whereas excessive rumination and worrying are observed in young college students, influencing the relationship between pain and anxiety/depressive symptoms [60].
The results support the view that generally, healthy older adults are more resilient than younger ones [32]. Psychological resilience has shown to contrast the negative effects of illness [61], especially in older adults [62,63], and contribute to a successful healthy aging. Conversely, the elevated ruminative scores observed in the young adults point to the growing concern about the steadily increasing poor mental health in young people [64], as well as the early onset of mental disorders such as depression and anxiety [65]. More studies are reporting associations between mental disorders and pain symptoms and higher rates of chronic pain in young adulthood [66,67]. Consequently, the different degree of catastrophizing responses observed in the present sample, between young and elderly, could lead to risk or protective factors depending on the age group considered.
Finally, whether pain catastrophizing changes as function of gender is not completely determined [68]; although evidence points to higher levels of pain catastrophizing in women [13,69,70], a recent meta-analysis showed that men with chronic pain syndrome who had psychosocial symptoms had elevated pain catastrophizing [71]. Although the present study did not address gender difference due to small sample size, it was observed that high levels of pain catastrophizing were scored by elderly men, which were significantly older (>70) than the women (<70). Although limited, the studies that considered oldest-old individuals showed an increasing demand of care and support for pain management in this population [72,73]. Consequently, pain catastrophizing and gender difference in oldest groups are warranted for investigations.
4.2 Differences in age-related changes in pain perception
Experimental studies have shown a greater variability in pain perception among healthy old and young individuals. This variability has been attributed to the type of noxious stimulus used and the modality of the pain induction. For example, decreased sensitivity has been observed when phasic, short duration stimuli were applied on the skin surface, whereas increased sensitivity has been observed when tonic, deep, and diffuse stimuli were used [4,74,75]. However, age-related changes in nociceptive pathways have also been implicated in these differences. Experimental studies have highlighted a reduced pain tolerance and a decrement in the endogenous pain modulatory system in healthy elderly when compared with the young ones [76,77,78].
In the present study, the pain intensity and pain unpleasantness ratings to pain pressure stimuli were significantly reduced among elderly individuals. The results are in line with some of the aforementioned findings, and these decrements could be due to an actual reduction of pain sensitivity due to the noxious experimental modality utilized. Alternatively, it could also be speculated that the decrements in pain ratings could had been the product of supraspinal processing that top-down regulates the descending modulatory pain system. Less catastrophizing was driven by less rumination and less helplessness dimensions which are cognitive processes governed by prefrontal cortical structures [79]. Additionally, elderly individuals exhibit positive associations with catastrophizing and unpleasant ratings, indicating that these two variables were somehow related and influenced by each other, mainly in elderly but not in the young ones. It could be hypothesized that compensatory cognitive and emotional mechanisms take place in healthy elderly individuals when dealing with physiological pain-related changes. Future studies should investigate this hypothesis and underline the interactive mechanisms of resilience observed in elderly individuals.
4.3 Methodological considerations and limitations
The present study has some limitations. First, the sample utilized here was selected as control sample for a primary study on pain in dementia. Consequently, the generalizability of the findings would be difficult, especially for the elderly group who might not be representative of the population since they were selected to be very fit. Young and older individuals with persistent and chronic pain might struggle with low mood, poorer physical function, disability, and social isolation and are at risk of depression. Depressed mood is the strongest predictor of health decline in the elderly [80], and catastrophizing in individuals with mild cognitive impairment could be a limiting factor for proper cognitive management and preventive treatments for dementia for this group [81]. However, studies investigating catastrophizing in individual with cognitive impairment are lacking at the present. In the elderly, dementia is likewise a major hurdle for optimized pain management [82] and for using different pain scales/questionnaires [83,84].
A better stratification of aging groups: youngest-old (ages 65–74), middle-old (ages 75–84), and oldest-old (>85), could have been more informative about the development of pain catastrophizing over the lifespan, especially now that the global aging population tends to be larger and the old classification of above 65 is becoming too reductive.
Second, this study investigated pain catastrophizing with the sole use of the PCS. Pain catastrophizing is a complex phenomenon, and it could be a limitation to measure it with only one scale [85]. Additionally, although age-related difference has been suggested, pain catastrophizing could also depend by personality traits and individual pain experiences gathered during life. Future studies should attempt to replicate the present findings adding a larger range of psychological variables considering the multidimensionality of pain catastrophizing, personality variables, social context of the sample, as well as assessing the pain descending modulatory system.
5 Conclusions
The study showed that healthy elderly reported lower PCSs than healthy young adults. Additionally, the different dimensions of pain catastrophizing showed that rumination and helplessness were reduced in the elderly group, suggesting better coping and emotional regulatory mechanisms. For the elderly population, positive correlations between catastrophizing levels and pain unpleasantness to standardized pressure pain stimuli were found. Understanding age-related psychophysical changes across lifespan can help in the development of intervention strategies that target different age periods accordingly.
Acknowledgments
Center for Neuroplasticity and Pain (CNAP) was supported by the Danish National Research Foundation (DNRF121).
-
Research ethics: The research complied with all relevant national regulations and institutional policies, and it was in accordance with the tenets of the Helsinki Declaration for conducting research on human volunteers. The local regional ethical committee (N-20130071; N-20210065) approved the project.
-
Informed consent: Informed consent was obtained from all individuals included in this study, or their legal guardians or wards.
-
Author contributions: The authors have accepted responsibility for the entire content of this manuscript and approved its submission.
-
Competing interests: Lars Arendt-Nielsen is a Honorary Editor and a Section Editor of the Scandinavian Journal of Pain. The authors report no conflicts of interest in this work.
-
Research funding: The authors state that no external funding is involved. Internal funds financed the study.
-
Data availability: The raw data can be obtained on request from the corresponding author.
References
[1] Uthaikhup S, Prasert R, Paungmali A, Boontha K. Altered pain sensitivity in elderly women with chronic neck pain. PloS One. 2015;10:e0128946. 10.1371/journal.pone.0128946.Search in Google Scholar PubMed PubMed Central
[2] El Tumi H, Johnson MI, Dantas PBF, Maynard MJ, Tashani OA. Age-related changes in pain sensitivity in healthy humans: A systematic review with meta-analysis. Eur J Pain Lond Engl. 2017;21:955–64. 10.1002/ejp.1011.Search in Google Scholar PubMed
[3] Riley JL, Gilbert GH. Orofacial pain symptoms: an interaction between age and sex. Pain. 2001;90:245–56. 10.1016/S0304-3959(00)00408-5.Search in Google Scholar PubMed
[4] Lautenbacher S, Peters JH, Heesen M, Scheel J, Kunz M. Age changes in pain perception: A systematic-review and meta-analysis of age effects on pain and tolerance thresholds. Neurosci Biobehav Rev. 2017;75:104–13. 10.1016/j.neubiorev.2017.01.039.Search in Google Scholar PubMed
[5] Molton IR, Terrill AL. Overview of persistent pain in older adults. Am Psychol. 2014;69:197–207. 10.1037/a0035794.Search in Google Scholar PubMed
[6] Petrini L, Matthiesen ST, Arendt-Nielsen L. The effect of age and gender on pressure pain thresholds and suprathreshold stimuli. Perception. 2015;44:587–96. 10.1068/p7847.Search in Google Scholar PubMed
[7] Jones MR, Ehrhardt KP, Ripoll JG, Sharma B, Padnos IW, Kaye RJ, et al. Pain in the Elderly. Curr Pain Headache Rep. 2016;20:23. 10.1007/s11916-016-0551-2 Search in Google Scholar PubMed
[8] Junior J, de Medeiros AGA, Fernandes A, Vasconcelos C, Amorim L, Queiroga M, et al. Hopelessness in the elderly: A systematic review. MOJ Gerontol Geriatr. 2018;3:273–8. 10.15406/mojgg.2018.03.00132.Search in Google Scholar
[9] Scheibe S, Carstensen LL. Emotional aging: recent findings and future trends. J Gerontol B Psychol Sci Soc Sci. 2010;65B:135–44. 10.1093/geronb/gbp132.Search in Google Scholar PubMed PubMed Central
[10] Carstensen LL, Turan B, Scheibe S, Ram N, Ersner-Hershfield H, Samanez-Larkin GR, et al. Emotional experience improves with age: evidence based on over 10 years of experience sampling. Psychol Aging. 2011;26:21–33. 10.1037/a0021285.Search in Google Scholar PubMed PubMed Central
[11] Petrini L, Arendt-Nielsen L. Understanding pain catastrophizing: putting pieces together. Front Psychol. 2020;11:603420. 10.3389/fpsyg.2020.603420.Search in Google Scholar PubMed PubMed Central
[12] Quartana PJ, Campbell CM, Edwards RR. Pain catastrophizing: a critical review. Expert Rev Neurother. 2009;9:745–58. 10.1586/ERN.09.34.Search in Google Scholar
[13] Sullivan M, Thorn B, Haythornthwaite JA, Keefe F, Martin M, Bradley LA, et al. Theoretical perspectives on the relation between catastrophizing and pain. Clin J Pain. 2001;17:52–64. 10.1097/00002508-200103000-00008.Search in Google Scholar PubMed
[14] Skrejborg P, Petersen KK, Kold S, Kappel A, Pedersen C, Østgaard SE, et al. Patients with high chronic postoperative knee pain 5 years after total knee replacement demonstrate low-grad inflammation, impairment of function, and high levels of pain catastrophizing. Clin J Pain. 2021;37:161–7. 10.1097/AJP.0000000000000907.Search in Google Scholar PubMed
[15] Keefe FJ, Rumble ME, Scipio CD, Giordano LA, Perri LM. Psychological aspects of persistent pain: Current state of the science. J Pain. 2004;5:195–211. 10.1016/j.jpain.2004.02.576.Search in Google Scholar PubMed
[16] Lackner JM, Quigley BM. Pain catastrophizing mediates the relationship between worry and pain suffering in patients with irritable bowel syndrome. Behav Res Ther. 2005;43:943–57. 10.1016/j.brat.2004.06.018.Search in Google Scholar PubMed
[17] Picavet HSJ, Vlaeyen JWS, Schouten JSAG. Pain catastrophizing and kinesiophobia: predictors of chronic low back pain. Am J Epidemiol. 2002;156:1028–34. 10.1093/aje/kwf136.Search in Google Scholar PubMed
[18] Hovik LH, Winther SB, Foss OA, Gjeilo KH. Preoperative pain catastrophizing and postoperative pain after total knee arthroplasty: a prospective cohort study with one year follow-up. Bmc Musculoskelet Disord. 2016;17:214. 10.1186/s12891-016-1073-0.Search in Google Scholar PubMed PubMed Central
[19] Meints SM, Mawla I, Napadow V, Kong J, Gerber J, Chan S-T, et al. The relationship between catastrophizing and altered pain sensitivity in patients with chronic low-back pain. Pain. 2019;160:833–43. 10.1097/j.pain.0000000000001461.Search in Google Scholar PubMed PubMed Central
[20] Dong H-J, Gerdle B, Bernfort L, Levin L-Å, Dragioti E. Pain catastrophizing in older adults with chronic pain: the mediator effect of mood using a path analysis approach. J Clin Med. 2020;9:2073. 10.3390/jcm9072073.Search in Google Scholar PubMed PubMed Central
[21] Park SJ, Lee R, Yoon DM, Yoon KB, Kim K, Kim SH. Factors associated with increased risk for pain catastrophizing in patients with chronic neck pain. Medicine (Baltimore). 2016;95:e4698. 10.1097/MD.0000000000004698.Search in Google Scholar PubMed PubMed Central
[22] Santavirta N, Björvell H, Solovieva S, Alaranta H, Hurskainen K, Konttinen YT. Coping strategies, pain, and disability in patients with hemophilia and related disorders. Arthritis Rheum . 2001;45:48–55. 10.1002/1529-0131(200102)45:1<48:AID-ANR83>3.0.CO;2-1.Search in Google Scholar
[23] Ruscheweyh R, Nees F, Marziniak M, Evers S, Flor H, Knecht S. Pain catastrophizing and pain-related emotions: influence of age and type of pain. Clin J Pain. 2011;27:578–86. 10.1097/AJP.0b013e31820fde1b.Search in Google Scholar
[24] Benyon K, Muller S, Hill S, Mallen C. Coping strategies as predictors of pain and disability in older people in primary care: a longitudinal study. BMC Fam Pract. 2013;14:67. 10.1186/1471-2296-14-67.Search in Google Scholar
[25] Sullivan MJL, Bishop SR, Pivik J. The pain catastrophizing Scale: development and validation. Psychol Assess. 1995;7:524–32. 10.1037/1040-3590.7.4.524.Search in Google Scholar
[26] Craner JR, Gilliam WP, Sperry JA. Rumination, magnification, and helplessness: How do different aspects of pain catastrophizing relate to pain severity and functioning? Clin J Pain. 2016;32:1028–35. 10.1097/AJP.0000000000000355.Search in Google Scholar
[27] Meints SM, Stout M, Abplanalp S, Hirsh AT. Pain-related rumination, but not magnification or helplessness, mediates race and sex differences in experimental pain. J Pain. 2017;18:332–9. 10.1016/j.jpain.2016.11.005.Search in Google Scholar
[28] Smith TW, Peck JR, Ward JR. Helplessness and depression in rheumatoid arthritis. Health Psychol. 1990;9:377–89. 10.1037/0278-6133.9.4.377.Search in Google Scholar
[29] Camacho EM, Verstappen SMM, Chipping J, Symmons DPM. Learned helplessness predicts functional disability, pain and fatigue in patients with recent-onset inflammatory polyarthritis. Rheumatology. 2013;52:1233–8. 10.1093/rheumatology/kes434.Search in Google Scholar
[30] Sütterlin S, Paap MCS, Babic S, Kübler A, Vögele C. Rumination and age: Some things get better. J Aging Res. 2012;2012:1–10. 10.1155/2012/267327.Search in Google Scholar
[31] Thomsen DK, Mehlsen MY, Olesen F, Hokland M, Viidik A, Avlund K, et al. Is there an association between rumination and self-reported physical health? a one-year follow-up in a young and an elderly sample. J Behav Med. 2004;27:215–31. 10.1023/B:JOBM.0000028496.41492.34.Search in Google Scholar
[32] Gooding PA, Hurst A, Johnson J, Tarrier N. Psychological resilience in young and older adults. Int J Geriatr Psychiatry. 2012;27:262–70. 10.1002/gps.2712.Search in Google Scholar PubMed
[33] Oosterman JM, Traxler J, Kunz M. The influence of executive functioning on facial and subjective pain responses in older adults. Behav Neurol. 2016;2016:e1984827. 10.1155/2016/1984827.Search in Google Scholar PubMed PubMed Central
[34] Kunz M, Crutzen-Braaksma P, Giménez-Llort L, Invitto S, Villani G, deTommaso M, et al. Observing pain in individuals with cognitive impairment: a pilot comparison attempt across countries and across different types of cognitive impairment. Brain Sci. 2021;11:1455. 10.3390/brainsci11111455.Search in Google Scholar PubMed PubMed Central
[35] Rainville P, Feine JS, Bushnell MC, Duncan GH. A psychophysical comparison of sensory and affective responses to four modalities of experimental pain. Somatosens Mot Res. 1992;9:265–77. 10.3109/08990229209144776.Search in Google Scholar PubMed
[36] Price DD, McGrath PA, Rafii A, Buckingham B. The validation of visual analogue scales as ratio scale measures for chronic and experimental pain. Pain. 1983;17:45–56. 10.1016/0304-3959(83)90126-4.Search in Google Scholar PubMed
[37] Wheeler CHB, Williams AC, de C, Morley SJ. Meta-analysis of the psychometric properties of the Pain catastrophizing scale and associations with participant characteristics. Pain. 2019;160:1946. 10.1097/j.pain.0000000000001494.Search in Google Scholar PubMed
[38] Field A. Discovering Statistics Using IBM SPSS Statistics. London, England: SAGE Publications Ltd. (4th Ed.); 2013.Search in Google Scholar
[39] Lawton MP. Emotion in later life. Curr Dir Psychol Sci. 2001;10:120–3. 10.1111/1467-8721.00130.Search in Google Scholar
[40] Urry HL, Gross JJ. Emotion regulation in older age. Curr Dir Psychol Sci. 2010;19:352–7. 10.1177/0963721410388395.Search in Google Scholar
[41] Gross JJ. Emotion and aging: Experience, expression, and control. Psychol Aging. 1997;12:590. 10.1037/0882-7974.12.4.590.Search in Google Scholar
[42] Molton I, Jensen MP, Ehde DM, Carter GT, Kraft G, Cardenas DD. Coping with chronic pain among younger, middle-aged, and older adults living with neurological injury and disease. J Aging Health. 2008;20:972–96. 10.1177/0898264308324680.Search in Google Scholar PubMed PubMed Central
[43] Rustøen T, Wahl AK, Hanestad BR, Lerdal A, Paul S, Miaskowski C. Age and the experience of chronic pain: differences in health and quality of life among younger, middle-aged, and older adults. Clin J Pain. 2005;21:513–23. 10.1097/01.ajp.0000146217.31780.ef.Search in Google Scholar PubMed
[44] Yong H-H, Gibson SJ, De L, Horne DJ, Helme RD. Development of a pain attitudes questionnaire to assess stoicism and cautiousness for possible age differences. J Gerontol B Psychol Sci Soc Sci. 2001;56:P279–84. 10.1093/geronb/56.5.P279.Search in Google Scholar PubMed
[45] Shackleton DA, Castillo LIR, Hampton AJD, Volodin A, Hadjistavropoulos T. Age differences in thermal pain responses: a direct laboratory comparison. J Gerontol Ser B. 2023;78:1521–5. 10.1093/geronb/gbad065.Search in Google Scholar PubMed
[46] Wittink H, Rogers W, Lipman A, McCarberg W, Ashburn M, Oderda G, et al. Older and younger adults in pain management programs in the United States: Differences and similarities. J Pain. 2005;6:S72. 10.1016/j.jpain.2005.01.286.Search in Google Scholar
[47] Prohaska TR, Leventhal EA, Leventhal H, Keller ML. Health practices and illness cognition in young, middle aged, and elderly adults. J Gerontol. 1985;40:569–78. 10.1093/geronj/40.5.569.Search in Google Scholar PubMed
[48] Ghandehari O, Gallant NL, Hadjistavropoulos T, Williams J, Clark DA. The relationship between the pain experience and emotion regulation in older adults. Pain Med Malden Mass. 2020;21:3366–76. 10.1093/pm/pnaa135.Search in Google Scholar PubMed
[49] Barrett LF, Bliss-Moreau E. She’s emotional. He’s having a bad day: attributional explanations for emotion stereotypes. Emotion. 2009;9:649–58. 10.1037/a0016821.Search in Google Scholar PubMed
[50] Seligman ME. Learned helplessness as a model of depression. Comment and integration. J Abnorm Psychol. 1978;87:165–79.10.1037//0021-843X.87.1.165Search in Google Scholar
[51] Seligman ME, Weiss J, Weinraub M, Schulman A. Coping behavior: learned helplessness, physiological change and learned inactivity. Behav Res Ther. 1980;18:459–512. 10.1016/0005-7967(80)90011-x.Search in Google Scholar PubMed
[52] Hochhauser M. Learned helplessness and substance abuse in the elderly. J Psychoactive Drugs. 1981;13:127–33. 10.1080/02791072.1981.10524294.Search in Google Scholar PubMed
[53] Brady TJ. Measures of self-efficacy, helplessness, mastery, and control: The Arthritis Helplessness Index (AHI)/Rheumatology Attitudes Index (RAI), Arthritis Self-Efficacy Scale (ASES), Children’s Arthritis Self-Efficacy Scale (CASE), Generalized Self-Efficacy Scale (GSES), Mastery Scale, Multi-Dimensional Health Locus of Control Scale (MHLC), Parent’s Arthritis Self-Efficacy Scale (PASE), Rheumatoid Arthritis Self-Efficacy Scale (RASE), and Self-Efficacy Scale (SES). Arthritis Rheum. 2003;49:S147–64. 10.1002/art.11413.Search in Google Scholar
[54] Lindroth Y, Strömbeck B, Brossner M, Gullberg B, Wollheim FA. Learned helplessness and its correlation to impairment, pain, anxiety and depression in rheumatoid arthritis. Scand J Rheumatol. 1994;23:299–304. 10.3109/03009749409099277.Search in Google Scholar PubMed
[55] Xie C, Li L, Zhou L, Sun C, Zhang Y, Li Y. Mediating role of learned helplessness’ components in the association between health literacy/social support and self-management among maintenance haemodialysis patients in Changsha, China: a cross-sectional study. BMJ Open. 2023;13:e068601. 10.1136/bmjopen-2022-068601.Search in Google Scholar PubMed PubMed Central
[56] Nowicka-Sauer K, Hajduk A, Kujawska-Danecka H, Banaszkiewicz D, Czuszyńska Z, Smoleńska Ż, et al. Learned helplessness and its associations with illness perception, depression and anxiety among patients with systemic lupus erythematosus. Fam Med Prim Care Rev. 2017;19:243–6. 10.5114/fmpcr.2017.69285.Search in Google Scholar
[57] Samwel H, Evers A, Crul B, Kraaimaat F. The role of helplessness, fear of pain, and passive pain-coping in chronic pain patients. Clin J Pain. 2006;22:245–51. 10.1097/01.ajp.0000173019.72365.f5.Search in Google Scholar PubMed
[58] Teitelman JL. Eliminating learned helplessness in older rehabilitation patients. Phys Occup Ther Geriatr. 1982;1:3–10. 10.1080/J148V01N04_02.Search in Google Scholar
[59] Roger D, Najarian B. The relationship between emotional rumination and cortisol under stress. Personal Individ Differ. 1998;24:531–8. 10.1016/S0191-8869(97)00204-3.Search in Google Scholar
[60] Rogers AH, Bakhshaie J, Ditre JW, Manning K, Mayorga NA, Viana AG, et al. Worry and rumination: Explanatory roles in the relation between pain and anxiety and depressive symptoms among college students with pain. J Am Coll Health. 2019;67:275–82. 10.1080/07448481.2018.1481071.Search in Google Scholar PubMed
[61] Windle G, Woods B, Markland D. Living with Ill-health in older age: The role of a resilient personality. J Happiness Stud. 2010;11:763–77. 10.1007/s10902-009-9172-3.Search in Google Scholar
[62] Nygren B, Aléx L, Jonsén E, Gustafson Y, Norberg A, Lundman B. Resilience, sense of coherence, purpose in life and self-transcendence in relation to perceived physical and mental health among the oldest old. Aging Ment Health. 2005;9:354–62. 10.1080/1360500114415.Search in Google Scholar PubMed
[63] Mehta M, Whyte E, Lenze E, Hardy S, Roumani Y, Subashan P, et al. Depressive symptoms in late life: associations with apathy, resilience and disability vary between young-old and old-old. Int J Geriatr Psychiatry. 2008;23:238–43. 10.1002/gps.1868.Search in Google Scholar PubMed
[64] Twenge JM, Cooper AB, Joiner TE, Duffy ME, Binau SG. Age, period, and cohort trends in mood disorder indicators and suicide-related outcomes in a nationally representative dataset, 2005-2017. J Abnorm Psychol. 2019;128:185–99. 10.1037/abn0000410.Search in Google Scholar PubMed
[65] Thapar A, Collishaw S, Pine DS, Thapar AK. Depression in adolescence. The Lancet. 2012;379:1056–67. 10.1016/S0140-6736(11)60871-4.Search in Google Scholar PubMed PubMed Central
[66] Hoftun GB, Romundstad PR, Rygg M. Factors associated with adolescent chronic non-specific pain, chronic multisite pain, and chronic pain with high disability: The young–hunt study 2008. J Pain. 2012;13:874–83. 10.1016/j.jpain.2012.06.001.Search in Google Scholar PubMed
[67] Eckhoff C, Straume B, Kvernmo S. Multisite musculoskeletal pain in adolescence and later mental health disorders: a population-based registry study of Norwegian youth: The NAAHS cohort study. BMJ Open. 2017;7:e012035. 10.1136/bmjopen-2016-012035.Search in Google Scholar PubMed PubMed Central
[68] Bartley EJ, Fillingim RB. Sex differences in pain: a brief review of clinical and experimental findings. Br J Anaesth. 2013;111:52–8. 10.1093/bja/aet127.Search in Google Scholar PubMed PubMed Central
[69] Sjörs A, Larsson B, Persson AL, Gerdle B. An increased response to experimental muscle pain is related to psychological status in women with chronic non-traumatic neck-shoulder pain. BMC Musculoskelet Disord. 2011;12:230. 10.1186/1471-2474-12-230.Search in Google Scholar PubMed PubMed Central
[70] Umar A, Mohammed A, Ayo J, Danjuma N, Isa A, Suleiman I, et al. Evaluation of Cold Pressor Pain Response and Pain Catastrophization in a Healthy Nigerian Adult Population. J Med Bas Sci Res. 2021;2:37–49. 10.5281/zenodo.5809673.Search in Google Scholar
[71] Huang X, Qin Z, Cui H, Chen J, Liu T, Zhu Y, et al. Psychological factors and pain catastrophizing in men with chronic prostatitis/chronic pelvic pain syndrome (CP/CPPS): A meta-analysis. Transl Androl Urol. 2020;9:485–93. 10.21037/tau.2020.01.25.Search in Google Scholar PubMed PubMed Central
[72] Mallon T, Ernst A, Brettschneider C, König H-H, Luck T, Röhr S, et al. Prevalence of pain and its associated factors among the oldest-olds in different care settings – results of the AgeQualiDe study. BMC Fam Pract. 2018;19:85. 10.1186/s12875-018-0768-8.Search in Google Scholar PubMed PubMed Central
[73] Mallon T, Eisele M, König H-H, Brettschneider C, Röhr S, Pabst A, et al. Lifestyle aspects as a predictor of pain among oldest-old primary care patients – a longitudinal cohort study. Clin Interv Aging. 2019;14:1881–8. 10.2147/CIA.S217431.Search in Google Scholar PubMed PubMed Central
[74] Edwards RR, Fillingim RB. Effects of age on temporal summation and habituation of thermal pain: Clinical relevance in healthy older and younger adults. J Pain. 2001;2:307–17. 10.1054/jpai.2001.25525.Search in Google Scholar PubMed
[75] Lautenbacher S, Kunz M, Strate P, Nielsen J, Arendt-Nielsen L. Age effects on pain thresholds, temporal summation and spatial summation of heat and pressure pain. Pain. 2005;115:410–8. 10.1016/j.pain.2005.03.025.Search in Google Scholar PubMed
[76] Edwards RR, Fillingim RB. Age-associated differences in responses to noxious stimuli. J Gerontol A Biol Sci Med Sci. 2001;56:M180–5. 10.1093/gerona/56.3.M180.Search in Google Scholar
[77] Edwards RR, Fillingim RB, Ness TJ. Age-related differences in endogenous pain modulation: a comparison of diffuse noxious inhibitory controls in healthy older and younger adults. Pain. 2003;101:155–65. 10.1016/s0304-3959(02)00324-x.Search in Google Scholar PubMed
[78] Naugle KM, Naugle KE, Riley JL. Reduced modulation of pain in older adults after isometric and aerobic exercise. J Pain. 2016;17:719–28. 10.1016/j.jpain.2016.02.013.Search in Google Scholar PubMed PubMed Central
[79] Seminowicz DA, Moayedi M. The dorsolateral prefrontal cortex in acute and chronic pain. J Pain Off. 2017;18:1027–35. 10.1016/j.jpain.2017.03.008.Search in Google Scholar PubMed PubMed Central
[80] Penninx BWJH, Guralnik JM, Ferrucci L, Simonsick EM, Deeg DJH, Wallace RB. Depressive symptoms and physical decline in community-dwelling older persons. JAMA. 1998;279:1720–6. 10.1001/jama.279.21.1720.Search in Google Scholar PubMed
[81] Rosenberg PB, Lyketsos C. Mild cognitive impairment: searching for the prodrome of Alzheimer’s disease. World Psychiatry. 2008;7:72–8.10.1002/j.2051-5545.2008.tb00159.xSearch in Google Scholar PubMed PubMed Central
[82] Nygaard HA, Jarland M. Are nursing home patients with dementia diagnosis at increased risk for inadequate pain treatment? Int J Geriatr Psychiatry. 2005;20:730–7. 10.1002/gps.1350.Search in Google Scholar PubMed
[83] Catananti C, Gambassi G. Pain assessment in the elderly. Surg Oncol. 2010;19:140–8. 10.1016/j.suronc.2009.11.010.Search in Google Scholar PubMed
[84] Herr K. Pain assessment strategies in older patients. J Pain. 2011;12:S3–13. 10.1016/j.jpain.2010.11.011.Search in Google Scholar PubMed
[85] Crombez G, Paepe ALD, Veirman E, Eccleston C, Verleysen G, Ryckeghem DMLV. Let’s talk about pain catastrophizing measures: an item content analysis. PeerJ. 2020;8:e8643. 10.7717/peerj.8643.Search in Google Scholar PubMed PubMed Central
© 2024 the author(s), published by De Gruyter
This work is licensed under the Creative Commons Attribution 4.0 International License.
Articles in the same Issue
- Editorial Comment
- From pain to relief: Exploring the consistency of exercise-induced hypoalgesia
- Christmas greetings 2024 from the Editor-in-Chief
- Original Articles
- The Scandinavian Society for the Study of Pain 2022 Postgraduate Course and Annual Scientific (SASP 2022) Meeting 12th to 14th October at Rigshospitalet, Copenhagen
- Comparison of ultrasound-guided continuous erector spinae plane block versus continuous paravertebral block for postoperative analgesia in patients undergoing proximal femur surgeries
- Clinical Pain Researches
- The effect of tourniquet use on postoperative opioid consumption after ankle fracture surgery – a retrospective cohort study
- Changes in pain, daily occupations, lifestyle, and health following an occupational therapy lifestyle intervention: a secondary analysis from a feasibility study in patients with chronic high-impact pain
- Tonic cuff pressure pain sensitivity in chronic pain patients and its relation to self-reported physical activity
- Reliability, construct validity, and factorial structure of a Swedish version of the medical outcomes study social support survey (MOS-SSS) in patients with chronic pain
- Hurdles and potentials when implementing internet-delivered Acceptance and commitment therapy for chronic pain: a retrospective appraisal using the Quality implementation framework
- Exploring the outcome “days with bothersome pain” and its association with pain intensity, disability, and quality of life
- Fatigue and cognitive fatigability in patients with chronic pain
- The Swedish version of the pain self-efficacy questionnaire short form, PSEQ-2SV: Cultural adaptation and psychometric evaluation in a population of patients with musculoskeletal disorders
- Pain coping and catastrophizing in youth with and without cerebral palsy
- Neuropathic pain after surgery – A clinical validation study and assessment of accuracy measures of the 5-item NeuPPS scale
- Translation, contextual adaptation, and reliability of the Danish Concept of Pain Inventory (COPI-Adult (DK)) – A self-reported outcome measure
- Cosmetic surgery and associated chronic postsurgical pain: A cross-sectional study from Norway
- The association of hemodynamic parameters and clinical demographic variables with acute postoperative pain in female oncological breast surgery patients: A retrospective cohort study
- Healthcare professionals’ experiences of interdisciplinary collaboration in pain centres – A qualitative study
- Effects of deep brain stimulation and verbal suggestions on pain in Parkinson’s disease
- Painful differences between different pain scale assessments: The outcome of assessed pain is a matter of the choices of scale and statistics
- Prevalence and characteristics of fibromyalgia according to three fibromyalgia diagnostic criteria: A secondary analysis study
- Sex moderates the association between quantitative sensory testing and acute and chronic pain after total knee/hip arthroplasty
- Tramadol-paracetamol for postoperative pain after spine surgery – A randomized, double-blind, placebo-controlled study
- Cancer-related pain experienced in daily life is difficult to communicate and to manage – for patients and for professionals
- Making sense of pain in inflammatory bowel disease (IBD): A qualitative study
- Patient-reported pain, satisfaction, adverse effects, and deviations from ambulatory surgery pain medication
- Does pain influence cognitive performance in patients with mild traumatic brain injury?
- Hypocapnia in women with fibromyalgia
- Application of ultrasound-guided thoracic paravertebral block or intercostal nerve block for acute herpes zoster and prevention of post-herpetic neuralgia: A case–control retrospective trial
- Translation and examination of construct validity of the Danish version of the Tampa Scale for Kinesiophobia
- A positive scratch collapse test in anterior cutaneous nerve entrapment syndrome indicates its neuropathic character
- ADHD-pain: Characteristics of chronic pain and association with muscular dysregulation in adults with ADHD
- The relationship between changes in pain intensity and functional disability in persistent disabling low back pain during a course of cognitive functional therapy
- Intrathecal pain treatment for severe pain in patients with terminal cancer: A retrospective analysis of treatment-related complications and side effects
- Psychometric evaluation of the Danish version of the Pain Self-Efficacy Questionnaire in patients with subacute and chronic low back pain
- Dimensionality, reliability, and validity of the Finnish version of the pain catastrophizing scale in chronic low back pain
- To speak or not to speak? A secondary data analysis to further explore the context-insensitive avoidance scale
- Pain catastrophizing levels differentiate between common diseases with pain: HIV, fibromyalgia, complex regional pain syndrome, and breast cancer survivors
- Prevalence of substance use disorder diagnoses in patients with chronic pain receiving reimbursed opioids: An epidemiological study of four Norwegian health registries
- Pain perception while listening to thrash heavy metal vs relaxing music at a heavy metal festival – the CoPainHell study – a factorial randomized non-blinded crossover trial
- Observational Studies
- Cutaneous nerve biopsy in patients with symptoms of small fiber neuropathy: a retrospective study
- The incidence of post cholecystectomy pain (PCP) syndrome at 12 months following laparoscopic cholecystectomy: a prospective evaluation in 200 patients
- Associations between psychological flexibility and daily functioning in endometriosis-related pain
- Relationship between perfectionism, overactivity, pain severity, and pain interference in individuals with chronic pain: A cross-lagged panel model analysis
- Access to psychological treatment for chronic cancer-related pain in Sweden
- Validation of the Danish version of the knowledge and attitudes survey regarding pain
- Associations between cognitive test scores and pain tolerance: The Tromsø study
- Healthcare experiences of fibromyalgia patients and their associations with satisfaction and pain relief. A patient survey
- Video interpretation in a medical spine clinic: A descriptive study of a diverse population and intervention
- Role of history of traumatic life experiences in current psychosomatic manifestations
- Social determinants of health in adults with whiplash associated disorders
- Which patients with chronic low back pain respond favorably to multidisciplinary rehabilitation? A secondary analysis of a randomized controlled trial
- A preliminary examination of the effects of childhood abuse and resilience on pain and physical functioning in patients with knee osteoarthritis
- Differences in risk factors for flare-ups in patients with lumbar radicular pain may depend on the definition of flare
- Real-world evidence evaluation on consumer experience and prescription journey of diclofenac gel in Sweden
- Patient characteristics in relation to opioid exposure in a chronic non-cancer pain population
- Topical Reviews
- Bridging the translational gap: adenosine as a modulator of neuropathic pain in preclinical models and humans
- What do we know about Indigenous Peoples with low back pain around the world? A topical review
- The “future” pain clinician: Competencies needed to provide psychologically informed care
- Systematic Reviews
- Pain management for persistent pain post radiotherapy in head and neck cancers: systematic review
- High-frequency, high-intensity transcutaneous electrical nerve stimulation compared with opioids for pain relief after gynecological surgery: a systematic review and meta-analysis
- Reliability and measurement error of exercise-induced hypoalgesia in pain-free adults and adults with musculoskeletal pain: A systematic review
- Noninvasive transcranial brain stimulation in central post-stroke pain: A systematic review
- Short Communications
- Are we missing the opioid consumption in low- and middle-income countries?
- Association between self-reported pain severity and characteristics of United States adults (age ≥50 years) who used opioids
- Could generative artificial intelligence replace fieldwork in pain research?
- Skin conductance algesimeter is unreliable during sudden perioperative temperature increases
- Original Experimental
- Confirmatory study of the usefulness of quantum molecular resonance and microdissectomy for the treatment of lumbar radiculopathy in a prospective cohort at 6 months follow-up
- Pain catastrophizing in the elderly: An experimental pain study
- Improving general practice management of patients with chronic musculoskeletal pain: Interdisciplinarity, coherence, and concerns
- Concurrent validity of dynamic bedside quantitative sensory testing paradigms in breast cancer survivors with persistent pain
- Transcranial direct current stimulation is more effective than pregabalin in controlling nociceptive and anxiety-like behaviors in a rat fibromyalgia-like model
- Paradox pain sensitivity using cuff pressure or algometer testing in patients with hemophilia
- Physical activity with person-centered guidance supported by a digital platform or with telephone follow-up for persons with chronic widespread pain: Health economic considerations along a randomized controlled trial
- Measuring pain intensity through physical interaction in an experimental model of cold-induced pain: A method comparison study
- Pharmacological treatment of pain in Swedish nursing homes: Prevalence and associations with cognitive impairment and depressive mood
- Neck and shoulder pain and inflammatory biomarkers in plasma among forklift truck operators – A case–control study
- The effect of social exclusion on pain perception and heart rate variability in healthy controls and somatoform pain patients
- Revisiting opioid toxicity: Cellular effects of six commonly used opioids
- Letter to the Editor
- Post cholecystectomy pain syndrome: Letter to Editor
- Response to the Letter by Prof Bordoni
- Response – Reliability and measurement error of exercise-induced hypoalgesia
- Is the skin conductance algesimeter index influenced by temperature?
- Skin conductance algesimeter is unreliable during sudden perioperative temperature increase
- Corrigendum
- Corrigendum to “Chronic post-thoracotomy pain after lung cancer surgery: a prospective study of preoperative risk factors”
- Obituary
- A Significant Voice in Pain Research Björn Gerdle in Memoriam (1953–2024)
Articles in the same Issue
- Editorial Comment
- From pain to relief: Exploring the consistency of exercise-induced hypoalgesia
- Christmas greetings 2024 from the Editor-in-Chief
- Original Articles
- The Scandinavian Society for the Study of Pain 2022 Postgraduate Course and Annual Scientific (SASP 2022) Meeting 12th to 14th October at Rigshospitalet, Copenhagen
- Comparison of ultrasound-guided continuous erector spinae plane block versus continuous paravertebral block for postoperative analgesia in patients undergoing proximal femur surgeries
- Clinical Pain Researches
- The effect of tourniquet use on postoperative opioid consumption after ankle fracture surgery – a retrospective cohort study
- Changes in pain, daily occupations, lifestyle, and health following an occupational therapy lifestyle intervention: a secondary analysis from a feasibility study in patients with chronic high-impact pain
- Tonic cuff pressure pain sensitivity in chronic pain patients and its relation to self-reported physical activity
- Reliability, construct validity, and factorial structure of a Swedish version of the medical outcomes study social support survey (MOS-SSS) in patients with chronic pain
- Hurdles and potentials when implementing internet-delivered Acceptance and commitment therapy for chronic pain: a retrospective appraisal using the Quality implementation framework
- Exploring the outcome “days with bothersome pain” and its association with pain intensity, disability, and quality of life
- Fatigue and cognitive fatigability in patients with chronic pain
- The Swedish version of the pain self-efficacy questionnaire short form, PSEQ-2SV: Cultural adaptation and psychometric evaluation in a population of patients with musculoskeletal disorders
- Pain coping and catastrophizing in youth with and without cerebral palsy
- Neuropathic pain after surgery – A clinical validation study and assessment of accuracy measures of the 5-item NeuPPS scale
- Translation, contextual adaptation, and reliability of the Danish Concept of Pain Inventory (COPI-Adult (DK)) – A self-reported outcome measure
- Cosmetic surgery and associated chronic postsurgical pain: A cross-sectional study from Norway
- The association of hemodynamic parameters and clinical demographic variables with acute postoperative pain in female oncological breast surgery patients: A retrospective cohort study
- Healthcare professionals’ experiences of interdisciplinary collaboration in pain centres – A qualitative study
- Effects of deep brain stimulation and verbal suggestions on pain in Parkinson’s disease
- Painful differences between different pain scale assessments: The outcome of assessed pain is a matter of the choices of scale and statistics
- Prevalence and characteristics of fibromyalgia according to three fibromyalgia diagnostic criteria: A secondary analysis study
- Sex moderates the association between quantitative sensory testing and acute and chronic pain after total knee/hip arthroplasty
- Tramadol-paracetamol for postoperative pain after spine surgery – A randomized, double-blind, placebo-controlled study
- Cancer-related pain experienced in daily life is difficult to communicate and to manage – for patients and for professionals
- Making sense of pain in inflammatory bowel disease (IBD): A qualitative study
- Patient-reported pain, satisfaction, adverse effects, and deviations from ambulatory surgery pain medication
- Does pain influence cognitive performance in patients with mild traumatic brain injury?
- Hypocapnia in women with fibromyalgia
- Application of ultrasound-guided thoracic paravertebral block or intercostal nerve block for acute herpes zoster and prevention of post-herpetic neuralgia: A case–control retrospective trial
- Translation and examination of construct validity of the Danish version of the Tampa Scale for Kinesiophobia
- A positive scratch collapse test in anterior cutaneous nerve entrapment syndrome indicates its neuropathic character
- ADHD-pain: Characteristics of chronic pain and association with muscular dysregulation in adults with ADHD
- The relationship between changes in pain intensity and functional disability in persistent disabling low back pain during a course of cognitive functional therapy
- Intrathecal pain treatment for severe pain in patients with terminal cancer: A retrospective analysis of treatment-related complications and side effects
- Psychometric evaluation of the Danish version of the Pain Self-Efficacy Questionnaire in patients with subacute and chronic low back pain
- Dimensionality, reliability, and validity of the Finnish version of the pain catastrophizing scale in chronic low back pain
- To speak or not to speak? A secondary data analysis to further explore the context-insensitive avoidance scale
- Pain catastrophizing levels differentiate between common diseases with pain: HIV, fibromyalgia, complex regional pain syndrome, and breast cancer survivors
- Prevalence of substance use disorder diagnoses in patients with chronic pain receiving reimbursed opioids: An epidemiological study of four Norwegian health registries
- Pain perception while listening to thrash heavy metal vs relaxing music at a heavy metal festival – the CoPainHell study – a factorial randomized non-blinded crossover trial
- Observational Studies
- Cutaneous nerve biopsy in patients with symptoms of small fiber neuropathy: a retrospective study
- The incidence of post cholecystectomy pain (PCP) syndrome at 12 months following laparoscopic cholecystectomy: a prospective evaluation in 200 patients
- Associations between psychological flexibility and daily functioning in endometriosis-related pain
- Relationship between perfectionism, overactivity, pain severity, and pain interference in individuals with chronic pain: A cross-lagged panel model analysis
- Access to psychological treatment for chronic cancer-related pain in Sweden
- Validation of the Danish version of the knowledge and attitudes survey regarding pain
- Associations between cognitive test scores and pain tolerance: The Tromsø study
- Healthcare experiences of fibromyalgia patients and their associations with satisfaction and pain relief. A patient survey
- Video interpretation in a medical spine clinic: A descriptive study of a diverse population and intervention
- Role of history of traumatic life experiences in current psychosomatic manifestations
- Social determinants of health in adults with whiplash associated disorders
- Which patients with chronic low back pain respond favorably to multidisciplinary rehabilitation? A secondary analysis of a randomized controlled trial
- A preliminary examination of the effects of childhood abuse and resilience on pain and physical functioning in patients with knee osteoarthritis
- Differences in risk factors for flare-ups in patients with lumbar radicular pain may depend on the definition of flare
- Real-world evidence evaluation on consumer experience and prescription journey of diclofenac gel in Sweden
- Patient characteristics in relation to opioid exposure in a chronic non-cancer pain population
- Topical Reviews
- Bridging the translational gap: adenosine as a modulator of neuropathic pain in preclinical models and humans
- What do we know about Indigenous Peoples with low back pain around the world? A topical review
- The “future” pain clinician: Competencies needed to provide psychologically informed care
- Systematic Reviews
- Pain management for persistent pain post radiotherapy in head and neck cancers: systematic review
- High-frequency, high-intensity transcutaneous electrical nerve stimulation compared with opioids for pain relief after gynecological surgery: a systematic review and meta-analysis
- Reliability and measurement error of exercise-induced hypoalgesia in pain-free adults and adults with musculoskeletal pain: A systematic review
- Noninvasive transcranial brain stimulation in central post-stroke pain: A systematic review
- Short Communications
- Are we missing the opioid consumption in low- and middle-income countries?
- Association between self-reported pain severity and characteristics of United States adults (age ≥50 years) who used opioids
- Could generative artificial intelligence replace fieldwork in pain research?
- Skin conductance algesimeter is unreliable during sudden perioperative temperature increases
- Original Experimental
- Confirmatory study of the usefulness of quantum molecular resonance and microdissectomy for the treatment of lumbar radiculopathy in a prospective cohort at 6 months follow-up
- Pain catastrophizing in the elderly: An experimental pain study
- Improving general practice management of patients with chronic musculoskeletal pain: Interdisciplinarity, coherence, and concerns
- Concurrent validity of dynamic bedside quantitative sensory testing paradigms in breast cancer survivors with persistent pain
- Transcranial direct current stimulation is more effective than pregabalin in controlling nociceptive and anxiety-like behaviors in a rat fibromyalgia-like model
- Paradox pain sensitivity using cuff pressure or algometer testing in patients with hemophilia
- Physical activity with person-centered guidance supported by a digital platform or with telephone follow-up for persons with chronic widespread pain: Health economic considerations along a randomized controlled trial
- Measuring pain intensity through physical interaction in an experimental model of cold-induced pain: A method comparison study
- Pharmacological treatment of pain in Swedish nursing homes: Prevalence and associations with cognitive impairment and depressive mood
- Neck and shoulder pain and inflammatory biomarkers in plasma among forklift truck operators – A case–control study
- The effect of social exclusion on pain perception and heart rate variability in healthy controls and somatoform pain patients
- Revisiting opioid toxicity: Cellular effects of six commonly used opioids
- Letter to the Editor
- Post cholecystectomy pain syndrome: Letter to Editor
- Response to the Letter by Prof Bordoni
- Response – Reliability and measurement error of exercise-induced hypoalgesia
- Is the skin conductance algesimeter index influenced by temperature?
- Skin conductance algesimeter is unreliable during sudden perioperative temperature increase
- Corrigendum
- Corrigendum to “Chronic post-thoracotomy pain after lung cancer surgery: a prospective study of preoperative risk factors”
- Obituary
- A Significant Voice in Pain Research Björn Gerdle in Memoriam (1953–2024)

