Abstract
Background and aims
A previously undescribed mechanism of pain in the ulnar side of the hand was observed in a series of four patients. All were found to have a sensitive point in the first interspace of the hand and possible entrapment of a terminal branch of ulnar nerve piercing the fascia in the first interphalangeal webspace was suggested.
Methods
Pressure on the sensitive point reproduced the ulnar sided hand pain. Diagnostic and therapeutic injection of the mixture of local anesthetic and corticosteroid were performed. The degree and duration of relief of pain was noted.
Results
In individuals with recent onset hand pain of this type the injections abolished pain for 2 or more years. In individuals with long-standing pain (longer than 3–6 months) the pain was abolished for periods of time lasting several hours to several weeks. The correspondence of the point, where injections were done with acupuncture point LI4 was noted.
Conclusions
The location of possible nerve entrapment corresponds with an acupuncture point LI4 and may additionally represent a previously undescribed myofascial trigger point.
Implications
The suggested mechanism of ulnar sided hand pain represents a miniature chronic constriction injury similar to the animal model of neuropathic pain and may have relevance for regional pain elsewhere in the body.
1 Introduction
An episode of hand pain led to an observation a number of years ago by a right-handed pain management physician. Unprovoked pain had developed in the ulnar side of the left hand. The pain intensity reached scores of 7–8, where 10 is maximal pain. The pain was somewhat diffuse, but centered on the hypothenar eminence, and was of an unpleasant character. There were no sensory losses or paraesthesiae, but the grip strength appeared weakened with a sense of clumsiness of the hand. A detailed examination of all known sites of nerve entrapment was unremarkable, as was a search for described active myofascial trigger points (MTPs) known to refer pain into the hand.
A point was located in the first interspace on the radial aspect of the second metacarpal half way down the shaft (Fig. 1).
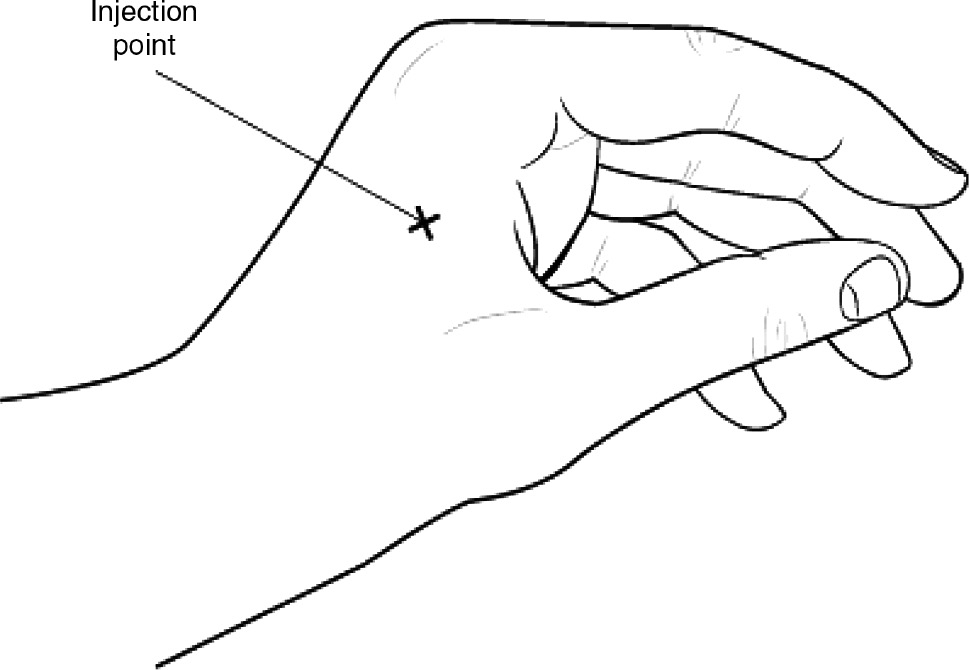
Location of the pain-producing point where injections were performed.
Pressure on this point caused intense reproduction of the ulnar pain. Injection of local anesthetic with low dose steroid (mixture of 2 mg bupivacaine, 2 mg lidocaine and 1 mg depo-methylprednisolone in 2 mL volume) into the point caused transient intense exacerbation of the pain, followed by complete resolution. This injection was performed on or about the 4th day after onset, and the pain did not recur till 2 years later, when it might have been provoked by prolonged holding of an anesthesia face mask. The same injection was performed, again with abolition of the pain; the pain has not recurred in the subsequent 14 years. This observation was used to advantage in a number of patients subsequently seen in the pain management practice.
2 Methods
2.1 Case reports
2.1.1 Case 1
Male, aged 32 when he first presented with bilateral ulnar sided hand pain. He was positive for HLA-B27 antigen (ankylosing spondylitis) and had severe chronic spinal pain with a number of MTPs in the paraspinal muscles. He was a semi-professional guitar-player and had been told to use exercise balls to “strengthen the grip” in an effort to treat the hand pain. This latter exercise appeared to worsen the condition. On examination he had intensely sensitive points in the location described above in both hands. They were injected as described, with transient (fraction of a second) intense pain followed by relief, which lasted 6–10 weeks. Over the next 7–8 years his hands were injected four to five times per year, each injection giving relief for several weeks. At no time did he have sensory problems and there was no evidence of dystonia.
2.1.2 Case 2
An obese 54-year old male was referred for treatment of chronic low back pain which was back dominant and caused by degenerative disease as well as multiple MTPs. He had recently been diagnosed with diabetes Type II. All relevant points were injected (paravertebral areas and paraspinal muscles) reducing the pain score from 7 to 0. On review 1 month later he stated his back had been much improved for 17–20 days. But he mentioned he had developed severe new pain in the ulnar side of his left hand and had been sent to see a neurologist, and had already undergone some tests. The left hand pain score was 9. On examination, the only painful point was the one in the first web-space as described above (Fig. 1). The point was injected as described, resulting in abolition of the hand pain. On review 1 month later the hand pain had not returned. He brought in results of the electrophysiological studies that had been performed at the university clinic prior to the injection. The results stated:
Abnormal study, in keeping with:
Moderate left median neuropathy at the level of the carpal tunnel.
Suspected mild length-dependent polyneuropathy (likely diabetic).
There is also some motor axonal loss in the left ulnar nerve territory, of uncertain significance. This study does not reveal focal ulnar nerve entrapment at the wrist or elbow.
2.1.3 Case 3
A 42 year-old woman was recently seen in consultation. She had multisite pain syndrome and reported she had had her carpal tunnels operated on twice in both hands and that a third procedure was scheduled to be performed on the left carpal tunnel due to persistent ulnar sided hand pain. She was found to have the same intensely sensitive point in the first web-space, upon injection of which her left hand pain was abolished. On follow-up via telephone she stated the left hand pain was gone for “several hours” and then it recurred. So she did undergo a third carpal tunnel surgery on the left hand. Electrophysiological studies were not repeated prior to this operation. There was no benefit to the left hand pain from the third surgery.
3 Diagnostics and treatment
Assessment of complaints of hand pain included questions about sensory losses or paraesthesiae, as well as clumsiness of the hand or subjective loss of grip strength. On examination, changes in skin color or temperature were sought (none noted), and testing for sensory changes was performed. Loss of muscle bulk in the intrinsic hand muscles could have been present in long-standing cases and objective loss of grip strength could also have been present but none of these changes were found in the above patients.
None of the patients were aware of the presence of the sensitive points, but their cooperation was required to determine the exact location. A pen with the ball-point retracted was used as a diagnostic tool. Firm pressure similar to that required to blanch a nail was required. Most patients gave very clear reactions, verbal or by “jumping” once pressure was applied to the correct point evoking “their” pain. A diagnostic injection was then performed (after informed consent). Electrophysiological studies were not required to diagnose the problem in these individuals since their pain was abolished by the diagnostic injections.
Injection of the mixture (containing 2 mg bupivacaine, 2 mg lidocaine and 1 mg depo-methylprednisolone in 2 mL volume) into the described point was done using a 27 gauge needle.
Low dose steroid added to the local anesthetic has empirically been found to prolong relief of injections into trigger points and entrapped nerves, so this combination of medications were used in these patients. This practice is supported by the findings by Shah et al. of inflammatory mediators in the dialysate of active trigger points [1].
Hand pain caused by the described mechanism was cured in individuals with pain of short duration. Individuals with long-standing pain had relief lasting a few hours to several weeks.
4 Discussion
The mechanism of ulnar sided hand pain described in these patients has not been previously described. This has led to misdiagnoses and counterproductive treatment strategies (Case 1), or to non-indicated and unhelpful surgical procedures (Case 3). The ease with which the problem can be diagnosed and treated underscores the tragedy of needless pain and dysfunction endured by these individuals.
The incidence of this type of pain needs to be determined in larger populations. The three cases described represent several others seen in our pain clinic. Some had long- standing pain similar to Case 1, and derived benefit of surprising duration from injections. Others had chronic pain elsewhere but developed “new” hand pain which was readily cured, similar to Case 2. Patients who have myofascial pain elsewhere may be more likely to develop this type of pain.
Hand and upper limb pain caused by nerve entrapments of median, ulnar and radial nerves or their branches represents a common complaint. When the complaint arises from entrapment of nerves at well-recognized locations such as the carpal or cubital tunnels, diagnoses and effective therapies are readily provided. Readers are referred to an online resource authored by a distinguished group of US clinicians/researchers [2]. This article updated in March 2016 describes all known entrapments of the three main nerves in the upper limb and their branches. A possible entrapment of the very distal ulnar nerve is not described. Morphological anatomical studies of the tissues at this point would be required to determine if this pain is due to actual nerve entrapment.
In the index case the pain was clearly felt in the ulnar area of the hand, hence the focus on entrapment relating to the ulnar nerve. Sensory branches join from the fifth and ulnar aspect of the fourth finger (see Fig. 2).
![Fig. 2:
Anatomical location of the distal ulnar nerve branches (drawn according to reference [3]).](/document/doi/10.1515/sjpain-2018-0090/asset/graphic/j_sjpain-2018-0090_fig_004.jpg)
Anatomical location of the distal ulnar nerve branches (drawn according to reference [3]).
The deep terminal branch of the ulnar nerve gives off motor branches to most intrinsic hand muscles in its course across the palm and the distal filaments pierce the fascia at about the point identified [3]. The nerve conduction and EMG study cited for Case 2 suggested non-specific abnormalities in motor axons of the ulnar nerve.
Several colleagues with knowledge of acupuncture noted that the location of the point identified, coincides with the hoku or Hegu point (LI4-WHO classification). Information on the morphology has been provided by Professor H. Heine, a German anatomist, who dissected the tissues surrounding this acupuncture point [4]. He described a nerve-vessel bundle piercing the fascia in this location. Branches of the ulnar as well as the median and radial nerves were included. From his illustration it appears the Hegu point corresponds closely to the point identified in the above patients [4].
In a previous study Heine had dissected four cadavers down to the fascia and found the points where microvascular bundles (all containing small branches of peripheral nerves) pierced the fascia, and determined that these locations corresponded to acupuncture points [5].
Adding information provided by Melzack et al. [6] demonstrating the co-localization of acupuncture points for pain and myofascial trigger points, it might appear that the described point is at once a well-known acupuncture point and a previously undescribed myofascial trigger point. Texts devoted to the subject of myofascial pain syndrome (MPS) and trigger points causing referred pain describe a number of points in the upper back, shoulder girdle and arms that can cause hand pain. Travell and Simons [7] pictured a superficially situated trigger point in the 1st dorsal interosseous muscle, which resembles Fig. 1 in our report [7]. However, the point described in our report is situated just ventral to this muscle. This observation of ours is supported by MRI imaging of the LI4 point, where the nerve-vessel bundle was found under the belly of the 1st dorsal interosseous muscle [8]).
Information on the mechanism of this pain, whether due to a trigger point or acupuncture point might be drawn from basic science. The first animal model of neuropathic pain, the chronic constriction injury (CCI) model was created by Bennett and Xie [9] by placing a loose ligature around the sciatic nerve in rats [9]. This caused pain that gradually involved the entire hind limb in the animals. (Questioned about the possible relevance to regional pain in humans Dr. Bennett did state that the chronic constriction injury mechanisms might cause pain involving “small no-name nerves” in humans, personal communication).
Combining the data on co-localization of trigger points with acupuncture points for pain and the morphology of acupuncture points, a hypothesis can be formulated, namely that these points represent miniature chronic constriction injuries, exacerbated by accidental lesions of small arteries of the hand [7]. Muscle injury or overuse can cause swelling of tissues sufficient to cause added compression on the neurovascular bundles where they pierce the fascia.
5 Conclusion
A previously undescribed mechanism of ulnar sided hand pain is presented, along with a very simple and effective mode of diagnosis and treatment. If injections are performed early on, cures can be induced. In patients whose pain has transitioned to chronicity prior to effective interventions, long periods of relief can still be induced using this method of treatment.
Beyond the simple description of a “new” cause for hand pain and its treatment, a discussion of pain mechanisms using information from the literature on acupuncture as well as Western medicine and basic science suggests a unifying mechanism with possible relevance for regional pain elsewhere in the body.
Acknowledgments
The authors thank Drs Vasco da Silva and Mary Redmond for careful review of the manuscript and the Studio N Graphic and Web Design, Peterborough, Ontario, for preparation of the figures.
-
Authors’ statements
-
Research funding: None.
-
Conflict of interest: None.
-
Informed consent: The three patients described gave specific written consent to have their cases described in this article.
-
Ethical approval: Not required for retrospective case series.
References
[1] Shah JP, Phillips TM, Danoff JV. An in vivo microanalytical technique for measuring the local biochemical milieu of human skeletal muscle. J Appl Physiol 2005;99:1977–84.10.1152/japplphysiol.00419.2005Search in Google Scholar PubMed
[2] Wilhelmi BJ, Neumeister M, Naffzinger R, Chang DW, Sudekum AE, Molnar JA. Nerve Compression Syndromes of the Hand. https://emedicine.medscape.com/article/1285531 .Search in Google Scholar
[3] Botte MJ, Cohen MS, Lavernia CJ, von Schroeder HP, Gellman H, Zinberg EM. The dorsal branch of the ulnar nerve: an anatomic study. J Hand Surg Am 1990;15:603–7.10.1016/S0363-5023(09)90022-3Search in Google Scholar
[4] Heine H. [Funktionelle Anatomie der Akupunkturpunkte Dickdarm 4 (LI4, Hegu) und Magen 36 (Ma 26, Zusanli)]. Dtsch Z Akupunktur 2001;44:168–75.10.1055/s-2001-17813Search in Google Scholar
[5] Heine H. Anatomical structure of acupoints. J Trad Chinese Med 1988;8:207–12.Search in Google Scholar
[6] Melzack R, Stillwell DM, Fox EJ. Trigger points and acupuncture points for pain: correlations and implications. Pain 1977;3: 3–23.10.1016/0304-3959(77)90032-XSearch in Google Scholar PubMed
[7] Travell JG, Simons DG. Myofascial pain and dysfunction. The trigger point manual. Baltimore: Williams and Wilkins, 1999;560.Search in Google Scholar
[8] Wong YM. An understanding of anatomy under the LI4 acupuncture point. Acupuncture Med 2013;31:333.10.1136/acupmed-2013-010371Search in Google Scholar PubMed
[9] Bennett GJ, Xie Y-K. A peripheral mononeuropathy in the rat that produces disorders of pain sensation like those seen in man. Pain 1988;33:87–108.10.1016/0304-3959(88)90209-6Search in Google Scholar PubMed
©2018 Scandinavian Association for the Study of Pain. Published by Walter de Gruyter GmbH, Berlin/Boston. All rights reserved.
Articles in the same Issue
- Frontmatter
- Editorial comment
- Support for mirror therapy for phantom and stump pain in landmine-injured patients
- Lifting with straight legs and bent spine is not bad for your back
- Bipolar radiofrequency neurotomy for spinal pain – a promising technique but still some steps to go
- Topical review
- Prevalence, localization, perception and management of pain in dance: an overview
- Clinical pain research
- Pain assessment in native and non-native language: difficulties in reporting the affective dimensions of pain
- Colored body images reveal the perceived intensity and distribution of pain in women with breast cancer treated with adjuvant taxanes: a prospective multi-method study of pain experiences
- Physiotherapy pain curricula in Finland: a faculty survey
- Mirror therapy for phantom limb and stump pain: a randomized controlled clinical trial in landmine amputees in Cambodia
- Pain and alcohol: a comparison of two cohorts of 60 year old women and men: findings from the Good Aging in Skåne study
- Prolonged, widespread, disabling musculoskeletal pain of adolescents among referrals to the Pediatric Rheumatology Outpatient Clinic from the Päijät-Häme Hospital District in southern Finland
- Impact of the economic crisis on pain research: a bibliometric analysis of pain research publications from Ireland, Greece, and Portugal between 1997 and 2017
- Measurement of skin conductance responses to evaluate procedural pain in the perioperative setting
- Original experimental
- An observational study of pain self-management strategies and outcomes: does type of pain, age, or gender, matter?
- Fibromyalgia patients and healthy volunteers express difficulties and variability in rating experimental pain: a qualitative study
- Effect of the market withdrawal of dextropropoxyphene on use of other prescribed analgesics
- Observational study
- Winning or not losing? The impact of non-pain goal focus on attentional bias to learned pain signals
- Gabapentin and NMDA receptor antagonists interacts synergistically to alleviate allodynia in two rat models of neuropathic pain
- Offset analgesia is not affected by cold pressor induced analgesia
- Central and peripheral pain sensitization during an ultra-marathon competition
- Reduced endogenous pain inhibition in adolescent girls with chronic pain
- Evaluation of implicit associations between back posture and safety of bending and lifting in people without pain
- Assessment of CPM reliability: quantification of the within-subject reliability of 10 different protocols
- Cerebrospinal fluid cutaneous fistula after neuraxial anesthesia: an effective treatment approach
- Pain in the hand caused by a previously undescribed mechanism with possible relevance for understanding regional pain
- The response to radiofrequency neurotomy of medial branches including a bipolar system for thoracic facet joints
- Letter to the Editor
- Diagnosis of carpal tunnel syndrome – implications for therapy
- Reply to the Letter to the Editor by Ly-Pen and Andréu
- Letter to the Editor regarding “CT guided neurolytic blockade of the coeliac plexus in patients with advanced and intractably painful pancreatic cancer”
- Reply to comments from Ulf Kongsgaard to our study
Articles in the same Issue
- Frontmatter
- Editorial comment
- Support for mirror therapy for phantom and stump pain in landmine-injured patients
- Lifting with straight legs and bent spine is not bad for your back
- Bipolar radiofrequency neurotomy for spinal pain – a promising technique but still some steps to go
- Topical review
- Prevalence, localization, perception and management of pain in dance: an overview
- Clinical pain research
- Pain assessment in native and non-native language: difficulties in reporting the affective dimensions of pain
- Colored body images reveal the perceived intensity and distribution of pain in women with breast cancer treated with adjuvant taxanes: a prospective multi-method study of pain experiences
- Physiotherapy pain curricula in Finland: a faculty survey
- Mirror therapy for phantom limb and stump pain: a randomized controlled clinical trial in landmine amputees in Cambodia
- Pain and alcohol: a comparison of two cohorts of 60 year old women and men: findings from the Good Aging in Skåne study
- Prolonged, widespread, disabling musculoskeletal pain of adolescents among referrals to the Pediatric Rheumatology Outpatient Clinic from the Päijät-Häme Hospital District in southern Finland
- Impact of the economic crisis on pain research: a bibliometric analysis of pain research publications from Ireland, Greece, and Portugal between 1997 and 2017
- Measurement of skin conductance responses to evaluate procedural pain in the perioperative setting
- Original experimental
- An observational study of pain self-management strategies and outcomes: does type of pain, age, or gender, matter?
- Fibromyalgia patients and healthy volunteers express difficulties and variability in rating experimental pain: a qualitative study
- Effect of the market withdrawal of dextropropoxyphene on use of other prescribed analgesics
- Observational study
- Winning or not losing? The impact of non-pain goal focus on attentional bias to learned pain signals
- Gabapentin and NMDA receptor antagonists interacts synergistically to alleviate allodynia in two rat models of neuropathic pain
- Offset analgesia is not affected by cold pressor induced analgesia
- Central and peripheral pain sensitization during an ultra-marathon competition
- Reduced endogenous pain inhibition in adolescent girls with chronic pain
- Evaluation of implicit associations between back posture and safety of bending and lifting in people without pain
- Assessment of CPM reliability: quantification of the within-subject reliability of 10 different protocols
- Cerebrospinal fluid cutaneous fistula after neuraxial anesthesia: an effective treatment approach
- Pain in the hand caused by a previously undescribed mechanism with possible relevance for understanding regional pain
- The response to radiofrequency neurotomy of medial branches including a bipolar system for thoracic facet joints
- Letter to the Editor
- Diagnosis of carpal tunnel syndrome – implications for therapy
- Reply to the Letter to the Editor by Ly-Pen and Andréu
- Letter to the Editor regarding “CT guided neurolytic blockade of the coeliac plexus in patients with advanced and intractably painful pancreatic cancer”
- Reply to comments from Ulf Kongsgaard to our study

