The association among fetal head position, fetal head rotation and descent during the progress of labor: a clinical study of an ultrasound-based longitudinal cohort study in nulliparous women
Abstract
Objectives
To elucidate the effects of the timing of fetal head rotation on the labor progress and outcomes.
Methods
A paired ultrasound measurement was performed at each of the three stages of labor: latency stage, active stage, and full-cervical-dilatation stage. The measurements included fetal head position, head-perineum distance (HPD) and the angle of progression (AOP).
Results
A total of 46 pregnancy women were included and a total of 102 effective measurements were collected. The cases in occipital anterior position were all eutocia. The rate of cesarean section in the left transverse occipital group was the highest (15.7 %, 3/19). There were 13 cases (37.1 %) with fetal head rotation occur during active phase, changing from occipital transverse to anterior. Ten cases (28.6 %) rotated in the second stage of labor. The average rotation degree of occipital transverse to anterior position was 62.6°. When AoP <95°, 100 % of the women were occipital transverse; When AoP ≥125°, 66.7 % was occipital anterior. The rate of oxytocin utilization and epidural analgesia in the occipital posterior group was higher than that in the other groups (71.4 and 85.7 %, respectively).
Conclusions
Occipital transverse is the most common fetal head position in the early stage of labor and fetal head rotation occurs mostly in the active phase and the second stage of labor. Sufficient time should be given in labor management for women that who tried vaginal delivery without contraindications.
Introduction
Fetal head position is a vital factor during labor. The continuous changing of fetal head position is an important indicator for the labor progress, and influencing decision-making for clinicians, especially for the prolonged or stagnant second stage of labor [1], 2]. Since Calkins et al. [3] reported his observation of the fetal head rotation during the labor, this phenomenon has been widely recognized in the clinical diagnosis and treatments. The determination of fetal head rotation was based on vaginal examination by obstetricians [4]. This method was simple and feasible, whereas, its accuracy had a great dependency on the experience of the performer with subtle subjective bias. The errors were inevitable, especially when fetal bone sutures overlap significantly. It has been postulated that the error rate of fetal head position via vaginal examination was as high as 68.5 % in the first stage of labor [5]. Besides, the frequent vaginal examination is a risk of amniotic cavity infection and we should avoid vaginal examinations by multiple healthcare professionals.
An increasing amount of evidence considered ultrasound might be a potent tool for determining fetal indexes during labor, not only for its objective and accuracy, but also for its learning course is much shorter than clinical examination [6], 7]. To date, the role of fetal head rotation via ultrasound on labor process and clinical decision making has not been clearly elucidated. In 2021, Hjartardóttir et al. [8] conducted a research on the fetal head rotation during the active phase of labor in primiparous women, and found that the proportion of occipital posterior position in the active phase was highest, reaching to 52.5 %. Recently, clinical practice guideline and recommendation by the World Association of Perinatal Medicine (WAPM) and the Perinatal Medicine Foundation (PMF) indicated that obstetricians could be competent in basic ultrasound techniques in order to recognize acute clinical emergencies as well as to improve the recognition of labor arrest [9].
Given the differences of pelvic types among Chinese and European women, it’s legitimate to pustulate that process of fetal head rotation during labor might be quite different in Chinese population. In this study, we aimed to characterize the process of fetal head rotation and its effects on the labor as well as pregnancy outcomes.
Subjects and methods
Study population and design
The study was approved by the Ethics Committee of the Nanjing Drum Tower Hospital (NO. 201717101) in accordance with the Declaration of Helsiniki. The retrospective study recruited nulliparous women who gave birth at Nanjing Drum Tower Hospital between 1 June 2021 and 31 August 2021. The inclusion criteria were: 1) Singleton primiparous women with head position; 2) gestation age of 37–41 weeks; 3) entering the labor process naturally or with labor induction; 4) presented a cervical dilation of 1∼6 cm at the first vaginal examination. The exclusive criteria were as follows: 1) multipara; 2) scarred uterus (women who had a history of cesarean section or myomectomy); 3) abnormal placental position; 4) abnormal fetal development; 5) multiple pregnancies; 6) stillbirth; 7) women with cervical dilation ≥6 cm during the first vaginal examination; 8) cognitive or intellectual impairment; 9) contraindications for vaginal delivery; 10) serious complications which may lead to cesarean section (such as preeclampsia, gestational diabetes mellitus, renal or heart disease, autoimmune diseases). All participants were informed of the experimental procedures and written informed consents were obtained. The procedures were blinded to the participant obstetrician and midwives.
Ultrasound measurement
Ultrasound measurements were performed at the latency stage (1 cm ≤cervical dilation <6 cm), active stage (cervical dilation ≥6 cm), and the first 15 min at the second stage of labor. Fetal head position, AOP and HPD were measured via transvaginal or/and transabdominal ultrasound. Fetal head position was determined using multiple indexes (including fetal spine, orbit, nasal bridge, eyeball, midline echo of the brain, and midline angle of the brain) as the previously published literature indicated [9]. In brief, fetal head position was divided into four groups according to the position of fetal brain midline: occiput anterior (OA: fetal brain midline at the area from 09:30 to 02:30 clockwise), left occiput transverse (LOT: fetal brain midline at the area from 02:30 to 03:30 clockwise), occiput posterior (OP: fetal brain midline at the area from 03:30 to 08:30 clockwise), and right occiput transverse (ROT: fetal brain midline at the area from 08:30 to 09:30 clockwise). The diagrammatic sketch was described previously and displayed in Figure 1.
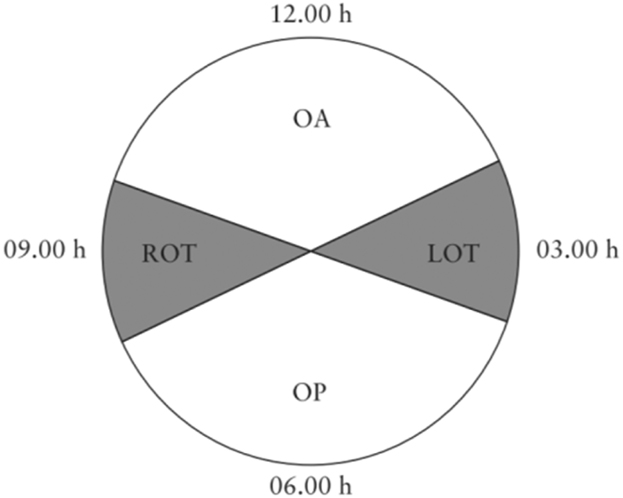
Schematic diagram of the clock dial for fetal position.
The standard AOP measurement should display the binary structure of the pubic symphysis with the maximum diameter and the lowest point of the skull cortex in the same section (Figure 2) [10], [11], [12]. Participants were encouraged to empty their bladder before measurement, and excessive residual urine detected by ultrasound would be catheterized if necessary. Ultrasound probe was placed at the pubic symphysis and pressed tightly against the vaginal opening at a longitudinal angle to obtain a standard section. A midsagittal image was obtained at the uterine contractions. Each patient was measured three times to take the average value. All the measurements were performed by two senior physicians, and images did not meet the standard were discarded.
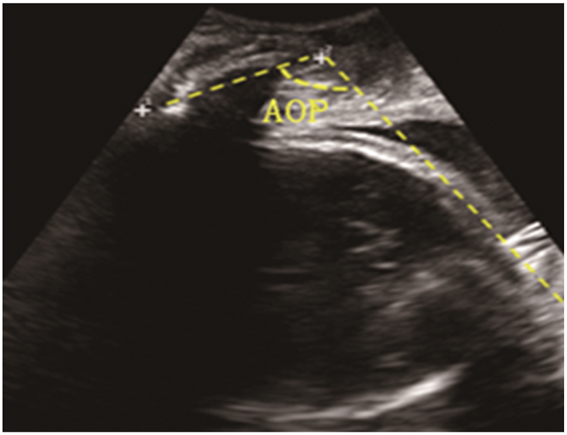
The standard image of angle of progression.
Statistical analysis
The statistical analysis was used by SPSS 18.0 software. Quantitative data were presented as mean±standard deviation (SD). Categorical variables, presenting percentages, were analyzed using Chi-square tests or Fisher exact tests. All p-values were two-sided, and p<0.05 was considered as significance.
Results
Characteristic of participants
During the observation and research period, a total of 75 pregnant women were recruited. Due to conflicts of doctors’ working hours, patients’ refusal to continue measuring, and loss of measurement data, a total of 46 pregnant women were ultimately included. Among them, 41 underwent vaginal delivery, four underwent cesarean section, and one underwent forceps delivery (Table 1). According to fetal head position at the first vaginal examination, 13 of them were in the OA group, 19 in the LOT group, 7 in the OP group, and 7 in the ROT group. Operations were only in the OP and LOT group, and the cesarean section rate was higher in the LOT group (15.7 %). OP group showed the highest rate of analgesia rate (71.4 %) and oxytocin usage rate (85.7 %). Moreover, the duration of labor was higher in the OP group compared to other groups. The newborn weight and postpartum hemorrhage in the OT group were slightly higher than those in the other two groups.
The characteristics of the pregnancy women based on the tire orientation during the first measurement.
| Fetal position, n | OA=13 | LOT=19 | OP=7 | ROT=7 |
|---|---|---|---|---|
| Pregnant women | ||||
| Age, year | 29 (28–31) | 30 (29–31) | 29 (28–30.5) | 29 (28–29) |
| BMI, kg/m2 | 27.1 (26.2–28.4) | 27.0 (24.4–29.2) | 27.6 (25.8–27.8) | 27.1 (25.8–27.8) |
| Oxytocin | 8 (61.5) | 11 (57.9) | 5 (71.4) | 3 (42.8) |
| Epidural analgesia | 6 (46.1) | 12 (63.1) | 6 (85.7) | 5 (71.4) |
| Gestational weeks, weeks | 39+6 (39+4∼40+6) | 39+1 (38+2∼39+6) | 39+5 (39+4∼39+6) | 39+4 (39+2∼40+4) |
| Natural labor | 6 (46.2) | 12 (63.2) | 5 (71.4) | 7 (100) |
| Induced labor | 7 (53.8) | 7 (36.8) | 2 (28.6) | 0 (0) |
| Neonate | ||||
| Birthweight, g | 3,360 (3,245–3,660) | 3,460 (3,165–3,575) | 3,250 (3,033–3,653) | 3,490 (3,388–3,745) |
| Apgar | 9–10 | 9–10 | 9–10 | 9–10 |
| pH in umbilical cord | 7.27 (7.26–7.30) | 7.30 (7.25–7.34) | 7.36 (7.30–7.36) | 7.29 (7.25–7.31) |
| Mode of delivery | ||||
| Cesarean section | 0 | 3 (15.7) | 1 (14.3) | 0 |
| Forceps delivery | 0 | 0 | 0 | 1 (14.3) |
| Eutocia | 13 (100) | 16 (84.2) | 6 (85.7) | 6 (85.7) |
| Blood loss after delivery, mL | 315 (230–450) | 400 (283–515) | 375 (325–555) | 580 (435–735) |
| Total stage of labor, min | 640 (435–943) | 531 (224–972) | 756 (387–1,108) | 590 (359–782) |
-
Data are presented as median (quartiles) or quantity (percentages). OA, occiput anterior; LOT, left occiput transverse; OP, occiput posterior; ROT, right occiput transverse.
The correlation of uterine orifice dilation and fetal head position
After eliminating the unsatisfied images, 102 valid data were obtained. A total of 97 data were obtained from 41 vaginal deliveries. Thirty six were at the latency stage, 32 were at the active stage and 29 were at the second stage of labor. According to the fetal head position detected at the uterine orifice dilation, occiput transverse position occupied the most part, with 38.9 % LOT and 19.4 % ROT (Table 2). At the active stage, more patients were presented with OA position and the percentage of OT position was decreased. As the uterine orifice dilated, AOP was increasing. While the HPD displayed a decreasing incline. The correlation of fetal head position, uterine orifice dilation, and the progress of labor were displayed in Figure 3.
Dilation of cervix and fetal head position in 41 cases of vaginal delivery.
| Dilation of cervix, cm | n | OA | LOT | OP | ROT | AOP° | HPD, cm | |
|---|---|---|---|---|---|---|---|---|
| Latency stage | 1 | 1 | – | – | – | 1 | 108.7 | 4.5 |
| 2 | 18 | 4 | 7 | 3 | 4 | 108.9 (93.8–121.9) | 4.4 (3.2–5.6) | |
| 3 | 10 | 3 | 2 | 2 | 4 | 108.9 (93.4–129.7) | 4.4 (3.6–5.4) | |
| 4 | 4 | 1 | 1 | 1 | 1 | 121.7 (106.3–137.7) | 3.3 (3.2–3.4) | |
| 5 | 3 | 1 | 2 | – | – | 115.8 (104.7–124.5) | 4.0 (3.75–4.4) | |
| Total | 36 | 9 (25) | 14 (38.9) | 6 (16.7) | 7 (19.4) | |||
| Active stage | 6 | 13 | 4 | 8 | 1 | – | 122.2 (100.3–148.8) | 3.64 (2.13–4.68) |
| 7 | 9 | 3 | 2 | 2 | 2 | 122.7 (98.8–141.6) | 3.36 (2.75–4.06) | |
| 8 | 9 | 4 | 1 | 2 | 2 | 128.8 (112.8–143.7) | 3.0 (1.51–3.85) | |
| 9 | 1 | – | – | 1 | – | 152.1 | 2.55 | |
| Total | 32 | 11 (34.3) | 11 (34.3) | 6 (18.6) | 4 (12.5) | |||
| Full-cervical-dilatation | 10 | 29 | 22 (75.9) | 2 (6.9) | 2 (6.9) | 3 (10.3) | 140.2 (113.7–169.8) | 2.6 (1.14–4.92) |
-
Data are expressed as quantity (percentage) and mean (minimum-maximum).
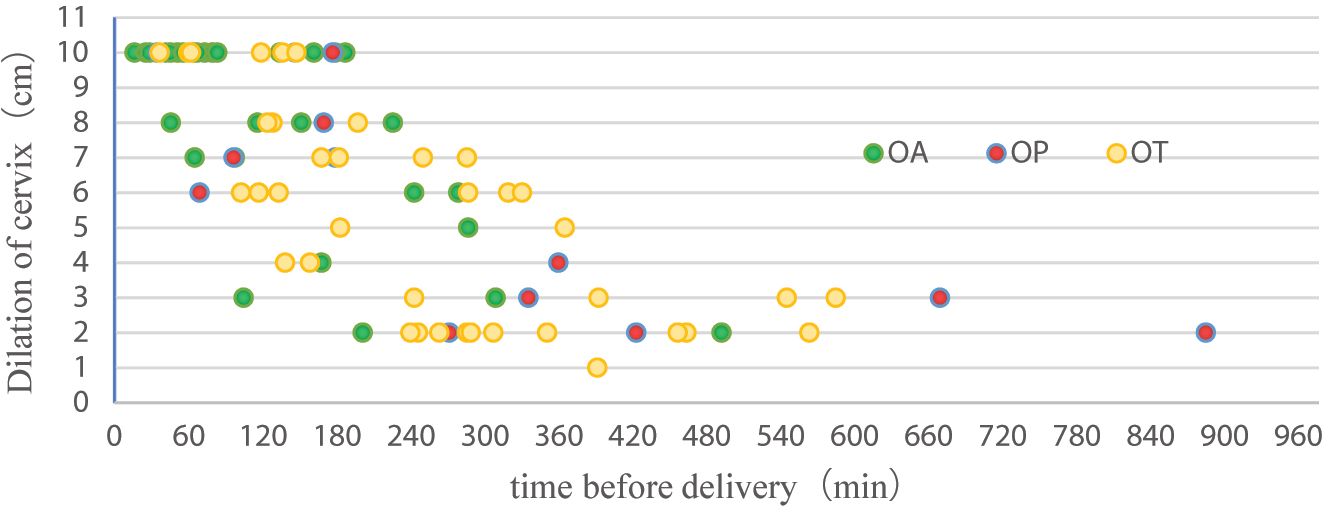
The relationship between fetal position, delivery time, and dilation of the cervix. The x-axis represents the delivery time, which is 0 and calculated in reverse from the delivery time. The y-axis represents dilation of the cervix (cm).
Fetal head rotation during labor
All data obtained during latency stage, active stage, fully opened uterine opening stages. To describe the rotation of the fetal head during the complete labor process, a descriptive analysis was conducted on 35 pregnant women who obtained measurement data during three periods. At the time of inclusion, the fetal orientation distribution was 6 cases in OP, 7 cases in OA, and 22 cases in OT. In the first stage of labor, 13 cases (13/22, 59.1 %) of OT rotated to OA, while all OP and 9 cases (41.9 %, 9/22) of OT did not rotate; In the second stage of labor, 5 cases underwent vaginal delivery after OP rotation to OA (including 3 cases of manual rotation of the fetal head), and one case underwent cesarean section due to persistent occipital posterior position; Among the 9 cases of OT that did not rotate during the first stage of labor, 5 cases rotated to OA during the second stage of labor, while the other 4 cases had OT. Two cases underwent cesarean section due to persistent occipital transverse position, one underwent manual rotation to OP position forceps for assisted delivery, and one underwent natural delivery. The average degree of rotation of the occipital lateral rotation is 62.6° in the occipital anterior position, with the highest rotation angle being 184.2°, occurring during LOT rotation to ROA. During the incubation stage, only 20 % of pregnant women have OA. After entering the second stage of labor, the proportion of OA increases to 85.7 %, mainly due to the rotation of OT towards OA. The rotation of OP occurs in the second stage of production (Table 3).
Fetal head rotation during the entire labor process (n=35).
| Latency stage | Active stage | Pregnancy outcomes | Rotation degree, ° | Additional remarks | ||||
|---|---|---|---|---|---|---|---|---|
| Fetal head position | n (%) | Fetal head position | n (%) | Fetal head position | n (%) | |||
| OP | 6 (17.1) | OP | 6 (17.1) | OP→OP | 1 (2.6) | Cesarean section | 20 | Surgical indication: persistent occipitoposterior |
| OA | 7 (20) | OP→OA | 5 | Eutocia | 100.0 (69.5–135.4) | 3 cases of manual fetal head rotation | ||
| OA→OA | 7 | OA→OA | 7 | Eutocia | 9.3 (1–24.3) | |||
| OT→OA | 13 | OT→OA | 18 | Eutocia | 62.6 (23.5–184.2) | 184.2° happened at LOT→ROA | ||
| Total | 20 (57.1) | Total | 30 (85.7) | |||||
| OT | 22 (62.9) | OT | 9 (25.7) | OT→OT | 3 (8.6) | Cesarean section (n=2), eutocia (n=1) | 7.9 (3–12.9) | Surgical indication: persistent occipitoposterior |
| OT→OP | 1 (2.6) | Forceps delivery | 88.1 | Secondary uterine atony during the second stage of labor, assisted with forceps delivery after manual transfer of the fetal head | ||||
-
“→” represented rotation. Data are expressed as quantity (percentage) and mean (minimum-maximum).
Fetal head rotation at different AOPs
In order to understand the relationship between fetal head descent and fetal orientation rotation, we described fetal orientation based on AOP angle. It was found that when AOP was less than 95°, all participants presented at OT position. When AOP was 95–124°, the proportion of OA increased, while OT still accounted for the most proportion of fetal position. When AOP was over 125°, OA becomes the main fetal position (Table 4).
Distribution of tire orientation at different AOP angles.
| Fetal head position | <95 (n=2) | 95–109 (n=23) | 110–124 (n=26) | ≥125 (n=45) |
|---|---|---|---|---|
| OA | 0 | 6 (26.1) | 6 (23.1) | 30 (66.7) |
| LOT | 2 (100) | 8 (34.8) | 12 (52.2) | 5 (11.1) |
| OP | 0 | 3 (13.0) | 6 (23.1) | 4 (8.9) |
| ROT | 0 | 6 (26.1) | 2 (7.7) | 6 (13.3) |
-
AOP, angle of progression. Data are expressed as quantity (percentage).
Discussion
This study aims to conduct an observational study characterizing the role of fetal head rotation of term postpartum primiparous women via ultrasound. In this study, we found that occipital transverse is the most common fetal head position in the early stage of labor and fetal head rotation occurs mostly in the active phase and the second stage of labor by ultrasound examination during the progress of labor. The most common situation is occipito-transverse to occipito-anterior. We should give enough time to pregnancy women who tried vaginal delivery without contraindications during labor management.
In a study conducted by the School of Medicine of the National University of Iceland in 2021, it was reported that 52.5 % of active postpartum women were in the occipital posterior position [8]. In this study, based on the observed fetal rotation during different stages of labor, the proportion of postpartum women in the occipital transverse position during the latency stage was the highest, of 62.9 %. At the active stage, occipital anterior position became the most common position, while the proportion of postpartum women in the active stage was only 16.2 %. The occipital transverse position is more commonly seen in the flat pelvis, while the occipital posterior position is more commonly seen in the male type pelvis. However, proportion of pelvis reported varies in different reports. Racial and the anatomical variation may responsible for the discrepancies in fetal orientation during the active stage.
From the perspective of fetal head rotation, more than half of the OT rotated to OA in the first stage of labor, and all OPs did not rotate. After entering the second stage of labor, five cases underwent vaginal delivery after rotating form OP to OA, of which three cases underwent manual rotation of the fetal head; More than half of OTs without rotation in the first stage of labor rotate into OA in the second stage. During the active stage, two postpartum women who underwent cesarean section due to labor process factors were OT, and one postpartum woman who underwent cesarean section in the second stage was OP. The majority non-OA pregnant women may undergo vaginal delivery after rotating to OA during the active phase and the second stage of labor. Therefore, the OT and OP positions in the first stage of labor should not be considered as positive signs themselves. Only sustained non-OA position may lead to delayed delivery and difficult labor. This is also consistent with previous clinical experience.
This study categorizes the fetal orientation of pregnant women into OA, LOT, OP, and ROT according to the four regions pattern of the clock chart (Figure 1). The proportion of LOT in women with occipital transverse position is higher than that of ROT, and the anatomical and physiological mechanisms of this phenomenon are not yet clear. However, from the perspective of delivery outcomes, the majority women with occipital transverse position can rotate to OA position during labor. Thus, further research is needed to determine whether L/ROT has an impact on delivery outcomes.
In addition to rotation, the descent of the fetal head is also an important factor determining the birth process, and AOP is a good ultrasound indicator that reflects the descent of the fetal head currently [10], [13], [14], [15]. Therefore, when measuring the fetal orientation, AOP values were obtained at the same time point and we attempted to describe the relationship between the fetal orientation and AOP. When the AOP value was 95–109°, only 26.1 % women were in the occipital anterior position. When the AOP value was ≥125°, 66.7 % women were in the occipital anterior position. These results fully demonstrated that the progression of the labor process was a continuous process with synchronous descent and rotation of the fetal head.
The advantage of this study lies in the exploratory use of ultrasound technology to accurately describe the process of fetal orientation rotation during labor, linking the timing of fetal head rotation with delivery outcome and AOP angle. This provides experience for the multidimensional exploration and application of ultrasound technology in labor, laying the foundation for future large-scale ultrasound research in labor, and has positive significance for ensuring delivery safety. In addition, although some literature reported that the progress of induced labor and natural labor were different [16], there was no difference in the management of the two groups after entering the labor process. Therefore, this study included both groups of women in the observation, and we believed that the observational data obtained from two gorups may have more reference significance for clinical practice.
This study also has certain limitations. Firstly, we did not evaluate the occiput spine angle (OSA) of fetuses in non-OP position and the chin to chest angle (CCA) of fetuses in OP position, which are important ultrasound indicators used to evaluate the flexion of the fetal head in the birth canal. The two indicators were associated with cesarean section causing by labor dystocia in women with prolonged active phase of labor [17]. Secondly, due to factors such as clinical work and maternal willingness, the selection of postpartum women is not continuous. Thirdly, the monitoring of the entire labor process is time-consuming, and continuous tracking requires a lot of manpower and time. This study attempts to conduct exploratory observational measurements without interfering with normal labor process management. The sample size is limited, and no statistical differences have been found between the baseline data of each group, making it impossible to conduct accurate statistical analysis. Further confirmation is needed from large-scale ultrasound related studies during labor.
-
Research ethics: The study was approved by the Ethics Committee of the Nanjing Drum Tower Hospital (NO. 201717101) in accordance with the Declaration of Helsiniki. All women provided written informed consent.
-
Informed consent: All women provided written informed consent.
-
Author contributions: JF performed the research and revised the paper. WW, ML and NG performed the data extraction and data analysis. All aspects of this research were supervised by YD. All authors have accepted responsibility for the entire content of this manuscript and approved its submission.
-
Use of Large Language Models, AI and Machine Learning Tools: None declared.
-
Conflict of interest: The authors state no conflict of interest.
-
Research funding: None declared.
-
Data availability: Not applicable.
References
1. Choi, SK, Park, YG, Lee da, H, Ko, HS, Park, IY, Shin, JC, et al.. Sonographic assessment of fetal occiput position during labor for the prediction of labor dystocia and perinatal outcomes. J Matern Fetal Neonatal Med 2016;29:3988–92. https://doi.org/10.3109/14767058.2016.1152250.Suche in Google Scholar PubMed
2. Haumonte, JB, Blanc, J, Castel, P, Mace, P, Auquier, P, d’Ercole, C, et al.. Uncertain fetal head engagement: a prospective randomized controlled trial comparing digital exam with angle of progression. Am J Obstet Gynecol 2022;227:625.e621–8. https://doi.org/10.1016/j.ajog.2022.04.018.Suche in Google Scholar PubMed
3. Calkins, LA. Occiput posterior presentation. Obstet Gynecol 1953;1:466–71.Suche in Google Scholar
4. Friedman, E. The graphic analysis of labor. Am J Obstet Gynecol 1954;68:1568–75. https://doi.org/10.1016/0002-9378(54)90311-7.Suche in Google Scholar PubMed
5. Shetty, J, Aahir, V, Pandey, D, Adiga, P, Kamath, A. Fetal head position during the first stage of labor: comparison between vaginal examination and transabdominal ultrasound. ISRN Obstet Gynecol 2014;2014:314617. https://doi.org/10.1155/2014/314617.Suche in Google Scholar PubMed PubMed Central
6. Malvasi, A, Marinelli, E, Ghi, T, Zaami, S. ISUOG Practice Guidelines for intrapartum ultrasound: application in obstetric practice and medicolegal issues. Ultrasound Obstet Gynecol 2019;54:421. https://doi.org/10.1002/uog.20399.Suche in Google Scholar PubMed
7. Wu, J, Lu, AD, Zhang, LP, Zuo, YX, Jia, YP. Study of clinical outcome and prognosis in pediatric core binding factor-acute myeloid leukemia. Zhonghua Xue Ye Xue Za Zhi 2019;40:52–7. https://doi.org/10.3760/cma.j.issn.0253-2727.2019.01.010.Suche in Google Scholar PubMed PubMed Central
8. Hjartardóttir, H, Lund, SH, Benediktsdottir, S, Geirsson, RT, Eggebo, TM. When does fetal head rotation occur in spontaneous labor at term: results of an ultrasound-based longitudinal study in nulliparous women. Am J Obstet Gynecol 2021;224:514.e511–9. https://doi.org/10.1016/j.ajog.2020.10.054.Suche in Google Scholar PubMed
9. Rizzo, G, Ghi, T, Henrich, W, Tutschek, B, Kamel, R, Lees, CC, et al.. Ultrasound in labor: clinical practice guideline and recommendation by the WAPM-World Association of Perinatal Medicine and the PMF-Perinatal Medicine Foundation. J Perinat Med 2022;50:1007–29. https://doi.org/10.1515/jpm-2022-0160.Suche in Google Scholar PubMed
10. Bibbo, C, Rouse, CE, Cantonwine, DE, Little, SE, McElrath, TF, Robinson, JN. Angle of progression on ultrasound in the second stage of labor and spontaneous vaginal delivery. Am J Perinatol 2018;35:413–20. https://doi.org/10.1055/s-0037-1608633.Suche in Google Scholar PubMed
11. Ghi, T, Conversano, F, Ramirez, ZR, Pisani, P, Dall’Asta, A, Lanzone, A, et al.. Novel artificial intelligence approach for automatic differentiation of fetal occiput anterior and non-occiput anterior positions during labor. Ultrasound Obstet Gynecol 2022;59:93–9. https://doi.org/10.1002/uog.23739.Suche in Google Scholar PubMed
12. Tang, H, Wang, W, Pan, Y, Liu, M, Shao, F, Xu, B, et al.. Process of fetal head descent as recorded by ultrasonography: how does this compare with the conventional first stage of labor? Int J Gynaecol Obstet 2022;156:28–33. https://doi.org/10.1002/ijgo.13605.Suche in Google Scholar PubMed
13. Kalache, KD, Duckelmann, AM, Michaelis, SA, Lange, J, Cichon, G, Dudenhausen, JW. Transperineal ultrasound imaging in prolonged second stage of labor with occipitoanterior presenting fetuses: how well does the ‘angle of progression’ predict the mode of delivery? Ultrasound Obstet Gynecol 2009;33:326–30. https://doi.org/10.1002/uog.6294.Suche in Google Scholar PubMed
14. Levy, R, Zaks, S, Ben-Arie, A, Perlman, S, Hagay, Z, Vaisbuch, E. Can angle of progression in pregnant women before onset of labor predict mode of delivery? Ultrasound Obstet Gynecol 2012;40:332–7. https://doi.org/10.1002/uog.11195.Suche in Google Scholar PubMed
15. Gillor, M, Vaisbuch, E, Zaks, S, Barak, O, Hagay, Z, Levy, R. Transperineal sonographic assessment of angle of progression as a predictor of successful vaginal delivery following induction of labor. Ultrasound Obstet Gynecol 2017;49:240–5. https://doi.org/10.1002/uog.15931.Suche in Google Scholar PubMed
16. Ostborg, TB, Romundstad, PR, Eggebo, TM. Duration of the active phase of labor in spontaneous and induced labors. Acta Obstet Gynecol Scand 2017;96:120–7. https://doi.org/10.1111/aogs.13039.Suche in Google Scholar PubMed
17. Dall’Asta, A, Rizzo, G, Masturzo, B, Morganelli, G, Di Pasquo, E, Schera, GBL, et al.. Intrapartum sonographic assessment of the fetal head flexion in protracted active phase of labor and association with labor outcome: a multicenter, prospective study. Am J Obstet Gynecol 2021;225:171.e1–12. https://doi.org/10.1016/j.ajog.2021.02.035.Suche in Google Scholar PubMed
© 2025 the author(s), published by De Gruyter, Berlin/Boston
This work is licensed under the Creative Commons Attribution 4.0 International License.
Artikel in diesem Heft
- Frontmatter
- Review
- Sex differences in lung function of adolescents or young adults born prematurely or of very low birth weight: a systematic review
- Original Articles – Obstetrics
- Shifts in peak month of births and socio-economic factors: a study of divided and reunified Germany 1950–2022
- The predictive role of serial transperineal sonography during the first stage of labor for cesarean section
- Gestational weight gain and obstetric outcomes in women with obesity in an inner-city population
- Placental growth factor as a predictive marker of preeclampsia in twin pregnancy
- Learning curve for the perinatal outcomes of radiofrequency ablation for selective fetal reduction: a single-center, 10-year experience from 2013 to 2023
- External validation of a non-invasive vaginal tool to assess the risk of intra-amniotic inflammation in pregnant women with preterm labor and intact membranes
- Placental fetal vascular malperfusion in maternal diabetes mellitus
- The importance of the cerebro-placental ratio at term for predicting adverse perinatal outcomes in appropriate for gestational age fetuses
- Comparing achievability and reproducibility of pulsed wave Doppler and tissue Doppler myocardial performance index and spatiotemporal image correlation annular plane systolic excursion in the cardiac function assessment of normal pregnancies
- Characteristics of the pregnancy and labour course in women who underwent COVID-19 during pregnancy
- Original Articles – Fetus
- Sonographic visualization and measurement of the fetal optic chiasm and optic tract and association with the cavum septum pellucidum
- The association among fetal head position, fetal head rotation and descent during the progress of labor: a clinical study of an ultrasound-based longitudinal cohort study in nulliparous women
- Fetal hypoplastic left heart syndrome: key factors shaping prognosis
- The value of ultrasound spectra of middle cerebral artery and umbilical artery blood flow in adverse pregnancy outcomes
- Original Articles – Neonates
- A family-centric, comprehensive nurse-led home oxygen programme for neonatal chronic lung disease: home oxygen policy evaluation (HOPE) study
- Effects of a respiratory function indicator light on visual attention and ventilation quality during neonatal resuscitation: a randomised controlled crossover simulation trial
- Short Communication
- Incidence and awareness of dysphoric milk ejection reflex (DMER)
Artikel in diesem Heft
- Frontmatter
- Review
- Sex differences in lung function of adolescents or young adults born prematurely or of very low birth weight: a systematic review
- Original Articles – Obstetrics
- Shifts in peak month of births and socio-economic factors: a study of divided and reunified Germany 1950–2022
- The predictive role of serial transperineal sonography during the first stage of labor for cesarean section
- Gestational weight gain and obstetric outcomes in women with obesity in an inner-city population
- Placental growth factor as a predictive marker of preeclampsia in twin pregnancy
- Learning curve for the perinatal outcomes of radiofrequency ablation for selective fetal reduction: a single-center, 10-year experience from 2013 to 2023
- External validation of a non-invasive vaginal tool to assess the risk of intra-amniotic inflammation in pregnant women with preterm labor and intact membranes
- Placental fetal vascular malperfusion in maternal diabetes mellitus
- The importance of the cerebro-placental ratio at term for predicting adverse perinatal outcomes in appropriate for gestational age fetuses
- Comparing achievability and reproducibility of pulsed wave Doppler and tissue Doppler myocardial performance index and spatiotemporal image correlation annular plane systolic excursion in the cardiac function assessment of normal pregnancies
- Characteristics of the pregnancy and labour course in women who underwent COVID-19 during pregnancy
- Original Articles – Fetus
- Sonographic visualization and measurement of the fetal optic chiasm and optic tract and association with the cavum septum pellucidum
- The association among fetal head position, fetal head rotation and descent during the progress of labor: a clinical study of an ultrasound-based longitudinal cohort study in nulliparous women
- Fetal hypoplastic left heart syndrome: key factors shaping prognosis
- The value of ultrasound spectra of middle cerebral artery and umbilical artery blood flow in adverse pregnancy outcomes
- Original Articles – Neonates
- A family-centric, comprehensive nurse-led home oxygen programme for neonatal chronic lung disease: home oxygen policy evaluation (HOPE) study
- Effects of a respiratory function indicator light on visual attention and ventilation quality during neonatal resuscitation: a randomised controlled crossover simulation trial
- Short Communication
- Incidence and awareness of dysphoric milk ejection reflex (DMER)

