Abstract
Objectives
Head to perineum distance (HPD) and angle of progression (AOP) are sonographic markers which have been investigated for the evaluation of labor progress. Here, we aimed to evaluate the predictive role of serially measured AOP and HPD during the first stage of labor in labor progress both in nulliparous and multiparous patients. Also, we firstly compared this role for labor progress.
Methods
This was a prospective longitudinal study including 299 patients. Patients were grouped as vaginal delivery (n=247) and cesarean section (n=52). Demographic and obstetric characteristics, HPD and AOP values, and vaginal examination findings were recorded and compared between groups.
Results
Slower changes in HPD and AOP values were detected in cesarean group. A HPD >38 mm predicted cesarean section with 86.9 % sensitivity and 59.2 % specificity (AUC=0.782, p<0.001) whereas AOP ≤117° predicted cesarean section with 93.5 % sensitivity and 65.1 % specificity in all patients (AUC=0.877, p<0.001). A HPD >37 mm predicted cesarean section with 84.2 % sensitivity and 55.2 % specificity (AUC=0.763, p<0.001) while AOP ≤110° predicted it with 82.7 % sensitivity and 73.3 % specificity in nulliparous patients (AUC=0.862, p<0.001). In multiparous patients, HPD>39 mm predicted cesarean section with 95.5 % sensitivity and 62.5 % specificity (AUC=0.824, p<0.001) and AOP ≤109° predicted cesarean section with 87.9 % sensitivity and 78.2 % specificity (AUC=0.909, p<0.001). AOP had superior predictive role than HPD in both nulliparous and multiparous groups (p<0.001 for both).
Conclusions
We suggest that differences in labor progress could be determined by using serial intrapartum sonography. However, more research is needed for the implementation of sonopartogram to the clinical obstetric practice.
Introduction
Labor dystosia, also defined as prolonged labor, is characterized by slow progression of labor [1]. It is tightly related to adverse perinatal outcomes such as instrumental delivery, fetal distress, increased cesarean section rates, postpartum bleeding, infection and mortality [2]. Digital vaginal examination is the gold standard way to evaluate labor progress. Fetal head descent, fetal head station, cervical effacement and dilatation could be assessed by digital examination. Unfortunately, it is a subjective and uncomfortable methods for patients and it increases the risk of ascending infection especially in premature rupture of membrane cases [3]. In a study of Rizzo et al. ultrasound examination was found to be a better tolerated method than vaginal examination for labor progress [4]. Considering this, intrapartum transperineal sonography has been investigated for the evaluation of labor progress. Although the use of sonography is not a standard practice, it could provide unbiased data about the progression of labor.
The abnormality in fetal head descent results in cesarean delivery. Thus, head to perineum distance (HPD) has claimed to be a marker for delivery mode and labor progress [5]. Head to perineum distance is defined as the distance between fetal skull and the perineum [6]. Another transperineal sonography marker is angle of progression (AOP). It is the angle from the maternal symphysis pubis to the leading part of the skull [1], 7]. In the literature, there has been studies searching the role of AOP and HPD in labor progress. In these studies, HPD and AOP has found to be correlated with fetal station and cervical dilatation findings in vaginal examination [8], [9], [10], [11]. These studies have also emphasized high interobserver correlation for HPD and AOP. However, they generally focused on single measurement, second stage of labor, and patient groups not classified as nulliparous and multiparous. In the present study, we aimed to evaluate the role of serially measured AOP and HPD in labor progress, assess the correlation of these markers with digital examination findings and determine these role both in nulliparous and multiparous patients. Also, we firstly compared the predictive role of HPD and AOP for labor progress.
Materials and methods
This was a prospective longitudinal study conducted at a university affiliated research and training hospital between November 2019 and January 2020. Institutional Ethical and Research Committee approved the present study with a decision number of 2011-KAEK-252019/10-16. The study was in accordance with the declaration of Helsinki. Written informed consent was obtained from all study participants.
Study population
In power analysis, the minimum number of patients to be included in the study was found to be 160 with 80 % power, 30 % difference and alfa value of 0.05. During the study period, 300 patients were enrolled to the study. The inclusion criteria were as follows: singleton pregnancy with a live fetus, being in the first stage of labor, having a baby with vertex presentation, who underwent induction of labor with intact membranes for various indications and being between 37 and 42 gestational week. The exclusion criteria were composed of having any contraindications to induction of labor, multiple pregnancies, having previous uterine surgery, suspicion of uterine rupture, abruptio of placenta and chorioamnionitis. After the selection due to the inclusion and exclusion criteria, a total of 299 patients were included and grouped as vaginal delivery group (n=247) and cesarean section group due to labor dystosia (n=52).
Patients characteristics such as age, weight, height, gravida, parity, gestational week, Bishop score, estimated fetal weight, birth weight, head circumference and Apgar scores were recorded and compared between groups. Body mass index (BMI) was calculated as dividing the weight to the square of height (kg/m2). Moreover, HPD, AOP and vaginal examination findings were recorded. Bishop score was evaluated at admission. Amniotomy followed by oxytocin was performed in patients with Bishop score >6 whereas 10 mg dinoprostone vaginal pessery was used for unfavorable cervix.
Sonographic measurement
Ultrasonographic measurements were performed by an obstetrician (E.K.) using a Voluson E8 (GE) ultrasonography device according to the WAPM Guideline [12]. Ultrasound probe was covered with sterile glove. Ultrasonographic measurements were made with the patient in the dorsal lithotomy position, with the hip and knee flexed at 45° and 90° angles, respectively, during uterine relaxation and with an empty bladder. First, the angle between the long axis of the symphysis pubis and the line extended from the lowest edge of the symphysis pubis tangential to the deepest part of the baby’s head was measured. This angle was defined as AOP [13]. Then, the probe was rotated 90° clockwise between the labia and placed on the posterior forchette. Light pressure was applied to compress the soft tissues against to pubic bone. The shortest distance between the most anterior outer border of the fetal skull and the perineum was measured and defined as HPD [14]. Both measurements were made three times and the averages were recorded. After ultrasonographic measurements, a classical vaginal examination was performed by the obstetrician of the delivery room unit and the cervical dilatation and fetal head station were recorded. Fetal head station was described between −5 and +5. In the follow-up of labor, patients underwent serial transperineal ultrasonography at 4-h intervals in latent phase. After ultrasonography, a classical vaginal examination was performed by the delivery room unit obstetrician. In the active phase, the patients’ ultrasonography measurements and examinations were repeated at 2-h intervals. The doctors who performed the ultrasonography measurements and the classical vaginal examination were completely unaware of each other’s measurements. Decisions regarding labor were made only by the delivery room unit obstetrician.
Statistical analysis
The normality assumption was evaluated with Shapiro Wilk test. For normally distributed variables, Independent two-sample t-test was used whereas Mann Whitney-U test was used for non-normally distributed variables for two group comparisons. Categorical data was compared with Fisher’s Exact Test and Pearson Chi-square tests. Descriptive statistics were shown as mean (standard deviation) and median (minimum–maximum) values for continuous variables while categorical variables were given with frequency and related percentages. For repeated measurements, generalized mixed effect model was used. To evaluate the role of AOP and HPD in the prediction cesarean section due to labor dystosia, a reciever operating characteristic analysis was performed for both multiparous and nulliparous patients. A p-value <0.05 was considered statistically significant. SPSS software version 22 was used in the statistical analysis.
Results
The sociodemographic and perinatal characteristics of patients were presented in Table 1. There was no significant difference between vaginal delivery and cesarean groups in terms of age, BMI, median gestational week, first and fifth minutes Apgar scores. The number of parity, the ratio of multiparous patients, BISHOP scores and duration of active phase were higher in vaginal delivery group. Estimated fetal weight, birth weight and head circumference were statistically significantly lower in vaginal delivery group.
The sociodemographic and perinatal characteristics of patients.
| Vaginal delivery (n=247) | Cesarean section (n=52) | p-Value | |
|---|---|---|---|
| Age, years | 24 (18–43) | 24 (18–45) | 0.610 |
| Body mass index, kg/m2 | 29 (21–39) | 28.5 (22–39) | 0.688 |
| Gestational week, week | 39 (37–42) | 39 (37–42) | 0.495 |
| Parity, n | 1 (0–6) | 0 (0–3) | <0.001 |
| Parity, n (%) | <0.001 | ||
| Nulliparous | 75 (30.4 %) | 37 (71.2 %) | |
| Multiparous | 172 (69.6 %) | 15 (28.8 %) | |
| Estimated fetal weight, g | 3,331.3±389.3 | 3,467.9±401.7 | 0.023 |
| BISHOP score | 5 (2–10) | 4 (0–9) | 0.007 |
| Birth weight, g | 3,270 (2,455–4,480) | 3,365 (2,230–4,380) | 0.034 |
| Head circumference, cm | 34 (24–37) | 35 (32–37) | 0.003 |
| First minutes Apgar scores | 9 (4–9) | 9 (7–9) | 0.799 |
| Fifth minutes Apgar scores | 10 (4–10) | 10 (9–10) | 0.700 |
-
p<0.05 was considered as statistically significant.
The serial measurements of HPD and AOP were presented in Table 2. Significant differences were found for each mesurement of HPD and AOP between vaginal delivery and cesarean groups. The chance in fetal head station, cervical dilatation, HPD and AOP were demonstrated in Figure 1. Delta values of head to perineum distance and angle of progression with the respect of first examination were presented in Table 3. There was significant difference between all measurements except ΔHPD1-2.
The serial measurements of head to perineum distance and angle of progression.
| Vaginal delivery | Cesarean section | p-Value | |
|---|---|---|---|
| HPD measurement 1, mm (nVD:247; nCS:52) |
46.91 | 53.6 | <0.001 |
| AOP measurement 1, ° (nVD:247; nCS:52) |
107.47 | 93.58 | <0.001 |
| HPD measurement 2, mm (nVD:243; nCS:51) |
39.97 | 49.47 | <0.001 |
| AOP measurement 2, ° (nVD:243; nCS:51) |
119.21 | 98.24 | <0.001 |
| HPD measurement 3, mm (nVD:207; nCS:40) |
33.8 | 46.63 | <0.001 |
| AOP measurement 3, ° (nVD:207; nCS:40) |
130.96 | 100.85 | <0.001 |
| HPD measurement 4, mm (nVD:148; nCS:30) |
30.28 | 45.17 | <0.001 |
| AOP measurement 4, ° (nVD:148; nCS:30) |
138.24 | 103.77 | <0.001 |
| HPD measurement 5, mm (nVD:92; nCS:18) |
27.58 | 42.89 | <0.001 |
| AOP measurement 5, ° (nVD:92; nCS:18) |
143.42 | 108.89 | <0.001 |
| HPD measurement 6, mm (nVD:47; nCS:8) |
25.47 | 41.5 | <0.001 |
| AOP measurement 6, ° (nVD:47; nCS:8) |
148.28 | 109.5 | <0.001 |
-
AOP, angle of progression; CS, cesarean section; HPD, head to perineum distance; VD, vaginal delivery. p<0.05 was considered as statistically significant.
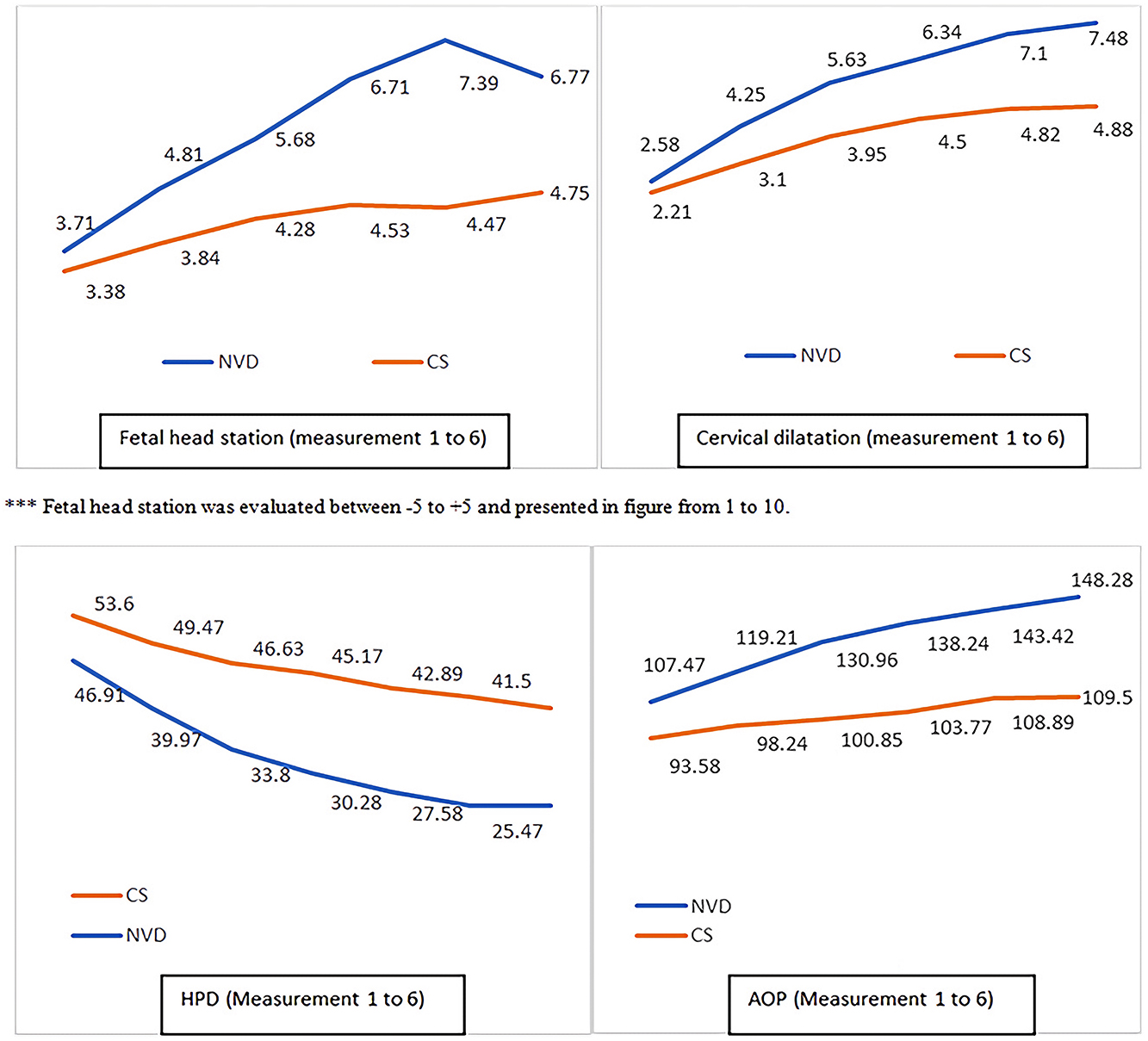
The chance in fetal head station, cervical dilatation, head to perineum distance and angle of progression. ***AOP, angle of progression; CS, cesarean section; HPD, head to perineum distance; NVD, vaginal delivery.
Delta values of head to perineum distance and angle of progression with the respect of first examination.
| Vaginal delivery | Cesarean section | p-Value | |
|---|---|---|---|
| ΔHPD1-2 (nVD:243; nCS:51) | −6 (−26:19) | −3 (−13:1) | 0.991 |
| ΔAOP1-2 (nVD:243; nCS:51) | 10 (−12:40) | 4 (−2:15) | 0.035 |
| ΔHPD1-3 (nVD:207; nCS:40) | −15 (−34:14) | −7 (−19:–1) | 0.045 |
| ΔAOP1-3 (nVD:207; nCS:40) | 24 (−12:58) | 7.5 (−92:32) | 0.001 |
| ΔHPD1-4 (nVD:148; nCS:30) | −21 (−42:0) | −9 (−23:–3) | 0.001 |
| ΔAOP1-4 (nVD:148; nCS:30) | 34 (3:63) | 11.5 (2–30) | <0.001 |
| ΔHPD1-5 (nVD:92; nCS:18) | −25.5 (−52:–2) | −15.5 (−24:–3) | <0.001 |
| ΔAOP1-5 (nVD:93; nCS:18) | 41 (4–79) | 14.5 (8–40) | <0.001 |
| ΔHPD1-6 (nVD:47; nCS:8) | −29 (−50:–4) | −17.5 (−20:–8) | <0.001 |
| ΔAOP1-6 (nVD:47; nCS:8) | 49 (7–87) | 16 (13–21) | <0.001 |
-
AOP, angle of progression; CS, cesarean section; HPD, head to perineum distance; VD, vaginal delivery. p<0.05 was considered as statistically significant.
In the correlation analysis using Spearman correlation coefficient, HPD was found to be inversely correlated with AOP (r=−0.839, p<0.001), cervical dilatation (r=−0.761, p<0.001) and head station (r=−0.761, p<0.001). Additionally, AOP was positively correlated with cervical dilatation (r=0.759, p<0.001) and head station (r=0.756, p<0.001) while it was negatively correlated with HPD (r=−0.839, p<0.001).
The predictive role of sonographic AOP and HPD for cesarean delivery in all patients was evaluated with receiver operating curve analysis and presented in Figure 2. Head perineum distance >38 mm was found to predict cesarean section with 86.9 % sensitivity and 59.2 % specificity (AUC=0.782, p<0.001). Angle of progression ≤117° was found to predict cesarean section with 93.5 % sensitivity and 65.1 % specificity (AUC=0.877, p<0.001). The predictive role of HPD and AOP in all patients was compared and AOP had superior predictive role than HPD (p<0.001).
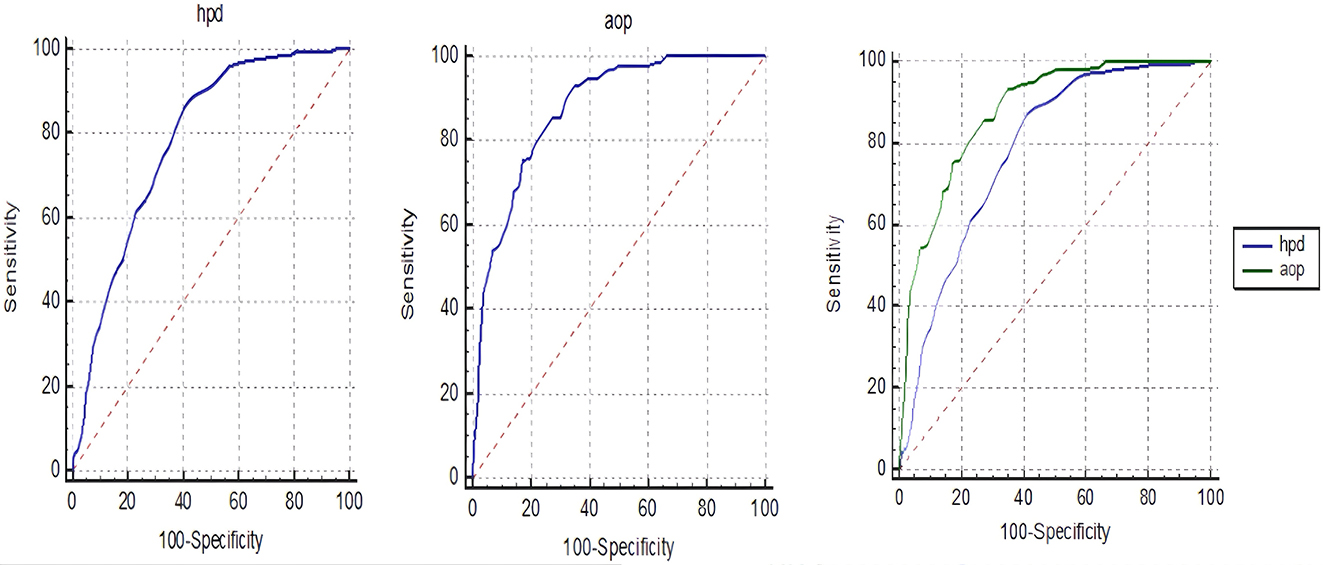
Receiver operating curve analysis evaluating the predictive role of angle of progression and head to perineum distance for cesarean delivery in all patients. AOP, angle of progression; HPD, head to perineum distance.
The predictive role of sonographic AOP and HPD for cesarean delivery in nulliparous patients was evaluated with receiver operating curve analysis and presented in Figure 3. Head perineum distance >37 mm was found to predict cesarean section with 84.2 % sensitivity and 55.2 % specificity (AUC=0.763, p<0.001). Angle of progression ≤110° was found to predict cesarean section with 82.7 % sensitivity and 73.3 % specificity (AUC=0.862, p<0.001). The predictive role of HPD and AOP in nulliparous patients was compared and AOP had superior predictive role than HPD (p<0.001).
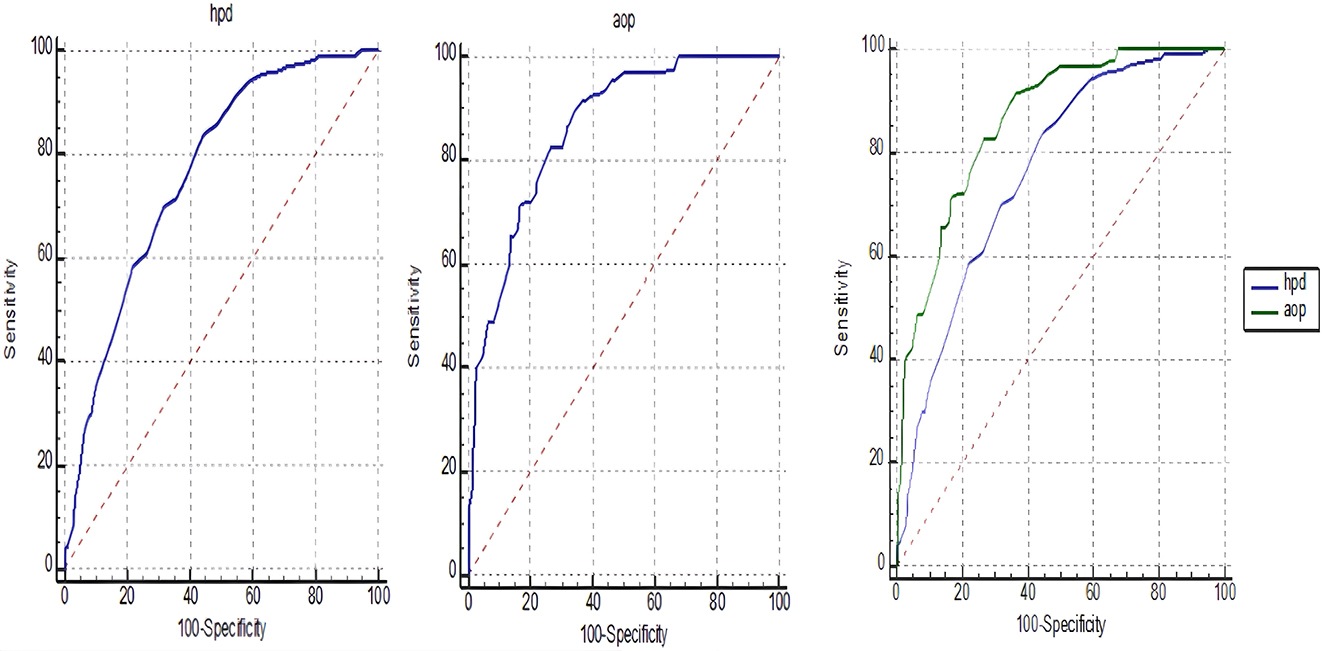
Receiver operating curve analysis evaluating the predictive role of angle of progression and head to perineum distance for cesarean delivery in nulliparous patients. AOP, angle of progression; HPD, head to perineum distance.
The predictive role of sonographic AOP and HPD for cesarean delivery in multiparous patients was evaluated with receiver operating curve analysis and presented in Figure 4. Head perineum distance >39 mm was found to predict cesarean section with 95.5 % sensitivity and 62.5 % specificity (AUC=0.824, p<0.001) in multiparous patients while AOP ≤109° was found to predict cesarean section with 87.9 % sensitivity and 78.2 % specificity (AUC=0.909, p<0.001). The predictive role of HPD and AOP in multiparous patients was compared and AOP had superior predictive role than HPD (p<0.001).
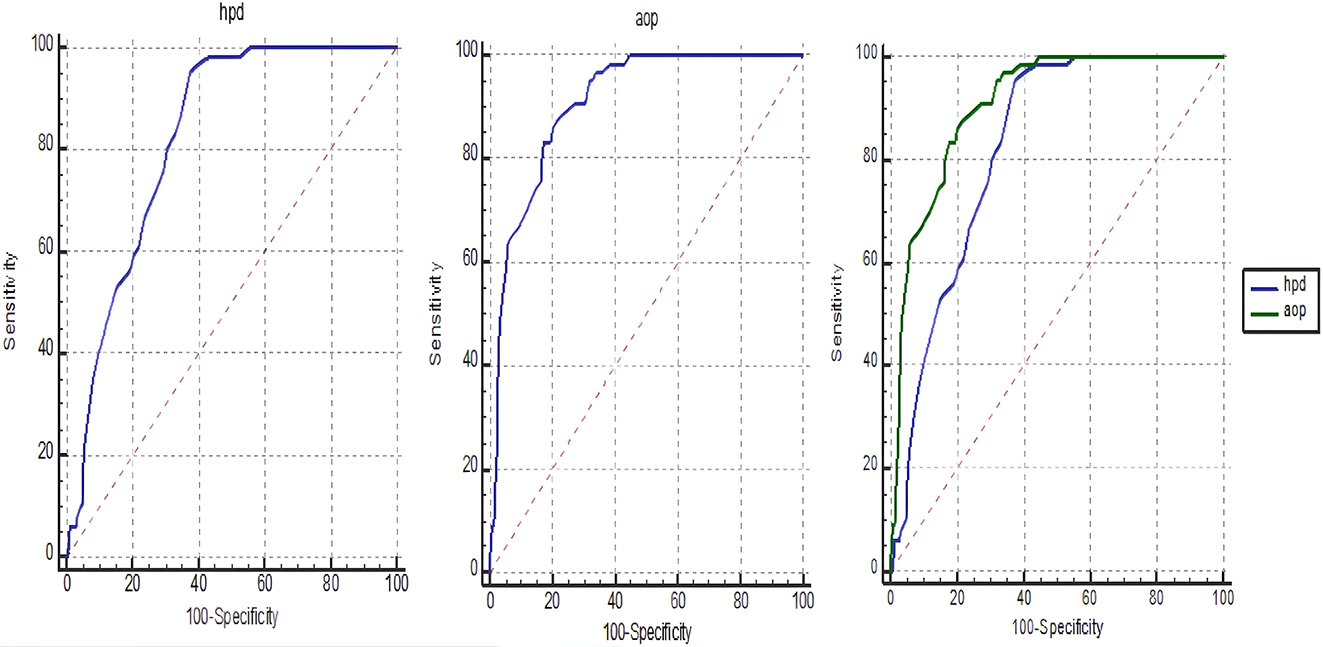
Receiver operating curve analysis evaluating the predictive role of angle of progression and head to perineum distance for cesarean delivery in multiparous patients. AOP, angle of progression; HPD, head to perineum distance.
Discussion
Integration of sonography on the labor ward for routine obstetric practice may be an alternative way to overcome various obstacles in obstetrics. Mappa et al. claimed that intrapartum sonography was related to decreased rate of incorrect diagnosis of fetal head station and position [15]. The first approach known as sonopartogram was first introduced in 2014 by Hassan et al. [8]. After this, many studies searching the role of sonography in labor progress have been performed. Sonographic cervical dilatation, AOP, HPD and head to symphysis distance were some of the sonographic parameters used in the evaluation of labor progress.
HPD is the simple method evaluating the fetal head descent [16]. In a study of Horst et al. higher HPD was related to cesarean section and a unit increase in HPD was found to be associated with 39.63 % decrease in vaginal delivery rate [17]. In a European study searching the role of HPD in vacuum extraction, patients with HPD ≤25 mm had significantly shorter extraction time and patients with HPD ≤35 mm had significantly lower cesarean section rates [18]. In another study, HPD 55 mm predicted vaginal delivery with 97 % sensitivity and 88.1 % specificity [19]. Kasbaoui et al. claimed that HPD ≥40 mm in the second stage of labor is associated with difficult instrumental delivery [20]. Moreover, Dall’Asta et al. reported that short HPD obtained in the second stage of labor is related to spontaneous vaginal delivery [21].
Another parameter showing the fetal head descent is AOP. When the AOP increases, fetal head descent increases during labor. In previous studies, AOP was shown to be a predictor for successful vacuum delivery in occiput anterior position and forceps delivery for non-occiput posterior fetuses [14], 22], 23]. Furthermore, AOP was significantly higher in spontaneous vaginal delivery group as compared to vacuum extraction or cesarean delivery group [24]. The studies searching the cut-off levels for AOP in the literature could be classified according to the parity and stage of labor. Bulut et al. evaluated AOP in first stage of labor in multiparous and nulliparous patients and found that AOP >132.3° predicted vaginal birth with 70 % sensitivity and 75 % specificity [25]. Similarly Vinod et al. reported a degree of AOP as ≥89 with 79.3 % sensitivity and 65.6 specificity [26]. Kandil et al. evaluated AOP in the first stage of labor in only nulliparous patients and found that AOP >104° predicted vaginal birth with 90 % sensitivity and 86 % specifity [27]. Likewise, Elkadi et al. and Ibrahim et al. reported an AOP level ≥97 and >107.5° in the first stage of labor respectively [28], 29].
Barbera et al. evaluated AOP in the second stage of labor in both multiparous and nulliparous patients and reported that all patients delivered vaginally when AOP exceeds 120° [7]. Yonetani et al. claimed that second stage AOP ≥160° predicted vaginal birth in nulliparous patients with 42.6 % sensitivity and 88.1 % specificity while AOP ≥150° predicted vaginal birth in multiparous patients with 51.8 % sensitivity and 78.6 % specificity [30]. Malik et al. assessed only nulliparous patients and claimed that AOP >116° predicted vaginal delivery with 96.49 % sensitivity and 96.43 % specificity [31]. Similarly, Hadad et al. reported 71.6 % sensitivity and 83.7 % specificity for AOP levels above 138° in nulliparous patients at second stage of labor [32]. In a systematic review searching eight studies reported that AOP between 108 and 119° at the beginning of second stage predicted vaginal delivery with 94 % sensitivity and 47 % specificity [33].
Many authors have focused on using AOP and HPD in previous studies. In a study of Eggobo et al., half of the women who had HPD >40 mm or AOP <110° delivered vaginally. This study reported 0.68 AUC (95 % CI, 0.55–0.80) for AOP and 0.67 AUC (95 % CI, 0.55–0.80) for HPD for spontaneous delivery. The likelihood of cesarean delivery was found to be 7 % when HPD is <40 mm whereas it increases up to 82 % when HPD is >50 mm. Likewise, the likelihood of cesarean delivery was 12 % for AOP >110° while it rose up 62 % for AOP <100° [34]. Hadad et al. found wider AOP and shorter HPD levels in the second stage of labor in spontaneous vaginal delivery [32]. Carvalho Neto showed that second stage AOP levels 129.9° and HPD levels 43 mm predicted vaginal delivery [5]. In contrast to these studies, Mitta et al. found no difference according to AOP levels between vaginal delivery, instrumental delivery and cesarean section groups. HPD values were different between vaginal and cesarean delivery groups and operative deliveries and cesarean delivery groups. Also, this study clarified that negative correlation was present between AOP and parity while HPD was positively correlated with BMI [14].
In the literature, only a few studies have focused on serial measurements of sonographic parameters for evaluating labor progress. In a study of Lee et al. 100 women between 37 and 41+6 weeks of gestation were assessed and slower change in parasagittal AOP and HPD were reported in cesarean section group. Moreover, cesarean group had higher estimated marginal mean of HPD and lower parasagittal AOP levels. In this study, measurements were taken in the first stage of labor serially but no cut-off value for cesarean section was obtained [35]. Another study using serial transperineal sonography in early labor included 183 nulliparous women and reported the feasibility of transperineal sonography for obstructed labor in early active phase [36]. Tse et al. evaluated 315 women in the first stage of labor. In this study, parity and obesity were found to effect ultrasound determined labor progress. Serial measurements of parasagittal AOP achieved a sensitivity of 80 % and specificity of 80 % for the prediction of cesarean delivery due to labor dystosia. This study evaluated parasagittal AOP and HPD per unit change of head station and cervical dilatation [1]. In the present study, we performed serial measurement of HPD and AOP. Consistent with the literature, we demonstrated slower changes in HPD and AOP values in cesarean section group. In our study, HPD >38 mm predicted cesarean delivery with 86.9 % sensitivity and 59.2 % specificity while AOP ≤117° predicted with 93.5 % sensitivity and 65.1 % specifity. Different from other studies, we compared the predictive role of these markers and found that AOP was superior than HPD in predicting cesarean delivery.
Another issue about sonographic parameters is the correlation of sonographic parameters with vaginal digital examination findings. In a study of Sweed et al. strong association were reported for cervical dilatation, moderate correlation for fetal head position and head station determined by HPD [3]. Similarly, Tse et al. reported positive correlation between parasagittal AOP and fetal head station or cervical dilatation whereas negative correlation was present between HPD and fetal head station or cervical dilatation [1]. HPD has known to be moderately correlated with digital vaginal examination head descent [8]. We found negative strong correlation between HPD and cervical dilatation or head station while AOP had strong positive association between cervical dilatation or head station.
The factors effecting fetal head descent determined by HPD and AOP was evaluated in the study of Chaemsaithong et al. [37]. Multiparity was found to be associated with faster head descent while obesity was related to slower fetal descent and higher HPD values. In our study, we classified according to parity and found different cut-off levels for multiparous and nulliparous patients supporting this finding. A HPD >39 mm predicted cesarean delivery with 95.5 % sensitivity and 62.5 % specificity while AOP ≤109° predicted with 87.9 % sensitivity and 78.2 % specifity in multiparous patients. In nulliparous patients, HPD >37 mm predicted cesarean delivery with 84.2 % sensitivity and 55.2 % specificity while AOP ≤110° predicted with 82.7 % sensitivity and 73.3 % specificity. The predictive role of AOP was superior than HPD in predicting cesarean delivery both in multiparous and nulliparous patients.
Strengths of the study include longitudinal design with serial sonographic measurements. Although interobserver variability is low, single sonographer performed all measurements in the present study. The study has larger sample size as compared to other repeated measurement studies. Blindness of clinicians and researchers minimized the bias. We classified patients as multiparous and nulliparous and suggested cut-off levels for cesarean section for each group.
This study also has some limitations. First, the findings could not be generalizable. Second, only term cases were included. Last, the results were limited to only Turkish patients.
In conclusion, we suggest that differences in labor progress could be determined by using serial intrapartum transperineal sonography. However, more research is needed for the implementation of sonopartogram to the clinical obstetric practice.
-
Research ethics: Institutional Ethical and Research Committee (Bursa Yuksek Ihtisas Research and Training Hospital) approved the present study with a decision number of 2011-KAEK-252019/10–16. This study was conducted in accordance with the Declaration of Helsinki.
-
Informed consent: Informed consent was obtained from all individuals included in this study, or their legal guardians or wards.
-
Author contributions: All authors have accepted responsibility for the entire content of this manuscript and approved its submission.
-
Use of Large Language Models, AI and Machine Learning Tools: None declared.
-
Conflict of interest: The authors state no conflict of interest.
-
Research funding: None declared.
-
Data availability: The datasets generated and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
1. Tse, WT, Chaemsaithong, P, Chan, WWY, Kwan, AHW, Huang, J, Appiah, K, et al.. Labor progress determined by ultrasound is different in women requiring cesarean delivery from those who experience a vaginal delivery following induction of labor. Am J Obstet Gynecol 2019;221:335.e1–18. https://doi.org/10.1016/j.ajog.2019.05.040.Search in Google Scholar PubMed
2. Karampas, G, Witkowski, M, Metallinou, D, Steinwall, M, Matsas, A, Panoskaltsis, T, et al.. Delivery progress, labor interventions and perinatal outcome in spontaneous vaginal delivery of singleton pregnancies between nulliparous and primiparous women with one previous elective cesarean section: a retrospective comparative study. Life 2023;13:2016. https://doi.org/10.3390/life13102016.Search in Google Scholar PubMed PubMed Central
3. Sweed, MS, Allam, IF, Ashoush, SA, Marwan, OA, NasrElDin, EA. Sonopartogram versus conventional partogram for monitoring progress of labor: a prospective observational study Egypt. J Radiol Nucl Med 2020;51:1–7.10.1186/s43055-020-00295-ySearch in Google Scholar
4. Rizzo, G, Aloisio, F, Bacigalupi, A, Mappa, I, Słodki, M, Makatsarya, A, et al.. Women’s compliance with ultrasound in labor: a prospective observational study. J Matern Fetal Neonatal Med 2021;34:1454–8. https://doi.org/10.1080/14767058.2019.1638903.Search in Google Scholar PubMed
5. Carvalho Neto, RH, Viana Junior, AB, Moron, AF, Araujo Júnior, E, Carvalho, FHC, Feitosa, HN. Assessment of the angle of progression and distance perineum-head in the prediction of type of delivery and duration of labor using intrapartum ultrasonography. J Matern Fetal Neonatal Med 2021;34:2340–8. https://doi.org/10.1080/14767058.2019.1666818.Search in Google Scholar PubMed
6. Eggebø, TM, Heien, C, Økland, I, Gjessing, LK, Romundstad, P, Salvesen, KA. Ultrasound assessment of fetal head-perineum distance before induction of labor. Ultrasound Obstet Gynecol 2008;32:199–204. https://doi.org/10.1002/uog.5360.Search in Google Scholar PubMed
7. Barbera, AF, Pombar, X, Perugino, G, Lezotte, DC, Hobbins, JC. A new method to assess fetal head descent in labor with transperineal ultrasound. Ultrasound Obstet Gynecol 2009;33:313–9. https://doi.org/10.1002/uog.6329.Search in Google Scholar PubMed
8. Hassan, WA, Eggebø, T, Ferguson, M, Gillett, A, Studd, J, Pasupathy, D, et al.. The sonopartogram: a novel method for recording progress of labor by ultrasound. Ultrasound Obstet Gynecol 2014;43:189–94. https://doi.org/10.1002/uog.13212.Search in Google Scholar PubMed
9. Dückelmann, AM, Bamberg, C, Michaelis, SA, Lange, J, Nonnenmacher, A, Dudenhausen, JW, et al.. Measurement of fetal head descent using the ‘angle of progression’ on transperineal ultrasound imaging is reliable regardless of fetal head station or ultrasound expertise. Ultrasound Obstet Gynecol 2010;35:216–22. https://doi.org/10.1002/uog.7521.Search in Google Scholar PubMed
10. Molina, FS, Terra, R, Carrillo, MP, Puertas, A, Nicolaides, KH. What is the most reliable ultrasound parameter for assessment of fetal head descent? Ultrasound Obstet Gynecol 2010;36:493–9. https://doi.org/10.1002/uog.7709.Search in Google Scholar PubMed
11. Kwan, AHW, Chaemsaithong, P, Tse, WT, Appiah, K, Chong, KC, Leung, TY, et al.. Feasibility, reliability, and agreement of transperineal ultrasound measurement: results from a longitudinal cohort study. Fetal Diagn Ther 2020;47:721–30. https://doi.org/10.1159/000507549.Search in Google Scholar PubMed
12. Rizzo, G, Ghi, T, Henrich, W, Tutschek, B, Kamel, R, Lees, CC, et al.. Ultrasound in labor: clinical practice guideline and recommendation by the WAPM-world association of perinatal medicine and the PMF-perinatal medicine foundation. J Perinat Med 2022;50:1007–29. https://doi.org/10.1515/jpm-2022-0160.Search in Google Scholar PubMed
13. Jung, JE, Lee, YJ. Intrapartum transperineal ultrasound: angle of progression to evaluate and predict the mode of delivery and labor progression. Obstet Gynecol Sci 2024;67:1–16. https://doi.org/10.5468/ogs.23141.Search in Google Scholar PubMed PubMed Central
14. Mitta, K, Tsakiridis, I, Dagklis, T, Kalogiannidis, I, Mamopoulos, A, Michos, G, et al.. Ultrasonographic evaluation of the second stage of labor according to the mode of delivery: a prospective study in Greece. J Clin Med 2024;13:1068. https://doi.org/10.3390/jcm13041068.Search in Google Scholar PubMed PubMed Central
15. Mappa, I, Tartaglia, S, Maqina, P, Makatsariya, A, Ghi, T, Rizzo, G, et al.. Ultrasound vs routine care before instrumental vaginal delivery: a systematic review and meta-analysis. Acta Obstet Gynecol Scand 2021;100:1941–8. https://doi.org/10.1111/aogs.14236.Search in Google Scholar PubMed
16. Sainz, JA, Borrero, C, Aquise, A, Serrano, R, Gutiérrez, L, Fernández-Palacín, A. Utility of intrapartum transperineal ultrasound to predict cases of failure in vacuum extraction attempt and need of cesarean section to complete delivery. J Matern Fetal Neonatal Med 2016;29:1348–52. https://doi.org/10.3109/14767058.2015.1048680.Search in Google Scholar PubMed
17. Horst, W, do Valle, JB, Godoy, EDP, Silva, J. Fetal head-to-perineum distance as a predictor of successful vaginal delivery: a secondary analysis of intrapartum ultrasound data: Distância da cabeça fetal ao períneo como preditor do parto vaginal: análise secundária de dados de ultrassom intraparto. Concilium 2024;24:74–85. https://doi.org/10.53660/CLM-3840-23P06.Search in Google Scholar
18. Kahrs, BH, Usman, S, Ghi, T, Youssef, A, Torkildsen, EA, Lindtjørn, E, et al.. Sonographic prediction of outcome of vacuum deliveries: a multicenter, prospective cohort study. Am J Obstet Gynecol 2017;217:69.e1–10. https://doi.org/10.1016/j.ajog.2017.03.009.Search in Google Scholar PubMed
19. Ali, J, Hebbar, S. Ultrasound assessment of foetal head-perineum distance prior to induction of labour as a predictor of successful vaginal delivery. J Obstet Gynaecol India 2019;69:129–35. https://doi.org/10.1007/s13224-018-1120-x.Search in Google Scholar PubMed PubMed Central
20. Kasbaoui, S, Séverac, F, Aïssi, G, Gaudineau, A, Lecointre, L, Akladios, C, et al.. Predicting the difficulty of operative vaginal delivery by ultrasound measurement of fetal head station. Am J Obstet Gynecol 2017;216:507.e1–9. https://doi.org/10.1016/j.ajog.2017.01.007.Search in Google Scholar PubMed
21. Dall’Asta, A, Rizzo, G, Masturzo, B, Di Pasquo, E, Schera, GBL, Morganelli, G, et al.. Intrapartum sonographic assessment of the fetal head flexion in protracted active phase of labor and association with labor outcome: a multicenter, prospective study. Am J Obstet Gynecol 2021;225:171.e1–12. https://doi.org/10.1016/j.ajog.2021.02.035.Search in Google Scholar PubMed
22. Kalache, KD, Dückelmann, AM, Michaelis, SA, Lange, J, Cichon, G, Dudenhausen, JW. Transperineal ultrasound imaging in prolonged second stage of labor with occipitoanterior presenting fetuses: how well does the ‘angle of progression’ predict the mode of delivery? Ultrasound Obstet Gynecol 2009;33:326–30. https://doi.org/10.1002/uog.6294.Search in Google Scholar PubMed
23. Bultez, T, Quibel, T, Bouhanna, P, Popowski, T, Resche-Rigon, M, Rozenberg, P. Angle of fetal head progression measured using transperineal ultrasound as a predictive factor of vacuum extraction failure. Ultrasound Obstet Gynecol 2016;48:86–91. https://doi.org/10.1002/uog.14951.Search in Google Scholar PubMed
24. Cuerva, MJ, Bamberg, C, Tobias, P, Gil, MM, De La Calle, M, Bartha, JL. Use of intrapartum ultrasound in the prediction of complicated operative forceps delivery of fetuses in non-occiput posterior position. Ultrasound Obstet Gynecol 2014;43:687–92. https://doi.org/10.1002/uog.13256.Search in Google Scholar PubMed
25. Bulut, AN, Ceyhan, V. Evaluation of the labour process with serial transperineal ultrasonography and prediction of the type of birth. J Perinat Med 2020;49:36–42. https://doi.org/10.1515/jpm-2020-0323.Search in Google Scholar PubMed
26. Vinod, V, Kotian, C, Shah, K, Bhat, SK. Prediction of the mode of delivery using intrapartum translabial ultrasound in a teaching hospital in south India–A prospective observational study. Thai J Obstet Gynaecol 2022;30:41–50. https://doi.org/10.14456/tjog.2022.6.Search in Google Scholar
27. Kandil, RA, El shahawy, ASZ, El Shafiey, MH, Alarabawy, RA. Values and validity of fetal parameters by ultrasound and Doppler as markers of fetal lung maturity. Egypt J Radiol Nucl Med 2021;52:1–10. https://doi.org/10.1186/s43055-021-00432-1.Search in Google Scholar
28. Elkadi, MA, Ewida, MR, Zenhom, AM. Role of ‘angle of progression’ in prediction of vaginal delivery in primiparous women. Gin Pol Med Project 2021;16:1–6.Search in Google Scholar
29. Ibrahim, GA, Nasr, AS, Atta, F, Reda, M, Abdelghany, H, ElDemiry, NM, et al.. The assessment of intrapartum transperineal ultrasonographic parameters for their effectiveness in evaluation of progress of labor and prediction of mode of delivery in Egyptian women. Open access maced. J Med Sci 2021;9:1037–43. https://doi.org/10.3889/oamjms.2021.7049.Search in Google Scholar
30. Yonetani, N, Yamamoto, R, Murata, M, Nakajima, E, Taguchi, T, Ishii, K, et al.. Prediction of time to delivery by transperineal ultrasound in second stage of labor. Ultrasound Obstet Gynecol 2017;49:246–51. https://doi.org/10.1002/uog.15944.Search in Google Scholar PubMed
31. Malik, R, Singh, S. Measurement of angle of descent (AOD) by transperineal ultrasound in labour to predict successful vaginal delivery. J Obstet Gynaecol India 2020;70:126–32. https://doi.org/10.1007/s13224-019-01300-9.Search in Google Scholar PubMed PubMed Central
32. Hadad, S, Oberman, M, Ben-Arie, A, Sacagiu, M, Vaisbuch, E, Levy, R. Intrapartum ultrasound at the initiation of the active second stage of labor predicts spontaneous vaginal delivery. Am J Obstet Gynecol MFM 2021;3:100249. https://doi.org/10.1016/j.ajogmf.2020.100249.Search in Google Scholar PubMed
33. Kahrs, BH, Usman, S, Ghi, T, Youssef, A, Torkildsen, EA, Lindtjørn, E, et al.. Descent of fetal head during active pushing: secondary analysis of prospective cohort study investigating ultrasound examination before operative vaginal delivery. Ultrasound Obstet Gynecol 2019;54:524–9. https://doi.org/10.1002/uog.20348.Search in Google Scholar PubMed
34. Eggebø, TM, Hassan, WA, Salvesen, KÅ, Lindtjørn, E, Lees, CC. Sonographic prediction of vaginal delivery in prolonged labor: a two-center study. Ultrasound Obstet Gynecol 2014;43:195–201. https://doi.org/10.1002/uog.13210.Search in Google Scholar PubMed
35. Lee, NMW, Lau, SL, Yeung, YK, Chiu, CPH, Liu, F, Lau, YY, et al.. Implementation of sonopartogram: multicenter feasibility study. Ultrasound Obstet Gynecol 2024;64:214–21. https://doi.org/10.1002/uog.27634.Search in Google Scholar PubMed
36. Chor, CM, Poon, LCY, Leung, TY. Prediction of labor outcome using serial transperineal ultrasound in the first stage of labor. J Matern Fetal Neonatal Med 2019;32:31–7. https://doi.org/10.1080/14767058.2017.1369946.Search in Google Scholar PubMed
37. Chaemsaithong, P, Kwan, AHW, Tse, WT, Lim, WT, Chan, WWY, Chong, KC, et al.. Factors that affect ultrasound-determined labor progress in women undergoing induction of labor. Am J Obstet Gynecol 2019;220:592.e1–592.e15. https://doi.org/10.1016/j.ajog.2019.01.236.Search in Google Scholar PubMed
© 2025 the author(s), published by De Gruyter, Berlin/Boston
This work is licensed under the Creative Commons Attribution 4.0 International License.
Articles in the same Issue
- Frontmatter
- Review
- Sex differences in lung function of adolescents or young adults born prematurely or of very low birth weight: a systematic review
- Original Articles – Obstetrics
- Shifts in peak month of births and socio-economic factors: a study of divided and reunified Germany 1950–2022
- The predictive role of serial transperineal sonography during the first stage of labor for cesarean section
- Gestational weight gain and obstetric outcomes in women with obesity in an inner-city population
- Placental growth factor as a predictive marker of preeclampsia in twin pregnancy
- Learning curve for the perinatal outcomes of radiofrequency ablation for selective fetal reduction: a single-center, 10-year experience from 2013 to 2023
- External validation of a non-invasive vaginal tool to assess the risk of intra-amniotic inflammation in pregnant women with preterm labor and intact membranes
- Placental fetal vascular malperfusion in maternal diabetes mellitus
- The importance of the cerebro-placental ratio at term for predicting adverse perinatal outcomes in appropriate for gestational age fetuses
- Comparing achievability and reproducibility of pulsed wave Doppler and tissue Doppler myocardial performance index and spatiotemporal image correlation annular plane systolic excursion in the cardiac function assessment of normal pregnancies
- Characteristics of the pregnancy and labour course in women who underwent COVID-19 during pregnancy
- Original Articles – Fetus
- Sonographic visualization and measurement of the fetal optic chiasm and optic tract and association with the cavum septum pellucidum
- The association among fetal head position, fetal head rotation and descent during the progress of labor: a clinical study of an ultrasound-based longitudinal cohort study in nulliparous women
- Fetal hypoplastic left heart syndrome: key factors shaping prognosis
- The value of ultrasound spectra of middle cerebral artery and umbilical artery blood flow in adverse pregnancy outcomes
- Original Articles – Neonates
- A family-centric, comprehensive nurse-led home oxygen programme for neonatal chronic lung disease: home oxygen policy evaluation (HOPE) study
- Effects of a respiratory function indicator light on visual attention and ventilation quality during neonatal resuscitation: a randomised controlled crossover simulation trial
- Short Communication
- Incidence and awareness of dysphoric milk ejection reflex (DMER)
Articles in the same Issue
- Frontmatter
- Review
- Sex differences in lung function of adolescents or young adults born prematurely or of very low birth weight: a systematic review
- Original Articles – Obstetrics
- Shifts in peak month of births and socio-economic factors: a study of divided and reunified Germany 1950–2022
- The predictive role of serial transperineal sonography during the first stage of labor for cesarean section
- Gestational weight gain and obstetric outcomes in women with obesity in an inner-city population
- Placental growth factor as a predictive marker of preeclampsia in twin pregnancy
- Learning curve for the perinatal outcomes of radiofrequency ablation for selective fetal reduction: a single-center, 10-year experience from 2013 to 2023
- External validation of a non-invasive vaginal tool to assess the risk of intra-amniotic inflammation in pregnant women with preterm labor and intact membranes
- Placental fetal vascular malperfusion in maternal diabetes mellitus
- The importance of the cerebro-placental ratio at term for predicting adverse perinatal outcomes in appropriate for gestational age fetuses
- Comparing achievability and reproducibility of pulsed wave Doppler and tissue Doppler myocardial performance index and spatiotemporal image correlation annular plane systolic excursion in the cardiac function assessment of normal pregnancies
- Characteristics of the pregnancy and labour course in women who underwent COVID-19 during pregnancy
- Original Articles – Fetus
- Sonographic visualization and measurement of the fetal optic chiasm and optic tract and association with the cavum septum pellucidum
- The association among fetal head position, fetal head rotation and descent during the progress of labor: a clinical study of an ultrasound-based longitudinal cohort study in nulliparous women
- Fetal hypoplastic left heart syndrome: key factors shaping prognosis
- The value of ultrasound spectra of middle cerebral artery and umbilical artery blood flow in adverse pregnancy outcomes
- Original Articles – Neonates
- A family-centric, comprehensive nurse-led home oxygen programme for neonatal chronic lung disease: home oxygen policy evaluation (HOPE) study
- Effects of a respiratory function indicator light on visual attention and ventilation quality during neonatal resuscitation: a randomised controlled crossover simulation trial
- Short Communication
- Incidence and awareness of dysphoric milk ejection reflex (DMER)

