Comparing achievability and reproducibility of pulsed wave Doppler and tissue Doppler myocardial performance index and spatiotemporal image correlation annular plane systolic excursion in the cardiac function assessment of normal pregnancies
Abstract
Objectives
Multiple techniques have been proposed for functional fetal cardiology, including pulsed-wave (PW) and tissue Doppler imaging (TDI), Myocardial Performance Index (MPI), annular plane systolic excursion (TAPSE/MAPSE) and spatiotemporal image correlation (STIC). We aimed to compare these techniques’ achievability and reproducibility to determine their clinical utility for each cardiac side.
Methods
Uncomplicated pregnancies from 22 to 39 weeks were recruited and images and volumes stored for offline analysis. PWD-MPI values were calculated using previously demonstrated automation algorithms, and the remaining volumes were evaluated by two experienced operators.
Results
Seventy-nine women were scanned generating 222 volumes, with high achievability (>86 %) for all three modalities on both cardiac sides; highest for TAPSE/MAPSE (94 %). Repeatability (ICC) on the right side of the heart was highest for TAPSE (inter-observer 0.86; intraobserver 0.73), compared to PWD-MPI (0.69) and TDI-MPI (0.83). For the left side, repeatability was high for both PWD-MPI (0.80) and TDI-MPI (0.86) though low for MAPSE (inter-observer 0.7, intra-observer 0.69). There was poor correlation between PWD-MPI and TDI-MPI values.
Conclusions
TAPSE appears most reliable for evaluation of right heart function, compared to PWD-MPI for the left. As TDI-MPI correlates poorly with PWD-MPI, the latter appears to be the functional tool of choice.
Introduction
Evaluation of fetal cardiac function involves quantifying chamber shape and size, cardiac volume and stroke volume, contractility and relaxation [1], to detect adaptation to strain [2], [3], [4]. The fetal and adult cardiovascular systems differ [5] with the fetus having parallel circulations, shunts, right heart dominance and differing sensitivity to loading conditions from the adult [6], [7], [8]. The fetal heart has a longitudinal myocardial fibre arrangement on the right and circumferential on the left [9], 10]. Several Doppler tools have been proposed for functional fetal cardiology.
The Myocardial Performance Index (MPI) is a pulse-wave Doppler-derived index of global myocardial function, relying on time intervals, therefore having the advantage of being relatively independent of precise imaging, anatomy, ventricular geometry and heart rate [11]. The Modified-MPI variation (Mod-MPI) introduced valve clicks to delineate time intervals better [12] although calliper placement varies across the literature [12], [13], [14], [15]. We have previously shown that automation for both left and right MPI removes the dependence on observer calliper placement, expertise and subjectivity [16], 17].
Tissue Doppler imaging (TDI) has been proposed as a robust tool for the detection of subclinical cardiac dysfunction with improved reproducibility over conventional Doppler [18], and unlike PW-TDI, the right TDI-MPI can be acquired in a single acquisition [19]. It is also possible to measure the tricuspid/mitral annular plane systolic excursion (TAPSE/MAPSE) or maximal longitudinal displacement of the valve annuli [20], 21]. TAPSE/MAPSE may also be measured using spatiotemporal image correlation (STIC) to overcome challenges arising from the orientation of the fetal cardiac longitudinal axis, through post-processing multi-planar reconstruction and manipulation [22].
Whilst these three independent modalities (PWD-MPI, TDI-MPI, and TAPSE/MAPSE) have been applied to cardiac function evaluation, we aimed to perform a multi-modality global cardiac function evaluation comparing their achievability and reproducibility.
Methods
This prospective, cross-sectional study recruited patients from a tertiary hospital antenatal clinic with local ethics committee approval (SESLHD HREC Reference 13/320).
Seventy-nine patients were consecutively recruited between February and November 2015, and within each case, the best images and volumes were selected. Women eligible to be included in the study were older than 18 years with an uncomplicated singleton pregnancy between 22 and 39 gestational weeks and a normal morphology scan. Women with known complications, whether maternal (such as hypertension, pre-eclampsia, diabetes) or fetal (such as IUGR or structural anomalies), were excluded. Women with insufficient English to consent were also excluded.
The necessary sample size for comparison of intra-observer repeatability comparing n=3 replicates per subject (for all three modalities) was calculated to be k=39.6, aiming for intra-observer ICC reliability of 0.7 with a minimum ICC>0.5 acceptable [23] and with a type I error of 0.05 and a type II error of 0.2 [24]. A larger sample size was planned to ensure sufficient sets of optimal scans.
One experienced operator performed the ultrasound scans. Following routine biometry and fetal well-being measurements, STIC volumes for TAPSE and MAPSE and PWD and TDI plots for MPI measurements were acquired, as depicted in Figure 1. Left PWD-MPI was acquired in the four-chamber view in an apical or basal position [12], 25]. Right PWD-MPI was acquired in two planes (tricuspid inflow and pulmonary outflow plots) [26]. Right and left TDI-MPI were acquired in the four-chamber view at either an apical or basal position [27], 28], and then multiple STIC volumes were acquired and saved to ensure at least three were of adequate quality for analysis. The insonation angle was maintained as close to the apex directly up or down, with a zoom into the region of interest at a minimal volume angle of 15° and an acquisition time of 7.5 s. Volumes with fetal movement were excluded and repeated, and total scanning time was recorded for each patient.

Study design.
All MPI waveforms and STIC volumes were reviewed offline, and the three clearest cardiac cycles in every waveform (TDI-left, TDI-right, PWD-left, two PWD-right plots) and the best three STIC volumes were chosen for each case by the lead researcher. TDI images were classified for quality (scale 1–3) [27]. The angle of insonation, defined as the angle between the ultrasound beam axis (from the sector tip to the distal field) and the cardiac axis (along the ventricular septum in the 2D image or STIC volume), was recorded. Individual 2D scans were excluded if: i) the time intervals (TDI) or valve clicks (PWD) were indistinguishable; ii) the automation program failed to identify clicks (PWD); iii) the measured difference in heart rate between the two PWD-right Doppler plots was greater than 10 beats per minute.
Both left and right TDI-MPI and Left PWD-MPI values were calculated as the sum of the isovolumetric time intervals divided by the ejection time
Data was anonymised, and two experienced operators evaluated all the volumes. Intra-observer repeatability was analysed by comparing the same operator’s measurements of three different volumes from the same patient. Inter-observer repeatability was analyzed by comparing both operators’ measurements of volume no. 1 from each patient. Data was collected using Excel 2010 (Microsoft Office, Redmond, Washington, USA) and statistical analysis using SPSS version 23.0 (IBM, Armonk, New York, USA). Descriptive statistics (mean, minimum and maximum) were determined for relevant characteristic variables. Achievability was measured as a percentage success rate of achieving the required measurements. TAPSE and MAPSE values were compared using a paired T-test. Intra-and inter-observer variability were assessed with intraclass correlation coefficients (ICC) and 95 % Confidence Interval (CI), using a two-way random model using single measurements for absolute agreement [36]. Finally, a sub-group analysis was performed by dividing the study group to three sub-groups according to their gestational age: 22–27 weeks, 28–33 weeks and 34–39 weeks.
Results
Seventy-nine women with uncomplicated pregnancies were recruited and scanned. Key demographic variables are summarised in Table 1. All growth and well-being ultrasound parameters, including estimated fetal weight, Doppler studies, and liquor, were reported to be within the normal range. The total scan time was recorded with a median of 38 min and an interquartile range of 19 min (Q1=32 and Q3=51 min).
Baseline characteristics.
| Characteristic | Mean | Standard deviation | Range | Fraction | Percentage |
|---|---|---|---|---|---|
| Gestational age at ultrasound, weeks | 30 + 5 | 4.4 | 22 + 6–38 + 6 | – | – |
| Maternal age, years | 31.6 | 4.8 | 20–43 | – | – |
| Pre-pregnancy maternal BMI, kg/m2 | 21.9 | 3.1 | 15.2–32.0 | – | – |
| Birthweight, g | 3,418.9 | 453.6 | 2,205–4,730 | – | – |
| Gestational age at delivery, weeks | 39.3 | 1.3 | 33.5–41.4 | – | – |
| Nulliparous | – | – | – | 50/79 | 63.3 |
| Smokers | – | – | – | 3/76 | 3.9 |
| IVF conception | – | – | – | 5/76 | 6.6 |
-
BMI, body mass index; IVF, in vitro fertilization.
Successful acquisition rates were 86 and 92 % for left and right TDI-MPI, respectively, 87 % for both left and right PWD-MPI, and 94 % for both TAPSE and MAPSE. To minimise bias, all 222 volumes appeared randomly in the study data set for the two operators to analyse.
Descriptive statistics and 95 % CIs, respectively, for the left and right TDI-MPI and PWD-MPI values and their time intervals are summarised in Table 2. Descriptive statistics for TAPSE and MAPSE are summarised in Table 3, with mean TAPSE values being significantly higher than MAPSE (difference 1.54 mm, p<0.0001; 95 % CI 1.32–1.75, SD 0.11).
Left and right myocardial performance absolute values by pulsed wave and tissue Doppler imaging.
| Left MPI | Mean | Min | Max | SD | 95 % CI |
|---|---|---|---|---|---|
| TDI-MPI | 0.59 | 0.4 | 0.9 | 0.11 | 0.56–0.62 |
| PWD-MPI | 0.51 | 0.39 | 0.75 | 0.08 | 0.49–0.53 |
| TDI-ICT, ms | 45.9 | 26.7 | 70.3 | 9.4 | 43.7–48.2 |
| PWD-ICT, ms | 35.9 | 24 | 52.3 | 7.4 | 34.4–37.7 |
| TDI-ET, ms | 166.7 | 131 | 206.7 | 14.3 | 162.2–170.1 |
| PWD-ET, ms | 164.2 | 13 | 182.3 | 9.8 | 161.9–166.6 |
| TDI-IRT, ms | 51.2 | 32 | 82.3 | 9.7 | 48.9–53.6 |
| PWD-IRT, ms | 47.5 | 34 | 62.6 | 6.5 | 45.9–49.0 |
| TDI-HR, bpm | 143 | 127 | 159 | 8 | 141–145 |
| PWD-HR, bpm | 142 | 127 | 159 | 8 | 139–144 |
| Right MPI | Mean | Min | Max | SD | 95 % CI |
|---|---|---|---|---|---|
| TDI-MPI | 0.53 | 0.35 | 0.86 | 0.11 | 0.50–0.55 |
| PWD-MPI | 0.58 | 0.37 | 0.9 | 0.1 | 0.55–0.60 |
| TDI-ICT, ms | 47.1 | 26.7 | 83.7 | 11.8 | 44.3–49.1 |
| TDI-ET, ms | 174.9 | 140.7 | 204.7 | 14 | 171.7–178.3 |
| TDI-IRT, ms | 43.9 | 22 | 68 | 8.7 | 41.9–46.0 |
| TDI-(ICT+IRT), ms | 91 | 67.3 | 141.3 | 15 | 57.5–94.5 |
| PWD-a, ms | 262.8 | 216.7 | 313 | 14.9 | 259.2–266.4 |
| PWD-b, ms | 167 | 139.6 | 189.8 | 10.2 | 164.5–169.4 |
| PWD-(a-b), ms | 95.8 | 66.2 | 130.1 | 13.8 | 92.5–99.1 |
| TDI-HR, bpm | 142 | 125 | 161 | 10 | 140–144 |
| PWD-HR, bpm | 142 | 123 | 163 | 8 | 140–144 |
-
MPI, myocardial performance index; TDI, tissue Doppler imaging; PWD, pulsed wave Doppler; ICT, isovolumetric contraction time; ET, ejection time; IRT, isovolumetric relaxation time; HR, heart rate.
Tricuspid annular plane systolic excursion and mitral annular plane systolic excursion absolute values by two operators.
| Mean, mm | Min, mm | Max, mm | S/D | ||
|---|---|---|---|---|---|
| TAPSE | Operator 1 | 6.4 | 4.2 | 9.1 | 1.2 |
| Operator 2 | 6.4 | 4.0 | 8.8 | 1.3 | |
| MAPSE | Operator 1 | 4.9 | 3.1 | 7.3 | 1.0 |
| Operator 2 | 4.7 | 2.4 | 7.9 | 1.1 |
-
TAPSE, Tricuspid annular plane systolic excursion; MAPSE, mitral annular plane systolic excursion; Min, minimum; Max, maximum; S/D, standard deviation.
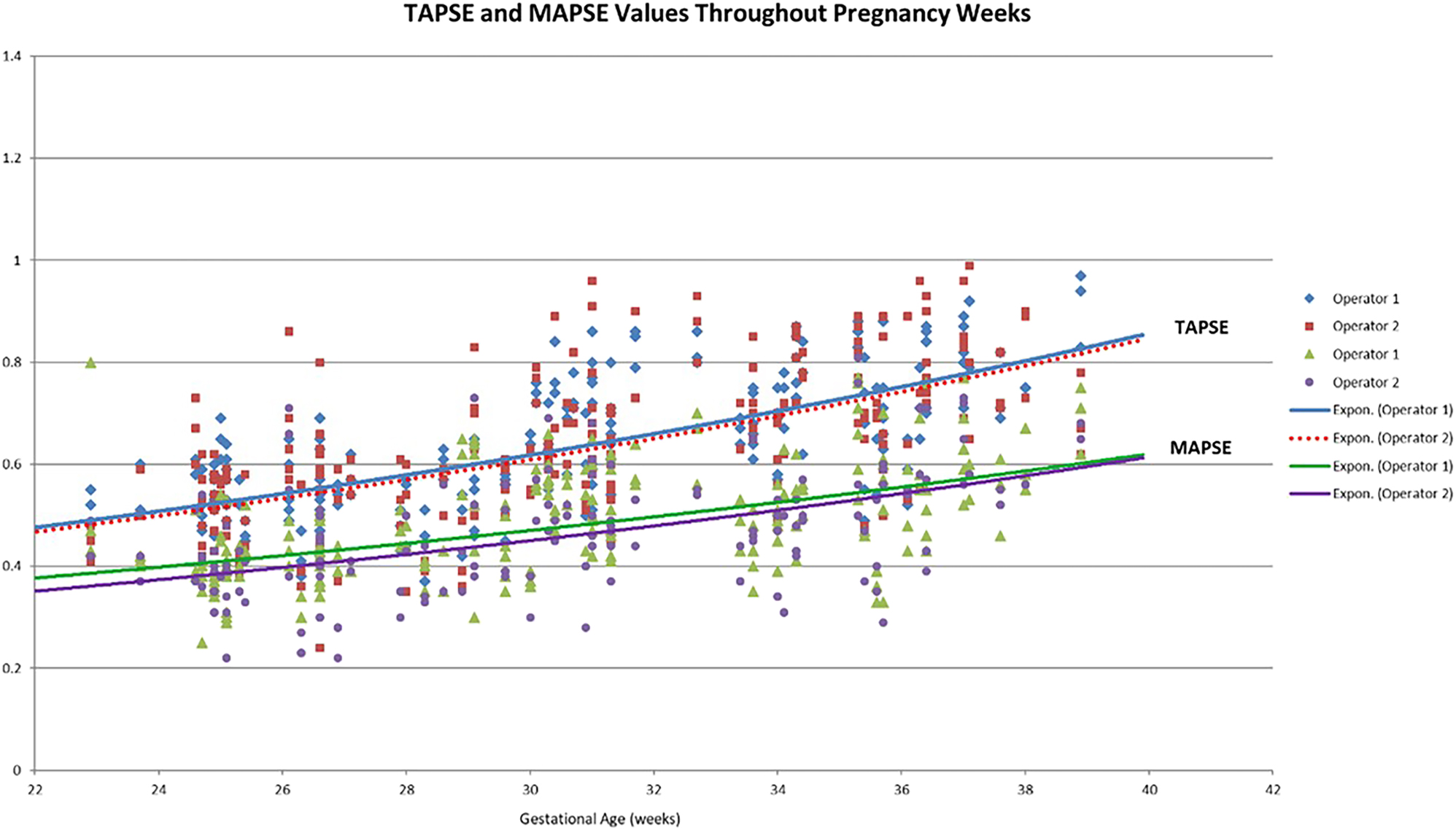
TAPSE and MAPSE values increased throughout gestation, as shown in Figure 2. In contrast to our group’s previous publication [37], there was no relationship between gestational age or fetal heart rate and either PWD or TDI MPI values. There was a poor correlation between PWD-MPI and TDI-MPI, as we have shown previously [38] Table 4 shows the repeatability for the left and right sides of the fetal heart for PWD-MPI, TDI-MPI, MAPSE, and TAPSE, and Table 5 shows the three sub-groups analysed according to gestational age.
Tricuspid annular plane systolic excursion and mitral annular plane systolic excursion absolute values by gestational age.
Pulsed wave myocardial performance index, tissue Doppler myocardial performance index and annular plane systolic excursion reliability.
| (A) Left | PWD | TDI | MAPSE |
|---|---|---|---|
| MPI | 0.80 (0.72–0.87) | 0.86 (0.81–0.91) | NA |
| ICT | 0.74 (0.65–0.82) | 0.88 (0.83–0.92) | NA |
| ET | 0.74 (0.65–0.82) | 0.88 (0.83–0.92) | NA |
| IRT | 0.67 (0.56–0.77) | 0.78 (0.70–0.85) | NA |
| Operator 1 Intra-observer |
NA | NA | 0.67 (0.55–0.76) |
| Operator 2 Intra-observer |
NA | NA | 0.71 (0.62–0.80) |
| Inter-observer | NA | NA | 0.70 (0.56–0.80) |
|
|
|||
| (B) Right | PWD | TDI | TAPSE |
|
|
|||
| MPI | 0.69 (0.57–0.78) | 0.83 (0.76–0.88) | NA |
| a | 0.84 (0.77–0.89) | NA | NA |
| b | 0.81 (0.73–0.87) | NA | NA |
| ICT | NA | 0.92 (0.88–0.94) | NA |
| ET | NA | 0.85 (0.79–0.90) | NA |
| IRT | NA | 0.78 (0.70–0.85) | NA |
| Operator 1 Intra-observer |
NA | NA | 0.81 (0.73–0.87) |
| Operator 2 Intra-observer |
NA | NA | 0.64 (0.53–0.74) |
| Inter-observer | NA | NA | 0.86 (0.75–0.90) |
-
MPI, myocardial performance index; TDI, tissue Doppler imaging; PWD, pulsed wave Doppler; ICT, isovolumetric contraction time; ET, ejection time; IRT, isovolumetric relaxation time; HR, heart rate.
Multi-modality reliability ICCs (95 % CI) by gestational age subgroups.
| Right heart | Total | 22–27w | 28–33w | 34–39w | |
|---|---|---|---|---|---|
| TAPSE inter-observer | 0.86(0.79–0.91) | 0.84(0.66–0.93) | 0.860.70–0.94) | 0.83(0.63–0.92) | |
| TAPSE intra-observer | Operator 1 | 0.83(0.77–0.88) | 0.81(0.64–0.91) | 0.90(0.81–0.95) | 0.87(0.76–0.94) |
| Operator 2 | 0.62(0.51–0.72) | 0.62(0.28–0.82) | 0.84(0.70–0.92) | 0.50(0.09–0.75) | |
| Average | 0.73 | 0.72 | 0.87 | 0.69 | |
| PWD-MPI intra-observer | 0.69(0.58–0.78) | 0.81(0.66–0.91) | 0.61(0.38–0.79) | 0.63(0.40–0.81) | |
| TDI-MPI intra-observer | 0.83(0.76–0.88) | 0.75(0.59–0.87) | 0.83(0.69–0.91) | 0.84(0.71–0.92) | |
|
|
|||||
| Left heart | Total | 22-27w | 28-33w | 34-39w | |
|
|
|||||
| MAPSE inter-observer | 0.70(0.57–0.79) | 0.68(0.28–0.85) | 0.52(0.01–0.77) | 0.84(066–0.93) | |
| MAPSE intra-observer | Operator 1 | 0.72(0.63–0.80) | 0.72(0.47–0.86) | 0.85(0.71–0.92) | 0.83(0.69–0.92) |
| Operator 2 | 0.67(0.57–0.76) | 0.81(0.64–0.91) | 0.72(0.48–0.86) | 0.84(0.70–0.92) | |
| Average | 0.69 | 0.76 | 0.79 | 0.83 | |
| PWD-MPI intra-observer | 0.8(0.72–0.86) | 0.84(0.70–0.92) | 0.8(0.65–0.90) | 0.75(0.57–0.87) | |
| TDI-MPI intra-observer | 0.86(0.80–0.91) | 0.90(0.80–0.95) | 0.90(0.82–0.95) | 0.77(0.59–0.89) | |
-
TAPSE, tricuspid annular plane systolic excursion; PWD, pulsed wave Doppler; MPI, myocardial performance index; TDI, tissue Doppler imaging; w, weeks of gestation.
Discussion
This study provides the first quantitative comparison between three novel fetal cardiac function modalities for their achievability and repeatability. This could potentially lead to the integration and optimisation of techniques for fetal cardiac evaluation.
Achievability rates were high for all three modalities for both sides of the heart and similar when sub-grouped by gestational age (all above 86 %). The PWD-MPI automation algorithm used in this study successfully calculates MPI (87 % of the cases) when it clearly locates the four valve clicks, effectively excluding poor-quality waveforms. Manual calliper placement in the same circumstance might have estimated the appropriate location, introducing more flexibility and variability. Lower-quality TDI scans, which were manually measured but were nevertheless deemed visually poor, were included in the analysis. Exclusion of suboptimal TDI scans by applying similar criteria to TDI-MPI would cause a significant reduction of the acquisition rate for both left and right TDI MPI (from 86 to 47 % and from 92 to 70 %, respectively). This indicates that using TDI to measure MPI in fetuses is easily achievable, though the waveform quality has considerable variability.
TAPSE and MAPSE high achievability rates (94 %) may have been a result of the novel STIC acquisition settings chosen for this study, designed to optimise annuli visualisation and favouring high-quality images. An optimal 2D image of the four-chamber view of the heart at any orientation was obtained, yet at an insonation angle as close to an apex up or apex down position. A region of interest encompassing the fetal heart was selected [39] and STIC acquisition parameters were set to the minimum volume angle of 15° and a minimal acquisition time of 7.5 s. This narrow angle maximizes the frame rate during the acquisition, improving the temporal resolution of the volume dataset, and enhancing image quality. The selected short acquisition time, minimizes the likelihood of artefacts related to fetal movement, while having the minor expense of spatial resolution [40].
As we have previously shown, PWD-MPI and TDI-MPI gave statistically significantly different and inconsistent values for both sides of the heart, with TDI-MPI measuring greater values for the left ventricle and lower values for the right, potentially reflecting the difference between measuring blood flow and myometrial contraction [27]. Variation in the TDI waveform and lack of definitive landmarks also contributes to time interval measurement inconsistency [19], 31], 41].
Fetal right heart dominance may be a reason for higher TAPSE values than MAPSE. An alternative explanation could lie in the twisting movement of the left muscle fibres compared to the more vertical motion on the right side generating a shorter vertical excursion of the mitral annulus [42].
Whilst our automated algorithm for PWD-MPI has previously shown a perfect ICC of 1.0 for the repeated measurement of the same cardiac cycle [16], 17], in this study PWD-MPI was measured across three cardiac cycles representing variability in repeat measurements completed on a single fetus during similar circumstances. This was lowest (ICC 0.69) for the right side of the heart, likely due to the introduction of variability while using two cardiac planes for recording tricuspid inflow and pulmonary outflow, adding to the underlying physiological Doppler variability.
For the right side of the fetal heart, TAPSE showed the best repeatability with inter-observer ICC of 0.86 and average intra-observer ICC of 0.73, potentially a consequence of the more distinct ultrasound appearance of the right lateral annulus with its more direct vertical motion. As expected, right PWD-MPI was only moderately [23] reliable (ICC 0.69), improved upon with TDI-MPI (ICC 0.83). These differences were notable yet did not reach statistical significance.
For the left side of the heart repeatability results for both PWD (0.80) and TDI (0.86) MPI measurement were good [23]. MAPSE results revealed only moderate repeatability with inter-observer ICC of 0.70 and average intra-observer ICC of 0.69. These differences did not reach statistical significance. As we have recently shown [27], TDI-MPI demonstrated very good intra-observer reliability (ICC 0.88–0.94) but low inter-observer ICCs (0.56), in part likely due to a high level of variation in waveform appearance. The poor correlation between TDI-MPI and PWD-MPI values, along with the variation in image appearance question the usefulness of TDI for MPI measurement. With intra- and inter-observer repeatability ICCs of 0.69 and 0.70 respectively MAPSE showed the poorest reliability within the left side evaluation, lower than PWD-MPI (ICC 0.80). Left TDI-MPI repeatability, similarly to the right-side assessment, revealed good intra-observer repeatability (ICC 0.86) although inter-observer repeatability could not be assessed. Given the same inconsistencies of appearance as seen in the right side of the heart, the automated PWD-MPI appears to be the most reliable for evaluation of left sided fetal cardiac function. For all three modalities evaluated for both sides of the heart, subgroup analysis did not find any significant differences or consistent trends comparing reliability between the different gestational age groups.
The main strength of this prospective study is that it focused on comparing three novel indices within both sides of the heart allowing a comprehensive multi-modality and global functional evaluation in a carefully selected cross-sectional study group of uncomplicated pregnancies.
This study had several limitations, including the research setting in which ultrasound scans were carried out. A dedicated research environment helps generating high acquisition rates for all cardiac function modalities offering more time to assess cardiac parameters. However, this could be at the fundamental expenses of generalizability of results to a clinical setting. Whilst there were notable differences in repeatability between the different modalities, these did not reach statistical significance for either side of the heart, which may have been overcome by a larger sample size. Use of only one ultrasound machine type may have been a limitation as our previous work has shown significant differences in TDI plots from different machines [27]. Finally, there is a lack of a gold standard fetal cardiac function modality for comparison. We acknowledge that other techniques for evaluating cardiac function are available (e.g. Doppler of AV valves and outflow tracts, cardiac biometry and indices of cardiac remodelling) and were not considered in this study.

Left pulsed wave myocardial performance index (a, b), left tissue Doppler imaging myocardial performance index measurement (c, d) and Spatio-temporal image correlation Tricuspid annulus plane excursion (e, f) and mitral annulus plane excursion measurements (g, h).
Conclusions
While no single method is definitively superior to the others in both heart sides, our results on achievability and repeatability suggest TAPSE to be more suited to the right heart and PWD-MPI to the left heart. TAPSE provides a well-defined distinct M-mode waveform delineating the more longitudinal vertical movement of the tricuspid annulus, due to the longitudinal muscle fibre organisation of the dominant right ventricle. Automated PWD-MPI provides a verified standardised, automated technique consistently and reliably measuring the left heart inflow and outflow in a single cardiac plane.
Acknowledgments
This work was conducted as part of the PhD thesis of Dr Hagai Avnet at the University of New South Wales, Sydney.
-
Research ethics: This study obtained ethical approval (SESLHD HREC Reference 13/320) by the Southeastern Sydney Local Health District Human Research Ethics Committee. The research was performed in accordance with the Declaration of Helsinki.
-
Informed consent: Informed consent was obtained from all individuals included in this study, or their legal guardians or wards.
-
Author contributions: All the authors have revised and contributed to drafting the manuscript. The authors have accepted responsibility for the entire content of this manuscript and approved its submission.
-
Use of Large Language Models, AI and Machine Learning Tools: None declared.
-
Conflict of interest: The authors state no conflict of interest
-
Research funding: None declared
-
Data availability: Not applicable.
References
1. DeVore, GR. Assessing fetal cardiac ventricular function. Semin Fetal Neonatal Med 2005;10:515–41. https://doi.org/10.1016/j.siny.2005.08.009.Search in Google Scholar PubMed
2. Crispi, F, Hernandez-Andrade, E, Pelsers, MM, Plasencia, W, Benavides-Serralde, JA, Eixarch, E, et al.. Cardiac dysfunction and cell damage across clinical stages of severity in growth-restricted fetuses. Am J Obstet Gynecol 2008;199:254 e1–8. https://doi.org/10.1016/j.ajog.2008.06.056.Search in Google Scholar PubMed
3. Rychik, J, Tian, Z, Bebbington, M, Xu, F, McCann, M, Mann, S, et al.. The twin-twin transfusion syndrome: spectrum of cardiovascular abnormality and development of a cardiovascular score to assess severity of disease2007 Oct, 392:e1–8 pp.10.1016/j.ajog.2007.06.055Search in Google Scholar PubMed
4. Tutschek, B, Schmidt, KG. Techniques for assessing cardiac output and fetal cardiac function. Semin Fetal Neonatal Med 2011;16:13–21. https://doi.org/10.1016/j.siny.2010.09.005.Search in Google Scholar PubMed
5. Kiserud, T. Physiology of the fetal circulation. Semin Fetal Neonatal Med 2005;10:493–503. https://doi.org/10.1016/j.siny.2005.08.007.Search in Google Scholar PubMed
6. Mielke, G, Benda, N. Cardiac output and central distribution of blood flow in the human fetus. Circulation 2001;103:1662–8. https://doi.org/10.1161/01.cir.103.12.1662.Search in Google Scholar PubMed
7. Reller, MD, Morton, MJ, Reid, DL, Thornburg, KL. Fetal lamb ventricles respond differently to filling and arterial pressures and to in utero ventilation. Pediatr Res 1987;22:621–6. https://doi.org/10.1203/00006450-198712000-00001.Search in Google Scholar PubMed
8. Rychik, J. Fetal cardiovascular physiology. Pediatr Cardiol 2004;25:201–9. https://doi.org/10.1007/s00246-003-0586-0.Search in Google Scholar PubMed
9. Crispi, F, Gratacós, E. Fetal cardiac function: technical considerations and potential research and clinical applications. Fetal Diagn Ther 2012;32:47–64. https://doi.org/10.1159/000338003.Search in Google Scholar PubMed
10. Simpson, J. Echocardiographic evaluation of cardiac function in the fetus. Prenat Diagn 2004;24:1081–91. https://doi.org/10.1002/pd.1065.Search in Google Scholar PubMed
11. Friedman, D, Buyon, J, Kim, M, Glickstein, JS. Fetal cardiac function assessed by Doppler myocardial performance index (Tei Index). Ultrasound Obstet Gynecol 2003;21:33–6. https://doi.org/10.1002/uog.11.Search in Google Scholar PubMed
12. Hernandez-Andrade, E, Lopez-Tenorio, J, Figueroa-Diesel, H, Sanin-Blair, J, Carreras, E, Cabero, L, et al.. A modified myocardial performance (Tei) index based on the use of valve clicks improves reproducibility of fetal left cardiac function assessment. Ultrasound Obstet Gynecol 2005;26:227–32. https://doi.org/10.1002/uog.1959.Search in Google Scholar PubMed
13. Meriki, N, Izurieta, A, Welsh, AW. Fetal left modified myocardial performance index: technical refinements in obtaining pulsed-Doppler waveforms. Ultrasound Obstet Gynecol 2012;39:421–9. https://doi.org/10.1002/uog.9090.Search in Google Scholar PubMed
14. Tei, C. New non-invasive index for combined systolic and diastolic ventricular function. J Cardiol 1995;26:135–6.Search in Google Scholar
15. Van Mieghem, T, Gucciardo, L, Lewi, P, Lewi, L, Van Schoubroeck, D, Devlieger, R, et al.. Validation of the fetal myocardial performance index in the second and third trimesters of gestation. Ultrasound Obstet Gynecol 2009;33:58–63. https://doi.org/10.1002/uog.6238.Search in Google Scholar PubMed
16. Welsh, AW, Maheshwari, P, Wang, J, Henry, A, Chang, D, Crispi, F, et al.. Evaluation of an automated fetal myocardial performance index. Ultrasound Obstet Gynecol 2015. https://doi.org/10.1002/uog.15770.Search in Google Scholar PubMed
17. Leung, V, Avnet, H, Henry, A, Wang, J, Redmond, S, Welsh, AW. Automation of the fetal right myocardial performance index to optimse repeatability. Fetal Diagn Ther 2018;44:28–35. https://doi.org/10.1159/000478928.Search in Google Scholar PubMed
18. Paladini, D, Lamberti, A, Teodoro, A, Arienzo, M, Tartaglione, A, Martinelli, P. Tissue Doppler imaging of the fetal heart. Ultrasound Obstet Gynecol 2000;16:530–5. https://doi.org/10.1046/j.1469-0705.2000.00251.x.Search in Google Scholar PubMed
19. Duan, Y, Harada, K, Wu, W, Ishii, H, Takada, G. Correlation between right ventricular Tei index by tissue Doppler imaging and pulsed Doppler imaging in fetuses. Pediatr Cardiol 2008;29:739–43. https://doi.org/10.1007/s00246-008-9215-2.Search in Google Scholar PubMed
20. Germanakis, I, Pepes, S, Sifakis, S, Gardiner, H. Fetal longitudinal myocardial function assessment by anatomic M-mode. Fetal Diagn Ther 2012;32:65–71. https://doi.org/10.1159/000330790.Search in Google Scholar PubMed
21. Gardiner, HM, Pasquini, L, Wolfenden, J, Barlow, A, Li, W, Kulinskaya, E, et al.. Myocardial tissue Doppler and long axis function in the fetal heart. Int J Cardiol 2006;113:39–47. https://doi.org/10.1016/j.ijcard.2005.10.029.Search in Google Scholar PubMed
22. Messing, B, Gilboa, Y, Lipschuetz, M, Valsky, DV, Cohen, SM, Yagel, S. Fetal tricuspid annular plane systolic excursion (f-TAPSE): evaluation of fetal right heart systolic function with conventional M-mode ultrasound and spatiotemporal image correlation (STIC) M-mode. Ultrasound Obstet Gynecol 2013;42:182–8. https://doi.org/10.1002/uog.12375.Search in Google Scholar
23. Koo, TK, Li, MY. A guideline of selecting and reporting intraclass correlation coefficients for reliability research. J Chiropr Med 2016;15:155–63. https://doi.org/10.1016/j.jcm.2016.02.012.Search in Google Scholar
24. Walter, SD, Eliasziw, M, Donner, A. Sample size and optimal designs for reliability studies. Stat Med 1998;17:101–10. https://doi.org/10.1002/(sici)1097-0258(19980115)17:1<101::aid-sim727>3.0.co;2-e.10.1002/(SICI)1097-0258(19980115)17:1<101::AID-SIM727>3.3.CO;2-5Search in Google Scholar
25. Api, O, Emeksiz, MB, Api, M, Ugurel, V, Unal, O. Modified myocardial performance index for evaluation of fetal cardiac function in pre-eclampsia. Ultrasound Obstet Gynecol 2009;33:51–7. https://doi.org/10.1002/uog.6272.Search in Google Scholar
26. Meriki, N, Izurieta, A, Welsh, A. Reproducibility of constituent time intervals of right and left fetal modified myocardial performance indices on pulsed Doppler echocardiography: a short report. Ultrasound Obstet Gynecol 2012;39:654–8. https://doi.org/10.1002/uog.10049.Search in Google Scholar
27. Avnet, H, Thomas, S, Beirne, G, Alphonse, J, Welsh, A. Poor correlation between fetal tissue Doppler imaging and pulsed wave myocardial performance indices. Fetal Diagn Ther 2023. https://doi.org/10.1159/000529945.Search in Google Scholar
28. Meriki, N, Welsh, AW. Development of Australian reference ranges for the left fetal modified myocardial performance index and the influence of caliper location on time interval measurement. Fetal Diagn Ther 2012;32:87–95. https://doi.org/10.1159/000334133.Search in Google Scholar
29. Meriki, N, Henry, A, Sanderson, J, Majajan, A, Wu, L, Welsh, AW. Development of normal gestational ranges for the right myocardial performance index in the Australian population with three alternative caliper placements. Fetal Diagn Ther. 2014;36:272-81, https://doi.org/10.1159/000362388.Search in Google Scholar
30. Bui, YK, Kipps, AK, Brook, MM, Moon-Grady, AJ. Tissue Doppler is more sensitive and reproducible than spectral pulsed-wave Doppler for fetal right ventricle myocardial performance index determination in normal and diabetic pregnancies. J Am Soc Echocardiogr 2013;26:507–14. https://doi.org/10.1016/j.echo.2013.02.006.Search in Google Scholar
31. Acharya, G, Pavlovic, M, Ewing, L, Nollmann, D, Leshko, J, Huhta, JC. Comparison between pulsed-wave Doppler- and tissue Doppler-derived Tei indices in fetuses with and without congenital heart disease. Ultrasound Obstet Gynecol 2008;31:406–11. https://doi.org/10.1002/uog.5292.Search in Google Scholar
32. Kurtulmus, S, Mese, T, Taner, CE, Oztekin, DC, Okyay, D, Uysal, A, et al.. Evaluation of tissue Doppler-derived myocardial performance index in fetuses with intracardiac echogenic focus. J Matern Fetal Neonatal Med 2013;26:1662–6. https://doi.org/10.3109/14767058.2013.797957.Search in Google Scholar PubMed
33. Aoki, M, Harada, K, Ogawa, M, Tanaka, T. Quantitative assessment of right ventricular function using Doppler tissue imaging in fetuses with and without heart failure. J Am Soc Echocardiogr 2004;17:28–35. https://doi.org/10.1016/j.echo.2003.09.012.Search in Google Scholar PubMed
34. Comas, M, Crispi, F. Assessment of fetal cardiac function using tissue Doppler techniques. Fetal Diagn Ther 2012;32:30–8. https://doi.org/10.1159/000335028.Search in Google Scholar PubMed
35. Comas, M, Crispi, F, Gomez, O, Puerto, B, Figueras, F, Gratacos, E. Gestational age- and estimated fetal weight-adjusted reference ranges for myocardial tissue Doppler indices at 24-41 weeks’ gestation. Ultrasound Obstet Gynecol 2011;37:57–64. https://doi.org/10.1002/uog.8870.Search in Google Scholar PubMed
36. McGraw, KO, Wong, SP. Forming inferences about some intraclass correlations coefficients (vol 1, pg 30, 1996). Psychol Methods 1996;1:390. https://doi.org/10.1037//1082-989x.1.4.390.Search in Google Scholar
37. Maheshwari, P, Alphonse, J, Henry, A, Wang, J, Redmond, SJ, Welsh, AW. Beat-to-beat variability of fetal myocardial performance index. Ultrasound Obstet Gynecol 2017;50:215–20. https://doi.org/10.1002/uog.16012.Search in Google Scholar PubMed
38. Avnet, H, Thomas, S, Beirne, G, Alphonse, J, Welsh, A. Poor correlation between fetal tissue Doppler imaging and pulsed wave myocardial performance indices. Fetal Diagn Ther 2023;50:225–35. https://doi.org/10.1159/000529945.Search in Google Scholar PubMed
39. Yagel, S, Cohen, SM, Shapiro, I, Valsky, DV. 3D and 4D ultrasound in fetal cardiac scanning: a new look at the fetal heart. Ultrasound Obstet Gynecol 2007;29:81–95. https://doi.org/10.1002/uog.3912.Search in Google Scholar PubMed
40. Gonçalves, LF, Lee, W, Espinoza, J, Romero, R. Examination of the fetal heart by four-dimensional (4D) ultrasound with spatio-temporal image correlation (STIC). Ultrasound Obstet Gynecol 2006;27:336–48. https://doi.org/10.1002/uog.2724.Search in Google Scholar PubMed
41. Amoozgar, H, Soltani, M, Borzoee, M, Ajami, G, Cheriki, S. Evaluation of pulsed Doppler-versus tissue Doppler-derived tei index of right and left ventricle in fetuses. Int Cardiovasc Res J 2011;5:134–8. https://doi.org/10.5812/icrj.3957.Search in Google Scholar
42. Sengupta, PP, Tajik, AJ, Chandrasekaran, K, Khandheria, BK. Twist mechanics of the left ventricle: principles and application. JACC Cardiovascular imaging 2008;1:366–76. https://doi.org/10.1016/j.jcmg.2008.02.006.Search in Google Scholar PubMed
© 2025 the author(s), published by De Gruyter, Berlin/Boston
This work is licensed under the Creative Commons Attribution 4.0 International License.
Articles in the same Issue
- Frontmatter
- Review
- Sex differences in lung function of adolescents or young adults born prematurely or of very low birth weight: a systematic review
- Original Articles – Obstetrics
- Shifts in peak month of births and socio-economic factors: a study of divided and reunified Germany 1950–2022
- The predictive role of serial transperineal sonography during the first stage of labor for cesarean section
- Gestational weight gain and obstetric outcomes in women with obesity in an inner-city population
- Placental growth factor as a predictive marker of preeclampsia in twin pregnancy
- Learning curve for the perinatal outcomes of radiofrequency ablation for selective fetal reduction: a single-center, 10-year experience from 2013 to 2023
- External validation of a non-invasive vaginal tool to assess the risk of intra-amniotic inflammation in pregnant women with preterm labor and intact membranes
- Placental fetal vascular malperfusion in maternal diabetes mellitus
- The importance of the cerebro-placental ratio at term for predicting adverse perinatal outcomes in appropriate for gestational age fetuses
- Comparing achievability and reproducibility of pulsed wave Doppler and tissue Doppler myocardial performance index and spatiotemporal image correlation annular plane systolic excursion in the cardiac function assessment of normal pregnancies
- Characteristics of the pregnancy and labour course in women who underwent COVID-19 during pregnancy
- Original Articles – Fetus
- Sonographic visualization and measurement of the fetal optic chiasm and optic tract and association with the cavum septum pellucidum
- The association among fetal head position, fetal head rotation and descent during the progress of labor: a clinical study of an ultrasound-based longitudinal cohort study in nulliparous women
- Fetal hypoplastic left heart syndrome: key factors shaping prognosis
- The value of ultrasound spectra of middle cerebral artery and umbilical artery blood flow in adverse pregnancy outcomes
- Original Articles – Neonates
- A family-centric, comprehensive nurse-led home oxygen programme for neonatal chronic lung disease: home oxygen policy evaluation (HOPE) study
- Effects of a respiratory function indicator light on visual attention and ventilation quality during neonatal resuscitation: a randomised controlled crossover simulation trial
- Short Communication
- Incidence and awareness of dysphoric milk ejection reflex (DMER)
Articles in the same Issue
- Frontmatter
- Review
- Sex differences in lung function of adolescents or young adults born prematurely or of very low birth weight: a systematic review
- Original Articles – Obstetrics
- Shifts in peak month of births and socio-economic factors: a study of divided and reunified Germany 1950–2022
- The predictive role of serial transperineal sonography during the first stage of labor for cesarean section
- Gestational weight gain and obstetric outcomes in women with obesity in an inner-city population
- Placental growth factor as a predictive marker of preeclampsia in twin pregnancy
- Learning curve for the perinatal outcomes of radiofrequency ablation for selective fetal reduction: a single-center, 10-year experience from 2013 to 2023
- External validation of a non-invasive vaginal tool to assess the risk of intra-amniotic inflammation in pregnant women with preterm labor and intact membranes
- Placental fetal vascular malperfusion in maternal diabetes mellitus
- The importance of the cerebro-placental ratio at term for predicting adverse perinatal outcomes in appropriate for gestational age fetuses
- Comparing achievability and reproducibility of pulsed wave Doppler and tissue Doppler myocardial performance index and spatiotemporal image correlation annular plane systolic excursion in the cardiac function assessment of normal pregnancies
- Characteristics of the pregnancy and labour course in women who underwent COVID-19 during pregnancy
- Original Articles – Fetus
- Sonographic visualization and measurement of the fetal optic chiasm and optic tract and association with the cavum septum pellucidum
- The association among fetal head position, fetal head rotation and descent during the progress of labor: a clinical study of an ultrasound-based longitudinal cohort study in nulliparous women
- Fetal hypoplastic left heart syndrome: key factors shaping prognosis
- The value of ultrasound spectra of middle cerebral artery and umbilical artery blood flow in adverse pregnancy outcomes
- Original Articles – Neonates
- A family-centric, comprehensive nurse-led home oxygen programme for neonatal chronic lung disease: home oxygen policy evaluation (HOPE) study
- Effects of a respiratory function indicator light on visual attention and ventilation quality during neonatal resuscitation: a randomised controlled crossover simulation trial
- Short Communication
- Incidence and awareness of dysphoric milk ejection reflex (DMER)

