Abstract
Background
We aim to investigate the protective effects and potential mechanisms in specneuzhenide (SPE) on renal injury in rats with diabetic nephropathy (DN).
Results
SPE could inhibit the decrease of body weight compared with the model group (P<0.05), and trigger improvement in the renal index (P<0.05). High dose and low dose SPE could trigger a significant decrease in serum IL1β, IL-6 and TNF-α compared with the model group (P<0.05). SPE could attenuate the glomerular lesions in DN rats. SPE induced up-regulation of podocin and CD2AP (P<0.05).
Conclusion
SPE showed protective effects on renal injury through attenuating the pathological injury and urine protein. This process may be closely related to the modulation of CD2AP and podocin expression.
1 Introduction
Diabetic nephropathy (DN), a common late-stage complication of diabetes mellitus, is one of the leading causes for end-stage renal disease [1, 2]. Nowadays, the incidence of DN is on an increasing trend. According to a recent survey, more than 100 million patients are suffering from DN [3]. To our best knowledge, the pathogenesis of DN is rather complex, involving genetic, metabolic, hemodynamic, oxidative stress and inflammatory factors. Nowadays, increasing interest has been given to the roles of podocyte injury. For example, the slit membrane serving as the last barrier for glomerular filtration, plays important roles in the generation of proteins [4]. The nephrin/ CD2AP/podocin complex is a key functional unit for the slit membrane. Nowadays, there are still lacking appropriate treatment options for DN, and most of the treatment options utilize the reduction of glucose, regulation of blood fat, and application of angiotensin converting enzyme inhibitor (ACEI) and angiotensin-receptor blocker (ARB) agents. Extensive studies have revealed that some active components of traditional Chinese medicine (TCM) could regulate glycometabolism and oxidative stress as these components are efficient in prevention and treatment of DN [5, 6, 7].
Specneuzhenide (SPE), an isomer of oleanolic acid, is extensively prevalent in herbal medicine and natural drugs. It has been reported to be involved in the anti-oxidation, anti-inflammation and decline of blood glucose [8]. Besides this, SPE has been approved to inhibit the expression of NF-κB in diabetic rats, which then inhibited the inflammatory reaction in the vascular tissues in the presence of diabetes [9, 10]. Moreover, SPE contributed to urine protein excretion and renal tissue pathological changes in diabetic rats. Furthermore, it may show protective effects on the kidneys through decreasing the tumor necrosis factor-α (TNF-α) and IL-6 that may inhibit the inflammation in renal tissues [11, 12]. In a previous study, SPE induced improvement of sugar tolerance and insulin resistance in KKAy mice, which may be associated with the elevation of GLUT4 protein transmission and expression in muscle cells.
In this study, a DN model was induced through Streptozotocin (STZ) and a high glucose/high fat diet. Then we investigated the effects of SPE of various concentrations on the pathogenesis of DN. We aim to investigate the protective effects of SPE on the pathogenesis of DN.
2 Methods
2.1 Animals
Male Sparague Dawely (SD) rats (specific pathogen free; weighing 220±20 g; approval No.: SYXK20130036) were provided by the Animal Center of Jiangsu University. The animals were housed in separated cages in a 12-h light/12-h dark cycle at a temperature of 23°C with a humidity of 40%. The animals were on a normal diet and had free access to food and water. All animal experimental protocols were carried out in compliance with the Ethics Committee of the Affiliated Hospital of Jiangsu University.
2.2 Establishing the DN model
The DN model was induced using a low dose of STZ and a high glucose-high fat diet according to the previous description [13]. Briefly, rats were fed on a diet containing high glucose and high fat for 4 weeks, followed by fasting for 12 hrs. STZ (1%, 60 mg/kg) was given via intraperitoneal injection. Blood sample collection was performed via the caudal vein to determine the blood glucose about 72 hrs after STZ treatment. A glucose level of ≥16.7 mmol/L was considered as DM.
2.3 Grouping
Thirty-six DN rats were randomly divided into the following groups: (i) model group (n=12) subject to distilled water via lavage per day, (ii) low dose SPE group, subject to SPE injection via lavage per day (30 mg/kg), and (iii) high dose SPE group, subject to SPE injection via lavage per day (60 mg/kg). The administration duration was 16 days in each group. Twelve normal mice with no DN induction were subjected to distilled water via lavage served as control.
2.4 Determination of blood glucose and urine protein
Blood glucose was determined after sample collection from the caudal veins on week 2, 5 and 8 after SPE treatment in high and low doses groups, or distilled water treatment in the model and control groups. Blood glucose was determined using a glucose device (Onetouch, Johnson & Johnson) according to the manufacturer’s instructions. The 24 h urine protein was determined using the commercial kit purchased from the Jiancheng Biotech (Category No. C035-2, Nanjing, China), according to the manufacturer’s instructions.
2.5 Evaluation of inflammatory factors, SOD, MDA and renal index
For the determination of inflammatory factors in serum and kidney, the blood samples (1.5 mL) were collected from the orbit of each rat, followed by centrifugation at 5,000 rpm for 10 min to collect the serum. About 1 hr after the last treatment, all rats were sacrificed to obtain the renal tissues. The tissues were homogenated at 12,000 rpm for 10 min to obtain the supernatant. The inflammatory factors including IL-1β, IL-6 and TNF-α were determined using ELISA kits purchased from Jiancheng Biotech (Nanjing, China).
To determine the SOD and MDA, the renal tissues were homogenated at 5,000 rpm at 4°C for 15 min to obtain the supernatant. Then the SOD and MDA was measured using the commercial kits purchased from Jiancheng Biotech (Nanjing, China), respectively.
To calculate the renal index, the kidneys were obtained, followed by drying the surface using a filter paper. Then the weight was determined, and the renal index was calculated using the following formula: renal index= renal weight/total body weight× 100 %.
2.6 HE and PAS staining
The renal cortex was fixed using 10% formaldehyde for 24 hrs, followed by dehydration in 70%, 80%, 90%, 95% and 100% ethanols for 30 min. Then the samples were embedded in paraffin. The sections (2 μm) were then subject to HE staining and PAS staining according to the previous description (Al-Amiri, Chatrath, Bhawan, & Stefanato, 2003; Fischer, Jacobson, Rose, & Zeller, 2008). The pathological changes were observed under a light microscope.
2.7 Western blot analysis
Total RNA was extracted from the renal tissues (60 mg) using RIPA lysis. Protein concentration was determined using a Bradord protein commercial kit. Protein (30 μg) was separated by 10% SDS-PAGE, and then the gel was transferred to a PVDF membrane. Membranes were blocked with 5% (w/v) milk in TBS-T buffer, followed by incubating with the rabbit anti-rat podocin antibody (1:1000, Abcam, CA, USA) and rabbit anti-rat CD2AP antibody (1:300, Abcam, CA, USA). The membrane was then incubated with HRP-conjugated secondary antibodies for 1h. The same membrane was probed for β-actin for loading control. The gray value was analyzed with the Quantity one v4.62 software (Bio-Rad, CA, USA).
2.8 Statistical analysis
All the data were presented as mean ± standard deviation. SPSS19.0 software was used for the statistical analysis. Analysis of variance was used for the comparison between groups. P<0.05 was considered to be statistically significant.
3 Results
3.1 Effects of SPE on glucose and urine protein in DN rats
3.1.1 SPE induced decline of blood glucose
No statistical differences were noticed in the blood glucose at the baseline levels among the four groups (P>0.05, Table 1). The blood glucose in the model group showed a significant increase at week 4, 8, 12 and 16 after DM induction compared with the control group (P<0.05, Table 1). In the SPE-L group, the blood glucose showed a decrease at week 12 and 16 compared with the model group (P<0.05). In the SPE-H group, compared with the model group, a significant decrease was noticed at week 4, 8, 12 and 16, respectively (P<0.05). These indicated that the SPE contributed to the decline of blood glucose.
Regulatory effects of SPE on glucose
| Group | Baseline | Week 4 | Week 8 | Week 12 | Week 16 |
|---|---|---|---|---|---|
| Control | 4.46 ± 0.02 | 4.49 ± 0.02 | 4.61 ± 0.08 | 4.51 ± 0.06 | 4.47 ± 0.03 |
| Model group | 4.48 ± 0.04 | 23.78 ± 0.21 | 25.53 ± 0.68 | 26.21 ± 0.62 | 25.30 ± 0.52* |
| SPE-L | 4.41 ± 0.02 | 23.34 ± 0.97 | 21.32 ± 0.96 | 16.96 ± 0.82 | 15.77 ± 0.79† |
| SPE-H | 4.45 ± 0.03 | 17.44 ± 0.68 | 12.78 ± 0.82 | 9.39 ± 0.64 | 8.46 ± 0.72† |
*P < 0.05 versus control; †P < 0.01 versus model group.
3.1.2 SPE induced significant decrease of 24h urine protein
Compared with normal control, a significant increase was noticed in the 24 h urine protein at week 4, 8, 12 and 16, respectively (P<0.01). Compared with the model group, significant improvement was noticed in the urine protein in SPE groups. At week 16, significant decrease was noticed in the 24 h urine protein in high dose group and low dose group compared with that of the model group (P<0.05, Table 2).
Comparison of 24 h urine protein in each group
| Group | Baseline | Week 4 | Week 8 | Week 12 | Week 16 |
|---|---|---|---|---|---|
| Control | 7.02 ± 0.63 | 7.68 ± 0.03 | 6.81 ± 0.16 | 6.42 ± 0.06 | 7.37 ± 0.23 |
| Model group | 7.37 ± 0.42 | 26.88 ± 0.49 | 28.44 ± 0.10 | 28.40 ± 0.25 | 32.64 ± 0.41* |
| SPE -L | 7.28 ± 0.61 | 24.55 ± 0.83 | 26.88 ± 0.94 | 25.98 ± 0.81 | 25.01 ± 0.86 † |
| SPE -H | 7.14 ± 0.64 | 21.39 ± 0.72 | 23.47 ± 0.73 | 24.49 ±0.75 | 21.76 ± 0.95 † |
*P < 0.01 versus control; †P < 0.05 versus model group.
3.1.3 Effects of SPE on the body weight, renal weight and renal index in DM rats
Compared with the normal control, the body weight in the model group showed a significant decrease, especially the weight of kidney and renal index (P<0.01). In the SPE-H group, a significant increase was noticed in the body weight compared with the model group (P<0.05). Besides this, a high dose of SPE contributed to the decrease of kidney weight and renal index compared with the model group. In contrast, low dose of SPE induced no statistical differences in the body weight, kidney weight and renal index compared with the model group (P>0.05, Table 3).
Effects of SPE on body weight, renal weight and index in DN rats
| Group | Weight (g) | Renal weight (g) | Renal index (×100) |
|---|---|---|---|
| Control | 406.32 ± 11.54 | 1.57 ± 0.04 | 0.38 ± 0.0045 |
| Model group | 327.83 ± 4.83 * | 1.74 ± 0.05 * | 0.53 ± 0.0201 * |
| SPE-L | 336.73 ± 3.09 | 1.66 ± 0.09 | 0.49 ± 0.0112 |
| SPE-H | 355.60 ± 5.19 † | 1.60 ± 0.12 † | 0.45 ± 0.0105 † |
*P < 0.05 versus control; †P < 0.01 versus model group.
3.2 SPE modulated the expression of inflammatory factors in DN rats
3.2.1 Effects of SPE on the inflammatory factors in serum and renal tissues in DM rats
Serum IL-1β showed significant elevation in the model group compared with that of the control group (P<0.05). Compared with the model group, a significant decrease was noticed in the IL-1β in SPE-H and SPE-L groups (P<0.05, Table 4).
Regulatory effects of SPE on serum IL-1β, IL-6 and TNF-α
| Group | Serum IL-1β (pg/mL) | Serum IL-6 (pg/mL) | Serum TNF-α (pg/mL) |
|---|---|---|---|
| Control | 10.10 ± 2.18 | 20.64 ± 2.03 | 16.96 ± 5.23 |
| Model group | 35.06 ± 3.18 * | 40.10 ± 2.72 * | 41.27 ± 3.02 * |
| SPE-L | 27.45 ± 1.66 † | 36.05 ± 1.49 | 32.33 ± 5.84 † |
| SPE-H | 26.34 ± 1.32 # | 32.80 ± 1.52 † | 27.98 ± 4.25 # |
*P < 0.05 versus control; †P < 0.05 versus model group; #P < 0.01 versus model group.
Serum IL-6 in the model group showed significant elevation compared with that of normal control (P<0.05, Table 4). Compared with the model group, the serum IL-6 in the SPE-H group showed a significant decrease (P<0.05). Compared with the model group, no statistical differences were noticed in the serum IL-6 in the SPE-L group (P>0.05, Table 4).
The TNF-α expression in the model group showed significant elevation compared to the normal control (P<0.05). Compared with the model group, a significant decline of TNF-α in DM rats was noticed in the SPE-H group (P<0.01). Compared with the model group, TNF-α in the SPE-L group showed a significant decrease (P<0.05, Table 4).
3.2.2 Effects of SPE on the IL-1β, IL-6 and TNF-α expression in renal tissues
Compared with the normal control, the level of IL-1β in renal tissues of DM rats showed significant increase in the model group. Nevertheless, compared with the model group, a significant decrease was noticed in IL-1β expression in renal tissues in the SPE-H and SPE-L groups, respectively (P<0.05, Table 5).
Regulatory effects of SPE on renal IL-1β, IL-6, SOD, MDA, podocin and CD2AP
| Group | Renal IL-1β (pg/mL) | Renal IL-6 (pg/mL) | Renal TNF-α (pg/mL) | Renal SOD (U/mL) | Renal MDA (nmol/mL) | Renal podocin | Renal CD2AP |
|---|---|---|---|---|---|---|---|
| Control | 3.67 ± 0.37 | 6.80 ± 0.62 | 4.71 ± 0.89 | 22.57 ± 0.08 | 36.56 ± 9.26 | 0.70 ±0.03 | 0.73 ± 0.02 |
| Model group | 9.59 ± 1.37 * | 9.71 ± 0.39 * | 11.06 ± 0.32 * | 9.09 ± 0.81 * | 91.56 ± 8.56 * | 0.06 ± 0.02 * | 0.07 ± 0.03 * |
| SPE-L | 7.37 ± 0.79 † | 9.65 ± 0.74 | 10.74 ± 0.86 | 16.43 ± 0.92 † | 67.48 ± 5.71 † | 0.21 ±0.03 † | 0.19 ± 0.04 † |
| SPE-H | 5.55 ± 0.67 △ | 7.23 ± 0.56 † | 8.17 ± 0.75 # | 22.31 ± 0.99 † | 53.68 ± 7.44 † | 0.51 ±0.05 3 | 0.49 ± 0.05 # |
*P < 0.05 versus control; †P < 0.05 versus model group; #P < 0.01 versus model group.
Compared with the normal control, a significant increase was noticed in IL-6 and TNF-α in renal tissues in model group (P<0.05, Table 5). IL-6 and TNF-α in renal tissues of DM rats showed significant decrease in SPE-H group compared with model group (P<0.05). In contrast, no statistical difference was noticed in the IL-6 and TNF-α in renal tissues of the SPE-L group compared with the model group (P>0.05, Table 5).
3.3 SPE affected the anti-oxidative stress in DN rats
3.3.1 Effects of SPE on the anti-oxidant indices in renal tissues of DM rats
Compared with the normal control, the SOD activity in renal tissues of the model group showed a significant decrease (P<0.05, Table 5). Compared with the model group, the SOD activity in the SPE-L and SPE-H groups showed significant elevation. This implied that SPE induced satisfactory anti-oxidant capacity.
Compared with the normal control, the MDA content in renal tissues showed significant elevation in the model group (P<0.05). The MDA activity in the renal tissues in the SPE-H and SPE-L groups showed a significant increase compared with the model group (P<0.01, Table 5). These indicated that SPE played important roles in anti-oxidation and modulation of renal injury.
3.4 SPE showed protective effects on the podocyte injury in DN rats
3.4.1 Expression of CD2AP and Podocin protein
SPE could obviously improve the expression of Podocin and CD2AP in the podocytes. Compared with the normal control, a significant decrease was observed in the expression of Podocin and CD2AP protein in the renal tissues in the model group (P<0.01). Compared with the model group, significant upregulation was noticed in the expression of Podocin and CD2AP protein in the renal tissues of the SPE-H group and SPE-L group, respectively (P<0.05, Table 5).
3.5 Protective effects of SPE on the renal function in DN rats
3.5.1 HE staining results
For HE staining, the morphology of the kidney in the normal control was normal. The anatomical structure was clear. The morphology of the renal glomerulus was regular. No dilatation was noticed in the capillary lumen. The arrangement of the renal tubule was regular and tight. The morphology of epithelial cells in the renal tubule was normal. No atrophy or hypertrophy was noticed in the renal glomerulus. Basilar membrane and mesenterium showed no thickening. Compared with the normal control, the glomerular volume in the model group showed enlargement. Obvious thickening was observed in the capillary basement membrane. The matrix of the mesenterium showed obvious hyperplasia. Vacuolation was noticed in the renal tubular epithelial cells, in which protein was observed. In the SPE treatment groups, the pathological changes showed attenuation in DM rats to some extent. Besides this, the morphology of the renal glomerulus was normal. Part of the basilar membrane showed thickening. Slight hyperplasia was noticed in the mesenterium. Few renal tubular epithelial cells showed vacuolation. Compared with the model groups, significant attenuation was noticed in the pathological changes in the SPE groups (Figure 1).
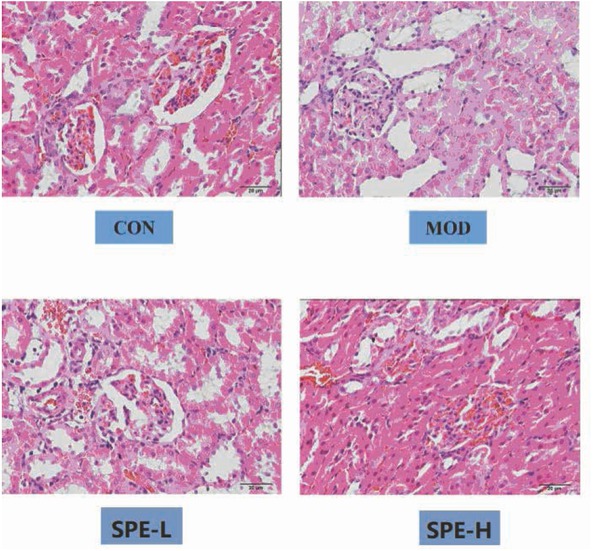
HE staining indicating the pathological changes in renal tissues. CON, control; MOD: model group; SPE-L, low dose group of SPE; SPE-H, high dose group of SPE.
3.5.2 PAS staining results
PAS staining results indicated that the ratio of area in renal tissues with positive staining showed significant elevation in the model group compared with the normal control. Compared with model group, the ratio showed significant decrease in the SPE groups, which were featured by inhibition of enlargement of renal glomerular volume, basilar membrane thickening and mesenteric hyperplasia (Figure 2).
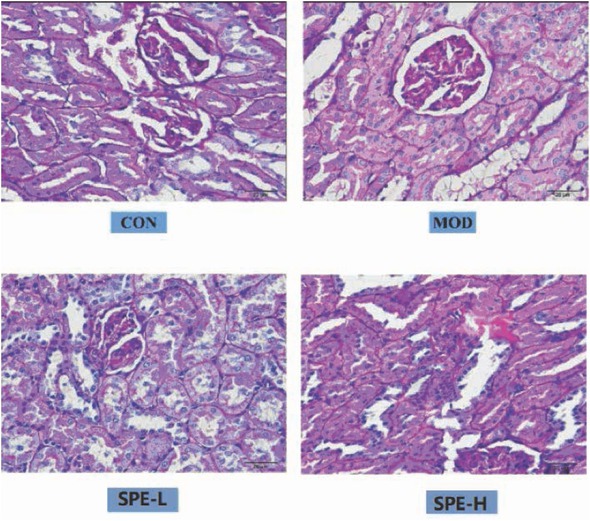
PAS staining for the pathological changes in renal tissues. CON, control; MOD: model group; SPE-L, low dose group of SPE; SPE-H, high dose group of SPE.
4 Discussion
In this study, the DN model was induced by STZ and a high glucose or high fat diet. Then we determined the expression of inflammatory factors (e.g. IL-1β, IL-6 and TNF-α) and podocyte related protein (e.g. podocin and CD2AP), as well as the pathological changes in the kidney. We investigated the potential effects of SPE on the DN.
SPE could effectively attenuate the blood glucose and the expression of inflammatory factors in serum and renal tissues. Besides this, it could enhance the anti-oxidant capacity of renal tissues, which then contributed to the improvement of renal function and renal protection. According to the previous description, high glucose was involved in mediating the oxidative stress, which participated in the pathogenesis and development of DNA [14, 15]. Reactive oxygen species (ROS) accumulation was a crucial feature for DN. ROS induced the generation of lipid peroxidation products such as MDA, hydroxyl groups and ketone groups, which then led to renal injury by modulating the oxidation of amino acids and protein. As a type of antioxidase, SOD was reported to reflex the clearance of free radicals and the anti-oxidant capacity that may involve in the protection of cells from injury [16]. To our best knowledge, the decrease of anti-oxidant capacity was an important indicator for oxidative stress [17]. In this study, compared with the normal control, the MDA in renal tissues showed a significant increase (P<0.01), and SOD activity showed a significant decrease (P<0.01) in the model group. This implied that oxidative stress in renal tissues showed a significant increase in DN rats. However, after SPE treatment, blood glucose and MDA in renal tissues showed a significant decline compared with the model group. A significant elevation was also noticed in SOD activity. This implied that SPE showed satisfactory anti-oxidant capacity and brought down the blood glucose, which was in line with the previous descriptions.
For the pathogenesis of inflammatory injury in DN, elevation of oxidative stress and hemokinesis imbalance mediated the infiltration of white blood cells, macrophages and T-lymphocytes, which contributed to the release of inflammatory cells including IL-1, IL-6, IL-1β, TNF-α and INF-γ [18]. These inflammatory factors could further induce the generation of chemotactic factor in renal tissues, which then induced the infiltration of inflammatory cells. Finally, such process may trigger a severe injury in renal tissues. As an important factor for renal injury, TNF-α triggered the overexpression of various inflammatory factors and chemotactic factors (e.g. IL-6) [19]. Besides, it may enhance the inflammatory reactions. The generated IL-6 may induce the expression of factors associated with fibrosis, which then resulted in hypertrophy and fibrosis of renal tissues [20]. Moreover, overexpression of IL-6 in DN induced changes of permeability of the renal endothelium, which contributed to the expression of fibronectin and thickening of the glomerular basement membrane [21]. In this study, the basic structure injuries that induced inflammation and cellular infiltration were obvious in the renal tissues of DN rats, while the expression of TNF-α and IL-6 in the renal tissues showed a significant increase, which then induced the significant down-regulation of renal function. Administration of SPE (16-week) could obviously inhibit the infiltration of inflammatory cells, and down-regulate the IL-6 and TNF-α. These triggered the gradual improvement of the renal function. Therefore, we speculated that SPE could inhibit the inflammatory factors induced renal injury through inhibiting the expression of inflammatory factors such as TNF-α, IL-6 and IL-1β.
Podocytes, the highly differentiated terminal cells of glomerular basement membrane, are important components for the glomerular filtration barrier [22]. These cells have been reported to be closely related to the pathogenesis of DN. Besides, the podocytes-associated proteins were regarded to be associated with podocyte skeletal framework [23]. For instance, Podocin, CD2AP and nephrin could form a protein complex, which is then involved in the maintenance of the slit diaphragm and podocyte skeletal framework stability [24]. The expression of nephrin, Podocin and CD2AP was significantly down-regulated in the renal tissues of DN patients, which then resulted in the injury of the slit diaphragm and an increase of urine protein [25]. In this study, the expression of Podocin and CD2AP showed significant up-regulation in SPE groups compared with the model group. The urine protein also showed significant decrease after SPE treatment compared with the model group (P<0.05). On this basis, we speculated that SPE could up-regulate the expression of Podocin and CD2AP, which then led to stabilization of the slit diaphragm and protection of the renal function in DN rats.
Indeed, there are some limitations in this study. Although we revealed the protective effects of SPE on podocyte function, we did not present the morphological changes of these cells. In future, we will add such information, in order to further present the potential mechanisms in this process.
5 Conclusions
In summary, SPE contributed to the attenuation of urine protein content, which then obviously decreased the blood glucose in DN rats. Additionally, SPE could up-regulate the expression of CD2AP and Podocin in the slit membrane in the renal tissues of DN rats. This implied that SPE could up-regulate the Podocin and CD2AP expression, which could protect the renal function in DN rats. The protective effects of SPE on the attenuation of urine protein and protection of renal function were associated with the renal podocytes and the expression of CD2AP and Podocin in the slit membrane.
-
Funding: This study was supported by the Key Research and Development Program (Social Development) of Zhenjiang City (No. SH2018054) and the Talent Program of the Affiliated Hospital of Jiangsu University (No. jdfyRC2018012).
-
Data availability: All the data were available upon appropriate request.
-
Authorship: YJN draft the work and revised it critically for important intellectual content; LGY finally approved the version to be published; JJ did substantial contributions to the conception, design of the work, the acquisition, analysis, and interpretation of data for the work; WHJ agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
-
Conflict of interest: The author(s) declare(s) that there is no conflict of interest regarding the publication of this paper.
Abbreviations
- DN
diabetic nephropathy;
- ROS
reactive oxygen species;
- SD
sparague Dawely;
- SPE
specneuzhenide;
- STZ
streptozotocin;
- TNF-α
tumor necrosis factor-α
References
[1] Saran R L.Y., Robinson B., US renal data system 2014 annual data report: Epidemiology of kidney disease in the United States, Am J Kidney Dis, 2015, 66, Svii,S1-30510.1053/j.ajkd.2015.05.001Suche in Google Scholar
[2] de Boer I.H., Rue T.C., Hall Y.N., Heagerty P.J., Weiss N.S., Himmelfarb J., Temporal trends in the prevalence of diabetic kidney disease in the United States, Jama, 2011, 305, 2532-2539; DOI: 10.1001/jama.2011.86110.1001/jama.2011.861Suche in Google Scholar
[3] Reutens A.T., Atkins R.C., Epidemiology of diabetic nephropathy, Contrib Nephrol, 2011, 170, 1-7; DOI: 10.1159/00032493410.1159/000324934Suche in Google Scholar
[4] Saurus P., Tolvanen T.A., Lindfors S., Kuusela S., Holthofer H., Lehtonen E., et al., Inhibition of SHIP2 in CD2AP-deficient podocytes ameliorates reactive oxygen species generation but aggravates apoptosis, 2017, 7, 10731; DOI: 10.1038/s41598-017-10512-w10.1038/s41598-017-10512-wSuche in Google Scholar
[5] Akash M.S., Rehman K., Chen S., Effects of coffee on type 2 diabetes mellitus, Nutrition, 2014, 30, 755-763; DOI: 10.1016/j.nut.2013.11.02010.1016/j.nut.2013.11.020Suche in Google Scholar
[6] Akash M.S., Rehman K., Chen S., Spice plant Allium cepa: dietary supplement for treatment of type 2 diabetes mellitus, Nutrition, 2014, 30, 1128-1137; DOI: 10.1016/j.nut.2014.02.01110.1016/j.nut.2014.02.011Suche in Google Scholar
[7] Akash M.S., Rehman K., Tariq M., Chen S., Zingiber officinale and Type 2 Diabetes Mellitus: Evidence from Experimental Studies, Crit Rev Eukaryot Gene Expr, 2015, 25, 91-11210.1615/CritRevEukaryotGeneExpr.2015013358Suche in Google Scholar
[8] Li H.F., Zhang X.L., [Comparation of gastrointestinal absorption studies of specnuezhenide with salidroside in rats], Zhongguo Zhong Yao Za Zhi, 2014, 39, 1107-1110Suche in Google Scholar
[9] Chen B., Wang L., Li L., Zhu R., Liu H., Liu C., et al., Fructus Ligustri Lucidi in Osteoporosis: A Review of its Pharmacology, Phytochemistry, Pharmacokinetics and Safety, Molecules, 2017, 22; DOI: 10.3390/molecules2209146910.3390/molecules22091469Suche in Google Scholar
[10] Shi L., Ma Y., Cai Z., Quantitative determination of salidroside and specnuezhenide in the fruits of Ligustrum lucidum Ait by high performance liquid chromatography, Biomed Chromatogr, 1998, 12, 27-30; 10.1002/(sici)1099-0801(199801/02)12:1<27::aid-bmc715>3.0.co;2-e10.1002/(SICI)1099-0801(199801/02)12:1<27::AID-BMC715>3.0.CO;2-ESuche in Google Scholar
[11] Zhong X., Zhong Y., Yan K., Xiao X., Duan L., Wang R., et al., Metabolomics approach based on ultra-high-performance liquid chromatography coupled with quadrupole-time-of-flight mass spectrometry to identify the chemical constituents of the Traditional Chinese Er-Zhi-Pill, J Sep Sci, 2017, 40, 2713-2721; DOI: 10.1002/jssc.20160142510.1002/jssc.201601425Suche in Google Scholar
[12] Li C.Q., Yao C., Zhu R.Y., Huang Y.X., Kang W.Y., Wang J.M., [Spectrum-effect relationship in antioxidant activity of Ligustri Lucidi Fructus based on DPPH, ABTS and FRAP assays], Zhongguo Zhong Yao Za Zhi, 2016, 41, 1670-1677; DOI: 10.4268/cjcmm2016091710.4268/cjcmm20160917Suche in Google Scholar PubMed
[13] Kitada M., Ogura Y., Koya D., Rodent models of diabetic nephropathy: their utility and limitations, Int J Nephrol Renovasc Dis, 2016, 9, 279-290; DOI: 10.2147/ijnrd.s10378410.2147/ijnrd.s103784Suche in Google Scholar
[14] Mima A., Inflammation and oxidative stress in diabetic nephropathy: new insights on its inhibition as new therapeutic targets, J Diabetes Res, 2013, 2013, 248563; DOI: 10.1155/2013/24856310.1155/2013/248563Suche in Google Scholar PubMed PubMed Central
[15] Hui L., Hong Y., Jingjing Z., Yuan H., Qi C., Nong Z., HGF suppresses high glucose-mediated oxidative stress in mesangial cells by activation of PKG and inhibition of PKA, Free Radic Biol Med, 2010, 49, 467-473; DOI: 10.1016/j.freeradbiomed.2010.05.00210.1016/j.freeradbiomed.2010.05.002Suche in Google Scholar PubMed
[16] Kim G.H., Kim J.E., Rhie S.J., Yoon S., The Role of Oxidative Stress in Neurodegenerative Diseases, Exp Neurobiol, 2015, 24, 325-340; DOI: 10.5607/en.2015.24.4.32510.5607/en.2015.24.4.325Suche in Google Scholar PubMed PubMed Central
[17] Victorino V.J., Panis C., Campos F.C., Cayres R.C., Colado-Simao A.N., Oliveira S.R., et al., Decreased oxidant profile and increased antioxidant capacity in naturally postmenopausal women, Age (Dordr), 2013, 35, 1411-1421; DOI: 10.1007/s11357-012-9431-910.1007/s11357-012-9431-9Suche in Google Scholar PubMed PubMed Central
[18] Pop-Busui R., Sima A., Stevens M., Diabetic neuropathy and oxidative stress, Diabetes Metab Res Rev, 2006, 22, 257-273; DOI: 10.1002/dmrr.62510.1002/dmrr.625Suche in Google Scholar PubMed
[19] Ramesh G., Reeves W.B., Inflammatory cytokines in acute renal failure, Kidney Int Suppl, 2004, S56-61; DOI: 10.1111/j.1523-1755.2004.09109.x10.1111/j.1523-1755.2004.09109.xSuche in Google Scholar PubMed
[20] Wynn T.A., Cellular and molecular mechanisms of fibrosis, J Pathol, 2008, 214, 199-210; DOI: 10.1002/path.227710.1002/path.2277Suche in Google Scholar PubMed PubMed Central
[21] Navarro-Gonzalez J.F., Mora-Fernandez C., The role of inflammatory cytokines in diabetic nephropathy, J Am Soc Nephrol, 2008, 19, 433-442; DOI: 10.1681/asn.200709104810.1681/asn.2007091048Suche in Google Scholar PubMed
[22] Arif E., Nihalani D., Glomerular Filtration Barrier Assembly: An insight, Postdoc J, 2013, 1, 33-45;10.14304/SURYA.JPR.V1N4.4Suche in Google Scholar
[23] Reiser J., Altintas M.M., Podocytes, F1000Res, 2016, 5; DOI: 10.12688/f1000research.7255.110.12688/f1000research.7255.1Suche in Google Scholar PubMed PubMed Central
[24] Li C., Ruotsalainen V., Tryggvason K., Shaw A.S., Miner J.H., CD2AP is expressed with nephrin in developing podocytes and is found widely in mature kidney and elsewhere, Am J Physiol Renal Physiol, 2000, 279, F785-792; DOI: 10.1152/ajprenal.2000.279.4.F78510.1152/ajprenal.2000.279.4.F785Suche in Google Scholar PubMed
[25] Jim B., Ghanta M., Qipo A., Fan Y., Chuang P.Y., Cohen H.W., et al., Dysregulated nephrin in diabetic nephropathy of type 2 diabetes: a cross sectional study, PLoS One, 2012, 7, e36041; DOI: 10.1371/journal.pone.003604110.1371/journal.pone.0036041Suche in Google Scholar PubMed PubMed Central
© 2019 Jiangning Yin et al., published by De Gruyter
This work is licensed under the Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Artikel in diesem Heft
- Research Article
- Prostate Cancer-Specific of DD3-driven oncolytic virus-harboring mK5 gene
- Case Report
- Pediatric acute paradoxical cerebral embolism with pulmonary embolism caused by extremely small patent foramen ovale
- Research Article
- Associations between ambient temperature and acute myocardial infarction
- Case Report
- Discontinuation of imatinib mesylate could improve renal impairment in chronic myeloid leukemia
- Research Article
- METTL3 promotes the proliferation and mobility of gastric cancer cells
- The C677T polymorphism of the methylenetetrahydrofolate reductase gene and susceptibility to late-onset Alzheimer’s disease
- microRNA-1236-3p regulates DDP resistance in lung cancer cells
- Review Article
- The link between thyroid autoimmunity, depression and bipolar disorder
- Research Article
- Effects of miR-107 on the Chemo-drug sensitivity of breast cancer cells
- Analysis of pH dose-dependent growth of sulfate-reducing bacteria
- Review Article
- Musculoskeletal clinical and imaging manifestations in inflammatory bowel diseases
- Research Article
- Regional hyperthermia combined with chemotherapy in advanced gastric cancer
- Analysis of hormone receptor status in primary and recurrent breast cancer via data mining pathology reports
- Morphological and isokinetic strength differences: bilateral and ipsilateral variation by different sport activity
- The reliability of adjusting stepped care based on FeNO monitoring for patients with chronic persistent asthma
- Comparison of the clinical outcomes of two physiological ischemic training methods in patients with coronary heart disease
- Analysis of ticagrelor’s cardio-protective effects on patients with ST-segment elevation acute coronary syndrome accompanied with diabetes
- Computed tomography findings in patients with Samter’s Triad: an observational study
- Case Report
- A spinal subdural hematoma induced by guidewire-based lumbar drainage in a patient with ruptured intracranial aneurysms
- Research Article
- High expression B3GAT3 is related with poor prognosis of liver cancer
- Effects of light touch on balance in patients with stroke
- Oncoprotein LAMTOR5 activates GLUT1 via upregulating NF-κB in liver cancer
- Effects of budesonide combined with noninvasive ventilation on PCT, sTREM-1, chest lung compliance, humoral immune function and quality of life in patients with AECOPD complicated with type II respiratory failure
- Prognostic significance of lymph node ratio in ovarian cancer
- Case Report
- Brainstem anaesthesia after retrobulbar block
- Review Article
- Treating infertility: current affairs of cross-border reproductive care
- Research Article
- Serum inflammatory cytokines comparison in gastric cancer therapy
- Behavioural and psychological symptoms in neurocognitive disorders: Specific patterns in dementia subtypes
- MRI and bone scintigraphy for breast cancer bone metastase: a meta-analysis
- Comparative study of back propagation artificial neural networks and logistic regression model in predicting poor prognosis after acute ischemic stroke
- Analysis of the factors affecting the prognosis of glioma patients
- Compare fuhrman nuclear and chromophobe tumor grade on chromophobe RCC
- Case Report
- Signet ring B cell lymphoma: A potential diagnostic pitfall
- Research Article
- Subparaneural injection in popliteal sciatic nerve blocks evaluated by MRI
- Loneliness in the context of quality of life of nursing home residents
- Biological characteristics of cervical precancerous cell proliferation
- Effects of Rehabilitation in Bankart Lesion in Non-athletes: A report of three cases
- Management of complications of first instance of hepatic trauma in a liver surgery unit: Portal vein ligation as a conservative therapeutic strategy
- Matrix metalloproteinase 2 knockdown suppresses the proliferation of HepG2 and Huh7 cells and enhances the cisplatin effect
- Comparison of laparoscopy and open radical nephrectomy of renal cell cancer
- Case Report
- A severe complication of myocardial dysfunction post radiofrequency ablation treatment of huge hepatic hemangioma: a case report and literature review
- Solar urticaria, a disease with many dark sides: is omalizumab the right therapeutic response? Reflections from a clinical case report
- Research Article
- Binge eating disorder and related features in bariatric surgery candidates
- Propofol versus 4-hydroxybutyric acid in pediatric cardiac catheterizations
- Nasointestinal tube in mechanical ventilation patients is more advantageous
- The change of endotracheal tube cuff pressure during laparoscopic surgery
- Correlation between iPTH levels on the first postoperative day after total thyroidectomy and permanent hypoparathyroidism: our experience
- Case Report
- Primary angiosarcoma of the kidney: case report and comprehensive literature review
- Research Article
- miR-107 enhances the sensitivity of breast cancer cells to paclitaxel
- Incidental findings in dental radiology are concerning for family doctors
- Suffering from cerebral small vessel disease with and without metabolic syndrome
- A meta-analysis of robot assisted laparoscopic radical prostatectomy versus laparoscopic radical prostatectomy
- Indications and outcomes of splenectomy for hematological disorders
- Expression of CENPE and its prognostic role in non-small cell lung cancer
- Barbed suture and gastrointestinal surgery. A retrospective analysis
- Using post transplant 1 week Tc-99m DTPA renal scan as another method for predicting renal graft failure
- The pseudogene PTTG3P promotes cell migration and invasion in esophageal squamous cell carcinoma
- Lymph node ratio versus TNM system as prognostic factor in colorectal cancer staging. A single Center experience
- Review Article
- Minimally invasive pilonidal sinus treatment: A narrative review
- Research Article
- Anatomical workspace study of Endonasal Endoscopic Transsphenoidal Approach
- Hounsfield Units on Lumbar Computed Tomography for Predicting Regional Bone Mineral Density
- Communication
- Aspirin, a potential GLUT1 inhibitor in a vascular endothelial cell line
- Research Article
- Osteopontin and fatty acid binding protein in ifosfamide-treated rats
- Familial polyposis coli: the management of desmoid tumor bleeding
- microRNA-27a-3p down-regulation inhibits malignant biological behaviors of ovarian cancer by targeting BTG1
- PYCR1 is associated with papillary renal cell carcinoma progression
- Prediction of recurrence-associated death from localized prostate cancer with a charlson comorbidity index–reinforced machine learning model
- Colorectal cancer in the elderly patient: the role of neo-adjuvant therapy
- Association between MTHFR genetic polymorphism and Parkinson’s disease susceptibility: a meta-analysis
- Metformin can alleviate the symptom of patient with diabetic nephropathy through reducing the serum level of Hcy and IL-33
- Case Report
- Severe craniofacial trauma after multiple pistol shots
- Research Article
- Echocardiography evaluation of left ventricular diastolic function in elderly women with metabolic syndrome
- Tailored surgery in inguinal hernia repair. The role of subarachnoid anesthesia: a retrospective study
- The factors affecting early death in newly diagnosed APL patients
- Review Article
- Oncological outcomes and quality of life after rectal cancer surgery
- Research Article
- MiR-638 repressed vascular smooth muscle cell glycolysis by targeting LDHA
- microRNA-16 via Twist1 inhibits EMT induced by PM2.5 exposure in human hepatocellular carcinoma
- Analyzing the semantic space of the Hippocratic Oath
- Fournier’s gangrene and intravenous drug abuse: an unusual case report and review of the literature
- Evaluation of surgical site infection in mini-invasive urological surgery
- Dihydromyricetin attenuates inflammation through TLR4/NF-kappaB pathway
- Clinico-pathological features of colon cancer patients undergoing emergency surgery: a comparison between elderly and non-elderly patients
- Case Report
- Appendix bleeding with painless bloody diarrhea: A case report and literature review
- Research Article
- Protective effects of specneuzhenide on renal injury in rats with diabetic nephropathy
- PBF, a proto-oncogene in esophageal carcinoma
- Use of rituximab in NHL malt type pregnant in I° trimester for two times
- Cancer- and non-cancer related chronic pain: from the physiopathological basics to management
- Case report
- Non-surgical removal of dens invaginatus in maxillary lateral incisor using CBCT: Two-year follow-up case report
- Research Article
- Risk factors and drug resistance of the MDR Acinetobacter baumannii in pneumonia patients in ICU
- Accuracy of tumor perfusion assessment in Rat C6 gliomas model with USPIO
- Lemann Index for Assessment of Crohn’s Disease: Correlation with the Quality of Life, Endoscopic Disease activity, Magnetic Resonance Index of Activity and C- Reactive Protein
- Case report
- Münchausen syndrome as an unusual cause of pseudo-resistant hypertension: a case report
- Research Article
- Renal artery embolization before radical nephrectomy for complex renal tumour: which are the true advantages?
- Prognostic significance of CD276 in non-small cell lung cancer
- Potential drug-drug interactions in acute ischemic stroke patients at the Neurological Intensive Care Unit
- Effect of vitamin D3 on lung damage induced by cigarette smoke in mice
- CircRNA-UCK2 increased TET1 inhibits proliferation and invasion of prostate cancer cells via sponge miRNA-767-5p
- Case report
- Partial hydatidiform mole and coexistent live fetus: a case report and review of the literature
- Research Article
- Effect of NGR1 on the atopic dermatitis model and its mechanisms
- Clinical features of infertile men carrying a chromosome 9 translocation
- Review Article
- Expression and role of microRNA-663b in childhood acute lymphocytic leukemia and its mechanism
- Case Report
- Mature cystic teratoma of the pancreas: A rare cystic neoplasm
- Research Article
- Application of exercised-based pre-rehabilitation in perioperative period of patients with gastric cancer
- Case Report
- Predictive factors of intestinal necrosis in acute mesenteric ischemia
- Research Article
- Application of exercised-based pre-rehabilitation in perioperative period of patients with gastric cancer
- Effects of dexmedetomidine on the RhoA /ROCK/ Nox4 signaling pathway in renal fibrosis of diabetic rats
- MicroRNA-181a-5p regulates inflammatory response of macrophages in sepsis
- Intraventricular pressure in non-communicating hydrocephalus patients before endoscopic third ventriculostomy
- CyclinD1 is a new target gene of tumor suppressor miR-520e in breast cancer
- CHL1 and NrCAM are primarily expressed in low grade pediatric neuroblastoma
- Epidemiological characteristics of postoperative sepsis
- Association between unstable angina and CXCL17: a new potential biomarker
- Cardiac strains as a tool for optimization of cardiac resynchronization therapy in non-responders: a pilot study
- Case Report
- Resuscitation following a bupivacaine injection for a cervical paravertebral block
- Research Article
- CGF treatment of leg ulcers: A randomized controlled trial
- Surgical versus sequential hybrid treatment of carotid body tumors
Artikel in diesem Heft
- Research Article
- Prostate Cancer-Specific of DD3-driven oncolytic virus-harboring mK5 gene
- Case Report
- Pediatric acute paradoxical cerebral embolism with pulmonary embolism caused by extremely small patent foramen ovale
- Research Article
- Associations between ambient temperature and acute myocardial infarction
- Case Report
- Discontinuation of imatinib mesylate could improve renal impairment in chronic myeloid leukemia
- Research Article
- METTL3 promotes the proliferation and mobility of gastric cancer cells
- The C677T polymorphism of the methylenetetrahydrofolate reductase gene and susceptibility to late-onset Alzheimer’s disease
- microRNA-1236-3p regulates DDP resistance in lung cancer cells
- Review Article
- The link between thyroid autoimmunity, depression and bipolar disorder
- Research Article
- Effects of miR-107 on the Chemo-drug sensitivity of breast cancer cells
- Analysis of pH dose-dependent growth of sulfate-reducing bacteria
- Review Article
- Musculoskeletal clinical and imaging manifestations in inflammatory bowel diseases
- Research Article
- Regional hyperthermia combined with chemotherapy in advanced gastric cancer
- Analysis of hormone receptor status in primary and recurrent breast cancer via data mining pathology reports
- Morphological and isokinetic strength differences: bilateral and ipsilateral variation by different sport activity
- The reliability of adjusting stepped care based on FeNO monitoring for patients with chronic persistent asthma
- Comparison of the clinical outcomes of two physiological ischemic training methods in patients with coronary heart disease
- Analysis of ticagrelor’s cardio-protective effects on patients with ST-segment elevation acute coronary syndrome accompanied with diabetes
- Computed tomography findings in patients with Samter’s Triad: an observational study
- Case Report
- A spinal subdural hematoma induced by guidewire-based lumbar drainage in a patient with ruptured intracranial aneurysms
- Research Article
- High expression B3GAT3 is related with poor prognosis of liver cancer
- Effects of light touch on balance in patients with stroke
- Oncoprotein LAMTOR5 activates GLUT1 via upregulating NF-κB in liver cancer
- Effects of budesonide combined with noninvasive ventilation on PCT, sTREM-1, chest lung compliance, humoral immune function and quality of life in patients with AECOPD complicated with type II respiratory failure
- Prognostic significance of lymph node ratio in ovarian cancer
- Case Report
- Brainstem anaesthesia after retrobulbar block
- Review Article
- Treating infertility: current affairs of cross-border reproductive care
- Research Article
- Serum inflammatory cytokines comparison in gastric cancer therapy
- Behavioural and psychological symptoms in neurocognitive disorders: Specific patterns in dementia subtypes
- MRI and bone scintigraphy for breast cancer bone metastase: a meta-analysis
- Comparative study of back propagation artificial neural networks and logistic regression model in predicting poor prognosis after acute ischemic stroke
- Analysis of the factors affecting the prognosis of glioma patients
- Compare fuhrman nuclear and chromophobe tumor grade on chromophobe RCC
- Case Report
- Signet ring B cell lymphoma: A potential diagnostic pitfall
- Research Article
- Subparaneural injection in popliteal sciatic nerve blocks evaluated by MRI
- Loneliness in the context of quality of life of nursing home residents
- Biological characteristics of cervical precancerous cell proliferation
- Effects of Rehabilitation in Bankart Lesion in Non-athletes: A report of three cases
- Management of complications of first instance of hepatic trauma in a liver surgery unit: Portal vein ligation as a conservative therapeutic strategy
- Matrix metalloproteinase 2 knockdown suppresses the proliferation of HepG2 and Huh7 cells and enhances the cisplatin effect
- Comparison of laparoscopy and open radical nephrectomy of renal cell cancer
- Case Report
- A severe complication of myocardial dysfunction post radiofrequency ablation treatment of huge hepatic hemangioma: a case report and literature review
- Solar urticaria, a disease with many dark sides: is omalizumab the right therapeutic response? Reflections from a clinical case report
- Research Article
- Binge eating disorder and related features in bariatric surgery candidates
- Propofol versus 4-hydroxybutyric acid in pediatric cardiac catheterizations
- Nasointestinal tube in mechanical ventilation patients is more advantageous
- The change of endotracheal tube cuff pressure during laparoscopic surgery
- Correlation between iPTH levels on the first postoperative day after total thyroidectomy and permanent hypoparathyroidism: our experience
- Case Report
- Primary angiosarcoma of the kidney: case report and comprehensive literature review
- Research Article
- miR-107 enhances the sensitivity of breast cancer cells to paclitaxel
- Incidental findings in dental radiology are concerning for family doctors
- Suffering from cerebral small vessel disease with and without metabolic syndrome
- A meta-analysis of robot assisted laparoscopic radical prostatectomy versus laparoscopic radical prostatectomy
- Indications and outcomes of splenectomy for hematological disorders
- Expression of CENPE and its prognostic role in non-small cell lung cancer
- Barbed suture and gastrointestinal surgery. A retrospective analysis
- Using post transplant 1 week Tc-99m DTPA renal scan as another method for predicting renal graft failure
- The pseudogene PTTG3P promotes cell migration and invasion in esophageal squamous cell carcinoma
- Lymph node ratio versus TNM system as prognostic factor in colorectal cancer staging. A single Center experience
- Review Article
- Minimally invasive pilonidal sinus treatment: A narrative review
- Research Article
- Anatomical workspace study of Endonasal Endoscopic Transsphenoidal Approach
- Hounsfield Units on Lumbar Computed Tomography for Predicting Regional Bone Mineral Density
- Communication
- Aspirin, a potential GLUT1 inhibitor in a vascular endothelial cell line
- Research Article
- Osteopontin and fatty acid binding protein in ifosfamide-treated rats
- Familial polyposis coli: the management of desmoid tumor bleeding
- microRNA-27a-3p down-regulation inhibits malignant biological behaviors of ovarian cancer by targeting BTG1
- PYCR1 is associated with papillary renal cell carcinoma progression
- Prediction of recurrence-associated death from localized prostate cancer with a charlson comorbidity index–reinforced machine learning model
- Colorectal cancer in the elderly patient: the role of neo-adjuvant therapy
- Association between MTHFR genetic polymorphism and Parkinson’s disease susceptibility: a meta-analysis
- Metformin can alleviate the symptom of patient with diabetic nephropathy through reducing the serum level of Hcy and IL-33
- Case Report
- Severe craniofacial trauma after multiple pistol shots
- Research Article
- Echocardiography evaluation of left ventricular diastolic function in elderly women with metabolic syndrome
- Tailored surgery in inguinal hernia repair. The role of subarachnoid anesthesia: a retrospective study
- The factors affecting early death in newly diagnosed APL patients
- Review Article
- Oncological outcomes and quality of life after rectal cancer surgery
- Research Article
- MiR-638 repressed vascular smooth muscle cell glycolysis by targeting LDHA
- microRNA-16 via Twist1 inhibits EMT induced by PM2.5 exposure in human hepatocellular carcinoma
- Analyzing the semantic space of the Hippocratic Oath
- Fournier’s gangrene and intravenous drug abuse: an unusual case report and review of the literature
- Evaluation of surgical site infection in mini-invasive urological surgery
- Dihydromyricetin attenuates inflammation through TLR4/NF-kappaB pathway
- Clinico-pathological features of colon cancer patients undergoing emergency surgery: a comparison between elderly and non-elderly patients
- Case Report
- Appendix bleeding with painless bloody diarrhea: A case report and literature review
- Research Article
- Protective effects of specneuzhenide on renal injury in rats with diabetic nephropathy
- PBF, a proto-oncogene in esophageal carcinoma
- Use of rituximab in NHL malt type pregnant in I° trimester for two times
- Cancer- and non-cancer related chronic pain: from the physiopathological basics to management
- Case report
- Non-surgical removal of dens invaginatus in maxillary lateral incisor using CBCT: Two-year follow-up case report
- Research Article
- Risk factors and drug resistance of the MDR Acinetobacter baumannii in pneumonia patients in ICU
- Accuracy of tumor perfusion assessment in Rat C6 gliomas model with USPIO
- Lemann Index for Assessment of Crohn’s Disease: Correlation with the Quality of Life, Endoscopic Disease activity, Magnetic Resonance Index of Activity and C- Reactive Protein
- Case report
- Münchausen syndrome as an unusual cause of pseudo-resistant hypertension: a case report
- Research Article
- Renal artery embolization before radical nephrectomy for complex renal tumour: which are the true advantages?
- Prognostic significance of CD276 in non-small cell lung cancer
- Potential drug-drug interactions in acute ischemic stroke patients at the Neurological Intensive Care Unit
- Effect of vitamin D3 on lung damage induced by cigarette smoke in mice
- CircRNA-UCK2 increased TET1 inhibits proliferation and invasion of prostate cancer cells via sponge miRNA-767-5p
- Case report
- Partial hydatidiform mole and coexistent live fetus: a case report and review of the literature
- Research Article
- Effect of NGR1 on the atopic dermatitis model and its mechanisms
- Clinical features of infertile men carrying a chromosome 9 translocation
- Review Article
- Expression and role of microRNA-663b in childhood acute lymphocytic leukemia and its mechanism
- Case Report
- Mature cystic teratoma of the pancreas: A rare cystic neoplasm
- Research Article
- Application of exercised-based pre-rehabilitation in perioperative period of patients with gastric cancer
- Case Report
- Predictive factors of intestinal necrosis in acute mesenteric ischemia
- Research Article
- Application of exercised-based pre-rehabilitation in perioperative period of patients with gastric cancer
- Effects of dexmedetomidine on the RhoA /ROCK/ Nox4 signaling pathway in renal fibrosis of diabetic rats
- MicroRNA-181a-5p regulates inflammatory response of macrophages in sepsis
- Intraventricular pressure in non-communicating hydrocephalus patients before endoscopic third ventriculostomy
- CyclinD1 is a new target gene of tumor suppressor miR-520e in breast cancer
- CHL1 and NrCAM are primarily expressed in low grade pediatric neuroblastoma
- Epidemiological characteristics of postoperative sepsis
- Association between unstable angina and CXCL17: a new potential biomarker
- Cardiac strains as a tool for optimization of cardiac resynchronization therapy in non-responders: a pilot study
- Case Report
- Resuscitation following a bupivacaine injection for a cervical paravertebral block
- Research Article
- CGF treatment of leg ulcers: A randomized controlled trial
- Surgical versus sequential hybrid treatment of carotid body tumors


