Abstract
Background and Aims
Chronic pain is a debilitating condition that requires prompt access to care for effective treatment. Wait times for care often exceed benchmark recommendations, with potential consequences to patient health outcomes. The goal of this paper is to gain the perspectives of patients attending a chronic pain clinic regarding the acceptability of current wait times and the impact of their experiences of waiting for chronic pain care.
Methods
The study took place in a chronic pain clinic at an academic-affiliated teaching hospital in Ottawa, Canada, which housed seven clinicians at the time of the study. New patients attending the chronic pain clinic between July 14, 2014 and August 5, 2015 were eligible to participate based on the availability of the research and clerical staff who administered the survey on a variety of days over the course of the study. Patients completed a self-administered 29-item survey. The survey took approximately five to ten minutes to complete. Questions pertained to patients’ socioeconomic factors, chronicity and burden of pain symptoms, and satisfaction with current wait times. Actual wait times were self-reported. Survey results were entered into an Excel spreadsheet, exported to SPSS, and coded numerically to facilitate descriptive analyses using comparative graphs and tables. Open-text responses were reviewed by the authors.
Results
Sixty-six patients completed the survey. While 83% of patients stated that their ideal wait time was less than three months, 32% reported receiving an appointment within this period, and 31% reported waiting a year or more. Only 37% of patients felt the wait time for their appointment was appropriate. During their wait,41% of patients reported receiving written information about chronic pain and 47% were referred to a local chronic pain management group. 94% reported interference with social/recreational activities and normal activities of daily living, 31% had to miss work or school due to the frequency of ongoing symptoms, and 22% reported being unable to attend work or school altogether. Furthermore, 37% of patients reported visiting the emergency room within the previous year and 65% worried about having a serious undiagnosed disease.
Conclusions
Our study found that wait times for chronic pain care, even those triaged as urgent cases, far exceeded what patients considered ideal. Only a third of patients received care within three months of making their appointment, while nearly another third waited over a year. During the waiting period, nearly all patients experienced some impact on their day-to-day activities and work or school attendance, half were unemployed, and nearly a quarter reported a complete inability to attend work or school because of pain.
Implications
Wait times for chronic pain care exceed timelines deemed acceptable by patients, causing anxiety and reducing function. The patient perspective must be considered in initiatives attempting to improve access to care for this population with specific needs and goals. Innovative solutions, such as electronic consultation and shared care models, hold promise.
1 Introduction
Chronic pain is a debilitating condition affecting millions of patients in Canada and the United States [1,2]. In order to effectively manage chronic pain, patients require prompt access to care. If delivered in a timely manner, appropriate pain therapy can substantially improve quality of life [3], whereas increased pain intensity and emotional distress become significant after as little as three months of waiting for chronic pain treatment [4]. In order to mitigate the negative effects of prolonged wait times, the Canadian Anesthesiology Society and the Wait Time Alliance established benchmark wait times for chronic pain treatment at a maximum of six months [5,6]. However, a study of multidisciplinary pain treatment facilities (MPTFs) found that wait times ranged from six months to five years [7,8]. While wait times are less extensive in the United States, research has identified disparities in access to pain treatment based on socioeconomic factors [9,10]. Patients facing poor access to pain treatment may experience health deterioration, lower quality of life, and a reduced ability to fully participate in work, school, and leisure activities [1,7]. Furthermore, chronic pain patients are two to three times more likely to experience suicidal ideation or commit suicide [3].
As part of a larger programme of research examining access to care and the impact of electronic consultation (eConsult) [11], we conducted a series of waiting room surveys to examine the perspectives of patients attending specialist clinics regarding current wait times and the impact of delays on their lives. Patient-reported outcomes are increasingly recognized as a critical aspect of health services improvement activities, and while we have shown that eConsult can improve access to chronic pain services [12], there was a need to better understand the patient experience of living with chronic pain.
The results of this research will help inform the next steps in implementation of eConsult on a broader scale by providing an in-depth look at the perspectives of people living with chronic pain. It will also be relevant for the development of other quality improvement initiatives for chronic pain patients and be of interest to innovators in other jurisdictions seeking to improve care for patients suffering from chronic pain.
2 Methods
2.1 Setting
The study took place in a chronic pain clinic at an academic- affiliated teaching hospital in Ottawa, Canada, which housed seven clinicians at the time of the study. The clinic holds approximately 380 full day chronic pain clinics per year, for a total of about 4350 visits from 1435 patients. At the time of the study, an estimated 500 new patients were seen by the clinic each year, of whom as many as seventy five percent are triaged as urgent and booked as early as possible, whereas those triaged as non-urgent face a wait time of over two years.
2.2 Participants
New patients attending the chronic pain clinic between July 14, 2014 and August 5, 2015 were eligible to participate based on the availability of the research and clerical staff who administered the survey on a variety of days over the course of the study. Patients who were less than 18 years of age, cognitively impaired, or unable to complete the survey in English or French were ineligible to participate.
2.3 Procedure
The clinic receptionist informed patients about the study when they checked in for their appointment and gave them an information sheet. Patients who agreed to participate met with a research assistant in a private location to complete informed consent forms. The patient completed a written self-administered survey prior to their specialist appointment.
2.4 Survey
Patients completed a self-administered 29-item survey. The survey took approximately five to ten minutes to complete, and was adapted from a previous study of patient wait times [13] to include additional questions pertaining to chronic pain. Questions pertained to patients’ socioeconomic factors, chronicity and burden of pain symptoms, and satisfaction with current wait times. Patients could also leave additional comments in an open-text field. Actual wait times were self-reported.
2.5 Analysis and interpretation
Survey results were entered into an Excel spreadsheet, exported to SPSS, and coded numerically to facilitate descriptive analyses using comparative graphs and tables. Open-text responses were reviewed by the authors.
3 Results
A total of 71 patients consented to the study, of whom 66 completed the self-administered waiting room survey. The five patients who did not complete the survey were called in to their specialist appointment prior to completion or decided to defer participation during the survey. In some cases, patients declined or were unable to answer questions, and consequently some surveys contain missing data.
Our sample had more women than men (56% versus 44%) and a broad age range (18 to 87 years) with a median of 53 years. The majority (68%) completed some form of post-secondary education. Among patients under 65 years of age, 38% were unemployed. Full demographic details are available in Table 1.
Patient characteristics.
| Characteristics | % |
|---|---|
| Gender (n = 65) | |
| Male | 44% |
| Female | 56% |
| Age (n = 66) | |
| Age range | 18–87 |
| Median age | 53 |
| Education (n =65) | |
| Elementary school | 3% |
| High school | 29% |
| College or technical school | 39% |
| University | 29% |
| Employment sector (n = 66) | |
| Public sector | 12% |
| Private sector | 16% |
| Self-employed | 7% |
| Not-for-profit organization | 1% |
| Domestic or homecare | 1% |
| Unemployed (under age 65) | 53% |
| Method of transportation to appointment (n = 66) | |
| Regular bus | 11% |
| Para transpo | 0% |
| Relative dropped them off | 18% |
| Walked | 2% |
| Biked | 0% |
| Car | 64% |
| Taxi | 3% |
| Other | 3% |
While 46% of referrals to the chronic pain clinic were from the patients’ usual family doctor, 48% came from another specialist (Table 2). Sixty-three percent of patients reported having seen another specialist for their pain problem prior to their pain clinic appointment. The most common specialties accessed by the study population prior to the pain clinic referral were orthopaedic surgery (23%), neurosurgery (19%), physical medicine and rehabilitation (11%), and anesthesiology (11%). In 83% of cases, patients reported seeing their family physician or another health care provider for their condition over the past 12 months or longer.
Appointment characteristics.
| Characteristics | % |
|---|---|
| Referrer (n = 59) | |
| Usual family doctor | 46% |
| Nurse practitioner | 2% |
| Walk-in clinic doctor | 0% |
| Emergency room doctor | 2% |
| Specialist doctor | 48% |
| Other | 3% |
| Wait time for this appointment (n = 65) | |
| Far too short | 0% |
| Somewhat too short | 0% |
| About right | 37% |
| Somewhat too long | 32% |
| Far too long | 31% |
| Frequency of ongoing symptoms causing missed work or school (n = 64) | |
| Never | 17% |
| Less than 5 days per month | 16% |
| Between 5 to 15 days per month | 8% |
| More than 15 days per month | 8% |
| Totally unable to work/go to school all the time | 22% |
| Not applicable (no ongoing symptoms or not working/going to school) | 30% |
| Length of time seeing family doctor/other health care provider for current problem | |
| 0–3 months | 3% |
| 3–6 months | 6% |
| 6–12 months | 8% |
| More than 12 months | 83% |
Ideal and actual wait times are reported in Fig. 1. While 83% of patients stated that their ideal wait time was less than three months, 32% reported receiving an appointment within this period, and 31% reported waiting a year or more. Only 37% of patients felt the wait time for their appointment was appropriate. During their wait, 41% of patients reported receiving written information about chronic pain and 47% were referred to a local chronic pain management group.
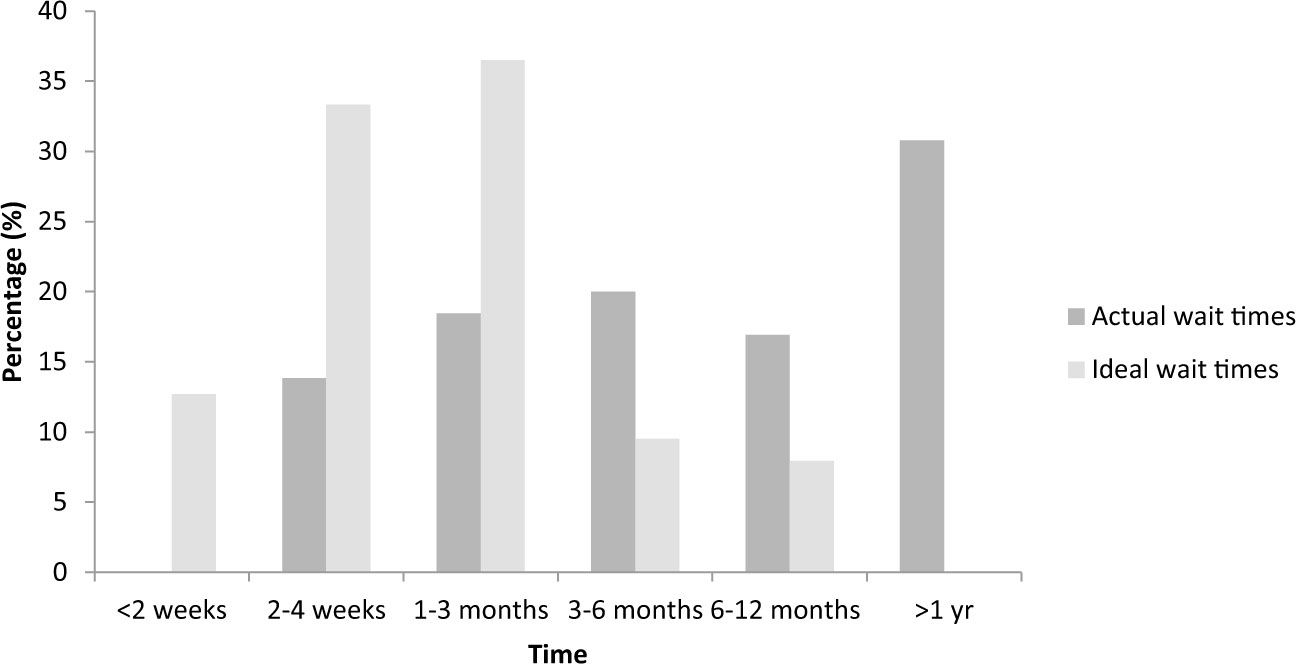
The proportion of actual and ideal wait times reported by patients.
Fig. 2 presents the proportion of respondents who reported experiencing various burdens associated with chronic pain. An overwhelming majority reported interference with social/recreational activities (94%) and normal activities of daily living (94%). Thirty-one percent had to miss work or school due to the frequency of ongoing symptoms, and 22% reported being unable to attend work or school altogether. Furthermore, 37% of patients reported visiting the emergency room within the previous year and 65% worried about having a serious undiagnosed disease.
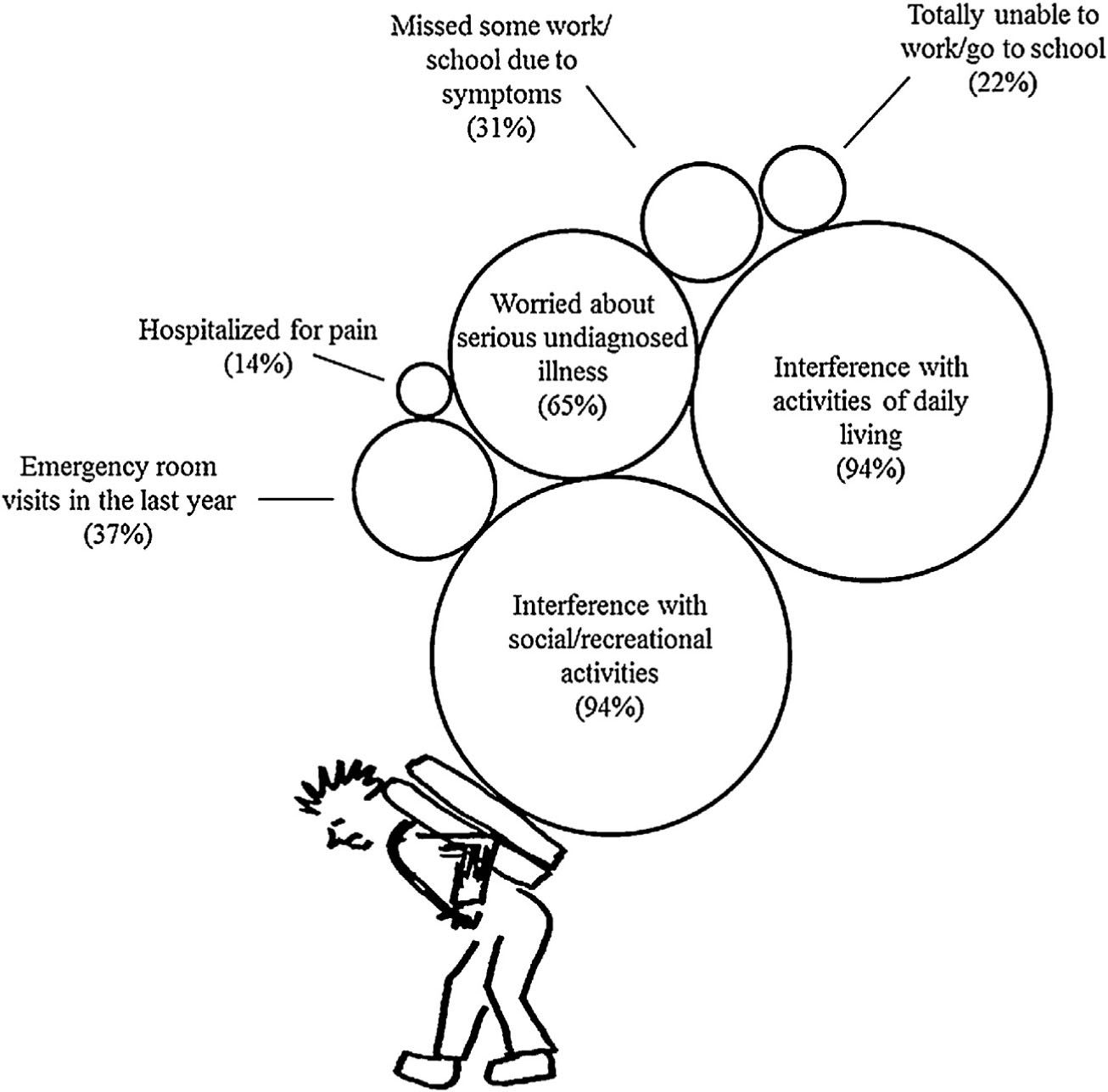
Percentage of patients reporting common burdens of living with chronic pain.
4 Discussion
Our study found that wait times for chronic pain care, even those triaged as urgent cases, far exceeded what patients considered ideal. Only a third of patients received care within three months of making their appointment, while nearly another third waited over a year. During the waiting period, nearly all patients experienced some impact on their day-to-day activities and work or school attendance, half were unemployed, and nearly a quarter reported a complete inability to attend work or school because of pain.
Our findings on the impact of wait times on patients reflect those of previous studies. A systematic review exploring benchmarks for chronic pain treatment found that waiting as little as five weeks for care was associated with deterioration in health-related quality of life [14]. Among eight university-affiliated MPTFs across Canada, 50% of chronic pain patients reported severe levels of depression [4]. Furthermore, research on the economic impact of chronic pain found that patients often miss work or lose employment altogether due to limited functioning associated with their illness, a problem compounded by the fact that many patients fund 95% of the additional costs of their care (a median of $1435 per month) themselves [15]. Many patients expressed interest in treatment strategies beyond pain management, including daily functioning and financial wellbeing [15,16]. Other researchers have found that when wait times are reduced, patients reported higher satisfaction and more active usage of management strategies to treat their pain [17].
Though access to pain management is considered by some as a fundamental human right [18], many patients do not receive care in a timely manner. Reasons for this delay include a lack of knowledge about pain management among family doctors and specialists, inadequate remuneration for the increased time required to care for patients with complex chronic pain, and poor access to publicly funded health practitioners such as physiotherapists, psychologists, and occupational therapists [14]. Many physicians have taken efforts to mitigate the effects of long waits by offering patients advice on self-management or information on community resources they can use while awaiting specialist care. Studies have demonstrated that using digital health and social media to engage patients can result in better psychological and emotional health [19,20]. However, such programmes may not always provide sufficient support to entirely mitigate the effects of long wait times; though nearly half of the patients in our study received written information and a recommendation to attend a chronic pain support group while waiting for a specialist consultation, reports of burden remained significantly high. Fragmentation of care is another serious issue facing chronic pain patients. In our study, nearly half of participating patients had been referred to the pain clinic by another specialist rather than their primary care provider (PCP). Specialist-to-specialist referrals may occur because specialists are more familiar with chronic pain as a specialty group, or as a way to triage patients whom the specialist feels could benefit from expert advice on chronic pain. However, referrals from specialists run the risk of removing PCPs from the centre of the patient’s care, which could lead to worse outcomes.
In response to these issues, many jurisdictions have recognized the need for new strategies to reduce wait times for chronic pain care. eConsult services may offer an alternative for chronic pain patients by facilitating communication between PCPs and specialists, allowing many patients to avoid face-to-face specialist appointments by giving PCPs the information they need to care for them directly [18]. eConsult services can also reduce fragmentation of care through adoption of specialist-to-specialist or case conferencing models, which help track the treatment process and ensure patients are receiving sufficient and timely care [11,21] . In a study of an eConsult service used to treat patients with chronic pain, researchers found that PCPs received responses form specialists in a median of 1.9 days, 36% of cases resulted in avoiding an unnecessary referral, and only 44% resulted in a specialist referral [12]. Likewise, in a study examining the perspectives of patients attending an endocrinology clinic, participants cited faster access, reduced travel time, and lower costs as potential benefits of an eConsult service [13].
4.1 Strengths and limitations of the study
This is the first Canadian study to assess patients’ perspectives on the impact of wait times for chronic pain specialist appointments. Although opportunities to improve the traditional referral-consultation model exist, the development of any new strategy should include patient feedback. An understanding of the patient experience is imperative in guiding healthcare administrators and policy-makers to create system improvements that are medically appropriate and align with patients’ goals.
There are several limitations in the present study. The survey took place in a single academic pain clinic using a convenience sample of patients, limiting its generalizability. The patients included in this study were fast-tracked to their appointments, and thus faced relatively short wait times compared to the general patient population, many of whom waited years for their appointments. Thus, the findings likely underestimate wait times. Although 53% of the sample was unemployed, the reason for unemployment, be it longterm disability, retirement, etc., cannot be distinguished. Future studies should seek to incorporate this into their analyses. Lastly, self-reported data is susceptible to bias.
5 Conclusion
Wait times for chronic pain care exceeded timelines deemed acceptable by patients, causing anxiety and reducing their capacity to participate in daily activities. Patient perspectives must be considered in improving access for this patient population, which has very specific needs. Innovative solutions, such as electronic consultation, should be evaluated as a means of reducing wait-times to pain care and improving patient outcomes.
Highlights
Wait times for chronic pain care exceeded patients’ preferences in most cases.
In 31% of cases, patients reported waiting over a year for care.
Nearly all patients (94%) felt wait times negatively affected their daily lives.
-
Ethical issues: This study did not involve any patient intervention and informed consent was not required. Ethics approval for the study was provided by The Ottawa Health Science Network Research Ethics Board.
-
Conflict of interest: None.
-
Role of funding source: Funding for this project was provided by the Ontario Ministry of Health and Long-Term Care, The Ottawa Hospital Academic Medical Organization Innovation Fund, e-Health Ontario, and the Champlain Local Health Integration Network. The funders had no role in the design of the study; the collection, analysis, or interpretation of the data; the writing of the article; or the decision to submit the article for publication.
Acknowledgements
The authors wish to thank the chronic pain clinic where the study took place and the patients who participated in the study. They would also like to thank Myka Caluyong and Chantal Rockwell, for conducting the surveys, and Justin Joschko for his assistance in editing the manuscript.
References
[1] Andrew R, Derry S, Taylor RS, Straube S, Phillips CJ. The costs and consequences of adequately managed chronic non-cancerpain and chronic neuropathic pain. Pain Pract 2014;14:79–94.Suche in Google Scholar
[2] Institute of Medicine (US).Relieving Pain in America: A Blueprint for Transforming Prevention, Care, Education, and Research. Washington: National Academies Press; 2011. Available from: https://www.ncbi.nlm.nih.gov/books/NBK91497/[accessed 29.03.17].Suche in Google Scholar
[3] Tang NK, Crane C. Suicidality in chronic pain: a review of the prevalence, risk factors and psychological links. Psychol Med 2006;36:575–86.Suche in Google Scholar
[4] Choiniere M, Dion D, Peng P, Banner R, Barton PM, Boulanger A, Clark AJ, Gordon AS, Guerriere DN, Guertin MC, Intrater HM, Lefort SM, Lynch ME, Moulin DE, Ong-Lam M, Racine M, Rashiq S, Shir Y, Taenzer P, Ware M. The Canadian STOP-PAIN project - Part 1: Who are the patients on the waitlists of multidisciplinary pain treatment facilities? Can J Anesth 2010;57:539–48.Suche in Google Scholar
[5] Wait Time Alliance. Wait Time Benchmarks for Patients with Chronic Pain; 2014. Available from: http://www.waittimealliance.ca/benchmarks/chronic-pain/[accessed 29.03.17].Suche in Google Scholar
[6] Canadian Anesthesiology Society. Wait Time Benchmarks for patients with Chronic Pain: Position of the Canadian Anesthesiologists Society. Ottawa: Wait Time Alliance; 2014. Available from: http://www.waittimealliance.ca/wp-content/uploads/2014/05/Position-of-the-Section-of-Chronic-Pain-on-Wait-Lists-Version-2012–1.pdf [accessed 29.03.17].Suche in Google Scholar
[7] Lynch ME, Campbell F, Clark AJ, Dunbar MJ, Goldstein D, Peng P, Stinson J, Tupper H. Asystematic review of the effect ofwaiting fortreatment forchronic pain. Pain 2008;136:97–116.Suche in Google Scholar
[8] Peng P, Choiniere M, Dion D, Intrater H, Lefort S, Lynch M, Ong M, Rashiq S, Tkachuk G, Veillette Y. STOPPAIN Investigators Group. Challenge in accessing multidisciplinary pain treatment facilities in Canada.Can J Anaesth 2007;54:977–84.Suche in Google Scholar
[9] Meghani SH, Byun E, Gallagher RM. Time to take stock: a meta-analysis and systematic review of analgesic treatment disparities for pain in the United States. Pain Med 2012;13:150–74.Suche in Google Scholar
[10] Davis K, Schoen C, Stremikis K, Fund C. Mirror, mirror on the wall: How the performance of the US health care system compares internationally: 2010 update. New York, NY: The Commonwealth Fund; 2010. Available from: http://www.resbr.net.br/wp-content/uploads/historico/Espelhoespelhomeu.pdf [accessed 29.03.17].Suche in Google Scholar
[11] Liddy C, Drosinis P, Keely E. Electronic consultation systems: worldwide prevalence and their impact on patient care - a systematic review. Fam Pract 2016;33:274–85.Suche in Google Scholar
[12] Liddy C, Smyth C, Poulin PA, Joschko J, Rebelo M, Keely E. Improving access to chronic pain services through econsultation: a cross-sectional study of the Champlain BASE eConsult Service. Pain Med 2016:nw038.Suche in Google Scholar
[13] Keely E, Traczyk L, Liddy C. Patient perspectives on wait times and the referral-consultation process while attending a tertiary diabetes and endocrinology centre: Is eConsultation an acceptable option? Can J Diabetes 2015;39: 325–9.Suche in Google Scholar
[14] Lynch ME, Campbell FA, Clark AJ, Dunbar MJ, Goldstein D, Peng P, Stinson J, Tupper H. Canadian Pain Society Wait Times Task Force. Waiting for treatment for chronic pain – a survey of existing benchmarks: toward establishing evidence-based benchmarks for medically acceptable waiting times.Pain Res Manag 2007;12:245.Suche in Google Scholar
[15] Guerriere DN, Choiniere M, Dion D, Peng P, Stafford-Coyte E, Zagorski B, Banner R, Barton PM, Boulanger A, Clark AJ, Gordon AS, Guertin MC, Intrater HM, Lefort SM, Lynch ME, Moulin DE, Ong-Lam M, Racine M, Rashiq S, Shir Y, Taenzer P, Ware M. The Canadian STOP-PAIN project-Part 2: What is the cost of pain for patients on waitlists of multidisciplinary paintreatment facilities? Can J Anesth 2010;57:549–58.Suche in Google Scholar
[16] Turk DC, Dworkin RH, Revicki D, Harding G, Burke LB, Cella D, Cleeland CS, Cowan P, Farrar JT, Hertz S, Max MB, Rappaport BA. Identifying important outcome domains for chronic pain clinical trials: an IMMPACT survey of people with pain. Pain 2008;137:276–85.Suche in Google Scholar
[17] Davies S, Quintner J, Parsons R, Parkitny L, Knight P, Forrester E, Roberts M, Graham C, Visser E, Antill T, Packer T, Schug SA. Preclinic group education sessions reduce waiting times and costs at public pain medicine units. Pain Med 2011;12:59–71.Suche in Google Scholar
[18] Cousins MJ, Lynch ME. The Declaration Montreal: access to pain management is a fundamental human right. Pain 2011;152:2673–4.Suche in Google Scholar
[19] Merolli M, Gray K, Martin-Sanchez F, Lopez-Campos G. Patient-reported outcomes and therapeutic affordances of social media: findings from a global online survey ofpeople with chronic pain. J Med Internet Res 2015;17:e20.Suche in Google Scholar
[20] Ranney ML, Duarte C, Baird J, Patry EJ, Green TC. Correlation of digital health use and chronic pai coping strategiesm. Health 2016;2.Suche in Google Scholar
[21] Liddy C, Rowan MS, Afkham A, Maranger J, Keely E. Building access to specialist care through e-consultation. Open Med 2013;7:e1–8.Suche in Google Scholar
© 2017 Scandinavian Association for the Study of Pain
Artikel in diesem Heft
- Observational study
- Perceived sleep deficit is a strong predictor of RLS in multisite pain – A population based study in middle aged females
- Clinical pain research
- Prospective, double blind, randomized, controlled trial comparing vapocoolant spray versus placebo spray in adults undergoing intravenous cannulation
- Clinical pain research
- The Functional Barometer — An analysis of a self-assessment questionnaire with ICF-coding regarding functional/activity limitations and quality of life due to pain — Differences in age gender and origin of pain
- Clinical pain research
- Clinical outcome following anterior arthrodesis in patients with presumed sacroiliac joint pain
- Observational study
- Chronic disruptive pain in emerging adults with and without chronic health conditions and the moderating role of psychiatric disorders: Evidence from a population-based cross-sectional survey in Canada
- Educational case report
- Management of patients with pain and severe side effects while on intrathecal morphine therapy: A case study
- Clinical pain research
- Behavioral inhibition, maladaptive pain cognitions, and function in patients with chronic pain
- Observational study
- Comparison of patients diagnosed with “complex pain” and “somatoform pain”
- Original experimental
- Patient perspectives on wait times and the impact on their life: A waiting room survey in a chronic pain clinic
- Topical review
- New evidence for a pain personality? A critical review of the last 120 years of pain and personality
- Clinical pain research
- A multi-facet pain survey of psychosocial complaints among patients with long-standing non-malignant pain
- Clinical pain research
- Pain patients’ experiences of validation and invalidation from physicians before and after multimodal pain rehabilitation: Associations with pain, negative affectivity, and treatment outcome
- Observational study
- Long-term treatment in chronic noncancer pain: Results of an observational study comparing opioid and nonopioid therapy
- Clinical pain research
- COMBAT study – Computer based assessment and treatment – A clinical trial evaluating impact of a computerized clinical decision support tool on pain in cancer patients
- Original experimental
- Quantitative sensory tests fairly reflect immediate effects of oxycodone in chronic low-back pain
- Editorial comment
- Spatial summation of pain and its meaning to patients
- Original experimental
- Effects of validating communication on recall during a pain-task in healthy participants
- Original experimental
- Comparison of spatial summation properties at different body sites
- Editorial comment
- Behavioural inhibition in the context of pain: Measurement and conceptual issues
- Clinical pain research
- A randomized study to evaluate the analgesic efficacy of a single dose of the TRPV1 antagonist mavatrep in patients with osteoarthritis
- Editorial comment
- Quantitative sensory tests (QST) are promising tests for clinical relevance of anti–nociceptive effects of new analgesic treatments
- Educational case report
- Pregabalin as adjunct in a multimodal pain therapy after traumatic foot amputation — A case report of a 4-year-old girl
- Editorial comment
- Severe side effects from intrathecal morphine for chronic pain after repeated failed spinal operations
- Editorial comment
- Opioids in chronic pain – Primum non nocere
- Editorial comment
- Finally a promising analgesic signal in a long-awaited new class of drugs: TRPV1 antagonist mavatrep in patients with osteoarthritis (OA)
- Observational study
- The relationship between chronic musculoskeletal pain, anxiety and mindfulness: Adjustments to the Fear-Avoidance Model of Chronic Pain
- Clinical pain research
- Opioid tapering in patients with prescription opioid use disorder: A retrospective study
- Editorial comment
- Sleep, widespread pain and restless legs — What is the connection?
- Editorial comment
- Broadening the fear-avoidance model of chronic pain?
- Observational study
- Identifying characteristics of the most severely impaired chronic pain patients treated at a specialized inpatient pain clinic
- Editorial comment
- The burden of central anticholinergic drugs increases pain and cognitive dysfunction. More knowledge about drug-interactions needed
- Editorial comment
- A case-history illustrates importance of knowledge of drug-interactions when pain-patients are prescribed non-pain drugs for co-morbidities
- Editorial comment
- Why can multimodal, multidisciplinary pain clinics not help all chronic pain patients?
- Topical review
- Individual variability in clinical effect and tolerability of opioid analgesics – Importance of drug interactions and pharmacogenetics
- Editorial comment
- A new treatable chronic pain diagnosis? Flank pain caused by entrapment of posterior cutaneous branch of intercostal nerves, lateral ACNES coined LACNES
- Clinical pain research
- PhKv a toxin isolated from the spider venom induces antinociception by inhibition of cholinesterase activating cholinergic system
- Clinical pain research
- Lateral Cutaneous Nerve Entrapment Syndrome (LACNES): A previously unrecognized cause of intractable flank pain
- Editorial comment
- Towards a structured examination of contextual flexibility in persistent pain
- Clinical pain research
- Context sensitive regulation of pain and emotion: Development and initial validation of a scale for context insensitive avoidance
- Editorial comment
- Is the search for a “pain personality” of added value to the Fear-Avoidance-Model (FAM) of chronic pain?
- Editorial comment
- Importance for patients of feeling accepted and understood by physicians before and after multimodal pain rehabilitation
- Editorial comment
- A glimpse into a neglected population – Emerging adults
- Observational study
- Assessment and treatment at a pain clinic: A one-year follow-up of patients with chronic pain
- Clinical pain research
- Randomized, double-blind, placebo-controlled, dose-escalation study: Investigation of the safety, pharmacokinetics, and antihyperalgesic activity of L-4-chlorokynurenine in healthy volunteers
- Clinical pain research
- Prevalence and characteristics of chronic pain: Experience of Niger
- Observational study
- The use of rapid onset fentanyl in children and young people for breakthrough cancer pain
- Original experimental
- Acid-induced experimental muscle pain and hyperalgesia with single and repeated infusion in human forearm
- Original experimental
- Swearing as a response to pain: A cross-cultural comparison of British and Japanese participants
- Clinical pain research
- The cognitive impact of chronic low back pain: Positive effect of multidisciplinary pain therapy
- Clinical pain research
- Central sensitization associated with low fetal hemoglobin levels in adults with sickle cell anemia
- Topical review
- Targeting cytokines for treatment of neuropathic pain
- Original experimental
- What constitutes back pain flare? A cross sectional survey of individuals with low back pain
- Original experimental
- Coping with pain in intimate situations: Applying the avoidance-endurance model to women with vulvovaginal pain
- Clinical pain research
- Chronic low back pain and the transdiagnostic process: How do cognitive and emotional dysregulations contribute to the intensity of risk factors and pain?
- Original experimental
- The impact of the Standard American Diet in rats: Effects on behavior, physiology and recovery from inflammatory injury
- Educational case report
- Erector spinae plane (ESP) block in the management of post thoracotomy pain syndrome: A case series
- Original experimental
- Hyperbaric oxygenation alleviates chronic constriction injury (CCI)-induced neuropathic pain and inhibits GABAergic neuron apoptosis in the spinal cord
- Observational study
- Predictors of chronic neuropathic pain after scoliosis surgery in children
- Clinical pain research
- Hospitalization due to acute exacerbation of chronic pain: An intervention study in a university hospital
- Clinical pain research
- A novel miniature, wireless neurostimulator in the management of chronic craniofacial pain: Preliminary results from a prospective pilot study
- Clinical pain research
- Implicit evaluations and physiological threat responses in people with persistent low back pain and fear of bending
- Original experimental
- Unpredictable pain timings lead to greater pain when people are highly intolerant of uncertainty
- Original experimental
- Initial validation of the exercise chronic pain acceptance questionnaire
- Clinical pain research
- Exploring patient experiences of a pain management centre: A qualitative study
- Clinical pain research
- Narratives of life with long-term low back pain: A follow up interview study
- Observational study
- Pain catastrophizing, perceived injustice, and pain intensity impair life satisfaction through differential patterns of physical and psychological disruption
- Clinical pain research
- Chronic pain disrupts ability to work by interfering with social function: A cross-sectional study
- Original experimental
- Evaluation of external vibratory stimulation as a treatment for chronic scrotal pain in adult men: A single center open label pilot study
- Observational study
- Impact of analgesics on executive function and memory in the Alzheimer’s Disease Neuroimaging Initiative Database
- Clinical pain research
- Visualization of painful inflammation in patients with pain after traumatic ankle sprain using [11C]-D-deprenyl PET/CT
- Original experimental
- Developing a model for measuring fear of pain in Norwegian samples: The Fear of Pain Questionnaire Norway
- Topical review
- Psychoneuroimmunological approach to gastrointestinal related pain
- Letter to the Editor
- Do we need an updated definition of pain?
- Narrative review
- Is acetaminophen safe in pregnancy?
- Book Review
- Physical Diagnosis of Pain
- Book Review
- Advances in Anesthesia
- Book Review
- Atlas of Pain Management Injection Techniques
- Book Review
- Sedation: A Guide to Patient Management
- Book Review
- Basics of Anesthesia
Artikel in diesem Heft
- Observational study
- Perceived sleep deficit is a strong predictor of RLS in multisite pain – A population based study in middle aged females
- Clinical pain research
- Prospective, double blind, randomized, controlled trial comparing vapocoolant spray versus placebo spray in adults undergoing intravenous cannulation
- Clinical pain research
- The Functional Barometer — An analysis of a self-assessment questionnaire with ICF-coding regarding functional/activity limitations and quality of life due to pain — Differences in age gender and origin of pain
- Clinical pain research
- Clinical outcome following anterior arthrodesis in patients with presumed sacroiliac joint pain
- Observational study
- Chronic disruptive pain in emerging adults with and without chronic health conditions and the moderating role of psychiatric disorders: Evidence from a population-based cross-sectional survey in Canada
- Educational case report
- Management of patients with pain and severe side effects while on intrathecal morphine therapy: A case study
- Clinical pain research
- Behavioral inhibition, maladaptive pain cognitions, and function in patients with chronic pain
- Observational study
- Comparison of patients diagnosed with “complex pain” and “somatoform pain”
- Original experimental
- Patient perspectives on wait times and the impact on their life: A waiting room survey in a chronic pain clinic
- Topical review
- New evidence for a pain personality? A critical review of the last 120 years of pain and personality
- Clinical pain research
- A multi-facet pain survey of psychosocial complaints among patients with long-standing non-malignant pain
- Clinical pain research
- Pain patients’ experiences of validation and invalidation from physicians before and after multimodal pain rehabilitation: Associations with pain, negative affectivity, and treatment outcome
- Observational study
- Long-term treatment in chronic noncancer pain: Results of an observational study comparing opioid and nonopioid therapy
- Clinical pain research
- COMBAT study – Computer based assessment and treatment – A clinical trial evaluating impact of a computerized clinical decision support tool on pain in cancer patients
- Original experimental
- Quantitative sensory tests fairly reflect immediate effects of oxycodone in chronic low-back pain
- Editorial comment
- Spatial summation of pain and its meaning to patients
- Original experimental
- Effects of validating communication on recall during a pain-task in healthy participants
- Original experimental
- Comparison of spatial summation properties at different body sites
- Editorial comment
- Behavioural inhibition in the context of pain: Measurement and conceptual issues
- Clinical pain research
- A randomized study to evaluate the analgesic efficacy of a single dose of the TRPV1 antagonist mavatrep in patients with osteoarthritis
- Editorial comment
- Quantitative sensory tests (QST) are promising tests for clinical relevance of anti–nociceptive effects of new analgesic treatments
- Educational case report
- Pregabalin as adjunct in a multimodal pain therapy after traumatic foot amputation — A case report of a 4-year-old girl
- Editorial comment
- Severe side effects from intrathecal morphine for chronic pain after repeated failed spinal operations
- Editorial comment
- Opioids in chronic pain – Primum non nocere
- Editorial comment
- Finally a promising analgesic signal in a long-awaited new class of drugs: TRPV1 antagonist mavatrep in patients with osteoarthritis (OA)
- Observational study
- The relationship between chronic musculoskeletal pain, anxiety and mindfulness: Adjustments to the Fear-Avoidance Model of Chronic Pain
- Clinical pain research
- Opioid tapering in patients with prescription opioid use disorder: A retrospective study
- Editorial comment
- Sleep, widespread pain and restless legs — What is the connection?
- Editorial comment
- Broadening the fear-avoidance model of chronic pain?
- Observational study
- Identifying characteristics of the most severely impaired chronic pain patients treated at a specialized inpatient pain clinic
- Editorial comment
- The burden of central anticholinergic drugs increases pain and cognitive dysfunction. More knowledge about drug-interactions needed
- Editorial comment
- A case-history illustrates importance of knowledge of drug-interactions when pain-patients are prescribed non-pain drugs for co-morbidities
- Editorial comment
- Why can multimodal, multidisciplinary pain clinics not help all chronic pain patients?
- Topical review
- Individual variability in clinical effect and tolerability of opioid analgesics – Importance of drug interactions and pharmacogenetics
- Editorial comment
- A new treatable chronic pain diagnosis? Flank pain caused by entrapment of posterior cutaneous branch of intercostal nerves, lateral ACNES coined LACNES
- Clinical pain research
- PhKv a toxin isolated from the spider venom induces antinociception by inhibition of cholinesterase activating cholinergic system
- Clinical pain research
- Lateral Cutaneous Nerve Entrapment Syndrome (LACNES): A previously unrecognized cause of intractable flank pain
- Editorial comment
- Towards a structured examination of contextual flexibility in persistent pain
- Clinical pain research
- Context sensitive regulation of pain and emotion: Development and initial validation of a scale for context insensitive avoidance
- Editorial comment
- Is the search for a “pain personality” of added value to the Fear-Avoidance-Model (FAM) of chronic pain?
- Editorial comment
- Importance for patients of feeling accepted and understood by physicians before and after multimodal pain rehabilitation
- Editorial comment
- A glimpse into a neglected population – Emerging adults
- Observational study
- Assessment and treatment at a pain clinic: A one-year follow-up of patients with chronic pain
- Clinical pain research
- Randomized, double-blind, placebo-controlled, dose-escalation study: Investigation of the safety, pharmacokinetics, and antihyperalgesic activity of L-4-chlorokynurenine in healthy volunteers
- Clinical pain research
- Prevalence and characteristics of chronic pain: Experience of Niger
- Observational study
- The use of rapid onset fentanyl in children and young people for breakthrough cancer pain
- Original experimental
- Acid-induced experimental muscle pain and hyperalgesia with single and repeated infusion in human forearm
- Original experimental
- Swearing as a response to pain: A cross-cultural comparison of British and Japanese participants
- Clinical pain research
- The cognitive impact of chronic low back pain: Positive effect of multidisciplinary pain therapy
- Clinical pain research
- Central sensitization associated with low fetal hemoglobin levels in adults with sickle cell anemia
- Topical review
- Targeting cytokines for treatment of neuropathic pain
- Original experimental
- What constitutes back pain flare? A cross sectional survey of individuals with low back pain
- Original experimental
- Coping with pain in intimate situations: Applying the avoidance-endurance model to women with vulvovaginal pain
- Clinical pain research
- Chronic low back pain and the transdiagnostic process: How do cognitive and emotional dysregulations contribute to the intensity of risk factors and pain?
- Original experimental
- The impact of the Standard American Diet in rats: Effects on behavior, physiology and recovery from inflammatory injury
- Educational case report
- Erector spinae plane (ESP) block in the management of post thoracotomy pain syndrome: A case series
- Original experimental
- Hyperbaric oxygenation alleviates chronic constriction injury (CCI)-induced neuropathic pain and inhibits GABAergic neuron apoptosis in the spinal cord
- Observational study
- Predictors of chronic neuropathic pain after scoliosis surgery in children
- Clinical pain research
- Hospitalization due to acute exacerbation of chronic pain: An intervention study in a university hospital
- Clinical pain research
- A novel miniature, wireless neurostimulator in the management of chronic craniofacial pain: Preliminary results from a prospective pilot study
- Clinical pain research
- Implicit evaluations and physiological threat responses in people with persistent low back pain and fear of bending
- Original experimental
- Unpredictable pain timings lead to greater pain when people are highly intolerant of uncertainty
- Original experimental
- Initial validation of the exercise chronic pain acceptance questionnaire
- Clinical pain research
- Exploring patient experiences of a pain management centre: A qualitative study
- Clinical pain research
- Narratives of life with long-term low back pain: A follow up interview study
- Observational study
- Pain catastrophizing, perceived injustice, and pain intensity impair life satisfaction through differential patterns of physical and psychological disruption
- Clinical pain research
- Chronic pain disrupts ability to work by interfering with social function: A cross-sectional study
- Original experimental
- Evaluation of external vibratory stimulation as a treatment for chronic scrotal pain in adult men: A single center open label pilot study
- Observational study
- Impact of analgesics on executive function and memory in the Alzheimer’s Disease Neuroimaging Initiative Database
- Clinical pain research
- Visualization of painful inflammation in patients with pain after traumatic ankle sprain using [11C]-D-deprenyl PET/CT
- Original experimental
- Developing a model for measuring fear of pain in Norwegian samples: The Fear of Pain Questionnaire Norway
- Topical review
- Psychoneuroimmunological approach to gastrointestinal related pain
- Letter to the Editor
- Do we need an updated definition of pain?
- Narrative review
- Is acetaminophen safe in pregnancy?
- Book Review
- Physical Diagnosis of Pain
- Book Review
- Advances in Anesthesia
- Book Review
- Atlas of Pain Management Injection Techniques
- Book Review
- Sedation: A Guide to Patient Management
- Book Review
- Basics of Anesthesia

