EGCG promotes the sensory function recovery in rats after dorsal root crush injury by upregulating KAT6A and inhibiting pyroptosis
-
Jianjun Wang
Abstract
Dorsal root injury usually leads to irreversible sensory function loss and lacks effective treatments. (−)-epigallocatechin-3-gallate (EGCG) is reported to exert neuroprotective roles in the nervous systems. However, the function of EGCG in treating dorsal root injury remains unclear. Hence, we built the dorsal root crush injury (DRCI) rat model to be treated with EGCG, followed by the western blot, Enzyme-linked immunosorbent assay, and sensory behavior tests. We observed that EGCG can upregulate the Lysine acetyltransferase 6A (KAT6A) level and inhibit the pyroptosis, indicated by downregulated gasdermin-D, caspase-1, and interleukin 18 protein levels, and alleviate the neuropathic pain, indicated by the decreased paw withdraw threshold in Plantar test and decreased paw withdraw latency in von Frey test, and downregulated calcitonin gene-related peptide, nerve growth factor, and c-Fos protein levels. But EGCG cannot alleviate the neuropathic pain when the KAT6A was inhibited by CTX-0124143 and pyroptosis was activated by Miltirone. These combined results indicated that EGCG can promote the sensory function recovery in rats after DRCI via upregulating KAT6A and inhibiting pyroptosis, laying the foundation for EGCG to be a novel candidate for the treatment of dorsal root injury.
1 Introduction
Peripheral nerve injury is the most common and frequent cause of disability and death, and is considered one of the world’s clinical medical treatment challenges [1]. Severe peripheral nerve injury caused by trauma results in irreparable damage to nerve fibers, which gradually rupture at the distal end (known as Wallerian degeneration) and ultimately interrupt synapses with target organs, accompanied by persistent pain [2]. In the past, scientists often focused on the recovery of motor function after peripheral nerve injury, but paid relatively little attention to the recovery of sensory function after injury. Therefore, studying the methods and mechanisms of promoting sensory function recovery after peripheral nerve injury is an extremely urgent scientific issue.
The natural polyphenol compounds contained in beverages have various beneficial properties. Epigallocatechin-3-gallate (EGCG), a major active polyphenol isolated from green tea, has been extensively studied in numerous studies [3,4]. EGCG inhibits TNF- α activated NF-κB pathway and enhances nuclear factor E2 related factor 2 protein levels in macrophages [5]. EGCG alleviates staurosporine-induced cytotoxicity and apoptosis by regulating BDNF TrkB/Akt and Erk1/2 signal axes in hippocampal neurons [6]. EGCG has neuroprotective effects on the retina of ischemia-reperfusion rabbits by activating Nrf2/HO-1 [7]. Research has shown that EGCG can provide neuroprotection against brain [8], spinal cord injury [9], and sciatic nerve injury [10], alleviate neuronal cell damage caused by focal cerebral ischemia in rats [11], and promote the recovery of peripheral nerve injury function [12]. These beneficial effects are mainly attributed to the antioxidant, anti-inflammatory, and anti-apoptotic properties of free radical scavenging or EGCG [13,14,15]. Latest research indicates that EGCG can improve motor function after brachial plexus avulsion [16] and promote functional recovery after spinal cord injury [17], but there is still a lack of research on its role in sensory function. This suggests that EGCG has the potential to treat spinal dorsal root nerve injury.
Lysine acetyltransferase (KATs) catalyzes the acetylation of lysine and is a reversible protein modification involving various disease states [18]. Lysine acetyltransferase 6A (KAT6A, also known as MYST3 and MOZ) is a histone acetyltransferase of the MYST family. It has been identified for the first time in patients with acute myeloid leukemia as a mammalian KAT6A, which can control cell life processes, including inhibiting cell aging through the INK4A ARF pathway [19]. Histone acetyltransferase KAT6A/B inhibitors induce aging and prevent tumor growth [20]. More and more evidence suggests that KAT6A has been found to regulate the proliferation of normal cells [21]. KAT6A upregulates PI3K/AKT signaling through TRIM24 binding [22].
Pyroptosis is a new type of programmed cell death discovered and confirmed in recent years, which is characterized by its dependence on caspase and the release of a large number of proinflammatory factors [23]. Unlike traditional cell apoptosis, pyroptosis is defined as a special type of inflammatory necrosis characterized by cell swelling, rupture, pore formation in the cell membrane, and release of cytoplasmic contents [24]. The activation of cytoplasmic inflammatory body complexes is considered a necessary step in neuroinflammation and a key trigger factor for neuronal death [25]. During the initiation and activation of inflammasome signaling, the activated inflammasome assembles and binds to and cleaves pre caspase-1 to form an active subunit, which activates interleukin (IL)-1 β precursors, IL-18 precursors, and gasdermin D (GSDMD), further leading to inflammatory reactions and pyrophosphorylation [26]. The activation of caspase-1 is a characteristic of pyroptosis, and the activation of inflammatory bodies leads to cytokine IL-1 β and the maturity of IL-18 [27]. During central nervous system injury, inflammasomes are activated by danger signals, which subsequently induce cell apoptosis [28]. It has been confirmed that the pharmacological or genetic inhibition of inflammasome signaling or direct elimination of caspase-1 has a protective effect on neurons in brain and spinal cord injury models [29,30].
2 Materials and methods
2.1 Animals
200–220 g male Sprague Dawley rats obtained from the Guangdong Medical Laboratory Animal Center (PR China) were maintained on a 12 h light/12 h dark cycle, and was offered food and water ad libitum.
2.2 Dorsal root crush injury (DRCI) model procedures and groups
Animals were anesthetized by intraperitoneal injection of a mixture of methylthiazide (8 mg/kg body weight) and Ketamine (80 mg/kg body weight). Under sterile conditions, a longitudinal incision was made from the C4 to T2 spinous process (approximately 3 cm long along the midline) to separate and remove the paraspinal muscles from C4 to T2. The connective tissues and muscles were removed to expose the right spinal segment from the 4th neck (C4) to the 2nd chest (T2) level. After C5 to T1 dorsal laminectomy and dural opening, the right C5 to T1 dorsal root was exposed. Each root is crushed three times (five times each time). There are seven tweezers between dorsal root ganglion and DREZ. The Sham surgery was performed in the same way, but there was no root injury. The muscles were sutured in layers and the skin was closed with a wound clamp after completing the injury.
To investigate the neuroprotective role of EGCG after DRCI, the rats were randomly divided into 4 groups with 9 rats in each group: (A) phosphate-buffered saline (PBS), (B) PBS + EGCG, (C) PBS + EGCG + CTX-0124143 (an inhibitor of KAT6A), and (D) PBS + EGCG + Miltirone (an agonist of pyroptosis). The treatment groups were intraperitoneally injected with phosphate-buffered saline (PBS) or EGCG (10 mg/kg/day) with or without CTX-0124143/Miltirone once daily after the surgery till the day of sacrifice. The rats without DRCI treatment were used as the Sham control.
2.3 Sensory behavioral tests
All injured animals were tested at least once prior to injury to obtain baseline responses. From the first week post-injury, the tests were made twice a week until 6 weeks post-injury. Animals (n = 9 per group) were first placed in the testing room and allowed to rest quietly for half an hour. For temperature sensation testing, the responses to thermal stimuli were measured by the Plantar Test (Ugo Basile) [31]. The footpads in the rats’ forepaws were stimulated with a noxious infrared light beam which was placed below the center of the tested paw plantar. The time elapsed between the onset of infrared stimuli and the rats withdrawing their paws were recorded. The testing was repeated three times with 5 min intervals in between; the thermal stimulus cut-off time was 20 s to avoid any tissue damage.
For pressure sensation assessment, a probe connected to an electronic von Frey anesthesiometer (2390–5; Life Science Instruments) [31] was applied to the central footpads of the forepaws. The pressure was gradually increased until the rats withdrew their forepaws; the response threshold was then recorded. The testing was repeated five times with 3 min intervals in between each trail and the pressure stimulus cut-off threshold was set at 100 g to avoid tissue damage.
2.4 Tissue processing
At 8 weeks after the surgery, the animals were euthanized by deep anesthesia with isoflurane to be sacrificed as previously described [32,33,34,35], and then the C7 segment of the spinal cord was collected for further analyses.
2.5 Enzyme-linked immunosorbent assay (ELISA)
The ELISA was performed, as previously described [12,36]. The dissected tissues were homogenized in ice-cold Tris-HCl buffer (pH = 7.4, Solarbio, Beijing, China) and centrifuged at 13,000×g at 4°C for 10 min. ELISA was performed using commercial assay kits shown in Table 1, according to the instructions.
Information on reagents
| Proteins | Catalog | Company |
|---|---|---|
| KAT6A | JM-11280R1 | Jingmei Biotechnology |
| GSDMD | H378 | Nanjing Jiancheng Bioengineering Institute |
| Caspase-1 | H074 | Nanjing Jiancheng Bioengineering Institute |
| IL-18 | H015-1-2 | Nanjing Jiancheng Bioengineering Institute |
| CGRP | H217 | Nanjing Jiancheng Bioengineering Institute |
| NGF | H043 | Nanjing Jiancheng Bioengineering Institute |
| c-Fos | SPS-10214 | Shanghai Peisen Biotechnology Institute |
2.6 Statistics
All statistical analyses were performed by using GraphPad Prism 6 software. Data were reported as mean value ± standard deviation (SD) and analyzed using ANOVA followed by the post-hoc Bonferroni test. P < 0.05 was considered statistical significance.
-
Ethical approval: The research related to animals’ use has been complied with all the relevant national regulations and institutional policies for the care and use of animals. The Laboratory Animal Ethics Committee at Xiangnan University approved all experimental protocols conducted on animals.
3 Results
3.1 EGCG can upregulate the KAT6A level after DRCI
To evaluate the effect of EGCG on KAT6A, ELISA was performed to determine the change in KAT6A protein level. We found that the KAT6A level was downregulated after DRCI, but EGCG can upregulate the KAT6A level. In rats treated with CTX-0124143 or Miltirone, EGCG did not increase the KAT6A protein level (Figure 1).

Effect of EGCG on KAT6A protein level in rats after DRCI. EGCG increased the protein levels of KAT6A (**p < 0.01, ***p < 0.001, n = 4, One-way ANOVA).
3.2 EGCG can inhibit the pyroptosis after DRCI
To evaluate the effect of EGCG on pyroptosis, ELISA was performed to determine the change in protein levels of GSDMD, caspase-1, and IL-18. As shown in Figure 2a, we observed that, DRCI increased the GSDMD protein level, whereas EGCG decreased the GSDMD protein level. In rats treated with CTX-0124143, EGCG did not decrease the GSDMD protein level. After treating the rats with Miltirone, EGCG did not decrease the GSDMD protein level. Similar patterns for the caspase-1 and IL-18 protein levels were also observed (Figure 2b and c).

Effect of EGCG on pyroptosis in rats after DRCI. EGCG inhibited pyroptosis, as indicated by the decreased protein levels of (a) GSDMD, (b) caspase-1, and (c) IL-18 (*p < 0.05, **p < 0.01, ***p < 0.001, n = 4, One-way ANOVA).
3.3 EGCG can alleviate the neuropathic pain after DRCI via upregulating KAT6A and inhibiting the pyroptosis
To evaluate the effect of EGCG on neuropathic pain, sensory behavioral tests (Plantar test and von Frey test) were performed. In Plantar test shown in Figure 3a, we observed that DRCI increased the paw withdraw threshold, whereas EGCG decreased the paw withdraw threshold. In rats treated with CTX-0124143, EGCG did not decrease the paw withdraw threshold. After treating the rats with Miltirone, EGCG did not decrease the paw withdraw threshold. A similar pattern for the paw withdraw latency in von Frey test was also observed (Figure 3b).

Effect of EGCG on functional recovery in rats after DRCI. EGCG upregulates KAT6A and inhibits pyroptosis to alleviate the neuropathic pain, as indicated by the decreased (a) paw withdraw threshold in von Frey test and (b) paw withdraw latency in Plantar test (***p < 0.0001, n = 9, Two-way ANOVA).
3.4 EGCG can downregulate the neuropathic pain-related proteins after DRCI via upregulating KAT6A and inhibiting the pyroptosis
To evaluate the effect of EGCG on neuropathic pain-related proteins, ELISA was performed to determine the change in protein levels of calcitonin gene-related peptide (CGRP), nerve growth factor (NGF), and c-Fos. As shown in Figure 4a, we observed that, DRCI increased the CGRP protein level, whereas EGCG decreased the CGRP protein level. In rats treated with CTX-0124143, EGCG did not decrease the CGRP protein level. After treating the rats with Miltirone, EGCG did not decrease the CGRP protein level. Similar patterns for the NGF and c-Fos protein levels were also observed (Figure 4b and c).
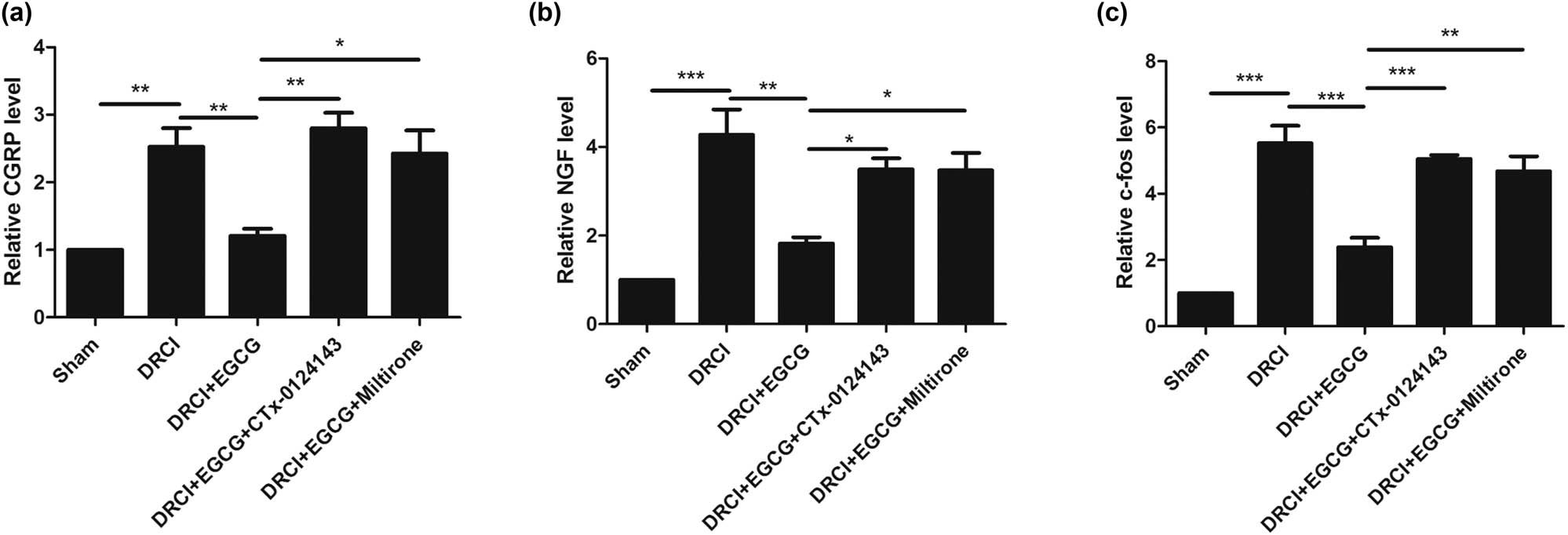
Effect of EGCG on neuropathic pain-related proteins in rats after DRCI. EGCG decreased the protein levels of (a) CGRP, (b) NGF, and (c) c-Fos (*p < 0.05, **p < 0.01, ***p < 0.001, n = 4, One-way ANOVA).
4 Discussion
In the previous studies, we have revealed the effect of EGCG on the brachial plexus root avulsion [16], complete spinal cord transection [12], and intracerebral hemorrhage [37]. In the current study, we observed that EGCG can promote the sensory function recovery in rats after DRCI through upregulating KAT6A and inhibiting pyroptosis.
Assessing the neurological function is a well-known measurement to determine the degree of lesion and the therapeutic effect of strategies. In the present study, we found that EGCG can alleviate the neuropathic pain after DRCI via upregulating KAT6A and inhibiting the pyroptosis.
Neurogenic pain is considered a refractory complication after lesion [38]. Multiple nociceptive stimuli can be used to activate c-Fos, a pain biomarker, in the spinal cord [39]. NGF and CGRP were considered to exert an essential role in the molecular mechanisms of inflammatory-associated diseases and are closely involved in nerve pain [40]. In the present study, we found that EGCG can downregulate these neuropathic pain-related proteins after DRCI via upregulating KAT6A and inhibiting the pyroptosis.
Although the results seem promising, this study still has some limitations: in the current study, we mainly focused on the effect of EGCG on the sensory recovery and the underlying mechanisms, further studies are no doubt needed to pay attention to the duration of dosage of EGCG during the treatment after DRCI.
Taken together, these combined results suggest that EGCG may be a novel strategy for treating dorsal root injury.
Acknowledgements
We thank Hunan Provincial College Student Innovation and Entrepreneurship Training Program Project (Xiang Jiao Tong [2021] No. 197); General Project of Hunan Natural Science Foundation (2021JJ30640); Research Project of Hunan Provincial Health Commission (Xiang Wei Han [2021] No. 260), Hunan Province Ordinary University Teaching Reform Research Project (Xiang Jiao Tong [2019] No. 291); The Nanling Mountain Medical Resources Innovation and Entrepreneurship Education Center (XJT [2020] No. 301) for support.
-
Conflict of interest: Authors state no conflict of interest.
-
Data availability statement: The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
[1] Balog BM, Askew T, Lin DL, Kuang M, Hanzlicek B, Damaser MS. The pudendal nerve motor branch regenerates via a brain derived neurotrophic factor mediated mechanism. Exp Neurol. 2020;334:113438.10.1016/j.expneurol.2020.113438Suche in Google Scholar PubMed
[2] Houdek MT, Shin AY. Management and complications of traumatic peripheral nerve injuries. Hand Clin. 2015;31(2):151–63.10.1016/j.hcl.2015.01.007Suche in Google Scholar PubMed
[3] Min SY, Yan M, Kim SB, Ravikumar S, Kwon SR, Vanarsa K, et al. Green tea epigallocatechin-3-gallate suppresses autoimmune arthritis through indoleamine-2,3-dioxygenase expressing dendritic cells and the nuclear factor, erythroid 2-like 2 antioxidant pathway. J Inflamm (London, Engl). 2015;12:53.10.1186/s12950-015-0097-9Suche in Google Scholar PubMed PubMed Central
[4] Shanmugam T, Selvaraj M, Poomalai S. Epigallocatechin gallate potentially abrogates fluoride induced lung oxidative stress, inflammation via Nrf2/Keap1 signaling pathway in rats: An in-vivo and in-silico study. Int Immunopharmacol. 2016;39:128–39.10.1016/j.intimp.2016.07.022Suche in Google Scholar PubMed
[5] Reddy AT, Lakshmi SP, Maruthi Prasad E, Varadacharyulu NC, Kodidhela LD. Epigallocatechin gallate suppresses inflammation in human coronary artery endothelial cells by inhibiting NF-κB. Life Sci. 2020;258:118136.10.1016/j.lfs.2020.118136Suche in Google Scholar PubMed
[6] Yang JR, Ren TT, Lan R, Qin XY. Tea polyphenols attenuate staurosporine-induced cytotoxicity and apoptosis by modulating BDNF-TrkB/Akt and Erk1/2 signaling axis in hippocampal neurons . IBRO Rep. 2020;8:115–21.10.1016/j.ibror.2020.04.002Suche in Google Scholar PubMed PubMed Central
[7] Rivera-Pérez J, Martínez-Rosas M, Conde-Castañón CA, Toscano-Garibay JD, Ruiz-Pérez NJ, Flores PL, et al. Epigallocatechin 3-gallate has a neuroprotective effect in retinas of rabbits with ischemia/reperfusion through the activation of Nrf2/HO-1. Int J Mol Sci. 2020;21(10):3716.10.3390/ijms21103716Suche in Google Scholar PubMed PubMed Central
[8] Hsieh DJ, Marte L, Kuo WW, Ju DT, Chen WS, Kuo CH, et al. Epigallocatechin-3-gallate preconditioned adipose-derived stem cells confer neuroprotection in aging rat brain. Int J Med Sci. 2020;17(13):1916–26.10.7150/ijms.46696Suche in Google Scholar PubMed PubMed Central
[9] Bosch-Mola M, Homs J, Álvarez-Pérez B, Puig T, Reina F, Verdú E, et al. (-)-epigallocatechin-3-gallate antihyperalgesic effect associates with reduced CX3CL1 chemokine expression in spinal cord. Phytother Res. 2017;31(2):340–4.10.1002/ptr.5753Suche in Google Scholar PubMed
[10] Renno WM, Benov L, Khan KM. Possible role of antioxidative capacity of (-)-epigallocatechin-3-gallate treatment in morphological and neurobehavioral recovery after sciatic nerve crush injury. J Neurosurg Spine. 2017;27(5):593–613.10.3171/2016.10.SPINE16218Suche in Google Scholar PubMed
[11] Park DJ, Kang JB, Koh PO. Epigallocatechin gallate alleviates neuronal cell damage against focal cerebral ischemia in rats. J Vet Med Sci. 2020;82(5):639–45.10.1292/jvms.19-0703Suche in Google Scholar PubMed PubMed Central
[12] Wang J, Chen Y, Chen L, Duan Y, Kuang X, Peng Z, et al. EGCG modulates PKD1 and ferroptosis to promote recovery in ST rats. Transl Neurosci. 2020;11(1):173–81.Suche in Google Scholar
[13] Yuan H, Li Y, Ling F, Guan Y, Zhang D, Zhu Q, et al. The phytochemical epigallocatechin gallate prolongs the lifespan by improving lipid metabolism, reducing inflammation and oxidative stress in high-fat diet-fed obese rats. Aging Cell. 2020;19:e13199.10.1111/acel.13199Suche in Google Scholar PubMed PubMed Central
[14] Meng J, Chen Y, Wang J, Qiu J, Chang C, Bi F, et al. EGCG protects vascular endothelial cells from oxidative stress-induced damage by targeting the autophagy-dependent PI3K-AKT-mTOR pathway. Ann Transl Med. 2020;8(5):200.10.21037/atm.2020.01.92Suche in Google Scholar PubMed PubMed Central
[15] Kian K, Khalatbary AR, Ahmadvand H, Karimpour Malekshah A, Shams Z. Neuroprotective effects of (-)-epigallocatechin-3-gallate (EGCG) against peripheral nerve transection-induced apoptosis. Nutr Neurosci. 2019;22(8):578–86.10.1080/1028415X.2017.1419542Suche in Google Scholar PubMed
[16] Tang Y, Wang J, Wan S, Luo L, Qiu Y, Jiang S, et al. Epigallocatechin gallate enhances the motor neuron survival and functional recovery after brachial plexus root avulsion by regulating FIG4. Folia Neuropathol. 2019;57(4):340–7.10.5114/fn.2019.90819Suche in Google Scholar PubMed
[17] Wang J, Chen Y, Chen L, Duan Y, Kuang X, Peng Z, et al. EGCG modulates PKD1 and ferroptosis to promote recovery in ST. Transl Neurosci. 2020;11:173–81.10.1515/tnsci-2020-0119Suche in Google Scholar PubMed PubMed Central
[18] Huang F. New KAT6 inhibitors induce senescence and arrest cancer growth. Synth Syst Biotechnol. 2018;3(4):244–5.10.1016/j.synbio.2018.10.006Suche in Google Scholar PubMed PubMed Central
[19] Sheikh BN, Phipson B, El-Saafin F, Vanyai HK, Downer NL, Bird MJ, et al. MOZ (MYST3, KAT6A) inhibits senescence via the INK4A-ARF pathway. Oncogene. 2015;34(47):5807–20.10.1038/onc.2015.33Suche in Google Scholar PubMed
[20] Baell JB, Leaver DJ, Hermans SJ, Kelly GL, Brennan MS, Downer NL, et al. Inhibitors of histone acetyltransferases KAT6A/B induce senescence and arrest tumour growth. Nature. 2018;560(7717):253–7.10.1038/s41586-018-0387-5Suche in Google Scholar PubMed
[21] Yu L, Liang Y, Cao X, Wang X, Gao H, Lin SY, et al. Identification of MYST3 as a novel epigenetic activator of ERalpha frequently amplified in breast cancer. Oncogene. 2017;36(20):2910–8.10.1038/onc.2016.433Suche in Google Scholar PubMed PubMed Central
[22] Lv D, Jia F, Hou Y, Sang Y, Alvarez AA, Zhang W, et al. Histone acetyltransferase KAT6A upregulates PI3K/AKT signaling through TRIM24 binding. Cancer Res. 2017;77(22):6190–201.10.1158/0008-5472.CAN-17-1388Suche in Google Scholar PubMed PubMed Central
[23] Gaidt MM, Hornung V. Pore formation by GSDMD is the effector mechanism of pyroptosis. EMBO J. 2016;35(20):2167–9.10.15252/embj.201695415Suche in Google Scholar PubMed PubMed Central
[24] Wang Y, Gao W, Shi X, Ding J, Liu W, He H, et al. Chemotherapy drugs induce pyroptosis through caspase-3 cleavage of a gasdermin. Nature. 2017;547(7661):99–103.10.1038/nature22393Suche in Google Scholar PubMed
[25] Liu W, Chen Y, Meng J, Wu M, Bi F, Chang C, et al. Ablation of caspase-1 protects against TBI-induced pyroptosis in vitro and in vivo. J Neuroinflammation. 2018;15(1):48.10.1186/s12974-018-1083-ySuche in Google Scholar PubMed PubMed Central
[26] de Rivero Vaccari JP, Dietrich WD, Keane RW. Activation and regulation of cellular inflammasomes: gaps in our knowledge for central nervous system injury. J Cereb Blood Flow Metab. 2014;34(3):369–75.10.1038/jcbfm.2013.227Suche in Google Scholar PubMed PubMed Central
[27] Lamkanfi M, Dixit VM. Mechanisms and functions of inflammasomes. Cell. 2014;157(5):1013–22.10.1016/j.cell.2014.04.007Suche in Google Scholar PubMed
[28] Lin WP, Xiong GP, Lin Q, Chen XW, Zhang LQ, Shi JX, et al. Heme oxygenase-1 promotes neuron survival through down-regulation of neuronal NLRP1 expression after spinal cord injury. J Neuroinflammation. 2016;13(1):52.10.1186/s12974-016-0521-ySuche in Google Scholar PubMed PubMed Central
[29] Zendedel A, Johann S, Mehrabi S, Joghataei MT, Hassanzadeh G, Kipp M, et al. Activation and regulation of NLRP3 inflammasome by intrathecal application of SDF-1a in a spinal cord injury model. Mol Neurobiol. 2016;53(5):3063–75.10.1007/s12035-015-9203-5Suche in Google Scholar PubMed
[30] Jiang W, Li M, He F, Zhou S, Zhu L. Targeting the NLRP3 inflammasome to attenuate spinal cord injury in mice. J Neuroinflammation. 2017;14(1):207.10.1186/s12974-017-0980-9Suche in Google Scholar PubMed PubMed Central
[31] Tan CL, Andrews MR, Kwok JC, Heintz TG, Gumy LF, Fässler R, et al. Kindlin-1 enhances axon growth on inhibitory chondroitin sulfate proteoglycans and promotes sensory axon regeneration. J Neurosci. 2012;32(21):7325–35.10.1523/JNEUROSCI.5472-11.2012Suche in Google Scholar PubMed PubMed Central
[32] Chen S, Wu L, He B, Zhou G, Xu Y, Zhu G, et al. Artemisinin facilitates motor function recovery by enhancing motoneuronal survival and axonal remyelination in rats following brachial plexus root avulsion. ACS Chem Neurosci. 2021;12(17):3148–56.10.1021/acschemneuro.1c00120Suche in Google Scholar PubMed
[33] Wang Y, Chen S, Tan J, Gao Y, Yan H, Liu Y, et al. Tryptophan in the diet ameliorates motor deficits in a rotenone-induced rat Parkinson’s disease model via activating the aromatic hydrocarbon receptor pathway. Brain Behav. 2021;11(8):e2226.10.1002/brb3.2226Suche in Google Scholar PubMed PubMed Central
[34] Chen S, He B, Zhou G, Xu Y, Wu L, Xie Y, et al. Berberine enhances L1 expression and axonal remyelination in rats after brachial plexus root avulsion. Brain Behav. 2020;10(10):e01792.10.1002/brb3.1792Suche in Google Scholar PubMed PubMed Central
[35] Chen S, Hou Y, Zhao Z, Luo Y, Lv S, Wang Q, et al. Neuregulin-1 accelerates functional motor recovery by improving motoneuron survival after brachial plexus root avulsion in mice. Neuroscience. 2019;404:510–8.10.1016/j.neuroscience.2019.01.054Suche in Google Scholar PubMed
[36] Chen SX, He JH, Mi YJ, Shen HF, Schachner M, Zhao WJ. A mimetic peptide of α2,6-sialyllactose promotes neuritogenesis. Neural Regen Res. 2020;15(6):1058–65.10.4103/1673-5374.270313Suche in Google Scholar PubMed PubMed Central
[37] Wang J, Kuang X, Peng Z, Li C, Guo C, Fu X, et al. EGCG treats ICH via up-regulating miR-137-3p and inhibiting parthanatos. Transl Neurosci. 2020;11(1):371–9.10.1515/tnsci-2020-0143Suche in Google Scholar PubMed PubMed Central
[38] Xian H, Xie R, Luo C, Cong R. Comparison of different in vivo animal models of brachial plexus avulsion and its application in pain study. Neural Plast. 2020;2020:8875915.10.1155/2020/8875915Suche in Google Scholar PubMed PubMed Central
[39] Xie W, Kang Z, Jiang C, Liu N. Administration of curcumin alleviates neuropathic pain in a rat model of brachial plexus avulsion. Pharmacology. 2019;103(5–6):324–32.10.1159/000496928Suche in Google Scholar PubMed
[40] Chakraborty A, Crescenzi R, Usman TA, Reyna AJ, Garza ME, Al-Ghadban S, et al. Indications of peripheral pain, dermal hypersensitivity, and neurogenic inflammation in patients with lipedema. Int J Mol Sci. 2022;23(18):10313.10.3390/ijms231810313Suche in Google Scholar PubMed PubMed Central
© 2023 the author(s), published by De Gruyter
This work is licensed under the Creative Commons Attribution 4.0 International License.
Artikel in diesem Heft
- Research Articles
- HIF-1α participates in secondary brain injury through regulating neuroinflammation
- Omega-3 polyunsaturated fatty acids alleviate early brain injury after traumatic brain injury by inhibiting neuroinflammation and necroptosis
- The correlation between non-arteritic anterior ischemic optic neuropathy and cerebral infarction
- Enriched environment can reverse chronic sleep deprivation-induced damage to cellular plasticity in the dentate gyrus of the hippocampus
- Middle cerebral artery dynamic cerebral autoregulation is impaired by infarctions in the anterior but not the posterior cerebral artery territory in patients with mild strokes
- Leptin ameliorates Aβ1-42-induced Alzheimer’s disease by suppressing inflammation via activating p-Akt signaling pathway
- TIPE2 knockdown exacerbates isoflurane-induced postoperative cognitive impairment in mice by inducing activation of STAT3 and NF-κB signaling pathways
- Does the patellar tendon reflex affect the postural stability in stroke patients with blocked vision?
- Inactivation of CACNA1H induces cell apoptosis by initiating endoplasmic reticulum stress in glioma
- miR-101-3p improves neuronal morphology and attenuates neuronal apoptosis in ischemic stroke in young mice by downregulating HDAC9
- A custom-made weight-drop impactor to produce consistent spinal cord injury outcomes in a rat model
- Arterial spin labeling for moyamoya angiopathy: A preoperative and postoperative evaluation method
- Thyroid hormone levels paradox in acute ischemic stroke
- Geniposide protected against cerebral ischemic injury through the anti-inflammatory effect via the NF-κB signaling pathway
- The clinical characteristics of acute cerebral infarction patients with thalassemia in a tropic area in China
- Comprehensive behavioral study of C57BL/6.KOR-ApoEshl mice
- Incomplete circle of Willis as a risk factor for intraoperative ischemic events during carotid endarterectomies performed under regional anesthesia – A prospective case-series
- HOTAIRM1 knockdown reduces MPP+-induced oxidative stress injury of SH-SY5Y cells by activating the Nrf2/HO-1 pathway
- Esmolol inhibits cognitive impairment and neuronal inflammation in mice with sepsis-induced brain injury
- EHMT2 affects microglia polarization and aggravates neuronal damage and inflammatory response via regulating HMOX1
- Hematoma evacuation based on active strategies versus conservative treatment in the management of moderate basal ganglia hemorrhage: A retrospective study
- Knockdown of circEXOC6 inhibits cell progression and glycolysis by sponging miR-433-3p and mediating FZD6 in glioma
- CircYIPF6 regulates glioma cell proliferation, apoptosis, and glycolysis through targeting miR-760 to modulate PTBP1 expression
- Relationship between serum HIF-1α and VEGF levels and prognosis in patients with acute cerebral infarction combined with cerebral-cardiac syndrome
- The promoting effect of modified Dioscorea pills on vascular remodeling in chronic cerebral hypoperfusion via the Ang/Tie signaling pathway
- Effects of enriched environment on the expression of β-amyloid and transport-related proteins LRP1 and RAGE in chronic sleep-deprived mice
- An interventional study of baicalin on neuronal pentraxin-1, neuronal pentraxin-2, and C-reactive protein in Alzheimer’s disease rat model
- PD98059 protects SH-SY5Y cells against oxidative stress in oxygen–glucose deprivation/reperfusion
- TPVB and general anesthesia affects postoperative functional recovery in elderly patients with thoracoscopic pulmonary resections based on ERAS pathway
- Brain functional connectivity and network characteristics changes after vagus nerve stimulation in patients with refractory epilepsy
- Association between RS3763040 polymorphism of the AQP4 and idiopathic intracranial hypertension in a Spanish Caucasian population
- Effects of γ-oryzanol on motor function in a spinal cord injury model
- Electroacupuncture inhibits the expression of HMGB1/RAGE and alleviates injury to the primary motor cortex in rats with cerebral ischemia
- Effects of edaravone dexborneol on neurological function and serum inflammatory factor levels in patients with acute anterior circulation large vessel occlusion stroke
- CST3 alleviates bilirubin-induced neurocytes’ damage by promoting autophagy
- Excessive MALAT1 promotes the immunologic process of neuromyelitis optica spectrum disorder by upregulating BAFF expression
- Evaluation of cholinergic enzymes and selected biochemical parameters in the serum of patients with a diagnosis of acute subarachnoid hemorrhage
- 7-Day National Institutes of Health Stroke Scale as a surrogate marker predicting ischemic stroke patients’ outcome following endovascular therapy
- Cdk5 activation promotes Cos-7 cells transition towards neuronal-like cells
- 10.1515/tnsci-2022-0313
- PPARα agonist fenofibrate prevents postoperative cognitive dysfunction by enhancing fatty acid oxidation in mice
- Predicting functional outcome in acute ischemic stroke patients after endovascular treatment by machine learning
- EGCG promotes the sensory function recovery in rats after dorsal root crush injury by upregulating KAT6A and inhibiting pyroptosis
- Preoperatively administered single dose of dexketoprofen decreases pain intensity on the first 5 days after craniotomy: A single-centre placebo-controlled, randomized trial
- Myeloarchitectonic maps of the human cerebral cortex registered to surface and sections of a standard atlas brain
- The BET inhibitor apabetalone decreases neuroendothelial proinflammatory activation in vitro and in a mouse model of systemic inflammation
- Carthamin yellow attenuates brain injury in a neonatal rat model of ischemic–hypoxic encephalopathy by inhibiting neuronal ferroptosis in the hippocampus
- Functional connectivity in ADHD children doing Go/No-Go tasks: An fMRI systematic review and meta-analysis
- Review Articles
- Human prion diseases and the prion protein – what is the current state of knowledge?
- Nanopharmacology as a new approach to treat neuroinflammatory disorders
- Case Report
- Deletion as novel variants in VPS13B gene in Cohen syndrome: Case series
- Commentary
- Translation of surface electromyography to clinical and motor rehabilitation applications: The need for new clinical figures
- Revealing key role of T cells in neurodegenerative diseases, with potential to develop new targeted therapies
- Retraction
- Retraction of “Eriodictyol corrects functional recovery and myelin loss in SCI rats”
- Special Issue “Advances in multimedia-based emerging technologies...”
- Evaluation of the improvement of walking ability in patients with spinal cord injury using lower limb rehabilitation robots based on data science
Artikel in diesem Heft
- Research Articles
- HIF-1α participates in secondary brain injury through regulating neuroinflammation
- Omega-3 polyunsaturated fatty acids alleviate early brain injury after traumatic brain injury by inhibiting neuroinflammation and necroptosis
- The correlation between non-arteritic anterior ischemic optic neuropathy and cerebral infarction
- Enriched environment can reverse chronic sleep deprivation-induced damage to cellular plasticity in the dentate gyrus of the hippocampus
- Middle cerebral artery dynamic cerebral autoregulation is impaired by infarctions in the anterior but not the posterior cerebral artery territory in patients with mild strokes
- Leptin ameliorates Aβ1-42-induced Alzheimer’s disease by suppressing inflammation via activating p-Akt signaling pathway
- TIPE2 knockdown exacerbates isoflurane-induced postoperative cognitive impairment in mice by inducing activation of STAT3 and NF-κB signaling pathways
- Does the patellar tendon reflex affect the postural stability in stroke patients with blocked vision?
- Inactivation of CACNA1H induces cell apoptosis by initiating endoplasmic reticulum stress in glioma
- miR-101-3p improves neuronal morphology and attenuates neuronal apoptosis in ischemic stroke in young mice by downregulating HDAC9
- A custom-made weight-drop impactor to produce consistent spinal cord injury outcomes in a rat model
- Arterial spin labeling for moyamoya angiopathy: A preoperative and postoperative evaluation method
- Thyroid hormone levels paradox in acute ischemic stroke
- Geniposide protected against cerebral ischemic injury through the anti-inflammatory effect via the NF-κB signaling pathway
- The clinical characteristics of acute cerebral infarction patients with thalassemia in a tropic area in China
- Comprehensive behavioral study of C57BL/6.KOR-ApoEshl mice
- Incomplete circle of Willis as a risk factor for intraoperative ischemic events during carotid endarterectomies performed under regional anesthesia – A prospective case-series
- HOTAIRM1 knockdown reduces MPP+-induced oxidative stress injury of SH-SY5Y cells by activating the Nrf2/HO-1 pathway
- Esmolol inhibits cognitive impairment and neuronal inflammation in mice with sepsis-induced brain injury
- EHMT2 affects microglia polarization and aggravates neuronal damage and inflammatory response via regulating HMOX1
- Hematoma evacuation based on active strategies versus conservative treatment in the management of moderate basal ganglia hemorrhage: A retrospective study
- Knockdown of circEXOC6 inhibits cell progression and glycolysis by sponging miR-433-3p and mediating FZD6 in glioma
- CircYIPF6 regulates glioma cell proliferation, apoptosis, and glycolysis through targeting miR-760 to modulate PTBP1 expression
- Relationship between serum HIF-1α and VEGF levels and prognosis in patients with acute cerebral infarction combined with cerebral-cardiac syndrome
- The promoting effect of modified Dioscorea pills on vascular remodeling in chronic cerebral hypoperfusion via the Ang/Tie signaling pathway
- Effects of enriched environment on the expression of β-amyloid and transport-related proteins LRP1 and RAGE in chronic sleep-deprived mice
- An interventional study of baicalin on neuronal pentraxin-1, neuronal pentraxin-2, and C-reactive protein in Alzheimer’s disease rat model
- PD98059 protects SH-SY5Y cells against oxidative stress in oxygen–glucose deprivation/reperfusion
- TPVB and general anesthesia affects postoperative functional recovery in elderly patients with thoracoscopic pulmonary resections based on ERAS pathway
- Brain functional connectivity and network characteristics changes after vagus nerve stimulation in patients with refractory epilepsy
- Association between RS3763040 polymorphism of the AQP4 and idiopathic intracranial hypertension in a Spanish Caucasian population
- Effects of γ-oryzanol on motor function in a spinal cord injury model
- Electroacupuncture inhibits the expression of HMGB1/RAGE and alleviates injury to the primary motor cortex in rats with cerebral ischemia
- Effects of edaravone dexborneol on neurological function and serum inflammatory factor levels in patients with acute anterior circulation large vessel occlusion stroke
- CST3 alleviates bilirubin-induced neurocytes’ damage by promoting autophagy
- Excessive MALAT1 promotes the immunologic process of neuromyelitis optica spectrum disorder by upregulating BAFF expression
- Evaluation of cholinergic enzymes and selected biochemical parameters in the serum of patients with a diagnosis of acute subarachnoid hemorrhage
- 7-Day National Institutes of Health Stroke Scale as a surrogate marker predicting ischemic stroke patients’ outcome following endovascular therapy
- Cdk5 activation promotes Cos-7 cells transition towards neuronal-like cells
- 10.1515/tnsci-2022-0313
- PPARα agonist fenofibrate prevents postoperative cognitive dysfunction by enhancing fatty acid oxidation in mice
- Predicting functional outcome in acute ischemic stroke patients after endovascular treatment by machine learning
- EGCG promotes the sensory function recovery in rats after dorsal root crush injury by upregulating KAT6A and inhibiting pyroptosis
- Preoperatively administered single dose of dexketoprofen decreases pain intensity on the first 5 days after craniotomy: A single-centre placebo-controlled, randomized trial
- Myeloarchitectonic maps of the human cerebral cortex registered to surface and sections of a standard atlas brain
- The BET inhibitor apabetalone decreases neuroendothelial proinflammatory activation in vitro and in a mouse model of systemic inflammation
- Carthamin yellow attenuates brain injury in a neonatal rat model of ischemic–hypoxic encephalopathy by inhibiting neuronal ferroptosis in the hippocampus
- Functional connectivity in ADHD children doing Go/No-Go tasks: An fMRI systematic review and meta-analysis
- Review Articles
- Human prion diseases and the prion protein – what is the current state of knowledge?
- Nanopharmacology as a new approach to treat neuroinflammatory disorders
- Case Report
- Deletion as novel variants in VPS13B gene in Cohen syndrome: Case series
- Commentary
- Translation of surface electromyography to clinical and motor rehabilitation applications: The need for new clinical figures
- Revealing key role of T cells in neurodegenerative diseases, with potential to develop new targeted therapies
- Retraction
- Retraction of “Eriodictyol corrects functional recovery and myelin loss in SCI rats”
- Special Issue “Advances in multimedia-based emerging technologies...”
- Evaluation of the improvement of walking ability in patients with spinal cord injury using lower limb rehabilitation robots based on data science

