Platelet-rich fibrin (PRF) in implants dentistry in combination with new bone regenerative flapless technique: evolution of the technique and final results
-
Antonio Cortese
Abstract
Most common techniques for alveolar bone augmentation are guided bone regeneration (GBR) and autologous bone grafting. GBR studies demonstrated long-term reabsorption using heterologous bone graft. A general consensus has been achieved in implant surgery for a minimal amount of 2 mm of healthy bone around the implant.
A current height loss of about 3-4 mm will result in proper deeper implant insertion when alveolar bone expansion is not planned because of the dome shape of the alveolar crest. To manage this situation a split crest technique has been proposed for alveolar bone expansion and the implants’ insertion in one stage surgery. Platelet-rich fibrin (PRF) is a healing biomaterial with a great potential for bone and soft tissue regeneration without inflammatory reactions, and may be used alone or in combination with bone grafts, promoting hemostasis, bone growth, and maturation.
Aim
The aim of this study was to demonstrate the clinical effectiveness of PRF combined with a new split crest flapless modified technique in 5 patients vs. 5 control patients.
Materials and methods
Ten patients with horizontal alveolar crests deficiency were treated in this study, divided into 2 groups: Group 1 (test) of 5 patients treated by the flapless split crest new procedure; Group 2 (control) of 5 patients treated by traditional technique with deeper insertion of smaller implants without split crest. The follow-up was performed with x-ray orthopantomography and intraoral radiographs at T0 (before surgery), T1 (operation time), T2 (3 months) and T3 (6 months) post-operation.
Results
All cases were successful; there were no problems at surgery and post-operative times. All implants succeeded osteointegration and all patients underwent uneventful prosthetic rehabilitation. Mean height bone loss was 1 mm, measured as bone-implant most coronal contact (Δ-BIC), and occurred at immediate T2 post-operative time (3 months). No alveolar bone height loss was detected at implant insertion time, which was instead identified in the control group because of deeper implant insertion.
Conclusion
This modified split crest technique combined with PRF appears to be reliable, safe, and to improve the clinical outcome of patients with horizontal alveolar crests deficiency compared to traditional implanting techniques by avoiding alveolar height-loss related to deeper insertion of smaller implants.
1 Introduction
Alveolar atrophy, which occurs following dental avulsion, has been ordinarily documented. The most significant bone loss observed is in the horizontal dimension with documented post-extractive alveolar reductions ranging between 3.8-6.1 mm over 3-12 months [1,2].
In these patients alveolar bone augmentation surgery is needed to obtain proper implant positioning and frontal teeth aesthetic of the smile [3,4].
The most common techniques for alveolar bone regeneration are guided bone regeneration (GBR) and autologous bone grafting [5,6].
GBR studies demonstrated long-term reabsorption using heterologous bone graft [7,8].
Problems may arise in autologous bone grafting and also from different conditions after mucosal dehiscence and graft infections with immediate or long-term reabsorption and unpredictable final bone volume [9].
The general consensus has been achieved in implant surgery for a minimal bone amount need of 2 mm of healthy bone tissue around the implant to achieve a good dental emergence and a correct prosthetic rehabilitation both for aesthetic and function [10-12].
Particularly, to preserve a healthy implant, a 1.5-2 mm thickness and a minimal alveolar width of about 7-8 mm is needed on the buccal cortical wall in relation to a 3.3-4.1 mm implant insertion [13-14].
Often, because of the dome shape of the alveolar crest, a height-loss of about 3-4 mm will be observed following deep implant insertion to avoid thread exposure, when alveolar bone expansion hasn’t been properly planned. To manage this situation, the split crest technique was proposed in the first original study by Osborn in 1985 for alveolar bone expansion and implant insertion in one stage surgery without the need for an autologous bone graft [15-16].
Further modifications were proposed adopting partial thickness mucosal flaps’ incision to preserve the periosteum adhesion to the alveolar bone [17].
In this way vascular supply and nourishment of the underlying bone was preserved, thereby avoiding bone resorption.
Moreover, bone substitute addition at the mid-crest osteotomy site was also proposed [18].
Since then, the split technique has undergone further evolution to solve several aesthetic and functional issues such as:
Buccal cortical wall reabsorption, managed by partial thickness flap or limited periosteal elevation [15].
Primary closure difficulties after bone expansion, managed by releasing incisions of the buccal periosteum [20].
To overcome some of the problems related to the technique and to achieve better aesthetic and functional results, we proposed an evolution of the procedure with the use of autologous protein rich fibrin at the osteotomy site.
PRF consists of an autologous leukocyte-platelet-rich fibrin matrix composed of a tetra molecular structure, with cytokines, platelets, and stem cells within, which acts as a biodegradable scaffold, and favors the development of micro-vascularization and is able to guide epithelial cell migration to its surface [21-22].
Some studies have demonstrated that PRF is a healing biomaterial with a great potential for bone and soft tissue regeneration, without inflammatory reactions, which may be used alone or in combination with bone grafts, promoting hemostasis, bone growth, and maturation [22-24].
Several studies have evaluated the effectiveness of PRF in intra bony and mandibular grade II defects and have found a positive clinical and radiographic outcome [25]. The routine use of such an inexpensive, autologous growth factor delivery system certainly offers an attractive option for the treatment of horizontal defects [22,26].
The aim of this study was to demonstrate the clinical effectiveness of PRF combined with a new split crest flapless modified technique also in elderly patients. In this study, patients in the study arm have been subjected to the new split crest flapless modified-technique with the use of PRF, and were compared with patients treated with traditional implanting techniques.
2 Materials and methods
This study was performed following the principles of the Declaration of Helsinki regarding research on humans; the signature of a written informed consent form from all patients was requested and obtained. Ten patients with horizontal alveolar crests deficiency were treated in this study, and were divided into 2 groups: group-1 (test group) consisting of 5 patients treated following the new flapless split crest procedure to optimize regenerative conditions by bone augmentation and implant insertion in a single stage procedure; and group-2 (control group) consisting of 5 patients treated by traditional implant surgery without split crest.
Orthopantomography and CT DentaScan/CT Cone beam were performed for every patient before treatment. In test group-1 autologous PRF was used to fill the split crest gap as regenerative material.
In control group-2, 5 patients showing similar alveolar crests horizontal deficiency were treated by a traditional technique with deeper insertion of smaller implants without any split crest. Follow-up was performed with x-ray, orthopantomography and intraoral radiographs at T0 before surgery, T1 (operation time), T2 (3 months) and T3 (6 months) from the operation time.
The patient’s past medical and social history were non-contributory, and all patients had good oral hygiene. All the patients had no contraindication to implant placement.
The operations were not performed in patients with systemic or psychological disorders that contraindicate oral surgery.
2.1 Surgical procedure
For every patient of group-1, after administration of a local anesthetic, the crestal mucosa incision was performed shifting it toward the palatal/lingual side to avoid positioning of the mucosa incision on the same site of the osteotomy line; flap elevation was performed by full thickness technique up to the buccal border of the alveolar crest. We did not perform any periosteum elevation on the buccal side to preserve vascular supply.
Linear osteotomies were performed by a scalpel blade #15 or by Beaver blade #64 on the upper jaw up to 1 mm from adjacent teeth or 4 mm exceeding expansion site limits in edentulous cases. Either bone chisel or piezo-surgery was used on the mandible in case of harder alveolar bone. No buccal bone release cuts were performed to preserving buccal bone fragment vascular supply. Expansion was possible by final oblique crest bone cuts at 1 mm from adjacent teeth without any buccal cuts (Figure 1) by splitting the buccal cortical wall from alveolar cortical wall.
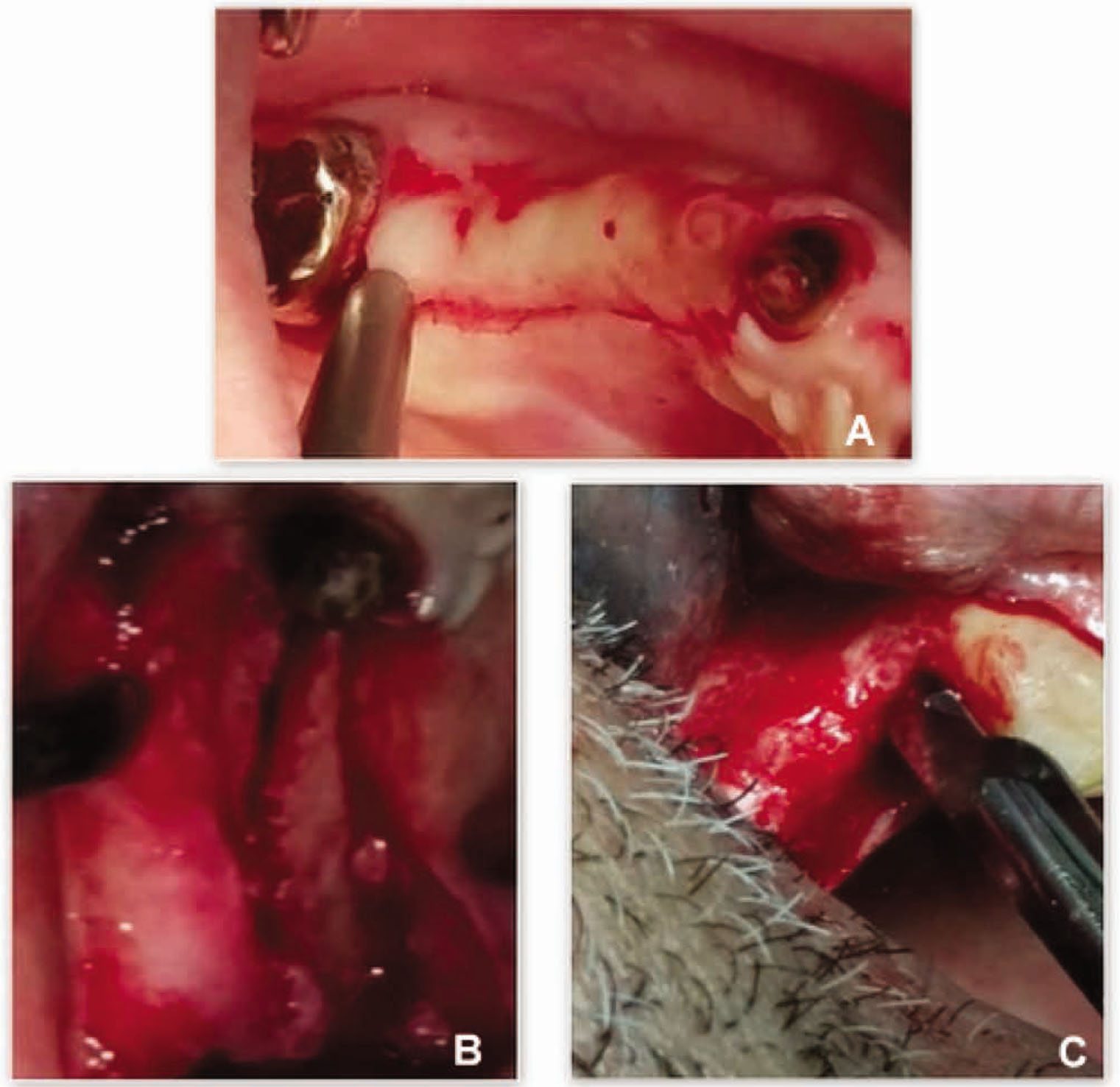
Clinical view of the initial surgical steps performed in one patient treated with the new flapless split crest procedure combined with PRF.
A: View of the crestal mucosa incision shifted toward the palatal/lingual side to avoid positioning of the mucosa incision at the same site of the osteotomy line;
B: View of full thickness flap elevation up to the buccal border of the alveolar crest. No periosteum elevation was performed on the buccal side to preserve vascular supply;
C: View of linear osteotomies performed on upper jaw up to 1 mm from adjacent teeth.
To obtain implant primary stability, a double level implant site preparation was performed: split crest was limited at the alveolar bone level by chisels; at the basal bone level site, preparation was performed by implant kit burs up to 2.8mm diameter, followed by round osteotomes or round burs up to 3.5 mm to avoid cortical wall damages. Due to the shape of the alveolar bones, thin at the top and expanded at the basal level, bone expansion was not usually needed at basal level, where implant site preparation by set kit burs followed by round osteotomes or ball burs, resulted in precise implant site preparation at basal level with good primary stability. Round osteotomes or ball burs were selected to avoid the risks of buccal wall fracture for bone fragment entrapment when drilling by larger (3.5) implant kit drills (Figure 2).
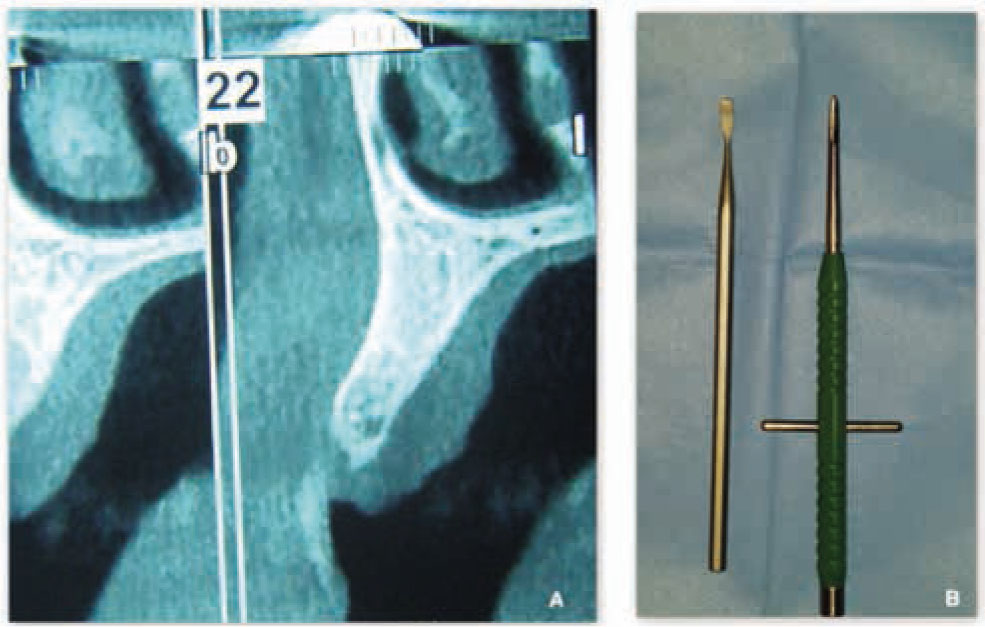
Double level implant site preparation.
A: To obtain implant primary stability, a double level implant site preparation is performed: split crest is limited at the alveolar bone level by chisels;
B: at the basal bone level site preparation is performed by implant kit burs up to 2.8mm diameter, followed by round osteotomes or round burs up to 3.5mm to avoid cortical wall damage.
To obtain expanded bone stability and promoting regeneration, osteotomy gaps were filled by autologous PRF and bone substitute, therefore combining regenerative technique with split crest (Figure 3).
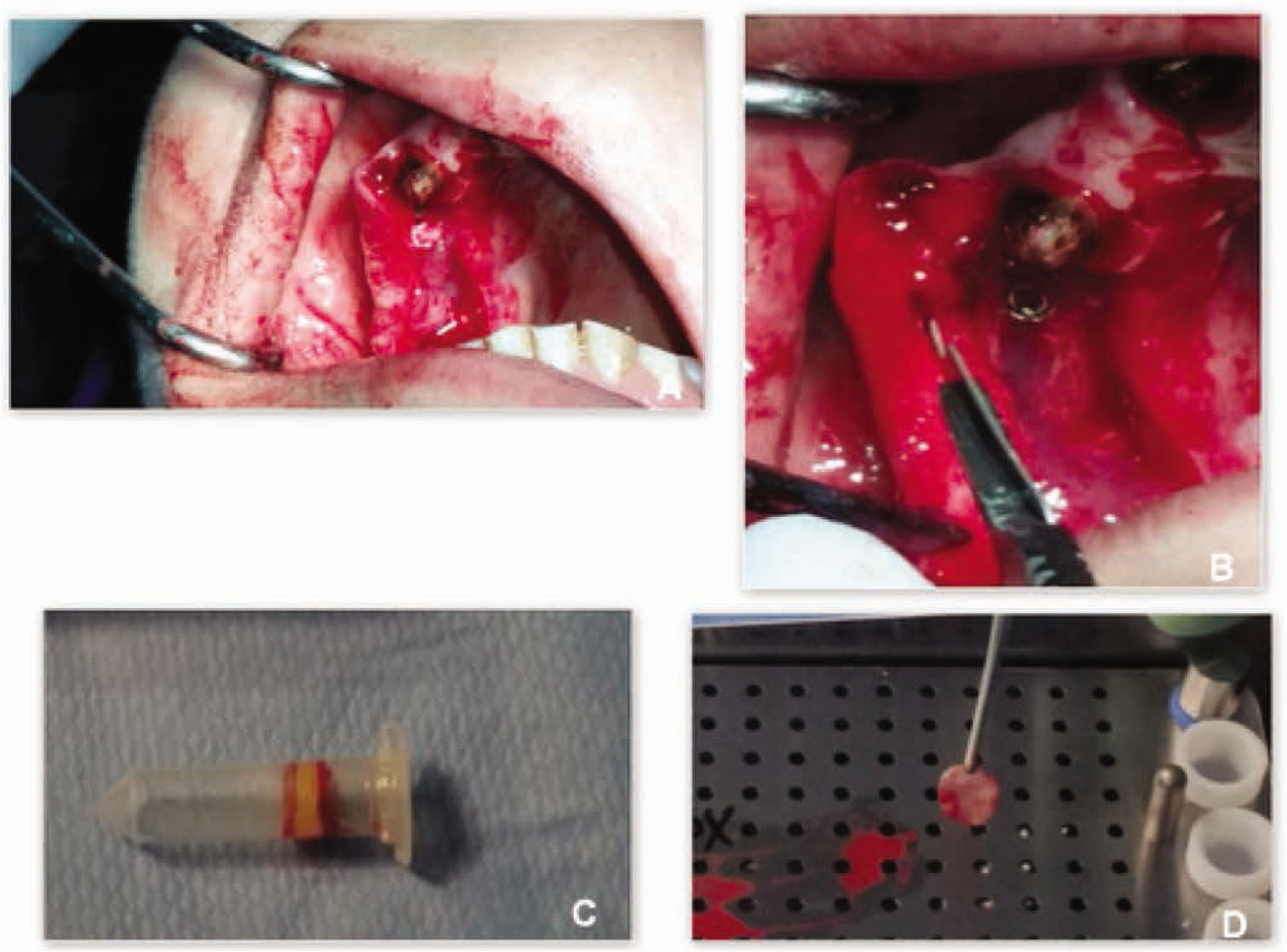
Clinical view of surgical steps performed in one patient treated with the new flapless split crest procedure combined with PRF.
A: To obtain expanded bone stability osteotomy gaps were filled by autologous PRF and bone substitute to combine regenerative technique with split crest;
B: To obtain primary closure of the wound, releasing incision was performed at the crestal mucosa level to gain sufficient lengthening for primary closure;
C: Blood samples were collected into an 8.5 ml tubes without any anticoagulant, and immediately centrifuged;
D: After centrifugation PRF was obtained from the middle of the tube.
To prepare the PRF, 20-40 ml of peripheral blood at the time of surgery were collected. Blood samples were collected into an 8.5 ml tubes without any anticoagulant, and immediately centrifuged at 2,700 rpm for 12 minutes to prevent coagulation cascades: this protocol was used in 2 of 5 cases, obtaining a normal gelling biomaterial to be used as regenerative and stimulating material. In the other three cases centrifugation time setting was 15-20 minutes at 3,000 rpm for more consistent substance to be used as a membrane in the split crest gap.
Centrifugation time changed in relation to consistency needed for the PRF: the longer the centrifugation time, the more the consistency of the PRF sample.
After centrifugation a PRF was obtained from the middle of the tube: red corpuscles centrifuged at bottom and acellular plasma at the top were discarded.
PRF was put directly inside the osteotomy gap mixed with coral bone substitute for larger defects, therefore combining both split crest technique and GBR (Figure 3).
To obtain primary closure of the wound, releasing incision was performed at the crestal mucosa level to gain sufficient lengthening for primary closure (Figure 4) [27].
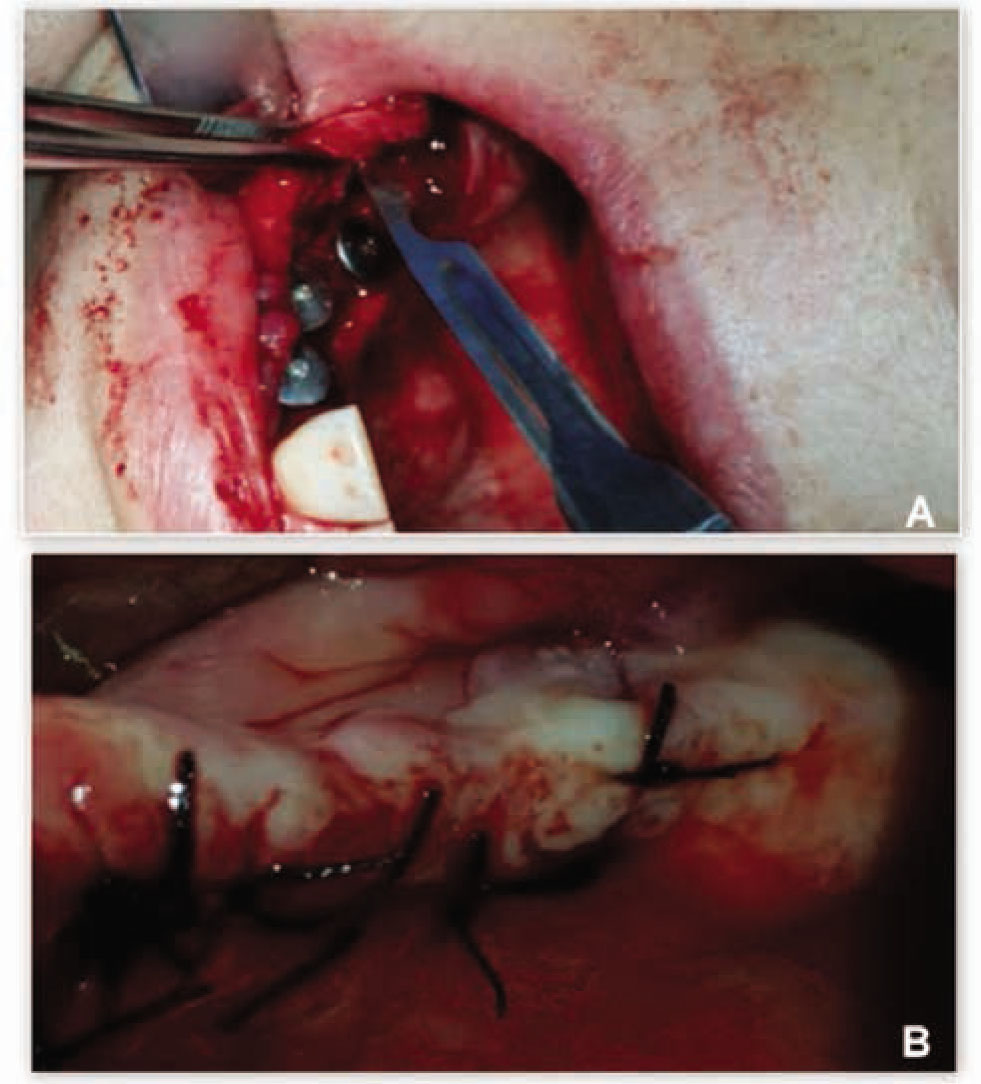
Clinical view of the final surgical steps performed in one patient treated with the new flapless split crest procedure combined with PRF.
A: Implant insertion and flap release incision;
B: Primary closure of the flap
In this way no periosteal elevation was performed on the buccal area preserving cortical plate nourishment. Also attached gingiva full coverage was obtained at the osteotomy sites by keratinized mucosa elongation for proper bone nourishment and stability.
Attention must be paid during the healing time to avoid any compression on the implant site by provisional prosthesis. Prosthesis must be trimmed to avoid compression on vertical and particularly on the horizontal dimension after alveolar arch expansion by splitting.
An orthopantomography and CT DentaScan/CT Cone beam were performed for every patient before surgery to have a preliminary radiological investigation and to get a general overview of the jawbones and relevant anatomic landmarks in a bi-dimensional plane (Figure 5). Also intraoral and face photographs were taken pre-operatively for aesthetic and functional evaluation of the patients status. For all the patients a beta-lactam antibiotic (Amoxicillin) was given orally, 2gr. one-hour before surgery. Post-operative therapy required good oral hygiene, rinsing with mouthwash containing 0.2% chlorhexidine solution twice a day and an evening application of the same product in gel form, as well as the administration of a non-steroidal anti-inflammatory drug (Ketoprofen 80mg) for three consecutive days.
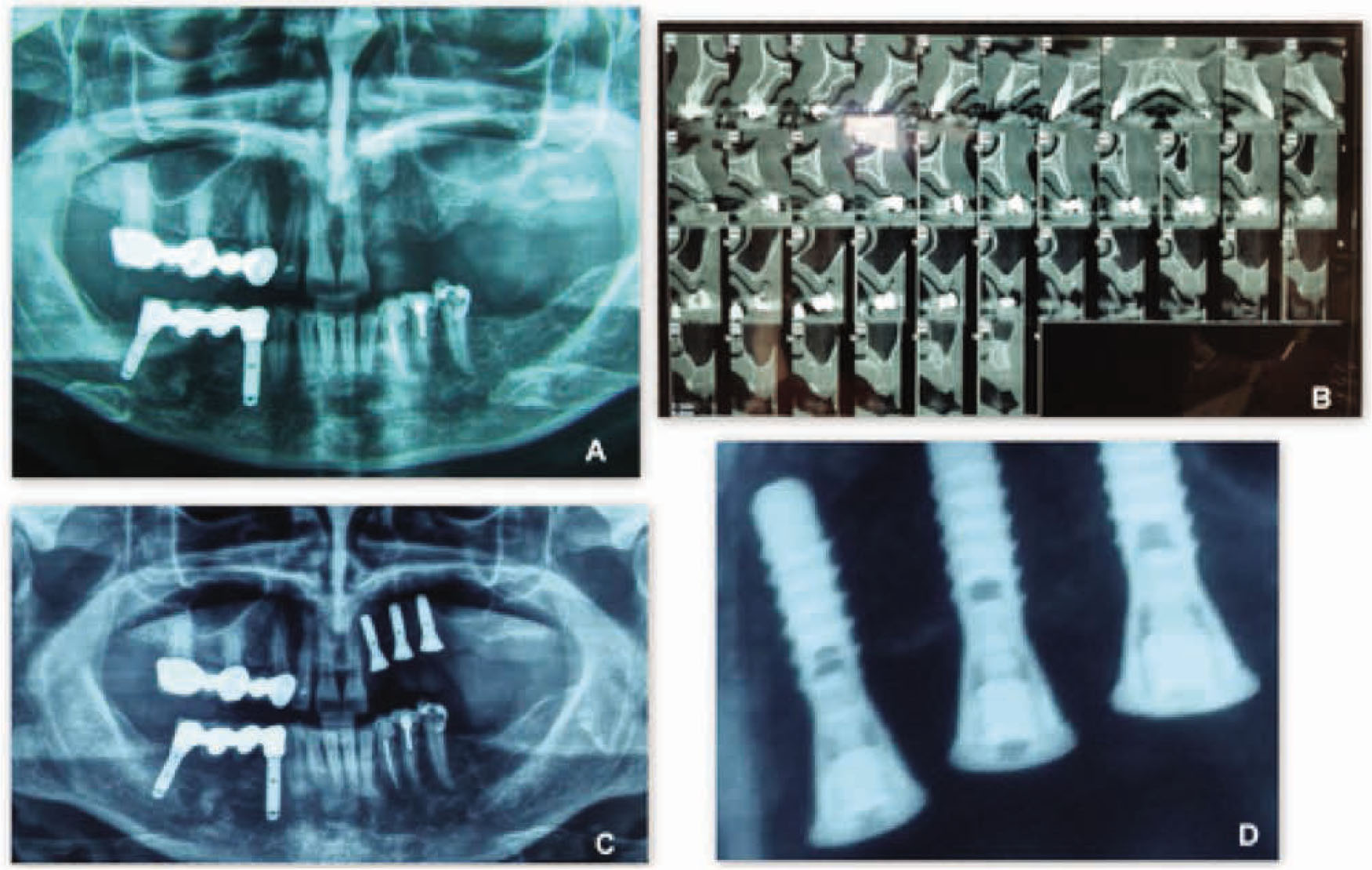
Radiographic views of a patient treated with the new flapless split crest procedure combined with PRF.
A: Pre-operative X-Ray Orthopantomography;
B: Pre-operative CT-Dentascan;
C: Post-operative X-Ray Orthopantomography;
D: 6 months post operative detail X-Ray image of the bone level at T3.

Final result and clinical oral view of a patient treated with the new flapless split crest procedure combined with PRF. Final aesthetic result obtained without any additional graft.
Follow-up was performed by conventional radiological imaging (orthopanoramic and intra-oral x-rays) at T1 (immediately after surgery), T2 (3-months after surgery) and T3 (6-months after surgery).
3 Results
All cases were successful; there were no problems at surgery time, as well as at post-operative and osteointegration periods. All implants achieved good osteointegration. These results were obtained by accurately managing the immediate and late postoperative period in all of the treated patients. All patients underwent uneventful implant surgery. All implants were placed according to the manufacturer’s instructions and achieved primary stability. No intra-operative surgical complications were recorded.
Particular attention was paid to oral hygiene, and to inappropriate early prosthodontic loading by provisional prosthesis at immediate and late postoperative time.
The main characteristics and results related to the 10 patients belonging to the study are presented in Tables 1 and 2 concerning the 5 cases of group-1 (test cases) and in Table 3 for the 5 cases of group-2 (control cases).
Demographic and clinical data from group-1 patients.
Table illustrates for five patients treated with split crest flapless technique, their implants distribution, type of PRF used, bone height loss measured from lower border of the mandible and from nasal and sinus floors to alveolar bridge (pre-op) and to highest bone-implant contact (post-op) at T0 (pre-operative time), T1 (immediate post-operative time), T2 (3 months after surgery), and T3 (6 months after surgery).
| Age | Implants placed | Implant length, mm | Torque, N.cm | PRF type | Bone height loss (T0, T1, T2, T3) mm | |
|---|---|---|---|---|---|---|
| Patient 1 | 53 | 1 | 11 | 35 | More consistent | T0:0; T1:0; T2:0; T3:1 |
| Patient 2 | 59 | 4 | ≥ 8;≤ 13 | 40 | Normal gel | T0:0; T1:0; T2:0; T3:1 |
| Patient 3 | 60 | 2 | 11 | 35 | More consistent | T0:0; T1:0; T2:1; T3:2 |
| Patient 4 | 57 | 1 | 8.5 | 35 | More consistent | T0:0; T1:0; T2:0; T3:1 |
| Patient 5 | 55 | 2 | ≥ 8;≤ 11 | 40 | Normal gel | T0:0; T1:0; T2:0; T3:1 |
Demographic and clinical data from group-1 patients.
Table illustrates for five patients treated with split crest flapless technique the initial and final alveolar crest width. The mean expansion by split crest technique in 10 cases was 3.35 mm.
| Age | Sex | Initial bone width | Final bone width | Number of implants | Timing of implant placement | Complications | |
|---|---|---|---|---|---|---|---|
| Patient 1 | 53 | F | 3.5 mm | 7.5 mm | 3 | Immediate | NO |
| Patient 2 | 59 | F | 4 mm | 7 mm | 4 | Immediate | NO |
| Patient 3 | 60 | F | 3 mm | 7 mm | 2 | Immediate | NO |
| Patient 4 | 57 | F | 4 mm | 7 mm | 1 | Immediate | NO |
| Patient 5 | 55 | F | 3.5 mm | 6.5 mm | 2 | Immediate | NO |
Bone heights before surgery were calculated by measuring the distances between alveolar crest and implant bone limits (sinus and nasal floors and the connecting lines) for the upper jaw and between the inferior border of the mandible and alveolar crest for the lower jaw.
At postoperative time, after implant insertion, bone height was measured from bone limits and the lower border of the mandible up to the most coronal level of bone to implant contact (BIC).
Comparing results shown in Table 1 and Table 3 for height decrease at T0, T1, T2 and T3 between the new split crest and the traditional technique, it is evident that the new split crest technique group experienced less bone height loss.
Demographic and clinical data from group-2 patients.
Table illustrates bone height loss for five control patients with similar alveolar crest thinness that were implanted by direct deeper insertion of smaller implants.
| Age | Implants placed | Implant length, mm | Torque, N.cm | Bone height loss (T0, T1, T2, T3), mm | |
|---|---|---|---|---|---|
| Patient 1 | 57 | 2 | 11 | 40 | T0:0; T1:2; T2:3; T3:3 |
| Patient 2 | 60 | 1 | 8 | 35 | T0:0; T1:3; T2:4; T3:4 |
| Patient 3 | 52 | 4 | ≥ 11; ≤ 13 | 35 | T0:0; T1:2; T2:2; T3:2 |
| Patient 4 | 55 | 2 | 11 | 40 | T0:0; T1:2; T2:2; T3:3 |
| Patient 5 | 57 | 2 | ≥ 8;≤ 11 | 35 | T0:0; T1:2; T2:2; T3:2 |
In group-1, as shown in Table 1, the mean final height bone loss was 1.2 mm mainly occurring at postoperative time T2 (3 months after surgery) measured by Δ-BIC at T2 and T3 in relation to T0.
In the control group, patients with similar alveolar crest thinness were implanted without any split crest bone expansion, but only by deeper insertion of smaller implants (Table 3). Final height bone loss was of 2.8 mm at T3, showing a bone loss of 2.2 mm at T1 (immediately after surgery) and of additional 0.6 mm at T3 (6 months after surgery) in relation to T0.
In test group operated by the modified split crest technique, the mean alveolar crest expansion was 3.35 mm. As shown in Table 2, the expansion measurements achieved by the new modified split crest technique are demonstrated by the initial (before surgery) and final (after surgery) alveolar crest measurements.
4 Discussion
Several advantages are achieved by the single stage split crest procedure for alveolar crest augmentation and implant insertion among which are: reduction of the morbidities and time needed for dental rehabilitation compared with other common regenerative procedures (guided bone regeneration and autologous bone graft) [15,19]; increment of bone height availability for implant insertion allowing fixture positioning at the marginal crest level by expansion.19 On the other hand we observed that traditional implant insertion in control group-2 patients with similar alveolar crest thinness who were implanted without any split crest, but only by deeper insertion of smaller implants, showed greater bone resorption at T1 because of bone height loss at implant insertion.
The main problem in alveolar expansion is the stability of the buccal cortical plates over time [28]. To prevent this risk, our modified surgical technique utilizes several procedures aimed at preserving nourishment of the buccal cortical plates by: 1) shifting the flap incisions on the palatal/lingual side without any buccal muco-periosteal elevation; 2) gentle osteotomy techniques for the alveolar crest that avoid medial and distal bone buccal cuts [19,29]; 3) autologous PRF positioning at osteotomy gap after expansion, for contemporary GBR by bone substitute addition for wider expansions; 4) preservation of periosteal attachment on buccal wall and osteotomy gap coverage by attached gingiva with primary closure by elongation of keratinized mucosa flap. All of these procedures seem to be effective for the quality of the final results [30].
In accordance with previously published data showing good results from the combination of split crest technique with GBR [27,31], we presented improved results achieved by the association of new developed split crest with the use of autologous PRF.
5 Conclusion
Although limitation of this study are the restricted number of cases and the shortness of the postoperative control time, this modified split crest technique appears to be reliable, safe and able to improve clinical results obtained, compared to traditional techniques by avoiding alveolar height loss related to deeper insertion of smaller implants.
Alternative procedures like GBR and autologous bone grafting both shows some disadvantages for membrane exposure risks with related bone resorption or implant and donor site morbidity risks with immediate-and longterm bone graft resorption.
Additional studies are needed to verify long-term survival of the buccal cortical walls by this modified split crest technique. Further evolutions may be possible in relation to the development of these significant new techniques in the Maxillofacial Surgery arena [32-35].
Conflict of interest: The authors declare that they do not have any conflict of interest related to this study.
References
[1] Schropp L, Wenzel A, Kostopoulos L, Karring T. Bone healing and soft tissue contour changes following single-tooth extraction: a clinical and radiographic 12-month prospective study. Int J Periodontics Restorative Dent. 2003; 23(4):313-323Suche in Google Scholar
[2] Avila-Ortiz G, Elangovan S, Kramer KW, Blanchette D, Dawson DV. Effect of alveolar ridge preservation after tooth extraction: a systematic review and meta-analysis. J Dent Res. 2014; 93(10):950-95810.1177/0022034514541127Suche in Google Scholar PubMed PubMed Central
[3] Atieh MA, Alsabeeha NH, Payne AG, Duncan W, Faggion CM, Esposito M. Interventions for replacing missing teeth: alveolar ridge preservation techniques for dental implant site development. Cochrane Database Syst Rev. 2015; 28;(5):CD01017610.1002/14651858.CD010176.pub2Suche in Google Scholar PubMed PubMed Central
[4] Cortese A, Pantaleo G, Amato M, Claudio PP. Chin Wing Osteotomy for Bilateral Goldenhar Syndrome Treated by “Chin Wing Mentoplasty”: Aesthetic, Functional, and Histological Considerations, J. Craniofac. Surg. 26; 2015; 1628-163010.1097/SCS.0000000000001859Suche in Google Scholar PubMed
[5] Meloni SM, De Riu G, Pisano M, Dell’aversana Orabona G, Piombino P, Salzano G, Quarato D, Riccardi E, Belli E, Ungari C. Computer-assisted implant surgery and immediate loading in edentulous ridges with dental fresh extraction sockets. Two years results of a prospective case series study. Eur Rev Med Pharmacol Sci. 2013; 17(21):2968-2973Suche in Google Scholar
[6] Sammartino G, Pantaleo G, Nuzzolo P, Amato M, Riccitiello F. Minimally invasive approaches to optimize block grafting: a case report. Journal of Oral Implantology 2016; 42(2):176-17910.1563/aaid-joi-D-14-00076Suche in Google Scholar PubMed
[7] Simion M, Dahlin C, Blair K, Schenk RK. Effect of different microstructures of e-PTFE membranes on bone regeneration and soft tissue response: a histologic study in canine mandible. Clin Oral Implants Res. 1999; 10(2):73-8410.1034/j.1600-0501.1999.100201.xSuche in Google Scholar PubMed
[8] Carlino F, Villani GP, Berti A, Pantaleo G, Cortese A, Claudio PP. Osteodistraction With Dental Implant-Borne Devices for Bone Regeneration in Atrophied Premaxilla. J Craniofac Surg. 2016 (in press)10.1097/SCS.0000000000003127Suche in Google Scholar PubMed
[9] Carlino F, Pantaleo G, Ciuffolo F, Claudio PP, Cortese A. New Technique for Mandibular Symphyseal Distraction by a Double-Level Anchorage and Fixation System: Advantages and Results. J Craniofac Surg. 2016; 27(6):1469-147510.1097/SCS.0000000000002831Suche in Google Scholar PubMed
[10] Misch CE, Perel ML, Wang HL, Sammartino G, Galindo-Moreno P, Trisi P, Steigmann M, Rebaudi A, Palti A, Pikos MA, Schwartz-Arad D, Choukroun J, Gutierrez-Perez JL, Marenzi G, Valavanis DK. Implant success, survival, and failure: the International Congress of Oral Implantologists (ICOI) Pisa Consensus Conference. Implant Dent. 2008; 17(1):5-1510.1097/ID.0b013e3181676059Suche in Google Scholar PubMed
[11] Mestas G, Alarcón M, Chambrone L. Long-Term Survival Rates of Titanium Implants Placed in Expanded Alveolar Ridges Using Split Crest Procedures: A Systematic Review. Int J Oral Maxillofac Implants. 2016; 31(3):591-59910.11607/jomi.4453Suche in Google Scholar PubMed
[12] Lo Giudice G, Iannello G, Terranova A, Lo Giudice R, Pantaleo G, Cicciù M. Transcrestal sinus lift procedure approaching atrophic maxillary ridge. A 60 months clinical and radiological follow-up evaluation. Int. J. Dent, 2015; 26165210.1155/2015/261652Suche in Google Scholar PubMed PubMed Central
[13] Chiapasco M, Romeo E, Vogel G. Vertical distraction osteogenesis of edentulous ridges for improvement of oral implant positioning: a clinical report of preliminary results. Int J Oral Maxillofac Implants. 2001; 16(1):43-51Suche in Google Scholar
[14] Nedir R, Bischof M, Szmukler-Moncler S, Bernard JP, Samson J.Clin Oral Implants. Predicting osseointegration by means of implant primary stability. Res. 2004; 15(5):520-52810.1111/j.1600-0501.2004.01059.xSuche in Google Scholar PubMed
[15] Waechter J, Leite FR, Nascimento GG, Carmo Filho LC, Faot F. The split crest technique and dental implants: a systematic review and meta-analysis. Int J Oral Maxillofac Surg. 2016 Sep 14. (in press)10.1016/j.ijom.2016.08.017Suche in Google Scholar PubMed
[16] Cortese A, Pantaleo G, Borri A, Caggiano M, Amato M. Platelet-rich fibrin (PRF) in implant dentistry in combination with new bone regenerative technique in elderly patients. Int J Surg Case Rep. 2016; 22;28:52-5610.1016/j.ijscr.2016.09.022Suche in Google Scholar PubMed PubMed Central
[17] Figliuzzi MM, Giudice A, Pileggi S, Pacifico D, Marrelli M, Tatullo M, Fortunato L. Implant-Prosthetic Rehabilitation in Bilateral Agenesis of Maxillary Lateral Incisors with a Mini Split Crest. Case Rep Dent. 2016; 2016:359132110.1155/2016/3591321Suche in Google Scholar PubMed PubMed Central
[18] Figliuzzi M, Mangano FG, Fortunato L, De Fazio R, Macchi A, Iezzi G, Piattelli A, Mangano C. Vertical ridge augmentation of the atrophic posterior mandible with custom-made, computer-aided design/computer-aided manufacturing porous hydroxyapatite scaffolds. J Craniofac Surg. 2013; 24(3):856-85910.1097/SCS.0b013e31827ca3a7Suche in Google Scholar PubMed
[19] Cortese A, Pantaleo G, Amato M, Claudio PP. Ridge Expansion by Flapless Split Crest and Immediate Implant Placement: Evolution of the Technique. J Craniofac Surg. 2016; 27(2):e123-12810.1097/SCS.0000000000002367Suche in Google Scholar PubMed
[20] Crespi R, Bruschi GB, Gastaldi G, Capparé P, Gherlone EF. Immediate Loaded Implants in Split-Crest Procedure. Clin Implant Dent Relat Res. 2015; 17 Suppl 2:e692-69810.1111/cid.12316Suche in Google Scholar PubMed
[21] Dohan DM, Choukroun J, Diss A, Dohan SL, Dohan AJ, Mouhyi J, Gogly B. Platelet-rich fibrin (PRF): a second-generation platelet concentrate. Part I: technological concepts and evolution. Oral. Surg. Oral. Med. Oral. Pathol. Oral. Radiol. Endod. 101; 2006; e37-4410.1016/j.tripleo.2005.07.008Suche in Google Scholar PubMed
[22] Miron RJ, Fujioka-Kobayashi M, Bishara M, Zhang Y, Hernandez M, Choukroun J. Platelet-Rich Fibrin and Soft Tissue Wound Healing: A Systematic Review. Tissue Eng Part B Rev. 2016; 10 (in press)10.1089/ten.teb.2016.0233Suche in Google Scholar PubMed
[23] Temmerman A, Vandessel J, Castro A, Jacobs R, Teughels W, Pinto N, Quirynen M. The use of leucocyte and platelet-rich fibrin in socket management and ridge preservation: a split-mouth, randomized, controlled clinical trial. J Clin Periodontol. 2016; 43(11):990-99910.1111/jcpe.12612Suche in Google Scholar PubMed
[24] Fujioka-Kobayashi M, Miron RJ, Hernandez M, Kandalam U, Zhang Y, Choukroun J. Optimized Platelet Rich Fibrin With the Low Speed Concept: Growth Factor Release, Biocompatibility and Cellular Response. J Periodontol. 2016; 2:1-1710.1902/jop.2016.160443Suche in Google Scholar PubMed
[25] Troiano G, Laino L, Dioguardi M, Giannatempo G, Lo Muzio L, Lo Russo L. Mandibular Class II Furcation Defect Treatment: Effects of the Addition of Platelet Concentrates to Open Flap: A Systematic Review and Meta-Analysis of Randomized Clinical Trials. J Periodontol. 2016; 87(9):1030-103810.1902/jop.2016.160058Suche in Google Scholar PubMed
[26] Joseph VR, Sam G, Amol NV. Clinical evaluation of autologous platelet rich fibrin in horizontal alveolar bony defects. J Clin Diagn Res. 2014; 8(11):ZC43-4710.7860/JCDR/2014/9948.5129Suche in Google Scholar PubMed PubMed Central
[27] Bassetti M, Kaufmann R, Salvi GE, Sculean A, Bassetti R. Soft tissue grafting to improve the attached mucosa at dental implants: A review of the literature and proposal of a decision tree. Quintessence Int. 2015; 46(6):499-510Suche in Google Scholar
[28] Venza M, Visalli M, Lo Giudice G., Cicciù M, Passi P, Teti D. Changes in inflammatory mediators in peri-implant fluid after implant insertion. J Periodontol. 2009; 80(2):297-30610.1902/jop.2009.080411Suche in Google Scholar PubMed
[29] Cortese A, Savastano M, Savastano G, Papa F, Howard CM, Claudio PP. Maxillary constriction treated by a new palatal distractor device: surgical and occlusal evaluations of 10 patients. J Craniofac Surg. 2010; 21(2):339-34310.1097/SCS.0b013e3181cf60e6Suche in Google Scholar PubMed
[30] Cortese A, Savastano G, Amato M, Cantone A, Boschetti C, Claudio PP. New palatal distraction device by both bone-borne and tooth-borne force application in a paramedian bone anchorage site: surgical and occlusal considerations on clinical cases. J. Craniofac. Surg, 25; 2014; 589-59510.1097/SCS.0000000000000674Suche in Google Scholar PubMed
[31] Bassetti MA, Bassetti RG, Bosshardt DD. The alveolar ridge splitting/expansion technique: a systematic review. Clin Oral Implants Res. 2016; 27(3):310-32410.1111/clr.12537Suche in Google Scholar PubMed
[32] Cortese A, Savastano G, Amato M, Pantaleo G, Claudio PP. Intraoral epimucosal fixation for reducible maxillary fractures of the jaws; surgical considerations in comparison to current techniques. J Craniofac Surg. 2014; 25(6):2184-218710.1097/SCS.0000000000001104Suche in Google Scholar PubMed
[33] Cortese A, Savastano G, Savastano M, Spagnuolo G, Papa F. New technique: Le Fort I osteotomy for maxillary advancement and palatal distraction in 1 stage. J Oral Maxillofac Surg. 2009; 67(1):223-22810.1016/j.joms.2007.08.005Suche in Google Scholar PubMed
[34] Cortese A, Pantaleo G, Ferrara I, Vatrella A, Cozzolino I, Di Crescenzo V, Amato M. Bone and soft tissue non-Hodgkin lymphoma of the maxillofacial area: report of two cases, literature review and new therapeutic strategies. Int J Surg. 2014; 12 Suppl 2:S23-2810.1016/j.ijsu.2014.08.388Suche in Google Scholar PubMed
[35] Cortese A, Savastano M, Cantone A, Claudio PP. A new palatal distractor device for bodily movement of maxillary bones by rigid self-locking miniplates and screws system. J Craniofac Surg. 2013; 24(4):1341-134610.1097/SCS.0b013e31828041a7Suche in Google Scholar PubMed
© 2017 Antonio Cortese et al.
This work is licensed under the Creative Commons Attribution-NonCommercial-NoDerivatives 3.0 License.
Artikel in diesem Heft
- Regular Articles
- Intravascular treatment of left subclavian artery aneurysm coexisting with aortic coarctation in an adult patient
- Regular Articles
- Effect of electrical stimulation on blood flow velocity and vessel size
- Regular Articles
- Live birth pregnancy outcome after first in vitro fertilization treatment in a patient with Systemic Lupus Erythematosus and isolated high positive IgA anti-β2glycoprotein I antibodies: a case report
- Regular Articles
- Periodontal ligament stem cells regulate apoptosis of neutrophils
- Regular Articles
- Platelet-rich fibrin (PRF) in implants dentistry in combination with new bone regenerative flapless technique: evolution of the technique and final results
- Regular Articles
- The significance of strong ion gap for predicting return of spontaneous circulation in patients with cardiopulmonary arrest
- Regular Articles
- Clinicopathology of EpCAM and EGFR in human epithelial ovarian carcinoma
- Regular Articles
- Intraosseous lipoma of the mandibula: A case report and review of the literature
- Regular Articles
- Transurethral resection of the prostate, bladder explosion and hyponatremic encephalopathy: a rare case report of malpractice
- Regular Articles
- Brain strokes related to aortic aneurysma – the analysis of three cases
- Regular Articles
- Effect of Bicyclol tablets on drug induced liver injuries after kidney transplantation
- Regular Articles
- Plasma free fatty acids in hyperemesis gravidarum pregnancy
- Regular Articles
- Impact of chromosomal rearrangement upon DNA methylation patterns in leukemia
- Regular Articles
- Gefitinib versus docetaxel in treated non-small-cell lung cancer: a meta-analysis
- Regular Articles
- The clinical characteristics of patients with chronic idiopathic anal pain
- Regular Articles
- Bone tunnel impaction reduced the tibial tunnel enlargement
- Regular Articles
- Effects of S-1 combined with radiotherapy in the treatment of nasopharyngeal cancer: a meta-analysis based on randomized controlled trials
- Regular Articles
- Predictions and outcomes of atrial fibrillation in the patients with acute myocardial infarction
- Regular Articles
- An accuracy study of the Intracavitary Electrocardiogram (IC-ECG) guided peripherally inserted central catheter tip placement among neonates
- Regular Articles
- Serum CA125, CA199 and CEA combined detection for epithelial ovarian cancer diagnosis: A meta-analysis
- Regular Articles
- Surface coil intensity correction in magnetic resonance imaging in spinal metastases
- Regular Articles
- Muscle stem cell and physical activity: what point is the debate at?
- Regular Articles
- MicroRNA let-7g directly targets forkhead box C2 (FOXC2) to modulate bone metastasis in breast cancer
- Regular Articles
- Monitoring health inequalities at the municipal level: Lithuanian experience
- Regular Articles
- Role of Epstein-Barr virus in the development of nasopharyngeal carcinoma
- Regular Articles
- Thrombectomy combined with indwelling-catheter thrombolysis is more effective than pure thrombectomy for the treatment of lower extremity deep venous thrombosis
- Regular Articles
- Expression of Hepcidin and Neogenin in colorectal cancer
- Regular Articles
- Carnitine and adiponectin levels in breast cancer after radiotherapy
- Regular Articles
- Pathophysiology of meningioma growth in pregnancy
- Regular Articles
- Causal neuro-immune relationships at patients with chronic pyelonephritis and cholecystitis. Correlations between parameters EEG, HRV and white blood cell count
- Regular Articles
- Measuring efficiency of secondary healthcare providers in Slovenia
- Regular Articles
- Galectin-3 expression in colorectal cancer and its correlation with clinical pathological characteristics and prognosis
- Regular Articles
- Model for studying anti- allergic drugs for allergic conjunctivitis in animals
- Regular Articles
- Barriers perceived by nurses in the optimal treatment of postoperative pain
- Regular Articles
- Tumor microenvironment in treatment of glioma
- Regular Articles
- Delirium risk of dexmedetomidine and midazolam in patients treated with postoperative mechanical ventilation: A meta-analysis
- Regular Articles
- Hemangioma of the rib: a rare case report and literature review
- Regular Articles
- The diagnostic accuracy of conventional forceps biopsy compared to ESD
- Regular Articles
- Increased miR-25 expression in serum of gastric cancer patients is correlated with CA19-9 and acts as a potential diagnostic biomarker
- Regular Articles
- Therapeutic nanomedicine surmounts the limitations of pharmacotherapy
- Regular Articles
- Relationship between PD-L1 expression and clinical characteristics in patients with breast invasive ductal carcinoma
- Regular Articles
- Trypsinogen activation peptide induces HMGB1 release from rat pancreatic acinar cells
- Regular Articles
- The effective regulation of pro- and anti-inflammatory cytokines induced by combination of PA-MSHA and BPIFB1 in initiation of innate immune responses
- Regular Articles
- Cell based therapeutic approach in vascular surgery: application and review
- Regular Articles
- Clinical efficacy of alprostadil combined with α-lipoic acid in the treatment of elderly patients with diabetic nephropathy
- Regular Articles
- Professional burnout and concurrent health complaints in neonatal nursing
- Regular Articles
- Esophageal xanthoma: presence of M2 macrophages suggests association with late inflammatory and reparative processes
- Regular Articles
- Cone beam computed tomography analysis in 3D position of maxillary denture
- Regular Articles
- CK20 mRNA expression in serum as a biomarker for colorectal cancer diagnosis: A meta-analysis
- Regular Articles
- Serum AFU, 5’-NT and AFP as biomarkers for primary hepatocellular carcinoma diagnosis
- Regular Articles
- Absolute reliability and concurrent validity of hand held dynamometry and isokinetic dynamometry in the hip, knee and ankle joint: systematic review and meta-analysis
- Regular Articles
- The Fountain of Youth: A tale of parabiosis, stem cells, and rejuvenation
- Regular Articles
- Foam sclerotherapy during shunt surgery for portal hypertension and varices
- Regular Articles
- Insomnia and depression: Japanese hospital workers questionnaire survey
- Regular Articles
- Serum NF-κBp65, TLR4 as biomarker for diagnosis of preeclampsia
- Regular Articles
- Docetaxel/cisplatin therapy in myasthenia gravis with hypertension/diabetes
- Regular Articles
- Fluid resuscitation and markers of glycocalyx degradation in severe sepsis
- Regular Articles
- Modified Sauve-Kapandji procedure for patients with old fractures of the distal radius
- Regular Articles
- Bile leakage after liver transplantation
- Regular Articles
- VEGF overexpression predicts poor survival in hepatocellular carcinoma
- Regular Articles
- Galen vein aneurysm– challenge for treatment
- Regular Articles
- Retrieval of a broken sewing needle from the sacrum aided by a permanent magnet: a case report and literature review
- Regular Articles
- HIV/STI prevention interventions: A systematic review and meta-analysis
- Regular Articles
- Aortic aneurysm as a complication of myeloperoxidase-antineutrophil cytoplasmic antibody-associated vasculitis
- Regular Articles
- Real-time monitoring of contrast-enhanced ultrasound for radio frequency ablation
- Regular Articles
- Successful drug-eluting stent implantation in a male patient with dextrocardia: a case report
- Regular Articles
- Primary pleomorphic liposarcoma of fallopian tube with recurrence: a case report and review of the literature
- Regular Articles
- Color Doppler Ultrasound in Uterine Arterial Embolization
- Regular Articles
- Pattern of alcohol consumption by young people from North Eastern Portugal
- Regular Articles
- Effects of out-of-hospital continuing nursing on schizophrenia patients' rehabilitation and quality of life
Artikel in diesem Heft
- Regular Articles
- Intravascular treatment of left subclavian artery aneurysm coexisting with aortic coarctation in an adult patient
- Regular Articles
- Effect of electrical stimulation on blood flow velocity and vessel size
- Regular Articles
- Live birth pregnancy outcome after first in vitro fertilization treatment in a patient with Systemic Lupus Erythematosus and isolated high positive IgA anti-β2glycoprotein I antibodies: a case report
- Regular Articles
- Periodontal ligament stem cells regulate apoptosis of neutrophils
- Regular Articles
- Platelet-rich fibrin (PRF) in implants dentistry in combination with new bone regenerative flapless technique: evolution of the technique and final results
- Regular Articles
- The significance of strong ion gap for predicting return of spontaneous circulation in patients with cardiopulmonary arrest
- Regular Articles
- Clinicopathology of EpCAM and EGFR in human epithelial ovarian carcinoma
- Regular Articles
- Intraosseous lipoma of the mandibula: A case report and review of the literature
- Regular Articles
- Transurethral resection of the prostate, bladder explosion and hyponatremic encephalopathy: a rare case report of malpractice
- Regular Articles
- Brain strokes related to aortic aneurysma – the analysis of three cases
- Regular Articles
- Effect of Bicyclol tablets on drug induced liver injuries after kidney transplantation
- Regular Articles
- Plasma free fatty acids in hyperemesis gravidarum pregnancy
- Regular Articles
- Impact of chromosomal rearrangement upon DNA methylation patterns in leukemia
- Regular Articles
- Gefitinib versus docetaxel in treated non-small-cell lung cancer: a meta-analysis
- Regular Articles
- The clinical characteristics of patients with chronic idiopathic anal pain
- Regular Articles
- Bone tunnel impaction reduced the tibial tunnel enlargement
- Regular Articles
- Effects of S-1 combined with radiotherapy in the treatment of nasopharyngeal cancer: a meta-analysis based on randomized controlled trials
- Regular Articles
- Predictions and outcomes of atrial fibrillation in the patients with acute myocardial infarction
- Regular Articles
- An accuracy study of the Intracavitary Electrocardiogram (IC-ECG) guided peripherally inserted central catheter tip placement among neonates
- Regular Articles
- Serum CA125, CA199 and CEA combined detection for epithelial ovarian cancer diagnosis: A meta-analysis
- Regular Articles
- Surface coil intensity correction in magnetic resonance imaging in spinal metastases
- Regular Articles
- Muscle stem cell and physical activity: what point is the debate at?
- Regular Articles
- MicroRNA let-7g directly targets forkhead box C2 (FOXC2) to modulate bone metastasis in breast cancer
- Regular Articles
- Monitoring health inequalities at the municipal level: Lithuanian experience
- Regular Articles
- Role of Epstein-Barr virus in the development of nasopharyngeal carcinoma
- Regular Articles
- Thrombectomy combined with indwelling-catheter thrombolysis is more effective than pure thrombectomy for the treatment of lower extremity deep venous thrombosis
- Regular Articles
- Expression of Hepcidin and Neogenin in colorectal cancer
- Regular Articles
- Carnitine and adiponectin levels in breast cancer after radiotherapy
- Regular Articles
- Pathophysiology of meningioma growth in pregnancy
- Regular Articles
- Causal neuro-immune relationships at patients with chronic pyelonephritis and cholecystitis. Correlations between parameters EEG, HRV and white blood cell count
- Regular Articles
- Measuring efficiency of secondary healthcare providers in Slovenia
- Regular Articles
- Galectin-3 expression in colorectal cancer and its correlation with clinical pathological characteristics and prognosis
- Regular Articles
- Model for studying anti- allergic drugs for allergic conjunctivitis in animals
- Regular Articles
- Barriers perceived by nurses in the optimal treatment of postoperative pain
- Regular Articles
- Tumor microenvironment in treatment of glioma
- Regular Articles
- Delirium risk of dexmedetomidine and midazolam in patients treated with postoperative mechanical ventilation: A meta-analysis
- Regular Articles
- Hemangioma of the rib: a rare case report and literature review
- Regular Articles
- The diagnostic accuracy of conventional forceps biopsy compared to ESD
- Regular Articles
- Increased miR-25 expression in serum of gastric cancer patients is correlated with CA19-9 and acts as a potential diagnostic biomarker
- Regular Articles
- Therapeutic nanomedicine surmounts the limitations of pharmacotherapy
- Regular Articles
- Relationship between PD-L1 expression and clinical characteristics in patients with breast invasive ductal carcinoma
- Regular Articles
- Trypsinogen activation peptide induces HMGB1 release from rat pancreatic acinar cells
- Regular Articles
- The effective regulation of pro- and anti-inflammatory cytokines induced by combination of PA-MSHA and BPIFB1 in initiation of innate immune responses
- Regular Articles
- Cell based therapeutic approach in vascular surgery: application and review
- Regular Articles
- Clinical efficacy of alprostadil combined with α-lipoic acid in the treatment of elderly patients with diabetic nephropathy
- Regular Articles
- Professional burnout and concurrent health complaints in neonatal nursing
- Regular Articles
- Esophageal xanthoma: presence of M2 macrophages suggests association with late inflammatory and reparative processes
- Regular Articles
- Cone beam computed tomography analysis in 3D position of maxillary denture
- Regular Articles
- CK20 mRNA expression in serum as a biomarker for colorectal cancer diagnosis: A meta-analysis
- Regular Articles
- Serum AFU, 5’-NT and AFP as biomarkers for primary hepatocellular carcinoma diagnosis
- Regular Articles
- Absolute reliability and concurrent validity of hand held dynamometry and isokinetic dynamometry in the hip, knee and ankle joint: systematic review and meta-analysis
- Regular Articles
- The Fountain of Youth: A tale of parabiosis, stem cells, and rejuvenation
- Regular Articles
- Foam sclerotherapy during shunt surgery for portal hypertension and varices
- Regular Articles
- Insomnia and depression: Japanese hospital workers questionnaire survey
- Regular Articles
- Serum NF-κBp65, TLR4 as biomarker for diagnosis of preeclampsia
- Regular Articles
- Docetaxel/cisplatin therapy in myasthenia gravis with hypertension/diabetes
- Regular Articles
- Fluid resuscitation and markers of glycocalyx degradation in severe sepsis
- Regular Articles
- Modified Sauve-Kapandji procedure for patients with old fractures of the distal radius
- Regular Articles
- Bile leakage after liver transplantation
- Regular Articles
- VEGF overexpression predicts poor survival in hepatocellular carcinoma
- Regular Articles
- Galen vein aneurysm– challenge for treatment
- Regular Articles
- Retrieval of a broken sewing needle from the sacrum aided by a permanent magnet: a case report and literature review
- Regular Articles
- HIV/STI prevention interventions: A systematic review and meta-analysis
- Regular Articles
- Aortic aneurysm as a complication of myeloperoxidase-antineutrophil cytoplasmic antibody-associated vasculitis
- Regular Articles
- Real-time monitoring of contrast-enhanced ultrasound for radio frequency ablation
- Regular Articles
- Successful drug-eluting stent implantation in a male patient with dextrocardia: a case report
- Regular Articles
- Primary pleomorphic liposarcoma of fallopian tube with recurrence: a case report and review of the literature
- Regular Articles
- Color Doppler Ultrasound in Uterine Arterial Embolization
- Regular Articles
- Pattern of alcohol consumption by young people from North Eastern Portugal
- Regular Articles
- Effects of out-of-hospital continuing nursing on schizophrenia patients' rehabilitation and quality of life

