Abstract
Objective
This preliminary study investigated the clinical safety and efficacy of foam sclerotherapy during shunt surgery to treat portal hypertension and gastroesophageal varices.
Methods
Seven patients with confirmed portal hypertension and a variceal bleeding history underwent mesocaval shunt with simultaneous polidocanol foam injection into the varices. Computed tomography and endoscopic reviews were conducted within two weeks following the procedures and around six months later.
Results
Six patients underwent side-to-side mesocaval shunt. One received a prosthetic mesocaval shunt. Polidocanol foam was injected into the gastric varices or the inferior mesenteric vein during the surgery. Surgical success and survival was achieved in all patients. Gastric ulcer formation and thrombocytopenia occurred in one patient respectively, which were ameliorated by conservative treatment. During 12 to 24 months’ follow-up, three patients had obvious decrease or eradication of gastroesophageal varices; four patients had obvious decrease of gastric varices but residual esophageal varices; and all patents had unobstructed shunts. Encephalopathy occurred in one patient two months postoperatively. No sclerosant-related complications were observed and no postoperative recurrent variceal bleeding occurred.
Conclusions
Foam sclerotherapy during shunt surgery is safe and effective for portal hypertension and varices treatment.
1 Introduction
Portal hypertension is a clinical syndrome that occurs when there is an increased resistance to blood flow in the portal venous system, causing the elevation in the pressure gradient between the portal vein and the inferior vena cava [1]. Portal hypertension can cause gastroesophageal varices and lead to variceal bleeding, which can be life threatening unless effectively controlled. Despite advancement in diagnostics and treatment, the mortality rate of patients with acute variceal hemorrhage can reach to 15-20% [2,3].
Currently, management of portal hypertension involves diverse treatments with drugs, endoscopic therapy, interventional therapy, surgery, and liver transplantation. Although minimal invasive treatments are developing rapidly, they have their limits. Endoscopic variceal ligation and endoscopic sclerotherapy are the first line treatments for acute gastroesophageal variceal bleeding or hemorrhage prophylaxis [4,5]. However, endoscopic therapy cannot reduce the high pressure of the portal venous system, and subsequent variceal re-bleeding may occur [6]. The transjugular intrahepatic portal–systemic shunt (TIPS) is an effective method to reduce portal venous pressure when endoscopy fails but this has a relatively high occlusion rate [7]. One other minimal invasive procedure is Balloon-occluded retrograde transvenous obliteration using foam sclerosant to control hemorrhage, however the method requires an autogenous gastrorenal shunt. Evidence indicates that the role of surgery including shunt surgeries and devascularization still cannot be replaced, especially in extra-hepatic portal hypertension [8,9].
To date, the management of portal hypertension and its complications requires a multidisciplinary approach. To take advantage of current treatments, we conducted this study to evaluate the safety and efficacy of our modified operation by combining shunt surgery with foam sclerotherapy.
2 Material and methods
2.1 Patients
Nine consecutive patients diagnosed with portal hypertension and gastroesophageal varices, between February 2015 to January 2016, were considered for shunt surgery combined with foam sclerotherapy.
Inclusion criteria were the following: 1. Portal hypertension and varices confirmed by sonography, contrast-enhanced computed tomography (CT), and endoscopy; 2. Previous failure of endoscopic treatment or other interventional treatment; or repeated variceal hemorrhage; 3. Child-Pugh class A or B liver function.
Exclusion criteria were: 1. Combined serious comorbidities; 2. Patient refused surgery. Two patients were excluded because one was complicated with renal carcinoma requiring simultaneous partial nephrectomy; the other refused operation. The other seven patients underwent shunt surgery combined with foam sclerotherapy and comprised the study group. Their medical records were retrospectively analyzed (Table 1).
Clinical characteristics of patients
| Patient No. | Age (y) | Sex | Diagnosis | Varices | Child-Pugh class | Previous variceal bleeding | Previous treatment |
|---|---|---|---|---|---|---|---|
| 1 | 58 | male | portal cavernoma | esophageal and gastric | A | yes | medication |
| 2 | 60 | male | portal cavernoma | esophageal and gastric | A | yes | endoscopic therapy |
| 3 | 61 | female | Budd-Chiari syndrome | esophageal and gastric | A | yes | medication |
| 4 | 40 | male | cirrhosis | esophageal and gastric | A | yes | interventional embolization |
| 5 | 44 | male | portal venous thrombosis | esophageal, gastric and rectal | A | yes | devascularization and endoscopic therapy |
| 6 | 34 | male | portal cavernoma | esophageal and gastric | A | yes | endoscopic therapy |
| 7 | 49 | female | portal venous thrombosis | esophageal and gastric | A | yes | medication |
Informed consent was also obtained from all patients before surgery. This study was approved by our institutional review board.
2.2 Procedures
All patients underwent a midline abdominal incision while under general anesthesia. After exploring the abdominal cavity and organs, the portal pressure was measured through the epiploic vein. A mesocaval shunt was then established by a side-to-side anastomosis, restricted to 1-cm – 1.5-cm in length, between the superior mesenteric vein and the inferior vena cava. In one case, an 8-mm in diameter prosthetic (W. L. Gore & Associates, Inc.) shunt was chosen because of the high-tension anastomosis between the two vessels. This was followed by exposing the gastric varices and foam sclerosant made up of 2-mL of 1% or 3% polidocanol (Aethoxysklerol, Kreussler, Germany) mixed with 8-mL of air by using the Tessari method was injected into the varices with a 10-mL syringe [10] (Figure 1a, 1b). Soon after the injection, the puncture site vessel was ligated. Normally, 2-mL or 4-mL of 1% polidocanol are administrated to each varicose vein. However, if the varices exceed 6-mm in diameter, 3% polidocanol is applied. In one case, Sclerosant injection was assisted by introducing a catheter through the inferior mesenteric vein to the distal varices (Figure 2a, 2b). Finally, the portal pressure was measured again before closing the incision.

Varicose veins before and after foam injection. a) Varicose veins at lesser gastric curvature (arrow). b) Occlusion of varicose veins after injection of Polidocanol foam.
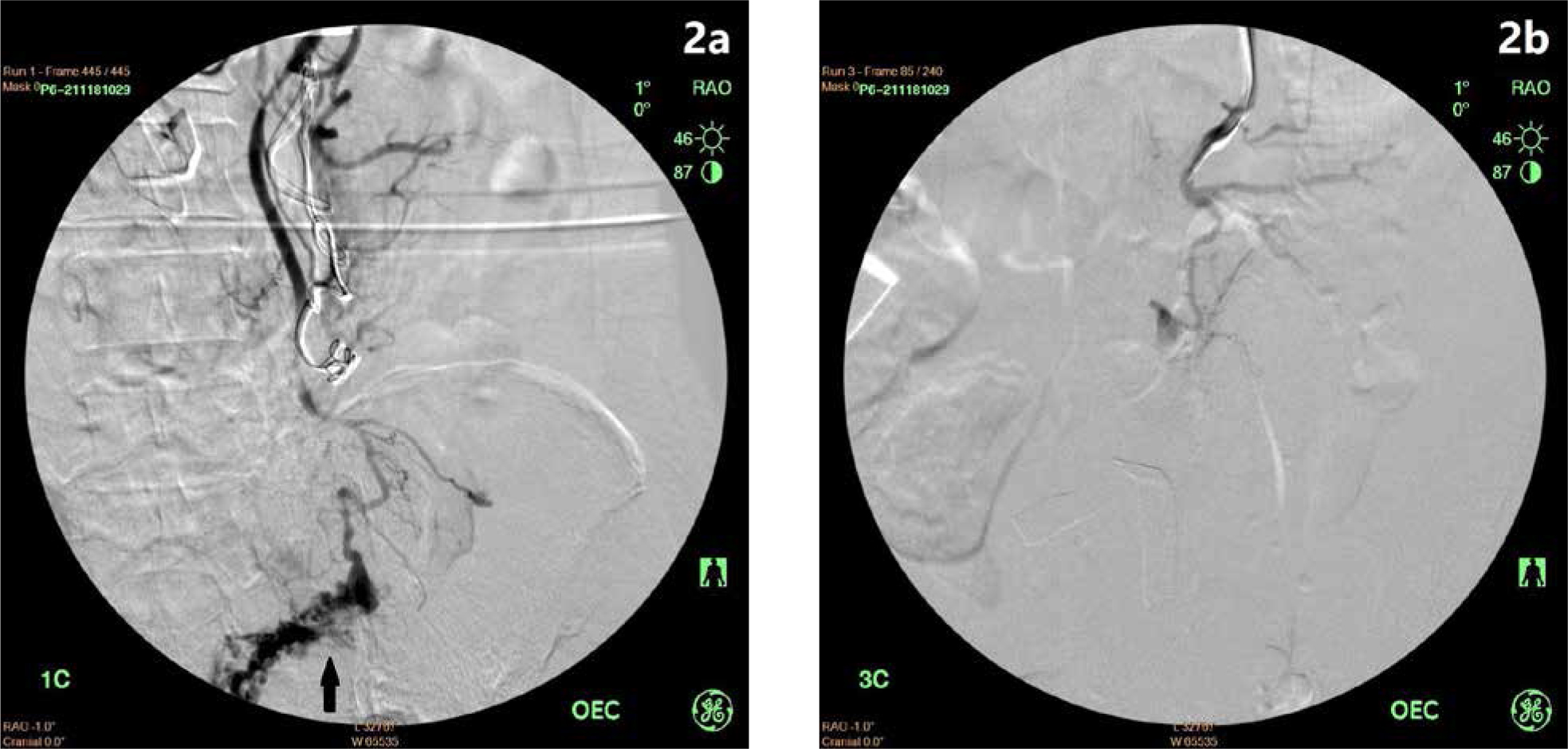
Rectal varices before and after foam injection. a) Rectal varices (arrow) at intra-operative angiography via inferior mesenteric vein. b) Occlusion of rectal varicose veins after injection of Polidocanol foam..
2.3 Investigation and follow up
We reviewed the medical records of the 7 patients retrospectively. All patients underwent enhanced CT with or without endoscopic review within two weeks postoperatively and around six months after surgery. Laboratory tests, including liver function, routine blood tests, and blood ammonia levels were all obtained during hospital admission and outpatient reviews. Surgical success was defined as completion of the shunt surgery combined with foam sclerotherapy, without operation related deaths.
Meanwhile, treatment success was defined as an obvious decrease of the varices and an unobstructed shunt on CT or endoscopic reexamination and no variceal re-bleeding during the follow-up period. The free of variceal bleeding time and survival time were measured from surgery until the date the incident occurred or the last outpatient review or telephone contact.
3 Results
All patients underwent shunt surgery combined with foam sclerotherapy with a side-to-side anastomosis mesocaval shunt, except for one patient who received a prosthetic mesocaval shunt. Additionally, 1% polidocanol foam was injected into the gastric varices in seven patients; one of them was simultaneously injected with 3% polidocanol foam via a catheter inserted into the inferior mesenteric vein to seal the rectal varicose vein. The dosage of polidocanol injection ranged from 8-mL to 20-mL (average 12.1-mL). Surgical success was achieved in all patients, with no operative death.
Gastric bleeding occurred in one patient three days after surgery because of fundal ulcer formation, which was confirmed by endoscopic examination and was relieved by acid suppression and blood transfusion. Thrombocytopenia was observed in one patient postoperatively, leading to uncontrolled nasal bleeding. This was managed by plasma transfusion and local hemostasis therapy. No sclerotherapy-related complications were found postoperatively.
The follow-up time ranged from 12 to 24 months (average 15.7 months). During follow up, obvious reduction or eradication of the gastroesophageal varices was observed in three patients; obviously decreased gastric varices but residual esophageal varices was also observed in four patients (Figure 3a, 3b). The patient with rectal varices was found to have obviously decreased varices by colonoscopy; moreover, all shunts were patent until the last CT review. Therefore, treatment success was also achieved in all patients.

Preoperative and reviewed enhanced CT or endoscopy images. a) Gastroesophageal varices at preoperative enhanced CT or endoscopy in 7 patients (arrows). b) Enhanced CT or endoscopy review of the 7 patients showing obviously decreased or eradicated gastric varices in all patients but residual esophageal varices in patient 3,4,5 and 7 after procedure (arrows).
Lastly, encephalopathy presenting with lethargy was found to have occurred in one patient two months postoperatively and was relieved by ammonia-lowering and lactulose treatment without recurrence. No variceal re-bleeding occurred after surgery, and all patients were alive at the last follow-up time (Table 2).
Postoperative results
| Post-surgery varices | Complications | Free of bleeding time (months) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Patient No. | Shunt type | Sclerosant injection site | Foam volume (mL) | Review | |||||
| CT | Endoscopy | Gastric | Esophageal | ||||||
| 1 | mesocaval | gastric vein | 15 | yes | refuse | decrease | decrease | no | 24 |
| 2 | mesocaval prosthetic graft | gastric vein | 10 | yes | yes | eradication | eradication | no | 17 |
| 3 | mesocaval | gastric vein | 8 | yes | refuse | decrease | persistence | no | 16 |
| 4 | mesocaval | gastric vein | 10 | yes | yes | eradication | persistence | no | 14 |
| 5 | mesocaval | gastric vein and inferior mesenteric vein | 20 | yes | yes | decrease of gastric and rectal varices | persistence | encephalopathy | 14 |
| 6 | mesocaval | gastric vein | 12 | yes | yes | decrease | decrease | gastric ulcer | 13 |
| 7 | mesocaval | gastric vein | 10 | yes | yes | eradication | persistence | thrombocytopenia | 12 |
4 Discussion
It is recognized that endoscopic therapy, including endoscopic variceal ligation and endoscopic sclerotherapy, is the first management choice for variceal hemorrhage caused by portal hypertension. However, recurrence of variceal bleeding is common and occurs in up to 70% of patients following medical and endoscopic treatment [11]. In addition, endoscopic treatment is not as effective for gastric varices as it is for esophageal varices [12], and the risk of re-bleeding is significantly higher [13]. When endoscopic therapy is difficult or fails, TIPS or other interventional treatment, surgery, or liver transplantation can be effective methods to prevent gastric varices re-bleeding. Although TIPS can reduce the re-bleeding rate and is minimally invasive [14], the high occlusion rate is still a concern.
In a prospective randomized trial of 140 patients with Child-Pugh class A or B liver function the results revealed that distal splenorenal shunt and TIPS had similar rates of re-bleeding, encephalopathy, and survival. However, the rate of thrombosis, stenosis, and reintervention were much higher for TIPS (82%) than distal splenorenal shunt (11%) [7]. Liver transplantation seemed to be an ideal treatment for cirrhotic portal hypertension but this is limited by the short supply of donor livers.
Nowadays, both shunt and non-shunt surgeries are still used to prevent recurrent variceal bleeding. Shunt surgery is an effective method for decompression and hemorrhage prevention, although encephalopathy is a concern. Non-shunt surgery, including several types of devascularization, has a certain effect on hemostasis but a relatively high rate of variceal recurrence and re-bleeding due to unresolved high pressure in the portal venous system [15, 16, 17]. Considering their advantages and disadvantages, many surgeons have performed complex combined shunt and devascularization surgeries.
Feng et al [18]. performed a mesocaval C graft shunt, ligation of the gastric and coronary vein, and partial splenectomy in 140 patients. Their results were encouraging, as 100 patients were followed up for one month to six years, with no recurrent hemorrhage or encephalopathy. At our hospital, we have performed combined surgery for the past five years. Owing to most of our patients being diagnosed with portal venous thrombosis or cavernoma, we usually perform a mesocaval shunt procedure. To avoid excessive shunt flow causing encephalopathy, the shunt anastomosis was restricted of 1 to 1.5-cm in length, or an 8-mm graft was used to maintain sufficient hepatic blood flow. Since its decompressing effect was less than that of total shunt, combined gastric varices devascularization was a complementary method to ensure prevention of variceal re-bleeding.
However, an effective devascularization procedure is sometimes needed to extend the surgical field to expose the gastric fundus and esophagus, which may lead to increased trauma. To simplify the procedure, we attempted to substitute foam sclerotherapy for devascularization because of the following reasons: foam sclerosant not only occludes the main gastric vessel but also occludes the collaterals, even extending to the esophageal vessels; some distal vessels such as rectal varices that are difficult to expose can be managed by catheter-guided sclerotherapy; the technique is easy to master; and Polidocanol foam is proved to be an effective and safe sclerosant used in the varicose veins of the lower extremities [19,20]. Compared with liquid sclerosants, polidocanol foam can reduce the amount of sclerosant needed and maximize the intimal irritation, causing vessel occlusion by increasing the contact surface area with the wall of the varices.
In terms of safety and efficacy, there were few complications reported after foam sclerotherapy with the recommended dose (2-mg/kg/day) by the manufacturer [21,22], even with greater doses than what is recommended [23]. Several studies have shown polidocanol to be as effective as other sclerosants for the treatment of both esophageal and gastric varices [24,25]. There are reports of polidocanol foam used for balloon-occluded retrograde transvenous obliteration of varices via a gastrorenal shunt. The gastric variceal obliteration rate was from 91% to 100%, and re-bleeding occurred in one case during follow up. No severe sclerotherapy-related complications were observed [26, 27, 28].
In our study, gastroesophageal varices were obviously decreased or eradicated in three patients postoperatively.
Although the other four cases had a decrease only in the gastric varices, it solved the problem, which often is the cause of re-bleeding after treatment. Following surgery, gastric bleeding occurred in one patient. However, endoscopy confirmed that this was not variceal bleeding but rather ulcer formation following endoscopic glue obturation, which had been reported as a severe complication related to glue embolization [29,30]. Despite this, no sclerosant-related complications were observed, and no recurrent variceal hemorrhage occurred during follow up, demonstrating that there is effectiveness and safety of shunt surgery combined with foam sclerotherapy.
This preliminary study was limited by its small sample size and the short-term outcomes. Due the domination of endoscopic therapy and interventional treatment, the demand for surgery has reduced considerably. However, based on the large number of patients in China, there are still enough patients suited for surgical treatment, which implies that large samples of patients may require such method in the future. Furthermore, a long-term investigation to monitor re-bleeding, encephalopathy, and survival rate should be continue.
5 Conclusion
Polidocanol foam injection of the varices is simpler in operating than conventional devascularization and provides confirmed variceal obliteration. The outcomes of foam sclerotherapy during shunt surgery indicates short-term efficacy and safety for preventing variceal re-bleeding, with a low complication rate. Further investigation of long-term results in a large sample should be undertaken.
Acknowledgments
None.
Conflict of interest
Conflict of interest statement: Authors state no conflict of interest.
References
[1] Robertson M., Hayes P., Management of portal hypertension, Budd–Chiari syndrome and portal vein thrombosis, Medicine, 2015, 43(11), 669-673, 10.1016/j.mpmed.2015.08.016Search in Google Scholar
[2] de Franchis R., Primignani M., Natural history of portal hypertension in patients with cirrhosis, Clin Liver Dis, 2001, 5(3), 645-663, 10.1016/S1089-3261(05)70186-0Search in Google Scholar
[3] Chalasani N., Kahi C., Francois F., Pinto A., Marathe A., Bini EJ., et al., Improved patient survival after acute variceal bleeding: a multicentre, cohort study, Am J Gastroenterol, 2003, 98(3), 653-659, 10.1016/S0002-9270(02)06016-1Search in Google Scholar
[4] Wright A.S., Rikkers L.F., Current management of portal hypertension, J Gastrointest Surg, 2005, 9(7), 992-1005, 10.1016/j.gassur.2004.09.028Search in Google Scholar PubMed
[5] Khanna R., Sarin S.K., Non-cirrhotic portal hypertension-diagnosis and management, J Hepatol, 2014, 60(2), 421-441, 10.1016/j.jhep.2013.08.013Search in Google Scholar PubMed
[6] Sarin S.K., Kumar A., Chawla Y.K., Baijal S.S., Dhiman R.K., Jafri W., et al., Noncirrhotic portal fibrosis/idiopathic portal hypertension: APASL recommendations for diagnosis and treatment, Hepatol Int, 2007, 1(3), 398-413, 10.1007/s12072-007-9010-9Search in Google Scholar PubMed PubMed Central
[7] Henderson J.M., Boyer T.D., Kutner M.H., Galloway J.R., Rikkers L.F., Jeffers L.J., et al., DIVERT Study Group. Distal splenorenal shunt versus transjugular intrahepatic portal-systematic shunt for variceal bleeding: a randomized trial, Gastroenterology, 2006, 130(6), 1643-1651, 10.1053/j.gastro.2006.02.008Search in Google Scholar PubMed
[8] Mercado M.A., Surgical treatment for portal hypertension, Br J Surg, 2015, 102(7), 717-718, 10.1002/bjs.9849Search in Google Scholar PubMed
[9] Pal S., Current role of surgery in portal hypertension, Indian J Surg, 2012, 74, 55–66, 10.1007/s12262-011-0381-8Search in Google Scholar PubMed PubMed Central
[10] Tessari L., Cavezzi A., Frullini A., Preliminary experience with a new sclerosing foam in the treatment of varicose veins, Dermatol Surg, 2001, 27(1), 58-60, 10.1111/j.1524-4725.2001.00192.xSearch in Google Scholar
[11] Burroughs A.K., The natural history of varices, J Hepatol, 1993, 17(Suppl 3), 510-513, 10.1016/S0168-8278(05)80448-9Search in Google Scholar
[12] Kapoor A., Dharel N., Sanyal A.J., Endoscopic Diagnosis and Therapy in Gastroesophageal Variceal Bleeding, Gastrointest Endosc Clin N Am, 2015, 25(3), 491-507, 10.1016/j.giec.2015.03.004Search in Google Scholar
[13] Weilert F., Binmoeller K.F., Endoscopic management of gastric variceal bleeding, Gastroenterol Clin North Am, 2014, 43(4), 807-818, 10.1016/j.gtc.2014.08.010Search in Google Scholar
[14] Papatheodoridis G.V., Goulis J., Leandro G., Patch D., Burroughs A.K., Transjugular intrahepatic portosystemic shunt compared with endoscopic treatment for prevention of variceal rebleeding: A meta-analysis, Hepatology, 1999, 30(3), 612-622, 10.1016/j.gtc.2014.08.010Search in Google Scholar
[15] Keagy B.A., Schwartz J.A., Johnson G., Should ablative operations be used for bleeding esophageal varices?, Ann Surg, 1986, 203(5), 463-469, 10.1097/00000658-198605000-00003Search in Google Scholar
[16] Burroughs A.K., Hamilton G., Phillips A., Mezzanotte G., McIntyre N., Hobbs K.E., A comparison of sclerotherapy with staple transection of the esophagus for the emergency control of bleeding from esophageal varices, N Engl J Med, 1989, 321(13), 857-862, 10.1056/NEJM198909283211303Search in Google Scholar
[17] Jin G., Rikkers L.F., Transabdominal esophagogastric devascularization as treatment for variceal hemorrhage, Surgery, 1996, 120(4), 641-647, 10.1016/S0039-6060(96)80011-0Search in Google Scholar
[18] Feng L.S., Li K., Peng Q.P., Ma X.X., Zhao Y.F., Xu P.Q., et al., Triplex operation for portal hypertension with esophageal variceal bleeding: report of 140 cases, Hepatobiliary Pancreat Dis Int, 2004, 3(4), 534-537Search in Google Scholar
[19] Guex J.J., Foam sclerotherapy: an overview of use for primary venous insufficiency, Semin Vasc Surg, 2005, 18(1), 25-29, 10.1053/j.semvascsurg.2004.12.008Search in Google Scholar
[20] Alòs J., Carreño P., López J.A., Estadella B., Serra-Prat M., Marinel-Lo J., Efficacy and safety of sclerotherapy using polidocanol foam: a controlled clinical trial, Eur J Vasc Endovasc Surg, 2006, 31(1), 101-107, 10.1016/j.ejvs.2005.08.018Search in Google Scholar
[21] Conrad P., Malouf G., Stacey M., The Australian polidocanol (Aethoxysklerol) study, Dermatol Surg, 2008, 21(4), 334–336, 10.1016/1076-0512(94)00282-USearch in Google Scholar
[22] Goldman M.P., Treatment of varicose and telangiectatic leg veins: double-blind prospective comparative trial between aethoxyskerol and sotradecol, Dermatol Surg, 2002, 28(1), 52-55, 10.1046/j.1524-4725.2002.01190.xSearch in Google Scholar
[23] Mimura H., Fujiwara H., Hiraki T., Gobara H., Mukai T., Hyodo T., et al., Polidocanol sclerotherapy for painful venous malformations: evaluation of safety and efficacy in pain relief, Eur Radiol, 2009, 19(10), 2474-2480, 10.1007/s00330-009-1442-1442Search in Google Scholar
[24] Bhargava D., Singh B., Dogra R., Dasarathy S., Sharma M.P., Prospective randomized comparison of sodium tetradecyl sulfate and polidocanol as variceal sclerosing agents, Am J Gastroenterol, 1992, 87(2), 182-186Search in Google Scholar
[25] Ravi M., Kate V., Ananthakrishnan N., Prospective randomized comparison of sodium tetradecyl sulphate & polidocanol for oesophageal variceal sclerotherapy, Indian J Med Res, 2001, 113, 228-233Search in Google Scholar
[26] Clements W., Cavanagh K., Ali F., Kavnoudias H., Kemp W., Roberts S., et al., Variant treatment for gastric varices with polidocanol foam using balloon-occluded retrograde transvenous obliteration: a pilot study, J Med Imaging Radiat Oncol, 2012, 56(6), 599-605, 10.1111/j.1754-9485.2012.02453.xSearch in Google Scholar
[27] Koizumi J., Hashimoto T., Myojin K., Itou C., Kagawa T., Nishibe T., et al., Balloon-occluded retrograde transvenous obliteration of gastric varices: use of CT-guided foam sclerotherapy to optimize technique, AJR Am J Roentgenol, 2012, 199(1), 200-207, 10.2214/AJR.11.7002Search in Google Scholar
[28] Choi S.Y., Won J.Y., Kim K.A., Lee D.Y., Lee K.H., Foam sclerotherapy using polidocanol for balloon-occluded retrograde transvenous obliteration (BRTO), Eur Radiol, 2011, 21(1), 122-129, 10.1007/s00330-010-1895-3Search in Google Scholar
[29] El Amin H., Abdel Baky L., Sayed Z., Abdel Mohsen E., Eid K., Fouad Y., et al., A randomized trial of endoscopic variceal ligation versus Cyanoacrylate injection for treatment of bleeding junctional varices, Trop Gastroenterol, 2010, 31(4), 279-284, 10.1016/S0168-8278(10)60843-4Search in Google Scholar
[30] Cheng L.F., Wang Z.Q., Li C.Z., Lin W., Yeo A.E., Jin B., Low incidence of complications from endoscopic gastric variceal obturation with butyl cyanoacrylate, Clin Gastroenterol Hepatol, 2010, 8(9), 760-766, 10.1016/j.cgh.2010.05.019Search in Google Scholar PubMed
© 2017 Zhe Zhang et al.
This work is licensed under the Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 License.
Articles in the same Issue
- Regular Articles
- Intravascular treatment of left subclavian artery aneurysm coexisting with aortic coarctation in an adult patient
- Regular Articles
- Effect of electrical stimulation on blood flow velocity and vessel size
- Regular Articles
- Live birth pregnancy outcome after first in vitro fertilization treatment in a patient with Systemic Lupus Erythematosus and isolated high positive IgA anti-β2glycoprotein I antibodies: a case report
- Regular Articles
- Periodontal ligament stem cells regulate apoptosis of neutrophils
- Regular Articles
- Platelet-rich fibrin (PRF) in implants dentistry in combination with new bone regenerative flapless technique: evolution of the technique and final results
- Regular Articles
- The significance of strong ion gap for predicting return of spontaneous circulation in patients with cardiopulmonary arrest
- Regular Articles
- Clinicopathology of EpCAM and EGFR in human epithelial ovarian carcinoma
- Regular Articles
- Intraosseous lipoma of the mandibula: A case report and review of the literature
- Regular Articles
- Transurethral resection of the prostate, bladder explosion and hyponatremic encephalopathy: a rare case report of malpractice
- Regular Articles
- Brain strokes related to aortic aneurysma – the analysis of three cases
- Regular Articles
- Effect of Bicyclol tablets on drug induced liver injuries after kidney transplantation
- Regular Articles
- Plasma free fatty acids in hyperemesis gravidarum pregnancy
- Regular Articles
- Impact of chromosomal rearrangement upon DNA methylation patterns in leukemia
- Regular Articles
- Gefitinib versus docetaxel in treated non-small-cell lung cancer: a meta-analysis
- Regular Articles
- The clinical characteristics of patients with chronic idiopathic anal pain
- Regular Articles
- Bone tunnel impaction reduced the tibial tunnel enlargement
- Regular Articles
- Effects of S-1 combined with radiotherapy in the treatment of nasopharyngeal cancer: a meta-analysis based on randomized controlled trials
- Regular Articles
- Predictions and outcomes of atrial fibrillation in the patients with acute myocardial infarction
- Regular Articles
- An accuracy study of the Intracavitary Electrocardiogram (IC-ECG) guided peripherally inserted central catheter tip placement among neonates
- Regular Articles
- Serum CA125, CA199 and CEA combined detection for epithelial ovarian cancer diagnosis: A meta-analysis
- Regular Articles
- Surface coil intensity correction in magnetic resonance imaging in spinal metastases
- Regular Articles
- Muscle stem cell and physical activity: what point is the debate at?
- Regular Articles
- MicroRNA let-7g directly targets forkhead box C2 (FOXC2) to modulate bone metastasis in breast cancer
- Regular Articles
- Monitoring health inequalities at the municipal level: Lithuanian experience
- Regular Articles
- Role of Epstein-Barr virus in the development of nasopharyngeal carcinoma
- Regular Articles
- Thrombectomy combined with indwelling-catheter thrombolysis is more effective than pure thrombectomy for the treatment of lower extremity deep venous thrombosis
- Regular Articles
- Expression of Hepcidin and Neogenin in colorectal cancer
- Regular Articles
- Carnitine and adiponectin levels in breast cancer after radiotherapy
- Regular Articles
- Pathophysiology of meningioma growth in pregnancy
- Regular Articles
- Causal neuro-immune relationships at patients with chronic pyelonephritis and cholecystitis. Correlations between parameters EEG, HRV and white blood cell count
- Regular Articles
- Measuring efficiency of secondary healthcare providers in Slovenia
- Regular Articles
- Galectin-3 expression in colorectal cancer and its correlation with clinical pathological characteristics and prognosis
- Regular Articles
- Model for studying anti- allergic drugs for allergic conjunctivitis in animals
- Regular Articles
- Barriers perceived by nurses in the optimal treatment of postoperative pain
- Regular Articles
- Tumor microenvironment in treatment of glioma
- Regular Articles
- Delirium risk of dexmedetomidine and midazolam in patients treated with postoperative mechanical ventilation: A meta-analysis
- Regular Articles
- Hemangioma of the rib: a rare case report and literature review
- Regular Articles
- The diagnostic accuracy of conventional forceps biopsy compared to ESD
- Regular Articles
- Increased miR-25 expression in serum of gastric cancer patients is correlated with CA19-9 and acts as a potential diagnostic biomarker
- Regular Articles
- Therapeutic nanomedicine surmounts the limitations of pharmacotherapy
- Regular Articles
- Relationship between PD-L1 expression and clinical characteristics in patients with breast invasive ductal carcinoma
- Regular Articles
- Trypsinogen activation peptide induces HMGB1 release from rat pancreatic acinar cells
- Regular Articles
- The effective regulation of pro- and anti-inflammatory cytokines induced by combination of PA-MSHA and BPIFB1 in initiation of innate immune responses
- Regular Articles
- Cell based therapeutic approach in vascular surgery: application and review
- Regular Articles
- Clinical efficacy of alprostadil combined with α-lipoic acid in the treatment of elderly patients with diabetic nephropathy
- Regular Articles
- Professional burnout and concurrent health complaints in neonatal nursing
- Regular Articles
- Esophageal xanthoma: presence of M2 macrophages suggests association with late inflammatory and reparative processes
- Regular Articles
- Cone beam computed tomography analysis in 3D position of maxillary denture
- Regular Articles
- CK20 mRNA expression in serum as a biomarker for colorectal cancer diagnosis: A meta-analysis
- Regular Articles
- Serum AFU, 5’-NT and AFP as biomarkers for primary hepatocellular carcinoma diagnosis
- Regular Articles
- Absolute reliability and concurrent validity of hand held dynamometry and isokinetic dynamometry in the hip, knee and ankle joint: systematic review and meta-analysis
- Regular Articles
- The Fountain of Youth: A tale of parabiosis, stem cells, and rejuvenation
- Regular Articles
- Foam sclerotherapy during shunt surgery for portal hypertension and varices
- Regular Articles
- Insomnia and depression: Japanese hospital workers questionnaire survey
- Regular Articles
- Serum NF-κBp65, TLR4 as biomarker for diagnosis of preeclampsia
- Regular Articles
- Docetaxel/cisplatin therapy in myasthenia gravis with hypertension/diabetes
- Regular Articles
- Fluid resuscitation and markers of glycocalyx degradation in severe sepsis
- Regular Articles
- Modified Sauve-Kapandji procedure for patients with old fractures of the distal radius
- Regular Articles
- Bile leakage after liver transplantation
- Regular Articles
- VEGF overexpression predicts poor survival in hepatocellular carcinoma
- Regular Articles
- Galen vein aneurysm– challenge for treatment
- Regular Articles
- Retrieval of a broken sewing needle from the sacrum aided by a permanent magnet: a case report and literature review
- Regular Articles
- HIV/STI prevention interventions: A systematic review and meta-analysis
- Regular Articles
- Aortic aneurysm as a complication of myeloperoxidase-antineutrophil cytoplasmic antibody-associated vasculitis
- Regular Articles
- Real-time monitoring of contrast-enhanced ultrasound for radio frequency ablation
- Regular Articles
- Successful drug-eluting stent implantation in a male patient with dextrocardia: a case report
- Regular Articles
- Primary pleomorphic liposarcoma of fallopian tube with recurrence: a case report and review of the literature
- Regular Articles
- Color Doppler Ultrasound in Uterine Arterial Embolization
- Regular Articles
- Pattern of alcohol consumption by young people from North Eastern Portugal
- Regular Articles
- Effects of out-of-hospital continuing nursing on schizophrenia patients' rehabilitation and quality of life
Articles in the same Issue
- Regular Articles
- Intravascular treatment of left subclavian artery aneurysm coexisting with aortic coarctation in an adult patient
- Regular Articles
- Effect of electrical stimulation on blood flow velocity and vessel size
- Regular Articles
- Live birth pregnancy outcome after first in vitro fertilization treatment in a patient with Systemic Lupus Erythematosus and isolated high positive IgA anti-β2glycoprotein I antibodies: a case report
- Regular Articles
- Periodontal ligament stem cells regulate apoptosis of neutrophils
- Regular Articles
- Platelet-rich fibrin (PRF) in implants dentistry in combination with new bone regenerative flapless technique: evolution of the technique and final results
- Regular Articles
- The significance of strong ion gap for predicting return of spontaneous circulation in patients with cardiopulmonary arrest
- Regular Articles
- Clinicopathology of EpCAM and EGFR in human epithelial ovarian carcinoma
- Regular Articles
- Intraosseous lipoma of the mandibula: A case report and review of the literature
- Regular Articles
- Transurethral resection of the prostate, bladder explosion and hyponatremic encephalopathy: a rare case report of malpractice
- Regular Articles
- Brain strokes related to aortic aneurysma – the analysis of three cases
- Regular Articles
- Effect of Bicyclol tablets on drug induced liver injuries after kidney transplantation
- Regular Articles
- Plasma free fatty acids in hyperemesis gravidarum pregnancy
- Regular Articles
- Impact of chromosomal rearrangement upon DNA methylation patterns in leukemia
- Regular Articles
- Gefitinib versus docetaxel in treated non-small-cell lung cancer: a meta-analysis
- Regular Articles
- The clinical characteristics of patients with chronic idiopathic anal pain
- Regular Articles
- Bone tunnel impaction reduced the tibial tunnel enlargement
- Regular Articles
- Effects of S-1 combined with radiotherapy in the treatment of nasopharyngeal cancer: a meta-analysis based on randomized controlled trials
- Regular Articles
- Predictions and outcomes of atrial fibrillation in the patients with acute myocardial infarction
- Regular Articles
- An accuracy study of the Intracavitary Electrocardiogram (IC-ECG) guided peripherally inserted central catheter tip placement among neonates
- Regular Articles
- Serum CA125, CA199 and CEA combined detection for epithelial ovarian cancer diagnosis: A meta-analysis
- Regular Articles
- Surface coil intensity correction in magnetic resonance imaging in spinal metastases
- Regular Articles
- Muscle stem cell and physical activity: what point is the debate at?
- Regular Articles
- MicroRNA let-7g directly targets forkhead box C2 (FOXC2) to modulate bone metastasis in breast cancer
- Regular Articles
- Monitoring health inequalities at the municipal level: Lithuanian experience
- Regular Articles
- Role of Epstein-Barr virus in the development of nasopharyngeal carcinoma
- Regular Articles
- Thrombectomy combined with indwelling-catheter thrombolysis is more effective than pure thrombectomy for the treatment of lower extremity deep venous thrombosis
- Regular Articles
- Expression of Hepcidin and Neogenin in colorectal cancer
- Regular Articles
- Carnitine and adiponectin levels in breast cancer after radiotherapy
- Regular Articles
- Pathophysiology of meningioma growth in pregnancy
- Regular Articles
- Causal neuro-immune relationships at patients with chronic pyelonephritis and cholecystitis. Correlations between parameters EEG, HRV and white blood cell count
- Regular Articles
- Measuring efficiency of secondary healthcare providers in Slovenia
- Regular Articles
- Galectin-3 expression in colorectal cancer and its correlation with clinical pathological characteristics and prognosis
- Regular Articles
- Model for studying anti- allergic drugs for allergic conjunctivitis in animals
- Regular Articles
- Barriers perceived by nurses in the optimal treatment of postoperative pain
- Regular Articles
- Tumor microenvironment in treatment of glioma
- Regular Articles
- Delirium risk of dexmedetomidine and midazolam in patients treated with postoperative mechanical ventilation: A meta-analysis
- Regular Articles
- Hemangioma of the rib: a rare case report and literature review
- Regular Articles
- The diagnostic accuracy of conventional forceps biopsy compared to ESD
- Regular Articles
- Increased miR-25 expression in serum of gastric cancer patients is correlated with CA19-9 and acts as a potential diagnostic biomarker
- Regular Articles
- Therapeutic nanomedicine surmounts the limitations of pharmacotherapy
- Regular Articles
- Relationship between PD-L1 expression and clinical characteristics in patients with breast invasive ductal carcinoma
- Regular Articles
- Trypsinogen activation peptide induces HMGB1 release from rat pancreatic acinar cells
- Regular Articles
- The effective regulation of pro- and anti-inflammatory cytokines induced by combination of PA-MSHA and BPIFB1 in initiation of innate immune responses
- Regular Articles
- Cell based therapeutic approach in vascular surgery: application and review
- Regular Articles
- Clinical efficacy of alprostadil combined with α-lipoic acid in the treatment of elderly patients with diabetic nephropathy
- Regular Articles
- Professional burnout and concurrent health complaints in neonatal nursing
- Regular Articles
- Esophageal xanthoma: presence of M2 macrophages suggests association with late inflammatory and reparative processes
- Regular Articles
- Cone beam computed tomography analysis in 3D position of maxillary denture
- Regular Articles
- CK20 mRNA expression in serum as a biomarker for colorectal cancer diagnosis: A meta-analysis
- Regular Articles
- Serum AFU, 5’-NT and AFP as biomarkers for primary hepatocellular carcinoma diagnosis
- Regular Articles
- Absolute reliability and concurrent validity of hand held dynamometry and isokinetic dynamometry in the hip, knee and ankle joint: systematic review and meta-analysis
- Regular Articles
- The Fountain of Youth: A tale of parabiosis, stem cells, and rejuvenation
- Regular Articles
- Foam sclerotherapy during shunt surgery for portal hypertension and varices
- Regular Articles
- Insomnia and depression: Japanese hospital workers questionnaire survey
- Regular Articles
- Serum NF-κBp65, TLR4 as biomarker for diagnosis of preeclampsia
- Regular Articles
- Docetaxel/cisplatin therapy in myasthenia gravis with hypertension/diabetes
- Regular Articles
- Fluid resuscitation and markers of glycocalyx degradation in severe sepsis
- Regular Articles
- Modified Sauve-Kapandji procedure for patients with old fractures of the distal radius
- Regular Articles
- Bile leakage after liver transplantation
- Regular Articles
- VEGF overexpression predicts poor survival in hepatocellular carcinoma
- Regular Articles
- Galen vein aneurysm– challenge for treatment
- Regular Articles
- Retrieval of a broken sewing needle from the sacrum aided by a permanent magnet: a case report and literature review
- Regular Articles
- HIV/STI prevention interventions: A systematic review and meta-analysis
- Regular Articles
- Aortic aneurysm as a complication of myeloperoxidase-antineutrophil cytoplasmic antibody-associated vasculitis
- Regular Articles
- Real-time monitoring of contrast-enhanced ultrasound for radio frequency ablation
- Regular Articles
- Successful drug-eluting stent implantation in a male patient with dextrocardia: a case report
- Regular Articles
- Primary pleomorphic liposarcoma of fallopian tube with recurrence: a case report and review of the literature
- Regular Articles
- Color Doppler Ultrasound in Uterine Arterial Embolization
- Regular Articles
- Pattern of alcohol consumption by young people from North Eastern Portugal
- Regular Articles
- Effects of out-of-hospital continuing nursing on schizophrenia patients' rehabilitation and quality of life

