Abstract
Garengeot’s hernia (GH) is defined as the presence of the appendix inside a femoral hernia. It occurs in 0.9% of femoral hernias and is usually an incidental finding during surgery. Its treatment is controversial and the aim of this article is to review the diagnostic methods and surgical considerations.
We report two cases diagnosed preoperatively by contrast-enhanced computed tomography (CT) and discuss the treatment options based on a review of the literature published in PubMed updated on 1 December, 2015.
Fifty articles reporting 64 patients (50 women, mean age 70 years) with GH were included in the analysis. Diagnosis was performed by preoperative CT in only 24 cases, including our two. The treatment of GH is emergency surgery. Several options are available laparoscopic or open approach: insertion of a mesh or simple herniorrhaphy, with or without appendectomy.
Conslusion
The preoperative diagnosis with CT can guide the choice of treatment. Appendectomy and hernioplasty should be performed via inguinotomy, if there is no perforation or abscess formation.
1 Introduction
Garengeot’s hernia (GH) is defined as the presence of the appendix in a femoral hernia [1]. Less common is the finding of an acute appendicitis inside the femoral hernia sac. Although some cases have been diagnosed preoperatively, it is usually found incidentally during repair. We report two cases with preoperative diagnostic contrast-enhanced computed tomography (CT) and discuss the surgical considerations through a literature review.
2 Case Report 1
An 86-year-old female came to the emergency department with a 5-day history of a right-sided groin mass which had appeared after an episode of vomiting. The patient reported no change in bowel habits and no further episodes of vomiting. Her medical history included arthrosis treated with anti-inflammatory medication. On physical examination, her vital signs were stable and she was afebrile. The abdomen was soft and non-tender, with a painful right groin mass on palpation (approximately 5x3cm). There was no erythema or crepitus, nor any rebound or rigidity. Laboratory data on admission were as follows: white blood cells 6.28 x103/mm3, with 76.4% neutrophils, and C-reactive protein (CRP) 20.7 mg/L. Abdominal X- ray did not reveal any significant abnormality. A CT was performed and revealed a right femoral hernia with the vermiform appendix in the hernia sac and mural thickening. There were no signs of perforation or abscess (Figure 1).

Case Report 1
Contrast-enhanced CT of the abdomen. (A) Axial view: tubular structure containing gas within the femoral hernia. (B) Coronal and (C) sagittal views: tubular structure extending from the caecal base.
An open exploration was chosen. Prior to surgery, the patient received 2g/200mg of amoxicillin/clavulanic acid i.v. and analgesia. Under general anaesthesia, the hernia sac was opened through a Gregoire incision and a phlegmonous appendix was found inside (Figure 2). An appendectomy was performed with a purse-string suture. The hernia sac was closed and the defect was repaired using a polypropylene mesh plug (Lichtenstein technique). Post-operative recovery was satisfactory, with three doses more of 1g/200mg amoxicillin/clavulanic acid i.v, and the patient was discharged on the third day. Histological examination of the appendix revealed acute appendicitis, as defined by infiltration of the appendicular muscularis propia by polymorphonuclear neutrophils. During the follow-up period of 20 months, the patient has not experienced complications or recurrence.
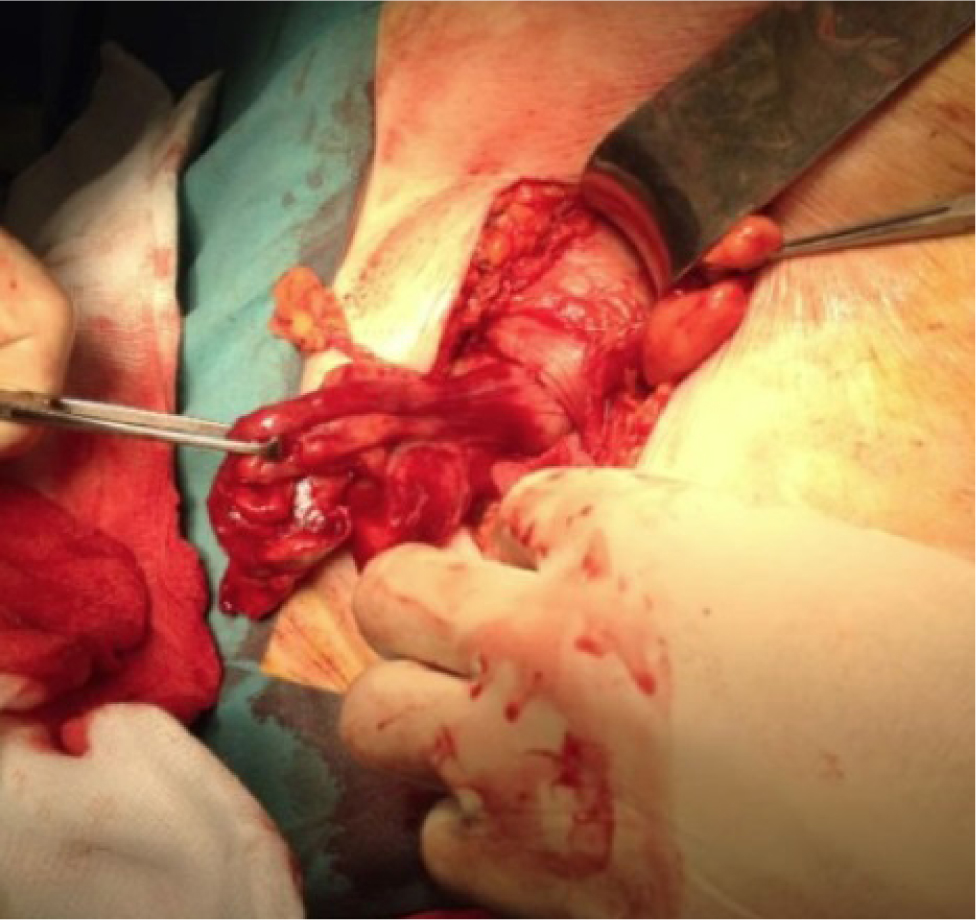
Case Report 1 Inflamed appendix inside the femoral hernia sac.
3 Case Report 2
A 77-year-old female was referred to the emergency department with diarrhea, vomiting and diffuse abdominal pain for two days. Her past medical history included hypertension, type 2 diabetes mellitus, dyslipemia, bronchial asthma, irritable bowel syndrome and hypothyroidism. On admission, the patient was haemodynamically stable and afebrile. Physical findings revealed a soft, non-distended abdomen with a tender mass in the right inguinal region measuring approximately 4x6cm. Laboratory tests showed a white blood cell count 12.30 x103/mm3, with 90.9% neutrophils, and CRP 2 mg/L. X- ray did not reveal bowel obstruction. A CT showed edematous appendix with an appendicolith inside it, in a right femoral hernia sac. The decision was taken to perform laparoscopic surgery. The patient received 2g/200mg of amoxicillin/clavulanic acid i.v. preoperatively. With general anaesthesia, an infraumbilical incision was made, and a pneumoperitoneum was obtained using Hasson’s open technique. A 5-mm abdominal port was placed suprapubically and a 12-mm port in the left iliac fossa. A 10-mm, 30-degree telescope was used to examine the abdominal cavity. A large portion of the appendix, which had undergone necrosis and perforated, was seen to pass through the femoral defect from where purulent fluid was evacuated. The mesoappendix was stapled and transected with a tissue sealing generator, and the base of the appendix with a linear cutter stapler. The femoral defect was repaired primarily with an absorbable suture. Post-operative recovery was uneventful and the patient was discharged on the sixth postoperative day. Histology showed acute ischaemic and necrotic appendicitis with perforation. During eight months of follow-up, the patient has not experienced complications.
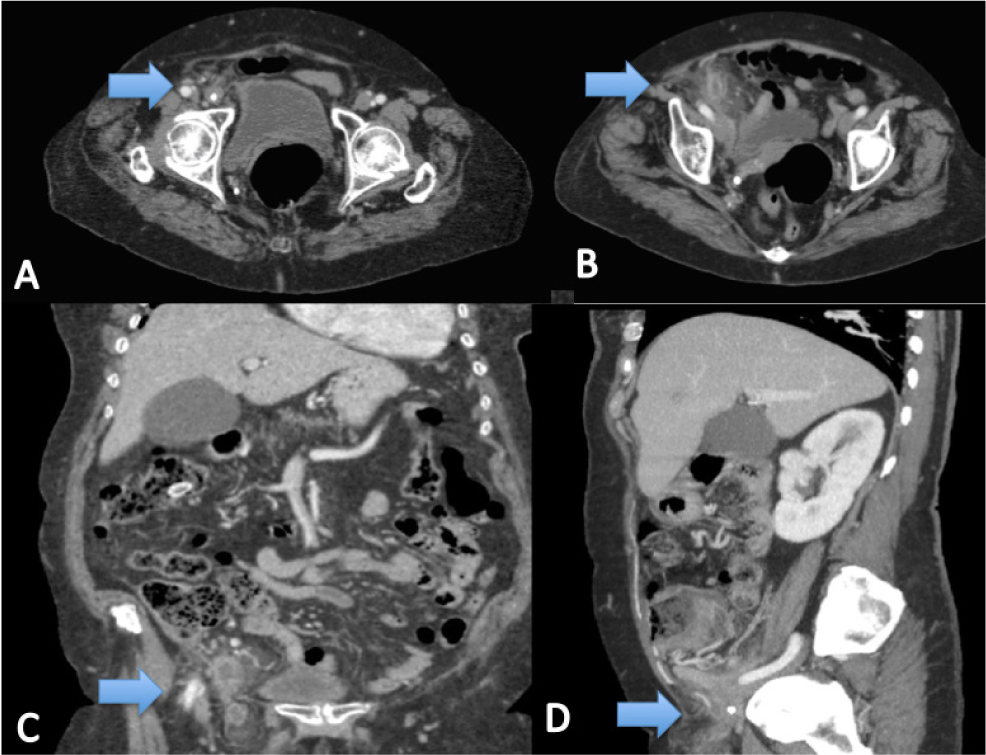
A, B, C, D Case Report 2. CT images Arrow: Appendix
4 Discussion
Garengeot’s hernia was first described in 1731 by Rene Jacques Croissant de Garengeot [1] and it accounts for 0.9% of femoral hernia repairs [2]. Moreover, acute appendicitis inside the sac is found in 0.08-0.13% of femoral hernias [3]. The first appendectomy in a GH was performed by Hevin in 1785 [4]. The difference with regard to Amyand’s hernia is that in the latter case the acute appendicitis is found in an inguinal hernia; it is named after the English surgeon Claudius Amyand, who performed the first appendectomy in an inguinal hernia sac in 1735 [4].
An unlimited literature search of the PubMed data base was performed on 1 December, 2015 with the following search criteria: ((Garengeot’s hernia) OR (Amyand’s hernia) OR (Hernia)) AND (Appendix). The search yielded 546 results. We initially identified 136 studies relevant to the subject, of which 81 were eligible for our analysis. The references of the selected studies were checked. We found 64 cases, 22 of them diagnosed on the basis of CT findings. The results of the review are listed in Table 1 [2,4,5-52].
Cumulative presentation of cases included.
| Author | Age | Sex | CT | Surgery | Mesh | Appendix |
|---|---|---|---|---|---|---|
| Shands AR et al (1903) [5]. | 29 | F | No | Open | No | NA |
| Gerami S et al (1970) [6]. | 71 | M | No | Open | No | perforated AA |
| Voitk AJ et al. (1974) [7]. | 59 | F | No | Open | No | Enterocutaneous fistula |
| Voitk AJ et al. (1974) [7]. | 76 | F | No | Open | No | perforated AA |
| Cutolo L et al (1978) [8]. | 78 | F | No | Open | No | gangrenous and perforated AA |
| Guirguis EM et al (1989) [9]. | 80 | F | No | NA | NA | gangrenous AA |
| Zissin L et al (2000)[10]. | 87 | F | Yes | Open | Yes | perforated AA |
| Isaacs LE et al (2002) [11]. | 76 | M | No | Open | No | NA |
| Mansari O et al (2002) [12]. | 60 | F | No | Open | No | catharral AA |
| Nguyen ET et al (2004) [13]. | 88 | M | No | Open | No | perforated AA |
| Barbaros U et al (2004) [14]. | 85 | F | No | Open | Yes | gangrenous AA |
| Fukukura Y et al (2005) [15]. | 54 | F | Yes | Open | No | phlegmonous AA |
| Priego P et al (2005) [16]. | 78 | F | No | Open | Yes | AA |
| Priego P et al (2005) [16]. | 83 | F | No | Open | No | AA |
| Priego P et al (2005) [16]. | 75 | F | No | Open | Yes | AA |
| Priego P et al (2005) [16]. | 75 | F | No | Open | No | AA |
| Priego P et al (2005) [16]. | 82 | F | No | Open | No | Normal |
| Priego P et al (2005) [16]. | 80 | F | No | Open | Yes | Normal |
| Akopian G et al (2005) [4] | 81 | F | No | Open | Yes | AA |
| D’Ambrosio N et al (2006) [17]. | 71 | F | Yes | NA | NA | perforated AA. Right hemicolectomy |
| Comman A et al (2007) [18]. | 38 | F | No | Laparoscopic | Yes | AA |
| Gillion JF et al (2007) [19]. | NA | NA | Yes | NA | NA | NA |
| Sharma H et al (2007) [20]. | NA | F | No | Open | ||
| Sharma H et al (2007) [20]. | NA | F | No | Open | 4 Yes | 1 perforated AA |
| Sharma H et al (2007) [20]. | NA | F | No | Open | 3 No | |
| Sharma H et al (2007) [20]. | NA | F | No | Open | ||
| Sharma H et al (2007) [20]. | NA | M | No | Open | ||
| Sharma H et al (2007) [20]. | NA | M | No | Open | ||
| Sharma H et al (2007) [20]. | NA | M | No | Open | ||
| Maizlin ZV et al (2007) [21]. | 83 | F | Yes | NA | NA | NA |
| Kibil W et al (2008) [22]. | NA | NA | NA | NA | NA | NA |
| Chung A et al (2009) [23]. | 83 | F | No | Open | No | necrotic AA |
| Ebisawa K et al (2009) [24]. | 90 | F | Yes | Open | Yes | AA |
| Thomas B et al (2009) [25]. | 77 | F | Yes | Both | No | AA |
| Ring A et al (2009) [26]. | 69 | F | NA | NA | NA | NA |
| Shah A et al (2010) [27]. | 46 | F | Yes | Both | No | AA |
| Caygill P et al (2011) [28]. | 78 | F | No | Open | No | AA |
| Konofaos P et al (2011) [2] | 60 | F | No | Open | Yes | gangrenous AA |
| Piperos P et al (2012) [29]. | 83 | F | No | Open | No | AA |
| Allen BC et al (2012) [30]. | 76 | F | Yes | Open | Yes | No appendectomy |
| Phillips AW et al (2012) [31]. | 73 | F | Yes | Open | No | AA |
| Salkade PR et al (2012) [32]. | 67 | F | Yes | Open | No | AA |
| Coskun K et al (2013) [33]. | 65 | F | Yes | Open | No | AA |
| Sen C et al (2013) [34]. | 58 | F | Yes | Open | No | gangrenous AA |
| Hamcan S et al (2013) [35]. | 66 | F | Yes | NA | NA | perforated AA |
| Moris D (2013) [36]. | 49 | F | No | Open | No | AA |
| Erdas E et al (2013) [37]. | 33 | F | No | Open | Yes | AA |
| Ardeleanu V et al (2013) [38]. | 76 | F | No | Open | No | AA |
| Beysens M et al (2013) [39]. | 64 | F | No | Laparoscopic | Yes | NA |
| Ramsingh J et al (2014) [40]. | 70 | F | Yes | Both | Yes | AA |
| Schäfer HM et al (2014) [41]. | 71 | F | No | Open | No | AA |
| Madiha A et al (2014) [42]. | 79 | F | No | Open | No | AA |
| Hao J et al (2014) [43]. | 81 | F | Yes | Open | Yes | Normal |
| Akbari K et al (2014) [44]. | 80 | F | No | Open | No | NA |
| Akbari K et al (2014) [44]. | 54 | F | No | Open | No | NA |
| Akbari K et al (2014) [44]. | 68 | F | Yes | Open | No | NA |
| Ahmed K et al (2014) [45]. | 71 | M | Yes | Open | No | AA perforated |
| Le H et al (2014) [46]. | 91 | F | Yes | Open | No | AA |
| Hussain A et al (2014) [47]. | 86 | F | No | Open | No | AA necrotic |
| Snoeks R et al (2014) [48]. | 76 | F | Yes | Laparoscopic | No | AA |
| Liipo TK et al (2015) [49]. | 60 | M | Yes | Open | Yes | AA |
| Talini C et al (2015) [50]. | 86 | M | No | Open | Yes | Normal |
| Pan CW et al (2015) [51]. | 50 | F | Yes | Open | Yes | gangrenous AA |
| Tancredi K et al (2015) [52]. | 85 | M | No | Open | No | AA |
| García-Amador C et al. (2015) | 86 | F | Yes | Open | Yes | phlegmonous AA |
| García-Amador C et al. (2015) | 77 | F | Yes | Laparoscopic | No | perforated AA |
NA= no available. AA=acute appendicitis.
Garengeot’s hernia is a rare occurrence. Two possible aetiologies have been proposed. According to the first theory, the appendix may be in an abnormal anatomical position owing to different degrees of intestinal rotation during embryological development, or to variations in caecal attachments. The second theory suggests that an anatomically large caecum forces the appendix into the pelvis, which therefore has a high risk of entering a hernial sac from the pelvic peritoneum [28]. The inflammatory process of the appendix is usually caused by the extraluminal obstruction of the appendix at the hernial neck, rather than by the more usual cause of intraluminal obstruction [10]. The obstruction of the neck leads to a vascular compromise which allows bacterial overgrowth [53]. Our case reports reflect the two presentations; in the first one, no obvious intraluminal obstruction was noted, and in the second an appendicolith was identified.
The female-to-male incidence ratio of GH is 5:1 with an age range from 29 to 91 years old (mean age 70). GH has been attributed to body changes during pregnancy. Other risk factors include increased intra-abdominal pressure, smoking, age and collagen disease. Most GHs occur on the right side [54]. Weakening of the transversalis fascia is also thought to play a role.
The clinical presentation usually takes the form of an incarcerated or strangulated femoral hernia and a painful groin mass. Abdominal pain, nausea, vomiting and diarrhoea are not usually reported. The narrowness and rigidity of the femoral canal usually prevents intraperitoneal spread of infection, and so there are no symptoms of peritonitis. Laboratory tests often show leucocytosis and elevated CRP [20]. X ray findings are usually nonspecific, but assist in recognizing small bowel obstruction if present.
In addition to inguinal hernia the differential diagnosis should include adnexitis, ectasia of the vena saphena magna, lymphomas, lipomas or other soft tissue tumors or a varix node [18].
Because of the rarity of the entity and the absence of the typical symptoms associated with acute appendicitis, achieving preoperative diagnosis is very difficult. Most patients are rushed to the surgical room with the inconclusive diagnosis of an incarcerated hernia. Most GH are diagnosed intraoperatively. Preoperative diagnosis by CT has been reported in only 24 cases, including the two case reports we present here. In our review, one more case was diagnosed using ultrasound [14].
In CT findings, GH should be considered when intramural air is present in an incarcerated femoral hernia sac without signs of bowel obstruction [24]. Therefore, a low-positioned caecum with a blind-ended tubular structure within the hernia sac and stranding of nearby fat on CT has been reported to have 98% sensitivity and specificity for the diagnosis of appendicitis inside a hernia sac [46].
The treatment of this disease is emergency surgery. Due to the rarity of the condition there is no standard procedure. The options available include laparoscopic or open approaches either with a mesh or simple herniorrhaphy, with or without appendectomy. In our review, most cases were performed via an open approach. Appendectomy via the hernial sac is considered appropriate; in case of perforation and abscess formation, a transabdominal access is preferred [24]. A combined approach was used in only three cases, all of which had been diagnosed preoperatively using CT. In two of them, the appendix was removed laparoscopically and the femoral hernia was repaired via a laparotomic approach [25,40]. In the other, laparoscopic drainage of the abscess and adhesiolysis were performed followed by a laparotomy for the appendectomy and herniorrhaphy [27].
Laparoscopy may be a valid technique for determining the condition of the hernia, but due to the difficulty of preoperative diagnosis it is unlikely to be the first choice for the surgical approach. In fact, in our review only three cases underwent laparoscopy [18,39,48], and only one of them had a preoperative diagnosis of GH [39].
In our two cases, the first one was treated via laparotomy and the second by laparoscopy. Both cases had been diagnosed preoperatively on the basis of the CT findings.
The appendectomy procedure is also controversial. It has been suggested that in the presence of a normal appendix appendectomy is not required. However, the surgery is not excessively complicated, and even in the absence of macroscopic inflammation the presence of microscopic inflammation from compression and ischemia within the hernia neck cannot be ruled out; for this reason, appendectomy should be performed [16]. In our review, the appendix was left in place in only one case [30].
Another controversial point is the use of a mesh, which was reported in only 55 cases in our review; in 35 a herniorrhaphy was performed. In the absence of abscess formation or perforation, the implantation of a mesh has been described as the hernia repair of choice [24]. In our first case, the surgery was performed immediately and there was no abscess formation in the hernia sac; a simultaneous appendectomy and primary hernioplasty using synthetic mesh was chosen. In the second case, as purulent fluid was evacuated, a herniorrhaphy was preferred.
The most important contributing factor to the increase in wound infection is delayed diagnosis [43]. The reported infection rates reached 29%, while severe complications such as necrotizing fasciitis and death were only rarely described [20].
5 Conclusion
GH is a rare condition which requires prompt treatment in order to avoid complications. Preoperative diagnosis with CT can indicate the correct management, that is, appendectomy via inguinotomy and hernioplasty if there is no perforation or abscess formation. More studies of procedures using the laparoscopic approach are required, especially in relation to the incidence of wound infection.
The Authors have no conflict of interest
Conflict of interest statement
Authors state no conflict of interest.
References
[1] De Garengeot RJC., Traite des operations de chirurgie, 2nd Ed Paris, Huart, 1731, 369-371Suche in Google Scholar
[2] Konofaos P., Spartalis E, Smirnis A., Kontzoglou K., Kouraklis G., De Garengeot’s hernia in a 60-year-old woman: a case report, Journal of Medical Case Reports, 2011, 5:25810.1186/1752-1947-5-258Suche in Google Scholar
[3] Rajan S.S., Girn H.R., Ainslie W.G., Inflamed appendix in a femoral hernia sac: de Garengeot’s hernia, Hernia, 2009, 13(5), 551-55310.1007/s10029-009-0472-7Suche in Google Scholar
[4] Akopian G., Alexander M., De Garengeot Hernia. Appendicitis within a Femoral Hernia, Am Surg, 2005, 71(6),526-52710.1177/000313480507100617Suche in Google Scholar
[5] Shands A.R., Inflamed Appendix in the Sac of a Femoral Hernia, Ann Surg, 1904, 40(3), 380-38110.1097/00000658-190440030-00011Suche in Google Scholar
[6] Gerami .S, Easley G.W., Mendoza C.B., Appendiceal abscess as contents of right femoral hernia. A case report, International Surgery, 1970, 53(5), 354-356Suche in Google Scholar
[7] Voitk A.J., MacFarlane J.K., Estrada R.L., Ruptured appendicitis in femoral hernias: report of two cases and review of the literature, Ann Surg, 1974, 179(1), 24-2610.1097/00000658-197401000-00005Suche in Google Scholar
[8] Cutolo L., Wasserman I., Pinck R., Mainzer R.A., Acute suppurative appendicitis occurring within a femoral hernia: report of a case, Dis Colon Rectum, 1978, 1(3), 203-20410.1007/BF02586573Suche in Google Scholar
[9] Guirguis E.M., Taylor G.A., Chadwick C.D., Femoral appendicitis: an unusual case, Can J Surg, 1989, 32(5),380-381Suche in Google Scholar
[10] Zissin R., Brautbar O., Shapiro-Feinberg M., CT diagnosis of acute appendicitis in a femoral hernia, Br J Radiol, 2000, 73(873),1013-101410.1259/bjr.73.873.11064659Suche in Google Scholar
[11] Isaacs L.E., Felsenstein C.H., Acute appendicitis in a femoral hernia: an unusual presentation of a groin mass, J Emerg Med, 2002, 23(1),15-1810.1016/S0736-4679(02)00455-9Suche in Google Scholar
[12] Mansari O., Sakit F., Janati M.I., Accute apendicitis on crural hernia, Presse Med, 2002, 31(24),1129-1130Suche in Google Scholar
[13] Nguyen E.T., Komenaka I.K., Strangulated femoral hernia containing a perforated appendix, Can J Surg, 2004, 47(1),68-69Suche in Google Scholar
[14] Barbaros U., Asoglu O., Seven R., Kalayci M., Appendicitis in incarcerated femoral hernia, Hernia, 2004, 8(3), 281-28210.1007/s10029-004-0209-6Suche in Google Scholar PubMed
[15] Fukukura Y., Chang S.D., Acute appendicitis within a femoral hernia: multidetector CT findings, Abdom Imaging, 2005, 30(5), 620-62210.1007/s00261-004-0283-3Suche in Google Scholar PubMed
[16] Priego P., Lobo E., Moreno I., Sánchez-Picot S., Gil M.A., Alonso N., et al, Acute apendicitis in an incarcerated crural hernia: analysis of our experience, Rev Esp Enferm Dig, 2005, 97(10),707-71510.4321/S1130-01082005001000004Suche in Google Scholar
[17] D’Ambrosio N., Katz Z., Hines J., Perforated appendix within a femoral hernia, AJR, 2006, 186(3), 906-90710.2214/AJR.05.0080Suche in Google Scholar PubMed
[18] Comman A., Gaetzschmann P., Hanner T., Behrend M., DeGarengeot hernia: transabdominal preperitoneal hernia repair and appendectomy, JSLS, 2007, 11(4),496-501Suche in Google Scholar
[19] Gillion J.F., Bornet G., Hamrouni A., Julles M.C., Convard J.P., Amyand and de Garengeot’hernias, Hernia, 2007, 11,289-29010.1007/s10029-007-0221-8Suche in Google Scholar PubMed
[20] Sharma H., Jha P.K., Shekhawat N.S., Memon B., Memon M.A., De Garengeot hernia: an analysis of our experience, Hernia, 2007, 11(3), 235-23810.1007/s10029-007-0208-5Suche in Google Scholar PubMed
[21] Maizlin Z.V., Mason A.C., Brown C., Brown J.A., CT findings of normal and inflamed appendix in groin hernia, Emerg Radiol, 2007, 14(2), 97-10010.1007/s10140-007-0601-5Suche in Google Scholar PubMed
[22] Kibil W., Jedrys J., Matyja A., Legutko J., Kulig J., Appendix incarcerated in femoral hernia-case report, Folia Med Cracov, 2008, 49(1-2), 45-48Suche in Google Scholar
[23] Chung A., Goel A., Images in clinical medicine. De Garengeot’s hernia, N Engl J Med, 2009, 361(11),1810.1056/NEJMicm0802611Suche in Google Scholar PubMed
[24] Ebisawa K., Yamazaki S., Kimura, Kashio M., Kurito K., Yasumuro S., et al, Acute appendicitis in an incarcerated femoral hernia: a case of de Garengeot hernia, Case Rep Gastroenterol, 2009, 3(3), 313-31710.1159/000250821Suche in Google Scholar PubMed PubMed Central
[25] Thomas B., Thomas M., McVay B., Chivate J., De Garengeot hernia, JSLS, 2009, 13(3),455-457Suche in Google Scholar
[26] Ring A., Gelis V., Klupscha C., Stenr J., De Garengeot appendicitis-rare variant of a common medical condition, Zentralbl Chirm, 2009, 134(6), 564-56610.1055/s-0029-1224564Suche in Google Scholar PubMed
[27] Shah A., Janardhan H.S., De Garengeot hernia: a case report and review of literature, Indian J Surg, 2013, 75(Suppl 1),439-44110.1007/s12262-012-0778-zSuche in Google Scholar PubMed PubMed Central
[28] Caygill P., Nair R., Sajjanshetty M., Francis D., An unusual groin exploration: de Garengeot’s hernia, Int J Surg Case Rep, 2011, 2(5),74-7510.1016/j.ijscr.2011.01.008Suche in Google Scholar PubMed PubMed Central
[29] Piperos T., Kalles V., Al Awhal Y., Konstantinou E., Skarpas G., Mariolis-Sapsakos T., Clinical significance of de Garengeot’s hernia: a case of acute appendicitis and review of the literature, Int J Surg Case Rep, 2012, 3(3),116-11710.1016/j.ijscr.2011.12.003Suche in Google Scholar PubMed PubMed Central
[30] Allen B.C., Kirsch J., Szomstein S., De Garengeot Hernia, Radiology, 2012, 265 (2), 640-64410.1148/radiol.12102051Suche in Google Scholar PubMed
[31] Phillips A.W., Aspinall S.R., Appendicitis and Meckel’s diverticulum in a femoral hernia: simultaneous De Garengeot and Littre’s hernia, Hernia, 2012, 16(6), 727-72910.1007/s10029-011-0812-2Suche in Google Scholar PubMed
[32] Salkade P.R., Chung A.Y., Law Y.M., De Garengeot’s hernia.: an unusual right groin mass due to acute appendicitis in an incarcerated femoral hernia, Hong Kong Med J, 2012, 18(5), 442-445Suche in Google Scholar
[33] Coskun K., Kilbas Z., Yigit T., Simsek A., Harlak A., De Garengeot’s hernia: the importance of early diagnosis and its complications, Hernia, 2012, 16(6),731-73310.1007/s10029-011-0814-0Suche in Google Scholar PubMed
[34] Sen C., Tanrikulu Y., Akkapulu N., De Garengeot’s hernia: a case of acute appendicitis in a femoral hernia sac, Ulus Travma Acil Cerrahi Derg, 2013, 19 (4), 380-38210.5505/tjtes.2013.37043Suche in Google Scholar PubMed
[35] Hamcan S., Akgun V., Battal B., Karaman B., Acute perforated appendicitis in femoral hernia sac: CT imaging findings, BMJ Case Rep, 2013, (in press), 10.1136/bcr-2013-200050Suche in Google Scholar PubMed PubMed Central
[36] Moris D., De Garengeot’s Hernia, Brief Reportd, 2013, 11.10.1177/000313481307901102Suche in Google Scholar
[37] Erdas E., Sias L., Licheri S., Secci L., Aresu S., Barbarossa M., et al, De Garengeot hernia with acute appendicitis, G Chir, 2013, 34(3),86-89Suche in Google Scholar
[38] Ardeleanu V., Chicos S., Tutnaru D., A rare case of acute abdomen: Garengeot hernia, Chirurgia Bucur, 2013, 108(6), 896-899Suche in Google Scholar
[39] Beysens M., Haeck L., Vindevoghel K., Laparoscopic appendectomy combined with TEP for de Garengeot hernia: case report, Acta Chir Belg, 2013, 113(6),468-47010.1080/00015458.2013.11680967Suche in Google Scholar
[40] Ramsingh J., Ali A., Cameron C., Al-Ani A., Hodnett R., Chorushyj C., De Garengeot’s hernia: diagnosis and surgical management of a rare type of femoral hernia, J Surg Case Rep, 2014, (in press), 10.1093/jscr/rju008Suche in Google Scholar PubMed PubMed Central
[41] Schäfer H.M., von Holzen U., Nebiker C., Swelling of the right thigh for over 30 years-The rare finding of a De Garengeot hernia, Int J Surg Case Rep, 2014, 5(12),1120-112210.1016/j.ijscr.2014.11.010Suche in Google Scholar PubMed PubMed Central
[42] Madiha A., Rares H., Abdus S., De Garengeot hernia: a forgotten rare entity?, BMJ Case Rep, 2014, (in press),10.1136/bcr-2013-201413Suche in Google Scholar PubMed PubMed Central
[43] Hao J., Yao J., Guo D., Sun W., Liang J., Jiang X., De Garengeot hernia: the ultrasound and computed tomographic findings in an 81-year-old woman, Am J Emerg Med, 2014, 32(5),48610.1016/j.ajem.2013.11.003Suche in Google Scholar PubMed
[44] Akbari K., Wood C., Hammad A., Midletton S., De Garengeot’s hernia: our experience of three cases and literature review, BMJ Case Rep, 2014, (in press), 10.1136/bcr-2014-205031Suche in Google Scholar PubMed PubMed Central
[45] Ahmed K., Bashar K., McHugh T.J., Appendicitis in De Garengeot’s Hernia Presenting as a Nontender Inguinal Mass: Case Report and Review of the Literature, Case Rep Surg, 2014, 10.1155/2014/932638Suche in Google Scholar PubMed PubMed Central
[46] Le H., Odom SR., Hsu A., Gupta A., Hauser C.J., A combined Richter’s and de Garengeot’s hernia, Int J Surg Case Rep, 2014, 5, 662-66410.1016/j.ijscr.2014.03.022Suche in Google Scholar PubMed PubMed Central
[47] Hussain A., Slesser A.A., Monib S., Maalo J., Soskin M., Arbuckle J., A De Garengeot Hernia masquerading as a strangulated femoral hernia, Int J Surg Case Rep, 2014, 5(10),656-65810.1016/j.ijscr.2014.08.001Suche in Google Scholar PubMed PubMed Central
[48] Snoekx R., Geyskens P., De Garengeot’s Hernia : Acute Appendicitis in a Femoral Hernia, Case Report and Literature Overview Acta Chir Belg, 2014, 114,149-15110.1080/00015458.2014.11681000Suche in Google Scholar
[49] Liipo T.K., Seppälä T.T., Mattila A., De Garengeot’s hernia: 40 years after Bassini inguinal hernioplasty, BMJ Case Rep, 2015, (in press), 10.1136/bcr-2014-208327Suche in Google Scholar PubMed PubMed Central
[50] Talini C., Oliveira L.O., Araújo A., De Garengeot hernia: Case report and review, Int J Surg Case Rep, 2015, (in press), 10.1016/j.ijscr.2014.12.042Suche in Google Scholar PubMed PubMed Central
[51] Pan C.W., Tsao M.J., Su C.S., A case of De Garengeot hernia requiring early surgery, BMJ Case Rep, 2015, (in press), 10.1136/bcr-2015-211102Suche in Google Scholar PubMed PubMed Central
[52] Tancredi A., Bellagamba R., Cotugno M., Impagnatiello E., Torre P., Masi M., et al., De Garengeot’s Hernia: a Diagnostic Challenge, Indian J Surg, 2015 (in press), 10.1007/s12262-015-1266-zSuche in Google Scholar PubMed PubMed Central
[53] Muffak K., Ramia J.M., Palomeque A., Segura M., Muñoz N., Garrote D., Ferron J.A., Hernia de Aymand. Cir And, 2004, 15, 155-156Suche in Google Scholar
[54] Kalles V., Mekras A., Mekras D., Papapanagiotou I., Harethee W., Sotiropoulos G., et al, De Garengeot’s hernia: a comprenhensive review, Hernia, 2013, 17, 177-18210.1007/s10029-012-0993-3Suche in Google Scholar PubMed
© 2016 Cristina Garcia-Amador et al.
This work is licensed under the Creative Commons Attribution-NonCommercial-NoDerivatives 3.0 License.
Artikel in diesem Heft
- Research Article
- The possible molecular regulation mechanism of CIK cells inhibiting the proliferation of Human Lung Adenocarcinoma NCL-H157 Cells
- Case Report
- Urethral stone of unexpected size: case report and short literature review
- Case Report
- Complete remission through icotinib treatment in Non-small cell lung cancer epidermal growth factor receptor mutation patient with brain metastasis: A case report
- Research Article
- FPL tendon thickness, tremor and hand functions in Parkinson’s disease
- Research Article
- Diagnostic value of circulating tumor cells in cerebrospinal fluid
- Research Article
- A meta-analysis of neuroprotective effect for traditional Chinese medicine (TCM) in the treatment of glaucoma
- Research Article
- MiR-218 increases sensitivity to cisplatin in esophageal cancer cells via targeting survivin expression
- Research Article
- Association of HOTAIR expression with PI3K/Akt pathway activation in adenocarcinoma of esophagogastric junction
- Research Article
- The role of interleukin genes in the course of depression
- Case Report
- A rare case of primary pulmonary diffuse large B cell lymphoma with CD5 positive expression
- Research Article
- DWI and SPARCC scoring assess curative effect of early ankylosing spondylitis
- Research Article
- The diagnostic value of serum CEA, NSE and MMP-9 for on-small cell lung cancer
- Case Report
- Dysphonia – the single symptom of rifampicin resistant laryngeal tuberculosis
- Review Article
- Development of epidermal growth factor receptor tyrosine kinase inhibitors against EGFR T790M. Mutation in non small-cell lung carcinoma
- Research Article
- Negative regulation of CDC42 expression and cell cycle progression by miR-29a in breast cancer
- Research Article
- Expression analysis of the TGF-β/SMAD target genes in adenocarcinoma of esophagogastric junction
- Research Article
- Blood cells in thyroid cancer patients: a possible influence of apoptosis
- Research Article
- Detected EGFR mutation in cerebrospinal fluid of lung adenocarcinoma patients with meningeal metastasis
- Mini-review
- Pathogenesis-oriented approaches for the management of corticosteroid-resistant or relapsedprimary immune thrombocytopenia
- Research Article
- GSTP1 A>G polymorphism and chemosensitivity of osteosarcoma: A meta-analysis
- Research Article
- A meta-analysis of adiponectin gene rs22411766 T>G polymorphism and ischemic stroke susceptibility
- Research Article
- The diagnosis and pathological value of combined detection of HE4 and CA125 for patients with ovarian cancer
- Research Article
- SOX7 inhibits tumor progression of glioblastoma and is regulated by miRNA-24
- Research Article
- Sevoflurane affects evoked electromyography monitoring in cerebral palsy
- Case Report
- A case report of hereditary spherocytosis with concomitant chronic myelocytic leukemia
- Case Report
- A case of giant saphenous vein graft aneurysm followed serially after coronary artery bypass surgery
- Research Article
- LncRNA TUG1 is upregulated and promotes cell proliferation in osteosarcoma
- Review Article
- Meningioma recurrence
- Case Report
- Endobronchial amyloidosis mimicking bronchial asthma: a case report and review of the literature
- Case Report
- A confusing case report of pulmonary langerhans cell histiocytosis and literature review
- Research Article
- Effect of hesperetin on chaperone activity in selenite-induced cataract
- Research Article
- Clinical value of self-assessment risk of osteoporosis in Chinese
- Research Article
- Correlation analysis of VHL and Jade-1 gene expression in human renal cell carcinoma
- Research Article
- Is acute appendicitis still misdiagnosed?
- Retraction
- Retraction of: application of food-specific IgG antibody detection in allergy dermatosis
- Review Article
- Platelet Rich Plasma: a short overview of certain bioactive components
- Research Article
- Correlation between CTLA-4 gene rs221775A>G single nucleotide polymorphism and multiple sclerosis susceptibility. A meta-analysis
- Review Article
- Standards of anesthesiology practice during neuroradiological interventions
- Research Article
- Expression and clinical significance of LXRα and SREBP-1c in placentas of preeclampsia
- Letter to the Editor
- ARDS diagnosed by SpO2/FiO2 ratio compared with PaO2/FiO2 ratio: the role as a diagnostic tool for early enrolment into clinical trials
- Research Article
- Impact of sensory integration training on balance among stroke patients: sensory integration training on balance among stroke patients
- Review Article
- MicroRNAs as regulatory elements in psoriasis
- Review Article
- Influenza A(H1N1)pdm09 and postpandemic influenza in Lithuania
- Review Article
- Garengeot’s hernia: two case reports with CT diagnosis and literature review
- Research Article
- Concept of experimental preparation for treating dentin hypersensitivity
- Research Article
- Hydrogen water reduces NSE, IL-6, and TNF-α levels in hypoxic-ischemic encephalopathy
- Research Article
- Xanthogranuloma of the sellar region diagnosed by frozen section
- Case Report
- Laparoscopic antegrade cholecystectomy: a standard procedure?
- Case Report
- Maxillary fibrous dysplasia associated with McCune-Albright syndrome. A case study
- Regular Article
- Sialoendoscopy, sialography, and ultrasound: a comparison of diagnostic methods
- Research Article
- Antibody Response to Live Attenuated Vaccines in Adults in Japan
- Conference article
- Excellence and safety in surgery require excellent and safe tutoring
- Conference article
- Suggestions on how to make suboptimal kidney transplantation an ethically viable option
- Regular Article
- Ectopic pregnancy treatment by combination therapy
- Conference article
- Use of a simplified consent form to facilitate patient understanding of informed consent for laparoscopic cholecystectomy
- Regular Article
- Cusum analysis for learning curve of videothoracoscopic lobectomy
- Regular Article
- A meta-analysis of association between glutathione S-transferase M1 gene polymorphism and Parkinson’s disease susceptibility
- Conference article
- Plastination: ethical and medico-legal considerations
- Regular Article
- Investigation and control of a suspected nosocomial outbreak of pan-drug resistant Acinetobacter baumannii in an intensive care unit
- Regular Article
- Multifactorial analysis of fatigue scale among nurses in Poland
- Regular Article
- Smoking cessation for free: outcomes of a study of three Romanian clinics
- Regular Article
- Clinical efficacy and safety of tripterygium glycosides in treatment of stage IV diabetic nephropathy: A meta-analysis
- Special Issue on Italian Society for the Study of Vascular Anomalies
- Prevention and treatment of peritoneal adhesions in patients affected by vascular diseases following surgery: a review of the literature
- Special Issue on Italian Society for the Study of Vascular Anomalies
- Surgical treatment of recidivist lymphedema
- Special Issue on Italian Society for the Study of Vascular Anomalies
- CT and MR imaging of the thoracic aorta
- Special Issue on Italian Society for the Study of Vascular Anomalies
- Role of FDG-PET scan in staging of pulmonary epithelioid hemangioendothelioma
- Special Issue on Italian Society for the Study of Vascular Anomalies
- Sternal reconstruction by extracellular matrix: a rare case of phaces syndrome
- Special Issue on Italian Society for the Study of Vascular Anomalies
- Prenatal diagnosis, 3-D virtual rendering and lung sparing surgery by ligasure device in a baby with “CCAM and intralobar pulmonary sequestration”
- Special Issue on Italian Society for the Study of Vascular Anomalies
- Serum levels of inhibin B in adolescents after varicocelelectomy: A long term follow up
- Special Issue on Italian Society for the Study of Vascular Anomalies
- Our experience in the treatment of Malignant Fibrous Hystiocytoma of the larynx: clinical diagnosis, therapeutic approach and review of literature
- Special Issue on Italian Society for the Study of Vascular Anomalies
- Delayed recurrent nerve paralysis following post-traumatic aortic pseudoaneurysm
- Special Issue on Italian Society for the Study of Vascular Anomalies
- Integrated therapeutic approach to giant solitary fibrous tumor of the pleura: report of a case and review of the literature
- Special Issue on Italian Society for the Study of Vascular Anomalies
- Celiac axis compression syndrome: laparoscopic approach in a strange case of chronic abdominal pain in 71 years old man
- Special Issue on Italian Society for the Study of Vascular Anomalies
- A rare case of persistent hypoglossal artery associated with contralateral proximal subclavian stenosis
- Focus on Medico-Legal and Ethical Topics in Surgery in Italy
- Contralateral risk reducing mastectomy in Non-BRCA-Mutated patients
- Focus on Medico-Legal and Ethical Topics in Surgery in Italy
- Professional dental and oral surgery liability in Italy: a comparative analysis of the insurance products offered to health workers
- Focus on Medico-Legal and Ethical Topics in Surgery in Italy
- Informed consent in robotic surgery: quality of information and patient perception
- Focus on Medico-Legal and Ethical Topics in Surgery in Italy
- Malfunctions of robotic system in surgery: role and responsibility of surgeon in legal point of view
- Focus on Medico-Legal and Ethical Topics in Surgery in Italy
- Medicolegal implications of surgical errors and complications in neck surgery: A review based on the Italian current legislation
- Focus on Medico-Legal and Ethical Topics in Surgery in Italy
- Iatrogenic splenic injury: review of the literature and medico-legal issues
- Focus on Medico-Legal and Ethical Topics in Surgery in Italy
- Donation of the body for scientific purposes in Italy: ethical and medico-legal considerations
- Focus on Medico-Legal and Ethical Topics in Surgery in Italy
- Cosmetic surgery: medicolegal considerations
- Focus on Medico-Legal and Ethical Topics in Surgery in Italy
- Voluntary termination of pregnancy (medical or surgical abortion): forensic medicine issues
- Review Article
- Role of Laparoscopic Splenectomy in Elderly Immune Thrombocytopenia
- Review Article
- Endoscopic diagnosis and treatment of neuroendocrine tumors of the digestive system
- Review Article
- Efficacy and safety of splenectomy in adult autoimmune hemolytic anemia
- Research Article
- Relationship between gastroesophageal reflux disease and Ph nose and salivary: proposal of a simple method outpatient in patients adults
- Case Report
- Idiopathic pleural panniculitis with recurrent pleural effusion not associated with Weber-Christian disease
- Research Article
- Morbid Obesity: treatment with Bioenterics Intragastric Balloon (BIB), psychological and nursing care: our experience
- Research Article
- Learning curve for endorectal ultrasound in young and elderly: lights and shades
- Case Report
- Uncommon primary hydatid cyst occupying the adrenal gland space, treated with laparoscopic surgical approach in an old patient
- Research Article
- Distraction techniques for face and smile aesthetic preventing ageing decay
- Research Article
- Preoperative high-intensity training in frail old patients undergoing pulmonary resection for NSCLC
- Review Article
- Descending necrotizing mediastinitis in the elderly patients
- Research Article
- Prophylactic GSV surgery in elderly candidates for hip or knee arthroplasty
- Research Article
- Diagnostic yield and safety of C-TBNA in elderly patients with lung cancer
- Research Article
- The learning curve of laparoscopic holecystectomy in general surgery resident training: old age of the patient may be a risk factor?
- Research Article
- Self-gripping mesh versus fibrin glue fixation in laparoscopic inguinal hernia repair: a randomized prospective clinical trial in young and elderly patients
- Research Article
- Anal sphincter dysfunction in multiple sclerosis: an observation manometric study
Artikel in diesem Heft
- Research Article
- The possible molecular regulation mechanism of CIK cells inhibiting the proliferation of Human Lung Adenocarcinoma NCL-H157 Cells
- Case Report
- Urethral stone of unexpected size: case report and short literature review
- Case Report
- Complete remission through icotinib treatment in Non-small cell lung cancer epidermal growth factor receptor mutation patient with brain metastasis: A case report
- Research Article
- FPL tendon thickness, tremor and hand functions in Parkinson’s disease
- Research Article
- Diagnostic value of circulating tumor cells in cerebrospinal fluid
- Research Article
- A meta-analysis of neuroprotective effect for traditional Chinese medicine (TCM) in the treatment of glaucoma
- Research Article
- MiR-218 increases sensitivity to cisplatin in esophageal cancer cells via targeting survivin expression
- Research Article
- Association of HOTAIR expression with PI3K/Akt pathway activation in adenocarcinoma of esophagogastric junction
- Research Article
- The role of interleukin genes in the course of depression
- Case Report
- A rare case of primary pulmonary diffuse large B cell lymphoma with CD5 positive expression
- Research Article
- DWI and SPARCC scoring assess curative effect of early ankylosing spondylitis
- Research Article
- The diagnostic value of serum CEA, NSE and MMP-9 for on-small cell lung cancer
- Case Report
- Dysphonia – the single symptom of rifampicin resistant laryngeal tuberculosis
- Review Article
- Development of epidermal growth factor receptor tyrosine kinase inhibitors against EGFR T790M. Mutation in non small-cell lung carcinoma
- Research Article
- Negative regulation of CDC42 expression and cell cycle progression by miR-29a in breast cancer
- Research Article
- Expression analysis of the TGF-β/SMAD target genes in adenocarcinoma of esophagogastric junction
- Research Article
- Blood cells in thyroid cancer patients: a possible influence of apoptosis
- Research Article
- Detected EGFR mutation in cerebrospinal fluid of lung adenocarcinoma patients with meningeal metastasis
- Mini-review
- Pathogenesis-oriented approaches for the management of corticosteroid-resistant or relapsedprimary immune thrombocytopenia
- Research Article
- GSTP1 A>G polymorphism and chemosensitivity of osteosarcoma: A meta-analysis
- Research Article
- A meta-analysis of adiponectin gene rs22411766 T>G polymorphism and ischemic stroke susceptibility
- Research Article
- The diagnosis and pathological value of combined detection of HE4 and CA125 for patients with ovarian cancer
- Research Article
- SOX7 inhibits tumor progression of glioblastoma and is regulated by miRNA-24
- Research Article
- Sevoflurane affects evoked electromyography monitoring in cerebral palsy
- Case Report
- A case report of hereditary spherocytosis with concomitant chronic myelocytic leukemia
- Case Report
- A case of giant saphenous vein graft aneurysm followed serially after coronary artery bypass surgery
- Research Article
- LncRNA TUG1 is upregulated and promotes cell proliferation in osteosarcoma
- Review Article
- Meningioma recurrence
- Case Report
- Endobronchial amyloidosis mimicking bronchial asthma: a case report and review of the literature
- Case Report
- A confusing case report of pulmonary langerhans cell histiocytosis and literature review
- Research Article
- Effect of hesperetin on chaperone activity in selenite-induced cataract
- Research Article
- Clinical value of self-assessment risk of osteoporosis in Chinese
- Research Article
- Correlation analysis of VHL and Jade-1 gene expression in human renal cell carcinoma
- Research Article
- Is acute appendicitis still misdiagnosed?
- Retraction
- Retraction of: application of food-specific IgG antibody detection in allergy dermatosis
- Review Article
- Platelet Rich Plasma: a short overview of certain bioactive components
- Research Article
- Correlation between CTLA-4 gene rs221775A>G single nucleotide polymorphism and multiple sclerosis susceptibility. A meta-analysis
- Review Article
- Standards of anesthesiology practice during neuroradiological interventions
- Research Article
- Expression and clinical significance of LXRα and SREBP-1c in placentas of preeclampsia
- Letter to the Editor
- ARDS diagnosed by SpO2/FiO2 ratio compared with PaO2/FiO2 ratio: the role as a diagnostic tool for early enrolment into clinical trials
- Research Article
- Impact of sensory integration training on balance among stroke patients: sensory integration training on balance among stroke patients
- Review Article
- MicroRNAs as regulatory elements in psoriasis
- Review Article
- Influenza A(H1N1)pdm09 and postpandemic influenza in Lithuania
- Review Article
- Garengeot’s hernia: two case reports with CT diagnosis and literature review
- Research Article
- Concept of experimental preparation for treating dentin hypersensitivity
- Research Article
- Hydrogen water reduces NSE, IL-6, and TNF-α levels in hypoxic-ischemic encephalopathy
- Research Article
- Xanthogranuloma of the sellar region diagnosed by frozen section
- Case Report
- Laparoscopic antegrade cholecystectomy: a standard procedure?
- Case Report
- Maxillary fibrous dysplasia associated with McCune-Albright syndrome. A case study
- Regular Article
- Sialoendoscopy, sialography, and ultrasound: a comparison of diagnostic methods
- Research Article
- Antibody Response to Live Attenuated Vaccines in Adults in Japan
- Conference article
- Excellence and safety in surgery require excellent and safe tutoring
- Conference article
- Suggestions on how to make suboptimal kidney transplantation an ethically viable option
- Regular Article
- Ectopic pregnancy treatment by combination therapy
- Conference article
- Use of a simplified consent form to facilitate patient understanding of informed consent for laparoscopic cholecystectomy
- Regular Article
- Cusum analysis for learning curve of videothoracoscopic lobectomy
- Regular Article
- A meta-analysis of association between glutathione S-transferase M1 gene polymorphism and Parkinson’s disease susceptibility
- Conference article
- Plastination: ethical and medico-legal considerations
- Regular Article
- Investigation and control of a suspected nosocomial outbreak of pan-drug resistant Acinetobacter baumannii in an intensive care unit
- Regular Article
- Multifactorial analysis of fatigue scale among nurses in Poland
- Regular Article
- Smoking cessation for free: outcomes of a study of three Romanian clinics
- Regular Article
- Clinical efficacy and safety of tripterygium glycosides in treatment of stage IV diabetic nephropathy: A meta-analysis
- Special Issue on Italian Society for the Study of Vascular Anomalies
- Prevention and treatment of peritoneal adhesions in patients affected by vascular diseases following surgery: a review of the literature
- Special Issue on Italian Society for the Study of Vascular Anomalies
- Surgical treatment of recidivist lymphedema
- Special Issue on Italian Society for the Study of Vascular Anomalies
- CT and MR imaging of the thoracic aorta
- Special Issue on Italian Society for the Study of Vascular Anomalies
- Role of FDG-PET scan in staging of pulmonary epithelioid hemangioendothelioma
- Special Issue on Italian Society for the Study of Vascular Anomalies
- Sternal reconstruction by extracellular matrix: a rare case of phaces syndrome
- Special Issue on Italian Society for the Study of Vascular Anomalies
- Prenatal diagnosis, 3-D virtual rendering and lung sparing surgery by ligasure device in a baby with “CCAM and intralobar pulmonary sequestration”
- Special Issue on Italian Society for the Study of Vascular Anomalies
- Serum levels of inhibin B in adolescents after varicocelelectomy: A long term follow up
- Special Issue on Italian Society for the Study of Vascular Anomalies
- Our experience in the treatment of Malignant Fibrous Hystiocytoma of the larynx: clinical diagnosis, therapeutic approach and review of literature
- Special Issue on Italian Society for the Study of Vascular Anomalies
- Delayed recurrent nerve paralysis following post-traumatic aortic pseudoaneurysm
- Special Issue on Italian Society for the Study of Vascular Anomalies
- Integrated therapeutic approach to giant solitary fibrous tumor of the pleura: report of a case and review of the literature
- Special Issue on Italian Society for the Study of Vascular Anomalies
- Celiac axis compression syndrome: laparoscopic approach in a strange case of chronic abdominal pain in 71 years old man
- Special Issue on Italian Society for the Study of Vascular Anomalies
- A rare case of persistent hypoglossal artery associated with contralateral proximal subclavian stenosis
- Focus on Medico-Legal and Ethical Topics in Surgery in Italy
- Contralateral risk reducing mastectomy in Non-BRCA-Mutated patients
- Focus on Medico-Legal and Ethical Topics in Surgery in Italy
- Professional dental and oral surgery liability in Italy: a comparative analysis of the insurance products offered to health workers
- Focus on Medico-Legal and Ethical Topics in Surgery in Italy
- Informed consent in robotic surgery: quality of information and patient perception
- Focus on Medico-Legal and Ethical Topics in Surgery in Italy
- Malfunctions of robotic system in surgery: role and responsibility of surgeon in legal point of view
- Focus on Medico-Legal and Ethical Topics in Surgery in Italy
- Medicolegal implications of surgical errors and complications in neck surgery: A review based on the Italian current legislation
- Focus on Medico-Legal and Ethical Topics in Surgery in Italy
- Iatrogenic splenic injury: review of the literature and medico-legal issues
- Focus on Medico-Legal and Ethical Topics in Surgery in Italy
- Donation of the body for scientific purposes in Italy: ethical and medico-legal considerations
- Focus on Medico-Legal and Ethical Topics in Surgery in Italy
- Cosmetic surgery: medicolegal considerations
- Focus on Medico-Legal and Ethical Topics in Surgery in Italy
- Voluntary termination of pregnancy (medical or surgical abortion): forensic medicine issues
- Review Article
- Role of Laparoscopic Splenectomy in Elderly Immune Thrombocytopenia
- Review Article
- Endoscopic diagnosis and treatment of neuroendocrine tumors of the digestive system
- Review Article
- Efficacy and safety of splenectomy in adult autoimmune hemolytic anemia
- Research Article
- Relationship between gastroesophageal reflux disease and Ph nose and salivary: proposal of a simple method outpatient in patients adults
- Case Report
- Idiopathic pleural panniculitis with recurrent pleural effusion not associated with Weber-Christian disease
- Research Article
- Morbid Obesity: treatment with Bioenterics Intragastric Balloon (BIB), psychological and nursing care: our experience
- Research Article
- Learning curve for endorectal ultrasound in young and elderly: lights and shades
- Case Report
- Uncommon primary hydatid cyst occupying the adrenal gland space, treated with laparoscopic surgical approach in an old patient
- Research Article
- Distraction techniques for face and smile aesthetic preventing ageing decay
- Research Article
- Preoperative high-intensity training in frail old patients undergoing pulmonary resection for NSCLC
- Review Article
- Descending necrotizing mediastinitis in the elderly patients
- Research Article
- Prophylactic GSV surgery in elderly candidates for hip or knee arthroplasty
- Research Article
- Diagnostic yield and safety of C-TBNA in elderly patients with lung cancer
- Research Article
- The learning curve of laparoscopic holecystectomy in general surgery resident training: old age of the patient may be a risk factor?
- Research Article
- Self-gripping mesh versus fibrin glue fixation in laparoscopic inguinal hernia repair: a randomized prospective clinical trial in young and elderly patients
- Research Article
- Anal sphincter dysfunction in multiple sclerosis: an observation manometric study


