Abstract
To the best of our knowledge, we report the first case of a successful antenatal intervention in a double twin reversed arterial perfusion (TRAP) sequence in a monoamniotic monochorial triplet pregnancy. After diagnosis during first-trimester ultrasound, fetoscopic coagulation and transection of the umbilical cords of both acardiac members was performed at 16 weeks of gestation. The immediate postoperative course was complicated with iatrogenic preterm premature rupture of membranes, which was successfully reversed with an amniopatch procedure. Consequent sonographic assessments showed a healthy fetus with normal growth and development, together with progressive atrophy of the acardiac fetuses. Owing to placental abruption, an urgent cesarean section was performed at 32 weeks. A baby girl of 1600 g was born in good general condition. Except for the butts of the transected umbilical cords, there were no remnants of the TRAP twins to be distinguished. After a neonatal follow up of 64 days, the baby girl could be discharged.
Introduction
Acardiac twinning or twin reversed arterial perfusion syndrome (TRAP) is the most extreme form of twin-to-twin transfusion syndrome and occurs in about 1 of 35,000 pregnancies. This aberrant pregnancy consists of at least one normal (pump) twin and one acardius. Left untreated, many possible complications are described, including heart failure, preterm premature rupture of membranes (PPROM), and intrauterine death of the pump twin.
To the best of our knowledge, this is the first case of a successful antenatal intervention in a double TRAP sequence. Although very little is known about possible fetal interventions, it can improve the outcome as described below. Thanks to the development and improvement of intrauterine interventions, we were able to successfully perform coagulation of both umbilical cords, thereby resulting in a live birth of a female infant.
Case report
A 27-year-old, gravida 2, para 1, first presented at the 8th week of a spontaneously conceived pregnancy. Her obstetric and medical history showed no complications. Detailed transvaginal ultrasound (US) at that time showed a fetus with normal growth. However, in the same gestational sac, a second poorly delineated mass with a single slowly beating heart (89/min) was seen (Figure 1). Differential diagnosis included a monochorionic monoamniotic (MCMA) TRAP sequence, conjoined twin, or dysmorphic fetus.
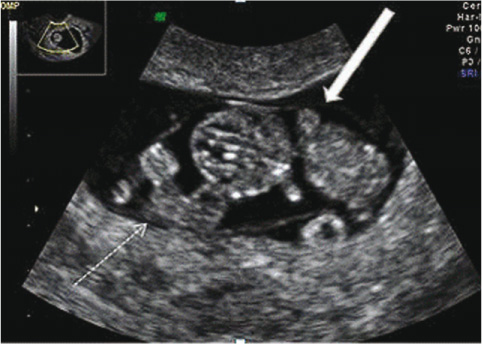
Detailed transvaginal US at 8 weeks of gestational age showed a fetus with normal growth and a second poorly delineated mass with a single slowly beating heart (89/min).
White dashed arrow, abnormal mass; white arrow: normal fetus.
First-trimester US at 11+5 weeks of gestational age showed a normal fetus (crown-rump length, 60 mm), with a nuchal translucency of 0.9 mm and the presence of a nasal bone, indicating a low risk for aneuploidy. Surprisingly, two additional dysmorphic masses were seen, suggesting a double TRAP sequence. One acardiacus consisted of a trunk and one limb with an irregular cardiac activity; the other mass was smaller with no recognizable shape and no cardiac activity.
Both acardiaca had a short individual cord connecting them to the common placenta with positive blood flow originating from the pump twin to the masses as confirmed by color Doppler. No dividing membrane between the healthy fetus nor the two masses could be observed. Follow-up US scan at 14+5 weeks of gestation revealed a further growth of the acardiac masses.
In view of the very unusual situation with a single pump twin, sustaining two growing masses, the parents chose early prenatal intervention. Laser coagulation with transection of the umbilical cords of both acardiaca was performed successfully at 15+6 weeks of gestation using a diode laser (D60 Multibeam Flexiplus, 20W; Dornier Medizintechnik, Wessling, Storz, Tuttlingen, Germany) in pulse and contact mode under direct fetoscopic view (7 French trocar and 1.3 mm fetoscope with 30.6 cm working length; Storz) (Figure 2). The procedure lasted for approximately 45 min and was performed under epidural anesthetics. Chromosomal studies performed on amniotic fluid revealed a normal female karyotype (46XX).
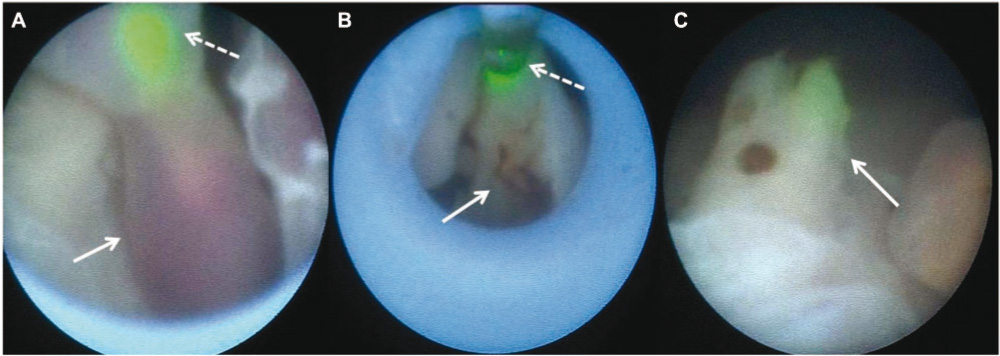
Fetoscopic view before, during, and after coagulation and transection of the umbilical cord using a diode laser.
White dashed arrows point to the green pilot light (A) and the laser fiber itself (B). White arrows show the umbilical cord of the acardiacus before (A), during (B), and after coagulation and transection (C).
Unfortunately, 24 h after the intervention, the patient developed an iatrogenic PPROM, which persisted, despite bed rest, reducing the amniotic fluid index (AFI). An amniopatch procedure was performed 4 days later. During this procedure, platelets and cryoprecipitate are injected in order to arrest the fluid leakage [4]. Weekly follow-up US showed normalization of the AFI and normal fetal growth (p10). At 25 weeks, a prophylactic course of betamethasone was administered in view of the high risk of premature delivery. Fetal growth and Doppler studies were reassuring. At 32 weeks, an urgent cesarean section needed to be done because of abruptio placentae. A girl of 1600 g was born in a good condition. Examination of the placenta showed the butts of the transected two cords, but no further remnants of the TRAP twins. The baby was observed in the neonatal intensive care unit for 64 days before being discharged in good general health.
Discussion and review
We present an MCMA triplet pregnancy, complicated by a double TRAP sequence. Left untreated, good outcomes have been described [2, 5, 7]. However, there is a mortality rate of 45% in triplet pregnancies, mainly due to congestive heart failure and polyhydramnion, leading to preterm delivery. Several possible fetal interventions have been described, including intervention on the umbilical cord (embolization, ligation, or laser coagulation), intrafetal ablation (chemosclerosis, laser coagulation, or radiofrequency ablation), and the older approach consisting of hysterotomy and selective delivery of the acardiac twin. (Table 1)
Outcome of five cases of treated triplet pregnancies complicated by TRAP sequence.
| First author | Number of acardiac members | Time at diagnosis (weeks) | Evolution | Treatment | Delivery (weeks, mode, and reason) | Outcome |
|---|---|---|---|---|---|---|
| Cavoretto et al. [1] | 1 | 11 | Growth of AC | LC of cord, 19 weeks | 35+1, SC due to abnormal Doppler findings | 2 healthy newborns, stillbirth of AC |
| Schild et al. [6] | 1 | 13 | Hydrops and cardiac failure of pump twin | Embolization anastomosis | 24+5, vaginal delivery | 1 surviving newborn, 1 newborn died, 1 stillbirth of AC |
| Sepulveda et al. [7] | 1 | 7 | Growth of AC | LC of interstitial vasculature, 17 weeks | 34, SC due to PL and BP | 2 healthy newborns, 1 remnant of AC |
| 1 | 16 | IUGR of pump twin | LC of interstitial vasculature, 17 weeks | 37, SC due to PL and BP | 1 healthy newborn, stillbirth pump twin, stillbirth of AC | |
| 1 | 23 | IUGR and MIU of pump twin | Amniodrainage | 32, SC due to PL | 1 healthy newborn, stillbirth of AC | |
| Holmes et al. [3] | 1 | – | Growth of AC | MC of intra abdominal vessels, 19 weeks | 38, – | 2 healthy newborns |
| Current case | 2 | 21 | Growth of 2 AC | LC and transection of cord, 15+6 weeks | 32, SC due to abruptio placentae | 1 healthy newborn, stillbirth of 2 AC |
Cavoretto et al. [1] performed an interstitial laser coagulation of a TRAP sequence within a dichorionic, triamniotic triplet at 19 weeks. Further pregnancy showed progressive atrophy of the acardiacus and normal development of the pump twin. Owing to abnormal Doppler findings, a cesarean section was carried out at 35+1 weeks of gestation. Two healthy twins were born. A follow-up at 9 months showed two children in good general condition.
Sepulveda et al. [7] presented five triplet pregnancies complicated by the presence of a single acardiac fetus. Two of the cases underwent a successful percutaneous intra-abdominal interstitial laser ablation of the umbilical cord. In a third case, amniodrainage, to reduce the risk of prematurity, was carried out.
Another method is monopolar coagulation of a major intra-abdominal vessel within the acardiacus. In the case of Holmes et al. [3], this led to the live birth of two healthy newborns at 38 weeks. Schild et al. [6] carried out an embolization of the anastomosis from the pump twin to the acardius using histoacryl, with arrest of blood flow in the umbilical artery after the second attempt. After premature labor at 24+5 weeks, two normal females and one acardiacus were born. Unfortunately, only one twin survived.
Triplets complicated by the presence of two acardiaca are even more exceptional. A previous case, presented by Ventura et al. [8], describes a monochorionic triamniotic triplet pregnancy compounded by a double TRAP sequence, diagnosed at 21 weeks of gestation. Except for a mild polyhydramnion, no other signs of cardiac failure were withheld. The parents renounced any intervention, and at 23+5 weeks of gestation the mother went into spontaneous labor. Ultrasound investigation at that time showed demise of the pump twin.
To our knowledge, this is the first case with successful treatment of a double TRAP sequence in a triplet pregnancy.
References
[1] Cavoretto C, Serafini A, Valsecchi L, Lanna M, Rustico MA. Early diagnosis, follow-up and prenatal treatment of a case of TRAP sequence occurring in a dichorionic triamniotic triplet pregnancy. J Clin Ultrasound. 2009;37:350–3.10.1002/jcu.20583Search in Google Scholar
[2] Dahiya P, Agarwal U, Sangwan K, Sen J. Antenatal diagnoses of twin-reversed arterial perfusion sequence (acardiac amorphous) in a triplet pregnancy: case report. Arch Gynecol Obstet. 2004;269:147–8.10.1007/s00404-002-0421-5Search in Google Scholar
[3] Holmes A, Jauniaux E, Rodeck C. Monopolar thermocoagulation in acardiac twinning. Br J Obstet Gynecol. 2001;108:1000–2.10.1016/S0306-5456(01)00234-0Search in Google Scholar
[4] Lewi L, Van Schoubroeck D, Van Ranst M, Bries G, Emonds M-P, Arabin B, et al. Successful patching of iatrogenic rupture of the fetal membranes. Placenta. 2004;25:352–6.10.1016/j.placenta.2003.09.003Search in Google Scholar
[5] Sanjaghsaz H, Bayram MO, Qureshi F. Twin reversed arterial perfusion sequence in conjoined, acardiac, acephalic twins associated with a normal triplet. A case report. J Reprod Med. 1998;43:1046–50.Search in Google Scholar
[6] Schild RL, Plath H, Födisch HJ, Bartmann P, Hansmann M. Triplet pregnancy with acardius acranius after preimplantation diagnosis. Fertil Steril. 1998;70:1167–8.10.1016/S0015-0282(98)00354-9Search in Google Scholar
[7] Sepulveda W, Wong AE, Bustos JC, Flores X, Alcalde JL. Acardiac fetus complicating a triplet pregnancy: management and outcome. Prenatal Diagn. 2009;29:794–9.10.1002/pd.2291Search in Google Scholar PubMed
[8] Ventura W, Nazario C, Ventura J. Triplet pregnancy complicated by two acardiac fetuses. Ultrasound Obstet Gynecol. 2011;38:362–3.10.1002/uog.9001Search in Google Scholar PubMed
-
The authors stated that there are no conflicts of interest regarding the publication of this article.
©2012 by Walter de Gruyter Berlin Boston
Articles in the same Issue
- Masthead
- Masthead
- Editorial
- Editorial
- Case reports – Obstetrics
- Sonographic presentations of uterine rupture following vaginal birth after cesarean – report of two cases 12 h apart
- Prenatal diagnosis of thrombocytopenia-absent radius syndrome
- Cervico-isthmic pregnancy with cervical placenta accreta
- Prelabor uterine rupture and extrusion of fetus with intact amniotic membranes: a case report
- Hyperreactio luteinalis in a spontaneously conceived pregnancy associated with polycystic ovarian syndrome and high levels of human chorionic gonadotropin
- Should clinicians advise terminating a pregnancy following the diagnosis of a serious fetal cardiac abnormality?
- Absence of hemolytic disease of fetus and newborn (HDFN) in a pregnancy with anti-Yka (York) red cell antibody
- Congenital midgut malrotation causing intestinal obstruction in midpregnancy managed by prolonged total parenteral nutrition: case report and review of the literature
- Skin popping scars – a telltale sign of past and present subcutaneous drug abuse
- Botulinum toxin for the treatment of achalasia in pregnancy
- Thrombotic stroke in association with ovarian hyperstimulation and early pregnancy rescued by thrombectomy
- Normal pregnancy outcome in a woman with chronic myeloid leukemia and epilepsy: a case report and review of the literature
- Three-dimensional power Doppler assessment of pelvic structures after unilateral uterine artery embolization for postpartum hemorrhage
- Deep congenital hemangioma: prenatal diagnosis and follow-up
- Case reports – Fetus
- Diagnosis of cleft lip-palate during nuchal translucency screening – case report and review of the literature
- Vein of Galen aneurysm that was diagnosed prenatally and supracardiac obstructed total anomalous pulmonary venous return with pulmonary hypertension: case report
- A fetus with 19q13.11 microdeletion presenting with intrauterine growth restriction and multiple cystic kidneya
- Prenatal detection of periventricular pseudocysts by ultrasound: diagnosis and outcome
- Twin-to-twin transfusion syndrome and limb ischemia: a case report
- Prenatal surgery in a triplet pregnancy complicated by a double twin reversed arterial perfusion (TRAP) sequence
- A case of a four-vessel umbilical cord: don’t stop counting at three!
- Case reports – Newborn
- Supratentorial hemorrhage suggested on susceptibility-weighted magnetic resonance imaging in an infant with hydranencephaly
- Differential diagnosis of pseudotrisomy 13 syndrome
- Carey-Fineman-Ziter syndrome: a spectrum of presentations
Articles in the same Issue
- Masthead
- Masthead
- Editorial
- Editorial
- Case reports – Obstetrics
- Sonographic presentations of uterine rupture following vaginal birth after cesarean – report of two cases 12 h apart
- Prenatal diagnosis of thrombocytopenia-absent radius syndrome
- Cervico-isthmic pregnancy with cervical placenta accreta
- Prelabor uterine rupture and extrusion of fetus with intact amniotic membranes: a case report
- Hyperreactio luteinalis in a spontaneously conceived pregnancy associated with polycystic ovarian syndrome and high levels of human chorionic gonadotropin
- Should clinicians advise terminating a pregnancy following the diagnosis of a serious fetal cardiac abnormality?
- Absence of hemolytic disease of fetus and newborn (HDFN) in a pregnancy with anti-Yka (York) red cell antibody
- Congenital midgut malrotation causing intestinal obstruction in midpregnancy managed by prolonged total parenteral nutrition: case report and review of the literature
- Skin popping scars – a telltale sign of past and present subcutaneous drug abuse
- Botulinum toxin for the treatment of achalasia in pregnancy
- Thrombotic stroke in association with ovarian hyperstimulation and early pregnancy rescued by thrombectomy
- Normal pregnancy outcome in a woman with chronic myeloid leukemia and epilepsy: a case report and review of the literature
- Three-dimensional power Doppler assessment of pelvic structures after unilateral uterine artery embolization for postpartum hemorrhage
- Deep congenital hemangioma: prenatal diagnosis and follow-up
- Case reports – Fetus
- Diagnosis of cleft lip-palate during nuchal translucency screening – case report and review of the literature
- Vein of Galen aneurysm that was diagnosed prenatally and supracardiac obstructed total anomalous pulmonary venous return with pulmonary hypertension: case report
- A fetus with 19q13.11 microdeletion presenting with intrauterine growth restriction and multiple cystic kidneya
- Prenatal detection of periventricular pseudocysts by ultrasound: diagnosis and outcome
- Twin-to-twin transfusion syndrome and limb ischemia: a case report
- Prenatal surgery in a triplet pregnancy complicated by a double twin reversed arterial perfusion (TRAP) sequence
- A case of a four-vessel umbilical cord: don’t stop counting at three!
- Case reports – Newborn
- Supratentorial hemorrhage suggested on susceptibility-weighted magnetic resonance imaging in an infant with hydranencephaly
- Differential diagnosis of pseudotrisomy 13 syndrome
- Carey-Fineman-Ziter syndrome: a spectrum of presentations

