Abstract
Carey-Fineman-Ziter syndrome is characterized by facial diplegia with an ophthalmoplegia comprising the Moebius sequence, Pierre Robin sequence with micrognathia, short stature, postnatal-onset microcephaly, hypotonia and muscular hypoplasia, extensive brainstem involvement, and pontine hypoplasia. We report a 38-week-gestation infant with features consistent with Carey-Fineman-Ziter syndrome but with phenotypical features that have not previously been described. The infant had severe hypoplasia of the pons and cerebellum, seizures, hypotonia, ophthalmoplegia, downslanting palpebral fissures, tongue hypoplasia, micrognathia, and facial diplegia. The karyotype was normal. Of note, there was a focal contour abnormality in the anterior two-thirds of the tongue, which necessitated tracheostomy on the third day of life to maintain the airway, and a well-circumscribed mass on both sides of the chest. These features have not been previously found to be associated with this syndrome, and the clinical significance is unknown. Case reports of rare disorders give significant information on the diagnosis, description, and evolving phenotype of rare syndromes.
Introduction
Carey-Fineman-Ziter syndrome is a rare syndrome initially described in 1982 [1]. It is characterized by facial diplegia with an ophthalmoplegia comprising the Moebius sequence, facial anomalies, the Pierre Robin sequence with micrognathia, short stature, postnatal-onset microcephaly, hypotonia and muscular hypoplasia, failure to thrive, and delayed motor milestones. Other reports have described similar characteristics and also relative macrocephaly and downslanting palpebral fissures [2, 5, 6]. Later reports describe extensive brainstem involvement and pontine hypoplasia [4]. Ryan et al. [5] described a case with scoliosis, talipes equinovarus, and non-specific primary myopathy as part of the syndrome. Dufke et al. [3] reported similar features associated with intermittent episodes of hypertension of unknown origin, Poland sequence (unilateral aplasia of the pectoralis muscle), and laryngostenosis. We describe additional features not previously described, which may suggest that this syndrome manifests as a spectrum of presentations.
Clinical report
The female infant was born at 38 weeks’ gestation by emergency cesarean section due to fetal distress, presence of meconium liquor, and antepartum hemorrhage. She was born with Apgars of 4 at 1 min and 9 at 5 min. The birth weight was 3080 g (45th centile), length was 49 cm (40th centile), and head circumference was 33 cm (20th centile). The mother was gravida 5, para 3, with a history of significant alcohol ingestion in the first trimester and a previous pregnancy complicated by an anencephalic fetus. Maternal serology was unremarkable, except for a history of Candida and Trichomonas. An ultrasound at 30 weeks found no gross fetal abnormalities and normal liquor volume.
Clinically, the infant was found to have Moebius sequence (ophthalmoplegia, facial diplegia, downward-slanting palpebral fissures) and Pierre Robin sequence (micrognathia, small mouth opening). In addition to these features, she also had a globular mass at the back of the tongue, fusion of the anterior margins of the tongue, gum comprising the floor of the mouth, and subcutaneous rubbery lesions (2.3×1.8 cm) below the left nipple.
Soon after birth, she developed respiratory distress requiring continuous positive airway pressure. She later had significant apnoeic and cyanotic episodes necessitating intubation. However, due to the lump at the back of her throat and recurrent upper airway obstruction, she required a tracheostomy on day 3 of life to maintain her airway.
She was also found to be hypotonic, with periodic jerking and stiffening of limbs, and with subclinical seizures on amplitude-integrated electroencephalography requiring treatment with phenobarbitone. She had a gag but no swallow or cough reflex, and was on gavage feeding. Magnetic resonance imaging revealed severe hypoplasia of the pons and cerebellum. The cerebrum was described to have normal sulcation with prominence of sulcal spaces suggestive of mild cerebral shrinkage (Figure 1). There was micrognathia with microglossia and an abnormal contour of the anterior two-thirds of the tongue, which may represent a dysplastic mass lesion (Figure 2). There was a well-circumscribed lesion on both sides of the anterior chest, which may be either mammary tissue or soft tissue lesions of indeterminate etiology. Chromosome analysis and fluorescence in situ hybridization showed a normal female karyotype, and no other abnormalities were detected (Figures 3–5). A microarray comparative genomic hybridization was not performed, as this was not widely available at the time of this case.

MRI demonstrating cerebellar and pontine hypoplasia.
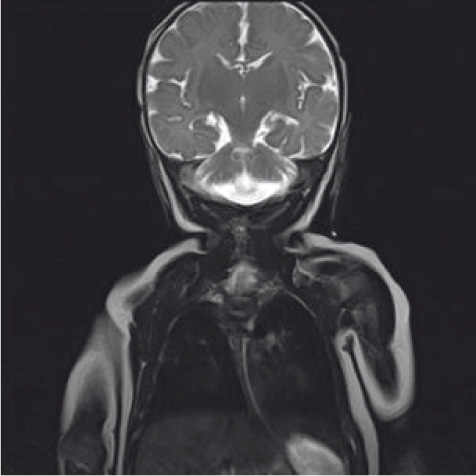
MRI head demonstrating cerebellar and pontine hypoplasia.

MRI demonstrating chest wall lesion

MRI demonstrating tongue abnormalities.

Photograph demonstrating tongue anomaly and micronathia.
Despite having a tracheostomy, she had severe hypoventilation with persistent apnoeic episodes requiring resuscitation. Owing to severe neurologic impairment and lack of progress, it was decided to suspend intensive care, and she died on day 25 of life. A postmortem was not performed.
Discussion
Carey-Fineman-Ziter syndrome has been described in the literature with a spectrum of presentations, which mainly include the Moebius sequence and the Pierre Robin sequence [1–6]. There have also been reports of brain abnormalities [4], and consistent with this, we report an infant with severe hypoplasia of the pons and the cerebellum. In addition to these features, our patient had new features not previously reported. There was a focal contour abnormality in the anterior two-thirds of the tongue necessitating tracheostomy early in life to maintain airway. We hypothesize that the tongue mass may be a variation in the manifestations of the Pierre Robin sequence. There was also a well-circumscribed lesion on both sides of the anterior chest, not previously reported with this syndrome. These may be mammary tissue or a soft tissue lesion, the significance and etiology of which is unknown. It can be postulated that this is a manifestation of the musculoskeletal involvement previously described in this syndrome.
There are still no known genetic testing or laboratory tests specific for Carey-Fineman-Ziter syndrome, and muscle biopsy of previous cases revealed mild non-specific myopathic changes [1–3, 6]. Inheritance is believed to be autosomal recessive, as sibling pairs have been reported in the literature [1, 2, 5, 7]. On the basis of previous findings in the literature, the major criteria for Carey-Fineman-Ziter syndrome include the Moebius and Robin sequences, hypotonia, facial anomalies, congenital non-progressive myopathy, and delayed motor development [3]. These features were present in our patient, although myopathy and motor development was not possible to determine, as our patient did not survive. In addition to this, we report an abnormal contour of the tongue and masses on both sides of the chest, a feature not previously associated with this syndrome.
The original siblings reported by Carey et al. [1, 2] who survived to adulthood had, in contrast to our case, normal computed tomography head scans and did not require mechanical ventilation. Their conditions were significantly different and quality of life was better achieved. Verloes and colleagues [7] reviewed nine unrelated cases of which two patients had severe hypoventilation and severe brainstem abnormalities and both did not survive.
For rare syndromes, reports of individual clinical cases may offer vital information in defining the spectrum of a specific clinical entity. It may be that this syndrome involves a spectrum of abnormalities and phenotypes that will become more apparent over time as more cases are reported.
Received May 7, 2012. Accepted October 15, 2012. Previously published online November 19, 2012.
References
[1] Carey JC. The Carey-Fineman-Ziter syndrome: follow-up of the original siblings and comments on pathogenesis (Editorial Comment). Am J Med Genet. 2004;127A:294–7.10.1002/ajmg.a.20689Suche in Google Scholar
[2] Carey JC, Fineman RM, Ziter FA. The Robin sequence as a consequence of malformation, dysplasia and neuromuscular syndromes. J Pediatr. 1982;101:858–68.10.1016/S0022-3476(82)80348-XSuche in Google Scholar
[3] Dufke A, Riethmuller J, Enders H. Severe congenital myopathy with Mobius, Robin and Poland sequences: new aspects of the Carey-Fineman-Ziter syndrome. Am J Med Genet. 2004;127A:291–3.10.1002/ajmg.a.20686Suche in Google Scholar
[4] Maheshwari A, Calhoun DA, Lacson A, Pereda L, Nelson RM, Saste MD, et al. Pontine hypoplasia in Carey-Fineman-Ziter (CFZ) syndrome. Am J Med Genet. 2004;127A:288–90.10.1002/ajmg.a.20688Suche in Google Scholar
[5] Ryan A, Marshall T, FitzPatrick DR. Carey-Fineman-Ziter (CFZ) syndrome: report on affected sibs. Am J Med Genet. 1999;82:110–3.10.1002/(SICI)1096-8628(19990115)82:2<110::AID-AJMG2>3.0.CO;2-OSuche in Google Scholar
[6] Schimke RN, Collins DL, Hiebert JM. Congenital nonprogressive myopathy with Mobius and Robin sequence – the Carey-Fineman-Ziter syndrome: a confirmatory report. Am J Med Genet. 1993;46:721–3.10.1002/ajmg.1320460625Suche in Google Scholar
[7] Verloes A, Bitoun P, Heuskin A, Amrom D, Van de Broeck H, Nikkel SM, et al. Mobius sequence, Robin complex and hypotonia: severe expression of brainstem disruption spectrum versus Carey-Fineman- Ziter syndrome. Am J Med Genet. 2004;127A: 277–87.10.1002/ajmg.a.20687Suche in Google Scholar
-
The authors stated that there are no conflicts of interest regarding the publication of this article.
©2012 by Walter de Gruyter Berlin Boston
Artikel in diesem Heft
- Masthead
- Masthead
- Editorial
- Editorial
- Case reports – Obstetrics
- Sonographic presentations of uterine rupture following vaginal birth after cesarean – report of two cases 12 h apart
- Prenatal diagnosis of thrombocytopenia-absent radius syndrome
- Cervico-isthmic pregnancy with cervical placenta accreta
- Prelabor uterine rupture and extrusion of fetus with intact amniotic membranes: a case report
- Hyperreactio luteinalis in a spontaneously conceived pregnancy associated with polycystic ovarian syndrome and high levels of human chorionic gonadotropin
- Should clinicians advise terminating a pregnancy following the diagnosis of a serious fetal cardiac abnormality?
- Absence of hemolytic disease of fetus and newborn (HDFN) in a pregnancy with anti-Yka (York) red cell antibody
- Congenital midgut malrotation causing intestinal obstruction in midpregnancy managed by prolonged total parenteral nutrition: case report and review of the literature
- Skin popping scars – a telltale sign of past and present subcutaneous drug abuse
- Botulinum toxin for the treatment of achalasia in pregnancy
- Thrombotic stroke in association with ovarian hyperstimulation and early pregnancy rescued by thrombectomy
- Normal pregnancy outcome in a woman with chronic myeloid leukemia and epilepsy: a case report and review of the literature
- Three-dimensional power Doppler assessment of pelvic structures after unilateral uterine artery embolization for postpartum hemorrhage
- Deep congenital hemangioma: prenatal diagnosis and follow-up
- Case reports – Fetus
- Diagnosis of cleft lip-palate during nuchal translucency screening – case report and review of the literature
- Vein of Galen aneurysm that was diagnosed prenatally and supracardiac obstructed total anomalous pulmonary venous return with pulmonary hypertension: case report
- A fetus with 19q13.11 microdeletion presenting with intrauterine growth restriction and multiple cystic kidneya
- Prenatal detection of periventricular pseudocysts by ultrasound: diagnosis and outcome
- Twin-to-twin transfusion syndrome and limb ischemia: a case report
- Prenatal surgery in a triplet pregnancy complicated by a double twin reversed arterial perfusion (TRAP) sequence
- A case of a four-vessel umbilical cord: don’t stop counting at three!
- Case reports – Newborn
- Supratentorial hemorrhage suggested on susceptibility-weighted magnetic resonance imaging in an infant with hydranencephaly
- Differential diagnosis of pseudotrisomy 13 syndrome
- Carey-Fineman-Ziter syndrome: a spectrum of presentations
Artikel in diesem Heft
- Masthead
- Masthead
- Editorial
- Editorial
- Case reports – Obstetrics
- Sonographic presentations of uterine rupture following vaginal birth after cesarean – report of two cases 12 h apart
- Prenatal diagnosis of thrombocytopenia-absent radius syndrome
- Cervico-isthmic pregnancy with cervical placenta accreta
- Prelabor uterine rupture and extrusion of fetus with intact amniotic membranes: a case report
- Hyperreactio luteinalis in a spontaneously conceived pregnancy associated with polycystic ovarian syndrome and high levels of human chorionic gonadotropin
- Should clinicians advise terminating a pregnancy following the diagnosis of a serious fetal cardiac abnormality?
- Absence of hemolytic disease of fetus and newborn (HDFN) in a pregnancy with anti-Yka (York) red cell antibody
- Congenital midgut malrotation causing intestinal obstruction in midpregnancy managed by prolonged total parenteral nutrition: case report and review of the literature
- Skin popping scars – a telltale sign of past and present subcutaneous drug abuse
- Botulinum toxin for the treatment of achalasia in pregnancy
- Thrombotic stroke in association with ovarian hyperstimulation and early pregnancy rescued by thrombectomy
- Normal pregnancy outcome in a woman with chronic myeloid leukemia and epilepsy: a case report and review of the literature
- Three-dimensional power Doppler assessment of pelvic structures after unilateral uterine artery embolization for postpartum hemorrhage
- Deep congenital hemangioma: prenatal diagnosis and follow-up
- Case reports – Fetus
- Diagnosis of cleft lip-palate during nuchal translucency screening – case report and review of the literature
- Vein of Galen aneurysm that was diagnosed prenatally and supracardiac obstructed total anomalous pulmonary venous return with pulmonary hypertension: case report
- A fetus with 19q13.11 microdeletion presenting with intrauterine growth restriction and multiple cystic kidneya
- Prenatal detection of periventricular pseudocysts by ultrasound: diagnosis and outcome
- Twin-to-twin transfusion syndrome and limb ischemia: a case report
- Prenatal surgery in a triplet pregnancy complicated by a double twin reversed arterial perfusion (TRAP) sequence
- A case of a four-vessel umbilical cord: don’t stop counting at three!
- Case reports – Newborn
- Supratentorial hemorrhage suggested on susceptibility-weighted magnetic resonance imaging in an infant with hydranencephaly
- Differential diagnosis of pseudotrisomy 13 syndrome
- Carey-Fineman-Ziter syndrome: a spectrum of presentations

