Abstract
Background and aims
Pain management for hospital inpatients remains suboptimal. Previously identified barriers to optimal pain management include staff communication difficulties, confusion around pain management roles and a lack of suitable resources for clinical staff. The emotional, relational and contextual complexities of gastrointestinal (GI) pain create particular challenges for frontline clinical staff attempting to implement a biopsychosocial approach to its management. The current study took place over 2 years, comprised an ethnographic and a feedback phase, and aimed to examine pain management processes with clinical staff in order to generate hypotheses and initiatives for improvement. This paper focuses on two overarching themes identified in the ethnographic phase of the study, centred on the neglected role of both staff and patient distress in GI pain management.
Methods
Grounded theory and thematic analysis methods were used as part of action research, which involves collaborative working with clinical staff. The study took place on a 60 bed GI ward in a university hospital in London. Participants were clinical staff who were either ward-based or involved in the care of particular patients. This latter group included doctors, nurses, psychologists and physiotherapists from the Acute and Complex Pain Teams. Qualitative data on pain management processes was gathered from staff interviews, consultation groups, and observations of patient-staff interactions. Recruitment was purposive and collaborative in that early participants suggested targets and staff groups for subsequent enquiry. Following the identification of initial ethnographic themes, further analysis and the use of existing literature led to the identification of two overarching pain management processes. As such the results are divided into three sections: (i) illustration of initial ethnographic themes, (ii) summary of relevant theory used, (iii) exploration of hypothesised overarching processes.
Results
Initially, two consultation groups, five nursing staff and five junior doctors, provided key issues that were included in subsequent interviews (n=18) and observations (n=5). Initial ethnographic themes were divided into challenges and resources, reflecting the emergent structure of interviews and observations. Drawing on attachment, psychodynamic and evolutionary theories, themes were then regrouped around two overarching processes, centred on the neglected role of distress in pain management. The first process elucidates the lack of recognition during pain assessment of the emotional impact of patient distress on staff decision-making and pain management practice. The second process demonstrates that, as a consequence of resultant staff distress, communication between staff groups was fraught and resources, such as expert team referral and pharmacotherapy, appeared to function, at times, to protect staff rather than to help patients. Interpersonal skills used by staff to relieve patient distress were largely outside systems for pain care.
Conclusions
Findings suggest that identified “barriers” to optimal pain management likely serve an important defensive function for staff and organisations.
Implications
Unless the impact of patient distress on staff is recognised and addressed within the system, these barriers will persist.
1 Introduction
Despite extensive research and clinical attention, pain management remains suboptimal in hospital settings [1], including the hospital in the current study [2], leading to increased costs, longer stays and patient dissatisfaction [3].
Though a biopsychosocial approach to pain management, particularly with gastrointestinal (GI) pain, is widely advocated [4], there is little consideration of how receptive to psychosocial aspects of pain frontline nursing and medical staff can be. Staff may experience a lack of clarity around pain management roles [5], with poor levels of staff support [6] and a tendency to rely on subjective estimates of patients’ pain rather than patient self-report, the primary indicator [7].
GI disorders can involve pain that is influenced significantly by only partially understood contextual, relational and psychological stressors and by processes of central sensitisation along the brain-gut axis [8]. Recognising the influence of such stressors on pain is challenging in hospital settings, where detachment from emotion can become the norm [9].
We aimed to investigate the ongoing problem of suboptimal GI pain management using an action research approach – comprising collaboration with clinical staff, thematic analysis and grounded theory methods – undertaken over 2 years on a large GI ward at a university hospital. This paper explores two overarching processes, identified in the ethnographic phase of the study, centred on the neglect of distress in GI pain management.
Although emotion is by definition an essential part of pain (“an unpleasant, sensory and emotional experience” [10]), “distress” is used here to refer more broadly to “unpleasant emotional experience of a psychological, social and/or spiritual nature which extends on a continuum from normal feelings of vulnerability, sadness and fears to disabling problems such as depression, anxiety, panic, social isolation and spiritual crisis” [11]. We take the position that while only the patient experiences sensory aspects of pain, both patient and clinician can experience the distress of pain.
2 Methods
2.1 Design
Qualitative methods were chosen because new hypotheses and directions for experimental intervention were sought. Action research involves collaboration of staff and researchers and is particularly suited to identifying problems and solutions in clinical practice [12], including pain management [13]. Broadly, it comprises an ethnographic phase, involving collaborative planning and fact finding, followed by the implementation of a plan generated from analysis, and further fact finding to evaluate the results of the action [12]. This paper will focus on the findings from the ethnographic phase of the study, involving staff consultation groups, followed by staff-patient observations and semi-structured interviews with staff. A feedback phase, reported elsewhere [14], involved disseminating data from the ethnographic phase to staff groups in a manner that provided a reflective space and promoted ownership of findings and flexibility in discussion of desirable changes in practice [12].
2.2 Sample
The study took place in a university hospital on a 60 bed GI ward with acute and chronic, pre-surgical, post-surgical and non-surgical patients. Participants were clinical staff who were either ward-based or involved in the care of particular patients. This latter group included doctors, nurses, psychologists and physiotherapists from the Acute and Complex Pain Teams. The Acute Team was primarily involved with post-surgical pain, and the Complex Pain Team was a recent initiative to improve pain management across the hospital. Recruitment was purposive and informed by principles of grounded theory in that initial participants and data analysis suggested subsequent targets of inquiry [15], [16]. The number of participants, along with termination of data collection and analysis, was informed by “saturation”: for themes when no new challenges or resources were raised in interviews, and for participants when all staff groups clinically affiliated to the ward had been approached.
2.3 Analysis
Interviews (maximum length 45 min) were audio-recorded and transcribed verbatim. Observations involved shadowing staff on an hourly basis or for the duration of a ward event. Notes were pooled with interview transcripts for analysis. A thematic analysis of the ethnographic data was guided by the stages outlined by Braun and Clarke [15], as shown in the left-hand column of Fig. 1.
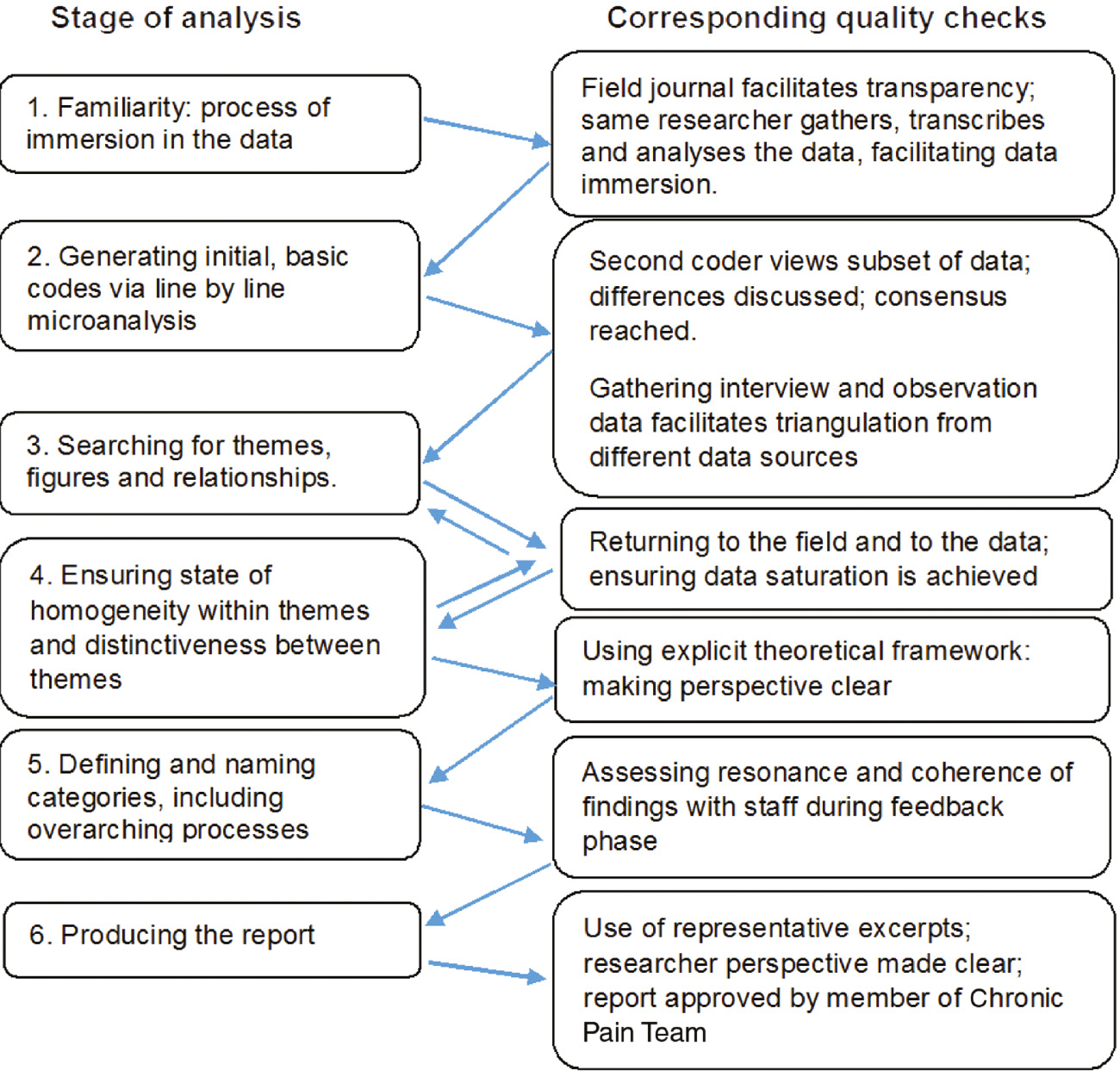
Stages of analysis and quality check diagram.
Simultaneously, ongoing data collection was guided by principles from grounded theory so that “design-like concepts” were developed during data gathering [16] and ongoing data analysis shaped the interview schedule. Subsequently, relevant literature was used to compare data against existing theory and generate hypotheses [15], [16]. The ethnographic results are divided into three sections:
Illustration of initial ethnographic themes
Summary of relevant theory used
Exploration of hypothesised overarching processes
2.4 Quality assurance
Quality principles [17] were utilised at each stage of the study, as shown in the right-hand column of Fig. 1. A consolidated criteria for reporting qualitative research (COREQ) checklist is included in Supplementary Materials.
3 Results
Table 1 shows staff involvement in different aspects of the study. Initially, two consultation groups, five nursing staff and five junior doctors, provided key issues that were included in subsequent interviews (n=18) and observations (n=5).
Staff involved in different aspects of the study.
| Staff group | Consultation | Interview | Observation |
|---|---|---|---|
| Consultant Gastroenterologist | 1 | 1 | 2 (2)a |
| Head Nurse | 1 | 1 (1) | |
| Nurse | 4 | 4 (4) | 1 |
| Nursing Assistant | 1 | 2 (1) | 1 |
| Junior Doctor | 5 | 3 (3) | 3 |
| Pharmacist | 1 | ||
| Specialist Nurse, Pain Teams | 1 | 2 (1) | |
| Project Manager, Complex Pain Team | 1 | ||
| Consultant Anaesthetist, Acute and Complex Pain Teams | 3 | ||
| Clinical Psychologist, Complex Pain Team | 1 | ||
| Totals | 12 | 18 | 9 (5b) |
-
a(n)=number of new staff, i.e. not involved in any previous stage, b(n)=total number of episodes of observation, i.e. nine staff were observed but some were observed in pairs.
3.1 Ethnographic findings
Illustration of initial ethnographic themes
As shown in Fig. 2, themes were initially divided into challenges and resources, reflecting the emergent structure of interviews and observations.
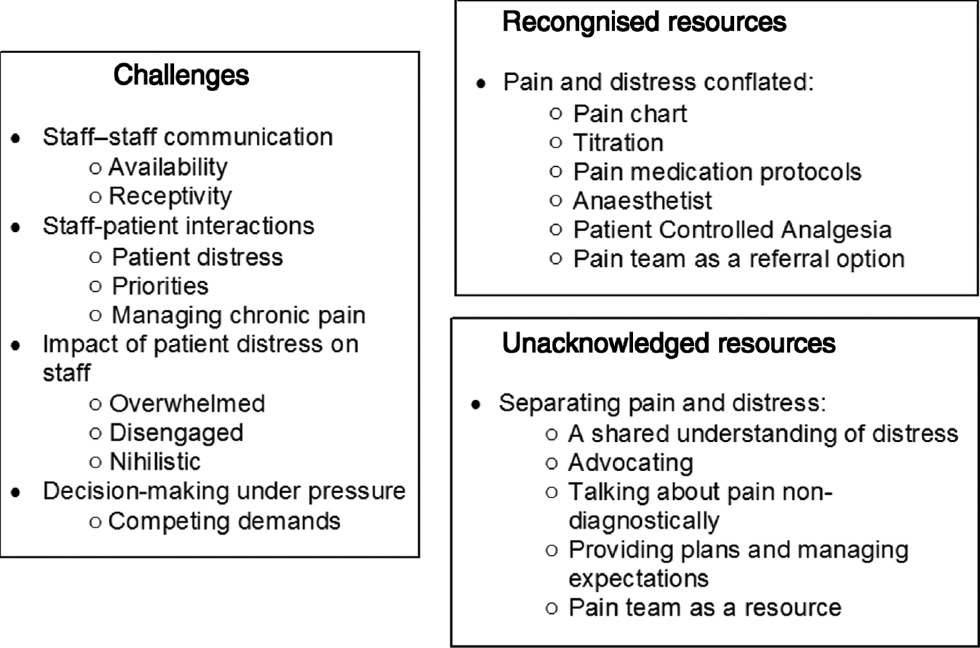 Fig. 2:
Fig. 2:Ethnographic themes: challenges and resources in GI pain management.
Researcher perspective: summary of relevant theory used
The framework for identifying overarching pain management processes from the ethnographic themes is grounded in evidence-based attachment [18], psychodynamic [19] and evolutionary [20] theories, according to which the experience of pain is fundamentally relational, affecting both parties, and beginning in the infant-caregiver relationship. In a seminal study applying such thinking to healthcare settings [21], the defensive processes observed in nurse-patient interactions – depersonalising the patient, blurring roles, avoiding accountability and weakening the bond between clinician and patient by breaking up tasks and introducing ritualistic task completion – closely parallel the observations in the current study and have recently been revisited in contemporary nursing and healthcare, with a focus on managing interpersonal distress and staff burnout [22].
Exploration of hypothesised overarching processes
Below, ethnographic themes (italics) are regrouped around two overarching processes. Process 1 posits that a central reason for the challenges in pain management was the unacknowledged impact of patient distress on staff. Process 2 posits that because of subsequent staff distress, resources were used in a defensive way, both individually and institutionally in pain management protocols. The two processes, summarised in Fig. 3, also roughly correspond to a typical pain management journey on the ward.
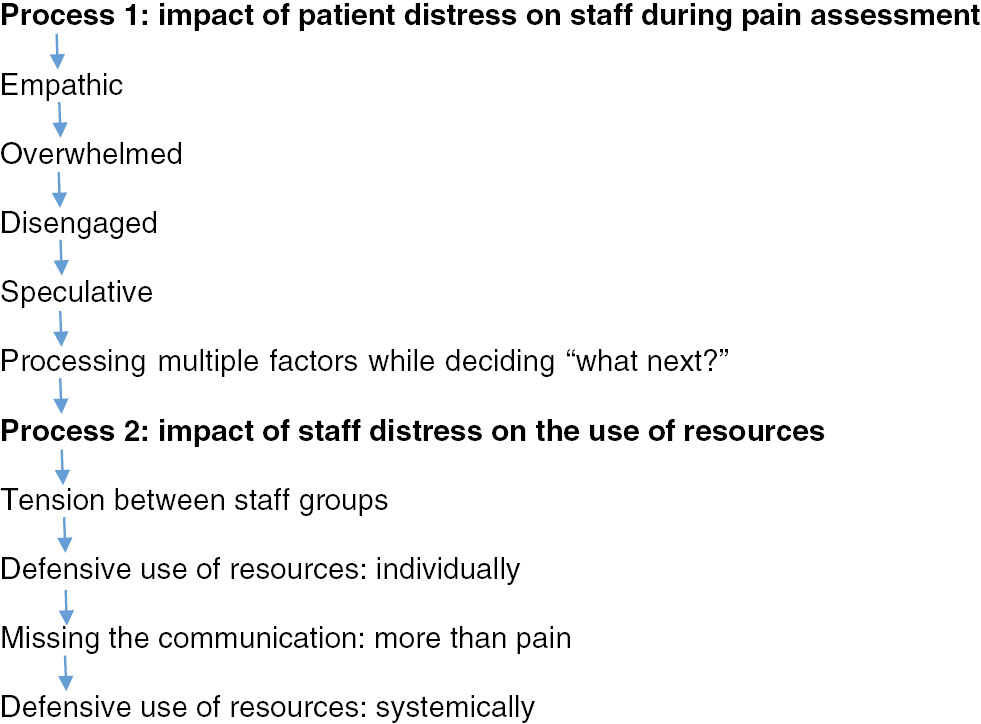 Fig. 3:
Fig. 3:Flowchart of overarching processes in GI pain management.
3.2 Process 1: the impact of patient distress on staff during pain assessment
For many patients, protocol-based pain management interventions met most of their pain-related needs. Other patients, including many with chronic pain that was poorly relieved by analgesics, experienced prolonged, difficult to treat or intense distress. A salient starting point to explore this issue was when patient distress was communicated to staff on the ward. The recipient of the communication was most often the nurse or nursing assistant assigned to that particular patient, leading to various responses:
3.2.1 Empathic
At manageable levels, the communication of distress affected staff members in a way that elicited a compassionate response:
Interviewee (I) 5…I feel very sorry, imagine, it must be very hard for a lot of these patients to accept that this [pain] will be there for a long time.
3.2.2 Overwhelmed
But as distress became harder to bear for the patient, the clinician too became more distressed:
I5: You are holding their hand, you are saying “I am doing my best…I’ll call the anesthetist because the doctor doesn’t know what to do anymore”.
Unlike the rational framework of pain relief intervention, such as the WHO pain ladder, nurses described the uncontained emotional impact of patients’ communications of distress, not only acutely but also longer term. Staff felt overwhelmed, and concerned with potential adverse effects on their health:
I8: I’m a firm person…I learn to take blows from [patients]…and I always say to the nurses “just ignore them they’re in pain”… but I’ve seen many nurses and managers break, literally tears.
Several nursing staff said they thought this pressure led to high turnover and staff sickness on the ward.
3.2.3 Disengaged
In order to cope with the pressure of patient demands and a sense of hopelessness, frontline staff distanced themselves from patients at the expense of the therapeutic relationship. Junior doctors described a tendency to become disengaged in response to ongoing patient distress:
Consultation Group (CG) 2: other people might think it but not say it: the patients who are quite demanding in terms of pain management, I think you almost become hardened to it…you pull away from having sympathy.
Among junior doctors, disengagement was also closely related to a sense of therapeutic nihilism:
CG2: You almost become dissociated from what they’re saying and just accept that…you can’t really improve that situation.
3.2.4 Speculative
Staff felt the burden most when managing chronic GI pain. Several senior clinicians explained how judgements could arise:
I16: Unless you are well-informed as a member of staff, you tend to think “these are both patients with pain side by side, yet you’re a good person because you’re responding to your oral morphine, you’re a bad person because you say you’re not”.
Nurses speculated about possible personal factors, including opioid dependence that might contribute to distress in such patients, and complicate pain assessment:
I3: If [patients are] tossing and turning, you can tell, but if they’re asleep and it’s 4 am and [gestures waking up]: “I need my pain relief” and then they’re asleep again…that feels like something different.
3.2.5 Processing multiple factors while deciding “what next?”
Thus, when attempting to consider pain management options, members of staff were simultaneously processing a range of powerful feelings and judgements elicited by the patient that would affect their decision-making but were not explicit in the pain assessment process. They were also simultaneously attempting to meet many competing demands:
I3: When there are a hundred people calling for different things; there might be a critical patient, [the on-call doctor] might be stuck with that patient; you’re calling for pain relief for your patient.
And, with chronic pain patients particularly, balancing their own authority against patient experience:
CG2: The patients have an extensive knowledge of these drugs and you don’t know all the drugs they’ve tried…So there’s trying to unscramble all of that while trying to deal with their pain in the moment.
3.3 Process 2: the impact of staff distress on the use of resources
The defensive tendency to disengage from patients, described above, clearly impacted on a key pain management resource: the therapeutic relationship. We posit that similar defensive tendencies and attempts to avoid becoming incapacitated by distress affected the use of other pain management resources, including communication between staff groups.
3.3.1 Tension between staff groups
Attempts to protect against distress caused a lack of receptivity and tension between staff groups:
CG2: There’s definitely tension if you try and discuss with the [pain team nurses]. They are under so much pressure – “you really don’t need to be ringing me now”.
Limited availability was also acknowledged by a consultant anesthetist who worked in the Acute and Complex Pain Teams:
I12: I don’t think that the pain team are often as approachable as they can be. So there’s a little barrier to any phone call or request…if you feel like you’re going to get told off or slightly have a negative reaction…[I] think it discourages the nurses to refer.
3.3.2 Defensive use of resources: at an individual level
Staff discussed a wide range of acknowledged resources, as shown in Fig. 2. However, the interpersonal climate in which these resources were used – that is, in the context of all parties wanting to avoid becoming flooded by distress – was unacknowledged. By not distinguishing patient distress from patient pain or from the clinicians’ own distress during assessment, distress was effectively subsumed under pain. This meant that staff had something tangible in the form of pharmacopoeia or expert referral to offer the patient without having to explore his or her needs further, even if the resource offered was in part to relieve the emotional discomfort of the staff member.
When interviewee 3, above, “calls for pain relief”, she is also requesting relief for herself; searching for someone with whom to share the burden, or to whom to transfer it. This was also recognised by junior doctors. Below, a registrar describes how the pain team was used as a defence for the staff member rather than a resource for the patient:
I10: If it’s the weekend when you see lots of patients and you’re in a rush…if the patient’s complaining of pain, I’ll say “oh, we’ll get the pain team to see you”, knowing full well there isn’t a specific pain team [at weekends] and it’s more of a “push the issue to the side”.
3.3.3 Missing the communication: more than pain
The subsuming of distress under pain meant that aspects of distress for which pharmacological intervention was inappropriate, including beliefs about pain; anxiety or anger about pain or about pain relief, or the experience of being in hospital, away from familiar support and routine, were largely unrecorded and unaddressed. While an assessment of these biopsychosocial factors was not often observed in staff-patient interactions, during interviews several staff members did appreciate their importance:
I17: patients are scared, have lost control and feel disempowered.
I15 In my experience, uncertainty adds to the overall distress and if the situation can be rationalised, some relief can be provided on top of medication.
For chronic GI pain patients in particular, complex situational, emotional and relational factors, including not feeling believed, intensified distress. This made communication with staff more fraught, increasing the likelihood of pharmacotherapy but not its effectiveness.
3.3.4 Defensive use of resources: at a systemic level
As is evident in the comments of interviewees 15 and 17, above, in no way were all staff unaware of patient distress and its complexities. A head nurse described the disjunction between recognising the value of understanding a patient’s experience of distress yet having to rely on pharmacological resources:
I6: You know how [the patient’s] pain is managed, you know how it works, you know how it functions for her…because you know them so well, but… “pain is what the patient says it is” and…we can only use the resources we have, and the only resource we have is the pain team, and then they’ve got other resources like they could then take a patient down and do a [local anaesthetic] infusion.
This nurse had an understanding not just of pain physiology but of “how it functions” for the patient. No routine resources were available to address this understanding of the pain problem. Instead, adhering to the mantra “pain is what the patient says it is” meant that clinical expertise and the pharmacopoeia constituted the sole resource. Despite being receptive to patient distress, this nurse was reliant on a system within which pain and distress were conflated.
Many staff described listening to, calming, advocating for and planning with patients. Here, a nurse described taking time to listen before reacting with protocol-based interventions:
I5: It is very important for [patients] that you take on board what they are saying to you and their feelings are important to you as a nurse… sometimes the patient is just anxious…you say “Do you need me to talk to you? Is it anxiety? Is it physical pain or is it more than that?”
These relational responses to distressed patients made patients’ experiences of pain more tolerable but were not included in accounts of existing pain management resources by nursing staff or, crucially, by senior staff and head nurses; nor were they recorded in nursing notes as interventions. They were unacknowledged resources; tasks that staff performed outside recognised pain management procedures.
The hospital/ward as an institution did not allot time to these resources. Many nurses expressed their frustration that they had very little time to talk to patients: they had so many other competing demands that talking was not seen as a productive way to spend time. Further, the impact of such interactions on staff, particularly on the most empathic staff members, was unacknowledged. There was no mention in interviews of supportive spaces for staff, nor appropriate training to make sense of patient distress. Consequently, the impact of patient distress on staff and their pain management decisions was made invisible.
4 Discussion
This action research study identified a rich overarching thematic framework centred on the neglected role of patient and staff distress in GI pain management. Shortcomings in staff-staff and staff-patient communication and a lack of suitable pain management resources recall the barriers identified in previous research [5], [6], [7]. Going beyond this, we posit that the unacknowledged impact of patient distress on staff is a key reason for repeated findings of suboptimal pain management and for the difficulty in implementing a biopsychosocial approach to treatment.
All staff groups in the current study discussed the impact of patient distress and their attempts to avoid becoming overwhelmed by it. These attempts negatively affected communication between staff members and interactions between staff and patients so that, at times, the function of pharmacological interventions or promises of referrals to specialist teams appeared to be primarily to protect staff members from becoming overwhelmed and, only secondarily, to help patients. Further, this function had become thoroughly institutionalised so that much of nurses’ working time was dominated by checklists and protocols introduced ostensibly to ensure optimum patient care but at the same time reducing time with patients.
Diverse evidence-based theories [18], [19], [20] can be used to understand the ethnographic findings in the context of the experience of conveying and responding to distress. All emphasise the inherently relational quality of pain, describing the strength of feeling that it elicits in those in close proximity, and the urge to protect oneself by seeking help or distancing oneself when unable to tolerate it.
Distress is integral to pain experience [8], [10], [11]. Patients need to feel believed as a starting point to negotiating a shared understanding of pain [9], [23] and to effective pain management. In the current study this was facilitated by the under-acknowledged communicative techniques used by nursing staff to target patient distress. However, as staff became increasingly overwhelmed, this shared understanding, along with the therapeutic relationship, was threatened; staff began judging patients and distancing themselves. Such factors are especially important in GI pain, where relational and psychological contributors are highly salient [8].
These findings have in common an understanding of pain assessment as an emotive social transaction [24] rather than as a measurement of a passive body by an objective clinician. Social and emotional dimensions of pain assessment were lacking from the pain initiative at the hospital, and from similar pain initiatives that prioritise protocol-based interventions alongside education, despite findings that nursing [25] and patient [26] education alone are weak ways to influence clinical outcomes.
4.1 Clinical implications
The findings of this study are particularly relevant where clinical staff are expected to be compassionate and are held accountable to high standards [27] but not provided with the necessary resources. Greater empathic concern risks burnout and mental health difficulties among medical and nursing staff, if not coupled with self-care [28]. While a degree of detachment is required to manage complex decisions in emotive environments, not engaging with emotions is likely to have serious adverse effects on patient and staff wellbeing [9], [22]. An overemphasis of sensory aspects of pain risks looking for solutions only in pharmacotherapy, particularly opioids [29]. Further, an absence of resources that allow staff to reflect on the impact of patient distress exacerbates the distance between clinical staff and patients as increasingly primitive and unhealthy defences emerge to manage overwhelming feelings, in turn increasing the risk of suboptimal or detrimental patient care [22].
In the current study, because patient and staff distress was unacknowledged by the institution from the point of assessment onward, staff were equipped only to provide patients with information, pharmacological intervention or specialist referral. Adding a further resource of being receptive and responsive to patient distress would require a top-down systemic shift within the medical and nursing professions in two ways. First, staff would require adequate training to acknowledge the impact of patient distress during pain assessment, recognise the ways in which it might influence their decision-making, and offer non-pharmacological resources for pain management. A template for this can be found in hospital settings where supervision and reflective thinking is embedded within the team and designed to increase staff wellbeing and prevent iatrogenic harm [30]. Second, the current stigma associated with supportive resources for clinicians and their emotional experiences must be challenged [9]. There was no discussion in the current study of formal supervision or support for staff or opportunities for informal support.
4.2 Limitations
The focus of the current study was staff; examining patient experiences of pain management is equally important, since patients play a crucial role in improving management of pain, by their expectations and by mobilising their own resources, for which they may require encouragement or permission from staff. The generalisability of the findings must be explored in further research but there is no reason to believe that specific characteristics of the ward or hospital account for the findings, given their resonance with problems in pain assessment and management across many settings and countries. The institutionalised defensive processes and heavy reliance on pharmacological resources reflect core processes of nursing and medical practice in relation to pain.
5 Conclusions
The current study recapitulated work by Menzies Lyth [21] that drew attention to the important defensive functions for staff of apparent barriers to optimal care. These phenomena are systemic and will likely persist unless the impact of patient distress on staff is factored into a biopsychosocial approach to pain management.
Acknowledgements
The authors are grateful to the receptive and insightful clinical staff linked with the studied ward, members of the Pain Teams at UCLH with whom much of the handover of findings took place, and Dr Anton Emmanuel for elucidating key issues in pain management in the areas of acute and chronic GI disorders.
-
Authors’ statements
-
Research funding: No funding was received other than from the host institution, UCL.
-
Conflict of interest: The authors are aware of no conflicts of interests.
-
Informed consent and ethical approval: NHS ethical approval (Ref 13/0732) allowed recruitment of staff from the relevant ward of University College London Hospital. All clinical staff were eligible.
-
Authors’ contributions
-
This work was completed as part of the first author’s doctoral dissertation. AW conceived of the study. AW and GD contributed to research design. GD was chief researcher in the field. AW was thesis supervisor. Both contributed to data analysis and write-up. Guarantor: University College London.
References
[1] Patients’ Association. Public Attitudes to Pain: Report, 2010. Available from: http://www.patients-association.org.uk/reports/public-attitudes-to-pain/. Accessed: 27 June 2017.Suche in Google Scholar
[2] Care Quality Commission. University College London Hospitals Quality Account, 2013/14. Available from: https://www.uclh.nhs.uk/aboutus/wwd/Annual%20reviews%20plans%20and%20reports%20archive/Quality%20account%202013-14.pdf. Accessed: 27 June 2017.Suche in Google Scholar
[3] Dr Foster Intelligence. National Pain Audit Final Report 2010–2012, British Pain Society: Healthcare Quality Improvement Partnership, 2012. Available from: http://www.nationalpainaudit.org/media/files/NationalPainAudit-2012.pdf. Accessed: 27 June 2017.Suche in Google Scholar
[4] Knowles SR, Mikocka-Walus AA, editors. Psychological aspects of inflammatory bowel disease: a biopsychosocial approach. London: Routledge, 2014.10.4324/9781315815374Suche in Google Scholar
[5] Powell AE, Davies HT. The struggle to improve patient care in the face of professional boundaries. Soc Sci Med 2012;75:807–14.10.1016/j.socscimed.2012.03.049Suche in Google Scholar PubMed
[6] Elcigil A, Maltepe H, Esrefgil G, Mutafoglu K. Nurses’ perceived barriers to assessment and management of pain in a university hospital. J Pediatr Hematol Oncol 2011;33:S33–8.10.1097/MPH.0b013e3182121befSuche in Google Scholar PubMed
[7] McCaffery M, Pasero C. Pain: a clinical manual, 2nd ed. Mosby: St Louis, 1999.Suche in Google Scholar
[8] Mayer EA, Tillisch K. The brain-gut axis in abdominal pain syndromes. Annu Rev Med 2011;62:381–96.10.1146/annurev-med-012309-103958Suche in Google Scholar PubMed PubMed Central
[9] Kerasidou A, Horn R. Making space for empathy: supporting doctors in the emotional labour of clinical care. BMC Med Ethics 2016;17:1.10.1186/s12910-016-0091-7Suche in Google Scholar PubMed PubMed Central
[10] International Association for the Study of Pain. Classification of chronic pain. Pain 1986;(Suppl 3);S1–226.10.1016/0304-3959(86)90069-2Suche in Google Scholar
[11] National Comprehensive Cancer Network. NCCN Clinical Practice Guidelines in Oncology: Distress Management. Pennsylvania: NCCN, 2011. Available from: http://www.nccn.org/professionals/physician_gls/pdf/distress.pdf. Accessed: 21 November 2016.Suche in Google Scholar
[12] Williamson G, Bellman L, Webster J. Action research in nursing and healthcare. London: Sage, 2012.10.4135/9781446289112Suche in Google Scholar
[13] Brown D, McCormack BG. Developing the practice context to enable more effective pain management with older people: an action research approach. Implement Sci 2011;6:1–14.10.1186/1748-5908-6-9Suche in Google Scholar PubMed PubMed Central
[14] Drake GF. Barriers and potential solutions to effective pain management on a gastro-intestinal ward: an action research study in a university hospital (Doctoral dissertation). University College London, 2015. Available from: http://discovery.ucl.ac.uk/1471122/1/Drake_Gareth_Thesis_final_volume_1_redacted.pdf. Accessed: 27 June 2017.Suche in Google Scholar
[15] Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol 2006;3:77–101.10.1191/1478088706qp063oaSuche in Google Scholar
[16] Strauss A, Corbin J. Basics of qualitative research: techniques and procedures for developing grounded theory, 2nd ed. Thousand Oaks, CA: Sage, 1998.Suche in Google Scholar
[17] Elliott R, Fischer CT, Rennie DL. Evolving guidelines for publication of qualitative research studies in psychology and related fields. Br J Clin Psychol 1999;38:215–29.10.1348/014466599162782Suche in Google Scholar PubMed
[18] Bowlby J, Fry M, Ainsworth MD. Child care and the growth of love. London: Penguin Books, 1965.Suche in Google Scholar
[19] Luyten P, van Houdenhove B, Lemma A, Target M, Fonagy P. A mentalization-based approach to the understanding and treatment of functional somatic disorders. Psychoanal Psychother 2012;26:121–40.10.1080/02668734.2012.678061Suche in Google Scholar
[20] Williams ACC. Facial expression of pain: an evolutionary account. Behav Brain Sci 2002;25:439–55.10.1017/S0140525X02000080Suche in Google Scholar PubMed
[21] Menzies Lyth I. Social systems as a defence against anxiety. Hum Relat 1960;13:95–121.10.1177/001872676001300201Suche in Google Scholar
[22] Evans M. ‘I’m beyond caring’, a response to the Francis Report: the failure of social systems in health care to adequately support nurses and nursing in the clinical care of their patients. Psychoanal Psychother 2014;28:193–210.10.1080/02668734.2014.914076Suche in Google Scholar
[23] Seers K. The patients’ experiences of their chronic non-malignant pain. J Adv Nurs 1996;24:1160–8.10.1111/j.1365-2648.1996.tb01021.xSuche in Google Scholar PubMed
[24] Schiavenato M, Craig KD. Pain assessment as a social transaction: beyond the “gold standard”. Clin J Pain 2010;26:667–76.10.1097/AJP.0b013e3181e72507Suche in Google Scholar PubMed
[25] Drake GF, Williams AC. Nursing education interventions for managing acute pain in hospital settings. Pain Manag Nurs 2017;18:3–15.10.1016/j.pmn.2016.11.001Suche in Google Scholar PubMed
[26] Ronco M, Iona L, Fabbro C, Bulfone G, Palese A. Patient education outcomes in surgery: a systematic review from 2004 to 2010. Int J Evid Based Healthc 2010;10:309–23.10.1111/j.1744-1609.2012.00286.xSuche in Google Scholar PubMed
[27] Department of Health. 2010–2015 Government policy compassionate care in the NHS, 2015. Available from: https://www.gov.uk/government/publications/2010-to-2015-government-policy-compassionate-care-in-the-nhs/2010-to-2015-government-policy-compassionate-care-in-the-nhs. Accessed: 27 June 2017.Suche in Google Scholar
[28] Harvey SB, Laird B, Henderson M, Hotopf M. The mental health of health care professionals: a review for the Department of Health. London: National Clinical Assessment Service, 2009. Available from: http://www.champspublichealth.com. Accessed: 27 June 2017.Suche in Google Scholar
[29] Els C, Jackson TD, Hagtvedt R, Kunyk D, Sonnenberg B, Lappi VG, Straube S. High-dose opioids for chronic non-cancer pain: an overview of Cochrane reviews. Cochrane Libr 2016;7:1–15.10.1002/14651858.CD012299Suche in Google Scholar
[30] Stern J. The relevance of applied psychoanalytic thinking to the treatment of medically symptomatic patients. In: Lemma A, Patrick M, editors. Off the couch: contemporary psychoanalytic applications. London: Routledge, 2010.Suche in Google Scholar
Supplementary Material
The online version of this article offers supplementary material (https://doi.org/10.1515/sjpain-2018-0045).
©2018 Scandinavian Association for the Study of Pain. Published by Walter de Gruyter GmbH, Berlin/Boston. All rights reserved
Artikel in diesem Heft
- Frontmatter
- Editorial comment
- Diagnosis of carpal tunnel syndrome
- Body image concerns and distortions in people with persistent pain
- The prevalence of recurrent pain in childhood is high and increases with age
- Friends in pain: pain tolerance in a social network
- Clinical pain research
- Correlation of clinical grading, physical tests and nerve conduction study in carpal tunnel syndrome
- Spectroscopic differences in posterior insula in patients with chronic temporomandibular pain
- Deconstructing chronicity of musculoskeletal pain: intensity-duration relations, minimal dimensions and clusters of chronicity
- “When I feel the worst pain, I look like shit” – body image concerns in persistent pain
- The prevalence of neck-shoulder pain, back pain and psychological symptoms in association with daytime sleepiness – a prospective follow-up study of school children aged 10 to 15
- The neglected role of distress in pain management: qualitative research on a gastrointestinal ward
- Pain mapping of the anterior knee: injured athletes know best
- The role of pain in chronic pain patients’ perception of health-related quality of life: a cross-sectional SQRP study of 40,000 patients
- The DoloTest® in a specialized headache center among patients receiving psychological treatment. A pilot study
- Observational study
- Chronic pelvic pain – pain catastrophizing, pelvic pain and quality of life
- Survey of chronic pain in Chile – prevalence and treatment, impact on mood, daily activities and quality of life
- Patients’ pre-operative general and specific outcome expectations predict postoperative pain and function after total knee and total hip arthroplasties
- The peer effect on pain tolerance
- Original experimental
- The effects of propranolol on heart rate variability and quantitative, mechanistic, pain profiling: a randomized placebo-controlled crossover study
- Idiographic measurement of depressive thinking: development and preliminary validation of the Sentence Completion Test for Chronic Pain (SCP)
- Adding steroids to lidocaine in a therapeutic injection regimen for patients with abdominal pain due to anterior cutaneous nerve entrapment syndrome (ACNES): a single blinded randomized clinical trial
- The influence of isometric exercise on endogenous pain modulation: comparing exercise-induced hypoalgesia and offset analgesia in young, active adults
- Do pain-associated contexts increase pain sensitivity? An investigation using virtual reality
- Differences in Swedish and Australian medical student attitudes and beliefs about chronic pain, its management, and the way it is taught
- An experimental investigation of the relationships among race, prayer, and pain
- Educational case report
- Wireless peripheral nerve stimulation for complex regional pain syndrome type I of the upper extremity: a case illustration introducing a novel technology
Artikel in diesem Heft
- Frontmatter
- Editorial comment
- Diagnosis of carpal tunnel syndrome
- Body image concerns and distortions in people with persistent pain
- The prevalence of recurrent pain in childhood is high and increases with age
- Friends in pain: pain tolerance in a social network
- Clinical pain research
- Correlation of clinical grading, physical tests and nerve conduction study in carpal tunnel syndrome
- Spectroscopic differences in posterior insula in patients with chronic temporomandibular pain
- Deconstructing chronicity of musculoskeletal pain: intensity-duration relations, minimal dimensions and clusters of chronicity
- “When I feel the worst pain, I look like shit” – body image concerns in persistent pain
- The prevalence of neck-shoulder pain, back pain and psychological symptoms in association with daytime sleepiness – a prospective follow-up study of school children aged 10 to 15
- The neglected role of distress in pain management: qualitative research on a gastrointestinal ward
- Pain mapping of the anterior knee: injured athletes know best
- The role of pain in chronic pain patients’ perception of health-related quality of life: a cross-sectional SQRP study of 40,000 patients
- The DoloTest® in a specialized headache center among patients receiving psychological treatment. A pilot study
- Observational study
- Chronic pelvic pain – pain catastrophizing, pelvic pain and quality of life
- Survey of chronic pain in Chile – prevalence and treatment, impact on mood, daily activities and quality of life
- Patients’ pre-operative general and specific outcome expectations predict postoperative pain and function after total knee and total hip arthroplasties
- The peer effect on pain tolerance
- Original experimental
- The effects of propranolol on heart rate variability and quantitative, mechanistic, pain profiling: a randomized placebo-controlled crossover study
- Idiographic measurement of depressive thinking: development and preliminary validation of the Sentence Completion Test for Chronic Pain (SCP)
- Adding steroids to lidocaine in a therapeutic injection regimen for patients with abdominal pain due to anterior cutaneous nerve entrapment syndrome (ACNES): a single blinded randomized clinical trial
- The influence of isometric exercise on endogenous pain modulation: comparing exercise-induced hypoalgesia and offset analgesia in young, active adults
- Do pain-associated contexts increase pain sensitivity? An investigation using virtual reality
- Differences in Swedish and Australian medical student attitudes and beliefs about chronic pain, its management, and the way it is taught
- An experimental investigation of the relationships among race, prayer, and pain
- Educational case report
- Wireless peripheral nerve stimulation for complex regional pain syndrome type I of the upper extremity: a case illustration introducing a novel technology

