Abstract
Background and aims
Medical students receive training in the management of chronic pain, but the training is often suboptimal. Considering that the basis for physician’s knowledge is their medical education, it is important to explore the attitudes and beliefs of medical students with respect both to chronic pain management and to their views on current pain education. Therefore, the aim of this study was to compare Swedish and Australian medical student’s attitudes and beliefs about patients with chronic pain, and their perceptions regarding their chronic pain management education.
Methods
An online survey was conducted with final year Australian and Swedish medical students from two different universities between December 2016 and February 2017. Attitudes and beliefs towards chronic pain patients were measured using the Health Care Providers’ Pain and Impairment Scale (HC-PAIRS). A thematic analysis was conducted on open end questions regarding their views on their education and important skills for chronic pain management.
Results
A total of 57 Swedish and 26 Australian medical students completed the HC-PAIRS scale. The Swedish medical students showed statistically significantly lower total mean HC-PAIRS scores compared to Australian medical students (46 and 51, respectively). Australian students had statistically significantly higher scores than the Swedish students for two of four factors: functional expectations and need for cure, whereas no significant differences were seen for the factors social expectations or for projected cognition. From the open end questions it was evident that final year medical students are knowledgeable about key chronic pain items described in clinical guidelines. However, both cohorts described their chronic pain training as poor and in need of improvement in several areas such as more focus on the biopsychosocial model, working in multidisciplinary teams, seeing chronic pain patients and pharmacological training.
Conclusions
Attitudes and beliefs are formed during medical education, and our study exploring attitudes of medical students towards chronic pain and how it is taught have provided valuable information. Our survey provided detailed and cohesive suggestions for education improvement that also are in line with current clinical guidelines. This study indicates that the Swedish final year students have a more positive attitude towards chronic pain patients compared to their Australian counterparts. The majority of students in both cohorts perceived chronic pain management education in need of improvement.
Implications
This study highlights several areas of interest that warrant further investigation, for example, the impact of a changed medical curriculum in alignment with these clinical guidelines requested by students in this survey, and correspondingly if their attitudes towards chronic pain patients can be improved through education. Further, we conclude that it would be valuable to align the implementation of the HC-PAIRS instrument in order to achieve comparable results between future studies.
1 Introduction
Chronic pain is prevalent, one in five Australians will experience chronic non-malignant pain during their lifetime and it is the third most costly health problem in that country [1], [2]. A similar prevalence has been reported in Sweden [3], [4]. Chronic pain places a major physiological, social, economic and psychological burden on both individuals and the society [5], [6], [7], [8]. The cost of chronic pain in Europe has been estimated as €300 billion. This figure includes both direct and indirect costs such as loss of income and welfare [9]. Clearly, there is much to gain from better management of chronic pain.
The biopsychosocial model first described by Gatchel et al. states that pain results from a dynamic and complex interaction among physiological, psychological, pathological and social factors. This model is now widespread and integrated in clinical guidelines [10], [11]. Nonetheless, numerous barriers to optimal treatment and guideline adherence have been described in the literature [12], [13], [14]. Time restrained appointments with physicians, poor access to specialists, lack of belief among the patients that their condition is treatable, health care not utilising the full expertise of all health care professionals and lack of chronic pain education are all part of preventing satisfactory chronic pain treatment [12], [13], [14].
Researchers and initiatives such as PainAustralia and the European Pain Federation have indicated that change is needed, not only within the health care per se, but also within both undergraduate and postgraduate medical education [9], [15]. It is common that chronic pain education is fragmented during undergraduate medical training rather than taught as a discrete subject [16]. In 2015, Briggs et al. published an overview of the current undergraduate pain education across Europe. The study concluded that only 12 h were spent, on average, teaching pain for compulsory dedicated pain modules and 9 h for other compulsory (non-pain specific) modules. Chronic pain curriculums varied greatly between universities, and in seven percent of cases, there was no evidence of any chronic pain education at all. Only two out of the seven Swedish universities studied were found to have a dedicated pain module together with pain teaching in other modules [17]. According to the American Academy of Pain Medicine (AAPM) in 2013, the top five subjects within chronic pain training that need the most attention in medical education curriculums are: awareness of acute and chronic pain, promotion of compassionate practises, skilfulness in clinical appraisal, displaying empathy towards the patient and knowledge of terms and definitions for substance abuse [18].
Sweden and Australia share similarities in terms of chronic pain prevalence and management. Both nations have comparable annual costs of chronic pain and have similar tax funded health care systems [4], [15]. Furthermore, both nations are undertaking progressive developments in health care, with Australia being the first in the world to create a national pain strategy [15]. Despite clear differences in area and population, both nations also encounter challenges in access to health care in large rural areas.
1.1 Aims
Considering that medical education is the basis of knowledge for physicians, it is important to explore the attitudes and beliefs of medical students with respect both to chronic pain management and to their views on current pain education [19], [20]. Hence this study compared Australian and Swedish medical students’ attitudes towards chronic pain. In particular, it asked:
What are medical students’ attitudes and beliefs about patients with chronic pain?
Are there any differences in Swedish medical students and Australian medical students’ attitudes and management towards chronic pain?
What are Swedish and Australian medical students’ perceptions regarding chronic pain and their education.
2 Methods
2.1 Medical education setting
Two universities participated in this study. The medical programme at the Swedish university extends over a 5½-year period consisting of 11 semesters, leading to the MD degree. Graduates then enter a 2-year general post graduate medical training programme “allmäntjänstgöring” (AT), to acquire a licence to practise medicine. Speciality training, “specialisttjänstgöring” (ST), can be initiated after this licence is obtained. At the Umeå university medical programme, clinical training including treating patients, starts in semester 6 (year 3; Swedish Universities use a two-term academic year). During semesters 9–11, topics such as psychiatry, paediatrics and research in the form of a master thesis are taught. As Chronic pain is not taught as a specific topic during these last three semesters at Umeå University, they were the ideal choice for our project. Basal pharmacology is taught as a discrete subject during 4 weeks in semester 5. In year 4, chronic pain education is given during semester eight (within the pain rehabilitation course). Two days are scheduled with clinical placements when the students participate in assessment of chronic pain patients together with an interdisciplinary team (including: physician, specialist in rehabilitation medicine, physiotherapist, occupational therapist, psychologist and social worker). The students also participate in case seminars about chronic pain and in group-based sessions about treatment methods and multimodal rehabilitation.
In Australia, the medical programme extends over 4–6 years depending on whether the student undertakes undergraduate training (5–6 years) or commences other studies before entering postgraduate training (4 years). The medical graduate then undergoes a 1-year internship followed by a residency (length determined by graduate) before undertaking specialist training after being accepted into a training programme. Depending on the medical school, students may be in the hospital from year 1 or from their penultimate year. At the School of Medicine at Notre Dame, Sydney, rotations start in year 3, then the students see patients alone and with supervising doctors. Experience specifically in a health care central setting is introduced during the 1st year during three afternoons with a GP, but is followed by a rotation of 5 weeks, also with a GP during the 3rd year. The remaining rotations occur in a hospital setting where one morning is scheduled at a hospital pain clinic during psychiatry rotation. Full responsibility for treating patients starts at the internship. Pharmacology is not taught as a discrete subject, instead pharmacology lectures are given throughout the courses. Similarly to Umeå University, problem based learning (PBL) using fictive patient cases, are also used.
2.2 Participant selection
The target group for the survey was medical students in their last three semesters at the school of medicine at Umeå University, Sweden, and final year (Year 4) medical students at the School of Medicine at Notre Dame, Sydney, Australia. The survey was available as an online questionnaire in SurveyMonkey® (SurveyMonkey, San Mateo, CA, USA). Multiple distribution channels were used to maximise the participation rate. For the Swedish arm of the study, an invitation letter and web link to the survey was sent to 327 medical students by email in December 2016. Two reminders were sent out during the 2-month period the survey was open. For the Australian arm of the study, students were notified in a broadcast via their education software (blackboard) with information about the study and a link to the online survey was sent in February 2017. A flyer providing details about the project and survey with contact details was also displayed in venues used by the students. Australian students were also given the option to enter a draw for a gift voucher upon completion of the survey.
2.3 Questionnaire development
There is no gold standard tool to evaluate medical student attitudes and knowledge about chronic (non-malignant) pain management. In consequence, the survey instrument was developed using key themes from the literature [19], [21], [22]. The initial version was in English and this was translated into Swedish then back-translated to English to ensure that the two versions were internally consistent. The Swedish version consisted of 27 questions and the Australian version of 25 questions. The extra two questions in section four of the questionnaire (described below) in the Swedish version were not relevant to the situation in Australia.
This questionnaire had four sections. Section one assessed attitudes towards chronic pain using a validated instrument; the Health Care Providers’ Pain and Impairment Relationship Scale (HC-PAIRS) [23]. HC-PAIRS is a widely used instrument for assessment of attitudes of health care professionals, and it has been shown be a reliable and valid tool for measuring health care providers’ attitudes and beliefs about the relationship between pain and impairment [22]. Although HC-PAIRS is a quite commonly used instrument to explore both health care students and professionals, scores between different studies are not always directly comparable due to different application of the instrument. Some studies use a seven-point rather than a six-point Likert-scale and there is also variation in how many items are included, particularly with respect to the questions relating to projected cognition (see below).
The HC-PAIRS questionnaire originally consisted of 15 items (see Supplementary Table S1 for the questions as used here) rated on a Likert scale ranging from “totally disagree” to “totally agree”. In the original study, the items were classified into four groups on the basis of a principal components analysis. These items, reflecting different dimensions of attitudes were classified under the following headings: 1, “functional expectations” (items 1–3, 6–9, 11–12); 2, “social expectations” (items 5, 7, 11, 14); 3, “need for cure” (items 4, 9, 15); and 4, “projected cognition” (items 10 and 13). Thus, items 7, 9 and 11 are included in two of the dimensions, due to the method in which they were derived (orthogonal principal component analyses, see [23]). In the original study, Rainville et al. [23] validated the method by comparing the scores for 144 community health care providers with 66 functional restoration providers, who would be expected to have lower scores. This was the case for the factors 1, 2 and 3 and the total score, but not for factor 4 [23]. Modified versions of the instrument can be found throughout the literature, and some authors only use the items in the first three factors [24], [25], [26], [27], [28]. A Swedish version has been published by Overmeer et al. [28]. This version consists of 15 statements with a six-point Likert scale where 1=Strongly disagree, 2=Disagree, 3=Slightly disagree, 4=Slightly agree, 4=Agree, 5=Strongly agree, with a final score ranging from 15 to 90. This version was used, following minor modifications (a few word changes were made after pilot testing better to suit current guideline terminology. For example, the term “disabled” was changed to “a person with a disability”). Higher HC-PAIRS scores reflect a stronger belief that chronic pain is in close relation to impairment and limitation of activities, and as a consequence, the person answering the questionnaire has less beneficial attitudes towards chronic pain. Internal consistency has been evaluated by Houben et al. [22] (Chronbach’s α=0.78–0.84, a good outcome) and Briggs et al. [29] showed that HC-PAIRS scores were well in line with clinical recommendations.
Section two of the questionnaire was a Best-Worst Scaling Experiment to compare factors affecting chronic (non-malignant) pain management (to be reported separately).
Section 3 included three open-ended questions about chronic pain education; Students were asked what areas they thought were important for knowledge and skills regarding chronic pain treatment, if there was any part of their chronic pain education that could be changed to improve their skill and knowledge, and about their overall view on chronic pain management and education.
The fourth section consisted of seven (Australian version) or nine (Swedish version) demographic questions such as age, gender, what speciality they would choose if they were to choose today and in which sector they would prefer to work. It also asked if they knew someone (a friend or a family member) who suffered from chronic pain (and in that case, if they thought that their treatment was satisfactory or not) and if they themselves had ever experienced chronic pain. The Swedish survey included two additional questions asking what semester they were currently in and what type of health care facility they would like to work in the future. These questions were not included in the Australian version since we only investigated final year medical students in Australia and since the health care facilities are not directly comparable between countries. Responses to sections 1, 3 and 4 are reported in this paper.
2.4 Pilot testing
The Swedish survey was tested by a former medical student who recently graduated from Umeå University and by one final year medical student from another university in Sweden. The Australian survey was tested by two former University of Notre Dame school of medicine students undertaking their intern year. A feed-back questionnaire was sent out together with an online link to the survey. Pilot testers where asked to give critical feedback in relation to language congruity, survey design and medical plausibility. The Australian pilot testers were given a $20 gift card as incentive to participate. Minor changes were made as result of the pilot testing. Furthermore, specialist medical doctors with specialities strongly linked to chronic pain in both Sweden, UK and Australia were consulted to assure general medical authenticity of the survey.
2.5 Data analysis
2.5.1 Quantitative data
Demographic data were analysed using either χ2 or Fisher’s exact tests, as appropriate, using GraphPad Prism v7 for the Macintosh (GraphPad Software Inc., San Diego, CA, USA). T-tests and Mann-Whitney U-tests were undertaken using the GraphPad prism programme. Mood’s median tests were undertaken using the function mood.medtest in the RVAideMemoire package version 0.9–68 for the statistical programme R version 3.4.1 [30]. Linear models describing the interaction between the question “Do you know someone, a relative or close friend, who suffers from chronic pain?” and Factor 1 and 3 for HC-PAIRS were constructed using the function lm in the stat package built into R. Cohen’s d values were calculated using the function cohensD in the package lsr version 0.5 for R. To avoid the risk of false positives due to multiple testing, we used a 5% false discovery rate [31] calculated on Microsoft Excel spreadsheets. Some authors give the adjusted p-values, but we have preferred to give the observed p-values and to state in the Table legend the critical value of p using a 5% false discovery rate. In this way, readers preferring other ways of adjusting for multiple testing can do this.
2.5.2 Qualitative data
There are many ways of analysing qualitative data. Popular methods include Qualitative content analysis and Thematic analysis, both of which are preferably used on larger data sets such as interviews and focus group transcripts. Other methods, such as Word Frequency Analysis does not allow for interpretation of the answers. Thus, we chose to apply Thematic analysis according to Braun and Clarke [32] on the open-end questions. Repeated reading of the answers by authors BMS and LR included the process of identifying patterns within the data. The full data set was always given equal attention during this process. This was followed by construction of themes. Refinement of themes took place in two steps where authors BMS and LR first discussed individually identified themes and then established a joint set of themes including definitions and theme names.
3 Results
3.1 Demographic characteristic
The total number of Swedish students who completed the survey was 80 (of 327 invited to participate, response rate 25%) and the number of Australian students that completed the survey was 30 (of 110 reached, response rate 27%). Figure 1 shows the number of participants from each country that completed each individual section of the survey. There was a considerable attrition rate, particularly at the level of Section 2, with the Swedish students showing a higher attrition rate at this (and subsequent levels) than the Australian students (p<0.01, Fisher’s exact test).
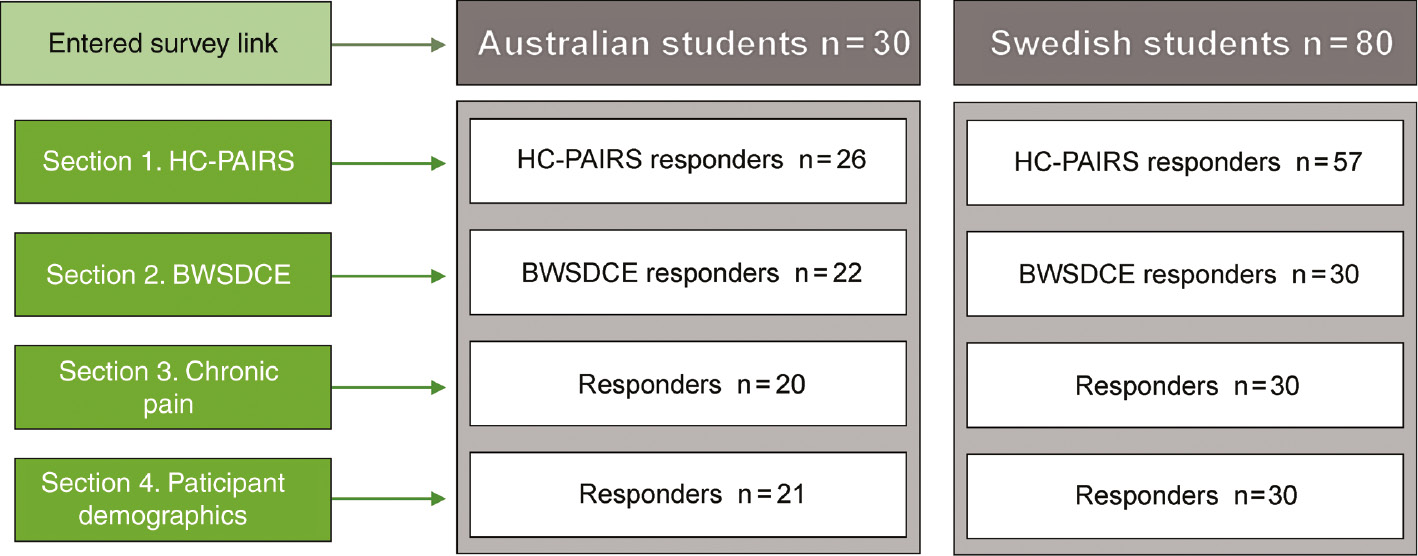
Number of Australian medical students and Swedish medical students completing each section of the survey.
The characteristics of the respondents are described in Table 1. With one exception (future workplace), there was no statistical significant difference between the two samples. In both cohorts, the majority of the respondents were female and aged between 25 and 29 years. Approximately 70% of the students knew someone who suffered from chronic pain and most of these pain sufferers believed that their treatment was inadequate. Approximately one in six of the responders had experienced chronic pain themselves.
Demographic characteristics of participants n (%) (Section 4 of the study).
| Australian medical students (n=21) n (%) | Swedish medical students (n=30) n (%) | p-Value | |
|---|---|---|---|
| Female | 16 (76) | 19 (63) | 0.37a |
| Age | |||
| Under 25 | 3 (14) | 10 (33) | 0.30b |
| 25–29 | 15 (71) | 16 (53) | |
| 30–34 | 2 (10) | 2 (7) | |
| 35–39 | 1 (5) | 1 (3) | |
| 45–49 | – | 1 (3) | |
| Know someone who suffers from chronic pain | 14 (67) | 22 (73) | 0.76a |
| Does not believe that their treatment is adequate | 11 (79) | 18 (82) | >0.99a |
| Ever experienced chronic pain themselves | 4 (19) | 4 (13) | 0.70a |
| Wish to pursue general medicine as medical speciality | 2 (8) | 4 (13) | >0.99a |
| Preferred future working sector | |||
| Public | 6 (29) | 28 (93) | <0.0001c |
| Private | – | 2 (7) | – |
| Both | 15 (71) | – | – |
| Health care facility | |||
| Teaching hospital | – | 13 (43) | – |
| Other type of hospital e.g. regional | – | 7 (23) | – |
| Health care centre | – | 4 (13) | – |
| Other | – | 1 (3) | – |
| Don’t know | – | 5 (17) | – |
-
p-Values for differences between the two countries using Fisher’s exact test or χ2 test when applicable.
-
aFisher exact test.
-
bχ2 test, for three age groups (<25, 25–29 and ≥30).
-
cFisher exact test for two groups (public and private/both).
-
At a 5% false discovery rate, the critical value of p is 0.0071.
The public sector was the most popular choice for future workplace amongst the Swedish students while 15/21 Australian students chose both private and public sector. The Swedish students were asked in which type of health care facility they would prefer to work, with teaching hospital being the most popular choice (43%) followed by regional hospital (23%). Only a small proportion of students in both countries (~10%) expressed the desire to pursue general medicine as their medical speciality.
3.2 Attitudes and beliefs towards chronic (non-malignant) pain patients
Attitudes and beliefs were assessed using HC-PAIRS scores. Median scores on the six point Likert scale for the 15 individual items are reported in Supplementary Table S1. Analysis of Likert scores is a somewhat contentious issue, but there are good arguments for analysing the data parametrically given that the score consists of a sufficient number of items and that the internal consistency of the scores is good [33]. This is certainly the case for the total scores for all items (15 items) and for those included in factors 1–3 (13 items) as well as for factor 1 (nine items), and possibly factor 2 (four items), but whether it holds for factors 3 (three items) and 4 (two items) is more open to debate. In consequence, we have presented the data for the scores both as means±SD in Table 2, and as medians and interquartile ranges in Supplementary Table S2 to allow the reader to make her/his own decision, and analysed these accordingly using a 5% false discovery rate to assign critical values of p [31]. Scatterplots showing the individual scores are shown in Supplementary Fig. S1.
HC-PAIRS dimension scores between Swedish and Australian students.
| HC-PAIRS |
Australian students (n=26) |
Swedish students (n=57) |
p-Value | ||
|---|---|---|---|---|---|
| Total scores and factors | Mean | SD | Mean | SD | |
| Total score | 51.0 | 6.4 | 46.0 | 6.2 | 0.0016 |
| 1. Functional expectations | 28.9 | 4.4 | 25.1 | 4.4 | 0.0007 |
| 2. Social expectations | 13.8 | 1.8 | 14.2 | 3.3 | 0.48 |
| 3. Need for cure | 9.5 | 2.6 | 7.5 | 2.6 | 0.0020 |
| 4. Projected cognition | 9.2 | 1.6 | 9.1 | 1.6 | 0.81 |
-
p-Values were calculated by two-tailed t-tests with Welch’s correction for unequal variances. At a 5% false discovery rate, the critical value of p was 0.03.
The Australian medical students show statistically significantly higher total HC-PAIRS scores than the Swedish medical students, see Table 2. Australian students had statistically significantly higher scores than the Swedish students for two of four factors: functional expectations and need for cure. The effect sizes (Cohen’s d) were 0.80, 0.86 and 0.77 for total score, factor 1 and factor 3, respectively. The differences between the groups for factor 2 (social expectations) and factor 4 (projected cognition) were not significant.
For the Swedish students, we investigated whether the mean scores were significantly different for the individuals completing vs. not completing the whole questionnaire (shown as filled and unfilled symbols, respectively, in Supplementary Fig. 1). For the total score and factors 1, 3 and 4, there were no significant differences between the two groups (p>0.36, two-tailed t-test with Welch’s correction). However, the score for factor 2 was higher for the completers than the non-completers (15.3±3.4, n=30 and 13.0±2.8, n=27, respectively, means±SD; p=0.0098, two-tailed t-test with Welch’s correction).
The demographic data for students completing the survey was well balanced between countries with respect to gender and whether they knew someone who suffered from chronic pain (Table 1). In order to determine whether or not these factors were associated with differences in the scores, linear models were constructed for all 51 students completing the surveys. For factor 1, the p-values for the main effects of land, gender and knowing someone suffering from chronic pain were 0.027, 0.18 and 0.30, respectively (Supplementary Table S2). A full interaction model gave no significant interactions between the parameters (p>0.5). Similar results were seen for factor 3 (Supplementary Table S2). Thus, gender and knowing someone suffering from chronic pain can be ruled out as factors affecting the observed scores of the students completing the survey.
3.3 Student assessment of their chronic pain education
3.3.1 What do you believe are the important areas of knowledge and skills in chronic pain management?
It can be concluded that pain assessment, patient attentiveness, pharmacological and non-pharmacological treatment, the biopsychosocial model and treatment strategies are all considered to be important knowledge and skills for chronic pain management noted by our students. There were some detectable differences between cohorts, where assessing pain through different approaches such as physiology, orthopaedics, neurology, different types of pain, and even psychology, was slightly more emphasised by the Swedish than the Australian students. A noticeable shift could also be seen for the Australian students that had a slightly larger focus on “Patient attentiveness” compared to the Swedish students. This can be exemplified by comments such as “…Being able to determine what is important to the patient in terms of sedation vs pain relief” as explained by one Australian student. Non-pharmacological treatment was mentioned as an important skill for chronic pain management by students from both cohorts, although it was clear that this has a somewhat lower status compared to other skills, as clarified by this Australian student: “Adjunct therapies have not been taught very much. Treating the pain pharmacologically is important but also strategies to help the patient cope and improve function are valuable. The attitude towards these seemed negative (like they are a bit of hocus-pocus)”.
3.3.2 During your training is there something that could have been done to improve your competency in chronic pain management?
Both cohorts decisively expressed the need for more chronic pain education in question two. Additionally, most students suggested changes that would improve their education; more experience seeing patients, pharmacological and non-pharmacological treatment plans, including what to expect from treatment and more focus on the biopsychosocial model.
Within the responses for “Pharmacology, including treatment plans and expectations” there was a difference in the responses from the Australian students who more often requested basic pharmacology education, as described by comments such as “a basic lecture on treatment would have been good” and “pharmacology tutorials on all medications but including pain medications would have been highly beneficial”, compared to the Swedish students who were more focused on applying their pharmacology knowledge in the clinic; “More clear guidelines on how to plan the treatment in these cases” and “Yes, I don’t believe it is clear what treatment to choose on what indications, and how different conditions can be expected to change over time”. The fact that opioids have little use in treating chronic non-malignant pain was reflected in our survey through many Australian students, for example: “Don’t give opioids – leads to centralisation of pain pathways and increases pain…” and “…Opioids are of little use and can make the situation worse…”.
Another difference was seen between countries within the theme “Patient experience”; Australian students provided answers that were more related to fictive patient cases and teaching within a pain clinic setting whilst the Swedish students expressed they like to see more chronic pain patients (example, see Table 3).
Identified themes during thematic analysis of open end questions.
| Theme | Theme definition | Example quotes |
|---|---|---|
| 1. Identified themes within the responses for the question “What do you believe are the important areas of knowledge and skills in chronic pain management?” | ||
| Patient attentiveness | Being empathic and understanding their patients pain, communicative skills to motivate and educate the patient regarding their condition and its treatment | “How the pain is affecting the patient. Encourage the patient to compliance even if they might not feel any improvement initial phase of treatment.” |
| Pain assessment | Assessing the pain, including pain analysis through different specialities and knowledge; such as physiology and the musculoskeletal system, orthopaedics, rehabilitation medicine, medical psychology, different origins and types of pain | “Aetiology, pain physiology…” “Different types of pain…” “Rehabilitation medicine, psychiatry…” |
| Pharmacological treatment | The pharmacology regarding chronic pain medications | “Pharmacology” “Drugs and their side effects” |
| Non-pharmacological treatment | Treatment regarding non-pharmacological methods | “Education regarding non-pharmacological treatment options such as TENS, physiotherapy and CBT.” |
| Biopsychosocial model | Recognising and implementing the biopsychosocial model and its association with multidisciplinary treatment | “…Chronic pain management needs a multidisciplinary approach with input from doctors, nurses, physiotherapists and psychologists.” |
| Treatment strategies | Treatment strategies and case-handling including flow charts. Knowing what pharmacological treatments to choose for different types of pain and patients | “Different types of treatment for different types of pain, combinations, where to turn for advice on treatment strategies for pain that is difficult to treat” |
| 2. Identified themes within the responses for the question “During your training is there something that could have been done to improve your competency in chronic pain management?” | ||
| Needing more chronic pain education | Participants who describe needing more chronic pain education but have no specific suggestion to in what form | “We did not get very much tutoring on chronic pain at all. I was first exposed to it on my psych rotation and have not had much other exposure.” |
| Needing more patient experience | Experience seeing patients, including both doctor-patient relationship and case handling | “Handling chronic pain patients in primary care.” |
| Needing more knowledge on pharmacology, treatment plans and expectations | Pharmacology, including treatment plans and strategies | “Pharmacology tutorials on all medications but including pain medications would have been highly beneficial.” |
| Needing more non-pharmacological treatment | Non-pharmacological treatment plans | “Adjunct therapies have not been taught very much. Treating the pain pharmacologically is important but also strategies to help the patient cope and improve function are valuable. The attitude towards these seemed negative (like they are a bit of hocus-pocus).” |
| Needing more focus on the biopsychosocial model | More focus on the biopsychosocial model and experience with multidisciplinary treatment | “Yes, everything involves psychosocial factors and I think we need to learn how to deal with this better.” “Getting experience with how physiotherapists manage patients with chronic pain. Not just "treatment" but also education, encouragement and follow-up with other allied health professionals. Not just sitting in on "chronic pain clinics" where doctors hand out medications.” |
| 3. Identified themes within the responses for the question “What are your overall thoughts about chronic pain management education?” | ||
| Complex and important | Chronic pain is an important topic and is difficult to comprehend and treat due to its complexity | “Very complex condition and hence very difficult to treat.” |
| Poor management and need of improvement | Chronic pain management is poor and there are different areas where there could be improvement regarding my education | “Somewhat lacking in regard to practical, everyday treatment of patients.” |
| Satisfied with my education | I consider my education on this subject as satisfactory and there were some specific aspects of my education that were exceptionally good | “I think it covers most sections” |
-
Theme and theme descriptions, along with example quotes from the open-end question is presented. Example quotes from the Swedish students have been translated into English.
3.3.3 What are your overall thoughts about chronic pain management education?
Both cohorts noted that chronic pain is an important topic that is difficult to treat due to its complexity. It could also be understood that both cohorts perceived chronic pain management education in need for improvement of improvement.
Some Australian students described the need for more practical training such as depicted in these comments by two individual Australian students: “Somewhat lacking in regards to practical, everyday treatment of patients” and “Overall the theory covered quite well yet practical cases based learning would be helpful”. Australian students moreover expressed their gratitude for being given a specific rotation: “I was lucky to do a week in the pain clinic at St Vincent’s Hospital during my psychiatry rotation in 3rd year. it was a great experience that all students should have” and another student wrote: “… I was lucky to have a rotation with exposure to chronic pain management.” Whilst the Swedish students appear to get equal exposure to the work at the pain clinic as described by one student: “Rehabilitation medicine during the eighth semester gave insight and lectures about chronic pain and treatment during a few days, which is perhaps somewhat short seeing how extensive this problem is”.
4 Discussion
In the present study, the attitudes of Australian and Swedish medical students towards patients suffering from chronic pain and their treatment have been investigated, using the HC-PAIRS scale providing the key data. The main finding from the HC-PAIRS scores is that Swedish final year students have a more positive attitude towards chronic pain patients than their Australian counterparts, as evidenced by the lower scores for factors 1 (functional expectations) and 3 (need for cure). Our results from the thematic analysis also highlight some important findings; final year medical students are well acquainted with key chronic pain concepts present in the current guidelines on chronic pain management as described though the thematic analysis, however, they report that their education is still in need of improvements to cover more of these skills and concepts.
4.1 HC-PAIRS
The considerable difference in total HC-PAIRS score between our cohorts may be due to the fact that Swedish medical students gain experience in treating patients earlier than the Australian students, resulting in the Australian students having less experience with patients. But it could also be due to possible differences in other education aspects of the medical programme, national or regional clinical guidelines and cultural differences.
To allow us to compare the score results from other studies, we have normalised the final scores to a percentage of the attainable maximum score (Table 4). The normalised mean scores range from 41 to 67%, with our scores of 51 and 46% (Australian and Swedish, respectively) being in the middle of the range. Interestingly, the normalised mean score for the Australian students is higher than the British medical students, who have similar education system and health care system. As a caveat, it should be pointed out that scores will be dependent upon the items selected for the study, since some use all 15 items, whereas others do not. It would be beneficial to align the implementation of the HC-PAIRS instrument in order to achieve comparable results between future studies.
HC-PAIRS scores [mean, SD] for different health professionals and students of different health care-oriented programmes reported in the literature.
| HC-PAIRS total scores, mean (SD) | HC-PAIRS total score | Number of HC-PAIRS items | Likert scale | Maximum possible score | Score re-scaled to maximum possible score of 100 | Reference |
|---|---|---|---|---|---|---|
| Australian final year medical students | 51.0 (6.4) | 15 | Six-point | 90 | 56.7 | |
| Swedish final year medical students | 46.0 (6.2) | 15 | Six-point | 90 | 51.1 | |
| Swedish physical therapists | 41.8 (6.8) | 15 | Six-point | 90 | 46.4 | [28] |
| Various therapists | 48.1 (9.4) | 15 | Six-point | 90 | 53.4 | [22] |
| Australian physiotherapy students | 53.3 (9.2) | 15 | Seven-point | 105 | 50.8 | [26] |
| British medical students | 43.6 (N.R) | 15 | Seven-point | 105 | 41.5 | [34] |
| Cross-discipline health students | 46.3 (10.1) | 13 | Seven-point | 91 | 50.9 | [29] |
| Brazilian physical therapy students | 66.4 (8.5) | 15 | Seven-point | 105 | 63.2 | [35] |
| Saudi physical therapy students | 70.4 (9.6) | 15 | Seven-point | 105 | 67.0 | [36] |
-
NR=not reported.
Investigating different items, we found the most negative scores for item 10 “When their pain gets worse, chronic pain patients find it very hard to concentrate on anything else” and for item 13 “Chronic pain patients find themselves frequently thinking about their pain and what it has done to their life”. Swedish and Australian students believe that for chronic pain patients, when the pain gets worse, they find it very hard to concentrate on anything else; and that the patients find themselves frequently thinking about their pain and what it has done to their life. These views are potentially stigmatising: it appears students expect that chronic pain patients in general dwell on their pain, which is a highly negative generalised view that may have a negative impact on chronic pain treatment. The association between negative attitudes and beliefs of health care professional has repeatedly been linked with more negative patient treatment outcomes [37], [38]. It has also been shown that attitudes can be changed through education. Thus, Jacobs et al. demonstrated an improvement in HC-PAIRS scores of physiotherapists following a day course raising awareness of the biopsychosocial model for chronic pain [25]. Morris et al. [34] found a progression in positive attitudes towards chronic pain patients between 1st and final year medical students. It is thus clear how important education and knowledge is to improve health care students’ attitudes towards chronic pain.
4.2 Chronic pain education
It is reassuring that both Australian and Swedish final year medical students have a clear notion of current recommendations of chronic pain management. The top five subjects within chronic pain that need the most attention according to AAPM [18] can be recognised in our thematic analysis for both cohorts through themes such as “Patient attentiveness” and “Pain assessment”. Moreover, key chronic pain concepts such as the biopsychosocial model and pain management in multidisciplinary teams were also repeatedly acknowledged by our students within the theme “Biopsychosocial model”. Observed differences between cohorts could similarly be explained due to differences in the medical programmes. The Swedish medical programme is longer, currently comprising 11 semesters (5.5 years of studies) before entering the post graduate training, whilst the Australian programme ranges over 4 years before post graduate training. It appears that Swedish students obtain more experience seeing patients during this time which could be the reason for their willingness to have even more experience with chronic patients compared to Australian students who more frequently mentioned wanting more clinical vignette-based learning. Furthermore, Australian students seem to be assigned to rotations in a way that will result in differences in gained chronic pain education between individual students.
Regarding pharmacology training, there was a tendency for Australian students asking for more basal pharmacology training compared to the Swedish students who requested more clinical pharmacology in terms of treatment plans. Students at Umeå university obtain a 5-week course in pharmacology in the fifth semester of their studies whilst students at Notre Dame receive their pharmacology lectures throughout the programme, and this might have an impact on their respective needs. The worldwide issue with increased opioid prescribing in chronic pain management was repeatedly addressed by the Australian students but not the Swedish, this might be due to the current large focus on this subject in Australia exemplified here by a review from the National drug and Alcohol Research Centre [12]. Other reasons for differences in open-end answers can naturally be differences in expression between different languages and cultural differences.
Both cohorts described that chronic pain education and management is complex but a very important topic. The majority of students stated a general need for more knowledge on the subject including many suggestions for improvements such as increased training with other health care practitioners, more focus on the biopsychosocial model, practical experience with patients, pharmacology and treatment plans, more exposure to pain clinics and increased knowledge about non-pharmacological treatment. We consider our findings to be in line with those of Briggs et al. [17] who concluded that chronic pain training is scattered and unsatisfactory.
4.3 What this study contributes
It is important to know more about health care professionals and medical students’ attitudes towards chronic pain. Attitudes and beliefs are formed during medical education, and our study exploring attitudes of medical students towards chronic pain and how it is taught have provided valuable information. Our survey provided detailed and cohesive suggestions for education improvement that also are in line with current clinical guidelines. This study highlights several areas of interest that warrant further investigation, for example, the impact of a changed medical curriculum in alignment with these clinical guidelines requested by students in this survey, and correspondingly if their attitudes towards chronic pain patients can be improved through education. Further, it would be valuable to align the implementation of the HC-PAIRS instrument in order to achieve comparable results between future studies and we consider this an important subject to be addressed by future research.
4.4 Strengths and limitations
Recruiting students was challenging in both countries and a higher response rate would have been favourable. Further there was a considerable attrition rate throughout, and these factors should be taken into consideration with respect to the interpretation of the data. Nonetheless, our results are in line with the results of other studies such as those on medical education across Europe [17], and our HC-PAIRS are within the range reported in other studies (see Table 4). We thus add HC-PAIRS scores from two key cohorts in near future chronic pain management, from two different countries to the literature, and the need for more chronic pain education amongst both student cohorts is evident through our thematic analysis.
There were more females than males who completed the study, and many of them knew someone suffering to chronic pain, thus suggesting there might be risk of selection bias. However, our linear model analysis would suggest that these factors did not significantly contribute to the outcome of the HC-PAIRS scores (see Supplementary Table 3).
5 Conclusions
Australian and Swedish medical students have different attitudes towards chronic non-malignant pain. Australian medical students have more negative attitudes towards chronic pain patients than Swedish medical students. Medical students in Sweden and Australia recognise important concepts included in chronic pain clinical guidelines. However, they call for more chronic pain education. Given the importance of education in shaping attitudes to patient treatment strategies, this call should be heeded.
Acknowledgments
The authors would like to thank the students and physicians helping us in pilot-testing the survey. We also want to thank Drs. Richard Day, Andrew Rice and Arja Lehti for their useful feedback and advice.
-
Authors’ statements
-
Research funding: Part of this work was supported by grants from the Swedish Research Council (a Scheele visiting fellowship to GG and a project grant, no. 12158 to CJF). For the remaining authors, none were declared.
-
Conflict of interest: No conflicts of interest are declared.
-
Informed consent: Consent was obtained from all study participants. All responses were codified and kept confidential.
-
Ethical approval: This study was reviewed by both the Regional Ethical Review Board in Umeå 2015-09-08 and by the University of Notre Dame Ethics Committee. Ethics approval was granted by The University of Notre Dame Ethics Committee (HREC Ref 0170025). The Regional Ethics Review Board in Umeå returned it with an advisory opinion; because participation in the survey was fully anonymized, it was not considered to require a formal approval.
References
[1] Blyth FM, March LM, Brnabic AJ, Jorm LR, Williamson M, Cousins MJ. Chronic pain in Australia: a prevalence study. Pain 2001;89:127–34.10.1016/S0304-3959(00)00355-9Search in Google Scholar PubMed
[2] MBF Foundation. The high price of pain: The economic impact of chronic pain in Australia 2007. Report conducted by Access Economics in collaboration with the University of Sydney University of Sydney Pain Management Reseach Institute. Australia; 2007 November.Search in Google Scholar
[3] Harker J, Reid KJ, Bekkering GE, Kellen E, Bala MM, Riemsma R, Worthy G, Misso K, Kleijnen J. Epidemiology of chronic pain in Denmark and Sweden. Pain Res Treat 2012;2012:371248.10.1155/2012/371248Search in Google Scholar PubMed PubMed Central
[4] Statens beredning för medicinsk utvärdering. Metoder för behandling av långvarig smärta: en systematisk litteraturöversikt. V. 1. V. 1. Stockholm: Statens beredning för medicinsk utvärdering (SBU); 2006.Search in Google Scholar
[5] International Organization for the Study of Pain (IASP). Classification of Chronic Pain, Second Edition (Revised). Available at: http://www.iasp-pain.org/PublicationsNews/Content.aspx?ItemNumber=1673&navItemNumber=677) Accessed: 10 Aug 2017.Search in Google Scholar
[6] Fornasari D. Pain mechanisms in patients with chronic pain. Clin drug invest 2012;32:45–52.10.2165/11630070-000000000-00000Search in Google Scholar PubMed
[7] Sarzi-Puttini P, Vellucci R, Zuccaro SM, Cherubino P, Labianca R, Fornasari D. The appropriate treatment of chronic pain. Clin drug invest 2012;32:21–33.10.2165/11630050-000000000-00000Search in Google Scholar PubMed
[8] Breivik H, Collett B, Ventafridda V, Cohen R, Gallacher D. Survey of chronic pain in Europe: prevalence, impact on daily life, and treatment. Eur J Pain 2006;10:287–333.10.1016/j.ejpain.2005.06.009Search in Google Scholar PubMed
[9] EFIC. Pain proposal improving the current and future management of chronic pain. A European Consensus Report. 2010. Available at: https://www.pfizer.es/docs/pdf/noticias/Pain_Proposal_European_Consensus_Report_FINAL.pdf. Accessed: 7 Feb 2018.Search in Google Scholar
[10] Gatchel RJ, McGeary DD, McGeary CA, Lippe B. Interdisciplinary chronic pain management: past, present, and future. Am Psychol 2014;69:119–30.10.1037/a0035514Search in Google Scholar PubMed
[11] Gatchel RJ, Peng YB, Peters ML, Fuchs PN, Turk DC. The biopsychosocial approach to chronic pain: Scientific advances and future directions. Psychol Bull 2007;133:581–624.10.1037/0033-2909.133.4.581Search in Google Scholar PubMed
[12] National Drug and Alcohol Research Centre. A review of opioid prescribing in Tasmania: a blueprint for the future. Sydney: UNSW, 2012.Search in Google Scholar
[13] Sinatra R. Causes and consequences of inadequate management of acute pain. Pain Med 2010;11:1859–71.10.1111/j.1526-4637.2010.00983.xSearch in Google Scholar PubMed
[14] Notcutt W, Gibbs G. Inadequate pain management: myth, stigma and professional fear. Postgrad Med J 2010;86:453–8.10.1136/pgmj.2008.077677Search in Google Scholar PubMed
[15] National Pain Summit Initiative. National Pain Strategy. Melbourne: Faculty of Pain Medicine, 2010.Search in Google Scholar
[16] Kress HG, Aldington D, Alon E, Coaccioli S, Collett B, Coluzzi F, Huygen F, Jaksch W, Kalso E, Kocot-Kępska M, Mangas AC, Ferri CM, Mavrocordatos P, Morlion B, Müller-Schwefe G, Nicolaou A, Hernández CP, Sichère P. A holistic approach to chronic pain management that involves all stakeholders: change is needed. Curr Med Res Opin 2015;31:1743–54.10.1185/03007995.2015.1072088Search in Google Scholar PubMed
[17] Briggs EV, Battelli D, Gordon D, Kopf A, Ribero S, Puig MM, Kress HG. Current pain education within undergraduate medical studies across Europe: Advancing the Provision of Pain Education and Learning (APPEAL) study. BMJ Open 2015;5:e006984.10.1136/bmjopen-2014-006984Search in Google Scholar PubMed PubMed Central
[18] Murinson BB, Gordin V, Flynn S, Driver LC, Gallagher RM, Grabois M. Recommendations for a new curriculum in pain medicine for medical students: toward a career distinguished by competence and compassion. Pain Med 2013;14:345–50.10.1111/pme.12051Search in Google Scholar PubMed PubMed Central
[19] Hirsh AT, Hollingshead NA, Bair MJ, Matthias MS, Kroenke K. Preferences, experience, and attitudes in the management of chronic pain and depression: a comparison of physicians and medical students. Clin J Pain 2014;30:766–74.10.1097/AJP.0000000000000035Search in Google Scholar PubMed
[20] Lancsar E, Louviere J. Conducting discrete choice experiments to inform healthcare decision making: a user’s guide. Pharmacoeconomics 2008;26:661–7.10.2165/00019053-200826080-00004Search in Google Scholar PubMed
[21] Hollingshead NA, Meints S, Middleton SK, Free CA, Hirsh AT. Examining influential factors in providers’ chronic pain treatment decisions: a comparison of physicians and medical students. BMC Med Educ 2015;15:164.10.1186/s12909-015-0441-zSearch in Google Scholar PubMed PubMed Central
[22] Houben RM, Vlaeyen JW, Peters M, Ostelo RW, Wolters PM, Stomp-van den Berg SG. Health care providers’ attitudes and beliefs towards common low back pain: factor structure and psychometric properties of the HC-PAIRS. Clin J Pain 2004;20:37–44.10.1097/00002508-200401000-00008Search in Google Scholar PubMed
[23] Rainville J, Bagnall D, Phalen L. Health care providers’ attitudes and beliefs about functional impairments and chronic back pain. Clin J Pain 1995;11:287–95.10.1097/00002508-199512000-00006Search in Google Scholar PubMed
[24] Epstein-Sher S, Jaffe DH, Lahad A. Are they complying? physicians’ knowledge, attitudes & readiness-to-change regarding low back pain treatment guideline adherence. Spine 2017;15;42:247–52.10.1097/BRS.0000000000001714Search in Google Scholar PubMed
[25] Jacobs CM, Guildford BJ, Travers W, Davies M, McCracken LM. Brief psychologically informed physiotherapy training is associated with changes in physiotherapists’ attitudes and beliefs towards working with people with chronic pain. Br J Pain 2016;10:38–45.10.1177/2049463715600460Search in Google Scholar PubMed PubMed Central
[26] Latimer J, Maher C, Refshauge K. The attitudes and beliefs of physiotherapy students to chronic back pain. Clin J Pain 2004;20:45–50.10.1097/00002508-200401000-00009Search in Google Scholar PubMed
[27] Slater H, Briggs AM, Smith AJ, Bunzli S, Davies SJ, Quintner JL. Implementing evidence-informed policy into practice for health care professionals managing people with low back pain in Australian rural settings: a preliminary prospective single-cohort study. Pain Med 2014;15:1657–68.10.1111/pme.12351Search in Google Scholar PubMed
[28] Overmeer T, Boersma K, Main CJ, Linton SJ. Do physical therapists change their beliefs, attitudes, knowledge, skills and behaviour after a biopsychosocially orientated university course? J Eval Clin Pract 2009;15:724–32.10.1111/j.1365-2753.2008.01089.xSearch in Google Scholar PubMed
[29] Briggs AM, Slater H, Smith AJ, Parkin-Smith GF, Watkins K, Chua J. Low back pain-related beliefs and likely practice behaviours among final-year cross-discipline health students. Eur J Pain 2013;17:766–75.10.1002/j.1532-2149.2012.00246.xSearch in Google Scholar PubMed
[30] R Core Team: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria, 2017; https://www.R-project.org.Search in Google Scholar
[31] Benjamini Y, Hochberg Y. Controlling the false discovery rate: a practical and powerful approach to multiple testing. JR Statist Soc B 2011;57:289–300.10.1111/j.2517-6161.1995.tb02031.xSearch in Google Scholar
[32] Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol 2006;3:77–101.10.1191/1478088706qp063oaSearch in Google Scholar
[33] Brown JD. Likert items and scales of measurement? SHIKEN: JALT Testing & Evaluation SIG Newsletter 2011;15:10–4.Search in Google Scholar
[34] Morris H, Ryan C, Lauchlan D, Field M. Do medical student attitudes towards patients with chronic low back pain improve during training? a cross-sectional study. BMC Med Educ 2012;12:10.10.1186/1472-6920-12-10Search in Google Scholar PubMed PubMed Central
[35] Ferreira PH, Ferreira ML, Latimer J, Maher CG, Refshauge K, Sakamoto A, Garofalo R. Attitudes and beliefs of Brazilian and Australian physiotherapy students towards chronic back pain: a cross-cultural comparison. Physiother Red Int 2004;9:13–23.10.1002/pri.296Search in Google Scholar PubMed
[36] Alshami AM, Albahrani YA. A comparison of the attitudes toward chronic low back pain in Saudi, Australian and Brazilian physical therapy students. J Taibah Uni Med Sci 2015;10:181–7.10.1016/j.jtumed.2014.11.008Search in Google Scholar
[37] Greville-Harris M, Dieppe P. Bad is more powerful than good: the nocebo response in medical consultations. Am J Med 2015;128:126–9.10.1016/j.amjmed.2014.08.031Search in Google Scholar PubMed
[38] Darlow B, Fullen BM, Dean S, Hurley DA, Baxter GD, Dowell A. The association between health care professional attitudes and beliefs and the attitudes and beliefs, clinical management, and outcomes of patients with low back pain: a systematic review: The association between health care professional attitudes and outcomes of patients with low back pain. Eur J Pain 2012;16:3–17.10.1016/j.ejpain.2011.06.006Search in Google Scholar PubMed
Supplementary Material
The online version of this article offers supplementary material (https://doi.org/10.1515/sjpain-2018-0039).
©2018 Scandinavian Association for the Study of Pain. Published by Walter de Gruyter GmbH, Berlin/Boston. All rights reserved.
Articles in the same Issue
- Frontmatter
- Editorial comment
- Diagnosis of carpal tunnel syndrome
- Body image concerns and distortions in people with persistent pain
- The prevalence of recurrent pain in childhood is high and increases with age
- Friends in pain: pain tolerance in a social network
- Clinical pain research
- Correlation of clinical grading, physical tests and nerve conduction study in carpal tunnel syndrome
- Spectroscopic differences in posterior insula in patients with chronic temporomandibular pain
- Deconstructing chronicity of musculoskeletal pain: intensity-duration relations, minimal dimensions and clusters of chronicity
- “When I feel the worst pain, I look like shit” – body image concerns in persistent pain
- The prevalence of neck-shoulder pain, back pain and psychological symptoms in association with daytime sleepiness – a prospective follow-up study of school children aged 10 to 15
- The neglected role of distress in pain management: qualitative research on a gastrointestinal ward
- Pain mapping of the anterior knee: injured athletes know best
- The role of pain in chronic pain patients’ perception of health-related quality of life: a cross-sectional SQRP study of 40,000 patients
- The DoloTest® in a specialized headache center among patients receiving psychological treatment. A pilot study
- Observational study
- Chronic pelvic pain – pain catastrophizing, pelvic pain and quality of life
- Survey of chronic pain in Chile – prevalence and treatment, impact on mood, daily activities and quality of life
- Patients’ pre-operative general and specific outcome expectations predict postoperative pain and function after total knee and total hip arthroplasties
- The peer effect on pain tolerance
- Original experimental
- The effects of propranolol on heart rate variability and quantitative, mechanistic, pain profiling: a randomized placebo-controlled crossover study
- Idiographic measurement of depressive thinking: development and preliminary validation of the Sentence Completion Test for Chronic Pain (SCP)
- Adding steroids to lidocaine in a therapeutic injection regimen for patients with abdominal pain due to anterior cutaneous nerve entrapment syndrome (ACNES): a single blinded randomized clinical trial
- The influence of isometric exercise on endogenous pain modulation: comparing exercise-induced hypoalgesia and offset analgesia in young, active adults
- Do pain-associated contexts increase pain sensitivity? An investigation using virtual reality
- Differences in Swedish and Australian medical student attitudes and beliefs about chronic pain, its management, and the way it is taught
- An experimental investigation of the relationships among race, prayer, and pain
- Educational case report
- Wireless peripheral nerve stimulation for complex regional pain syndrome type I of the upper extremity: a case illustration introducing a novel technology
Articles in the same Issue
- Frontmatter
- Editorial comment
- Diagnosis of carpal tunnel syndrome
- Body image concerns and distortions in people with persistent pain
- The prevalence of recurrent pain in childhood is high and increases with age
- Friends in pain: pain tolerance in a social network
- Clinical pain research
- Correlation of clinical grading, physical tests and nerve conduction study in carpal tunnel syndrome
- Spectroscopic differences in posterior insula in patients with chronic temporomandibular pain
- Deconstructing chronicity of musculoskeletal pain: intensity-duration relations, minimal dimensions and clusters of chronicity
- “When I feel the worst pain, I look like shit” – body image concerns in persistent pain
- The prevalence of neck-shoulder pain, back pain and psychological symptoms in association with daytime sleepiness – a prospective follow-up study of school children aged 10 to 15
- The neglected role of distress in pain management: qualitative research on a gastrointestinal ward
- Pain mapping of the anterior knee: injured athletes know best
- The role of pain in chronic pain patients’ perception of health-related quality of life: a cross-sectional SQRP study of 40,000 patients
- The DoloTest® in a specialized headache center among patients receiving psychological treatment. A pilot study
- Observational study
- Chronic pelvic pain – pain catastrophizing, pelvic pain and quality of life
- Survey of chronic pain in Chile – prevalence and treatment, impact on mood, daily activities and quality of life
- Patients’ pre-operative general and specific outcome expectations predict postoperative pain and function after total knee and total hip arthroplasties
- The peer effect on pain tolerance
- Original experimental
- The effects of propranolol on heart rate variability and quantitative, mechanistic, pain profiling: a randomized placebo-controlled crossover study
- Idiographic measurement of depressive thinking: development and preliminary validation of the Sentence Completion Test for Chronic Pain (SCP)
- Adding steroids to lidocaine in a therapeutic injection regimen for patients with abdominal pain due to anterior cutaneous nerve entrapment syndrome (ACNES): a single blinded randomized clinical trial
- The influence of isometric exercise on endogenous pain modulation: comparing exercise-induced hypoalgesia and offset analgesia in young, active adults
- Do pain-associated contexts increase pain sensitivity? An investigation using virtual reality
- Differences in Swedish and Australian medical student attitudes and beliefs about chronic pain, its management, and the way it is taught
- An experimental investigation of the relationships among race, prayer, and pain
- Educational case report
- Wireless peripheral nerve stimulation for complex regional pain syndrome type I of the upper extremity: a case illustration introducing a novel technology

