Abstract
Background and aims:
Pressure pain threshold (PPT) and PPT maps are commonly used to quantify and visualize mechanical pain sensitivity. Although PPT’s have frequently been reported from patients with knee osteoarthritis (KOA), the absolute and relative reliability of PPT assessments remain to be determined. Thus, the purpose of this study was to evaluate the test-retest relative and absolute reliability of PPT in KOA. For that purpose, intra- and interclass correlation coefficient (ICC) as well as the standard error of measurement (SEM) and the minimal detectable change (MDC) values within eight anatomical locations covering the most painful knee of KOA patients was measured.
Methods:
Twenty KOA patients participated in two sessions with a period of 2 weeks±3 days apart. PPT’s were assessed over eight anatomical locations covering the knee and two remote locations over tibialis anterior and brachioradialis. The patients rated their maximum pain intensity during the past 24 h and prior to the recordings on a visual analog scale (VAS), and completed The Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) and PainDetect surveys. The ICC, SEM and MDC between the sessions were assessed. The ICC for the individual variability was expressed with coefficient of variance (CV). Bland-Altman plots were used to assess potential bias in the dataset.
Results:
The ICC ranged from 0.85 to 0.96 for all the anatomical locations which is considered “almost perfect”. CV was lowest in session 1 and ranged from 44.2 to 57.6%. SEM for comparison ranged between 34 and 71 kPa and MDC ranged between 93 and 197 kPa with a mean PPT ranged from 273.5 to 367.7 kPa in session 1 and 268.1–331.3 kPa in session 2. The analysis of Bland-Altman plot showed no systematic bias. PPT maps showed that the patients had lower thresholds in session 2, but no significant difference was observed for the comparison between the sessions for PPT or VAS. No correlations were seen between PainDetect and PPT and PainDetect and WOMAC.
Conclusions:
Almost perfect relative and absolute reliabilities were found for the assessment of PPT’s for KOA patients.
Implications:
The present investigation implicates that PPT’s is reliable for assessing pain sensitivity and sensitization in KOA patients.
1 Introduction
Knee osteoarthritis (KOA) is the most common type of arthrosis. In year 2010, approximately 250 million people suffered from KOA more or less caused by the breakdown of joint tissues from mechanical loading and inflammation [1], [2], [3]. Pain and pain sensitization are key symptoms of KOA impacting the healthcare utilization and quality of life. Different quantitative measures, e.g. mechanical, thermal, electrical and chemical modalities have been developed to assess pain sensitization in patients with KOA [4], [5].
Pressure algometry has been used as a method to assess mechanical pain sensitivity in different anatomical regions for KOA patients and to construct pressure pain threshold (PPT) maps [6]. The handheld algometer provides quantitative values related to deep structures. By applying it perpendicular to the skin, it co-activate group III and group IV muscle nociceptors [7]. The PPT maps enable the visualization and quantification of the spatial distribution of mechanical sensitivity to pain [8], [9], [10], [11], [12]. Central sensitization is assumed to be one of the underlying factors for OA patients. Continuous and intense nociceptive input from a damaged joint may contribute to sensitization by enhanced pain responses, the spread of pain to larger body areas, and outside the symptomatic joint [8], [13], [14]. Previous studies have demonstrated PPT to have a high relative reliability in various anatomical locations like knee [15], [16], neck [17], [18], and lower back [19], [20] both in patients and in healthy humans. However, the reliability of PPT is influenced by factors such as gender, age, investigator and [19], [21]. Although, studies have concluded that PPT is a useful pain assessment tool in patients with KOA [22], [23] the standard error of measurement (SEM), intra- and interclass correlation coefficients (ICCs), and minimum detectable change (MDC) have not been fully evaluated in KOA. In order to e.g. monitor the effectiveness of an intervention, it is essential to have reliable tools assessing mechanical pressure sensitivity to pain. The aim of the present study was to establish the test-retest reliability of PPT for patients with KOA as well as to determine the MDC, ICCs, and SEM. The present study complies with the guidelines for reporting reliability and agreement studies (GRRAS) [24].
2 Methods
2.1 Participants
Twenty KOA patients, ranging from 59 to 80 years participated in this study (Table 1). The KOA patients were recruited from a centralized database at the Centre for Clinical and Basic Research (CCBR) and diagnosed according to American College of Rheumatology classification. Clinical data was collected from patients, including radiological evaluation, medication and pain duration. The inclusion criteria were aged 18–80 years, clinically diagnosed with knee OA, Kellgren-Lawrence X-ray grade ≥2, pain while walking according to the patient and BMI <35. No subjects had used any analgesics within the previous 24 h prior to the experiment. The subjects were given a detailed written and verbal explanation and they signed an informed consent form before participating in the study. The study had been approved by the local Ethics Committee (VN-20160081) and conducted according to the Declaration of Helsinki.
Characteristics of the subjects.
| Characteristics | Mean±SD |
|---|---|
| Age (years) | 70.3 (5.8) |
| Sex (female/male) | 9/11 |
| Body mass (kg) | 81.5 (12.6) |
| Height (cm) | 169.8 (8.8) |
| Body mass index, BMI (kg/m2) | 28.1 (2.6) |
| Kellgren Lawrence score (left/right) | 2.7 (0.8) |
-
Demographics of the patients with knee osteoarthritis included in the study. Values are presented as mean (±SD) (n=20).
2.2 Experimental protocol
The experiment consisted of two sessions was conducted at CCBR. Session 1 was followed 2 weeks±3 days later by session 2. All the subjects were asked to rate the maximum intensity of pain on a 0–10 cm horizontal visual analog scale (VAS) ranging from 0 to 10 for the worst pain from the most painful knee during the past 24 h and after 5 min rest prior to the PPT recordings. The VAS was anchored with 0=no pain and 10=worst pain imaginable, and the distance (cm) of the subject’s mark on the horizontal line was the outcome measure. The most painful knee was selected for assessment for all the patients. The subjects were lying comfortably in a supine position. A handheld algometer (type II, Somedic AB, Sweden) with a tip area of 1 cm2 was used to assess PPTs from ten anatomical locations in a randomized order. All assessments were made by the same examiner. A mechanical pressure stimulus with an ascending pressure gradient of 30 kPa/s was applied continuously until the subjects felt pain and pressed a stop-button. The pressure indicated on the algometer display corresponding to the PPT where noted by the examiner. The PPT recordings were performed three times and the mean value was used for statistical analysis. To avoid temporal integration [9], [25], a 1-min interval was observed between the PPT assessments. To make sure the subject was confident with the method, a test PPT measurement was tested prior to recordings on the bulk of the tibialis anterior on the contralateral leg. Additionally, each subject completed a knee-directed The Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) survey and a PainDetect survey. WOMAC is a standardized subject-rated instrument for measuring pain severity and pain interference scores [26]. The WOMAC questionnaire consists of 24 questions focusing on pain (score range 0–20), stiffness (score range 0–8), and functional limitations (score range 0–68) of the OA knee during the past 48 h [26].
PainDetect is a questionnaire to assess the neuropathic components of chronic pain conditions [27]. A total score of ≤12 indicate a neuropathic pain component is unlikely, and a total score of ≥19 indicate that a neuropathic pain component is likely. A total score of 13–18 are uncertain [27].
2.3 Pressure pain threshold
Eight PPT sites were marked over the knee in the peripatellar region and two control points according to our previous study [8]. The eight test points are defined as (1) 2 cm distal to the inferomedial edge of patella; (2) 2 cm distal to the inferolateral edge of patella; (3) 3 cm lateral to the center of the lateral edge of patella; (4) 2 cm proximal to the superolateral edge of patella; (5) 2 cm proximal to the superior edge of patella; (6) 2 cm proximal to the superomedial edge of patella; (7) 3 cm medial to the center of the medial edge of patella; (8) on the center of patella. The two extra segmental sites were (9) the belly of the tibialis anterior muscle and (10) in the center of brachioradialis ipsilateral to the selected knee (Fig. 1). Points 9 and 10 enabled to assess from external sites to evaluate generalized sensitization.
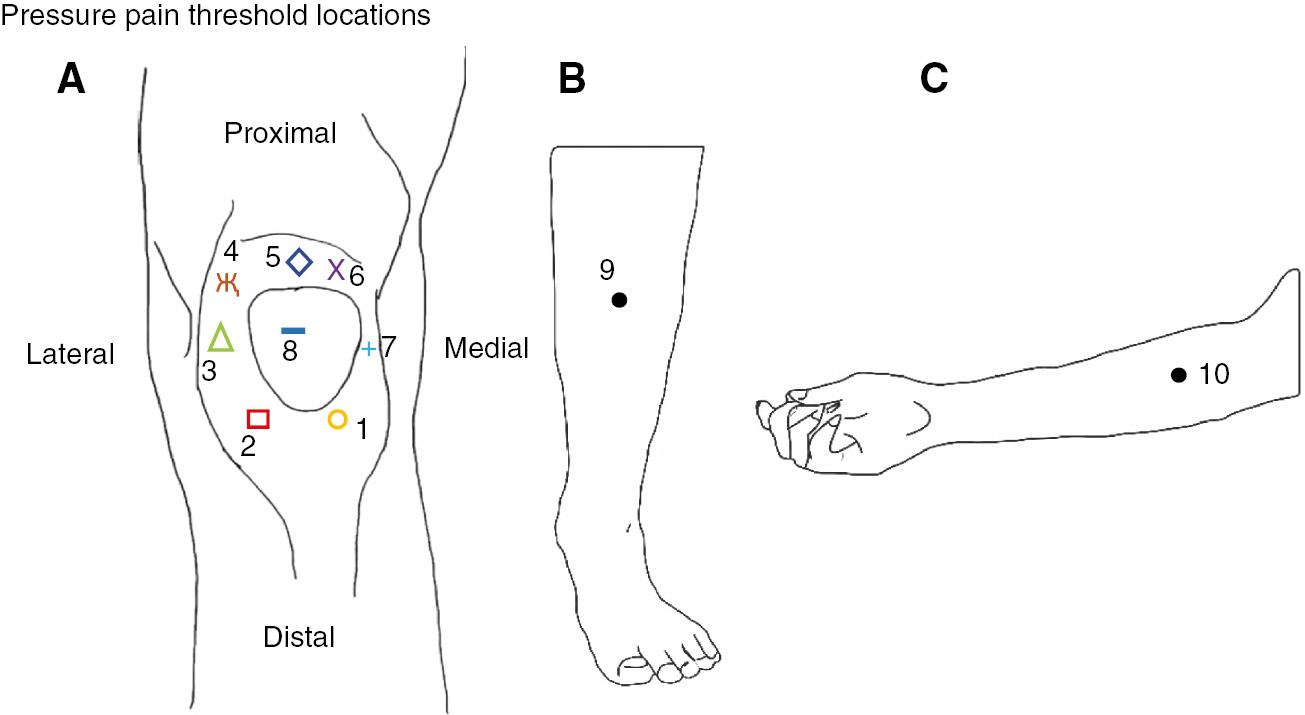
Location of the assessed eight pressure pain threshold (PPT) points on the knee (A) and the two control points (B and C).
PPT maps were generated by interpolating mean PPT values using an inverse distance-weighted interpolation to compute PPT values of the unknown locations. This was obtained by using mean scores from the known PPT values and locations [8], [9].
2.4 Data analysis
The data were analyzed using a repeated measure of variance (ANOVA) with the factor sites (10 test sites) and sessions (two sessions). A student t-test for pair-wise comparisons was used as post hoc test to compare PPT’s between the sessions, in case of significant main effect. A paired sample t-test was performed to test for differences in VAS between the sessions and for differences in WOMAC sub scores between the sessions. The relative and absolute reliability across the sessions were computed using intra-class correlation coefficients (ICC2,1 for absolute agreement), SEM and MDC. ICC were interpreted according to Landis and Koch in which an ICC between 0.00 and 0.20 is considered “poor”, 0.21–0.40 is “fair”, 0.41–0.60 is “moderate”, 0.61–0.80 is “substantial”, and 0.81–1.00 is “almost perfect” [28]. The inter-class correlation coefficient was calculated with the coefficient of variance (CV) and reflects the overall variability of the model. CV is expressed in % and is calculated as:
SEM represents measurement error, which means it represent if a patient’s measurements vary if the test is repeated without any underlying change in the patient. SD is the standard deviation of the PPT from patients in both sessions and the ICC are the relative reliability. SEM has the same unit as pain sensitivity (kPa) and are calculated with the following formula [29]:
MDC indicates the minimum value for which a difference can be considered as real. The formula for MDC is the following [30]:
Furthermore, Bland Altman plot of differences between sessions against their mean and limits of agreement (LOA) were used to assess the disagreement between the PPT’s in the two sessions. A real change can be considered, in case a difference between sessions are seen outside LOA [29]. The Spearmans correlation test between PainDetect and WOMAC sub-scores and PainDetect and PPT’s for both sessions were analyzed. All the statistical analysis was performed using the statistical program software IBM SPSS version 25, and p<0.05 was considered significant.
3 Results
3.1 Intra- and inter-session reliability
The intra-session reliability indicators at each PPT location are reported in Table 2 and inter-session reliability are reported in Table 3. The ICCs of the 10 anatomical locations were “almost perfect” according to the definition [28] ranging from 0.85 to 0.96. The inter-individual variation (CV) was smaller in session 1 (44.2–57.6%) than session 2 (47.9–62.7%). SEM values ranged from 34 to 71 kPa and MDC ranged from 93 to 196 kPa and the mean PPT ranged from 273.5 to 367.7 kPa in session 1 and 268.1–331.3 kPa in session 2. The analysis of the Bland-Altman plot showed that no apparent systematic bias was present in the data and that zero was included in the 95% confidence interval. Upper-lower LOA were 216 and −156 kPa while the bias was 30 kPa. Differences between the sessions can be seen outside LOA, which indicates a real change (Fig. 2).
Mean, standard deviation (SD), intra-class correlation coefficient (ICC), standard error of measurement (SEM) and minimum detectable change (MDC) for pressure pain threshold (PPT) assessed over 10 locations (PPT 1–PPT 8) over the most painful knee as well as the two extra segmental sites (PPT 9–PPT 10) between the mean of the session 1 and session 2.
| Point | Session 1 (mean±SD, kPa) | Session 2 (mean±SD, kPa) | ICC [95% CI] | SEM (kPa) | MDC (kPa) |
|---|---|---|---|---|---|
| PPT 1 | 353.7±167.3 | 324±180.6 | 0.89 [0.73, 0.96] | 57.2 | 158.6 |
| PPT 2 | 349.7±201.4 | 322.8±171.2 | 0.85 [0.62, 0.94] | 70.8 | 196.3 |
| PPT 3 | 331.2±168.3 | 315.8±198.0 | 0.91 [0.78, 0.97] | 52.2 | 144.8 |
| PPT 4 | 305.9±163.0 | 274.1±143.8 | 0.89 [0.72, 0.96] | 49.6 | 137.4 |
| PPT 5 | 348.1±162.6 | 306.4±161.9 | 0.92 [0.77, 0.97] | 45.4 | 125.9 |
| PPT 6 | 320.7±170.0 | 288.9±156.2 | 0.96 [0.87, 0.98] | 33.5 | 92.9 |
| PPT 7 | 324.5±178.9 | 288.4±171.1 | 0.94 [0.83, 0.98] | 42.2 | 117.0 |
| PPT 8 | 336.1±148.4 | 312.1±154.1 | 0.90 [0.76, 0.96] | 45.5 | 126.2 |
| PPT 9 | 367.7±178.9 | 331.3±158.6 | 0.85 [0.64, 0.94] | 63.0 | 174.6 |
| PPT 10 | 273.5±136.2 | 268.1±132.5 | 0.88 [0.70, 0.95] | 44.6 | 123.7 |
-
Test-retest reliability at each PPT location. Values in parentheses are 95% confidence interval.
Coefficient of variance (CV) expressed in % for session 1 and session 2.
| PPT 1 | PPT 2 | PPT 3 | PPT 4 | PPT 5 | PPT 6 | PPT 7 | PPT 8 | PPT 9 | PPT 10 | |
|---|---|---|---|---|---|---|---|---|---|---|
| Session 1 CV (%) | 47.3 | 57.6 | 50.8 | 53.3 | 46.7 | 53.0 | 55.1 | 44.2 | 48.64 | 49.8 |
| Session 2 CV (%) | 55.8 | 53.0 | 62.7 | 52.5 | 52.8 | 54.1 | 59.4 | 49.4 | 47.9 | 49.4 |
-
Inter-individual correlation coefficient. CV reflects the overall variability of the model.
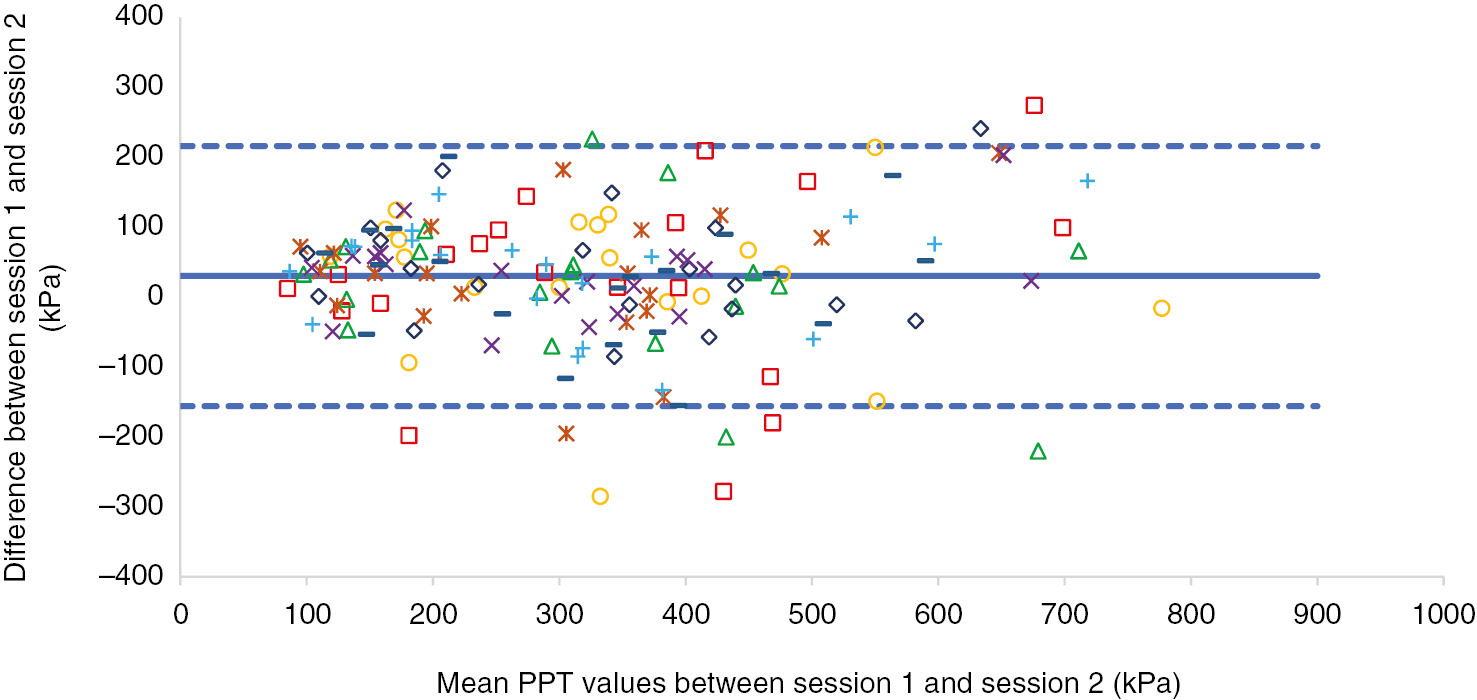
Bland and Altman analysis plotted for the differences of patient’s pressure pain threshold (PPT) in the eight locations around the knee for the mean of session 1 and session 2. Solid line represents mean difference and the dashed lines the limits of agreement (LOA). Upper LOA, 216 kPa; lower LOA, −156 kPa; bias, 30 kPa. PPT locations around the knee: 1:  , 2:
, 2:  , 3:
, 3:  , 4:
, 4:  , 5:
, 5:  , 6:
, 6:  , 7:
, 7:  , 8:
, 8:  .
.
3.2 Pressure pain threshold
PPT maps showed that the patients were most sensitive at the location of superolateral edge of patella (PPT 4), superomedial edge of patella (PPT 6) and medial to the center of the medial edge of patella (PPT 7) (Fig. 3). The PPT’s from the 10 anatomical locations were not significantly different from session 1 to session 2 (p=0.074) though lower PPT was seen in session 2 (Table 2). Likewise, the VAS scores for the past 24 h and after resting in 5 min were not significantly different between the sessions (Fig. 4).
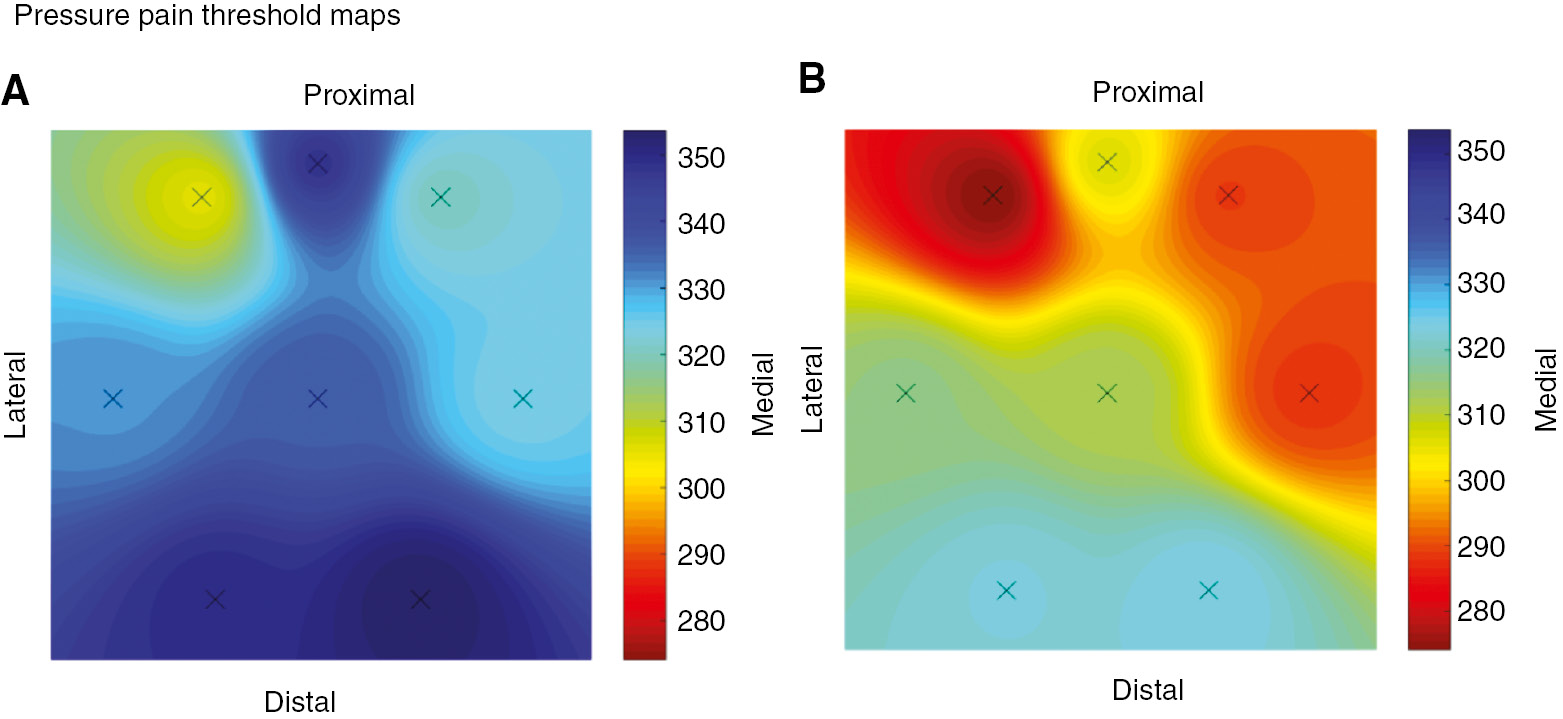
Anterior view of mean pressure pain threshold (PPT) maps from the eight anatomical locations on the knee (kPa) in session 1 (A) and session 2 (B). No significant difference was seen between the sessions (n=20).
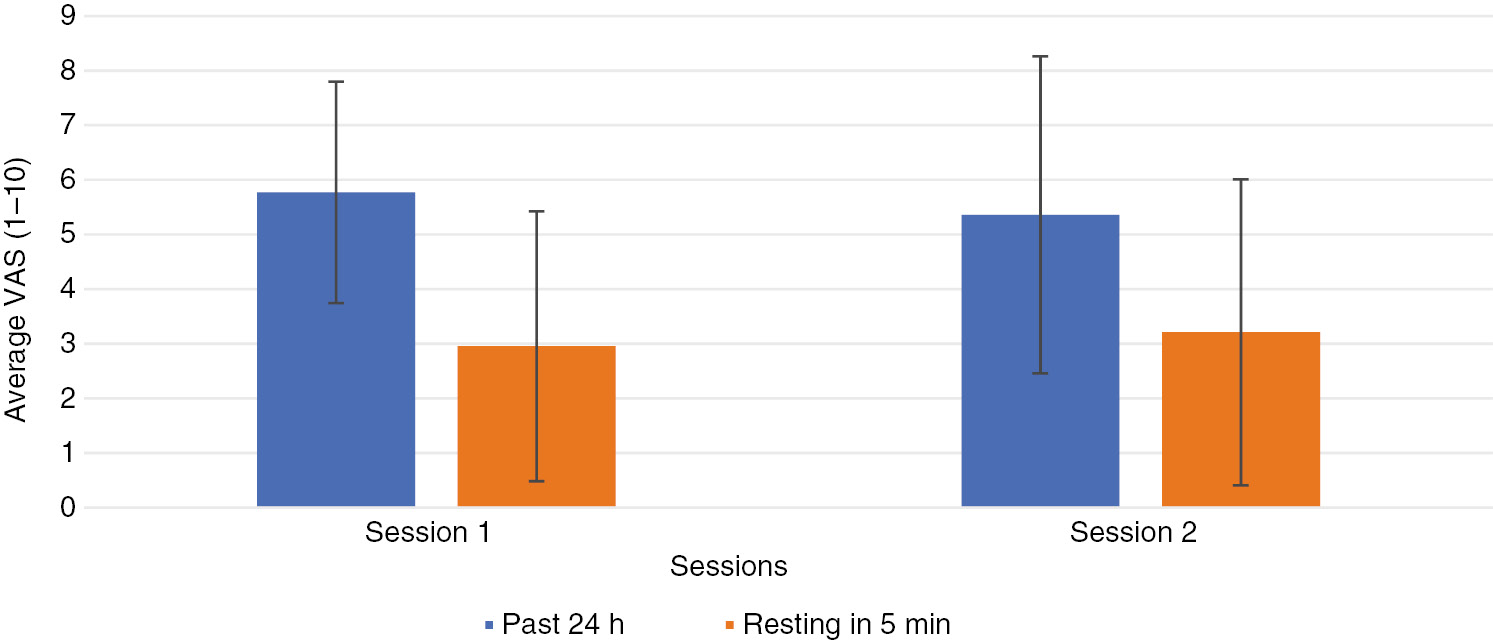
Mean±SD visual analog scale (VAS) values for the maximum pain in the most painful knee in the past 24 h and after resting for 5 min. X-axis indicates the session and Y-axis indicates VAS score (0–10).
No significant correlations were found between PainDetect and WOMAC for pain, stiffness, function or total score and between PainDetect and PPTs when evaluating data from session 1.
3.3 Pain questionnaire surveys
The PainDetect questionnaire was calculated with a maximum possible score of 38 and a minimum score of −1. At screening, 11 subjects had a score ≤12, and only two had a score ≥19 in session 1 and in session 2, 13 subjects had a score ≤12, and two subjects had a score ≥19 indicating that most of the subjects had pain, but unlikely to have neuropathic component. For the WOMAC sub scores, a significant difference was seen for stiffness between the two sessions (p=0.002), but no difference in total score for pain or physical function were seen between the two sessions (Table 4).
The three subscales are pain, stiffness and physical function.
| Session 1 | Session 2 | % Change | Difference, p | |
|---|---|---|---|---|
| Pain total | 172 | 163 | 5.2 | 0.407 |
| Stiffness total | 77 | 63 | 18.2 | 0.002a |
| Function total | 474 | 482 | 1.7 | 0.764 |
| Total score | 723 | 708 | 2.1 | 0.630 |
-
Mean WOMAC subscale and total scores. The percentage changes between the sessions are given. p Indicates differences between groups and aindicates significant difference.
4 Discussion
This study demonstrated an almost perfect intra-session reliability of the PPT’s measured over eight locations around the knee in KOA patients. The inter-individual reliability (CV%) showed a high variation in both sessions whereas the individual variance was acceptable. The individual difference of sensitivity to painful stimuli could be considered as factors that might affect the inter-individual variance besides gender and age differences. There were no significant differences between sessions among the eight PPTs at the various knee locations. However, the PPT maps illustrated the tendency towards lower PPT values in session 2 compared with session 1. This tendency was actually associated with higher VAS after resting for 5 min. These tendencies underlined temporal changes (approx. 2 weeks separated the two sessions) in pain intensity and mechanical sensitivity in patients with KOA supporting previous findings that the PPT as a measure for muscle hyperalgesia also reflect changes in clinical pain intensity [31].
The findings are supporting the study by Wylde et al. [32] who showed no significant difference over a period of 1-week for the PPT at the medial side of right and left knee for KOA patients. The reliability between the sessions was in agreement with the WOMAC scores where a change of total score was within 2.1% in the present study.
Wessel [22] assessed PPT’s on six locations above the knee in KOA patients, taken 5–10 days apart and found ICC’s ranged between 0.58 and 0.91 and Moss et al. [33] reported ICC’s of 0.98 of the most tender point on the medial aspect of the affected knee. In the current study particular care was taken to explain the procedures to make sure patients had a comprehensive understanding of the purposes. This might have contributed to the high ICC values.
In the present study, the means of three PPT recordings were used resulting in “almost perfect” ICC. However, it has been suggested that the first PPT assessment should be considered as training and be excluded [34]. Other studies have suggested that the highest ICC values are obtained when the mean score of three PPT recordings is used [20], [35], [36]. The findings from the current study indicates that there is a high similarity between PPT values from the patients, even when testing is performed 2 weeks apart and using mean value of three PPT recordings. In our study a training PPT session was performed to ensure optimal compliance. Only few studies have reported the absolute reliability. Mutlu and Ozdincler [37] assessed reliability of PPT measurements in KOA patients at two anatomical sites (medial femoral tubercle and medial malleolus). They reported a SEM ranged from 4.55 to 4.83 kPa and MDC 10.55–11.17 kPa (mean PPT=37.7–51.71 kPa before treatment and mean PPT=52.3–56.5 kPa after treatment) meanwhile, the SEM in the present study ranged from 34 to 71 kPa and MDC ranged from 93 to 196 kPa (mean PPT=273.5–367.7 kPa in session 1 and mean PPT=268.1–331.3 kPa in session 2). However, Mutlu and Ozdincler [37] only assessed at two anatomical locations and their participants were asked to verbally state when the pain threshold was reached. The reported SEM and MDC in the present study are similar to what has been reported in other studies. Balaguier et al. [19] tested PPT’s in the low back region of vine-workers and reported a SEM ranged from 53.5 to 77.5 kPa and MDC ranged from 148.4 to 214.7 kPa (mean PPT=459.5–516.0 kPa in trial 1 and mean PPT=468.7–540.8 kPa in trial 2) between the first and second trials. Walton and colleagues [38] tested at the trapezius muscle and at tibialis anterior and obtained SEM ranged from 18.2 to 73.8 kPa and MDC ranged from 42.7 to 171.3 kPa (mean PPT=251.8 kPa and 334.1 kPa). The current findings suggest that PPT assessments are reliable and may be used to determine the effects of interventions [16], [39], [40], [41].
No significant difference was seen for clinical VAS ratings between the sessions. A study by Breivik [42] explain the difficulties for chronic pain patients in remembering their pain during the last 24 h and to express the degree of pain on a single pain intensity scale. However, VAS is the most commonly used tool for assessing the experienced pain [42], [43] and found to be reliable in the present study for KOA patients.
5 Conclusions
In conclusion, this study tested the test-retest reliability of PPT’s at 10 anatomical locations for KOA patients. The study shows that PPT is a reliable way to assess mechanical pain sensitivity in KOA patients. This suggests that PPT can be a used to monitor KOA patients over time and relate to e.g. disease progression or interventions.
Acknowledgements
Aina Sætre Lihn and Mette Neumann are acknowledged for recruitment of patients and their contribution to the preparation of the experiments at CCBR. Rasmus Elbæk Andersen is thanked for practical assistance in the laboratory.
-
Authors’ statements
-
Research funding: The individualized osteoarthritis interventions (IOI) project has received funding from Innovation Fund Denmark (grant nr. 40-2014-3).
-
Conflict of interest: All authors disclosed potential conflict of interest with regard to the present work.
-
Informed consent: All subjects signed an informed consent form before participating in the study.
-
Ethical approval: The study had been approved by the local Ethics Committee (VN-20160081) and conducted according to the Declaration of Helsinki.
References
[1] Peat G, McCarney R, Croft P. Knee pain and osteoarthritis in older adults: a review of community burden and current use of primary health care. Ann Rheum Dis 2001;60:91–7.10.1136/ard.60.2.91Suche in Google Scholar PubMed PubMed Central
[2] Cross M, Smith E, Hoy D, Nolte S, Ackerman I, Fransen M, Bridgett L, Williams S, Guillemin F, Hill CL, Laslett LL, Jones G, Cicuttini F, Osborne R, Vos T, Buchbinder R, Woolf A, March L. The global burden of hip and knee osteoarthritis: estimates from the Global Burden of Disease 2010 study. Ann Rheum Dis 2014;73:1323–30.10.1136/annrheumdis-2013-204763Suche in Google Scholar PubMed
[3] Wallace IJ, Worthington S, Felson DT, Jurmain RD, Wren KT, Maijanen H, Woods RJ, Lieberman DE. Knee osteoarthritis has doubled in prevalence since the mid-20th century. Proc Natl Acad Sci 2017;114:9332–6.10.1073/pnas.1703856114Suche in Google Scholar PubMed PubMed Central
[4] Pavlaković G, Petzke F. The role of quantitative sensory testing in the evaluation of musculoskeletal pain conditions. Current Rheumatol Rep 2010;12:455–61.10.1007/s11926-010-0131-0Suche in Google Scholar PubMed PubMed Central
[5] Suokas AK, Walsh DA, McWilliams DF, Condon L, Moreton B, Wylde V, Arendt-Nielsen L, Zhang W. Quantitative sensory testing in painful osteoarthritis: a systematic review and meta-analysis. Osteoarthritis Cartilage 2012;20:1075–85.10.1016/j.joca.2012.06.009Suche in Google Scholar PubMed
[6] Madeleine P, Camargo PR, Salvini TF. Spotlight on topographical pressure pain sensitivity maps: a review. J Pain Res 2018;11:215–25.10.2147/JPR.S135769Suche in Google Scholar PubMed PubMed Central
[7] Mense S, Simon DG. Muscle pain: understanding its nature, diagnosis, and treatment. Acupunct Med 2001;20:385.Suche in Google Scholar
[8] Arendt-Nielsen L, Nie H, Laursen MB, Laursen BS, Madeleine P, Simonsen OH, Graven-Nielsen T. Sensitization in patients with painful knee osteoarthritis. Pain 2010;149:573–81.10.1016/j.pain.2010.04.003Suche in Google Scholar PubMed
[9] Binderup A, Arendt-Nielsen L, Madeleine P. Pressure pain threshold mapping of the trapezius muscle reveals heterogeneity in the distribution of muscular hyperalgesia after eccentric exercise. Eur J Pain 2010;14:705–12.10.1016/j.ejpain.2009.11.001Suche in Google Scholar PubMed
[10] Binderup A, Arendt-Nielsen L, Madeleine P. Pressure pain threshold mapping – a new imaging modality of muscle sensitivity to pain. In: 2008 Annual IEEE Student Paper Conference. IEEE; 2008:1–4.10.1109/AISPC.2008.4460549Suche in Google Scholar
[11] Finan PH, Buenaver LF, Bounds SC, Hussain S, Park RJ, Haque UJ, Campbell CM, Haythornthwaite JA, Edwards RR, Smith MT. Discordance between pain and radiographic severity in knee osteoarthritis: Findings from quantitative sensory testing of central sensitization. Arthritis Rheum 2013;65:363–72.10.1002/art.34646Suche in Google Scholar PubMed PubMed Central
[12] Graven-Nielsen T, Wodehouse T, Langford RM, Arendt-Nielsen L, Kidd BL. Normalization of widespread hyperesthesia and facilitated spatial summation of deep-tissue pain in knee osteoarthritis patients after knee replacement. Arthritis Rheum 2012;64:2907–16.10.1002/art.34466Suche in Google Scholar PubMed
[13] Arendt-Nielsen L, Skou ST, Nielsen TA, Petersen KK. Altered central sensitization and pain modulation in the CNS in chronic joint pain. Curr Osteoporos Rep 2015;13:225–34.10.1007/s11914-015-0276-xSuche in Google Scholar PubMed
[14] Arendt-Nielsen L. Central sensitization in humans: assessment and pharmacology. Handb Exp Pharmacol 2015;227:79–102.10.1007/978-3-662-46450-2_5Suche in Google Scholar PubMed
[15] Pelfort X, Torres-Claramunt R, Sánchez-Soler JF, Hinarejos P, Leal-Blanquet J, Valverde D, Monllau JC. Pressure algometry is a useful tool to quantify pain in the medial part of the knee: An intra- and inter-reliability study in healthy subjects. Orthop Traumatol Surg Res 2015;101:559–63.10.1016/j.otsr.2015.03.016Suche in Google Scholar PubMed
[16] Skou ST, Simonsen OH, Rasmussen S. Examination of muscle strength and pressure pain thresholds in knee osteoarthritis: test-retest reliability and agreement. J Geriatr Phys Ther 2015;38:141–7.10.1519/JPT.0000000000000028Suche in Google Scholar PubMed
[17] Jørgensen R, Ris I, Falla D, Juul-Kristensen B. Reliability, construct and discriminative validity of clinical testing in subjects with and without chronic neck pain. BMC Musculoskelet Disord 2014;15:408.10.1186/1471-2474-15-408Suche in Google Scholar PubMed PubMed Central
[18] Walton DM, Levesque L, Payne M, Schick J. Clinical pressure pain threshold testing in neck pain: comparing protocols, responsiveness, and association with psychological variables. Phys Ther 2014;94:827–37.10.2522/ptj.20130369Suche in Google Scholar PubMed PubMed Central
[19] Balaguier R, Madeleine P, Vuillerme N. Intra-session absolute and relative reliability of pressure pain thresholds in the low back region of vine-workers: ffect of the number of trials. BMC Musculoskelet Disord 2016;17:350.10.1186/s12891-016-1212-7Suche in Google Scholar PubMed PubMed Central
[20] Balaguier R, Madeleine P, Vuillerme N. Is one trial sufficient to obtain excellent pressure pain threshold reliability in the low back of asymptomatic individuals? A test-retest study. Smalheiser NR, editor. PLoS One 2016;11:e0160866.10.1371/journal.pone.0160866Suche in Google Scholar PubMed PubMed Central
[21] Arendt-Nielsen L. Reliability of pressure pain threshold testing in healthy pain free young adults. Scand J Pain 2015;9:38–41.10.1016/j.sjpain.2015.05.004Suche in Google Scholar PubMed
[22] Wessel J. The reliability and vatidity of pain threshold measurements in osteoarthritis of the knee. Scand J Rheumatol 1995;24:238–42.10.3109/03009749509100881Suche in Google Scholar PubMed
[23] Skou ST, Graven-Nielsen T, Lengsoe L, Simonsen O, Laursen MB, Arendt-Nielsen L. Relating clinical measures of pain with experimentally assessed pain mechanisms in patients with knee osteoarthritis. Scand J Pain 2013;4:111–7.10.1016/j.sjpain.2012.07.001Suche in Google Scholar PubMed
[24] Kottner J, Audigé L, Brorson S, Donner A, Gajewski BJ, Hróbjartsson A, Roberts C, Shoukri M, Streiner DL. Guidelines for Reporting Reliability and Agreement Studies (GRRAS) were proposed. J Clin Epidemiol 2011;64:96–106.10.1016/j.jclinepi.2010.03.002Suche in Google Scholar PubMed
[25] Nie H, Graven-Nielsen T, Arendt-Nielsen L. Spatial and temporal summation of pain evoked by mechanical pressure stimulation. Eur J Pain 2009;13:592–9.10.1016/j.ejpain.2008.07.013Suche in Google Scholar PubMed
[26] Bellamy N, Buchanan WW, Goldsmith CH, Campbell J, Stitt LW. Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J Rheumatol 1988;15:1833–40.Suche in Google Scholar
[27] Freynhagen R, Baron R, Gockel U, Tölle TR. Pain DETECT: a new screening questionnaire to identify neuropathic components in patients with back pain. Curr Med Res Opin 2006;22:1911–20.10.1185/030079906X132488Suche in Google Scholar PubMed
[28] Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics 1977;33:159.10.2307/2529310Suche in Google Scholar
[29] Harvill LM. Standard error of measurement. Items 1991;10:181–9.10.1111/j.1745-3992.1991.tb00195.xSuche in Google Scholar
[30] Donoghue D, Murphy A, Jennings A, McAuliffe A, O’Neil S, Charthaigh EN, Griffin E, Gilhooly L, Lyons M, Galvin R, Gallagher S, Ward S, Mhaille EN, Stokes EK. How much change is true change? The minimum detectable change of the Berg Balance Scale in elderly people. J Rehabil Med 2009;41:343–6.10.2340/16501977-0337Suche in Google Scholar PubMed
[31] Herren-Gerber R, Weiss S, Arendt-Nielsen L, Petersen-Felix S, Di Stefano G, Radanov BP, Curatolo M. Modulation of central hypersensitivity by nociceptive input in chronic pain after whiplash injury. Pain Med 2004;5:366–76.10.1111/j.1526-4637.2004.04055.xSuche in Google Scholar PubMed
[32] Wylde V, Palmer S, Learmonth ID, Dieppe P. Test-retest reliability of Quantitative Sensory Testing in knee osteoarthritis and healthy participants. Osteoarthr Cartil 2011;19:655–8.10.1016/j.joca.2011.02.009Suche in Google Scholar PubMed
[33] Moss P, Sluka K, Wright A. The initial effects of knee joint mobilization on osteoarthritic hyperalgesia. Man Ther 2007;12:109–18.10.1016/j.math.2006.02.009Suche in Google Scholar PubMed
[34] Lacourt TE, Houtveen JH, van Doornen LJP. Experimental pressure-pain assessments: Test-retest reliability, convergence and dimensionality. Scand J Pain 2012;3:31–7.10.1016/j.sjpain.2011.10.003Suche in Google Scholar PubMed
[35] Chesterton LS, Sim J, Wright CC, Foster NE. Interrater reliability of algometry in measuring pressure pain thresholds in healthy humans, using multiple raters. Clin J Pain 2007;23:760–6.10.1097/AJP.0b013e318154b6aeSuche in Google Scholar PubMed
[36] Nussbaum EL, Downes L. Reliability of clinical pressure-pain algometric measurements obtained on consecutive days. Phys Ther 1998;78:160–9.10.1093/ptj/78.2.160Suche in Google Scholar PubMed
[37] Mutlu EK, Ozdincler AR. Reliability and responsiveness of algometry for measuring pressure pain threshold in patients with knee osteoarthritis. J Phys Ther Sci 2015;27:1961–5.10.1589/jpts.27.1961Suche in Google Scholar PubMed PubMed Central
[38] Walton D, MacDermid J, Nielson W, Teasell R, Chiasson M, Brown L. Reliability, standard error, and minimum detectable change of clinical pressure pain threshold testing in people with and without acute neck pain. J Orthop Sport Phys Ther 2011;41:644–50.10.2519/jospt.2011.3666Suche in Google Scholar PubMed
[39] Madeleine P, Hoej BP, Fernández-de-las-Peñas C, Rathleff MS, Kaalund S. Pressure pain sensitivity changes after use of shock-absorbing insoles among young soccer players training on artificial turf: a randomized controlled trial. J Orthop Sport Phys Ther 2014;44:587–94.10.2519/jospt.2014.5117Suche in Google Scholar PubMed
[40] Arendt-Nielsen L, Curatolo M. Mechanistic, translational, quantitative pain assessment tools in profiling of pain patients and for development of new analgesic compounds. Scand J Pain 2013;4:226–30.10.1016/j.sjpain.2013.07.026Suche in Google Scholar PubMed
[41] Schliessbach J, Siegenthaler A, Bütikofer L, Vuilleumier P, Jüni P, Arendt-Nielsen L, Curatolo M. Quantitative sensory tests fairly reflect immediate effects of oxycodone in chronic low-back pain. Scand J Pain 2017;17:107–15.10.1016/j.sjpain.2017.07.004Suche in Google Scholar PubMed
[42] Breivik H. Patients’ subjective acute pain rating scales (VAS, NRS) are fine; more elaborate evaluations needed for chronic pain, especially in the elderly and demented patients. Scand J Pain 2017;15:73–4.10.1016/j.sjpain.2017.01.001Suche in Google Scholar PubMed
[43] Skovlund E, Breivik H. Analysis of pain-intensity measurements. Scand J Pain 2016;13:123–4.10.1016/j.sjpain.2016.08.005Suche in Google Scholar PubMed
©2018 Scandinavian Association for the Study of Pain. Published by Walter de Gruyter GmbH, Berlin/Boston. All rights reserved.
Artikel in diesem Heft
- Frontmatter
- Topical review
- Reducing risk of spinal haematoma from spinal and epidural pain procedures
- Clinical pain research
- A multiple-dose double-blind randomized study to evaluate the safety, pharmacokinetics, pharmacodynamics and analgesic efficacy of the TRPV1 antagonist JNJ-39439335 (mavatrep)
- Reliability of three linguistically and culturally validated pain assessment tools for sedated ICU patients by ICU nurses in Finland
- Superior outcomes following cervical fusion vs. multimodal rehabilitation in a subgroup of randomized Whiplash-Associated-Disorders (WAD) patients indicating somatic pain origin-Comparison of outcome assessments made by four examiners from different disciplines
- Morning cortisol and fasting glucose are elevated in women with chronic widespread pain independent of comorbid restless legs syndrome
- Chronic pain experience and pain management in persons with spinal cord injury in Nepal
- The Standardised Mensendieck Test as a tool for evaluation of movement quality in patients with nonspecific chronic low back pain
- Exploring effect of pain education on chronic pain patients’ expectation of recovery and pain intensity
- Pain, psychological distress and motor pattern in women with provoked vestibulodynia (PVD) – symptom characteristics and therapy suggestions
- Relative and absolute test-retest reliabilities of pressure pain threshold in patients with knee osteoarthritis
- The influence of pre- and perioperative administration of gabapentin on pain 3–4 years after total knee arthroplasty
- Observational study
- CT guided neurolytic blockade of the coeliac plexus in patients with advanced and intractably painful pancreatic cancer
- Prescription of opioids to post-operative orthopaedic patients at time of discharge from hospital: a prospective observational study
- The psychological features of patellofemoral pain: a cross-sectional study
- Prevalence of self-reported musculoskeletal pain symptoms among school-age adolescents: age and sex differences
- The association between back muscle characteristics and pressure pain sensitivity in low back pain patients
- Postural control in subclinical neck pain: a comparative study on the effect of pain and measurement procedures
- Original experimental
- Exercise-induced hypoalgesia in women with varying levels of menstrual pain
- Exercise does not produce hypoalgesia when performed immediately after a painful stimulus
- Effectiveness of neck stabilisation and dynamic exercises on pain intensity, depression and anxiety among patients with non-specific neck pain: a randomised controlled trial
Artikel in diesem Heft
- Frontmatter
- Topical review
- Reducing risk of spinal haematoma from spinal and epidural pain procedures
- Clinical pain research
- A multiple-dose double-blind randomized study to evaluate the safety, pharmacokinetics, pharmacodynamics and analgesic efficacy of the TRPV1 antagonist JNJ-39439335 (mavatrep)
- Reliability of three linguistically and culturally validated pain assessment tools for sedated ICU patients by ICU nurses in Finland
- Superior outcomes following cervical fusion vs. multimodal rehabilitation in a subgroup of randomized Whiplash-Associated-Disorders (WAD) patients indicating somatic pain origin-Comparison of outcome assessments made by four examiners from different disciplines
- Morning cortisol and fasting glucose are elevated in women with chronic widespread pain independent of comorbid restless legs syndrome
- Chronic pain experience and pain management in persons with spinal cord injury in Nepal
- The Standardised Mensendieck Test as a tool for evaluation of movement quality in patients with nonspecific chronic low back pain
- Exploring effect of pain education on chronic pain patients’ expectation of recovery and pain intensity
- Pain, psychological distress and motor pattern in women with provoked vestibulodynia (PVD) – symptom characteristics and therapy suggestions
- Relative and absolute test-retest reliabilities of pressure pain threshold in patients with knee osteoarthritis
- The influence of pre- and perioperative administration of gabapentin on pain 3–4 years after total knee arthroplasty
- Observational study
- CT guided neurolytic blockade of the coeliac plexus in patients with advanced and intractably painful pancreatic cancer
- Prescription of opioids to post-operative orthopaedic patients at time of discharge from hospital: a prospective observational study
- The psychological features of patellofemoral pain: a cross-sectional study
- Prevalence of self-reported musculoskeletal pain symptoms among school-age adolescents: age and sex differences
- The association between back muscle characteristics and pressure pain sensitivity in low back pain patients
- Postural control in subclinical neck pain: a comparative study on the effect of pain and measurement procedures
- Original experimental
- Exercise-induced hypoalgesia in women with varying levels of menstrual pain
- Exercise does not produce hypoalgesia when performed immediately after a painful stimulus
- Effectiveness of neck stabilisation and dynamic exercises on pain intensity, depression and anxiety among patients with non-specific neck pain: a randomised controlled trial

