When Diseases Return from the Epidemiological Honeymoon: The Reemergence of Smallpox in 19th Century Germany and its Lessons for Public Health Policies after COVID-19
-
Katharina Muehlhoff
Katharina Muehlhoff is an associate researcher at the Center for Population Health at Stanford Medical School and the Heidelberg Institute of Global Health (HIGH). She studied at the University of Mannheim, where she completed her PhD in economic history and development economics in 2016. Afterwards, she worked as an assistant professor of economic history and demography at Carlos III University of Madrid. Her research focus is on historical epidemiology, demography and population health. In 2024 she joined the HIGH to investigate non-pathogen specific side effects of vaccination. Her current projects investigate the possibility that herpes zoster vaccination might prevent or delay the onset of neurological disorders like Alzheimer’s disease.
Abstract
The COVID-19 pandemic has overwhelmed public health systems around the world. At the same time, misinformation about vaccines spread with unprecedented speed. Governments and international organizations are currently evaluating strategies for future outbreaks of infectious diseases. This paper provides historical evidence about the last large-scale smallpox epidemic that ravaged Germany in 1870 to 1872. The health authorities of the different German states faced almost the same problems as their 21st century counterparts: Mounting pressure from anti-vaccination groups and increasing mobility and demographic change that facilitated the spread of pathogens. Using both qualitative sources and statistical evidence, the paper shows that the 1870 to 1872 outbreak was mostly due to incomplete vaccination uptake and the corresponding accumulation of susceptible individuals. This phenomenon – also referred to as a post-honeymoon-epidemic – was dramatically exacerbated because smallpox incidence shifted from very young age-groups to highly mobile adolescents and adults. The main conclusion from this historic German experience is that a rise in vaccine hesitancy requires resolute and sustained public health responses.
1 Introduction
With an estimated death toll of seven million worldwide, the Covid-19 pandemic has brutally exposed the vulnerability of modern societies to newly emerging infectious diseases. In the aftermath of the outbreak, the idea of a global health architecture for prevention, preparedness and response gained political traction and lead to the ratification of the Pandemic Agreement in 2025. [1] While collaborative global research efforts, equitable access to vaccines, and rapid deployment of therapeutics and diagnostics are necessary conditions for the successful control of newly emerging pathogens, the Pandemic Agreement potentially underestimates another risk. Due to disruptions in immunization programs during the Covid-19 emergency, armed conflict, vaccine hesitancy and misinformation, routine vaccination against endemic diseases has declined substantially in many countries. If this trend continues, it is likely that we will not only be threatened by new diseases, but we will also face the return of seemingly tamed diseases in the near future.
History offers unique opportunities to study how old diseases re-emerge after having been under control for a long time. This paper will discuss how smallpox – the Plague of the 18th century – went from killing over 400,000 Europeans per year to near extinction in the middle of the 19th century and then sprung back to unleash an epidemic with more than 500,000 casualties in the 1870s. [2]
In the early 19th century, a new disease, cholera, arrived in Europe and caused such considerable panic that smallpox was temporarily pushed from collective consciousness. This shift in risk awareness turned out to be a fatal mistake. During the 1820s and 1830s this development was understandable: Since the discovery of the cowpox vaccine by Edward Jenner in 1798, a safe and efficient means of preventing smallpox had spread across the continent. Vaccination uptake varied in terms of speed and institutional framework, but generally, immunization had led to sizeable reductions in smallpox prevalence wherever it had been introduced.
Yet, this success was short-lived: In the 1860s, smallpox started to return and in 1870 to 1872, the German Empire became the epicenter of a pandemic that killed with a ferocity not seen since the introduction of vaccination. The events of 1870 to 1872 are particularly unsettling because the outbreak could have been averted or at least mitigated if the German states had set up effective and coordinated prevention policies during the first half of the century. Hence, the question is: Why did this outbreak happen, despite the fact that vaccination had been available for decades? And: What insights does the lead-up to the catastrophe of 1870 to 1872 provide for the prevention of infectious diseases today?
In order to answer these questions, this paper is organized as follows: Section 2 introduces the historical context of smallpox prevention in the 19th century. Section 3 briefly describes the epidemiological theories that explain large-scale outbreaks after long periods of seemingly successful prevention and reviews related literature. Section 5 looks at exogenous factors including demographic dynamics and the impact of increased mobility in the second half of the 19th century. Section 6 concludes.
2 Historical Context
In 1798, the scientific community was excited by Edward Jenner’s findings about the possibility of inducing immunity against smallpox by inoculating patients with cowpox, a relatively harmless disease of the skin. Knowledge about the new method spread rapidly from England to the European continent and by the turn of the 19th century doctors all over Europe had started to vaccinate people with pus from cowpox blisters. The tremendous impact of Jenner’s modest 75-page paper was no surprise: At the time it appeared in print, smallpox was one of, if not the most devastating epidemic disease in the world. Its death toll was so overwhelming that 18th century scholars claimed that the ravages of smallpox and the Black Death were nearly the same. Only because smallpox killed mainly children, whose deaths were not always counted in the church registers, mortality tended to be underestimated. [3] Concerning prevalence, contemporary sources from France and Germany estimated that approximately 80 percent of each cohort would become infected with smallpox during their lives – a number which present-day research only slightly corrected to 66 to 75 percent. [4]
Getting a grip on smallpox promised such considerable economic and strategic benefits that most European governments encouraged vaccination by means of information campaigns and free public vaccinations. Some German states, including Bavaria, Baden and Wurttemberg even passed legislation which required the universal vaccination of all infants. Following the first wave of mass vaccination, smallpox incidence and mortality declined rapidly. For example, the state of Wurttemberg had recorded between 2000 and 3000 deaths from smallpox per year in the period 1780-1810. In the decade 1810-1820 when vaccination had been introduced, this number dropped to roughly 180 per year. [5]
The initial success notwithstanding, enthusiasm for vaccination cooled down in Germany when the time limit of vaccine induced immunity became apparent: more and more adults who had been vaccinated as children got infected with smallpox and the vaccine’s absolute protective capacity became increasingly contested. When people realized that smallpox vaccination was not invincible, this dealt a severe blow to the newly forming science of medicine and created the breeding ground for alternative medicine and the first organized anti-vaccination movements. The academic dispute among doctors and scientists, as well as popular movements against vaccination influenced immunization policies, because they jeopardized political support for vaccination. Policymakers of the revolutionary 1840s were reluctant to crack down on vaccine refusal, because well-organized bourgeois and liberal circles largely rejected mandatory vaccination.
German states dealt with smallpox prevention very differently. The South-Western states, as well as Oldenburg and Hannover, required the vaccination of all infants and often encouraged the revaccination of school-age children. By contrast, Prussia mandated only the vaccination of soldiers but not the civilian population. Saxony, parts of Thuringia and the Hanseatic cities passed no regulations at all.
We will see shortly that this policy patchwork ultimately determined the course of the 1870 to 1872 epidemic. Yet, to analyze the consequences of uncoordinated vaccination strategies within the German Confederation (Deutscher Bund, an association of German states in place since 1815, prior to the creation of the German Empire in 1871), some knowledge about the dynamics of reemerging infectious diseases and of public health economics is necessary. The next section discusses these topics and reviews the most relevant literature.
3 Re-emerging Infectious Diseases
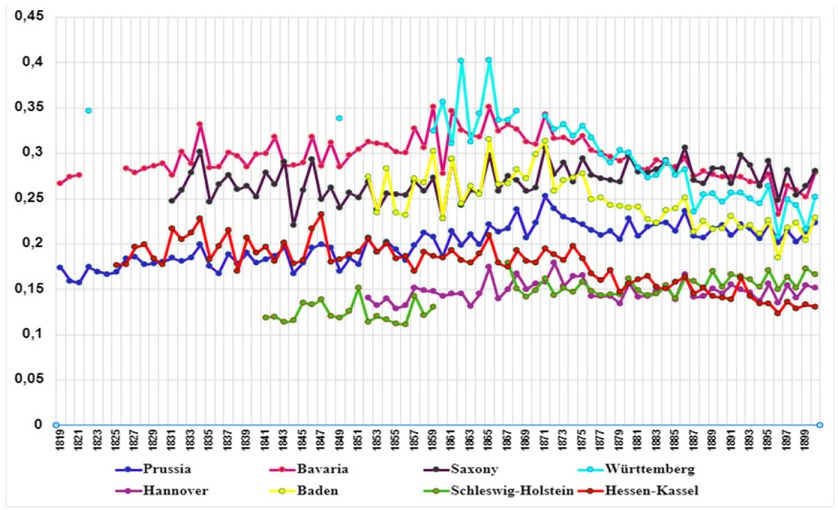
Figure 1 shows the number of smallpox deaths in selected German states. Mortality initially fluctuated on very low levels in the states with mandatory vaccination (Baden, Bavaria and Wurttemberg). In Prussia, where vaccination of the civilian population was voluntary, it was moderate, but annual deaths begin to increase in the late 1850s. Finally, by 1870, the disease re-emerged in all states and deathrates spiked at levels not seen in decades.
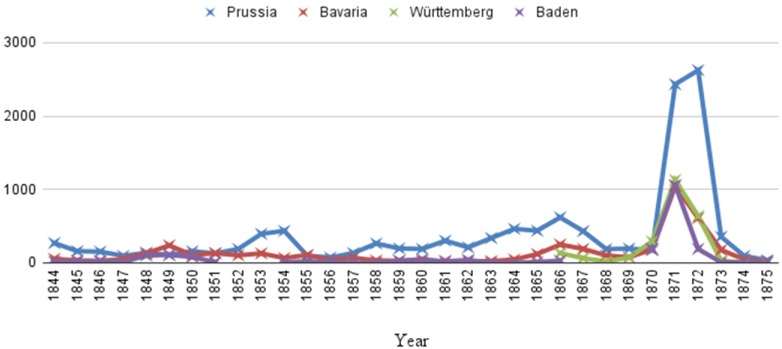
Smallpox Mortality in Selected German States, 1844 to 1875. Note: Deaths per million inhabitants. Sources: For Prussia, Bavaria and Wurttemberg: E. Edwardes, A Concise History of Small-Pox and Vaccination in Europe, London 1902; for Baden: F. Loetz, Vom Kranken zum Patienten. “Medikalisierung” und medizinische Vergesellschaftung am Beispiel Badens 1750–1850, Stuttgart 1993, p. 327; Generallandesarchiv Karlsruhe (GLA Karlsruhe), Records of the Sanitary Commission 236 Nr. 16032.
How can this phenomenon be explained? Was it merely a consequence of the Franco-Prussian War, as many contemporaries believed at first? Was it due to cooled down enthusiasm for vaccination? Or did various epidemiological and societal mechanisms jointly fuel the epidemic?
The spread of diseases after a long period of mass vaccination is best understood in comparison to the situation of an epidemiologically naive population, that is, a population whose members acquire immunity only via natural infection. In such a naive population, disease prevalence oscillates between epidemic and non-epidemic years. The amplitude of the oscillations and the length of the inter-epidemic interval depend on the biology of the pathogen and the demographic characteristics of the population under study. An example of the pre-vaccination dynamics of smallpox is shown in Figure 2, which depicts smallpox deaths in Berlin in the 18th and early 19th century.
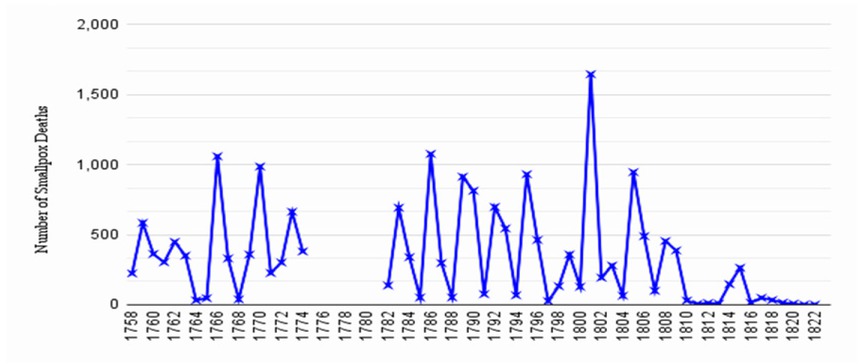
Epidemic Fluctuations in Berlin, 1750s to 1820s. Note: This graphic shows the epidemic fluctuations in an immunologically naive population. Sources: Edwardes, A Concise History of Small-Pox, statistical appendix.
As can be seen, epidemics occur almost mechanically roughly every three to four years. This regularity stems from the fact that highly contagious diseases like smallpox were almost impossible to contain by the medical means available in the 18th century. Thus, an outbreak inevitably affected all susceptible individuals in reach of the virus. Once the epidemic abated, it left many dead, while the survivors acquired life-long immunity. This means that the re-emergence of the virus did not immediately lead to a new outbreak. Depending on the growth rate of the population, it took a certain amount of time until the pool of infectible individuals had been replenished by the arrival of newborn children. When the susceptible population had grown to a size that sustained an epidemic, new infections would produce the next peak in incidence as shown in Figure 2.
When vaccination was introduced in Germany in the early 19th century, this pattern of regular epidemic spikes disappeared. Theoretically, a vaccine can have two different effects on the epidemiology of the targeted disease. In the ideal case, mass-vaccination permanently mimics the situation immediately after a large epidemic: It removes infants directly from the pool of susceptibles and starves the pathogen of potential hosts. In the long term, this leads to a situation of herd immunity and – ultimately – to the eradication of the disease.
Unfortunately, this optimal scenario is hard to reach because vaccine efficacy is imperfect, and uptake tends to fall short of the critical threshold. For public health officials in the 19th century, the situation was extremely problematic because statistical data like case counts did not indicate if the vaccination rate was sufficiently high to prevent future outbreaks. The reason for this is that the number of susceptibles declines and the time interval between two epidemic outbreaks becomes longer when a mass immunization campaign is implemented. As a result, low prevalence can indicate that the disease is on the way towards eradication. However, it can also hide an imminent threat: If health officials wrongly assume that herd immunity is reached, although the actual immunity level is below the critical threshold, more and more susceptible children accumulate, and older individuals – when they continue to be exposed to the virus – become infectible again due to weakening immunity. If not corrected by revaccination, this build-up of a large pool of susceptibles leads to a paradoxical situation: Epidemics in incompletely protected populations rival or even surpass the typical size of outbreaks in the pre-vaccination era. In other words: Vaccinating too few may lead to worse outcomes than vaccinating nobody.
Epidemiologists refer to the period of low prevalence followed by subsequent epidemics as the epidemiological honeymoon and the post-honeymoon epidemic respectively. As will be shown below, there is a rich literature of mathematical models that helps to understand the biological mechanisms behind post-honeymoon epidemics. This literature can also be used to predict the spread of diseases in incompletely immunized populations. However, from the historian’s point of view, a purely mathematical analysis sidesteps a crucial question: What institutional conditions cause countries to end up trapped in a post-honeymoon epidemic? To see how the epidemiological and the historical perspective can be connected, let us therefore briefly consider the state of research in these different fields.
The present paper builds on three distinct strands of literature. The first consists of papers that study the dynamics of post-honeymoon epidemics. Interest in this phenomenon came up in the 1980s when various countries experienced unexpectedly large outbreaks of diseases like the measles, which had been thought to be under control after the development of the MMR vaccine. R. M. Anderson and Angela McLean’s 1988 paper Measles in developing countries. The predicted impact of mass vaccination was a milestone because it was the first to provide a rigorous theoretical model that explained the sudden relapse to high incidence. Afterward, several authors have studied the transitional dynamics of infectious diseases after mass-vaccination, including David Earn et al., [6] Almut Scherer and Angela McLean, [7] Carla Scarbrough Lefebvre et al., [8] and Brandon Hollingsworth et al. [9]. A central result of these papers is the already mentioned fact that incomplete vaccination can push cumulative incidence above the level of an outbreak with no immunization. Epidemiologists of the 20th and 21st centuries have documented empirical cases of honeymoon epidemics in various countries and for different diseases. [10] The case of the 1870 to 1872 smallpox epidemic in Germany adds valuable insights to this literature because it allows us to study the factors that contributed to an extremely large post-honeymoon outbreak over a period of almost 70 years. That is, the historical case offers a long-term perspective that is typically not feasible for current epidemiological studies.
So far, economists have hardly studied the particularities of post-honeymoon epidemics. However, interest in vaccination has been intense in various fields of economic research for a long time. Specifically, herd immunity has been studied extensively by theorists of public and health economics, for example by Mark Gersovitz and Jeffrey Hammer, [11] Eili Klein et al., [12] Dagobert Brito et al., [13] Pierre-Yves Geoffard and Tomas Philipson, [14] Bryan Boulier et al., [15] Scott Barrett [16] and Katharina Hauck. [17] Their common conclusion is that decentralized vaccination almost always misses the social optimum because individuals do not account for the protective effect of herd immunity on others.
Finally, turning to the humanities and social sciences, it is true that smallpox has attracted the interest of social historians before, for example: Peter Baldwin, [18] Peter Sköld [19] and José Rigau-Pérez [20] being but a few examples. Yet for one, this work is typically more concerned with the evolution of public health policies within single countries and less with international interdependencies. If cross-country spillovers are discussed, the main emphasis is on cultural aspects and less on economic costs and benefits. This fact is particularly palpable in the literature on the political economy of immunization. Studies in this subfield – especially those focusing on the US – have attributed the slow spread of universal immunization to the inability of liberal constitutional governments to override popular resistance against (mandatory) vaccination. The German case rejects a simple democracy vs. autocracy dichotomy. For example, the Grand Duchy of Baden was one of the first states that imposed strict mandatory vaccination laws and maintained very high immunization uptake throughout the 19th century. Yet, contradicting the predictions of the literature, Baden was one of the least autocratic states in the German Confederation and had passed a constitution that guaranteed civil rights and constrained the state’s power as early as 1818! Thus, as the following sections will show, the catastrophic post-honeymoon outbreak of 1870 to 1872 was less a matter of political systems but rather of an unfortunate interplay between epidemiological, demographic, and economic factors that synergistically contributed to the growth of the epidemic.
4 The Epidemiological Honeymoon in 19th Century Germany
The epidemic of 1870 to 1872 was fueled by suboptimal vaccination coverage and by coordination failure among the German states. As shown in Figure 3, the drivers of the outbreak can be further classified based on whether they were endogenous (marked red) or exogenous (marked green). Endogenous drivers refer to deliberate decisions and behaviors taken by individuals, doctors or policymakers that contributed to the honeymoon epidemic. Exogenous factors or externalities were outside the direct control of any of these actors but may have been influenced by one or several of the endogenous causes.
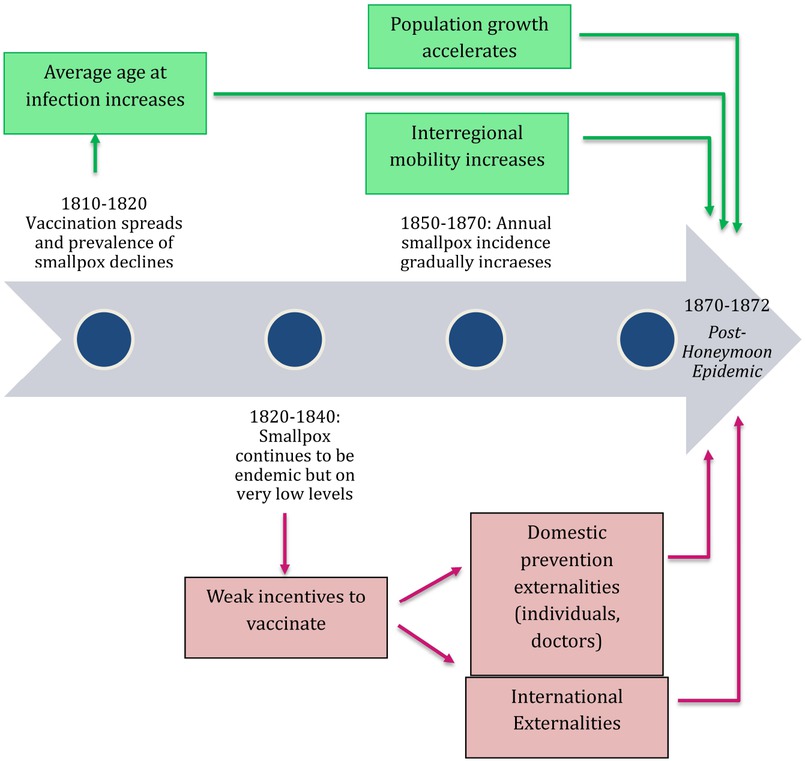
Exogenous and Endogenous Causes of the German Smallpox Epidemic (1870 to 1872).
The start of the timeline in Figure 3 corresponds to the first wave of successful mass vaccination in the 1810s and 1820s. As can be seen, the low incidence in the partly immunized population created both endogenous behavioral responses and an exogenous change in the demographic structure of the susceptible population. Moreover, toward the middle of the century, additional exogenous factors (technological change, population growth and mobility) added to the influence of externalities and age-at-infection-related dynamics. The following sub-sections will disentangle the impact of these different causal channels, starting with individual and international externalities and finishing with the impact of structural demographic changes and increased interregional mobility.
4.1 Externalities: Private Incentives vs. Herd Immunity
From an economic perspective, the behavioral responses to falling prevalence are best understood as variants of the canonical tragedy of the commons-problem. Vaccination – or more precisely, the immunity it creates – clearly exhibits public good characteristics: Vaccinated individuals cannot infect others (or do so with lower probability) and they themselves develop no or only mild to negligible symptoms. At the same time, unvaccinated free riders also benefit from herd immunity.
Two types of externalities can occur: The first stems from the fact that private utility only reflects the avoided costs of the vaccinated person’s illness that did not happen. When deciding whether to get vaccinated or not, individual agents do not account for the social savings from a reduced burden of disease. Of course, governments could – in principle at least – motivate their citizens to take socially optimal vaccination decisions – by offering appropriate incentives. However, even if policymakers created an effective incentive scheme, vaccination rates might still be insufficient due to a second externality at the international level. This cross-country externality occurs when states blindly follow seemingly successful standard policies or when they take advantage of their neighbors’ prevention efforts. If international mobility is sufficiently high to facilitate the spread of the pathogen, under-vaccinated populations turn into a reservoir for the virus and spark epidemic outbreaks elsewhere.
For the sake of clarity, it is helpful to analyze the domestic and international prevention externality one at a time. Yet, readers should be aware that the two were often mutually connected. Thus, although the next subsections describe the incentives of individuals, doctors, and policy makers separately, it is important to keep in mind that these groups acted interdependently and that their behaviors contributed simultaneously to sub-optimal immunization outcomes.
4.2 Domestic Externalities: Individual Perspective
As discussed earlier, a number of German states – Bavaria, Baden and Wurttemberg being the forerunners – legally obliged parents to have their infants vaccinated in the 1810s and 1820s. [21] This measure was the final point in a series of laws and regulations that imposed indirect pressure (e.g. admitting only vaccinated children to public schools) or mandated vaccination for certain groups of the population (e.g. soldiers, orphans). Coercion can thereby be seen as a means of last resort that governments adopted after observing that popular distrust and misinformation led to stalling vaccination uptake.
There is an impressive number of sources left by vaccinators, local officials and central government statisticians that illustrates how health administrations struggled to identify the causes of vaccine hesitancy. A representative example of this body of evidence is the following passage from a report of the sanitary commissioner of the Bavarian district of Ellingen in 1806:
“[...] the population strongly opposes [vaccination]. This opposition is fueled by false rumors about the detrimental impact of the vaccine on the human organism. Moreover, some families seem to welcome the ‘Death Angel of Smallpox’ because he takes some of their children and thus reduces the burden of the household. Others state frankly that it would be better to fall victim to smallpox than to perish in the war.” [22]
Smallpox as a form of ex-post family planning has been described before, [23] but the main reasons for sub-optimal vaccination demand have been identified as lack of knowledge, deeply rooted folk beliefs or fear that the vaccine would weaken the body in the long-term. [24] The risks outweighed the benefits of immunization in the eyes of many 19th century families.
By mandating universal vaccination, governments ultimately chose an approach that seems paternalistic if not downright authoritarian. However, for policymakers in the early 19th century it was a natural choice: As early vaccine hesitancy was mainly a phenomenon of the countryside and the urban poor, government officials and academically trained doctors saw no reason to bother with the opposition of ignorant peasants. This changed only when vaccine refusal took hold among the educated and politically organized middle- and upper classes. Once this point was reached, physicians risked losing a solvent clientele and governments were less willing to enforce vaccination rigorously: The risk of causing further outrage in the conflict-ridden 1840s was arguably too high.
The fact that class conflict and political division eventually thwarted the fight against smallpox is remarkable. Up to the turn of the 19th century, the disease had been responsible for 10 to 20 percent of all deaths. [25] Moreover, it had never been a typical disease of the poor but killed with little regard for wealth or social status. It even came to be described as a “communist disease” by 19th century medical historians. [26] That the first generation who had grown up with the protection of widespread immunization proved incapable of reaching a common consensus about the means to protect their own offspring, carries an important lesson: Legal coercion alone was insufficient to guarantee stable vaccination rates and protection against smallpox. In fact, states that had imposed strict vaccination laws did not necessarily attain higher levels of population immunity than those with more permissive policies. Thus, Wurttemberg which had made vaccination mandatory in 1818 vaccinated only about 65 percent of the children born in the capital city of Stuttgart in the 1840s. At the same time, in Berlin, where parents were free to vaccinate their children nor not, the ratio of births/vaccinations was 66 percent. [27] Conversely, those states or regions which had low vaccine hesitancy typically provided for an infrastructure that made the procedure as accessible, low-cost (or free-of-charge) and safe as possible. Information campaigns could be as simple as regular word-to-mouth recommendations by community leaders like teachers, clergymen, doctors, local officials or – as in Grand Duchy of Baden – midwives. A good example for the importance of involving local elites is Jaxtkreis in Wurttemberg where – thanks to the ongoing commitment of doctors and schoolteachers – vaccination and revaccination were above 80 percent, while other Wurttemberg districts hovered around 60 percent. [28]
Some states like Baden and Bavaria went even further and created a sophisticated system of mass immunization, ensuring that vaccination campaigns were held bi-annually in every village. An important feature of this arrangement was that vaccination dates were carefully chosen to avoid an overlap with the planting and harvesting seasons. For the inhabitants of rural areas this reduced the opportunity costs of vaccination dramatically and increased their willingness to comply with the policy. A farmer from Baden summarized this effect pointedly by stating that he finally decided to comply with the vaccination mandate which “[…] before the change in campaign timing] he used to oppose because he couldn’t afford having his children made sick [from cowpox] when all hands were needed on the fields”. [29]
Bavaria and Baden, as well as Hannover, also sought to centralize vaccine production by creating so-called vaccination institutes (Impfinstitute) that provided vaccinators with lymph material of reasonable quality at little or no cost. At the same time, these states also decided to restrict the right to vaccinate, in order to academically trained doctors. This was an important step toward improving the safety of mass vaccinations and to avoid tampering with contaminated or putrid lymph material – given reports of unskilled vaccinators inflicting cuts of more than 5 cm in length or moistening the dried vaccine with their own saliva. [30]
Of course, these additional measures were no panacea to alleviate fears or to boost popular support. Nevertheless, they underscore that formal laws are not sufficient for high vaccination uptake. How important the supporting infrastructure really was for the success of smallpox vaccination can be illustrated by one of the few surviving pieces of numerical evidence that has survived in the state archive of Baden (Generallandesarchiv). Baden had consistently backed its mandatory vaccination laws with measures that reduced individual effort costs (e.g. regular vaccination campaigns) and enlisted the support of local influencers (e.g. midwives, clergymen, rabbis and country doctors). As Figure 4 shows, this institutional framework kept vaccination rates continuously around or above the herd immunity threshold. In fact, substantial deviations from the critical immunization level were recorded only twice: in 1846 (when bad harvests caused severe economic distress and famine) and during the 1848/1849 Revolution.
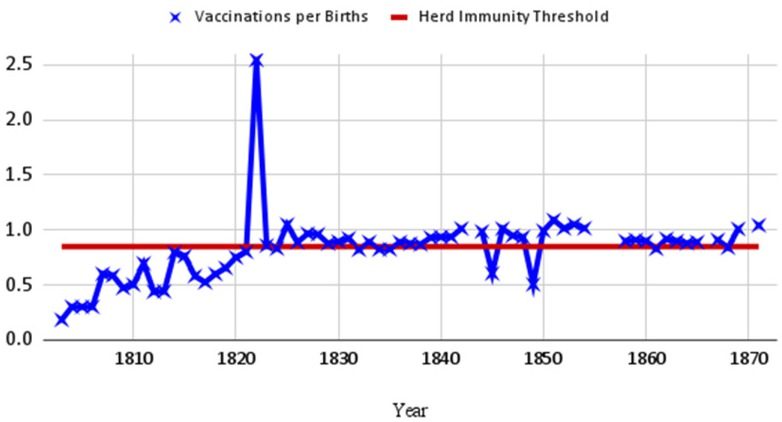
Vaccination Rate in Baden (vaccinations per 100 births). Sources: Documents of the Ministry of Inner Affairs, Health Department, Vaccination Lists. Call number: GLA Karlsruhe 236/16045, For later years, starting from 1830, the data are available in print: Mitteilungen des badischen ärztlichen Vereins, Vol. 9, Karlsruhe 1855.
In summary, statistical and anecdotal evidence suggests that informal institutions play a critical role in stabilizing legal immunization policies. Thus, to avoid that the private prevention externality escalates into anti-vaccination sentiment, formal laws and regulations must be supported by a smooth supply-chain and effective pro-vaccine influencing at the grassroots level. Concretely, this implies that addressing petty inconveniences of immunization becomes more important as the threat of becoming infected with a disease becomes less palpable.
4.3 Domestic Externalities: Doctors’ Perspective
The institutional backing discussed in the previous subsection helped to reduce monetary and non-monetary costs for those getting vaccinated. However, the historical case offers another insight: Ensuring the collaboration of medical practitioners is as important for resolving the prevention externality as is compliance with the policy. In the case of smallpox, doctors’ commitment to the vaccination campaign was especially important for an obvious reason: Unlike present-day vaccines, cowpox vaccinations relatively often failed to provoke a sufficient immune response. As a result, vaccinators needed to assess the success of the procedure five to seven days after inoculation. [31] If a physician did not take this duty seriously, the official vaccination lists would give a biased impression of the size of the susceptible population. Vaccinations with insufficient immune response would not be repeated and the overly optimistic vaccination lists rendered targeted emergency re-vaccinations impossible.
A second problem for doctors was that once vaccination had become a contested issue, naturopathic doctors and alternative healers without academic training started to offer vaccinations with diluted vaccines or issued or forged certificates of medical exemption. In regions with strong anti-vaccination movements like Saxony and Thuringia, up to 20 percent of all children submitted such exemption certificates when entering public schools. [32] Similarly, in the late 19th century, the city of Dresden ordered the re-vaccination of more than 2,500 individuals who had received diluted serum with little immunization effect. [33]
Performing mass vaccinations was no particularly popular task for doctors. This was especially true when the state – as for instance in Wurttemberg or Saxony – did not provide a supportive infrastructure for vaccine production and supply. Left to their own devices, many doctors eventually lost their enthusiasm, as shown by a Wurttemberg doctor who in a letter to the health authorities complained that: “[… he had not] studied medicine to examine every single wart on the udders of the cows in the neighboring villages [to collect fresh vaccine […]”. [34] A constant lack of vaccine and diligent vaccinators contributed to stalling smallpox immunization rates in many states from mid-century onwards.
Finally, the case of Germany in the 19th century highlights a problem that even today’s health planners face when trying to control a disease by means of vaccination: Initially, both the duration and the level of vaccine-induced immunity are unknown. Hence, vaccinated individuals may eventually become susceptible again and/or they may become unintentional spreaders, if the vaccine prevents clinical symptoms but not infection. In the case of smallpox, it soon became apparent that vaccination did not confer life-long, but only temporary protection. For doctors seeking to convince their patients to vaccinate, this posed a formidable challenge: Since the immunological mechanisms behind vaccination were not properly understood until the 20th century, they had to sell a product entirely based on empirical observation. In other words, vaccination was largely a matter of trust and the willingness to follow the recommendations of experts and governments. Many academically trained doctors and government health officials responded to this challenge by framing vaccination as a symbol of progress and rationality. But this strategy came at a cost: It was hard for its proponents to admit that their golden bullet against smallpox was not infallible. Consequently, increasing numbers of health professionals avoided engaging in lengthy discussions with their patients – not the least because vaccinations promised negligible profit compared with other services. Much the same, most governments decided against making universal re-vaccination mandatory, although by mid-century it had been clear that two shots were necessary to reach lasting immunity. [35]
Again, some states, notably Bavaria and Baden, were better able to maintain popular trust and compliance with routine vaccination schemes. One reason for this was the already discussed institutionalization of mass vaccination and the provision of logistic support (e.g. vaccine procurement) for the annual vaccination campaigns. Yet, another important factor was that these states restricted the right to vaccinate to authorized doctors who were directly responsible to the national health department. As a result, vaccination was firmly placed outside the realm of alternative medicine and became part of a systematic public health strategy. Moreover, vaccinating public doctors (Amtsärzte) were hired, supervised and salaried by the state. Their income depended less on payment by individual patients or their families, but on the diligence with which they fulfilled their public duties. As a result, they showed little inclination to join the vaccine-critical discourse.
Another important advantage was that in states where there was broad professional support for stringent immunization policies, prominent scientists were willing to step up for the cause of vaccination. For example, Adolf Kussmaul (the Dean of the Medical Faculty at Freiburg University, Baden) and Rudolf Virchow (Professor at University of Würzburg, Bavaria) published articles in newspapers or magazines and gave public lectures, in order to disseminate knowledge about vaccination among lay audiences.
4.4 International Externalities
So far, the focus has been on the role of individuals who should be vaccinated and doctors. This perspective is incomplete because national governments tend to ignore the effect of their vaccination policies on neighboring countries. In the absence of internationally binding commitments, this produces negative disease spillovers between regions linked through trade, labor mobility or migration flows. Given that Germany consisted of many independent states until 1871, this study is able to look at cross-border effects in some detail.
An important feature of this international prevention externality is that its impact varies systematically with the level of population immunity. Computational models have shown that mobility between two incompletely vaccinated populations has the biggest impact on the potential size of an outbreak if vaccination rates are not at a low level, but at medium or high levels. [36]
Although the mathematical derivation of this result is complex, the underlying thought can be illustrated graphically: To begin with, note that the marginal effect of vaccinating one additional individual varies depending on how many others are immune. Figure 5 shows this relationship for a simple epidemiological model in which the population is divided in two sub-groups (which could be two mutually connected regions) with different vaccination rates. The final size of an outbreak then depends on two factors, namely: (i) the probability with which the pathogen manages to enter both communities, and (ii) the level of immunity within each community. If the two groups or regions are unconnected, the final size of the epidemic cannot exceed the population size of the infected community. Similarly, if both groups are above the herd immunity threshold, the outbreak cannot grow because the infection fails to spread. Obviously, neither of these scenarios describes the smallpox epidemic of 1870 to 1872.
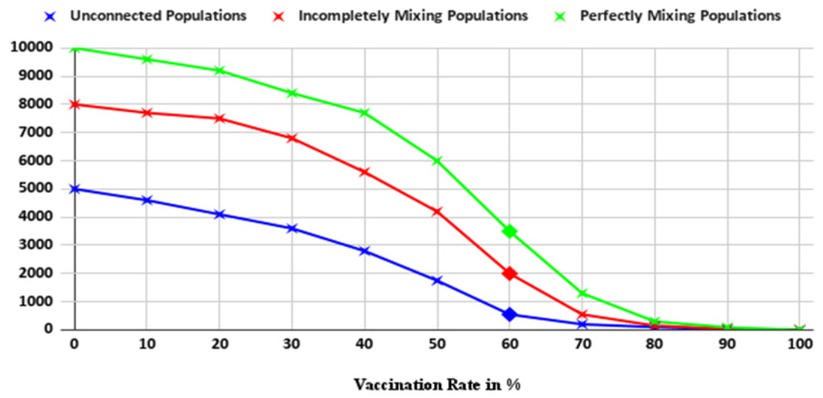
Expected Final Size of an Epidemic in Open Populations. Note and sources: Author’s own calculations.
Let us therefore focus on the realistic case of mutually connected populations with incomplete immunity. To do so, assume first, that both regions have identical levels of immunity. Then, the expected size of an epidemic depends only on the level of connectedness between the two regions. For any given level of vaccination uptake, mixing populations increases the expected size of the epidemic as indicated by the arrow in Figure 5 a.
Next, assume that the level of mixing between the two regions is constant, but vaccination rates differ. Figures 5 b and 5 c show that protecting one more person from becoming fully infected or infective has little impact on the spread of the disease in any of the two countries when vaccination rates are low and the pathogen can draw from a large pool of potential victims. Yet, as the vaccination rate increases, transmission chains are interrupted since the probability increases that infected persons have only contact with immune persons. Hence, the curves in figures 5 b and 5 c become steeper at medium levels of immunization uptake. Finally, as the population approaches herd immunity, the effect of further increasing the vaccination rate declines toward zero because uninterrupted transmission is highly unlikely near the herd immunity threshold.
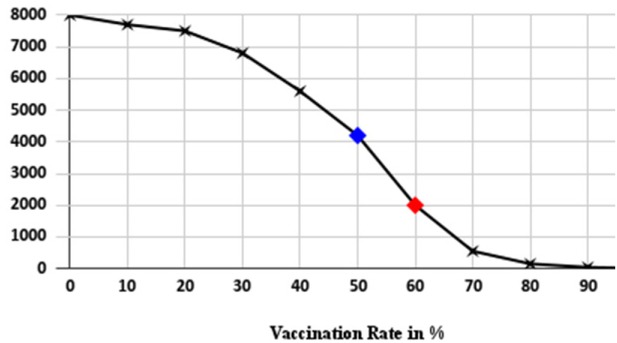
Expected Final Size of an Epidemic in Country 1. Note and sources: Author’s own calculations.

Expected Final Size of an Epidemic in Country 2. Note and sources: Author’s own calculations.
Based on this explanation, it is straight-forward to compare the expected size of an epidemic that involves countries or regions with varying rates of population immunity. To see this, turn again to Figures 5 b and 5 c. The red dot shows the baseline scenario where both countries have the same vaccination rate. If country 1 marginally decreases its vaccination rate and country 2 increases population immunity by the same amount, the expected size of an outbreak is depicted by the blue dots. Since the slope of the epidemic size curve is steeper to the left than to the right, having fewer individuals vaccinated in country 1 will lead to more infections than infections avoided by vaccinating more in country 2. Hence, if initial vaccination coverage is in a critical zone, with medium population immunity, the global burden of the disease increases, if countries fail to coordinate their immunization efforts. Moreover, as shown in Figure 5 a, negative disease spillovers between two countries are larger, the more closely they are connected (i.e. geographically or via trade or migration).
These findings carry clear implications for our understanding of both the German smallpox epidemic of the 19th century and the prevention of future epidemics: Lack of international coordination has potentially disastrous effects, if vaccination is widespread, but not universal.
The previous sections have shown that the German states had introduced vaccination at the beginning of the 19th century and increased the levels of vaccine-derived immunity with varying success. It is important to note that the different states showed little inclination to synchronize their anti-smallpox strategies prior to the 1870 to 1872 epidemic. This is illustrated in Figure 6: The bigger German states are on the vertical axis, while the horizontal axis captures calendar years. For each state, I analyzed if vaccination had been mandatory in a given year.
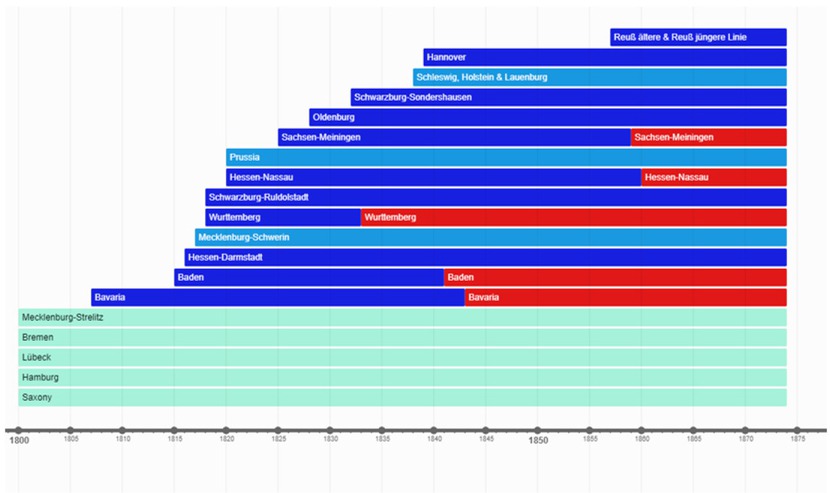
German Vaccination Laws in the 19th century .Note: The different colors correspond to the following cases: (i) Vaccination is completely voluntary (=light blue), (ii) Vaccination is mandatory for the military and/or major subgroups of the population (e.g. children in public schools) (=middle blue), (iii) Vaccination is mandatory for all infants and unvaccinated adults (=dark blue), (iv) Vaccination is mandatory for all infants and revaccination is mandatory at least for subgroups of the population (e.g. soldiers, schoolchildren) (=red). Sources: Medical Department of the Prussian Ministry of War, Die Pocken bei den Deutschen Heeren im Kriege gegen Frankreich 1870/71, unter Berücksichtigung der entsprechenden Verhältnisse bei den Französischen Armeen, bei den kriegsgefangenen Franzosen und bei der Civilbevölkerung der kriegführenden Staaten, Berlin 1885, pp. 116-125.
The occasional smaller epidemic outbreaks (in 1848/1849, 1854 and 1866) had little impact on the legislation of the different states. In fact, the timeline in Figure 6 reveals that no modifications were implemented in the aftermath of 1848/1849 in any of the larger states. In the 1850s only three states took action: In 1857, Baden increased the fee for parents who refused to have their children vaccinated; in 1856 and 1859 respectively, Anhalt-Dessau and Sachsen-Meiningen made the revaccination of schoolchildren mandatory. [37] However, considering the amount of time that had elapsed between the peaks in smallpox cases and the enactment of more rigorous laws, it is questionable if the initiatives were caused by the epidemics or by other considerations.
If the political response to the epidemics in 1848/1849 and 1854 had been lukewarm, the reaction to the prolonged increase in smallpox incidence in the 1860s (which culminated in 1866) was virtually absent: Only one small state (Hessen-Darmstadt) passed regulations mandating the re-vaccination of military recruits. This implies that the vast majority of German states were either unwilling or unable to adjust their vaccination policies to changing epidemic risks.
The persistent heterogeneity in vaccination policies – and the corresponding differences in population immunity – would have been insufficient to create an international prevention externality. To produce substantial disease spillovers, international mobility must be sufficiently high to guarantee an uninterrupted circulation of the pathogen across borders. That this requirement was fulfilled in the second half of the 19th century can be illustrated by simple transport statistics. Between 1850 and 1870, the German railway network that connected German states grew from less than 6,000 to almost 24,000 km. At the same time, passenger volume increased from below 800 to more than 5,600 passengers per km. [38]
Although quantitative data on the spread of diseases are scarce, it is possible to show that regions in the German Confederation integrated not just economically but also epidemiologically during the 19th century. One example of this phenomenon is provided by reports on smallpox mortality published in official statistical reports from Prussia. [39] One report collected data in six Prussian provinces between 1810 and 1816, that is, after the introduction of the cowpox vaccine, but before the arrival of the railway. The second report and set of data come from the period 1862 to 1871 and includes the effect of the transport revolution. When analyzing the two data sets, it turns out that epidemics were largely confined to small geographical areas at the beginning of the century. As depicted in Figure 7, smallpox mortality followed different trends even in neighboring provinces like Eastern and Western Prussia.

Smallpox Mortality in Selected Prussian Provinces, 1810 to 1816 and 1862 to 1871 (per 100,000 inhabitants). Sources: Preussisches Statistisches Landesamt, Karl Friedrich Wilhelm Dieterici (Ed.), Mitteilungen des Statistischen Bureaus (1848–1860), Vol. 4, 1851, p. 309; Zeitschrift des Königlich Preussischen Statistischen Bureaus, Vol. 13.
This is supported by the statistical results in Tables 1 and 2: No pairwise correlation coefficient reaches statistical significance at the 5 percent or 10 percent level in 1810 to 1816. Conversely, in the 1860s and 1870s, smallpox produced very similar patterns of mortality in all provinces and the graphical evidence translates into statistical significance in almost all cases.
Pairwise Correlation Coefficients of Smallpox Mortality 1810 to 1816 (p-values in parenthesis).
| Ostpreußen | Westpreußen | Brandenburg | Berlin | Pommern | Schlesien | |
|---|---|---|---|---|---|---|
| Ostpreußen | 1.00 | |||||
| Westpreußen | 0,006 | 1.00 | ||||
| (0,989) | ||||||
| Brandenburg | -0,621 | -0,082 | 1.00 | |||
| (0,136) | (0,859) | |||||
| Berlin | -0,417 | 0,287 | 0,868* | 1.00 | ||
| (0,352) | (0,655) | (0,011) | ||||
| Pommern | 0,044 | 0,587 | -0,239 | -0,334 | 1.00 | |
| (0,926) | (0,166) | (0,606) | (0,465) | |||
| Schlesien | 0,279 | 0,723 | -0,169 | -0,073 | 0,851 | 1.00 |
| (0,544) | (0,066) | (0,717) | (0,877) | (0,135) |
Pairwise Correlation Coefficients of Smallpox Mortality 1861 to 1872 (p-values in parenthesis).
| Ostpreußen | Westpreußen | Brandenburg | Berlin | Pommern | Schlesien | |
|---|---|---|---|---|---|---|
| Ostpreußen | 1.00 | |||||
| Westpreußen | 0,778** | 1.00 | ||||
| (0,008) | ||||||
| Brandenburg | 0,782** | 0,946*** | 1.00 | |||
| (0,008) | (0,000) | |||||
| Berlin | 0,769** | 0,951*** | 0,999*** | 1.00 | ||
| (0,009) | (0,000) | (0,000) | ||||
| Pommern | 0,767** | 0,924*** | 0,976*** | 0,979*** | 1.00 | |
| (0,007) | (0,000) | (0,000) | (0,000) | |||
| Schlesien | 0,781** | 0;944*** | 0,983*** | 0,982*** | 0,938** | 1.00 |
| (0,008) | (0,000) | (0,000) | (0,000) | (0,010) |
5 Exogenous Effects of Sub-optimal Immunization Levels
The previous section focused on prevention externalities. Externalities explain sub-optimal demand for immunization but fail to account for exogenous factors that contributed to the return of smallpox in the late 19th century. One decisive element was the transport revolution mentioned in the previous section. Other potential explanations include rising levels of urbanization and population density during industrialization. However, the impact of these factors would have been less dramatic if they had not been reinforced by profound changes in Germany’s demographic and epidemiological conditions.
In the pre-vaccination era, smallpox had been a disease of infants and young children. Due to the periodicity of epidemic spikes, the typical age at infection was between a few months and five years of age. This changed when vaccination replaced immunity from natural infection and constant re-exposition to the virus. Since vaccine-induced immunity waned over time, more and more adolescents and adults contracted smallpox and developed less severe or atypical symptoms when they became infected. In fact, the first decades of the 19th century witnessed an ardent scientific debate about a seemingly new infection – termed varioloid disease – whose etiology puzzled the medical community. Recognizing smallpox in vaccinated individuals was a great challenge: In immunologically naive patients the onset of smallpox is quick with high fevers, headaches, intense back- or abdominal pain, followed by the eruption of smallpox lesions. By contrast, vaccinated individuals show diverse symptoms ranging from almost full clinical manifestation to no more than general malaise with few lesions and little to no pustulation. This diversity of symptoms in previously immunized patients made it virtually impossible to distinguish smallpox from other diseases of the skin. Today, serological testing would easily reveal that the varioloid disease was indeed smallpox, which was taking a more benign or mild course in vaccinated patients. However, in the 19th century, this finding had to be established by meticulous observational and statistical analysis and took a long time to become generally accepted. [40]
Detecting and responding to outbreaks was therefore not only difficult because local doctors had to procure enough vaccine in a short amount of time. It was also hard because the disease was not always recognized for what it really was when the first cases occurred. Anecdotal evidence for this problem can be found in a medical journal, where a Prussian district doctor wrote in 1833:
“There were numerous cases of varioloid disease which – due to the mildness of the symptoms – remained undetected. Smallpox was therefore often spread unwittingly to others and the epidemic raged horribly among those who had not been vaccinated before.” [41]
The upward trend in age-specific incidence was not only problematic because it was harder to detect and contain smallpox or varioloid disease. The rising number of infected adults and adolescents also enhanced the virus’ capacity to travel long distances. To understand why this happened, one has to know at which age smallpox incidence peaked in the pre- and post-vaccination eras respectively. Taking Prussia, the biggest German state, as an example, contemporary sources report the following age decomposition for smallpox deaths in a set of outbreaks in the late 18th century: In Berlin, 7,668 patients died of smallpox between 1782 and 1800, half of whom were children below the age of five. In an epidemic which occurred in Silesia in 1796, 409 lethal cases occurred in children between 0 and 6 years of age, while only four adult deaths were recorded. In the same year, an outbreak in the province of Posen claimed 1,250 lives, with 743 deaths in the 0 to 5 age bracket and no casualties among adults aged 20 and above. [42]
Although mortality is an imperfect indicator for morbidity, the small numbers of adult deaths in pre-vaccination era outbreaks are remarkable. Other infectious diseases typically exhibit a U-shaped mortality distribution, with peaks for young infants and for elderly adults. Due to the long-lasting immunity following natural infection, this is not the case for smallpox, where – unless the population is vaccinated – mortality reaches its maximum among children. This finding is confirmed by qualitative evidence: 18th and early 19th century sources typically classify smallpox as a childhood disease (Kinderkrankheit). Contemporary statisticians also complained that death registers did not record smallpox mortality accurately because church records often excluded infants who had died during the first year of life. [43]
An important consequence of the high incidence of smallpox in the youngest age cohorts was that outbreaks used to be limited to relatively small geographical areas. Since infants and young children were less likely to travel long distances than adults, it took epidemic waves a long time to hit localities that were far from their point of origin. A good example for this self-limiting behavior of the disease is the detailed account of a smallpox epidemic in the city of Göttingen in 1766/1767. Göttingen had approximately 8,000 inhabitants, living in 947 houses. The first smallpox cases occurred in the spring of 1766 and the outbreak did not grow beyond adjacent streets until September of the same year. In total, the epidemic caused an excess mortality of 27 percent within the city boundaries, with the disease mostly killing children in the age range of 2 to 6. [44] Contagion outside the city is not mentioned in the otherwise highly detailed source document.
However, data from other states show a similar pattern. For instance, in the 1810s, long-distance transmission was so sporadic in the state of Wurttemberg that sources identify the patient zero who carried the virus into a town or village. For example, an outbreak of smallpox occurred in the district of Ravensburg in the spring of 1813, when a servant girl who had visited family members in Switzerland fell ill upon her return. In 1816, various patients of a surgeon, whose daughter had developed smallpox, were infected after visiting his practice. In the same year, a school in Tübingen had to be closed, after children who had just recovered from the disease had infected twenty of their classmates. [45]
If the relative immobility of young children had limited the speed of transmission in immunologically naive populations, vaccination removed this barrier. Primary immunization led to medium to high immunity in the youngest age cohort. However, individuals who had been vaccinated in infancy but not revaccinated later in childhood lost their protection in adulthood. Since almost no state enforced the re-vaccination of the civilian population and only few practiced the re-vaccination of military recruits, new infections in the 1870 to 1872 epidemic clustered among highly mobile populations (young adults) who also often had the mild varioloid variant of the disease. A report about the 1870 to 1872 epidemic summarized assumptions about the spread of the disease:
“A main determinant of the spread of the epidemic was the enormous volume of traffic in 1870 and 1871. [...] It is likely that the peak of the outbreak in June 1871 was mainly due to the return of soldiers from the war and the influx of travelers during the celebrations of the victory in all bigger cities.” [46]
The fact that the main age at infection had shifted from small children to young adults was certainly an important exogenous driver of the epidemic. This effect was reinforced by another demographic shift. In 1870 to 1872, the smallpox virus could draw on a substantially larger pool of potential victims than in previous outbreaks. One reason for this was the previously discussed loss of vaccine-induced immunity, which added adults to the pool of susceptible population. Yet equally important, population growth also increased the number of unvaccinated infants.
Figure 8 shows that birth rates went up in the 1850s and 1860s. Higher birth rates implied that the absolute number of unvaccinated children would have increased even if the vaccination quota had remained constant. However, as discussed earlier this was not the case and demand for the vaccine had been on a downward trend in many states. The gap between births and vaccinations therefore started to grow rapidly in the decades before 1870.
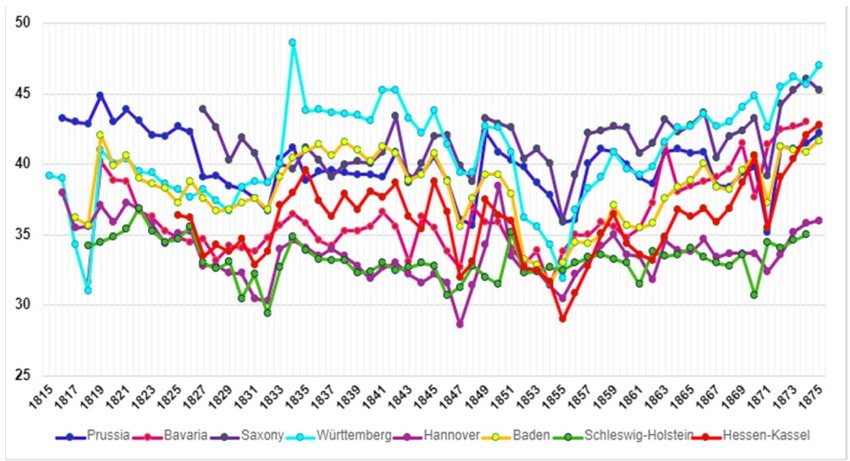
Births rates in Selected German States, 1815 to 1875. Note: Births per 1,000 inhabitants. Sources: A. Kraus/W. Köllmann (Ed.), Quellen zur Bevölkerungsstatistik Deutschlands 1815–1875, Band I, in: Quellen zur Bevölkerungs-, Sozial- und Wirtschaftsstatistik Deutschlands 1815–1875, Boppard am Rhein 1980, https://histat.safe-frankfurt.de/ (10.01.2025).
Infant Mortality Rate in Selected German States, 1820 to 1900. Sources: R. Gehrmann, Säuglingssterblichkeit in Deutschland im 19. Jahrhundert, 1816–900, in: Zeitschrift für Bevölkerungswissenschaft 36/4, 2011, pp. 807-838.
The general decrease in infant mortality, that was happening as part of the demographic transition, was fueling the trend to more unvaccinated infants. States like Bavaria, Wurttemberg and, to a lesser extent, Baden and Hessen-Kassel, all saw a downward trend in infant mortality in the 19th century. Thus, population growth accelerated after mid-century and with it the number of unvaccinated infants and children.
A direct consequence of these trends was that even the states with the strictest vaccination laws were insufficiently prepared when the 1870 to 1872 epidemic occurred. Although their vaccination rates had been higher than elsewhere, the sheer number of persons with missing vaccinations ultimately overwhelmed the public health system. In other words: As the virus began to ravage among a susceptible population that was much larger than in previous epidemics, there was neither enough vaccine nor enough personnel available to stop the outbreak before it became uncontrolled. [47] Demographic trends therefore clearly contributed to the post-honeymoon epidemic of 1870 to 1872 and the death toll of more than 100,000 lives lost in the German Empire alone. [48]
6 Conclusion
Motivated by the COVID-19 pandemic, the aim of this paper was to highlight the risks associated with the re-emergence of formerly controlled vaccine-preventable diseases. I have drawn on historical evidence from the fight against smallpox in 19th century Germany. Early attempts to eliminate the disease failed spectacularly when the so-called honeymoon-epidemic of 1870 to 1872 occurred.
The outbreak had formed against the backdrop of two externalities: A domestic prevention externality stemming from adverse incentives for doctors and individuals and an international prevention externality stemming from coordination failure among the German states. A clear message from the analysis of the international externality is that multilateral agreements, like the 2025 Pandemic Agreement, will play a key role in mitigating the impact of future epidemics. The reason for this is that national epidemic response policies are path-dependent and do not respond flexibly to new epidemiological conditions.
Thus, although the transport revolution dramatically increased mobility between the states of the later German Empire in the second half of the 19th century, national legislation hardly reflected the increased risk of large-scale outbreaks. Similarly, there was little systematic and resolute government action when the growing private prevention externality weakened incentives for immunization and nourished anti-vaccination movements in various German states.
States like Bavaria or Baden, which proved relatively immune to the influence of vaccine-hesitant agitation, had implemented an institutional framework at the beginning of the vaccination-era which, decades later, turned out crucial for sustained popular support of vaccination. The main characteristics of this framework were a high degree of vaccination accessibility for individuals (i.e. regular mass vaccinations), and the dominance of publicly hired and supervised vaccinators, who had easy access to high-quality vaccination lymph.
Translated into the current post-pandemic situation, these findings suggest that the resilience of public health systems against the impact of vaccine-related misinformation depends strongly on the systems’ capacity to establish vaccination habits and to ensure continued support from the medical profession. Measures that serve these aims include regular information campaigns (like the bi-annual smallpox campaigns in Baden), lobbyism by key stakeholders like teachers (similar to the initiatives by teachers and clergy for re-vaccination in Wurttemberg’s Jaxtkreis), or the provision of information material in nontechnical language by respected experts (like Adolf Kussmaul or Rudolf Virchow). Modern media has influenced both the fast spread of misinformation, as well as the potential outreach of evidence-based health communication, but this difference between the 19th and the 21st century is subtle.
The main finding remains that mass vaccination only succeeds when it turns into routine vaccination in the literal sense: It needs to be a generally accepted habit and social norm. Conversely, if vaccination causes more excitement or outrage than the mandate to fasten a seatbelt, even modern industrialized societies will find it hard to attain herd immunity which – for many diseases – requires immunization rates of more than 90 percent.
The historical case of Germany also demonstrates that demographic changes can reinforce the negative impact of sub-optimal vaccination coverage. Thus, regions with fast population growth – and a correspondingly high number of infectible newborns – are at particular risk of experiencing large-scale post-honeymoon epidemics. The potential size and burden of these epidemics further increase due to a shift in the mean age at infection. Historical data from various German states have shown that the age-specific incidence of smallpox shifted from being mostly a childhood disease to being a disease that affected all age groups, particularly adolescents and young adults. This shift was problematic because many of these patients had been vaccinated in infancy and developed only mild and unspecific symptoms. Moreover, increased migration and mobility among and across population was more pronounced among young adults than little children. Accordingly, epidemics were not only harder to detect but also difficult to contain. These historical observations should be understood as warnings for policy makers dealing with future outbreaks of vaccine preventable diseases. In fact, it is not hard to cite examples of current risks that are similar to the factors that contributed to the outbreak of smallpox in the 1870s. Thus, present-day health experts have repeatedly voiced concerns about the fact that pertussis might spread unnoticed in under-vaccinated populations due to the asymptomatic transmission among adults. This is extremely worrisome because infants are too young to be vaccinated, yet they are at disproportionately high risk of severe disease outcomes, including hospitalization and death. Another example is the upward shift in the age-specific incidence of rubella which used to be a childhood disease before the widespread introduction of the MMR vaccine. Today, rubella outbreaks are rare and affect not only children but also unvaccinated adults. This age-shift is a serious concern because rubella causes severe complications in pregnant women.
If anything, the historical case therefore suggests that international efforts to speed up the response to outbreaks of new pathogens are a central but not the only component of an effective epidemic preparedness strategy. Besides coping mechanisms for new public health threats, resilience to old diseases will be equally important to reducing the global burden of morbidity and mortality. Establishing and maintaining this resilience is a gradual and time-consuming process that depends on the continued involvement of health professionals, state officials and individual citizens. The costs of maintaining population immunity above the herd immunity threshold are high – but so are the benefits. If polio, diphtheria, pertussis or measles get a chance to return, just as smallpox did in 19th century Germany, these diseases will return. And the expected harm will exceed the costs of vaccination programs by great magnitude.
About the author
Katharina Muehlhoff is an associate researcher at the Center for Population Health at Stanford Medical School and the Heidelberg Institute of Global Health (HIGH). She studied at the University of Mannheim, where she completed her PhD in economic history and development economics in 2016. Afterwards, she worked as an assistant professor of economic history and demography at Carlos III University of Madrid. Her research focus is on historical epidemiology, demography and population health. In 2024 she joined the HIGH to investigate non-pathogen specific side effects of vaccination. Her current projects investigate the possibility that herpes zoster vaccination might prevent or delay the onset of neurological disorders like Alzheimer’s disease.
© 2025 Katharina Muehlhoff, published by De Gruyter
This work is licensed under the Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Articles in the same Issue
- Frontmatter
- Obituary for Eckart Schremmer
- Special Issue Articles
- Epidemics and Pandemics in Economic-historical Perspective – An Introduction
- Cholera in the City of Poznań: Did the Death Toll of the 1866 Cholera Epidemic Reflect Social and Economic Differences?
- The Mortality Impact of Cholera in Germany
- When Diseases Return from the Epidemiological Honeymoon: The Reemergence of Smallpox in 19th Century Germany and its Lessons for Public Health Policies after COVID-19
- On the Economic Costs of the Spanish Flu Pandemic in Germany: An attempt at Assessing GNP Lost for 1918
- Malaria in Catania/Sicily: Local Manifestations and International Scientific Cooperation During a Pandemic in the 1920s
- Geographical Aspects of Diphtheria in England and Wales: Immunisation and the Spatial Sequence of Retreat to Effective Elimination, 1921 to 1964
- Pandonomics: Why Economics was Unprepared for COVID-19-Policies
- Research Forum
- “Stupid” German Money? Bonus Interest Rate Payments on Savings Deposits During the Stagflation of 1967 to 1984
- Geography and Space in Recent Economic History
Articles in the same Issue
- Frontmatter
- Obituary for Eckart Schremmer
- Special Issue Articles
- Epidemics and Pandemics in Economic-historical Perspective – An Introduction
- Cholera in the City of Poznań: Did the Death Toll of the 1866 Cholera Epidemic Reflect Social and Economic Differences?
- The Mortality Impact of Cholera in Germany
- When Diseases Return from the Epidemiological Honeymoon: The Reemergence of Smallpox in 19th Century Germany and its Lessons for Public Health Policies after COVID-19
- On the Economic Costs of the Spanish Flu Pandemic in Germany: An attempt at Assessing GNP Lost for 1918
- Malaria in Catania/Sicily: Local Manifestations and International Scientific Cooperation During a Pandemic in the 1920s
- Geographical Aspects of Diphtheria in England and Wales: Immunisation and the Spatial Sequence of Retreat to Effective Elimination, 1921 to 1964
- Pandonomics: Why Economics was Unprepared for COVID-19-Policies
- Research Forum
- “Stupid” German Money? Bonus Interest Rate Payments on Savings Deposits During the Stagflation of 1967 to 1984
- Geography and Space in Recent Economic History

