Comparison of the effectiveness of eHealth self-management interventions for pain between oncological and musculoskeletal populations: a systematic review with narrative synthesis
-
Margaux Evenepoel
Abstract
Objectives
The aim of this systematic review is to compare the effectiveness of eHealth self-management interventions on pain intensity between oncological and musculoskeletal populations and to examine barriers and facilitators of the use of eHealth self-management tools.
Content
In March 2021, a systematic search of the literature was conducted using the databases PubMed and Web of Science. Studies that investigated the effect of eHealth self-management interventions on pain intensity in an oncological and/or a musculoskeletal population were included.
Summary
No study was found with a direct comparison of the two populations. Of the ten included studies, only one (musculoskeletal) found a significant interaction effect in favor of the eHealth program and three (musculoskeletal and breast cancer) showed a significant time-effect of the eHealth intervention. In both populations user-friendliness of the tool was considered as a facilitator, the length of the program and the lack of an in-person session as barrier. Due to the absence of a direct comparison, no conclusion can be made on how the effectiveness differs between both populations.
Outlook
Further research should incorporate patient-experienced barriers and facilitators and there is a high need of studies making the direct comparison of the effect of an eHealth self-management intervention on pain intensity in an oncological vs. a MSK population.
Introduction
Pain is one of the most common, complex and persisting symptoms worldwide [1, 2]. Pain has a considerable impact on a person’s life as it is often associated with other symptoms such as fear of movement, anxiety, sleep disturbances as well as a decrease in physical activity, social functioning and quality of life [3], [4], [5], [6].
The ICD-11 (International classification of diseases 11th revision) classifies pain into acute and chronic pain. Other classifications, based on the established pathophysiology of pain, are prevalent in the existing literature resulting in a categorization of non-cancer vs. cancer-related pain [7]. Cancer-related pain has a prevalence of 39 % after curative cancer treatment, 55 % during cancer treatment and 66 % in advanced stages of cancer [8]. Within the non-cancer related pain group, pain associated with musculoskeletal (MSK) conditions has the highest prevalence [9, 10].
Pain is an individual experience, that is influenced by biological, social and psychological factors [11], [12], [13], [14]. The dichotomy between cancer and non-cancer related pain is focused on the associated condition, which is only one aspect of pain. As mentioned before, psychological and social factors are also involved in the experience of pain. Which could explain why, regardless of the abovementioned categorization, there are a number of similarities as to what the best evidence for pain management is in both populations [11], [12], [13].
Patient education and exercise therapy are core concepts of chronic pain management, both in MSK-related or cancer-related pain [11], [12], [13]. In acute pain management, pharmaceuticals are recommended as first line treatment. However, due to the risk of these treatments, like opioid-tolerance, there is a trend to use non-pharmacological approaches in acute pain, similar to those used in chronic pain management [15]. Next to that, clinical guidelines in both populations also emphasize the need for a more individual and patient-centered approach. In this patient-centered care, self-management interventions are highlighted due to their integration of the patient’s perspective and preferences.
Self-management interventions have been proven to positively influence the wellbeing of patients with pain [16, 17]. Within the literature, there is a lack of agreement on the definition of self-management. The most used definition is: “Individual’s ability to manage the symptoms, treatment, physical and psychosocial consequences and lifestyle changes inherent in living with a chronic condition”. This definition has evolved to include all health conditions. Within self-management, the role of the health-care provider (HCP) is regarded to be a more supportive role [18]. For the purpose of this review, we regard self-management as the patients’ ability to self-manage their pain individually, without the active involvement of an HCP.
New opportunities for supporting self-management skills can be found in eHealth. EHealth describes any form of digital technology that assists health care [19]. It can provide a solution for barriers of in-person interventions such as financial costs, time-consumption or limited access to health care facilities [20]. Despite these benefits, implementing eHealth also provides challenges on an individual, environmental and technical level [21].
The literature on the use and effectiveness of eHealth is growing. Several reviews show that these interventions are effective in the management of pain in subgroups of an MSK [22], [23], [24] as well as an oncological population [25].
The positive effect of self-management through eHealth suggests that a similar approach to pain management might be possible in both populations. However, it remains unclear how these interventions are organized and how their design compares within both oncological and musculoskeletal (MSK) populations. Next to that, the comparison of the effectiveness of these eHealth self-management interventions in these two populations has yet to be fully explored. In light of these gaps in the literature, the purpose of this review is to provide an overview of how these eHealth self-management interventions are organized in an oncological vs. a MSK population and how they compare to each other in terms of design and effectiveness.
Methods
This systematic review was registered within the International Prospective Register of Systematic Reviews (PROSPERO reference 245857) and adhered to the PRISMA statement recommendations [26].
Data sources and searches
The systematic search of the literature was conducted using the databases PubMed and Web of Science. In Table 1, the key words of this systematic search are shown, which was performed on 3rd March 2021. The search was built based on the primary research question regarding the design and the effectiveness of an eHealth self-management intervention on pain intensity. Secondary, information on barriers and facilitators was extracted from the retrieved literature. However, as this was no eligibility criteria, it was not included in the search strategy.
Key words search strategy.
| Key words | MESH-terms |
|---|---|
| Cancer OR neoplasms OR musculoskeletal AND Online OR internet OR digital OR web OR telehealth OR mhealth OR mobile OR eHealth OR telemedicine OR technology OR app OR application AND Education OR self-management OR self management AND Pain |
Neoplasms OR musculoskeletal system AND Online system OR internet OR web-browser OR Telemedicine OR Internet-based intervention OR educational technology OR Medical informatics applications OR mobile applications AND Self-management OR education OR patient education as topic OR health education AND Pain OR cancer pain OR musculoskeletal pain |
Study selection
Original experimental trials that investigated the effect of an eHealth self-management intervention (I) on pain intensity (O) in an adult oncological or MSK population (p) were included in this review. No distinction was made between acute or chronic pain. Self-management was considered as: “The patients’ ability to manage their pain individually, without the active support of an HCP.”
Included articles had to be published in English, Dutch, French or German. Exclusion criteria were: pain intensity not included as outcome measure; studies in children or adolescents; studies conducted in nursing homes (because of the often more advanced disease stage in these patients) and studies including patients with metastases, palliative patients and patients with leukemia or lymphoma. When it was unclear which population was included, the author was contacted. If this information remained unclear after a time-frame of two weeks, the study was excluded. When the intervention as well as the control group was a combination of a digital and an in-person session, had active involvement of an HCP or when the eHealth was solely carried out in a clinical setting, like in a hospital, the study was also excluded. After removing duplicates, title and abstract were screened double-blinded by two independent authors (M.E. and S.V.D.). The remaining full texts were screened and conflicts were further discussed and resolved through consensus. A third reviewer (A.D.G.) was involved when conflicts were not resolved through consensus.
To screen the included articles, we made use of the software Covidence to manage our systematic review (www.covidence.org) [27].
Data extraction
Data extracted for this systematic review included: author(s), year of publication, study design, setting, continent and country of origin, sex, age, sample size, type of cancer or MSK condition, cancer stage if applicable, description of the intervention and eventual control group, method of data collection, results, pain definition and method of pain measurement, type and duration of pain and pain recall period (point, week, month, year). When applicable, barriers and facilitators for the self-management interventions were registered.
Quality assessment
Two reviewers (M.E. and S.V.D.) independently evaluated the risk of bias of included studies, using the Revised Cochrane risk-of-bias tool for randomized trials (RoB2.0). Conflicts were discussed and resolved through consensus. A third reviewer (A.D.G.) was involved when conflicts were not resolved through consensus.
Data synthesis and analysis
Because of the heterogeneity of the included studies, statistical analyses were not performed within this systematic review. This systematic review adopted a narrative description of the effect of an eHealth self-management intervention on pain intensity, without distinguishing between the different questionnaires to measure pain intensity.
Results
Study search
The initial search included 2,670 articles (see Figure 1). After removing duplicates, 2,389 articles were included for title/abstract screening. After title/abstract screening, 60 articles were included for full-text screening. A total of 49 articles were excludes for various reasons. In conclusion, 11 articles, consisting of 10 individual studies, met the predefined eligibility criteria and were included in this systematic review.
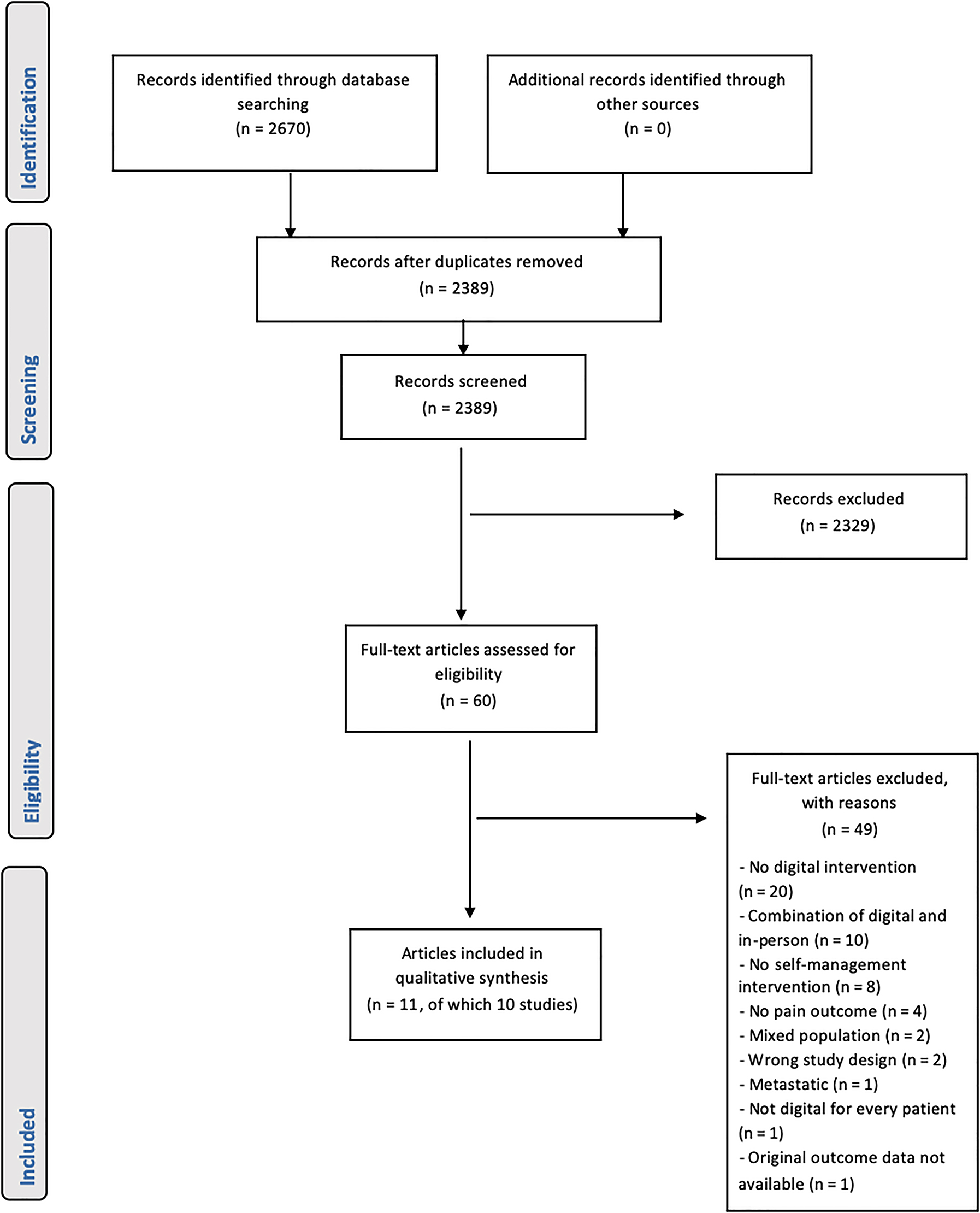
Flow chart of the study selection process.
Risk of bias
Figure 2 gives an overview of the assessment of risk of bias. All studies contained at least one domain with a high risk of bias, resulting in an overall high risk of bias score [28], [29], [30], [31], [32], [33], [34], [35], [36], [37], [38]. The uncontrolled have a high risk of bias on all domains except domain 5. The lack of control group results in no randomization process (D1), no concealment of assigned intervention (item 2.1 domain 2, Figure 2), important non-protocol interventions cannot be balanced across different groups (item 2.3 domain 2, Figure 2) and as there is no comparison group we cannot assess if measurements differ between two groups (D4, Figure 2) [31], [32], [33]. Two RCTs were also scored with a high risk of bias on D1 (bias arising from the randomization process), because the allocation sequence was not concealed until participants were enrolled and assigned to the interventions [36], [37], [38], five studies with a high risk of bias on D2 (bias due to deviations from the intended intervention), because of an inappropriate or absent analyses to estimate the effect of adhering to intervention [28, 29, 35], [36], [37], [38], and three studies with a high risk of bias on D3 (bias due to missing outcome data), due to a drop-out of more than 5 % and due to a lack of evidence that the result was not biased by missing outcome data [29, 30, 37, 38].
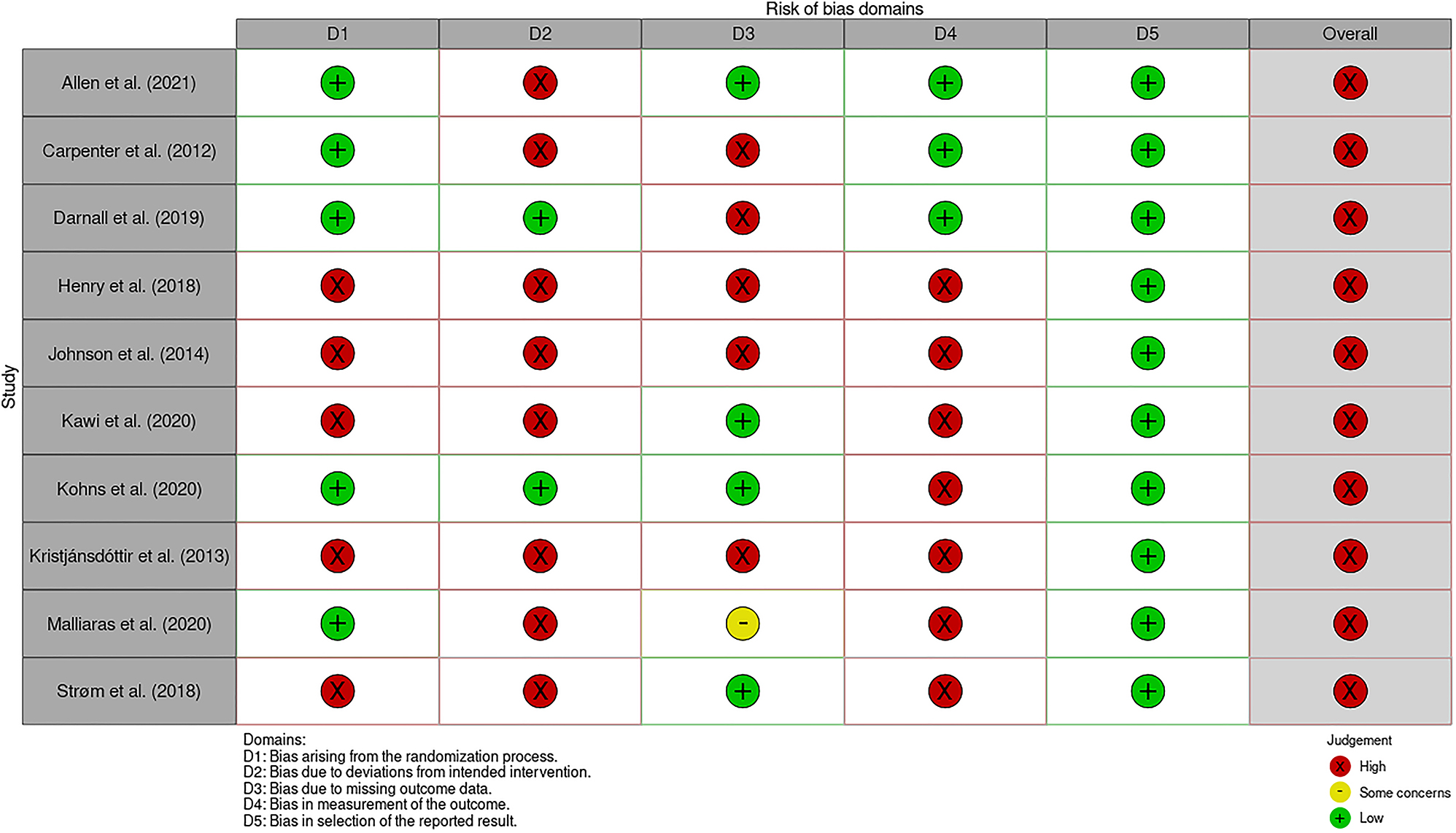
Risk of bias assessment.
Study characteristics
The study characteristics can be found in Table 2. None of the studies performed a direct comparison between the populations. Out of the 10 included studies, only two studies evaluated an oncological population, namely breast cancer [30, 31], and eight studies evaluated MSK conditions [28, 29, 32], [33], [34], [35], [36], [37], [38], including patients with knee osteoarthritis (n=1) [28], low back pain (n=2) [29, 36], overall chronic MSK pain (n=3) [32], [33], [34], fibromyalgia and chronic widespread pain (n=1) [37, 38] and patients with rotator-cuff related shoulder pain (n=1) [35].
The design of the studies with a breast cancer population were an uncontrolled clinical pilot trial [31] and an RCT [30]. Pain intensity was measured in both studies with the Patient-Reported Outcomes Measurement Information System - 29 (PROMIS-29) [30, 31]. The studies that evaluated patients with MSK-related pain consisted of two uncontrolled studies [32, 33], including one pilot study [32], and six RCTs [28, 29, 34], [35], [36], [37], [38], including two pilot studies [34, 35]. Pain intensity was measured with the Brief Pain Inventory (BPI) questionnaire [33, 34], a Numeric Rating Scale (NRS) [29, 32], a Visual Analogue Scale (VAS) [35, 37, 38], the Western Ontario and McMasters Universities Osteoarthritis Index (WOMAC) [28] and with the Low Back Pain Rating Scale (LBPRS) [36].
Characteristics of the eHealth self-management interventions.
| Study | Populationa | Groupb | Durationc | Frequencyd | Digital mediume | Formatf | Contente |
|---|---|---|---|---|---|---|---|
| Darnall et al. [30] | BC | I “my surgical success” | 90 min | O/A | W | Video audio |
CBT skills to regulate cognition, emotion, hyperarousal related to pain such as thought reframing, relaxation and attention modulation Education on mind–body science |
| C | O/A | W | Written material | Education on health and nutrition in terms of recovery after surgery | |||
| Henry et al [31] | BC | I “PROSPECT” | 8 week | U/A | W | Written material video | Education on late effects of therapy, symptom management and lifestyle change |
| Allen et al. [28] | MSK | I “STEP-KOA” | 3 month | U/A | W | Written material pictures video | Exercise recommendation stretching, strengthening and aerobic exercise with 7 levels, including progression based on WOMAC-scores |
| C | 9 month | Every 2 week | Written material | Education on topics related to osteoarthritis and its management | |||
| Carpenter et al. [29] | MSK | I “Wellness Workbook” | 3 week | U/A | W |
Interactive format:
Written material |
CBT cognitive restructuring, stress management, relaxation training, mindfulness, and values-based behavioral activation Education on pain and biopsychosocial pain management |
| C | 3 week | Wait-list | |||||
| Kohns et al. [34] | MSK | I | 20–25 min | O/A | W | Written material video |
Education on cognitive, emotional, social, and developmental processes and the neuroscience of pain Self-assessment of pain location, of signs of central sensitization and psychological factors |
| C | 20–25 min | O/A | W | Written material video |
Education on general health Self-assessment of health behaviors |
||
| Kristjánsdóttir et al. [37, 38] | MSK | I | 4 week | U/A | S |
Interactive format:
Written material Audio HCP-interaction |
CBT ACT exercises, Mindfulness, self-reflection, feedback on exercises and self-reflection by HCP |
| C | 4 week | U/A | W | Written material Audio |
CBT non-interactive exercises (ACT, mindfulness) | ||
| Malliaras et al. [35] | MSK | I1 | 12 week | U/A | W |
Interactive format:
Written material Infographics Video |
Exercise recommendation shoulder exercises based on best-evidence and expert consensus Education on causes of RCRSP, pain mechanisms, exercise and other treatments |
| I2 | 12 week | U/A | W |
Interactive format:
Written material Infographics Video HCP interaction |
Exercise recommendation shoulder exercises based on best-evidence and expert consensus Education on causes of RCRSP, pain mechanisms, exercise and other treatments Telerehabilitation weekly session with a physiotherapist |
||
| C | 12 week | U/A | W | Written material Infographics | Education on rotator cuff muscles, risk factors and advice on activity-modulation | ||
| Strøm et al. [36] | MSK | I “w-SPIINA program” | 1–5 week | U/A | W | Written material Video |
Education on course of treatment and rehabilitation CBT information and use of images to reduce anxiety, catastrophic thoughts, and misconceptions in relation to surgery Online support group self-assessment of pain and physical ability |
| C | In person | Orally written material | Standard course of treatment, rehabilitation, and information | ||||
| Johnson et al. [32] | MSK | I | 30 day | U/A | W + S |
Interactive format:
Written material Game design |
CBT behavioral change based on TTM: Stage-matched guidance on decisional balance, self-efficacy, processes of change and goal setting Education on stress-management, healthy sleep habits and pain coping skills Online support group self- assessment of pain symptoms |
| Kawi et al. [33] | MSK | I | 8 min | U/A | S | Video | Instruction and demonstration on auricular point acupressure |
-
aBC, breast cancer; MSK, musculoskeletal; bI, intervention group; C, control group; cW, weeks, Mo, months; D, days; Min, minutes; dU/A, unrestricted access; O/A, one time access; eW, web-based; S, smartphone-based; fHCP, health care provider; gCBT, cognitive behavioral therapy; WOMAC, Western Ontario & McMaster Universities Osteo-arthritis Index; ACT, acceptance and commitment therapy; RCRSP, rotator cuff–related shoulder pain; TTM, transtheoretical model.
Most studies were conducted in the USA (n=7) [28, 29, 32], [33], [34], one study in Norway [37, 38], one in Australia [35] and one in Denmark [36].
Characteristics of the eHealth Self-management interventions
Details of the characteristics of the eHealth self-management interventions can be found in Table 2.
Medium
A website was the most used medium in both populations to share written material and videos. Within the studies of the musculoskeletal population, smartphone based formats were also used, ranging from an interactive game design [32], an app [33] or a mobile accessible a webpage with information [28, 29, 34], [35], [36].
Content
Similarities within the oncological studies were the modalities to facilitate self-management, namely patient education and a cognitive-behavioral approach. Comparing this to the MSK population, additional modalities including advice for physical exercise, self-report of symptoms and social support were used.
The content of educational material varied form study to study. Themes that were only seen in oncological studies was information on mind-body science [30] and specific information on late effects of oncological therapy [31]. Other educational themes that were incorporated in all studies were condition-specific information [28, 35, 36], symptom management, lifestyle changes. Themes that only occurred in the musculoskeletal population were education on pain itself [29, 32, 34] or specific instructions on a technique [33].
Concepts of cognitive behavioral therapy (CBT) were another similarity. The modalities in the oncological studies were limited to thought reframing [30], goal setting [31] or relaxation exercises [30, 31]. All these modalities were also part of the CBT in musculoskeletal populations, with the addition of meditation exercises [29], self-evaluation and self-reflection exercises [34], guidance on decisional balance, improving self-efficacy, and acceptance and commitment therapy [37, 38].
In the studies with a musculoskeletal population, there were some additions in content that were not prevalent in the oncological studies: self-evaluation of symptoms [36], [37], [38], instructions and recommendations for physical exercise [28, 35] and-lastly, the use of peer support [32, 36].
Within the control groups of the RCTs, two studies used another eHealth program [28, 34]. These programs consisted of education on topics related to osteoarthritis and its management [28] and of education and self-assessment on general health behaviors [34].
Delivery
Two studies compared an individual intervention to one with support of an HCP [35, 37, 38]. In one study, the non-HCP supported group consisted of non-interactive CBT exercises [37, 38] and in the other of education on rotator cuff muscles, risk factors and advice on activity-modulation [35].
Duration
The duration of the interventions varied between a video of 8 min to a program of 3 months, with most interventions being around the one-month duration.
The effect of an eHealth self-management intervention on pain intensity
Oncological population
One RCT, reporting on post-operative pain after curative breast cancer surgery, found no significant interaction effect in pain intensity (p time x group=0.53) [30]. However, a significant decrease in pain intensity over time was seen within the intervention group (p=0.0002) which received pain education and CBT in comparison to the control group, who received general health information [30].
The uncontrolled trial, that used an education intervention cancer-specific symptom management after curative treatment, found that none of the symptoms significantly improved in the group of patients who reported pain as their primary symptom. However, in the large cohort of the sample, which consisted of patients with a primary complaint of pain or fatigue or insomnia, significant decrease in pain intensity over time at eight weeks follow-up was shown (p<0.001) [31].
MSK population
Of the six RCT’s [28, 29, 34], [35], [36], [37], [38], only two RCTs reported a significant difference in treatment effects between groups [34, 36], one in favor of the experimental group [34], one in favor of the control group. [36].
Kohns et al. [34] observed a significant decrease in pain intensity in the intervention group (eHealth: biopsychosocial pain education) in comparison with the control group (eHealth: general health education) at one month follow-up (p time x group=0.024), but not at 10 months follow-up (p time x group=0.434) [34]. The other RCT, studying post-operative pain in patients after lumbar fusion surgery, reported a significant difference in leg pain two days after surgery within the control group (usual treatment) (p time x group=0.01), vs. the eHealth group, who received education on the treatment and rehabilitation, CBT, learned self-assessment of pain and physical ability and had access to an online support group [36].
One uncontrolled pilot trial reported a significant decrease over time in all pain outcomes after 30 days of self-management intervention [32]. This pilot study included CBT, pain education, an online support group and self-assessment of symptoms.
Other studies [28, 29, 33, 35, 37, 38] did report results in favor of the eHealth intervention, albeit non-significant. Details of the includes studies can be found in Table 3.
Effect of an EHealth self-management intervention on pain intensity.
|
Study IDa |
Inclusion and exclusion criteria | Patient characteristicsb | Interventionc (more information within Table 3) | Outcome measuresd | Resultse |
|---|---|---|---|---|---|
| Age: mean (SD or range) | |||||
| Darnall et al. RCT (pilot) USA (N-A)[30] |
Inclusion criteria
|
|
Intervention group (n=36):
Before surgery: “My surgical success” Control group (n=32): Before surgery: Digital general health education |
Method of data collection
Questionnaire/interview Tools used for data collection PROMIS (of last 7 day): Pain intensity subscale Times of data collection T0: Baseline T1: 2 weeks after surgery T2: 4 weeks T3: 8 weeks T4: 12 weeks |
Mean (SEM)
Within groups Intervention T0: 1.47, SEM=0.12 T4: 1.98, SEM=0.10 p=0.0002a Control T0: 1.75, SEM=0.13 T4: 1.86, SEM=0.10 p=0.4191 Between groups Intervention vs. Control I: 1.73, SEM=0.09 C: 1.81, SEM=0.09 p=0.53 |
| Henry et al. UT (pilot) USA (N-A)[31] |
Inclusion criteria
A diagnosis of obstructive sleep apnea or restless leg syndrome that was currently interfering with sleep |
(A) Total cohort
|
Intervention:
“PROSPECT” cancer-specific symptom management |
Method of data collection
Questionnaire Tools used for data collection PROMIS-29: Subscale pain intensity Times of data collection T0: Baseline T1: 8 weeks |
(A)
Mean T0: 3.62 T1: 2.66 Difference mean (SD) T0–T1: −0.89 ± 1.7 p<0.001a (B) Mean T0: 4.9 T1: 4.4 Difference mean (SD) T0–T1: −0.5 ± 1.8 p=0.44 |
| Allen et al. RCT USA (N-A) [28] |
Inclusion criteria
|
|
Intervention group (n=230):
STEP-KOA, step 1: Exercise program Control group (n=115): Educational materials |
Method of data collection
Interview Tools used for data collection WOMAC: Pain subscale Times of data collection T0: Baseline T1: 3 months |
Mean difference (range)
Within groups Intervention T0–T1: −1.0 (−1.5 to −0.5) Control T0–T1: −0.1 (−0.7 to 0.5) Between groups: Mean difference T1 I-C: −0.9 (−1.7 to −0.1) |
| Carpenter et al. RCT USA (N-A) [29] |
Inclusion criteria
See inclusion criteria |
|
Intervention group (n=70): “Wellness Workbook” Control group (n=71): Wait-list control group, after 3 weeks access to wellness workbook |
Method of data collection
Questionnaire Tools used for data collection NRS (of the last 7 day):
T0: Baseline T1: 3 weeks after start intervention T2: 6 weeks after start intervention |
Mean (SD)
Within groups Average pain score: Intervention T0: 5.2 (1.5) T1: 5.2 (1.5) T2: / Control T0: 5.7 + 1.7 T1: 5.7 + 1.7 T2: / Lowest pain score Intervention T0: 3.1 + 1.8 T1: 3.3 + 1.9 T2: / Control T0: 3.7 + 2.0 T1: 4.0 + 2.0 T2: / Highest pain score Intervention T0: 7.2 + 1.6 T1 7.0 + 1.8 T2: / Control T0: 7.4 + 1.6 T1: 7.3 + 1.6 T2: / Between groups Average pain score: T1: p=0.507 Lowest pain score T1: p=0.549 Highest pain score T1: p=0.784 |
| Kohns et al. RCT (pilot) USA (N-A) [34] |
Inclusion criteria
|
|
Intervention (n=51):
PPN self-evaluation intervention Control (n=53): General health education |
Method of data collection
Questionnaire Tools used for data collection BPI (last 7d): mean of:
T0: Baseline T1: 1 month T2: 10 months |
Mean (SD)
Within groups Intervention T0: 4.98 ± 1.54 T1: 4.03 ± 0.18 T2: 4.46 ± 0.23 Control T0: 4.50 ± 1.73 T1: 4.60 ± 0.17 T2: 4.21 ± 0.23 Between groups Intervention vs. control T1: p=0.024a T2: p=0.434 |
| Kristjánsdóttir et al. RCT Norway (EU) [37, 38] |
Inclusion criteria
|
|
Intervention group (n=68):
Self-help pain management material Control group (n=48): An interactive CBT-intervention + HCP interaction + self-help pain management material |
Method of data collection
Questionnaire Tools used for data collection VAS Times of data collection T1: Baseline, after inpatient rehabilitation program T2: Completion smartphone intervention (4 weeks) T3: 6 months after T1 T4: 12 months after T1 |
Within groups
Mean (SD) intervention T1: 52.99 ± 21.27 T2: 50.56 ± 23.37 T3: 58.45 ± 22.46 T4: 55.85 ± 2.73 Control T1: 53.07 ± 22.20 T2: 54.14 ± 24.06 T3: 51.96 ± 23.76 T4: 56.28 ± 28.24 Mean difference (range) Intervention T2–T3: −0.99 (−7.48 to 5.50) (p=0.76) T2–T4: 5.82 (−1.26 – 12.90) (p=0.10) Control T2–T3: 1.11 (−3.94 to 6.16) (p=0.66) T2–T4: 0.61 (−7.03 to 8.24) (p=0.87) Between groups Effect size T2: −0.15 (p=0.49) T3: 0.28 (p=0.22) |
| Malliaras et al. RCT (pilot) Australia (O) [35] |
Inclusion criteria
|
|
Intervention group (n=12)
|
Method of data collection Questionnaire Tools used for data collection VAS: Worst pain last 7 days Times of data collection T0: Baseline T1: 6 weeks T2: 12 weeks |
Mean (SD)
Within groups Intervention Advice only: T0: 56.8 ± 17.9 T1: 55.7 ± 22.2 T2: 41.8 ± 23.1 Recommended care T0: 51.6 ± 22.4 T1: 41.5 ± 22.2 T2: 44.8 ± 28.1 Control Recommended care and telerehabilitation T0: 59.7 ± 21.1 T1: 31.9 ± 23.1 T2: 28.1 ± 25.6 |
| Strøm et al. RCT Denmark (EU) [36] |
Inclusion criteria
|
|
Intervention group (n=48):
|
Method of data collection
Questionnaire Tools used for data collection LBPRS Times of data collection T0: Baseline (1–5 week before surgery) T1: 2 days after surgery T2: 3 months T3: 6 months |
Median (IQR)
Within groups Back pain−back pain right now Intervention T1: 6 (5–7) T0-T1: 1 (2–0) T2: 3 (1–5) T0–T2: −2 (−1 to −4) T3: 3 (2–4) T0–T3: −3 (−1 to −4) Control T1: 5 (3.5–7) T0–T1: 0 (−2 to 2) T2: 3 (1–4) T0–T2: −3 (−1 to −4) T3: 3 (1–5) T0–T3: −2 (−1 to −4) Between groups Between group difference p-value T1: p=0.42 T2: p=0.38 T3: p=0.51 Within groups Back pain−the worst back pain within the last 14 days Intervention T1: 9 (8–10); 1 (2–0) T2: 6 (3–8); −2 (−4 to 0) T3: 5 (3–7); −3 (−4 to 0) Control T1: 9 (8–10) T0–T1: 1 (2–0) T2: 5 (2–8) T0–T2: −3 (−5 to 0) T3: 5 (2–7) T0–T3: −3 (−5 to 0) Between groups Between group difference p-value T1: p=0.78 T2: p=0.24 T3: p=0.59 Within groups Back pain−median back pain within the last 14 days Intervention T1: 6 (5–7) T0–T1: 0 (1 to −1) T2: 3 (2–5) T0-T2: −2 (−0.5 to −3.5) T3: 3 (2–5) T0–T3: −2 (−1 to −4) Control T1: 8 (5–8) T0–T1: 0 (1 to −1) T2: 3 (1.5–5) T0–T2: −3 (−1 to −4) T3: 4 (2–5) T0–T3: −2 (−1 to −4) Between groups Between group difference p-value T1: p=0.79 T2: p=0.26 T3: p=0.98 Within groups Leg pain−leg pain right now Intervention T1: 3 (2–6) T0–T1: 1 (3–2) T2: 2 (0–5) T0–T2: −2 (−5 to 0) T3: 1 (0–5) T0–T3: −2.5 (−5 to 0) Control T1: 2 (0–4) T0–T1: 3 (5–0) T2: 1 (0–3) T0–T2: −3 (−5 to −1) T3: 1 (0–4) T0–T3: −3 (−5 to −1) Between groups Between group difference p-value T1: p=0.01a T2: p=0.17 T3: p=0.38 Within groups Leg pain−the worst leg pain within the last 14 days Intervention T1: 7 (6–9) T0–T1: 1 (0–3) T2: 3 (1–7) T0–T2: −1.5 (−4 to 0) T3: 4 (1–8) T0–T3: −2 (-4 to −1) Control T1: 7.5 (5.5–9) T0–T1: 1.5 (0–4) T2: 1 (0–5) T0–T2: −2 (−4 to 0) T3: 2 (0–6) T0–T3: −2(−4 to 0) Between groups Between group difference p-value T1: p=0.40 T2: p=0.73 T3: p=0.62 Within groups Leg pain–median leg pain within the last 14 days Intervention T1: 5 (5–7) T0–T1: 0 (−2 to 0) T2: 2 (1–5) T0–T2: −3 (−5 to −1) T3: 2 (1–6) T0–T3: −2 (−5 to −1) Control T1: 5 (3–7) T0–T1: 0 (1 to −2) T2: 1 (0–3) T0–T2: −3 (−5 to −1) T3: 1 (0–5) T0–T3: −3 (−5 to 0) Between groups Between group difference p-value T1: p=0.20 T2: p=0.55 T3: p=0.51 |
| Johnson et al. UT (pilot) USA (N-A) [32] | Inclusion criteria
Currently undergoing treatment with a psychologist, psychiatrist, or other mental health professional for a condition such as bipolar disorder, anxiety, or substance abuse |
|
Intervention:
Health eRide program |
Method of data collection
Questionnaire Tools used for data collection NRS (last 7d):
T0: Baseline T1: After 30202Fdays |
Mean (SD)
Pain now T0: 5.8 ± 2.1 T1: 5.0 ± 2.0 T0-T1: p=0.002a Usual pain past week T0: 6.8 ± 1.6 T1: 5.4 ± 1.9 T0–T1: p<0.001a Best pain past week T0: 4.9 ± 2.1 T1: 4.0 ± 2.1 T0–T1: p=0.002a Worst pain past week T0: 8.3 ± 1.4 T1: 7.0 ± 1.7 T0–T1: p<0.001a |
| Kawi et al. UT USA (N-A) [33] |
Inclusion criteria
Any allergy to latex (tapes used on ear points) |
|
Intervention:
Auricular point acupressure instructions |
Method of data collection
Questionnaire Tools used for data collection BPI (last 7 day) I:
T1: Baseline T2: Immediately post intervention T3: 1 month after |
Mean (SD)
T1: 7.2 ± 1.8 T2: 4.7 ± 2.86 T3: 5.0 ± 2.67 |
-
aEU, Europe; N-A, Nord-America; O, Oceania; UT, uncontrolled trial; RCT, randomized controlled trial; bM, male; F, female; MSK, musculoskeletal; cHCP, health care provider; CBT, cognitive behavioral therapy; PPN, pain psychology and neuroscience; dWOMAC, Western Ontario and McMasters Universities Osteoarthritis Index; PROMIS-29, Patient-Reported Outcomes Measurement Information System−29; VAS, Visual Analogue Scale; BPI, Brief Pain Inventory; NRS, Numeric Rating Scale; LBPRS, Low Back Pain Rating Scale. eIQR, interquartile range (25th and 75th percentile); SD, standard deviation; *=p<0.05.
Experienced barriers and facilitators
Only two of the 10 studies specifically asked about barriers and facilitators for the use of an eHealth self-management intervention through an interview [33] and an online questionnaire [32].
In a mobile program for chronic MSK pain, patients reported that the program was too long, that is was unclear how they had to answer some of the questions, that the design of the program was confusing, that they got the idea of not getting new information by the program and that there was a lack of audio and video fragments [32]. However, they all liked the content and information and found the program easy to use [32]. After using the Auricular Point Acupressure Smartphone app, barriers were that the screen on their smartphone was too small to look at the videos (n=4), they had to watch the videos multiple times to know where the ear point locations are situated (n=5) and five persons reported to prefer a face-to-face training session [33]. They also reported that the eHealth intervention was user friendly and that it empowered them to come to self-management [33].
Discussion
No study was found that made a direct comparison between both populations when examining the design or effects of an eHealth self-management intervention. Concerning the effectiveness, only two studies in an MSK population, reported a significant difference between the control and intervention group [34, 36], with only one in favor of the self-management intervention [34]. Looking at the clinical trials that only reported on time effect, two breast cancer studies reported a significant decrease in pain intensity over time [30, 31], as well as one MSK study [32]. However, with no control group, these time-effects have little value in proving effectiveness. Additionally, these effects were not very long lasting. The other included studies reported no significant difference over time or between groups [28, 29, 33, 35, 37, 38].
The high risk of bias and several other factors of the included studied hinder firm conclusions on the effect of an eHealth self-management intervention on pain intensity within these populations.
First, different measurement methods of pain intensity were used. Because of the subjectivity and complexity of pain, it is important to select the most sensitive and accurate outcome measure [39]. The VAS is considered as the ‘gold standard’ for measuring pain intensity as it is universal in application, simple and quick to administer and easily understood by the patient [40].
Second, according to the biopsychosocial model, pain has many influencing factors which are unique to the individual [41]. Different pain mechanisms can be present and psychological and social factors vary in each person. Due to the individuality of pain, a more tailored approach to the individual might be more applicable and group research might not be able to represent the effect on the individual adequately.
Lastly, studies on acute and chronic pain management were included. Two studies used a pre-operative intervention for acute post-operative pain relief and showed inconclusive evidence. The study with a breast cancer population [30] found a beneficial time effect in the group with education on mind–body science but found no difference in comparison to the control group who received general health information, both delivered through eHealth. In contrast, the study in low back pain patients [36] who underwent spinal fusion surgery, reported a beneficial effect in favor of the usual treatment-control group over the group who also received an additional eHealth program. Although, this finding was only present in one outcome, namely immediate leg pain 2–3 days after surgery. The absence of pre-operative pain in breast cancer patients might offer an explanation. Providing education, regardless if it is specific on pain or more general, might decrease anxiety around surgery resulting in a lower pain intensity post-operatively. This finding might contribute to the trend of adding pre-operative education as part of post-operative pain management.
Only one study in a chronic pain population found a significant result between groups [34]. Most interventions for chronic pain management target reconceptualization of pain and behavioral changes [42, 43]. As this takes time, it might be that the follow-up length was too short to see a possible effect.
The focus of this review was the effect of the interventions on pain intensity, which is only one aspect within the complexity of pain. When considering other pain-related outcomes in the included studies, assessments included outcomes related to the impact of pain on a patients daily activities and functioning (e.g. pain interference, pain disability) and other outcomes related to pain experience (e.g. pain-related beliefs, pain catastrophizing and pain coping).
In the first category of outcomes related to the impact of pain on daily functioning, only one study, including a MSK population, reported a significant effect on pain interference [34] and two studies, also including a MSK population, reported a significant effect on pain disability [32, 37]. In contrast, some significant effects were found on pain-related beliefs [29, 31] and pain catastrophizing [29] in both populations. In the studies that include an MSK-populations, there were significant effects on additional pain-related outcomes such as pain coping [32], psychological/brain attributions and readiness for pain self-management [34].
Despite the positive effects in other pain-related outcomes, there was a consistent lack of transfer to pain intensity. Additionally, some studies reported an effect on outcomes related to pain experience, but not on the outcomes related to a patients daily activities and functioning. Future research is required to explore the interaction between these different outcomes and to determine how eHealth self-management interventions should be tailored to address this interaction. Lastly, it would be of interest to take other health-related outcome measures, like quality of life, into account when looking at the effect of an eHealth self-management intervention.
Barriers and facilitators
Very limited information was provided on barriers and facilitators for the use of an eHealth self-management intervention. Previous literature on barriers and facilitators of an eHealth intervention identified three themes: individual, environmental and organizational, and technical barriers [44]. To our knowledge, there yet exists no valid tool that inventories barriers and facilitators. Tools that are often used are user satisfaction questionnaires or interviews. Future research should focus on developing valid research methods to identify the experienced barriers and facilitators of an eHealth intervention.
Recommendations
The findings of this review indicate that design characteristics are similar in both populations. Despite the limited amount of included studies, a high risk of bias and a high amount of heterogeneity between the different eHealth self-management interventions, some cautious recommendations on design of eHealth self-management support programs can be made. In both populations, targeted education was used, be it on pain itself or more condition-specific education [30, 31, 34], [35], [36]. Targeted education appears to be more beneficial then only providing general information such as information on surgical treatment [36] or instructions on a technique [33]. Contemporary pain science education has already been proven to be a successful intervention in pain mediation in oncological and MSK pain populations. All studies reporting significant effects contained at least one aspect of CBT, suggesting that this might be an important modality [30], [31], [32, 34, 36]. At the same time, other studies who also implemented CBT as part of their intervention, found no significant results [29, 37, 38]. CBT comprehends multiple strategies with the aim of behavior change [42]. No clear similarities were seen in which elements were effective. We hypothesize that the combination of elements is likely more important than the isolated elements.
In line with the existing literature on positive effects of peer support to promote health behavior, the included studies who used a form of social support similarly showed beneficial effects [32, 36]. Previous literature shows that higher levels of pain have been associated with a decrease in social support [45]. Because of this vulnerability, social support should be facilitated and eHealth can provide an easier way to engage with other patients for example through online support groups. Although, this addition of social support into the intervention was only used within the MSK studies, previous research has shown that a low level of social support has a negative predictive effect on pain, inflammation and depression after breast cancer treatment [46]. Therefore, we recommend the use of social support in both populations.
Some studies made the comparison of an individual and an HCP-supported eHealth intervention, resulting in a better outcome on pain intensity for the HCP-supported group, albeit not significant [35, 37, 38]. Another benefit of HCP-support is a higher adherence to the intervention [47]. A barrier that was reported in one study, was the lack of in-person sessions, indicating that patients have a need for additional support of HCPs when using eHealth interventions.
Limitations and strengths
A first limitation is the large heterogeneity in how the outcome measure of interest, i.e. pain intensity, is assessed, making a meta-analysis impossible.
A second limitation concerns the high risk of bias of the included studies. To investigate the effectiveness of an intervention, RCTs have a higher level of evidence then uncontrolled trials. However, due to the limited available studies in the oncological population, we decided to also include uncontrolled trials. To depict the risk of bias in a uniform way, the same scoring tool was used for both study designs. However, this leads to a high risk of bias of the uncontrolled trials as this design contains only one group. Within the RCT studies, the lack of a well-designed control group is a first contributor to the high risk of bias. Second, a high amount of drop-out was found in the included studies and third, most studies did not use an appropriate analysis to correct for the bias due to missing outcome data. EHealth self-management interventions are often paired with a low adherence and a high drop-out [47]. Participants might not be motivated enough to follow the complete program due to the lack of feedback and personal interaction with an HCP [47]. Lastly, we also included pilot studies, the lack of an appropriate sample size leads to statistical underpowered studies. Because of the reasons mentioned above, the reported results should be interpreted with caution.
A strength of this systematic review is that we included both MSK-and cancer-related pain, resulting in a broad overview. Another important strength of this systematic review is that we only included studies where at least the intervention or control group existed of an individual eHealth intervention with no active interference of an HCP. This differs from the already existing reviews of Hernandez-Silva et al. (2018) and Thurnheer et al. (2019), both systematic reviews found beneficial effects of eHealth self-management interventions in pain management and Thurnheer et al. (2019) reported that eHealth interventions are well liked by both the patients and the health care providers [16]. These findings are in contrast with the low evidence retrieved in the present review and suggests the importance of the active role of HCPs in supporting self-management. Consequently, this systematic review provides an overview of the sole effect of an eHealth self-management intervention without the need for a health care provider on pain intensity.
Conclusions
The aim of this review was to look at the comparison of the effect of an eHealth self-management intervention on pain intensity in oncological vs. MSK populations. This review is innovative as it looks at self-management without the active involvement of HCPs. Overall, the available literature is limited and the included studies are too heterogenous to make a valid conclusion on the comparison of the two population groups. Regarding each separate population, the evidence is still preliminary, due to the lack of sound RCT’s. However, lessons can be learned from both populations. Education, aspects of cognitive behavioral therapy and social support seem universally applicable, regardless of population.
Further research should incorporate patient-experienced barriers and facilitators and there is a high need of studies making the direct comparison of the effect of an eHealth self-management intervention on pain intensity in an oncological vs. a MSK population.
-
Research funding: This work was supported by the University of Antwerp [grant number: 41776, 2020].
-
Author contributions: All authors have accepted responsibility for the entire content of this manuscript and approved its submission.
-
Competing interests: Authors state no competing of interest.
References
1. IASP n.d. Available from: https://www.iasp-pain.org/GlobalYear/CancerPain [Accessed 16 Mar 2021].Search in Google Scholar
2. El-Tallawy, SN, Nalamasu, R, Salem, GI, LeQuang, JAK, Pergolizzi, JV, Christo, PJ. Management of musculoskeletal pain: an update with emphasis on chronic musculoskeletal pain. Pain Ther 2021;10:181–209. https://doi.org/10.1007/s40122-021-00235-2.Search in Google Scholar PubMed PubMed Central
3. Kumar, SP. Cancer pain: a critical review of mechanism-based classification and physical therapy management in palliative care. Indian J Palliat Care 2011;17:116–26. https://doi.org/10.4103/0973-1075.84532.Search in Google Scholar PubMed PubMed Central
4. Jeong, H, Lee, Y. Sex-based differences in the quality of life of elderly koreans with chronic musculoskeletal pain. Int J Environ Res Publ Health 2020;17:743. https://doi.org/10.3390/ijerph17030743.Search in Google Scholar PubMed PubMed Central
5. Booth, J, Moseley, GL, Schiltenwolf, M, Cashin, A, Davies, M, Hübscher, M. Exercise for chronic musculoskeletal pain: a biopsychosocial approach. Muscoskel Care 2017;15:413–21. https://doi.org/10.1002/msc.1191.Search in Google Scholar PubMed
6. Hawker, GA. The assessment of musculoskeletal pain. Clin Exp Rheumatol 2017;35:S8–12.Search in Google Scholar
7. ICD-11 n.d. Available from: https://icd.who.int/en [Accessed 10 Jun 2021].Search in Google Scholar
8. Van Den Beuken-Van Everdingen, MHJ, Hochstenbach, LMJ, Joosten, EAJ, Tjan-Heijnen, VCG, Janssen, DJA. Update on prevalence of pain in patients with cancer: systematic review and meta-analysis. J Pain Symptom Manag 2016;51:1070–90.e9. https://doi.org/10.1016/j.jpainsymman.2015.12.340.Search in Google Scholar PubMed
9. Alshehri, MA, Alzaidi, J, Alasmari, S, Alfaqeh, A, Arif, M, Alotaiby, SF, et al.. The prevalence and factors associated with musculoskeletal pain among pilgrims during the hajj. J Pain Res 2021;14:369–80. https://doi.org/10.2147/JPR.S293338.Search in Google Scholar PubMed PubMed Central
10. Global regional, and national incidence, prevalence, and years lived with disability for 328 diseases and injuries for 195 countries, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet 2017;390:1211–59. https://doi.org/10.1016/S0140-6736(17)32154-2.Search in Google Scholar PubMed PubMed Central
11. Louw, A, Zimney, K, Puentedura, EJ, Diener, I. The efficacy of pain neuroscience education on musculoskeletal pain: a systematic review of the literature. Physiother Theory Pract 2016;32:332–55. https://doi.org/10.1080/09593985.2016.1194646.Search in Google Scholar PubMed
12. O’Connor, SR, Tully, MA, Ryan, B, Bleakley, CM, Baxter, GD, Bradley, JM, et al.. Walking exercise for chronic musculoskeletal pain: systematic review and meta-analysis. Arch Phys Med Rehabil 2015;96:724–34.E3. https://doi.org/10.1016/J.APMR.2014.12.003.Search in Google Scholar
13. De Groef, A, Penen, F, Dams, L, Van der Gucht, E, Nijs, J, Meeus, M. Best-evidence rehabilitation for chronic pain Part 2: pain during and after cancer treatment. J Clin Med 2019;8:979. https://doi.org/10.3390/jcm8070979.Search in Google Scholar PubMed PubMed Central
14. Robinson, JH, Callister, LC, Berry, JA, Dearing, KA. Patient-centered care and adherence: definitions and applications to improve outcomes. J Am Acad Nurse Pract 2008;20:600–7. https://doi.org/10.1111/j.1745-7599.2008.00360.x.Search in Google Scholar PubMed
15. Hargett, JL, Criswell, AC. Non-pharmacological interventions for acute pain management in patients with opioid abuse or opioid tolerance: a scoping review protocol. JBI Database System Rev Implement Rep 2019;17:1283–9. https://doi.org/10.11124/JBISRIR-2017-003878.Search in Google Scholar PubMed
16. Thurnheer, SE, Gravestock, I, Pichierri, G, Steurer, J, Burgstaller, JM. Benefits of mobile apps in pain management: systematic review. JMIR Mhealth Uhealth 2018;6:e11231. https://doi.org/10.2196/11231.Search in Google Scholar PubMed PubMed Central
17. Barlow, J, Wright, C, Sheasby, J, Turner, A, Hainsworth, J. Self-management approaches for people with chronic conditions: a review. Patient Educ Counsel 2002;48:177–87. https://doi.org/10.1016/S0738-3991(02)00032-0.Search in Google Scholar
18. Lorig, KR, Holman, HR. Self-management education: history, definition, outcomes, and mechanisms. Ann Behav Med 2003;26:1–7. https://doi.org/10.1207/S15324796ABM2601_01.Search in Google Scholar PubMed
19. Oh, H, Rizo, C, Enkin, M, Jadad, A, Powell, J, Pagliari, C. What is eHealth (3): a systematic review of published definitions. J Med Internet Res 2005;7:e1. https://doi.org/10.2196/jmir.7.1.e1.Search in Google Scholar PubMed PubMed Central
20. Peng, P, Choiniere, M, Dion, D, Intrater, H, LeFort, S, Lynch, M, et al.. Challenges in accessing multidisciplinary pain treatment facilities in Canada. Can J Anesth 2007;54:977–84. https://doi.org/10.1007/BF03016631.Search in Google Scholar PubMed
21. Björn, Pobiruchin, M, Strotbaum, V, Suleder, J, Wiesner, M, Bergh, B. Barriers and facilitators to the implementation of eHealth services: systematic literature analysis. J Med Internet Res 2019;21:e14197. https://doi.org/10.2196/14197.Search in Google Scholar PubMed PubMed Central
22. Nicholl, BI, Sandal, LF, Stochkendahl, MJ, McCallum, M, Suresh, N, Vasseljen, O, et al.. Digital Support interventions for the self-management of low back pain: a systematic review. J Med Internet Res 2017;19:e14197. https://doi.org/10.2196/JMIR.7290.Search in Google Scholar
23. Najm, A, Gossec, L, Weill, C, Benoist, D, Berenbaum, F, Nikiphorou, E. Mobile health apps for self-management of rheumatic and musculoskeletal diseases: systematic literature review. JMIR Mhealth Uhealth 2019;7:e14730. https://doi.org/10.2196/14730.Search in Google Scholar PubMed PubMed Central
24. Du, S, Liu, W, Cai, S, Hu, Y, Dong, J. The efficacy of e-health in the self-management of chronic low back pain: a meta analysis. Int J Nurs Stud 2020;106:103507. https://doi.org/10.1016/j.ijnurstu.2019.103507.Search in Google Scholar PubMed
25. Silva, EH, Lawler, S, Langbecker, D. The effectiveness of mHealth for self-management in improving pain, psychological distress, fatigue, and sleep in cancer survivors: a systematic review. J Cancer Survivorship 2019;13:97–107. https://doi.org/10.1007/s11764-018-0730-8.Search in Google Scholar PubMed
26. Page, MJ, McKenzie, JE, Bossuyt, PM, Boutron, I, Hoffmann, TC, Mulrow, CD, et al.. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Br Med J 2021;372:n71. https://doi.org/10.1136/bmj.n71.Search in Google Scholar PubMed PubMed Central
27. Covidence – better systematic review management software n.d. Available from: https://get.covidence.org [Accessed 18 Jun 2021].Search in Google Scholar
28. Allen, KD, Woolson, S, Hoenig, HM, Bongiorni, D, Byrd, J, Caves, K, et al.. Stepped exercise program for patients with knee osteoarthritis : a randomized controlled trial. Ann Intern Med 2021;174:298–307. https://doi.org/10.7326/M20-4447.Search in Google Scholar PubMed PubMed Central
29. Carpenter, KM, Stoner, SA, Mundt, JM, Stoelbc, B. An online self-help CBT intervention for chronic lower back pain. Clin J Pain 2012;28:14–22. https://doi.org/10.1097/AJP.0b013e31822363db.Search in Google Scholar PubMed PubMed Central
30. Darnall, BD, Ziadni, MS, Krishnamurthy, P, Flood, P, Heathcote, LC, MacKey, IG, et al.. “My surgical success”: effect of a digital behavioral pain medicine intervention on time to opioid cessation after breast cancer surgery - a pilot randomized controlled clinical trial. Pain Med 2019;20:2228–37. https://doi.org/10.1093/pm/pnz094.Search in Google Scholar PubMed PubMed Central
31. Henry, NL, Kidwell, KM, Alsamarraie, C, Bridges, CM, Kwiatkowski, C, Clauw, DJ, et al.. Pilot study of an internet-based self-management program for symptom control in patients with early-stage breast cancer. JCO Clin Cancer Inform 2018;2:1–12. https://doi.org/10.1200/cci.17.00106.Search in Google Scholar
32. Johnson, SS, Levesque, DA, Broderick, LE, Bailey, DG, Kerns, RD. Pain self-management for veterans: development and pilot test of a stage-based mobile-optimized intervention. JMIR Med Inform 2017;5:e40. https://doi.org/10.2196/medinform.7117.Search in Google Scholar PubMed PubMed Central
33. Kawi, J, Yeh, CH, Li, M, Caswell, BSK, Mazraani, MDM, Lukkahatai, PD, et al.. Auricular point acupressure smartphone application to manage chronic musculoskeletal pain: a longitudinal, one-group, open pilot trial. Glob Adv Health Med 2021;10: 216495612098753. https://doi.org/10.1177/2164956120987531.Search in Google Scholar PubMed PubMed Central
34. Kohns, DJ, Urbanik, CP, Geisser, ME, Schubiner, H, Lumley, MA. The effects of a pain psychology and neuroscience self-evaluation internet intervention: a randomized controlled trial. Clin J Pain 2020;36:683–92. https://doi.org/10.1097/AJP.0000000000000857.Search in Google Scholar PubMed
35. Malliaras, P, Cridland, K, Hopmans, R, Ashton, S, Littlewood, C, Page, R, et al.. Internet and telerehabilitation-delivered management of rotator cuff–Related shoulder pain (INTEL trial): randomized controlled pilot and feasibility trial. JMIR Mhealth Uhealth 2020;8:e24311. https://doi.org/10.2196/24311.Search in Google Scholar PubMed PubMed Central
36. Strøm, J, Nielsen, CV, Jørgensen, LB, Andersen, NT, Laursen, M. A web-based platform to accommodate symptoms of anxiety and depression by featuring social interaction and animated information in patients undergoing lumbar spine fusion: a randomized clinical trial. Spine J 2019;19:827–39. https://doi.org/10.1016/j.spinee.2018.11.011.Search in Google Scholar PubMed
37. Kristjánsdóttir, ÓB, Fors, EA, Eide, E, Finset, A, Stensrud, TL, van Dulmen, S, et al.. A smartphone-based intervention with diaries and therapist-feedback to reduce catastrophizing and increase functioning in women with chronic widespread pain: randomized controlled trial. J Med Internet Res 2013;15:e5. https://doi.org/10.2196/jmir.2249.Search in Google Scholar PubMed PubMed Central
38. Kristjánsdóttir, ÓB, Fors, EA, Eide, E, Finset, A, Stensrud, TL, Van Dulmen, S, et al.. A smartphone-based intervention with diaries and therapist feedback to reduce catastrophizing and increase functioning in women with chronic widespread pain. part 2: 11-month follow-up results of a randomized trial. J Med Internet Res 2013;15:e72. https://doi.org/10.2196/jmir.2442.Search in Google Scholar PubMed PubMed Central
39. Younger, J, McCue, R, Mackey, S. Pain outcomes: a brief review of instruments and techniques. Curr Pain Headache Rep 2009;13:39–43. https://doi.org/10.1007/s11916-009-0009-x.Search in Google Scholar PubMed PubMed Central
40. Yarnitsky, D, Sprecher, E, Zaslansky, R, Hemli, JA. Multiple session experimental pain measurement. Pain 1996;67:327–33. https://doi.org/10.1016/0304-3959(96)03110-7.Search in Google Scholar PubMed
41. Fillingim, RB. Individual differences in pain: understanding the mosaic that makes pain personal. Pain 2017;158:S11. https://doi.org/10.1097/J.PAIN.0000000000000775.Search in Google Scholar PubMed PubMed Central
42. Knoerl, R, Smith, EML, Weisberg, J. Chronic pain and cognitive behavioral therapy: an integrative review. West J Nurs Res 2016;38:596–628. https://doi.org/10.1177/0193945915615869.Search in Google Scholar PubMed
43. Louw, A, Diener, I, Butler, DS, Puentedura, EJ. The effect of neuroscience education on pain, disability, anxiety, and stress in chronic musculoskeletal pain. Arch Phys Med Rehabil 2011;92:2041–56. https://doi.org/10.1016/J.APMR.2011.07.198.Search in Google Scholar PubMed
44. Schreiweis, B, Pobiruchin, M, Strotbaum, V, Suleder, J, Wiesner, M, Bergh, B. Barriers and facilitators to the implementation of eHealth services: systematic literature analysis. J Med Internet Res 2019;21:e14197. https://doi.org/10.2196/14197.Search in Google Scholar PubMed PubMed Central
45. Zaza, C, Baine, N. Cancer pain and psychosocial factors: a critical review of the literature. J Pain Symptom Manag 2002;24:526–42. https://doi.org/10.1016/S0885-3924(02)00497-9.Search in Google Scholar PubMed
46. Hughes, S, Jaremka, LM, Alfano, CM, Glaser, R, Povoski, SP, Lipari, AM, et al.. Social support predicts inflammation, pain, and depressive symptoms: longitudinal relationships among breast cancer survivors. Psychoneuroendocrinology 2014;42:38–44. https://doi.org/10.1016/J.PSYNEUEN.2013.12.016.Search in Google Scholar
47. Schäfer, AGM, Zalpour, C, Von Piekartz, H, Hall, TM, Paelke, V. The efficacy of electronic health-supported home exercise interventions for patients with osteoarthritis of the knee: systematic review. J Med Internet Res 2018;20:e152. https://doi.org/10.2196/jmir.9465.Search in Google Scholar PubMed PubMed Central
© 2023 Walter de Gruyter GmbH, Berlin/Boston
Articles in the same Issue
- Frontmatter
- Systematic Review
- Comparison of the effectiveness of eHealth self-management interventions for pain between oncological and musculoskeletal populations: a systematic review with narrative synthesis
- Topical Review
- Shifting the perspective: how positive thinking can help diminish the negative effects of pain
- Clinical Pain Researches
- Pain acceptance and psychological inflexibility predict pain interference outcomes for persons with chronic pain receiving pain psychology
- A feasibility trial of online Acceptance and Commitment Therapy for women with provoked vestibulodynia
- Relations between PTSD symptom clusters and pain in three trauma-exposed samples with pain
- Short- and long-term test–retest reliability of the English version of the 7-item DN4 questionnaire – a screening tool for neuropathic pain
- Chronic post-thoracotomy pain after lung cancer surgery: a prospective study of preoperative risk factors
- Pain sensitivity after Roux-en-Y gastric bypass – associations with chronic abdominal pain and psychosocial aspects
- Barriers in chronic prostatitis/chronic pelvic pain syndrome (CP/CPPS) management: perspectives from health practitioners
- Observational studies
- Spontaneous self-affirmation: an adaptive coping strategy for people with chronic pain
- COVID-19 and processes of adjustment in people with persistent pain: the role of psychological flexibility
- Presence and grade of undertreatment of pain in children with cerebral palsy
- Sex-related differences in migraine clinical features by frequency of occurrence: a cross-sectional study
- Recurrent headache, stomachache, and backpain among adolescents: association with exposure to bullying and parents’ socioeconomic status
- Original Experimentals
- Temporal stability and responsiveness of a conditioned pain modulation test
- Anticipatory postural adjustments mediate the changes in fear-related behaviors in individuals with chronic low back pain
- The role of spontaneous vs. experimentally induced attentional strategies for the pain response to a single bout of exercise in healthy individuals
- Acute exercise of painful muscles does not reduce the hypoalgesic response in young healthy women – a randomized crossover study
- Short Communications
- Nation-wide decrease in the prevalence of pediatric chronic pain during the COVID-19 pandemic
- A multidisciplinary transitional pain service to improve pain outcomes following trauma surgery: a preliminary report
Articles in the same Issue
- Frontmatter
- Systematic Review
- Comparison of the effectiveness of eHealth self-management interventions for pain between oncological and musculoskeletal populations: a systematic review with narrative synthesis
- Topical Review
- Shifting the perspective: how positive thinking can help diminish the negative effects of pain
- Clinical Pain Researches
- Pain acceptance and psychological inflexibility predict pain interference outcomes for persons with chronic pain receiving pain psychology
- A feasibility trial of online Acceptance and Commitment Therapy for women with provoked vestibulodynia
- Relations between PTSD symptom clusters and pain in three trauma-exposed samples with pain
- Short- and long-term test–retest reliability of the English version of the 7-item DN4 questionnaire – a screening tool for neuropathic pain
- Chronic post-thoracotomy pain after lung cancer surgery: a prospective study of preoperative risk factors
- Pain sensitivity after Roux-en-Y gastric bypass – associations with chronic abdominal pain and psychosocial aspects
- Barriers in chronic prostatitis/chronic pelvic pain syndrome (CP/CPPS) management: perspectives from health practitioners
- Observational studies
- Spontaneous self-affirmation: an adaptive coping strategy for people with chronic pain
- COVID-19 and processes of adjustment in people with persistent pain: the role of psychological flexibility
- Presence and grade of undertreatment of pain in children with cerebral palsy
- Sex-related differences in migraine clinical features by frequency of occurrence: a cross-sectional study
- Recurrent headache, stomachache, and backpain among adolescents: association with exposure to bullying and parents’ socioeconomic status
- Original Experimentals
- Temporal stability and responsiveness of a conditioned pain modulation test
- Anticipatory postural adjustments mediate the changes in fear-related behaviors in individuals with chronic low back pain
- The role of spontaneous vs. experimentally induced attentional strategies for the pain response to a single bout of exercise in healthy individuals
- Acute exercise of painful muscles does not reduce the hypoalgesic response in young healthy women – a randomized crossover study
- Short Communications
- Nation-wide decrease in the prevalence of pediatric chronic pain during the COVID-19 pandemic
- A multidisciplinary transitional pain service to improve pain outcomes following trauma surgery: a preliminary report

