Abstract
Objectives
To evaluate the rate of subsequent spontaneous preterm birth in patients with previous induction of labour at term compared to women with previous spontaneous labour at term.
Methods
This was a retrospective cohort study of all women with consecutive births at the Royal Brisbane and Women’s Hospital between 2014 and 2018. All nulliparous women with a singleton pregnancy and induction of labour at term or in spontaneous labour at term in the index pregnancy were included. Data was extracted from electronic medical records. The outcome of spontaneous preterm birth in the subsequent pregnancy was compared between patients with previous term induction of labour and in previous term spontaneous labour.
Results
A total of 907 patients with consecutive births met the inclusion criteria; of which 269 (29.7%) had a term induction of labour and 638 (70.3%) had a term spontaneous labour in the index pregnancy. The overall subsequent spontaneous preterm birth rate was 2.3%. Nulliparous women who underwent term induction of labour were less likely to have a subsequent preterm birth compared to nulliparous women in term spontaneous labour (0.74 vs. 2.98%; odds ratio [OR], 0.25; 95% confidence interval, 0.06–1.07; p=0.0496) in the index pregnancy. This however was not significant once adjusted for confounders (adjusted OR, 0.29; p=0.10). Spontaneous preterm birth was associated with a previous spontaneous labour compared to induction of labour between 37 to 37+6 and 38 to 38+6 weeks (adjusted OR 0.18 and 0.21; p=0.02 and 0.004 respectively).
Conclusions
Term induction of labour does not increase the risk of subsequent spontaneous preterm birth compared to spontaneous labour at term in nulliparous women. Further research is needed to validate these findings in a larger cohort of women and to evaluate the effect of elective IOL among low-risk nulliparous women.
Introduction
Induction of labour (IOL) is defined as techniques used to stimulate uterine contractions to accomplish birth prior to the onset of spontaneous labour. IOL is a common obstetric intervention where approximately one in four women in high-income countries are induced at term [1]. Birth prior to the onset of spontaneous labour is often indicated when maternal or fetal risks associated with continuation of pregnancy are assessed to be greater than delivery. Examples of indications for IOL include post term pregnancy, premature rupture of membranes (PROM), hypertensive disorders of pregnancy (HDP) defined as gestational hypertension or preeclampsia, gestational diabetes mellitus (GDM), obstetric cholestasis, fetal growth restriction (FGR) and others. IOL is dictated by the cervical status commonly assessed by a Bishop score [2]. If the cervix is deemed unfavourable, specific agents are employed to assist with cervical ripening. These include mechanical agents such as insertion of balloon catheters and pharmacological agents such as vaginal prostaglandins [3], [4], [5].
As the rate of IOL continues to increase, it is important to assess the potential effects of this intervention on future pregnancies. In 2010, the rate of IOL in Australia was 25.2% (25.3% of singleton pregnancies and 18.9% of multiple pregnancies) [6]. Since then, this rate has increased to 32.5% in 2017 [6] (32.7% of singleton pregnancies and 21.0% of multiple pregnancies). Of note, the incidence of preterm births (PTB) in Australia has also increased during this period; from 8.3% in 2010 to 8.7% in 2018 [7]. Neonatal morbidity associated with PTB includes respiratory distress syndrome, necrotizing enterocolitis, retinopathy of prematurity, intraventricular haemorrhage and sepsis [8]; moreover, neonatal mortality is common, particularly in extreme prematurity [9].
There are a small number of studies investigating the relation between IOL and the risk of subsequent spontaneous preterm birth (sPTB). As IOL involves iatrogenic change to the cervix, concerns are raised about the effects on the cervix in the long term. Although the outcome of IOL is the same as in spontaneous labour, there is a lack of evidence on its effects on any future pregnancies and labour. Therefore, our study aims to evaluate the rate of subsequent sPTB in patients with a previous IOL at term compared to patients with a previous spontaneous labour at term in their index pregnancy with a distribution of patient groups that better represents the general population to minimise confounding factors.
Materials and methods
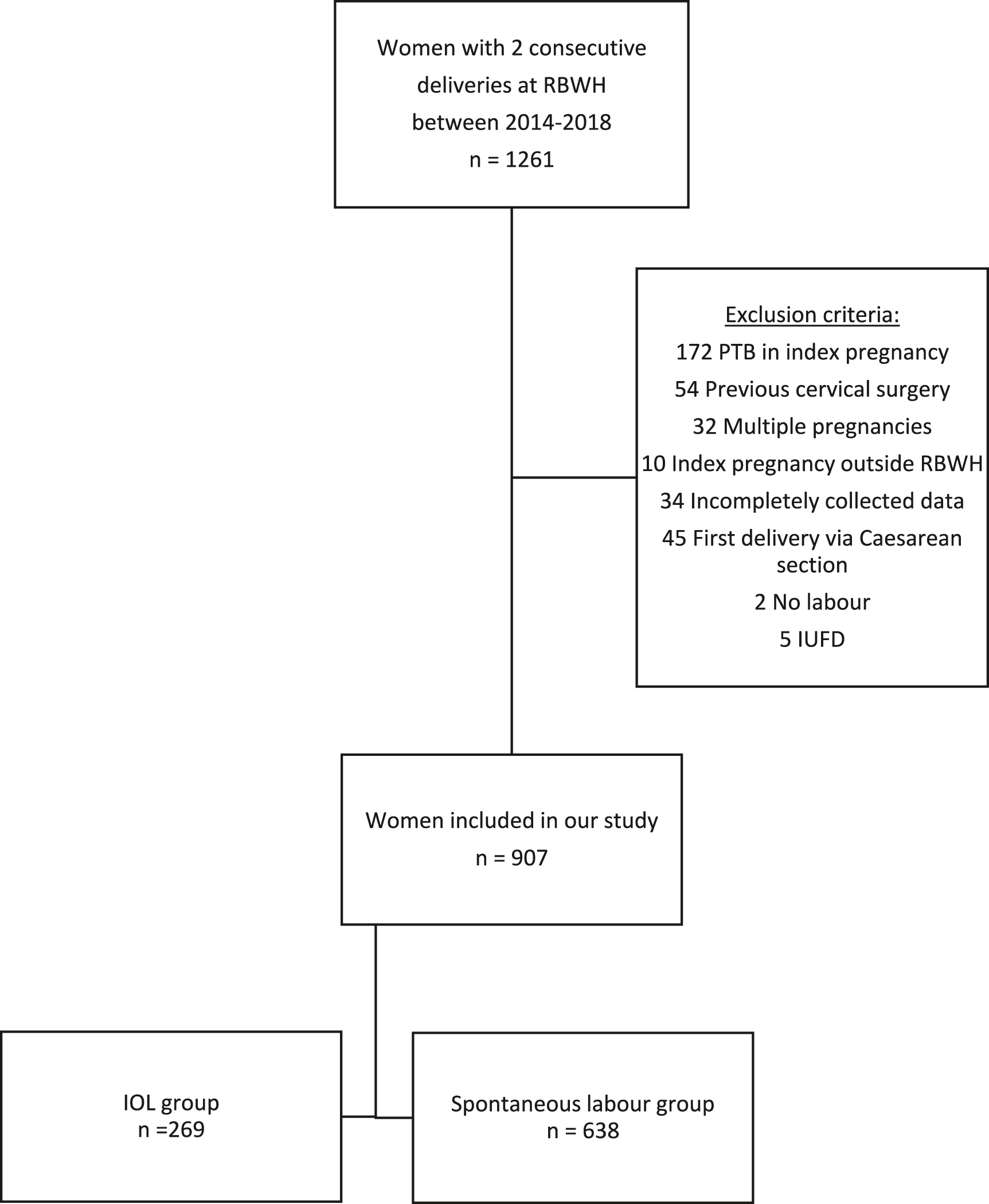
This was a retrospective cohort study of all women who gave birth at the Royal Brisbane and Women’s Hospital (RBWH) in their index and subsequent pregnancy between 01 January 2014 and 31 December 2018. The institution’s Human Research Ethics Committee granted approval for this study (Reference number: LNR/2020/QRBW/62589). Index pregnancy was defined as the woman’s first term pregnancy between early term (37+0 to 38+6 weeks) [10] to post term (after 42+0 weeks) in this time period. The next pregnancy after the index pregnancy during this time period was defined as the subsequent pregnancy. Women with a preterm birth (before 37 weeks of gestation) or caesarean section prior to the onset of labour in the index pregnancy, cervical incompetence secondary to previous cervical surgery, multiple gestations, intrauterine fetal demise and patients with incompletely collected data were excluded from the study.
Spontaneous labour was defined as regular painful contractions with cervical effacement and dilatation greater than or equal to 4 cm [11, 12]. IOL was defined as the use of a cervical ripening agents such as vaginal prostaglandin [Cervidil® (Ferring Pharmaceuticals Inc., Saint Prex, Switzerland) or Prostin® (Pfizer Inc., Manhattan, New York City, USA)] or balloon catheter [Cook® catheter (Cook Group Incorporated, Bloomington, Indiana, USA)], artificial rupture of membranes (ARM) or the use of oxytocin in the setting of cervical dilation less than or equal to 4 cm. Data was collected from electronic medical records. These included maternal demographics, obstetric and medical history, social history and gestational age at each consecutive birth. Induction parameters including indication for IOL, induction agents and the sequence and number of agents used were also collected. Mode of birth and neonatal outcomes including outcomes of birth, Apgar scores and birth weight were collected for both consecutive births.
Patients were stratified into two groups (IOL and spontaneous labour group) depending on the presentation in the index pregnancy. The primary aim of the study was to evaluate the risk of subsequent sPTB in nulliparous women undergoing IOL in their index pregnancies from 37+0 weeks compared to nulliparous women who presented in term spontaneous labour in their index pregnancies.
Statistical analysis
Data analysis involved analysis by Mann Whitney U Tests for nonparametric continuous variables and descriptive Chi-square tests and Fisher extract test for categorical variables. Data were reported as mean ± standard deviation or as the number of observations with the percentage of total. Logistic regression was be used to calculate odds ratios (OR) with 95% confidence intervals. Multivariate analysis was adjusted for confounders of BMI, gestational diabetes mellitus, hypertensive disorders in pregnancy and gestational age at index birth. All statistical analyses were performed using SPSS Statistics for Macintosh (IBM Corp, Armonk, NY).
Results
There was a total of 907 women with their first two consecutive pregnancies managed between 2014 and 2018. Of these, 269 (29.7%) women underwent IOL and 638 (70.3%) women presented in spontaneous labour in their index pregnancies (Figure 1). Demographic/obstetrics characteristics and birth outcomes are presented in Table 1. The mean maternal age was similar between both groups. The rate of GDM and HDP was significantly higher in the IOL group in the index pregnancy (p=0.0075 and p<0.0001 respectively). Substance use including cigarette smoking, alcohol and illicit drug use were similar in both groups. The rate of caesarean delivery in the index delivery was significantly higher among the IOL group as compared to the spontaneous labour (p<0.0001). Late and post term pregnancy (40 weeks or more) was more common in the IOL group compared to women who presented in spontaneous labour at term (p<0.0001). There was no significant difference in the inter-pregnancy interval between both groups.
Definitions of the study group.
Demographics and index pregnancy characteristics.
| IOL group (n=269) | Spontaneous labour group (n=638) | p-Value | |
|---|---|---|---|
| Maternal age, years | 30.00 ± 5.11 | 29.94 ± 4.94 | 0.472 |
| BMI, kg/m2 | 26.46 ± 6.96 | 23.90 ± 4.89 | 0.027 |
| Medical comorbidities EHTN GDM HDP |
1 (0.4%) 30 (11.2%) 42 (15.6%) |
2 (0.3%) 38 (6.0%) 19 (3.0%) |
0.8911 0.0075 <0.0001 |
| Ethnicity Caucasian Asian Others |
199 (74.0%) 23 (8.6%) 47 (17.4%) |
436 (68.3%) 77 (12.1%) 125 (19.6%) |
0.188 |
| Substance use Cigarettes Alcohol Illicit drugs |
9 (3.3%) 5 (1.9%) 1 (0.4%) |
23 (3.6%) 9 (1.4%) 0 (0%) |
0.847 0.617 0.123 |
| Mode of delivery at index birth Vaginal delivery Caesarean section |
203 (75%) 66 (25%) |
555 (87%) 83 (13%) |
<0.0001 |
| Apgar score | 8.91 ± 0.81 | 8.92 ± 0.78 | 0.573 |
| Birth weight, g | 3509.47 ± 488.5 | 3459.3 ± 506.0 | 0.755 |
| Gestational age at index birth (weeks) 37+0 to 37+6 38+0 to 38+6 39+0 to 39+6 40+ |
19 (7.1%) 36 (13.4%) 39 (14.5%) 175 (65.1%) |
28 (4.4%) 71 (11.1%) 174 (27.3%) 365 (57.2%) |
<0.0001 |
| Inter-pregnancy interval, months | 25.2 ± 8.5 | 25.4 ± 8.4 | 0.352 |
-
EHTN, essential hypertension; GDM, gestational diabetes mellitus; HDP, hypertensive disorders in pregnancy.
The overall PTB rate was 4.1% and the sPTB rate was 2.3%. The IOL group had a lower rate of sPTB in the subsequent pregnancy compared to the spontaneous labour group (0.74 vs. 2.98%, OR 0.25, 95% CI 0.06–1.07, p=0.0496) (Table 2). However once adjusted for confounders, this finding was not statistically significant (p=0.10).
Risk of preterm birth in the subsequent pregnancy among the two groups.
| IOL group (n=269) | Spontaneous labour group (n=638) | OR | 95% CI | p-Value | Adjusted OR | 95% CI | p-Value | |
|---|---|---|---|---|---|---|---|---|
| sPTB | 2 (0.74%) | 19 (2.98%) | 0.25 | 0.06–1.07 | 0.0496 | 0.29 | 0.07–1.27 | 0.10 |
| PTB total | 10 (3.72%) | 27 (4.2%) | 0.87 | 0.42–1.83 | 0.7207 | 1.04 | 0.48–2.27 | 0.92 |
-
sPTB, spontaneous preterm birth; PTB total, sPTB + iatrogenic PTB.
The baseline characteristics for the IOL group are detailed in Table 3. The IOL group was subdivided according to the methods of IOL and indications for induction. The majority of women (57.9%) underwent IOL using a single pharmacological agent (Prostin® or Cervidil®) compared to 5.0% of women with mechanical ripening of the cervix using a Cook® catheter. 1.5% of the women in the IOL group required a mix of both pharmacological and mechanical agents. A woman who underwent ARM only and a second woman who utilised syntocinon only in the induction for their index pregnancy were the only 2 cases of subsequent sPTB in the IOL group. ARM was associated with increased risk of subsequent sPTB (OR 31.38, CI 1.80–547.77, p=0.01). All the other methods of IOL including cervical ripening agents showed no statistical difference in the risk of subsequent sPTB.
Risk of subsequent sPTB based on various methods of induction of labour compared to women in spontaneous labour in the index pregnancy.
| sPTB n (%) |
OR | CI | p-Value | |
|---|---|---|---|---|
| Method of IOL (n=261) | ||||
| Cervical ripening agent Cook® catheter only (n=13) Pharmacological agents only (n=151) Mixed agents (n=4) ARM only (n=9) ARM & syntocinon (n=41) Syntocinon only (n=43) |
0 (0) 0 (0) 0 (0) 1 (11.1) 0 (0) 1 (11.1) |
3.65 0.14 11.36 31.38 1.05 5.17 |
0.17–79.89 0.01–3.01 0.47–272.04 1.80–547.77 0.05–22.34 0.32–84.24 |
0.41 0.21 0.13 0.01 0.97 0.25 |
| Indication for IOL | ||||
| PROM (n=30) Late & post term (n=104) Maternal (n=65) Fetal (n=55) Elective (n=7) |
1 (0.38) 1 (0.38) 0 (0) 0 (0) 0 (0) |
7.93 1.51 0.59 0.74 6.73 |
0.48–130.25 0.09–24.49 0.02–12.53 0.03–15.57 0.30–152.80 |
0.15 0.77 0.74 0.84 0.23 |
The IOL group were also subdivided according to indications which included late & post term (39.8%), maternal indications (24.9%), fetal indications (21.1%) and PROM (11.5%). Maternal indications included symphysis pubis dysfunction, HDP, obstetric cholestasis, GDM, antepartum haemorrhage, advanced maternal age, mental health and pre-existing medical conditions including cardiac conditions.
Gestational age of the index birth for both the IOL and spontaneous labour groups were also assessed for the risk of sPTB in the subsequent pregnancy (Table 4). Early term spontaneous births between 37+0 to 37+6 weeks and 38+0 to 38+6 weeks were associated with subsequent sPTB once adjusted for confounders (p=0.02 and p=0.004 respectively). There was no significant difference in the risk of subsequent sPTB among women who delivered between 39+0 to 39+6 weeks and after 40+0 weeks in the index pregnancy (p=0.79 and p=0.37 respectively).
Risk of subsequent sPTB risk among different gestational age in the index pregnancy.
| Gestation of index birth | IOL group | Spontaneous labour group | OR | 95% CI | p-Value | Adjusted OR | 95% CI | p-Value |
|---|---|---|---|---|---|---|---|---|
| 37+0 to 37+6 | 1 (5.6%) | 2 (7.4%) | 0.19 | 0.05–0.76 | 0.19 | 0.18 | 0.05–0.73 | 0.02 |
| 38+0 to 38+6 | 0 (0%) | 7 (9.9%) | 0.03 | 0.07–0.59 | 0.003 | 0.21 | 0.08–0.60 | 0.004 |
| 39+0 to 39+6 | 0 (0%) | 3 (1.8%) | 0.80 | 0.31–4.54 | 1.19 | 1.19 | 0.31–4.57 | 0.79 |
| ≥40+0 | 1 (0.6%) | 7 (1.9%) | 0.29 | 0.04–2.40 | 0.25 | 0.36 | 0.04–3.10 | 0.37 |
Discussion
We investigated the risk of subsequent sPTB among nulliparous women following term IOL and term spontaneous labour in a tertiary institution and found no significant difference following adjustment for confounders due to the small number of sPTB in both group (0.74 vs. 2.98%; adjusted OR, 0.29; p=0.10). In the only previous study evaluating the effect of IOL at term to the risk of sPTB in the subsequent pregnancy, Levine et al. reported that term inductions were less likely to have a subsequent sPTB compared with term spontaneous labour (6 vs. 11%; adjusted OR, 0.55; p=0.04) [13]. The risk of sPTB for both groups was much less in our study and this may be due to the following key differences between the studies. Firstly, our study was limited to nulliparous women whereas Levine et al. included multiparous women up to their fifth pregnancy. This poses as a confounder as increasing parity leads to an increased risk for spontaneous preterm birth [14]. Secondly, there were 2.3 times as many women in the spontaneous labour group compared to the IOL group in our study. In contrast, there were only 0.4 times as many women in the spontaneous group compared to the IOL group in the study by Levine et al. as a result of a calculated sample size with the intention to enable subdivision of patients into the IOL group [13]. Finally, Levine et al. did not disclose any exclusion of patients with risk factors for preterm birth including previous cervical surgery or multiple gestations.
We have found that both cervical ripening with a balloon catheter and pharmacological methods such as Prostin®, Cervidil® or both were not associated with an increased risk of sPTB in the subsequent pregnancy, and this is consistent with the findings in previous studies [15,16]. Our analysis has shown that amniotomy alone was associated with a significant increase in the risk of subsequent sPTB (11%, p= 0.01). This is not to suggest amniotomy increases the risk of sPTB, as the majority of women who were induced with pharmacological and mechanical methods would also have had an amniotomy performed once the cervix was favourable. However, this was not shown to be associated with an increased risk of subsequent sPTB. We hypothesise that the increased risk of subsequent sPTB was due to the fact that these women had a more favourable cervix at the time of amniotomy secondary to less structural integrity compared to other nulliparous IOL women. There was no significant increase in the risk of sPTB with the use of syntocinon alone. The various indications for IOL were not shown to be associated with any increase risk of subsequent sPTB following a previous IOL, and again this is consistent with the Levine et al. study [13]. However, size of subgroups for methods of IOL were small and the results should be treated with caution.
In regard to the subsequent sPTB risk among different gestational age categories, we found that early spontaneous delivery between 37+0 and 38+6 weeks gestation in the index pregnancy was associated with a significantly higher risk of subsequent sPTB compared to IOL (p=0.02 and p=0.004). This is consistent with a study reporting that women with a prior spontaneous early term birth were at an increased risk for subsequent preterm birth [17] and suggests that term IOL does not increase the risk of subsequent sPTB.
The majority of women underwent IOL in the index pregnancy when it was clinically indicated in our study, therefore if IOL in low-risk nulliparous women leads to an increase in the risk of subsequent sPTB remains unanswered. The ARRIVE trial showed that IOL at 39 weeks in low-risk nulliparous women resulted in a significantly lower frequency of caesarean delivery [18]. In addition, the randomised trial noted significantly lower rates in the IOL group of gestational hypertension and preeclampsia, as well as need for neonatal respiratory support within the first 72 h of life. While it is reasonable to offer elective IOL to low-risk nulliparous women at 39 weeks gestation based on the findings, further studies investigating the risk of subsequent sPTB following an elective IOL in low-risk nulliparous women are required.
Our study was retrospective in nature and it posed a limitation in assigning a test group and a control group. Women who present in spontaneous labour in the index pregnancy were grouped in the control group and women who underwent IOL in the index pregnancy including both elective and clinically indicated IOL were grouped in the test group. The clinically indicated IOL and spontaneous onset of labour are parameters that cannot be properly controlled for, and needs to be addressed in future studies by conducting a randomised prospective trial.
Another limitation of our study include its retrospective nature and the distribution of women between the spontaneous labour and IOL groups. There were twice as many women in the spontaneous labour group compared to the IOL group and this might have impacted the statistical analysis. Finally, women included in this study were a heterogenous group of both low-risk and high-risk pregnancies. This reflected the representation of the general population; however, this study was unable to account for potential confounders associated with high-risk pregnancies which would have required greater surveillance with a tendency for earlier intervention. Indications for IOL varied widely with a lack of standardised protocols which can confound our results but were difficult to exclude from the study.
In conclusion, our study suggested that IOL at term was not associated with subsequent sPTB. PTB is a global health concern with implications not only to the mothers and their babies but also significant economic implications to the healthcare system. As the rate of IOL increases for multiple reasons, it is vital to understand the risk of PTB in subsequent pregnancies associated with IOL in the index pregnancy. Future research should therefore target risk factors as well as explore potential protective factors for early birth in order to achieve a safe reduction of PTB.
-
Research funding: None declared.
-
Author contributions: All authors have accepted responsibility for the entire content of this manuscript and approved its submission.
-
Competing interests: Authors state no conflict of interest.
-
Informed consent: Informed consent was not obtained from all individuals included in this study. The institution’s Human Research Ethics Committee granted waiver of consent.
-
Ethical approval: The institution’s Human Research Ethics Committee granted approval for this study (Reference number: LNR/2020/QRBW/62589).
References
1. World Health Organisation. WHO recommendations for induction of labour. Geneva: Department of Reproductive Health and Research; 2011.Search in Google Scholar
2. Bishop, EH. Pelvic scoring for elective induction. Obstet & Gynecol 1964;24:266–8.Search in Google Scholar
3. Vaknin, Z, Kurzweil, Y, Sherman, D. Foley catheter balloon vs locally applied prostaglandins for cervical ripening and labor induction: a systematic review and metaanalysis. Am J Obstet Gynecol 2010;203:418–29.10.1016/j.ajog.2010.04.038Search in Google Scholar
4. Chen, W, Xue, J, Peprah, MK, Wen, SW, Walker, M, Gao, Y, et al.. A systematic review and network meta-analysis comparing the use of Foley catheters, misoprostol, and dinoprostone for cervical ripening in the induction of labour. BJOG 2016;123:346–54.10.1111/1471-0528.13456Search in Google Scholar
5. de Vaan, MD, Ten Eikelder, ML, Jozwiak, M, Palmer, KR, Davies-Tuck, M, Bloemenkamp, KW, et al.. Mechanical methods for induction of labour. Cochrane Database Syst Rev 2019;10. CD001233.10.1002/14651858.CD001233.pub3Search in Google Scholar
6. AIHW. Women who gave birth, by onset of labour, 2010 to 2017 (Per cent); 2019. [cited 21st February 2020]. Available from: https://www.aihw.gov.au/reports/mothers-babies/australias-mothers-babies-2017-data-visualisations/contents/labour-and-birth/onset-of-labour.Search in Google Scholar
7. AIHW. Babies, by gestation age (pre-term), 2010 to 2018 (Per cent); 2020. [cited 12 January 2021]. Available from: https://www.aihw.gov.au/reports/mothers-babies/australias-mothers-babies-2017-data-visualisations/contents/baby-outcomes/gestational-age.Search in Google Scholar
8. Khoshnood, SM, Karimi, Z, Rezaienejad, M, Basiri, A, Torkestani, F, Gargari, SS. Perinatal complications associated with preterm deliveries at 24 to 33 weeks and 6 days gestation (2011–2012): a hospital-based retrospective study. Iran J Reproductive Med 2015;13:697–702.Search in Google Scholar
9. Glass, HC, Costarino, AT, Stayer, SA, Brett, CM, Cladis, F, Davis, PJ. Outcomes for extremely premature infants. Anesth Analg 2015;120:1337–51.10.1213/ANE.0000000000000705Search in Google Scholar
10. Spong, CY. Defining “term’ pregnancy: recommendations from the defining “term” pregnancy workgroup. JAMA 2013;309:2445–6.10.1001/jama.2013.6235Search in Google Scholar
11. National Institute for Health and Care Excellence (NICE). Intrapartum care for healthy women and babies. Clinical guideline 190. [Internet]; 2017. [cited 12 January 2021]. Available from: https://www.nice.org.uk.Search in Google Scholar
12. Friedman, E. The graphic analysis of labor. Am J Obstet Gynecol 1954;68:1568–75.10.1016/0002-9378(54)90311-7Search in Google Scholar
13. Levine, LD, Bogner, HR, Hirshberg, A, Elovitz, MA, Sammel, MD, Srinivas, SK. Term induction of labor and subsequent preterm delivery. Am J Obstet Gynecol 2014;210:354.10.1016/j.ajog.2013.10.877Search in Google Scholar PubMed PubMed Central
14. Koullali, B, van Zijil, MD, Kazemier, BM, Oudijk, MA, Mol, BWJ, Pajkrt, E, et al.. The association between parity and spontaneous preterm birth: a population based study. BMC Pregnancy Childbirth 2020;20:233.10.1186/s12884-020-02940-wSearch in Google Scholar PubMed PubMed Central
15. Zafran, N, Garmi, G, Zuarez-Easton, Nachum, Z, Salim, R. Cervical ripening with the balloon catheter and the risk of subsequent preterm delivery. J Perinatol 2015;35:799–802.10.1038/jp.2015.69Search in Google Scholar PubMed
16. Sciscione, A, Larkin, M, O’Shea, A, Pollock, M, Hoffman, M, Colmorgen, G. Preinduction cervical ripening with the Foley catheter and the risk of subsequent preterm birth. Am J Obstet Gynecol 2004;190:751–4.10.1016/j.ajog.2003.10.696Search in Google Scholar PubMed
17. Yang, J, Baer, RJ, Berghella, V, Chambers, C, Chung, P, Coker, T, et al.. Recurrence of preterm birth and early term birth. Obstet Gynecol 2016;128:364–72.10.1097/AOG.0000000000001506Search in Google Scholar PubMed PubMed Central
18. Grobman, WA, Rice, MM, Reddy, UM, Tita, ATN, Silver, RM, Mallett, G, et al.. Labor induction versus expectant management in low-risk nulliparous women. N Engl J Med 2018;379:513–23.10.1056/NEJMoa1800566Search in Google Scholar PubMed PubMed Central
© 2022 Nicole Ho et al., published by De Gruyter, Berlin/Boston
This work is licensed under the Creative Commons Attribution 4.0 International License.
Articles in the same Issue
- Frontmatter
- Review
- Neonatal and child mortality – are they different in developing and developed countries?
- WAPM Guideline
- First trimester examination of fetal anatomy: clinical practice guideline by the World Association of Perinatal Medicine (WAPM) and the Perinatal Medicine Foundation (PMF)
- Original Articles – Obstetrics
- Symptoms of maternal psychological distress during pregnancy: sex-specific effects for neonatal morbidity
- Efficacy of the lactate dehydrogenase (LDH)/lymphocyte ratio (LLR) to reduce the need for X-ray in pregnant patients with COVID-19
- Attitude of pregnant and lactating women toward COVID-19 vaccination in Jordan: a cross-sectional study
- Association between maternal thyroid function and risk of gestational hypertension and preeclampsia
- Evaluation of umbilical cord immune cells in pregnancies with autoimmune disorders and/or methylenetetrahydrofolate reductase polymorphisms
- The association between induction of labour in nulliparous women at term and subsequent spontaneous preterm birth: a retrospective cohort study
- Transvaginally surgically treatment of early postpartum hemorrhage caused by lower uterine segment atony
- Value of soluble fms-like tyrosine kinase-1/placental growth factor test in third trimester of pregnancy for predicting preeclampsia in asymptomatic women
- Fetal growth regulation via insulin-like growth factor axis in normal and diabetic pregnancy
- Intrapartum cardiotocography in pregnancies with and without fetal CHD
- Racial and ethnic representation in 17-hydroxyprogesterone caproate preterm birth prevention studies: a systematic review
- Original Articles – Fetus
- Improved method for revising the Israel birthweight references
- A single center experience in 90 cases with nonimmune hydrops fetalis: diagnostic categories ‒ mostly aneuploidy and still often idiopathic
- Original Articles – Neonates
- Diagnosis of congenital infections in premature, low-birthweight newborns with intrauterine growth restriction caused by cytomegalovirus (CMV), herpes simplex virus (HSV), Parvo-B 19, and Zika virus: a systematic review
- The impact of COVID-19 on smoking cessation in pregnancy
- Letter to the Editor
- Early placenta previa percreta and treatment with supracervical abortion hysterectomy
Articles in the same Issue
- Frontmatter
- Review
- Neonatal and child mortality – are they different in developing and developed countries?
- WAPM Guideline
- First trimester examination of fetal anatomy: clinical practice guideline by the World Association of Perinatal Medicine (WAPM) and the Perinatal Medicine Foundation (PMF)
- Original Articles – Obstetrics
- Symptoms of maternal psychological distress during pregnancy: sex-specific effects for neonatal morbidity
- Efficacy of the lactate dehydrogenase (LDH)/lymphocyte ratio (LLR) to reduce the need for X-ray in pregnant patients with COVID-19
- Attitude of pregnant and lactating women toward COVID-19 vaccination in Jordan: a cross-sectional study
- Association between maternal thyroid function and risk of gestational hypertension and preeclampsia
- Evaluation of umbilical cord immune cells in pregnancies with autoimmune disorders and/or methylenetetrahydrofolate reductase polymorphisms
- The association between induction of labour in nulliparous women at term and subsequent spontaneous preterm birth: a retrospective cohort study
- Transvaginally surgically treatment of early postpartum hemorrhage caused by lower uterine segment atony
- Value of soluble fms-like tyrosine kinase-1/placental growth factor test in third trimester of pregnancy for predicting preeclampsia in asymptomatic women
- Fetal growth regulation via insulin-like growth factor axis in normal and diabetic pregnancy
- Intrapartum cardiotocography in pregnancies with and without fetal CHD
- Racial and ethnic representation in 17-hydroxyprogesterone caproate preterm birth prevention studies: a systematic review
- Original Articles – Fetus
- Improved method for revising the Israel birthweight references
- A single center experience in 90 cases with nonimmune hydrops fetalis: diagnostic categories ‒ mostly aneuploidy and still often idiopathic
- Original Articles – Neonates
- Diagnosis of congenital infections in premature, low-birthweight newborns with intrauterine growth restriction caused by cytomegalovirus (CMV), herpes simplex virus (HSV), Parvo-B 19, and Zika virus: a systematic review
- The impact of COVID-19 on smoking cessation in pregnancy
- Letter to the Editor
- Early placenta previa percreta and treatment with supracervical abortion hysterectomy

