Abstract
Purpose
This study evaluates the clinical usefulness of patient-rated and objective measures to identify physically-oriented functional changes after an intensive chronic pain program in a pediatric setting. Past studies have demonstrated the importance of adolescents’ perception of their abilities and measurement tools used for rehabilitation outcomes within physical and occupational therapy; however, these tools used are not often easily utilized or have not been examined with a pediatric chronic pain population. In chronic pain rehabilitation, it is important to have a primary focus on functional improvement not on pain reduction as a leading outcome. This study examines how both self-report and objective physical activity measures can be meaningful constructs and can be used as reliable outcome measures. It was hypothesized that adolescents completing an interdisciplinary pain rehabilitation program would report functional gains from admission to discharge, and that perceived gains in physical ability would be associated with objective physical activities. Further, it was hypothesized that gains in functioning would be associated with mild pain reduction.
Methods
Data from 78 children and adolescents with chronic pain that participated in an intensive multidisciplinary treatment program completed self-report measures including the Lower Extremity Functional Scale (LEFS), Upper Extremity Functional Index (UEFI). In addition, adolescents were objectively monitored for repetitions of selected physical activities for 1 min intervals.
Results
Data demonstrated significant gains in all measures of functioning during the program. Correlations between self-report and objective outcomes suggest they are measuring similar yet distinct factors.
Conclusions
The LEFS, UEFI, and objective exercises provide a meaningful way to track progress in pediatric chronic pain rehabilitation. Despite similarities, they appear to track separate but related aspects of rehabilitation and capture important short-term response to rehabilitation. Both measures appear distinct from pain as an outcome. These findings increase our understanding of rehabilitation practices provide opportunities to promote clinical improvement in pediatric pain.
Implications
The use of self-report measures along with objective measures can help therapists gain understanding in regards to a patient’s insight and how that may impact their overall outcome compared to the use of a single outcome measure. Viewing these rated measures at any point in the rehabilitation process can be useful to facilitate discussion about challenges they can identify and how therapies can facilitate improvement and functional gains.
1 Introduction
1.1 Background
Pediatric chronic pain is on the rise, affecting up to 40% of adolescents, causing significant functional impairments (5–10%) [1, 2, 3, 4]. Adolescents with chronic pain often struggle with every day activities, family interactions, participation in sports or leisure activities, and consistent school attendance. As a result, many begin to experience worsened self-perceived health status [5, 6], including their perception and ability to complete physical tasks.
An interdisciplinary rehabilitation approach is a useful model of care for adolescents severely affected by chronic pain and functional disability [5, 7, 8, 9, 10]. Given the nature of chronic pain, dramatic reduction in pain is not anticipated or targeted as an early outcome to intervention. Rather, treatment aims to increase independent symptom management and improved daily functioning [2, 11]. Research supports education and participation in physical activity/exercise can reduce pain and limit disability [12]; therefore daily physical, occupational, and recreational therapies are a necessary part of rehabilitation. Therapy goals for adolescents with chronic pain are to improve independent, consistent daily physical functioning, and to reduce sedentary habits and activity avoidance.
Due to a global sense of impairment and lack of insight, many adolescents who experience chronic pain often perceive that they are limited in daily functional tasks and basic physical activity [7, 13]. For this reason, gains in therapy physical functioning should be measured with both self-report and objective measures. Selfreport tools help track perceived functional gains and demonstrate the psychological aspects of independent functioning. Objective measures can enhance assessment of functional gains by isolating the psychological aspects of perceived confidence.
There is limited research supporting specific outcome measures for adolescents with chronic pain in rehabilitation, specifically targeting physical or occupational therapy interventions. Commonly used therapeutic objective measures and assessments include the BOT [14], GMFM [15], and TUG [16]. Although helpful, these standardized tests can be time consuming, require additional resources, and be limited by areas of functioning or age ranges. Other standardized physical measures exist for high level athletes (PACER test, shuttle run, etc. [17]), but are less ideal in deconditioned adolescents. Few easily administered and appropriate objective measures exist for evaluating and tracking physical function for adolescents with chronic pain.
There exists a need for easily administered self-report and objective measures to examine adolescent functioning and change in functioning following chronic pain rehabilitation. Past research suggests the utility of self-report measures, but the utility of objective measures and their relation to self-report measures remain unknown.
1.2 Hypothesis
This study examines the use of two self-report measures and 5 objective fitness exercises to track physically oriented functional gains within a pediatric chronic pain rehabilitation program. Hypotheses include:
Adolescents completing a multidisciplinary pain rehabilitation program, which targets physical functioning, will report perceived functional gains from admission to discharge.
Adolescents will similarly demonstrate improvements in objective measures as they do in their rating of perceived functional gains.
Self-report and objective measures will correlate at both admission and discharge.
While we do not expect a large decrease in pain during rehabilitation, we anticipate that adolescents who report or demonstrate gains in physical ability will also demonstrate a mild reduction in reported pain intensity.
2 Methods
2.1 Participants
116 Children and adolescents (hereafter referred to as adolescents) ranging in age from 8–19 years old, with varying chronic pain diagnoses, were treated in this chronic pain rehabilitation program. Data for this study was collected retrospectively on all program participants. The most common diagnoses include headaches and migraines, back pain, abdominal pain, amplified musculoskeletal pain syndrome (AMPS) and complex regional pain syndrome (CRPS) (Fig. 1). Adolescents were excluded from data analysis if they: opted out of specific treatment, left the program early, withdrew consent, incomplete data forms, or participation in the program was extended past the typical 3–4 weeks (38 adolescents). Data of both self-report and objective measures for 78 adolescents was reported.
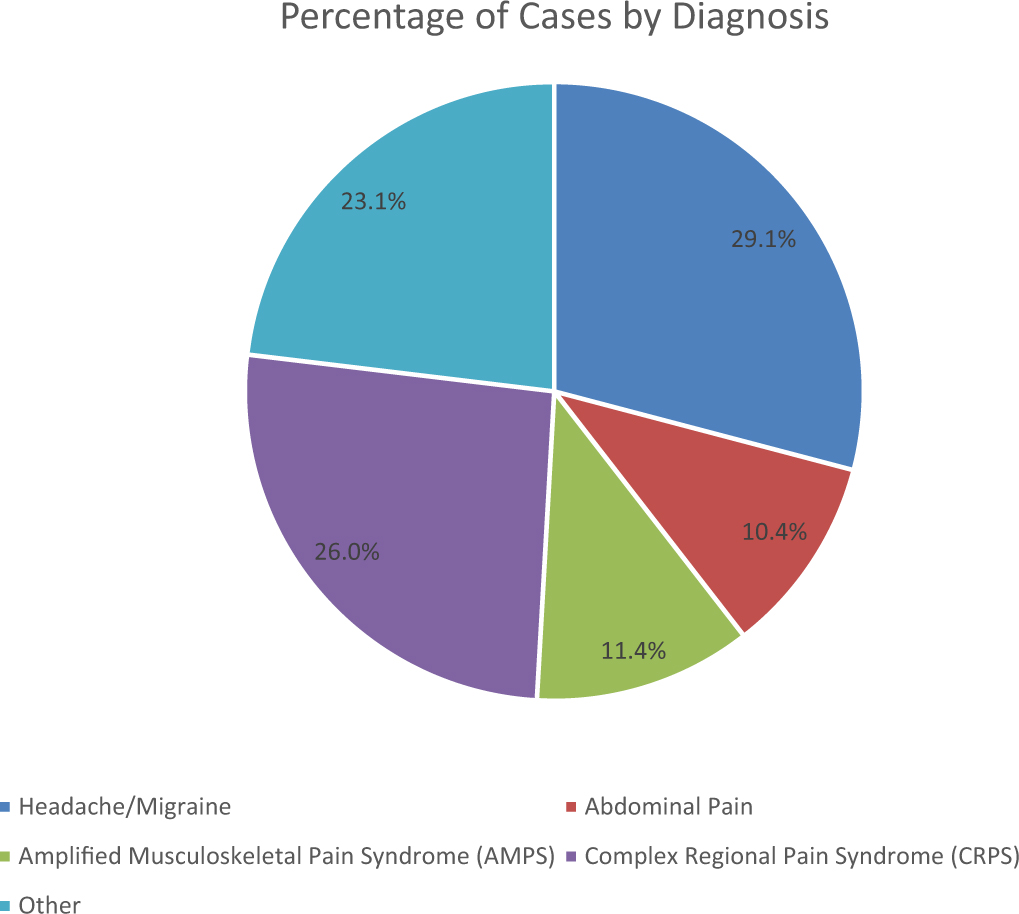
Percentage of cases by diagnosis.
2.2 Program/procedure
Chronic pain rehabilitation on a multidisciplinary level focuses on improved strength and endurance, facilitating return to daily life activities, and using appropriate self-directed coping and pain management skills [5, 6, 7]. Participants were typically seen for three weeks including both inpatient and day hospital care for full days. Within the program, adolescents participated in rehabilitation therapies, psychological services, medical subspecialty care, alternative therapies, and school services. Since an adolescent is part of a family unit, parents were also involved in education and observations with providers to help them support continued progress once home [6].
The goal of chronic pain rehabilitation has evolved from eliminating pain to managing pain so that overall functioning is improved. Progress is measured in part by physical functioning despite continuation of pain and symptoms [7].
2.3 Physical and occupational therapy treatment
Physical and occupational therapies were completed in both group and individual sessions for 3–4 h daily in land and pool settings. In therapy sessions, adolescents worked on isolated strengthening of appropriate musculature, endurance, proprioceptive and sensory training techniques, and other exercises or skills to help each adolescent return to highest level of function necessary. All adolescents spent time working on individual goal-oriented activities and independence with strengthening and endurance tasks while focusing on improved body mechanics and posture during exercises [6]. Limited time was spent on passive therapeutic interventions (e.g., massage, micro current, TENS), as the goal of therapies is to promote independence [18]. Parents were included for weekly education on therapeutic activities, barriers to improved function, appropriate modifications and accommodations, and expectations for going home [6]. At times, this included parents being more hands-on, working on behavioral planning, and observing an increased number of sessions. At a clinical level, improvements were measured by meeting specific therapy goals relating to improvements with presenting impairments, functional limitations or restrictions [19] (e.g., walking 100 yards without a walker/cane or tolerating a daily stretching and exercise regimen without pain complaints).
2.4 Measures
The reported data was collected upon the day of admission and at the day of discharge and retrospectively reviewed. Data collection through REDCap has been approved by the Institutional Review Board and is on the clinical database registry [20].
2.5 Lower Extremity Functioning Scale (LEFS) and Upper Extremity Functioning Index (UEFI)
Self-report tools have been useful to track perceived functional gains and demonstrate the psychological aspects of independent functioning. The Lower Extremity Functional Scale (LEFS) [21] and the Upper Extremity Functional Index (UEFI) [22] are self-report measures that were developed because of the need for a simple outcome tool that could be used to track an individual’s function level throughout the course of rehabilitation. Additional benefits to these measures that may not be realistic for other functional outcome measures include ease of administration, application to any musculoskeletal disorder, and generalizability to settings outside of the clinic or hospital. Both measures can be easily incorporated into individual or group treatment sessions, and are completed by the adolescent with guidance from a physical or occupational therapist [6]. Past research using these measures has demonstrated their utility as an outcome measure in pediatric pain rehabilitation [6].
The LEFS and UEFI are 20-item self-report measure about one’s perceived ability to perform everyday tasks with lower extremities and upper extremities, respectively. Individuals rated each item on a 0–4 likert scale (0 = extreme difficulty or cannot perform and 4 = no difficulty). Scores were summed for a possible score of 0–80. The LEFS has demonstrated good internal consistency (Cronbach’s alpha = .96) as well as test-retest reliability (r = .86). The UEFI has demonstrated good internal consistency (Cronbach’s alpha = .94) as well as test-retest reliability (r = .95). Both scales are also sensitive to change in functioning—a minimum detectable change score of 9 points is considered clinically important [6, 19, 23].
2.6 Objective measures
Simplistic objective measures, such as activities used in nationally recognized fitness tests for school aged children (i.e., fitness gram test [24]), may effectively provide information on improvements in function. Therapists in this program have used consistent objective measures of function as part of clinical care. Some measures are used with typical developing peers within the school setting [18, 23, 25, 26, 27, 28].
The objective measures used in programming for data collection included: push-ups, crunches, prone extension, step ups, and jump rope (number of repetitions during 60 s). The therapist kept track of time and provided prompting to improve alignment and body mechanics while the patient self-counted repetitions and logged them, as would be done in a school setting [24]. The ability for participants to self-count and track information is important as taking a more independent role in their progress can help promote long term gains [29]. Adolescents completed these activities in group setting and tracked these measures weekly throughout the program allowing for visualization of progress. The amount of repetitions for each exercise was recoded into an ordinal variable: zero, 1–5,6–10,11–20,21–30,31–40,41 + reps. Admission and discharge data were recorded for this study.
2.7 Pain
A single-item measure evaluated pain severity rating in last 24 h using a numerical rating scale (NRS) from 0 (no pain) to 10 (worst pain) [19].
2.8 Analysis plan
This data was captured in a REDCap database [20], then converted to an SPSS 22.0 dataset for analyses. Paired t-tests evaluated change in self-report measures (LEFS, UEFI and pain) over time. Wilcoxon signed ranks tests evaluated change in objective performance on standard measures over time. Spearman correlation coefficients were calculated to evaluate the relationship between self-report ratings of functioning and objective performance measures at admission and discharge. In order to demonstrate the association between change in physical functioning and change in self-reported pain, a series of regression analyses were performed. First, baseline measures of LEFS, UEFI, objective measures and pain were entered to predict these same measures at discharge. Standardized residuals were retained to represent change scores. Next, residualized changes scores for LEFS, UEFI, and objective measures were entered to predict residualized change in pain in seven separate models.
3 Results
3.1 Participants
Out of the 116 adolescents enrolled in the study, 78 met inclusion criteria. There was no significant difference between patients included versus excluded in analysis on any demographic, diagnosis, or other major study variable. The average age was 15.1 years (SD = 1.83) and the majority (77%) were female, consistent with other research on this population. Adolescents had various diagnoses including headaches and migraines (29.1%), abdominal pain (10.4%), AMPS (11.4%) and CPRS (26%) as seen in Fig. 1. Other diagnoses included back pain, fibromyalgia, reflex neurovascular dystrophy, postural orthostatic tachycardia syndrome, foot pain, and Ehlers–Danlos syndrome. Most participants also presented with at least one other secondary pain diagnoses. The chronicity of pain was recorded as less than 6 months (13.5%), 6–12 months (18.8%), 12–18 months (10.4%), 18–24 months (13.5%), and almost half (43.8%) of the participants experienced chronic pain for more than 24 months.
3.2 Self-report data
Self-report data is presented in Table 1. Participants reported a statistically significant increase in lower extremity functioning (t = −9.080, p − 0.001) throughout rehabilitation. They also reported statistically significant increase in upper extremity functioning (t = −8.439, p < 0.001). Using criteria reported by scale developers, clinically significant increase in lower and upper extremities were identified in 70.5% and 55.1% of participants, respectively. Participants also reported a mild reduction in pain from 6.7 to 5.5 during rehabilitation (t = 2.879, p = 0.006). Secondary analysis evaluated whether functional improvements differed across clinical diagnosis; there were no significant differences in self-reports between diagnosis groups.
Group differences at baseline and discharge.
| Admission | Discharge | % Clinical change | Change statistic | p-Value | |
|---|---|---|---|---|---|
| LEFS | 43.1 (15.46) | 59.2(14.41) | 70.5% | −9.080[a] | <0.001 |
| UEFI | 56.2(14.57) | 68.1 (10.73) | 55.1% | −8.439[a] | <0.001 |
| Push ups[b] | −6.576[b] | <0.001 | |||
| Crunches[b] | −5.842[b] | <0.001 | |||
| Prone extensions[b] | −5.622[b] | <0.001 | |||
| Step ups[b] | −6.786[b] | <0.001 | |||
| Jump rope[b] | −2.640[b] | 0.008 | |||
| Pain | 7.2(2.15) | 6.9 (2.29) | 1.051[a] | 0.296 | |
| Pain 24 | 6.7 (2.09) | 5.5 (3.41) | 2.879[a] | 0.006 |
3.3 Objective data
Using objective measures of functioning revealed similar results. In Fig. 2 repetitions of standard exercises from admission and discharge data was reported. The median scores at admission were, respectively: push-ups (11–20), crunches (21–30), prone extensions (31–40), step ups (21–30), and jump rope (41+). The median scores at discharge were, respectively: push-ups (31–40), crunches (41+) prone extensions (41+), step ups (31–40), and jump rope (41+). All scores were significantly improved across the three weeks of rehabilitation (Table 1). Wilcoxon signed ranks tests demonstrated significant change in all measures (p <0.001, with the exception of prone extensions with p = 0.008).
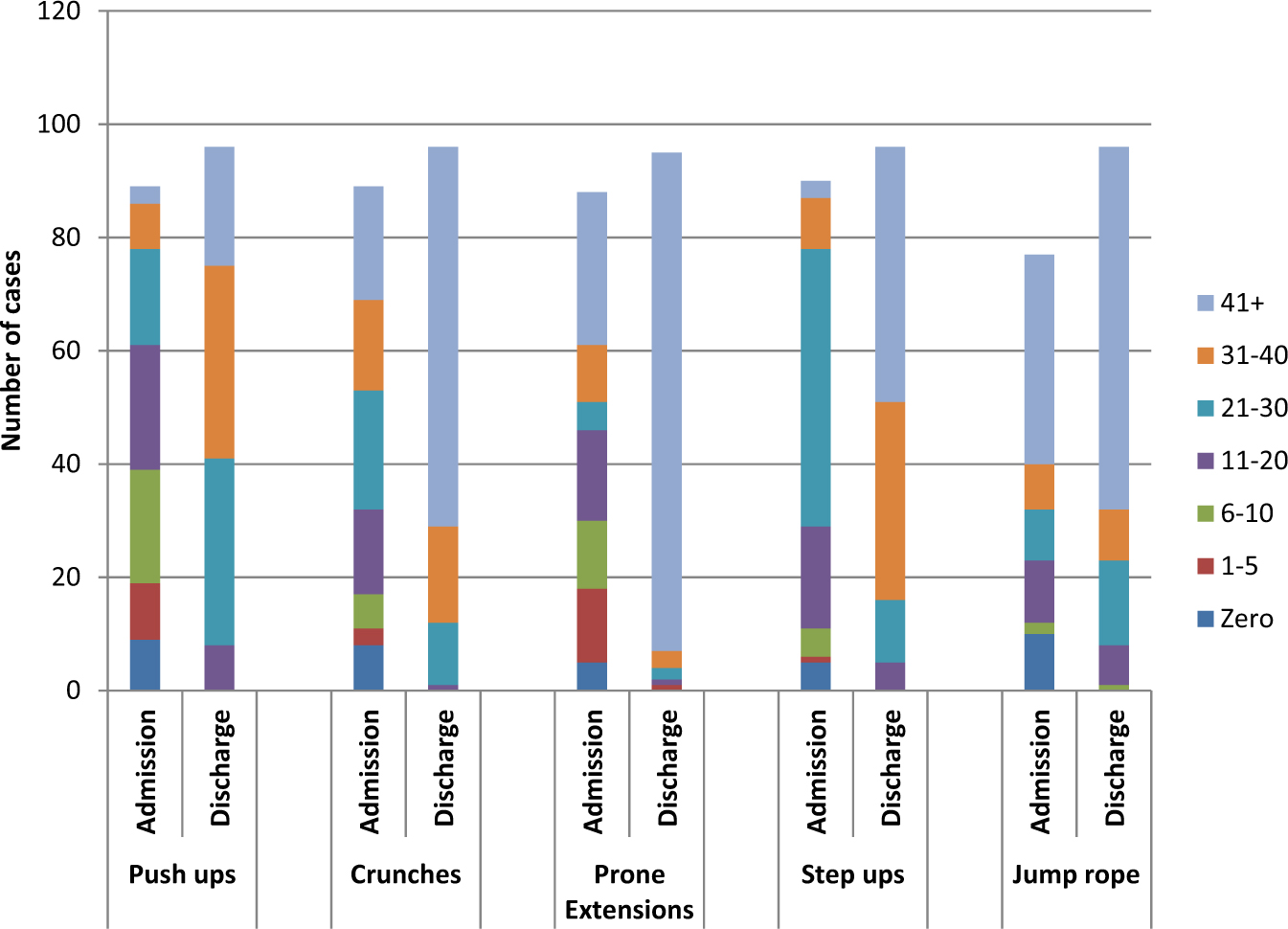
Performance on objective measures of physical functioning for participants in pediatric chronic pain rehabilitation, at admission and discharge.
3.4 Association between self-report and objective measures
Spearman correlations are listed on Table 2. Self-report measures (LEFS and UEFI) were significantly associated with most objective measures of functioning at baseline (sig. r’s ranged from .256 to .631). Correlations were slightly weaker at the discharge from the program (sig. r’s ranged from .224 to .399) with more nonsignificant associations. At both time points, self-report measures of functioning held stronger associations with self-report of pain, though again these associations were weaker at discharge.
Spearman correlations between major study variables.
| LEFS | UEFI | Push ups | Crunches | Prone extentions | Step ups | Jump rope | Pain | |
|---|---|---|---|---|---|---|---|---|
| LEFS | .774[***] | .243 | .284[*] | .343[**] | .452[***] | .423[***] | -.326[**] | |
| UEFI | 790[***] | .301[*] | .405[***] | .278[*] | .256[*] | .338[**] | -.386[***] | |
| Push ups | .129 | .091 | .504[***] | .439[***] | .181 | .520[***] | -.129 | |
| Crunches | 398[***] | .312[**] | .425[***] | .631[***] | .349[**] | .513[***] | -.320[*] | |
| Prone extentions | .039 | .080 | .323[**] | .141 | .335[**] | .620[***] | -.212 | |
| Step ups | 399[***] | .224[*] | .317[**] | .138 | -.003 | .479[***] | -.099 | |
| Jump rope | .338[**] | .261[*] | .146 | .153 | .212 | .509[***] | -.247 | |
| Pain | -.197 | -.275[*] | -.080 | -.048 | .020 | .011 | -.219 |
-
Unshaded region is admit data. Shaded region is discharge data.
3.5 Association between functioning and pain
Change in self-report measures of functioning did not significantly predict change in pain ratings during the 3-week rehabilitation program (Table 3). Change in self-reported functioning accounting for only approximately 3% of the variance in change in pain in both LEFS and UEFI (both F statistics nonsignificant). When evaluating objective measures, only change in jump ropes predicted change in pain. An increase in one’s ability to jump rope predicted a reduction in pain over the three weeks (F = 6.412, p < 0.05). All other measures were non-significant, accounting for less than 1% of change in pain scores.
Change in functional measures predicting change in pain over 3 weeks.
| R 2 | F-statistic | Standardized beta | p-Value | |
|---|---|---|---|---|
| LEFS | .033 | 2.628 | −.183 | 0.109 |
| UEFI | .027 | 2.106 | −.164 | 0.151 |
| Push ups | .006 | .398 | −.080 | 0.531 |
| Crunches | .001 | .033 | .023 | 0.856 |
| Prone extensions | .001 | .094 | .038 | 0.760 |
| Step ups | .001 | .059 | .030 | 0.808 |
| Jump rope | .104 | 6.412 | −2.532 | 0.014[*] |
4 Discussion
Many studies demonstrate overall improvement following chronic pain rehabilitation [5, 7, 8, 30], however less focus is paid on the combination of perceived physical functioning and objective abilities as an outcome. The primary goal of pediatric pain rehabilitation is to improve functioning despite pain and to limit activity avoidance. This study evaluated measures related to physical and occupational therapy components of programming.
4.1 Self-report
Data supported the hypothesis, and current efforts in rehabilitation [30], that adolescents would demonstrate statistically significant gains in both upper and lower extremity functioning following the program. More than half also report clinically significant gains in functioning over the 3 weeks of rehabilitation. Frequent practice of individualized functional tasks (i.e., simulation of school mobility, completion of house hold chores, and practice of leisure and recreation) during the program may lead to increased perception of physical functioning. This material can help demonstrate how self-report reflects ones sense of confidence and the importance of perceived outcomes on improving quality of life [7, 13, 30, 31, 32].
4.2 Objective measures
Patients also objectively demonstrated significant gains in functioning. Most patients demonstrated significant improvements in all 5 exercises from admission to discharge, completing higher repetitions at the end of the rehabilitation process as captured in Fig. 2. Not only can exercise intervals be used to track objective gains but are inherent to a rehabilitation process. Strength training is an important component to the rehabilitation process to promote functional gains in patients with chronic pain [33]. It was highlighted by therapists that the adolescents should focus on alignment, breathing, efficient and coordinated use of muscle groups, and quality of movement instead of the specific quantity of repetitions. To this end, participants at times made less significant increases in repetitions counted due to improvements in overall body mechanics.
4.3 Correlation between all measures
Both self-report measures and objective measures are helpful outcomes for assessing physical functioning and in this specific study correlated at both admission and (to a lesser degree) discharge (Table 2). Objective data correlated at admission with self-report data and pain intensity. At discharge objective data partially correlated with self-report data, more specifically lower extremity measures compared to the upper extremity measures (Table 2).
Patients with higher self-reports of function completed a higher number of repetitions with objective tests, further validating the use of self-measurement as outcome variables. However, less significant correlations at discharge suggest these measures are distinct constructs, each adding unique value to understand patient and his/her response to rehabilitation. Self-rated and objective tools each have their strengths and together may show a more global picture of physical functioning from admission to discharge. These correlations also support that when perception and confidence in one’s functional abilities was higher, the patient was able to participate at a higher level of activity. Higher correlations between UEFI/LEFS and pain perception, suggest both more closely address cognitive or perceptual aspects of patient disability than objective measures of function. Given the lower correlation with self-report pain at discharge, we would also conclude that those who understand the program philosophy (i.e., that functional gains must occur prior to potential decreases in pain), show increases in self-reported and objective functioning, even though they still report pain.
While our data did indicate a modest decrease in pain, this is not surprising. Clinically, we often notice changes in pain occurring after extended periods of increased functioning. While we anticipated changes in pain would be associated with improvements in functioning, the lack of this finding is not surprising, especially after only 3 weeks of rehabilitation.
4.4 Limitations
This study did have limitations that should be addressed, many of which point to areas for future research. First, neither selfreport nor objective measures had control groups consisting of adolescents without pain or adolescents with chronic pain not undergoing pain rehabilitation; future research could examine LEFS and UEFI as outcome measures using a group comparison model. Second, formal long-term changes in functioning were not assessed; while short term changes were captured, one cannot assume gains will be maintained at home. It will be important for future studies to assess functioning at a distant time point after rehabilitation to evaluate carryover effects of rehabilitation. Third, the objective measures originally used and collected for this study may not be the most suitable to accurately reflect change in functional strength and endurance. Further research and application of alternative functional strength and endurance exercises may be more helpful.
5 Conclusion
Impaired physical functioning is a significant issue for adolescents with chronic pain as it impacts his/her abilities and perception of capabilities to participate in age-appropriate activities. The measures used for this study (LEFS, UEFI, objective exercises) provide a realistic and meaningful way to track progress in chronic pain rehabilitation. In addition the use of objective measures of physical functioning support self-report assessments and further validates patient improvement. Although both measures may be helpful they both identify different components of the rehabilitation process in regards to return to age appropriate functioning and were found to be separate constructs. In this study gains are not directly linked to the noted reduction in pain over the 3 weeks of rehabilitation however was also not surprising due to the short time span of three weeks. Regression statistics suggest that functional improvements are independent of self-report pain reports and should be evaluated as a separate outcome in pain rehabilitation. It is uncertain what factors predict short term reductions in pain, but cognitive or emotional changes in response to rehabilitation are likely involved.
6 Implications
The use of self-report measures along with objective measures can help therapists gain understanding in regards to a patient’s insight and how that may impact their overall outcome compared to the use of a single outcome measure. It was helpful that the measures were realistic to use and review in a clinical setting. Using a verbal pain scale (0–10), self-rated functional scales, and functional strengthening exercises to track progress can also be implemented across various settings. The ability to easily view these measures at any point in the rehabilitation process can be useful to facilitate discussion about challenges the adolescent can identify and how therapies can facilitate improvement and functional gains. Given that therapy goals are patient specific, this method allows one to aggregate data across patients to evaluate the program, not just the patient. Further research should include evaluation of alternate objective measures to better capture functional strength and endurance. In addition, research using short and long term follow up data to assess maintenance of functional gains could be valuable to improve understanding of adolescents’ functional gains in intensive rehabilitation programs.
Highlights
Measures of adolescent physical functioning during pain rehabilitation are needed.
Subjective measures capture change in functioning and perceived ability.
Additional objective measures enhance monitoring of functioning.
Functional changes in pediatric pain rehabilitation are independent of pain scores.
DOI of refers to article: http://dx.doi.org/10.1016/j.sjpain.2016.11.015.
-
Author contributions: HK, RH, and EB all contributed to conceptualization and design, literature review, and some components of manuscript. HK collected data for this study using REDCap database [20]. EB ran data for statistics and data analysis. HK and EB created figures and tables. HK, EB, and RH completed further editing and critical revisions to prepare and submit manuscript.
-
Ethical issues: Data for this study was extracted retrospectively from an IRB-approved clinical database. All data collection procedures are overseen by our IRB. Information about data collection was provided to participants with an option to opt out of the clinical database, however written informed consent was not required. There were no adverse events reported as part of this study.
-
Source of support: There are no financial disclosures for this paper.
-
Conflict of interest
Conflict of interest statement: There are no conflicts of interest with this paper.
References
[1] King S, Chambers CT, Huguet A, MacNevin RC, McGrath PJ, MacDonald AJ. The epidemiology of chronic pain in children and adolescents revisited: a systematic review. Pain 2011;152:2729–38.Search in Google Scholar
[2] Stanford EA, Chambers CT, Biesanz JC, Chen E. The frequency, trajectories and predictors of adolescent recurrent pain: a population-based approach. Pain 2008;138:11–21.Search in Google Scholar
[3] Wojtowicz AA, Banez GA. Adolescents with chronic pain and associated functional disability: a descriptive analysis. J Child Health Care 2015;19:478–84.Search in Google Scholar
[4] Huguet A, Miro J. The severity of chronic pediatric pain: an epidemiological study. J Pain 2008;9:226–36.Search in Google Scholar
[5] Eccleston C, Malleson PN, Clinch J, Connell H, Sourbut C. Chronic pain in adolescents: evaluation of a programme of interdisciplinary cognitive behaviour therapy. Arch Dis Child 2003;88:881–5.Search in Google Scholar
[6] Kempert H, Benore E, Heines R. Easily administered patient reported outcome measures: adolescents’ perceived functional changes after completing an intensive chronic pain rehabilitation program. Arch Phys Med Rehabil 2016, http://dx.doi.org/10.1016/j.apmr.2016.08.471.Search in Google Scholar
[7] Maynard CS, Amari A, Wieczorek B, Christensen JR, Slifer KJ. Interdisciplinary behavioral rehabilitation of pediatric pain-associated disability: retrospective review of an inpatient treatment protocol. J Pediatr Psychol 2010;35:128–37.Search in Google Scholar
[8] Hechler T, Dobe M, Kosfelder J, Damschen U, Hubner B, Blankenburg M, Sauer C, Zernikow B. Effectiveness of a 3-week multimodal inpatient pain treatment for adolescents suffering from chronic pain: statistical and clinical significance. Clin J Pain 2009;25:156–66.Search in Google Scholar
[9] Turk DC. Clinical effectiveness and cost-effectiveness of treatments for patients with chronic pain. Clin J Pain 2002;18:355–65.Search in Google Scholar
[10] Yazdani S, Zeltzer L. Treatment of chronic pain in children and adolescents. Pain Manag 2013;3:303–14.Search in Google Scholar
[11] Townsend CO, Rome JD, Bruce BK, Hooten WM. Interdisciplianry pain rehabilitation programs. In: Ebert MH, Kerns RD, editors. Behavioral and psychpharmacologic pain management. Cambridge, UK: Cambridge University Press; 2011. p. 114–28.Search in Google Scholar
[12] Cheng CH, Su HT, Yen LW, Liu WY, Cheng HY. Long-term effects of therapeutic exercise on nonspecific chronic neck pain: a literature review. J Phys Ther Sci 2015;27:1271–6.Search in Google Scholar
[13] Guite JW, Logan DE, Sherry DD, Rose JB. Adolescent self-perception: associations with chronic musculoskeletal pain and functional disability. J Pain 2007;8:379–86.Search in Google Scholar
[14] Deitz JC, Kartin D, Kopp K. Review of the Bruininks–Oseretsky Test of Motor Proficiency, Second Edition (BOT-2). Phys Occup Ther Pediatr 2007;27:87–102.Search in Google Scholar
[15] Russell D, Rosenbaum P, Wright M, Avery L. Gross Motor Function Measure (GMFM-66 and GMFM-88) user’s manual. 2nd ed. London, UK: Mac Keith Press; 2013.Search in Google Scholar
[16] Bohannon RW. Reference values for the timed up and go test: a descriptive meta-analysis. J Geriatr Phys Ther 2006;29:64–8.Search in Google Scholar
[17] McClain J, Welk GJ, Ihmels M, Schaben JW. Comparison of two versions of the PACER aerobic fitness test. J Phys Act Health 2006;3(Suppl. 2):S47–57.Search in Google Scholar
[18] Aronoff G. Physical therapy evaluation and treatment of chronic pain. In: Aronoff G, editor. Evaluation and treatment of chronic pain. Baltimore, MD: Lippincott Williams and Wilkins; 1999.Search in Google Scholar
[19] McGrath PJ, Walco GA, Turk DC, Dworkin RH, Brown MT, Davidson K, Eccelston C, Finley GA, Goldschneider K, Haverkos L, Hertz SH, Ljungman G, Palermo T, Rapport BA, Rhodes T, Schechter N, Scott J, Sethna N, Svensson OK, Stinson J, Von Baeyer CL, Walker L, Weisman S, White RE, Zajicek A, Zeltzer L, PedIMMPAC T. Core outcome domains and measures for pediatric acute and chronic/recurrent pain clinical trials: PedIMMPACT recommendations. J Pain 2008;9:771–83.Search in Google Scholar
[20] Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap) – a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 2009;42:377–81.Search in Google Scholar
[21] Binkley JM, Stratford PW, Lott SA, Riddle DL. The Lower Extremity Functional Scale (LEFS): scale development, measurement properties, and clinical application. North American Orthopaedic Rehabilitation Research Network. Phys Ther 1999;79:371–83.Search in Google Scholar
[22] Stratford PW, Binkley JM, Stratford DM. Development and initial validation of the upper extremity functional index. Physiother Can 2001;53: 259–67.Search in Google Scholar
[23] Eccleston C, Jordan A, McCracken LM, Sleed M, Connell H, Clinch J. The Bath Adolescent Pain Questionnaire (BAPQ): development and preliminary psychometric evaluation of an instrument to assess the impact of chronic pain on adolescents. Pain 2005;118:263–70.Search in Google Scholar
[24] Plowman SA, Meredith MD, editors. Fitnessgram/activitygram reference guide. 4th ed. Dallas, TX: The Cooper Institute; 2013.Search in Google Scholar
[25] Cook G, Burton L, Hoogenboom BJ, Voight M. Functional movement screening: the use of fundamental movements as an assessment of function – Part 1. Int J Sports Phys Ther 2014;9:396–409.Search in Google Scholar
[26] Cook G, Burton L, Hoogenboom BJ, Voight M. Functional movement screening: the use of fundamental movements as an assessment of function – Part 2. Int J Sports Phys Ther 2014;9:549–63.Search in Google Scholar
[27] Wright MD, Portas MD, Evans VJ, Weston M. The effectiveness of 4 weeks of fundamental movement training on functional movement screen and physiological performance in physically active children. J Strength Cond Res 2015;29:254–61.Search in Google Scholar
[28] Swinkels RA, van Peppen RP, Wittink H, Custers JW, Beurskens AJ. Current use and barriers and facilitators for implementation of standardised measures in physical therapy in the Netherlands. BMC Musculoskelet Disord 2011;12:106.Search in Google Scholar
[29] Courtois I, Cools F, Calsius J. Effectiveness of body awareness interventions in fibromyalgia and chronic fatigue syndrome: a systematic review and metaanalysis. J Bodyw Mov Ther 2015;19:35–56.Search in Google Scholar
[30] Banez GA, Frazier TW, Wojtowicz AA, Buchannan K, Henry DE, Benore E. Chronic pain in children and adolescents: 24–42 month outcomes of an inpatient/day hospital interdisciplinary pain rehabilitation program. J Pediatr Rehabil Med 2014;7:197–206.Search in Google Scholar
[31] Hunfeld JA, Perquin CW, Duivenvoorden HJ, Hazebroek-Kampschreur AA, Passchier J, Van Suiklekom-Smith LW, Van Der Wouden JC. Chronic pain and its impact on quality of life in adolescents and their families. J Pediatr Psychol 2001;26:145–53.Search in Google Scholar
[32] Benore E, D’Auria A, Banex GA, Worley S, Tang A. The influence of anxiety reduction on clinical response to pediatric chronic pain rehabilitation. Clin J Pain 2015;31:375–83.Search in Google Scholar
[33] Mannerkorpi K, Iversen MD. Physical exercise in fibromyalgia and related syndromes. Best Pract Res Clin Rheumatol 2003;17:629–47.Search in Google Scholar
© 2016 Scandinavian Association for the Study of Pain
Articles in the same Issue
- Scandinavian Journal of Pain
- Editorial comment
- Patients with chronic neck-pain after trauma do not differ in type of symptoms and signs, but suffer more than patients with chronic neck pain without a traumatic onset
- Observational study
- Chronic neck pain patients with traumatic or non-traumatic onset: Differences in characteristics. A cross-sectional study
- Editorial Comment
- Re-enforcing therapeutic effect by positive expectations of pain-relief from our interventions
- Original experimental
- Effect of expectation on pain assessment of lower- and higher-intensity stimuli
- Editorial comment
- Objective methods for the assessment of the spinal and supraspinal effects of opioids
- Topical review
- Objective methods for the assessment of the spinal and supraspinal effects of opioids
- Editorial Comment
- Multi-target treatment of bone cancer pain using synergistic combinations of pharmacological compounds in experimental animals
- Original experimental
- Synergistic combinations of the dual enkephalinase inhibitor PL265 given orally with various analgesic compounds acting on different targets, in a murine model of cancer-induced bone pain
- Editorial comment
- Terminal cancer pain intractable by conventional pain management can be effectively relieved by intrathecal administration of a local anaesthetic plus an opioid and an alfa2-agonist into the cerebro-spinal-fluid
- Observational study
- Multimodal intrathecal analgesia in refractory cancer pain
- Editorial comment
- Treatment success in neck pain: The added predictive value of psychosocial variables in addition to clinical variables
- Observational study
- Treatment success in neck pain: The added predictive value of psychosocial variables in addition to clinical variables
- Editorial comment
- Why are some patients with chronic pain from anterior abdominal nerve entrapment syndrome (ACNES) refractory to peripheral treatment with neurectomy?
- Clinical pain research
- Treatment response and central pain processing in Anterior Cutaneous Nerve Entrapment Syndrome: An explorative study
- Editorial comment
- Gain in functions before pain reduction during intensive multidisciplinary paediatric pain rehabilitation programme
- Clinical pain research
- Physical and occupational therapy outcomes: Adolescents’ change in functional abilities using objective measures and self-report
- Editorial comment
- Complex Regional Pain Syndrome (CRPS): High risk of CRPS after trauma in another limb in patients who already have CRPS in one hand or foot: Lasting changes in neural pain modulating systems?
- Clinical pain research
- The risk of pain syndrome affecting a previously non-painful limb following trauma or surgery in patients with a history of complex regional pain syndrome
- Editorial Comment
- Positive affect could reduce the impact of pain
- Original experimental
- The buffering role of positive affect on the association between pain intensity and pain related outcomes
- Editorial comment
- The meaning and consequences of amputation and mastectomy from the perspective of pain and suffering – Lessons to be learned and relearned
- Clinical pain research
- The meaning and consequences of amputation and mastectomy from the perspective of pain and suffering
- Editorial comment
- Invasive intervention for “intractable” Complex Regional Pain Syndromes (CRPS)?
- Educational case report
- Intrathecal management of complex regional pain syndrome: A case report and literature
- Observational study
- Item response theory analysis of the Pain Self-Efficacy Questionnaire
- Announcement
- Scandinavian Association for the Study of Pain (SASP): Annual Meeting 2017
Articles in the same Issue
- Scandinavian Journal of Pain
- Editorial comment
- Patients with chronic neck-pain after trauma do not differ in type of symptoms and signs, but suffer more than patients with chronic neck pain without a traumatic onset
- Observational study
- Chronic neck pain patients with traumatic or non-traumatic onset: Differences in characteristics. A cross-sectional study
- Editorial Comment
- Re-enforcing therapeutic effect by positive expectations of pain-relief from our interventions
- Original experimental
- Effect of expectation on pain assessment of lower- and higher-intensity stimuli
- Editorial comment
- Objective methods for the assessment of the spinal and supraspinal effects of opioids
- Topical review
- Objective methods for the assessment of the spinal and supraspinal effects of opioids
- Editorial Comment
- Multi-target treatment of bone cancer pain using synergistic combinations of pharmacological compounds in experimental animals
- Original experimental
- Synergistic combinations of the dual enkephalinase inhibitor PL265 given orally with various analgesic compounds acting on different targets, in a murine model of cancer-induced bone pain
- Editorial comment
- Terminal cancer pain intractable by conventional pain management can be effectively relieved by intrathecal administration of a local anaesthetic plus an opioid and an alfa2-agonist into the cerebro-spinal-fluid
- Observational study
- Multimodal intrathecal analgesia in refractory cancer pain
- Editorial comment
- Treatment success in neck pain: The added predictive value of psychosocial variables in addition to clinical variables
- Observational study
- Treatment success in neck pain: The added predictive value of psychosocial variables in addition to clinical variables
- Editorial comment
- Why are some patients with chronic pain from anterior abdominal nerve entrapment syndrome (ACNES) refractory to peripheral treatment with neurectomy?
- Clinical pain research
- Treatment response and central pain processing in Anterior Cutaneous Nerve Entrapment Syndrome: An explorative study
- Editorial comment
- Gain in functions before pain reduction during intensive multidisciplinary paediatric pain rehabilitation programme
- Clinical pain research
- Physical and occupational therapy outcomes: Adolescents’ change in functional abilities using objective measures and self-report
- Editorial comment
- Complex Regional Pain Syndrome (CRPS): High risk of CRPS after trauma in another limb in patients who already have CRPS in one hand or foot: Lasting changes in neural pain modulating systems?
- Clinical pain research
- The risk of pain syndrome affecting a previously non-painful limb following trauma or surgery in patients with a history of complex regional pain syndrome
- Editorial Comment
- Positive affect could reduce the impact of pain
- Original experimental
- The buffering role of positive affect on the association between pain intensity and pain related outcomes
- Editorial comment
- The meaning and consequences of amputation and mastectomy from the perspective of pain and suffering – Lessons to be learned and relearned
- Clinical pain research
- The meaning and consequences of amputation and mastectomy from the perspective of pain and suffering
- Editorial comment
- Invasive intervention for “intractable” Complex Regional Pain Syndromes (CRPS)?
- Educational case report
- Intrathecal management of complex regional pain syndrome: A case report and literature
- Observational study
- Item response theory analysis of the Pain Self-Efficacy Questionnaire
- Announcement
- Scandinavian Association for the Study of Pain (SASP): Annual Meeting 2017

