A small group Whiplash-Associated-Disorders (WAD) patients with central neck pain and movement induced stabbing pain, the painful segment determined by mechanical provocation: Fusion surgery was superior to multimodal rehabilitation in a randomized trial
Graphical Abstract
Abstract
Background
The majority of patients suffering from a whiplash injury will recover, but some will have symptoms (Whiplash Associated Disorders, WAD) for years despite conservative treatment. Some of these patients perceive neck pain that might come from a motion segment, possibly the disc. In comprehensive reviews no evidence has been found that fusion operations have a positive treatment effect on neck pain in WAD patients.
Purpose
Our aim was to evaluate the possibility of (a) selecting a subgroup of chronic WAD patients based on specified symptoms possibly indicating segmental pain, and (b) treating said segmental pain through fusion operation based on non-radiological segment localization. The hypothesis was that fusion operation in this selected subgroup of chronic WAD patients could alleviate perceived neck pain.
Methods
Eligible patients for the study had a traffic accident as the origin for their neck pain, and no previous neck symptoms. Neck pain should be the predominant symptom and the pain origin reported to be in the midline, being dull, aching in character and at sudden movements combined by a stabbing pain in the same area. Forty-nine patients with these specified symptoms were identified among a large number of chronic WAD patients. Those selected had pronounced symptoms for a median of around 50 months and had previously been investigated and fully treated within the ordinary healthcare system without success.
No neurological abnormalities were to be found at clinical examination and no specific changes to be seen on X-ray and MRI. The patients were randomized to either cervical fusion operation or multimodal rehabilitation. By using a mechanical provocation test the level/s to be fused were identified. In all but one patient the surgery was performed anteriorly using microsurgical technique and a right-sided Smith-Pedersen approach and plate fixation. The multimodal rehabilitation at the Clinic of Medical Rehabilitation, Karolinska Hospital, Stockholm, included outpatient treatment for four days a week for six weeks and included treatment by physician, physiotherapists, occupational therapist, psychologists, social-service worker and nurses. Perceived change in neck pain was assessed using the Balanced Inventory for Spinal Disorders questionnaire at the 2-year-follow-up.
Results
Mean age of the patients was 38 and 40 years (surgery and rehabilitation groups, respectively), the most common type of accident being rear-end collision. At clinical examination muscle tenderness was not an outstanding sign. In most patients the mid-cervical region appeared to be the painful area but one patient localized the pain to C1. At follow-up 67% of the patients in the surgery group and 23% in the rehabilitation group assessed improvements in the ITT analysis. Corresponding proportions in the per protocol analysis were 83% and 12%, respectively.
Conclusions
The results support the supposition that among patients with central neck pain for long periods of time following a whiplash injury there are some in whom the neck pain emanates from a motion segment, probably the disc, a situation suitable for fusion surgery.
Implications
Thorough individual symptom evaluation in patients with chronic WAD may identify patients who will benefit from cervical fusion surgery.
1 Introduction
The large majority of patients with acute whiplash injuries will recover within weeks or months, but in 10-40 percent of the victims severe symptoms have been reported for years [1, 2, 3, 4,5]. In a recent Swedish study the symptoms, disabilities and life satisfaction of Whiplash Associated Disorders (WAD) patients were studied five years after the injury [6]. It was found that at that time many patients reported symptoms similar to those for mild traumatic brain injury but also that 46% of the women and 49% of the men still reported neck pain, and in 17% (women) and 6% (men) it was severe. The authors concluded that “continuous research within this area may provide a possibility to identify subgroups of the dominating symptoms in patients with WAD such as somatic, emotional or cognitive”. To the best of our knowledge we classified patients with dominating neck pain as a somatic subgroup, but within this group there might also be further subgroups based on the origin of the pain.
In comprehensive reviews [7, 8, 9, 10] no evidence has been found that fusion operations have a positive treatment effect in WAD patients, nor in patients suffering solely from neck pain for other reasons [9]. In our experience some chronic WAD patients report neck pain symptoms similar to segmental pain in the lumbar spine [11], indicating the possibility of pain from a motion segment, possibly the disc. Our aim was therefore to evaluate if it is possible to identify and select a subgroup of chronic WAD patients based on specified symptoms probably indicating segmental pain. And secondly, if this segment, although not radiologically evident, could be localized and treated by fusion operation in order to alleviate perceived neck pain among those identified patients.
For selection, chronic WAD patients were examined to find those with cervical symptoms similar to those in chronic lumbar pain patients that have been improved from fusion operation [11]. In a randomized controlled trial, the change in neck pain perceived by patients in this group after cervical fusion surgery was compared with the change in neck pain of those receiving best possible multidimensional rehabilitation treatment. The focus of this paper is to describe the specific patient selection procedure and the treatments as well as the patients’ assessments of overall perceived change in neck pain.
2 Materials and methods
This study was undertaken from July 1999 until March 2005, with a second follow-up ending in March 2010.
2.1 Patient selection
2.1.1 Inclusion criteria
Eligible patients for this study had a traffic accident as the origin of their neck pain and pronounced symptoms lasting for at least one year. Further inclusion criteria were an age of 18-60 years, working full time until the accident, and without previous neck pain. After the accident all included patients should have been fully investigated and fully treated within the ordinary healthcare system, but with continued pronounced symptoms. They should have had an ordinary plain X-ray, also in flexion and extension, and an MRI. Only patients who showed no specific changes on X-ray and MRI were included. All patients should have a marked reduction in working capacity, and be able to work a maximum of halftime.
2.1.2 Symptoms and signs
To be included the patients should present primarily with pronounced neck pain with or without pain and/or paresthesias in one or both arms, and often also in combination with headache. The neck pain should be the predominant symptom, and in the patient interviews its origin should be reported to be in the midline and to feel localized to a restricted part in height of the cervical spine. The character of the pain should be dull, aching, and when increasing possibly with radiation in the cranial or caudal direction from the origin. With sudden movements, such as missing a step or quickly turning the head, there should be a stabbing pain in the midline in the same area as the origin of the continuous dull aching pain. The sensations in the arms should be of a minor degree, including either diffuse radiation of pain or paresthesias such as tingling, pricking or numbness with varying extension. Headache as well as other commonly noticed sensations among WAD patients such as vertigo, blurred vision, sensitivity to light or sound, etc., should be of negligible importance.
At clinical examination, no motor, sensory or reflex disturbances should be present. Restriction in movement of the head and neck might be found as well as muscular tenderness in the neck, shoulders and arms. On gentle midline palpation over the spinal processes and interspinally, the origin of pain felt by the patient should be found in a restricted part of the cervical spine and pressure in that area should provoke the deep pain, which is not provoked at higher or lower levels.
In summary: to be included for randomization the patients should present with dominating neck pain, this being localized in the midline, the continuous pain mostly being aching in character and most important, the presence of a stabbing pain in the same area at sudden movements, and furthermore provocation of this deep central neck pain at pressure in the area.
Besides the selection of patients fulfilling these criteria, a group of patients with similar but not exactly the same symptoms and signs was also selected, representing a comparison group (Group C) of “ordinary” WAD patients. These patients did not report central stabbing pain and their continuous neck pain was not perceived to be restricted to the midline. Furthermore, they showed more pronounced muscle tenderness in the neck than the patients selected for randomization. The reasons for including this Group C was to illustrate the difference in symptoms and signs between the patients selected for randomization (Groups S and R) and those in Group C (Tables 2 and 4).
2.2 Sample size
Assuming a difference in the proportion of favorable outcomes (improvement in neck pain) between treatment groups of 65% vs 25% will require a group sample size of 22 in order to detect such a difference with a power of 80% at a significance level of 5% [12].
This sample size is also in accordance with the suggestions presented by Carragee et al. [9].
2.3 Patient recruitment
The patients were recruited from July 1999 to July 2002. After advertising for chronic WAD patients in Stockholm newspapers for three years, we were in contact with 1052 patients of whom 254 were seen at an outpatient examination by one of the authors (BN). No other patients were included in the study. After this three-year period no more chronic WAD patients were found and recruitment therefore stopped. Among the 254 patients examined, 49 patients fulfilling the criteria were selected. The remaining patients had lateral neck pain without central continuous pain and no stabbing central pain and were thus not in scope for our study. Only 19 of those were selected as comparison Group C.
2.4 Assessment
All patients in the study completed the disease specific Balanced Inventory for Spinal Disorders (BIS) questionnaire. The BIS is a multi-dimensional Swedish questionnaire aiming at evaluating to what extent spinal disorders affect the physical health, social life, mental health and quality of life as perceived by the patient. All 18 item-scales have five ordered categories with the verbal descriptive categories formulated to fit the different items. The follow-up version of the BIS has additional transition scales for the core variables with the categories of change: much better, somewhat better, unchanged, somewhat worse, much worse.
Comprehensive quality evaluations by non-parametric statistical methods that are appropriate for ordered categorical data have confirmed the validity, the test-retest reliability and responsiveness of the BIS items. The commonly used and recommended questionnaires, the Oswestry Disability Index (ODI), the generic quality-of-life questionnaire Short-Form-36 (SF-36), and the European Quality of Life Scale (EQ-5D) have been used for validation [13, 14, 15].
2.5 Trial design
The 49 patients who fulfilled the inclusion criteria and the 19 who did not exactly fulfill these criteria, representing “ordinary” WAD patients, filled in the BIS questionnaire and were examined by four independent examiners from different disciplines: neurology, orthopedics, physical medicine and psychology. The 49 patients who fulfilled the criteria were randomized to surgery (S, 25 pat.) or multimodal rehabilitation (R, 24 pat.).
2.6 Randomization
Randomization was performed by one of the authors (AT), a statistician not involved in the treatment of the patients. A series of closed envelopes numbered 1-50 were delivered to the Clinic of Spinal Surgery in Strangnas (CSS) before inclusion of patients to the study. The message inside the envelopes was either “operate” or “do not operate”. The statistician performing the randomization (unknown to the clinics) decided to randomize in blocks of four consecutive patients. If two patients in each block are to be operated on and two are to have rehabilitation, this can be determined in six different ways (permutations). For each block of four patients the permutation was decided by selecting a number from 1 to 6 from a table of random numbers.
2.7 Treatment
Patients in Group S wer einvestigated further in order to be operated on at CSS, and those in Group R were similarly investigated and treated non-surgically at the Clinic of Medical Rehabilitation, Karolinska Hospital, Stockholm. The patients in Group C continued their ongoing ordinary therapy without specific advice from the selecting physician.
2.7.1 Group S, surgical treatment
According to our hypothesis the neck pain of the patients selected for randomization might be of segmental origin, possibly discogenic. Since the inclusion criteria stated that there should be no specific radiological abnormalities on either plain X-ray or MRI, the level for a possibly painful disc had to be analyzed by other means.
Discography with reproduction of concordant pain, and also with pain improvement following injection of local anesthetics into the disc, have been described as methods to pinpoint a painful disc in the neck [16, 17, 18, 19, 20, 21, 22, 23], but this procedure has also been met with major criticism [24,25]. Nevertheless, we tried this technique in our first patient. We used no local anesthetics in the skin or subcutaneously. Using X-ray we localized the discs by needle contact with the front of the cervical spine. The patient found the procedure as painful as the ordinary pain and therefore recognition and possible concordance with pain elicited from a disc was difficult. We therefore abandoned this technique.
In order to obtain information regarding possible segmental pain we used the open mechanical provocation test, previously used in lumbar spine surgery [26]. The patient is awake during the procedure and in prone position. After administering successive small volumes of local anesthetics cutaneously and subcutaneously a midline incision is made, and under visual control further small volumes of local anesthetics are injected in the midline down to the spinal processes, which are now dissected free. No local anesthetics are injected deeper, and therefore facet joints, ligaments and discs are unaffected. The spinal processes can now be gently tapped in turn using a specially designed punch and mallet to allow, if possible, the patients to report concerning recognition and localization of their ordinary pain. The spinous processes were tapped one by one and the patients were instructed to report whether the tapping was felt above, below or close to their ordinary pain. When spinous processes close to the ordinary pain were found, two processes forming a pair were compared, always called number one and number two, and were tested in one direction and the other until a restricted localization to one or maximum two levels seemed to be present. Then fusion of these segments was decided upon. Since the patients had to be focused and as mentally alert as possible for localization of the neck pain, no premedication was given before the test procedure. In some of the first patients a similar testing procedure was performed percutaneously with 18 gauge (1.2 mm) needles applied to the spinal processes during X-ray: the percutaneous mechanical provocation test. Due to difficulties in applying the needles to the spinal processes in the lower cervical spine, where a lateral X-ray view is difficult to obtain due to the shoulders, the percutaneous test was omitted after the first trials.
The fusion operation was performed some weeks after the testing procedure. In all but one patient the surgery was performed anteriorly using microsurgical technique and a right-sided Smith-Pedersen approach and a standard Caspar retractor system (Aesculap, Tuttlingen, Germany). The discs regarded as possible pain generators were removed, and the adjacent bony surfaces of the vertebral bodies were drilled to create a bleeding surface for the transplant taken from the iliac crest. The transplant was rectangular in form and fit into the intervertebral space, and the respective vertebral bodies were fixed by plate and screws (CSLP, De Puy, Synthes). In one patient the painful segment seemed to be C1-C2 and in this case posterior interlaminar bone transplantation and fixation was performed.
The patients in Group S were all re-admitted to the Clinic three months after surgery for a five days stay. Treatment during this stay included training in body awareness, water aerobics, circle training, outdoor pole walk, massage and lessons and training in ergonomics.
2.7.2 Group R, multimodal rehabilitation
The multimodal treatment at the Clinic of Medical Rehabilitation at Karolinska Hospital, Stockholm, was given by a team including a physician specialized in rehabilitation medicine, physiotherapists with special skills in orthopedic medicine and neurological rehabilitation, an occupational therapist, psychologists, a social-service worker and nurses. A neurologist specialized in diagnostics and treatment of neuropathic pain was associated with the team.
The ambitious program included outpatient treatment for four days a week for six weeks. The patients were initially examined by the specialist in rehabilitation medicine and this included evaluation of the patient’s present pain, its development, and previous treatments. The physiotherapists performed a supplementary examination of the musculoskeletal system with further pain analysis. The occupational therapist examined the patient’s function and described the possible working capacity, which later comprised the basis for ergonomic instruction and training. The psychologist performed an individual psychological examination followed by supportive dialog. The social-service worker carried out a social survey.
The treatment included lectures in ergonomics, and the patients were filmed during various activities. These films were shown to the patient groups and discussed together with the therapists, resulting in individual information and advice. The ergonomic part of the program included four lessons, supplemented by training in working technique on eight occasions. Four lessons in anatomy, pain physiology and pharmacological treatment of long-standing pain were given by a physician or nurse. Physiotherapy, including training in body awareness, was performed on four occasions totaling six hours. In addition, water aerobics was conducted three times and work with exercise equipment nine times during the treatment period. The psychological and social consequences of long-standing pain and decreased activity were discussed during four group lessons in psychology, which also included problem solving and handling stress. One further lesson dealt with the effects of long-standing pain on cognitive functioning. The social service worker gave lessons concerning possibilities and obstacles regarding rehabilitation. At the end of the treatment period there was a meeting for the patients along with their closest relatives.
The treatment program included 64 h of lessons and training instructions. During the treatment period it was also possible for the patients to have individual contact with all members of the treatment staff if they wanted to discuss various medical aspects, use of analgesics or other medicines, legal insurance aspects, or to discuss other methods of treating pain, i.e. transcutaneous nerve stimulation. All patients were offered individual conversations with the social-service worker or psychologist.
The patients in Group R were instructed to continue training at home along the lines given during the treatment period.
2.7.3 Group C, comparison group, not randomized
Patients in this group were free to continue any ongoing therapy but got no advice from the selecting physician (BN) regarding any specific therapy.
2.8 Evaluation
The patients assessed their perceived neck pain on the BIS questionnaire [13, 14, 15] at the start of the study and on the follow-up occasion. The item (question) and the categories of the BIS neck pain scale were: How severe has your neck pain been during the last four weeks? No pain, negligible, moderate, rather severe or very severe.
The primary endpoint was the patient’s perceived change in neck pain assessed on the follow-up occasion on the transitional scale in the BIS follow-up questionnaire; the categories of change were: much worse, somewhat worse, unchanged, somewhat better, much better or pain completely disappeared (no pain).
2.9 Drop-outs
In Group S comprising 25 patients, 18 underwent surgery. Among the seven who did not undergo the treatment four were hesitant about surgery, one was informed by his insurance company that surgery would mean losing financial compensation, one found preoperative testing too painful and did not fulfill and one suffered from mental insufficiency.
In Group R comprising 24 patients, 17 carried out the treatment. Among the seven who did not do so three argued that they had undergone similar treatment before without improvement, one patient gave no reason for not doing so, two suffered from mental insufficiency and one patient started job training.
At the follow-up occasion six patients from Group S and five from Group R had not fulfilled the allocated treatment. In the per- protocol (PP) evaluation data from these eleven non-compliant patients were assigned to a separate group, Group D, Table 6.
2.10 Follow-up
The follow-up evaluations were performed at a mean of 21 months (median 20 months, range 17-47) for the patients in Group S, at 25 months (median 22, range 17-48) for those in Group R and at 23 months (median 22, range 17-50) for those in Group C.
2.11 Statistical methods
The intention-to-treat (ITT) analysis was performed to evaluate the effectiveness of the treatments, which is the overall effect of the planned interventions irrespective of the patients’ compliance with the allocated treatments.
An important aim of this study was to evaluate the efficacy of surgery in a well-defined group of patients, which motivates the choice of additional per-protocol (PP) analyses. This means that only those patients who complied with the allocated treatments were included in the analyses.
The frequency distributions of assessments on the outcome scale categories, for the different ITT and PP groups are shown together with the median categories. Possible differences in distributions between the groups were analyzed by the Kruskal-Wallis test.
The proportions of patients in the different groups who assessed the outcome as somewhat or much better or perceived no pain on the follow-up occasion were calculated. The differences between the groups in the proportions of patients who perceived improvements and the 95 percentage confidence intervals (95% CI) were also calculated 12,27].
An alternative approach to evaluating change was carried out on the set of paired data from the patients’ assessments on the BIS neck pain scale at the onset of the study and at follow-up. The pattern of change in assessments of neck pain is described by the frequency distribution of the pairs of data in a square contingency table, and the number of patients who assessed a lower level of neck pain at the follow-up assessments will appear above the main diagonal of unchanged assessments. The marginal totals show the frequency distributions of assessments made on each occasion. Different marginal distributions indicate the presence of systematic change that is attributed to the group. The measure of systematic change in the position of the scale assessments between the two occasions, the relative position, RP, was calculated. The RP expresses the extent to which the assessments at the follow-up are shifted toward lower levels of neck pain rather than the opposite when compared with the assessments made before treatment. Possible values of RP range from (-1) to 1. Therefore a systematic group change toward pain relief will be revealed by a positive RP-value. Additional individual variations are expressed by the relative rank variance, RV, which is a rank based measure of the observed individual variability. The measures of RP and RV and the 95% confidence intervals (CI) of the measures were calculated by a free software program [28]. The approach is presented in detail in Ref. [29] and illustrated by a practical application in Ref. [30].
2.12 Ethics
The study was approved by the Medical Ethics Committee, Örebro, Sweden, No. 368/96.
All patients were thoroughly informed, both verbally and in written text, concerning all parts of the study and gave their written informed consent.
2.13 Registration
The study is registered in ClinicalTrials.gov (Registration No. NCT01994044).
3 Results
The allocated treatment was received by 18 patients in the surgery group and 17 patients in the rehabilitation group. At follow- up, 24 of the 25 patients in the surgery group and 22 of the 24 patients in the rehabilitation group were examined. In the comparison group, where no specific treatment was received, 15 of the 19 patients were seen at follow-up. See the CONSORT flow chart (Fig. 1).
The ages of the 68 participating patients ranged from 23 to 53 years, and 69% were women, see Table 1. The type of accident that induced the symptoms, the time span to symptom debut, and the duration of symptoms are also shown.
Basic descriptive data of the patients in the three groups, S (surgery), R (rehabilitation) and C (comparison).
| Basic patient characteristics | |||
|---|---|---|---|
|
|
|||
| Group S | Group R | Group C | |
| No. of patients | 25 | 24 | 19 |
| Age (years) | |||
| Mean (SD) | 38 (6.8) | 40 (6.8) | 37 (9.0) |
| Range | 24-53 | 29-53 | 23-52 |
| Sex | |||
| Men | 10 | 5 | 6 |
| Women | 15 | 19 | 13 |
| Type of accident | |||
| Rear-end | 15 | 13 | 11 |
| Frontal | 3 | 5 | 2 |
| Side crash | 1 | 3 | 2 |
| Single accident | 5 | 3 | 4 |
| Airplane crash | 1 | ||
| Symptom debut | |||
| Median | 1 day | 1 day | 1 day |
| Range | 1 h to 3 weeks | 2 h to 2 weeks | 2 h to 4 months |
| Q1 | 1 day | 1 day | 1 day |
| Q3 | 2 days | 1-2 days | 5-6 days |
| Symptom duration (months) | |||
| Median (range) | 55 (13-241) | 46 (18-177) | 51 (11-172) |
The frequency distributions of perceived neck pain in the three groups of patients are shown in Table 2 together with descriptions of the localization and character of the neck pain and the most provoking situation. The frequency distributions of WAD symptoms other than neck pain are shown in Table 3, and clinical and radiological observations are shown in Table 4.
Neck pain severity, localization and provocation in the three patient groups, S (surgery), R (rehabilitation) and C (comparison).
| Neck pain analysis | |||
|---|---|---|---|
|
|
|||
| Group S | Group R | Group C | |
| No. of patients | 25 | 24 | 19 |
| Perceived level of neck pain | |||
| No pain | |||
| Negligible | |||
| Moderate | 2 | 1 | |
| Rather severe | 15 | 15 | 11 |
| Very severe | 8 | 8 | 8 |
| Neck pain localization | |||
| Central | |||
| Stabbing+aching | 17 | 16 | |
| Stabbing + aching + smarting + burning | 5 | 5 | |
| Stabbing+smarting+burning | 3 | 2 | |
| Aching | 6 | ||
| Smarting + burning | 1 | ||
| Central and lateral | |||
| Stabbing + aching | 1 | ||
| Aching + smarting | 1 | ||
| Just lateral | |||
| Aching | 4 | ||
| Aching + stabbing | 4 | ||
| Aching + smarting + burning | |||
| The whole neck | |||
| Aching | 1 | ||
| Most provoking situation | |||
| Bending forward | 14 | 11 | 7 |
| Bending backward | 4 | 3 | 3 |
| Movements | 2 | 8 | 5 |
| Being still | 3 | ||
| Lifting | 4 | 1 | 1 |
| None | 1 | 1 | |
WAD symptoms other than neck pain in the three patient groups, S (surgery), R (rehabilitation) and C (comparison).
| WAD symptoms other than neck pain | |||
|---|---|---|---|
|
|
|||
| Group S | Group R | Group C | |
| No. of patients | 25 | 24 | 19 |
| Radiation in arms | |||
| Pain, varying extension | 8 | 10 | 10 |
| Pain + paresthesias | 2 | 3 | |
| Paresthesias | 11 | 10 | 8 |
| None | 4 | 1 | 1 |
| Headache | |||
| Occipital | 18 | 18 | 10 |
| Crown | 3 | 1 | 2 |
| Frontal | 3 | 3 | 2 |
| On side/s | 1 | 1 | 3 |
| None | 1 | 2 | |
| Other WAD symptoms | |||
| Vertigo | 4 | 4 | 1 |
| Vertigo + sensitivity to sound | 1 | ||
| Tinnitus | 1 | ||
| Concentration problems | 1 | ||
| Sensitivity to sound | 1 | ||
| Numbness in face | 1 | ||
| None | 19 | 19 | 16 |
Clinical and radiological observations in the three patient groups, S (surgery), R (rehabilitation) and C (comparison).
| Clinical and radiological observations | |||
|---|---|---|---|
|
|
|||
| Group S | Group R | Group C | |
| No. of patients | 25 | 24 | 19 |
| Muscle tenderness in the neck | |||
| None or slight | 16 | 15 | 1 |
| Moderate | 5 | 3 | |
| Pronounced | 4 | 6 | 18 |
| ROM (range ofneck movement) | |||
| Normal or slightly reduced | 14 | 15 | 15 |
| Moderately reduced | 10 | 5 | 3 |
| Much reduced | 1 | 4 | 1 |
| Radiological observations | |||
| Normal | 11 | 9 | 9 |
| Slight disc bulging, 1 or 2 levels | 3 | 7 | 6 |
| Slight disc degeneration, 1-3 levels | 10 | 7 | 3 |
| MRI not performed | 1 | ||
| Block vertebra | 1 | 1 +disc bulging | |
At radiological examination, including plain X-ray, also with flexion and extension images, and MRI, minor deviations from normal were seen in 50-60 percent of the patients in all three groups. Slight disc bulging means no contact between this disc and any nervous structure, but simply slight bulging into the epidural space. The observation of slight disc degeneration in some of the patients in all three groups is to be expected as normal for persons at these ages [31].
3.1 Preoperative investigations, Group S
3.1.1 Disc injection
As previously mentioned discography and injection of local anesthetics into the discs was tried in only one patient, the first in the series. He reported injection at the C4-5 disc to provoke his genuine neck pain but had no relief from local anesthetics. Injection at the C5-6 disc did not provoke the ordinary pain as much as in the disc above, but after local anesthetics in the C5-6 disc he got substantial pain relief. At later percutaneous mechanical provocation (see below) the patient localized the neck pain to C4 and 5.

The figure shows the CONSORT flow diagram of the study.
3.1.2 Percutaneous mechanical provocation test
This test was performed in nine patients, with a distinct pain localization in one patient, a good localization in six patients, and indifferent results in two. In one of the latter patients open mechanical provocation (see below) was performed later, with restricted pain localization to C4 and 5. The other patient with an indifferent percutaneous test result found the examinations too extensive and did not continue.
3.1.3 Open mechanical provocation test
This test was performed in 14 patients, three of whom had previously undergone the percutaneous test. In seven of the patients localization of the neck pain appeared distinct, in a further six there was a good localization, and in one the localization was somewhat unclear but was nevertheless restricted to two neighboring spinal processes when they were slightly tapped. One of the patients with a good localization later developed mental insufficiency and did not undergo surgery. The level/levels to be fused were those beneath the respective spinal processes. Thus if recognition was felt on spinal processes C4 and C5, fusion was to be performed on levels C4-5 and C5-6, and this was based on experiences gained with this test in lumbar surgery.
3.2 Opioid requirements
In most patients the levels appearing to be the painful ones were those of the mid-cervical region, C4-5 and C5-6, but one patient localized his pain to C1 (Table 5). During surgery the discs were inspected through the operation microscope. Although the discs differed in consistency, with some that were drier and others more elastic, there were none with separation of the vertebral endplates. Fissures in the discs were not seen. Bleeding during surgery was scanty and there were no neurological or other complications, nor any long-standing pain from the donor site at the iliac crest.
Number of patients operated on at the levels indicated.
| Operated levels No | |
|---|---|
| C1-2 | 1 |
| C3-4 + C4-5 | 2 |
| C4-5 + C5-6 | 8 |
| C5-6 + C6-7 | 4 |
| C6-7 + C7-Th1 | 3 |
3.3 Perceived change in neck pain
3.3.1 Intention-to-treat (ITT) evaluation
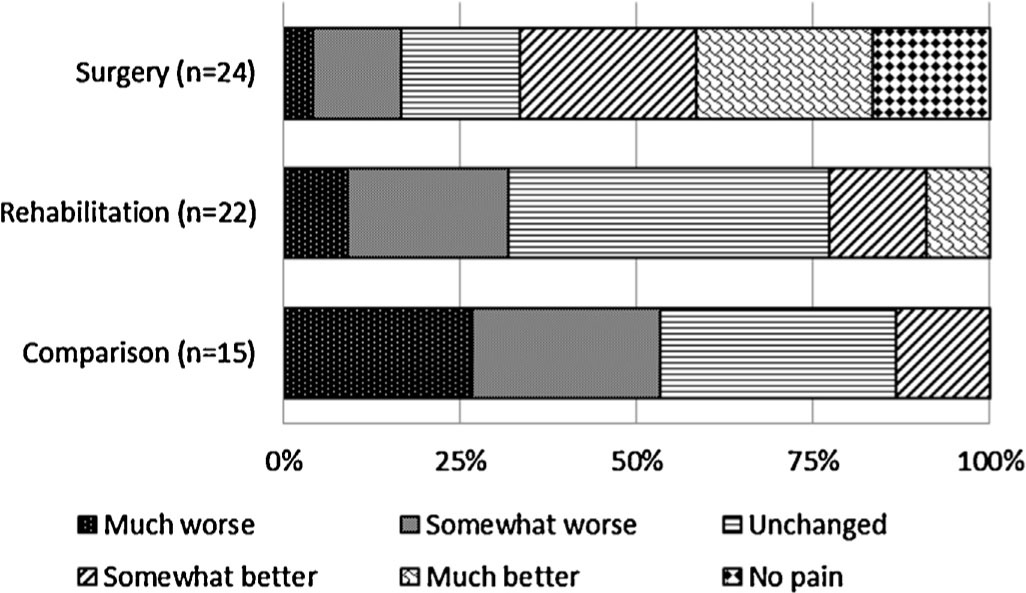
The frequency distributions of the assessments of change made by the patients on the follow-up occasion differed between the three groups in significant favor of the surgery group (S) (p = 0.0007), with the median level of change being somewhat better, see Table 6 and Fig. 3.
Frequency distributions of intention-to-treat(ITT) and per-protocol (PP) out comes according to the assessments made by the patients on the BIS outcome scale in the surgery (S), rehabilitation (R), and comparison (C) groups. The D group includes the patients randomized to surgery (6 patients) or rehabilitation (5 patients) but not fulfilling the treatments. The overall p-value from the Kruskal-Wallis analysis of possible differences in distributions and the median categories are shown.
| Outcome, change in perceived neck pain | |||||||
|---|---|---|---|---|---|---|---|
|
|
|||||||
| Much worse | Somewhat worse | Unchanged | Somewhat better | Much better | No pain | Overall p-value Median change | |
| ITT analysis | |||||||
| Group | |||||||
| Patients | p=0.0007 | ||||||
| Group S | 1 | 3 | 4 | 6 | 6 | 4 | Somewhat better |
| Group R | 2 | 5 | 10 | 3 | 2 | Unchanged | |
| Group C | 4 | 4 | 5 | 2 | Somewhat worse | ||
| PP analysis | |||||||
| Group | |||||||
| Patients | p=0.0006 | ||||||
| Group S | 3 | 5 | 6 | 4 | Much better | ||
| Group R | 2 | 4 | 9 | 1 | 1 | Unchanged | |
| Group C | 4 | 4 | 5 | 2 | Somewhat worse | ||
| Group D | 1 | 1 | 5 | 3 | 1 | Unchanged | |
This significant effect of surgery on the perceived change in neck pain related to the whip-lash injury was confirmed by the test of difference in the proportions of patients who assessed somewhat or much better or no neck pain on the follow-up occasion.
Four of the patients in the surgery group (S) perceived no neck pain and another 12 assessed their neck pain as somewhat or much better, which means that 67% of the patients in Group S assessed improvements two years after surgery. Correspondingly, five of the 22 patients (23%) in Group R, and two of the 15 patients (13%) in Group C who completed the BIS on the follow-up occasion assessed some level of improvement. This means that 44 percentage units (p.u.) more patients in Group S than in Group R assessed an improvement. The 95% confidence interval for this difference in proportions from 15 p.u. to 64 p.u. confirms the significant difference in treatment effects on perceived neck pain in favor of the surgery group as compared to the rehabilitation group. This is the most important conclusion from our trial. Corresponding differences in proportions of improvements were 54 percentage units (95% CI, 25 p.u. to 72 p.u) between Group S and Group C, and 10 percentage units (95% CI, -18 p.u. to 32 p.u.) between Group Rand Group C.
3.3.2 Per-protocol (PP) evaluation
In the per-protocol evaluation only those patients who consented to and completed the allocated treatments were evaluated as S, R and C patients, respectively. Group D, comprising the 11 non- compliers, also participated in the follow-up examinations. The frequency distributions of assessments of change in the four groups are shown in Table 6 together with the overall p-value for the analysis of possible differences in distributions. The distributions of outcome assessments and the median levels were significantly in favor of the patients who underwent surgery (S), with much better as the median level of change (p = 0.0006). No statistically significant differences in outcomes were found between groups R, C and D.
These findings were confirmed by the differences in the proportions of patients who assessed improved outcomes on the follow-up occasion. A majority, 83%, of the 18 patients who underwent surgery (S) perceived improvements as compared to 12% and 13% of the patients with improvements in the R and C groups, respectively. Hence, 71 percentage units more patients with treatment S than with treatment R assessed improvements (95% CI: 40; 85), and thus the same conclusion as in the ITT-analysis. The corresponding difference between S patients and C patients was 70 percentage units (95% CI: 37; 85). The difference in the proportions of patients who perceived improvements between the 18 patients with surgery (S) and the 11 non-compliers (D) was 47 percentage units (95% CI: 11; 71).
As evident from Table 6, the proportions of patients with perceived improvements in groups R, C, and D were 12%, 13%, and 36%, respectively. The differences in proportions between R vs C, -1 (95% CI: -28; 23) p.u., R vs D, -24 (95% CI: -54; 6) p.u., and C vs D -23 (95% CI: -53; 9) p.u. also show the lack of evidence for a better outcome in patients after treatment R compared with the outcomes assessed by the patients in groups C or D.
3.3.3 Change in paired assessments of neck pain
The ITT evaluation of the change in paired assessments is based on the paired distribution of assessments of neck pain made by the patients at study start and on the follow-up occasion. Fig. 2A shows that 15 patients in Group S assessed lower levels of neck pain two years after surgery, and eight patients assessed equal levels on both occasions. This decrease in perceived neck pain was confirmed by the significant measure of systematic group change in neck pain, RP, 0.45 (95% CI: 0.23; 0.69). This means that in the patients randomized to surgery it is about 0.23-0.69 more likely to perceive lower than higher neck pain levels than the reverse two years after surgery. The additional individual variability in pain assessments after surgery, with six patients changing from very or rather severe pain to negligible or no pain after surgery and the other patients with fewer categorical changes is revealed by RV 0.16 (95% CI: 0; 0.36).
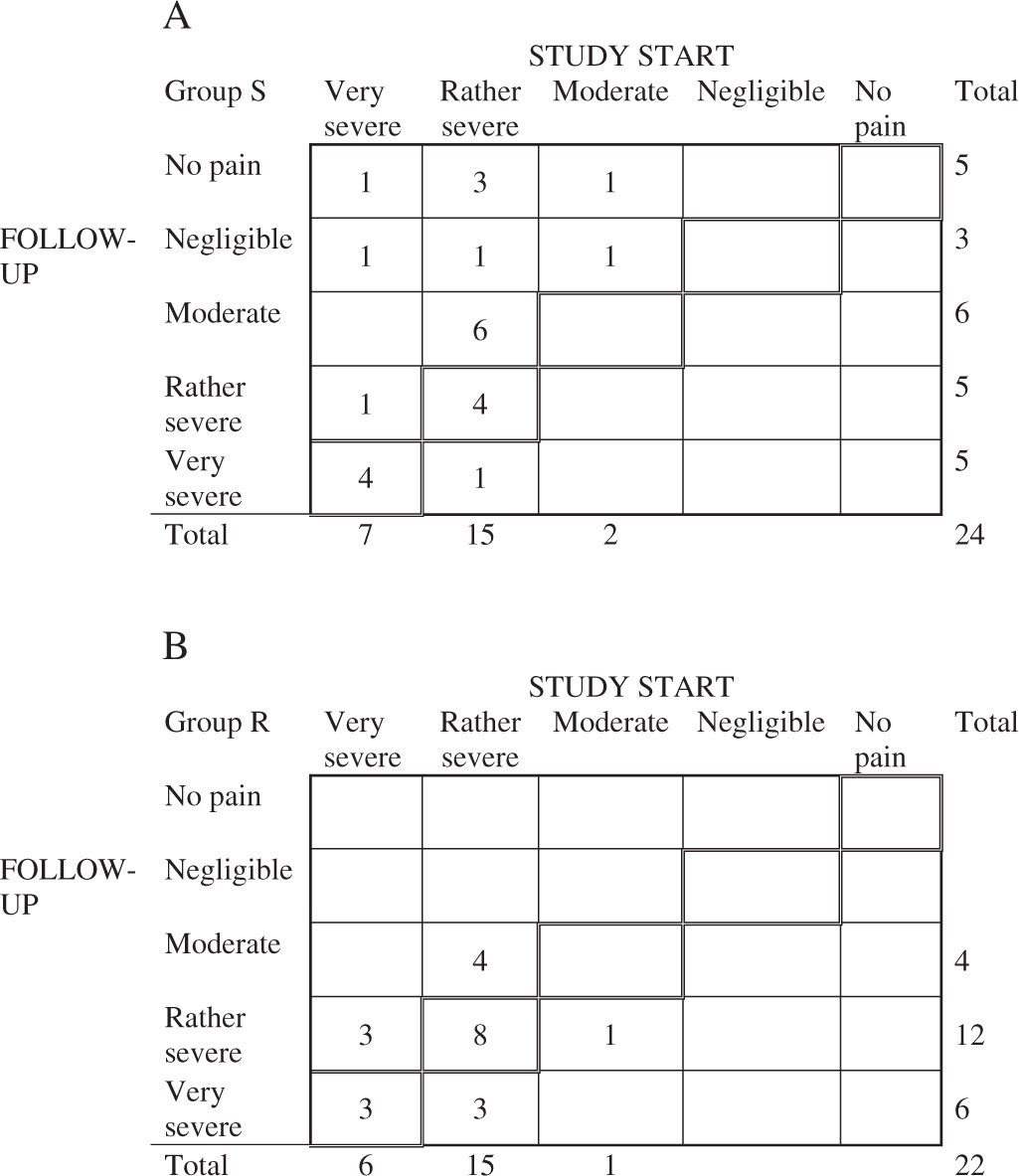
The frequency distribution of the pairs of assessments of perceived neck pain made by the patients in Group S (A), and in Group R (B) at study start and on the follow-up occasion. The diagonal of unchanged assessments is marked.
The pattern of change in assessments by the rehabilitation Group R, Fig. 2B, shows that 11 (50%) patients assessed equal levels of neck pain on both occasions, and another seven assessed a one category lower level of neck pain on the follow-up occasion. The measure of this slight non-significant systematic decrease in perceived neck pain, RP, was 0.10 (95% CI: -0.13; 0.33), and the individual dispersion was negligible, RV 0.04 (95% CI: 0; 0.18).
The paired assessments of neck pain in the comparison group were similar to those in Fig. 2B, but seven of the 15 patients assessed a one category higher level of neck pain on the follow-up occasion. This systematic non-significant increase is evident as seen by the RP, -0.11 (95% CI: -0.40; 0.18). The RV was 0.19 (95% CI: 0; 0.45). This strong evidence for different treatment effects on perceived neck pain between the groups of patients is illustrated in Fig. 3.

The frequency distribution of the pairs of assessments of perceived neck pain made by the patients in Group S (A), and in Group R (B) at study start and on the follow-up occasion. The diagonal of unchanged assessments is marked.
The PP evaluation of the pattern of change in assessments of neck pain shows similar results. The systematic decrease in neck pain for the 18 patients who underwent surgery was more pronounced, RP = 0.62 (95% CI: 0.34; 0.89). For the 17 patients who completed the rehabilitation treatment, RP = 0.08 (95% CI: -0.20; 0.37).
4 Discussion
Neck pain following whiplash injury, as well as neck pain for other reasons, often shows spontaneous variability. This was one of the reasons we included only patients who had had symptoms for long periods of time (a mean of about four years) and who had been fully treated within the ordinary healthcare system without success, and still presented with pronounced symptoms. At that stage the symptom variability had probably decreased. The other reason was that among such a group of patients treatment success was rather unrealistic and therefore, if it actually occurred, it might indicate causal therapy.
In the present study we included only patients with a special character and localization of their neck pain for randomization to either type of treatment. Patients with similar but slightly different symptoms, judged as ordinary WAD patients, were not included for randomization, Group C (see Tables 2 and 3).
The basis for our selection of patients for randomization, dull aching pain localized in a restricted area in the midline of the cervical spine and combined with stabbing pain in the same area upon sudden movements is an application of the results previously found in chronic low back pain patients improved by fusion operation [11]. Among those patients the actual symptoms were considered to indicate segmental, discogenic pain, and consequently the subgroup selected for randomization among the chronic WAD patients might have the same reason for their neck pain.
In previous studies concerning fusion operations for neck pain, patients with whiplash injuries have been included as part of the patient material, and clear improvement in neck pain following the operation has been reported by some authors 32,33], but not by others 34,35]. Surgery has been tried in the late chronic stage of genuine WAD, although not in randomized controlled studies [36, 37, 38]. In the review by Carragee et al. [9], the authors concluded that up until 2008 no studies had been published concerning treatment of neck pain by cervical fusion that were scientifically admissible according to the Neck Pain Task Force, and therefore there was no evidence that fusion operations in such patients had a treatment effect. The same conclusion was reached in the latest review published byTeasell et al. [10].
However, biomechanical studies have shown that cervical inter-vertebral discs may be at risk for injury during whiplash situations [39], and disc lesions are also described in post-mortem material from WAD patients [40, 41, 42, 43]. Thus the possibility exists that chronic neck pain in some WAD patients might be of discogenic origin. If those patients were to be selected, localization of the actual painful segment/disc would remain. To that end we used a mechanical provocation test. Although this test has been used for a long period of time in lumbar fusion surgery [26], it is not validated. Therefore, if a better instrument for localization of a painful disc were at hand, results might be further improved. Grob et al. [37] used external fixation as a tool for possibly localizing a painful segment and reported that 17 out of 21 whiplash patients operated on by fusion showed much improvement at follow-up 12.9 months after surgery. External fixation has, however, not been found to be of value in lumbar fusion surgery [44].
In our study both the ITT and the PP evaluations of the patients’ perceived change in neck pain showed a significant improvement in patients in Group S, and the treatment effect in Group S was more pronounced than in the other groups. The patient’s own global assessment has previously been found to be a valid outcome measure with a high degree of relationship to other outcome instruments, at least in lumbar fusion surgery [45]. Based on our study it can be concluded that in a selected group of WAD patients suffering from long-term neck pain of the specific type and localization described here, it is most likely that about 40-85 percentage units more patients will perceive significant neck pain relief after cervical fusion surgery than after rehabilitation treatment. The evaluation of paired assessments of neck pain made at study start and on the follow-up occasion showed that the change in neck pain assessments toward lower pain levels was significantly pronounced in the surgery group of patients. This supports the hypothesis that the patients selected for randomization represent a subgroup of chronic WAD patients in whom the pain appears to emanate from a motion segment, probably the disc.
In forthcoming papers more detailed results regarding the patients’ perceived outcomes in quality-of-life and functioning made on the Short-Form 36 (SF-36) and on the Balanced Inventory for Spinal Disorders (BIS) questionnaires will be presented. Furthermore, we will separately publish comprehensive analyses of possible differences in assessments of outcomes between four examiners, each representing disciplines that are commonly involved in whiplash injuries: neurology, orthopedic surgery, physical medicine, and psychology.
5 Limitations of the study
The sample sizes of 25 and 24 patients in the respective arms seem to imply a risk for false positive results, further accentuated by the fairly large proportion of patients not receiving the allocated treatment. However, in this study we have used rank-based statistical methods that are appropriate for evaluation of dependent and independent small sets of ordered categorical data. Similar sample sizes have been recommended, for example by the Bone and Joint Decade 2000-2010 Task Force on Neck Pain (see Ref. [9]). As described in Section 2.3 we searched for more chronic WAD patients but after three years no more such patients were to be found in the area around Stockholm. Patients from other areas were not possible to include due to practical reasons, especially for treatment R, outpatient rehabilitation treatment.
6 Conclusion
In conclusion, cervical fusion surgery in a group of chronic WAD patients with specific symptomatology was found to be significantly better than multimodal rehabilitation in relieving neck pain, as assessed by the patients themselves, when analyzed at a follow- up time of around two years. This supports the supposition that among patients with central neck pain for long periods of time following a whiplash injury there are some in whom the neck pain emanates from a motion segment, probably the disc.
Highlights
Some patients with Whiplash- Associated-Disorder (WAD) have central neck pain and movement induced stabbing pain.
Such WAD-patients were evaluated for possible segmental pain and surgical fusion.
A mechanical provocation test determined segmental fusion level/s.
Cervical fusion was compared with multimodal rehabilitation in a randomized trial.
Fusion was significantly better than rehabilitation in relieving neck pain.
DOI of refers to article: http://dx.doi.org/10.1016/j.sjpain.2016.03.004.
Acknowledgments
We gratefully acknowledge the financial support from the Marianne and Marcus Wallenberg Foundation, the Axel and Margaret Ax:sonJohnsson Foundation, Volvo and Vägverket. We express our sincere thanks to the independent examiners Associate Professor Ake Siden, Professor Ian Goldie, Professor NilsInge Landrö and Associate Professor Peer Staff for their assessments of the patients before and after treatment, assessments to be described in forthcoming papers.
-
Conflict of interest: The authors have no conflict of interest.
References
[1] Carroll LJ, Holm LW, Hogg-Johnson S, Cote P, Cassidy JD, Haldeman S, Nordin M, Hurwitz EL, Carragee EJ, van der Velde G, Peloso PM, Guzman J. Course and prognostic factors for neck pain in whiplash-associated disorders (WAD). Spine 2008;33:S83-92.Search in Google Scholar
[2] Gargan MF, Bannister GC. Long-term prognosis of soft-tissue injuries of the neck.J Bone Joint Surg Br 1990;72-B:901-3.Search in Google Scholar
[3] Jonsson H, Cesarini K, Sahlstedt B, Rauschning W. Findings and outcome in whiplash-type neck distortions.Spine 1994;19:2733-43.Search in Google Scholar
[4] Sterling M, Hendrikz J, Kenardy J. Compensation claim lodgement and health outcome developmental trajectories following whiplash injury: a prospective study. Pain 2010;150:22-8.Search in Google Scholar
[5] Watkinson A, Gargan MF, Bannister GC.Prognostic factors in soft tissue injuries of the cervical spine. Injury 1991;22:307-9.Search in Google Scholar
[6] Styrke J, Sojka P, Björnstig U, Stälnacke B-M. Symptoms, disabilities, and life satisfaction five years after whiplash injuries. Scand J Pain 2014;5:229-36.Search in Google Scholar
[7] Spitzer WO, Skovron ML, Salmi LR, Cassidy JD, Duranceau J, Suissa S, Zeiss E. Scientific monograph of the Quebec task force on whiplash-associated disorders: redefining “Whiplash” and its management. Spine 1995;20(Suppl. 8S):S1-73.Search in Google Scholar
[8] Conlin A, Bhogal S, Sequeira K, Teasell R. Treatment of whiplash-associated disorders—Part II: Medical and surgical interventions. Pain Res Manag 2005;10:33-40.Search in Google Scholar
[9] Carragee EJ, Hurwitz EL, Cheng I, Carroll LJ, Nordin M, Guzman J, Peleso P, Holm LW, Hogg-Johnson S, van der Velde G, Cassidy JD, Haldeman S. Treatment of neck pain. Injections and surgical interventions: results of the Bone and Joint Decade 2000-2010Task Force on Neck Pain and its associated disorders. Spine 2008;33:S153-69.Search in Google Scholar
[10] Teasell RW, McClure JA, Walton D, PrettyJ, Salter K, Meyer M, Sequeira K, Death B. A research synthesis of therapeutic interventions for whiplash-associated disorder(WAD): Part 5 - Surgicaland injection-based interventions forchronic WAD. Pain Res Manag 2010;15:323-34.Search in Google Scholar
[11] Nyström B. Segmental lumbarpain. Ups J Med Sci 1993;(Suppl.52):67.Search in Google Scholar
[12] Altman DG. Practical statistics for medical research. London: Chapman and Hall; 1991.Search in Google Scholar
[13] Svensson E, Schillberg B, Kling A-M, Nyström B. The Balanced Inventory for Spinal Disorders.The validity ofadisease specific questionnaire for evaluation of outcomes in patients with various spinal disorders. Spine 2009;34:1976-83.Search in Google Scholar
[14] Svensson E, Schillberg B, Kling A-M, Nyström B. Reliability of the Balanced Inventory for Spinal Disorders, a questionnaire for evaluation of outcomes in patients with various spinal disorders. J Spinal Disord Tech 2012;25:196-204.Search in Google Scholar
[15] Svensson E, Schillberg B, Zhao X, Nyström B. Responsiveness of the Balanced Inventory for Spinal Disorders, a questionnaire for evaluation of outcomes in patients with various spinal disorders. J Spine Neurosurg 2015;4:2, http://dx.doi.org/10.4172/2325-9701.1000184.Search in Google Scholar
[16] Bogduk N, Aprill C. On the nature of neck pain, discography and cervical zygapophysial joint blocks. Pain 1993;54:213-7.Search in Google Scholar
[17] Cloward RB. Cervical diskography. Technique, indications and use in diagnosis of ruptured cervical disks. Am J Roentgenol Radium Ther Nucl Med 1958;79:563-74.Search in Google Scholar
[18] Grubb SA, Kelly CK. Cervical discography: clinical implications from 12 years of experience. Spine 2000;25:1382-9.Search in Google Scholar
[19] Palit M, Schofferman J, Goldthwaite N, Reynolds J, Kerner M, Keaney D, Lawrence-Miyasaki L. Anterior discectomy and fusion for the management of neck pain. Spine 1999;24:2224-8.Search in Google Scholar
[20] Roth DA. Cervical analgesic discography. A new test for the definitive diagnosis ofthe painful-disk syndrome. JAMA 1976;235:1713-4.Search in Google Scholar
[21] Schellhas KP, Smith MD, Gundry CR, Pollei SR. Cervical discogenic pain. Prospective correlation of magnetic resonance imaging and discography in asymptomatic subjects and pain sufferers. Spine 1996;21:300-12.Search in Google Scholar
[22] Simmons EH, Bhalla SK. Anterior cervical discectomy and fusion with a note on Discography: technique and interpretation of results (WP Butt).JBoneJoint Surg Br 1969;51B:225-37.Search in Google Scholar
[23] Whitecloud TS, Seago RA. Cervical discogenic syndrome. Results of operative intervention in patients with positive discography. Spine 1987;12:313-6.Search in Google Scholar
[24] Nordin M, Carragee EJ, Hogg-Johnson S, Schecter Weiner S, Hurwitz EL, Peloso PM, Guzman J, van der Velde G, Carroll LJ, Holm LW, Côté P, Cassidy JD, Haldeman S. Assessment of neck pain and its associated disorders. Results of the Bone and Joint Decade 2000-2010 Task Force on neck pain and its associated disorders. Spine 2008;33:S101-22.Search in Google Scholar
[25] Shinomiya K, Nakao K, Shindoh S, Mochida K, Furuya K. Evaluation of cervical diskography in pain origin and provocation. J Spinal Disord 1993;6: 422-6.Search in Google Scholar
[26] Nyström B. Open mechanical provocation under local anesthesia: a definitive method for locating the focus in painful mechanical disorder of the motion segment. In: Fifth international conference on lumbar fusion and stabilization. 1991. p. 198.Search in Google Scholar
[27] Altman DG, Machin F, Bryant TN, Gardner MJ. Statistics with confidence. 2nd ed. Bristol: BMJ Books; 2000.Search in Google Scholar
[28] Avdic A, Svensson E. Svensson method 1. Interactive software supporting Svensson’s method. 1st ed; 2010, Örebro. Accessed from: http://www-oru.se/hh/elisabeth_svensson.Search in Google Scholar
[29] Svensson E. Ordinal invariant measures for individual and group changes in ordered categorical data. Stat Med 1998;17:2923-36.Search in Google Scholar
[30] Svensson E, Starmark JE. Evaluation of individual and group changes in social outcome after aneurismal subarachnoid haemorrhage: a long-term follow-up study. J Rehab Med 2002;34:241-9.Search in Google Scholar
[31] Matsumoto M, Fujimura Y, Suzuki N, Nishi Y, Nakamura M, Yutaka Y, Shiga H. MRI of cervical intervertebral discs in asymptomatic subjects. J Bone Joint Surg Br 1998;80-B:19-24.Search in Google Scholar
[32] Cloward RB. Lesions of the intervertebral disks and their treatment by inter body fusion methods. Clin Orthoped 1963;27:51-77.Search in Google Scholar
[33] Garvey TA, Transfeldt EE, Malcolm JR, Kos P. Outcome of anterior cervical discectomy and fusion as perceived by patients treated for dominant axial- mechanical cervical spine pain. Spine 2002;27:1887-95.Search in Google Scholar
[34] Löfgren H, Thesis. Linköping, Sweden Outcome and bone grafts in surgical treatment of cervical disc disease; 2000.Search in Google Scholar
[35] Zoёga B, Thesis. Gothenburg, Sweden Cervical discectomy and fusion with or without plate fixation. A randomized clinical and radiographic study on outcome and cost-utility; 1998.Search in Google Scholar
[36] Algers G, Pettersson K, Hildingsson C, Toolanen G. Surgery for chronic symptoms after whiplash injury. Follow-up of 20 cases. Acta Orthop Scand 1993;64:654-6.Search in Google Scholar
[37] Grob D, Dvorak J, Panjabi MM, Antinnes JA. Fixateur externe an der Halswirbelsäule - ein neues diagnostisches Mittel. Unfallchirurg 1993;96:416-21.Search in Google Scholar
[38] Long DM, Davis RF, Speed WG, Hendler NH. Fusion for occult posttraumatic cervical facet injury. Neurosurg Q 2006;16:129-34.Search in Google Scholar
[39] Panjabi MM, Ito S, Pearson AM, Ivancic PC. Injury mechanisms of the cervical intervertebral disc during simulated whiplash. Spine 2004;29:1217-25.Search in Google Scholar
[40] Barnsley L, Lord S, Bogduk N. Clinical Review. Whiplash injury. Pain 1994;58:283-307.Search in Google Scholar
[41] Curatolo M, Bogduk N, Ivancic PC, McLean SA, Siegmund GP, Winkelstein BA. The role of tissue damage in Whiplash-Associated Disorders. Spine 2011;36:S309-15.Search in Google Scholar
[42] Jonsson H, Bring G, Rauschning W, Sahlstedt B. Hidden cervical spine injuries in traffic accident victims with skull fractures. J Spinal Disord 1991;4:251-63.Search in Google Scholar
[43] Taylor JR, Twomey LT. Acute injuries to cervical joints. An autopsy study of neck sprain. Spine 1993;18:1115-22.Search in Google Scholar
[44] Elmans L, Willems PC, Anderson PG, van Limbeek J, de Kleuver M, van der Schaaf D. Temporary external transpedicular fixation of the lumbosacral spine. A prospective, longitudinal study in 330 patients. Spine 2005;30:2813-6.Search in Google Scholar
[45] Hägg O, Fritzell P, Odén A, Nordwall A. Simplifying outcome measurement. Evaluation of instruments for measuring outcome after fusion surgery for chronic low back pain. Spine 2002;27:1213-22.Search in Google Scholar
© 2016 Scandinavian Association for the Study of Pain
Articles in the same Issue
- Scandinavian Journal of Pain
- Editorial comment
- Depressive symptoms associated with poor outcome after lumbar spine surgery: Pain and depression impact on each other and aggravate the burden of the sufferer
- Clinical pain research
- Depressive symptoms are associated with poor outcome for lumbar spine surgery
- Editorial comment
- Chronic compartment syndrome is an under-recognized cause of leg-pain
- Observational study
- Prevalence of chronic compartment syndrome of the legs: Implications for clinical diagnostic criteria and therapy
- Editorial comment
- Genetic susceptibility to postherniotomy pain. The influence of polymorphisms in the Mu opioid receptor, TNF-α, GRIK3, GCH1, BDNF and CACNA2D2 genes
- Clinical pain research
- Genetic susceptibility to postherniotomy pain. The influence of polymorphisms in the Mu opioid receptor, TNF-α, GRIK3, GCH1, BDNF and CACNA2D2 genes
- Editorial comment
- Important development: Extended Acute Pain Service for patients at high risk of chronic pain after surgery
- Observational study
- New approach for treatment of prolonged postoperative pain: APS Out-Patient Clinic
- Editorial comment
- Working memory, optimism and pain: An elusive link
- Original experimental
- The effects of experimental pain and induced optimism on working memory task performance
- Editorial comment
- A surgical treatment for chronic neck pain after whiplash injury?
- Clinical pain research
- A small group Whiplash-Associated-Disorders (WAD) patients with central neck pain and movement induced stabbing pain, the painful segment determined by mechanical provocation: Fusion surgery was superior to multimodal rehabilitation in a randomized trial
- Editorial comment
- Social anxiety and pain-related fear impact each other and aggravate the burden of chronic pain patients: More individually tailored rehabilitation need
- Clinical pain research
- Characteristics and consequences of the co-occurrence between social anxiety and pain-related fear in chronic pain patients receiving multimodal pain rehabilitation treatment
- Editorial comment
- Transcranial magnetic stimulation, paravertebral muscles training, and postural control in chronic low back pain
- Original experimental
- Influence of paravertebral muscles training on brain plasticity and postural control in chronic low back pain
- Editorial comment
- Is there a place for pulsed radiofrequency in the treatment of chronic pain?
- Clinical pain research
- Pulsed radiofrequency in clinical practice – A retrospective analysis of 238 patients with chronic non-cancer pain treated at an academic tertiary pain centre
- Editorial comment
- More postoperative pain reported by women than by men – Again
- Observational study
- Females report higher postoperative pain scores than males after ankle surgery
- Editorial comment
- The relationship between pain and perceived stress in a population-based sample of adolescents – Is the relationship gender specific?
- Observational study
- Pain is prevalent among adolescents and equally related to stress across genders
- Editorial comment
- The Brief Pain Inventory (BPI) – Revisited and rejuvenated?
- Clinical pain research
- Confirmatory factor analysis of 2 versions of the Brief Pain Inventory in an ambulatory population indicates that sleep interference should be interpreted separately
- Editorial comment
- Pain research reported at the 40th scientific meeting of the Scandinavian Association for the Study of Pain in Reykjavik, Iceland May 26–27, 2016
- Abstracts
- Pain management strategies for effective coping with Sickle Cell Disease: The perspective of patients in Ghana
- Abstracts
- PEARL – Pain in early life. A new network for research and education
- Abstracts
- Searching for protein biomarkers in pain medicine – Mindless dredging or rational fishing?
- Abstracts
- Effectiveness of smart tablets as a distraction during needle insertion amongst children with port catheter: Pre-research with pre-post test design
- Abstracts
- Postoperative oxycodone in breast cancer surgery: What factors associate with analgesic plasma concentrations?
- Abstracts
- Sport participation and physical activity level in relation to musculoskeletal pain in a population-based sample of adolescents: The Young-HUNT Study
- Abstracts
- “Tears are also included” - women’s experience of treatment for painful endometriosis at a pain clinic
- Abstracts
- Predictors of long-term opioid use among chronic nonmalignant pain patients: A register-based national open cohort study
- Abstracts
- Coupled cell networks of astrocytes and chondrocytes are target cells of inflammation
- Abstracts
- Changes in opioid prescribing behaviour in Denmark, Sweden and Norway - 2006-2014
- Abstracts
- Opioid usage in Denmark, Norway and Sweden - 2006-2014 and regulatory factors in the society that might influence it
- Abstracts
- ADRB2, pain and opioids in mice and man
- Abstracts
- Retrospective analysis of pediatric patients with CRPS
- Abstracts
- Activation of epidermal growth factor receptors (EGFRs) following disc herniation induces hyperexcitability in the pain pathways
- Abstracts
- Pain rehabilitation with language interpreter, a multicenter development project
- Abstracts
- Trait-anxiety and pain intensity predict symptoms related to dysfunctional breathing (DB) in patients with chronic pain
- Abstracts
- Emla®-cream as pain relief during pneumococcal vaccination
- Abstracts
- Use of Complimentary/Alternative therapy for chronic pain
- Abstracts
- Effect of conditioned pain modulation on long-term potentiation-like pain amplification in humans
- Abstracts
- Biomarkers for neuropathic pain – Is the old alpha-1-antitrypsin any good?
- Abstracts
- Acute bilateral experimental neck pain: Reorganise axioscapular and trunk muscle activity during slow resisted arm movements
- Abstracts
- Mast cell proteases protect against histaminergic itch and attenuate tissue injury pain responses
- Abstracts
- The impact of opioid treatment on regional gastrointestinal transit
- Abstracts
- Genetic variation in P2RX7 and pain
- Abstracts
- Reversal of thermal and mechanical allodynia with pregabalin in a mouse model of oxaliplatin-induced peripheral neuropathy
- Clinical pain research
- Pain-related distress and clinical depression in chronic pain: A comparison between two measures
Articles in the same Issue
- Scandinavian Journal of Pain
- Editorial comment
- Depressive symptoms associated with poor outcome after lumbar spine surgery: Pain and depression impact on each other and aggravate the burden of the sufferer
- Clinical pain research
- Depressive symptoms are associated with poor outcome for lumbar spine surgery
- Editorial comment
- Chronic compartment syndrome is an under-recognized cause of leg-pain
- Observational study
- Prevalence of chronic compartment syndrome of the legs: Implications for clinical diagnostic criteria and therapy
- Editorial comment
- Genetic susceptibility to postherniotomy pain. The influence of polymorphisms in the Mu opioid receptor, TNF-α, GRIK3, GCH1, BDNF and CACNA2D2 genes
- Clinical pain research
- Genetic susceptibility to postherniotomy pain. The influence of polymorphisms in the Mu opioid receptor, TNF-α, GRIK3, GCH1, BDNF and CACNA2D2 genes
- Editorial comment
- Important development: Extended Acute Pain Service for patients at high risk of chronic pain after surgery
- Observational study
- New approach for treatment of prolonged postoperative pain: APS Out-Patient Clinic
- Editorial comment
- Working memory, optimism and pain: An elusive link
- Original experimental
- The effects of experimental pain and induced optimism on working memory task performance
- Editorial comment
- A surgical treatment for chronic neck pain after whiplash injury?
- Clinical pain research
- A small group Whiplash-Associated-Disorders (WAD) patients with central neck pain and movement induced stabbing pain, the painful segment determined by mechanical provocation: Fusion surgery was superior to multimodal rehabilitation in a randomized trial
- Editorial comment
- Social anxiety and pain-related fear impact each other and aggravate the burden of chronic pain patients: More individually tailored rehabilitation need
- Clinical pain research
- Characteristics and consequences of the co-occurrence between social anxiety and pain-related fear in chronic pain patients receiving multimodal pain rehabilitation treatment
- Editorial comment
- Transcranial magnetic stimulation, paravertebral muscles training, and postural control in chronic low back pain
- Original experimental
- Influence of paravertebral muscles training on brain plasticity and postural control in chronic low back pain
- Editorial comment
- Is there a place for pulsed radiofrequency in the treatment of chronic pain?
- Clinical pain research
- Pulsed radiofrequency in clinical practice – A retrospective analysis of 238 patients with chronic non-cancer pain treated at an academic tertiary pain centre
- Editorial comment
- More postoperative pain reported by women than by men – Again
- Observational study
- Females report higher postoperative pain scores than males after ankle surgery
- Editorial comment
- The relationship between pain and perceived stress in a population-based sample of adolescents – Is the relationship gender specific?
- Observational study
- Pain is prevalent among adolescents and equally related to stress across genders
- Editorial comment
- The Brief Pain Inventory (BPI) – Revisited and rejuvenated?
- Clinical pain research
- Confirmatory factor analysis of 2 versions of the Brief Pain Inventory in an ambulatory population indicates that sleep interference should be interpreted separately
- Editorial comment
- Pain research reported at the 40th scientific meeting of the Scandinavian Association for the Study of Pain in Reykjavik, Iceland May 26–27, 2016
- Abstracts
- Pain management strategies for effective coping with Sickle Cell Disease: The perspective of patients in Ghana
- Abstracts
- PEARL – Pain in early life. A new network for research and education
- Abstracts
- Searching for protein biomarkers in pain medicine – Mindless dredging or rational fishing?
- Abstracts
- Effectiveness of smart tablets as a distraction during needle insertion amongst children with port catheter: Pre-research with pre-post test design
- Abstracts
- Postoperative oxycodone in breast cancer surgery: What factors associate with analgesic plasma concentrations?
- Abstracts
- Sport participation and physical activity level in relation to musculoskeletal pain in a population-based sample of adolescents: The Young-HUNT Study
- Abstracts
- “Tears are also included” - women’s experience of treatment for painful endometriosis at a pain clinic
- Abstracts
- Predictors of long-term opioid use among chronic nonmalignant pain patients: A register-based national open cohort study
- Abstracts
- Coupled cell networks of astrocytes and chondrocytes are target cells of inflammation
- Abstracts
- Changes in opioid prescribing behaviour in Denmark, Sweden and Norway - 2006-2014
- Abstracts
- Opioid usage in Denmark, Norway and Sweden - 2006-2014 and regulatory factors in the society that might influence it
- Abstracts
- ADRB2, pain and opioids in mice and man
- Abstracts
- Retrospective analysis of pediatric patients with CRPS
- Abstracts
- Activation of epidermal growth factor receptors (EGFRs) following disc herniation induces hyperexcitability in the pain pathways
- Abstracts
- Pain rehabilitation with language interpreter, a multicenter development project
- Abstracts
- Trait-anxiety and pain intensity predict symptoms related to dysfunctional breathing (DB) in patients with chronic pain
- Abstracts
- Emla®-cream as pain relief during pneumococcal vaccination
- Abstracts
- Use of Complimentary/Alternative therapy for chronic pain
- Abstracts
- Effect of conditioned pain modulation on long-term potentiation-like pain amplification in humans
- Abstracts
- Biomarkers for neuropathic pain – Is the old alpha-1-antitrypsin any good?
- Abstracts
- Acute bilateral experimental neck pain: Reorganise axioscapular and trunk muscle activity during slow resisted arm movements
- Abstracts
- Mast cell proteases protect against histaminergic itch and attenuate tissue injury pain responses
- Abstracts
- The impact of opioid treatment on regional gastrointestinal transit
- Abstracts
- Genetic variation in P2RX7 and pain
- Abstracts
- Reversal of thermal and mechanical allodynia with pregabalin in a mouse model of oxaliplatin-induced peripheral neuropathy
- Clinical pain research
- Pain-related distress and clinical depression in chronic pain: A comparison between two measures

