Abstract
Background and aims
The symptoms of pain and depression often present concomitantly, but little is known as to how the different subtypes of depression affect surgical outcome. The aim of this study was to determine whether there is a difference in outcome after lumbar spine surgery between non-depressed patients and patients with different subtypes of depressive symptoms: non-melancholic (NmDS) and melancholic depression (MDS).
Methods
This was a cross-sectional postal survey. A self-made questionnaire, the Beck Depression Inventory (BDI) and the Oswestery Low Back Disability Questionnaire (ODI) were sent to patients who had undergone lumbar spine surgery in the Oulu University Hospital between June, 2005 and May, 2008. BDI ≤ 10 were further classified into NmDS or MDS.
Results
A total of 537 patients (66%) completed the survey. Of these, 361 (67%) underwent disc surgery, 85 (16%) stabilizing surgery and 91 (17%) decompression. Participants were divided into three groups: BDI< 10 N=324 (60%), NmDS N=153 (29%) and MDS N=60 (11%). The mean ODI (SD) in the BDI<1 0 group was 16 (15), in the NmDS group 36 (15), and in the MDS group 41 (18) (p<0.001). The ODI profiles were different between the groups (p<0.001). Pain was more frequent in depressive patients (88% of MDS, 81% in NmDS and 40% in BDI < 10 patients experienced pain, p<0.001). The intensity of pain and pain-related disability was lowest among the patients in the BDI <10 group and highest among the MDS patients. Regular pain medication was used by 87% of patients in the MDS group, 93% of patients in the NmDS group, and 71% of patients in the BDI< 10 group (p<0.001). Response to pain medication with NRS (0–10) was 5.6 among MDS, 5.8 among NmDS and 6.5 among BDI< 10 patients (p<0.001).
Conclusion
Different types of depressive symptoms are associated with poor outcome after lumbar spine surgery. The outcome was worst in patients suffering from the MDS subtype. This was observed in pain intensity, functional disability and response to pain medication.
Implication
It would be important to evaluate depression pre- and postoperatively. Offering a tailored rehabilitation programme to MDS patients should be considered.
© 2016 Scandinavian Association for the Study of Pain. Published by Elsevier B.V. All rights reserved.
1 Introduction
Depression is one of the most prevalent diseases globally: 6% of the population meets the major depressive disorder criteria at some point in time [1]. According to the Health 2000 Study, the prevalence of depression is 6.5% in Finland [2]. The lifetime prevalence of depressive disorders was almost 18% in the latest Finnish study among younger population subjects [3]. Depression affects one out of every six adults during their lifetime, women being affected twice as often as men [4]. The biological mechanisms behind depression include the autonomous nervous system and monoamine neurotransmission dysfunction, cytokine- mediated inflammatory reactions [5,6,7], and overactivity of the hypothalamic-pituitary-adrenal (HPA) axis [8,9,10]. Psychological factors may also play a significant role, as the metabolic syndrome is associated with a passive life attitude and negative self-image, both of which may contribute to the development of depression [11,12].
Patients seeking care for a pain problem often also report symptoms of depression. Depression is associated with the development of chronic pain as well as with poor results for treatment [13]. On average, 65% of patients seeking care for depression have comorbid pain problems and about half of the patients with chronic pain fulfil the criteria for depression [14].
Depression can be divided into two main subgroups: melancholic (MDS, ‘typical’) and non-melancholic (NmDS, ‘atypical’) depression [15]. These two depression types have different symptom profiles. NmDS is marked by fatigue, increased appetite and weight gain, mood reactivity and interpersonal rejection sensitivity. MDS is characterized by anhedonia, non-reactive mood, and symptoms of insomnia, loss of appetite, mood variation and impaired concentration [1]. Approximately 45-70% of depressive individuals are MDS type and 15–30% are NmDS type [16, \17]. Melancholic depression is considered to be a more multifaceted biological condition [1,18]. Reduced, dysfunctional serotonergic and noradrenergic neurotransmission may contribute to pain perception [19].
We have previously reported functional capacity and quality of life after lumbar spine surgery in a Finnish, working-aged patient cohort [20]. Pain and depression often present together, but little is known as to what extent the different subtypes of depression affect surgical outcome. The aim of this study was to investigate how the two main subtypes of depressive symptoms (NmDS, MDS) influence outcome in lumbar spine surgery.
2 Materials and methods
To investigate the postoperative results of lumbar spine surgery in patients treated in the Oulu University Hospital, patients were identified using ICD-10 procedure codes for lumbar spine operations during the period 1.6.2005 to 31.5.2008. Surgical procedures due to acute traumas were excluded. Only working-aged patients (18–65 years) were included. Each patient was listed only once, and the index operation was defined as the last lumbar spine surgery during the above-mentioned period. Based on medical records, patient who had undergone lumbar spine reoperation after 1.6.2008 and patients with insufficient capacity in the Finnish language, major abuse problem or progressive, severe illness (e.g., cancer, dementia) were excluded. The ICD-10 diagnosis code for spinal disease and previous lumbar spine operations before the index operation were recorded. The study protocol was approved by the local ethics committee, and patients gave their written informed consent.
The questionnaires and a consent form were sent to all traceable patients in September 2009. The patients were asked to fill in a self-made questionnaire, the Beck Depression Inventory (BDI) and the Oswestery Low Back Disability Questionnaire (ODI).
The self-made questionnaire included questions regarding the occurrence of pain (never, occasionally, daily or almost daily, and all the time), the average intensity of pain (on a numerical rating scale, NRS, 0–10) and pain-associated disability (NRS 0-10). Axial low back pain and radicular pain were assessed separately. Regularly and occasionally used medications for low back pain were queried. Patients evaluated the efficacy of pain medication with an NRS (0= no relief at all, 10= complete pain relief). Patients were asked to record their weight (kg) and height (m), from which their body mass index (BMI) was calculated. Leisure-time physical activity was assessed by asking how many periods of over 30min exercise sessions per week each patient practised. Sleep disturbance caused by pain was queried using options 0 = “not at all”, 1= ’’mild, wakenings, but easily falls asleep again”, 2= “moderate, sleep disturbed many nights a week” and 3= “severe, sleep severely disturbed every night”.
The Beck Depression Inventory is a 21-item self-report questionnaire to assess possible depression and has been validated in Finnish [21,22,23]. The cut-off point for increased depressive symptoms (DS) was 10, and has thereby been reported to be a feasible instrument for depression screening [22]. In order to examine the effect of the subtypes of DS, we used a summary score of melancholic symptoms in BDI based on the DSM-IV defined criteria for melancholic depression (sadness, past failure, loss of pleasure, guilty feelings, punishment feelings, loss of interest, irritability, change of sleeping and appetite), dividing the participants with increased DS into melancholic (MDS) and non-melancholic depressive symptom (NmDS) subgroups in a manner similar to that which has been previously published [24, 6, 25, 26].
The ODI contains ten items each with six statements graded from zero (lowest disability) to five (greatest disability). The total score is calculated as a sum of each completed item and expressed as a percentage of the maximum number of possible points, i.e. related to the number of items the patient has answered [27]. Scores are defined on a scale according to the original publication: 0–20 minimal, 20–40 moderate and 40–60 severe disability. A score 60–80 indicates a crippled patient and 80–100 indicates that the patient is either bed-bound or exaggerating their symptoms [28].
2.1 Statistical methods
The data are presented as means with standard deviations (SD) or as counts with percentages. Statistical comparisons were made using the analysis of variance (ANOVA), chi-square test or Fisher–Freeman–Halton exact test. When adjusting for confounding factors, an analysis of covariance (ANCOVA) or logistic models was applied. The bootstrap (10,000 replications) method was used when the theoretical distribution of the test statistics were unknown or in the case of violation of the assumptions (e.g. non-normality). Differences in the ODI item-profiles between the groups were determined using a bootstrap-type, multivariate approach with the Hotelling T-squared test; it is a method to compare means of all variables of interest simultaneously (in the present analysis the ODI items) while maintaining the chosen magnitude of Type I error. The normality of variables was evaluated by the Shapiro-Wilk W test. The Stata 14.0, StataCorp LP (College Station, TX, USA) statistical package was used for the analyses.
3 Results
During the study period 1.6.2005 to 31.5.2008, a lumbar spine operation due to non-traumatic lumbar disease was performed in 1180 patients in our hospital. Of these, 11 had passed away by the beginning of this study. Of the surviving patients, 273 were excluded due to age, 43 due to other diseases, 28 due to a subsequent lumbar spine surgery after the index operation, 7 due to severe abuse problem and 4 due to insufficient capacity in the Finnish language. Hence the postal survey was mailed to 814 patients, of whom 537 (66%) replied.
The BDI score was ≤10 in 213 of 537 patients (39%). When DS patients were further analysed we found 153 (28%) patients with NmDS and 60 (11%) with MDS. The clinical characteristics of patients without DS (a BDI score <10), with NmDS and with MDS are illustrated in Table 1. There were gender differences between the DS groups. Patients without DS were younger than patients with NmDS or MDS. BMI was highest in the NmDS group. There were more reoperations in the NmDS and MDS groups. There were relatively fewer cases of disc surgery and more cases of stabilizing and decompression surgery in the NmDS and MDS groups.
Clinical characteristics of patients without DS, with NmDS and with MDS.
| BDI<10 | NmDS | MDS | p-value | |
|---|---|---|---|---|
| N = 324 | N = 153 | N = 60 | ||
| Number of females, n (%) | 134(41) | 72(47) | 37(62) | 0.013 |
| Age, years, mean (SD) | 44(11) | 47(10) | 48(10) | 0.003 |
| BMI, mean(SD) | 26.7(4.0) | 28.6(5.6) | 27.8(6.1) | <0.001 |
| Index operation, first, n (%) | 293(90) | 126(82) | 48(80) | 0.012 |
| Follow-up time, months, mean (SD) | 31(10) | 31(10) | 32(11) | 0.84 |
| Surgery, n (%) | <0.001 | |||
| Disc surgery | 245(76) | 84(55) | 32 (53) | |
| Stabilizing surgery | 39(12) | 34(22) | 12(20) | |
| Decompression | 40(12) | 35(23) | 16(27) | |
| Diagnosis, n (%) | <0.001 | |||
| M51.1[a] | 255(79) | 89(58) | 33(55) | |
| M51.3[b] | 6(2) | 10(7) | 3(5) | |
| M48.0[c] | 43(13) | 36(24) | 17(28) | |
| M43.1[d] | 11(3) | 8(5) | 2(3) | |
| M96[e] | 9(3) | 10(7) | 5(8) | |
| Beck index, mean (SD) | 4.0(2.9) | 17.6(6.8) | 19.9(10.5) | <0.001 |
| Sleep disturbances[f], n(%) | 48(15) | 72(47) | 38 (63) | <0.001 |
| High frequency of pain[g], n (%) | 129(40) | 124(81) | 53(88) | <0.001 |
| ODI, mean (SD) | 16(15) | 36(15) | 41(18) | <0.001 |
| Leisure time physical activity, n (%) | 0.17 | |||
| Low | 60(20) | 36(26) | 14(25) | |
| Moderate | 225(73) | 92 (66) | 34(61) | |
| High | 22(7) | 11(8) | 8(14) |
Mean BDI in the NmDS group was 17.6 and in the MDS group 19.9, with no significant difference between them. Sleep disturbances were significantly more common among DS patients compared to patients without DS. When comparing DS subtypes, MDS patients had significantly more disturbed sleep compared to NmDS patients (p= 0.033).
There was a significant difference in functional disability between the DS groups (p < 0.001) (Table 1). Items from the ODI are illustrated in Fig. 1. The ODI profiles were different between the groups (p<0 .001 after adjusted age, gender and follow-up time). Profiles were also different between the NmDS and MDS groups (p= 0.012). MDS patients had higher scores compared to NmDS patients in the following items: personal care (p = 0.025), walking (p= 0.049) and sleep (p<0.001).
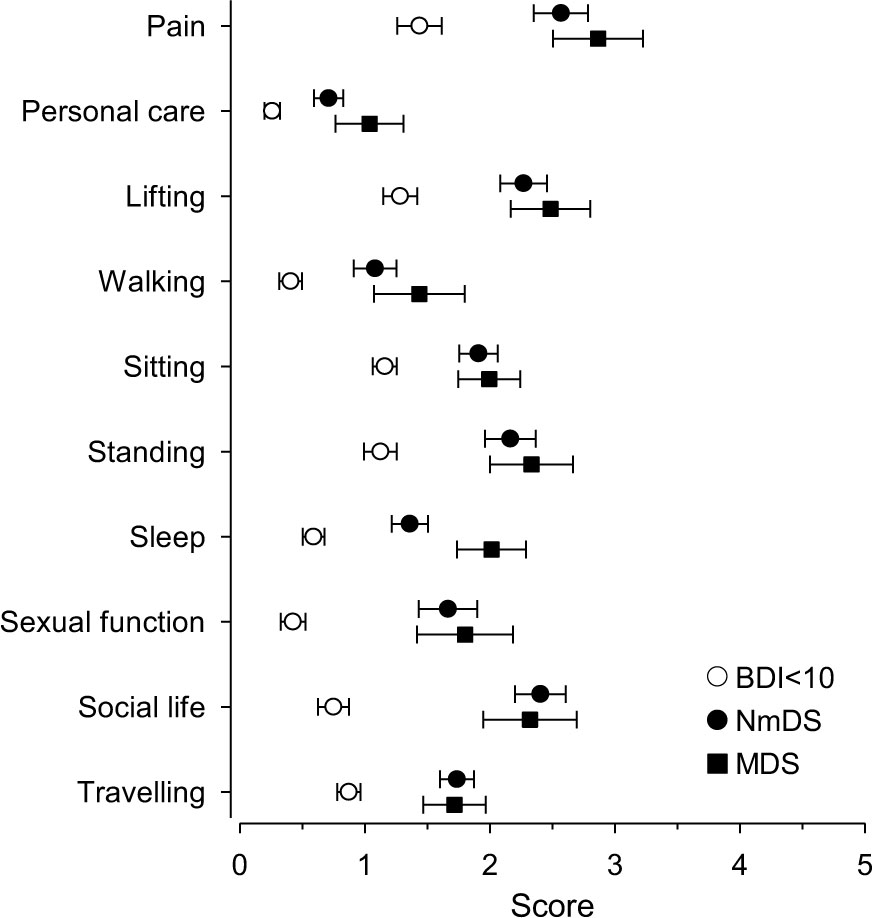
ODI profiles with 95% CI in different groups of depressive symptoms.
NmDS and MDS patients suffered more frequently from pain (81% and 88%, respectively) compared to patients without DS (40%) (p<0.001). There were significant differences in the mean intensity of local lower back pain, radiculating leg pain and pain-related disability (Fig. 2).
The use of pain medication and antidepressants is presented in Table 2. There were significant differences in the use of regular pain medication between the groups. Regular medication for pain was used by 231 (71%) patients in the BDI< 10 group, 143 (93%) in the NmDS and 52 (87%) in the MDS group (p < 0.001 after adjusted age, gender and follow-up time). The mean response to pain medication (NRS 0–10) was 6.5 (SD 2.3) in the BDI< 10 group, 5.8 (SD 2.3) in NmDS and 5.6 (SD 2.5) in MDS patients’ group (p <0.001 after adjusted age, gender and follow-up time).
The use of regular pain medication in different groups of depressive symptoms.
| Regular pain medication | BDI <10 | NmDS | MDS | p-value[a] |
|---|---|---|---|---|
| N = 324 | N = 153 | N = 60 | ||
| NSAID, n (%) | 153(47) | 75(49) | 26(43) | 0.74 |
| Paracetamol, n (%) | 45(14) | 34(22) | 21(35) | 0.008 |
| Opioids, n (%) | ||||
| Weak | 68(21) | 71(46) | 29(48) | <0.001 |
| Strong | 2(1) | 12(8) | 2(3) | 0.003 |
| Tricyclic antidepressants, n (%) | 19(6) | 19(12) | 7(12) | 0.058 |
| Gapabentinoids, n (%) | 20(6) | 31(20) | 11(18) | <0.001 |
| Centrally acting muscle relaxants, n (%) | 23(7) | 23(15) | 4(7) | 0.015 |
| SNRI-antidepressants, n (%) | 1(1) | 8(5) | 1(2) | <0.001 |
| Sodium channel blockers, n (%) | 0(0) | 4(3) | 0(0) | 0.061 |
-
NSAID, non-steroidal anti-inflammatory drug; SNRI, serotonin-norepinephrine reuptake inhibitor.

Numerical rating (0–10) of mean low back pain, leg pain and pain related disability in different depression groups; adjusted age, gender and follow-up time.
4 Discussion
The main finding of this study was that different types of depressive symptoms are associated with poor outcome after lumbar spine surgery. Especially MDS patients had higher levels of pain, higher incidences of sleep disturbances by pain and poorer functional disability. They used pain medication on a more regular basis, while receiving less benefit from its use. The use of antidepressants was very low in this study population, even amongst patients who scored high in the BDI questionnaire.
Depressive symptoms have been shown to predict poorer surgical outcome after lumbar spine surgery [29,30,31,32,33], which finding is in accordance with our observation. To our knowledge, this is the first study to examine the role that different depression subtypes play in modifying the postoperative result after spinal surgery. We demonstrated that MDS patients had a poorer outcome after lumbar surgery in comparison to NmDS patients or patients without depression, which is in agreement with the monoaminergic hypothesis of depression [5].
The relative number of cases of stabilizing and decompression surgery increased in the NmDS and MDS groups. More complicated surgery in the depressive patients could be one important reason for the poorer outcome observed. We know that outcome regarding pain, functional capacity and quality of life is less favourable after stabilizing and decompression surgery compared to disc surgery [20]. MDS patients still have poorer overall results in all groups compared to our previous study.
The response elicited to analgesic medication was poorer in both DS groups compared to the non-depressive. The three most commonly used pain medications were non-steroidal anti-inflammatory drugs (NSAID), weak opioids and paracetamol in this order. Nearly half of the patients used NSAIDs, one third used weak opioids and one fifth used paracetamol. This is in agreement with the Finnish Current Care Guideline for treatment of low back pain [34]. Depressive patients used pain medication on a more regular basis than did non-depressive. This could be seen in the use of paracetamol, weak opioids, tricyclic antidepressants, gabapenti- noids (gabapentin, pregabalin) and central acting muscle relaxants (titzanidine, clonazepam, orphenadrine citrate).
The use of strong opioids was rare. It was most common in the NmDS group, of which only 8% used strong opioids. Systematic reviews have demonstrated scant evidence of efficacy in the use of strong opioids for chronic low back pain [35]. Opioids have a short-term analgesic efficacy, but the long term effectiveness and safety of opioids are unknown. The regular use of strong opioids may cause more harm than benefits. In this material, the prevalence of the regular use of strong opioids was adequately low. The use of muscle relaxant was common, though there is only weak evidence of its efficacy [36].
In the material included in this study, depression was neither detected nor treated during the follow-up. The use of serotonin- norepinephrine reuptake inhibitors (SNRIs) was unusual: only 5% of NmDS and 2% of MDS patients used SNRIs. According to a Cochrane Review, there is no clear evidence to support the use of antidepressants for patients with chronic lower back pain [37]. In spite of this, the Cochrane Review does not imply that depressed patients with low pain should not be treated with antidepressants. Traditionally, NmDS patients displayed a better response to monoamine oxidase inhibitor antidepressants than to other antidepressants [38]. Antidepressive medications with this mechanism ofaction are very seldom used in the treatment of depression in Finland, and there were none in our material.
When ODI was examined in the different depression subtypes, MDS patients displayed a significantly worse outcome. When single items from the ODI were analysed separately, significant differences could be seen in walking, personal care and sleep. MDS patients also reported more moderate and severe sleep disturbances than NmDS patients. This can partly be explained by the symptom profile of MDS, which is characterised by symptoms of insomnia [1], but may also be due to higher pain intensity and its interference with sleep. NmDS patients have been shown to have an increased appetite and weight gain, a higher BMI and a higher incidence of metabolic syndrome [16]. This was also our finding: NmDS patients had a higher BMI than other two groups.
The strengths of our study include a large study population from a geographically defined area and a high response rate to postal questioning. One limitation of this study is that we had no preoperative information regarding pain, ODI or BDI. In our material, it is not clear whether depressive symptoms predisposed to low back pain or was the depression a reaction to low back pain. The use of sleep medication was not required in this study. We concentrated on patients of a working-age, thus the results may not be generalized to patients outside the age range of 18–65 years.
5 Conclusion
Depression has an effect on coping with disease and pain, surgical outcome, the rehabilitation process and response to pain management. According to our study, different types of depressive symptoms are associated with poor outcome after lumbar spine surgery. The outcome was least acceptable in patients suffering from the MDS subtype, as was determined from pain intensity, functional disability and response to pain medication.
6 Implication
An evaluation of depression and its subtypes pre- and postoperatively would be very important. In particular, MDS is associated with poor outcome after lumbar surgery. This group of patients should be identified preoperatively and offered a tailored rehabilitation programme.
Highlights
Of 537 responders after lumbar surgery 39% had Beck Depression Inventory ≥ 10.
Of these 28% had non-melancholic (NmDS) and 11% melancholic depression (MDS).
MDS patients had more pain, sleep disturbances by pain and poorer functional disability.
MDS patients used more regular pain medication and received less benefit from its use.
MDS patients need tailored pre- and postoperative rehabilitation programme.
DOI of refers to article: http://dx.doi.org/10.1016/j.sjpain.2016.04.006.
-
Conflict of interest: There are no conflicts of interest.
Acknowledgements
The authors would like to thank the personnel of the pain clinic in the Oulu University Hospital for their help collecting the data. The study received financial support from the Health Care Foundation of North Finland.
References
[1] Penninx BW, Milaneschi Y, Lamers F, Vogelzangs N. Understanding the somatic consequences of depression: biological mechanisms and the role of depression symptom profile. BMC Med 2013;11:129, 7015-11-129.Search in Google Scholar
[2] Pirkola SP, Isometsa E, Suvisaari J, Aro H, Joukamaa M, Poikolainen K, Koskinen S, Aromaa A, Lonnqvist JK. DSM-IV mood-, anxiety- and alcohol use disorders and their comorbidity in the Finnish general population - results from the health 2000 study. Soc Psychiatry Psychiatr Epidemiol 2005;40:1–10.Search in Google Scholar
[3] Suvisaari J, Aalto-Setala T, Tuulio-Henriksson A, Harkanen T, Saarni SI, Perala J, Schreck M, Castaneda A, Hintikka J, Kestila L, Lahteenmaki S, Latvala A, Koski- nen S, Marttunen M, Aro H, Lonnqvist J. Mental disorders in young adulthood. Psychol Med 2009;39:287–99.Search in Google Scholar
[4] Alonso J, Angermeyer MC, Bernert S, Bruffaerts R, Brugha TS, Bryson H, de Girolamo G, Graaf R, Demyttenaere K, Gasquet I, Haro JM, Katz SJ, Kessler RC, Kovess V, Lepine JP, Ormel J, Polidori G, Russo LJ, Vilagut G, Almansa J, Arbabzadeh-Bouchez S, Autonell J, Bernal M, Buist-Bouwman MA, Codony M, Domingo-Salvany A, Ferrer M, Joo SS, Martinez-Alonso M, Matschinger H, Mazzi F, Morgan Z, Morosini P, Palacin C, Romera B, Taub N, Vollebergh WA, ESEMeD/MHEDEA 2000 Investigators. European Study of the Epidemiology of Mental Disorders (ESEMeD) Project. Prevalence of mental disorders in Europe: Results from the European study of the epidemiology of mental disorders (ESEMeD) project. Acta Psychiatr Scand Suppl 2004;420:21–7.Search in Google Scholar
[5] Dunn AJ, Swiergiel AH, de Beaurepaire R. Cytokines as mediators of depression: what can we learn from animal studies? Neurosci Biobehav Rev 2005;29: 891–909.Search in Google Scholar
[6] Ovaskainen Y, Koponen H, Jokelainen J, Keinanen-Kiukaanniemi S, Kumpusalo E, Vanhala M. Depressive symptomatology is associated with decreased interleukin-1 beta and increased interleukin-1 receptor antagonist levels in males. Psychiatry Res 2009;167:73–9.Search in Google Scholar
[7] Meyer T, Stanske B, Kochen MM, Cordes A, Yuksel I, Wachter R, Luers C, Scherer M, Binder L, Pieske B, Herrmann-Lingen C. Serum levels of interleukin-6 and interleukin-10 in relation to depression scores in patients with cardiovascular riskfactors. Behav Med 2011;37:105–12.Search in Google Scholar
[8] Brown ES, Varghese FP, McEwen BS. Association of depression with medical illness: does cortisol play a role? Biol Psychiatry 2004;55:1–9.Search in Google Scholar
[9] Licht CM, Vreeburg SA, van Reedt Dortland AK, Giltay EJ, Hoogendijk WJ, DeRijk RH, Vogelzangs N, Zitman FG, de Geus EJ, Penninx BW. Increased sympathetic and decreased parasympathetic activity rather than changes in hypothalamic- pituitary-adrenal axis activity is associated with metabolic abnormalities. J Clin Endocrinol Metab 2010;95:2458–66.Search in Google Scholar
[10] Alexopoulos GS, Morimoto SS. The inflammation hypothesis ingeriatric depression. Int J Geriatr Psychiatry 2011;26:1109–18.Search in Google Scholar
[11] Vogelzangs N, Beekman AT, Boelhouwer IG, Bandinelli S, Milaneschi Y, Ferrucci L, Penninx BW. Metabolic depression: a chronic depressive subtype? Findings from the InCHIANTI study ofolder persons.J Clin Psychiatry 2011;72:598–604.Search in Google Scholar
[12] van Reedt Dortland AK, Vreeburg SA, Giltay EJ, Licht CM, Vogelzangs N, van Veen T, de Geus EJ, Penninx BW, Zitman FG. The impact of stress systems and lifestyle on dyslipidemia and obesity in anxiety and depression. Psychoneuroendocrinology 2013;38:209–18.Search in Google Scholar
[13] Linton SJ, Bergbom S. Understanding the link between depression and pain. Scand J Pain 2011;2:47–54.Search in Google Scholar
[14] Bair MJ, Robinson RL, Katon W, Kroenke K. Depression and pain comorbidity: a literature review. Arch Intern Med 2003;163:2433–45.Search in Google Scholar
[15] American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th ed. text revision Washington, DC: American Psychiatric Publishing; 2000.Search in Google Scholar
[16] Lamers F, de Jonge P, Nolen WA, Smit JH, Zitman FG, Beekman AT, Penninx BW. Identifying depressive subtypes in a large cohort study: results from the Netherlands study of depression and anxiety (NESDA). J Clin Psychiatry 2010;71:1582–9.Search in Google Scholar
[17] Lamers F, Burstein M, He JP, Avenevoli S, Angst J, Merikangas KR. Structure of major depressive disorder in adolescents and adults in the US general population. Br J Psychiatry 2012;201:143–50.Search in Google Scholar
[18] Fried EI, Nesse RM. Depression is not a consistent syndrome: an investigation of unique symptom patterns in the STAR*D study. J Affect Disord 2014;172C:96–102.Search in Google Scholar
[19] Stahl S, editor. Neuroscientific basis and practical applications. 3rd ed. Cambridge, UK: Cambridge University Press; 2007.Search in Google Scholar
[20] Järvimäki V, Juurikka L, Vakkala M, Kautiainen H, Haanpaa M. Results of lumbar spine surgery: a postal survey. Scand J Pain 2015;6:9–13.Search in Google Scholar
[21] Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Arch Gen Psychiatry 1961;4:561–71.Search in Google Scholar
[22] Beck A, Steer R. Manual of the beck depression inventory. San Antonio Texas: Psychology Corporation; 1988.Search in Google Scholar
[23] Viinamaki H, Tanskanen A, Honkalampi K, Koivumaa-Honkanen H, Haatainen K, Kaustio O, Hintikka J. Is the beck depression inventory suitable for screening major depression in different phases of the disease? Nord J Psychiatry 2004;58:49–53.Search in Google Scholar
[24] Steer RA, Ball R, Ranieri WF, Beck AT. Dimensions of the beck depression inventory-II in clinically depressed outpatients.J Clin Psychol 1999;55:117–28.Search in Google Scholar
[25] Vanhala M, Jokelainen J, Keinanen-Kiukaanniemi S, Kumpusalo E, Koponen H. Depressive symptoms predispose females to metabolic syndrome: a 7-year follow-up study. Acta Psychiatr Scand 2009;119:137–42.Search in Google Scholar
[26] Seppälä J, Vanhala M, Kautiainen H, Eriksson J, Kampman O, Mäntyselkä P, Oksa H, Ovaskainen Y, Viikki M, Koponen H. Prevalence ofmetabolic syndrome in subjects with melancholic and non-melancholic depressive symptoms. A Finnish population-based study. J Affect Disord 2012;136:543–9.Search in Google Scholar
[27] Fairbank JC, Couper J, Davies JB, O’Brien JP. The oswestry low back pain disability questionnaire. Physiotherapy 1980;66:271–3.Search in Google Scholar
[28] Fairbank JC, Pynsent PB. The oswestry disability index. Spine (Phila Pa 1976) 2000;25:2940–52. Discussion 2952.Search in Google Scholar
[29] Hagg O, Fritzell P, Ekselius L, Nordwall A. Swedish Lumbar Spine Study. Predictors of outcome in fusion surgery for chronic low back pain. A report from the Swedish lumbar spine study. Eur Spine J 2003;12:22–33.Search in Google Scholar
[30] LaCaille RA, DeBerard MS, Masters KS, Colledge AL, Bacon W. Presurgical biopsychosocial factors predict multidimensional patient: outcomes of inter body cage lumbar fusion.Spine J 2005;5:71–8.Search in Google Scholar
[31] Trief PM, Ploutz-Snyder R, Fredrickson BE. Emotional health predicts pain and function after fusion: a prospective multicenter study. Spine (Phila Pa 1976) 2006;31:823–30.Search in Google Scholar
[32] Sinikallio S, Aalto T, Airaksinen O, Lehto SM, Kroger H, Viinamaki H. Depression is associated with a poorer outcome of lumbar spinal stenosis surgery: a two- year prospective follow-up study. Spine (Phila Pa 1976) 2011;36:677–82.Search in Google Scholar
[33] Wahlman M, Hakkinen A, Dekker J, Marttinen I, Vihtonen K, Neva MH. The prevalence of depressive symptoms before and after surgery and its association with disability in patients undergoing lumbar spinal fusion. Eur Spine J 2014;23:129–34.Search in Google Scholar
[34] Low back pain (online). Current Care guideline. Working group set up by the Finnish Medical Society Duodecim and the Finnish Society of Physiatrists [Internet]; 2014.Available from:http://www.kaypahoito.fiSearch in Google Scholar
[35] Deyo RA, Von Korff M, Duhrkoop D. Opioids for low back pain. BMJ 2015;350:g6380.Search in Google Scholar
[36] Bernstein E, Carey TS, Garrett JM. The use of muscle relaxant medications in acute low back pain. Spine (Phila Pa 1976) 2004;29:1346–51.Search in Google Scholar
[37] Urquhart DM, Hoving JL, Assendelft WW, Roland M, van Tulder MW. Antide pressants for non-specific low back pain. Cochrane Database Syst Rev 2008. CD001703.Search in Google Scholar
[38] Stewart JW. Treating depression with atypical features. J Clin Psychiatry 2007;68:25–9.Search in Google Scholar
© 2016 Scandinavian Association for the Study of Pain
Articles in the same Issue
- Scandinavian Journal of Pain
- Editorial comment
- Depressive symptoms associated with poor outcome after lumbar spine surgery: Pain and depression impact on each other and aggravate the burden of the sufferer
- Clinical pain research
- Depressive symptoms are associated with poor outcome for lumbar spine surgery
- Editorial comment
- Chronic compartment syndrome is an under-recognized cause of leg-pain
- Observational study
- Prevalence of chronic compartment syndrome of the legs: Implications for clinical diagnostic criteria and therapy
- Editorial comment
- Genetic susceptibility to postherniotomy pain. The influence of polymorphisms in the Mu opioid receptor, TNF-α, GRIK3, GCH1, BDNF and CACNA2D2 genes
- Clinical pain research
- Genetic susceptibility to postherniotomy pain. The influence of polymorphisms in the Mu opioid receptor, TNF-α, GRIK3, GCH1, BDNF and CACNA2D2 genes
- Editorial comment
- Important development: Extended Acute Pain Service for patients at high risk of chronic pain after surgery
- Observational study
- New approach for treatment of prolonged postoperative pain: APS Out-Patient Clinic
- Editorial comment
- Working memory, optimism and pain: An elusive link
- Original experimental
- The effects of experimental pain and induced optimism on working memory task performance
- Editorial comment
- A surgical treatment for chronic neck pain after whiplash injury?
- Clinical pain research
- A small group Whiplash-Associated-Disorders (WAD) patients with central neck pain and movement induced stabbing pain, the painful segment determined by mechanical provocation: Fusion surgery was superior to multimodal rehabilitation in a randomized trial
- Editorial comment
- Social anxiety and pain-related fear impact each other and aggravate the burden of chronic pain patients: More individually tailored rehabilitation need
- Clinical pain research
- Characteristics and consequences of the co-occurrence between social anxiety and pain-related fear in chronic pain patients receiving multimodal pain rehabilitation treatment
- Editorial comment
- Transcranial magnetic stimulation, paravertebral muscles training, and postural control in chronic low back pain
- Original experimental
- Influence of paravertebral muscles training on brain plasticity and postural control in chronic low back pain
- Editorial comment
- Is there a place for pulsed radiofrequency in the treatment of chronic pain?
- Clinical pain research
- Pulsed radiofrequency in clinical practice – A retrospective analysis of 238 patients with chronic non-cancer pain treated at an academic tertiary pain centre
- Editorial comment
- More postoperative pain reported by women than by men – Again
- Observational study
- Females report higher postoperative pain scores than males after ankle surgery
- Editorial comment
- The relationship between pain and perceived stress in a population-based sample of adolescents – Is the relationship gender specific?
- Observational study
- Pain is prevalent among adolescents and equally related to stress across genders
- Editorial comment
- The Brief Pain Inventory (BPI) – Revisited and rejuvenated?
- Clinical pain research
- Confirmatory factor analysis of 2 versions of the Brief Pain Inventory in an ambulatory population indicates that sleep interference should be interpreted separately
- Editorial comment
- Pain research reported at the 40th scientific meeting of the Scandinavian Association for the Study of Pain in Reykjavik, Iceland May 26–27, 2016
- Abstracts
- Pain management strategies for effective coping with Sickle Cell Disease: The perspective of patients in Ghana
- Abstracts
- PEARL – Pain in early life. A new network for research and education
- Abstracts
- Searching for protein biomarkers in pain medicine – Mindless dredging or rational fishing?
- Abstracts
- Effectiveness of smart tablets as a distraction during needle insertion amongst children with port catheter: Pre-research with pre-post test design
- Abstracts
- Postoperative oxycodone in breast cancer surgery: What factors associate with analgesic plasma concentrations?
- Abstracts
- Sport participation and physical activity level in relation to musculoskeletal pain in a population-based sample of adolescents: The Young-HUNT Study
- Abstracts
- “Tears are also included” - women’s experience of treatment for painful endometriosis at a pain clinic
- Abstracts
- Predictors of long-term opioid use among chronic nonmalignant pain patients: A register-based national open cohort study
- Abstracts
- Coupled cell networks of astrocytes and chondrocytes are target cells of inflammation
- Abstracts
- Changes in opioid prescribing behaviour in Denmark, Sweden and Norway - 2006-2014
- Abstracts
- Opioid usage in Denmark, Norway and Sweden - 2006-2014 and regulatory factors in the society that might influence it
- Abstracts
- ADRB2, pain and opioids in mice and man
- Abstracts
- Retrospective analysis of pediatric patients with CRPS
- Abstracts
- Activation of epidermal growth factor receptors (EGFRs) following disc herniation induces hyperexcitability in the pain pathways
- Abstracts
- Pain rehabilitation with language interpreter, a multicenter development project
- Abstracts
- Trait-anxiety and pain intensity predict symptoms related to dysfunctional breathing (DB) in patients with chronic pain
- Abstracts
- Emla®-cream as pain relief during pneumococcal vaccination
- Abstracts
- Use of Complimentary/Alternative therapy for chronic pain
- Abstracts
- Effect of conditioned pain modulation on long-term potentiation-like pain amplification in humans
- Abstracts
- Biomarkers for neuropathic pain – Is the old alpha-1-antitrypsin any good?
- Abstracts
- Acute bilateral experimental neck pain: Reorganise axioscapular and trunk muscle activity during slow resisted arm movements
- Abstracts
- Mast cell proteases protect against histaminergic itch and attenuate tissue injury pain responses
- Abstracts
- The impact of opioid treatment on regional gastrointestinal transit
- Abstracts
- Genetic variation in P2RX7 and pain
- Abstracts
- Reversal of thermal and mechanical allodynia with pregabalin in a mouse model of oxaliplatin-induced peripheral neuropathy
- Clinical pain research
- Pain-related distress and clinical depression in chronic pain: A comparison between two measures
Articles in the same Issue
- Scandinavian Journal of Pain
- Editorial comment
- Depressive symptoms associated with poor outcome after lumbar spine surgery: Pain and depression impact on each other and aggravate the burden of the sufferer
- Clinical pain research
- Depressive symptoms are associated with poor outcome for lumbar spine surgery
- Editorial comment
- Chronic compartment syndrome is an under-recognized cause of leg-pain
- Observational study
- Prevalence of chronic compartment syndrome of the legs: Implications for clinical diagnostic criteria and therapy
- Editorial comment
- Genetic susceptibility to postherniotomy pain. The influence of polymorphisms in the Mu opioid receptor, TNF-α, GRIK3, GCH1, BDNF and CACNA2D2 genes
- Clinical pain research
- Genetic susceptibility to postherniotomy pain. The influence of polymorphisms in the Mu opioid receptor, TNF-α, GRIK3, GCH1, BDNF and CACNA2D2 genes
- Editorial comment
- Important development: Extended Acute Pain Service for patients at high risk of chronic pain after surgery
- Observational study
- New approach for treatment of prolonged postoperative pain: APS Out-Patient Clinic
- Editorial comment
- Working memory, optimism and pain: An elusive link
- Original experimental
- The effects of experimental pain and induced optimism on working memory task performance
- Editorial comment
- A surgical treatment for chronic neck pain after whiplash injury?
- Clinical pain research
- A small group Whiplash-Associated-Disorders (WAD) patients with central neck pain and movement induced stabbing pain, the painful segment determined by mechanical provocation: Fusion surgery was superior to multimodal rehabilitation in a randomized trial
- Editorial comment
- Social anxiety and pain-related fear impact each other and aggravate the burden of chronic pain patients: More individually tailored rehabilitation need
- Clinical pain research
- Characteristics and consequences of the co-occurrence between social anxiety and pain-related fear in chronic pain patients receiving multimodal pain rehabilitation treatment
- Editorial comment
- Transcranial magnetic stimulation, paravertebral muscles training, and postural control in chronic low back pain
- Original experimental
- Influence of paravertebral muscles training on brain plasticity and postural control in chronic low back pain
- Editorial comment
- Is there a place for pulsed radiofrequency in the treatment of chronic pain?
- Clinical pain research
- Pulsed radiofrequency in clinical practice – A retrospective analysis of 238 patients with chronic non-cancer pain treated at an academic tertiary pain centre
- Editorial comment
- More postoperative pain reported by women than by men – Again
- Observational study
- Females report higher postoperative pain scores than males after ankle surgery
- Editorial comment
- The relationship between pain and perceived stress in a population-based sample of adolescents – Is the relationship gender specific?
- Observational study
- Pain is prevalent among adolescents and equally related to stress across genders
- Editorial comment
- The Brief Pain Inventory (BPI) – Revisited and rejuvenated?
- Clinical pain research
- Confirmatory factor analysis of 2 versions of the Brief Pain Inventory in an ambulatory population indicates that sleep interference should be interpreted separately
- Editorial comment
- Pain research reported at the 40th scientific meeting of the Scandinavian Association for the Study of Pain in Reykjavik, Iceland May 26–27, 2016
- Abstracts
- Pain management strategies for effective coping with Sickle Cell Disease: The perspective of patients in Ghana
- Abstracts
- PEARL – Pain in early life. A new network for research and education
- Abstracts
- Searching for protein biomarkers in pain medicine – Mindless dredging or rational fishing?
- Abstracts
- Effectiveness of smart tablets as a distraction during needle insertion amongst children with port catheter: Pre-research with pre-post test design
- Abstracts
- Postoperative oxycodone in breast cancer surgery: What factors associate with analgesic plasma concentrations?
- Abstracts
- Sport participation and physical activity level in relation to musculoskeletal pain in a population-based sample of adolescents: The Young-HUNT Study
- Abstracts
- “Tears are also included” - women’s experience of treatment for painful endometriosis at a pain clinic
- Abstracts
- Predictors of long-term opioid use among chronic nonmalignant pain patients: A register-based national open cohort study
- Abstracts
- Coupled cell networks of astrocytes and chondrocytes are target cells of inflammation
- Abstracts
- Changes in opioid prescribing behaviour in Denmark, Sweden and Norway - 2006-2014
- Abstracts
- Opioid usage in Denmark, Norway and Sweden - 2006-2014 and regulatory factors in the society that might influence it
- Abstracts
- ADRB2, pain and opioids in mice and man
- Abstracts
- Retrospective analysis of pediatric patients with CRPS
- Abstracts
- Activation of epidermal growth factor receptors (EGFRs) following disc herniation induces hyperexcitability in the pain pathways
- Abstracts
- Pain rehabilitation with language interpreter, a multicenter development project
- Abstracts
- Trait-anxiety and pain intensity predict symptoms related to dysfunctional breathing (DB) in patients with chronic pain
- Abstracts
- Emla®-cream as pain relief during pneumococcal vaccination
- Abstracts
- Use of Complimentary/Alternative therapy for chronic pain
- Abstracts
- Effect of conditioned pain modulation on long-term potentiation-like pain amplification in humans
- Abstracts
- Biomarkers for neuropathic pain – Is the old alpha-1-antitrypsin any good?
- Abstracts
- Acute bilateral experimental neck pain: Reorganise axioscapular and trunk muscle activity during slow resisted arm movements
- Abstracts
- Mast cell proteases protect against histaminergic itch and attenuate tissue injury pain responses
- Abstracts
- The impact of opioid treatment on regional gastrointestinal transit
- Abstracts
- Genetic variation in P2RX7 and pain
- Abstracts
- Reversal of thermal and mechanical allodynia with pregabalin in a mouse model of oxaliplatin-induced peripheral neuropathy
- Clinical pain research
- Pain-related distress and clinical depression in chronic pain: A comparison between two measures

