Abstract
Context
Globally self-medication is an important public health problem, with prevalence ranging from 11.7 to 92 % worldwide and around 52 % in India. It is nevertheless common, particularly in developing nations like India, despite the possible hazards, including adverse drug reactions and the risk of drug resistance.
Objectives
This study estimates the prevalence of self-medication, examines associated factors and explores attitudes toward self-medication among young adults in Bengaluru.
Methods
Community-based cross-sectional study, conducted from August 1 to September 30, 2023, involved 453 young adults aged 18–22 in four Bengaluru colleges. Participants were selected using a multistage random sampling technique. Data were collected through a pre-tested, self-administered questionnaire covering socio-demographic details, self-medication practices, and attitudes. Data were analyzed using EpiData 3.1 analysis software. Chi-square, Fisher exact tests, and Binary logistic regression were used to identify significant predictors of self-medication.
Results
The prevalence of self-medication among young adults is found to be 93 % and it was influenced by factors such as age, gender, and education. Common reasons included time-saving (40 %) and possession of old prescriptions (35 %). The most frequently self-medicated conditions were headaches (61 %) and fever (55 %). Significant predictors of self-medication included age (20–22 years) with an adjusted odds ratio of 0.4 (95 % CI 0.1–0.8).
Conclusions
Self-medication practices were highly prevalent among young adults in urban Bengaluru, driven by factors such as convenience and cost-saving. There is a need for targeted health education and stricter enforcement of drug sale regulations to mitigate these risks.
Key messages
In Bengaluru, self-medication is very common among young individuals, driven by convenience and cost-saving.
The practice poses significant risks, including adverse effects and drug resistance.
There is an urgent need for targeted health education and stricter regulation of drug sales to mitigate these risks.
Introduction
With prevalences ranging from 11.7 to 92 % worldwide, self-medication is a significant public health issue [1]. Self-medication, according to the World Health Organisation (WHO), is the use of medications to treat illnesses or symptoms that one diagnoses or the intermittent or continuous use of prescribed medications for symptoms of a chronic or recurrent illness [1]. It is a crucial component of self-care, which includes self-treatment without drugs, first aid for common illnesses, using medication that has not been recommended by a doctor, and being encouraged by friends, elders, and other people. It also involves using medicines issued without a prescription, sharing medicines prescribed with friends or family without consultation with a registered doctor, buying medicines with old prescriptions, or using stored medicines at home for quick relief [2], 3]. Such over-the-counter drugs are designed to treat symptoms or sickness rather than to prevent or treat diseases which remains a well-known aspect of health care globally [4], 5].
The WHO Expert Committee on National Drug Policies in 1995 stated that “Self-medication is widely practiced in both developed and developing countries” [6]. In industrialised countries such as Switzerland, Australia, Germany, and the USA, the prevalence of self-medication is lower, at 8 %, 11%, 11%, and 13 %, respectively.
It is higher in developing nations like India, Nigeria, and, Pakistan [7]. As per the literature review (2015) in India around 52 % of people self-medicate [7]. One of the most common and preferred strategies employed by patients in underdeveloped countries where universal access to healthcare has not yet been established is self-medication. This is because it is a less expensive and time-consuming option for individuals who, for whatever reason, cannot afford clinical services. Negligent self-medication practices can lead to dangerous, unwarranted side effects such as allergic reactions, overdose poisoning, and potentially fatal drug interactions, as well as drug resistance and dependence. All of these factors add to the overall cost of seeking medical attention and the burden of morbidity [7].
People are influenced without doing their research in the modern age, when the internet offers “easy solutions” for any issue. Without a solid scientific foundation, some medications have been marketed as helpful, and some people may have fallen for it [8]. Inaccurate self-diagnosis, careless and inappropriate drug use, drug interactions, and the associated repercussions are all brought up by this [9]. Young adults are more susceptible to these adverse influences as they are in a phase where they develop a sense of being a legal adult. They start to recognize not as an extension of their parents but develop a sense of individuality, decision-making ability, and independence [10].
Although the Indian government discourages the sale of over-the-counter medications without a prescription, the practice is widespread in India because of the ease and unrestricted availability of medications over-the-counter without proper supervision. The health care utilization and problems related to young adults have not been addressed much and also during the ongoing COVID-19 pandemic, there is a likely chance that these numbers might have gone up [8]. In light of this, the current study was conducted to determine the incidence of self-medication among young adults and to search for a correlation between self-medication and sociodemographic traits. Another aspect of this study’s focus was the attitudes of young adults towards self-medication.
Subjects and methods
Study Design and setting: This community-based cross-sectional study was carried among the young adults studying in degree and diploma colleges of Bengaluru West between August 1, 2023, and September 30, 2023.
Young adults in the age group of 18–22 years, studying in degree and diploma colleges were included in the study. Young adults doing MBBS, pharmacy, and other health-related degrees with knowledge of medications were excluded from the study. Those who did not give consent and those who were not present on the day of the study were also excluded from the study.
Sample size: Considering the mean prevalence of self-medication practices in India to be 53.6 % as per the study conducted by Muhammed Rashid et al., [11] the minimum estimated sample size was calculated to be 347 using the formula 4p (1−p)/d2, where p is prevalence and d is precision with a desired confidence limit of 95 % and relative precision of 5 %. However, we included 453 study participants in our study.
The sampling method used in this study is multistage random sampling. All of the colleges that fall under Bengaluru West were included after receiving the Institutional Ethics Committee’s certification and approval. Sampling frame consists of the young adults studying in degree colleges of Bengaluru West.
Stage 1: Using a simple random sampling technique, four degree and diploma colleges were chosen from the list. Permission was obtained from the head of the college to conduct the study.
Stage 2: The total number of classes running various courses in each college was recorded. Assuming an average of 30 students per class, we decided to select 12 classes from these 4 colleges. The selection of classes was done using probability proportional to size, meaning that colleges with more courses had more classes chosen, while those with fewer courses had fewer classes selected.
All the students in the class were invited to participate in the study. Those who gave consent were finally included in the study. In each class, the study questionnaire was explained to the students beforehand so that they could answer correctly with the collaboration of class teachers. Each session took approximately twenty-five to 30 minutes as far as possible, and free time was used for the study so that routine classes remained unaffected. The required data was collected through the self-administration technique. Confidentiality of the information was maintained. In the end, Health education regarding self-medication practices was given after the study.
A pre-tested questionnaire comprising of detailed socio-demographic profile of participants’ age, gender, educational status, income of the family per month, and existing health conditions if any were collected. For participants acknowledging self-medication practices, details regarding factors influencing the practices and the types of drugs taken were taken. Attitude regarding self-medication was also assessed. The operational definition of self-medication was the use of over-the-counter drugs or any allopathic drug for self-treatment, without prior consultation with a certified allopathic doctor with a minimum MBBS degree [1].
The survey was piloted with 20 participants and face-validated with two subject-matter experts. All the questions were checked for internal consistency using Cronbach’s alpha. The study included the questions that were assigned a value that exceeded 0.7. The final questionnaire incorporated the validators’ suggestions.
Statistical Analysis: All the data were captured in a paper-based data collection format and then double-entered in Microsoft Excel. The data was analyzed using EpiData 3.1 analysis software. The magnitude was expressed in percentage along with its 95 % confidence interval (CI). Categorical variables were presented as proportions (%). The Chi-square and Fisher exact test were used to study the association. In bivariate analysis, chi-square values were calculated wherever appropriate and a p-value less than 0.05 was considered statistically significant. Binary logistic regression was also applied and an odds ratio with a 95 % confidence interval was calculated.
Throughout the study, all information collected was kept private, and participants were also given the assurance that their identities would not be revealed. The ICMR STS Program has granted approval for the investigation. Additionally, Institutional Review Board approval was acquired. Institutional Approval Number No. 532/L/11/12; date- 26/6/2023.
Results
Coming to the socio-demographic profile of the students, the majority around 40 % were 18 years of age and 51 % were female. Around 42 % were found to be studying in BCom. The majority around 95 % were Hindu and around 50 % were BPL card holders (Table 1).
Sociodemographic profile of the study participants. (n=453).
| Sl no | Variables | Categories | Frequency (percentage) n (%) |
|---|---|---|---|
| 1 | Age (in years) | 18 | 182 (40.2) |
| 19 | 111 (24.5) | ||
| 20 | 105 (23.2) | ||
| 21 | 32 (7.1) | ||
| 22 | 23 (5.1) | ||
| 2 | Gender | Male | 220 (48.6) |
| Female | 233 (51.4) | ||
| 3 | Education | BA | 31 (6.8) |
| BCom | 191 (42.2) | ||
| BSc | 17 (3.8) | ||
| BBA | 27 (6) | ||
| BE | 36 (7.9) | ||
| BCA | 40 (8.8) | ||
| BTech | 18 (4) | ||
| Diploma | 93 (20.5) | ||
| 4 | Religion | Hindu | 429 (94.7) |
| Muslims | 15 (3.3) | ||
| Christian | 8 (1.8) | ||
| Others | 1 (0.2) | ||
| 5 | Marital status | Married | 2 (0.4) |
| Unmarried | 451 (99.6) | ||
| 6 | BPL card holder | Yes | 229 (50.6) |
| No | 167 (36.9) | ||
| Don’t know | 57 (12.6) |
-
aBPL, Below poverty line.
The distribution of study participants according to self-medication practices. Around 70 % had a self-medication history in the past 6 months and the majority around 79 % followed the allopathic type of medicine when compared to ayurveda (18 %), homeopathy (7.6 %), and home remedies (5.5 %). The majority (42 %) of students took recommendations from trustworthy people while selecting drugs for self-medication and 45 % read instructions for medication usage (dosage, timing, duration of therapy) sometimes before using it. For more than half of the students (60 %) self-medication has worked most of the time and the majority of them (90 %) didn’t express side effects being experienced after taking self-medication. Among those who have experienced side effects around 41 % stopped taking medication. The majority of the students (57 %) didn’t prescribe self-medication to others and 76.2 % of parents/guardians were always informed about self-medication, irrespective of who prescribed self-medication (Table 2).
Distribution of study participants according to self-medication (SM) practices (n=421).
| Sl no | Variables | Categories | Frequency (percentage) n (%) |
|---|---|---|---|
| 1 | SM in the last 6 months | Yes | 317 (70) |
| No | 136 (30) | ||
| 2 | Type/form of medication taken (multiple response) | Allopathic | 333 (79.1) |
| Ayurveda | 76 (18) | ||
| Homeopathic | 32 (7.6) | ||
| Home remedies | 23 (5.5) | ||
| 3 | Factors considered while selecting drug (multiple response) | Price | 74 (17.6) |
| Brand | 167 (39.7) | ||
| Ayurvedic | 63 (15) | ||
| Homeopathic | 20 (4.8) | ||
| Recommendations from trustworthy people | 175 (41.6) | ||
| Past experience | 10 (2.4) | ||
| 4 | Source of information | Yes, always | 154 (34) |
| Yes, sometimes | 203 (44.8) | ||
| No, never | 64 (14.1) | ||
| NA | 32 (7.1) | ||
| 5 | Instruction was obtained from (n=357) | Came along with the drug | 88 (24.6) |
| Internet | 108 (30.3) | ||
| Books/newspaper/TV | 11 (3.1) | ||
| Family/friends | 199 (55.7) | ||
| 6 | Understood the instructions (n=357) | Fully understood | 71 (19.9) |
| Partially understood | 264 (73.9) | ||
| Not understood | 22 (6.2) | ||
| 7 | Self-medication has worked | Always | 54 (12.8) |
| Most of the times | 252 (59.9) | ||
| Worked half the times | 87 (20.7) | ||
| Barely works | 17 (4) | ||
| Never | 11 (2.6) | ||
| 8 | Side effects experienced after taking self-medication | Yes | 44 (10.5) |
| No | 377 (89.5) | ||
| If yes explain (n=44) | Sedation | 30 (68.2) | |
| Rash | 5 (11.4) | ||
| Stomach pain & loose stools | 7 (15.9) | ||
| Body pain | 2 (4.5) | ||
| 9 | Response to adverse events experienced after self-medication (n=44) | Private doctor | 16 (36.5) |
| Primary health care center | 7 (15.9) | ||
| Pharmacist | 4 (9.1) | ||
| Stop taking medication | 18 (40.9) | ||
| 10 | Self-medication for any chronic disease | Yes | 8 (1.9) |
| No | 413 (98.1) | ||
| If yes, disease and time period (n=8) | Allergic | 5 (62.5) | |
| Nonallergic | 3 (37.5) | ||
| Time: <1 year | 5 (62.5) | ||
| ≥1year | 3 (37.5) | ||
| 11 | Prescribed self-medication to others | Yes | 183 (43.5) |
| No | 238 (56.5) | ||
| 12 | If yes whom (n=183) (multiple response) | Friends | 155 (84.7) |
| Family | 83 (45.4) | ||
| Others | 2 (1.1) | ||
| 13 | Parents/guardians always informed about self-medication practices, irrespective of who prescribed it | Yes | 345 (76.2) |
| No | 76 (16.8) |
-
aSM, self-medication.
The majority of the students strongly agreed with the statements that caution must be taken before self-medication (45 %), and thorough information regarding the medicines must be known before self-medication (46 %). Agreed with the statements that self-medication is a part of self-care (53 %), it is acceptable to self-medication on the recommendation of a pharmacist/peers (52 %), self-medication is an acceptable practice for common ailments (49 %), a prescription-based medication will help minimizing side effects related to medicines (38 %), medical knowledge regarding the adverse events of self-medication will make me more cautious (43 %), information leaflet, if provided along with medications, must be read thoroughly before self-medication (49 %) and the neither agree nor disagree with the statements like self-medication should be avoided because of the unknown side-effects (36 %) and self-medication gives us confidence with respect to management of diseases (37 %) (Table 3).
Attitude among study participants towards Self-Medication. (n=453).
| Sl no | Variables | Categories | ||||
|---|---|---|---|---|---|---|
| Strongly agree | Agree | Neither agree nor disagree | Disagree | Strongly disagree | ||
| 1 | Self-medication is a part of self-care. | 121 (26.7) | 241 (53.2) | 60 (13.2) | 25 (5.5) | 6 (1.3) |
| 2 | It is acceptable to self-medicate on the recommendation of a pharmacist/peers. | 43 (9.5) | 238 (52.5) | 107 (23.6) | 47 (10.4) | 18 (4) |
| 3 | Self-medication is acceptable practice for common ailments. | 69 (15.2) | 221 (48.8) | 121 (26.7) | 40 (8.8) | 2 (0.4) |
| 4 | Caution must be taken before self-medicating. | 203 (44.8) | 180 (39.7) | 44 (9.7) | 24 (5.3) | 2 (0.4) |
| 5 | A prescription-based medication will help minimizing side effects related to medicines. | 121 (26.7) | 170 (37.5) | 104 (23) | 45 (9.9) | 13 (2.9) |
| 6 | Thorough information regarding the medicines must be known before self-medication. | 207 (45.7) | 188 (41.5) | 34 (7.5) | 21 (4.6) | 3 (0.7) |
| 7 | Medical knowledge regarding the adverse events of self-medication will make me more cautious. | 101 (22.3) | 196 (43.3) | 116 (25.6) | 36 (7.9) | 4 (0.9) |
| 8 | Information leaflet, if provided along with medications, must be read thoroughly before self-medication. | 136 (30) | 222 (49) | 72 (15.9) | 15 (3.3) | 8 (1.8) |
| 9 | Self-medication should be avoided because of the unknown side-effects. | 69 (15.2) | 148 (32.7) | 164 (36.2) | 51 (11.3) | 21 (4.6) |
| 10 | Self-medication gives us confidence with respect to management of diseases. | 55 (12.1) | 152 (33.6) | 168 (37.1) | 62 (13.7) | 16 (3.5) |
Table 4 shows the results of both bivariate analysis of self-medication and bivariate logistic regression. In bivariate analysis, higher odds were observed among students in the 20–22 years age group (2.9 [95 % CI 1.3–6]) which is found to be significant, and in bivariate logistic regression, only students in the 20–22 years age group (0.4 [95 % CI 0.1–0.8]) is found to be significant.
Association of self-medication with select variables among study participants. (n=453).
| Sl no | Variables | Categories | Self-medication | Or (95 % CI) | Adjusted OR (95 % CI) | |
|---|---|---|---|---|---|---|
| Yes (n=421) | No (n=32) | |||||
| 1 | Age (in years) | 18–19 | 280 (66.5) | 13 (40.6) | 1 | 1 |
| 20–22 | 141 (33.5) | 19 (59.4) | 2.9 (1.3–6)a | 0.4 (0.1–0.8)2 | ||
| 2 | Gender | Male | 202 (47.9) | 18 (56.3) | 1 | 1 |
| Female | 219 (52.1) | 14 (43.7) | 0.7 (0.3–1.4) | 1.4 (0.6–3) | ||
| 3 | Education | Degree | 331 (78.6) | 29 (90.6) | 1 | 1 |
| Diploma | 90 (21.4) | 3 (9.4) | 0.3 (0.1–1.2) | 1.8 (0.5–6.6) | ||
| 4 | Religion | Hindu | 389 (94.5) | 31 (96.9) | 1 | 1 |
| Muslim/Others | 23 (5.5) | 1 (3.1) | 0.5 (0.07–4.2) | 1.8 (0.2–14.1) | ||
| 5 | BPL card holder | Yes | 217 (51.5) | 12 (37.5) | 1 | 1 |
| No | 204 (48.5) | 20 (62.5) | 1.7 (0.8–3.7) | 0.5 (0.2–1.2) | ||
In Figure 1 majority around 93 % of students were found to be taking self-medication in the past.
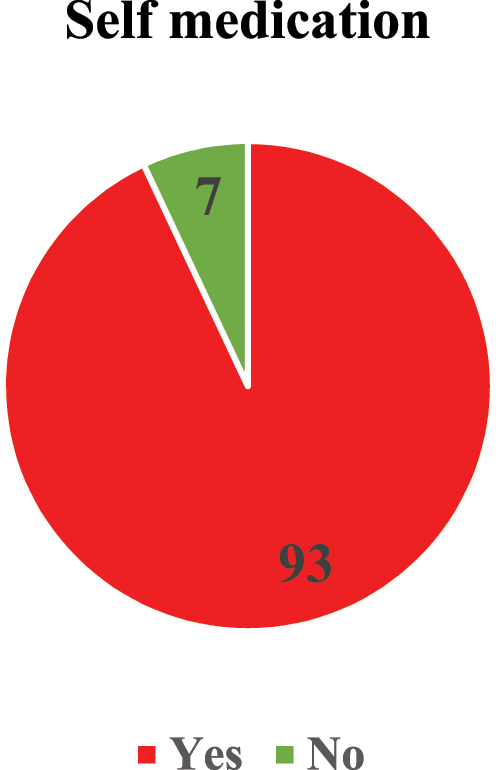
Distribution of study participants according to the self-medication practices. (n=453).
In Figure 2, the reason for self‐medication, 40 % stated to save time, 35 % had an old prescription, 33 % as they had medicines of family members, and around 23 % for high fees of the doctor.
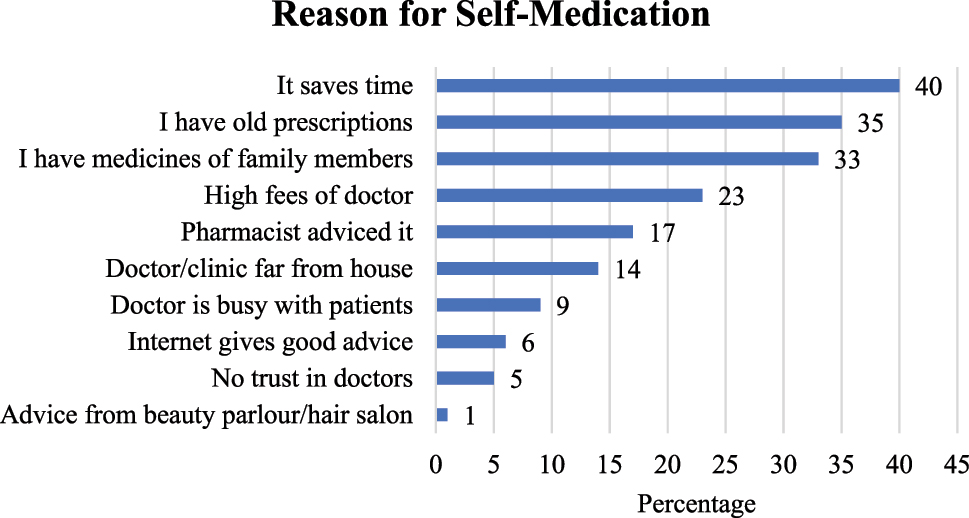
Distribution of study participants according to the reason for SM practices. (n=421).
In Figure 3, self-medication was practiced for the following symptoms or diseases Headache (61 %), Fever (55 %), Cough (46 %), Body pain (39 %), Vomiting (12 %), Hair fall (12 %), Dandruff (10 %), Acidity (10 %) and Throat infection (10 %).
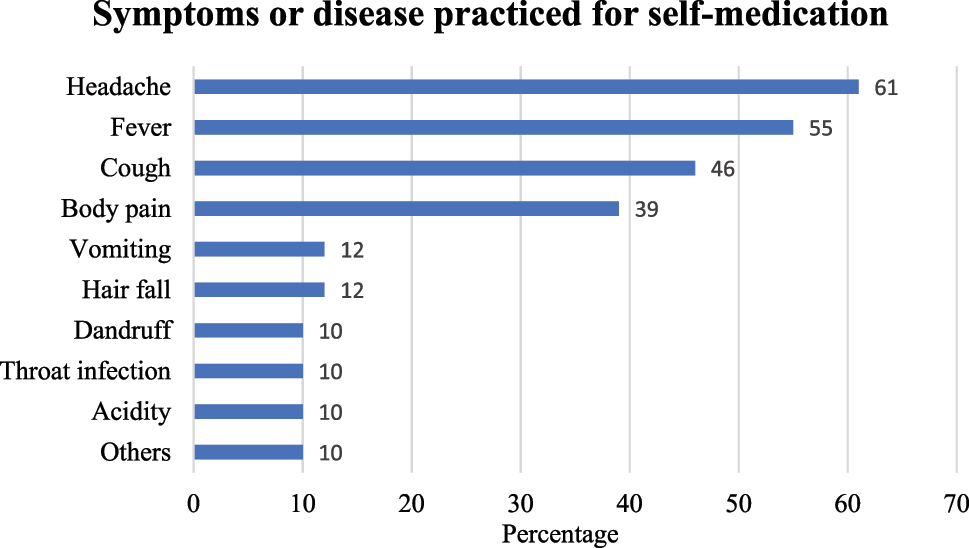
Distribution of study participants according to symptoms or disease practiced for SM. (n=421).
Discussion
The findings of this study show that among 453 young adults, 93 % were found to be practicing self-medication. Similarly, in a study from Delhi, 92.8 % of the participants were reported of practicing self-medication [12]. A study from Telangana found the proportion of self-medicating among respondents to be 73 %, in Rajasthan it is found to be 73.8 %, in a Maharashtra-based study it is found to be 68 %, in Andhra Pradesh it is found to be 68.1 %, whereas another study from Karnataka noted this number to be low as 40.5 % [13]. The use of various definitions of self-medication, variances in the ways that people seek health care, societal factors, and the seasonality of illnesses could all contribute to the variety in prevalence shown within the countries.
In our study among those who are practicing Self-medication around 48 % of them were male and 52 % were females. In another study 173 (78.6 %) adolescents were found to be practicing self-medication; out of which, 123 (55.9 %) of them were females and 147 (66.8 %) were males [14]. The prevalence among females is seen more than the males. Social variables and gender norms might also be important since women might be more proactive in seeking self-medication relief and more at ease talking about and addressing health issues, even minor illnesses. Women may also be more accustomed to taking care of their health because of their possible roles as the family’s primary carers, which makes them more likely to engage in self-care activities.
In our study, the prevalence is seen to be high with the majority of its participants practicing self-medication where around 37 % stated the reason that it saves time. Along similar lines, a study from Hyderabad noted that 42 % of the participants found self-medication to be a time-saving option [15]. Another study, by Keshari S et al. [16] reported the chief reason for self-medication to be “time-saving”. Another study indicates that the majority of its participants (57.7 %) self-medicate, and that the most often stated reason by these participants (34.7 %) was that they did not feel the need to see a certified medical professional before taking pharmaceuticals [7]. Visiting healthcare personnel is often time-consuming and adds to the financial burden of a family, which forces them to choose a quick fix to treat family members’ ailments in a way that saves money and time. Also, stocks of medicine at home make self-medication a more viable option [17].
Friends were the primary sources of information for the respondents in this study regarding the medication selection for self-medication. Similar to a study where pharmacists and family members played a role [1]. This may be because people often heed the counsel of those closest to them when it comes to matters of health and illness.
In our study, the most common symptom for which self-medication was practiced was headache, followed by fever and cough. In a similar study where fever was the commonest morbidity, followed by cough-cold for which the participants self-medicated (27.6 and 24.5 %, respectively) [15], 18]. Fever and headache were the most common, as reported by studies from Rajasthan and Andhra Pradesh [13], 18]. Fevers and headaches are often seen as minor ailments that can be easily managed with over-the-counter medications, one may feel comfortable using them based on past experiences without serious consequences or recommendations from others.
Conclusions
The present study revealed that self-medication was quite prevalent. It was observed that the female gender was associated with an increased likelihood of consuming medicines without a prescription from a medical practitioner. Furthermore, it was shown that a college education did not prevent persons from developing the dangerous habit of self-medication; rather, it played a significant role in it. The current study’s subjects had self-medicated for mild symptoms including headaches and fever. However, even for relatively minor ailments, self-medication can be dangerous and occasionally result in fatal complications.
Recommendations
Self-medication is likely to be impacted by health education and activities meant to alter people’s perceptions of the affordability and accessibility of medical facilities. The public needs to be alerted about antibiotic resistance and serious medication side effects by the media, using its power. Enforcement of drug laws must be strengthened, and strict sales control is crucial. Because most young people watch commercials on the internet and in other mass media, it is crucial to outlaw the advertising and sales of medications without a prescription.
Limitations
The study’s cross-sectional design prevents the inference of causal relationships and limits the generalizability of the findings. The present study used a six-month recall period, which might have led to a recall bias. Efforts were made to minimize this bias by using a well-designed, simple, and easy-to-understand questionnaire.
Funding source: Indian Council of Medical Research
Acknowledgments
We are grateful to the Indian Council of Medical Research (ICMR) for giving financial support to this project. We are thankful to all study participants for cooperating well and providing the required information.
-
Research ethics: Clearance and approval from the Institutional Ethics Committee taken.
-
Informed consent: The authors certify that they have obtained all appropriate participant consent forms. In the form, the participant(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The participants understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
-
Author contributions: All the authors have equally contributed to the manuscript.
-
Use of Large Language Models, AI and Machine Learning Tools: None declared.
-
Conflict of interest: Authors declare no conflict of interest.
-
Research funding: Indian Council of Medical Research (ICMR) STS grants for the year 2023.
-
Data availability: On request.
References
1. Rathod, P, Sharma, S, Ukey, U, Sonpimpale, B, Ughade, S, Narlawar, U, et al.. Prevalence, pattern, and reasons for self-medication: a community-based cross-sectional study from central India. Cureus 2023;15:e33917. https://doi.org/10.7759/cureus.33917.Suche in Google Scholar PubMed PubMed Central
2. Kumar, N, Kanchan, T, Unnikrishnan, B, Rekha, T, Mithra, P, Kulkarni, V, et al.. Perceptions and practices of self-medication among medical students in coastal south India. PLoS One 2013;8:e72247. https://doi.org/10.1371/journal.pone.0072247.Suche in Google Scholar PubMed PubMed Central
3. Loyola Filho, AI, Lima-Costa, MF, Uchôa, E. Bambuí Project: a qualitative approach to self-medication. Cad Saude Publica 2004;20:1661–9.10.1590/S0102-311X2004000600025Suche in Google Scholar
4. Bennadi, D. Self-medication: a current challenge. J Basic Clin Pharm 2014;5:19. https://doi.org/10.4103/0976-0105.128253.Suche in Google Scholar PubMed PubMed Central
5. Hughes, CM, McElnay, JC, Fleming, GF. Benefits and risks of self medication. Drug Saf 2001;24:1027–37. https://doi.org/10.2165/00002018-200124140-00002.Suche in Google Scholar PubMed
6. World Health Organization, Regional Office for South-East Asia. National drug policy 2005: Bangladesh [Internet]. New Delhi: WHO SEARO; 2005 [cited 2025 May 27]. Available from: https://www.who.int/docs/default-source/s earo/hsd/edm/nmp-ban-2005-goweb-ok.pdf Suche in Google Scholar
7. Gupta, S, Chakraborty, A. Pattern and practice of self medication among adults in an urban community of West Bengal. J Family Med Prim Care 2022;11:1858. https://doi.org/10.4103/jfmpc.jfmpc-1823-20.Suche in Google Scholar
8. Patil, AD, Sharma, H, Tetarbe, T. COVID-19 and concerns related to self-medication. Int J Basic Clin Pharmacol 2020;9:1475. https://doi.org/10.18203/2319-2003.ijbcp20203638.Suche in Google Scholar
9. Burak, LJ, Damico, A. College students’ use of widely advertised medications. J Am Coll Health 2000;49:118–21. https://doi.org/10.1080/07448480009596293.Suche in Google Scholar PubMed
10. Bonnie, RJ, Stroud, C, Breiner, H. Committee on improving the health, safety, and well-being of young adults. US: National Academies Press (US); 2015.Suche in Google Scholar
11. Rashid, M, Chhabra, M, Kashyap, A, Undela, K, Gudi, SK. Prevalence and predictors of self-medication practices in India: a systematic literature review and meta-analysis. Curr Clin Pharmacol 2020;15:90–101. https://doi.org/10.2174/1574884714666191122103953.Suche in Google Scholar PubMed PubMed Central
12. Kumar, V, Mangal, A, Yadav, G, Raut, D, Singh, S. Prevalence and pattern of self-medication practices in an urban area of Delhi, India. Med J DY Patil Univ 2015;8:16–20. https://doi.org/10.4103/0975-2870.148828.Suche in Google Scholar
13. Rangari, GM, Bhaisare, RG, Korukonda, V, Chaitanya, YL, Hanumanth, N. Prevalence of self-medication in rural area of Andhra Pradesh. J Family Med Prim Care 2020;9:2891–9. https://doi.org/10.4103/jfmpc.jfmpc-204-20.Suche in Google Scholar
14. Mathias, EG, D’souza, A, Prabhu, S. Self-medication practices among the adolescent population of south Karnataka, India. J Environ Public Health 2020:90–21819. https://doi.org/10.1155/2020/9021819.Suche in Google Scholar PubMed PubMed Central
15. Katkuri, S, Chauhan, P, Shridevi, K, Kokiwar, P, Gaiki, V. Prevalence of self-medication practices among urban slum dwellers in Hyderabad, India. Int J Community Med Public Health 2016;3:1816–9. https://doi.org/10.18203/2394-6040.ijcmph20162048.Suche in Google Scholar
16. Keshari, SS, Kesarwani, P, Sengar, MM. Prevalence and pattern of self-medication practices in rural area of Barabanki. Indian J Med Res 2014;25:636–9.Suche in Google Scholar
17. Chakravarthy, SA, Maiya, GR. Prevalence of self-medication and its associated factors among students of an engineering college in Chennai. J Family Med Prim Care 2021;10:1204–8. https://doi.org/10.4103/jfmpc.jfmpc-1654-20.Suche in Google Scholar
18. Jain, M, Prakash, R, Bapna, D, Jain, R. Prevalence and pattern of self-medication practices in Urban area of Southern Rajasthan. Ntl J of Community Med 2015;6:474–7.Suche in Google Scholar
© 2025 the author(s), published by De Gruyter, Berlin/Boston
This work is licensed under the Creative Commons Attribution 4.0 International License.
Artikel in diesem Heft
- Frontmatter
- Review
- Effects of anti-obesity drugs on cardiometabolic risk factors in pediatric population with obesity: a systematic review and meta-analysis of randomized controlled trials
- Physical Activity, Sleep, and Lifestyle Behaviours
- Prevalence of risk factors for non-communicable diseases and its association with hypertension among young adults in urban Meghalaya: a cross sectional study
- Mental Health and Well-being
- Psychosocial predictors of adolescent stress: insights from a school-going cohort
- Chronic Illness and Transition to Adult Care
- Barriers and facilitators in the transition from pediatric to adult care in people with cystic fibrosis in Europe – a qualitative systematized review
- Substance Use and Risk Behaviours
- Self-care or self-risk? examining self-medication behaviors and influencing factors among young adults in Bengaluru
- Health Equity and Access to Care
- Clinical heterogeneity of adolescents referred to paediatric palliative care; a quantitative observational study
- Adolescent Rights, Participation, and Health Advocacy
- ‘We need transparency and communication to build trust’: exploring access to primary care services for young adults through community-based youth participatory action research and group concept mapping
Artikel in diesem Heft
- Frontmatter
- Review
- Effects of anti-obesity drugs on cardiometabolic risk factors in pediatric population with obesity: a systematic review and meta-analysis of randomized controlled trials
- Physical Activity, Sleep, and Lifestyle Behaviours
- Prevalence of risk factors for non-communicable diseases and its association with hypertension among young adults in urban Meghalaya: a cross sectional study
- Mental Health and Well-being
- Psychosocial predictors of adolescent stress: insights from a school-going cohort
- Chronic Illness and Transition to Adult Care
- Barriers and facilitators in the transition from pediatric to adult care in people with cystic fibrosis in Europe – a qualitative systematized review
- Substance Use and Risk Behaviours
- Self-care or self-risk? examining self-medication behaviors and influencing factors among young adults in Bengaluru
- Health Equity and Access to Care
- Clinical heterogeneity of adolescents referred to paediatric palliative care; a quantitative observational study
- Adolescent Rights, Participation, and Health Advocacy
- ‘We need transparency and communication to build trust’: exploring access to primary care services for young adults through community-based youth participatory action research and group concept mapping

