Abstract
Introduction
Brain fog is an experiential phenomenon, often described by persons with chronic pain. The term “brain fog” emerged from discussions among persons with lived experiences (PWLE) and clinicians. Despite several patient-guided sources describing the profound impact of this experience, its legitimacy remains debated in the medical literature.
Methods
To explore the public understanding of this phenomenon, we performed a concept analysis of text-based postings on two popular social media platforms. Results were examined using descriptive content analysis.
Findings
A total of 247 social media posts were identified. Posts were primarily written by PWLE. Brain fog was described as a fluctuating experience, with some participants feeling cloudiness, mental heaviness, or dissociation. The antecedents of brain fog could be attributed to pain, cognitive overload, environmental factors, or random occurrences. Brain fog could cause cognitive (e.g., thinking and remembering) and bodily (e.g., exhaustion and emotional challenges) impacts that affect meaningful participation and perception of self. Challenges to managing symptoms included not knowing where to start, misleading information, or not feeling comfortable discussing brain fog with others.
Conclusion
The results of this study demonstrate the (1) impacts of brain fog on the well-being and perception of self in PWLE and (2) importance of bridging a possible disconnect between clinicians and PWLE of chronic pain.
1 Introduction
1.1 Overview
“Brain fog” is the term used for an experiential phenomenon, emerging from discourses of persons with lived experience (PWLE) [1] trying to communicate their symptoms to others. It is commonly experienced by persons with chronic pain and is identified by feelings of mental cloudiness, creating difficulties in thinking, remembering, and concentrating, impeding participation in daily activities [2,3]. Despite several patient-guided sources describing the profound impact of this experience [4,5,6], its legitimacy remains debated in the medical literature [2]. To better understand the public understanding of this phenomenon, we performed a concept analysis of text-based postings on Twitter and Facebook.
1.2 Brain fog in chronic pain
Brain fog is described as a significant challenge in the daily lives of people with chronic pain; however, there is limited research on how brain fog can be most effectively managed [2,3,7]. In chronic pain, brain fog can produce cognitive and emotional impacts, hindering an individual’s participation in their everyday activities and self-management of their health [2,8].
Mechanisms of brain fog are typically attributed to oxidative stress in conditions like long COVID [9] or hormonal imbalances in persons with menopause [7]. One scoping review stated that brain fog in chronic pain may be attributed to continuous pain processing, mental health challenges, and environmental changes (e.g., stress and lack of sleep) (removed for anonymization) Other studies have argued that the mechanisms of brain fog may be attributed to pre-existing conditions and that use of the term may contribute to potential confusion in understanding patient experiences and appropriate approaches to management [10]. Qualitative research exploring the experiences of brain fog and its key features can support in resolving this lack of clarity and better understanding of patients’ needs.
Existing qualitative studies exploring brain fog in painful populations have described brain fog as a general cognitive slowness, creating challenges with completing daily tasks (e.g., grocery shopping and word finding [11,12]. Similar findings have been found in qualitative studies of other populations. Issues with communicating and word finding may also cause individuals to self-isolate due to embarrassment or not knowing how to explain their symptoms [8,13], which is particularly problematic for persons with chronic pain who are likely to self-isolate [14]. Brain fog may also create strains on families, with spouses or children having to take on a caregiver role or bear additional responsibilities [8,13,15]. Additionally, brain fog is an invisible experience, which is often highly stigmatized and difficulty for people to understand [13]. This may make it challenging for people to explain brain fog to their employers to receive accommodations at work, which may lead to individuals being overlooked for promotions or completely withdrawing from their employment [16]. The stigma associated with brain fog may also make it harder for PWLE to confide in their healthcare professionals, out of fear that they will not be taken seriously [8,13,15]. Individuals may also feel discouraged and believe that there is nothing they can do to manage brain fog [15]. Overall, these challenges can negatively impact how one views themself and potentially discourage efforts for symptom management [13,15].
Currently, there are several patient-driven sources providing potential management strategies for brain fog [5,6]; however, there are few rigorous studies evaluating the effectiveness of potential management strategies. Some possible suggestions from the literature include physical activity, anti-inflammatory diets, or cognitive training [17]. In long COVID, a multidisciplinary approach, including reducing inflammation and managing mental health symptoms, may be helpful [18]. For chronic pain, brain fog may also hinder participation in strategies to manage pain, as they are typically education-focused and require substantive concentration [8,19]. Another stigmatizing aspect of brain fog is produced if PWLE forget to take their medications or go to appointments [8], which could be further mis-interpreted as non-compliance. Overall, there are currently no well-tested interventions for the management of brain fog. Ultimately, this may result in people with brain fog being left on their own to self-educate and self-manage their symptoms and experiences.
Social media is a powerful tool that people with chronic pain often leverage to self-educate and manage their pain [20,21]. PWLE may use social media to seek information from others to identify management strategies or better understand their condition [21,22,23]. This may also include learning how to self-advocate [24]. Further, PWLE use social media to share their personal experiences and maintain social connections with those with similar experiences [25,26,27,28]. Individuals may be more comfortable utilizing social media to advance or convey their beliefs about a particular construct in a free and unconstrained manner or to share opinions and insights that they would not feel comfortable sharing with a healthcare provider [20,25,27,28]. Therefore, using social media content as data allow a unique opportunity for researchers to explore and critically analyze different phenomena, potentially capturing beliefs that are not shared in traditional health and/or academic settings. Raw accounts of lived experience, as may be found in social media posts, can help researchers develop an understanding of a phenomenon and identify potential strategies to support with PWLE [22,23].
1.3 Objectives
The overarching objective of this study was to explore how chronic pain-related brain fog is described in the public forum of social media. Our specific research question was: what attributes, antecedents, symptoms, and management strategies for chronic pain-related brain fog are described in public discourses on social media?
2 Methods
The full methods have been previously published in our protocol in PLoS One’s Journal of Digital Health. A summarized version is provided below. The methods are guided by the Standards for Reporting Qualitative Research Guideline [29].
2.1 Reflexivity
RD is a joint PhD and occupational therapy student, focused on researching chronic pain and brain fog in Veterans. ACA is an undergraduate student, novel to this area. TP is an occupational therapist and faculty member with decades of experience in pain research and care.
2.2 Search strategy
Text-based social media posts on Twitter and Facebook were searched using hashtags and keywords regarding brain fog and chronic pain (see Appendix A for search strategy). An initial search of social media databases was performed to select relevant key terms and the appropriate databases. The search was run by the primary researcher (RD) using a social media account created solely for this project, with no affiliations to any groups or communities [30]. All searches were conducted on the week of September 24, 2023. All searched posts were downloaded into a Microsoft Excel™ spreadsheet for screening.
2.3 Eligibility criteria
The inclusion criteria for this study were identified posts (1) discussing brain fog in adults with a painful chronic condition (e.g., chronic pain, chronic musculoskeletal pain), (2) explicitly referring to chronic pain in the actual posts, profile, and/or adjacent thread, (3) posted by a public account, and (4) written in English. Posts were excluded if they were related to brain fog of a condition other than chronic pain (e.g., long COVID) or if they focused on children, as the perception of brain fog may differ in these groups. Commercial posts were excluded as we were focused on understanding the experience, rather than advertisements. Next, posts in languages other than English or those that were image-based were excluded as we did not have the capacity to meaningfully analyze them. Sources from closed community support groups were excluded as these are private spaces [30]. Lastly, retweets or reposts and duplicated posts were excluded.
2.4 Data generation tool
All posts that met the eligibility criteria were saved into an Excel sheet to facilitate data generation, stored on a password-protected device. Data generation was grounded in the two frameworks: (a) the Internet Specific Ethical Questions Framework to protect data anonymity [30] and (b) (removed for anonymization) 2023 model of brain fog derived from the medical literature to guide extraction. The form was piloted using the first ten posts, and no modifications were made. Data extraction was completed manually by two independent researchers (RD and ACA).
2.5 Data processing and analysis
Data were analyzed using descriptive content analysis methods to conduct a concept analysis: this was supported by using the qualitative software Quirkos™ [31]. Representative quotes were captured for analysis, but synthetic quotes are presented in the results to maintain anonymity [30]. Synthetic quotes were written by the authors by reorganizing sentence structure, using synonyms, and combining similar quotes [30].
The concept analysis was guided by Foley and Davis’ 2017 guide to concept analysis [32], identifying attributes, antecedents, symptoms, and management strategies.
All changes in the codebook were captured in the audit trail and were confirmed in discussion among all researchers. All coding was completed by two independent researchers, who kept a record of segment memos (RD and ACA).
2.6 Strategies for trustworthiness
Strategies for trustworthiness, recommended by Lincoln and Guba, were applied throughout this study [33]. Analytical steps were recorded in an audit trail, and peer examination occurred through discussions with the research team to promote credibility [33]. In-depth details of the study procedure are provided for dependability [33].
-
Ethical statement: We received a waiver of ethics from the Hamilton Integrated Research Ethics Board, which determined that data from social media did not require a full ethics application. To account for data anonymity, we followed recommendations from the Internet Specific Ethical Questions Framework to protect data anonymity [30].
3 Results
3.1 Sample characteristics
After screening, 1,566 results were identified, with 274 posts included for final extraction; screening is represented in the PRISMA diagram (Figure 1). Most posts were about unspecified chronic pain or multiple pain conditions (general chronic pain n = 229, fibromyalgia n = 99, complex regional pain syndrome n = 4) and were primarily written by PWLE (PWLE n = 240, organization n = 32, researcher n = 14, and clinicians n = 1).
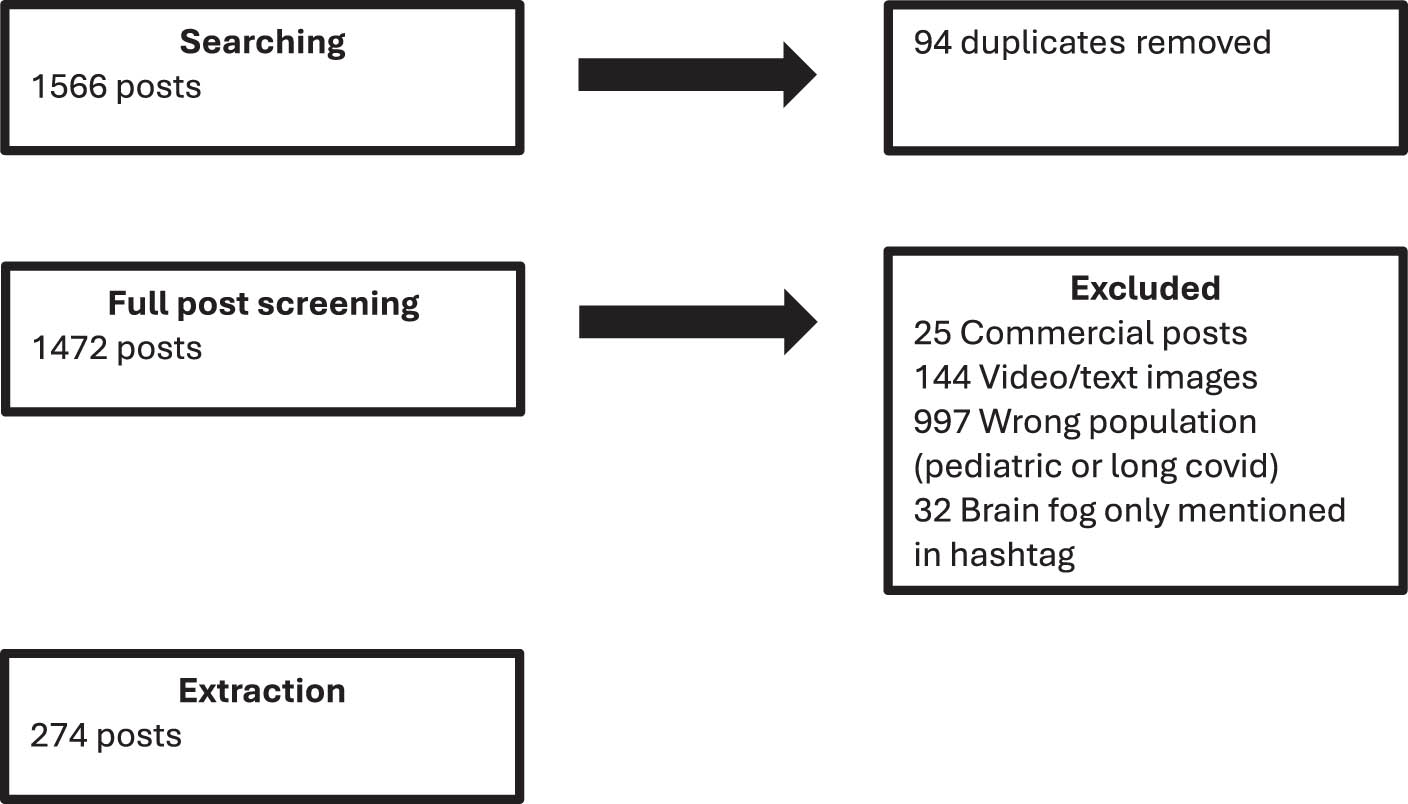
PRISMA diagram.
3.1.1 What are the attributes of brain fog?
A total of 147 posts described attributes of brain fog. In most cases, brain fog was described as a feeling of cloudiness and slowness, like having a permanent buffering image in your mind. Next, brain fog was discussed as a feeling of heaviness, “like trying to get through a field of melted marshmallows” (synthetic quote). Brain fog was also described as a dissociative experience: “I feel like an outsider in my own body” (synthetic quote). A visual depiction of the three experiences is presented in Figure 2. In all experiences, brain fog was described to take a toll on one’s mental capacity and energy, often leading to feelings of frustration and embarrassment: “my brain isn’t what it used to be- it’s hard to be around other people” (synthetic quote).
Illustration of attributes of brain fog. This is a visual representation of the descriptions of brain fog identified in the data. Source: Created by authors.
3.1.2 What are the antecedents of brain fog?
Antecedents of brain fog were discussed in 86 posts. The most described antecedents were painful symptoms and flare ups: “I think brain fog is a natural part of pain and its messages with the brain” (synthetic quote). Constant pain signaling was discussed as a distractor, taking away attention and consuming mental capacity. On a related note, many individuals attributed the emotional processing associated with mental health concerns and stress to brain fog: “my brain fog might be more because of my trauma than pain, but they are both related” (synthetic quote). One person suggested that this relationship could occur due to decreased serotonin levels, creating challenges with learning. Inflammation or reduced cerebral blood flow due to increased cytokine release, attributed to being the result of pain, poor diets, or mental health concerns, was also thought to affect cognition: “nobody knows how important gut health is- a lack of vitamins can really affect your body” (synthetic quote). Brain fog was believed to occur most often in distracting environments or instances of cognitive overload (e.g., multitasking). Some factors had conflicting reports about their influences. For example, some persons stated medications could worsen the symptoms of brain fog: “the gabapentin fog is real” (synthetic quote), while others declared that medications could relieve pain to help regain control over their thinking: “I think so much better without the pain” (synthetic quote). A lack of sleep was reported to trigger brain fog, while others believed that adequate sleep was not sufficient to relieve symptoms. Lastly, 10 individuals characterized brain fog as a fluctuating experience that could not be linked to any antecedents: “I don’t know why it starts or how I can stop it” (synthetic quote).
3.1.3 What are the symptoms of brain fog?
Along with the subjective attributable feelings of experiencing brain fog, brain fog was described to impact daily activities and bodily functions in 153 posts. Many activities affected by brain fog were attributed to cognition. In descending order, deficits in remembering, word finding, paying attention, thinking, comprehension, multitasking, and planning were reported. Brain fog reportedly interacts with body functions by causing physical exhaustion, difficulties with sleeping, and magnifying emotional challenges such as anxiety and depression. Cumulatively, the effects of brain fog were reported to impact one’s participation and perception of self.
The impacts of brain fog on activities and body functions affected meaningful participation. Brain fog could get in the way of everyday activities like grocery shopping, remembering birthdays and gifts, paying bills, playing games, reading, and virtually any activity requiring attention, thinking, and remembering: “simple tasks are harder, I put the milk in the pantry instead of the fridge” (synthetic quote). Brain fog’s limitations with participation became particularly problematic when it affected an individual’s livelihood, health, and overall well-being: I can’t do the things I was good at anymore and I feel like I’m not contributing to the team (synthetic quote). Individuals noted that brain fog specifically interfered with their tasks at work in a variety of ways: (a) restricting their ability to pay attention in meetings, (b) reducing their capacity to contribute new ideas and become involved with projects, and (c) making it more difficult to read materials, remember their tasks, or adhere to timelines.
I used to be known for my ideas and quality of work. Now, it can take an entire workday just to get my thoughts in order (synthetic quote).
Next, the fluctuating nature of brain fog and its effects on remembering led to issues with symptom management. Individuals described difficulties with monitoring their symptoms, remembering to take their medications or go to doctors’ appointments, and describing their experiences to their healthcare workers: “I can’t remember if I took meds or to bring it up to my doctor” (synthetic quote). Lastly, brain fog could affect overall well-being by creating challenges with social engagement and communication. Individuals described having trouble expressing themselves, finding the appropriate words, or paying attention during conversations. As a result of these challenges, individuals reported being too nervous, frustrated, or embarrassed to initiate or engage in conversations.
I spend most of my time by myself because I’m too scared to talk to “normal” people. I never know if my brain will freeze or if I’ll be able to communicate what I want to say (synthetic quote).
The symptoms of brain fog on daily activities, body function, and participation influence how individuals are perceived by themselves and those in their environment. Difficulty with cognitive tasks, feelings of anxiety, and exhaustion hinder engagement with daily tasks. These tasks may have been previously taken for granted and can lead to a diminished sense of self.
When I have brain fog, it feels like a part of me is stolen and will never return. I used to be so smart and now I feel so stupid (synthetic quote).
One’s perception of self can also be influenced by treatment by others. Individuals described feeling misunderstood or having their experiences doubted by those around them. Reductions in one’s sense of self can hinder social engagement and make it more challenging to seek out management strategies.
How am I supposed to explain brain fog to people? No one understand what it is like unless they experience it. They just look at me and laugh (synthetic quote).
3.1.4 What are the management strategies used by PWLE or suggested by others?
Strategies to relieve brain fog were described in 43 posts. Managing physical and mental health was the most common strategy described to relieve symptoms of brain fog. Painful symptoms were the most common antecedent of brain fog, and in direct response, managing pain was described to reduce brain fog. Pain was managed using non-pharmacological treatments, such as acupuncture, pacing, journaling for symptom tracking, and mental health counselling: “managing my symptoms and taking time to rest helps me work better” (synthetic quote). Pharmacological management strategies were controversially discussed; both increasing and decreasing the number and dosage of medications were described to reduce brain fog: “my meds are the only things that help me get on with my day” (synthetic quote). In one discourse, increasing medication (e.g., cannabis and Lyrica) reduced pain, which reduced brain fog. A contrasting discourse posited that lowering medication doses decreased the side effects inherently associated with these medications, including brain fog. Moreover, general health-promoting behaviors, including sufficient sleep, regular exercise, and a well-balanced diet, were described to reduce inflammation and the associated brain fog: “I try to keep my favorite anti-inflammatory snacks around and keep moving” (synthetic quote).
The remainder of the management strategies described were targeted toward increasing participation and social support. To support cognitive activities, individuals recommended calendar reminders and journals. Participation could also be supported by positive coping strategies, including humor and optimistic outlooks, which subsided the emotional challenges of brain fog: “sometimes it’s best to just laugh about it” (synthetic quote). Next, having reliable persons in their social network who understand the limitations of brain fog was described to reduce cognitive load and the emotional challenges of brain fog: “my family loves and accepts me, we have an understanding that sometimes my brain just can’t English” (synthetic quote). However, in some instances, caregivers were reported to become overburdened with cognitive load and faced their own cognitive challenges: “my son is my backup brain and that can take a toll on his mental load” (synthetic quote). Ultimately, managing brain fog appeared to be dependent on individual factors.
4 Discussion
4.1 Overview
This study examined how brain fog in chronic pain is described on social media platforms. Brain fog was characterized as a fluctuating experience, with some participants feeling cloudiness, mental heaviness, or dissociation. The antecedents of brain fog could be attributed to pain, cognitive overload, environmental factors, or random occurrences. Brain fog could reportedly cause cognitive (e.g., thinking and remembering) and bodily (e.g., exhaustion and emotional challenges) impacts that affected meaningful participation and perception of self. The findings of this study also revealed a potential hesitancy among PWLE to disclose brain fog to employers and healthcare professionals. Overall, the findings of this study demonstrate the impacts of brain fog, the need for exploration of mechanisms by researchers, and the value of validation from healthcare professionals.
Social media research can provide an understanding of how concepts are understood and discussed within a community. In this study, we saw variation in how brain fog was experienced, with some individuals noting slowness, heaviness, or dissociation. Differences in descriptions may be because brain fog is a broad experience that can be perceived differently across individuals [34,35]. One recent study exploring how brain fog is described in Reddit posts stated that brain fog should not be described on its own and instead accompanied by more specific experiences, due to its heterogeneous nature [28]. It is also plausible that these individuals may be experiencing different phenomena but do not know the correct terminology and, so, utilize “brain fog” as a “catch all” term (removed for anonymization [10]). This might occur as people with brain fog and chronic pain often experience multiple health comorbidities that may have overlapping symptoms with brain fog (removed for anonymization). As an example, post-traumatic stress disorder is often associated with dissociation, which is common among those experiencing brain fog [3]. Additionally, people with long COVID are likely to experience mental health comorbidities [36]. As emphasized by a review of brain fog across conditions, overuse or incorrect use of the term “brain fog” may contribute to miscommunication in literature, hindering a true understanding of both brain fog and related conditions [10]. Further, social media postings highlight possible motor aspects of brain fog, including slowed motor control and reduced frequency of movement, which, to our knowledge, is not reflected in the medical literature. Overall, the findings of this study align with the proposed definition by (removed for anonymization) but highlight variations in experiences. This is also aligned with a study identifying that brain fog could be understood using an adapted version of the episodic disability framework, which allows consideration of variation in experiences of social, internal, and societal factors [29].
The variability in descriptions of experiences of brain fog also highlights the need for research exploring the mechanisms and relationships across conditions to guide management [10,17].
Next, the social media discourses around brain fog illustrate a disconnect between PWLE and the academic community. Most discussion on brain fog is centered around its symptoms and the impacts it has on the lived experiences of persons with chronic pain, while management strategies are the least discussed. Using a typical healthcare model, patients tend to look to healthcare workers and researchers to identify solutions [37]. In this study, healthcare workers and researchers rarely contributed to this online discourse. While some individuals described having support from their healthcare workers, many expressed discomfort in describing their experience or feeling like they were not being taken seriously. This is similar to a study exploring social media use of persons with endometriosis, a condition that is also poorly understood and overlooked in clinical settings [38]. Alternatively, the disconnect between PWLE and healthcare professionals may suggest that individuals were opting to self-manage their symptoms. Self-management and self-education are also quite common in chronic pain and other chronic conditions; particularly, if individuals do not feel like there is much else that can be done to support them, or as a form of autonomy and control over their health [39,40]. Research explicitly exploring the barriers and facilitators to patients disclosing symptoms of and seeking care for brain fog from healthcare professionals is needed. Healthcare professionals can use this information to proactively have discussions with their patients to help them feel heard and supported.
Of note, we located and excluded n = 25 commercial posts. This volume of posts suggests that some companies may take advantage of the gap between PWLE and healthcare professionals by offering strategies that may not be supported by evidence. This might be particularly problematic for equity-deserving groups (e.g., individuals from lower socioeconomic statuses) who (1) are more likely to experience multimorbidity associated with brain fog and (2) have fewer educational resources to advocate for their care [37,41]. The potential disconnect between PWLE, researchers, and clinicians highlights an opportunity for researchers and healthcare workers to take a proactive role in supporting persons with chronic pain and brain fog. Understanding lived experiences [42] and the impacts of brain fog on individuals’ well-being and perception of self can help healthcare workers understand how to provide meaningful support.
4.2 Limitations
As stated in the introduction, there are limitations to using social media as a data source. While social media can help to understand the perspectives of those who may not be included in traditional research methods, there is no way to confirm the experiences and characteristics of the individuals included in this study [43]. Additionally, capturing key demographic variables related to pain, namely, race, age, and gender, is difficult to accurately account for [43]. Next, this study is limited to using only two social media platforms. Other platforms, such as Reddit, may have fostered more detailed conversations and produced more insightful results; however, due to limited resources, we were unable to analyze all possible social media platforms. Additionally, as we were not directly asking participants questions, we organized posts into relevant categories (e.g., symptoms vs management strategies) based on our understanding; however, this may differ from the original intention of the authors. Lastly, social media is constantly updating, and discourses are constantly evolving as new information is presented [43]. Finally, the exclusion of non-English posts introduces a language bias and limits the generalizability of our analysis to a broader, global population.
4.3 Conclusion and future direction
This study examined the public discourse of brain fog in persons with chronic pain on social media, highlighting key attributes, antecedents, symptoms, and management strategies. These findings have identified an understanding of how chronic pain-related brain fog is discussed on social media and areas of exploration for future research. To facilitate disclosure of the experience by PWLE, healthcare workers can utilize the described antecedents and attributes to proactively identify brain fog and suggest possible management strategies. Researchers may use the antecedents to systematically explore the hypothesized correlates and mechanisms of brain fog. Lastly, these findings can be used to develop educational materials to enable PWLE to self-advocate in clinical and work settings. These tools can be mobilized through social media platforms through official and reputable accounts to educate PWLE, families or companions of PWLE, or communities working on addressing this issue. To summarize, exploring the discourse of brain fog in persons with chronic pain contributes to our understanding of the phenomenon and highlights the need to bridge lived experiences with clinical decision-making.
-
Funding information: Authors state no funding involved.
-
Author contributions: All authors have accepted responsibility for the entire content of this manuscript and consented to its submission to the journal, reviewed all the results and approved the final version of the manuscript. RD assisted with study design, data extraction, analysis, and writing of the manuscript. ACA assisted with data extraction, analysis, and writing of the manuscript. TP assisted with study design, analysis, and writing of the manuscript. TP also provided supervision for the project.
-
Conflict of interest: Authors state no conflict of interest.
-
Data availability statement: Due to the qualitative nature of this study and potential for participants to be identified from raw data, raw data are not available for this study.
Appendix A Search strategy
Using the advanced function on Twitter and Facebook, the following terms will be searched:
January 1, 2016, to December 31, 2019
January 1, 2020, to current
#Brainfog chronic pain
Brain fog chronic pain
#Brainfog #chronic pain
Brain fog #chronicpain
Facebook:
#Brainfog chronic pain
Brain fog chronic pain
#Brainfog #chronic pain
Brain fog #chronicpain
References
[1] Yong E. One of long COVID’s worst symptoms is also its most misunderstood. Atl. 2022. https://www.theatlantic.com/health/archive/2022/09/long-covid-brain-fog-symptom-executive-function/671393.Suche in Google Scholar
[2] Dass R, Kalia M, Harris J, Packham T. Understanding the experience and impacts of brain fog in chronic pain: A scoping review. Can J Pain. 2023;7(1):1–23.10.1080/24740527.2023.2217865Suche in Google Scholar PubMed PubMed Central
[3] Lucius K. Brain fog: exploring a symptom commonly encountered in clinical practice. Mary Ann Liebert. 2021;27(1):1–9.10.1089/act.2020.29313.kluSuche in Google Scholar
[4] British Colombia’s Womens Health Centre. 2023.http://www.bcwomens.ca/Specialized-Services-Site/Documents/Complex%20Chronic%20Diseases%20%28CCDP%29/Brain%20Fog%20Mar%2028%202021.pdf.Suche in Google Scholar
[5] Centre of Spine and Orthopedics. How to manage brain fog and chronic pain. 2024. https://www.spineorthocenter.com/brain-fog-and-chronic-pain.Suche in Google Scholar
[6] MoreGoodDays. Why is my brain foggy with chronic pain and what can i do about it, Pain Management Program for Fibromyaglia. 2023. https://www.moregooddays.com/post/why-brain-fog-with-chronic-pain.Suche in Google Scholar
[7] Samuels MH, Bernstein LJ. Brain fog in hypothyroidism: What is it, how is it measured, and what can be done about it’. Rev Sch Dialogue. 2022;32:752–63.10.1089/thy.2022.0139Suche in Google Scholar PubMed PubMed Central
[8] Dass R, Kadakia Z, Rosen NP, Clarke-Tizzard S, Harris J, Velikonja D, et al. Interrelationship of brain fog, pain, and psychological distress with quality of life of Veterans with painful symptoms. J Mil Veteran Family Health. 2024;11(3):1–14.10.3138/jmvfh-2024-0021Suche in Google Scholar
[9] Altuna M, Sánchez-Saudinós M, Lleó A. Cognitive symptoms after COVID-19. Neurol Perspect. 2021;1:16–24.10.1016/j.neurop.2021.10.005Suche in Google Scholar PubMed PubMed Central
[10] Denno P, Zhao S, Husain M. Defining brain fog across medical conditions. Trends Neurosci. 2025;48(5):330–48.10.1016/j.tins.2025.01.003Suche in Google Scholar PubMed
[11] Kratz A, Whibley D, Kim S, Sliwinski M, Clauw D, Williams D. Fibrofog in daily life: An examination of ambulatory subjective and objective cognitive function in fibromyalgia. Arthritis Care Res. 2020;72(12):1669–77.10.1002/acr.24089Suche in Google Scholar PubMed PubMed Central
[12] Walitt B, Čeko M, Khatiwada M, Gracely J, Rayhan R, VanMeter J, et al. Characterizing “fibrofog”: Subjective appraisal, objective performance, and task-related brain activity during a working memory task. NeuroImage Clin. 2016;11(1):173–80.10.1016/j.nicl.2016.01.021Suche in Google Scholar PubMed PubMed Central
[13] Chasco E, Dukes K, Jones D, Comellas A, Hoffman R, Garg A. Brain fog and fatigue following COVID-19 infection: An exploratory study of patient experiences of long COVID. Int J Environ Res Public Health. 2022;19(23):1–12.10.3390/ijerph192315499Suche in Google Scholar PubMed PubMed Central
[14] Bannon S, Greenberg J, Mace R, Lacascio J, Vranceanu A. The role of social isolation in physical and emotional outcomes among patients with chronic pain. Gen Hosp Psychiatry. 2021;69:50–4.10.1016/j.genhosppsych.2021.01.009Suche in Google Scholar PubMed PubMed Central
[15] Callan C, Ladds E, Husain L, Pattinson K, Greenhalgh T. I can’t cope with multiple inputs’: A qualitative study of the lived experience of brain fog’ after COVID-19’. BMJ Open. 2022;12(2):1–10.10.1136/bmjopen-2021-056366Suche in Google Scholar PubMed PubMed Central
[16] Hobson G, Dennis N. “I can’t be dealing with this brain fog”: A workplace focus group study investigating factors underpinning the menopausal experience for NHS staff. Maturitas. 2024;180:1–7.10.1016/j.maturitas.2023.107889Suche in Google Scholar PubMed
[17] Haywood D, Rossell S, Hart N. Cutting through the fog: Recognising brain fog as a significant public health concern. BMC Public Health. 2025;25(1230):1–4.10.1186/s12889-025-22525-6Suche in Google Scholar PubMed PubMed Central
[18] Krishnan K, Lin Y, Prewitt K, Potter D. Multidisciplinary approach to brain fog and related persisting symptoms post COVID-19. J Health Serv Psychol. 2022;48:31–8.10.1007/s42843-022-00056-7Suche in Google Scholar PubMed PubMed Central
[19] Lamper C, Beckers L, Kroese M, Verbunt J, Huijnen I. Interdisciplinary care networks in rehabilitation care for patients with chronic musculoskeletal pain: A systematic review. J Clin Med. 2021;10(9):1–64.10.3390/jcm10092041Suche in Google Scholar PubMed PubMed Central
[20] Zhou L, Zhang D, Yang C, Wang Y. Harnessing social media for health information. PMC. 2019;27(1):139–51.10.1016/j.elerap.2017.12.003Suche in Google Scholar PubMed PubMed Central
[21] Milller E, Woodward A, Flinchum G, Young J, Tabor H, Halley M. Opportunities and pitfalls of social media research in rare genetic diseases: A systematic review. Genet Med. 2021;23(11):2250–9.10.1038/s41436-021-01273-zSuche in Google Scholar PubMed PubMed Central
[22] Kivle B, Espedal G. Identifying values through discourse analysis. In: Researching values: Methodological approaches for understanding values work in organisations and leadership. Cham: Springer International Publishing; 2022. p. 177–82.10.1007/978-3-030-90769-3Suche in Google Scholar
[23] Steinmann G, Van de Bovenkamp H, de Bont A, Delnoij D. Redefining value: a discourse analysis on value-based health care. BMC Health Serv Res. 2020;20(1):1–13.10.1186/s12913-020-05614-7Suche in Google Scholar PubMed PubMed Central
[24] Harter C, Ness M, Goldin A, Lee C, Merenda C, Riberdy A, et al. Exploring chronic pain and pain management perspectives: Qualitative pilot analysis of web-based health community posts. JMIR Infodemiol. 2023;3:1–24.10.2196/41672Suche in Google Scholar PubMed PubMed Central
[25] Pagoto S, Waring ME, Xu R. A call for a public health agenda for social media research. JMIR Publ. 2019;21(12):1–22.10.2196/16661Suche in Google Scholar PubMed PubMed Central
[26] Hughes R, Beers L, Robinson-Whelen S. Health information seeking by women with physical disabilities: A qualitative analysis. Disabil Health. 2022;15(2):101268.10.1016/j.dhjo.2022.101268Suche in Google Scholar PubMed PubMed Central
[27] Pester B, Tankha H, Cano A, Grekin E, Bruinsma J, Gootee J, et al. Facing pain together: A randomized controlled trial of the effects of facebook support groups on adults with chronic pain. J Pain. 2022;23(12):2121–34.10.1016/j.jpain.2022.07.013Suche in Google Scholar PubMed
[28] Goudman L, Smedt A, Moens M. Social media and chronic pain: What do patients discuss? J Pers Med. 2022;15(5):797.10.3390/jpm12050797Suche in Google Scholar PubMed PubMed Central
[29] O’Brien BC, Harris IB, Beckman TJ, Reed DA, Cook DA. Standards for reporting qualitative research: A synthesis of recommendations. Acad Med. 2014;89(9):1245–51.10.1097/ACM.0000000000000388Suche in Google Scholar PubMed
[30] Markham A, Buchanan E. Ethical decision making and internet research recommendations from the AoIR Ethics Working Committee. J Gen Intern Med. 2012;34(1):154–8.Suche in Google Scholar
[31] Quirkos. [Internet]. 2022.Suche in Google Scholar
[32] Foley A, Davis A. A guide to concept analysis. Clin Nurse Specialist. 2017;31(2):70–3.10.1097/NUR.0000000000000277Suche in Google Scholar PubMed
[33] Lincoln Y, Guba E. Naturalistic inquiry. California, United States: Sage publications; 1985. p. 7–415.Suche in Google Scholar
[34] Bell T, Crowe M, Novack T, Davis R, Stavrinos D. Severity and correlates of mental fog in people with traumatic brain injury’. Res Nurs Health. 2022;46(1):136–47.10.1002/nur.22280Suche in Google Scholar PubMed PubMed Central
[35] Theoharides T, Cholevas C, Polyzoidis K, Politis A. Long-COVID syndrome-associated brain fog and chemofog: luteolin to the rescue. BioFactors. 2021;47(2):232–41.10.1002/biof.1726Suche in Google Scholar PubMed PubMed Central
[36] Feltz-Cornelis C, Turk F, Sweetman J, Khunti K, Gabbay M, Sheperd J, et al. Prevalence of mental health conditions and brain fog in people with long COVID: A systematic review and meta-analysis. Gen Hosp Psychiatry. 2024;88:10–22.10.1016/j.genhosppsych.2024.02.009Suche in Google Scholar PubMed
[37] Montori V. Turning away from industrial health care toward careful and kind care. Acad Med. 2019;94(6):768–70.10.1097/ACM.0000000000002534Suche in Google Scholar PubMed
[38] Lehembre-Shiah E, Kronfel H, Eisenberg J, Naroji S, Grunebaum A. Understanding tiktok as a source of medical information about endometriosis. JMIG. 2023;30(11):1.10.1016/j.jmig.2023.08.064Suche in Google Scholar
[39] Miller M, Arefanian S, Blatnik J. The impact of internet-based patient self-education of surgical mesh on patient attitudes and healthcare decisions prior to hernia surgery. Surg Endosc. 2020;34:132–41.10.1007/s00464-019-07300-0Suche in Google Scholar PubMed
[40] Nouri-Parto D, Carlesso L, Macedo L, Katz L. Effectiveness and engagement in self-education: A mixed methods study for veterans living with chronic pain. Poster presentation: Canadian Institute for Military and Veteran Health Research Forum Oct 17-19th, 2022: Halifax, NS. 2022.Suche in Google Scholar
[41] Braveman P. What are health disparities and health equity? We need to be clear. Public Health Rep. 2019;129(2):5–8.10.1177/00333549141291S203Suche in Google Scholar PubMed PubMed Central
[42] Jiang S. The roles of worry, social media information overload, and social media fatigue in hindering health fact-checking. Soc Media + Soc. 2022;1:1–12.10.1177/20563051221113070Suche in Google Scholar
[43] Hunter RF, Gough, A, O’Kane, N, McKeown, G, Fitzpatrick, A, Walker, T, et al. Ethical issues in social media research for public health. Am J Public Health. 2018;108(3):343–8.10.2105/AJPH.2017.304249Suche in Google Scholar PubMed PubMed Central
© 2025 the author(s), published by De Gruyter
This work is licensed under the Creative Commons Attribution 4.0 International License.
Artikel in diesem Heft
- Research Articles
- Relationship between body mass index and quality of life, use of dietary and physical activity self-management strategies, and mental health in individuals with polycystic ovary syndrome
- Evaluating the challenges and opportunities for diabetes care policy in Nigeria
- Body mass index is associated with subjective workload and REM sleep timing in young healthy adults
- Prediction of hypoglycaemia in subjects with type 1 diabetes during physical activity
- Investigation by the Epworth Sleepiness Scale of daytime sleepiness in professional drivers during work hours
- Understanding public awareness of fall epidemiology in the United States: A national cross-sectional study
- Impact of Covid-19 stress on urban poor in Sylhet Division, Bangladesh: A perception-based assessment
- Impact of the COVID-19 pandemic on mental health, relationship satisfaction, and socioeconomic status: United States
- Psychological factors influencing oocyte donation: A study of Indian donors
- Cervical cancer in eastern Kenya (2018–2020): Impact of awareness and risk perception on screening practices
- Older LGBTQ+ and blockchain in healthcare: A value sensitive design perspective
- Trends and disparities in HPV vaccination among U.S. adolescents, 2018–2023
- Do cell towers help increase vaccine uptake? Evidence from Côte d’Ivoire
- In search of the world’s most popular painkiller: An infodemiological analysis of Google Trend statistics from 2004 to 2023
- Brain fog in chronic pain: A concept analysis of social media postings
- Association between multidimensional poverty intensity and maternal mortality ratio in Madagascar: Analysis of regional disparities
- A “disorder that exacerbates all other crises” or “a word we use to shut you up”? A critical policy analysis of NGOs’ discourses on COVID-19 misinformation
- Smartphone use and stroop performance in a university workforce: A survey-experiment
- Review Articles
- The management of body dysmorphic disorder in adolescents: A systematic literature review
- Navigating challenges and maximizing potential: Handling complications and constraints in minimally invasive surgery
- Examining the scarcity of oncology healthcare providers in cancer management: A case study of the Eastern Cape Province, South Africa
- Dietary strategies for irritable bowel syndrome: A narrative review of effectiveness, emerging dietary trends, and global variability
- The impact of intimate partner violence on victims’ work, health, and wellbeing in OECD countries (2014–2025): A descriptive systematic review
- Nutrition literacy in pregnant women: a systematic review
- Short Communications
- Experience of patients in Germany with the post-COVID-19 vaccination syndrome
- Five linguistic misrepresentations of Huntington’s disease
- Letter to the Editor
- PCOS self-management challenges transcend BMI: A call for equitable support strategies
Artikel in diesem Heft
- Research Articles
- Relationship between body mass index and quality of life, use of dietary and physical activity self-management strategies, and mental health in individuals with polycystic ovary syndrome
- Evaluating the challenges and opportunities for diabetes care policy in Nigeria
- Body mass index is associated with subjective workload and REM sleep timing in young healthy adults
- Prediction of hypoglycaemia in subjects with type 1 diabetes during physical activity
- Investigation by the Epworth Sleepiness Scale of daytime sleepiness in professional drivers during work hours
- Understanding public awareness of fall epidemiology in the United States: A national cross-sectional study
- Impact of Covid-19 stress on urban poor in Sylhet Division, Bangladesh: A perception-based assessment
- Impact of the COVID-19 pandemic on mental health, relationship satisfaction, and socioeconomic status: United States
- Psychological factors influencing oocyte donation: A study of Indian donors
- Cervical cancer in eastern Kenya (2018–2020): Impact of awareness and risk perception on screening practices
- Older LGBTQ+ and blockchain in healthcare: A value sensitive design perspective
- Trends and disparities in HPV vaccination among U.S. adolescents, 2018–2023
- Do cell towers help increase vaccine uptake? Evidence from Côte d’Ivoire
- In search of the world’s most popular painkiller: An infodemiological analysis of Google Trend statistics from 2004 to 2023
- Brain fog in chronic pain: A concept analysis of social media postings
- Association between multidimensional poverty intensity and maternal mortality ratio in Madagascar: Analysis of regional disparities
- A “disorder that exacerbates all other crises” or “a word we use to shut you up”? A critical policy analysis of NGOs’ discourses on COVID-19 misinformation
- Smartphone use and stroop performance in a university workforce: A survey-experiment
- Review Articles
- The management of body dysmorphic disorder in adolescents: A systematic literature review
- Navigating challenges and maximizing potential: Handling complications and constraints in minimally invasive surgery
- Examining the scarcity of oncology healthcare providers in cancer management: A case study of the Eastern Cape Province, South Africa
- Dietary strategies for irritable bowel syndrome: A narrative review of effectiveness, emerging dietary trends, and global variability
- The impact of intimate partner violence on victims’ work, health, and wellbeing in OECD countries (2014–2025): A descriptive systematic review
- Nutrition literacy in pregnant women: a systematic review
- Short Communications
- Experience of patients in Germany with the post-COVID-19 vaccination syndrome
- Five linguistic misrepresentations of Huntington’s disease
- Letter to the Editor
- PCOS self-management challenges transcend BMI: A call for equitable support strategies


