Impact of the COVID-19 pandemic on mental health, relationship satisfaction, and socioeconomic status: United States
-
Anthony Coetzer-Liversage
, Irena Mikhalyuk
Abstract
Background
The coronavirus disease 2019 pandemic disproportionately impacted mental health and relationship satisfaction, particularly among individuals from lower socioeconomic status (SES) backgrounds.
Aim
The aim of this study is to examine the relationship between the pandemic and mental health outcomes (depression, anxiety, substance use, and psychological distress) using a mediated moderation analysis.
Method
Secondary data analysis was conducted using data from a state-wide screening, brief intervention, and referral to treatment project, with 1,718 participants throughout Rhode Island, United States. The Client Outcome Measures for Discretionary Programs tool was administered during interviews. A mediated moderation model assessed the pandemic’s impact (independent variable), relationship satisfaction (mediator), and SES (moderator) on five outcomes: alcohol use, cannabis use, anxiety, depression, and psychological distress. Generalized Linear Mixed Effects Models estimated associations, adjusting for participant and regional variations.
Results
While no significant total mediated effects were found (p > 0.05), higher relationship satisfaction was associated with lower anxiety (β = −0.13, p < 0.0001), depression (β = −0.18, p < 0.0001), and psychological distress (β = −0.16, p < 0.0001). A small positive association with alcohol use was found (β = 0.04, p = 0.0938) with relationship satisfaction. SES moderated mental health outcomes, with low-income participants experiencing greater depression (β = −0.09, p = 0.0015) and psychological distress (β = −0.12, p = 0.0015).
Conclusion
Findings underscore the role of SES and relationship satisfaction in mental health during crises. Targeted interventions and policies addressing SES disparities, and relationship-based services are recommended.
1 Introduction
The coronavirus disease 2019 (COVID-19) pandemic has had widespread effects on public health, social relatoinships, and economic stability. While its effects have lessened over time, mortality rates continue to remain higher than those of seasonal influenza [1]. Experts agree that future pandemics are inevitable, underscoring the need for improved prevention, preparedness, and crisis management [2]. Research emphasizes that to better handle future crises, it is critical to invest in healthcare, ensure robust governance, and advance technological solutions that can enhance community resilience and response efforts [3]. Understanding the pandemic’s impact on social relationships, income, work, education, and health is essential for shaping policies and public health interventions that will strengthen future crises response.
The pandemic and the implementation of prevention measures (e.g., social distancing and isolation) have impacted social relationships, income, work/school interactions, and health [4]. Social distancing and financial concerns can impact mental health by promoting feelings of isolation, hopelessness, and anxiety [5]. Wang et al. [6] found that one in three adults among the global population experienced psychological distress during the COVID-19 pandemic, often as a result of coping with emotional responses during the pandemic and related prevention measures implemented [7,8,9]. Furthermore, the pandemic has presented significant characteristics of a traumatic event, including prolonged exposure to the social stressor, unpredictability, and threat to health or life [10]. Individuals who experience trauma have a higher likelihood of developing adverse mental or behavioral health conditions, such as substance use, depressive or anxiety disorders, impairment in daily and/or social functioning, and physical conditions [11]. Given this increased risk of mental health concerns, early access to mental health services is critical to prevent the progression of these issues and avoid negative outcomes related to social, occupational, and educational functioning.
Several factors have been proposed to influence the relationship between the pandemic and mental health outcomes, including social relationships and socioeconomic status (SES). SES reflects the extent to which individuals hold socially and economically valued resources [12]. While social relationships can serve as protective factors against deleterious post-traumatic responses, the relationships can also be strained during major stressful events [13,14]. Social support theory [15] suggests that social support – whether emotional, instrumental, or informational – can buffer individuals against the adverse effects of stress, including those caused by the pandemic. The social determinants of health theory suggests that social and economic conditions, including SES and social relationships, significantly shape individuals’ health outcomes, especially during crises like the pandemic [16]. For example, Luk et al. [17] highlighted the intersection of race/ethnicity, socio-economic status, and mental health during the pandemic, emphasizing the need for culturally sensitive interventions to address medical mistrust and improve engagement with mental health and addiction treatment, especially among racial/ethnic minorities and those with a history of alcohol use disorder (AUD). Additionally, Kim et al. [18] found that both minimal changes and complete disruptions in daily life during the pandemic were linked to higher rates of depression and suicidal thoughts. Unexpectedly, positive changes like increased income or improved work conditions were also associated with worse mental health outcomes, likely due to added stress and burnout, especially among frontline workers [18]. Other research also highlights significant mental health challenges following the pandemic, with elevated rates of depression, anxiety, and stress strongly associated with lower quality of life [19]. Key risk factors included older age, marital status, unemployment, excessive social media use, smoking, and the loss of family members to COVID-19 [19].
Relationship satisfaction refers to an individual’s overall evaluation of their social relationships, including emotional support, communication, and fulfillment [20,21,22]. Satisfaction among social relationships has been found to be positively correlated with psychological well-being, and the disruption of these relationships during crises, such as the pandemic, can significantly exacerbate mental health challenges [23]. Conversely, a lack of social support during a health crisis may increase feelings of loneliness and isolation, leading to poorer mental health outcomes [24]. Relationship satisfaction may be impacted by factors such as SES [25,26,27,28]. Social relationships, particularly during times of crisis, serve both as protective factors and as sources of stress, depending on the context [23,29]. The disruption of social relationships during the pandemic has highlighted the vital role of social support in fostering mental health resilience, making it essential to understand how this disruption interacts with SES factors to identify pathways to resilience [23]. Given that social relationships can be affected by crises, which in turn impacts mental health outcomes, it is important to understand whether and how relationships mediate the association between the pandemic and mental health.
During the pandemic restrictions, requests for substance use service significantly decreased, likely due to reduced social opportunities and access to treatment, while requests for mental health-services increased, reflecting heightened psychological distress from isolation, fear, and financial challenges [30]. After restrictions were lifted, requests for substance use services rose, requests for alcohol services resumed their pre-pandemic decline, and mental health-related continued to decrease [30]. Ogeil et al. [31] found that pandemics and disasters, including lockdowns, contributed to increased alcohol consumption and related harms, particularly among those with pre-existing mental health conditions. This placed additional strain on emergency services, leading to significant rises in alcohol-related issues for those with comorbid conditions. Similarly, while youth alcohol consumption decreased overall, particularly among social drinkers, it increased among high-risk users, highlighting the need to address high-risk drinking in disaster planning and to intervene early to reduce the global burden of alcohol consumption [32].
Since the early stages of the pandemic, vulnerable populations have been disproportionately impacted by COVID-19 [33]. Vulnerable populations are identified based on factors, such as financial strains, place of residence, race and ethnicity, age, and chronic health conditions [34]. Individuals from racial/ethnic minoritized groups, with low SES or who have pre-existing mental health conditions, are more likely to face barriers in accessing community health resources, including COVID-19 testing/treatment and mental health services [33,35,36,37]. These barriers increase the likelihood of experiencing poor mental health outcomes [38]. A systematic review that examined the prevalence of psychological distress among participants from 19 countries found individuals residing in areas of lower SES strata to be associated with higher odds of depression and anxiety during the COVID-19 pandemic [6].
While much is known about the individual impacts of relationship satisfaction and SES on mental health during past global health emergencies, no studies have simultaneously explored these factors as mediators and moderators within the context of the pandemic [39].
1.1 Purpose of this study
While numerous studies have examined the relationship between the pandemic and mental health, the mechanisms underlying these associations remain unclear. Relationship satisfaction and SES have been identified as key factors in mental health outcomes during previous global health crises; however, research remains limited on how relationship satisfaction functions as a mediator and SES as a moderator in the link between the pandemic and mental health. This study is guided by the following research questions:
Does relationship satisfaction mediate the association between the pandemic and mental health outcomes (i.e., anxiety, depression, substance use, and psychological distress)?
Does SES moderate the mediating effect of relationship satisfaction on mental health outcomes?
Using a large state-wide database from healthcare settings directly impacted by the pandemic, this study tests two key hypotheses: (1) relationship satisfaction mediates the relationship between the pandemic and mental health outcomes, and (2) SES moderates the mediating effect of relationship satisfaction, shaping its influence on mental health outcomes.
2 Methodology
2.1 Sample and data
This study utilized secondary data from multiple organizations cooperating with the Rhode Island Department of Behavioral Healthcare, Developmental Disabilities, & Hospital (RI-BHDDH) for a state-wide implementation of screening, brief intervention, and referral to treatment (SBIRT) as funded by Substance Abuse and Mental Health Services Administration (SAMHSA; TI-16-007). Organizations included primary care clinics, behavioral health centers, inpatient units, critical care sites, outreach community programs, and the Department of Corrections. Many of these sites served low-income and historically minoritized populations. Institutional Review Board approval was obtained for de-identified data to be used for this study.
SBIRT targeted adults at risk of substance misuse or diagnosed with substance use disorders. Using the Client Outcome Measures for Discretionary Programs (COM; [40]), data were collected as stipulated by the Government performance and results act (GPRA; [41]) and entered into the SAMHSA Performance Accountability and Reporting System by the organizations. Data collection included patient intake screenings, informed consent, demographic data, emotional and social functioning, and substance use. Depending on screening results, patients received brief interventions, brief therapy, or referral treatment, with appropriate COM sections administered at intake, discharge, and 6 months post-treatment. Follow-up efforts included outreach, patient satisfaction surveys, and a $20 gift card incentive for participation. Ten percent of clients in each intervention group were tracked for follow-up as mandated by SAMHSA. To maximize participants available for model-building, baseline data were utilized in analyses (i.e., only 10% mandated for follow-up tracking at 6 months and discharge).
Informed consent was obtained from participants during initial data collection. Participants were included in this study if they were screened prior to the first COVID-19 case reported in the state (i.e., March 1, 2020) and screened after the first case was reported. Clients in the study were screened from October 1, 2019 to May 31, 2020. This yielded a subsample of N = 1,718 available for analyses (pre-pandemic n = 1,625; during the pandemic n = 93). See Section 2.3 for consideration of balanced groups. Participants, on average, were 40 years old and endorsed the following identities: 45% female, 12.8% Hispanic/Latinx, 67.3% White, 12.4% Black, 2.5% American Indian, 1% Asian, and 0.3% Hawaiian or Pacific Islander.
-
Ethical approval: This study was approved by the Institutional Review Board of the University of Rhode Island, Kingston, RI 02881. All procedures in this study were conducted in accordance with the Institutional Review Board of the University of Rhode Island, Kingston, RI 02881.
-
Informed consent: All study participants, or their legal guardian(s), provided informed written consent prior to study enrollment.
2.2 Measures
The COM [40] collects client data as stipulated by the GPRA [41]. It is based on standardized and validated instruments such as the AUDs Identity Test-10 [42] and the Drug Abuse Screening Test-10 [43]. COM is required by SAMHSA for program monitoring and client outcomes, and is delivered through structured interview by trained and supervised staff from each organization. From COM, the below constructs were collected.
2.2.1 Demographics
Variables in this section included age (in years), gender (male, female, transgender, and other), ethnicity (Hispanic or Latino), and race (Black or African American, Asian, Native Hawaiian, or other Pacific Islander, Alaska Native, White, and American Indian). Employment status was also asked and coded as 0 (unemployed), 0.5 (part-time employed), and 1 (full-time employed).
2.2.2 Substance use
Variables in this section included frequency of substance use (e.g., alcohol, marijuana, crack/cocaine, opioids, etc.) in the past 30 days. A sample item includes: During the past 30 days, how many days have you used alcohol?
2.2.3 Family and living conditions
Variables in this section included: (1) Client’s satisfaction with their living situation (e.g., How satisfied are you with the conditions of your living space?) measured on a 5-point Likert scale (1 = very dissatisfied to 5 = very satisfied); and (2) number of children participants endorsed having (e.g., How many children do you have?). Higher scores suggest greater satisfaction with living situation.
2.2.4 Mental and physical health problems
Clients were asked to rate their overall health status on a 5-point Likert scale (1 = poor to 5 = excellent). Higher scores suggest better overall health. Additionally, they reported their daily experience of anxiety (In the past 30 days, not due to your use of alcohol or drugs, how many days have you experienced serious anxiety or tension?) and depression (In the past 30 days, not due to your use of alcohol or drugs, how many days have you experienced serious depression?). Finally, clients rated how much they have been bothered by psychological or emotional problems in the past 30 days on a 5-point Likert scale (1 = not at all to 5 = extremely). This item was referred to as psychological distress for this study. Lower scores suggest less psychological distress.
2.2.5 Relationship satisfaction
Clients reported how satisfied they were with their personal relationships, rated on a 5-point Likert scale of (1 = very dissatisfied to 5 = very satisfied). Higher scores suggest higher relationship satisfaction.
2.2.6 SES
SES was measured as median income of the zip-code where the clients received health services.
2.3 Analytical plan
The analysis focused on mediated moderation [44]. We hypothesized that the pandemic would adversely impact mental health and substance outcomes; however, we believed that social relations could either exacerbate or mitigate this relationship. Further, we reasoned that pandemic lock-down restrictions may allow for more enjoyable time together, or conversely strain relations due to being in constant close quarters. Finally, as the burden of daily life disruptions were disproportionately felt in low income communities (CITE) [45,46], we hypothesized that the magnitude of association would be stronger for people from lower SES backgrounds.
Generalized linear mixed effects modeling was used to estimate the mediational relationships [47]. The impact of the pandemic was estimated as a linear spline, measured in days before or after March 1, 2020. This allowed us to model how attitudes about personal relationships and mental health outcomes changed going into the pandemic. The following covariate confounding variables were included to control for possible extraneous variation in the outcome: age, living condition, number of children, employment, and health status. Finally, random intercepts were included to account for variation attributable to participant characteristics (i.e., treatment recommendations by screener) and regional nesting (i.e., screening location).
Separate models of the same design were estimated for each outcome, specifically: alcohol use, cannabis use, anxiety, depression, and difficulties with psychological distress.
Evidence of mediated moderation can be tested in the total mediated effect, which means multiplying the regression coefficient from the first leg of the hypothesized series of events (changes in average ratings of relationship satisfaction during the pandemic) by the regression coefficient for the second leg of the hypothesized series of events (relationship satisfaction prevent poor mental health outcomes). Bootstrapping was used to infer the standard error to test the total mediated effect, and address missing data by multiple imputation (e.g., ∼5–10% per variable) [48]. Refer Supplemental Materials for more information regarding bootstrapping.
3 Results
Distributions of the variables included in the analysis are presented in Table 1.
Descriptive statistics for mediated moderation, covariates, and outcome variables
| Variable | Mean | SD | Skew | Kurtosis |
|---|---|---|---|---|
| Mediated moderation | ||||
| Days into pandemic | −499.52 | 287.06 | 0.62 | −0.27 |
| Median income (US Dollars) | 79386.6 | 15699.48 | 1.00 | 1.07 |
| Relationship satisfaction | 3.34 | 1.23 | −0.40 | −0.85 |
| Covariates | ||||
| Age (years) | 40.04 | 12.07 | 0.45 | −0.4 |
| Living condition | 3.19 | 1.32 | 0.05 | −1.3 |
| Number of children | 0.7 | 0.52 | −0.4 | −1.33 |
| Employment | 4.42 | 2.25 | −0.27 | −1.1 |
| Health status | 3.69 | 1.25 | −0.13 | −0.38 |
| Outcomes | ||||
| Alcohol use | 7.76 | 10.9 | −0.30 | 0.26 |
| Cannabis use | 4.83 | 9.99 | 1.85 | 1.85 |
| Anxiety | 20.13 | 11.57 | −0.63 | −1.02 |
| Depression | 16.73 | 12.06 | −0.12 | −1.6 |
| Psychological distress | 3.81 | 1.22 | −0.77 | −0.41 |
Note. SD = standard deviation.
Covariate associations are presented in the supplementary data. Female-identifying respondents experienced more negative mental health outcomes (anxiety, β = 0.12, p < 0.0001; depression, β = 0.08, p = 0.0029; psychological distress, β = 0.11, p < 0.0001). People with more children (β = 0.10, p = 0.0001) and better living conditions (β = −0.22, p < 0.0001) reported more relationship satisfaction.
Our hypothesis was mediated moderation. That is, as the pandemic endured, relationships became strained, resulting in exacerbated problems with mental health, especially for persons from low SES backgrounds. A conceptual diagram of the analysis is presented in Figure 1. Tests of the total mediated effect are reported in Table 2 (full model results are available in the supplemental material). There was no mediation.
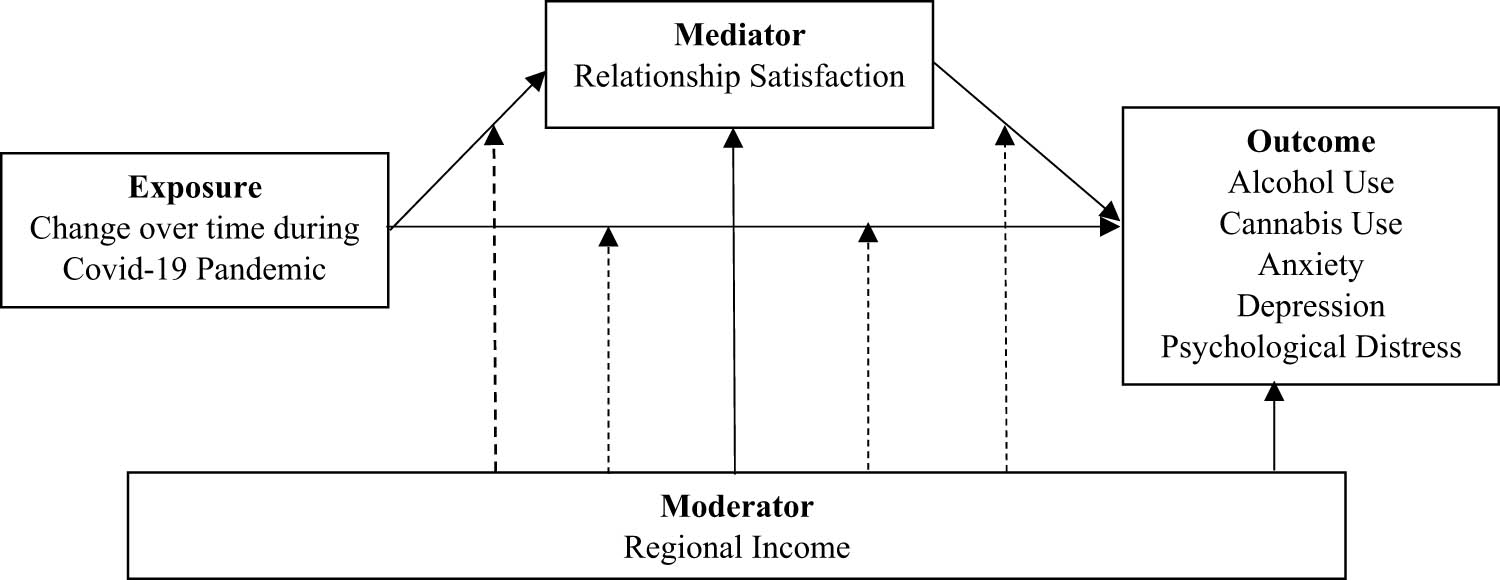
Analysis framework.
Tests of the total mediated effect
| Outcome | Total mediated effect | Z | p |
|---|---|---|---|
| Alcohol | 0.00 | −0.16 | 0.8753 |
| Cannabis | 0.00 | −0.05 | 0.9629 |
| Anxiety | 0.01 | 0.17 | 0.8652 |
| Depression | 0.01 | 0.15 | 0.8838 |
| Psychological distress | 0.01 | 0.17 | 0.8611 |
Note. The primary reason the total mediated effect is small is because there were minimal changes identified in average ratings of relationship satisfaction going into the pandemic (β = 0.05, p = 0.2482).
Across all outcomes, all tests of mediated moderation were nonsignificant (p > 0.05), with total mediated effects close to zero. When examining individual path coefficients, this was likely because there were not large changes in relationship satisfaction during the pandemic (p = 0.2482). Relationship satisfaction increased slightly during the pandemic, though only a small amount (β = 0.05). Meaningful associations were identified between relationship satisfaction and mental health outcomes (anxiety, depression, and psychological distress, p < 0.0001). Respondents who reported greater relationship satisfaction tended toward moderately better mental health outcomes (anxiety, β = −0.13; depression, β = −0.18; psychological distress, β = −0.16). The association between relationship satisfaction and drinking evidenced marginal non-significance (p = 0.0938, β = 0.04, a small effect). There was some evidence of moderation by SES. While most respondents did not show large changes in average levels of the outcome variables going into the pandemic (|β| < 0.05, p > 0.05), this was not the case for respondents in low SES areas for depression (p = 0.0015) and psychological distress outcomes (p = 0.0015). Specifically, participants from low-income areas showed increases in depression (β = −0.09) and psychological distress (β = −0.12) as the pandemic bore on.
4 Discussion
The pandemic disrupted daily life, affecting living conditions, social relationships, and income, which in turn impacted mental health [49]. This study explored whether relationship satisfaction and SES influenced the link between the pandemic and mental health outcomes (depression, anxiety, substance use, and psychological distress). While no direct effects of the pandemic on mental health or relationship satisfaction were found, relationship satisfaction was found to correlate with anxiety, depression, and psychological distress. A small non-significant mediation effect emerged for alcohol use, with higher relationship satisfaction associated with slightly increased alcohol consumption. SES did not moderate the pandemic’s impact on substance use and anxiety, but did for depression and psycholigical distress. These findings underscore the complexity of pandemic-related stressors, suggesting that while direct pandemic effects were not observed, social and economic factors continued to influence individuals’ mental health and substance use patterns.
Specifically, participants from low-income areas tended toward faster increases in depression and psychological distress as the pandemic continued. This finding was consistent with global research findings, which found individuals residing in areas of lower SES strata to be associated with higher odds of psychological distress (e.g., depression) during the pandemic [6]. Limited research has focused on the impact of the pandemic on psychological distress among individuals with low SES. This study highlights the need to better understand how economic hardship contributes to emotional and cognitive coping challenges, particularly in crisis situations. Individuals facing financial strain may have access to resources, such as mental health services, which can limit opportunities to learn adaptive coping mechanisms. This lack of resources may increase their vulnerability to emotional distres, maladaptive coping mechanisms, and long-term psychological consequences. Results suggest the importance of not only mobilizing outreach for financially vulnerable communities, but doing so in a timely manner to mitigate the effects of the pandemic, particularly in areas with limited access to mental health services.
Whereas prior studies have provided support for separate pathways examined in this study, the current study examined a well-powered, single model in its entirety with all paths included. Although most studies found that individuals were more likely to report declines in relationship satisfaction during stressful external events [50,51,52], several studies found that relationship satisfaction increased for some individuals during the pandemic [51]. The current study did not find a significant association between days into the pandemic and relationship satisfaction, which may explain the lack of mediating effect found for relationship satisfaction. This suggests that the impact of the pandemic on relationships may be more individualized, with some relationships strengthening due to increased time together, while others may deteriorate under stress. Future research should explore the factors that determine whether relationship satisfaction improves or declines in times of crisis.
As stated earlier, individuals with higher relationship satisfaction were more likely to report experiencing better mental health outcomes. Several studies have found evidence for the influence of relationship satisfaction on mental health outcomes during external stressful events [13,14,51,53]. Findings in the current study are consistent with prior literature demonstrating an association between intimate relationship satisfaction and mental health [13]. Since past studies have examined relationship satisfaction with respect to intimate relationships and this study measured relationship satisfaction more broadly (i.e., any relationship), this finding is particularly noteworthy. This indicates that support from any type of close relationship – whether romantic, familial, or platonic – may serve as a protective factor against mental health deterioration. Future interventions should consider utilizing social support networks beyond intimate partners during crises.
Participants with better relationship satisfaction tended to use slightly more alcohol during the pandemic (marginal effects). Participants on average were found to increase their drinking days per month by 28% from before to during the pandemic. Our finding that alcohol consumption increased during the pandemic aligns with studies conducted within the United States, as well as the United Kingdom and Ireland [54,55]. A large review of drinking during the pandemic [56] suggested increased drinking was associated with restricted social rewards and the ability to drink in isolation, thus avoiding judgment from others; however, the current study suggests a more nuanced approach may be needed to fully understand the association between alcohol, the pandemic, and mediating social relationships (i.e., relationship satisfaction may offer rewards and mitigate isolation). While relationship satisfaction is typically protective of mental health, it may not necessarily lead to reduced alcohol consumption. Instead, individuals with strong social bonds may engage in drinking as a shared activity, using alcohol as a way to connect or manage stress together [57]. This highlights the need for targeted messaging about alcohol use in social contexts, particularly during crises.
As noted above, SES moderated the relationship between the pandemic and mental health outcomes (i.e., depression and psychological distress). Specifically, individuals with low SES were more likely to experience increased symptoms of depression and psychological distress as the pandemic progressed. Similar to this finding, prior research has found that individuals who experienced income instability during the pandemic were more likely to report higher rates of depression and other adverse mental health outcomes compared to individuals not experiencing income instability [58]. This may be explained by the lack of control and increased distressful emotions that individuals with low SES may experience due to external stressors [59]. This suggests that economic disparities not only impact financial security but also shape individuals’ emotional resilience. Given that those with lower SES may face higher chronic stress and reduced access to mental health care, policies addressing financial relief and accessible mental health interventions should be prioritized in future crisis responses.
This study also found that respondents with more children and better living conditions were more likely to report experiencing more relationship satisfaction. Consistent with this finding, prior research found parent–child relationships to be positively impacted by having more than one child during the pandemic [60]. This suggests that having multiple children may provide built-in socialization opportunities that ease parental stress, while better living conditions may buffer against pandemic-related relationship strain. Future studies should explore how housing and family dynamics interact to shape well-being during the times of crisis.
4.1 Limitations and future directions
The biggest limitation of the study is the timeframe. This was a study on the psychological and social impacts of living through a pandemic. We examined changing clients needs at intake from an agency’s perspective starting with the first case of COVID-19 because it represented a tipping point for stress related to the pandemic [61]. Although it is difficult to know which may cause more distress (initial reports of a deadly pandemic vs lockdown to prevent spread), the process likely unfolds over time, which is why we looked at clients pre- abd post- pandemic to understand this. This analysis accounted for the longitudinal changes in the pandemic, however, it was still an early pandemic sample. At the time of study, prioritization was set on better understanding the role of the ongoing pandemic on mental health and health behavior. Future studies may wish to examine longer term impacts of the COVID-19 pandemic. Another consideration for timing is that the data were cross-sectional with respect to the client. To maximize data availability for analyses, client baseline data were used as the funding agency required only 10% of the sample followed at 6 months and at dicharge. Future studies can expand follow-up samples to use longitudinal data for mediated moderation.
Another limitation is the reliance on self-reported evaluations, which, while valuable for capturing subjective experiences and covert behaviors, such as substance use [62,63], can be influenced by social desirability bias, particularly when addressing sensitive and stigmatized topics [64].
Finally, reduced clinical contact during the pandemic may have introduced bias, as individuals who maintained contact with clinical services may have been either more resilient or in greater need of care than those who did not. Future research should investigate this potential bias and explore the role of clinical engagement in mitigating pandemic-related mental health effects.
5 Conclusion
5.1 Implications
This study contributes to the understanding of clinical care during community disasters. While the study found that individuals of lower SES experienced more adverse mental health outcomes as the pandemic progressed, there was no evidence associating these outcomes with personal relationships. Although marginally non-significant, the findings suggest that, individuals who reported higher satisfaction with their relationships tended to drink 28% more during the pandemic. This raises the question of whether increased alcohol consumption might represent a form of social bonding, rather than an escape from strained family dynamics. Although mediated moderation was not observed in this study, the results offer an important step in examining a model of the pandemic’s impact, and factors that may be more or less important to outcomes. Further research is needed to determine whether relationship satisfaction influences alcohol use behaviors in pandemic contexts.
5.2 Policy implications
The findings of this study have important implications for mental health practice, particularly in understanding the impact of SES disparities on mental health during crises. Given the heightened vulnerability of individuals with low SES to adverse mental health outcomes during the pandemic, mental health professionals should integrate SES considerations into clinical assessment and treatment planning. This includes screening for financial stressors and providing tailored interventions, such as referrals to supportive resources or therapies addressing economic-related distress.
This study also underscores the role of relationship satisfaction in mental health outcomes. Given its strong association with psychological well-being, mental health care should consider relational factors in treatment approaches. Integrating couples counseling, family therapy, or interpersonal interventions may enhance overall mental health outcomes.
Finally, the study suggests a complex relationship between relationship satisfaction and alcohol use during the pandemic, with higher satisfaction linked to increased drinking, albeit marginally non-significant. Future mental health research should further explore the interplay between social relationships, substance use, and mental health, informing targeted interventions for alcohol misuse, particularly during periods of societal stress.
5.3 Future research
Future research should focus on the long-term mental health effects of the pandemic, particularly for individuals with low SES and varying relationship satisfaction. Studies should explore the complex links between relationship satisfaction, alcohol use, and psychological distress, while also considering gendered stressors and caregiving burdens. Additionally, examining outcomes for persons who do not outreach to mental health would be important for crisis planning.
Acknowledgements
This work is the sole responsibility of the authors and does not necessarily represent the official views of the Center for Substance Abuse Treatment, or agencies affiliated with the authors.
-
Funding information: This work was supported by the Substance Abuse & Mental Health Services Administration (SAMHSA), Grant Number: TI026664-01 to Department of Behavioral Healthcare, Developmental Disabilities & Hospitals (BHDDH).
-
Author contributions: All authors have accepted responsibility for the entire content of this manuscript and consented to its submission to the journal. All authors have reviewed and approved the final version of the manuscript. A.C.L. led the team in revision of the study, addressing all issues relating to the analysis, interpretations, and write-up of the study. I.M. led the conceptualization and methodology, and contributed to reviewing and editing. J.R.T. contributed to conceptualization, methodology, and formal analysis, as well as writing, reviewing, and editing. E.Q.S. and V.M.R.G. contributed to conceptualization, methodology, writing, reviewing, and editing. L.A.S. contributed to conceptualization, methodology, resources, writing, reviewing, and editing, and provided supervision. Additionally, L.A.S. was responsible for obtaining grant funding, grant oversight, and budgetary oversight.
-
Conflict of interest: Authors state no conflict of interest.
-
Data availability statement: Data available on request from the authors.
References
[1] Lippi G, Sanchis-Gomar F. Mortality of post-COVID-19 condition: 2025 update. COVID. 2025;5(1):11.10.3390/covid5010011Search in Google Scholar
[2] Coccia M. Sources, diffusion and prediction in COVID-19 pandemic: lessons learned to face next health emergency. AIMS Public Health. 2023;10(1):145.10.3934/publichealth.2023012Search in Google Scholar PubMed PubMed Central
[3] Coccia M, Benati I. Negative effects of high public debt on health systems facing pandemic crisis: Lessons from COVID-19 in Europe to prepare for future emergencies. AIMS Public Health. 2024;11(2):477.10.3934/publichealth.2024024Search in Google Scholar PubMed PubMed Central
[4] Kumar A, Nayar KR. COVID 19 and its mental health consequences. J Ment Health. 2021;30(1):1–2.10.1080/09638237.2020.1757052Search in Google Scholar PubMed
[5] Amerio A, Aguglia A, Odone A, Gianfredi V, Serafini G, Signorelli C, et al. Covid-19 pandemic impact on mental health of vulnerable populations. Acta Biomedica Atenei Parmensis. 2020;91(9-S):95–6.Search in Google Scholar
[6] Wang Y, Kala MP, Jafar TH. Factors associated with psychological distress during the coronavirus disease 2019 (COVID-19) pandemic on the predominantly general population: A systematic review and meta-analysis. PLoS One. 2020;15(12):e0244630.10.1371/journal.pone.0244630Search in Google Scholar PubMed PubMed Central
[7] Mariani R, Renzi A, Di Monte C, Petrovska E, Di Trani M. The impact of the COVID-19 pandemic on primary emotional systems and emotional regulation. Int J Environ Res Public Health. 2021;18(11):5742.10.3390/ijerph18115742Search in Google Scholar PubMed PubMed Central
[8] Restubog SLD, Ocampo ACG, Wang L. Taking control amidst the chaos: Emotion regulation during the COVID-19 pandemic. J Vocat Behav. 2020;119:103440. 10.1016/j.jvb.2020.103440Search in Google Scholar PubMed PubMed Central
[9] Panayiotou G, Panteli M, Leonidou C. Coping with the invisible enemy: The role of emotion regulation and awareness in quality of life during the COVID-19 pandemic. J Contextual Behav Sci. 2021;19:17–27.10.1016/j.jcbs.2020.11.002Search in Google Scholar
[10] Denckla CA, Gelaye B, Orlinsky L, Koenen KC. REACH for mental health in the COVID19 pandemic: an urgent call for public health action. Eur J Psychotraumatology. 2020;11(1):1762995.10.1080/20008198.2020.1762995Search in Google Scholar PubMed PubMed Central
[11] Center for Substance Abuse T. Trauma-informed care in behavioral health services. Rockville, MD: Substance abuse and mental health administration; 2014.Search in Google Scholar
[12] Antonoplis S. Studying socioeconomic status: Conceptual problems and an alternative path forward. Perspect Psychol Sci. 2023;18(2):275–92.10.1177/17456916221093615Search in Google Scholar PubMed PubMed Central
[13] Bonanno GA, Brewin CR, Kaniasty K, Greca AML. Weighing the costs of disaster: Consequences, risks, and resilience in individuals, families, and communities. Psychol Sci Public Interest. 2010;11(1):1–49.10.1177/1529100610387086Search in Google Scholar PubMed
[14] Umberson D, Karas Montez J. Social relationships and health: A flashpoint for health policy. J Health Soc Behav. 2010;51(1_suppl):S54–66.10.1177/0022146510383501Search in Google Scholar PubMed PubMed Central
[15] Cohen S, Wills TA. Stress, social support, and the buffering hypothesis. Psychol Bull. 1985;98(2):310.10.1037//0033-2909.98.2.310Search in Google Scholar
[16] Dean HD, Williams KM, Fenton KA. From theory to action: applying social determinants of health to public health practice. Los Angeles, CA: SAGE Publications Sage CA; 2013. p. 1–4.10.1177/00333549131286S301Search in Google Scholar PubMed PubMed Central
[17] Luk JW, Sewell L, Stangl BL, Vaughan CL, Waters AJ, Schwandt ML, et al. Disparities in group-based medical mistrust and associations with mental health symptoms during the COVID-19 pandemic. J Affect Disord. 2025;375:517–24.10.1016/j.jad.2025.01.137Search in Google Scholar PubMed PubMed Central
[18] Kim W-H, Kim J, Oh J, Lee S, Chang J, Kim Y. Unexpected effects of pandemic-related changes on mental health: Evidence from a nationwide survey in South Korea. PLoS One. 2025;20(1):e0317493.10.1371/journal.pone.0317493Search in Google Scholar PubMed PubMed Central
[19] Mahikul W, Srichan P, Narkkul U, Soontarawirat I, Kitro A, Pumipuntu N, et al. Mental health status and quality of life among Thai people after the COVID-19 outbreak: a cross-sectional study. Sci Rep. 2024;14(1):25896.10.1038/s41598-024-77077-3Search in Google Scholar PubMed PubMed Central
[20] Fincham FD, Beach SRH. Relationship satisfaction. Camb Handb Personal Relatsh. 2006;2:29.10.1017/CBO9780511606632.032Search in Google Scholar
[21] Fuller-Iglesias HR. Social ties and psychological well-being in late life: The mediating role of relationship satisfaction. Aging Ment Health. 2015;19(12):1103–12.10.1080/13607863.2014.1003285Search in Google Scholar PubMed
[22] Frazier PA, Tix AP, Barnett CL. The relational context of social support: Relationship satisfaction moderates the relations between enacted support and distress. Personality Soc Psychol Bull. 2003;29(9):1133–46.10.1177/0146167203254545Search in Google Scholar PubMed
[23] Vigl J, Strauss H, Talamini F, Zentner M. Relationship satisfaction in the early stages of the COVID-19 pandemic: A cross-national examination of situational, dispositional, and relationship factors. PLoS One. 2022;17(3):e0264511.10.1371/journal.pone.0264511Search in Google Scholar PubMed PubMed Central
[24] Leigh-Hunt N, Bagguley D, Bash K, Turner V, Turnbull S, Valtorta N, et al. An overview of systematic reviews on the public health consequences of social isolation and loneliness. Public Health. 2017;152:157–71.10.1016/j.puhe.2017.07.035Search in Google Scholar PubMed
[25] Amato PR. Alone together: How marriage in America is changing. Cambridge, MA: Harvard University Press; 2007.10.4159/9780674020184Search in Google Scholar
[26] Proulx CM, Helms HM, Buehler C. Marital quality and personal well‐being: A meta‐analysis. J Marriage Family. 2007;69(3):576–93.10.1111/j.1741-3737.2007.00393.xSearch in Google Scholar
[27] Umberson D, Williams K. Marital quality, health, and aging: Gender equity? J Gerontology: Ser B. 2005;60(Special_Issue_2):S109–13.10.1093/geronb/60.Special_Issue_2.S109Search in Google Scholar
[28] Umberson D, Williams K, Powers DA, Liu H, Needham B. You make me sick: Marital quality and health over the life course. J Health Soc Behav. 2006;47(1):1–16.10.1177/002214650604700101Search in Google Scholar PubMed PubMed Central
[29] Tepeli Temiz Z, Elsharnouby E. Relationship satisfaction and well-being during the COVID-19 pandemic: Examining the associations with interpersonal emotion regulation strategies. Cognit Ther Res. 2022;46(5):902–15.10.1007/s10608-022-10317-wSearch in Google Scholar PubMed PubMed Central
[30] Demir M, Park S. The effect of COVID-19 restrictions on calls for service on drugs, alcohol, and mental health. Am J Crim Just. 2024;50:253–81.10.1007/s12103-024-09783-7Search in Google Scholar
[31] Ogeil RP, McGrath M, Grigg J, Peart A, Meddings JI, Greenwood CJ, et al. Diverging trends in alcohol-related harms: The role of comorbid mental health, suicide and self-harm behaviors in ambulance attendances for alcohol intoxication during the COVID-19 pandemic in Victoria, Australia. J Affect Disord. 2025;371:170–6.10.1016/j.jad.2024.11.012Search in Google Scholar PubMed
[32] Botella-Juan L, Vargas-Caraballo D, Molina AJ, Hernández-Segura N, Fernández-Villa T. Impact of the COVID-19 pandemic on alcohol consumption in young adults: A systematic review. Public Health. 2025;240:1–11.10.1016/j.puhe.2025.01.004Search in Google Scholar PubMed
[33] Golestaneh L, Neugarten J, Fisher M, Billett HH, Gil MR, Johns T, et al. The association of race and COVID-19 mortality. EClinicalMedicine. 2020;25:100455.10.1016/j.eclinm.2020.100455Search in Google Scholar PubMed PubMed Central
[34] CDC. People with Certain Medical Conditions and COVID-19 Risk Factors; 2025 https://www.cdc.gov/covid/risk-factors/index.html.Search in Google Scholar
[35] Chung RY-N, Dong D, Li MM. Socioeconomic gradient in health and the covid-19 outbreak. BMJ. 2020;369:m1329.10.1136/bmj.m1329Search in Google Scholar PubMed
[36] Dunlop A, Lokuge B, Masters D, Sequeira M, Saul P, Dunlop G, et al. Challenges in maintaining treatment services for people who use drugs during the COVID-19 pandemic. Harm Reduct J. 2020;17(1):26.10.1186/s12954-020-00370-7Search in Google Scholar PubMed PubMed Central
[37] Dodds C, Fakoya I. Covid-19: ensuring equality of access to testing for ethnic minorities. BMJ. 2020;369:m2122.10.1136/bmj.m2122Search in Google Scholar PubMed
[38] Maisel NC, Karney BR. Socioeconomic status moderates associations among stressful events, mental health, and relationship satisfaction. J Family Psychol. 2012;26(4):654.10.1037/a0028901Search in Google Scholar PubMed
[39] Kozák M, Bakken A, von Soest T. Psychosocial well-being before, during and after the COVID-19 pandemic: a nationwide study of more than half a million Norwegian adolescents. Nat Ment Health. 2023;1(7):501–13.10.1038/s44220-023-00088-ySearch in Google Scholar
[40] SAMHSA. CSAT GPRA Client Outcome Measures Tool; 2022 https://spars.samhsa.gov/content/new-1212023-csat-gpra-client-outcome-measures-tool.Search in Google Scholar
[41] Office UGA. Government performance and results act. Washington DC: Government Printing Office; 1993.Search in Google Scholar
[42] Babor TF, Higgins-Biddle JC, Saunders JB, Monteiro MG. The alcohol use disorders identification test. Guidelines for use in primary care. 2 edn. Geneva: World Health Organization; 2001.Search in Google Scholar
[43] Skinner HA. The drug abuse screening test. Addict Behav. 1982;7(4):363–71.10.1016/0306-4603(82)90005-3Search in Google Scholar PubMed
[44] Fairchild AJ, MacKinnon DP. A general model for testing mediation and moderation effects. Prev Sci. 2009;10(2):87–99.10.1007/s11121-008-0109-6Search in Google Scholar PubMed PubMed Central
[45] Geranios K, Kagabo R, Kim J. Impact of COVID-19 and socioeconomic status on delayed care and unemployment. Health Equity. 2022;6(1):91–7. 10.1089/heq.2021.0115.Search in Google Scholar PubMed PubMed Central
[46] Masterson JM, Luu M, Dallas KB, Daskivich LP, Spiegel B, Daskivich TJ. Disparities in COVID-19 disease incidence by income and vaccination coverage – 81 communities, Los Angeles, California, July 2020–September 2021. MMWR Morb Mortal Wkly Rep. 2023;72:728–31. 10.15585/mmwr.mm7226a5.Search in Google Scholar PubMed PubMed Central
[47] Faraway JJ. Extending the linear model with R: generalized linear, mixed effects and nonparametric regression models. New York: Chapman and Hall/CRC; 2016.10.1201/9781315382722Search in Google Scholar
[48] Koopman J, Howe M, Hollenbeck JR, Sin H-P. Small sample mediation testing: misplaced confidence in bootstrapped confidence intervals. J Appl Psychol. 2015;100(1):194.10.1037/a0036635Search in Google Scholar PubMed
[49] Czeisler MÉ. Mental health, substance use, and suicidal ideation during the COVID-19 pandemic – United States, June 24–30, 2020. MMWR Morbidity Mortal Wkly Rep. 2020;69(32):1049–57.10.15585/mmwr.mm6932a1Search in Google Scholar PubMed PubMed Central
[50] Schmid L, Wörn J, Hank K, Sawatzki B, Walper S. Changes in employment and relationship satisfaction in times of the COVID-19 pandemic: Evidence from the German family Panel. Eur Societies. 2021;23(S1):S743–58.10.1080/14616696.2020.1836385Search in Google Scholar
[51] Williamson HC, Karney BR, Bradbury TN. Financial strain and stressful events predict newlyweds’ negative communication independent of relationship satisfaction. J Family Psychol. 2013;27(1):65–75.10.1037/a0031104Search in Google Scholar PubMed PubMed Central
[52] Neff LA, Karney BR. How does context affect intimate relationships? Linking external stress and cognitive processes within marriage. Personality Soc Psychol Bull. 2004;30(2):134–48.10.1177/0146167203255984Search in Google Scholar PubMed
[53] Pietromonaco PR, Overall NC. Applying relationship science to evaluate how the COVID-19 pandemic may impact couples’ relationships. Am Psychologist. 2021;76(3):438–50.10.1037/amp0000714Search in Google Scholar PubMed
[54] Kilian C, Rehm J, Allebeck P, Braddick F, Gual A, Barták M, et al. Alcohol consumption during the COVID‐19 pandemic in Europe: a large‐scale cross‐sectional study in 21 countries. Addiction. 2021;116(12):3369–80.10.1111/add.15530Search in Google Scholar PubMed
[55] Sohi I, Chrystoja BR, Rehm J, Wells S, Monteiro M, Ali S, et al. Changes in alcohol use during the COVID‐19 pandemic and previous pandemics: A systematic review. Alcohol: Clin Exp Res. 2022;46(4):498–513.10.1111/acer.14792Search in Google Scholar PubMed PubMed Central
[56] Roberts A, Rogers J, Mason R, Siriwardena AN, Hogue T, Whitley GA, et al. Alcohol and other substance use during the COVID-19 pandemic: A systematic review. Drug Alcohol Dependence. 2021;229:109150.10.1016/j.drugalcdep.2021.109150Search in Google Scholar PubMed PubMed Central
[57] Hull JG, Bond CF. Social and behavioral consequences of alcohol consumption and expectancy: a meta-analysis. Psychol Bull. 1986;99(3):347.10.1037//0033-2909.99.3.347Search in Google Scholar
[58] Panchal N, Kamal R, Orgera K, Cox C, Garfield R, Hamel L, et al. The implications of COVID-19 for mental health and substance use. Kais Family Found. 2020;21:1–16.Search in Google Scholar
[59] Wanberg CR, Csillag B, Douglass RP, Zhou L, Pollard MS. Socioeconomic status and well-being during COVID-19: A resource-based examination. J Appl Psychol. 2020;105(12):1382–96.10.1037/apl0000831Search in Google Scholar PubMed PubMed Central
[60] Uzun H, Karaca NH, Metin Ş. Assesment of parent-child relationship in Covid-19 pandemic. Child Youth Serv Rev. 2021;120:105748.10.1016/j.childyouth.2020.105748Search in Google Scholar
[61] Manchia M, Gathier AW, Yapici-Eser H, Schmidt MV, de Quervain D, van Amelsvoort T, et al. The impact of the prolonged COVID-19 pandemic on stress resilience and mental health: A critical review across waves. Eur Neuropsychopharmacol. 2022;55:22–83.10.1016/j.euroneuro.2021.10.864Search in Google Scholar PubMed PubMed Central
[62] Paulhus DL, Vazire S. The self-report method. Handb Res Methods Personality Psychol. 2007;1(2007):224–39.Search in Google Scholar
[63] Del Boca FK, Darkes J. The validity of self‐reports of alcohol consumption: state of the science and challenges for research. Addiction. 2003;98:1–12.10.1046/j.1359-6357.2003.00586.xSearch in Google Scholar PubMed
[64] Warnecke RB, Johnson TP, Chávez N, Sudman S, O’Rourke DP, Lacey L, et al. Improving question wording in surveys of culturally diverse populations. Ann Epidemiol. 1997;7(5):334–42.10.1016/S1047-2797(97)00030-6Search in Google Scholar
© 2025 the author(s), published by De Gruyter
This work is licensed under the Creative Commons Attribution 4.0 International License.
Articles in the same Issue
- Research Articles
- Relationship between body mass index and quality of life, use of dietary and physical activity self-management strategies, and mental health in individuals with polycystic ovary syndrome
- Evaluating the challenges and opportunities for diabetes care policy in Nigeria
- Body mass index is associated with subjective workload and REM sleep timing in young healthy adults
- Prediction of hypoglycaemia in subjects with type 1 diabetes during physical activity
- Investigation by the Epworth Sleepiness Scale of daytime sleepiness in professional drivers during work hours
- Understanding public awareness of fall epidemiology in the United States: A national cross-sectional study
- Impact of Covid-19 stress on urban poor in Sylhet Division, Bangladesh: A perception-based assessment
- Impact of the COVID-19 pandemic on mental health, relationship satisfaction, and socioeconomic status: United States
- Psychological factors influencing oocyte donation: A study of Indian donors
- Cervical cancer in eastern Kenya (2018–2020): Impact of awareness and risk perception on screening practices
- Older LGBTQ+ and blockchain in healthcare: A value sensitive design perspective
- Trends and disparities in HPV vaccination among U.S. adolescents, 2018–2023
- Do cell towers help increase vaccine uptake? Evidence from Côte d’Ivoire
- In search of the world’s most popular painkiller: An infodemiological analysis of Google Trend statistics from 2004 to 2023
- Brain fog in chronic pain: A concept analysis of social media postings
- Association between multidimensional poverty intensity and maternal mortality ratio in Madagascar: Analysis of regional disparities
- A “disorder that exacerbates all other crises” or “a word we use to shut you up”? A critical policy analysis of NGOs’ discourses on COVID-19 misinformation
- Smartphone use and stroop performance in a university workforce: A survey-experiment
- Review Articles
- The management of body dysmorphic disorder in adolescents: A systematic literature review
- Navigating challenges and maximizing potential: Handling complications and constraints in minimally invasive surgery
- Examining the scarcity of oncology healthcare providers in cancer management: A case study of the Eastern Cape Province, South Africa
- Dietary strategies for irritable bowel syndrome: A narrative review of effectiveness, emerging dietary trends, and global variability
- The impact of intimate partner violence on victims’ work, health, and wellbeing in OECD countries (2014–2025): A descriptive systematic review
- Nutrition literacy in pregnant women: a systematic review
- Short Communications
- Experience of patients in Germany with the post-COVID-19 vaccination syndrome
- Five linguistic misrepresentations of Huntington’s disease
- Letter to the Editor
- PCOS self-management challenges transcend BMI: A call for equitable support strategies
Articles in the same Issue
- Research Articles
- Relationship between body mass index and quality of life, use of dietary and physical activity self-management strategies, and mental health in individuals with polycystic ovary syndrome
- Evaluating the challenges and opportunities for diabetes care policy in Nigeria
- Body mass index is associated with subjective workload and REM sleep timing in young healthy adults
- Prediction of hypoglycaemia in subjects with type 1 diabetes during physical activity
- Investigation by the Epworth Sleepiness Scale of daytime sleepiness in professional drivers during work hours
- Understanding public awareness of fall epidemiology in the United States: A national cross-sectional study
- Impact of Covid-19 stress on urban poor in Sylhet Division, Bangladesh: A perception-based assessment
- Impact of the COVID-19 pandemic on mental health, relationship satisfaction, and socioeconomic status: United States
- Psychological factors influencing oocyte donation: A study of Indian donors
- Cervical cancer in eastern Kenya (2018–2020): Impact of awareness and risk perception on screening practices
- Older LGBTQ+ and blockchain in healthcare: A value sensitive design perspective
- Trends and disparities in HPV vaccination among U.S. adolescents, 2018–2023
- Do cell towers help increase vaccine uptake? Evidence from Côte d’Ivoire
- In search of the world’s most popular painkiller: An infodemiological analysis of Google Trend statistics from 2004 to 2023
- Brain fog in chronic pain: A concept analysis of social media postings
- Association between multidimensional poverty intensity and maternal mortality ratio in Madagascar: Analysis of regional disparities
- A “disorder that exacerbates all other crises” or “a word we use to shut you up”? A critical policy analysis of NGOs’ discourses on COVID-19 misinformation
- Smartphone use and stroop performance in a university workforce: A survey-experiment
- Review Articles
- The management of body dysmorphic disorder in adolescents: A systematic literature review
- Navigating challenges and maximizing potential: Handling complications and constraints in minimally invasive surgery
- Examining the scarcity of oncology healthcare providers in cancer management: A case study of the Eastern Cape Province, South Africa
- Dietary strategies for irritable bowel syndrome: A narrative review of effectiveness, emerging dietary trends, and global variability
- The impact of intimate partner violence on victims’ work, health, and wellbeing in OECD countries (2014–2025): A descriptive systematic review
- Nutrition literacy in pregnant women: a systematic review
- Short Communications
- Experience of patients in Germany with the post-COVID-19 vaccination syndrome
- Five linguistic misrepresentations of Huntington’s disease
- Letter to the Editor
- PCOS self-management challenges transcend BMI: A call for equitable support strategies


