Abstract
Objectives
To analyze pregnancy outcomes and factors influencing early-onset intrahepatic cholestasis of pregnancy (ICP), offering insights to improve the management, diagnosis, and treatment of ICP during pregnancy.
Methods
We categorized 127 pregnant women with ICP into two groups based on a gestational age cutoff of 28 weeks. The analysis centered on biochemical markers, pregnancy complications, and outcomes to identify factors influencing early-onset ICP.
Results
We found that biochemical markers including alanine aminotransferase, aspartate aminotransferase, gamma-glutamyl transferase (GGT), alkaline phosphatase, total bilirubin, direct bilirubin (DBIL), indirect bilirubin, and cholesterol were significantly lower in early-onset ICP compared to late-onset ICP. Importantly, premature birth rates were higher in the early-onset ICP group. Through univariate and multivariate logistic regression analyses of these biochemical markers, GGT and DBIL emerged as significant predictive factors (OR=0.84 and 0.54).
Conclusions
Early-onset ICP is characterized by its early onset, prolonged duration, and a higher incidence of premature births compared to late-onset ICP, leading to adverse perinatal outcomes. This research underscores the protective role of GGT and DBIL in early-onset ICP.
Introduction
Intrahepatic cholestasis of pregnancy (ICP) typically occurs during the third trimester and shows significant regional and ethnic variations in incidence rates [1]. Globally, ICP incidence ranges from 0.2 to 2 %, with higher rates observed in specific regions of South America, Northern Europe, and China [2], [3], [4]. The main clinical manifestations of ICP include pruritus (itching) and elevated bile acid levels, sometimes accompanied by abnormal liver function tests. Postpartum, both symptoms and biochemical abnormalities associated with ICP generally resolve. Despite a favorable maternal prognosis, ICP can lead to serious short-term and long-term complications for the fetus, such as distress, preterm birth, growth restriction, and in severe cases, sudden or stillbirth [1].
Recent clinical studies have identified an increasing incidence of early-onset ICP, prompting exploration into its clinical characteristics and perinatal outcomes [5], 6]. However, research in this area remains limited. There is no consensus on the gestational week threshold defining early-onset ICP. While some researchers classify early-onset ICP as occurring before the 28th week of gestation, others suggest thresholds at 32 or 34 weeks [7], [8], [9], [10]. Pan Yue’s research indicates that significant differences exist in serum biochemical indicators and perinatal outcomes among patients whose ICP onset occurs around 28 weeks of gestation. In contrast, no significant differences are observed among patients whose ICP onset occurs around 32 weeks [11]. Nevertheless, early detection and precise definition of early-onset ICP are critical for effective clinical management.
In our study, we used the 28-week gestational mark as the cutoff to examine differences in biochemical markers, incidence of pregnancy complications, and outcomes between early- and late-onset ICP. Additionally, we explored factors influencing adverse pregnancy outcomes among women with early-onset ICP. This research aims to offer clinicians insights to improve management, diagnosis, and treatment strategies for ICP, with the goal of reducing its adverse effects on pregnancy outcomes.
Materials and methods
Patients selection
In this study, 127 pregnant women with singleton pregnancies diagnosed with ICP were included, who were admitted to and delivered at Fujian Provincial Maternity and Children's Hospital Hospital from January 1, 2022, to December 31, 2022. The research protocol received ethical approval from the Ethics Committee of Fujian Provincial Maternity and Children’s Hospital (approval date: February 24, 2023; reference number: 2023YJ003). All participants provided informed consent for data collection.
Inclusion criteria, exclusion criteria, and ICP grading
Inclusion criteria
Diagnosis and classification of ICP followed the 2015 guidelines set by the Chinese Medical Association of Obstetrics and Gynecology. Diagnostic criteria included unexplained skin itching, fasting total bile acids ≥10 μmol/L, unexplained liver function abnormalities with normal bile acid levels, mild to moderate elevation in serum alanine aminotransferase (ALT) and aspartate aminotransferase (AST) levels potentially accompanied by increased gamma-glutamyl transferase (GGT) and bilirubin levels, and resolution of skin itching and liver function normalization after delivery.
Exclusion criteria
Cases with incomplete medical records, twin pregnancies, and pregnancies complicated by medical or surgical conditions such as hypertension, primary liver disease, scarred uterus, and central placenta previa were excluded.
ICP grading
Mild ICP was defined as total serum bile acid levels ranging from 10 to 39.9 μmol/L, with pruritus as the primary symptom, with no other symptoms. Severe ICP was characterized by total serum bile acid levels of ≥40 μmol/L, often accompanied by factors such as multiple pregnancy, hypertensive disorders, recurrent ICP, history of stillbirth due to ICP, or neonatal asphyxia.
Research methods
The 127 pregnant women were categorized into two groups based on the gestational age at onset of ICP: Group A (early-onset ICP, <28 weeks) comprised 71 cases, and Group B (late-onset ICP, ≥28 weeks) comprised 56 cases. General characteristics, biochemical markers, the occurrence of pregnancy complications, and pregnancy outcomes for both groups were examined.
The collected data encompassed variables such as age, gravida, para, body mass index, weight gain during pregnancy, history of ICP, smoking status, pruritus symptoms, and biochemical markers (ALT, AST, GGT, alkaline phosphatase [ALP], total bilirubin [TBIL], direct bilirubin [DBIL], indirect bilirubin [IBIL], total bile acids [TBA], and cholesterol [CHOL]). Additionally, information on the incidence of pregnancy complications (e.g., gestational hypertension, preeclampsia, gestational diabetes mellitus, fetal growth restriction [FGR], premature rupture of membranes, placental abruption) and pregnancy outcomes (e.g., premature delivery, cesarean section, meconium-stained amniotic fluid, fetal distress, postpartum hemorrhage, neonatal birth weight) was recorded. Observational parameters, such as rates of cesarean section, premature delivery, meconium-stained amniotic fluid, fetal distress, postpartum hemorrhage, neonatal asphyxia, and neonatal birth weight, were also documented for both groups.
Univariate logistic analysis was performed on these biochemical markers to identify significant factors, which were subsequently included in a multivariate logistic regression analysis to ascertain the influential factors of early-onset ICP. The flow diagram is shown in Figure 1.
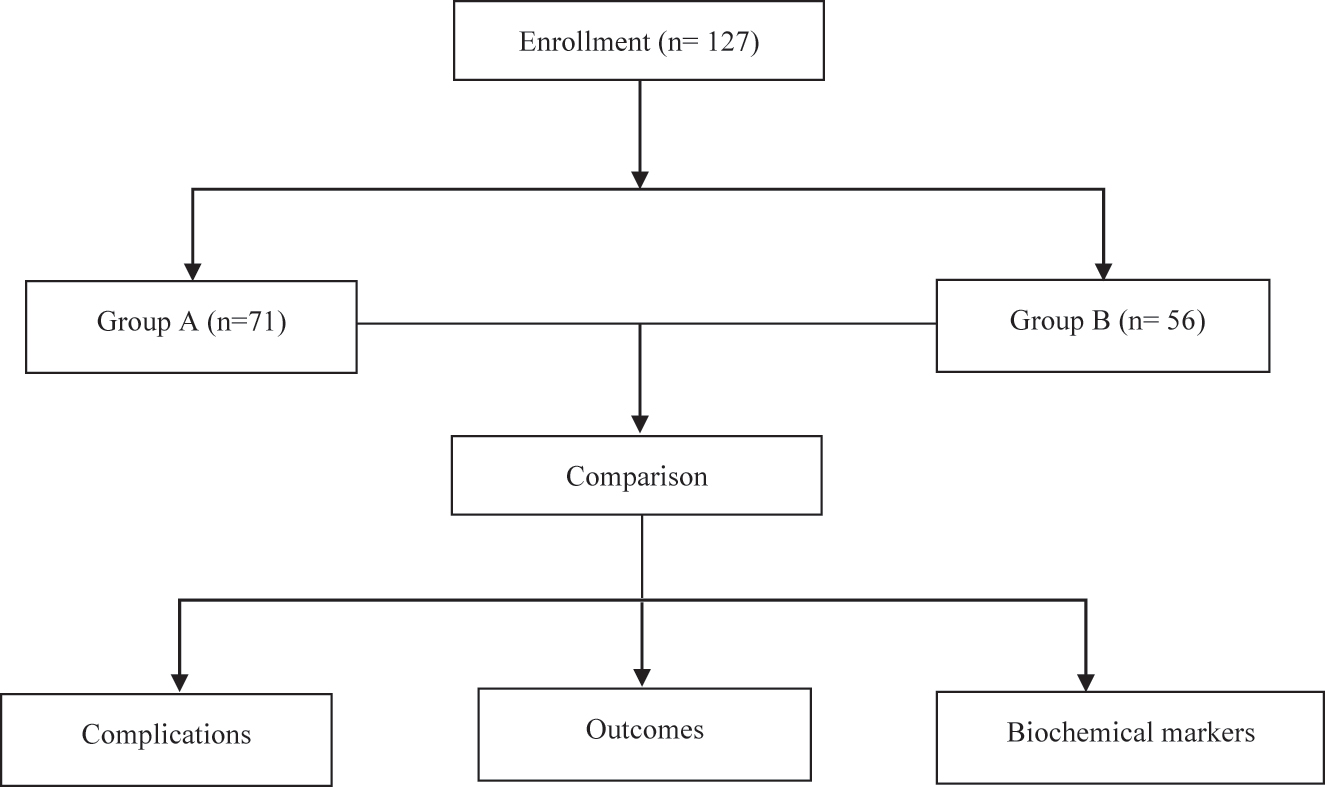
Flow diagram of the present study.
Statistical analysis
All data were analyzed using SPSS version 25.0. Measurement data were initially assessed for normal distribution and reported as mean±standard deviation if normally distributed, or as median and interquartile range if not. For normally distributed data with homogeneous variance, a t-test was used. When the data were not normally distributed, the Mann-Whitney U test (Wilcoxon rank-sum test) was applied to compare differences between two groups. Categorical data were analyzed using the chi-squared (χ2) test. Multivariate logistic regression analysis was conducted to identify factors influencing early-onset ICP, with variable selection performed using stepwise selection (both forward and backward) based on the Akaike Information Criterion (AIC). Statistical significance was set at p<0.05.
Results
The comparison of general data and biochemical markers between early- and late-onset ICP is detailed in Tables 1 and 2, respectively. The analysis revealed no significant differences in age, parity, body mass index, weight gain during pregnancy, history of ICP, pruritus symptoms, or other markers between the two groups. However, levels of ALT, AST, GGT, ALP, TBIL, DBIL, and IBIL were significantly lower in the early-onset ICP group compared to the late-onset group. Although there was no significant difference in TBA levels between the two groups, the early-onset ICP group had higher TBA levels than the late-onset group. Levels of CHOL were similar between both groups.
Summary of enrolled pregnant women: comparative data between early-onset and late-onset intrahepatic cholestasis of pregnancy (Groups A and B).
| Group A (n=71) | Group B (n=56) | t or χ2 | p-Value | |
|---|---|---|---|---|
| Age, years | 30.59±4.15 | 30.25±3.95 | 0.47 | 0.63 |
| Gravida (times) | 2 [1, 2] | 1 [1, 2] | −1.02 | 0.30 |
| Para (times) | 0 [0, 1] | 0 [0, 1] | −1.57 | 0.11 |
| Body mass index, kg/m2 | 20.24±2.72 | 20.81±3.74 | −0.99 | 0.32 |
| Weight gain during pregnancy, kg | 12.07±3.61 | 11.82±3.65 | 0.38 | 0.70 |
| ICP medical history, n (%) | 2 (2.8 %) | 1 (1.8 %) | 0 | 1 |
| Pruritus symptoms, n (%) | 1 (1.4 %) | 5 (8.9 %) | 3.55 | 0.06 |
-
ICP, intrahepatic cholestasis of pregnancy.
Comparison of biochemical markers between early-onset and late-onset intrahepatic cholestasis of pregnancy (Groups A and B).
| Group A (n=71) | Group B (n=56) | t or U | p-Value | |
|---|---|---|---|---|
| ALT | 10.65 [8.25, 14.87] | 14.90 [10, 24.40] | 1,398.5 | 0.004b |
| AST | 15.70 [13.47, 18.78] | 18.80 [14.40, 26.60] | 1,344.5 | 0.002b |
| GGT | 9.15 [7.80, 11.52] | 15.40 [8.70, 26.80] | 1,107.0 | <0.0001 |
| ALP | 152.42±49.08 | 189.39±66.46 | −3.53 | <0.001 |
| TBIL | 6.86±2.82 | 9.21±5.21 | −3.15 | 0.002b |
| DBIL | 1.88±1.06 | 3.14±2.5 | −3.73 | <0.001 |
| IBIL | 4.98±2.34 | 6.07±3.53 | −2.02 | 0.045a |
| TBA | 34.81±24.32 | 27.18±25.18 | 1.72 | 0.09 |
| CHOL | 6.35±1.08 | 6.76±1.15 | −1.97 | 0.05 |
-
ALT, alanine aminotransferase; AST, aspartate aminotransferase; GGT, gamma-glutamyl transferase; ALP, alkaline phosphatase; TBIL, total bilirubin; DBIL, direct bilirubin; IBIL, indirect bilirubin; TBA, total bile acid; CHOL, cholesterol. aRepresentative differences are statistically significant. bRepresentative differences are highly statistically significant.
Comparison of pregnancy complications and pregnancy outcomes between early- and late-onset ICP
Table 3 displays the incidence of pregnancy complications. There were no significant differences between the groups in terms of gestational hypertension, preeclampsia, gestational diabetes mellitus, thyroid disease, liver damage, FGR, placental abruption, premature rupture of membranes, or oligohydramnios. Table 4 displays the rates of cesarean section, premature birth, and fetal distress. The early-onset ICP group showed higher rates in these categories. Specifically, the premature birth rate demonstrated a statistically significant difference. Additionally, neonates in the early-onset ICP group tended to have lower birth weights compared to those in the late-onset group (p-value=0.058).
Comparison of pregnancy complications between early-onset and late-onset intrahepatic cholestasis of pregnancy (Groups A and B).
| Group A (n=71) | Group B (n=56) | p-Value | |
|---|---|---|---|
| Pregnancy-induced hypertension, n (%) | 3 (4.2 %) | 1 (1.8 %) | 0.43 |
| Pre-eclampsia, n (%) | 2 (2.85) | 1 (1.8 %) | 0.7 |
| Gestational diabetes, n (%) | 17 (24 %) | 17 (30 %) | 0.41 |
| Hypothyroidism during pregnancy, n (%) | 4 (5.6 %) | 2 (3.5 %) | 0.58 |
| Hyperthyroidism during pregnancy, n (%) | 0 % | 1 (1.8 %) | 0.25 |
| Thyroiditis during pregnancy, n (%) | 4 (5.6 %) | 3 (5.3 %) | 0.94 |
| Pregnant liver damage, n (%) | 2 (2.8 %) | 5 (8.9 %) | 0.13 |
| FGR, n (%) | 8 (11.3 %) | 3 (5.3 %) | 0.23 |
| Placental abruption, n (%) | 3 (4.2) | 0 % | 0.11 |
| Premature rupture of membranes, n (%) | 7 (10 %) | 9 (16.1 %) | 0.29 |
| Oligohydramnios, n (%) | 2 (2.8 %) | 0 % | 0.2 |
-
FGR, fetal growth restriction.
Comparison of pregnancy outcomes between early-onset and late-onset intrahepatic cholestasis of pregnancy (Groups A and B).
| Group A (n=71) | Group B (n=56) | p-Value | |
|---|---|---|---|
| Caesarean section, n (%) | 33 (46.5 %) | 21 (37.5 %) | 0.31 |
| Premature delivery, n (%) | 12 (16.9 %) | 3 (5.4 %) | 0.049a |
| Fetal distress, n (%) | 6 (8.5 %) | 4 (7.1 %) | 0.78 |
| Postpartum bleeding, n (%) | 0 % | 0 % | 0.11 |
| Amniotic fluid pollution, n (%) | 8 (11.3 %) | 11 (19.6 %) | 0.18 |
| Newborn weight, g | 2,951.9±504.89 | 3,114.29±435.83 | 0.058 |
-
aRepresentative differences have statistical significance.
Comparison of biochemical markers between early- and late-onset ICP
Table 5 shows the results of univariate analysis of biochemical markers, highlighting significant differences in GGT, ALP, TBIL, and DBIL between the two groups of ICP. Subsequently, a multivariate logistic regression analysis was performed with early-onset ICP as the dependent variable and those factors with p<0.20 as independent variables. Table 6 presents the findings from the stepwise selection process (both forward and backward), which identified the most parsimonious model for predicting early-onset ICP. In the multivariate analysis, both GGT (p=0.0009, odds ratio (OR): 0.84, 95 % CI: 0.74–0.92) and DBIL (p=0.005, OR: 0.54, 95 % CI: 0.33–0.80) demonstrated significant predictive value in the final model. Specifically, each unit increase in GGT levels was associated with a 16 % reduction in the risk of early-onset ICP, while each unit increase in DBIL levels was associated with a 46 % reduction in risk.
Univariate logistic regression analysis of biochemical markers linked to early-onset intrahepatic cholestasis of pregnancy.
| Factor | β | SE | Wald χ2 | p-Value | OR | 95 % CI |
|---|---|---|---|---|---|---|
| ALT | 0.44 | 0.0049 | 2.4 | 0.12 | 0.99 | 0.98–1.00 |
| AST | 0.45 | 0.0045 | 2.4 | 0.12 | 0.99 | 0.98–1.00 |
| GGT | −0.37 | 0.17 | 4.4 | 0.034a | 0.69 | 0.46–0.91 |
| ALP | −0.11 | 0.036 | 10 | 0.0015b | 0.89 | 0.82–0.95 |
| TBIL | −0.16 | 0.055 | 7.9 | 0.005b | 0.85 | 0.76–0.95 |
| DBIL | −0.48 | 0.14 | 10.4 | 0.0012b | 0.62 | 0.45–0.81 |
| IBIL | 0.99 | 0.068 | 3.8 | 0.05 | 0.88 | 0.76–0.99 |
| CHOL | 0.33 | 0.17 | 3.7 | 0.05 | 0.71 | 0.50–1.00 |
-
ALT, alanine aminotransferase; AST, aspartate aminotransferase; GGT, gamma-glutamyl transferase; ALP, alkaline phosphatase; TBIL, total bilirubin; DBIL, direct bilirubin; IBIL, indirect bilirubin; CHOL, cholesterol; CI, confidence interval. Odds ratios (ORs) are presented per 10-unit increase in ALP and GGT. aRepresentative differences are statistically significant. bRepresentative differences are highly statistically significant.
Multivariate logistic regression analysis of biochemical markers in early-onset intrahepatic cholestasis of pregnancy.
| Factor | β | SE | Wald χ2 | p-Value | OR | 95 % CI |
|---|---|---|---|---|---|---|
| AST | 0.017 | 0.022 | 0.59 | 0.44 | 1.02 | 0.99–1.06 |
| GGT | −0.18 | 0.053 | 10.93 | <0.001 | 0.84 | 0.74–0.92 |
| DBIL | −0.61 | 0.22 | 7.82 | <0.01 | 0.54 | 0.33–0.80 |
-
AST, aspartate transaminase; GGT, gamma-glutamyl transferase; DBIL, direct bilirubin; SE, standard error; OR, odds ratio; CI, confidence interval.
Discussion
Previously, ICP was predominantly believed to occur in the third trimester, with about 80 % of cases emerging after 30 weeks [5]. However, recent clinical studies indicate a potential earlier onset of ICP during pregnancy, possibly occurring in the early trimesters. Importantly, earlier onset of ICP is associated with elevated bile acid levels and an increased risk of adverse perinatal outcomes [9], [10], [11], [12].
In this analysis, patients with ICP were categorized based on onset at <28 weeks for early-onset ICP and ≥28 weeks for late-onset ICP. Differences in biochemical markers, pregnancy complications, and pregnancy outcomes between the two groups were investigated. Clinically, TBA, ALP, liver enzymes such as ALT and AST, and other biochemical markers are pivotal for diagnosing ICP and assessing prognosis [13]. Bilirubin, due to its cytotoxic nature and interaction with bile acids, remains critical for clinical evaluation. The results revealed significantly lower levels of ALT, AST, GGT, ALP, TBIL, DBIL, and IBIL in the early-onset ICP group compared to the late-onset group. This difference may be attributed to increased estrogen levels in the third trimester, which can exacerbate liver stress. Additionally, TBA levels were generally higher in the early-onset ICP group, potentially contributing to intensified liver cell damage. This could explain the elevated biochemical markers observed more frequently in late-onset ICP compared to early-onset cases.
When comparing pregnancy complications, early-onset ICP showed a tendency toward higher rates of gestational hypertension, preeclampsia, thyroid disorders, FGR, and placental abruption, although these differences did not reach statistical significance between the two groups. Cesarean section rates, fetal distress, postpartum hemorrhage, and amniotic fluid contamination were similar across both groups. Neonatal birth weight was lower in the early-onset ICP group (p-value 0.058), consistent with findings from a meta-analysis suggesting an association between early-onset ICP and reduced neonatal birth weight [14]. This underscores that earlier and prolonged duration of ICP may increase the risk of pregnancy complications and adverse perinatal outcomes.
In addition, ICP increases the risk of preterm birth by 24 %. This heightened risk is likely attributed to elevated blood bile acid levels, which stimulate the release of prostaglandins – a critical factor in inducing labor [15]. Bile acids also enhance the expression of oxytocin receptors and increase the sensitivity of uterine muscle fibers to oxytocin, potentially triggering premature labor [15]. Our findings indicated higher blood bile acid levels in the early-onset ICP group, suggesting a greater susceptibility to preterm birth in these cases. Consequently, ICP significantly impacts fetal health, with prolonged and intensified bile acid production amplifying the risk of adverse perinatal outcomes [16].
Due to the significant impact of ICP on fetuses, the longer and higher the duration and levels of elevated bile acids, the greater the risk of adverse perinatal outcomes for infants. Early identification and management of influencing factors associated with early-onset ICP during pregnancy are crucial for improving maternal and infant outcomes. Therefore, a univariate analysis was conducted on biochemical indicators (ALT, AST, GGT, ALP, TBIL, DBIL, IBIL, CHOL) for the two groups of pregnant women. Significant differences were found in GGT, ALP, TBIL, and DBIL levels between the two groups. Univariate logistic analysis further confirmed the statistical significance of GGT, ALP, TBIL, and DBIL levels. Multivariate logistic regression identified GGT and DBIL as a predictive factors for early-onset ICP.
Elevated ALP and GGT are prominent serum biochemical indicators of cholestasis, with GGT showing earlier and more sustained elevation compared to other liver enzymes, making it highly sensitive in detecting liver dysfunction [17]. GGT is predominantly found in the cytoplasm of liver cells and bile duct epithelial cells, playing a crucial role in liver protein metabolism. It correlates well with various liver and gallbladder disorders, reflecting the extent of liver cell damage. In conditions where liver function is impaired, especially in cases involving bile stasis or biliary obstruction, the accumulation of bile acids in liver cells leads to hepatotoxicity. This results in the release of GGT, ALT, AST, ALP, and bilirubin into the bloodstream, thereby increasing their serum concentrations [18]. Lower levels of GGT were observed in early-onset ICP compared to late-onset cases, in this study. Each unit increase in GGT levels was associated with a 16 % reduction in the risk of early-onset ICP, indicating a protective role. Similarly, each unit increase in DBIL levels was associated with a 46 % reduction in risk, further highlighting the protective effects of these biomarkers. This finding suggests a potential link to elevated estrogen levels in late pregnancy, which may exacerbate liver strain and worsen liver cell damage from bile acids.
Conclusions
Pregnant women with early-onset ICP experience increased risks of preterm birth and poorer perinatal outcomes. Elevated GGT and DBIL levels serve as a predictive marker for early-onset ICP, with each incremental unit decreasing the associated risk. Early identification of factors influencing ICP is vital for timely diagnosis and treatment, improving pregnancy management and mitigating adverse maternal-infant outcomes. However, due to the retrospective design and relatively small sample size of this study, further research with larger cohorts is necessary to gain comprehensive insights.
-
Research ethics: This study was conducted in accordance with the Declaration of Helsinki (as revised in 2013) and approved by the Ethics Committee of Fujian Provincial Maternity and Children’s Hospital (approval number: 2023YJ003).
-
Informed consent: Informed consent was obtained from all individuals included in this study, or their legal guardians or wards.
-
Author contributions: Conception and design of the research: Xiufang Shao, Mian Pan, Acquisition of data: Xiufang Shao, Haiyan Tang, Yingling Xiu, Analysis and interpretation of the data: Yingling Xiu, Kunhai Ren, Statistical analysis: Xiufang Shao, Haiyan Tang, Kunhai Ren, Writing of the manuscript: Xiufang Shao, Yingling Xiu, Critical revision of the manuscript for intellectual content: Mian Pan, All authors have accepted responsibility for the entire content of this manuscript and approved its submission.
-
Use of Large Language Models, AI and Machine Learning Tools: None declared.
-
Conflict of interest: The authors state no conflict of interest.
-
Research funding: None declared.
-
Data availability: The datasets generated and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
1. Williamson, C, Geenes, V. Intrahepatic cholestasis of pregnancy. Obstet Gynecol 2014;124:120–33. https://doi.org/10.1097/AOG.0000000000000346.Suche in Google Scholar PubMed
2. Gao, XX, Ye, MY, Liu, Y, Li, JY, Li, L, Chen, W, et al.. Prevalence and risk factors of intrahepatic cholestasis of pregnancy in a Chinese population. Sci Rep 2020;10:16307. https://doi.org/10.1038/s41598-020-73378-5.Suche in Google Scholar PubMed PubMed Central
3. Gardiner, FW, McCuaig, R, Arthur, C, Carins, T, Morton, A, Laurie, J, et al.. The prevalence and pregnancy outcomes of intrahepatic cholestasis of pregnancy: a retrospective clinical audit review. Obstet Med 2019;12:123–8. https://doi.org/10.1177/1753495X18797749.Suche in Google Scholar PubMed PubMed Central
4. Piechota, J, Jelski, W. Intrahepatic cholestasis in pregnancy: review of the literature. J Clin Med 2020;9:1361. https://doi.org/10.3390/jcm9051361.Suche in Google Scholar PubMed PubMed Central
5. Gabzdyl, EM, Schlaeger, JM. Intrahepatic cholestasis of pregnancy: a critical clinical review. J Perinat Neonatal Nurs 2015;29:41–50. https://doi.org/10.1097/JPN.0000000000000077.Suche in Google Scholar PubMed
6. Jin, J, Pan, SL, Huang, LP, Yu, YH, Zhong, M, Zhang, GW. Risk factors for adverse fetal outcomes among women with early- versus late-onset intrahepatic cholestasis of pregnancy. Int J Gynaecol Obstet 2015;128:236–40. https://doi.org/10.1016/j.ijgo.2014.09.013.Suche in Google Scholar PubMed
7. Chao, TT, Sheffield, JS. Primary dermatologic findings with early-onset intrahepatic cholestasis of pregnancy. Obstet Gynecol 2011;117:456–8. https://doi.org/10.1097/AOG.0b013e3181f61b11.Suche in Google Scholar PubMed
8. Smolarczyk, R, Grymowicz, M, Sienko, J, Czajkowski, K. Successful perinatal outcome in an early onset intrahepatic cholestasis of pregnancy with extremely high serum hepatic function tests. Gynecol Endocrinol 2009;25:475–6. https://doi.org/10.1080/09513590902945147.Suche in Google Scholar PubMed
9. Lin, J, Gu, W, Hou, Y. Diagnosis and prognosis of early-onset intrahepatic cholestasis of pregnancy: a prospective study. J Matern Fetal Neonatal Med 2019;32:997–1003. https://doi.org/10.1080/14767058.2017.1397124.Suche in Google Scholar PubMed
10. Uyar, I, Gulhan, I, Oztekin, D, Gezer, C, Ekin, A, Karaca Kurtulmus, S, et al.. Intrahepatic cholestasis of pregnancy may lead to low birth weight. Turk J Med Sci 2015;45:723–8. https://doi.org/10.3906/sag-1403-7.Suche in Google Scholar PubMed
11. Pan, Y, Li, EQ. Analysis of biochemical indicators of intrahepatic cholestasis of pregnancy and perinatal prognosis in different gestational weeks. China Fam Plan Obstet Gynecol 2019;11:53–5. https://doi.org/10.3969/j.issn.1674-4020.2019.01.14.Suche in Google Scholar
12. Zhou, L, Qi, HB, Luo, X. Analysis of clinical characteristics and perinatal outcome of early-onset intrahepatic cholestasis of pregnancy. Zhonghua Fu Chan Ke Za Zhi 2013;48:20–4.Suche in Google Scholar
13. Ekiz, A, Kaya, B, Avci, ME, Polat, I, Dikmen, S, Yildirim, G, et al.. Alanine aminotransferase as a predictor of adverse perinatal outcomes in women with intrahepatic cholestasis of pregnancy. Pakistan J Med Sci 2016;32:418–22. https://doi.org/10.12669/pjms.322.9057.Suche in Google Scholar PubMed PubMed Central
14. Li, L, Chen, YH, Yang, YY, Cong, L. Effect of intrahepatic cholestasis of pregnancy on neonatal birth weight: a meta-analysis. J Clin Res Pediatr Endocrinol 2018;10:38–43. https://doi.org/10.4274/jcrpe.4930.Suche in Google Scholar PubMed PubMed Central
15. Germain, AM, Kato, S, Carvajal, JA, Valenzuela, GJ, Valdes, GL, Glasinovic, JC. Bile acids increase response and expression of human myometrial oxytocin receptor. Am J Obstet Gynecol 2003;189:577–82. https://doi.org/10.1067/s0002-9378(03)00545-3.Suche in Google Scholar PubMed
16. Ovadia, C, Seed, PT, Sklavounos, A, Geenes, V, Di Illio, C, Chambers, J, et al.. Association of adverse perinatal outcomes of intrahepatic cholestasis of pregnancy with biochemical markers: results of aggregate and individual patient data meta-analyses. Lancet 2019;393:899–909. https://doi.org/10.1016/S0140-6736(18)31877-4.Suche in Google Scholar PubMed PubMed Central
17. Pieters, A, Gijbels, E, Cogliati, B, Annaert, P, Devisscher, L, Vinken, M. Biomarkers of cholestasis. Biomarkers Med 2021;15:437–54. https://doi.org/10.2217/bmm-2020-0691.Suche in Google Scholar PubMed
18. Smith, DD, Rood, KM. Intrahepatic cholestasis of pregnancy. Clin Obstet Gynecol 2020;63:134–51. https://doi.org/10.1097/GRF.0000000000000495.Suche in Google Scholar PubMed
© 2025 the author(s), published by De Gruyter, Berlin/Boston
This work is licensed under the Creative Commons Attribution 4.0 International License.
Artikel in diesem Heft
- Frontmatter
- Reviews
- AI and early diagnostics: mapping fetal facial expressions through development, evolution, and 4D ultrasound
- Investigation of cardiac remodeling and cardiac function on fetuses conceived via artificial reproductive technologies: a review
- Commentary
- A crisis in U.S. maternal healthcare: lessons from Europe for the U.S.
- Opinion Paper
- Selective termination: a life-saving procedure for complicated monochorionic gestations
- Original Articles – Obstetrics
- Exploring the safety and diagnostic utility of amniocentesis after 24 weeks of gestation: a retrospective analysis
- Maternal and neonatal short-term outcome after vaginal breech delivery >36 weeks of gestation with and without MRI-based pelvimetric measurements: a Hannover retrospective cohort study
- Antepartum multidisciplinary approach improves postpartum pain scores in patients with opioid use disorder
- Determinants of pregnancy outcomes in early-onset intrahepatic cholestasis of pregnancy
- Copy number variation sequencing detection technology for identifying fetuses with abnormal soft indicators: a comprehensive study
- Benefits of yoga in pregnancy: a randomised controlled clinical trial
- Atraumatic forceps-guided insertion of the cervical pessary: a new technique to prevent preterm birth in women with asymptomatic cervical shortening
- Original Articles – Fetus
- Impact of screening for large-for-gestational-age fetuses on maternal and neonatal outcomes: a prospective observational study
- Impact of high maternal body mass index on fetal cerebral cortical and cerebellar volumes
- Adrenal gland size in fetuses with congenital heart disease
- Aberrant right subclavian artery: the importance of distinguishing between isolated and non-isolated cases in prenatal diagnosis and clinical management
- Short Communication
- Trends and variations in admissions for cannabis use disorder among pregnant women in United States
- Letter to the Editor
- Trisomy 18 mosaicism – are we able to predict postnatal outcome by analysing the tissue-specific distribution?
Artikel in diesem Heft
- Frontmatter
- Reviews
- AI and early diagnostics: mapping fetal facial expressions through development, evolution, and 4D ultrasound
- Investigation of cardiac remodeling and cardiac function on fetuses conceived via artificial reproductive technologies: a review
- Commentary
- A crisis in U.S. maternal healthcare: lessons from Europe for the U.S.
- Opinion Paper
- Selective termination: a life-saving procedure for complicated monochorionic gestations
- Original Articles – Obstetrics
- Exploring the safety and diagnostic utility of amniocentesis after 24 weeks of gestation: a retrospective analysis
- Maternal and neonatal short-term outcome after vaginal breech delivery >36 weeks of gestation with and without MRI-based pelvimetric measurements: a Hannover retrospective cohort study
- Antepartum multidisciplinary approach improves postpartum pain scores in patients with opioid use disorder
- Determinants of pregnancy outcomes in early-onset intrahepatic cholestasis of pregnancy
- Copy number variation sequencing detection technology for identifying fetuses with abnormal soft indicators: a comprehensive study
- Benefits of yoga in pregnancy: a randomised controlled clinical trial
- Atraumatic forceps-guided insertion of the cervical pessary: a new technique to prevent preterm birth in women with asymptomatic cervical shortening
- Original Articles – Fetus
- Impact of screening for large-for-gestational-age fetuses on maternal and neonatal outcomes: a prospective observational study
- Impact of high maternal body mass index on fetal cerebral cortical and cerebellar volumes
- Adrenal gland size in fetuses with congenital heart disease
- Aberrant right subclavian artery: the importance of distinguishing between isolated and non-isolated cases in prenatal diagnosis and clinical management
- Short Communication
- Trends and variations in admissions for cannabis use disorder among pregnant women in United States
- Letter to the Editor
- Trisomy 18 mosaicism – are we able to predict postnatal outcome by analysing the tissue-specific distribution?

