Breast cancer risk factors in Iran: a systematic review & meta-analysis
-
Amir Shamshirian
, Keyvan Heydari
, Zahra Shams
, Danial Shamshirian
, Omid Reza Tamtaji
, Zatollah Asemi
, Layla Shojaie
, Neda Mohammadi
, Keyvan Karimifar
and Reza Alizadeh-Navaei
Abstract
Objectives
Breast cancer is known as one of the deadliest forms of cancer, and it is increasing globally. There are a variety of proven and controversial risk factors for this malignancy. Herein, we aimed to undertake a systematic review and meta-analysis focus on the epidemiology of breast cancer risk factors in Iran.
Methods
We performed a systematic search via PubMed, Scopus, Web of Science, and Persian databases for identifying studies published on breast cancer risk factors up to March 2019. Meta-analyses were done for risk factors reported in more than one study. We calculated odds ratios (ORs) with corresponding 95% confidence intervals (CIs) using a fixed/random-effects models.
Results
Thirty-nine studies entered into the meta-analysis. Pooling of ORs showed a significant harmful effect for risk factors including family history (OR: 1.80, 95%CI 1.47–2.12), hormonal replacement therapy (HRT) (OR: 5.48, 95%CI 0.84–1.74), passive smokers (OR: 1.68, 95%CI 1.34–2.03), full-term pregnancy at age 30 (OR: 3.41, 95%CI 1.19–5.63), abortion (OR: 1.84, 95%CI 1.35–2.33), sweets consumption (OR: 1.71, 95%CI 1.32–2.11) and genotype Arg/Arg (crude OR: 1.59, 95%CI 1.07–2.10), whereas a significant protective effect for late menarche (OR: 0.58, 95%CI 0.32–0.83), nulliparity (OR: 0.68, 95%CI 0.39–0.96), 13–24 months of breastfeeding (OR: 0.68, 95%CI 0.46–0.90), daily exercise (OR: 0.59, 95%CI 0.44–0.73) and vegetable consumption (crude OR: 0.28, 95%CI 0.10–0.46).
Conclusions
This study suggests that factors such as family history, HRT, passive smokers, late full-term pregnancy, abortion, sweets consumption and genotype Arg/Arg might increase risk of breast cancer development, whereas late menarche, nulliparity, 13–24 months breastfeeding, daily exercise and vegetable consumption had an inverse association with breast cancer development.
Introduction
Breast cancer is one of the most common health concerns throughout the world [1], [2], [3], [4], which includes 30% of female cancers [5], [6]. It is also known as the second cause of death in developed countries and the third leading cause of death in less developed countries [7], [8], [9]. Surprisingly, approximately 502,000 women die due to breast cancer annually [10]. According to the World Health Organization (WHO) prediction, up to 2.3 million women will be diagnosed for breast cancer by 2050 [11], [12].
In Iran, breast cancer has been identified as the most common cancer and also the fifth main cause of death among Iranian women [4], [13]. The standardized incidence rate (ASR) is about 28 per 100,000 people, which has increased in recent years [14]. There are a variety of proven and controversial risk factors for breast cancer. The American Cancer Society has reported that only about a quarter of breast cancers are due to identified risk factors. These factors include aging, urban life, social class (upper-middle class), marital status (single), white race, history of ovarian cancer, early menarche age, late menopause age, history of breast cancer, history of fibrocystic breast disease, family history of breast, uterine and ovarian cancers, and history of radiation exposure. However, it seems that numerous factors have not yet been identified [15].
According to the Iran, aging, history of breast cancer, genetic modification, chest radiation therapy, diethylstilbestrol (DES) intervention, using hormonal replacement therapy (HRT), low levels of vitamin D, exposure to chemicals in cosmetics, diet, obesity [16], smoking [17], alcohol, fertility and hormonal factors, contraceptives, early menarche, late menopause, high age at first birth, absence of labor history, other malignancies such as ovarian and endometrial carcinoma, are all the most commonly reported risk factors for breast cancer [18], [19].
Considering the incidence and prevalence of breast cancer, the high cost of treatment, risk of involvement in women who are productive in social and socioeconomic settings (>35-year-old) and lack of national screening or early diagnosis, breast cancer is an important subject, the importance of which is reported widely [20], [21], [22], [23].
Despite the importance of the associated risk factors with this malignancy, there is no nationwide study in this regard according to our knowledge. Hence, we aimed to undertake a systematic review and meta-analysis focus on the epidemiology of breast cancer risk factors in Iran. We hope our findings could provide a comprehensive report to be useful for future studies.
Method
Search strategy
We followed Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guideline for study design, search protocol, screening, and reporting. A systematic search was performed via international databases of PubMed, Scopus, and Web of Science until 05 March 2019. Moreover, for finding Persian papers, we used Google Scholar database and national databases of Scientific Information Database (SID), Iranmedex, and Magiran. The search strategy included MeSH terms and free keywords as follows: ((Breast OR Mammary) AND (Cancer* OR Neoplasm* OR Tumor* OR Malignancy* OR Carcinoma*) AND (“Risk factor” OR “Risk factors” OR “Population at Risk” OR “Populations at Risk”) AND AND Iran). Persian equivalent words were used for searching in national databases. There was no limitation about the date of publications in our search.
Criteria study selection
Two group members (A.SH and K.HD) selected the papers independently and discussed to solve the disagreements. Studies met the following criteria included in the meta-analysis: (1) comparative studies with a control group such as case-control and cross-sectional; and (2) studies reported the risk factors of female breast cancer patients in Iran. Studies were excluded if they were: (1) conference abstracts, comments, letters, animal studies, reviews, case reports, and in vitro studies; (2) duplicate publications; and (3) included insufficient data for calculating desired parameters.
Data extraction & quality assessment
Two researchers (Z.SH and K.HD) have independently evaluated the quality of studies and extracted data from included papers. The supervisor (R.AN) resolved any disagreements in this part. Data extraction checklist included the name of the first author, publication year, a region of study, number of patients, mean age, quantitative information of risk factors, clinicopathological features, and available correlations.
The Newcastle-Ottawa Scale (NOS) checklist was used to value the selected papers in relation to various aspects of the methodology and study process.
Data analysis
Statistical analysis was performed using STATA v.11 software. To assess the heterogeneities, we used the I-square (I2) test. According to the studies heterogeneity, we pooled results using a fixed-effects or random-effects model as appropriate for heterogeneity more or less than 50%, respectively.
Results
Study selection process
Our initial search through databases resulted in 562 papers. After excluding duplicated papers, remained papers screened using title and abstract. Finally, after eligibility assessment of 84 full texts, 41 studies entered into qualitative synthesis, and finally, 39 studies entered into the meta-analysis. PRISMA flow diagram for the study selection process is presented in Figure 1.
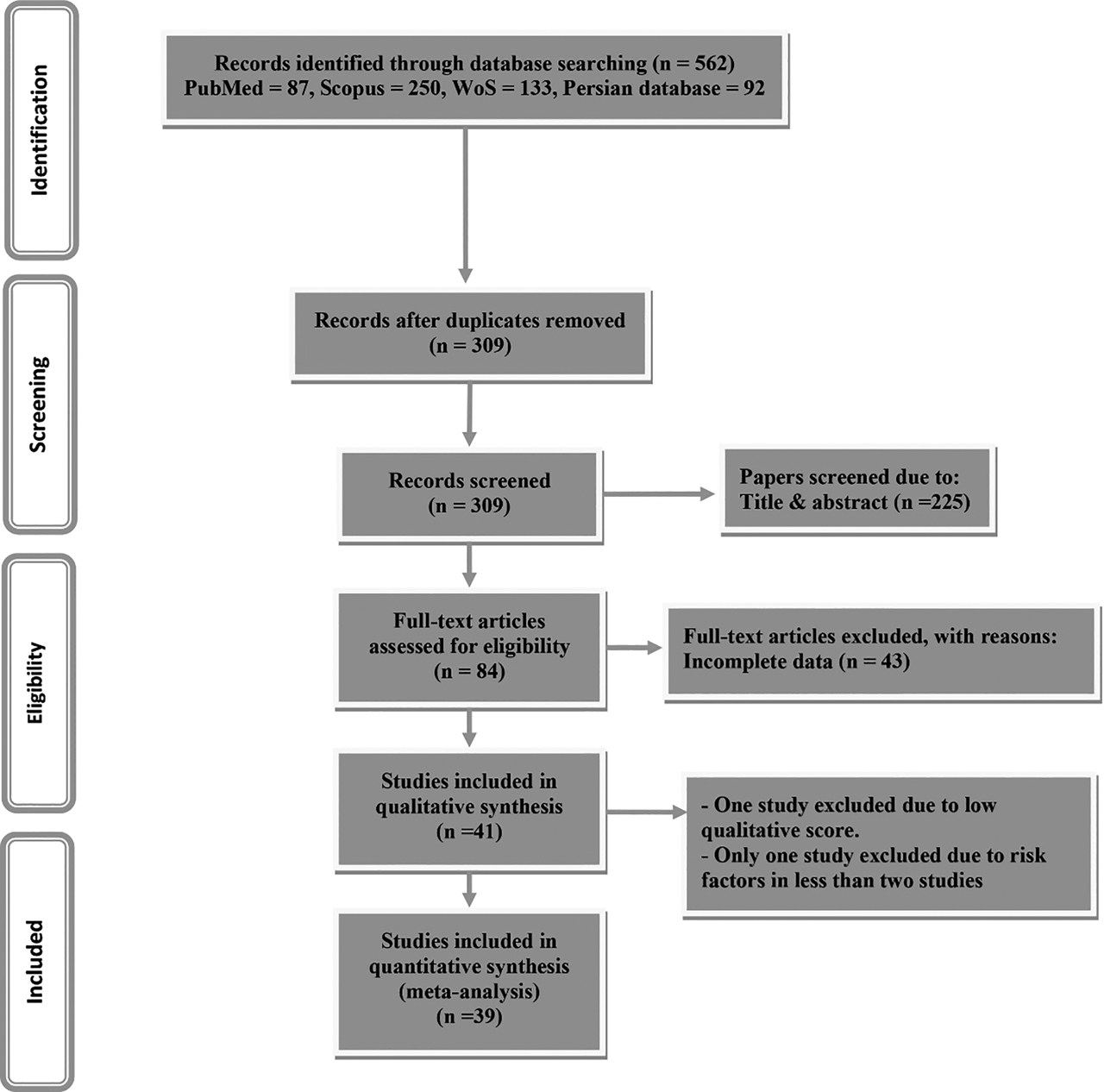
PRISMA flowchart for study selection process.
Study characteristics
Out of 39 included studies, 35 studies were case-control, and four of them were cross-sectional studies. The studies’ sample size ranged from 93 to 25,592, including 54,347 participants. Nine studies were conducted in Tehran province, six in Fars, four in Mazandaran, four in Isfahan, three in East Azerbaijan, two in Guilan, two in Kermanshah, one in West Azerbaijan, one in Golestan, one in Yazd, one in Hormozgan, one in Khuzestan, and one in Razavi Khorasan. Moreover, one study was a joint study between Mazandaran and Guilan, and one study between Tehran and East Azerbaijan. Characteristics of studies entered into meta-analysis presented in Table 1.
Characteristics of studies entered into the systematic review.
| Author, year | Design | Region C/P | No. of participants | Case | Control | Risk factors | Adjusted by |
|---|---|---|---|---|---|---|---|
| (Case/Control) | Mean age, SD | Mean age, SD | |||||
| Ebrahimi et al. (2002) [24] | CC | Tehran C | 535(286/249) | 47.5(12.8) | 44.2(13.2) | Age (+), parity (+), FH (+), OCP (−), MeS (+), MaS (+), ES (+), nulliparity (+), AFFTP (+) | |
| Pesaran et al. (2003) [25] | CC | Isfahan C | 352(176/176) | 49(11.3) | 47(11.4) | FH (+) | |
| Montazeri et al. (2004) [26] | CC | Tehran C | 729(243/486) | 46.6(11.2) | 45.5(10.1) | Age (=), FH (+), OCP (+), MeS (−), MeAS (−), MaS (*), ES (+), depression (+), Hopelessness (+), quality of life (−), AFFTP (+), anxiety (+), psychiatric medications (+) | MeAS, FH, depression and hopelessness |
| Yavari et al. (2005) [27] | CC | Tehran C | 606(303/303) | 48.8(9.8) | 50.2(11.1) | FH (+), PBBD (+), OCP (+), MeS (+), MeAS (+), MaS (+), XE (+), ES (+), parity (+), abortion (−), BF (*) | FH, PBBD, OCP, MeS, MeAS, MaS, XE, ES, abortion, BF |
| Mahouri et al. (2007) [28] | CC | Bandar-Abbas C | 672(168/504) | 48.6(13.7) | 48.4(13.6) | FH (+), PBBD (+), OCP (−), MeS (−), MaS (+), MeAS (+), smoking (+), HRT (+), Nulliparity (+), abortion (+), BF (−), AFFTP (+) | |
| Naieni et al. (2007) [29] | CC | Mazandaran P | 750(250/500) | 48.7(11.3) | 48(11.4) | FH (+), PBBD (+), OCP (+), MeS (+), MeAS (+), smoking (+), ES (+), BMI (+), income (=), SS (=), BF (−), parity (−), IM (+) | Unclear adjustment |
| Lotfi et al. (2008) [30] | CC | Yazd C | 160(80/80) | 48.9(9.7) | 49.1(9.8) | FH (+), OCP (−), MeS (+), MeAS (+), MaS (+), occupation (+), XE (+), PhA (+), ES (+), BMI (+), BF (+), GS (+) | Occupation, FH |
| Kazemi et al. (2009) [31] | CC | Rasht & Tonekabon C | 102(42/60) | TP53 codon 72 polymorphism (+) | |||
| Ghiasvand et al. (2010) [32] | CC | Shiraz C | 1042(521/521) | 41.24 | 41.06 | FH (+), OCP (+), MeAS (−), MaS (+), occupation (+), ES (+), BMI (*), AFFTP (*), parity (−), MA (+) | Age, HP, height, weight, BMI, OCP, BF. MeS, MeAS, ES, MaS |
| Hajian-tilaki and Kaveh-ahangar (2011) [33] | CC | Babol C | 300(100/200) | 51.2(9.6) | 51.1(9.3) | MeS (−), MeAS (*), AFFTP (+), Parity (−), abortion (+), BF (−) | Parity |
| Hajian-tilaki (2011) [34] | CC | Babol C | 300(100/200) | 51.2(9.6) | 51.1(9.3) | ES (−) | Re, MeAS, parity, abortion, MeS, BF, OCP, FH, XE, smoking, exercise, BMI |
| Motie et al. (2011) [35] | CC | Golestan P | 267(134/133) | 47.15(10.36) | 42.96(11.93) | FH (+), XE (*), MaS (+), MeAS (−), PBBD (+), infertility (*) | Unclear adjustment |
| Ghiasvand et al. (2012) [36] | CC | Shiraz C | 986(493/493) | 58.2(7.2) | 58(7.4) | FH (+), OCP (+), MeAS (+), Occupation (+), ES (+), BMI (*) | Age, Re |
| Sigaroodi et al. (2012) [37] | CC | Sari C | 130(79/51) | 47.77(12.55) | 34.2(9.7) | Age (−), human papillomavirus (+) | |
| Ahmadinejad et al. (2013) [38] | CS | Tehran C | 728(184/544) | 48.6(8.3) | Age (*), MeS (−), MaS (−), smoking (−), Parity (−), AFFTP (+), BMI (−), occupation (+) | MeAS, parity, AFD | |
| Kaviani et al. (2013) [39] | CS | Tehran C | 646 | Unclear adjustment | |||
| Pourzand et al. (2013) [40] | CC | Tabriz C | 400(200/200) | 50.05(11.47) | 49.91(11.83) | GS (+), SS (+) | |
| Zare et al. (2013) [41] | CC | Tabriz & Tehran | 25592(111/25481) | 49.18(8.86) | 46.65(9.4) | Age (+), FH (+), occupation (+), OCP (−), MeS (+), MaS (*), HRT (+), ES (*), BMI (*), MA (+) | Age, occupation, ES, BMI, MeS, HRT, OCP |
| Bidgoli and Azarshab (2014) [42] | CC | Sabzevar C | 176(60/116) | 36.45(7.02) | 34.2(5.7) | SLE (−), SI (*), diet (*) | |
| Hosseinzadeh et al. (2014) [43] | CC | Tabriz C | 420(140/280) | 47.6(10.7) | 46.8(10.4) | FH (+), PBBD (+), OCP (+), MeAS (*), MeS (+), MaS (+), smoking (+), PS (+), HRT (+), ES (+), BMI (+), Migration (+), diet (*), nulliparity (+), Abortion (+), BF (−), infertility (+) | MeS, BF, PBBD, MeAS, parity, AFD, abortion, OCP |
| Mobarakeh et al. (2014) [44] | CC | Tehran C | 93(53/40) | 40.02(10.01) | 39.78(11.21) | BMI (+), diet (*) | Age, BMI, ES |
| Sepandi (2014) [45] | CC | Shiraz C | 11850(197/11653) | 49.4(8.7) | 40.9(10.5) | FH (+), OCP (+), MeS (+), MeAS (−), MaS (*), occupation (+), ES (−), BMI (+), Nulliparity (*), parity (*), AFFTP (+) | Age, MeAS, AFP, occupation, parity, FH, BF, OCP |
| Tazhibi et al. (2014) [46] | CC | Isfahan P | 257(216/41) | OCP (−), MeS (+), MaS (+), HRT (+) | Occupation, age, MaS, MeS, OCP, HRT | ||
| Salarabadi et al. (2015) [47] | CC | Kermanshah C | 152(47/105) | Diet (*), SI (+) | |||
| Tajaddini (2015) [48] | CC | Tabriz C | 615(306/309) | 46.4(10.2) | 41.4(9.6) | Diet (*) | Age, MeS, parity, BMI |
| Veisy et al. (2015) [49] | CC | West Azerbaijan P | 194(111/830) | 47.6 | 46.5 | OCP (+), MeAS (*), AFFTP (*) | |
| Ahmadnia et al. (2016) [50] | CC | Guilan P | 450(225/225) | Diet (*) | |||
| Jafari-Mehdiabad et al. (2016) [51] | CC | Isfahan P | 296(98/198) | MaS (+), ES (−), BF (+), income (−) | |||
| Jafarinia et al. (2016) [52] | CC | Dezful C | 340(170/170) | 45.4(11) | 45 | FH (+), OCP (*), HRT (+), PhA (*), AFFTP (+), BF (−) | ES, BF, parity, MaS |
| Montazeri et al. (2016) [53] | CC | Tehran C/Tabriz C | 975(432/543) | 48.6(4.7) | 40.6(10.7) | BF (+), MeAS (−), AFFTP (+) | MeS, AFP, age, BF |
| Dehghan et al. (2017) [54] | CC | Isfahan P | 182(86/96) | 52.88(11.92) | 40.31(16.82) | Age (+), FH (+) | FH, occupation, MaS, age, MeAS, MeS, HRT, abortion, BMI |
| Dianatinasab et al. (2017) [55] | CC | Shiraz C | 1052(526/526) | 47.8(10.58) | 46.75(11.08) | FH (+), OCP (+), MeS (+), MaS (+), Smoking (+), PS (+), occupation (+), XE (+), PhA (−), ES (*), hair coloring (+), BMI (+), SQ (*), parity (*), AFFTP (+), BF (*) | MaS, AFD, parity, birth spacing, BF, MeAS |
| Dianatinasab-2 et al. (2017) [56] | CS | Shiraz C | 497 | Age (−), FH (+), smoking (−), XE (+), PhA (−), income (−), CD (+) | |||
| Mirfarhadi et al. (2017) [57] | CS | Rasht C | 232 | FH (+), MaS (+), ES (−), RR (+), IC (+), income (+) | |||
| Vahid et al. (2017) [58] | CC | Tehran C | 293(145/148) | 49.8(11.8) | 48.5(11.9) | SI (−) | Age, BMI, ES, smoking, MeAS, occupation, MeS |
| Fararouei et al. (2018) [59] | CC | Shiraz C | 1010(505/505) | 41.78(10.56) | 42.24(10.62) | FH (+), OCP (+), smoking (+), PS (+), occupation (+), PhA (−), ES (+), MA (−), diet (−) | Diet, PhA, ES, occupation, PBBD, OCP, smoking |
| Pouladi et al. (2018) [60] | CC | Tabriz C | 303(143/160) | TP53 codon 72 polymorphism (+) | |||
| Vahid et al. (2018) [61] | CC | Tehran C | 293(145/148) | 49.83(11.86) | 48.54(12) | Age, ES, exercise, BMI, smoking, FH, MeAS, parity, MaS, MeS, OCP, HRT | |
| Marzbani et al. (2019) [62] | CC | Kermanshah C | 620(212/408) | 41.5(6.2) | 39.5(7.1) | Age (+), MaS (−), S (+), BMI (*), Diet (+), RR (+), IC (+), occupation (*) | Age, sex, ES, BMI |
(+), risk-increasing; (−), risk-reducing; (=), null; (*), consists of various effects; C, City; P, Province; CC, Case-control; CS, Cross-sectional; FH, Familial history; OCP, Oral contraceptive pill; MeS, Menopause status; MaS, Marital status; ES, Educational status; AFFTP, Age at first full-term pregnancy; HRT, Hormone replacement therapy; SLE, Sunlight exposure; SI, Supplement intake; XE, X-ray exposure; PhA, Physical activity; CD, Chronic diseases; PS, Passive smoker; SQ, Sleep quality; MeAS, Menarche age status; BF, Breastfeeding; IM, Irregular menstruation; PBBD, Previous benign breast disease; RR, Rural residency; Re, Residence area; IC, Insurance coverage; SS, Socioeconomic status; GS, Genital surgery; OC, Ovary cancer; HP, History of pregnancy; AFD, age at the first delivery; MA, Marriage age.
Quality assessment
According to quality assessment using the NOS checklist, 39 studies earned the minimum eligibility score and entered into the meta-analysis. It is remarkable that the NOS modified checklist was used for cross-sectional studies [63]. Only one paper was excluded due to a low score. Summary of risk of bias presented in Figure 2. for details, see Supplementary material 2.
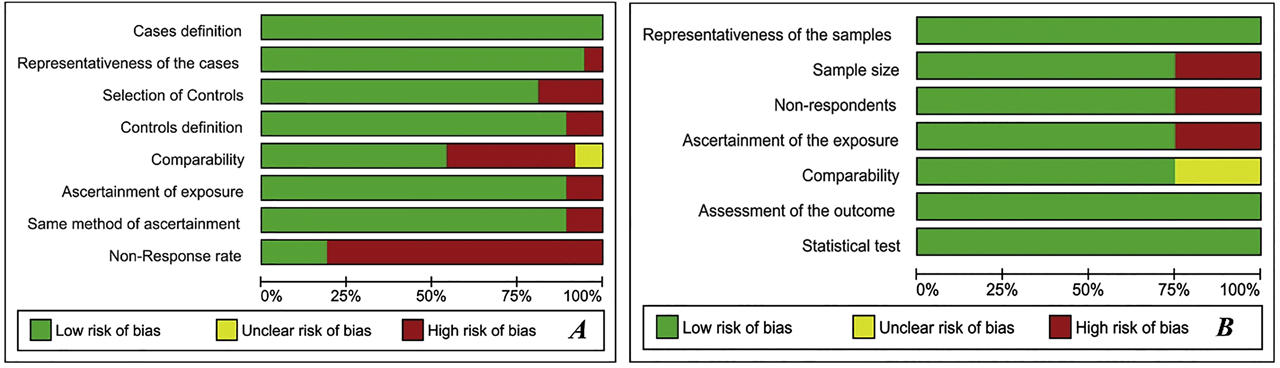
Risk of bias summary. A: Case-control studies; B: Cross-sectional studies.
Risk factors for breast cancer
According to included studies, over 20 risk factors were reported for breast cancer. The factors reported in only one study, which seems to be rare are as follows: High-fat foods and dairy (e. g. milk, yogurt, and cheese) [62], Fast foods [62], Genital surgery (surgeries related to uterus and ovary such as hysterectomy or oophorectomy) [30], [40], Hopelessness [26], Hair coloring [55], Human papillomavirus infection [37], Epstein–Barr virus infection [64], Ovarian cancer [41], Supplements of selenium, calcium, Vit B12 and Vit D [58].
The factors reported in more than one study are as follows: Age, Family history, Menarche age, Body mass index (BMI), Relationship status, Education Level, Smoking status, Daily exercise, Menopausal status, HRT, Oral contraceptive, birth-giving status, Abortion status, Benign Breast Conditions, X-ray exposure, Breastfeeding duration, Dietary status (including sweets, egg, fish, and vegetables), Genotype status and Residency status.
Only clear well-known risk factors reported in two or more studies entered into the meta-analysis.
Individual-related risk factors (Table 2)
Summarized pooled ORs of considered risk factors.
| Risk factor | Number of studies | I-squared; crude, % | p-Value; crude | OR (95%CI); crude | Number of studies | I-squared; adjusted, % | p-Value; adjusted | OR (95%CI); adjusted |
|---|---|---|---|---|---|---|---|---|
| Age | 5 | 94.2 | 0.000 | 0.97 (0.92, 1.02) | 2 | 80.6 | 0.023 | 1.04 (0.97, 1.11) |
| Family history | 18 | 24.6 | 0.165 | 2.31 (1.95, 2.86) | 12 | 24.3 | 0.205 | 1.80 (1.47, 2.12) |
| Menarche age status | ||||||||
| Unknown categorization | 2 | 89.6 | 0.002 | 2.25 (−0.80, 5.30) | ||||
| Less than 12 years | 5 | 81.4 | 0.000 | 1.31 (0.23, 2.40) | ||||
| Between 12 and 15 years | 2 | 54.8 | 0.137 | 0.52 (0.26, 0.78) | 2 | 77.3 | 0.036 | 0.55 (0.07, 1.03) |
| Less than 13 years | 5 | 0.0 | 0.710 | 1.19 (0.94, 1.44) | ||||
| Less than 14 years | 5 | 38.6 | 0.164 | 0.91 (0.68, 1.15) | ||||
| More than 15 years | 5 | 75.5 | 0.003 | 0.81 (0.39, 1.23) | 4 | 35.3 | 0.201 | 0.58 (0.32, 0.83) |
| Body mass index status | ||||||||
| Unknown categorization | 3 | 65.3 | 0.056 | 1.02 (1.00, 1.05) | 2 | 77.9 | 0.034 | 1.04 (0.99, 1.09) |
| Between 25 and 29.9 | 6 | 0.0 | 0.699 | 1.09 (0.91, 1.28) | 3 | 0.0 | 0.766 | 1.07 (0.82, 1.32) |
| More than 30 | 5 | 0.0 | 0.433 | 1.15 (0.91, 1.39) | 3 | 0.0 | 0.994 | 1.21 (0.90, 1.52) |
| Relationship status | ||||||||
| Single | 11 | 13.6 | 0.315 | 0.98 (0.74, 1.23) | ||||
| Married | 2 | 0.0 | 0.678 | 0.64 (−0.25, 1.54) | ||||
| Divorced | 7 | 0.0 | 0.619 | 1.15 (0.87, 1.43) | ||||
| Education level | ||||||||
| Basic education | 14 | 75.5 | 0.000 | 1.23 (0.94, 1.51) | 9 | 87.5 | 0.000 | 1.18 (0.70, 1.66) |
| Academic education | 12 | 71.4 | 0.000 | 1.21 (0.80, 1.62) | 8 | 69.8 | 0.002 | 0.67 (0.24, 1.10) |
| Smoking status | ||||||||
| Active smoker | 5 | 63.5 | 0.027 | 1.49 (0.89, 2.08) | 3 | 66.3 | 0.051 | 1.70 (0.66, 2.74) |
| Passive smoker | 2 | 0.0 | 0.657 | 1.84 (1.43, 2.25) | 3 | 0.0 | 0.442 | 1.68 (1.34, 2.03) |
| Daily exercise | 4 | 73.5 | 0.010 | 0.40 (0.05, 0.75) | 3 | 0.0 | 0.678 | 0.59 (0.44, 0.73) |
| Menopausal status | 12 | 88.9 | 0.000 | 1.53 (1.06, 1.99) | 9 | 73.9 | 0.000 | 1.29 (0.84, 1.74) |
| Hormone replacement therapy | 4 | 61.9 | 0.049 | 1.80 (0.36, 3.23) | 3 | 0.0 | 0.509 | 5.48 (2.71, 8.25) |
| Oral contraceptive | 14 | 80.0 | 0.000 | 1.18 (0.93, 1.44) | 10 | 86.9 | 0.000 | 1.17 (0.77, 1.57) |
| Age at first full-term pregnancy | ||||||||
| 20–24 years | 3 | 68.0 | 0.044 | 1.48 (0.79, 2.17) | 2 | 0.0 | 0.484 | 1.92 (1.14, 2.71) |
| 25–29 years | 5 | 0.0 | 0.560 | 1.40 (1.00, 1.80) | 4 | 5.3 | 0.367 | 1.55 (0.82, 2.29) |
| 30 years | 5 | 0.0 | 0.758 | 2.23 (1.45, 3.01) | 3 | 0.0 | 0.970 | 3.41 (1.19, 5.63) |
| Birth giving status | ||||||||
| Nulliparity | 6 | 40.4 | 0.136 | 0.77 (0.55, 0.98) | 3 | 28.0 | 0.249 | 0.68 (0.39, 0.96) |
| Abortion | 5 | 86.9 | 0.000 | 1.25 (0.57, 1.93) | 3 | 0.0 | 0.393 | 1.84 (1.35, 2.33) |
| Previous benign breast | 5 | 0.0 | 0.672 | 1.24 (0.82, 1.67) | ||||
| X-ray exposure | 5 | 0.0 | 0.676 | 1.42 (1.18, 1.66) | 3 | 83.6 | 0.002 | 1.02 (0.19, 1.86) |
| Breastfeeding duration | ||||||||
| Breastfeeding | 3 | 0.0 | 0.526 | 0.58 (0.30, 0.85) | 2 | 88.1 | 0.004 | 0.73 (0.14, 1.31) |
| 1–12 months | 3 | 40.0 | 0.189 | 0.95 (0.41, 1.49) | ||||
| 13–24 months | 4 | 0.0 | 0.602 | 0.57 (0.42, 0.72) | 2 | 0.0 | 0.624 | 0.68 (0.46, 0.90) |
| 25–48 months | 2 | 92.1 | 0.000 | 1.12 (−0.68, 2.92) | 2 | 0.0 | 0.402 | 0.24 (−0.46, 0.94) |
| More than 49 months | 2 | 0.0 | 0.410 | 0.10 (−0.25, 0.44) | ||||
| Dietary status | ||||||||
| Egg | 2 | 82.7 | 0.016 | 0.92 (−0.64, 2.47) | ||||
| Fish | 2 | 0.0 | 0.462 | 1.47 (0.68, 2.25) | ||||
| Sweets | 2 | 73.2 | 0.053 | 2.83 (1.38, 4.29) | 2 | 0.0 | 0.391 | 2.21 (1.56, 2.87) |
| Vegetables | 3 | 56.1 | 0.102 | 0.28 (0.10, 0.46) | ||||
| Genotype status | ||||||||
| Arg/Arg | 2 | 0.0 | 0.835 | 1.59 (1.07, 2.10) | ||||
| Arg/Pro | 2 | 0.0 | 0.824 | 0.69 (0.37, 1.00) | ||||
| Genital surgery | 2 | 0.0 | 0.325 | 2.23 (0.91, 3.55) | ||||
| Residency status | ||||||||
| Rural | 2 | 0.0 | 0.875 | 1.37 (0.87, 1.86) | ||||
Age
Age was considered as a risk factor in four papers. The meta-analysis showed no significant difference between groups for breast cancer occurrence regarding age (OR: 1.04, 95%CI 0.97–1.11). A significant heterogeneity was observed (I2=80.6%, p=0.023) (Supplementary material 1).
Family history
Eighteen studies reported on a family history of breast cancer. The meta-analysis between two groups showed that the odds of breast cancer development was 1.80 times higher in subject with a family history of breast cancer (OR: 1.80, 95%CI 1.47–2.12). A modest heterogeneity was observed (I2=24.3%, p=0.205) (Supplementary material 1).
Menarche age
This factor was studied in Nine articles. The meta-analysis showed a significant protective effect for menarche age more than 15 (OR: 0.58, 95%CI 0.32–0.83). Moderate heterogeneity was observed in this regard (I2=35.3%, p=0.201) (Supplementary material 1).
Body mass index
BMI was investigated in nine studies. The meta-analysis indicated no significant differences between groups for BMI status (OR: 1.04, 95%CI 0.99–1.09), BMI 25–29.9 (OR: 1.07, 95%CI 0.82–1.32) and BMI more than 30 (OR: 1.21, 95%CI 0.90–1.52) (Supplementary material 1).
Relationship status
Thirteen papers were studied relationship status. The meta-analysis found that there were no significant differences between groups regarding single status (crude OR: 0.98, 95%CI 0.74–1.23), married status (crude OR: 0.64, 95%CI −0.25 to 1.54) and divorced status (crude OR: 1.15, 95%CI 0.87–1.43) (Supplementary material 1).
Education level
This factor was studied in 15 papers. According to meta-analysis, no significant differences were found for both basic education level (OR: 1.18, 95%CI 0.70–1.66) and academic education level (OR: 0.67, 95%CI 0.24–1.10) (Supplementary material 1).
Smoking status
Six papers studied this factor. The meta-analysis showed that the odds of breast cancer occurrence was 1.68 times higher in the passive smokers (OR: 1.68, 95%CI 1.34–2.03). However, no significant relationships were observed for active smokers (OR: 1.70, 95%CI 0.66–2.74) (Supplementary material 1).
Daily exercise
Three studies were included with this factor. The daily exercise showed a protective effect on the occurrence of breast cancer (OR: 0.59, 95%CI 0.44–0.73). No heterogeneity was observed (I2=0.0%, p=0.678) (Supplementary material 1).
Menopausal status
Thirteen studies have investigated this factor. No significant relationships were observed between groups in this regard (OR: 1.29, 95%CI 0.84–1.74). High heterogeneity was observed (I2=73.9%, p<0.0001) (Supplementary material 1).
Hormone replacement therapy
HRT was studied in five papers. The meta-analysis indicated that the odds of breast cancer occurrence was 5.48 time higher in the group with HRT history (OR: 5.48, 95%CI 0.84–1.74). No significant heterogeneity was observed (I2=0.0%, p=0.509) (Supplementary material 1).
Oral contraceptive
A history of OCP intake was discussed in 15 papers. The meta-analysis showed no significant differences between groups in this regard (OR: 1.17, 95%CI 0.77–1.57). High heterogeneity was observed (I2=86.9%, p<0.0001) (Supplementary material 1).
Birth giving status
Age at first full-term pregnancy was considered in six studies. Meta-analysis showed a significant difference for age 20 to 24 (OR: 1.92, 95%CI 1.14–2.71) and age 30 (OR: 3.41, 95%CI 1.19–5.63) in this regard, but no substantial relationships were found for age 25 to 29 (OR: 1.55, 95%CI 0.82–2.29) (Supplementary material 1).
Six studies investigated the relation of nulliparity and chance of breast cancer development. The meta-analysis results indicated that this condition has an inverse relation with the occurrence of breast cancer (OR: 0.68, 95%CI 0.39–0.96) (Supplementary material 1).
Moreover, five papers studied the history of abortion. A significant difference in odds was observed in the meta-analysis of two groups. Subjects with a history of abortion have a higher chance of breast cancer development (OR: 1.84, 95%CI 1.35–2.33). No significant heterogeneity was observed (I2=0.0%, p=0.393) (Supplementary material 1).
Benign breast conditions
Data from five studies were combined for the meta-analysis of benign breast history as a risk factor to develop breast cancer. No significant difference was observed in this regard (crude OR: 1.24, 95%CI 0.82–1.67) (Supplementary material 1).
X-ray exposure
This factor was studied in four papers. No significant differences were observed regarding the history of X-rays exposure between cases and controls (OR: 1.02, 95%CI 0.19–1.86). A significant heterogeneity was observed (I2=83.6%, p=0.002) (Supplementary material 1).
Breastfeeding duration
This factor was investigated in seven studies. The meta-analysis revealed that 13–24 months of breastfeeding has an inverse association with breast cancer occurrence (OR: 0.68, 95%CI 0.46–0.90). No significant heterogeneity was observed (I2=0.0%, p=0.624) (Supplementary material 1).
Dietary status
This factor was studied for egg, fish, sweets, and vegetables. The meta-analysis revealed that egg (crude OR: 0.92, 95%CI −0.64 to 2.47) and fish (crude OR: 1.47, 95%CI 0.68–2.25) do not affect the chance of breast cancer occurrence significantly (Supplementary material 1). However, findings showed that the odds of developing breast cancer were higher in individuals with high sweets consumption (OR: 1.71, 95%CI 1.32–2.11) (Supplementary material 1) and lower in subjects with regular vegetable consumption (crude OR: 0.28, 95%CI 0.10–0.46) (Supplementary material 1).
Genotype status
Two studies were investigated p53 codon 72 polymorphisms as a breast cancer risk factor. Although genotype Arg/Pro (crude OR: 0.69, 95%CI 0.37–1.00) was not related to the odds of breast cancer development, a significantly higher chance found for genotype Arg/Arg (crude OR: 1.59, 95%CI 1.07–2.10) in this regard (Supplementary material 1).
Genital surgery
Genital surgery was considered in two studies. No significant differences were found regarding the history of genital surgery for breast cancer development (crude OR: 1.37, 95%CI 0.87–1.86) (Supplementary material 1).
Residency status
The place of living was investigated in two studies. The meta-analysis delivered no significant difference between two groups with rural and urban residency status for breast cancer occurrence (crude OR: 1.37, 95%CI 0.87–1.86) (Supplementary material 1).
Discussion
We undertook this systematic review and meta-analysis to identify the risk factors contributing to the occurrence of female breast cancer in Iran. Out of 39 included papers, more than 60 factors were studied as breast cancer risk factors, of which only 27 factors entered the meta-analysis. Out of all risk factors, factors including family history, HRT, passive smokers, late full-term pregnancy, abortion, sweets consumption, and genotype Arg/Arg indicated to be significantly associated with a higher chance of breast cancer development. In contrast, factors of late menarche, nulliparity, 13–24 months of breastfeeding, daily exercise, and vegetable consumption, were demonstrated to be protective. The other remaining risk factors were not associated with the development of breast cancer.
A family history of breast cancer was one of the associated risk factors for breast cancer development in our study. In one of the first meta-analysis on “Family history and the risk of breast cancer”, Pharoah et al. [65] pooled estimate of relative risk (RR) indicated that the probability of breast cancer occurrence is higher in those individuals with a family history of this malignancy (RR: 1.9, 95%CI, 1.7–2.0). They also found that this probability is higher in first-degree relatives, especially mother and sister (RR: 3.6, 95%CI 2.5–5.0). There are many other studies that reported the association of family history with the risk of breast cancer [66], [67], [68].
High levels of estrogen can increase the chance of breast cancer development through genotoxic stress induction and breast tissue mutations [69], [70]. Therefore, receiving external estrogen through HRT may increase the risk of breast cancer development. In this regard, HRT users showed the highest chance of developing breast cancer in our meta-analysis (OR: 5.48, 95%CI 0.84–1.74), inconsistent with several studies [71], [72], [73]. In contrast, the study of Bae et al. reported no significant association in this regard among Korean Women [74].
In our meta-analysis, although passive smokers were at higher risk of breast cancer development, no significant association was found for active smokers in this case. Our findings were in the same line with the systematic review of Chen et al. [75] among Chinese females, which implied that passive smokers were at higher risk of breast cancer development (OR: 1.62, 95%CI 1.39–1.85), but not active smokers (OR: 1.04, 95%CI 0.89–1.20). Moreover, some other studies reported a significant association between passive smoking and the risk of breast cancer [76], [77], [78].
Regarding the age at first full-term pregnancy, our results were in the same line with previous studies, which indicated the increased risk of breast cancer in individuals with late first full-term pregnancy (at age 30 or older) [79], [80]. For nulliparity conditions, our study showed an inverse association with breast cancer development, which was in contrast with several previous reports [81], [82].
Numerous investigators have studied the association of induced abortion and the risk of breast cancer throughout the world. One of the oldest studies titled “Induced abortion as a cancer risk factor” discussed the induced abortion as a breast cancer risk factor [83]. Similarly, some meta-analysis also reported the same conclusions [84], [85]. In this regard, our meta-analysis found that induced abortion was significantly associated with the risk of breast cancer in Iranian women. Besides, the study of Deng et al. demonstrated that induced abortion might be related to the risk of breast cancer in parous women (OR: 1.11, 95%CI 1.02–1.20, p = 0.01), but not in nulliparous women (OR :1.02, 95%CI 0.86–1.21, p = 0.85). In contrast, several studies arrived at contradictory conclusions [86], [87].
The meta-analysis findings showed a significant association between sweet foods consumption and the risk of breast cancer. Although we did not find a specific systematic review in this regard, several epidemiological studies in different regions reported the association of sweet foods consumption and risk of breast cancer [88], [89], [90], [91]. For example, Tavani et al. performed a comprehensive case-control study in Italy and found a direct relationship between sweet foods consumption and risk of breast cancer development [91]. In fact, excessive sweets intake with a high glycemic index may cause insulin resistance as well as insulin-related growth factors as promoters of breast carcinogenesis. Moreover, ovarian steroid secretion, including estrogens and androgens, might be stimulated by insulin. Altogether, these processes end up at an increased risk of breast cancer [92], [93].
Previous studies have investigated the relationships of p53 codon 72 polymorphisms and the risk of breast cancer development in different regions [94]. In this investigation, we found that the genotype Arg/Arg is associated with the development of breast cancer, which was inconsistent with the study of Al-Qasem et al. among Saudi women, and in contrast with meta-analysis carried out by Ma et al. and Hou et al. studies [95], [96].
Menarche age does not precisely match with the breast cancer onset. However, they are significantly correlated [97]. This meta-analysis demonstrated an inverse association between late menarche age and risk of breast cancer (OR: 0.58, 95%CI 0.32–0.83). Our findings were in the same direction with two other meta-analyses carried out by Li et al. [98] and Collaborative Group on Hormonal Factors in Breast Cancer [99].
We found that longer breastfeeding duration (13–24 months) plays a protective rule against breast cancer development, inconsistent with numerous meta-analysis in various populations [100], [101], [102], [103]. In this regard, according to one of the most comprehensive studies on “Breast cancer and breastfeeding” including 47 epidemiological studies in 30 countries, breast cancer development would be reduced by 42%, especially in developing countries because women in these countries usually have a long duration of breastfeeding throughout their lives [104]. In contrast, short breastfeeding duration, which is usual among women in developed countries with small family size, would contribute to a higher risk of breast cancer development in such countries [104].
The updated report “Food, Nutrition, Physical Activity, and the Prevention of Cancer: A Global Perspective” in 2007, recommended physical activity as a protective factor against cancers, especially post-menopausal breast cancer [105]. It was also recommended by the “American Cancer Society Guidelines on nutrition and physical activity for cancer prevention” [106]. Our findings also support this hypothesis as a preventive factor for breast cancer development. In fact, physical activities affect the risk of cancer development through mechanisms such as metabolic, reproductive effects, hormonal, and immunity enhancement, etc. [107]. The comprehensive study of Moore et al. [108] titled “Association of Leisure-Time Physical Activity with Risk of 26 Types of Cancer in 1.44 Million Adults” reported the significant association for high and low physical activity and lower risk of breast cancer (hazard ratio (HR): 0.9, 95%CI 0.87–0.93).
The association between vegetable intake and risk of breast cancer was always controversial. Our results suggest a protective effect of vegetable consumption on the risk of breast cancer. In the same direction, meta-analyses carried out by Liu et al., Woo et al., and Aune et al. indicated a significant association between various types of vegetables and dietary fiber consumption and risk of breast cancer development [109], [110], [111]. In contrast, several systematic reviews and meta-analysis showed no significant relationships in this regard [112], [113], and some others were controversial regarding the types of vegetables and their combination intake with fruits as well as breast cancer types [114], [115].
According to the retrospective nature of the included studies, it is recommended to design some longitudinal cohort investigations in order to examine the fundamental role of these risk factors in breast cancer development.
Conclusion
Based on this systematic review and meta-analysis, factors including a family history of breast cancer, HRT, passive smokers, abortion, sweets consumption, and genotype Arg/Arg, play a significant role in the development of breast cancer. In contrast, late menarche, nulliparity, long breastfeeding duration, regular physical activity, and consumption of vegetables showed a significant inverse association with breast cancer occurrence.
Research funding: None.
Author contributions: ASH, RAN, ZSH, and KH designed the study protocol and wrote the manuscript. RAN performed the statistical analysis. ARA, DSH, ORT, ZA, LS, HM, NM, BZ, KK, BZ, and AHO contributed to the study screen, quality assessment, and made critical comments on the manuscript. All authors have read and approved the final manuscript.
Competing interests: The authors declare that they have no competing interests.
Informed consent: Not applicable.
Ethical approval: Not applicable. The protocol of this systematic review and meta-analysis was registered in the International Prospective Register of Systematic Reviews (PROSPERO) with the code CRD42019127382.
References
1. Clegg, LX, Reichman, ME, Miller, BA, Hankey, BF, Singh, GK, Lin, YD, et al. Impact of socioeconomic status on cancer incidence and stage at diagnosis: selected findings from the surveillance, epidemiology, and end results: national longitudinal mortality study. Cancer Causes Control 2009;20:417–35. https://doi.org/10.1007/s10552-008-9256-0.10.1007/s10552-008-9256-0Search in Google Scholar
2. Ferlay, J, Soerjomataram, I, Dikshit, R, Eser, S, Mathers, C, Rebelo, M, et al. Cancer incidence and mortality worldwide: sources, methods and major patterns in GLOBOCAN 2012. Int J Cancer 2015;136:E359–86. https://doi.org/10.1002/ijc.29210.10.1002/ijc.29210Search in Google Scholar
3. Mahboobi, A, Alvandi, S, Navaei, RA. An analytical survey on breast lesions in mammography. J Babol Univ Med Sci 2004;6:52–5.Search in Google Scholar
4. Mousavi, SM, Gouya, MM, Ramazani, R, Davanlou, M, Hajsadeghi, N, Seddighi, Z. Cancer incidence and mortality in Iran. Ann Oncol 2008;20:556–63. https://doi.org/10.1093/annonc/mdn642.10.1093/annonc/mdn642Search in Google Scholar
5. Dean, T, Armando, E. Breast cancer. novak. In: Berek, J, editor. Novak’s gynecology, 13th ed. Philadelphia: Lippincott William & Wilkins; 2002.Search in Google Scholar
6. Harris, J, Lippman, M, Morrow, M, Osborne, C. Diseases of the breast, 5th ed. Philadelphia: Wolters Kluwer/Lippincott Williams & Wilkins Health; 2014.Search in Google Scholar
7. Fitzmaurice, C, Dicker, D, Pain, A, Hamavid, H, Moradi-Lakeh, M, MacIntyre, MF, et al. The global burden of cancer 2013. JAMA Oncol 2015;1:505–27. https://doi.org/10.1001/jamaoncol.2015.0735.10.1001/jamaoncol.2015.0735Search in Google Scholar
8. Jemal, A, Bray, F, Center, MM, Ferlay, J, Ward, E, Forman, D. Global cancer statistics. CA Cancer J Clin 2011;61:69–90. https://doi.org/10.3322/caac.20107.10.3322/caac.20107Search in Google Scholar
9. Parkin, D, Läärä, E, Muir, C. Estimates of the worldwide frequency of sixteen major cancers in 1980. Int J Cancer 1988;41:184–97. https://doi.org/10.1002/ijc.2910410205.10.1002/ijc.2910410205Search in Google Scholar
10. Izquierdo, A, Gispert, R, Saladie, F, Espinàs, JA. Análisis de la incidencia, la supervivencia y la mortalidad según las principales localizaciones tumorales, 1985–2019: cáncer de mama. Med Clín 2008;131:50–2. https://doi.org/10.1016/s0025-7753(08)76433-9.10.1016/S0025-7753(08)76433-9Search in Google Scholar
11. Hortobagyi, GN, de la Garza Salazar, J, Pritchard, K, Amadori, D, Haidinger, R, Hudis, CA, et al. The global breast cancer burden: variations in epidemiology and survival. Clin Breast Cancer 2005;6:391–401. https://doi.org/10.3816/cbc.2005.n.043.10.3816/CBC.2005.n.043Search in Google Scholar
12. YektaKooshali, M, Esmaeilpour-Bandboni, M, Sharemi, S, Alipour, Z. Survival rate and average age of the patients with breast cancer in Iran: systematic review and meta-analysis. J Babol Univ Med Sci 2016;18:29–40.Search in Google Scholar
13. Akbari, M, Abachizadeh, K, Khayamzadeh, M, Tabatabaee, M, Esnaashari, F, Motlagh, A. Iran cancer report. Tehran, Qom: Cancer Research Center, Shahid Beheshti University of Medical Sciences. Darolfekr; 2008.Search in Google Scholar
14. Razi, S, Salehiniya, H, Dizaji, MFL. Epidemiology of prevalent cancer among Iranian women and its incidence trends from 2003–2009 in Iran. J Arak Univ Med Sci 2015;18:17–24.Search in Google Scholar
15. Kelsey, JL, Berkowitz, GS. Breast cancer epidemiology. Cancer Res 1988;48:5615–23.Search in Google Scholar
16. Hajian, K, Gholizadehpasha, A, Bozorgzadeh, SH. Association of obesity and central obesity with breast cancer risk in pre-and post-menopausal women. J Babol Univ Med Sci 2013;15:7–15.Search in Google Scholar
17. Sani, NA, Garan, MS, Nasiri, MG, Setayesh, Y. The effect of active and passive smoking associated with breast cancer. J Babol Univ Med Sci 2005;7:63–8.Search in Google Scholar
18. Hajizadeh, N, Pourhoseingholi, M, Emadedin, M, Baghestani, A, Fazeli, Z. Incidence rate of breast cancer in iranian women, trend analysis from 2003 to 2009. Int J Pharma Biomed Sci 2015;4:107–12.Search in Google Scholar
19. Yaghmaei, S, Hashemi, GB, Ghorbani, R. Survival rate following treatment of primary breast cancer in Semnan, Iran (1991–2002). Koomesh 2008;9:111–6.Search in Google Scholar
20. Huo, D, Adebamowo, C, Ogundiran, T, Akang, E, Campbell, O, Adenipekun, A, et al. Parity and breastfeeding are protective against breast cancer in Nigerian women. Br J Cancer 2008;98:992. https://doi.org/10.1038/sj.bjc.6604275.10.1038/sj.bjc.6604275Search in Google Scholar PubMed PubMed Central
21. Motamed, N, Hadi, N, Talei, A. A Survey on risk factors of breast cancer in women over 35 years of age (Shiraz-2000). J Adv Med Biomed Res 2004;12:25–32.Search in Google Scholar
22. Naieni, KH, Ardalan, A, Mahmoodi, M, Motevalian, A, Yahyapoor, Y, Yazdizadeh, B. Risk factors of breast cancer in north of Iran: a case-control in Mazandaran Province. Asian Pac J Cancer Prev 2007;8:395.Search in Google Scholar
23. Peterson, NB, Huang, Y, Newcomb, PA, Titus-Ernstoff, L, Trentham-Dietz, A, Anic, G, et al. Childbearing recency and modifiers of premenopausal breast cancer risk. Cancer Epidemiol Biomarkers Prev 2008;17:3284–7. https://doi.org/10.1158/1055-9965.epi-08-0577.10.1158/1055-9965.EPI-08-0577Search in Google Scholar PubMed PubMed Central
24. Ebrahimi, M, Vahdaninia, M, Montazeri, A. Risk factors for breast cancer in Iran: a case-control study. Breast Cancer Res 2002;4:R10. https://doi.org/10.1186/bcr454.10.1186/bcr454Search in Google Scholar PubMed PubMed Central
25. Pesaran, Z, Rezaei, A, Kia, RT, Siydat, A. Evaluation of breast cancer risk factors for using in hormone replacement therapy of corticosteroid- treated post-menopausal women. J Shahrekord Univ Med Sci 2003;5:70–5.Search in Google Scholar
26. Montazeri, A, Jarvandi, S, Ebrahimi, M, Haghighat, S, Ansari, M. The role of depression in the development of breast cancer: analysis of registry data from a single institute. Asian Pac J Cancer Prev 2004;5:316–9.Search in Google Scholar
27. Yavari, P, Mosavizadeh, M, Sadrolhefaz, iB, Khodabakhshi, R, Madani, H, Mehrabi, Y. Reproductive characteristics and the risk of breast cancer: a case-control study. Iran J Epidemiol 2006;1:11–9.Search in Google Scholar
28. Mahouri, K, Zahedani, MD, Zare, S. Breast cancer risk factors in south of Islamic Republic of Iran: a case-control study. East Mediterr Health J 2007;13:1265–73. https://doi.org/10.26719/2007.13.6.1265.10.26719/2007.13.6.1265Search in Google Scholar PubMed
29. Naieni, KH, Ardalan, A, Mahmoodi, M, Motevalian, A, Yahyapoor, Y, Yazdizadeh, B. Risk factors of breast cancer in north of Iran: a case-control in Mazandaran Province. Asian Pac J Cancer Prev 2007;8:395–8.Search in Google Scholar
30. Lotfi, M, Charkhati, S, Shobairi, S. Breast cancer risk factors in an urban area of Yazd City-Iran, 2006. Acta Med Iran 2008;46:258–64.Search in Google Scholar
31. Kazemi, M, Salehi, Z, Chakosari, RJ. TP53 codon 72 polymorphism and breast cancer in Northern Iran. Oncol Res 2009;18:25–30. https://doi.org/10.3727/096504009789745629.10.3727/096504009789745629Search in Google Scholar PubMed
32. Ghiasvand, R, Maram, ES, Tahmasebi, S, Tabatabaee, SH. Risk factors for breast cancer among young women in Southern Iran. Int J Cancer 2010;129:1443–9. https://doi.org/10.1002/ijc.25748.10.1002/ijc.25748Search in Google Scholar PubMed
33. Hajian-Tilaki, KO, Kaveh-Ahangar, T. Reproductive factors associated with breast cancer risk in Northern Iran. Med Oncol 2011;28:441–6. https://doi.org/10.1007/s12032-010-9498-z.10.1007/s12032-010-9498-zSearch in Google Scholar PubMed
34. Hajian-Tilaki, K, Kaveh-Ahangar, T, Hajian-Tilaki, E. Is educational level associated with breast cancer risk in Iranian women?. Breast Cancer 2011;19:64–70. https://doi.org/10.1007/s12282-011-0273-6.10.1007/s12282-011-0273-6Search in Google Scholar PubMed
35. Motie, MR, Besharat, S, Torkjazi, R, Shojaa, M, Besharat, M, Keshtkar, A, et al. Modifiable risk of breast cancer in Northeast Iran: hope for the future. A case-control study. Breast Care 2011;6:453–6. https://doi.org/10.1159/000335203.10.1159/000335203Search in Google Scholar PubMed PubMed Central
36. Ghiasvand, R, Bahmanyar, S, Zendehdel, K, Tahmasebi, S, Talei, A, Adami, H-O, et al. Post-menopausal breast cancer in Iran; risk factors and their population attributable fractions. BMC Cancer 2012;12:414. https://doi.org/10.1186/1471-2407-12-414.10.1186/1471-2407-12-414Search in Google Scholar PubMed PubMed Central
37. Sigaroodi, A, Nadji, SA, Naghshvar, F, Nategh, R, Emami, H, Velayati, AA. Human papillomavirus is associated with breast cancer in the north part of Iran. Sci World J 2012;2012:837191. https://doi.org/10.1100/2012/837191.10.1100/2012/837191Search in Google Scholar PubMed PubMed Central
38. Ahmadinejad, N, Movahedinia, S, Movahedinia, S, Naieni, KH, Nedjat, S. Distribution of breast density in Iranian women and its association with breast cancer risk factors. Iran Red Crescent Med J 2013;15:e16615. https://doi.org/10.5812/ircmj.16615.10.5812/ircmj.16615Search in Google Scholar PubMed PubMed Central
39. Kaviani, A, Neishaboury, M, Mohammadzadeh, N, Ansari-Damavandi, M, Jamei, K. Effects of obesity on presentation of breast cancer, lymph node metastasis and patient survival: a retrospective review. Asian Pac J Cancer Prev 2013;14:2225–9. https://doi.org/10.7314/apjcp.2013.14.4.2225.10.7314/APJCP.2013.14.4.2225Search in Google Scholar PubMed
40. Pourzand, A, Farajkhah, H, Azhough, R, Fakhree, MBA. Breast cancer risk factors among women without family history in North West of Iran. Life Sci J 2013;10:482–9.Search in Google Scholar
41. Zare, N, Haem, E, Lankarani, KB, Heydari, ST, Barooti, E. Breast cancer risk factors in a defined population: weighted logistic regression approach for rare events. J Breast Cancer 2013;16:214–9. https://doi.org/10.4048/jbc.2013.16.2.214.10.4048/jbc.2013.16.2.214Search in Google Scholar PubMed PubMed Central
42. Bidgoli, SA, Azarshab, H. Role of vitamin D deficiency and lack of sun exposure in the incidence of premenopausal breast cancer: a case control study in Sabzevar, Iran. Asian Pac J Cancer Prev 2014;15:3391–6. https://doi.org/10.7314/apjcp.2014.15.8.3391.10.7314/APJCP.2014.15.8.3391Search in Google Scholar PubMed
43. Hosseinzadeh, M, Eivazi Ziaei, J, Mahdavi, N, Aghajari, P, Vahidi, M, Fateh, A, et al. Risk factors for breast cancer in Iranian women: a hospital-based case-control study in Tabriz, Iran. J Breast Cancer 2014;17:236–43. https://doi.org/10.4048/jbc.2014.17.3.236.10.4048/jbc.2014.17.3.236Search in Google Scholar PubMed PubMed Central
44. Mobarakeh, ZS, Mirzaei, K, Hatmi, N, Ebrahimi, M, Dabiran, S, Sotoudeh, G. Dietary habits contributing to breast cancer risk among Iranian women. Asian Pac J Cancer Prev 2014;15:9543–7. https://doi.org/10.7314/apjcp.2014.15.21.9543.10.7314/APJCP.2014.15.21.9543Search in Google Scholar PubMed
45. Sepandi, M, Akrami, M, Tabatabaee, H, Rajaeefard, A, Tahmasebi, S, Angali, KA, et al. Breast cancer risk factors in women participating in a breast screening program: a study on 11,850 Iranian females. Asian Pac J Cancer Prev 2014;15:8499–502. https://doi.org/10.7314/apjcp.2014.15.19.8499.10.7314/APJCP.2014.15.19.8499Search in Google Scholar PubMed
46. Tazhibi, M, Dehghani, M, Babazadeh, S, Makkarian, F, Tabatabaeian, M, Sadeghi, M, et al. Hormonal and reproductive risk factors associated with breast cancer in Isfahan patients. J Educ Health Promot 2014;3:69. https://doi.org/10.4103/2277-9531.145917.10.4103/2277-9531.145917Search in Google Scholar PubMed PubMed Central
47. Salarabadi, A, Bidgoli, SA, Madani, SH. Roles of Kermanshahi oil, animal fat, dietary and non- dietary vitamin D and other nutrients in increased risk of premenopausal breast cancer: a case control study in Kermanshah, Iran. Asian Pac J Cancer Prev 2015;16:7473–8. https://doi.org/10.7314/apjcp.2015.16.17.7473.10.7314/APJCP.2015.16.17.7473Search in Google Scholar
48. Tajaddini, A, Pourzand, A, Sanaat, Z, Pirouzpanah, S. Dietary resistant starch contained foods and breast cancer risk: a case-control study in northwest of Iran. Asian Pac J Cancer Prev 2015;16:4185–92. https://doi.org/10.7314/apjcp.2015.16.10.4185.10.7314/APJCP.2015.16.10.4185Search in Google Scholar PubMed
49. Veisy, A, Lotfinejad, S, Salehi, K, Zhian, F. Risk of breast cancer in relation to reproductive factors in North-West of Iran, 2013–2014. Asian Pac J Cancer Prev 2015;16:451–5. https://doi.org/10.7314/apjcp.2015.16.2.451.10.7314/APJCP.2015.16.2.451Search in Google Scholar PubMed
50. Ahmadnia, Z, Joukar, F, Hasavari, F, Roushan, ZA, Khalili, M. Dietary patterns and risk of breast cancer in women in Guilan Province, Iran. Asian Pac J Cancer Prev 2016;17:2035–40. https://doi.org/10.7314/apjcp.2016.17.4.2035.10.7314/APJCP.2016.17.4.2035Search in Google Scholar
51. Jafari-Mehdiabad, F, Savabi-Esfahani, M, Mokaryan, F, Kazemi, A. Relationship between breastfeeding factors and breast cancer in women referred to Seyed Al-Shohada Hospital in Isfahan, Iran. Iran J Nurs Midwifery Res 2016;21:622–7. https://doi.org/10.4103/1735-9066.197670.10.4103/1735-9066.197670Search in Google Scholar PubMed PubMed Central
52. Jafarinia, B, Bahadorzai, M, Delpisheh, A, Sayehmiri, K, Tavakoli, M. Risk factors of breast cancer in Dezful city of Iran: a case-control study. Tehran Univ Med J 2016;74:135–9.Search in Google Scholar
53. Montazeri, V, Sadegh, FJ, Hosseinpour, S, Mirzaei, H, Akbari, E, Ehsani, M, et al. Reproductive risk factors of breast cancer among women in Tehran and northwest of Iran: a case-control study. Iran J Epidemiol 2016;12:1–9.Search in Google Scholar
54. Dehghan, Z, Sadeghi, S, Tabatabaeian, H, Ghaedi, K, Azadeh, M, Fazilati, M, et al. ESR1 single nucleotide polymorphism rs1062577 (c.*3804T>A) alters the susceptibility of breast cancer risk in Iranian population. Gene 2017;611:9–14. https://doi.org/10.1016/j.gene.2017.02.016.10.1016/j.gene.2017.02.016Search in Google Scholar PubMed
55. Dianatinasab, M, Fararouei, M, Mohammadianpanah, M, Zare-Bandamiri, M, Rezaianzadeh, A. Hair coloring, stress, and smoking increase the risk of breast cancer: a case-control study. Clin Breast Cancer 2017;17:650–9. https://doi.org/10.1016/j.clbc.2017.04.012.10.1016/j.clbc.2017.04.012Search in Google Scholar PubMed
56. Dianatinasab, M, Mohammadianpanah, M, Daneshi, N, Zare-Bandamiri, M, Rezaeianzadeh, A, Fararouei, M. Socioeconomic factors, health behavior, and late-stage diagnosis of breast cancer: considering the impact of delay in diagnosis. Clin Breast Cancer 2017;18:239–45. https://doi.org/10.1016/j.clbc.2017.09.005.10.1016/j.clbc.2017.09.005Search in Google Scholar PubMed
57. Mirfarhadi, N, Ghanbari, A, Khalili, M, Rahimi, A. Predictive factors for diagnosis and treatment delay in Iranian women with breast cancer. Nurs Midwifery Stud 2017;6:e27452. https://doi.org/10.5812/nmsjournal.27452.10.5812/nmsjournal.27452Search in Google Scholar
58. Vahid, F, Hatami, M, Sadeghi, M, Ameri, F, Faghfoori, Z, Davoodi, SH. The association between the index of nutritional quality (INQ) and breast cancer and the evaluation of nutrient intake of breast cancer patients: a case-control study. Nutrition 2017;45:11–6. https://doi.org/10.1016/j.nut.2017.06.011.10.1016/j.nut.2017.06.011Search in Google Scholar PubMed
59. Fararouei, M, Iqbal, A, Rezaian, S, Gheibi, Z, Dianatinasab, A, Shakarami, S, et al. Dietary habits and physical activity are associated with the risk of breast cancer among young Iranian women: a case-control study on 1010 premenopausal women. Clin Breast Cancer 2018;19:e127–34. https://doi.org/10.1016/j.clbc.2018.10.011.10.1016/j.clbc.2018.10.011Search in Google Scholar PubMed
60. Pouladi, N, Dehghan, R, Feizi, MH, Dastmalchi, N. Association of P53 (+ 16ins-Arg) haplotype with the increased susceptibility to breast cancer in Iranian-Azeri women. J Kerman Univ Med Sci 2018;25:9–17.Search in Google Scholar
61. Vahid, F, Shivappa, N, Hatami, M, Sadeghi, M, Ameri, F, Naeini, YJ, et al. Association between dietary inflammatory index (DII) and risk of breast cancer: a case-control study. Asian Pac J Cancer Prev 2018;19:1215–21. https://doi.org/10.22034/APJCP.2018.19.5.1215.Search in Google Scholar
62. Marzbani, B, Nazari, J, Najafi, F, Marzbani, B, Shahabadi, S, Amini, M, et al. Dietary patterns, nutrition, and risk of breast cancer: a case-control study in the west of Iran. Epidemiol Health 2019;41:e2019003. https://doi.org/10.4178/epih.e2019003.10.4178/epih.e2019003Search in Google Scholar PubMed PubMed Central
63. Modesti, PA, Reboldi, G, Cappuccio, FP, Agyemang, C, Remuzzi, G, Rapi, S, et al. Panethnic differences in blood pressure in Europe: a systematic review and meta-analysis. PloS One 2016;11:e0147601. https://doi.org/10.1371/journal.pone.0147601.10.1371/journal.pone.0147601Search in Google Scholar PubMed PubMed Central
64. Aghdam, MK, Nadji, SA, Khoddami, M, Dezfuli, HB, Khademi, Y. Epstein-barr virus and breast carcinoma in Iran. Jundishapur J Microbiol 2017;10:e12800. https://doi.org/10.5812/jjm.12800.10.5812/jjm.12800Search in Google Scholar
65. Pharoah, PD, Day, NE, Duffy, S, Easton, DF, Ponder, BA. Family history and the risk of breast cancer: a systematic review and meta-analysis. Int J Cancer 1997;71:800–9. https://doi.org/10.1002/(sici)1097-0215(19970529)71:5<800::aid-ijc18>3.0.co;2-b.10.1002/(SICI)1097-0215(19970529)71:5<800::AID-IJC18>3.0.CO;2-BSearch in Google Scholar
66. Brewer, HR, Jones, ME, Schoemaker, MJ, Ashworth, A, Swerdlow, AJ. Family history and risk of breast cancer: an analysis accounting for family structure. Breast Cancer Res Treat 2017;165:193–200. https://doi.org/10.1007/s10549-017-4325-2.10.1007/s10549-017-4325-2Search in Google Scholar
67. Nindrea, RD, Aryandono, T, Lazuardi, L. Breast cancer risk from modifiable and non-modifiable risk factors among women in Southeast Asia: a meta-analysis. Asian Pac J Cancer Prev 2017;18:3201–6. https://doi.org/10.22034/APJCP.2017.18.12.3201.Search in Google Scholar
68. Tao, P, Hu, YY, Huang, Y, Li, JY. Risk factors of breast cancer in Asian women: a meta-analysis. Zhonghua liu xing bing xue za zhi=Zhonghua liuxingbingxue zazhi. 2011;32:164–9.Search in Google Scholar
69. Germain, D. Estrogen carcinogenesis in breast cancer. Endocrinol Metab Clin North Am 2011;40:473–84, vii. https://doi.org/10.1016/j.ecl.2011.05.009.10.1016/j.ecl.2011.05.009Search in Google Scholar
70. Yager, JD, Davidson, NE. Estrogen carcinogenesis in breast cancer. N Engl J Med 2006;354:270–82. https://doi.org/10.1056/nejmra050776.10.1056/NEJMra050776Search in Google Scholar
71. Anothaisintawee, T, Wiratkapun, C, Lerdsitthichai, P, Kasamesup, V, Wongwaisayawan, S, Srinakarin, J, et al. Risk factors of breast cancer: a systematic review and meta-analysis. Asia Pac J Public Health 2013;25:368–87. https://doi.org/10.1177/1010539513488795.10.1177/1010539513488795Search in Google Scholar
72. Chen, C-L, Weiss, NS, Newcomb, P, Barlow, W, White, E. Hormone replacement therapy in relation to breast cancer. J Am Med Assoc 2002;287:734–41. https://doi.org/10.1001/jama.287.6.734.10.1001/jama.287.6.734Search in Google Scholar
73. Sillero-Arenas, M, Delgado-Rodriguez, M, Rodigues-Canteras, R, Bueno-Cavanillas, A, Galvez-Vargas, R. Menopausal hormone replacement therapy and breast cancer: a meta-analysis. Obstet Gynecol 1992;79:2286–94.10.1016/0020-7292(92)90949-JSearch in Google Scholar
74. Bae, JM, Kim, EH. Hormone replacement therapy and risk of breast cancer in Korean women: a quantitative systematic review. J Prev Med Public Health 2015;48:225–30. https://doi.org/10.3961/jpmph.15.046.10.3961/jpmph.15.046Search in Google Scholar
75. Chen, C, Huang, YB, Liu, XO, Gao, Y, Dai, HJ, Song, FJ, et al. Active and passive smoking with breast cancer risk for Chinese females: a systematic review and meta-analysis. Chin J Cancer 2014;33:306–16. https://doi.org/10.5732/cjc.013.10248.10.5732/cjc.013.10248Search in Google Scholar
76. Chen, Z, Shao, J, Gao, X, Li, X. Effect of passive smoking on female breast cancer in China: a meta-analysis. Asia Pac J Public Health 2015;27:NP58–64. https://doi.org/10.1177/1010539513481493.10.1177/1010539513481493Search in Google Scholar
77. Johnson, KC, Miller, AB, Collishaw, NE, Palmer, JR, Hammond, SK, Salmon, AG, et al. Active smoking and secondhand smoke increase breast cancer risk: the report of the Canadian expert panel on tobacco smoke and breast cancer risk (2009). Tob Control 2011;20:e2. http://dx.doi.org/10.1136/tc.2010.035931.10.1136/tc.2010.035931Search in Google Scholar PubMed
78. Macacu, A, Autier, P, Boniol, M, Boyle, P. Active and passive smoking and risk of breast cancer: a meta-analysis. Breast Cancer Res Treat 2015;154:213–24. https://doi.org/10.1007/s10549-015-3628-4.10.1007/s10549-015-3628-4Search in Google Scholar PubMed
79. Albrektsen, G, Heuch, I, Hansen, S, Kvale, G. Breast cancer risk by age at birth, time since birth and time intervals between births: exploring interaction effects. Br J Cancer 2005;92:167–75. https://doi.org/10.1038/sj.bjc.6602302.10.1038/sj.bjc.6602302Search in Google Scholar PubMed PubMed Central
80. Ramon, JM, Escriba, JM, Casas, I, Benet, J, Iglesias, C, Gavalda, L, et al. Age at first full-term pregnancy, lactation and parity and risk of breast cancer: a case-control study in Spain. Eur J Epidemiol 1996;12:449–53. https://doi.org/10.1007/bf00143995.10.1007/BF00143995Search in Google Scholar PubMed
81. Balekouzou, A, Yin, P, Pamatika, CM, Bekolo, CE, Nambei, SW, Djeintote, M, et al. Reproductive risk factors associated with breast cancer in women in Bangui: a case-control study. BMC Women’s Health 2017;17:14. https://doi.org/10.1186/s12905-017-0368-0.10.1186/s12905-017-0368-0Search in Google Scholar PubMed PubMed Central
82. Nelson, HD, Zakher, B, Cantor, A, Fu, R, Griffin, J, O’Meara, ES, et al. Risk factors for breast cancer for women aged 40 to 49 years: a systematic review and meta-analysis. Ann Intern Med 2012;156:635–48. https://doi.org/10.7326/0003-4819-156-9-201205010-00006.10.7326/0003-4819-156-9-201205010-00006Search in Google Scholar PubMed PubMed Central
83. Remennick, LI. Induced abortion as cancer risk factor: a review of epidemiological evidence. J Epidemiol Community Health 1990;44:259–64. https://doi.org/10.1136/jech.44.4.259.10.1136/jech.44.4.259Search in Google Scholar PubMed PubMed Central
84. Brind, J, Chinchilli, VM, Severs, WB, Summy-Long, J. Induced abortion as an independent risk factor for breast cancer: a comprehensive review and meta-analysis. J Epidemiol Community Health 1996;50:481–96. https://doi.org/10.1136/jech.50.5.481.10.1136/jech.50.5.481Search in Google Scholar PubMed PubMed Central
85. Huang, Y, Zhang, X, Li, W, Song, F, Dai, H, Wang, J, et al. A meta-analysis of the association between induced abortion and breast cancer risk among Chinese females. Cancer Causes Control 2014;25:227–36. https://doi.org/10.1007/s10552-013-0325-7.10.1007/s10552-013-0325-7Search in Google Scholar PubMed
86. Guo, J, Huang, Y, Yang, L, Xie, Z, Song, S, Yin, J, et al. Association between abortion and breast cancer: an updated systematic review and meta-analysis based on prospective studies. Cancer Causes Control 2015;26:811–9. https://doi.org/10.1007/s10552-015-0536-1.10.1007/s10552-015-0536-1Search in Google Scholar PubMed
87. Michels, KB, Hsieh, CC, Trichopoulos, D, Willett, WC. Abortion and breast cancer risk in seven countries. Cancer Causes Control 1995;6:75–82. https://doi.org/10.1007/bf00051683.10.1007/BF00051683Search in Google Scholar PubMed
88. Landa, MC, Frago, N, Tres, A. Diet and the risk of breast cancer in Spain. Eur J Cancer Prev 1994;3:313–20. https://doi.org/10.1097/00008469-199407000-00003.10.1097/00008469-199407000-00003Search in Google Scholar PubMed
89. Lubin, JH, Burns, PE, Blot, WJ, Ziegler, RG, Lees, AW, Fraumeni, JFJr. Dietary factors and breast cancer risk. Int J Cancer 1981;28:685–9. https://doi.org/10.1002/ijc.2910280605.10.1002/ijc.2910280605Search in Google Scholar PubMed
90. Potischman, N, Coates, RJ, Swanson, CA, Carroll, RJ, Daling, JR, Brogan, DR, et al. Increased risk of early-stage breast cancer related to consumption of sweet foods among women less than age 45 in the United States. Cancer Causes Control 2002;13:937–46. https://doi.org/10.1023/a:1021919416101.10.1023/A:1021919416101Search in Google Scholar
91. Tavani, A, Giordano, L, Gallus, S, Talamini, R, Franceschi, S, Giacosa, A, et al. Consumption of sweet foods and breast cancer risk in Italy. Ann Oncol 2005;17:341–5. https://doi.org/10.1093/annonc/mdj051.10.1093/annonc/mdj051Search in Google Scholar PubMed
92. Augustin, LS, Dal Maso, L, La Vecchia, C, Parpinel, M, Negri, E, Vaccarella, S, et al. Dietary glycemic index and glycemic load, and breast cancer risk: a case-control study. Ann Oncol 2001;12:1533–8. https://doi.org/10.1023/a:1013176129380.10.1023/A:1013176129380Search in Google Scholar
93. Dobson, R. Sweet foods increase breast cancer risk. BMJ 2005;331:1102. https://doi.org/10.1136/bmj.331.7525.1102-b.10.1136/bmj.331.7525.1102-bSearch in Google Scholar
94. He, XF, Su, J, Zhang, Y, Huang, X, Liu, Y, Ding, DP, et al. Association between the p53 polymorphisms and breast cancer risk: meta-analysis based on case-control study. Breast Cancer Res Treat 2011;130:517–29. https://doi.org/10.1007/s10549-011-1583-2.10.1007/s10549-011-1583-2Search in Google Scholar PubMed
95. Hou, J, Jiang, Y, Tang, W, Jia, S. p53 codon 72 polymorphism and breast cancer risk: a meta-analysis. Exp Ther Med 2013;5:1397–402. https://doi.org/10.3892/etm.2013.1019.10.3892/etm.2013.1019Search in Google Scholar PubMed PubMed Central
96. Ma, Y, Yang, J, Liu, Z, Zhang, P, Yang, Z, Wang, Y, et al. No significant association between the TP53 codon 72 polymorphism and breast cancer risk: a meta-analysis of 21 studies involving 24,063 subjects. Breast Cancer Res Treat 2011;125:201–5. https://doi.org/10.1007/s10549-010-0920-1.10.1007/s10549-010-0920-1Search in Google Scholar PubMed
97. Marshall, WA, Tanner, JM. Variations in pattern of pubertal changes in girls. Arch Dis Child 1969;44:291–303. https://doi.org/10.1136/adc.44.235.291.10.1136/adc.44.235.291Search in Google Scholar
98. Li, H, Sun, X, Miller, E, Wang, Q, Tao, P, Liu, L, et al. BMI, reproductive factors, and breast cancer molecular subtypes: a case-control study and meta-analysis. J Epidemiol 2017;27:143–51. https://doi.org/10.1016/j.je.2016.05.002.10.1016/j.je.2016.05.002Search in Google Scholar
99. Cancer CGoHFiB. Menarche, menopause, and breast cancer risk: individual participant meta-analysis, including 118,964 women with breast cancer from 117 epidemiological studies. Lancet Oncol 2012;13:1141–51. https://doi.org/10.1016/S1470-2045(12)70425-4.10.1016/S1470-2045(12)70425-4Search in Google Scholar
100. Bernier, MO, Plu-Bureau, G, Bossard, N, Ayzac, L, Thalabard, JC. Breastfeeding and risk of breast cancer: a meta-analysis of published studies. Hum Reprod Update 2000;6:374–86. https://doi.org/10.1093/humupd/6.4.374.10.1093/humupd/6.4.374Search in Google Scholar
101. Islami, F, Liu, Y, Jemal, A, Zhou, J, Weiderpass, E, Colditz, G, et al. Breastfeeding and breast cancer risk by receptor status--a systematic review and meta-analysis. Ann Oncol 2015;26:2398–407. https://doi.org/10.1093/annonc/mdv379.10.1093/annonc/mdv379Search in Google Scholar
102. Unar-Munguia, M, Torres-Mejia, G, Colchero, MA, Gonzalez de Cosio, T. Breastfeeding mode and risk of breast cancer: a dose-response meta-analysis. J Hum Lactation 2017;33:422–34. https://doi.org/10.1177/0890334416683676.10.1177/0890334416683676Search in Google Scholar
103. Zhou, Y, Chen, J, Li, Q, Huang, W, Lan, H, Jiang, H. Association between breastfeeding and breast cancer risk: evidence from a meta-analysis. Breastfeed Med 2015;10:175–82. https://doi.org/10.1089/bfm.2014.0141.10.1089/bfm.2014.0141Search in Google Scholar
104. Collaborative Group on Hormonal Factors in Breast Cancer. Breast cancer and breastfeeding: collaborative reanalysis of individual data from 47 epidemiological studies in 30 countries, including 50,302 women with breast cancer and 96,973 women without the disease. Lancet 2002;360:187–95. https://doi.org/10.1016/S0140-6736(02)09454-0.10.1016/S0140-6736(02)09454-0Search in Google Scholar
105. Fund WCR, Research AIfC. Food, nutrition, physical activity, and the prevention of cancer: a global perspective. Arlington, VA: American Institute for Cancer Research; 2007.Search in Google Scholar
106. Kushi, LH, Doyle, C, McCullough, M, Rock, CL, Demark-Wahnefried, W, Bandera, EV, et al. American Cancer Society guidelines on nutrition and physical activity for cancer prevention: reducing the risk of cancer with healthy food choices and physical activity. CA Cancer J Clin 2012;62:30–67. https://doi.org/10.3322/caac.20140.10.3322/caac.20140Search in Google Scholar PubMed
107. McTiernan, A, Ulrich, C, Slate, S, Potter, J. Physical activity and cancer etiology: associations and mechanisms. Cancer Causes Control 1998;9:487–509. https://doi.org/10.1023/a:1008853601471.10.1023/A:1008853601471Search in Google Scholar
108. Moore, SC, Lee, IM, Weiderpass, E, Campbell, PT, Sampson, JN, Kitahara, CM, et al. Association of leisure-time physical activity with risk of 26 types of cancer in 1.44 million adults. JAMA Intern Med 2016;176:816–25. https://doi.org/10.1001/jamainternmed.2016.1548.10.1001/jamainternmed.2016.1548Search in Google Scholar PubMed PubMed Central
109. Aune, D, Chan, DS, Greenwood, DC, Vieira, AR, Rosenblatt, DA, Vieira, R, et al. Dietary fiber and breast cancer risk: a systematic review and meta-analysis of prospective studies. Ann Oncol 2012;23:1394–402. https://doi.org/10.1093/annonc/mdr589.10.1093/annonc/mdr589Search in Google Scholar PubMed
110. Liu, X, Lv, K. Cruciferous vegetables intake is inversely associated with risk of breast cancer: a meta-analysis. Breast 2013;22:309–13. https://doi.org/10.1016/j.breast.2012.07.013.10.1016/j.breast.2012.07.013Search in Google Scholar PubMed
111. Woo, HD, Park, S, Oh, K, Kim, HJ, Shin, HR, Moon, HK, et al. Diet and cancer risk in the Korean population: a meta- analysis. Asian Pac J Cancer Prev 2014;15:8509–19. https://doi.org/10.7314/apjcp.2014.15.19.8509.10.7314/APJCP.2014.15.19.8509Search in Google Scholar
112. Smith-Warner, SA, Spiegelman, D, Yaun, SS, Adami, HO, Beeson, WL, van den Brandt, PA, et al. Intake of fruits and vegetables and risk of breast cancer: a pooled analysis of cohort studies. J Am Med Assoc 2001;285:769–76. https://doi.org/10.1001/jama.285.6.769.10.1001/jama.285.6.769Search in Google Scholar PubMed
113. van Gils, CH, Peeters, PH, Bueno-de-Mesquita, HB, Boshuizen, HC, Lahmann, PH, Clavel-Chapelon, F, et al. Consumption of vegetables and fruits and risk of breast cancer. J Am Med Assoc 2005;293:183–93. https://doi.org/10.1001/jama.293.2.183.10.1001/jama.293.2.183Search in Google Scholar PubMed
114. Aune, D, Chan, DS, Vieira, AR, Rosenblatt, DA, Vieira, R, Greenwood, DC, et al. Fruits, vegetables and breast cancer risk: a systematic review and meta-analysis of prospective studies. Breast Cancer Res Treat 2012;134:479–93. https://doi.org/10.1007/s10549-012-2118-1.10.1007/s10549-012-2118-1Search in Google Scholar PubMed
115. Jung, S, Spiegelman, D, Baglietto, L, Bernstein, L, Boggs, DA, van den Brandt, PA, et al. Fruit and vegetable intake and risk of breast cancer by hormone receptor status. J Natl Cancer Inst 2013;105:219–36. https://doi.org/10.1093/jnci/djs635.10.1093/jnci/djs635Search in Google Scholar PubMed PubMed Central
Supplementary Material
The online version of this article offers supplementary material (https://doi.org/10.1515/hmbci-2020-0021).
© 2020 Amir Shamshirian et al., published by De Gruyter, Berlin/Boston
This work is licensed under the Creative Commons Attribution 4.0 International License.
Articles in the same Issue
- Letter to the Editor
- Evidence-based medicine is a valuable tool for a successful decision-making on risk-reducing bilateral mastectomy
- Original Articles
- Melatonin inhibits high glucose-induced ox-LDL/LDL expression and apoptosis in human umbilical endothelial cells
- Effects of metformin and insulin therapy regimens on postpartum oral glucose tolerance test results in pregnant women with gestational diabetes mellitus: a comparative study
- Association of IL-33 gene rs16924159 polymorphism and recurrent pregnancy loss in Iranian Azeri women
- Greater effects of high- compared with moderate-intensity interval training on thyroid hormones in overweight/obese adolescent girls
- Effect of Artemisia absinthium ethanolic extract on oxidative stress markers and the TLR4, S100A4, Bax and Bcl-2 genes expression in the kidney of STZ-induced diabetic rats
- Associations of endothelial biomarkers, nitric oxide metabolites and endothelin, with blood pressure and coronary lesions depend on cardiovascular risk and sex to mark endothelial dysfunction on the SCORE scale
- Association of nitric oxide synthase 3 gene rs1799983 G/T polymorphism with idiopathic asthenozoospermia in Iranian Azeri males: a case-control study
- Adiponectin and leptin levels in normal weight women with polycystic ovary syndrome
- Review Articles
- Association between vitamin D deficiency and prevalence of metabolic syndrome in female population: a systematic review
- Vitamin D and sleep duration: Is there a bidirectional relationship?
- Challenges of post-traumatic stress disorder (PTSD) in Iraq: biochemical network and methodologies. A brief review
- Female urine incontinence: vaginal erbium laser (VEL) effectiveness and safety
- Breast cancer risk factors in Iran: a systematic review & meta-analysis
- Effects of melatonin supplementation on oxidative stress: a systematic review and meta-analysis of randomized controlled trials
Articles in the same Issue
- Letter to the Editor
- Evidence-based medicine is a valuable tool for a successful decision-making on risk-reducing bilateral mastectomy
- Original Articles
- Melatonin inhibits high glucose-induced ox-LDL/LDL expression and apoptosis in human umbilical endothelial cells
- Effects of metformin and insulin therapy regimens on postpartum oral glucose tolerance test results in pregnant women with gestational diabetes mellitus: a comparative study
- Association of IL-33 gene rs16924159 polymorphism and recurrent pregnancy loss in Iranian Azeri women
- Greater effects of high- compared with moderate-intensity interval training on thyroid hormones in overweight/obese adolescent girls
- Effect of Artemisia absinthium ethanolic extract on oxidative stress markers and the TLR4, S100A4, Bax and Bcl-2 genes expression in the kidney of STZ-induced diabetic rats
- Associations of endothelial biomarkers, nitric oxide metabolites and endothelin, with blood pressure and coronary lesions depend on cardiovascular risk and sex to mark endothelial dysfunction on the SCORE scale
- Association of nitric oxide synthase 3 gene rs1799983 G/T polymorphism with idiopathic asthenozoospermia in Iranian Azeri males: a case-control study
- Adiponectin and leptin levels in normal weight women with polycystic ovary syndrome
- Review Articles
- Association between vitamin D deficiency and prevalence of metabolic syndrome in female population: a systematic review
- Vitamin D and sleep duration: Is there a bidirectional relationship?
- Challenges of post-traumatic stress disorder (PTSD) in Iraq: biochemical network and methodologies. A brief review
- Female urine incontinence: vaginal erbium laser (VEL) effectiveness and safety
- Breast cancer risk factors in Iran: a systematic review & meta-analysis
- Effects of melatonin supplementation on oxidative stress: a systematic review and meta-analysis of randomized controlled trials

