SIDM2022 15th Annual International Conference
October 16-18, 2022
Planning Committee
Andrew Olson, MD | Chair
Christina L. Cifra, MD, MS | Chair
Dan Berg
Eliana Bonifacino, MD, MS
John D. Bundrick, MD, MACP
Joseph A. Grubenhoff, MD, MSCS
Helen Haskell, MA
Abraham Jacob, MD, MHA
Marie Jaffe
Rebecca Jones, MBA, BSN, RN, CPHRM, CPPS
Janice Kwan, MD, MPH
David L. Meyers, MD, MBE, FACEP
Sandra Monteiro, PhD
Ruth Ryan, RN-ret, BSN, MSW
Kathryn Schaefer, MSN, RN, CPHRM, CHCP, FASHRM
Verity Schaye, MD, MHPE
Suz Schrandt, JD
Divvy K. Upadhyay, MD, MPH
Ronald Wyatt, MD, MHA
Abstract Selection Committee
Christina L. Cifra, MD, MS
Janice Kwan, MD, MPH
Ava Liberman, MD
Najlla Nassery, MD, MPH
Rebecca Jones, MBA, BSN, RN, CPHRM, CPPS
Thilan Wijesekera, MD, MHS
Poster Session 1
Sunday, October 16
5:00 PM – 6:00 PM
A Real Headache: A Delayed Diagnosis of GCA
N. Gregorich 1, B. Pollitt Golden1
1University of Wisconsin School of Medicine and Public Health, Milwaukee, WI
Learning Objectives: 1) Understand real world presentation of Giant Cell Arteritis (GCA). 2) Identify types of bias leading to a delayed GCA diagnosis.
Case Report: A 72-year-old male presented with multiple complaints, including scrotal pain, transient vision loss, fatigue, weight loss and new headaches. ED work-up showed leukocytosis and aortic dilation on imaging. Clinicians recommended further work-up for possible infection but did not raise concern for GCA. The patient declined admission but re-presented 2 days later endorsing similar symptoms. Ultrasound showed epididymitis for which he received Bactrim. He presented to clinic several days later with “confusion” which was attributed to Bactrim. The following week, he represented with scrotal pain and confusion. Ultrasound showed improving epididymitis, but his symptoms were attributed to epididymitis, and he was prescribed cefpodoxime. Three days later, he re-presented with worsening headaches, temporal swelling, and elevated CRP, prompting admission. He underwent temporal artery biopsy which confirmed GCA.
Discussion: GCA is the most common systemic vasculitis and should be considered for patients over 50 who have new headaches, visual disturbances, and vascular abnormalities. Patients may also present with confusion. Prompt identification and treatment with corticosteroids is imperative as untreated GCA can progress to blindness. Despite his age and multiple complaints consistent with GCA, this diagnosis was not initially considered. His presentation was attributed to epididymitis, which interestingly has been associated with GCA. This patient is emblematic of broader issues in prompt GCA diagnosis, which takes a mean of 9 weeks from symptom onset. Heuristics are a helpful tool for physicians to make diagnoses. However, using mental shortcuts may have played a role in this delay, as GCA is more common in females. Anchoring bias may also have contributed. This patient endorsed persistent scrotal pain and was diagnosed with epididymitis, which may have clouded his additional complaints.
Anchoring on Ultrasound: Need for Point-of-Care-Ultrasound Competencies in Medicine Residencies
K. Huber 1, E. Breitbach2, M. Knees1
1University of Colorado, Aurora, CO
2Rocky Mountain Regional VA Medical Center, Aurora, CO
Learning Objectives: Describe existing standards for point-of-care ultrasound (POCUS) training for resident physicians. Highlight risks of utilizing new technologies for trainees without clear standardization or proof of competency.
Case Description: A 57-year-old man with end-stage renal disease on hemodialysis and heart failure with reduced ejection fraction presented to the hospital for evaluation of lower extremity edema, paroxysmal nocturnal dyspnea, and syncopal episodes. His initial exam was notable for normal vital signs, 2+ pitting edema, and elevated JVP. Initial labs revealed a normal CBC and CMP, normal troponin, and a pBNP of 9000. His EKG had diffusely low amplitude voltages and chest x-ray showed cardiomegaly. The overnight admitting resident utilized POCUS—for which they had received informal training during residency—to perform a bedside cardiac ultrasound where they noted no appreciable pericardial effusion. During morning handoff, the resident noted the lack of pericardial effusion on bedside ultrasound and the primary team-initiated treatment for presumed decompensated heart failure. During dialysis the following day, the patient became more hypotensive with a pulsus paradoxus of 14. A formal TTE was obtained which demonstrated a large circumferential pericardial effusion; the patient was taken for emergent pericardiocentesis.
Discussion: Point-of-care ultrasound is rapidly becoming a standard tool utilized during internal medicine residency training. While there is growing evidence regarding the clinical and educational merits of implementing POCUS training, there is no clear guidance on quality markers of proficiency. We present a case of early anchoring bias based on inaccurate POCUS assessment that resulted in delayed diagnosis and care. Competency assessments and standardization, like procedure certifications mandated elsewhere in graduate medical training, are one way to prevent similar errors. Proficiency assessments are a necessary component for much of residency training and should be extended to the rising use of POCUS in care.
Assessing Clinical Reasoning in Medical Students Using a Virtual Patient Simulator
R. Abdulnour 1, M. O’Rourke2, T. Smith3
1Harvard Medical School, Boston, MA
2NEJM Group, Waltham, MA
3Lake Erie College of Osteopathic Medicine, Erie, PA
Background:
– NEJM Healer is a computer-based simulator using illness script theory to enhance the teaching and assessment of clinical reasoning.
– During a virtual patient encounter, learners must select data, write problem representations, build a differential diagnosis, and propose a management plan
– After the encounter, learners perform informed self-assessments of their problem representations, management plan, and level of confidence in their lead diagnosis.
– They are given formative assessment on their lead diagnostic accuracy, differential diagnostic accuracy (DDxA), and illness script concordance.
– Educators can view all the feedback data in the NEJM Healer Educator Portal, including informed self-assessment of problem representations, management plan, and level of confidence.
Objectives:
– To augment deliberate practice for over 1100 medical students at Lake Erie College of Osteopathic Medicine (LECOM) dispersed across several campuses.
– To compare performance in NEJM Healer with learner clinical experience in a cross-sectional analysis.
Results:
– Normalized data was used to support early identification of learners who could use additional support for developing clinical reasoning skills using a defined framework.
– Comparative cross-sectional analysis of all encounters showed that pre-clerkship students spent significantly more time per encounter and had significantly lower diagnostic accuracy than post-clerkship students.
– In one encounter of medium-difficulty, DDxA was significantly lower after history-taking than after physical exam and review of diagnostic interventions (Fig. 1). DDxA of pre-clerkship students was significantly lower than post-clerkship students at every stage of the encounter.
– Post-clerkship students were significantly more confident of their diagnosis than pre-clerkship students.
– Diagnostic accuracy in NEJM Healer significantly but weakly correlated with NBOME COMLEX-USA Level 2 CE test scores.
Conclusion:
– Performance in NEJM Healer identified students who could use additional support for developing clinical reasoning skills.
– Clinical reasoning performance in NEJM Healer correlated with clinical-student experience level.
– While differential diagnostic accuracy was significantly correlated with COMLEX Level-2 CE scores in this large sample size, very little of the variation between students was predicted by their knowledge test scores, indicating that clinical reasoning requires a distinct set of skills in addition to clinical knowledge.

Challenging Nursing Students to Apply Clinical Judgment in an Online Learning Environment
L. Benike 1, R. Linck2
1University of Minnesota, Rochester, MN
2University of St. Thomas, St. Paul, MN
Purpose/Problem: For health sciences students, achieving clinical judgment demands the ability to recognize clinical cues, generate and weigh hypotheses, and take action to arrive at a satisfactory clinical outcome. Teaching to achieve clinical judgment is important and complex and requires the ability for learners to actively engage with complex clinical scenarios in a realistic context.
Description of Program: We utilized Zoom and Mentimeter technologies to facilitate an online “Active Learning Day” in an advanced nursing course for 175 senior Bachelor of Science in Nursing (BSN) students with the primary objectives of demonstrating clinical judgment and responding effectively to acute changes in patient conditions. During a 115-minute synchronous course session, students experienced complex case studies in patient care, care interruptions that required immediate intervention, NCLEX-style questions, problem solving in pairs, and faculty-led debriefing. Students were challenged to demonstrate clinical judgment by Assessing, Analyzing, and Acting upon recognized clinical cues in real-time. Mentimeter technology and Zoom breakout rooms were used to support anonymous participation amongst participants.
Outcomes: The Active Learning Day was designed to: a) achieve high learner engagement with case-based learning scenarios, b) achieve good clinical judgment as evidenced by learner responses to clinical scenarios. Participants were surveyed on their learning experience. We received a 35% survey response rate. Of those who responded, 77% (48/62) reported high engagement throughout the session, 95% (59/62) agreed the scenarios included during the session felt applicable to clinical practice, and 84% (52/62) of participants agreed that the session left them feeling better prepared to manage similar clinical situations in the future.
Discussion and Significance: Interactive learning supported by digital technology provides clinical learners with opportunities to apply clinical judgment to patient care scenarios. The use of anonymous submission functions within Mentimeter supports all learners to submit their thoughts, ideas, and responses without fear of judgment from their peers or instructors. Students engage with delivered content through Zoom connection, and by following along in a simplified format in Mentimeter using an additional personal device such as a cellphone or tablet. Learners without access to an additional device are able to engage with Mentimeter using an internet browser on their computer. Anonymity enhances the ability and willingness for students to share their thinking, which often results in richer sharing and enhanced individual metacognition during the learning session.
Characteristics of Diagnostic Errors in Outpatients Referred for Diagnosis in a University Hospital
S. Katsukura 1, T. Shimizu2, Y. Otaka2, Y. Harada2
1Dokkyo Medical University, Mibu, Japan
2Department of Diagnostic and Generalist Medicine, Dokkyo Medical University, Mibu, Japan
Background: The characteristics of diagnostic errors in primary care and emergency department settings have been investigated; however, there are scarce data regarding the characteristics of diagnostic errors in referred outpatients for diagnosis in the tertiary care setting. This study aimed to describe the characteristics of diagnostic errors in outpatients referred to a tertiary hospital for diagnostic evaluation.
Methods: We reviewed medical records of consecutive outpatients referred for diagnosis to the Department of Diagnostic and Generalist Medicine in a university hospital between January 1st, 2019, and December 31st, 2019. Diagnostic errors were judged using the Revised Safer Dx Instrument. In the cases of diagnostic errors, we conducted further reviews to clarify the contributing factors and outcomes of diagnostic errors using the Safer Dx Process Breakdown Supplement. Age, sex, referral pattern, the reason for referral, the final diagnosis, the duration, and the number of outpatient visits between the index visit and the time the final diagnosis was made, the outcome of diagnostic errors, and contributing factors for diagnostic errors were collected.
Results: A total of 534 cases were included in the analysis. Diagnostic errors were observed in 12 cases (2.2%). In the cases of diagnostic errors, the median age was 68 (57-76) years, 5 (41.7%) were women, and 5 (41.7%) were referred from other departments within the hospital. The most common reason for referral was abnormal test results (3/12, 25.0%). Based on the ICD-10 classification, the most common missed diagnosis category was ""Neoplasms"" (6/12, 50.0%: lung cancer, 2; gastric cancer, 2; pancreatic cancer, 1, cardiac myxoma, 1). The median duration and number of outpatient visits between the index visit and when the final diagnosis was made were 169 (111-310) days, and 8 (4-12) visits, respectively. Diagnostic errors resulted in temporary or permanent harm in 8 (66.7%) cases. The top three most common contributing factors for diagnostic errors were ""problems with data integration and interpretation"" (8/12, 66.7%), ""problems ordering diagnostic tests for further workup"" (5/12, 41.7%), and ""problems with monitoring patients through follow-up"" (3/12, 25.0%).
Conclusion: In referred outpatients who experienced diagnostic errors, neoplasms were missed in 50%, and 67% of diagnostic errors resulted in temporary or permanent harm. Considering the period from the index visit to the time that the final diagnosis was made in this study, reviewing 6-12 months of medical records should be required to survey diagnostic errors for referred outpatients in tertiary care settings.
Codesigning Tools to Overcome Barriers to Diagnostic Safety for Underrepresented Patients
T. Giardina 1, S. Jefferson2, M. Graber3
1Baylor College of Medicine and Houston VA, Houston, TX
2Baylor College of Medicine, Houston, TX
3Society to Improve Diagnosis in Medicine, Alpharetta, GA
Background: The NASEM report, Improving Diagnosis in Health Care, recommends partnerships with patients and families to facilitate patient engagement in the diagnostic process. While several such efforts have begun, engagement with marginalized patients needs additional focus as many patients may not be specifically included in such initiatives. Increased engagement with diverse patient populations will ensure identification of diagnostic issues that would otherwise go unnoticed and create a foundation for reducing inequality in diagnostic safety. Using a health equity lens, we conducted codesign workshops to develop a patient-centered structured tool to engage underrepresented patients in the diagnostic process following an outpatient visit.
Methods: To identify potential participants, we contacted (i.e., telephone and email) local community organizations focused on health equity and access in marginalized communities and a Veterans association in Houston, Texas. We met with the leadership at two organizations and presented a project overview and objectives. Once approved, we recruited participants via email. Interested participants were split into two groups, community health workers (CHWs, n= 5) and Veterans (n=11). To reduce burden, workshops were designed to be completed in 3-4 one-hour meetings and included: 1. Empathy mapping to identify patient concerns, 2. Developing a list of high priority concerns, 3. Developing questions, and 4. Reviewing final tool design. Workshops were conducted by an experienced qualitative methodologist via Zoom. Participants were compensated for their time. Together participants and the facilitator co-produced key areas of concern and began developing associated questions.
Results: Thus far, we have conducted 9 one-hour codesign workshops with 16 participants total. Participants were majority female (n=14) and the groups were diverse in race and ethnicity. Four participants self-disclosed as disabled. Empathy mapping helped create a shared understanding amongst participants about the experiences of diagnostic errors and to identify concerns and gaps in care. Key concerns included: bedside manner (e.g., I’d rather be sick than pushed [rushed] through. I can feel the difference), communication (e.g., There is a difference between listening and feeling heard), uncertainty (e.g., multiple referrals and diagnosis is unknown) and bias (e.g., They [doctors] do not believe Black and Brown patients.). We are currently developing questions to represent these key diagnostic safety concerns.
Conclusions: While this tool remains in development, working closely with community members holds promise for identifying relevant diagnostic concerns in diverse patient populations.
Database Design: Ensuring Positive Fecal Immunochemical Test Follow-up and Diagnostic Error Tracking
P. Foulis 1, K. Legard1, S. Bhaskar1, J. Kreinbrook2*
(*Presenting Author)
1James A. Haley Veterans’ Hospital, Tampa, FL
2Tampa VA Clinical Research and Education Foundation, Tampa, FL
Statement of the Problem: The COVID-19 pandemic disrupted colorectal cancer (CRC) screening globally, reducing screening colonoscopies. In the Veterans’ Health Administration (VHA), we overcame this by utilizing mail-out fecal immunochemical testing (FIT), a stool-based screening test. However, minimizing inappropriately administered FIT and following-up on any positive FIT (+FIT) with diagnostic colonoscopy became noticeable issues in our system. Inappropriate FIT testing is a diagnostic error as it lacks the appropriate sensitivity and specificity outside of CRC screening. Alongside mail-out FIT, we initiated a FIT navigator program to facilitate +FIT follow-up. While navigators traditionally aid in test follow-up, overcoming known patient, provider, and system-level barriers; they are also poised to capture data regarding inappropriate FIT utilization (i.e., diagnostic error).
Process Improvement Description: A FIT navigator process was introduced in late 2020 at our local VA, James A. Haley Veterans’ Hospital, with no improvement in 180-day compliance: the uptake of colonoscopy <180 days (180-day compliance). We noted a steady decline of this metric even after FIT navigator introduction, prompting this QI project which began with retrospective chart review and stakeholder meetings.
Findings to Date: Of 512 index +FIT from October 2020 (FIT navigator introduction) to August 2021, 214 did not meet 180-day compliance and 14 had an unknown colonoscopy completion due to poor documentation, yielding 286 (65.1%) with compliant follow-up. When removing inappropriately ordered FIT (N=123; 24.0%), the successful follow-up proportion dropped from 65.1% to 60.0%. In the 214 who did not meet our metric, 75 refused follow-up (35.0%). 24 of these (33.3%) failing to reach the FIT navigator. Poor system communication and transportation issues were also major factors. This data informed our inclusion of inappropriate FIT tracking into our planned intervention, a Microsoft Access database which semi-automates +FIT data retrieval and navigator tasks while also tracking FIT order appropriateness.
Lessons Learned: While +FIT navigation is an evidence-based intervention, local implementation teams should incorporate inappropriately ordered FIT tracking to capture diagnostic error. Additionally, interventions should place navigators as close as possible to the +FIT result, easing the burden on primary care providers and ensuring that barriers to follow-up are identified.

Deliberate Practice of Clinical Reasoning Reveals Important Diagnostic Justification Insights
J. Waechter 1, L. Zwaan2, J. Staal2
1University of Calgary, Calgary, Canada
2Erasmus University, Rotterdam, Netherlands
Purpose: Diagnostic errors are a large burden on patient safety and improving clinical reasoning (CR) education could contribute to reducing these errors. To this end, calls have been made to implement CR training as early as the first year of medical school. However, much is still unknown about pre-clerkship students’ reasoning processes and which aspects could be improved. The current study therefore aimed to observe how pre-clerkship students use clinical information during the diagnostic process.
Methods: In a prospective observational study, first- and second-year medical students at one medical school completed self-directed online CR diagnostic case vignettes. CR skills that were measured included: creation of the differential diagnosis (Ddx), diagnostic justification (DxJ), ordering investigations, and the final ranking of the most probable diagnosis. We also analyzed how students used history, physical exam, and investigation data, as well as pertinent positive and pertinent negative data, in their DxJ process.
Results: 121 of 133 (91%) medical students consented to the research project and completed 10 clinical cases each. We collected over 100 data per case on average, analyzing over 121,000 data. Compared with scores obtained for creation of the Ddx, ordering tests, and identifying the correct diagnosis, students scored much lower with DxJ (30-48%, p < 0.001). Specifically, students under-utilized physical exam data (p < 0.001) and pertinent negative information (p < 0.001). We observed that DxJ scores increased 40% with 10 practice cases (p < 0.001). We analyzed scores for building a Ddx, DxJ and ordering investigations and observed that higher scores in each category were independently associated with lower rates of misdiagnoses.
Conclusions: We implemented deliberate practice with formative feedback for CR starting in the first year of medical school. Students underperformed in DxJ, particularly with analyzing the physical exam data and pertinent negative data. We observed improvement in DxJ performance with increased practice and an association between higher scores in individual CR tasks and lower rates of misdiagnosis.

Development and Psychometrics of the Diagnostic Competency During Simulation-based Learning Tool
L. Burt 1, A. Olson2
1University of Illinois Chicago, Evanston, IL
2University of Minnesota School of Medicine, Minneapolis, MN
Even though diagnostic errors impact as estimated 12 million people in the United States each year, educational strategies that foster diagnostic accuracy among healthcare learners remain elusive (1-4). One solution is to focus explicitly, rather than tacitly, on competencies that are fundamental for diagnostic excellence. Individual diagnostic reasoning competencies address actions, processes and knowledge that contribute to diagnostic accuracy through information acquisition, problem representation, prioritization, decision support, and critical thinking (5). As a learning modality that allows educators to directly observe learner behaviors, simulation-based learning can be leveraged to provide behaviorally anchored feedback that will foster student competency mastery. Currently, there are no tools that comprehensively address individual diagnostic reasoning competencies during simulated learning (6-14). Our research team sought to remedy this deficit by developing and exploring psychometric properties of the “Diagnostic Competency During Simulation-based (DCDS) Learning Tool.” The purpose of this study is (1) to develop an assessment tool to quantify learner progression towards mastery of the individual diagnostic reasoning competencies during simulation and (2) to explore preliminary evidence of reliability and validity. The DCDS Learning Tool is a 28-item, behaviorally anchored tool assessing six individual diagnostic reasoning competencies (1). Items are stratified between six competencies and are rated on a 4-point ordinal scale. Educators are encouraged to leverage ratings to analyze learner behaviors, identifying trends and asymmetry between competencies, in preparation for feedback conversations. Final individual competency domain scale CVI scores ranged between 0.9175 and 1.0 and the total scale CVI score was 0.96, reflecting adequate construct representation. Inter-rater reliability is currently pending. The DCDS tool expands the current landscape of diagnostic reasoning assessment by providing educators with granular, actionable, individual competency-specific assessment measures. Linking competencies to behaviors observed during simulation, the tool can be applied by educators to facilitate conversations guided by principles of high-quality feedback—i.e., explanatory feedback tied to specific behaviors. As more healthcare disciplines pivot to competency-based education, integrating this tool into the existing landscape of simulation-based learning will aid educators striving to foster diagnostic competency. Exploratory data supports the DCDS Learning Tool as a reliable and valid instrument that can be utilized by educators to promote individual diagnostic reasoning competency growth.
Diagnostic Analysis of Initial Non – Contrast CT for Abdominal Pain During a Contrast Shortage
J. Ha 1, J. Thomas2
1Penn State College of Medicine, Hershey, PA
2Penn State Health, Dept. of Radiology, Hershey, PA
Background: An increase in COVID–19 in 2022 resulted in significant shortage of Iohexol Iodinated Contrast media. Our institution adopted contrast restrictions on 5/9/2022, including that patients presenting to the emergency department (ED) with atraumatic abdominal pain would not receive contrast. ACR recommendations for imaging of abdominal pain primarily recommend CT with contrast as the most appropriate imaging. This presents an opportunity to assess patterns of contrast utilization for improvement.
Methods: We conducted a retrospective review of CT abdomen & pelvis (a/p) exams without contrast ordered in the ED for abdominal pain from 5/9/2022-5/27/2022. Cases were categorized by indication for imaging as per ACR appropriateness criteria. Appropriateness of CT without contrast ordered was compared to appropriateness of CT with contrast. Clinical outcomes were qualitatively categorized into three groups. We also recorded types of final diagnoses, patient repeat or additional imaging, and patient outcomes.
Results: 421 CT a/p examinations were ordered in the ED from 5/9/2022-5/27/2022. 164 were excluded due to indications of trauma and sole flank pain for renal calculus. 257 cases were screened for ACR appropriateness, and 126 cases qualified for ACR appropriateness. CT with contrast was more appropriate in 86 cases, equally appropriate with ACR criteria evidence level of 4,5,6 in 16 cases and equally appropriate with ACR evidence level of 7,8,9 in 24 cases. Clinical outcome distribution is summarized in the figure. The most common final diagnoses were no diagnosis (36/126), appendicitis (9/126), and small bowel obstruction (8/126). In clinical diagnoses where CT with contrast was more appropriate abdominopelvic CT findings were still well visualized. In diagnoses where CT with and without contrast were equally appropriate, 30% (12/40) patients had no CT findings and were discharged. In diagnoses where CT with contrast was more appropriate 24% (21/86) patients had no CT findings and were discharged with none returning to the ED within 72 hrs.
Conclusion: For imaging indications where CT with and without contrast are equally appropriate this preliminary data supports CT without contrast as an acceptable alternative. This preliminary analysis suggests that CT without contrast may be an acceptable alternative for contrast CT, with room for improvement in resource utilization.

Diagnostic Correction in a Curious Case of Pylephlebitis
N. Faraci 1, G. Olenginski1
1University of Pittsburgh Medical Center, Pittsburgh, PA
Learning Objectives: 1. Explain the diagnostic process for the rare diagnosis of pylephlebitis. 2. Discuss how additional testing was needed beyond the preferred diagnostic methods to lead to the correct diagnosis.
Case Information: A 67-year-old woman with history of diverticulitis presented with subacute fatigue, malaise, anorexia, and progressive epigastric discomfort. On examination, she was afebrile, BP 84/53 mmHg, HR 134 bpm, and mildly tender to palpation in the epigastrium with decreased capillary refill. Labs demonstrated leukocytosis to 20.9 K, mild cholestatic liver injury, and lactic acidosis to 2.2 which prompted CT scan of her abdomen and pelvis with IV contrast to assess for a source of her sepsis. Acute sigmoid diverticulitis without abscess or perforation was demonstrated, as well as ill-defined right liver lobe hypodensity with intrahepatic biliary ductal dilation with associated narrowing/effacement of the right portal vein concerning for cholangiocarcinoma. She was resuscitated with crystalloid and started on empiric piperacillin-tazobactam. The next day she underwent MRCP which demonstrated pylephlebitis and thrombosis of the posterior right portal vein. Her blood cultures were without growth. She was treated with 4 weeks of piperacillin-tazobactam as well as a 3-6 month course of anticoagulation with apixaban.
Discussion: Pylephlebitis is infective thrombosis of the portal vein and can complicate intraabdominal sepsis of any etiology. Diagnosis is often delayed due to its nonspecific presenting symptoms, and it is an uncommon condition. CT and ultrasonography are typical first line diagnostic studies for pylephlebitis. This is where we were led astray in the present case, since the findings of pylephlebitis on CT scan were called as concerning for cholangiocarcinoma by the interpreting radiologist. Pursuing further imaging with MRCP allowed re-direction to the final diagnosis, which had profound impacts on her management – long-term antibiotics and anticoagulation…rather than surgical consultation.
Diagnostic Delays of MSK Infections and Clinical Pathway Execution
J. Grubenhoff 1, L. A. Bakel1, J. Searns1
1University of Colorado School of Medicine, Aurora, CO
Background: Clinical pathways (CPs) aim to align best evidence with local practice and resources and overcome the bounded rationality of diagnosticians. Some studies indicate reductions in diagnostic error (DxE) attributable to shorter time to diagnosis for emergent conditions after CP implementation. Few studies have explored diagnostic delays associated with incomplete execution of CP elements. Our objectives were to compare the clinical characteristics of patients with and without delayed diagnosis of musculoskeletal infections (MSKI) and identify repeatedly missed opportunities when applying an MSKI diagnostic CP.
Methods: E-trigger followed by manual screening identified children with unplanned admission within 10 days of index ED encounters from 1/1/2018-12/31/2021. Cases with disparate but potentially related diagnoses at index encounter and hospital discharge were reviewed using the Revised SaferDx to determine presence of DxE. The diagnostic evaluation of patients discharged with pyomyositis, osteomyelitis or septic arthritis during the index encounter was compared to the recommended diagnostic testing and consultation in the CP. Descriptive statistics comparing patients with and without MSKI diagnostic delays were performed: X2 for proportions and Wilcoxon Rank Sum for continuous variables.
Results: 3407 patients met e-trigger criteria. 774 (22.7%) screened in for SaferDx review and 163 had DxE. 33 patients (4.2%) had MSKI; 23 (63.6%) experienced diagnostic delays accounting for 14.1% of all DxEs. Patients did not differ in age, sex, race, language, triage acuity or presence of fever. Patients with MSKI DxE more often had fever + limb/back pain (57.1% vs 16.7%; p=0.02). The differential diagnosis included MSKI more often in patients with DxE (61.9% vs 25.0%; p=0.04). Patients with MSKI DxE returned 4 days sooner than those without DxE [median days to diagnosis 2.9 (IQR 1.9-3.8) vs 6.9 (IQR 3.8-8.6); p<0.01]. The figure shows the diagnostic trajectories of the two groups.
Conclusions: Despite having a history concerning for and differential diagnosis including MSKI, patients with delayed diagnoses demonstrated three distinct CP failure points: not receiving indicated labs; not receiving consultation; and not receiving indicated imaging. Incomplete execution of an MSKI CP delayed diagnosis of MSKI.

Driving Close the Loop Communication with Medicaid Quality Incentive
T. Anderson 1
1Washington State Hospital Association, Seattle, WA
The Medicaid Quality Incentive program is a driver of change and reward for accomplishments of quality improvement for the state. Hospitals in Washington State can earn a one percent incentive payment under the Medicaid Quality Incentive Program. The payment is funded in part from a Safety Net Assessment and federal matching dollars. The Association develops 12 quality measurement guidelines for the Medicaid Quality Incentive each year. In selecting the measures, national guidelines and clinical experts are utilized to identify potential measures that are evidence-based and significant for Medicaid patients. The final selection of measures was done by the Medicaid Administrator for the state. Eligible hospitals wishing to earn the quality incentive will report on accomplished measures for specified care units. One of the newer association strategies for the Safety & Quality team and the hospitals is Diagnostic Excellence. This topic does not have well-established, published, and satisfactory baseline measures. The Association’s Subcommittee on Diagnostic Excellence desired to understand the completeness of close-the-loop communications surrounding critical lab and imaging results to an actionable provider. Data was collected on critical lab and imaging studies communications, as well as the total number of critical labs and studies as well as the total number of completed labs and studies for a hospital. Aggregated findings will be discussed as well as plans to continue to drive improvement on this measure.
Electronic Triggers to Study Diagnostic Errors in Pediatric Emergency Departments
P. Mahajan 1, A. Payne2, K. Shaw3, H. Singh4, M. Carney1, K. O’Connell2, D. Morrison Ponce5, J. Chamberlain2, J. Corboy6, R. Ruddy7, E. Alpern8, B. Ku9, N. Klekowski1, E. White1, A. Krack10, E. Freiheit1
1University of Michigan, Ann Arbor, MI
2Children’s National Health System, Washington, D.C.
3University of Pennsylvania Perelman School of Medicine, Philadelphia, PA
4Baylor College of Medicine and Houston VA, Houston, TX
5Uniformed Services University of the Health Sciences F. Edward Hebert School of Medicine, Bethesda, MD
6Ann & Robert H. Lurie Children’s Hospital of Chicago, Chicago, IL
7University of Cincinnati, Cincinnati, OH
8Northwestern University, Evanston, IL
9Children’s Hospital of Philadelphia, Philadelphia, PA
10University of Colorado, Denver, Denver, CO
Background: Diagnostic errors, or missed opportunities for improving diagnosis (MOIDs), lead to safety concerns in pediatric emergency departments (EDs). We sought to identify triggers to screen ED records for diagnostic errors. After pilot testing, we applied three electronic triggers (eT) to study frequency and contributory factors of diagnostic errors in pediatric EDs: return visits within 10 days resulting in admission (eT1), care escalation to intensive care unit within 24 hours of ED presentation (eT2), and death within 24 hours of ED visit (eT3).
Methods: We created a standardized electronic query and reporting template for the 3 eTs and applied them to electronic health record systems of 5 pediatric EDs. Using ED visits from 2019, we included a random subset of 400 ED visits for eT1 and all visits for eT2 and eT3 at each site. We trained 2 clinicians from each ED to review the triggered cases. Each reviewer manually screened the chart and initially categorized charts as “unlikely for MOIDs” or “unable to rule out MOIDs”. For the latter category, reviewers performed a detailed chart review using Revised Safer Dx Instrument to categorize as MOIDs or no MOIDs, dichotomized as a score ≥ 5 out of 7 on a Likert scale as suggestive of a MOID.
Results: 2785 ED records met trigger criteria (eT1 1885 (68%), eT2 786 (28%), eT3 114 (4%)), of which 2638 (95%) were categorized as unlikely for MOIDs. The Safer Dx Instrument was applied to 147 (5%) records and 72 (49%) had MOIDs. The proportion of charts with MOIDs ranged from 0.6% to 4.3% across sites. The overall frequency of MOIDs in the triggered charts was 2.6% (72/2785) for the entire cohort, 3.0% (57/1885) for eT1, 1.9% (15/786) for eT2, and 0% (0/114) for eT3. The most common diagnoses associated with MOIDs were pneumonia (10/72) and appendicitis (7/72). 54% (39/72) had patient harm due to MOIDs. Contributing factors were most often able to be assigned to patient-provider factors (36/72), followed by patient factors (16/72), system factors (10/72), and provider factors (8/72).
Conclusions: Electronic triggers with selective record review is an efficient way to screen large numbers of medical records to identify diagnostic errors in pediatric ED visits. Detailed chart review of 5% of charts revealed MOIDs in half, of which half were harmful. Triggers can be an integral part of diagnostic safety measurement systems and can identify cases for additional review, analysis, and improvement.
Emphysematous Pyelonephritis in a Kidney Transplant Recipient: A Diagnosis Not to Miss!
R. Lomanto Silva 1, C. Caglayan1, R. Correa Fabiano Filho1
1University of Pittsburgh Medical Center, Pittsburgh, PA
Learning Objectives: Emphysematous pyelonephritis (EPN) is a necrotizing infection of the urinary tract with gas formation. This condition affects almost exclusively (90-96%) patients with diabetes mellitus or urinary tract obstruction. EPN carries high mortality thus early recognition is crucial. It can present with vague complaints and develop a fulminant course. We highlight here a rather unusual case of a female with systemic erythematous lupus (SLE) who presented with delusions and non-specific symptoms, making EPN a diagnostic challenge.
Case Information: 41-year-old female with SLE and lupus nephritis post failed kidney transplant on dialysis presented with reports of being assaulted by spirits. Due to a history of mental illness and no signs of physical trauma, she was recommended outpatient psychiatric follow-up. Two days later, she returns to the hospital with chest pressure, anorexia, fatigue, dysuria, and body aches. Initial vital signs and basic laboratory studies were unremarkable. CRP was elevated. Urinalysis (UA) revealed >900 white blood cells, leukocyte esterase, many bacteria. Chest x-ray showed small pleural effusions. Empiric coverage for community-acquired pneumonia (CAP) was started. Over the next 48 hours, patient became subfebrile, tachycardic, and hypotensive. Per results of UA, dysuria, and unsatisfying diagnosis of CAP, we pursued CT abdomen/pelvis. CT showed EPN on the transplanted kidney. After transplant nephrectomy and antibiotics, delusions and systemic symptoms resolved.
Discussion: From a death sentence decades ago, in modern medicine mortality due to EPN is decreased with the advent of antibiotics with percutaneous drainage, ureteral stenting, or nephrectomy. A nonspecific presentation leading to delayed radiographic workup has a central role in detrimental outcomes, as EPN’s diagnosis is established with imaging. We wish to underscore the importance of sensitizing providers to the seriousness of this disease, especially considering the literature on EPN on non-diabetic patients without obstructive uropathy is still scarce.
Exploring Diagnosis through Clinical Pathways: A Qualitative Study
Y. Fatemi 1, S. Mamede2, J. Shea3, J. Hart1, A. Costello1, S. Coffin1, K. Shaw4, L. Lieberman1
1Children’s Hospital of Philadelphia, Philadelphia, PA
2Erasmus University Rotterdam, Rotterdam, Netherlands
3University of Pennsylvania, Philadelphia, PA
4University of Pennsylvania Perelman School of Medicine, Philadelphia, PA
Background: Clinical pathways adapt evidence-based recommendations to local settings. They have been shown to improve patient outcomes and reduce resource utilization by decreasing unnecessary admissions, improving time to treatment, and decreasing variations in care. However, it is unknown how physicians integrate clinical guidelines into their diagnostic reasoning and how clinical pathways affect the diagnostic re-evaluation process.
Methods: We conducted a single-center qualitative study involving one-on-one semi-structured interviews of pediatric residents and pediatric hospitalist attendings between August 2021 and March 2022. Recruitment of participants was conducted primarily via email with some targeted recruitment of residents due to initial low response. Interviews were audio-recorded and professionally transcribed. We utilized an inductive thematic analysis strategy to code data and identify themes.
Results: We interviewed a total of 27 physicians: 15 pediatric residents and 12 pediatric hospitalists. Thematic analysis of interview transcripts revealed 4 themes related to physician utilization of and experience with clinical pathways: 1) clinical pathways use as a tool, 2) clinical pathways as a representation of standardization of care in medicine, 3) clinical pathways as a reflection of institutional culture, and 4) the dynamic relationship between clinical pathways and clinician diagnostic process. Within theme 4, the clinician’s experience was integral to choosing a clinical pathway. Additionally, clinical pathways were felt to influence the overall diagnostic process with many participants expressing concern for cognitive biases such as diagnostic momentum leading to missed or delayed diagnoses.
Conclusions: Clinical pathways are an integral component of many healthcare practices and systems. These pathways are also part of a clinician’s diagnostic framework. Pathways are commonly used as a reference and teaching tool, operationalize standardization of care in medicine, reflect local institutional culture, and can influence the diagnostic process. Further research is required to determine optimal clinical pathway design to augment and not impede the diagnostic process. In particular, further exploration of “diagnostic pauses” may address concerns about diagnostic momentum.

Gabapentin Induced Myoclonus
R. Deshpande 1, R. Thirumaran1, T. S. Rajmohan1, N. V. D. Kagita1, A. S. Shaik1
1Mercy Fitzgerald Hospital, Newtown, PA
Learning Objective: Evaluation of gabapentin adverse effects.
Case: A 71-year-old woman with a past medical history of hypertension, hyperlipidemia, coronary artery disease, and peripheral neuropathy with recent history of urinary tract infection presented with myoclonic jerks of both upper extremities and altered mental status for 6 hours. Her home medications included amlodipine, aspirin, clopidogrel, statin, gabapentin, and acetaminophen. Initial vitals were notable for tachycardia to 110 beats/min, hypotension to 80/60 mm Hg, tachypnea to 24 respirations/min. Labs showed creatinine-5.2 mg/dl, serum potassium-7.5mmol/L, and lactate-3.5 mmol/L. Resuscitation with 30 mL/kg body weight of normal saline was performed and broad-spectrum antibiotics were started. Due to persistent hypotension post-resuscitation, norepinephrine infusion was initiated. Her blood pressure and heart rate improved, but the myoclonic jerks persisted. Thus, gabapentin was withheld. Creatinine improved and the patient’s myoclonic jerks then subsided. She remained symptom free and was discharged with an adjusted dose of gabapentin for her creatinine clearance.
Discussion: Gabapentin is a neurotransmitter structurally similar to GABA, and freely crosses the blood-brain barrier. It has a half-life (t1/2) of 6-7 hours and is renally excreted after approximately 48 hours which is 7-8 half lives. Gabapentin toxicity usually remains asymptomatic but may present with myoclonus as seen in our patient. The exact mechanism, though unknown, is attributed to serotonin involvement. Serum concentrations of >/=15 μg/mL, end stage renal disease, and acute kidney injury are most commonly associated with it. The t½ is prolonged with extended release preparations and in patients with renal impairment, thus requiring dose adjustment based on creatinine clearance. Treatment is mainly supportive, and severe cases may require dialysis. Gabapentin has many off-label uses and hence understanding of its pharmacokinetics, toxicity and dosing in renal failure is important to all clinicians.
God, I could sure use a vodka!
T. Schousek 1
1Vital Innovations LLC, Houlton, WI
The patients subject to diagnostic error included a twenty-nine-year-old female, white, professional electrical engineer, pregnant, and a newborn, male, white, whom shall be referred to as Patient 1 and Patient 2, respectively.
Patient 1 had received routine prenatal care for six months. Patient experienced symptoms of first trimester bleeding that subsided. Symptoms, including visual distortion, lethargy and breathlessness during exertion, intensified in the four weeks prior to the Serious Adverse Event (SAE). Conversation regarding increasing symptoms with scheduling receptionist yielded an appointment six weeks from previous check-up.
At last check-up, a maternal blood triple test was conducted. Patient obtained the triple test results by fax, after intentional delays and thwarted attempts to see the provider. These were motivated by personal anti-abortion beliefs of the provider’s staff. Patient’s sister, a physician, reviewed the test results and indicated the need for an ultrasound to assess validity of the test. Patient 1, unable to get a near-term appointment, sought an ultrasound at an abortion provider who provided a next day appointment. Ultrasound indicated no likely fetal abnormalities. This, however, did not fully explain the positive test results in the odd pattern. No diagnosis was given. These test results were known to indicate problems with the pregnancy, such as preeclampsia and placental abruption. (Cnattingius S, et al., 1997)
Patient 1 presented at a small rural hospital emergency room with vaginal bleeding and pain. Bleeding persisted with patient in tetanic labor. The ob/gyn broke the water during a dilation digital examination. This prompted an emergency, classical c-section and preterm delivery. Ob/gyn ‘nicked’ the newborn badly, leading to a copious amount of blood loss. Pulse rate dropped to 60 bpm and newborn expired.
Ultimate diagnosis was suspected preeclampsia leading to placental abruption. Upon reflection, there were clear signs of preeclampsia that Patient 1 provided to her primary ob/gyn’s staff. The delay in access ultimately led to the death of Patient 2 and the near death of Patient 1.
Other reflections include the observation that:
Provider was unaware of patient’s symptoms and efforts to reach her.
Providers/staff with political agendas may work against the patient’s best interest.
Rural hospitals are ill equipped for any type of uncommon emergency.
Opportunities for learning and research include:
Catastrophic failures are predictable.
Attempts to reach a provider should be logged.
Diagnostic error events are frequently preceded by provider or institution switching.
Cost of Fear “is appalling” (Walton, 1986)
Rarely does diagnostic error exist in a vacuum.
Hypercholesterolemia in Nephrotic Syndrome
R. Deshpande 1, N. V. D. Kagita1, A. U. Kulkarni1, A. S. Shaik1, A. Shah1
1Mercy Fitzgerald Hospital, Newtown, PA
Learning Objective: Evaluation of Hypercholesterolemia
Case: A 21-year-old male with a past medical history of asthma presented for bilateral lower extremity pitting edema and bilateral eyelid swelling. Significant labs were as follows- Cholesterol: 819 mg/dL, LDL: 753 mg/dL, triglycerides: 175 mg/dL, albumin: <1.5 g/dL, proteinuria: >500 mg/dL, and occult hematuria. Nephrology suggested serologies for double-stranded DNA, ANA, PLA-2 antibody complements, and Hepatitis B/C panels which were negative. Cryoglobulin, as well as antibodies for glomerular basement membrane, proteinase, and myeloperoxidase were negative. Renal ultrasound showed bilateral echogenic kidneys with maintained cortical thickness. Other labs included ApoB >240 mg/dL, urine protein/creatinine ratio of 7.13. Protein electrophoresis showed elevated alpha-2 globulins at 35.7% and serum viscosity remained normal at 1.5. Patient was started on atorvastatin for hyperlipidemia, lisinopril for proteinuria and furosemide for pedal edema. Patient improved symptomatically and was discharged to follow up outpatient with renal biopsy showing membranous nephropathy.
Discussion: Nephrotic syndrome is glomerular disease with heavy proteinuria, hypoalbuminemia, and peripheral edema. Membranous nephropathy (MN) is one of the most common causes which can be secondary to conditions like Hepatitis B/C or systemic lupus erythematosus and primary as seen in our patient which is diagnosed after ruling out secondary causes. Hyperlipidemia in nephrotic syndrome occurs with 87% having >200 mg/dl of cholesterol levels with only 25% having levels >400 mg/dL, which likely is due to upregulation of apoprotein B production secondary to reduced plasma oncotic pressure. Our case is unique because of the marked elevation in cholesterol and LDL. Treatment for MN includes statin therapy and an ACE inhibitor for underlying kidney disease which usually reverses hyperlipidemia. Nephrotic syndrome secondary to membranous nephropathy should be suspected in patients presenting with unduly high lipid panel and edema.
Identifying Diagnostic Opportunities Using Clinical Trajectories: Case Study in Colorectal Cancer
J. Koola 1, D. Laub1, S. Nemati1, R. El-Kareh1
1University of California San Diego, San Diego, CA
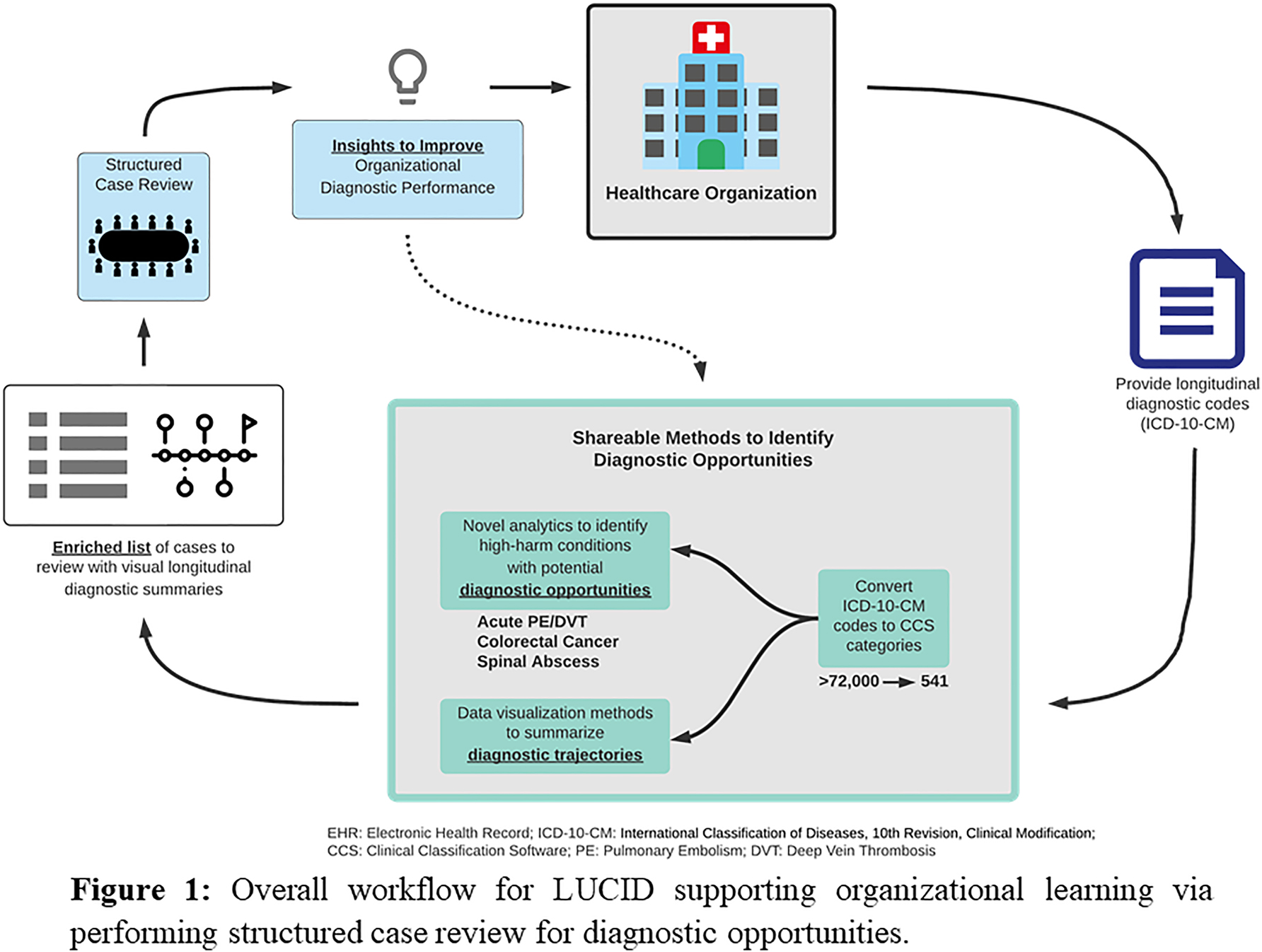
Background: Identifying organizational opportunities to improve diagnostic safety often requires retrospective chart review—a time-intensive process. To support organizational learning from diagnostic opportunities, Longitudinal Analysis of Codes to Identify Diagnostic Opportunities (LUCID) identifies high yield cases for chart review (Figure 1). LUCID summarizes diagnostic trajectories and meaningful transitions prior to the target diagnosis. We hypothesized that these trajectories and transitions provide a signal for diagnostic opportunities.
Methods: We extracted data for adult patients with CRC, defined using International Classification of Diseases 10 (ICD10) codes. We created a matched control cohort based on demographics and healthcare utilization. To identify diagnostic transitions, we mapped ICD10 codes to Agency for Healthcare Research and Quality Clinical Classifications Software (CCS) categories and identified new CCS categories in the 180-day pre-CRC diagnosis “lookback” period. We constructed a logistic regression model predicting CRC diagnosis with these new categories as predictors and assessed model discrimination and calibration. Using clinical trajectory visualizations and summaries, we performed structured case reviews to identify diagnostic opportunities for a random sample of CRC subjects with a new CCS in the lookback period. We compared presence of diagnostic opportunity to quartiles of predicted probability from the regression model.
Results: We analyzed a cohort of 387 CRC subjects who met inclusion criteria. The logistic regression model had an AUC of 0.74 and the Hosmer-Lemeshow test showed acceptable calibration. Cases had a median predicted CRC probability of 13.4% (IQR:5.6%–48.5%). Of the 27 subjects where we performed chart review to date, 15 (55.6%) had potential diagnostic opportunities. Within the lowest to highest quartiles of predicted CRC probability there were 4/9 (44.4%), 4/5 (80.0%), 4/6 (66.7%), and 3/7 (42.9%) opportunities.
Discussion: Our LUCID system pilot demonstrated feasibility of using longitudinal codes to highlight cases for diagnostic learning. Diagnostic opportunities were common in LUCID-identified cases and the summaries facilitated efficient case review. We are performing additional CRC case reviews to adequately power an analysis between quartiles of predicted probability and diagnostic opportunities. The LUCID workflow is generalizable to any target diagnosis, and our future work will assess its utility for other conditions at risk for diagnosis-related harm.
Implementation of a Novel Electronic Handoff Tool in ICU-to-ward Transitions of Care
E. Fukui 1, E. Harris2, L. Santhosh2, P. G. Lyons3, E. K. McCune2, J. C. Rojas4
1University of California, San Francisco School of Medicine, San Francisco, CA
2University of California, San Francisco Medical Center, San Francisco, CA
3Washington University in St. Louis School of Medicine, St. Louis, MO
4University of Chicago Medical Center, Chicago, IL
Statement of Problem: The transition of hospitalized patients from the intensive care unit (ICU) to the inpatient ward is a particularly high-risk period due to medical complexity, reduced monitoring, and diagnostic uncertainty. Miscommunication during clinician handoff (e.g., missing or unclear information, ambiguous responsibility for patients) increases the likelihood of medical errors and adverse events (Lyons et al., 2016), as well as cognitive errors such as anchoring bias and premature closure. Although standardized handoff processes are known to reduce medical errors and adverse outcomes (Starmer et al., 2014), these approaches are understudied at the ICU-ward interface, which remains vulnerable to non-standard and suboptimal practices (van Sluisveld et al., 2017).
Description of the Intervention: The ICU-PAUSE is a user-centered, electronic ICU-to-ward transfer tool created using Human-Centered Design methods with focus groups of Internal Medicine residents across three academic medical centers (Santhosh et al., 2022) (Figure 1). It explicitly embeds a diagnostic pause at the time of transfer of care, acknowledging that this is a high-risk period for patients. ICU-PAUSE was piloted in the medical ICU at Barnes-Jewish Hospital, the teaching hospital of Washington University School of Medicine in St. Louis, in 2019 and 2020.
Findings to Date: The ICU-PAUSE offers a structured ICU-ward template to synthesize key information, communicate clinical reasoning, and prevent associated medical errors in the handoff process (Santhosh et al., 2019). Thus far, six of ten participating sites have begun implementation and data analysis, including analysis of equity metrics (e.g., diagnostic uncertainty as it relates to age, sex, race/ethnicity). Post-implementation analysis will evaluate the feasibility, acceptability, and adoption of ICU-PAUSE into the physician transfer workflow. We will assess the perceived impact by residents and hospitalists on communication failures and clinical reasoning during transfer.
Lessons Learned: We used Human-Centered Design to co-create a novel standard communication framework for patients transitioning from the ICU to the ward, called ICU-PAUSE, which explicitly embeds a diagnostic pause at transition of care. The inclusion of a diagnostic “pause” in the ICU-PAUSE tool allows explicit acknowledgment and discussion of diagnostic uncertainty to decrease the risk of communication errors and prevent premature closure.

Improvement of Diagnostic Accuracy of Artificial Intelligence-based Differential Diagnosis Lists
A. Hayashi 1, Y. Harada1*, S. Tomiyama1, R. Kawamura1, T. Sakamoto1, T. Shimizu1, M. Yokose1
(*Presenting Author)
1Department of Diagnostic and Generalist Medicine, Dokkyo Medical University, Shimotsuga, Japan
Background: Recently the concept of “collective intelligence” has been expected to improve the accuracy of diagnosis. An Artificial Intelligence (AI) -based automated medical history taking system (AI-AMHTS) collects appropriate information prior to consultation and presents a list of differential diagnoses (DDx), but the diagnostic accuracy of single AI-AMHTS is said to be low. This study aims to clarify whether combining the DDx lists from multiple AIs (collective intelligence of AI) improves diagnostic accuracy.
Methods: We used charts and DDx lists developed by an AI-AMHTS with a DDx generator (system A) from a cohort of 103 patients aged 18 years and older who visited the outpatient department of a community hospital in Japan and were admitted within 30 days from the index outpatient visit between January 1 and December 31, 2020. Two researchers (researchers A and B) read the charts made by system A and inputted items into two commercially available differential diagnosis generators (system B and C, respectively) to develop additional DDx lists without seeing the DDx lists of system A. Other independent researchers assessed whether the correct diagnosis was included in the DDx lists of systems A, B, and C. The primary outcome was the prevalence of cases where the correct diagnosis was included in the DDx lists of AIs (correct diagnosis rates). We used McNemar’s tests to compare the correct diagnosis rates.
Results: A total of 103 cases were included in this study. The baseline correct diagnosis rate of system A was 45.6%. The correct diagnosis rates were improved by using combined DDx lists of the three systems (researcher A, 63.1%, p < 0.001; researcher B, 66.0%, p < 0.001). Furthermore, in 55 cases (53.4%) that one or more same diagnoses were included in each DDx list of the three systems, compared to the correct diagnosis rate of system A (49.1%), the correct diagnosis rates of the combined DDx lists were further improved to 74.5% (researcher A, p=0.01) and 70.9% (researcher B, p=0.001), respectively.
Conclusion: The accuracy of DDx lists of AI-AMHTS can be improved by combining other AI-based DDx generators.
Correct diagnosis rates of each and combined DDx lists of AI-based DDx generators
| Researcher A | p-Value (vs. system A) | Researcher B | p-Value (vs. system A) | |
|---|---|---|---|---|
| System A | 47/103 (45.6%) | N/A | 47/103 (45.6%) | N/A |
| System B | 40/103 (38.8%) | 0.24 | 44/103 (42.7%) | 0.75 |
| System C | 32/103 (31.1%) | 0.02 | 23/103 (22.3%) | <0.001 |
| At least one system included correct diagnosis | 65/103 (63.1%) | <0.001 | 68/103 (66.0%) | <0.001 |
| At least two systems included correct diagnosis | 38/103 (36.9%) | 0.052 | 33/103 (32.0%) | 0.006 |
| All systems included correct diagnosis | 16/103 (15.5%) | <0.001 | 13/103 (12.6%) | <0.001 |
Inclusion of the PE in SyncoPE
D. Amin 1, A. Vasa1
1Cook County Stroger Hospital, Chicago, IL
Learning Objectives: • Analyze the common but less recognized presentation of a pulmonary embolism. • Describe the pathophysiology of syncope caused by a pulmonary embolism.
Case: 79-year-old female history of coronary artery disease status post stents, diabetes, heart failure with preserved ejection fraction and obstructive sleep apnea presented to the emergency department (ED) after a witnessed syncopal episode in the lobby of the hospital. On arrival she was neurologically intact and found to be in atrial fibrillation on EKG. VS: 36.3ºC (oral), HR 00, BP 111/58, RR 21, SaO2 88%on 2 liters of oxygen. Exam showed small hematoma to the back of head with non-labored respirations and clear lung sounds. Head CT and chest x-ray were negative. Labs were normal. She continued to be hypoxic while on 2L of oxygen in the ED. A chest CT was pursued the next day and revealed large pulmonary emboli in bilateral main pulmonary arteries with extension to bilateral lobar and subsegmental levels. Patient taken urgently for thrombectomy with interventional cardiology.
Discussion: The diagnosis of pulmonary embolism (PE) is challenging and diagnostic error or delays in diagnosis can lead to death or severe morbidity. Failure to diagnose PE leads to devastating complications, with up to 30% of untreated patients die. Our patient was found to be in atrial fibrillation without being on anticoagulation which was her largest risk factor for PE. The prevalence of PE in patients presenting with syncope to the ED is unknown but investigation should be guided by the patient’s history and physical and risk factors. PE-induced syncope can be explained by three mechanisms. First, occlusion of more than 50% of pulmonary vessels leads to right ventricular failure and left ventricular filling impairment, causing a sudden drop in cardiac output and cerebral blood flow. Second, PE may induce arrhythmias from right ventricular strain. Third, the embolism itself may provoke a vasovagal reflex leading to neurogenic syncope. Early identification is vital to avoid hemodynamic compromise and to optimize survival.
International Classification of Disease (ICD) Code Set for Adverse Drug Event Detection and Quality
T. Adam 1, M. Rafiei2
1University of Minnesota, Minneapolis, MN
2St. Catherine University, St. Paul, MN
Statement of Problem: Adverse drug events (ADEs) lead to injury or death for 1.6 million patients annually in the United States, according to the 2007 Institute of Medicine report, “Preventing Medication Errors”. Adverse drug events can include allergic reactions, untoward medication-specific side effects, or unexpectedly large medication effects resulting in toxicity. ADE identification is a key starting point to investigate ADE causes such as diagnostic error, inappropriate prescribing, and drug-drug interactions.
Description of Program: The ADE program utilized available data sources for retrospective screening of ADEs for quality improvement and research. A previously developed ADE terminology, using ICD9 codes, was reviewed and updated.1 The ICD9-based ADE terminology was mapped to ICD10 using web-based mapping tools, Center for Medicare and Medicaid Services general equivalence mapping files, text matching and expert clinical review. The 2015 National Inpatient Sample was used to provide inpatient adverse event data for ADE validation.
Findings to Date: The ICD mapping and ADE validation results are in Table 1. The mapping of the ADE codes is notable for a larger number of ICD codes which are relevant for ADEs with ICD10 codes (533 codes for ICD9 and 1409 codes for ICD10). The relative numbers of ADEs identified with ICD9 codes (Events9) are compared to those identified with ICD10 codes (Events10).
Lessons Learned: The greater granularity of ICD10 yields more ADE-related ICD codes. The number of identified events was relatively lower in some drug categories and higher in others which will require additional evaluation for mapping quality. The ICD10 mapping appears to provide sufficient representation to identify ADEs. Future work will replicate the results in another large clinical data with more recent data.
References: 1. Adam TJ, Wang J. “Adverse Drug Event Ontology: Gap Analysis Clinical Surveillance Application” AMIA Jt Summits Trans Sci Proc.(2015) 16–20.

Measuring Missed Opportunity in Diagnosis in Abnormal Test Result Follow up In Post ED Visit
V. Vaghani 1, U. Mushtaq1, H. Singh2, D. Sittig3, D. Murphy1, U. Mir1, W. Li4
1Baylor College of Medicine, Houston, TX
2Baylor College of Medicine and Houston VA, Houston, TX
3University of Texas School of Biomedical Informatics, Houston, TX
4Michael E. DeBakey Veterans Affairs Medical Center and Baylor College of Medicine, Houston, TX
Background: Missed opportunities in diagnosis (MOD) resulting from failures in abnormal test result communication are a significant patient safety concern in outpatient settings and often lead to patient harm and malpractice claims. Electronic health records (EHRs) are used to communicate abnormal test results to providers and to patients and can help to ensure reliable delivery of important clinical information. However, they do not guarantee that this communication results in appropriate follow-up action. In this study, we aimed to measure MODs due to follow-up failures related to three abnormal test results in the post-ED visit setting.
Methods: We developed a new e-trigger using the Safer Dx Trigger Tools Framework. Based on current literature and our prior work on test result communication failures in outpatient primary care settings, we developed an algorithm to detect abnormal urine cultures, blood cultures, and thyroid stimulating hormone (TSH) test results ordered in treat and release ED visits that had not been followed-up. We excluded patients who were enrolled in hospice or palliative care and terminal cancer patients. One physician served as the primary reviewer for all records, and a second physician-reviewer independently evaluated a random subset of 20% of records to assess the reliability of judgements related to MODs. Prior to the validation chart review, we pilot-tested the chart review process using operational definitions and standardized procedures. Physician-reviewers were trained to use structured electronic data collection instruments to ensure standardized data collection and to minimize data entry errors.
Results: The e-trigger was applied to >9 million patient records, and 105 randomly selected trigger-positive cases, including 35 each of trigger-positive cases for Urine culture, Blood culture, and TSH were identified. Of 100 trigger-positive cases reviewed thus far (Table 1), 52 (52%) cases had MODs, and 48 (48%) had no MODs. Nine (25.7%) of 35 Blood culture, 22 (62.9%) of 35 TSH, and 21 (70.0%) of 30 Urine culture results had MODs. Thus, positive predictive value (PPV) of this e-trigger is 52.0%.
Conclusion: An abnormal test result-based e-trigger using data mining and confirmatory record reviews identified patients with MODs with high PPV. This e-trigger could be used to proactively identify and track patients who need follow-up in order to prevent delays in diagnosis.
Table 1 Baseline Characteristics of Patients in MOD (missed opportunity in diagnosis) and No MOD group
| Overall (n=100) | MOD (n=52) | No MOD (n=48) | |
|---|---|---|---|
| Age (mean, SD) | 68.9 (15.8) | 70.2 (15.2) | 67.6 (16.4) |
| Gender | |||
| Male | 87 (87.0%) | 46 (88.8%) | 41 (85.4%) |
| Female | 13 (13.0%) | 06 (11.5%) | 07 (14.6%) |
| Race | |||
| White | 69 (69.0%) | 38 (73.0%) | 31 (64.5%) |
| African American | 16 (16.0%) | 6 (11.5%) | 10 (20.8%) |
| Native Indians | 1 (1.0%) | 1 (1.9%) | 0 (0.0%) |
| Others | 8 (8.0%) | 3 (5.7%) | 5 (10.4%) |
| Decline to answer | 7 (7.0%) | 5 (9.6%) | 2 (4.1%) |
| Ethnicity | |||
| Hispanic or Latino | 07 (7.0%) | 04 (7.6%) | 03 (6.2%) |
| Non-Hispanic or Latino | 87 (87.0%) | 46 (88.4%) | 41 (85.4%) |
| Other | 06 (6.0%) | 02 (3.8%) | 04 (8.3%) |
| Ordered Test | |||
| Blood culture | 35 (35.0%) | 9 (17.3%) | 26 (54.2%) |
| TSH | 35 (35.0%) | 22 (42.3%) | 13 (27.1%) |
| Urine culture | 30 (30.0%) | 21 (40.4%) | 9 (18.8%) |
Nothing About Us Without Us: Creation of a Family Advisory Board to Drive Diagnostic Equity
A. Mack 1, J. Schaffer1, I. Rasooly1, U. Nawab1, A. Kratchman1, A. Colfer1
1Children’s Hospital of Philadelphia, Philadelphia, PA
Problem: Engagement with patients and families as collaborators in the diagnostic process has been recognized as a primary driver of diagnostic excellence. Strategies for sustained collaboration with patients/families are needed.
Method: As a part of our institution’s efforts to improve diagnosis and enhance patient safety we established a family advisory panel with the goal of prioritizing involvement of patients and families as we establish best practices for promoting diagnostic excellence. Participants were recruited through our already-established Research Family Partners program, with the goal of recruiting a diverse group of parents who have one or more children currently or previously treated at the Children’s Hospital of Philadelphia. Meetings were held virtually on a quarterly basis and scheduled for two-hour sessions in the evenings to allow for participation of people employed during the workday. Participants were compensated monetarily for their time. Initial topics for discussion focused on communication styles between families and hospital staff. Conversations were facilitated by team members. Detailed notes were taken during each meeting to share with the larger group, and to be reflected on in subsequent team meetings in a form of qualitative analysis.
Results: This dedicated family advisory council was developed to reflect the community composition, including disadvantaged populations at risk for disparate care. On average, five parents were able to attend each meeting, with a 6th partner joining our third meeting. Retention, participation. Within these first 3 meetings family advisory council members gave input on best practices to communicate uncertainty with families, discussed patient post-care survey comments that addressed concepts such as feeling dismissed and being left out of their child’s care, and talked through the utility of family access to patient medical records. Record. To date, this endeavor has informed improvement efforts such as working to improve communication of uncertainty in the emergency department, including developing note templates, revamping MD to MD handoff, and brainstorming future PDSA cycles.
Conclusion: Through its first three council sessions, the organizers have received positive feedback from the family partners and the larger diagnostic excellence project alike. This council is enabling us to build improvement initiatives in partnerships with the families, rather than asking for feedback on already established practices. Our experience is that we have found that family advisory councils are a feasible, valuable approach to engaging diverse stakeholders in the diagnostic improvement process.
Patients’ and Clinicians’ Experiences and Views on Safety-netting Advice and its Use in Consultation
R. Fernholm 1, K. Pukk Härenstam1
1Karolinska Institutet, Solna, Sweden
Background: One of the biggest patient safety problems in emergency and primary care is the failure to follow up uncertain diagnoses, with the risk of leading to preventable diagnostic harm. A promising approach is to use safety-netting, which has received increased attention in recent years. However, there is still limited knowledge about how to successfully apply safety-netting strategies in practice and few studies have accounted for patient experiences in this area. Objective: To explore clinicians’ and patients’ experiences of diagnostic uncertainty and their ideas/views on how safety-netting can be successfully applied in primary and emergency care settings.
Method: The study was performed in a Swedish setting. An exploratory research design was used, based on six interviews and two focus group discussions, involving a total of nine clinicians working in primary and emergency care, as well as seven patients and one family caregiver with experiences of diagnostic uncertainty. Data were analyzed inductively, using the framework method. The COREQ guidelines for reporting qualitative research were used.
Results: To manage diagnostic uncertainty, clinicians and patients emphasized the need to understand preconditions for the consultation (i.e., the patient’s capacity and their social context; aspects influencing the patient-clinician collaboration; the healthcare context) and gain shared situational awareness regarding the patient’s perspective and experiences, as well as the need for safety-netting. We identified six strategies for successfully applying safety-netting: 1) openness about uncertainties; 2) communicating expected course of events; 3) tailoring information; 4) using multiple modalities; 5) teach-back; 6) facilitate re-consultation.
Conclusions: The understanding of preconditions for the clinical encounter and the establishment of shared situational awareness between the clinician and the patient were identified as vital aspects for the successful selection, tailoring, and application of safety-netting strategies. Implications for practice can be that safety-netting can be systematically built in the consultation technique taking these aspects in consideration.

Physics in Medicine: Pedagogical Reforms Focused on More Effective, Accurate and Expedient Diagnoses
E. Szuszczewicz 1
1George Mason University, Haymarket, VA
Learning modules are under design and development with innovations providing more effective diagnoses, treatments, and cures for everything from cardiovascular and neurological diseases to cancer. The focus is on physics as the foundational science of all life sciences, with the Physics in Medicine (PIM) program designed to educate students of medicine, and the medical and physics teaching and research communities, on the needs-for and applications-of a first-principles cause-effect understanding of life science and medical care processes. The effort is in response to mandates from numerous panels that have raised concerns about the basic science content in medical education and have advocated for reform in curricular and competency requirements. These critical needs are manifested in data pointing to 40,000-80,000 deaths/year resulting from misdiagnoses. Learning modules are concentrated on six major medical themes, with the most fundamental theme considered to be “Neuroscience, Electrodynamics and Cellular Biology - The Mind and the Brain - The Pathways to Cognition, Sensory Perception and Bio-Feedback”. It is considered most fundamental, with electrodynamics at the core of all human functionality. And the theme is being built on learning modules starting with single-cell electrodynamics, working into biological system and subsystem applications. To meet the challenges of educational structures, student workloads, and mandated reforms, PIM has a team of practitioners, academicians and researchers from the medical and physics communities that focuses not only on content but on approach, and on the development of quantitative predictive skills and adaptive thinking capabilities that transcend the current algorithm-based diagnostic protocols of medicine’s evidence-based training. The underlying strategy involves not just an accumulation of facts and the study of the laws of physics, but the development of an inquiring scientific mind and a method of cause-effect inquiry, thinking, and problem solving based on first-principles analysis. In the end, the students will be far better prepared to meet the challenges to their understanding and use of ever-advancing technologies, and the intellectual demands of causal processes and ever-expanding databases dealing with disease onset, progression and controls. Indeed, the onset of all diseases, their progression and their in vivo controls are traceable to the attributes of cell and tissue properties controlled by atomic and molecular physics and an arsenal of electrical, kinetic, thermodynamic, fluidic and gradient-driven forces. Early-stage testing of PIM concepts within pre-medical, grand-rounds, residency, and critical-care venues has reinforced its goals, approach and developing curricular deliverables.
Physics in the Medical School Curriculum: Foundational Science Content to Support Medical Diagnosis
L. LaConte 1, B. Roth2, N. Donaldson3, E. Szuszczewicz4, E. Redish5
1Virginia Tech Carilion School of Medicine, Roanoke, VA
2Oakland University, Rochester, MI
3Rockhurst University, Kansas City, MO
4George Mason University, Haymarket, VA
5University of Maryland, College Park, MD
The pre-clinical medical school years are a final formal educational opportunity to ground a physician’s medical knowledge and diagnostic approach in the scientific principles of physics. Unfortunately, many medical students have a weak grasp of physics; undergraduate coursework has not translated into an intuitive understanding of physics as integrated with other science and medical disciplines. As a result, students may not view physics principles as tools from which an understanding of (patho)physiology can be derived but instead compartmentalize physics concepts as distinct from biological and medical sciences. Efforts in undergraduate physics education (e.g., Living Physics Portal, Physics of Living Systems) are addressing this challenge, but disciplinary change takes time and is best accomplished with interdisciplinary efforts. In medical school, intentional integration of foundational physics principles into pre-clinical teaching will not only strengthen an understanding of physics but also provide future physicians a framework to easily integrate biomedical research findings, make well-founded hypotheses to advance medical knowledge, and most importantly, accurately diagnose their patients. The practical task of integrating physics into pre-clinical medical education requires deep understanding of both relevant physics concepts and medical knowledge to be mastered. The United States Medical Licensing Examination (USMLE) Step 1 exam assesses whether students “understand and can apply important concepts of the sciences basic to the practice of medicine”. The USMLE Step 1 content outline forms the core of most pre-clinical medical education. The sheer volume of Step 1 subject matter often results in students relying on mnemonics rather than deep understanding. Medical educators feel pressure to prepare students for this exam but lack curricular time to reinforce general principles. In short, re-envisioning pre-clinical medical education to emphasize fundamental physics principles must create curricular efficiencies to ensure adoption. Here we will describe our work with the Physics in Medicine (PIM) program to create a unifying framework specific to pre-clinical medical education, with top-level concepts representing foundational, cross-cutting “physics in medicine” (PIM) principles connected to USMLE Step 1 topics. This PIM concept map is the foundation for a PIM toolbox that pre-clinical medical educators can employ in a modular fashion. Introductory content for foundational PIM sessions will provide a basis for later content-specific sessions. The PIM concept map and learning modules will allow medical educators with limited time or physics expertise to sustain a thread of cross-cutting PIM concepts throughout the pre-clinical curriculum.
Prevalence of Diagnostic Errors in Outpatients Consulted by Generalists in a Tertiary Care Setting
Y. Harada 1, S. Katsukura2, T. Shimizu1, Y. Otaka1
1Department of Diagnostic and Generalist Medicine, Dokkyo Medical University, Mibu, Japan
2Dokkyo Medical University, Mibu, Japan
Background: The high prevalence of diagnostic errors has been reported in outpatients of primary care settings, where generalists are usually in charge of care with limited resources for diagnostic investigation. On the other hand, in the tertiary care setting, where generalists also work as diagnostic consultants or gatekeepers with sufficient diagnostic resources, the prevalence of diagnostic errors in outpatients consulted by generalists remains unknown. In addition, there are scarce data regarding whether consultation patterns (appointed visit with referral, urgent visit, and emergency visit) are associated with the risk of diagnostic errors or not. This study was conducted to clarify the prevalence of diagnostic errors in outpatients consulted by generalists in the university hospital setting.
Methods: We reviewed medical records of consecutive outpatients consulted by physicians from the Department of Diagnostic and Generalist Medicine in a university hospital between January 1, 2019, and December 31, 2019. Diagnostic process was assessed by at least two independent reviewers using the Revised Safer Dx Instrument. Diagnostic errors were defined as at least two reviewers scoring five or more, and non-diagnostic errors were defined as at least two reviewers scoring three or less in item 13 in the instrument; otherwise, decisions were made by discussion of the three reviewers. The primary outcome was the prevalence of diagnostic errors, and secondary outcomes were the prevalence of diagnostic errors in the subgroups of consultation patterns (appointed visit with referral, urgent visit, or emergency visit) as well as age and sex. Prevalence of diagnostic errors in the subgroups was compared by using chi-square test. P<0.05 was defined as statistically significant.
Results: A total of 1992 cases were included in the analysis. Diagnostic errors were observed in 28 cases (1.4%; 95%CI, 0.9-2.0%). The prevalence of diagnostic errors was significantly different among consultation patterns: urgent visit, 3/599 (0.5%); emergency visit, 13/859 (1.5%), and appointed visit with referral 12/534 (2.2%) (P=0.04). Besides, a higher prevalence of diagnostic errors was observed in the group aged over 50 (24/1121, 2.1%) compared to that in the group aged 50 or younger (4/871, 0.5%) (P=0.002). In the cases of diagnostic errors, neoplasm was the most common missed category of diagnosis. The most common contributing factor for diagnostic errors was “Problems with data integration and interpretation” (16/28, 57.1%).
Conclusion: The prevalence of diagnostic errors is estimated to be 0.5-2.2% in patients consulted by generalists in the tertiary care setting. The consultation patterns and age can be associated with the risk of diagnostic errors.
Renal Mad-Libs: Clinical Reasoning Seminar for Medical Students with a Focus on Glomerular Disease
D. Kudlowitz 1, A. Mednick1, K. Karpin1, V. Schaye1, P. Taunk1, K. Eaton1, J. Noyes1, K. Crotty1, S., Al Najjar1, N. Sherpa1, M. Robak1
1NYU Grossman School of Medicine, New York, NY
Purpose/Problem: Medical school pre-clinical curriculum can focus on medical knowledge and not the clinical reasoning (CR) process to apply that knowledge to patient care. Additionally, gamification is a teaching strategy that can foster clinical problem-solving skills that is not often utilized. NYU Grossman School of Medicine has successfully integrated CR into most pre-clerkship organ modules, however, our renal module lacked an organized CR educational activity. To remedy this, we created a renal CR seminar using gamification techniques to foster application of this medical knowledge content domain.
Description of Program: The seminar is 2 hours divided into two parts. First year medical students in 3 groups of 4 students spend the first half of the seminar creating an illness script chart of assigned paired diseases—focusing on epidemiology, pathophysiology, clinical presentation, diagnosis, and treatment. Given the importance of comparing and contrasting in the formation of illness scripts, we paired diseases that share key similarities focusing on glomerular diseases. Disease pairs included Post-streptococcal Glomerulonephritis and IgA nephropathy, Granulomatosis with Polyangiitis and anti-GBM disease, and Minimal Change Disease and Class V Lupus nephritis. Then each small group share their charts, focusing on a discussion that compares and contrasts the individual components of the illness scripts. For the second half, students fill out a mad-libs paragraph scenario for each assigned pair of diseases, highlighting key differences. As an example, for IgA nephropathy and Post-streptococcal glomerulonephritis: “A 28-year-old female who works as a(n) (insert type of job) developed (name a color) urine (at the same time as/1 week after contracting) an upper respiratory infection.” Each group of students then presents their completed “mad-libs” to the other small groups who determine which disease is being described.
Outcomes: Thus far we have collected data at the reaction level of the Kirkpatrick model of program evaluation. Seventy-five percent of students (N=6) strongly agreed that the seminar aligned well with the renal module curriculum and that the seminar helped consolidate material. A representative comment: “I loved how this session was […] geared to what we have been learning about, with some interesting clinical pearls and really relevant ways of thinking about these diseases and their differences and similarities.”
Conclusions/Significance: Reviewing glomerular disease through an innovative, gamified, method of comparing and contrasting illness scripts is an engaging method to teach pre-clinical learners CR. Next steps are to gather further data on program evaluation to help inform changes in other organ system modules.
The Pulmonary Embolus that Wasn’t
N. deQuillfeldt 1, A. Baduashvili1
1University of Colorado Anschutz, Denver, CO
Recent literature suggests that CT angiograms (CTPE) may not be as accurate as previously thought, potentially leading to overdiagnosis of PE (1,2). A 53-year-old man with history of depression and amphetamine use disorder presented to the emergency department to obtain a refill of bupropion. Review of systems noted progressive dyspnea on exertion over several months and intermittent swelling of bilateral hands and feet. His Wells Score for PE (3) was 1.5 due to tachycardia to 114. He had no history of malignancy, recent surgery or immobilization. CTPE was obtained with findings suggestive of a solitary subsegmental PE. Due to contrast bolus timing, the vessels were not optimally visualized. Anticoagulation was initiated and he was admitted to the hospital. Upon reevaluation, there was concern that his pre-test probability for PE was lower than initially thought as he was never hypoxic and his tachycardia was likely explained by positive urine drug screen for amphetamines. A study in which expert radiologists with >10 years of experience reviewed 937 CTPEs identified that up to 66.7% of solitary subsegmental PE diagnoses were considered negative on retrospective review (2), calling into question this patient’s imaging findings. Furthermore, according to the American College of Chest Physicians 2012 Guidelines and other data, a negative d-dimer precludes need for further imaging (4-6). EKG/echocardiography subsequently did not find evidence of right heart strain, venous duplex ultrasonography (VDU) of bilateral lower extremities were negative for DVT, and D-dimer was <270 ng/mL. It was thus concluded that the patient did not have a PE and anticoagulation was discontinued. This case highlights the importance of questioning the diagnosis when pre-test probability is very low and the diagnostic test not strongly convincing. This is particularly true when the selected therapy carries significant potential risk for harm, such as lifelong anticoagulation for a presumed unprovoked PE (7).
Transient Ischaemic Attacks: A Noisy World
T. Cassidy 1, L. Chapman1
1St Vincent’s University Hospital, Dublin, Ireland
Background: Studies have demonstrated that a high percentage of referrals to a Transient Ischaemic Attack Clinic are mimics. The diagnosis of a transient ischaemic attack (TIA) depends upon a good clinical history by an expert clinician. The non-specialist will often get the diagnosis wrong either due to bias or noise. Noise is defined as an undesirable variability in judgement. In real world situations, the amount of noise is higher than one would expect. A frequent misconception is that unwanted variability in judgements will cancel each other out. However, in noisy systems they add up and can lead to cumulative problems. St Vincent’s University Hospital (SVUH) admits patients with a TIA from their Emergency Department (ED). In 2021, 252 patients were discharged with the clinical coding of TIA. Their mean age was 72.3 years, and their average length of stay was 3.5 days
Method: We reviewed a random sample of 50 of these discharges. This was a case note audit of their in-patient stay and subsequent out-patient clinic attendance. We looked for whether their final clinic diagnosis was in agreement with their discharge diagnosis. Secondly, whether the patient had been discharged on appropriate secondary prevention treatment as per the guidelines of the Royal College of Physicians London (RCPLondon).
Results: 50 patients (23 males), Mean age 77.8, Median 78 (Range 55 – 94) years were reviewed. In their hospital stay, they were under the care of 18 GIM specialists, but 3 GIM covered 27 patients. Only 23 (46%) patients were referred to stroke out-patients, 7 (14%) to neurology, 8 (16%) to Geriatric Medicine and 11 patients with no follow -up. On discharge, 33 patients had been treated with high dose aspirin (300mg / day) followed by normal maintenance treatment (75mg/day). 5 patients had commenced an oral anticoagulant due to their atrial fibrillation, only 2 patients were treated with dual antiplatelet therapy and 9 patients treated with high dose aspirin followed by clopidogrel therapy as per RCP London guidelines. Of the 39 patients who attended a clinic, only 10 patients were thought to have had a TIA, 3 patients were re-classified as stroke; 4 patients had a Transient Global Amnesia, 3 Migraines, 12 patients had a “Geriatric Medical problem”.
Conclusions: There is considerable noise in the diagnosis and management of a TIA patient presenting to SVUH. This may partly be explained by the large numbers of GIM specialists involved in their care. The use of a clinical algorithms and or a specialist nurse in stroke may decrease the noise and improve care in this cohort of patients.
Wernicke’s Encephalopathy in the Setting of Hyperemesis Gravidarum; A Challenging Diagnosis
T. Herrin 1, E. Perez-Colon1, I. Cha1
1University of South Florida Morsani College of Medicine, Tampa, FL
Learning Objectives: Diagnosing Wernicke’s encephalopathy (WE) in the setting of hyperemesis gravidarum (HG) has proven to be a difficult diagnosis. The learning objectives of this clinical vignette are to highlight a rare yet important risk factor, emphasize sensitive investigations and explore recovery.
Case Information: 30-year-pregnant female at 17 weeks with a medical history significant for HG presented from a community hospital for encephalopathy after being admitted for vomiting and increased fatigue. Upon transfer to our institution, the patient was not oriented to self, place, or date. Her initial labs showed hemoglobin of 7.9, MCV of 90, folate of 4.3, and vitamin B12 of 776. Head imaging was unremarkable. The patient started empirically on high-dose intravenous thiamine and later transitioned to oral thiamine and folic acid. The patient showed clinical improvement. Thiamine level after supplementation was adequate.
Discussion: WE results from thiamine deficiency and is classically described as the triad of ataxia, confusion, and opthamalgias (1), often as a consequence of alcohol abuse. However, approximately half of the patients presented with this triad (3). In this clinical vignette, we would like to underscore three points for appropriate diagnosis and management of WE induced by HG. First, due to the acute onset of thiamine deficiency in HG, malnutrition, and increased metabolic demand, pregnant women with HG are at risk of WE(2). Second, the workup should include timely vitamin levels and an MRI brain scan showing lesions at the periventricular thalamus, although this was shown to be only 46% sensitive (4). Lastly, the importance of treating HG immediately when neurological symptoms appear. Despite appropriate and prompt treatment, approximately only 30% of patients make a full recovery and permanent impairments are common (3). High suspicion for WE in the setting of HG and immediate treatment may improve chances of recovery.
References: 1) PMID: 31171116. 2) PMID: 30889425. 3) PMID: 16551377. 4) PMID: 9763009.
Oral Abstracts 1
Monday, October 17
10:00 AM – 11:30 AM
Contribution of Limited English Proficiency to Diagnostic Errors in Pediatric ED Patients
J. Lowe 1, J. Grubenhoff1, M. Mendenhall1, J. Leonard1, K. Widmer1
1University of Colorado School of Medicine, Aurora, CO
Background: National patient surveys indicate that limited English proficiency (LEP) increases the odds of experiencing diagnostic errors 4-fold compared to those proficient in English (EP). Children in LEP families had twice the odds of an emergency department (ED) or office visit prior to definitive appendicitis diagnosis. However, little other objective data exist assessing risk of diagnostic error (DxE) related to language proficiency in pediatric acute care. We evaluated the association between LEP and DxEs leading to unplanned admission in children evaluated in a large, multi-site pediatric ED & urgent care (UC) system with ∼170,000 annual visits.
Methods: E-trigger followed by manual screening identified children with unplanned admission within 10 days of an index ED/UC encounter from 1/1/2018-2/28/2022. Cases with disparate diagnoses at index encounter and hospital discharge were reviewed using the Revised SaferDx to determine presence of a DxE. Caregiver reported language preference, other demographic and encounter variables were abstracted from the electronic record. Primary outcome was proportion of DxE in LEP and EP groups. Univariate comparisons: chi-square for proportions; Wilcoxon rank sum for continuous variables. Variables from univariate analysis (p<0.2) plus preferred language were entered into multivariable logistic regression and remained (p<0.1) using backward selection to identify independent predictors of DxE.
Results: 3551 patients met e-trigger criteria. 806 (22.7%) screened in for SaferDx review of which 8 were excluded due to reviewer disagreement. 172 (21.3%) experienced DxE. Table shows univariate comparisons (EP vs LEP). Equal proportions of EP and LEP patients experienced a diagnostic error (21.5% vs 21.7%; p=0.97). Triage acuity, consultation, diagnostic test acquisition, and consideration of the correct final diagnosis were similar. In the multivariate analysis, only age and prior admission remained after backward selection, and no difference existed in the odds of DxE for LEP patients (aOR 0.90, 95% CI 0.56-1.47).
Conclusion: In a single large pediatric ED/UC system, LEP was not associated with increased risk of experiencing a DxE resulting in admission. Diagnostic evaluation was similar between groups suggesting that clinicians obtained appropriate historical and exam information to direct data acquisition, likely through use of telephonic/video interpreters.
Table
| English proficient (n=678) |
Limited English Proficient (n=120) |
p-value | |
|---|---|---|---|
| Diagnostic Error by SaferDx, n (%) | 146 (21.5%) | 26 (21.7%) | 0.97 |
| Age, years, median (IQR) | 6.8 (1.9–13.2) | 10.0 (3.3–15.3) | 0.01 |
| Male, n (%) |
351 (51.8%) |
65 (54.2%) |
0.63 |
| Race, n (%) Asian Black White Other |
17 (2.6%) 60 (9.2%) 436 (66.7%) 141 (21.5%) |
8 (6.7%) 10 (8.3%) 47 (39.2%) 55 (45.8%) |
<0.001
|
| Ethnicity, n (%) Latino Not Latino |
199 (30.9%) 445 (69.1%) |
95 (79.8%) 24 (20.2%) |
<0.001
|
| ESI triage acuity, n (%) L1-L2 L3-L5 |
128 (18.9%) 550 (81.1%) |
22 (18.3%) 98 (81.7%) |
0.89 |
| Index visit arrival time 6am – 2pm 2pm – 10pm 10pm – 6am |
242 (35.7%) 322 (47.5%) 114 (16.8%) |
45 (37.5%) 54 (45.0%) 21 (17.5%) |
0.88 |
| Index visit encounter location, n (%) Urgent care center Emergency department |
140 (20.6%) 538 (79.4%) |
9 (7.5%) 111 (92.5%) |
0.001
|
| Financial class Contract Medicaid Other |
346 (51.0%) 300 (44.3%) 32 (4.7%) |
20 (16.7%) 95 (79.2%) 5 (4.2%) |
<0.001
|
| Number of hospitalizations in the prior 6 months, median (IQR) | 0 (0–0) | 0 (0–0) | 0.51 |
| Number of ED visits in the prior 6 months, median (IQR) | 0 (0–1) | 0 (0–1) | 0.60 |
| Index visit involved a handoff between providers, n (%) | 187 (27.6%) | 23 (19.2%) | 0.05 |
| Subspecialist consult obtained during the index visit, n (%) | 156 (26.9%) | 28 (28.0%) | 0.83 |
| Differential diagnosis acted upon through testing/consultation, n (%) | 457 (78.9%) | 84 (84.9%) | 0.43 |
| Correct final diagnosis considered at the index visit, n (%) | 297 (51.3%) | 52 (52.5%) | 0.82 |
| Number of different studies ordered, median (IQR) | 1 (0–2) | 1 (0.5–2) | 0.93 |
Informing Diagnostic Care in LGBTQ+ Communities: A Qualitative Study of Challenges and Solutions
F. Zannath 1, A. Wiegand1, K. McDonald1, T. Sheikh2, V. Dukhanin3
1Johns Hopkins University School of Nursing, Baltimore, MD
2Johns Hopkins University, Baltimore, MD
3Johns Hopkins Bloomberg School of Public Health, Baltimore, MD
Background: Lesbian, gay, bisexual, transgender, queer (LGBTQ+) individuals experience barriers to accessing medical care due to mistrust, discrimination, violence, and socioeconomic disparities. LGBTQ+ individuals may delay seeking or receive poor diagnostic care, leading to diagnostic delays, misdiagnosis, or miscommunication. The reasons and solutions for diagnostic disparities are not well understood. We aim to identify barriers to accurate, timely, and well-communicated diagnosis and solutions to reduce diagnostic error in LGBTQ+ communities.
Methods: Qualitative study with semi-structured interviews. Participants were recruited via convenience and snowball sampling, screened for eligibility: 18 years or older, LGBTQ+, experienced diagnostic error(s), speak English, and consented. Virtual interviews were audio-recorded and transcribed. Three reviewers developed and reached agreement on a codebook, and transcripts were coded to identify major themes.
Results: 20 participants were interviewed. Participants varied in age, sexual orientation, gender, race, ethnicity, and location. Major themes were grouped as: 1) barriers and 2) facilitators to accurate, timely, and well-communicated diagnosis, 3) impacts of and 4) solutions to diagnostic error. Participants reported LGBTQ+-specific barriers including provider bias; fear of being outed or misgendered; fear of low-quality care due to homo- or transphobia; not being taken seriously due to gender identity; avoiding testing due to discomfort around gender; care refusal; providers falsely attributing symptoms to STIs, HIV, or gender-affirming hormones; asking inappropriate questions related to gender or sexuality; and failing to collect relevant information. Intersectional barriers included age, sexual violence, race, cultural, religious, and weight stigma; non-supportive institutional policies; lack of insurance; transportation or income; inadequate testing or follow-up; and long wait times. Participants identified facilitators including self-advocacy; affirming partners, parents, or providers; health literacy; insurance; social media venues; and resources. Outcomes included worsened mental and physical health, disengaging from healthcare, mistrust, but also increased self-advocacy and community activism. Participants suggested solutions including diagnosis co-production and shared decision-making; inclusive language, signs, and intake forms; provider training and medical education on LGBTQ+ topics; trauma-informed care; quality measures on LGBTQ+ health, changes to insurance and provider incentives; and hiring of LGBTQ+ providers.
Conclusion: LGBTQ+ individuals reported experiencing specific and intersectional challenges and suggested solutions that can be implemented as social or structural change.
Patient and Care Partner’s Perceptions of Diagnostic Accuracy and Excellence from a National Sample
V. Dukhanin 1, K. Gleason2, K. McDonald2, N. Gonzalez3
1Johns Hopkins Bloomberg School of Public Health, Baltimore, MD
2Johns Hopkins University School of Nursing, Baltimore, MD
3Johns Hopkins University, Baltimore, MD
Background: Diagnostic excellence from the patient perspective is relatively understudied, yet critical for improvement efforts. We aimed to analyze qualitatively patient and care partners’ perceptions of diagnostic experience in relation to their acceptance (or not) of the diagnostic explanation as true.
Methods: As a part of developing a patient-reported measure of diagnostic excellence, in February 2022 we surveyed a nationally representative panel of adults who had an emergency department or urgent care visit in the past month. We asked for free-text responses (English or Spanish) about why they indicated (dis)agreement with two survey statements: explanation of the patient’s health received during the visit was true; explanation described what to expect of the health problem. Those paired responses were qualitatively analyzed by two independent reviewers according to themes created inductively.
Results: 1,116 patients (59%) and care partners (41%) participated in the survey, and 987 provided pertinent free-text responses. With the average of 1.6 themes per paired response, this resulted in 1,560 instances under 10 main themes. Almost half of respondents (Table) relied on their perception of overall diagnostic process - several components of the process were listed as contributing or missing vs. their expectations. Around 20% relied on the (mis)alignment of the test results, their medical knowledge, or their post-visit health trajectory with the diagnosis. Around 10% relied on their perception of team attitudes, lack of explanation or uncertainty around the diagnosis, general logic, or (mis)match of their symptoms with the diagnosis. Around 5% relied on general beliefs or another doctor’s opinion. Those who strongly disagreed or disagreed that their diagnosis was true (7% of respondents) did not rely on general beliefs or general logic, relied more on their perception of the process, attitudes, uncertainty around the explanation, or on another doctor’s opinion. They also relied less on test results or on their medical knowledge. Those who neither agreed nor disagreed that their diagnosis was true relied more on their perception of uncertainty around the explanation.
Conclusion: Patients and their care partners provided sound reasoning for their perception of diagnostic accuracy. Free-text data collection offers valuable information for diagnostic excellence.
| Theme | Overall respondents mentioned | Select illustrative quote |
|---|---|---|
| Perception of diagnostic process | 48% | They listened and addressed my problem. They asked questions to make sure that everything was addressed. |
| (Mis)alignment with test results | 21% | They provided me with all the tests and screenings they did. |
| (Mis)alignment with health trajectory | 20% | After visit the condition went away. My wife felt better and was able to sleep every night since then. |
| (Mis)alignment with medical knowledge | 20% | I basically knew it was food poisoning. The doctor just confirmed what I looked up. |
| Uncertainty around the explanation | 11% | They couldn’t explain why the vein bled nor if it would start bleeding again. |
| (Mis)match of symptoms with the explanation | 11% | Diagnosis made sense considering the symptoms. |
| General logic | 10% | It made sense to me. It was a simple ear thing. |
| Perception of team’s attitudes | 9% | I was accused to being a drug and alcohol addict because of how I came in that evening I guess. |
| General beliefs | 6% | Because the doctor told me, and I trust them. |
| (Mis)alignment with another doctor | 5% | My doctor confirmed the diagnosis later. |
Prevalence and Causes of Diagnostic Errors in Patients Who Died or Were Transferred to an ICU
A. Auerbach 1, J. Schnipper2, T. Lee1, G. Valdes1, E. Flynn3, A. Dalal2, J. Boscardin1, S. Ranji4, A. Harris3, K. Raffel5*, C. Hubbard1
(*Presenting Author)
1UCSF, San Francisco, CA
2Brigham and Women’s Hospital, Boston, MA
3Vizient, Inc., Irving, TX
4San Francisco General Hospital, San Francisco, CA
5Denver Health, Denver, CO
Background: Diagnostic errors (DEs), defined as missed opportunities to make a correct or timely diagnosis based on the available evidence, are a critical but understudied cause of patient harm. While previous efforts have focused on examining the incidence and factors contributing to DEs in ambulatory and emergency room settings, fewer studies have examined incidence of DEs in hospitals.
Methods: We carried out a retrospective study of patients admitted to 1 of 31 medical centers affiliated with the Hospital Medicine Reengineering Network between January 1, 2018, and December 31, 2019. We used Vizient administrative data to identify adults meeting CMS definition of an admission for a medical diagnosis, within which we identified patients who died in hospital or who were transferred to an ICU more than 48 hours after admission. Reviewers screened randomly selected cases in order until 100 per site were identified. We excluded patients admitted for a specialty diagnosis, never cared for by an internal medicine physician, or admitted primarily for comfort care or after out-of-hospital resuscitation. Included cases underwent structured 2-physician adjudications following rigorous training to maximize reliability. Adjudications determined whether a DE took place during the hospitalization, the most important diagnostic process faults associated with DEs, and harms associated with those DEs. We used bivariable statistics to compare patients with and without DE, and multivariable models to determine which process faults or patient factors were most associated with DE.
Results: More than a half-million patients were admitted with medical diagnoses (N=525,793) during the study period, of which 26,915 were transferred to the ICU or died after admission. Of these, 4931 were randomly selected and screened, 3035 total charts identified as eligible, and 2493 adjudicated. Five hundred and sixty-three (22.5%) of adjudicated cases had a DE; patients with and without DEs were similar in terms of age, gender, ethnicity, dependencies in activities of daily living, and prevalence of substance use or tobacco use disorders. In multivariable models, factors most strongly associated with DEs were problems with assessment (adjusted odds 13.9, 95% CI 10.6-18.2), errors in test selection or interpretation (adjusted odds 12.0, 95% I 8.8, 16.5), and physical exam errors (adjusted odds 9.6, 95% CI 5.6, 16.4). DEs were harmful; 246 (43.7%) resulted in temporary harm and 230 (40.8%) resulted in permanent harm or death. Among patients who died, a DE was a contributor in 30%.
Conclusion: In this large multicenter study of patients who died in hospital or were unexpectedly transferred to an ICU after admission, DEs were common and harmful.
| DEER Diagnostic Process faults | Patients with diagnostic error (n=563) | Patients without diagnostic error (n=1930) | Unadjusted odds for diagnostic error | (95% CI) | Adjusted odds for diagnostic error | (95% CI) |
|---|---|---|---|---|---|---|
| Access/presentation faults | 34 (6.0%) | 231 (12.0%) | 0.5 | (0.3, 0.7) | 0.8 | (0.5, 1.3) |
| Errors in history taking | 56 (9.9%) | 79 (4.1%) | 2.6 | (1.8, 3.7) | 2.8 | (1.8, 4.4) |
| Errors in physical exam | 49 (8.7%) | 19 (1.0%) | 9.6 | (5.6, 16.4) | 6.9 | (3.6, 13.2) |
| Errors in testing | 159 (28.2%) | 61 (3.2%) | 12.0 | (8.8, 16.5) | 13.7 | (9.5, 19.5) |
| Errors in patient follow-up and monitoring | 80 (14.2%) | 48 (2.5%) | 6.5 | (4.5, 9.4) | 7.2 | (4.6, 11.2) |
| Errors in obtaining referrals | 58 (10.3%) | 42 (2.2%) | 5.2 | (3.4, 7.8) | 6.0 | (3.6, 9.9) |
| Errors in teamwork | 11 (2.0%) | 4 (0.2%) | 9.6 | (3.0, 30.2) | 10.1 | (2.6, 39.8) |
| Errors in communication | 2 (0.4%) | 5 (0.3%) | 1.4 | (0.3, 7.1) | 0.8 | (0.1, 6.2) |
| Errors in assessment | 223 (39.6%) | 87 (4.5%) | 13.9 | (10.6, 18.2) | 13.5 | (9.9, 18.4) |
The Association of Race and Ethnicity with Negative Descriptors in Clinical Texts
A. Zimolzak 1, T. Scott1, T. Giardina2, D. Choi1, D. Dawson1, T. Fletcher1
1Baylor College of Medicine, Houston, TX
2Baylor College of Medicine and Houston VA, Houston, TX
Background: Racial and ethnic inequities in healthcare remain a significant public health problem in the United States. Women, Black patients, patients with mental health diagnoses, and patients from marginalized populations are at higher risk for diagnostic error, partly due to bias/stigma in the healthcare system. Physicians may contribute to disparities via biases in decision-making (e.g., racial/ethnic disparities have been found in cardiac tests, ER diagnostic imaging, and procedures, which may contribute to worse health outcomes in minority groups). We sought to study this bias by measuring the association of demographics with negative descriptor words in clinical texts.
Methods: We adapted a validated list of negative descriptors to local data. We used natural language processing, calculating term frequencies in clinical notes for negative descriptors [(non-)adherent, aggressive, agitated, angry, challenging, combative, (non-)compliant, confront, (non-)cooperative, defensive, exaggerate, hysterical, (un-)pleasant, refuse, resist]. We used stemming to include word variants (e.g., refuses, refusing). The unit of analysis was the clinical note. We analyzed 13,506 notes, from 100 patients with an ER visit and admission. Distributions of demographics (race, ethnicity, sex) were compared using a 2-sided Fisher’s exact test, with p<0.05 considered significant.
Results: Hispanic or Latino patients are overrepresented among notes containing any negative descriptor, compared to notes without descriptors (28 vs. 23 percent, p=0.008). Black patients are also overrepresented among notes with negative descriptors, compared to notes without (49 vs. 48 percent, p=0.003). Women were not significantly over- or underrepresented in the two groups of notes (62 vs. 65 percent, p=0.125). Considering the combination of race and ethnicity fields, (major groups being Black, Hispanic, and Non-Hispanic White) there is a significant difference in race/ethnicity distribution, between notes with vs. without a negative descriptor (p<0.001, with Non-Hispanic White patients less common among negative descriptor notes, and Black or Hispanic patients more common).
Conclusions: We show a positive association of race/ethnicity with negative descriptors in clinical text, validating prior work indicating racial/ethnic bias in health workers’ documentation. Most prominently, more Hispanic/Latino patients were represented among notes with negative descriptors than notes without. Limitations include the lack of definitive word categorization as a negative descriptor and the lack of adjustment for other factors. Identifying and eliminating bias (e.g., racism and discrimination) for patients of color is essential for developing reliable and equitable diagnostic safety.
The Influence of Socioeconomic Disparities on the Cancer Diagnostic Pathway and Health Care Outcomes
T. Ward 1, W. Hamilton1, R. Mujica-Mota1, A. Spencer1, A. Medina-Lara1
1University of Exeter, Exeter, England
Introduction: Published evidence has highlighted disparities in cancer survival outcomes by socioeconomic status (SES) and geographical location in England, however, there remains a paucity of knowledge with respect to how socioeconomic disparities and geographic inequalities contribute to misdiagnosis, time to diagnosis and differences in health care resource use in England. The aim of this analysis is to explore and quantify the impact of socioeconomic and geographic heterogeneity on the diagnostic route, time to diagnosis and the clinical care pathway of colorectal, lung and ovarian cancer patients, and their subsequent survival and resource use outcomes.
Methods: Adult patients with a diagnosis of colorectal, lung or ovarian cancer on or after the 1st of January 2013 were identified from the Clinical Practice Research Datalink dataset. Data was linked to National Health Service Hospital Episode Statistics data, National Cancer Registration and Analysis Service data and Office for National Statistics mortality data. Survival analysis was undertaken and assessed from the time of cancer diagnosis, focusing on patient groups stratified by SES and geographical region. Univariable and multivariable analyses were undertaken, evaluating the impact of common influential factors on survival, with route to diagnosis and time to diagnosis evaluated as mediating variables. Resource use was quantified in terms of health care visits, health care specialist time, testing procedures, prescriptions, and treatments. A ‘non-cancer’ control group, matched to cancer cases on age, gender, ethnicity, SES and geographical region, was used to assess relative differences in both survival and resource use.
Results: Survival outcomes were notably correlated with SES, geographical location, and several other patient attributes. Furthermore, there is evidence to suggest that patients in different socioeconomic groups and geographical regions observe subtly different clinical care pathways and are made up of patients with different clinical characteristics, compounding differences in outcomes. Health care resource use significantly increased after cancer diagnosis, and was similarly associated with SES and geographical location, although such associations were reduced when adjusting for mediating factors, such as diagnosis route and time to diagnosis, and other relevant factors.
Conclusion: Patient clinical and demographic heterogeneity impact on the clinical care pathway and the survival and resource use outcomes of cancer patients, with diagnostic patterns notably impacting outcomes. In the discussion we explore the implications of findings for improving future cancer diagnostic practices and health care resource allocation in England.
Oral Abstracts 2
Monday, October 17
12:45 PM – 2:15 PM
A Digital Clinical Reasoning Test: What Does it Add?
L. Ruczynski 1, B. Schouwenberg2, M. van de Pol3, E. Custers4, L. Fluit1
1Radboud University Medical Center, Radboud umc Health Academy, Nijmegen, Netherlands
2Radboud University Medical Center, Department of Internal Medicine/Pharmacology & Toxicology, Nijmegen, Netherlands
3Radboud University Medical Center, Department of Primary and Community Care, Nijmegen, Netherlands
4University Medical Center Utrecht, Center for Research and Development of Education, Utrecht, Netherlands
Purpose: A digital clinical reasoning test (DCRT) was introduced in the medical Master’s curriculum at Radboud University Medical Center Nijmegen (Netherlands) in January 2019 to evaluate student’s clinical reasoning skills. Research was conducted to map the added value.
Description of Assessment: Using scientific literature, the DCRT has been developed wherein a combination of question types are used: script concordance test questions, comprehensive integrated puzzles, extended matching questions, multiple choice questions and short- and long-answer questions. The test is administered shortly after the clerkship with a total number of six DCRTs throughout the Master’s curriculum.
Outcomes: A mixed method research was conducted with Kane’s validity perspective as a framework. Cross-sectional comparison was done between students’ results on the Dutch Progress Test (DPT; a comprehensive test that also tests clinical reasoning) versus the DCRT to determine if the DCRT met the intended assessment frame. Results showed that they have an average correlation of 0.523. Insufficient scoring students did significantly so on both tests (p<0.001). An interview study is currently conducted to provide insight into the influence the DCRT has on the learning behaviour of students in practice. First results show that students mostly use the DCRT for assessment of learning despite institutional efforts to broaden their view. Nevertheless, it does help them to fine-tune their learning strategies. Another preliminary result is that students find certain challenges in connecting clinical (learning) practice with the DCRT and vice versa. Finally, residents of two clinical departments (internal medicine and surgery) will complete the DCRT medio 2022 to understand what skill level was tested with the DCRT.
Discussion: Looking at the first results, the DCRT has added value to an assessment program. The correlation with the DPT indicates that both tests assess clinical-reasoning skills but not in a way that one of both would make the other superfluous. They complement each other because insufficient scoring students do so on both tests. Although students use this test mostly for assessment of learning, it does not rule out a component of assessment as – or for – learning. The results of the ongoing data gathering will be added to (dis)prove our results.
Significance of Findings: This DCRT and this research will provide useful information for others to implement such a test in other contexts. Secondly, there is no scientific literature yet on DCRTs where this combination of question types is used.
Development of a National Public Repository for Diagnostic Feedback Resources
B. Rosner 1
1University of California San Francisco, San Francisco, CA
Problem Statement: Feedback about diagnostic performance is key to calibration, the process by which a clinician’s diagnostic confidence aligns with actual diagnostic accuracy. However, diagnostic performance feedback in healthcare, compared to performance feedback in other industries, remains low, in part due to operational, cultural, contextual, fiscal, and technical barriers. However, for organizations dedicated to improving diagnostic calibration, there remains no centralized source of information detailing the various resources that exist and that could be operationalized. Overcoming a purely informational barrier such as this, could help drive more widespread adoption of diagnostic feedback.
Description of the Program: Our goal was to develop a national, publicly available, searchable online toolkit of scalable resources capable of providing or augmenting diagnostic performance feedback. Our activities were twofold: identify resources, through extensive literature and landscape analyses, with which to populate the toolkit; and design, build, and disseminate the toolkit in a way resonating with target users. To identify resources, we conducted extensive structured reviews of the internet and of the peer-reviewed and gray literature. We also reached out to healthcare systems and national organizations to discover internal resources not publicly visible. Concurrently, we convened two 8-member groups of national stakeholders: one consisting of subject matter experts to help identify and adjudicate resources, and the other consisting of executive leaders at major healthcare organizations to design and promote the toolkit’s dissemination, awareness, and adoption.
Findings to Date: To date, we have identified over 40 unique resources, and have characterized them along two axes: the stages in the diagnostic arc they serve, and the type of user or technology they involve. (Figure 1) We will present to SIDM attendees an advance glimpse of the toolkit that will go live on April 1, 2023.
Lessons Learned: The number of resources implementable in an automated or semi-automated manner to support diagnostic performance feedback may be greater than broadly recognized. While few resources provide “end-to-end” solutions beginning with identifying the diagnostic encounter, and ending with feedback to the clinician, we find that there are powerful opportunities to create custom suites of these resources that span the diagnostic arc.

Diagnosing the Curriculum: Leveraging Student Leadership to Grow Clinical Reasoning Education
T. Wijesekera 1, J. Tang1, I. Freedman1, M. Gazzola1, M. Zheng1, A. Trant1
1Yale School of Medicine, New Haven, CT
Background: While incorporation of student feedback into course development is common in undergraduate medical education, the literature is limited in student leadership of didactic courses, particularly in clinical reasoning. We developed a novel strategy to increase clinical reasoning curricular content and student engagement at our institution’s medical school clinical reasoning course by recruiting senior students as associate course directors (ACDs).
Description: From June 2020 to March 2022, we recruited three clinical reasoning ACDs per year (9 total) at a single medical school in the Northeast United States. The ACDs were senior students in their third or fourth years who were selected for a mutually renewable one-year term by the faculty course director (T.P.W) based on their interest in clinical reasoning and their background in education. The faculty course director and ACDs met weekly to biweekly to develop curricular activities for students (pre-clinical, clinical) and faculty audiences. Students were empowered to provide in-the-moment feedback during curricular development, lead creation of course activities, and facilitate didactic sessions for peers and faculty.
Outcomes: By the end of the 2021–2022 academic year, student course directors helped design, develop, and facilitate over 75 hours of new clinical reasoning education reaching over 450 medical students and 200 faculty. Medical student activities included creation of a virtual concept-mapping tool, five additional didactics, and 18 additional workshops (i.e., different types of clinical problem-solving exercises). Faculty development sessions included 13 highly-rated workshops on teaching clinical reasoning, where student participation was rated a valuable feature. Satisfaction was high among ACDs – non-graduating ACDs chose to stay in the role for the subsequent year.
Discussion: To our knowledge, this is the first example of student leadership in an undergraduate medical school clinical reasoning course. Prior models of student leadership in preclinical courses have been successful and enhanced participants’ leadership skills. Limitations include a small sample size at a single institution. Future directions include, among, other curricular endeavors, creating a clinical reasoning consultation program for students and growing durable educational materials (e.g., training videos) for faculty development.
Conclusions/Significance: It is feasible to recruit senior students into active leadership roles for clinical reasoning education, in which they offer unique expertise and perspectives. Given the potential to significantly expand education on this valuable clinical skill, this model can and should be adopted into other courses and institutions.
e-Biopsy: Addressing Missed Diagnoses of Ectopic Pregnancies Through Decision Support Enhancements
M. Au 1, K. Litman2, M. Kanter2, L. Saporito2, S. Liang2, L. Lurvey1, A. Ghobadi2
1Southern California Permanente Medical Group, Pasadena, CA
2Kaiser Permanente Bernard J. Tyson School of Medicine, Pasadena, CA
Background: In 2010, Kaiser Permanente Southern California developed a novel methodology called ‘e-Biopsy’, to study cases with diagnostic and quality errors and suggest system improvements. Here we use ‘e-Biopsy’ to help diagnose ectopic pregnancy (EP), a pregnancy outside the uterus, a life-threatening condition, and suggest system improvements.
Methods: We identified 3,264 patients in our Electronic Health Record (EHR) with EP between January 2016 and December 2018. 42 patients of these were randomly selected and charts reviewed by 4 Ob/Gyn and 2 non-OB physicians using a specially designed review tool based on a widely accepted algorithm. 16 of the 42 patients were identified as having a Pregnancy of Unknown Location (PUL) and serum hCG above the discriminatory zone (3,500 mIU/mL), which the algorithm considers as potential cases of EP. Only 9 of those 16 patients (56%) were offered diagnostic follow up and treatment recommended by the algorithm. Non-obstetricians (emergentologists/urgent care/primary care clinicians) had delays in ordering recommended ultrasounds in 3/42 (7%) cases; consideration of EP as a diagnosis during the initial visit in 8/42 (19%); and consulting the OB/Gyn specialist in 6/42 (14%) of cases. Several system interventions were developed to improve the diagnosis/management of patients with EP including: 1) All early pregnancy ultrasounds without documented intrauterine pregnancy now have standardized recommendations in the report including reminding clinicians to consider referral to ob/gyn. 2) All lab hCG results now include recommendations for serial testing and consideration of ob/gyn consultation if <36% rise in values is seen in 48 hours. Repeat hCG values show the percent rise to assist in this determination. 3) A new EHR “Orderset” (orders in a checklist format) makes it easier for clinicians to order appropriate studies. 4) A “SureNet” system was created to catch any patients with abnormal increase in sequential hCG results and no follow up visit scheduled. The SureNet leads to urgent messaging of the ordering clinician.
Results: In its first 4 months, the SureNet system alone identified 45 patients with potential EP based on abnormal rise of hCG, which led to immediate notification of their clinicians. Two of these patients ultimately were diagnosed with EP, a diagnosis expedited by this program. Several cases were also identified by the Sure Net of spontaneous abortion, which led to earlier care of these patients as well.
Conclusions: EP is life-threatening but diagnostic errors remain common and guidelines are often not followed. System changes can help reduce these errors.
fMRI Reveals a High-Risk Neurocognitive State Associated with Radiologists’ Perceptual Errors
M. Bruno 1, T. Mosher1, K. Sathian1, S. Bunce1, P. Karunanayaka1, E. Krupinski2
1Penn State University, State College, PA
2Emory University, Atlanta, GA
Background: The most common type of error made by radiologists are perceptually based, wherein abnormalities later determined to be present on medical images are not identified prospectively. This sometimes includes the failure to perceive findings which appear highly conspicuous in retrospect and may account for as many as 70-80% of radiologists’ errors in practice. It is a tempting hypothesis that such errors may be due to momentary lapses in attention, sometimes referred to as “mind-wandering,” (MW) which is known to occur involuntarily and without the individual’s knowledge or awareness. An emerging literature has suggested a correlate to MW: spontaneous, episodic co-activation of two brain networks that normally function in opposition, the default mode network (DMN) and the fronto-parietal executive network (FPN). Our study was designed to evaluate this phenomenon in practicing radiologists performing a visual continuous-attention task, to determine the relationship between errors and the MW state.
Methods: A pilot study was performed involving 10 practicing radiologists (8 men, 2 women, ages 37–65), who were studied with fMRI as they performed a 15-minute continuous attention visual task. While not difficult, the task is designed to identify even brief/momentary lapses in a participants’ attention. The cortical regions known to subtend the DMN and FPN networks were identified and group-level network dynamic analysis was performed.
Results: As shown in the figure, DMN and FPN network activity was mostly in opposition, which is the expected network behavior, however, all of our participants demonstrated several brief episodes (average of 8/session) of spontaneous dual-network co-activation. These MW episodes were usually several seconds in duration. Perceptual errors were highly correlated with these MW states (74.4% of errors, p<0.01), suggesting that they corresponded to attentional lapses.
Conclusion: We have identified a neurocognitive state (MW) that is highly correlated with perceptual errors in practicing radiologists. These errors appear to be due to attentional lapses, which may be very brief and of which the participant is not aware. In ongoing work, we are seeking ways to better detect this high-risk neurocognitive state unobtrusively and to develop effective intervention strategies in order to reduce this entire class of errors in practice.

Validity and Reliability of Brier Scoring for Assessment of Probabilistic Diagnostic Reasoning
N. Stehouwer 1, K. Qua1, A. Rowland-Seymour1, L. Gruppen2
1Case Western Reserve University School of Medicine, Cleveland, OH
2University of Michigan Medical School, Ann Arbor, MI
Purpose: Diagnostic excellence requires the ability to reliably recognize uncertainty. However, few tools exist to directly assess health professions trainees’ diagnostic predictions in probabilistic terms. The Brier score compares forecasts with actual outcomes and rewards accurate appraisal of uncertainty. We performed a pilot reliability and validity study on an assessment tool utilizing Brier scoring to evaluate students’ probabilistic diagnostic assessments.
Description of Assessment: Senior medical students were assigned 13 clinical cases. For each case, students were given a short vignette, made probabilistic diagnostic assessments, ordered diagnostic tests and received results in series, then chose a final diagnosis. 17 students were included in analysis. We calculated student Brier score and its component parts, resolution and calibration, to measure probabilistic diagnostic skill. Brier scores were calculated as the average of the squared different between student forecasts and correct outcomes. Calibration and resolution were calculated by grouping each students’ forecasts into quintiles. Calibration was calculated by squaring the difference between observed and predicted outcomes for each quintile. Resolution, the ability to differentiate high and low probability events, was calculated by squaring the difference between observed frequency and the overall average frequency. Outcome measures included quantity of tests ordered, final diagnostic accuracy, United States Medical Licensing Exam (USMLE) scores, National Board of Medical Examiners (NBME) scores, clerkship grades, and Clinical Skills Exam (CSE) scores. This study was approved by the Case Western Reserve University School of Medicine Institutional Review Board. Outcomes. Brier scores had good reliability in this sample (Cronbach alpha = 0.73.) Brier scores were not significantly associated with test ordering or final diagnostic accuracy. Brier score overall was not correlated significantly with USMLE, NBME, CSE scores or number of clerkship honors, but Resolution was positively correlated with average NBME results (R2=0.32, p<0.05).
Discussion: An objective assessment tool for probabilistic diagnostic reasoning would be valuable for medical educators. In this pilot study, Brier scoring had good reliability but did not strongly correlate with external validity metrics. This may be due to the fact that Brier scoring assesses skills such as metacognition, calibration, and numerical fluency which are not well assessed by current standard metrics. Resolution was strongly correlated with traditional knowledge-based assessments.
Significance of Findings: This pilot study shows the feasibility and reliability of Brier scoring for Health Professions Trainees. Further studies are needed.
Poster Session 2
Monday, October 17
3:45 PM – 4:45 PM
Assessment of Novel Clinical Reasoning Workshop for First-year Medical Students on Diagnostic Reason
N. Latifi 1, A. Pahwa1, E. Murphy1, T. Kumra1
1Johns Hopkins School of Medicine, Baltimore, MD
Purpose: Teaching clinical reasoning (CR) in pre-clinical years is valuable, but it is unclear how education may impact diagnostic accuracy. We developed a workshop to introduce first-year medical students to CR, including fast- and slow-thinking, through a standardized patient (SP) case, and performed an analysis of differential diagnoses (DDx) generated.
Description of the Program: During the longitudinal ambulatory clerkship, 121 students participate in a 3-hour workshop scheduled after the completion of the infectious disease (ID) pathophysiology course. As prework, students reviewed videos that provided a framework for CR, including generating a DDx from a problem representation. During the workshop, the faculty reviewed that same framework and applied it to a chest pain case. The students divided into small groups for the SP, a patient with flu-like symptoms and social risk factors for HIV acquisition. Students built a history, and SPs complete a checklist on the history obtained. Students created a “fast-thinking” DDx during the 5 minutes following the case. Students then applied the CR framework to the SP case with their facilitator and original larger groups to create a second “slow-thinking” DDx.
Outcomes: Although there was no significant difference in likelihood of HIV diagnosis between fast- and slow-thinking (90.9% vs. 100% with HIV in DDx, p= 0.25 and 68.2% vs. 78.6% with HIV as top diagnosis, p=0.50), HIV made up more of the total diagnoses during slow-thinking (27.4% vs. 52.3%, p=0.007). In two-tailed T-test analysis, students listed more ID diagnoses during fast-thinking (2.88 diagnoses vs. 2.50, p=0.043). In univariate analysis of the obtained social history and HIV diagnosis, during fast-thinking, students were more likely to include HIV in the DDx if they asked about condom use (p=0.025) and as their top diagnosis if they asked about sexual practices (p=0.034). During slow thinking, obtaining specific social history components did not predict HIV diagnosis.
Discussion: Most first year students correctly diagnosed an SP with HIV, and all groups made the correct diagnosis after applying the CR framework. Although the students recently completed their ID course, HIV was diagnosed more frequently during slow thinking with a broader DDx. Incomplete histories predicted less accurate DDx during fast-thinking, but this effect was not seen during slow-thinking.
Significance of Findings: Our workshop shows effectiveness of early introduction to CR framework with improved diagnostic reasoning in first-year medical student. Our findings also underscore the importance of a thorough history in CR, and the role of applying a CR framework to reduce diagnostic error when the history is limited.
Ataxia is More Sensitive for Stroke than ABCD2 Vascular Risk or NIH Stroke Scale in Acute Vertigo
D. Newman-Toker 1, W. Meurer2, T. Economas1, A. Batazzi1, A. Saber Tehrani1, J. Carey1, A. Kheradmand1, V. Eslami1, N. Ostapkovich1, Y. Zhu3, A. Blitz4, M. Iacobelli1, K. Lane1, J. Kattah5, J. Goldstein6, D. Hanley1, M. Hildreth1, D. Gold1, R. Omron1, Z. Wang3, D. Lin1, N. Tevzadze1, Y. Wang1, K. Kerber2, S. Badihian1, N. McBee1, D. Zee1, J. Edlow7, S. Peterson1, T. Chang1, R. Rothman1, J. Jen8, J. Gruber1
1Johns Hopkins University School of Medicine, Baltimore, MD
2University of Michigan Medical School, Ann Arbor, MI
3Johns Hopkins Bloomberg School of Public Health, Baltimore, MD
4Case Western Reserve University School of Medicine, Cleveland, OH
5University of Illinois College of Medicine at Peoria, Illinois Neurological Institute, Peoria, IL
6Massachusetts General Hospital, Boston, MA
7Beth Israel Deaconess Medical Center, Harvard Medical School
8Icahn School of Medicine at Mount Sinai
Background: Acute dizziness/vertigo is a common symptom often misdiagnosed in the emergency department (ED). A misdiagnosis could be life-threatening when the underlying etiology is cerebrovascular disease (CVD). Various standardized scores have been suggested to help diagnose CVD in acute dizziness, but comparisons are lacking.
Methods: AVERT was a phase II randomized diagnostic strategy trial (NCT02483429) conducted at six tertiary-care EDs (2/6/2018-3/9/2020). Trained research coordinators enrolled ED patients with acute dizziness/vertigo, captured a structured history, recorded a battery of eye movement examinations using video-oculography, and assessed standardized neurologic rating scales. Scales included the ABCD2 vascular risk score, National Institute of Health Stroke Scale (NIHSS), and Scale for Assessment and Rating of Ataxia (SARA). Randomized patients underwent detailed one-week follow-up including MRI and in-person assessment by an oto-neurologist plus one-month phone/record follow-up. A 5-member multi-disciplinary expert panel reviewed all findings and adjudicated the best explanatory diagnosis. For this analysis, we measured diagnostic sensitivity/specificity of ABCD2 (range 0–7), NIHSS (range 0-42), and SARA (range 0-40) scores with respect to patients with CVD. We plotted receiver operating characteristic (ROC) curves for each scale.
Results: We randomized 130 patients—14 had CVD (9 ischemic strokes, 4 transient ischemic attacks, 1 hemorrhage). Median (range, interquartile range) scores in CVD cases were ABCD2 2.5 (0–6, 1-3.25), NIHSS 0.5 (0-5, 0-1.25), and SARA 6.5 (0-17, 3.38-11). Median (range, interquartile range) scores in non-CVD cases were ABCD2 1 (0-6, 1-3), NIHSS 0 (0-4, 0-1), and SARA 3 (0-26, 1-7.375). SARA had greater diagnostic power for resolving CVD from non-CVD cases. The area under the ROC curve (compared with a null hypothesis of area not greater than 0.5) for SARA (0.680, p=0.028) was slightly greater than for ABCD2 (0.628, p=0.118) and NIHSS (0.623, p=0.135), neither of which was statistically greater than the null (Figure). SARA permitted more sensitive CVD detection below cutoff scores (sensitivity/specificity) as follows: 1.5 (100%/26%), 2.75 (93%/42%), and 3.25 (79%/55%).
Conclusion: Ataxia appears to be a more potent clinical differentiator of CVD from non-CVD in acute dizziness/vertigo than vascular risk factors or stroke-focused neurologic exam, but none were accurate enough to serve alone as clinical decision rules.

Figure: Receiver Operating Characteristics curves of ABCD2, NIHSS, and SARA scores for diagnosing cerebrovascular diseases
Behcet’s as a Cause of Status Epilepticus - A Rare Case Report
R. Deshpande 1, N. V. D. Kagita1, N. S. Patel1, A. S. Shaik1, R. Thirumaran1
1Mercy Fitzgerald Hospital, Newtown, PA
Learning Objective: Diagnosis and management of patients presenting with atypical symptoms in Behcet’s disease.
Case: A 22-year-old male with a past medical history of Behcet’s disease (diagnosed at the age of 6) complicated by cerebral venous sinus thrombosis (treated with warfarin), and pseudotumor cerebri presented with status epilepticus. His home medications included adalimumab, azathioprine, colchicine, 5-aminosalicylic acid and baclofen. Initial vitals and labs were normal. CT brain was negative for hemorrhage. MRI brain showed abnormal hyperintense lesions in the basal ganglia and temporal lobe. He was treated with intravenous levetiracetam, methylprednisolone, which were subsequently changed to oral levetiracetam, and prednisone. Patient did not have any further seizures and was discharged home on long term steroid therapy.
Discussion: Behcet’s disease is a multisystem vasculitis. It is rare in the United States and has a prevalence of 5.2–6.6 per 100000 population with 10–20% (0.52–1.32 per 100000 population) presenting with CNS involvement and is common in males as compared to females. The exact cause of Behcet’s disease is unknown, but few may have genetic predisposition. The diagnosis is based on ICBD criteria. Patients can have CNS symptoms including seizures either due to CVST or the parenchymal involvement. It is rare to have both in the same patient as seen in ours. As per EULAR 2018 recommendations, the treatment for parenchymal involvement includes high-dose glucocorticoids which should be started together with an immunosuppressant like azathioprine. Patients who have severe onset of disease, relapse, failure of treatment, and chronic progression may benefit from monoclonal anti-TNF antibodies. An acute CVST episode should be treated with high-dose glucocorticoids to obtain rapid remission. Anticoagulants may be added for a short duration in those with an additional prothrombotic condition. Prognosis is better in patients with CVST.
Challenges of Microscopic CSF Identification in Isolated CNS TB
J. Lowery 1, S. Noor1, J. Cunico1, L. Officer1
1Brooke Army Medical Center, San Antonio, TX
Intro: Symptoms and imaging findings of CNS tuberculosis can often be non-specific and a challenging diagnosis to make. Sarcoidosis is a multisystem granulomatous disorder that is characterized pathologically by the presence of noncaseating granulomas. Both CNS tuberculosis and neurosarcoidosis can have similar clinical presentations and imaging findings, making for a challenging diagnosis.
Case: A 66 year-old female born in Tijuana, Mexico and immigrated to the United States when she was 17 with no significant medical history, presenting to the hospital with two year history of recurrent, episodic right arm numbness and weakness in addition to gradual development of headaches, vertigo and fevers. Initial MRI demonstrated an enhancing round mass at the left postcentral sulcus with linear extension of abnormal tissue along the postcentral sulcus contacting the dura. Additional imaging revealed no lymphadenopathy or pulmonary involvement. Lumbar puncture showed monocytic pleocytosis and elevated protein and patient was started on empiric antifungal coverage with amphotericin. Despite this, patient rapidly deteriorated becoming encephalopathic and minimally responsive and subsequently developed acute communicating hydrocephalus and repeat MRI demonstrating progressive diffuse leptomeningeal enhancement. She was then taken to operating room for urgent external ventricular drainage and brain biopsy. Initial biopsy report revealed non-caseating granulomas further raising suspicion for neurosarcoidosis, however final path report growing acid fast bacilli confirming diagnosis of TB.
Discussion: The diagnosis of CNS TB can be a challenging diagnosis given the similar clinical manifestations, radiographic findings and overlap with neurosarcoidosis. This case highlights the importance of maintaining a high-index of suspicion for CNS TB when initial radiographic findings and biopsy results are suggestive of neurosarcoidosis. Given the opposing treatment for these two pathological processes, one must remain vigilant and early consideration given to empiric anti-TB treatment.
Co-designing Interventions to Improve Diagnosis in the Emergency Department
P. Mahajan 1, Z. Zhang2, S. Y. Park1, C. Mangus1, H. Singh3, S. Datta1, G. Elshobary1, S. Parker1, R. Ma1, K. Pasupathy4
1University of Michigan, Ann Arbor, MI
2Pace University, New York, NY
3Baylor College of Medicine and Houston VA, Houston, TX
4University of Illinois Chicago, Chicago, IL
Statement of Problem: Emergency departments (ED) are prone to diagnostic errors. Obtaining frontline providers’ perspectives on the diagnostic process and involving them in intervention co-design has been underutilized for improving patient safety.
Description of the Program: Our program develops interventions via a two-phase participatory design process. In Phase 1, ED providers participated in semi-structured interviews. Through transcript analysis, we identified vulnerabilities in the diagnostic process and potential solutions. In Phase 2, ED providers participated in design sessions to evaluate potential interventions. To identify interventions, we reviewed diagnostic error literature and created a list of 80+ interventions corresponding to challenges identified in Phase 1. This list was refined based on feasibility, measurability, sufficiency of empiric basis, and potential to reduce diagnostic errors. Design sessions were then conducted virtually with stakeholders. After discussing a demonstration of storyboard interventions, participants ranked interventions based on importance and feasibility. Finally, participants spent time designing or enhancing an intervention.
Findings to Date: We have conducted 17 interviews with staff from adult and pediatric ED settings. Interviews identified that clinicians often establish differential diagnoses based on patient symptoms, nursing notes, and history presented by trainees before seeing the patient to ensure emergent conditions are not missed. Nurses identified pattern recognition as an integral part of their evaluation, especially in differentiating severity of conditions. Modifying physical aspects of the department, integrating nursing and trainees throughout the diagnostic process, and empowering nurses in patient communication were identified as areas for future interventions. We have conducted 4 participatory design workshops to develop interventions. Participants ranked a diagnostic safety dashboard as the most important potential intervention. The dashboard would update in real-time and display relevant patient information and those most in need of assessment. Participants envisioned a diagnostic pause or team huddle to allow for situational awareness within care teams. Participants suggested a visual timeline intervention that could assess new clinical information in real-time or explain orders to patients and families, with use of the timeline varying based on the user’s role. Our project’s next steps include refining interventions, developing a series of prototypes, and evaluating feasibility in a field-like setting.
Lessons Learned: Frontline providers can be utilized to understand the diagnostic process and participate in designing context-specific intervention to improve diagnostic safety.
Diagnostic Error in Emergency Transfers Associated with Increased Mortality and Length of Stay
S. Mehta 1, C. Hanna1, H. Stinson1, M. Congdon1, M. Galligan1, I. Rasooly1, R. Sutton1, C. Philips1, N. Muthu1, J. Ruiz1
1Children’s Hospital of Philadelphia, Philadelphia, PA
Background: Unrecognized in-hospital deterioration is a significant source of preventable harm. Emergency Transfers (ETs) to the pediatric intensive care unit (ICU)—deterioration events in which hospitalized children require intubation, vasopressor, or ≥60ml/kg fluids within 1 hour of transfer— represent late recognition of deterioration and are associated with increased mortality and length of stay (LOS). Rapid response systems (RRS) can avert ETs through early recognition and response for at-risk patients. While diagnostic error (DE) has been implicated in ICU morbidity and mortality, the contribution of DE to ETs has not been characterized and diagnosis has not been a focus of RRS. We aim to characterize the incidence of DE among patients with ET and assess association with outcomes.
Methods: We conducted a retrospective cohort study of ET occurring between Jan 2015 and June 2019 at a single quaternary, freestanding children’s hospital. ET cases were identified through automated queries of the enterprise data warehouse. Demographic and outcomes data were obtained from the institutional Virtual Pediatrics Systems database. Only the first unplanned transfer during admission was evaluated. Transfers to the neonatal or cardiac ICU or involving patients with active DNR orders were excluded. The primary exposure was presence of DE, identified by two pediatric physicians using the Revised Safer Dx Instrument. Each pair included a critical care physician and either a general pediatrics or oncology physician - the most common transfer services in the cohort. The primary outcomes were in-hospital mortality, ICU LOS and post-transfer LOS. Outcomes were compared with unadjusted logistic and linear regression.
Results: Of 2037 PICU transfers in the study period; 129 met criteria for ET (6.3%). We identified DE in 26 ETs (20%). DEs did not differ significantly by age, gender, race, pre-transfer LOS, deterioration category, or transferring service (Table 1). DE event rates by service were 22% (5/18) in General Pediatrics, 14% (8/56) in Oncology, 45% (5/11) in Surgical Services, and 21% (8/39) in Medical Subspecialties. Compared to non-DEs, ETs with DE had higher mortality (27% vs 10%; Odds Ratio 3.4; 95% Confidence Interval (CI95) 1.2–10.1; p=0.026) and longer ICU length of stay (median 7 days [Interquartile range (IQR) 3-12] vs 4 days [IQR 2-8]; Point Estimate (PE) 9.7 days; CI95 1.4-18.1; p=0.02), but not significantly longer post-transfer LOS (median 24 days [IQR 11-45] vs 13 days [IQR 7-25]; PE 14 days; CI95 –0.5-29.2; p = 0.058).
Conclusion: DE is common in pediatric ETs and associated with increased risk of mortality and LOS. RRS should incorporate diagnostic improvement strategies to support earlier recognition and response to deterioration.
Table 1: Emergency Transfer Cohort characteristics by Presence or Absence of Diagnostic Error
Comparison of characteristics for patients with emergency transfer, deterioration events in which hospitalized children require intubation, vasopressor, or ≥60ml/kg fluids within 1 hour of transfer, who were identified as having diagnostic error or not. Deterioration category based on grouping of VPS STAR Code Diagnosis for primary ICU diagnosis at admission to the ICU grouped into relevant physiologic categories. Data are presented as n (%). All P values are the result of χ2 test of independence.
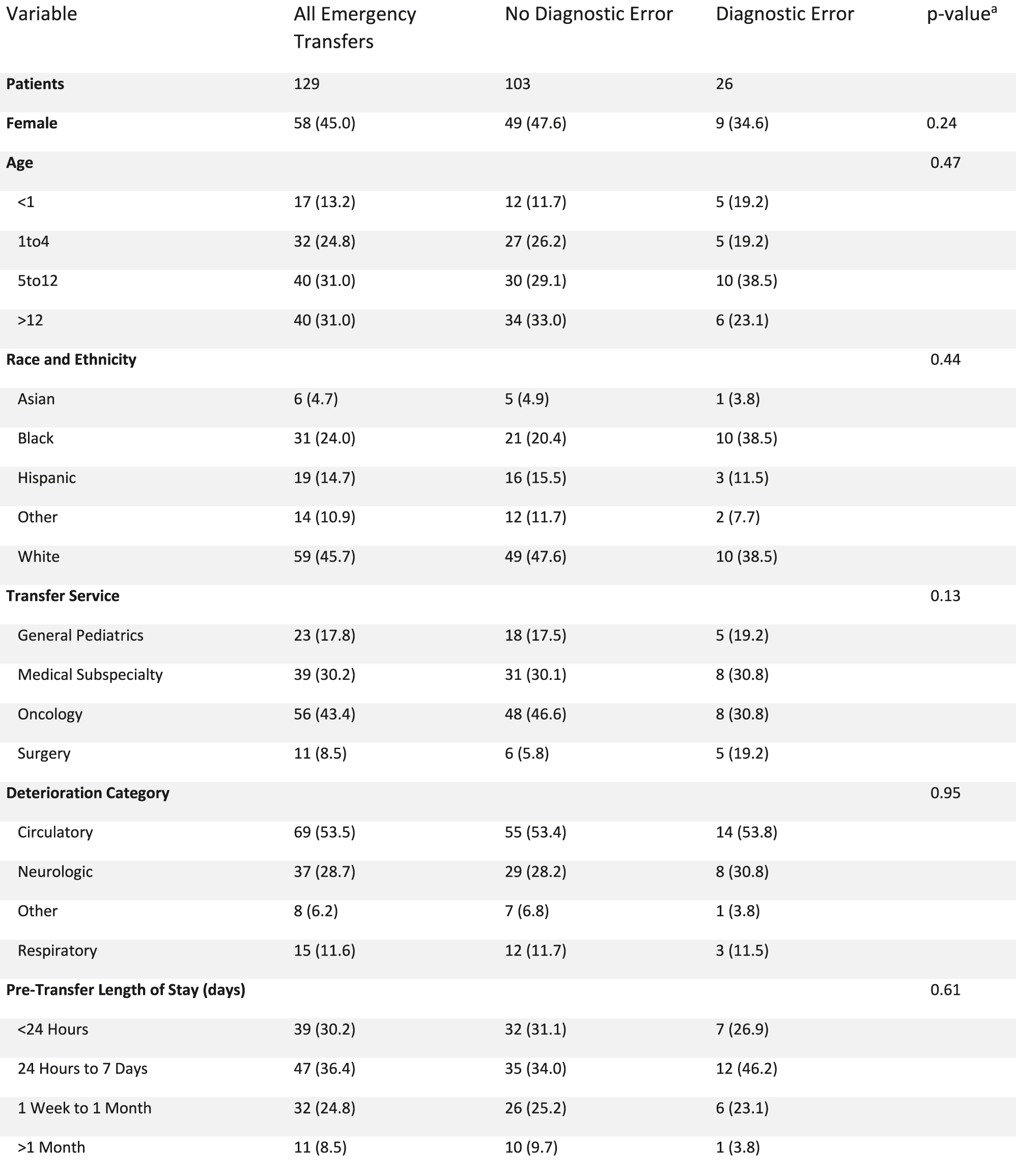
|
Diagnostic Error Prevalence of Subarachnoid Hemorrhage and its Associated Factors
T. Suzuki 1, T. Abe2, Y. Tokuda3
1Department of Hospital Medicine, Urasoe General Hospital, Okinawa, Japan
2Department of Emergency Medicine, Tsukuba Memorial Hospital, Ibaraki, Japan
3Muribushi Okinawa Center for Teaching Hospitals
Background: We aimed to determine the diagnostic error frequency in patients with subarachnoid hemorrhage (SAH) and evaluate factors associated with the error.
Methods: In the 10-year retrospective cohort study, we collected data on adult patients with a final discharge diagnosis of SAH in a tertiary care community teaching hospital. We obtained the clinical characteristics of patients and hospitals/clinics where the patients visited. After cases of possible diagnostic errors were identified by reviewing medical records by two independent physician investigators, cases of diagnostic error and their contributory factors were confirmed by the Revised Safer Dx Tool, a validated instrument for diagnostic error. We evaluated factors associated with cases of error using univariate analysis and multivariate-adjusted logistic regression models.
Results: There were 276 patients with SAH (mean age 60±15, male 31%), and the overall diagnostic error was identified in 8.0% (22/276; 95%CI, 5.1–11.8%). Among the patients with less initial clinical severity (Glasgow Coma Scale of 15 points), the diagnostic error was 12% (14/121; 95% CI, 6.5–19%), which was greater (odds ratio, 17; 95%CI, 2.2–132) than in patients with more (0.8% (1/132); 95%CI, 0.02–4.1%). Despite being of lower initial severity (GCS at initial presentation to any healthcare facilities 15 for those with diagnostic error vs range 9-15 with 55% having GCS<15 among those without), the patients with diagnostic error experienced similarly severe outcomes, including SAH complicated by vasospasm, hospital length of stay, ability to return directly home at hospital discharge, in-hospital mortality, 28-day post-hospital mortality, and modified Rankin scale disability at discharge. The Revised Safer Dx Tool revealed that cognitive bias was a major contributory factor in diagnostic error. Errors in the integration or interpretation of clinical information involved in more than 80% of the patients and interpretation of test results contributed to diagnostic error, for example, recognizing a consequence of fresh bleeding as the old one. While inappropriate follow-up/disposition plans were found in about 60% of patients, including the two with neurological consultation. Furthermore, patients with diagnostic error underwent diagnostic tests and therapy, which were less relevant to SAH.
Conclusions: Diagnostic error potentially worse the clinical outcome in patients with SAH; nevertheless, patients with diagnostic error showed less severity in clinical condition on their initial presentation, and diagnostic error may lead to less relevant diagnostic tests and treatment for SAH. Improvement of the diagnostic process in terms of cognitive error should be implemented.
Diagnostic Excellence Grand Rounds (DExGR) – Clinical Reasoning in Action!
M. Arteaga-Garavito 1, B. Wells1, K. Tran1*, M. Jancis1*, M. Hugh1
(*Presenting Author)
1Southern California Permanente Medical Group, Pasadena, CA
The Southern California Permanente Medical Group (SCPMG) implemented the Diagnostic Excellence Grand Rounds (DExGR) – Clinical Reasoning in Action! inspired by the SIDM session Clinical Problem Solving in Action. Our educational strategy hopes to elevate the culture of diagnostic excellence in quality care for our patients. Each virtual session has a panel of clinicians analyzing a case with diagnostic uncertainty in real time. The goal is to provide a psychologically safe educational environment for learners to rekindle the joy of medicine by identifying barriers in the diagnostic process and tools to overcome these barriers. Continuous education is crucial for practicing clinicians to provide high-quality patient-centered care, especially in mitigating diagnostic errors. Our DEx Grand Rounds interleave new and existing enduring materials, leverages meeting technologies, and educational formats to engage busy clinicians to practice psychological safety, self-awareness of biases and highlights the importance of collaborating with colleagues in solving cases with diagnostic uncertainty. The participation of patients during a session has been discussed and will be implemented in our next phase. For each session there is monitoring of live attendance, recordings, polling/chat participation, CME survey completion and participant feedback. Each session has had at least 100 live attendees, and about 40 recording views. Below are some of the comments received from attendees:
– “Great presentation, hope there are many more of these with rotating panelists. Improves culture of learning.”
– “Well done, would like to see other variations on this same type of process.”
– “Perhaps more audience participation but i highly enjoyed it as is.”
– “Please keep going and can’t wait to learn more both the bias and case studies helping us stay on our feet/toes so to speak.”
– “Please have more cases.”
– “Panel and expert comments were fantastic as the case unfolded.”
Direct Hospital Admissions from Freestanding ED for Ischemic Stroke: A Friend or a Foe?
S. Noor 1, W. Hoffman1, L. Officer1, J. Cunico1
1Brooke Army Medical Center, San Antonio, TX
Learning Objectives: 1. Describe what imaging should be considered prior to transfer to an external facility in a patient with concern for acute stroke. 2. Identify three factors that might increase the risk for transitions in care when transferring a patient from an emergency department (ED) to a separate hospital inpatient service.
Case Information: A 41-year-old male with history of hypertension presented to a freestanding emergency department with continuous vertigo and gait ataxia. He was transferred to our tertiary facility as a direct admission overnight to the internal medicine service for rule out of posterior circulation stroke. Shortly after admission, he became progressively agitated, at which time neurology was consulted. An emergent CT head and CT angiogram (CTA) head and neck revealed a large cerebellar stroke with significant cerebral edema, obstructive hydrocephalus, and an ipsilateral vertebral dissection. He underwent an emergent suboccipital craniotomy as well as placement of external ventricular drain within a few hours of admission. After a prolonged hospital course, the patient was discharged to an acute rehabilitation facility. On 3-month follow-up, the patient had minimal residual ataxia.
Discussion: This case illustrates a sentinel event which occurred during a direct admission from a freestanding ED. Transitions in care are notoriously high-risk, but especially so for patients with acute ischemic stroke due to the rapidly evolving neurologic status. This case highlights the challenges in assessing patients’ acuity over the phone for high-risk transfers, and the need for standardized training for residents faced with these decisions. Standardized checklists can play a crucial role in preventing such sentinel events. For concern of acute stroke, the inclusion of imaging in addition to expert consultation with neurology could allow for accurate triage and disposition. Lastly, ED to ED transfers should be encouraged for high-risk transfers with potential of rapid deterioration during transport.
ECO-Design Workshops for Increasing Clinician Participation in Diagnostic Safety Interventions
A. Meyer 1, A. Offner1, U. Shahid1, H. Patel2, T. Giardina3, A. Savoy4, H. Singh3
1Houston VA and Baylor College of Medicine, Houston, TX
2Center for Health Information and Communication, Richard L Roudebush VA Medical Center, Indianapolis, IN
3Baylor College of Medicine and Houston VA, Houston, TX
4Purdue School of Engineering and Technology, Indiana University-Purdue University, Indianapolis, IN
Background: Participation from clinician stakeholders can improve the design and implementation of diagnostic safety interventions. Participatory design methods, especially co-design methods, comprise stakeholder-led design activities that are time consuming. Competing work demands and increasing workloads make clinicians’ commitments to typical participatory methods even harder. The COVID-19 pandemic further exacerbated barriers to clinician participation in such interventions. As such, we explored a virtual participatory design approach to conduct brief electronic co-design (ECO-design) workshops with primary care clinicians. This was then used to codevelop feedback interventions regarding abnormal test result follow-up in primary care.
Methods: We adapted traditional in-person co-design workshops to online delivery and adapted co-design workshop series to fit within a single, one-hour session. We applied this ECO-design workshop approach to codevelop feedback interventions regarding abnormal test result follow-up in primary care. We conducted ECO-design workshops with primary care clinicians at a medical center in Southern Texas using videoconference software. Each workshop focused on one of three types of feedback interventions: social, sociotechnical, and technical. We paired electronic materials and software features to facilitate participant interactions, prototyping, and data collection. The workshop protocol included four main activities: problem identification, solution generation, prototyping, and debriefing. Two facilitators were assigned to each workshop and one researcher resolved technical problems. After the workshops, our research team met to debrief and evaluate workshops.
Results: Twenty-eight primary care clinicians participated in our ECO-design workshops. We completed four parallel workshops, each with 5-10 participants. We conducted traditional analyses and generated a clinician persona (representative description) and user-interface prototypes. Also, we formulated recommendations for conducting future ECO-design workshops’ recruitment, technology, facilitation, and data collection (Table). Overall, our adapted workshops successfully enabled primary care clinicians to participate without increasing their workload, even during a pandemic.
Conclusion: ECO-design workshops are a viable, economical alternative to traditional approaches. This approach fills a need for efficient methods to involve busy clinicians in the design of diagnostic safety interventions.
Table. Selected observations and recommendations.
| WORKSHOP COMPONENT | OBSERVATION OR LESSON (FACILITATOR OR BARRIER) | RECOMMENDATION |
|---|---|---|
| Recruitment | Invitees may not be from the desired stakeholder group (barrier). | Plan to excuse excluded participants or remove their data. |
| Technology | Dial-in users and users with no or disabled cameras limit assessment of engagement (barrier). | Encourage participation via video. |
| Facilitation | Participants who self-identified as experts were prompted to contribute at different points during the workshop (facilitator). | Employ at least 3 people in the session: moderator, notetaker, and technical facilitator. |
| Activities | Established relationships among participants expedited introductions (facilitator). | Define the problem beforehand; allocate workshop time only to describe and confirm the problem. |
| Allow time for participants to evaluate the session. | ||
| Data collection | More difficult to engage participants in completing workbooks or other tasks (barrier). | Before adjourning, collect workbooks regardless of completeness. |
| Save the chat log for analysis. |
Experimental Methods for Understanding Diagnostic Difficulty
J. Sloane 1, A. Meyer2, H. Singh3, B. Newell4, C. Donkin5
1Center for Innovations in Quality, Effectiveness and Safety (IQuESt), Houston, TX
2Houston VA and Baylor College of Medicine, Houston, TX
3Baylor College of Medicine and Houston VA, Houston, TX
4UNSW
5LMU
Background: Diagnostic decision-making is a complex process; while some cases may be perceived as “easy”, often cases are not so straightforward. Although several studies have explored decision processes in “easier” vs “more difficult” cases1–3, what makes a case difficult can affect how clinicians respond to and diagnose patients. For example, a case may be difficult because it generates many potential diagnoses that are hard to rule out (i.e., “hard”). In this scenario, clinicians would likely seek out more information (e.g., second opinions, additional testing). Conversely, a case may be difficult because of misleading information (i.e., a “trick”), which could result in inaccurate diagnosis and overconfidence. This study aimed to help disentangle the unique effects of hard and trick cases on diagnostic reasoning.
Methods: We created three types of general medical cases (i.e., easy, hard, and trick) with the help of a senior medical resident. We then asked medical students to read the cases and provide a differential diagnosis and rate their confidence for each case. The cases were designed to elicit different responses with respect to accuracy, number of differential diagnoses, and confidence (See Table 1). Specifically, we predicted confidence would be lower for hard cases compared to trick cases. We analyzed the confidence ratings using t-tests.
Results: Out of the 6 cases we originally designed, 3 successfully fit into the anticipated categories (1 easy, 1 hard, 1 trick). Our results showed participants had statistically higher confidence on incorrect diagnoses for trick cases compared to hard cases (p = 0.01). Additionally, participants provided a total of 12 unique diagnoses for hard cases, but only 4 for trick cases.
Conclusion: We developed novel easy, hard, and trick cases and found clear differences with how participants responded to hard vs trick cases, even though both are “difficult”. These cases lay the groundwork for understanding how clinicians respond to different kinds of difficult cases. Future research can use these cases when testing interventions to improve diagnostic decision-making (e.g., testing if feedback interventions will be differentially effective on hard vs trick cases).
Exploring Differences in Summary Statement Synthesis Between Experts and Novices
C. McQuade 1, S. Rothenberger2, L. Zwaan3, J. Lister4, A. Olson4, E. Bonifacino1, M. Simonson1
1University of Pittsburgh Medical Center, Pittsburgh, PA
2University of Pittsburgh School of Medicine, Pittsburgh, PA
3Erasmus University, Rotterdam, Netherlands
4University of Minnesota School of Medicine, Minneapolis, MN
Formulating a problem representation is a fundamental step in diagnostic reasoning. Trainees practice this mental task by learning to write summary statements (SS). However, little consensus exists on what characterizes a good SS. This project analyzed differences in SS construction between novices and experts and investigated which characteristics correlate with diagnostic accuracy. Internal medicine interns (“novices”) and teaching faculty (“experts”) were given 2 written clinical vignettes and instructed to write a SS and 3-item differential diagnosis for each. Deductive content analysis was completed on each SS using a codebook which was refined iteratively. Two authors coded 25% (n=32) of the SS and differences were resolved by consensus. One author coded the remainder. The primary outcome was differences in SS characteristic frequencies between groups. Secondarily we investigated which characteristics correlated with diagnostic accuracy. Mixed-effects regression with random effects modeling compared case-level outcomes by group to account for within-participant correlation. Overall, 125 statements were analyzed from 24 novices and 39 experts. Experts wrote an average of 0.8 fewer comorbidities (p=0.001) and 0.6 more examination findings (p=0.02) than novices while using a similar word count (p=0.34). Experts were less likely to include a diagnosis (OR 0.3, CI 0.1-0.9) or report inaccurate information (OR 0.3, CI 0.1-0.99). Frequencies of temporal descriptors, semantic qualifiers, and pertinent negatives were similar between groups. Experts tended to rename clinical data using more abstract terms (e.g., leukocytosis instead of “WBC 14”) but the difference was not significant (p=0.06). Regardless of expertise level, writing fewer comorbidities, fewer total clinical findings, and fewer inaccuracies correlated with diagnostic accuracy (p<0.05). Overall diagnostic accuracy was similar between novices and experts (p=0.56). Creating a summary statement is a key diagnostic step but how summary quality correlates with diagnostic accuracy is unknown. In this study diagnostic accuracy was associated with summaries including fewer extraneous details and inaccuracies. Expertise level did not correlate with diagnostic accuracy, but novices more frequently included irrelevant or inaccurate information. This may reflect more experienced clinicians’ ability to identify signal vs. noise in a patient’s clinical data. This study represents the first exploration characterizing features of summary statements by expertise level and what factors are associated with diagnostic accuracy. Future studies should determine the causes of novice-expert differences and if targeted educational or other interventions for summary statements improve diagnostic accuracy.
Guess Not, Miss Not: Better Detection of IBD by Learning from Diverse Patients
S. Schrandt 1
1Society to Improve Diagnosis in Medicine, Alpharetta, GA
The landmark National Academies of Sciences, Engineering, and Medicine (NASEM) report: “Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care” outlined almost twenty years ago stark differences in the healthcare and health outcomes of racial and ethnic minorities in the U.S. and unfortunately the gap has only widened since then. Only in recent years has mythology about racial or ethnic differences in pain tolerance, kidney function, and other biological processes been debunked. Adding to this deficit, is a lack of cultural competency training in medical schools and in continuing medical education programs. Preconceived notions or assumptions that go unchecked can lead to delays or mistakes in diagnosis, and less than optimal treatment approaches. Just as in other diseases and conditions, the structural inequities in IBD are immense, beginning with a long-held belief that IBD is less common in people of color.
Meanwhile, patient engagement is an increasingly integral component of health professions training, and its importance in CME has been codified by the Accreditation Council on Continuing Medical Education’s Criterion 24. In this project, a survey of racially and ethnically diverse diagnosed IBD patients was used to inform a Continuing Medical Education (CME) course for gastroenterologists and primary care clinicians about optimal diagnosis and treatment of IBD, with a focus on people of color. The survey, co-designed by two IBD patient faculty members, two gastroenterologist faculty members, a patient engagement expert, two medical education researchers, and informed by a host of key informant interviews of IBD patient advocates, was drafted to capture the barriers and facilitators in the diagnostic process.
Among the key findings for consideration and uptake by learners were for those who had a hard time getting diagnosed, a.) their symptoms were incorrectly blamed on lifestyle choices, diet, and stress, b.) they did not feel that they were listened to or believed, and c.) they delayed their initial medical consultations because they did not realize their symptoms were that abnormal—i.e., “nobody talks about poop”. This material was curated for a panel discussion among the two clinician faculty and the two patient faculty, who were able to provide practical and tangible suggestions for how to be aware of these challenges and work to avoid and overcome them. Grounding CME in the lived experience of patients is an and effective way of providing practical guidance to clinicians about pitfalls to avoid and best practices to emulate in diagnosis.
Have We Somewhere Misdiagnosed Cyclic Thrombocytopenia for Immune Thrombocytopenia?
M. Yokoe 1
1Japanese Red Cross Aichi Medical Center Nagoya Daini Hospital, Nagoya, Japan
Statement of Problem: Cyclic thrombocytopenia (CTP) is very rare hematological disorder in which patients with low platelet counts at varying times. Clinical features are similar to those of Immune thrombocytopenia (ITP), so patients are frequently misdiagnosed as ITP. CTP is only taken into consideration when ITP-specific treatments have repeatedly failed. Among the thrombocytopenia deferential diagnosis, ITP is most common and likely to have been diagnosed by physicians without doubt of CTP. As a result, the patients diagnosed as ITP are usually treated with steroids, rituximab, or splenectomy. To prevent from giving unnecessary therapies for CTP patients, an adequate procedure should have been established.
Description of the Intervention Program: ITP is a diagnosis of exclusion in which patients have low platelet counts less than the lower limit of normal. CTP is characterized by periodic platelet count fluctuations at intervals of a few weeks with mild symptoms. Cycle duration varies individually and usually ranges between 14 and 36 days, potentially reflecting different etiologies. Therefore, frequent complete blood counts weekly or biweekly are reveled the fluctuations of platelet count if the patient is CTP not ITP. Exactly for the patient with anxiety of the risk of major bleeding on thrombocytopenia, an initial watch-and-wait strategy is hardly tolerable, neither for the patients nor for their doctors. However, this intervention is most important and easy procedure for diagnosing as CTP. Kyle et al. suggested frequent blood count monitoring and Sumnu practiced every week platelet count check.
Findings to Date: From our experience, A 74-year-old man with purpura and thrombocytopenia was consulted. He was a doctor and had chances of frequent blood check in his clinic every or every 2weeks. The result was shown in Figure1. His bleeding conditions were mild with a recurrent pattern of fluctuations of platelet count. In addition, deferential diagnosis with CTP, specific ITP therapies would not be selected. As for CTP administration, this strategy is advisable.
Lesson Learned: To prevent from giving unnecessary specific ITP therapies for CTP patients, when considering CTP, weekly or biweekly blood tests should be taken for the thrombocytopenia patients.

Identification of Unintentional Weight Loss from Electronic Health Records Data
K. Ufholz 1, G. Rao2, H. Menegay2, M. Beno3, P. Saroufim3
1Case Western Reserve University, Department of Family Medicine and Community Health, Cleveland, OH
2Case Western Reserve University and University Hospitals, Cleveland, OH
3Case Western Reserve University, Cleveland Institute for Computational Biology, Cleveland, OH
Background: Unintentional weight loss (UWL) is a common clinical problem, with an annual incidence of roughly 7% among all adults, and 27% among frail adults age ≥ 65 years. UWL is associated with a higher risk of all-cause mortality. The underlying etiology varies widely, and includes cancer, gastrointestinal problems, infections, psychiatric diagnoses, and social conditions such as food insecurity. Preliminary evidence suggests that clinician recognition of UWL is poor and as many as 60% of cases are missed. Given the high incidence of UWL and evidence of poor recognition, an examination of underlying physician diagnostic practices is important.
Methods: We applied several commonly used criteria to identify UWL re: loss of >5% body weight within 6 months, loss of 5-10% body weight in 12 months, etc) and analyzed results which met one or more criterion. Data were extracted from the EHR records of primary care patients (aged 18-89) with at least two primary care appointments in 2020-2021. We used structured data fields to exclude patients with ICD codes for diagnoses or medications known to cause weight loss. Free text notes were analyzed using the Electronic Medical Record Search Engine (EMERSE) and were used to distinguish between voluntary and unintentional weight loss. We reviewed individual charts to further identify intentional weight loss and to assess outcomes and prognosis.
Results: Out of 766 patients meeting inclusion criteria, UWL was found in 295 (38.5%) and 471 were determined to have lost weight voluntarily. UWL was recognized by providers in just 69 (23.4%). When recognized, providers’ practices were highly variable. Even recognized UWL was often not investigated, especially in elderly, medically-complex patients with symptoms of greater urgency.
Conclusion: UWL is common complaint among primary care patients. Unfortunately, it is rarely recognized by providers. Often UWL appears as part of a constellation of symptoms and may be left unevaluated. Greater provider awareness and standardized diagnostic pathways may help increase UWL recognition rates and also help identify serious underlying causes such as malignancy.
Implementing a Social Determinants of Health Questionnaire in a Family Medicine Residency Program
B. Iyengar 1
1Ascension St. Vincent’s Family Medicine Department, Jacksonville, FL
Given the increased recognition that our patient’s health issues are not only predicated on the biomedical issues, but they are influenced by psychosocial factors, it became clearer that social issues have a powerful impact on the health of our patients. This was further crystallized with the rest pandemic and other areas of civil unrest. With this increased recognition of these factors, we implemented a Social Determinants of Health Questionnaire to a subset of our patients to get a snapshot of the social issues that impact their health.
We used the already developed AAFP Social Needs Screening Tools and distributed them to our adult patients who came to our clinic. The survey is a 14-question screening tool which looks at categories from housing issues, food insecurity, transportation, utilities, childcare, employment, education, finance, and personal safety.
The disquieting reality was that many of our patients were dealing with social issues, many of which had the potential to impact their wellbeing. The number of our patients who were contending with social issues was not negligible. The most sobering fact from this subset of individuals is that many of them are not only experiencing inequities in the system but are wanting and willing to take assistance to help alleviate some of these inequities.

Improving Delays in Children’s Cancer Diagnoses
S. Giusto 1
1Friends of Cathryn Foundation, Laguna Beach, CA
Cancer in children is very rare. In fact, most pediatricians may see 1-3 case in the term of their careers. With only 10,000 children under the age of 15 diagnosed each year, Cancer in children is not something most pediatricians or parents are thinking of when a child begins to show non-specific symptoms. However, when these symptoms do present it’s important that parents and their medical providers are aware of signs that could indeed be cancer.
When my daughter, Cathryn, was beginning to experience back discomfort, headaches, and fatigue at age 4 1/2, she saw her pediatrician to figure out what these symptoms could be. Her symptoms were confounding because she was an otherwise very healthy and happy little girl. Her physician ruled out spine issues by looking at her alignment and ruled her perfectly healthy despite my concerns and intuition that something was very off. As her back pain remitted and returned over the course of a few months, Cathryn one day told me “It really hurts when you hug me”. My alarm bells went off and I insisted on an x-ray (previously denied, deemed unnecessary). That x-ray showed an avocado sized tumor in this now 5-year old’s chest with metastases throughout her body by that time. If we had gone one more month without intervention, Cathryn would have become more sick, paralyzed by the tumors close proximity and invasion of her spine for certain. I often wondered how we missed it, what if we’d caught it sooner, what if, what if, what if……it haunted me. Turns out, that same question haunted many parents like us.
In 2020, 10 years after Cathryn was out of treatment and the founding of The Friends of Cathryn Foundation (to support research), I developed a survey of other Neuroblastoma parents to ask about their diagnosis journeys and what symptoms other children experienced and which symptoms were missed or misdiagnosed. 300 parents shared eerily similar journeys as ours: months of persistent symptoms ruled out as constipation, growing pains, pulled muscles, attempts to get attention, temporary viruses. I gathered a list of the ten most common symptoms and most common misdiagnosis. I also learned about the number of doctor appointments and the length of time between the onset of symptoms to the point of diagnosis. All of this information, plus a emotional and factual testimonials from over 180 parents were put into a presentation called Improving the Time to Diagnosis and is now being shared with medical providers, pediatricians, educational institutions and other members of the children’s cancer community. We’re partnering with other cancer parents and organizations in the UK to share this effort, get the word out and improve the delays to diagnosis in all children’s cancers. Our work is just beginning, and we look forward to making great progress with groups such as SIDM.
Our poster is a piece we developed for the medical community to share as a reminder of what symptoms could be cancer in children.
Investigating Emergency Department Diagnostic Processes: Video Ethnography Methodology Development
P. Mahajan 1, A. Wang1, M. Manojlovich1, S. Parker1, D. Ryamukuru1, C. Cassady2, H. Singh3, E. Davis1, K. Pasupathy4
1University of Michigan, Ann Arbor, MI
2Wayne State University, Detroit, MI
3Baylor College of Medicine and Houston VA, Houston, TX
4University of Illinois Chicago, Chicago, IL
Statement of Problem: Emergency departments (EDs) are prone to diagnostic errors, partially because provider decision-making processes operate at a habitual or subconscious level making it difficult to examine and possibly change diagnostic thinking.
Description of the Program: We demonstrate the feasibility of filming in-situ clinical practice in EDs and describe video analysis of the patient interaction. These are novel tools for mapping the anatomy of the diagnostic process using video-based ethnography. Physician participants wear a micro-camera and microphone to capture first-person perspectives. This provides unique insights into provider thought processes that are not usually apparent. We held short information sessions, distributed one page study overviews, and described opt-out procedures to ED physicians and nurses. We shadowed providers in both ED settings for over 8 hours prior to filming to test feasibility. Our strategy captures first-person perspectives with a small head-mounted camera at eye-level for approximately 2 hours during a clinical shift. During these sessions, a trained member of our research team observes what is occurring around the physician to note contextual factors or influences that the camera may not capture. The physician participant, other staff, or patients are briefed on study procedures with an information sheet prior to observations and may request to have recording stopped at any point. Afterwards, physicians participate in individual recall interviews, where they “think aloud” while watching short video clips of their practice and provide insight into how physicians think in actual settings. Watching clips of their own practice brings habitual, subconscious behaviors to the conscious level for deliberation and reveals insights into diagnostic decision making.
Findings to Date: We have filmed one physician to date. We aim to film a total of ten physicians and have recruited seven so far. We have begun iterative analysis during the data collection process. Members of our research team first independently review each video-recorded session to note points from the video that were particularly important or interesting in the diagnostic process. We then discuss findings and prioritize clips for the recall interview. Using an open coding method, we will review the videos for recurring themes guided by distributed cognition theory.
Lessons Learned: It is labor intensive to engage providers in video-based ethnography, but once deployed, will give unique insights that can help understand and unravel the cognitive aspect of diagnosis and get a sense of how diagnostic cognition is distributed across providers, settings, and tools.
Legionella and Cold Agglutinin Disease; A Case Report
K. Shakfeh 1, C. Mateja1, F. Shotande1
1University of South Florida, Tampa, FL
Learning Objectives: 1) To highlight the presentation and management of Legionnaire’s Disease 2) To highlight the presentation and management of Cold Agglutinin Hemolytic Anemia 3) Specific areas of improvement in the workup of both diseases
Case Information: A 40-year-old previously healthy gentleman was admitted with new anemia and community acquired pneumonia. The workup was significant for Legionella and his antibiotics were tailored accordingly. He had concurrent Cold Agglutinin Hemolytic Anemia and was kept warm. It was unclear if it was primary or secondary, as he claimed a history of feeling unwell in winters. Following source control and being kept warm, his symptoms dramatically improved, and his symptoms resolved outpatient. Unfortunately, outpatient workup for primary vs secondary cold agglutinin disease was never completed. His total hospitalization lasted 3 days, with his admission diagnoses being identified on the night of admission.
Discussion: While Mycoplasma species are known to be associated with cold agglutinin disease, there is a lower association with Legionella. However, the patient’s symptoms and laboratory findings increased our suspicion for Legionella. Following antibiotic therapy and ambient warming, his acute phase reactants dropped dramatically. His hemolysis stopped on follow up labs during his hospitalization as well. While our practice generally discharges patients admitted for pneumonia on the same day as transition to oral antibiotics, the degree of his hemolysis and elevation of his acute phase reactants made us more conservative.

Measurement of Diagnostic Performance in the Emergency Department for Pulmonary Embolism
J. Sather 1
1Yale School of Medicine, New Haven, CT
Statement of Problem: –Pulmonary embolism (PE) is a unique use-case for the measurement and improvement of diagnostic performance. –PE is the third most common cardiovascular disease after coronary artery disease and stroke and can be lethal if misdiagnosed. –Over-utilization of advanced imaging may also induce patient harm without increasing the diagnostic yield of PE evaluations. CT imaging for PE is costly, time-consuming, and exposes patients to the risks of ionizing radiation and contrast media. –The diagnostic framework for PE has been extensively studied and epitomizes the precarious balance between the benefits of accuracy and the harm associated with over testing. –Prior work has demonstrated that PE is still often missed, and utilization and yield of CT are variable. No balanced measures of diagnostic performance have been developed that acknowledge these cognitive pressures on the diagnostic process. –We received funding from the Gordon and Betty Moore Foundation through their Diagnostic Excellence Initiative to develop a suite of measures of diagnostic performance for PE that incorporates three components: accuracy, CT utilization, and CT yield.
Description of the Intervention or Program: –We developed an Artificial Intelligence (AI)-derived phenotype using natural language processing (NLP) and structured electronic health record data to reliably capture Yale-New Haven Health system-wide diagnoses of PE from 2014-19. –We evaluated ED diagnostic opportunities within an antecedent 7-day window of a system-wide PE. –We reported measures of diagnostic accuracy, CT utilization, CT diagnostic yield during the 5-year window across the Yale New Haven Health System (YNHHS) (2014-19).
Findings to Date: –Please refer to attached table.
Lessons Learned: –Measures of PE diagnostic accuracy suggest a focus for quality improvement (QI) initiatives. –As QI efforts are implemented to improve diagnostic accuracy, our balanced suite of measures can monitor impact of these interventions on utilization and yield measures to optimize diagnostic safety. –ICD-10 code-based identification of PE diagnosis is unreliable. AI-supported models using NLP are feasible and more reliably capture clinically relevant diagnostic events. –Our suite of measures for PE diagnostic performance can be used by providers and institutional leadership to align practice with established evidence-based guidelines to reduce patient harm from misdiagnosis and over-utilization of diagnostic testing.

Medical Image Flipping is a Risk Factor for Wrong-Site Procedures
J. Taylor 1
1Cleveland Clinic Lerner College of Medicine, Cleveland, OH
Background: Wrong-site, -person, -procedure errors (WSS) are among the most common sentinel events in health care. Inadvertent flipping of images has led to wrong-side brain surgery. In dermatology wrong-site procedures have occurred in the absence of photographs.
Methods: Dermatology Department members were surveyed for examples of actual and potential image manipulation as a risk factor for WSS. And the scope of available medical image devices, software, practices, and standards were reviewed.
Results: Two examples of near misses were identified; 1) In post-op follow-up of two separate Mohs microscopic surgery procedures the reviewing nurse noted that the images submitted through the patient portal for the EMR showed the healing scars to be on the opposite side of the face than the original; in these cases, the root causes appear to be selfie images that were not reversed. and 2) In pre-operative Mohs surgery photos taken in the office over a period of several visits, the dermatologic surgeon noted that the images of the scalp were flipped in one instance. The root cause was the result of the camera image having to be stored in a separate folder (RIS), which required dicomizing, during which it was flipped, before being uploaded to the ""get images"" file in the EMR. Office-generated photographs may be stored a) natively in an EMR or b) in a separate medical imaging system or PACS (Picture Archiving and Communications System). Most photographs may be manipulated including image flipping. In our EMR native Haiku and PACS stored photos, visible images may be manually flipped by the provider and return to their initial non-flipped state when the programs are closed (see flipped hand images). Patient-generated photographs are used often in dermatology: Smart-phone photos submitted through EMR patient portals. Teledermatology images submitted usually through smart phones, as part of “store and forward” asynchronous process. Smart phone “Selfies”, take a mirror image which are usually (but not always) auto-flipped. Software is available to prevent auto-flipping.
Conclusions: Lessons learned to minimize image manipulation errors: Patients and providers should be educated as to the vagaries of the multiple cameras and software used. Enterprise- and office-generated photographs should be stored in their initial unaltered RAW format. Patients should not use image editing software. A printed word or object (e.g., face side of a dime) in the photograph may help quickly identify a flipped image. Teledermatology standards for photography are published and ATA has promoted DICOM standards Adoption of DICOM standards may allow for standardized metadata definitions that are specific to each specialty and unique to each imaging modality.
Odynophagia, a Unique Presenting Symptom of Giant Cell Arteritis: A Case Report
C. Marcano 1, C. Anyanwoke1, V. Hsu1, M. Newman1, S. Quo1
1Department of Internal Medicine, University of Miami-Holy Cross Hospital, Fort Lauderdale, FL
Learning Objectives: Giant Cell Arteritis (GCA), also known as temporal arteritis, is a systemic inflammatory granulomatous vasculitis of medium and large-sized arteries that arises in adults, mostly in females, above the age of 50 (1). It is the most common vasculitis in the western countries and presenting symptoms include headache, jaw claudication and temporal scalp tenderness, while the most feared complication is that of irreversible visual loss (1). We present a rare case of a patient diagnosed with giant cell arteritis, whose presenting symptom was odynophagia.
Case Information: 81-year-old lady with a past medical history of hypertension, hyperlipidemia, a previous TIA, and recent diagnosis of oropharyngeal candidiasis one month prior for which she was prescribed nystatin mouthwash, presented for progressively worsening odynophagia with associated neck pain. Associated symptoms included 10-pound weight loss over a 3-week period and generalized weakness. Outpatient, she underwent an EGD which was negative for esophageal candidiasis. Patient was admitted and started on fluconazole IV with no improvement. CT Neck and CT Brain revealed no acute abnormalities. Inflammatory markers were elevated, ESR 101 and CRP 61. Neurology was consulted due to concern for GCA. She was started on Solumedrol 250mg IV, then subsequently tapered to Solumedrol to 60mg while pending biopsy results. Patient reported improvement of odynophagia upon Solumedrol initiation. Both right and left muscular temporal arteries biopsy results showed marked arteritis which confirmed diagnosis of temporal (giant cell) arteritis.
Discussion: GCA may initially present with oropharyngeal candidiasis, odynophagia, and neck/jaw refractory to treatment. Given the potential unwanted complications of not treating this condition, we encourage physician to include GCA in their differential diagnosis when encountering a patient with odynophagia of unclear etiology.
Performance of E-Triggers to Identify Diagnostic Errors in High-risk Clinical Presentation in ED
V. Vaghani 1, W. Li2, D. Sittig3, A. Gupta2, U. Mushtaq1, H. Singh4, U. Mir1
1Baylor College of Medicine, Houston, TX
2Michael E. DeBakey Veterans Affairs Medical Center and Baylor College of Medicine, Houston, TX
3University of Texas School of Biomedical Informatics, Houston, TX
4Baylor College of Medicine and Houston VA, Houston, TX
Background: Methods to identify and understand missed opportunities for diagnosis (MODs) in emergency departments (ED) can inform improvement efforts. A rules-based electronic health record (EHR)-based trigger (e-trigger) algorithm has been used to identify selected patients likely to have MODs based on unexpected return visits. Building on this work, we developed two e-triggers and examined their performance in identifying MODs in patients with high-risk clinical presentation in the ED.
Methods: We developed two new e-triggers using the Safer Dx Trigger Tools Framework (Trigger I & II). For Trigger I, we used a refined symptom-disease dyad approach based on our recent work and identified stroke hospitalizations within 30 days of treat and release ED visits for dizziness in patients with 2 or more stroke risk factors. For Trigger II, we performed literature reviews and gathered expert input to develop an algorithm to detect hospitalization within 10 days after treat and release ED visit for abdominal pain with high (T>99. F or >37.5 C) or low body temperature (T<96.8 F or <36.3 C). Both e-triggers were applied to Veteran Affairs EHR data warehouse for years 2018-2019. One physician served as the primary reviewer for all records, and a second physician-reviewer independently evaluated a random subset of 20% of records to assess the reliability of judgements related to MOD. Prior to the study, we pilot-tested both e-triggers and objective data collection instruments using operational definitions and standardized procedures.
Results: The e-triggers were applied to >9 million patient records, and 100 randomly selected trigger-positive cases were identified for each trigger. 91 cases for Trigger I and 86 cases for Trigger II met trigger inclusion and exclusion criteria during chart review. Of 91 cases for Trigger I, 48 (52.6%) cases had MODs, 39 (42.8%) had no MODs, and 4 (4.6%) had coding errors. Of 86 cases for Trigger II, 26 (30.2%) had MODs and 60 (69.8%) had no MODs. Reviewer agreement was72.7% and 72.2% for Trigger I &II.
Conclusion: A high-risk clinical presentation-based e-trigger appears to be valuable in identifying MODs in emergency care although 1 of 10 records had unreliable diagnosis and procedure coding. A refined symptom-disease based e-trigger focusing on high-risk patients had much superior performance (52.6% vs. 30.2%) compared to simple symptom-disease dyad-based trigger in our prior work. Using multiple e-triggers such as the ones we developed can serve as the foundation for safety improvement efforts in ED settings.
Relationship Between the Clinical Learning Environment and Resident Clinical Reasoning Documentation
V. Schaye 1, J. Burk Rafel1, B. Guzman1, K. Hauck1, D. Sartori1, I. Reinstein1, M. Haller1
1NYU Grossman School of Medicine
Background: The clinical learning environment (CLE) – sum of organizational structures and cultures that trainees encounter – can have a significant impact on resident performance which can be difficult to quantify. We explore the relationship between CLE changes at one academic internal medicine program and resident clinical reasoning (CR) documentation assessed using a previously developed machine learning (ML) model that classifies CR documentation as high- or low-quality.
Methods: We conducted a retrospective cross-sectional analysis of trends in resident CR documentation quality determined by the ML model among all general medicine admissions (n = 11,584 admissions, n = 318 residents) from July 2017-June 2021. During this time, two significant changes to the CLE occurred: (1) in July 2018, staffing changed from a night-float model with episodic night admitting coverage to a continuous care model with night intern-resident dyads integrated into each team to improve continuity of care; and 2) from March 2020-May 2020, a COVID-19 hospitalization surge that disrupted staffing. Descriptive statistics and chi squared testing, including tests for linear test, were performed with the R statistical package.
Results: CR documentation quality significantly improved following the night admitting team changes, from 44.7% pre-change to 63.2% the following year, with further increases in subsequent years (p<.0001 for heterogeneity; p<.0001 for linear trend, Table 1). Although there was a significant decrease in CR documentation quality during the COVID-19 surge (67.5% to 58.3%, p<.0001), quality recovered post-surge.
Conclusions: We observed program-wide improvements in resident CR documentation following team structure changes emphasizing night-to-day continuity of care, which continued to improve over the subsequent years. There were likely additional changes to the CLE difficult to quantify during this time accounting for the continued improvements. There was not a sustainable impact of the disruptive COVID-19 surge on CR documentation quality. Our findings highlight the utility of using an automated ML model to explore the relationship between CLE changes and resident performance. However, the cross-sectional design of this study precludes causal claims. Next steps will be to analyze the impact of these changes using a multiple logistic regression model to control for factors such as volume of admissions.
Table 1. Trends in Clinical Reasoning Documentation Quality Among 11,584 Admission Notes Written by 318 Internal Medicine Residents from 7/2017-6/2021

SARS-CoV-2 and a Blood-Curdling Headache
S. Zeeshan 1
1MCW Green Bay, Green Bay, WI
Introduction: Cerebral venous thrombosis is a rare cerebrovascular disease accounting for 0.5-1% of strokes.1 Several viral infections (VZV, CMV, HSV) have been associated with cerebral venous thrombosis. In this report, we present the case of a woman with a catastrophic cerebral venous thrombosis with SARS-CoV-2. Presentation -16-year-old non-smoker on OCP with severe headache, vomiting and anorexia. -GCS 15/15. Afebrile -SBP 140mmHg -No neurological deficit. Investigations -COVID+ -Elevated D-dimer -CT head - Hyperdensity in the sagittal, torcula, straight and transverse sinuses. -MRI/MRV - Complete occlusion of all major sinuses Initial Treatment Loading dose of IV heparin followed by infusion Progress Day 3- Onset of diplopia, dysconjugate gaze and left-sided weakness. Urgent biplane cerebral angiogram and venous thrombectomy treating complete venous sinus occlusion with arterial congestion. Recurrent thrombus on the left side during thrombectomy so continuous TPA Infusion catheter placed into sagittal sinus. Day 4 - CTA revealed persistent thrombus in vein of Galen despite TPA infusion. Day 5 - Repeat cerebral angiogram with venous thrombectomy and sigmoid sinus dilation All sinuses clear and draining post-procedure Day 6 – Extubated and began rehab. Subsequent MRI: Edema of the splenium of the corpus callosum and several small foci of acute ischemia in both parietal lobes Coumadin with heparin bridge Discharged on day 12 clinically markedly improved Two weeks post-discharge: oWeakness resolved oDiplopia resolving oHeadaches mild
Discussion/Conclusion: CVST is uncommon in SARS-CoV-2, but the neurologic effects are severe if not detected and treated early. Anticoagulants are a mainstay of CVT treatment, even in the case of haemorrhagic infarction.2 In this case, the patient had recurrent thrombus despite heparinisation and thrombectomy. This is due to increased systemic hypercoagulability and thromboembolism in SARS-CoV-2 infection.3 Timely neuro-vasc
Seeing With Your Own MRIs: Anchoring on Radiographic Findings in a Case of PRES
N. Luche 1, C. McQuade1
1University of Pittsburgh Medical Center, Pittsburgh, PA
Learning Objectives: - Anchoring bias and confirmation bias are risk factors for diagnostic delay and can predispose patients to unnecessary procedures - Disease syndromes with poorly-defined diagnostic criteria can be especially susceptible to bias
Case: A 54-year-old woman with HTN, HLD, CAD, and PAD, presented with chronic progressive headaches, blood pressure 163/147 mmHg, and witnessed seizure requiring intubation. MRI brain showed subtle signal abnormality involving leptomeninges and cortex in frontoparietal and occipital regions, read as suggestive of leptomeningeal carcinomatosis. CT pan-scan and lumbar puncture were unrevealing. After extubation, the patient had persistent severe hypertension, vision loss, and paretic left foot. Repeat MRI brain showed progressive parietooccipital findings with ischemia, read as suspicious for vasculitis. Patient underwent brain biopsy to confirm vasculitis, but pathology showed ischemic tissue. A third MRI on hospital day 14 showed maturing infarcts likely from posterior reversible encephalopathy syndrome (PRES). Symptoms improved with tightened blood pressure control. In retrospect, the patient’s presentation with neurologic changes, severe hypertension, and posterior MRI abnormalities fits the illness script for PRES. However, PRES is a clinical diagnosis subject to cognitive biases like anchoring bias (relying heavily on early information in a case) and confirmation bias (favoring supportive evidence over discordant information) (1-2). Diagnostic certainty in radiology reports is often misinterpreted and may have contributed to anchoring bias early in this case (3-4). Confirmation bias also led to a brain biopsy to support an incorrect radiographic diagnosis of vasculitis. Diagnostic errors are made in an estimated 3-4% of radiographic interpretations (2), and initially missed radiographic diagnoses may be missed again in one-third of repeat imaging studies (5). Thus, vigilance against anchoring on radiographic diagnosis is important, particularly when time to diagnosis can impact prognosis, as in PRES (6).
Works Cited:
(1) Fugate JE, Rabinstein AA. Posterior reversible encephalopathy syndrome: clinical and radiological manifestations, pathophysiology, and outstanding questions. The Lancet Neurology. 2015 Sep; 14(9): 914–925. doi:10.1016/S1474-4422(1500111-8).
(2) Busby LP, Courtier JL, Glastonbury CM. Bias in radiology: the how and why of misses and misinterpretations. RadioGraphics. 2018; 38: 236–247.
(3) Khorasani R, Bates DW, Teeger S, Rothschild JM, Adams DF, Seltzer SE. Is terminology used effectively to convey diagnostic certainty in radiology reports? Acad Radiol. 2003 Jun; 10(6): 685-688.
(4) Mityl MI, Gilcrease-Garcia B, Searleman A, Demertzis JL, Gunn AJ. Interpretive differences between patients and radiologists regarding the diagnostic confidence associated with commonly used phrases in the radiology report. Am J Roentgenol. 2018 Jan; 210(1): 123-126. doi:10.2214/AJR.17.18448.
(5) Kim YW, Mansfield LT. Fool me twice: delayed diagnoses in radiology with emphasis on perpetuated errors. American Journal of Roentgenology. 2014; 202: 465-470. doi:10.2214/AJR.13.11493.
(6) Legriel S, Schraub O, Azoulay E, Hantson P, Magalhaes E, Coquet I, et al. Determinants of recovery from severe posterior reversible encephalopathy syndrome. PLoS ONE. 2012; 7(9): e44534. doi:10.1371/journal.pone.0044534
Teaching the Toggle: Peer Review as a Metacognitive Educational Tool
R. Grosso 1
1University Hospitals Cleveland Medical Center, Cleveland, OH
Emergency Physicians use extensive Type 1 thinking, or pattern recognition, in their daily practice. However, they need to be nimble enough to quickly apply the slower Type 2 to more challenging cases that do not fit the mold of the previous patterns. These metacognitive systems are rarely taught in formal medical education outside of the rare lecture or two, yet often are the key to understanding diagnostic errors that occur in cases discussed in the traditional Peer Review process. However, traditional Peer Review is typically organized in a top-down model where senior physicians review cases for provider opportunities for improvement, leading to a feeling of verdicts being handed down rather than a learning opportunity for the provider. Better incorporating discussions of metacognition into Peer Review can alleviate this judgmental culture and enhance trainee and faculty’s ability to recognize when they should toggle from Type 1 to Type 2 thinking in future cases. This oral presentation will describe a novel metacognitive approach to Peer Review with a focus on cognitive errors, both self-identified by providers and those identified by the committee discussion, as a way to shift culture from blame to one of improving the care of the next patient. This shift requires acknowledgement and discussion of the cognitive approach to that case. Through open discussions that focus on the moments where errors made in during Type 1, or heuristic, thinking effected a patient’s outcome, this approach to Peer Review identifies and refines the “toggle”, or the moments when we must switch to slower, Type 2 thinking, to avoid errors in future cases. Because we believe that teaching the “toggle” to trainees is an important part of successful lifelong learning, this model of Peer Review prioritizes discussions about cases in the presence of trainees, instead of behind closed doors. Metacognition is typically taught to medical trainees via lecture and the subject matter can often seem distant and abstract. In reality, metacognition plays a huge role in the bedside care of every patient. This presentation will demonstrate how linking metacognition to an emotionally and intellectually powerful outcome, as is often true of cases that make it to Peer Review, providers can be taught to apply the “toggle” in real time during the care of the next patient. This approach can help to bring metacognition out of the abstract world of thought and into application at the bedside.

The Tale of Two Cousins
C. Hemmelgarn 1, M. Lenz
1MedStar Institute Quality and Safety, Littleton, CO
The aim of this Case Study is to demonstrate the evolution of sepsis care at the same organization experienced by two cousins, separated by ten years. One survived and is thriving…the other did not. Alyssa was a nine-year-old healthy female diagnosed with Acute Lymphoblastic Leukemia (ALL), on February 26, 2007, and died ten days later. During the admission process, a resident documents in the medical record she was anxious; however, this was never discussed with the parents to confirm if Alyssa suffered from anxiety. On March 7th, in the nurses’ notes, the nurse documents that this is the best day Alyssa has had since her admission. However, as the day progresses Alyssa is starting to decline. She continues to say how her belly hurts, does not want to be touched and is visibly uncomfortable. Alyssa is seen by a resident who prescribes Ativan because she believes she is anxious. As the hours past Alyssa’s vital signs are changing. Her pulse is escalating, her blood pressure is dropping, and she now requires oxygen. This is documented in the medical record. I continue to tell the healthcare providers that something is wrong, something just is not right, but my words nor palpable concern resonates with the care team. Once again, she receives more Ativan. This pattern continues for over twelve hours until the morning and a new care team arrives. At this point, Alyssa was cognitively not present and when her fathered touched her foot it was ice cold. A rapid response team was called, and she was rushed to the PICU.
Alyssa was a classic case of failure to rescue and was septic. The care team was anchored in their diagnosis that she was anxious and could not see that she was failing.
After Alyssa died, I became involved in improvement projects in the organization. While there was a Rapid Response Team it could not be activated by patients and families. I was part of getting this changed so patients and families could activate the RRT. We created educational materials for patients and families and did teaching for the staff. I was invited to be part of sepsis committee. Over the years we have focused on creating resources to support teams in doing the right things around sepsis. We have done mandatory trainings on recognizing sepsis, created order sets, continue to educate parents and loved ones on looking for signs of sepsis, and review sepsis cases to discover future improvement areas.
Ten years later, my niece was admitted to the same hospital after being ill for a couple of days. The care team could not figure out what was going on. She had a consult from Rheumatology and Infectious disease, but no diagnosis was determined. On her second day in the hospital my sister-in-law called me in the early morning hours saying she was worried about my niece. She did not seem to be herself; she had been put on oxygen, and cognitively was coming in and out. I told her to go to the care team and ask them to assess.
Time is Tissue: Chronic Limb-Threatening Ischemia
D. Amin 1, M. Couture1
1Cook County Stroger Hospital, Chicago, IL
Learning Objective: Describe common presentation of patients with critical limb ischemia; Discuss causes of diagnostic errors in evaluation of critical limb ischemia
Case: 55 y/o male with history of hypertension, polysubstance abuse, and peripheral arterial disease presented to the ED with chronic right lower extremity calf and foot pain worsening over the past one month, but present for years. Vitals 192/96 HR 94 RR 20 Temp 36.7 the patient was diagnosed with plantar fasciitis after initial assessment and exam, with tenderness of the plantar aspect of the foot. When reassessed next team there were non-palpable or dopplerable distal pulses in the affected limb. Further history illustrated claudication symptoms for years, which now progressed to pain at rest, worse with leg elevation and improved with dangling of the affected limb off his bed at night. CT angiography of legs showed extensive disease burden from thrombosed infrarenal abdominal aortic aneurysm to bilateral popliteal arteries. Diagnosed with chronic limb-threatening ischemia (CLTI) and started on heparin drip, aspirin, statin, and underwent urgent revascularization with vascular surgery.
Discussion: Chronic limb ischemia is characterized by reproducible, intermittent claudication with exercise without temporal components. Symptoms progressing to pain at rest signify progression to limb threatening ischemia. Causes for delay in diagnosis include unfamiliarity with clinical presentation and delayed imaging. Additionally, inadequate risk factor analysis, history, or physical examination and CLTI mimics also contributes to delays in diagnosis. Accurate, prompt diagnosis of CLTI is difficult, but crucial in the ED setting. Providers must maintain a high index of suspicion in patients with risk factors and history of PAD and perform a complete, in-depth history and physical. Imaging should be obtained in a timely fashion to facilitate prompt diagnosis and expedite treatment as the one-year mortality after onset of CLTI is more than 25%.
Toxic Uncertainty: A Challenging Case of Carbon Monoxide Poisoning
D. Scudder 1, L. Pepin2, M. Patel3, S. Ruchman1, C. Dietsche3
1University of Colorado School of Medicine, Departments of Internal Medicine and Pediatrics, Aurora, CO
2Rocky Mountain Poison & Drug Safety, Denver, CO
3University of Colorado, Department of Internal Medicine, Division of Hospital Medicine, Aurora, CO
Objectives: 1) Recognize the importance of obtaining collateral history when determining the cause of encephalopathy. 2) Recall the presentation and evaluation of carbon monoxide toxicity.
Case: A 52-year-old woman with unknown medical history was found unresponsive in a heated trailer next to a deceased man. On arrival, she was febrile, tachycardic, and tachypneic. Labs showed elevated leukocytes, creatinine, troponin, and creatine kinase. Urine drug screen, electrocardiogram, lumbar puncture, electroencephalogram and computed tomography (CT) brain were negative for acute findings. CT chest showed a right lower lobe consolidation. Carboxyhemoglobin (COHb) sent in the emergency department was elevated at 13%. The patient was admitted and placed on oxygen therapy by non-rebreather mask. Transfer for hyperbaric oxygen was declined. MRI brain showed multiple acute watershed infarcts. The patient was diagnosed with carbon monoxide (CO) poisoning complicated by strokes, cardiomyopathy, rhabdomyolysis, and aspiration pneumonia. Autopsy of her partner showed elevated COHb. Ultimately, the patient’s mental status returned to baseline, and she was discharged home.
Discussion: Determining the cause of encephalopathy requires high-quality collateral. History from emergency responders raised suspicion of CO poisoning, but because the initial COHb level seemed insufficiently elevated to explain the patient’s encephalopathy, we developed a broad differential diagnosis. Symptoms of CO poisoning may appear disproportionate to COHb concentration due to variability in COHb half-life. Co-oximetry results in isolation often do not predict clinical course reliably. Ultimately, we excluded common causes of encephalopathy, and an autopsy revealed elevated COHb in the deceased partner, supporting the diagnosis. CO poisoning underlies several thousand hospitalizations annually for encephalopathy with multi-organ complications. In the setting of diagnostic uncertainty, identification of risk factors raises suspicion for CO poisoning as an otherwise uncommon etiology of encephalopathy.
Use of an Oncology Fast Track E-Consult to Improve Diagnosis of Suspected Cancers in the ED
G. Maloney 1
1US Department of Veterans Affairs, Bay Village, OH
Problem Statement: During evaluation in the emergency department, incidental findings that are concerning for possible malignancy are a common occurrence. In the absence of coordinated post-ED care, these patients are at risk for a delay in diagnosis. To improve follow-up on these patients, a specific e-consult was created in conjunction with the oncology service.
Intervention: A “Concern for cancer” fast track e-consult was created in the EHR. When a finding concerning for malignancy is discovered, then an e-consult is placed with relevant clinical information and contact information for the patient. The consult is followed up the next business day by the designated oncologist. They will arrange the initial necessary testing and specialty appointments after reviewing the chart. The referring provider is automatically tagged on the resulting recommendations and follow-up visits. Specific cancers that have a pathway already developed (such as breast mass) or are followed by a non-oncology service (such as urologic or gynecologic cancers) were not included in this intervention.
Findings to Date: The program was initiated in May 2018 and in the first 12 months a total of 103 consults were placed from the ED, with 88 patients successfully completing the recommended follow-up care. 7 patients were unable to be contacted and 8 were contacted but did not receive an evaluation; 6 were visiting from out of state and received their care primarily at another VA, and two refused any further workup. Of the 7 who were unable to be contacted, 3 ultimately returned to the VA ED within 6 months of initial appointment and were subsequently followed up at that point.
Lessons Learned: The program has proved highly successful in ensuring follow-up with veterans in our catchment area. Patients traditionally at risk for care coordination failures, such as the homeless and those with serious mental health or substance abuse issues, accounted for most of the lost to follow-up cases and need more intensive efforts outreach efforts. Development of better coordination with other VA medical centers for follow-up of travelling patients is also needed.
Use of Virtual Reality-based Cases to Teach and Assess Reasoning Skills in the Medical Curriculum
D. Webster 1, K. Bishop1, S. Williams1, S. Nunez1
1Texas Tech University Health Sciences Center-Lubbock, Lubbock, TX
Purpose/Problem: Clinical reasoning is defined as the application of hypothetico-deductive reasoning to a clinical scenario, combined with pattern recognition and algorithm-based decision-making to reach a reasonable conclusion about patient diagnosis, and the development of an appropriate diagnostic workup or treatment plan. Case-based presentations have been used extensively to provide instruction in the development of clinical reasoning skills using a variety of formats, including straightforward, paper-based cases to more complex computer-based formats. In this project, we describe the application of a virtual-reality (VR)-based format to provide an interactive learning experience that engages learners and provides both formative and summative assessment of clinical reasoning skills in learners at various stages within the undergraduate curriculum.
Program: We used an online learning environment created using Unity gaming software that immerses learners in a clinical encounter where they collect information (history, physical exam, diagnostic tests) and develop a differential diagnosis for each case. The program incorporates an array of statistical support that rewards students for making correct decisions and provides feedback on correct and incorrect decisions. The program can be run in both learning mode (where expert support is provided continuously) and assessment mode (where students must make these decisions on their own) and can be supplemented with tutorial material, images and test results to enhance the learning experience.
Outcomes: This VR platform has been used in our educational program in two ways, first as a teaching tool for students in the pre-clerkship curriculum in coursework focused on organ system pathophysiology and clinical decision-making, and as a supplement to standardized patient-based Objective Structured Clinical Examinations to enhance summative assessments of clinical skills in clerkships. Students in the pre-clerkship curriculum engage more deeply with the cases presented using this platform when compared to more classic paper or computer-based cases. Clerkship students can be assessed directly on clinical decision-making using these cases in a system that is highly reproducible and easily scalable.
Discussion and Significance: VR-based cases, such as those presented here, provide a forum for engaging learners in clinical decision-making in a format that is cost-effective, enjoyable and adaptable for both novice and advanced learners.
When it’s Not Myositis: A Rare Case of Acquired Hemophilia A Secondary to Rheumatoid Arthritis
R. Lomanto Silva 1, K. Miller1, J. Peugh1
1University of Pittsburgh Medical Center, Pittsburgh, PA
Learning Objectives: Acquired hemophilia (AH) is a severe bleeding diathesis caused by autoantibodies to coagulation factors, most commonly factor VIII. 4-8% of cases are associated with rheumatoid arthritis (RA). The Zürich Hemophilia Forum recently highlighted how effective care for AH is constrained by a challenging diagnostic process and low awareness of AH outside specialist settings. We underscore a case of AH secondary to RA that was initially misdiagnosed as RA-associated vasculitis.
Case Information: 65-year-old male with seropositive RA presented with acute spontaneous right lower extremity swelling and extensive thigh ecchymosis. Labs revealed hemoglobin (Hgb) 6.6 g/dL (baseline 15 g/dL). Leg MRI showed edematous right vastus lateralis and centralis concerning for myonecrosis. Upon transfer to our hospital, patient was hemodynamically unstable with down-trending Hgb despite transfusions. Investigation revealed undetectable FVIII level, high anti-FVIII titer, and prolonged PTT that did not correct on mixing study. Our team discussed the MRI findings with radiology and the consensus was that the imaging actually represented a large hematoma in the setting of AH and not muscular destruction from vasculitis. The patient was promptly started on AH treatment with a great outcome.
Discussion: Our patient had multiple risk factors for extraarticular manifestations of RA as a male with active untreated RA and history of smoking. His clinical presentation with multiple ecchymoses and classical soft tissue hematomas, acute anemia, prolonged PTT, normal PT, normal platelet count, and a positive mixing study, undetectable FVIII levels, and elevated anti-FVIII titers was diagnostic for AH and therefore should raise concern for a misdiagnosis upon MRI read of myonecrosis. AH can pose a diagnostic challenge, however, in a patient without a known bleeding disorder with an isolated remarkably elevated PTT, providers should have a high clinical suspicion for an acquired factor deficiency as early treatment is imperative to improve outcomes.
Oral Abstracts 3
Tuesday, October 18
10:15 AM – 11:45 AM
Frequency and Duration of Diagnostic Delays for Q Fever
A. Miller 1, J. Cavanaugh2, P. Polgreen1, S. Koeneman2, J. Hodges1, A. Arakkal2
1University of Iowa, College of Medicine, Iowa City, IA
2University of Iowa, College of Public Health, Iowa City, IA
Background: Q fever is a disease caused by the bacterium Coxiella burnetii, with both acute and chronic manifestations. Infection is primarily zoonotic in origin and typically caused by exposure to livestock (e.g., cattle, sheep, goats). Q fever can be successfully treated if identified early, although untreated and chronic disease can result in pneumonia, endocarditis or death. Q fever is considered to be a challenging diagnosis due to varied and non-specific symptoms along with low disease incidence. Moreover, because Q fever is relatively rare, the frequency of diagnostic delays is not well understood and difficult to observe at a single institution or even across a network of institutions.
Methods: We identified cases of Q Fever from 2001 through 2017 using a large population of administrative claims data (IBM MarketScan). We identified the index diagnosis of Q Fever and validated cases using treatment with doxycycline. We then identified symptomatic visits in the year prior to diagnosis by considering symptoms (e.g., fever, fatigue, headache) and symptomatically-similar diseases (e.g., pneumonia). We applied a simulation-based approach that we previously developed to estimate the frequency and duration of diagnostic delays. Finally, we evaluated trends in healthcare utilization after diagnosis between patients who experienced a diagnostic delay and those who did not.
Results: We identified 532 cases of Q Fever meeting inclusion criteria. An increase in symptomatic visits occurred up to 105 days prior to diagnosis. We estimated that 49.0% (95% CI: 42.3-56.2) of patients experienced a diagnostic delay. Among patients who experienced a delay, the mean duration of delay was 37.5 days (CI: 26.7 - 50.7) and patients experienced an average of 2.6 healthcare visits (CI: 2.3-3.1) representing a diagnostic opportunity. The majority of diagnostic opportunities occurred in outpatient settings. Patients who experienced a delayed diagnosis tended to incur greater healthcare utilization in the 90 days following diagnosis. Compared to patients who were not delayed, patients with a diagnostic delay had an average of 3.1 (CI: 1.4 – 4.9) additional healthcare visits following diagnosis.
Conclusions: We found that around 50% of patients with Q Fever experience a diagnostic delay and that delays typically last around a month or longer. Diagnostic delays are also associated with a greater than expected level of healthcare utilization in the 90 days following diagnosis and treatment. These findings help validate the challenges previously described in diagnosing Q Fever. Moreover, our approach demonstrates a method for surveillance of diagnostic delays for rare diseases.
Heads Will Roll: Overutilization of MRI in Diagnosis of Posterior Circulation Stroke
L. Officer 1, S. Noor1, L. Sweet1, C. Cavacece1
1Brooke Army Medical Center, San Antonio, TX
Background: Vertigo is a common presenting complaint in the emergency department, and it presents a unique challenge to the clinician. The differential diagnosis for vertigo is broad - spanning benign etiologies as well as neurologic emergencies. The most feared neurologic emergency is a posterior circulation stroke (PCS). Unfortunately, more than 50% of posterior strokes lack associated symptoms and simply present with isolated vertigo and nausea. This diagnostic challenge is thought to create overreliance on advanced neuroimaging, namely the magnetic resonance imaging (MRI) of the brain. There is strong evidence that rapid bedside exams, including the Dix-Hallpike and HINTS exams, are more sensitive than MRI in the acute phase, but are often more time-consuming. We postulate that the high utilization of expedited MRI and inpatient admissions are of relatively low yield with high resource utilization – without leading to improvement in clinical outcomes.
Methods: This study is a retrospective review of inpatient admissions of patients with isolated vertigo who were admitted to the internal medicine service over a 1-year period from June 2020 to June 2021 for evaluation of PCS at a level one military trauma hospital. All patients meeting criteria for PCS evaluation were reviewed for a variety of factors including physical exam findings, HINTS exam, and neurology consultation. All patients obtained an MRI brain in evaluation of PCS.
Results: Of 1200 patients admitted for PCS during the time frame, only 128 patients met inclusion criteria. Out of all patients, less than 2% of patients had an acute ischemic stroke on MRI. Unexpectedly, all patients with acute stroke found on MRI did not obtain a computed tomography (CT) of head or CT angiogram upon admission, which are standard of care in PCS evaluation. In addition, 70% of admissions did not perform or report Dix-Hallpike, HINTS exam, or orthostatic vital signs, which are clinically indicated. In total, the MRI changed management in less than 3% of cases.
Conclusion: These findings reveal a significant deficiency in appropriate evaluation and diagnosis of PCS. Our results unexpectedly reveal that clinicians do not reliably perform standard of care initial neuroimaging when suspecting PCS. In addition, despite higher diagnostic utility, appropriate bedside testing with HINTS exam, Dix-Hallpike, and orthostatic vital signs are not routinely performed. Instead, clinicians rely on advanced neuroimaging with the MRI, despite its lower diagnostic utility and increased cost. This study reveals a clear and cost-effective opportunity to improve physician competency in diagnosis of posterior circulation strokes and ultimately save lives.
Identifying Info. Factors for Diagnostic Error Involving Emergency Medicine Transitions of Care
R. Matin 1, R. Murphy1, B. King2, H. Singh3, A. Mehta4, A. Franklin5
1School of Biomedical Informatics, University of Texas Health Science, Houston, TX
2University of Maryland School of Medicine, Baltimore, MD
3Baylor College of Medicine and Houston VA, Houston. TX
4McGovern Medical School, University of Texas Health Science Houston, Houston, TX
5UTHealth, School of Biomedical Informatics, Houston, TX
Background: Emergency department (ED) sign-outs are essential to maintain care continuity. They usually involve short interactions, where pertinent information and responsibility for patient care are transferred to another physician assuming care. However, information features in these exchanges may contribute to cognitive vulnerabilities on the receiving end, leading to erroneous decision-making and incorrect diagnoses. Information features that increase the risk of diagnostic error during sign-outs are not well described.
Methods: We conducted a within-subjects experiment to assess how four variables influenced clinician diagnostic decision-making. These included: 1) how evolved the diagnostic process was at sign-out (middle or late stage), 2) explicitness of the information included in the sign-out, which reflected how unpacked the information was (explicit or implicit), 3) site, and 4) clinician role. The study involved randomized assignment to emergency medicine clinician participants (N= 69) across two academic ED sites; one that used sign-out protocols in clinical practice and one that did not. The experiment was administered using Qualtrics and involved patient case vignettes of control cases and stimuli cases containing the test conditions. The cases were presented in the narrative format of sign-out communications; presentation, history, exam, test results. Participants were required to provide a primary working diagnosis, differential and indicate their confidence in their diagnosis, for each case.
Results: The results indicated that ED site (χ2 =0.491, df=1 p=0.48) and clinician role (χ2 =0.024, df=2 p=0.99) did not affect diagnostic accuracy. Diagnostic accuracy was significantly influenced by the stage in the diagnostic process of stimuli cases (χ2 =19.945, df=1 p<0.01). Middle stage cases had lower diagnostic accuracy (33%) and involved lower physician confidence in diagnosis (48.9%) compared to late-stage cases (t=5.404, df=273, p<0.01) for both diagnostic accuracy (60%) and confidence in diagnosis (64.1%). However, the variable of explicitness of sign-out information didn’t significantly influence either clinicians’ diagnostic accuracy (χ2 =0.364, df=1 p=0.55) or their confidence in the diagnosis (t=0.514, df=273, p=0.61).
Conclusion: The explicitness of sign-out information didn’t affect either diagnostic accuracy or confidence clinicians had in their diagnosis. However, the stage of the case was highly influential and sign-out information for cases earlier in the diagnostic process was associated with lower diagnostic accuracy and confidence. This suggests additional support during sign-out for the oncoming ED team or possible enhancements to handoff protocols may be required for cases that are earlier in the diagnostic process.
Learning from Correct Diagnoses: A Safety-II Approach
R. Roos 1, C. van Nieuwkoop1, M. van Aken1, G. Kamps2, V. Valk1, L. Zwaan3, M. Maranus4, I. Meynaar1
1Haga Teaching Hospital, Den Haga, Netherlands
2Intergo International Centre for Safety, Ergonomics & Human Factors, Amersfoort, Netherlands
3Erasmus University, Rotterdam, Netherlands
4Erasmus Medical Centre, Rotterdam, Netherlands
Diagnostic errors reflect an important patient safety problem as they occur frequently and can have severe consequences. Diagnostic errors have mainly been addressed using a Safety-I approach, i.e., learning from errors and near misses. Recently, an alternative approach called Safety-II has been proposed, which focuses on learning from what goes well. In this project, we used the Safety-II approach to improve the diagnostic process by learning from best-practices in the emergency department (ED). The ED is a complex work environment, and therefore reliant on the resilience of clinicians, which results in substantial practice variation in the diagnostic process. To identify best-practices, we conducted three observation cycles (10-15 patients each) presenting to the ED with non-specific symptoms (e.g., fever, dyspnoea). The findings of each observation cycle were discussed during a co-creation session with a group of stakeholders (e.g., physicians, patient-representatives, risk managers), and the most promising interventions were identified. The effect of the interventions was observed and improved during the subsequent observation cycles. Several situations in the diagnostic process showed substantial practice variation during the observations. Examples from the completed observation cycles are: 1. Clinical information that was obtained and recorded in the electronic health record (EHR) on referred patients before their arrival at the ED, varied highly. The diagnostic process started particularly smooth if information such as the main reason for ED-visit, relevant medical history and the working diagnosis, was available to the physician upon arrival of the patient. During the co-creation session, the stakeholders identified seven important pieces of information that could facilitate the diagnostic process. The ‘Successful 7’ list was developed and introduced in the diagnostic process (and facilitated in the EHR). 2.Observations showed that when the required laboratory tests were specified before the patient arrived at the ED, a diagnosis was made earlier in the process (by avoiding ordering of additional tests, requiring taking of extra blood samples). Based on this observation, documenting the required laboratory tests in the EHR upon arrival of the patient has been adopted in the operating procedures. The Safety-II approach is effective to improve the diagnostic process in a complex and adaptive environment as the ED. Besides the examples above, several other improvements in the diagnostic process were made based on observed best-practices. Furthermore, the participating clinicians and stakeholders are now familiar with the Safety-II approach and can better identify best-practices, which contributes to an improved learning environment.
Recognizing Excellence in Diagnosis - Leapfrog’s New Project REDx
M. Graber 1*, J. Tilly2*, M. Danforth2, H. Singh3, M. Austin4
(*Presenting Author)
1Society to Improve Diagnosis in Medicine Alpharetta, GA
2The Leapfrog Group, Washington, D.C.
3Baylor College of Medicine and Houston VA, Houston, TX
4Johns Hopkins School of Medicine, Baltimore, MD
Statement of Problem: Reducing the harm associated with diagnostic error is an urgent national imperative. Although a few pioneering healthcare organizations (HCO’s) have started to address the problem, most remain on the sidelines, with little clear incentive to engage in efforts to improve diagnostic performance. Hospitals have specifically cited a lack of measures and clear goals for improvement as a key barrier to taking specific actions to address the problem.
Description of the Program: To provide a strong incentive to initiate performance improvement regarding diagnosis, the Leapfrog Group is developing a new, national benchmarking survey to promote diagnostic excellence in US hospitals and Emergency Departments. The survey will comprise a new section of the existing Leapfrog Hospital Survey, already in use at over 2200 US hospitals, and will focus exclusively on the quality, safety, and efficiency of diagnosis. An environmental scan was performed to identify interventions proposed in the NAM report on Improving Diagnosis in Health Care in 2015, and in publications since that date. An expert advisory group helped prioritize the list of possible interventions, focusing on those that were evidence based, feasible, likely to improve care and reduce harm, and important to patients and payers.
Findings to Date: The advisory group identified a group of 29 recommended practices that will be included in pilot tests to be conducted in the next 18 months, with an expected roll out of the final survey in 2024. Interventions were classified in two major groups: those focusing on leadership and available resources, and a second group relating to diagnostic practice. Examples from each group will be presented, along with the requirement for compliance. Specific practices apply to leadership commitment and accountability, to improving the diagnostic process, and in regard to patient engagement.
Lessons Learned: The existing Leapfrog Hospital Survey has improved healthcare quality in a number of areas, and the incentive of comparative benchmarking will be a key motivator for improving diagnostic performance as well. The new survey addition, focused on diagnosis, will provide concrete recommendations and expectations that US hospitals and Emergency Departments can use to begin their own journeys towards diagnostic excellence.
Remote Expert Diagnosis is More Accurate than In-Person ED Diagnosis in Acute Vertigo (AVERT Trial)
D. Newman-Toker 1, A. Saber Tehrani1, Y. Zhu2, S. Badihian1, R. Rothman1, D. Zee1, N. Tevzadze1, V. Eslami1, S. Peterson1, D. Hanley1, K. Lane1, M. Hildreth1, A. Blitz3, J. Edlow4, D. Lin1, T. Chang1, N. Ostapkovich1, J. Gruber1, A. Kheradmand1, D. Gold1, W. Meurer5, M. Iacobelli1, Y. Wang1, J. Goldstein6, A. Batazzi1, J. Kattah7, Z. Wang2, J. Carey1, T. Economas1, K. Kerber5, N. McBee1, J. Jen8, R. Omron1
1Johns Hopkins University School of Medicine, Baltimore, MD
2Johns Hopkins Bloomberg School of Public Health, Baltimore, MD
3Case Western Reserve University School of Medicine, Cleveland, OH
4Beth Israel Deaconess Medical Center, Harvard Medical School, Boston, MA
5University of Michigan Medical School, Ann Arbor, MI
6Massachusetts General Hospital, Boston, MA
7University of Illinois College of Medicine at Peoria, Illinois Neurological Institute, Peoria, IL
8Icahn School of Medicine at Mount Sinai, New York, NY
Background: Acute vertigo/dizziness is common and often misdiagnosed. Specialists use eye movements to differentiate stroke from inner ear diseases. Remote diagnosis incorporating video-oculography (VOG) might facilitate greater diagnostic accuracy and offer a scalable diagnostic solution.
Methods: Phase II randomized diagnostic strategy trial (AVERT, NCT02483429) at six tertiary-care EDs (2/6/2018-3/9/2020). We prospectively screened adult ED patients with acute vertigo/dizziness. Research coordinators captured eye movements using an FDA-approved VOG recording device (ICS Impulse by Otometrics) and assessed neurologic rating scales. Patients with nystagmus or gait/limb ataxia were eligible, and those available for follow-up testing (and without contraindications) were randomized to receive either VOG-guided rapid triage (VRT) or standard ED care (without access to VOG results). VRT was real-time, algorithmic diagnostic decision support, supervised by fellow-level oto-neurologists. Diagnosis adjudication occurred in stages. Senior experts masked to allocation arm, pathway/ED diagnoses, and imaging rendered their diagnoses based on ED VOG and a brief clinical history from ED notes, simulating a pre-imaging tele-consult. A multi-disciplinary panel rendered gold-standard diagnoses using ED charts, structured history/exam (including VOG), one-week oto-neurology evaluation (with repeat VOG, MRI), and one-month follow-up (record review, phone call). The prespecified primary outcome was total diagnostic accuracy in six categories (posterior canal benign paroxysmal positional vertigo [pcBPPV], vestibular neuritis, other peripheral, central, non-neurovestibular [medical/psychiatric], unknown) compared across arms (VRT vs. standard care). The prespecified main secondary outcome was senior expert VOG diagnosis vs. final ED diagnosis (non-randomized comparison for all subjects) analyzed using diagnostic accuracy in schemas of varying granularity (3-/6-/12-category) and diagnostic sensitivity for common conditions.
Results: We randomized 130 subjects (52.3% female; 76.9% white, non-Hispanic; mean age 59.2±15 years); 21 with unknown final diagnoses despite adequate follow-up were excluded. VRT outperformed in-person ED diagnosis on the primary outcome, 6-category diagnostic accuracy (37.9% vs. 17.6%; n=109; relative risk for VRT correct diagnosis 2.1, p<0.001). Senior expert accuracy was even higher (Table). Central (brain) lesions (n=23) were erroneously called peripheral (inner ear) more often by ED than senior expert (13% vs. 0%, p=0.06).
Conclusion: Remote VOG evaluation by oto-neurologists in ED vertigo/dizziness presentations could substantially improve diagnostic accuracy, especially for common inner ear disorders.
Table. Diagnostic accuracy for acute dizziness (ED versus senior oto-neurology expert)
| Final Adjudicated Diagnosis after 1-Month Follow-up | ED Clinical Team Accuracy, % (95% CI) | Senior Expert Accuracy by VOG, % (95% CI) | ∆ Dx Accuracy, Relative Risk Dx Error with VOG | p-value (McNemar’s test) |
|---|---|---|---|---|
|
All Causes (n=109*)
|
||||
| 3-Category Schema † (n=109) | 22.9% (15-32) | 72.5% (63-81) ‡ | ↑216%, 0.32 | <0.001 |
| 6-Category Schema § (n=109) | 18.3% (12-27) | 63.3% (54-72) ‡ | ↑245%, 0.29 | <0.001 |
| 12-Category Schema £ (n=109) |
17.4% (11-26) |
61.5% (52-71) ‡ |
↑253%, 0.28 |
<0.001 |
|
Subset with Most Common Inner Ear & Brain Diseases (n=82)
|
||||
| BPPV (n=43) | 9.3% (3-22) | 69.8% (54-83) | ↑650%, 0.13 | <0.001 |
| Vestibular neuritis (n=25) | 20.0% (7-41) | 80.0% (59-93) | ↑300%, 0.25 | 0.001 |
| Cerebrovascular events (n=14) ¶ | 42.9% (18-71) ¶ | 57.1% (29-82) ¶ | ↑33%, 0.75 | 0.5 |
-
* Excludes 21 cases with an unknown final diagnosis despite follow-up (2% [n=3/130] lost to follow-up). † 3-Category: central [i.e., brain], peripheral [i.e., inner ear], or other/unknown. ‡ The majority of inaccurate senior expert diagnoses were “unknown” (n=29), and 3 had trivial discrepancies from a neuro-otological perspective (e.g., vestibular neuritis vs. labyrinthitis or pcBPPV vs. multi-canal BPPV with dominantly posterior canal involvement). Thus, senior expert diagnoses rendered were incorrect in just 9% (n=10/109), and none of these cases involved misclassification of a central vestibular disorder as peripheral. § 6-Category: pcBPPV, vestibular neuritis, other peripheral, central, non-neurovestibular, or unknown. £ 12-Category: pcBPPV, vestibular neuritis, horizontal canal BPPV, other BPPV, Menière’s disease, vestibular migraine, other peripheral, thiamine deficiency, cerebrovascular, other central, non-neurovestibular, or unknown. ¶ There were 9 ischemic strokes, 4 transient ischemic attacks, and 1 brain hemorrhage. The senior expert using VOG detected 8/14 cerebrovascular cases, deeming the other cases unknown and in need of further workup. By contrast, the ED team ultimately discharged two of the cerebrovascular cases as unknown “dizziness” (one after an observation stay under internal medicine). Furthermore, the brain hemorrhage was in a 47-year-old woman with an actively bleeding cavernous angioma abutting the 4th ventricle who was misdiagnosed 4 times over 9 days (2 ED visits, 1 physical therapy visit, 1 primary care visit) before a vestibular physical therapist recognized her to have central nystagmus and sent her back to a different ED, where she was seen and enrolled in the AVERT trial.
Best of the Best Oral Abstracts
Tuesday, October 18
1:00 PM – 2:30 PM
A Code that Means “Undiagnosed” to Shorten the Rare Disease Diagnostic Odyssey
H. Hernandez 1, L. Muli1
1KAL Research Initiatives, Katy, TX
Reaching a diagnosis for a rare disease can be particularly challenging as medical professionals cannot reasonably be expected to know signs and symptoms of several thousand diseases that they are unlikely to ever encounter. This results in a diagnostic “odyssey” that commonly lasts several years for these patients and sometimes a diagnosis is never reached. The rare and undiagnosed community understands what it means to be undiagnosed but there is not a consistent way to formally describe someone as such. Furthermore, if there were, it is unclear how this designation could be leveraged to effectively move resources across healthcare systems to help an individual achieve a diagnosis and access any associated care plan. To address this, we have recently launched the R69 Initiative which aims to develop consensus around how a code like the ICD-10 code R69, (meaning illness, unspecified), could be used for just such a purpose and then promote the implementation to key stakeholders and communities. This is a global initiative seeking diverse perspectives to develop usage guidelines in support of the underserved rare disease community. A series of roundtables and stakeholder listening sessions will continue throughout 2022 to discuss and refine the approach and anticipate challenges. Thus far we have shared the concept at 3 international events/platforms, held an inaugural roundtable discussion, and had numerous meetings with individual stakeholders to assess the relevance of this concept. We have identified a few potential barriers to implementation including that medical professionals may see using the code as detrimental to their career/reputation perceiving it as an acknowledgement that they do not have the answer for a patient. From the findings thus far, we anticipate several specific challenges and expect that additional perspectives will need to be considered to develop a robust strategy for implementation of an “undiagnosed” code, such as R69 which is poised for wide-spread use. We will present these challenges alongside our proposed strategies to address them and will continue to seek input from additional stakeholders.

Bayesian Network Analysis Identifies Patterns of Diagnostic Delay in Juvenile Idiopathic Arthritis
M. Ong 1, M. Natter2
1Harvard Medical School & Harvard Pilgrim Health Care Institute, Boston, MA
2Boston Children’s Hospital, Boston, MA
Background: Juvenile idiopathic arthritis (JIA) is a chronic childhood-onset rheumatic disorder with substantive morbidity when disease activity is inadequately controlled. Because symptoms of JIA are often non-specific, patients with JIA frequently experience prolonged diagnostic delay. We developed a Bayesian network approach to discern patterns of diagnostic delay in JIA using linked electronic health record (EHR) and registry data.
Methods: Study subjects included 290 children with JIA (<18 years old) who were enrolled in the Childhood Arthritis and Rheumatology Research Alliance (CARRA) Registry at a large tertiary care children’s hospital for whom linked EHR data were available. We used self-reported dates of symptom onset and JIA diagnosis captured in the registry to define diagnostic interval (i.e., interval from JIA symptom onset to diagnosis). Diagnoses recorded in the EHR during this interval were extracted and a Bayesian network was constructed to model the inter-relationships among these diagnoses and how they relate to a diagnostic delay of >=6 months.
Results: The median and mean interval from JIA symptom onset to diagnosis in our cohort were 3 and 8.3 months, respectively. The derived network (Fig) reveals a distinct cluster of diagnoses linked to a diagnostic delay of >=6 months, identifying two JIA subtypes most at risk of diagnostic delay (i.e., enthesitis-related arthritis, undifferentiated JIA). Additionally, the model captures well-established patterns of misdiagnoses occurring in JIA patients, as well as clustering of comorbidities consistent with the classification criteria for JIA subtypes, thus validating the approach. Importantly, the network identifies potentially novel and under-recognized diagnostic patterns, providing impetus for deeper investigation.
Conclusions: Application of network-based machine learning approach to longitudinal clinical datasets can facilitate investigation of patterns of potential misdiagnoses leading to prolonged diagnostic delay in JIA. While our study population was limited to patients seen at a tertiary care health system with a presumptively higher level of training in recognition of musculoskeletal diseases than most community providers, we were nonetheless able to detect a variety of patterns of diagnostic delay. Applying this approach to more typical community health care settings has the potential to yield additional insights to reduce delays in JIA diagnosis.

Communication of Diagnostic Uncertainty Across Teams and With Families at Admission
U. Nawab 1, A. Costello1, A. Mack1, J. Schaffer1, A. Kratchman1, M. Prieto1, I. Rasooly1, V. Fairchild1, K. O’Shea1, A. Colfer1
1Children’s Hospital of Philadelphia, Philadelphia, PA
Background: Diagnostic uncertainty (DU) is the subjective perception of an inability to provide an accurate explanation of a patient’s health problem. Recognition and communication of DU impacts multiple drivers of diagnostic excellence. We completed a baseline assessment of communication of DU between the Emergency Department (ED), admitting teams, and patients/families during admission to general pediatrics within our quaternary care children’s hospital.
Methods: Baseline assessment of communication of DU was completed between Nov 30, 2020, and Sept 30, 2021. Hospital medicine physician and research assistants completed 44 phone interviews of ED clinicians, inpatient hospital medicine physicians, and families shortly after general pediatric admission orders were placed. Clinicians were asked whether a working diagnosis had been established (and what it was), to identify other diagnoses being considered, and to rate the ED clinician’s communication of their degree of diagnostic uncertainty on a five-point scale ranging from (1, “not certain” to 5, “very certain”). Families were asked “What does the emergency department think is going on with your child (i.e., their diagnosis)?” “Are there any other diagnoses they are thinking about?” and “What did the team say the next steps would be?” Responses were recorded in Redcap. Demographic information and admission and discharge notes were abstracted from the electronic health record. A driver diagram of communication of DU was completed by a family consultant and clinicians from the ED, General Pediatrics, Patient Safety, and pediatric intensive care.
Results: ED clinicians identified diagnostic uncertainty (and alternate diagnoses) in 50% (22) of cases. There was discordance in the communication of uncertainty between ED and hospital medicine clinicians in 18% of cases. Family understanding of alternate diagnosis differed from the ED clinician’s understanding of uncertainty/alternate diagnoses in 79% of the 34 families interviewed. Multiple drivers of communication of DU were identified. First order drivers of DU communication included patient/family needs and preferences, patient preferred language and health literacy, clinician comfort with uncertainty, diagnostic team interactions and dynamics, the complexity of the diagnostic process, and time constraints/interruptions to work.
Conclusion: There are opportunities to improve recognition and communication of DU for patients admitted from the ED to general pediatrics. Next steps include educational sessions to introduce strategies for communicating DU coupled with the development and testing of tools to structure verbal and written communication about DU. Future work will also explore disparities in DU and DU communication.

Impact of Automated Patient Outcome Feedback on Emergency Medicine Resident Patient Follow-up
R. El-Kareh 1, F. Rudolf2, L. Oyama2
1University of California San Diego, La Jolla, CA
2University of California, San Diego Health, San Diego, CA
Purpose/Problem: Emergency medicine (EM) physicians desire, but often lack reliable feedback of patient outcomes following handoffs to other providers. This gap is a substantial barrier to calibrating their diagnostic decision-making and learning.
Description of Program, Assessment, or Study: To address this educational priority, we developed and evaluated the Post-Handoff Reports of Outcomes (PHAROS) system--an automated electronic health record (EHR)-based system to deliver provider-specific patient outcome feedback.
Program Description: PHAROS includes: 1) individualized lists of patients seen by residents and brief summaries of each case; 2) flags for important post-handoff events; and 3) links to charts to facilitate review. Starting June 2020, we coupled PHAROS with a resident educational session and individualized emails every two weeks outlining the number of patients, number of post-handoff events and instructions to access the PHAROS system.
Assessment: Primary outcome: From July 2017 through April 2022, we measured the proportion of resident handoffs that were followed by reaccessing the patients’ charts between 2 and 14 days post-handoff—a proxy for following up on the patient’s post-handoff outcomes. We performed an interrupted time series analysis on this outcome to determine if PHAROS was associated with a significant change in the level or slope over time. Our secondary outcome was the number of times PHAROS was viewed each month.
Outcomes: The 58 months of our primary outcome are shown in Figure 1. Our primary outcome had a significant increase in the slope over time (+0.13%/month, p=0.03) after the intervention and a non-significant change (-1.6%, p=0.07) at the time of the intervention. The median number of views of PHAROS per month was 33.2 (IQR 23.75-38.75).
Discussion: The PHAROS system was associated with a significant increase in the rate of post-handoff chart reaccess among EM residents over time. Once established, this system required very little investment in person-time, which enabled consistent use despite significant clinician time demands during the COVID-19 pandemic.
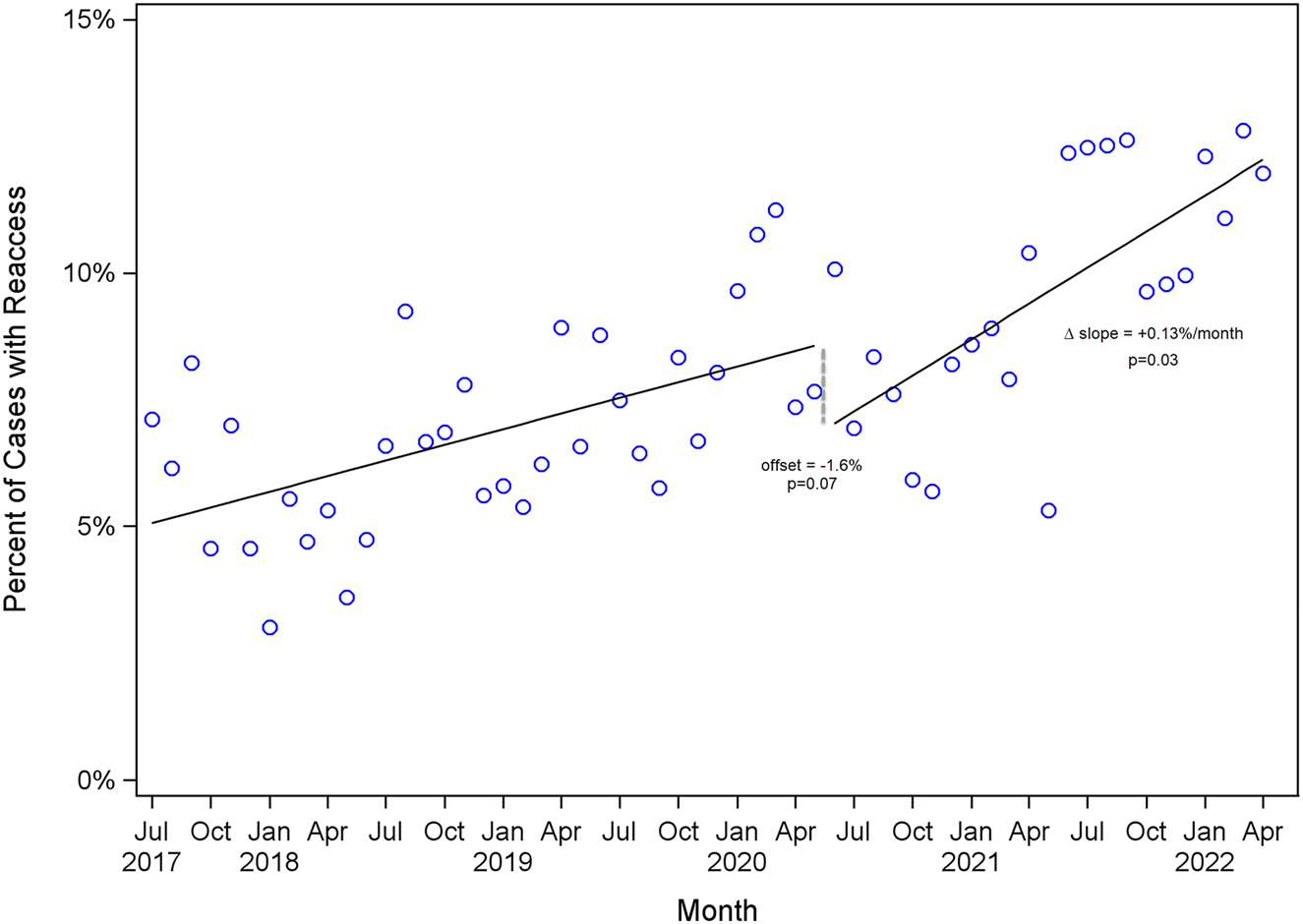
Significance of Findings: The PHAROS project demonstrated the feasibility of harnessing the capabilities of a modern EHR to create an automated system to support EM trainee feedback of patient outcomes—a key component of diagnostic calibration and learning.
Implementation, Validation, and Mortality Association of 2 Cancer Diagnosis Digital Quality Measures
A. Zimolzak 1, S. Korukonda2, G. Abel3, P. Kapadia1, H. Singh4, R. Murugaesh Rekha2, U. Mir1, A. Offner5, L. Mounce3, D. Murphy1, G. Lyratzopoulos6, D. Upadhyay2, U. Mushtaq1
1Baylor College of Medicine, Houston, TX
2Geisinger, Danville, PA
3University of Exeter, Exeter, England
4Baylor College of Medicine and Houston VA, Houston, TX
5Houston VA and Baylor College of Medicine, Houston, TX
6University College London, London, England
Background: In the US, 1/3 of patients with cancer experience a missed or delayed diagnosis, and cancer is a leading cause of malpractice claims. However, missed opportunities in diagnosis (MODs) that drive these outcomes are not easily detected in existing data. The Centers for Medicare & Medicaid Services recently emphasized the need for digital quality measures (dQMs). Therefore, we developed, implemented, and validated two outcome dQMs for cancer diagnosis at two US health systems. dQMs can serve as proxy measures of breakdowns in cancer diagnosis and inform interventions.
Methods: We adapted emergency presentation definition used in England, and a late-stage (III/IV) definition, while using the Safer Dx Trigger Tools Framework for developing electronic safety algorithms. We consulted a panel of physicians, quality professionals, system leaders, and patients, to establish dQM criteria. We developed two dQMs (cancer emergency presentation and late-stage presentation) based on electronic health record data. Emergency presentation (EP) was defined as ""emergency department visit or unplanned inpatient admission, followed by first cancer diagnosis within 30 days."" We applied the dQMs to patients with lung and colorectal cancer (CRC) at Veterans Affairs (VA) and Geisinger during 2016–2020. Two clinicians reviewed a sample of EP and late-stage records from 2019 at both sites using standard forms to assess dQM accuracy (e.g., whether the emergency visit was truly for cancer symptoms) and for MODs (e.g., whether a past visit for hemoptysis was likely cancer-related). We analyzed survival stratified by dQM.
Results: At VA, EPs were seen in 3,401/14,674 cases (23%) of CRC and 8,039/37,691 (21%) lung cancers. Late-stage presentations were seen in 36% of CRC and 46% of lung cancer. Chart review showed dQM accuracy ≥70% across measures and MODs in 50–81% of cases. EP of CRC had 1-year all-cause mortality of 31.3%, significantly higher than non-EP, with 12.9%. Likewise, EP of lung cancer had 56.1% mortality, versus non-EP with 32.1%.
Conclusions: We used large data warehouses to implement and validate 2 outcome dQMs of cancer diagnosis in 2 US health care systems. Emergency and late-stage presentations are common, can be detected at large scale, and are associated with MODs and mortality, representing a high signal for opportunities for improvement. Health systems can use diagnostic dQMs to identify high- or low-performing sites to learn from them, or to track performance over time. To our knowledge, these are the first two dQMs to focus specifically on diagnostic quality.
Using Medical Record Reviews to Verify Patient-Reported Diagnostic Concerns: What are We Missing?
T. Giardina 1, S. Korukonda2, T. Scott3, V. Vaghani3, H. Singh1, C. Spitzmueller4, D. Upadhyay2
1Baylor College of Medicine and Houston VA, Houston, TX
2Geisinger, Danville, PA
3Baylor College of Medicine, Houston, TX
4University of Houston, Houston, TX
Background: Providing patients electronic access to their doctors’ notes presents a unique opportunity for improving diagnostic safety. We previously developed the Safer Dx Patient instrument to allow patients to evaluate recent visits for diagnostic concerns while reviewing their online visit notes. Building on that work, we examined the use of medical record review to further explore patient-reported diagnostic concerns.
Methods: We conducted secondary data analysis on 486 patients who completed the Safer Dx Patient instrument, 51 of which reported a diagnostic concern. The cohort includes patients aged 18-85 who actively used patient portals and were identified using an electronic trigger algorithm based on unexpected visit patterns – a primary care visit followed by an unplanned return visit within 14 days. Two clinician-chart reviewers conducted detailed medical record reviews of all 486 patients using the Revised Safer Dx Instrument to evaluate for missed opportunities in diagnosis (MOD) at the initial visit. We conducted an inductive qualitative content analysis using the chart reviewer notes and open-ended responses on the Safer Dx Patient.
Results: In 486 cases, clinician-chart reviewers identified 20 (4.1%) MODs but only in 8 (15.7%) of the 51 patient-reported diagnostic concerns. In the 435 cases without a patient-reported diagnostic concern, chart reviewers found an additional 12 (2.8%) MOD cases. Upon analysis of chart reviewer notes and the patient comments, we found inconsistencies between the patient reports and medical records (e.g., patient indicated that the doctor offered ‘anxiety meds’ for troubled breathing while medical notes reported screening was normal and no mention of medication recommendation). Often, standard of care was met based on medical record review, but patients indicated there was a failure to address their symptoms and/or provide a diagnosis. Finally, we found several cases of normal evolution of a diagnosis (e.g., “thigh pain” at first visit that develops into shingles; sinus congestion at first visit and bronchitis on second visit) that patients reported as a diagnostic concern. For the 8 cases where patient and chart reviewer agreed, we found issues related to failure to refer, appropriate testing not ordered, and failure to consider all symptoms.
Conclusion: Patient-reported diagnostic concerns are not adequately captured in the medical record. Additionally, patients and clinicians also appear to have some differences in their mental models of what each considers as a diagnostic concern. Highlighting these differences in perspective can help inform development and use of robust methods for collecting data on potential missed/delayed diagnoses from patients.
© 2023 Walter de Gruyter GmbH, Berlin/Boston
Articles in the same Issue
- Frontmatter
- Editorials
- An equation for excellence in clinical reasoning
- Quantifying diagnostic excellence
- Review
- A scoping review of distributed cognition in acute care clinical decision-making
- Opinion Papers
- Context matters: toward a multilevel perspective on context in clinical reasoning and error
- Occam’s razor and Hickam’s dictum: a dermatologic perspective
- Original Articles
- Differences in clinical reasoning between female and male medical students
- Introducing second-year medical students to diagnostic reasoning concepts and skills via a virtual curriculum
- Bad things can happen: are medical students aware of patient centered care and safety?
- Impact of diagnostic checklists on the interpretation of normal and abnormal electrocardiograms
- Cerebrospinal fluid lactate as a predictive biomarker for tuberculous meningitis diagnosis
- Empowering quality data – the Gordian knot of bringing real innovation into healthcare system
- Collective intelligence improves probabilistic diagnostic assessments
- Why people fail to participate in annual skin cancer screening: creation of the perceptions of annual skin cancer screening scale (PASCSS)
- Instructions on appropriate fasting prior to phlebotomy; effects on patient awareness, preparation, and biochemical parameters
- Clinician factors associated with delayed diagnosis of appendicitis
- Real-world assessment of the clinical performance of COVID-VIRO ALL IN rapid SARS-CoV-2 antigen test
- Lack of a prompt normalization of immunological parameters is associated with long-term care and poor prognosis in COVID-19 affected patients receiving convalescent plasma: a single center experience
- Letters to the Editor
- Uncontrolled confounding in COVID-19 epidemiology
- VAPES: a new mnemonic for considering paroxysmal disorders
- Congress Abstracts
- SIDM2022 15th Annual International Conference
Articles in the same Issue
- Frontmatter
- Editorials
- An equation for excellence in clinical reasoning
- Quantifying diagnostic excellence
- Review
- A scoping review of distributed cognition in acute care clinical decision-making
- Opinion Papers
- Context matters: toward a multilevel perspective on context in clinical reasoning and error
- Occam’s razor and Hickam’s dictum: a dermatologic perspective
- Original Articles
- Differences in clinical reasoning between female and male medical students
- Introducing second-year medical students to diagnostic reasoning concepts and skills via a virtual curriculum
- Bad things can happen: are medical students aware of patient centered care and safety?
- Impact of diagnostic checklists on the interpretation of normal and abnormal electrocardiograms
- Cerebrospinal fluid lactate as a predictive biomarker for tuberculous meningitis diagnosis
- Empowering quality data – the Gordian knot of bringing real innovation into healthcare system
- Collective intelligence improves probabilistic diagnostic assessments
- Why people fail to participate in annual skin cancer screening: creation of the perceptions of annual skin cancer screening scale (PASCSS)
- Instructions on appropriate fasting prior to phlebotomy; effects on patient awareness, preparation, and biochemical parameters
- Clinician factors associated with delayed diagnosis of appendicitis
- Real-world assessment of the clinical performance of COVID-VIRO ALL IN rapid SARS-CoV-2 antigen test
- Lack of a prompt normalization of immunological parameters is associated with long-term care and poor prognosis in COVID-19 affected patients receiving convalescent plasma: a single center experience
- Letters to the Editor
- Uncontrolled confounding in COVID-19 epidemiology
- VAPES: a new mnemonic for considering paroxysmal disorders
- Congress Abstracts
- SIDM2022 15th Annual International Conference

